Intersectoral Action on Health
Live in fragments no longer. Only connect….
—E.M. Forster, (1910)
The health of a nation is shaped by more than medical care, or by the choices that individuals make to maintain their health, such as quitting cigarette smoking or controlling diabetes. The major contributors to disease—risk factors under the control of individuals (e.g., obesity, tobacco use), exposure to a hazardous environment, or inadequate health care—are themselves influenced by circumstances that are nominally outside the health domain, such as education, income, and the infrastructure and environment that exist in workplaces, schools, neighborhoods, and communities. In this chapter, the committee discusses the implications of the social determinants of health for the actions of various stakeholders, with a focus on non-health policies that affect population health (see Box 4-1 for a few examples). Here, the committee reviews the frameworks and models that exist for the engagement of non-health actors in considering the health outcomes of their policies, and even, perhaps, in improving their positive contributions to achieving health objective.
The literature linking population health outcomes with these antecedents (i.e., the determinants of health) is robust and includes decades of work by Marmot, Wilkinson, and colleagues (Marmot et al., 1991, 1997; The Marmot Review, 2010), including the World Health Organization Commission on the Social Determinants of Health, Adler and the MacArthur Research Network on Health and socioeconomic status (SES), and many others.
The health significance of “non-health” factors is often overlooked. Education is a prime example. People with a college degree are one third less likely to smoke than those who have not completed high school. Miech et al.
BOX 4-1
Examples of Non-Health Policies with Health Effects
Federal agricultural subsidies are enacted with agricultural, economic, and trade objectives in mind, but their effects on health are significant. Similarly, transportation planning may have as a primary objective the optimal way to facilitate goods movement or to commute between home and work, but related issues must be considered, including local economic development that may be enhanced or impaired by public transportation, road design and other physical features (access to public transportation); community functioning (e.g., when a busy highway divides a neighborhood); and health, which may be positively or negatively impacted depending on the extent to which transportation planning considers whether to encourage and facilitate pedestrian and bicycle traffic.
(2009) reported that adults ages 40 to 64 with only a high school education are more than three times more likely to die from diabetes than those who have graduated from college. Educational attainment determines whether individuals can obtain good jobs and whether they acquire the knowledge, health literacy, and other tools needed to make informed choices about their health.
Income is another important factor. Certainly, low-income individuals are less likely to have health insurance, but income also affects health by enabling families to live in healthy neighborhoods and housing and to afford nutritious groceries, fitness clubs, copayments for doctor’s visits, and prescription medications. Income is a health determinant in all social classes, not just for the poor. Americans with incomes that were 201 to 400 percent of the poverty level had shorter lives and a greater likelihood of fair or poor health than were those with incomes more than 400 percent of the poverty level (Braveman and Egerter, 2008). Woolf and colleagues (2007) reported that 25 percent of all deaths in Virginia would have been averted if the entire state experienced the mortality rate of those living in the five most affluent counties and cities.
Place affects health—neighborhood and community environments exert their own health influences, independent of the risk factors associated with individuals and households. Research links social and economic features of neighborhoods “with mortality, general health status, disability, birth outcomes, chronic conditions, health behaviors and other risk factors for chronic disease, as well as with mental health, injuries, violence and other important health indicators” (Cubbin et al., 2008). People living in poor neighborhoods with inadequate housing, high levels of crime, high density of alcohol outlets, and a scarcity of fresh food retailers are more likely to
experience a range of health problems. These problems are related to obesity, physiologic consequences of chronic exposure to stress, living in an environment lacking in social capital, and other factors.
PATHWAYS BETWEEN HEALTH AND ITS DETERMINANTS
“Upstream” or distal determinants of health—conditions that influence the more proximal factors such as blood pressure and health care services—include individual, household, and area-based factors. Examples of individual factors include a person’s race or ethnicity, which cannot be changed, and modifiable factors such as behavioral choices and educational attainment.1Household-level health factors define a family’s income level, health insurance coverage, and housing conditions. Area-based or place-based conditions affect individuals and households throughout the neighborhood and community and are characteristics of a geographic area, such as a Census tract or block. Examples include ambient air pollution, crime rates, social cohesion, walkways and green space, the quality of local schools, health care facilities, access to healthful foods, the density of fast-food restaurants, marketing of tobacco and liquor, and access to affordable public transportation.
Individual, household, and environmental factors form a complex causal web that complicates observed associations between health outcomes and any one factor in isolation. For example, in the arena of environmental factors, substandard housing is a known associate of poor health. However conditions other than housing itself (e.g., pests, proximity to sources of pollution, unsafe streets, unhealthful occupations, lack of medical care) also explain occupants’ greater experience of asthma, mental illness, and malnutrition (e.g., examples of research on the links between housing and health can be found in Braveman et al., 2010; Britten, 1938; Dalla Valle, 1937; EPA, 2011; Erickson and Marks, 2011; Krieger and Higgins, 2002). Confounding relationships between interrelated causal factors make it important to determine the degree to which socioeconomic and contextual conditions are markers for other factors that play equally important causal roles (for an illustration of the multiple pathways linking education and health, see Braveman et al., 2011a). For example, the evidence linking income and health is extensive and goes back decades and even centuries, but questions about causality remain pervasive and further research is needed to disentangle the complexity of the pathways linking the two (see, for example, Chandra and Vogl, 2010; Muennig, 2008).
__________________________
1 There are also levels of modifiability, including the degree of difficulty, time requirements, and the importance of a given factor compared to others potentially implicated in causing the health outcome of concern.
THE ROLE OF POLICY AS A DETERMINANT OF HEALTH
Although many socioeconomic and environmental factors affect health, only some are under the personal control of individuals and families. People can make the effort to complete high school, pursue higher education, make informed choices to improve their health, and obtain a job that is good for health—a job that promotes wellness, limits exposure to occupational stress or injuries, offers health insurance benefits, and provides an income that makes health care, healthy behaviors, and healthy neighborhoods affordable. However, the success of these efforts depends in part on factors outside the control of individuals and families. The quality of schools, the strength of the job market, worksite safety, and the healthfulness of neighborhoods and communities are determined by decisions taken by policymakers outside the family and the health sector (Adler et al., 2007; Commission on Social Determinants of Health, 2008; Lovasi et al., 2009; Marmot and Bell, 2011; Marmot and Wilkinson, 1999; Marmot et al., 1997; The Marmot Review, 2010).
In corporate boardrooms, legislatures, and the executive branches of government, decisions that ultimately affect the public’s health emerge from policies that few view as health decisions. Initiatives to promote jobs, corporate growth, transportation infrastructure, and community development are deliberated by officials, executives, and other decision-makers who often are unaware of or overlook the connection to health. School boards, educational agencies, and ballot initiatives determine funding for local schools and set policies that affect children’s learning, educational attainment, physical activity, and diet. The ability of adults to find work, a stable income, and good health insurance benefits is shaped by legislation, labor policy, economic strategy, the tax code, and deals negotiated between managers and unions.
The healthfulness of neighborhoods and communities is shaped by the decisions of private developers, local officials, businesses, and voters. Federal tax policy, corporate competition, zoning regulations, advertising, and the local economy influence whether residents have access to supermarkets and parks or are exposed to air and water pollution, fast foods, liquor stores, and tobacco advertising. Land use decisions determine whether the built environment is conducive to physical activity, for example, whether builders add sidewalks, bicycle paths, and greenways (e.g., paths or trails for recreation, pedestrians, and bicycles) to roadway construction projects (American Planning Association, 2002; Cubbin et al., 2008). Decisions to forego economic development and community investment set the path for neighborhood deterioration and the emergence of urban decay, unhealthy housing, pollution, violent crime, and the departure of businesses, jobs, schoolteachers, and quality medical care—and their attendant health benefits—to more attractive neighborhoods (Kelly, 2004). Decisions about
public transit serve not only to limit exposure to automobile emissions, but also to help individuals reach jobs with health benefits, medical care, educational opportunities for themselves and their families, and nutritious groceries (Cubbin et al., 2008).
Specific policy examples of these connections between non-health policies and health effects are increasing. For example, in agricultural policy, evidence shows that corn subsidies may contribute to unhealthful American diets (see Alstona et al., 2008; Harvie and Wise, 2009; Wallinga, 2010), which in turn contribute to obesity, diabetes and cardiovascular disease. Other countries have shifted government agricultural subsidies to gradually modify industry practices and to support the cultivation and increase the affordability of more healthful crops, such as vegetables and fruits (Capewell and Lloyd-Jones, 2010). Urban planning provides another example. Freeways that divide neighborhoods to facilitate commuter traffic can harm health, quality of life, and community well-being (Wier et al., 2009). One group of researchers summarized the recent efforts directed at freeway “deconstruction” as reflective of urban and land use planning priorities that are “shifting away from designing cities to enhance mobility,” “toward promoting economic and environmental sustainability, livability, and social equity” (Cevero et al., 2009, pp. 31, 32).
In its information gathering, the committee learned about New York City’s FRESH program that represents a collaboration among the health and planning agencies and the local economic development corporation and provides incentives to bring grocery stores to areas that lack access to fresh fruits and vegetables (Bryon, 2010; IOM, 2010). In San Francisco, the Federal Reserve Bank has been exploring opportunities for cross-sectoral partnership between community development and health (see, for example, Federal Reserve Bank of San Francisco, 2010). Other examples of links between non-health policies and health outcomes have been building over decades of experience and research. These include a rich evidence base that has demonstrated that the poor health outcomes in adulthood that is associated with disadvantage in childhood can be effectively prevented by policy interventions as varied as home health visiting programs, early stimulation in child care programs, and preschool settings (i.e., Early Head Start and Head Start) (Adler and Stewart, 2010; Braveman et al., 2010; Evans and Kim, 2010; Kawachi et al., 2010).
In 2009, the National Center for Healthy Housing conducted a review of the evidence of the health effects of housing policies (Jacobs and Baeder, 2009). They found evidence for the use of several housing interventions, including rental housing vouchers, structural modifications (e.g., asthma interventions, pest management, and radon mitigation), as well as smoking bans and lead hazard control. In 2010, the Urban Institute published findings from their evaluation of the Chicago Family Case Management
Demonstration, which is an “effort to test the feasibility of using public and assisted housing as a platform for providing services to vulnerable families” (The Urban Institute, 2010). Participants in the program reported gains in employment, housing, neighborhood conditions, and health with reduced fear and anxiety (Popkin et al., 2010; The Urban Institute, 2010).
Altering the Built/Physical Environment
The notion that communities can shape the environment to be healthier or more health supportive is a fundamental belief underlying this report. A wide range of policy tools (included among the tools described in Chapter 3) are available to address features of the built environment, and several jurisdictions across the country have successfully experimented with land use interventions, including in the areas of zoning and transportation. This type of tools, however, differs somewhat from many others listed earlier because they go beyond the purview of the public health agency and require involvement and leadership from other parts of government and from the private sector.
The boundaries between health and non-health policies, such as zoning, are not always sharply delineated. For example, in recent years, zoning decisions have increasingly incorporated health as a specific objective, so-called “health zoning” (Abdollah, 2007; Chen and Florax, 2010; Mair et al., 2005). Local governments have banned gun dealers in residential areas to reduce crime and violence in communities, and have made zoning decisions to limit the density or avoid school proximity to alcohol sources and more recently, fast-food outlets (Chen and Florax, 2010; Gostin, 2010). In some cases, urban planners, transportation officials, and other non-health professionals have been the ones to initiate activities to redesign the built environment in ways that promote and support healthier choices.
The built environment is strongly linked with several types of health outcomes in the population (Bauman and Bull, 2007; Brownson et al., 2006; Communities Count, 2008; TRB and IOM, 2005). Obesity is perhaps the most prominent current concern, and is related not only to the food one consumes and one’s level of physical activity, but to environmental features such as
- a community’s zoning laws that dictate the density of fast-food outlets, and incentivize (or not) the introduction of supermarkets and other fresh-food outlets (California Center for Public Health Advocacy et al., 2008; Diller and Graff, 2011);
- transportation plans and laws that encourage (or not) pedestrian and bicycle use rather than motor vehicle use (Brownson et al., 2005; McCann et al., 2009);
- planning guidelines that expand green and recreational spaces, and school requirements that allow community use of athletic fields (Garcia and White, 2006; Lovasi et al., 2009); and
- a community’s ability to set aside and use land for community gardens (NPLAN, 2010; Twiss et al., 2003).
Laws and other types of public policy can change these and other aspects of physical or built environment.
THE “HEALTH IN ALL POLICIES” MOVEMENT
Interest has been growing both in the United States and abroad, in “Health In All Policies” (HIAP), an approach to policymaking in which decision-makers outside the health sector routinely consider health outcomes: benefits, harms, and health-related costs. Kickbush and Buckett (2010, p. 12) define HIAP as “public service agencies working across portfolio boundaries to achieve a shared goal and an integrated government response to particular issues. Approaches can be formal or informal, and can focus on policy development, program management and service delivery.” Although the HIAP concept emerged in connection with government organizations, its meaning has been extended to include private and non-profit policies as well. Examples of public health-relevant policies in the private and nonprofit sectors include employer policies and practices (e.g., in response to safety requirements imposed by insurers), building standards that exceed government requirements (such as LEED2 “green” building certification), and principles for sustainable investment (e.g., yielding financial, social, and environmental returns3).
Rationale
Most decision-makers who set policies on housing, agricultural crop incentives, or highway construction do not usually consider the public health dimensions, in part because they have not had traditional, or statutory, responsibility for those areas. Also, health entities in the government, private, and not-for-profit sectors are similarly unlikely to connect or collaborate with those who may be considered stakeholders in the public’s health. These failures to connect have consequences for all involved. Too often, proponents of a policy overlook potential health benefits in making their case or in calculating the return on investment to argue the value proposition.
Conversely, advocates of a policy do not always consider the potential
__________________________
2 Originally denoted “Leadership in Energy and Environmental Design.”
3 See, for example, Emerson et al. (2008).
harms to public health, and resulting costs, or how those harms could be mitigated. Overlooking health seems incompatible with good policymaking, not only because it creates an incomplete picture of the full outcomes of a proposed course of action, but also because it can undermine the ability to coordinate efforts across sectors to address important public health and economic priorities. For example, a coordinated approach to the obesity epidemic—a health outcome that imposes great cost on the economy (CDC, 2010; Wang et al., 2008; Wolf and Colditz, 1998) and on employers (Finkelstein et al., 2005; Goetzel et al., 1998; Schmier et al., 2006), and may present a risk for developing other poor health outcomes such as diabetes and heart disease—requires synergistic changes in schools, workplaces, advertising, the food industry, restaurants, parks, public transportation, tax policy, and clinical care. A coordinated approach to this problem therefore requires policymakers in each of these sectors to consider their respective role in addressing obesity and how best to harmonize their efforts with other sectors. Working across sectors can improve effectiveness in addressing public health problems by tackling root causes that are outside the traditional health sector. It could also maximize the use of existing government, institutional, and policy resources by promoting synergy, identifying economies of scale, and reducing duplication of effort (Baxter, 2010). Adopting a HIAP approach could cost little or nothing in many areas of local government. For example, in transportation, land use, or zoning decisions, some modifications that influence health may have minor or no budgetary implications for the implementing agencies (Boufford, 2011, offers the example of using regularly scheduled bus stop renovations to make them more accessible to older adults, and thus provide support for healthier aging).
Cross-governmental collaboration is hardly a novel notion for public health agencies. Those capacities were evident after September 11, 2001, when bioterrorism preparedness planning brought public health practitioners into closer discussions with fire, law enforcement, and emergency management communities. A need for broader collaboration to address the rising prevalence of chronic disease has strengthened the imperative for coordinated efforts across the public and private sector.
Ultimately, the health of a nation is instrumental in its economic strength and competitiveness. Businesses can rise and fall on the strength of their employees’ physical and mental health, which influence levels of productivity and, ultimately, the economic outlook of employers (World Economic Forum, 2008). The United States’ lower life expectancy and lower health-related quality of life has implications for all sectors in society in terms of opportunity and other costs (financial, human potential, social, and other). Reform of the medical care delivery system is envisioned to handle issues of quality and cost of services, but the committee concurs that “[h]ealth in all policies represents the most comprehensive level of health reform” and
“broadens the definition of health reform to include a consideration of the intentional or unintentional impact of all policies—health, social, economic and others—on individual or population health” (Georgia Health Policy Center, 2008, p. 17).
HIAP and the Federal Government
In the past several years, reports from U.S. blue ribbon panels have offered recommendations for a coordinated, intersectoral approach to governing. For example, the Center for the Study of the Presidency and Congress issued a report by its Commission on U.S. Federal Leadership in Health and Medicine, which recommended the implementation of a HIAP approach across federal departments and agencies, including the creation of a federal coordinating council (Commission on the U.S. Federal Leadership in Health and Medicine, 2009). This approach was consonant with that expressed in a 2008 report from the Center for American Progress and the Institute on Medicine as a Profession, The U.S. Health Care System: A Blueprint for Reform, as follows:
National and local policies, programs, and funding allocations that support health—not just health care—must be realigned and prioritized in order to meaningfully improve population health. This process can be informed by examining the factors underlying the health status measure “life expectancy from birth” which incorporates the main causes of premature death. These reside in five domains: behavioral patterns, social circumstances, environmental exposures, health care, and genetics. (Center for American Progress and The Institute on Medicine as a Profession, 2008, p. 98)
Many of the themes of HIAP surfaced in the evolution of health care reform legislation and took statutory form in some of the provisions included in the Affordable Care Act (ACA) by Congress in 2010. Specifically, the law called for the establishment of the National Prevention, Health Promotion, and Public Health Council. The Council, created by executive order of the President and convened by the Surgeon General of the US Public Health Service, constitutes the highest-profile HIAP action in the federal government. It brings together cabinet secretaries and heads of major agencies to develop a prevention strategy for the nation and to address national health priorities from an interdepartmental and interagency perspective. Despite the distinct statutory roles, responsibilities and priorities of the separate agencies, the Council calls on its executives to think creatively about ways in which their interests may be furthered by contributing to the nation’s prevention, health promotion, and public health strategy.
Another example of HIAP in action is the Partnership for Sustainable Communities, a joint initiative by the Environmental Protection Agency (EPA), the Departments of Transportation (DOT), and Department of
Housing and Urban Development (HUD) that is intended to “stimulate a new generation of sustainable and livable communities that connect housing, employment, and economic development with transportation and other infrastructure improvements” (EPA, 2011). The partnership has identified six livability principles, two of which explicitly refer to health.4 The initiative, which includes $100 million to fund regional plans in 45 regions of the country, exemplifies a holistic, or cross-cutting public policy approach that aims to “connect the dots” among the many factors that make communities livable and healthy: good schools, economic development, decent and affordable housing, accessible transportation infrastructures, and other features.
The Healthy Food Financing Initiative is another example of intersectoral action on health. The initiative “supports projects that increase access to healthy, affordable food in communities that currently lack these options, [t]hrough a range of programs at Departments of Agriculture, Treasury, and Health and Human Services (HHS)” (HHS, 2010). State food financing initiatives, such as the Pennsylvania Fresh Food Financing Initiative begun in 2004, have led to the establishment of supermarkets in underserved areas. These not only make fresh and healthier foods available to communities, but they also serve as anchors for other types of economic activity, including other retail outlets (Cantor et al., 2009; PolicyLink, 2010; The Reinvestment Fund, 2008).
HIAP in State and Local Governments
Some state and local governments have already adopted HIAP approaches. In February 2010, the governor of California issued Executive Order S-04-10, which authorized the California Strategic Growth Council (SGC) to establish a Health in All Policies Task Force as part of its larger mission to develop a sustainable economy for the state. This action explicitly linked economic growth to the health of the people of California. The Task Force was charged with identifying “priority programs, policies, and strategies to improve the health of Californians while advancing the SGC’s goals.” To accomplish this, a multi-agency council was assembled to facilitate collaboration in several areas, including air and water quality, protection of natural resources, availability of affordable housing, promotion of public health, sustainable land use planning, and climate change goals
__________________________
4 “Provide more transportation choices. Develop safe, reliable, and economical transportation choices to decrease household transportation costs, reduce our nation’s dependence on foreign oil, improve air quality, reduce greenhouse gas emissions, and promote public health.” and “Value communities and neighborhoods. Enhance the unique characteristics of all communities by investing in healthy, safe, and walkable neighborhoods—rural, urban, or suburban.”
(Health In All Policies Task Force, 2010b, p. 9). The SGC-convened Task Force includes 19 agencies, including the Office of the Attorney General, business, transportation, education, social services, and housing (Health In All Policies Task Force, 2010b). After a process that included soliciting and receiving public input and defining a vision of a healthy community, the task force developed a report with 34 recommendations. These were based on a set of criteria, including population health impact, overlap with SGC objectives, availability of supportive evidence, ability to foster collaboration, equity impact, measurability, feasibility, and ability to transform state government culture (Health In All Policies Task Force, 2010a). The report was adopted by the Strategic Growth Council.
A HIAP approach has also been adopted in the master plan for Fort McPherson, an army base in Atlanta that is slated for closure (McPherson Planning Local Redevelopment Authority, 2006). A major objective of the redevelopment partnership’s effort is to meet a range of community needs, including those of vulnerable disadvantaged populations living in neighborhoods surrounding the installation. The partnership (involving the local redevelopment authority and public health experts) developed a list of guidelines that would be incorporated in the Master Plan for redevelopment and would call for specific features that benefit health (McPherson Planning Local Redevelopment Authority, 2006). The city of Atlanta agreed to incorporate the partnership’s recommendations for zoning requirements. Multiple efforts were made to involve surrounding communities in the planning discussions, which led to a plan based on principles of sustainable urbanism, including promoting public health. Access to a full-service supermarket, multi-income housing, recreation, green spaces, public transportation, and other amenities were among planners’ objectives (Avey, 2011).
In an effort facilitated by the New York Academy of Medicine, and with the collaboration of the American Association of Retired Persons, the city of New York has implemented a variety of activities to become one of the World Health Organization’s (WHO’s) network of 35 age-friendly cities. The effort began with convening 22 city agencies, and has led to a range of commitments to make the city’s transportation, education, business, and other sectors and systems accessible to people of any age (Boufford, 2011). The WHO guidelines identify the following domains of urban life necessary for healthy aging: outdoor spaces and buildings, transportation, housing, social participation, respect and social inclusion, civic participation and employment, communication and information, and community support and health services (WHO, 2009).
The field of community development finance is finding synergies with community health improvement efforts. Richter (2009) has observed that the vulnerable groups targeted by the Community Reinvestment Act are not only at risk financially, but also in terms of their health. These two
conditions, poor health and low income, are mutually exacerbating, and community development financial institutions (CDFIs) have been making investments that aim to improve both the conditions for health and for future financial well-being of disadvantaged families. For example, CDFIs have invested in bringing supermarkets to underserved areas, and in increasing the availability of early child care, quality education, affordable housing, and recreational opportunities for youth. Models of community development finance investment in health and human development are being tested (Richter, 2009).
The HIAP approach offers great promise not as an approach that prioritizes health above other important societal objectives, but rather, as a wide range of intersectoral efforts to achieve synergies from policy action. Seen from the perspective of other sectors, HIAP could enhance their ability to achieve their own objectives because improvements in population health will have wide-reaching effects on many aspects of society. For example, in the case of the Atlanta military base closure, the HIAP effort being planned means that government property has the potential of being redeveloped in a manner that can lead to the creation of a thriving community. If the community succeeds in meeting HIAP objectives, the community will enhance the economic and social vitality of the area, and benefit diverse groups in surrounding neighborhoods by expanding housing, employment, recreational and educational opportunities. The committee finds that multi-sector strategies that consider the impact of non-health sectors’ action on the health of Americans can create progress in those sectors, while increasing the quality of life, longevity and economic productivity of the population.
Recommendation 7: The committee recommends that states and the federal government develop and employ a Health In All Policies (HIAP) approach to consider the health effects—both positive and negative—of major legislation, regulations, and other policies that could potentially have a major impact on the public’s health.
HIAP: Some Findings from International Examples
The pertinence of intersectoral policies to population health status was a key message of WHO conferences in the 1970s, 1980s, and 1990s. HIAP became a signature focus of the Finnish presidency of the European Union—a significant fact because of Finland’s North Karelia health promotion project, launched in 1972, which exemplified one of the early uses of a HIAP approach to address a major and pervasive health challenge. In the 1970s Finland had the highest rate of cardiovascular disease (CVD) in the world. The North Karelia project targeted CVD by forming a collaboration among government and private and civil society sectors to change the
social, physical, and policy environment. Over a 30-year period, mortality from CVD decreased by 85 percent (Puska, 2008). (For more information see Box 4-2.)
Another example of intersectoral action to improve the health of a population is found in the French project Ensemble Prevenons l’Obesite Des Enfants (EPODE), which aimed to develop local land use planning processes to create a “healthy town” and involved a partnership of planners, the nonprofit sector, health professionals, and the education sector (Aylott et al., 2008). EPODE succeeded in significantly reducing the rate of overweight in boys (by half) and in girls (by one-third) in the project area.
Climate change is one area of national policy where HIAP could play a crucial role, but at this point that role has been minimally explored. On the one hand, there are examples of sectors working in isolation and not considering the potential of common means to achieve complementary ends. For example, researchers or decision-makers who are concerned about global climate change and its consequences for food, water, weather, and biodiversity may not consider health impacts as seriously or at all (McMichael et al., 2009). On the other hand, the British government’s report Tackling Obesities noted that the goal of slowing down climate change and the goal of reversing obesity trends are linked (Aylott et al, 2008). For example, avoiding motor vehicle use in favor of walking or riding a bicycle implies no greenhouse gas emissions and has the added benefit of facilitating the burning of calories consumed (Butland et al., 2008). This recognition offers an opportunity for intersectoral action.
BOX 4-2
North Karelia:
An Early Example of Multi-Sector Action for Health
“[C]omprehensive approaches were needed to make healthier dietary habits easier for people” (Puska and Ståhl, 2010, p. 317).
The Finnish government heavily subsidized the dairy industry which specialized in the butter, full-fat milk, and other products favored by consumers. Gradually, industry opposition and concern were addressed and the industry shifted to producing lower-fat dairy products. The meat industry similarly shifted to producing more lean meat products. Also, subsidies were changed to encourage berry and vegetable production. A variety of communication strategies involving community groups were implemented to replace butter with canola and other vegetable oils for cooking, among other changes.
SOURCE: Puska and Ståhl (2010).
The Law and HIAP
HIAP in its broadest form involves collaboration among government and the private and not-for-profit sectors to fully implement coordinated strategies. Redesigning the built environment, promoting healthier diets, improving education, and creating jobs are tasks that require leadership by businesses and community organizations. Later, this chapter returns to a discussion of this important public-private nexus of HIAP and proposes a mechanism for building that collaboration, but the paragraphs that follow focus on the role the government plays in HIAP and the place of the law as a tool for implementation.
The implementation of HIAP by government agencies requires policymakers, with the support of the public health agency, to adopt a collaborative and structured approach to considering the health effects of major public policies across government sectors. Although HIAP initiatives in government do not necessarily involve explicit legal authorities, the law is often an important tool for institutionalizing an infrastructure for HIAP and for requiring agencies to ensure that the policies they pursue serve to protect and promote public health. The most effective health-improvement tools available at a population level are often legal and policy tools.
Based on its reading of the pertinent literature, the committee notes a continuum of objectives and actions where HIAP can be applied within law and public policy.
- HIAP can be seen, at a minimum, as a manifestation of the precautionary principle: first, do no harm to health through policies or laws enacted in other sectors of government.
- HIAP can be used affirmatively to improve population health by maximizing a non-health policy’s positive effects on health.
- HIAP can be used as a proactive, targeted approach to addressing the most distal factors (i.e., the socioeconomic fundamentals of jobs, schooling, and financial stability and self-sufficiency) that are associated with poor population health outcomes.
The first type of application for HIAP, that is, as an embodiment of the precautionary principle, is exemplified by California’s Clean Air Act. The Act marked the culmination of multiple activities, including efforts by community groups who sought to address the environmental triggers of asthma attacks in children. High asthma rates bore a known association with exposure to agriculture-related sources of pollution that had been exempted from the state’s older air quality laws (Bell and Standish, 2005). The Act’s objective was to set, within environmental law, a standard for air quality that would mitigate asthma attack rates. An example of the second application of HIAP, that is, the implementation of a non-health policy that
achieves a positive impact on health, is the case of agricultural subsidies. Laws that are intended to protect the viability of American farmers can also be designed to have a positive impact on health by changing what crop is subsidized. Increasing access to fruits and vegetables by subsidizing foods that have greater nutritional value and away from agricultural products such as corn, which find their way into unhealthful foods, can be done in ways that support farmers and health simultaneously. The third application of HIAP is seen in the federal partnership among the EPA, DOT, and HUD as described above—an effort that is premised on an acknowledgment of the deep interconnections among the various dimensions of the built and natural environments and their effects on human health and community well-being.
In some cases this continuum of objectives is achieved through legislation, as illustrated earlier by the HIAP initiatives stipulated by Congress in the provisions of the Affordable Care Act and the Prevention Council, or through actions of the chief executive, as illustrated by the creation of the HIAP task force by California’s governor. In other cases, the law invokes public health concerns as a basis for placing restrictions on commerce, transportation, and other domains outside the normal auspices of public health agencies. Examples include laws regarding the sale of firearms, the design and use of safety features in motor vehicles, environmental protections, agricultural subsidies and tax incentives, food labeling, and indoor smoking bans. More broadly, legislatures and the agencies of the Executive Branch of the federal, state, and local governments—acting on their constitutional authorities—exert broad influence on the design of economic policy, employment opportunities, the tax code, school reforms, financial aid for college, and other factors that, as noted earlier, are strongly associated with health outcomes.
Challenges to Implementing HIAP
The ease of implementation and the success of HIAP approaches is dependent on (1) the level of compatibility of interests among the relevant sectors; (2) the extent to which health policy or intersectoral action of some sectors can bring about the desired change on their own (compared to how much of it is dependent on changes or constraining factors in other sectors); and (3) the costs of strategies (e.g., financial, political, social) and the fact that benefits are often harder to calculate than immediate costs (Sihto et al., 2006). Challenges to implementing health in all policies approaches also include the health sector’s limited connectedness to other sectors; intersectoral differences in aims and values and organizational culture and politics; and the costs and opportunity costs of focusing on health as a primary outcome of policy (see, for example, Ollila et al., 2006; Piot et al., 2010; Sihto et al., 2006).
The challenges for HIAP are reflected at their most fundamental level in vigorous debates surrounding legislation that simply seeks to use the precautionary principle. For example, for many years, legal arguments have surrounded the constitutionality of imposing restrictions on the sale of tobacco, firearms, and alcoholic beverages. The tobacco impasse was due in part to the deeply entrenched interests of the agricultural sector and tobacco-growing states. Such debates are partly a matter of legal argument, but they are also political. The debates focus on where to balance the responsibility of government to protect the health of the public against its obligation to preserve individual autonomy and a free market in which consumers, rather than government, determine their actions and consumption of products and services. Another example comes from the contentious realm of firearms, where making reasonable public policy requires that policymakers “take into account conflicting constitutional claims and divided public opinion as well as facts about the relationship between guns and violence. And in doing so they must try to strike what they regard as a reasonable balance between the costs and the benefits of private gun ownership” (IOM, 2004, p. 1).
Politics and political acceptability form an important backdrop to HIAP approaches, which seek to coordinate efforts to implement a policy. Conflicting political ideologies sometimes complicate the effort to determine preferred policy directions. For example, education and income are universally valued by American society and, as noted earlier, have powerful associations with improved health outcomes, but conservatives and liberals favor different strategies to achieve these common aims. All sides share the desire to improve the education of America’s children, but some policymakers favor greater competition and voucher programs for private schools, while others want to raise tax revenue for public schools. All policymakers want Americans to earn more income. Some believe this is best accomplished by removing tax and regulatory burdens on businesses to help them thrive and create more jobs, while others favor direct assistance programs for low-income families and the unemployed. The HIAP approach is inherently non-partisan; it calls on policymakers of all political persuasions to consider the health implications of a new or revisited policy or law. For example, an advocate of lowering taxes on businesses might cite the health benefits to workers if tax relief prevents layoffs and creates new jobs: stable incomes, health insurance coverage, and the ability to afford to live in a healthier neighborhood. Another policymaker might champion the extension of unemployment benefits to protect individuals from poverty. Both policy initiatives can be readily reviewed through the lens of HIAP development. However, because HIAP could be subject to political manipulation, with claims made based on political ideology, evaluation of the impact of all policies created under this banner is imperative. The committee returns to the area of evaluating the evidence of policy effectiveness later in this chapter.
The notion that policymakers should be obliged to consider the health outcomes of proposed policies raises philosophical questions about the limits of jurisdiction and responsibility. Although public health professionals believe health is a primary value and that value is self-evident, policymakers in non-health sectors have portfolios that require them to advance other public goods of high priority to government and society. As a practical matter, in a resource-strained environment, energy, transportation, or national security may gain more prominence for the public and its elected officials than improvements in population health.
Therefore, it is important to note that a HIAP ethos need not limit actions that are critical to accomplishing work in other sectors. Rather, the HIAP approach asks all sectors, including public health, to direct attention to ways in accomplishing their objectives that will not detract from, and may at times enhance, the health of the public. Public health leaders and practitioners need to listen to colleagues in other sectors of government, understand their agendas and priorities, and find ways to identify mutually beneficial approaches to communicating and accomplishing their objectives. The public health community must also learn to convey clearly and compellingly the linkages between health with its multiple determinants and other societal objectives, such as prosperity, productivity, and competitiveness.
For their part, public health officials may themselves resist the premise that their mandate extends beyond core public health functions to include transportation, housing, and school reform. Is it appropriate for public health professionals and scientists to cast their gaze on the broader causes of poor health and thus enlarge their field’s purview and sphere of influence and the breadth of their interventions? Or should the field remain focused on the more proximal causes of poor health, such as risky behaviors and infectious diseases, and refrain from attempts to influence and intervene in distal policy spheres? Thoughtful reflection on the statutory and professional responsibilities of governmental public health requires these organizations to communicate about data and evidence, and convene other sectors and stakeholders toward health-supporting policy action that extends beyond the historical arenas in which these institutions have worked.
Apart from politics and philosophical questions, the fragmented structure of government is itself an obstacle to the HIAP approach. Federal, state, and local governments are often balkanized in silos—agencies with discrete policy interests and regulatory concerns that lack the culture, tools, and language to cross boundaries and coordinate with counterparts in other agencies. An infrastructure that supports such collaboration, such as an interagency task force, cannot be formed or operate effectively without hard work to build relationships and solve interagency barriers that impede communication, collaboration, and the sharing of resources. The committee believes these philosophical and structural obstacles—both external and
internal to the public health community—need to be overcome through concerted efforts by all governmental actors. These actions will allow this nation to make good on the promise of the level of health that a wealthy nation should furnish its population.
STRUCTURES TO SUPPORT COLLABORATION IN PROMOTING HEALTH IN ALL POLICIES
In its purest form, the HIAP approach entails collaboration among multiple sectors, reaching beyond the government, to foster the conditions for good health. Public health agencies or, more broadly, government, cannot alone be effective in helping a community to address tobacco use, reduce obesity, redesign the built environment, produce jobs, and improve children’s education. Nor can the private sector do this alone. Effective strategies require collaboration as well as coordination, with the latter being important to marshal and leverage limited resources, avoid duplication, and use the talents and assets that each partner offers. Few would dispute the merits of coordination and collaboration, but the infrastructure for forming such partnerships is lacking in most communities.
What is the role of the public health department in facilitating action? Two key roles of governmental public health agencies to date have not been systematized to their full potential: (1) as communicators/reporters about a community’s health and its causal or associated factors, and (2) as conveners/facilitators of independent and collaborative action by other organizations and sectors (Pomeranz, 2011).5 Across the nation, new working relationships are being formed among private, non-profit, and governmental agencies, bringing new challenges and bridging to enable shared responsibilities. Policy, in both the public and private sectors, can facilitate and guide these partnerships.
In its first report, the committee discussed the topic of accountability for population health and presented a measurement framework for accountability in two contexts. The first is contract accountability, applicable to the funding, statutory, and fiduciary relationships among those who are funded to “do” public health work (government agencies and others) and their funders (i.e., higher level of government, taxpayers) to whom they are accountable. The second is compact or mutual accountability, which characterizes the relationships among public health agencies and the many
__________________________
5 Pomeranz (2011, p. e2) writes: “By coordinating cross-agency conversations and policymaking, health departments can insert health concerns into a vast range of policymaking activities within their jurisdictions. This approach, called health in all policies, brings health issues from the traditional health sectors into other government entities, thereby positively influencing transportation, housing, environment, education, and fiscal policies.”
stakeholders in the health system: schools, businesses, community organizations, medical care providers, and community members. The framework for accountability in any context can be outlined in three steps: (1) agreement among implementers and those holding them accountable on specific plans of action targeting health priorities; (2) holding implementers accountable for execution of agreed-on plans; and (3) measurement of execution and outcomes of those plans, and further agreement on revisions to the action plan.
In the present report, the committee endeavors to give structure to the process described in the first report. For example, given the notion of non-public health implementers (e.g., diverse arrays of community organizations, medical care organizations, employers, and others) holding each other and the group accountable for accomplishing intended improvements in a community’s health requires some type of governance entity, such as a coalition or board. The question the committee seeks to answer in this section is how do legal, or more broadly, policy frameworks, inform the structures needed for effective multi-sector engagement on population health, where there are and where there are not statutory or funding relationships that serve as the natural bases for holding participants accountable? Despite the fact that an estimated half the overall public health expenditures are incurred by nongovernmental actors (see Mays et al., 2004) mechanisms to track the achievements and create accountability for those investments are often limited to reporting obligations between funders and grantees, but are not easily identified for use with larger, intersectoral networks of actors with multiple crisscrossing relationships. Such a mechanism is needed to give some organizational structure to the diagram provided in Figure 4-1 (from the committee’s report on measurement [IOM, 2011]), which describes the multi-sectoral, multi-stakeholder health system and a measurement framework to enable it to plan, implement, and evaluate its effects on the community’s health.
Accordingly, the committee looked for models that could create accountability that span public and private action and investments. Several models are available to inform efforts to develop advisory mechanisms that involve the private sector. These may be drawn from the Healthy Cities/Healthy Communities movement, which included the development of multi-sectoral coalitions that planned, implemented, and evaluated their efforts (Kegler et al., 2009). Other examples of governance mechanisms, including some oriented toward public oversight of government expenditures, are found in the context of international urban governance arrangements (Burris et al., 2008). Fawcett and colleagues (2000, 2010) have also described community partnership models. Other examples may be found in foundation-supported efforts around the country, such as the California Endowment’s Building Healthy Communities Initiative, a 10-year community grant program that
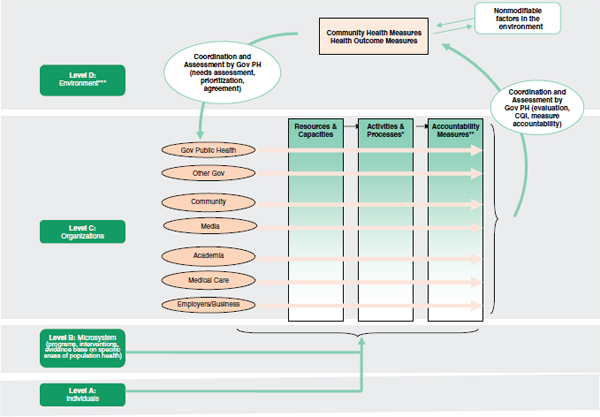
FIGURE 4-1 A framework for measurement in accountability.
NOTE: Gov = Government; PH = Public Health; CQI = Continuous Quality Improvement
*Activities and processes are influenced by agreed-on strategies (strategies agreed on by those being held accountable and those holding other parties accountable through contracts or compact agreements).
**Accountability measures assess how well the agreed-on strategies are executed and this may also be thought of as strategy execution measures.
***Stakeholder activities both influence the environment and work within it to shape outcomes.
SOURCES: Adapted from Berwick (2002); IOM (2001, 2011).
includes the establishment of hubs, or “central tables,” around which all stakeholders gather to plan, assess, and celebrate achievements.
The model the committee found most useful is the National Prevention, Health Promotion, and Public Health Council established by ACA. The National Council is an attractive model in that it (1) creates a structure that specifically crosses government lines and brings different sectors of government to the table to talk about health in a structured way; (2) engages both the Legislative and Executive Branches at very high levels in an ongoing fashion; (3) focuses on creation and agreement on strategy to achieve outcomes, one of the key points in the committee’s first report; and (4) enables engagement of a broader range of nongovernment interests and input through an advisory mechanism.
The committee believes that state and local versions of the National Prevention Council can create opportunities for private and civil society engagement, similar to what federal legislation has envisioned for the National Prevention Council. The organizational structure in Figure 4-1 (from the committee’s report on measurement [IOM, 2011]) describes a multi-sectoral, multi-stakeholder health system and a measurement framework that enables it to plan, implement, and evaluate its effects on the community’s health (see Berwick, 2002; IOM, 2001). In that context, a framework was provided to demonstrate the changes needed in the US medical care delivery system, and four levels were described: Level A, the experience of patients and communities; Level B, the microsystem of care (for example, provider practices); Level C, organizations (for example, managed-care organizations); and Level D, the environment shaped by policy, payment, regulation, and accreditation. The present committee believes that that framework holds relevance for its own examination of measurement in the context of accountability and has adapted it for its own purposes.
The cycle begins after a needs assessment has been done, priorities set, and a plan agreed on. Level A in the committee’s adaptation of the framework includes communities, neighborhoods, families and individuals (whose aggregated health information constitutes health-outcome measures) and neighborhoods. Level B refers to microsystems, which in the context of population health6 are programs, policies, and interventions that may be thought to refer to the points of contact or interactions between community groups, local businesses, others in the neighborhood, and their local public health agencies and allied entities. An example of microsystems is an interaction among a health department, a local medical care provider, community coalition, or local business concerning a particular health outcome. Specifically, a health department could assist a food retailer in facilitating healthful customer choices or could support a local business in developing
__________________________
6 As is sometimes pointed out, the patient in public health practice is the community.
a workplace prevention and wellness program. Often in public health, such microsystems need to align and integrate across organizations; for example, the local cancer-control program should feed into the statewide cancer-control program, which feeds into the national program. Level C consists of organizations described as actors in the public health system in the 2003 IOM report The Future of the Public’s Health in the 21st Century (IOM, 2003) and as components of the health system. The organizations include the local public health agency, hospitals and other clinical-care entities, community organizations, schools, businesses, religious congregations, and many others that perform roles that influence health outcomes. Level D refers to the environment, which includes a variety of social, physical (both naturally occurring and constructed), and economic factors and is shaped in part by social realities, large-scale policies (and political will), and economic arrangements (Syme and Ritterman, 2009). Figure 4-1 also depicts accountability pathways for all levels but focuses on Level C—the organizations that perform functions that affect health outcomes.
In the context of this report, developing a structure to operationalize intersectoral action on health is useful for several reasons. First, it establishes a forum for stakeholders to come together and creates mechanisms for interested parties to provide input, and it also creates an entity that is appropriately placed and configured to adopt a HIAP approach. Finally, a multi-sectoral group that brings together the thinking, experience, and financial resources of many community actors will facilitate more nuanced planning, implementation and evaluation of policies that are intended to simultaneously serve both health and other key objectives of a local community. The following recommendation intends to describe the role of the public and private sectors in jointly implementing health in all policies approaches.
Recommendation 8: The committee recommends that state and local governments
- create health councils of relevant government agencies convened under the auspices of the Chief Executive;
- engage multiple stakeholders in a planning process; and
- develop an ongoing, cross-sector, community health improvement plan informed by a HIAP approach. Stakeholders will advise in plan development and in monitoring its implementation.
THE ROLE OF SCIENTIFIC EVIDENCE IN HIAP
When a policy is considered worth enacting, the key government sector or organization will work to bring together the relevant stakeholders and find ways to align their interests and compel them to engage in action. At
that point in the process, all involved stakeholders would work on identifying data from which to project effects, that is, benefits, harms, and costs, and refining analytic methods, including attribution. Stakeholders will examine a policy idea through multiple lenses, including feasibility, effectiveness, acceptability, affordability, and legality.7 Policymakers seek evidence about the effectiveness, projected outcomes, and value to judge the merits of proposed policies. This is particularly true when policies are seen as posing a risk to public health.
The effectiveness of public policies in general, and of legal interventions in particular, historically has been poorly studied, although the body of evidence is growing (see Burris et al., 2010). Some of the strongest examples are found in the work of the Task Force on Community Preventive Services and of the Cochrane Collaboration, both of which use the approach of systematic assessment of the effectiveness of certain laws and their enforcement on behaviors with health consequences. The Task Force has identified and recommended effective legislative or regulatory interventions in several areas of interest to public health. These include the prevention of motor vehicle injuries and deaths, where the evidence supports recommending laws and enforcement of child safety seat use (Evans and Graham, 1990; Guerin and MacKinnon, 1985; Margolis et al., 1988; Rock, 1996; Seekins et al., 1988; Sewell et al., 1986; Wagenaar et al., 1987a,b; Williams and Wells, 1981), and laws, primary enforcement, and enhanced enforcement programs of safety belt use (Barancik et al., 1988; Bernstein et al., 1989; Campbell et al., 1991; Chorbat et al., 1988; Desai and You, 1992; Preusser et al., 1987; Streff et al., 1990; Thyer and Robertson, 1993; Ulmer et al., 1995). Another example is state and municipal clean indoor air laws to reduce exposure to secondhand tobacco smoke (a risk factor for cancer, heart disease, and child health problems, including Sudden Infant Death Syndrome). Bans on indoor smoking have led, within months, to decreases in hospital admissions for acute coronary heart disease events such as heart attacks (Juster et al., 2007; Sargent et al., 2004). Other examples include the effect of Corporate Average Fuel Economy standards on lowering energy consumption and carbon dioxide emissions; the effect of state immunization requirements for school and child care entry on increasing immunization rates; the effect of primary education requirements on educational achievement; and the effects of ignition interlock policies, retail outlet density, and taxation on high-risk alcohol consumption. An example of an assessment done before a law’s enactment is the menu labeling analysis in Los Angeles that led to the passage of a menu labeling ordinance (Simon et al., 2008) that was eventually preempted by both the state of California and by ACA. Post-enactment evaluations are sometimes done, though
__________________________
7 The discussion of scientific evidence here is framed in terms of governmental laws and policies, but the approach also holds relevance to major changes in private sector policies.
not necessarily by the government. Examples include gun control ordinances, ignition interlocks for drivers with alcohol-related driving convictions, alcohol outlet density restrictions, and tobacco laws.
Burris and colleagues (2010, p. 169) have described the growing body of public health law research as the “scientific study of the relation of law and legal practices to population health.” This young field, they assert, can help to make the case for laws that improve health, not only through the realm of laws intended to influence population health and establish the power, duties, and infrastructure of public health, but also through laws in other sectors of government, which may powerfully influence health, but have not until recently been examined for their implications for health.
Health Impact Assessments
“In the environmental field, new construction projects are required to file an environmental impact report. In the health field, there should be a similar health impact report that makes explicit what effect new social policies will have on population health and how negative results could be mitigated,” wrote Schroeder and Hughes (2008, p. 108). Health impact assessments (HIAs) have emerged as an important tool to assist policymakers with weighing the merits of a proposed policy.8 As defined by the Health Impact Project (2010), an HIA is a policymaking tool “that identifies the health consequences of new policies and develops practical strategies to enhance their health benefits and minimize adverse effects.”9 Ongoing HIAs listed by the Health Impact Project are addressing questions such as the effect on air pollution of a new light-rail transit line to connect Minneapolis and St. Paul; the potential health effects of a proposed subway and other mass-transit alternatives through Los Angeles’ high-density, high-traffic Wilshire Corridor; the trade-off of increased employment versus increased emissions from a coal gasification project in Owensboro, Kentucky; the optimal agriculture plan in Hawaii; the health benefits of having a Chicago electric utility use “smart meters”; a proposed “cap-and-trade” regulation in California; and the benefits of proposed legislation in Oregon to use state funds to purchase locally-grown foods for schools and establish school teaching gardens. The San Francisco Bay Area’s Health Impact Assessment Collaborative provides several specific examples of policy discussions that explicitly incorporated a health assessment component, and engaged a variety of stakeholders to
__________________________
8 After the release of the present IOM report, the National Research Council released Improving Health in the United States: The Role of Health Impact Assessment to provide guidance on conducting HIA.
9 An RWJF and PEW national initiative.
examine all facets of considered public policy decisions (Health Impact Assessment Collaborative-San Francisco Bay Area, 2010).
HIAP is frequently conflated with HIA. Although HIAP and HIAs are closely related concepts, the former refers to a broad approach to public policy and the latter to a decision-support tool that may be used in evaluating that approach. It has been asserted that the health consequences of policies can be predicted, and tools such as the health impact assessments and simulation modeling can be used to enable policymakers to foresee the outcomes of choosing different options (Burris et al., 2010; Kemm, 2006). However, HIAs can be difficult, time-consuming, and costly to complete. As noted below, meaningful evidence and data are not always available to arrive at definitive conclusions. It is therefore important for the law to impose some parsimony in dictating requirements for conducting HIAs. Apart from the administrative burden, it is neither necessary nor useful for policymakers to commission HIAs for every policy proposal. For example, enacting a modest retail redevelopment policy where the health impact is foreseen (i.e., through a “back of the envelope,” informal analysis) to be negligible would likely not benefit from the development of a full or comprehensive HIA. In other cases, assessing the evidence is critical, as in the cases of federal laws with the potential for broad health impact that require periodic authorization. Examples here include the federal farm bill, which pertains to agricultural subsidies and policies on production and distribution of farm products; the transportation bill, which includes allocations for alternative transportation, such as bike paths, and public transportation in addition to roads and infrastructure; large local/state projects, for example, water distribution in Western states; and proposed large scale industrial plants or major redevelopment efforts. Although the administrative and methodological tasks of such research are challenging, the committee adopts as a general principle the obligation of policymakers to study, to whatever degree possible, the potential ramifications of policies in any sector that could substantially affect the health of the public.
Recommendation 9: The committee recommends that state and federal governments evaluate the health effects and costs of major legislation, regulations, and policies that could have a meaningful impact on health. This evaluation should occur before and after enactment.
This recommendation applies to both public health and non-public health agencies working in concert. Before and after enactment, a scientific assessment would be conducted whenever possible. Before enactment of such policies, the vested authority (e.g., the public health agency) would study the potential health impact and/or cost-effectiveness. After enactment, the
authority would review the health outcomes and costs associated with implementation of the policy and would, where appropriate, offer recommendations to the chief executive and legislature on changes that would improve outcomes.
Such evaluation and assessment could be conducted by the responsible agency, such as through National Environmental Policy Act (NEPA) requirements, or by the public health agency. There are several existing models for requiring and conducting assessments of health policy impact (see Box 4-3 for examples of tools available to support implementing health in all policies). These include the state of California, where a consortium of universities conducts assessments, including actuarial analyses, of the impact of many health policies, and the requirements of NEPA, which calls for an environmental assessment to first determine whether an action or project is environmentally significant. If yes, an environmental impact statement must be prepared. If no, a Finding of No Significant Impact may be issued by the responsible agency.
Scientific and Methodological Challenges to Measuring the Outcomes of Public Policies
Data and analytic methodology are often lacking for estimating the likely outcomes of proposed policies, laws, and regulations. The interven-
BOX 4-3
Making Evidence Useful to Policy Makers
Other researchers have sought to understand and explain the attitudes and behaviors of policymakers with regard to evidence. Researchers have found that evidence evaluation and reporting tools such as systematic reviews may not be helpful to policymakers because they do not make clear the reviews of policy applications (Jewell and Bero, 2008). Clancy et al. (2006) found that evidence syntheses for policymakers must be structured to answer policy questions and provide policy conclusions and also identified certain features of policymakers that make them better consumers of evidence. Both Sorian and Baugh (2002) and Clancy et al. (2006) report that two types of products are useful in communicating with policymakers about evidence on health policy: short summaries or briefs and longer, more detailed and technical studies or reports. Also, researchers found that it is useful to policymakers if the policy briefs and other materials prepared for them are designed to communicate about impacts in concrete ways, explaining benefits, harms, and costs; who will be affected; and how different policy options would work (Jewell and Bero, 2008; Sorian and Baugh, 2002). Additional essential ingredients include personal contact between policy researchers and policymakers, and timeliness or relevance of research (Innvaer et al., 2002).
tions that such proposals advocate are rarely the subject of empirical studies, making it difficult for policymakers to adopt the degree of evidence-based rigor that has become more common in medicine and public health practice. Even when such studies are available, accepted criteria for grading the quality of studies are lacking. The classic gold-standard in evaluating the efficacy of clinical interventions is the randomized controlled trial, followed by observational studies (time series, cohort studies, natural experiments). Braveman and colleagues (2011b) have outlined the deficiencies of this traditional evidence hierarchy in evaluating population-based interventions. The somewhat limited applicability of this hierarchy to public health interventions is well-discussed in the literature, but the classic evidentiary standards seem even less useful to the domains of laws, regulations, and policies.
Many other useful approaches and tools from other disciplines are available and can be applied with methodological care and rigor. For example, various forms of simulation and predictive modeling can be useful in projecting the likely outcomes of proposed policies by piecing together bodies of evidence and data from different domains (see, for example, the SIM SMOK tobacco control simulation model) (Levy et al., 2006). A need exists for experts from multiple disciplines to pool their knowledge in marshalling the proper methodologies for evaluating the effects of public policy and for reaching consensus on criteria for grading their quality. That effort would build on several decades of literature that has proposed various schemes for evaluating the evidence for population-based interventions.
Prior work has identified a variety of methodological challenges of measuring outcomes in this context. Accurate and complete assessment of the outcomes and benefits of laws, in public health or other arenas, is complicated by the fact that the effects are often distributed across multiple segments within the population, across multiple health and social endpoints, and across long time horizons. For example, laws that address the built environment through promotion of active transportation may have short-term effects on the well-being and quality of life of users; intermediate effects on neighborhood desirability, housing prices, and air quality; and longer-term effects on chronic disease incidence and progression, including cardiovascular disease, diabetes, and asthma. Assessing the impact of public health laws requires careful measurement and analytic strategies that take these details into consideration. Also, the work of the Task Force on Community Preventive Services indicates that multiple, different, and ongoing interventions are sometimes necessary to achieve a substantial and sustained effect on health outcomes and health behaviors (this was the case with tobacco, as discussed in Chapter 3, and similarly multifaceted interventions are likely needed to address physical activity, high school graduation rates, and living wages).
Ideally, outcome measures for public health laws should consider not only epidemiological measures of mortality and morbidity but also measures of population preferences, well-being, and quality of life. Just as the
development of patient-centered outcome measures has become a priority for comparative effectiveness research and evaluation under health reform, to be implemented through the Patient-Centered Outcomes Research Institute (PCORI), community-centered outcome measures, together with distal outcomes such as health-adjusted life expectancy, are needed to evaluate the full impact of laws on outcomes of importance to the public.
Although the committee accepts the principle that all population health interventions, including laws, should be based on the best evidence available, it notes that the policy context determines the level of acceptable uncertainty in the data. In particular, the risk of harm (economic or health-related) that arises from implementing or failing to implement a law is highly relevant. More limited evidence may be used to craft legal interventions when health threats and potential harms from inaction are large; when opportunity costs and unintended harms from action are within acceptable limits; and when the time demands and/or other costs required for gathering more definitive evidence are large relative to the expected value of the additional evidence (a “value of information” analysis).10 Using weaker forms of evidence has the potential to increase the risk of false positives—the consequences of assuming a public health law is effective when in fact it is not—but this risk needs to be balanced against the risk of false negatives—the consequences of inaction and delays in the implementation of potentially effective new laws. When weaker levels of evidence are used to justify new laws, stronger prospective evaluations are needed to assess impact and produce additional evidence over time. According to Kindig (2010), early childhood intervention is one area where inaction may have grave consequences. The evidence for various policy and other approaches is mixed and there are important remaining gaps in our knowledge, but the risk from not acting on what is known, or even partially supported by the evidence, can be great, as a generation of children grows up without some of the potentially essential ingredients for healthy development.
A framework or matrix could be developed to illustrate the level of certainty and magnitude of effects that policymakers need depending on the type of policy decision.11 Variables that could be used to structure such a framework would include the level of risk presented by the legal intervention, the population impact of the health risk factors being targeted, and the type of legal action. Other factors include the potential scope of the policy, severity and frequency of the potential health effects, availability of other
__________________________
10 In some cases, it may be possible to undertake research during policy implementation (including so-called natural experiments that compare a jurisdiction that implements a specific policy to a similar jurisdiction that does not), or to implement in a manner that allows study of a policy’s effects.
11 A comprehensive discussion of evidentiary standards for population health interventions is available at: http://healthypeople.gov/2020/default.aspx.
options, prior experience using the intervention, and acceptability of potential risks. Such a framework could help policymakers determine what type of evidence would be sufficient to enact a proposed policy: a recommendation from a credible source such as the Task Force on Community Preventive Services or the Cochrane Collaboration; a well-conducted evaluation of another jurisdiction’s experience with the policy; or simulation modeling that estimates the policy’s potential impact. In the case of a policy targeting a major risk factor for poor health, the combination of a well-constructed hypothesis and high risk to the population may call for applying the precautionary principle and for taking action even in the absence of definitive evidence.
Costs, along with health benefits and harms, are an increasingly important concern in evaluating the likely outcomes of proposed laws, policies, and regulations. Strategic planning requires the allocation of scarce resources. It is often assumed that legal interventions have few costs. However, the cost analyses may not account for all relevant costs and externalities and may apply an individual or government perspective rather than tabulating costs to society or to the agencies responsible for implementation and monitoring. Ultimately, the population health benefit and cost effectiveness of legal interventions might be compared directly with other investments, including medical care, designed to improve individual and/or population health. Finally, legal interventions deserve to be studied not only for their effectiveness, but for their comparative effectiveness (both against other legal intervention and compared to other kinds of interventions). In an example of the former, Sturm et al. (2010) found that taxes applied to carbonated beverages that are reflected in the price on the shelf (i.e., excise tax) are more effective than taxes applied at the register (i.e., sales tax) in deterring consumer selection of such products. Moreover, the experience with tobacco taxes has taught public health officials about price elasticity—the extent to which smokers reduce demand for cigarettes as a result of cost increases (IOM, 2007).
Research on the comparative effectiveness and health impact of public health laws and policies could be conducted by documenting geographic variation and temporal change in population exposure to specific policy and legal interventions. The system also can be used to track the progress of efforts to expand the geographic reach of effective policies and laws, and to identify unmet needs for policy development and advocacy strategies. A knowledge base exists for crafting an accepted framework for evaluating the evidence of public policies, but work by an interdisciplinary team of experts is needed to build on the existing literature, review methodological challenges, and arrive at a consensus on preferred criteria. An expert panel, given dedicated time and resources for the effort, could consider the various schemes that have been proposed for grading the evidence for outcomes
assessments of policies and regulations and derive new guidelines that the HIAP movement could embrace in setting evidence-based policy.
Recommendation 10: The Committee recommends that HHS convene relevant experts to enhance practical methodologies for assessing the strength of evidence regarding the health effects of public policies as well as to provide guidance on evidentiary standards to inform a rational process for translating evidence into policy.
Although functioning as convener, HHS would be one actor among many in this process. The guidance developed would include: (1) methods for assessing the certainty of effectiveness (benefits and harms), and, if effective, the magnitude of effect, for suitable populations; (2) methods for assessing the effectiveness of interventions (policies and programs) when used alone or in combination (i.e., their incremental and or synergistic benefits); and (3) priorities for and consideration of the contextual issues that should be taken into account when determining whether (and where) to implement policies. The contextual issues to be considered include importance of the problem (severity, frequency, burden of disease, cost), feasibility (affordability, acceptability), availability of alternatives, demand, fairness (equity), preferences and values, cost effectiveness, potential to advance other societal objectives, potential for harms, legal and ethical considerations, and administrative options. The intention of this recommendation is to develop methodologies, but not to assess each individual policy. Not all policy that impacts health has governmental origins. Because the vast majority of U.S. economic activity is in the private sector, formal and informal policies adopted by business, foundations, and others have the potential to profoundly influence health. However, public health practitioners have limited knowledge of policy development and implementation in the nongovernmental sectors.
Another important priority is to establish a clearinghouse of evidence to which policymakers (and developers of HIAs) can turn to study the outcomes of prior legal interventions. The practice of evidence-based medicine and public health is aided by the existence of powerful search tools that enable users to query bibliographic databases and professional publications to identify, often within seconds, the best evidence for a clinical intervention. Building a similar capacity to evaluate the effects of agriculture, tax, housing, economic, and education policies is a worthy priority:
Unlike many other areas of public health research, research on public health law and policy has developed few surveillance systems…. Gathering information about the patterns of public health law adoption and implementation across states and local governments over time generally is done de novo in each research project. Maintaining and updating databases of laws would dramatically
improve researchers’ ability to conduct rigorous policymaking, mapping, intervention, implementation, and mechanism studies at low cost. High standards of transparency concerning the data-collection and coding protocols for such databases would allow subsequent researchers to update publicly available data sets at reasonable marginal cost. (Burris et al., 2010, pp. 194–195)
A pilot project could be developed and implemented to assess the feasibility of monitoring and measuring this activity. To track laws and policies (largely public sector, but including, where practical, major policy areas in the private sector) that successfully influence the health of populations, a health policy surveillance system could be developed, pilot-tested, and supported by CDC. Such a system would gather information on the geographic reach, scope, and timing of significant new laws and policies designed to promote health and prevent disease and disability at the population level.
The surveillance system could include such health-related laws and policies adopted at federal, state, and local government levels, including laws that define regulatory and enforcement powers and duties for public health agencies and for other governmental entities. Although more difficult to capture and assess, significant new health-related policies adopted by private organizations could also be included in the surveillance system, such as those adopted by employers, schools, health care institutions, and community-based organizations, to the extent such policies are made public and are brought to the attention of the surveillance system. A range of different methodologies for capturing information on private-sector health policies could be tested to determine an appropriate balance of validity, reliability, and feasibility. Some combination of active surveillance approaches and passive surveillance reporting through local public health agencies may be required.
This second report of the committee has identified historical and extant approaches to the use of law and policy in protecting and improving the health of the public. Law has been and will remain critical for creating the infrastructure that supports directed and accountable action, as well as for limiting some actions that diminish health, or requiring actions that enhance it.
As the nation looks to true reform in its health system, and the ultimate goal of optimizing the health of the public, challenges, but also opportunities, exist in revisiting, refashioning, and applying laws to improve the health of Americans. The challenges are by no means minimal. The committee is aware of the bureaucratic and administrative burdens and political turbulence that sometimes accompany the development or implementation of legislation, regulations, and policies. In addition, building the evidence base as it relates to forecasting potential benefits, harms, and costs, will be methodologically challenging, and will itself consume resources. Mandating efforts to do so is only appropriate when the methods, evidence and analytic
capacity are present. But building capacity to conduct this type of evidence-based evaluation and governance is key to understanding what works, to bring data and facts to a domain populated by opinions and politics, and to implement policies that are successful and efficient.
The opportunity to substantially enhance public health—and with it the nation’s economy and workforce productivity—turns on the ability of government and the private sector to shape public policies with closer and more mindful attention to health outcomes. Working together toward a goal of common interest—better health, a stronger economy, a vibrant society—also provides an opportunity for communities to build new models of collaboration and coordination that reduce inefficiency and maximize impact. This effort to bring partners and stakeholders together thereby becomes a vehicle not only for healthier communities but also a model for more productive discourse and policy formulation in other sectors.
Abdollah, T. 2007. A strict order for fast food: The city council may consider a moratorium on allowing new outlets in south LA, where obestiy rates are high. Los Angeles Times. http://articles.latimes.com/2007/sep/10/local/me-fastfood10 (May 31, 2011).
Adler, N. E., and J. Stewart. 2010. Health disparities across the lifespan: Meaning, methods, and mechanisms. Annals of New York Academy of Sciences 1186:5-23.
Adler, N., J. Stewart, S. Cohen, M. Cullen, A. Diez Roux, W. Dow, G. Evans, I. Kawachi, M. Marmot, K. Matthews, B. McEwen, J. Schwartz, T. Seeman, and D. Williams. 2007. Reaching for a Healthier Life: Facts on Socioeconomic Status and Health in the U.S. Chicago, IL: The John D. and Catherine T. MacArthur Foundation Research Network on Socioeconomic Status and Health.
Alstona, J. M., D. A. Sumnera, and S. A. Vostia. 2008. Farm subsidies and obesity in the United States: National evidence and international comparisons. Food Policy 33(6):1-4.
American Planning Association. 2002. Policy guide on smart growth: Motion to adopt a definition of smart growth. Washington, DC: American Planning Association.
Avey, H., and K. Minyard. 2011 (February 23). A Health In All Policies Approach to Large Scale Redevelopment: Fort McPherson BRAC (Base Realignment and Closure). Presentation to the Roundtable on the Promotion of Health Equity and the Elimination of Health Disparities. Washington, DC: IOM.
Aylott, J., I. Brown, R. Copeland, and D. Johnson. 2008. Tackling Obesities: The Foresight Report and Implications for Local Government. South Yorkshire, UK: Sheffield Hallam University.
Barancik, J. I., C. F. Kramer, H. C. Thode, and D. Harris. 1988. Efficacy of the New York State seat-belt law—preliminary assessment of occurrence and severity. Bulletin of the New York Academy of Medicine 64(7):742-749.
Bauman, A. E., and F. C. Bull. 2007. Environmental Correlates of Physical Activity and Walking in Adults and Children. London, England: National Institute of Health and Clinical Excellence.
Baxter, R. J. 2010. Making better use of the policies and funding we already have. Preventing Chronic Disease Public Health Research, Practice, and Policy 7(5):1-6. http://www.cdc.gov/pcd/issues/2010/sep/10_0055.htm (March 18, 2010).
Bell, J., and M. Standish. 2005. Communities and health policy: A pathway for change. Health Affairs 24(2):339-342.
Bernstein, E., D. Pathak, L. Rutledge, and G. Demarest. 1989. New Mexico safety restraint law: Changing patterns of motor vehicle injury, severity, and cost. The American Journal of Emergency Medicine 7(3):271-277.
Berwick, D. M. 2002. A user’s manual for the IOM’s “Quality Chasm” report. Health Affairs 21(3):80-90.
Boufford, J. I. 2011 2011 AARP-UN Briefing Series on Global Aging. New York, NY: AARP and United Nations.
Braveman, P., and S. Egerter. 2008. Overcoming Obstacles to Health: Report from the Robert Wood Johnson Foundation to the Commision to Build a Healthier America. Princeton, NJ: Robert Wood Johnson Foundation.
Braveman, P. A., C. Cubbin, S. Egerter, D. R. Williams, and E. Pamuk. 2010. Socioeconomic disparities in health in the United States: What the patterns tell us. American Journal of Public Health 100:S186-S196.
Braveman, P., S. Egerter, and D. R. Williams. 2011a. The social determinants of health: Coming of age. Annual Review of Public Health 32:381-398.
Braveman, P. A., S. A. Egerter, S. H. Woolf, and J. S. Marks. 2011b. When do we know enough to recommend action on the social determinants of health? American Journal of Preventive Medicine 40(Suppl 1):S58-S66.
Britten, R. H. 1938. Housing and health. American Journal of Public Health 28:957-960.
Brownson, R. C., T. K. Boehmer, and D. A. Luke. 2005. Declining rates of physical activity in the United States: What are the contributors? Annual Review of Public Health 26:421-443.
Brownson, R. C., D. Haire-Joshu, and D. A. Luke. 2006. Shaping the context of health: A review of environmental and policy approaches in the prevention of chronic diseases. Annual Review of Public Health 27(1):341-370.
Bryon, J. 2010 (September). Planning: Many Avenues Toward Health Improvement, Presentation to the Institute of Medicine Committee on Public Health Strategies to Improve Health. Washington, DC: IOM.
Burris, S., T. Hancock, V. Lin, and A. Herzog. 2008. Emerging principles of healthy urban governance-thematic paper 5. Toronto, ON, Canada: Knowledge Network on Urban Settings and WHO Centre for Health Development.
Burris, S., A. C. Wagenaar, J. Swanson, J. K. Ibrahim, J. Wood, and M. M. Mello. 2010. Making the case for laws that improve health: A framework for public health law research. The Milbank Quarterly 88(2):169-210.
Butland, B., S. Jebb, P. Kopelman, K. McPherson, S. Thomas, J. Mardell, and V. Parry. 2008. Tackling Obesities: Future Choices. England: Government Office for Science.
California Center for Public Health Advocacy, PolicyLink, and UCLA Center for Health Policy Research. 2008. Designed for Disease: The Link Between Local Food Environments and Obesity and Diabetes. Davis, CA: California Center for Public Health Advocacy, PolicyLink, and UCLA Center for Health Policy Research.
Campbell, B. J., J. R. Stewart, and D. W. Reinfurt. 1991. Change in injuries associated with safety belt laws. Accident Analysis & Prevention 23(1):87-93.
Cantor, J., L. Mikkelsen, D. Butler, and O. Sahak. 2009. Residents Live in Communities with Health-Promoting Land Use, Transportation, and Community Development. Los Angeles, CA: The California Endowment.
Capewell, S., and D. M. Lloyd-Jones. 2010. Optimal cardiovascular prevention strategies for the 21st century. Journal of the American Medical Association 304(18):2057-2058.
CDC (Centers for Disease Control and Prevention). 2010. Overweight and Obesity: Economic Consequences. http://www.cdc.gov/obesity/causes/economics.html (June 29, 2010).
Center for American Progress, and The Institute on Medicine as a Profession. 2008. The Health Care Delivery System: A Blueprint for Reform. Washington DC: Center for American Progress.
Cevero, R., K. Junhee, and S. Kevin. 2009. From elevated freeways to surface boulevards: Neighborhood and housing price impacts in San Francisco. Journal of Urbanism: International Research on Placemaking and Urban Sustainability 2(1):31-50.
Chandra, A., and T. S. Vogl. 2010. Rising up with shoe leather? A comment on fair society, healthy lives (the Marmot review). Social Science & Medicine 71(7):1227-1230; discussion 1254-1228.
Chen, S. E., and R. J. G. M. Florax. 2010. Zoning for health: The obesity epidemic and opportunities for local policy intervention. The Journal of Nutrition 140(6):1181-1184.
Chorbat, T. L., D. Reinfurt, and B. S. Hulka. 1988. Efficacy of mandatory seat-belt use legislation: The North Carolina experience from 1983 through 1987. Journal of the American Medical Association 260(24):3593-3597.
Clancy, C., L. Bilheimer, and D. Gagnon. 2006. Health policy roundtable: Producing and adapting research syntheses for use by health-system managers and public policymakers. Health Research and Education Trust 41(3):905-918.
Commission on Social Determinants of Health. 2008. Closing the Gap in a Generation. Geneva, Switzerland: World Health Organization.
Commision on the U.S. Federal Leadership in Health and Medicine. 2009. New Horizons for a Healthy America: Recommendations to the New Administration. Washington, DC: Center for the Study of the Presidency and Congress.
Communities Count. 2008. Natural and built environments. In Communities Count 2008: Social and Health Indicators Across King County. Seattle, WA: Communities Count. Pp. 90-106.
Cubbin, C., V. Pedregon, S. Egerter, and P. Braveman. 2008. Where We Live Matters for Our Health: Neighborhoods and Health. Princeton, NJ: Robert Wood Johnson Foundation.
Dalla Valle, J. M. 1937. Some factors which affect the relationship between housing and health. Public Health Reports 52(30):989.
Desai, A., and M.-B. You. 1992. Policy implications from an evaluation of seat belt use regulation. Evaluation Review 16(3):247-265.
Diller, P. A., and S. Graff. 2011. Regulating food retail for obesity prevention: How far can cities go? Journal of Law, Medicine & Ethics 39:89-93.
Emerson, J., T. Freundlich, and S. Berenbach. 2008. Triple-bottom line investing: Balancing financial, social and environmental returns. Community Investments–The Green Issue 20(2):17-20. http://www.frbsf.org/publications/community/investments/0808/summer_2008.pdf (April 8, 2011).
EPA (Environmental Protection Agency). 2011. HUD-DOT-EPA Interagency Partnership for Sustainable Communities. http://www.epa.gov/smartgrowth/partnership/index.html#background (September 8, 2010).
Erickson, D., and J. S. Marks. 2011. The Federal Reserve wants to rebuild main street. In The Health Care Blog. http://thehealthcareblog.com/blog/2010/08/16/the-federal-reservewants-to-rebuild-main-street/ (April 7, 2011).
Evans, G. W., and P. Kim. 2010. Multiple risk exposure as a potential explanatory mechanism for the socioeconomic status—health gradient. Annals of the New York Academy of Sciences 1186(1):174-189.
Evans, W. D., and J. D. Graham. 1990. An estimate of the lifesaving benefit of child restraint use legislations. Journal of Health Economics 9:121-142.
Fawcett, S., J. Schultz, J. Watson-Thompson, M. Fox, and R. Bremby. 2010. Building multisectoral partnerships for population health and health equity. Preventing Chronic Disease Public Health Research, Practice, and Policy 7(6):A118-A124.
Fawcett, S. B., V. T. Francisco, A. Paine-Andrews, and J. A. Schultz. 2000. A model memorandum of collaboration: A proposal. Public Health Reports 115(2-3):174-179.
Finkelstein, E. A., C. J. Ruhm, and K. M. Kosa. 2005. Economic causes and consequences of obesity. Annual Review of Public Health 26(1):239-257.
Federal Reserve Bank of San Francisco (FRBSF). 2010. Community Investments Online. http://www.frbsf.org/publications/community/investments/1012/index.html (April 8, 2011).
Garcia, R., and A. White. 2006. Healthy Parks, Schools, and Communities: Mapping Green Access and Equity for the Los Angeles Region: Policy Report. Los Angeles, CA The City Project.
Georgia Health Policy Center. 2008. Finding the Voice of Public Health in the National Health Reform Dialogue: An Integrative Model for Health System Transformation. Atlanta, GA: Georgia State University.
Goetzel, R. Z., D. R. Anderson, R. W. Whitmer, R. J. Ozminkowski, R. L. Dunn, J. Wasserman, and The Health Enhancement Research Organization Research Committee. 1998. The relationship between modifiable health risks and health care expenditures: An analysis of the multi-employer hero health risk and cost database. Journal of Occupational and Environmental Medicine 40(10):843-854.
Gostin, L. O. 2010. Healthy people, healthy places: How to have a healthy life, commmunity, and country. Insights on Law and Society 11(1):12-30.
Guerin, D., and D. P. MacKinnon. 1985. An assessment of the California child passenger restraint requirement. American Journal of Public Health 75(2):142-144.
Harvie, A., and T. A. Wise. 2009. Sweetening the pot: Implicit subsidies to corn sweeteners and the U.S. obesity epidemic. Global Development and Environment Insititute. Policy Brief No. 09-01. Medford, MA: Tufts University.
Health Impact Assessment Collaborative-San Francisco Bay Area. 2010. Case Studies. http://www.hiacollaborative.org/case-studies (April 8, 2011).
Health Impact Project. 2010. About Health Impact Assessment. http://www.healthimpactproject.org/hia (February 17, 2010).
Health In All Policies Task Force. 2010a. About Us. http://sgc.ca.gov/HIAP/about.html (April 8, 2011).
Health In All Policies Task Force. 2010b. Health In All Policies Task Force: Final Report to the Strategic Growth Council. Sacramento, CA: Strategic Growth Council.
HHS (Department of Health and Human Services). 2010. Healthy Food Financing Initiative. http://www.acf.hhs.gov/programs/ocs/ocs_food.html (May 31, 2011).
Innvaer, S., G. Vist, M. Trommald, and A. Oxman. 2002. Health policy-makers’ perceptions of their use of evidence: A systematic review. Journal of Health Services Research Policy 7(4):239-244.
IOM (Institute of Medicine). 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press.
IOM. 2003. The Future of The Public’s Health in the 21st Century. Washington, DC: The National Academies Press.
IOM. 2004. Firearms and Violence: A Critical Review. Washington, DC: The National Academies Press.
IOM. 2007. Ending the Tobacco Problem: A Blueprint for the Nation. Washington, DC: The National Academies Press.
IOM 2010. Transcript, Sixth Meeting of the Institute of Medicine Committee on Public Health Strategies to Improve Health. Washington, DC: IOM
IOM. 2011. For the Public’s Health: The Role of Measurement in Action and Accountability. Washington, DC: National Academies Press.
Jacobs, D. E., and A. Baeder. 2009. Housing Interventions and Health: A Review of the Evidence. Columbia, MD: National Center for Healthy Housing.
Jewell, C. J., and L. A. Bero. 2008. “Developing good taste in evidence”: Facilitators of and hinderances to evidence-informed health policy making in state government. The Milbank Quarterly 86(2):177-208.
Juster, H. R., B. R. Loomis, T. M. Hinman, M. C. Farrelly, A. Hyland, U. E. Bauer, and G. S. Birkhead. 2007. Declines in hospital admissions for acute myocardial infarction in New York State after implementation of a comprehensive smoking ban. American Journal of Public Health 97(11):2035-2039.
Kawachi, I., N. E. Adler, and W. H. Dow. 2010. Money, schooling, and health: Mechanisms and causal evidence. Annals of the New York Academy of Sciences 1186(1):56-68.
Kegler, M. C., J. E. Painter, J. M. Twiss, R. Aronson, and B. L. Norton. 2009. Evaluation findings on community participation in the California Healthy Cities and Communities Program. Health Promotion International 24(4):300-310.
Kelly, J. J. 2004. Refreshing the heart of the city: Vacant building receivership as a tool for neighborhood revitalization and community empowerment. Journal of Affordable Housing 13(2):210-238.
Kemm, J. 2006. Health impact assessment and health in all policies. In Health In All Policies: Prospects and Potentials, edited by T. Stahl, M. Wismar, E. Ollila, E. Lahtinen, and K. Leppo. Finland: Finnish Ministry of Social Affairs and Health and Health and European Observatory on Health Systems and Policies. Pp. 189-207.
Kickbusch, I., and K. Buckett, eds. 2010. Implementing Health In All Policies: Adelaide 2010. Adelaide, South Australia: Department of Health, Government of South Australia.
Kindig, D. A. 2010. Can we afford to wait for better evidence on improving child health? In Improving Population Health: Policy. Practice. Research: University of Wisconsin.
Krieger, J., and D. L. Higgins. 2002. Housing and health: Time again for public health action. American Journal of Public Health 92(5):758-768.
Levy, D. T., J. E. Bauer, and H.-R. Lee. 2006. Simulation modeling and tobacco control: Creating more robust public health policies. American Journal of Public Health 96(3):494-498.
Lovasi, G. S., M. A. Hutson, M. Guerra, and K. M. Neckerman. 2009. Built environments and obesity in disadvantaged populations. Epidemiologic Reviews 31(1):7-20.
Mair, J. S., M. W. Pierce, and S. P. Teret. 2005. The Use of Zoning to Restrict Fast Food Outlets: A Potential Strategy to Combat Obesity. Baltimore, MD, and Washington, DC: The Center for Law and the Public’s Health at Johns Hopkins and Georgetown Universities.
Margolis, L. H., A. C. Wagenaar, and W. Liu. 1988. The effects of a mandatory child restraint law on injuries requiring hospitalization. American Journal of Diseases in Children 142:1099-1103.
Marmot, M., and R. G. Wilkinson, eds. 1999. Social Determinants of Health. Oxford, UK: Oxford Press.
Marmot, M. G., and R. G. Bell. 2011. Improving health: Social determinants and personal choice. American Journal of Preventive Medicine 40(1 Suppl):s73-s77.
Marmot, M. G., S. Stansfeld, C. Patel, F. North, J. Head, I. White, E. Brunner, A. Feeney, and G. D. Smith. 1991. Health inequalities among British civil servants: The Whitehall ii study. The Lancet 337(8754):1387-1393.
Marmot, M. G., H. Bosma, H. Hemingway, E. Brunner, and S. Stansfeld. 1997. Contribution of job control and other risk factors to social variations in coronary heart disease incidence. The Lancet 350(9073):235-239.
Mays, G. P., P. K. Halverson, E. L. Baker, R. Stevens, and J. J. Vann. 2004. Availability and perceived effectiveness of public health activities in the nation’s most populous communities. American Journal of Public Health 94(6):1019-1026.
McCann, B., L. McRee, S. L. Handy, E. Meharg, L. Bailey, and R. Ewing. 2009. The Regional Response to Federal Funding for Bicycle and Pedestrian Projects. Davis, CA: Institute of Transportation Studies, University of California, Davis.
McMichael, A. J., M. Neira, R. Bertollini, D. Campbell-Lendrum, and S. Hales. 2009. Climate change: A time of need and opportunity for the health sector. Lancet 36(9):62031-62036.
McPherson Planning Local Redevelopment Authority. 2006. McPherson Planning LRA. http://www.mcphersonredevelopment.com/planning_lra.html.
Miech, R. A., J. Kim, C. McConnell, and R. F. Hamman. 2009. A growing disparity in diabetes-related mortality: U.S. trends, 1989-2005. American Journal of Preventive Medicine 36(2):126-132.
Muennig, P. 2008. Health selection vs. causation in the income gradient: What can we learn from graphical trends? Journal of Health Care for the Poor and Underserved 19:574-579.
NPLAN (National Policy & Legal Analysis Network to Prevent Childhood Obesity). 2010. Establishing Land Use Protections for Community Gardens. Oakland, CA: NPLAN.
Ollila, E., E. Lahtinen, T. Melkas, M. Wismar, T. Stahl, and K. Leppo. 2006. Towards a healthier future. In Health In All Policies: Prospects and Potentials, edited by T. Stahl, M. Wismar, E. Ollila, E. Lahtinen and K. Leppo. Finland: Finnish Ministry of Social Affairs and Health and European Observatory on Health Systems and Policies. Pp. 269-279.
Piot, P., D. E. Bloom, and P. C. Smith. 2010. Towards a New Paradigm for Health for All. Geneva, Switzerland: World Economic Forum.
PolicyLink. 2010. A Healthy Food Financing Initiative: An Innovative Approach to Improve Health and Spark Economic Development. Oakland, CA: PolicyLink.
Pomeranz, J. 2011. The unique authority of state and local health departments to address obesity. American Journal Public Health:e1-e6, http://ajph.aphapublications.org/cgi/content/abstract/AJPH.2010.300023v1 (May 12, 2011).
Popkin, S. J., B. Theodos, L. Getsinger, and J. Parilla. 2010. An Overview of the Chicago Family Case Management Demonstration. Washington, DC: The Urban Institute.
Preusser, D. F., A. F. Williams, and A. K. Lund. 1987. The effect of New York’s seat belt use law on teenage drivers. Accident Analysis & Prevention 19(2):73-80.
Puska, P. 2008. The North Karelia project: 30 years successfully preventing chronic diseases. Diabetes Voice 53:26-29.
Puska, P., and T. Ståhl. 2010. Health In All Policies—the Finnish initiative: Background, principles, and current issues. Annual Review of Public Health 31(1):315-328.
Richter, L. 2009. Prescription for healthy communities: Community development finance. Community Development Investment Review—Federal Reserve of San Fransisco 5(3):14-42.
Rock, S. M. 1996. Impact of the Illinois Child Passenger Protection Act: A retrospective look. Accident Analysis & Prevention 28(4):487-492.
Sargent, R. P., R. M. Shepard, and S. A. Glantz. 2004. Reduced incidence of admissions for myocardial infarction associated with public smoking ban: Before and after study. British Medical Journal 328(7446):977-980.
Schmier, J. K., M. L. Jones, and M. T. Halpern. 2006. Cost of obesity in the workplace. Scandinavian Journal of Work, Environment & Health 32(1):5-11.
Schroeder, S. A., and D. L. Hughes. 2008. An agenda to improve the health of the public In The Health Care Delivery System: A Blueprint for Reform. Washington DC: Center for American Progress. Pp. 96-111.
Seekins, T., S. B. Fawcett, S. H. Cohen, J. P. Elder, L. A. Jason, J. F. Schnelle, and R. A. Winett. 1988. Experimental evaluation of public policy: The case of state legislation for child passenger safety. Journal of Applied Behavior Analysis 21(3):233-243.
Sewell, C. M., H. F. Hull, J. Fenner, H. Graff, and J. Pine. 1986. Child restraint law effects on motor vehicle accident fatalities and injuries: The New Mexico experience. Pediatrics 78(6):1079-1084.
Sihto, M., E. Ollila, and M. Koivusalo. 2006. Principles and challenges of health in all policies. In Health In All Policies: Prospects and Potentials, edited by T. Stahl, M. Wismar, E. Ollila, E. Lahtinen, and K. Leppo. Finland: Finnish Ministry of Social Affairs and Health and European Observatory on Health Systems and Policies. Pp. 3-20.
Simon, P., C. J. Jarosz, T. Kuo, and J. E. Fielding. 2008. Menu Labeling as a Potential Strategy for Combating the Obesity Epidemic: A Health Impact Assessment (HIA). Los Angeles, CA: Los Angeles County Department of Public Health.
Sorian, R., and T. Baugh. 2002. Power of information: Closing the gap between research and policy. Health Affairs 21(2):264-273.
Streff, F. M., A. C. Wagenaar, and R. H. Schultz. 1990. Reductions in police-reported injuries associated with Michigan’s safety belt law. Journal of Safety Research 21(1):9-18.
Sturm, R., L. M. Powell, J. F. Chriqui, and F. J. Chaloupka. 2010. Soda taxes, soft drink consumption, and children’s body mass index. Health Affairs 29(5):1052-1058.
Syme, S. L., and M. L. Ritterman. 2009. The importance of community development for health and well-being. Community Development Investment Review 5(3):1-13.
The Marmot Review. 2010. Fair Society, Health Lives: Strategic Review of Health Inequalities in England Post 2010. London, UK: The Marmot Review.
The Reinvestment Fund. 2008. The economic impacts of supermarkets on their surrounding communities. Reinvestment Brief 4:1-18.
The Urban Institute. 2010. An Overview of the Chicago Family Case Management Demonstration. http://www.urban.org/publications/412254.html (April 8, 2011).
Thyer, B. A., and M. Robertson. 1993. An initial evaluation of the Georgia safety belt use law. Environment and Behavior 25(3):506-513.
TRB (Trasportation Research Board) and IOM (Institute of Medicine). 2005. Does the Built Environment Influence Physical Activity? Examining the Evidence—Special Report 282. Washington, DC: The National Academies Press.
Twiss, J. M., J. Dickinson, S. Duma, T. Kleinman, H. Paulsen, and L. Rilveria. 2003. Community gardens: Lessons learned from California healthy cities and communities. American Journal of Public Health 93(9):1435-1438.
Ulmer, R. G., C. W. Preusser, D. F. Preusser, and L. A. Cosgrove. 1995. Evaluation of California’s safety belt law change from secondary to primary enforcement. Journal of Safety Research 26(4):213-220.
Wagenaar, A. C., D. W. Webster, and R. G. Maybee. 1987a. Effects of child restraint laws on traffic fatalities in eleven states. The Journal of Trauma 27(7):726-732.
Wagenaar, A. C., R. G. Maybee, and K. P. Sullivan. 1987b. Michigan’s Compulsory Restraint Use Policies: Effects on Injuries and Deaths. Ann Arbor, MI: University of Michigan Transportation Research Institute.
Wallinga, D. 2010. Agricultural policy and childhood obesity: A food systems and public health commentary. Health Affairs 29(3):405-410.
Wang, Y., M. A. Beydoun, L. Liang, B. Caballero, and S. K. Kumanyika. 2008. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity 16(10):2323-2330.
WHO. 2009. WHO Global Network of Age-Friendly Cities, edited by WHO. Geneva, Switerland.
Wier, M., C. Sciammas, E. Seto, R. Bhatia, and T. Rivard. 2009. Health, traffic, and environmental justice: Collaborative research and community action in San Francisco, California. American Journal of Public Health 99(Suppl 3):s499-s504.
Williams, A. F., and J. K. Wells. 1981. Evaluation of the Rhode Island child restraint law. American Journal of Public Health 71(7):742-743.
Wolf, A. M., and G. A. Colditz. 1998. Current estimates of the economic cost of obesity in the United States. Obesity Research 6(2):97-106.
Woolf, S. H., R. E. Johnson, R. L. Phillips, Jr., and M. Philipsen. 2007. Giving everyone the health of the educated: An examination of whether social change would save more lives than medical advances. American Journal of Public Health 97(4):679-683.
World Economic Forum. 2008. Working Towards Wellness: The Business Rationale. Geneva, Switzerland: World Economic Forum.






































