2
Setting the Stage for the Coexistence of Food Insecurity and Obesity
|
Key Messages Noted by Participants
|
During the first session of the workshop, three speakers provided an overview of the issues associated with food insecurity and obesity. They explored the relationship between food insecurity and obesity, in both chil-
dren and adults, and differences that exist by gender, age, and race/ethnicity. They provided an introduction to many of the issues discussed during the remainder of the workshop, including the relationship of food insecurity to stress, the relationship between food insecurity and health outcomes, and the role of the Supplemental Nutrition Assistance Program (SNAP) and other federal nutrition assistance programs. The speakers also suggested future research directions. Box 2-1 defines a number of terms related to food insecurity that were discussed during the workshop.
The literature on this relationship is “really mixed,” said Mary Story, professor and associate dean at the University of Minnesota School of Public Health, who moderated the session. Some studies show that there is a positive association between food insecurity and obesity; others do not. What accounts for this discrepancy, Story asked, and what are the strengths and limitations of the current research?
PREVALENCE AND MEASUREMENT OF FOOD INSECURITY
Food security exists when “people at all times have physical, social, and economic access to sufficient, safe, and nutritious food which meets their dietary needs and food preferences for an active and healthy life” (FAO, 1996). The U.S. Department of Agriculture (USDA) monitors food security as an ongoing measure of the effectiveness of federal nutrition assistance programs, private food assistance programs, and other public-private initiatives in reducing the food insecurity of low-income households. “Food insufficiency” and “food insecurity” are related but distinct concepts. Food insufficiency is defined as an inadequate amount of food intake due to a lack of resources (Briefel and Woteki, 1992). Food insecurity is the ability to access sufficient, safe, and nutritious foods in socially acceptable ways (FAO, 1996). Food insecurity describes a “broader condition” that includes food insufficiency and additionally psychological and other qualitative aspects of the food supply and food intake (Casey et al., 2001).
Prevalence of Food Insecurity
Prior to 2008, food insecurity for all households in the United States hovered between 10 and 12 percent, with a higher prevalence among Latino and African-American households (Figure 2-1). The prevalence, however, increased sharply in 2008 to almost 15 percent, with the most recent measures showing a continuation of that high level (Nord et al., 2010). “The economic downturn has had an impact on food insecurity,” said Barbara Laraia, associate professor in the Department of Medicine at the University of California at San Francisco.
|
BOX 2-1 Food Security Definitions Food security Access to enough food for an active, healthy life; at minimum, includes (1) the ready availability of nutritionally adequate and safe foods and (2) an ensured ability to acquire acceptable foods in socially acceptable ways (NRC, 2006). High food security Households that report no indicators of food insecurity on the U.S. Department of Agriculture (USDA) survey (Nord et al., 2010). Households had no problems, or anxiety about, consistently accessing adequate food.a Marginal food security Households reporting one to two indicators of food insecurity on the USDA survey (Nord et al., 2010). Households had problems at times, or anxiety about, accessing adequate food, but the quality, variety, and quantity of their food intake were not substantially reduced.a Low food security A range of food insecurity in which households report multiple indications of food access problems, but typically report few, if any, indications of reduced food intake on the USDA survey (Nord et al., 2010). Households reduced the quality, variety, and desirability of their diets, but the quantity of food intake and normal eating patterns were not substantially disrupted. Prior to 2006, USDA described households with low food security as “food insecure without hunger.”a Very low food security A severe range of food insecurity on the USDA survey in which the food intake of some household members was reduced and normal eating patterns were disrupted because of limited resources. At times during the year, eating patterns of one or more household members were disrupted and food intake reduced because the household lacked money and other resources for food. Prior to 2006, USDA described households with very low food security as “food insecure with hunger” (Nord et al, 2010).a Food insecurity Limited or uncertain ability to acquire acceptable foods in socially acceptable ways (Anderson, 1990). Food insufficiency An inadequate amount of food intake due to a lack of resources (Briefel and Woteki, 1992). Hunger The uneasy or painful sensation caused by a lack of food; the recurrent and involuntary lack of food (NRC, 2006). |
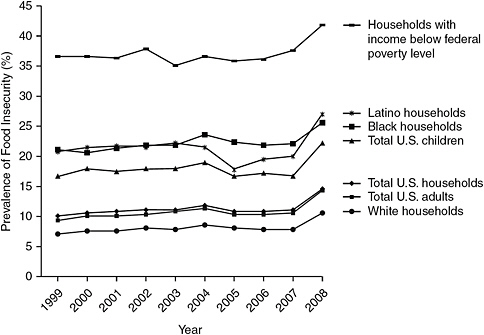
FIGURE 2-1 Prevalence of food insecurity in the United States, 1999-2008.
NOTE: Data are from the USDA food security reports, which are based on an annual survey conducted by the U.S. Census Bureau as a supplement to the monthly Current Population Survey.
SOURCE: Seligman and Schillinger, 2010. Hunger and socioeconomic disparities in chronic disease. New England Journal of Medicine 363(1):6-9. Copyright © 2010 Massachusetts Medical Society.
Measuring Food Insecurity
Craig Gundersen, associate professor in the Department of Agricultural and Consumer Economics at the University of Illinois at Urbana-Champaign, briefly described the tool used to determine food insecurity in the United States. A household’s food insecurity status is calculated from responses to a series of questions in the Core Food Security Module (CFSM), which ask about conditions and behaviors known to characterize households having difficulty meeting basic food needs (Nord et al., 2010); these methods have been described by Hamilton and colleagues (1997) as well as others. The following are example questions from the CFSM:
-
Did you worry whether your food would run out before you got money to buy more?
-
Did you or the other adults in your household ever cut the size of your meals or skip meals because there wasn’t enough money for food?
-
Were you ever hungry but did not eat because you couldn’t afford enough food?
-
Did a child in the household ever not eat for a full day because you couldn’t afford enough food?
The CFSM has a total of 18 questions. Ten items are asked of all households, and 8 additional questions are asked of only households with children. Responses to these questions are used to assign households to food security categories. Households are classified as food insecure (having low food security) if they have affirmative responses to three or more of the CFSM questions. Households are further classified into “very low food security” based on the presence or absence of children in the household. Households are classified as having “very low food security” if they have 6 or more affirmative responses in households without children or 10 or more affirmative responses in households with children.
THE RELATIONSHIP BETWEEN FOOD INSECURITY AND OBESITY
Gundersen emphasized the importance of using measures of obesity collected by trained personnel when examining the relationship between food insecurity and obesity. The definition of obesity and other terms used to classify weight status are in Box 2-2. For example, a paper by Lyons et al. (2007) found a connection between food insecurity and obesity when self-reports of weight status were used. However, when body mass index (BMI) was calculated using measured weight and height, there was no relationship. Because of such discrepancies, Gundersen limited his comments to papers that used trained personnel to measure obesity because measured values are more accurate than self-reported data. Gundersen also only included papers that used the CFSM as a measure of food insecurity and excluded from consideration papers focusing on children under the age of 2 years because of challenges associated with measuring obesity at such young ages.
Children
Gundersen et al. (2009a) did not find a relationship between food in-security and childhood obesity in a cross-sectional study that used multiple measures of obesity and a sample of children from the 1999-2002 National Health and Nutrition Examination Survey (NHANES). The sample was confined to children below 200 percent of the poverty line, which, according to the authors, captures the majority of households experiencing food insecurity. In separate analyses of boys, girls, and racial/ethnic groups (non-Hispanic white, non-Hispanic black, and Hispanic), no relationship
|
BOX 2-2 Definitions of Terms Used to Classify Weight Status Body Mass Index (BMI) An indirect measure of body fat, calculated as the ratio of a person’s body weight (in kilograms) to the square of a person’s height (in meters): BMI (kg/m2) = weight (kilograms) ÷ height (meters2) BMI (lb/in2) = weight (pounds) ÷ height (inches2) × 703 Overweight For adults 20 years of age and older, a BMI between 25.0-29.9 is considered overweight. For children and youth ages 2-19, BMI is based on growth charts for age and gender and is referred to as BMI-for-age, which is used to assess underweight, overweight, and risk for overweight. According to the Centers for Disease Control and Prevention, a child with a BMI-for-age that is equal to or between the 85th and 95th percentiles is overweight. Obese For adults 20 years of age and older, a BMI ≥ 30 is obese. For children and youth ages 2-19, a child with a BMI-for-age that is ≥ the 95th percentile, on the growth charts as explained above, is considered obese. |
was found. This study used “state-of-the-art data, state-of-the-art methods of measuring obesity, and there’s no relationship between food insecurity and obesity [in children],” Gundersen said.
Another study looked at how the effects of food insecurity differ over time (Bhargava et al., 2008). Using 1999-2003 data from the Early Childhood Longitudinal Study, BMI as a measure of obesity, and a dynamic random effects model that controls for unobserved factors, the study found no effect of food insecurity on BMI. It is “another paper showing no effect using state-of-the-art methods,” said Gundersen.
In response to the question of whether children in food-insecure households are more likely to be obese, Gundersen’s answer was “probably not” for children as a whole. Published studies such as Larson and Story (2010) provide support for this conclusion, but Gundersen said he would answer with an even more emphatic “no” if unpublished studies were taken into account. Gundersen underscored the importance of publication bias—explaining that the authors of studies that find no relationship are less likely to submit their work for publication. This bias against publishing statistically insignificant results leads to a lack of published confirmation of the absence of a relationship between food insecurity and obesity in children.
Counterfactuals
Gundersen examined the use of “counterfactuals” in obesity research, involving such questions as the effects on obesity of making all food-insecure households food secure. The problem with such exercises is that it is impossible to measure the potential effect of food insecurity on obesity for food-secure children or the potential effect of food security on obesity for food-insecure children. “We don’t observe the counterfactual. You only observe a food-insecure child…. You don’t observe a food-insecure child who’s food secure, and vice versa.” For this reason, it is not possible to measure accurately the effects on obesity of making everyone in society food secure or food insecure (Gundersen and Kreider, 2009).
Adults
Laraia summarized the documentation of the association between household food insecurity and weight status among adults, based on a large research literature (Olson, 1999; Townsend et al., 2001; Adams et al., 2003; VanEenwyk and Sabel, 2003; Vozoris and Tarasuk, 2003; Kaiser et al., 2004; Laraia et al., 2004; Jones and Frongillo, 2006, 2007; Wilde and Peterman, 2006; Hanson et al., 2007; Whitaker and Sarin, 2007). Among many groups there is no association, but there are positive or negative associations for other groups (Figure 2-2). There was a modest association
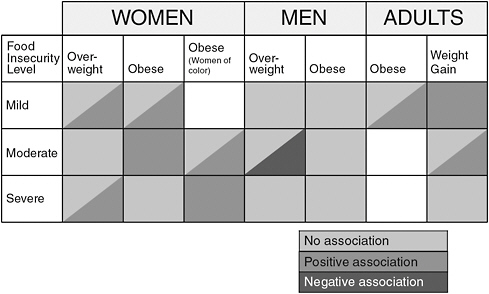
FIGURE 2-2 Summary of findings for food insecurity and weight status.
SOURCE: Laraia, 2010.
between food insecurity and obesity among women, especially women of color, that is, women who were food insecure were more likely to be obese than women who were food secure. Among men there was either a negative or a null association between food insecurity status and overweight and a null association with obesity. For men undergoing a mild or moderate amount of food insecurity there was a significant negative association, i.e., men who were food insecure were less likely to be overweight than men who were food secure.
Laraia also discussed studies of pregnancy in which one study found higher weight gain among women from food-insecure households and a greater risk of gestational diabetes (Laraia, 2010). Another prospective study found that obese rural childbearing women were more likely to become food insecure over time (Olson and Strawderman, 2008).
OTHER IMPLICATIONS OF FOOD INSECURITY
Poverty
The definition of food insecurity has an economic component through material deprivation, said Laraia. Thus, food insecurity is a sensitive measure of the stresses that families are under, she continued, although it is not necessarily specific.
Laraia explained that food insecurity is not the same as poverty. For households with incomes below the federal poverty level, the prevalence of food insecurity was between 35 and 40 percent for most of the past decade, with an increase since 2008. Some households below the poverty level are not food insecure, and some households well above the poverty line are food insecure. Factors such as a job loss, divorce, or other unexpected events that are not captured by an annual income measure could affect a household’s food security status. Furthermore, some households experience food insecurity episodically, even though their annual incomes are well above the poverty line (Nord et al., 2010).
Diet Quality
The definition of food insecurity also has a nutritional component, reflecting a compromise between food quality and food quantity, Laraia said. Little research to date has found a clear association among diet variety, diet quality, meal patterns, or nutrient intake, added Laraia. She noted examples of research examining these issues:
-
Drewnowski and Specter (2004) showed that energy-dense foods are much less expensive than nutrient-dense foods. Under stress, people are often drawn to energy-dense foods, Laraia noted.
-
Individuals from households that are food insecure have slightly lower average scores on indices of healthful eating compared to individuals in food-secure households (Basiotis and Lino, 2002).
-
Another study observed that there was no significant difference in total energy intake when comparing adults (ages 20-59) from food-insufficient to food-sufficient families, but there were lower intakes of calcium in that group of adults from food-insecure families. Older adults (> 60 years) from food-insufficient families had both lower intakes of calories and several micronutrients (i.e., vitamin B6, magnesium, iron, and zinc) compared to their food-sufficient counterparts (Dixon, 2001).
Negative Health Outcomes
Food insecurity is associated with numerous negative health outcomes, said Gundersen, citing a large number of studies showing a relationship between food insecurity and various health outcomes (Jyoti et al., 2005; Slack and Yoo, 2005; Cook et al., 2006; Skalicky et al., 2006; Whitaker et al., 2006; Chilton and Booth, 2007; Rose-Jacobs et al., 2008; Eicher-Miller et al., 2009; Gundersen and Kreider, 2009; Hernandez and Jacknowitz, 2009; Yoo et al., 2009; Zaslow et al., 2009; Kirkpatrick et al., 2010). “Food insecurity is one of the most important public health threats in the United States,” he said. “It has serious negative health consequences.” This observation alone argues for devoting resources to alleviating food insecurity in the United States.
Diet-Sensitive Chronic Disease
An association between food insecurity and diet-sensitive chronic disease has been observed. Seligman et al. (2010) found a modest association between food insecurity, hypertension, and hyperlipidemia and less of an association with diabetes. When the authors restricted their data to households with very low food security, they found more than a twofold increase in the risk of diabetes compared to those in food-secure households. Adults with diabetes in food-insecure households also exhibited higher hemoglobin A1c values than adults living in food-secure households, suggesting that food-insecure adults are not managing their disease well through their diets.
Stress
Numerous studies have shown an association between food insecurity and mental well-being, stress, and depression, Laraia said. The concept of household food insecurity is multidimensional, she said, and its definition captures the psychological effects that food insecurity might have in households.
Food insecurity is very stressful to families, Gundersen pointed out. Food insecurity may interact with stress to foster obesity. For example, Lohman et al. (2009) found that increased levels of individual stressors led to an increased probability of obesity and that food-insecure adolescents between 10 and 15 years of age whose mothers experience stress were more likely to be obese. In contrast, another study found that younger food-secure children (under the age of 10 years) in families below 200 percent of the poverty line were more likely to be obese (Gundersen et al., 2008). In this case, Gundersen said, children who experience stress may eat comfort foods to make themselves feel better, and they are more likely to have food readily available if they belong to food-secure families.
The emerging research on stress is provocative and important but also complicated, noted Laraia. Under stressful conditions where humans or animal subjects are threatened, they tend to lose weight. However, even with a loss of weight, fat is redistributed into the viscera, becoming abdominal fat, which is more likely to produce adverse health effects than other kinds of fat because of its increased metabolic activity and its proximity to visceral organs, she said (Adam and Epel, 2007).
Food insecurity is a form of threat to humans, said Laraia. It can stimulate the hypothalamus-pituitary-adrenal (HPA) axis, which is a stress feedback mechanism that ultimately influences metabolic outcomes. In this way, stress can trigger hunger and an increased drive for feeding. Eating in the presence of stress also can lead to insulin resistance and visceral fat accumulation, and it can create a desire for palatable foods, because the high fat content of these foods dampens the stress response (Adam and Epel, 2007). “It feels good psychologically, emotionally, [and] biologically.”
In a study of pregnant women, stress, anxiety, depression, and other measures of distress were higher among women from marginally secure and food-insecure households, while measures of self-esteem and mastery decreased as food insecurity increased (Laraia et al., 2006). Furthermore, women who scored high in dietary restraint—measured by dieting, restrained eating to regulate weight, and a history of weight cycling—who were from food-insecure households gained the greatest amount of weight on average during the gestational period. These women also had a higher ratio of observed-to-recommended weight gain than did other women.
Animal models have been used to study stress. In most cases, animals under stress lose weight. However, in mice fed different kinds of foods and put under different amounts of stress, the mice under stress and fed a diet high in fat and sugar developed the most abdominal fat. Mice subjected to swimming in lukewarm water for an hour did not experience fat accumulation, while mice subjected to stress by swimming in ice-cold freezing water for an hour or placed in a cage with an aggressive male mouse for 10 minutes did experience fat accumulation (Kuo et al., 2007).
Regarding biochemical changes and stress, mice subjected to stress and fed a diet high in fat and sugar had increased levels of insulin and neuropeptide Y, two factors that regulate energy. Neuropeptide Y, in addition to serving as an energy regulator, causes a drive to eat, increases the likelihood of sedentary behavior, and shunts energy to be stored as abdominal fat. After 4 months of stress and the diet high in fat and sugar, the mice had full-blown metabolic syndrome. Yet when the researchers blocked neuropeptide Y, they saw no fat accumulation (Kuo et al., 2007). This “ties together the energy regulation path and the stress path,” said Laraia.
Another line of animal research involves macaque monkeys and the variable foraging demand protocol. In this 16-week protocol, mother monkeys alternated 2-week periods in which food was relatively easy to obtain (low foraging demand) or more difficult to obtain (high foraging demand). The difficulty of the foraging demand was varied through the use of a foraging cart, a device in which food can be hidden in differing amounts of wood chip, with openings on the side of the cart through which the mother monkeys search. Coplan and colleagues (2006) found that when nursing mothers were exposed to variable foraging, there was no change in levels of maternal corticotropin-releasing factor, which is another factor in the HPA axis. However, when their infants were being weaned, variable foraging caused an increase in maternal corticotropin-releasing factor, indicating a higher stress response. In both cases, the corticotropin-releasing factor of the infant monkeys increased. “There was a stress response in the infant even though there was no calorie restriction, and it was the stress response of not knowing whether they were going to get their food during those intermittent periods of foraging.”
Kaufman and colleagues (2007) extended the research on late variable foraging. If mothers were subjected to variable foraging while weaning their offspring, the adolescent monkeys had higher weight, increased BMI, and greater abdominal circumference. This research concluded that “early-life stress during a critical period of neurodevelopment can result in the peripubertal emergence of obesity and insulin resistance,” said Laraia.
POLICY IMPLICATIONS
Would reductions in poverty lead to reductions in childhood obesity? Gundersen asked. Absolutely yes, he said, citing a variety of research results (Miech et al., 2006; Phipps et al., 2006; Shrewsbury and Wardle, 2008; Singh et al., 2008). “If we got rid of poverty, we’d definitely make a huge dent in the level of obesity in the country.” More importantly, poverty is a very serious problem in the United States, and “eliminating it would be good in and of itself.”
An increasing amount of work has convincingly demonstrated that reducing stress also would lead to reductions in childhood obesity (Sweeting et al., 2005; Crossman et al., 2006; Gibson et al., 2007; Zeller et al., 2007; Koch et al., 2008; Garasky et al., 2009; Van Jaarsveld et al., 2009; Stenhammar et al., 2010). Yet would reducing food insecurity lead to reductions in childhood obesity? No, replied Gundersen. There are many reasons for eliminating food insecurity, but reducing obesity is not one of those reasons. “We should eliminate food insecurity for other reasons.”
SNAP has been extraordinarily effective in alleviating food insecurity and poverty (Gundersen and Oliveira, 2001; Van Hook and Balistreri, 2006; Gundersen and Kreider, 2008; DePolt et al., 2009; Gundersen et al., 2009b; Nord and Golla, 2009). To the extent that SNAP further reduces poverty, it will reduce childhood obesity, Gundersen remarked. However, if its only effect is to reduce food insecurity, according to the existing research, it will not have an effect on obesity. “Without a doubt, SNAP plays a huge role in our efforts in society to relieve obesity because it reduces poverty and because it reduces stress,” said Gundersen. Yet the fact that SNAP leads to reductions in food insecurity will not have an impact on obesity, he concluded.
A RESEARCH AGENDA
Should scarce research dollars be spent on further study of the connection between food insecurity and childhood obesity? Gundersen said no, even though some of his research has been on that very topic. The connection already has been studied extensively, and it is not clear that more research in this area is needed. “It’s not what the conference probably wanted to hear, so I apologize.”
The U.S. government has set a goal to eliminate childhood hunger by 2015.1 In that case, said Gundersen, much more needs to be learned about the determinants of childhood hunger. “We don’t know much about what
|
1 |
See http://obama.3cdn.net/c4b14802fd5e66ee67_xum6bn6nu.pdf (accessed January 26, 2011). |
the determinants of childhood hunger are, outside of some broad sweeping generalizations about it … let’s devote our resources to that.”
The effect of stress among low-income households on childhood obesity warrants further research. Early work suggests that the effects of stress are substantial, but many questions surround the determinants and effects of stress. “Looking more at this is really important,” Gundersen advised. If additional work did demonstrate a connection between food insecurity and obesity, the results of studies on stress would be relevant.
Another important research question, according to Laraia, is whether overweight or obese women perceive their household food situation differently than normal-weight women, which could create a spurious relationship between food insecurity and obesity. Perhaps they are stressed by many things and getting their next meal is first and foremost in their minds, she suggested.
Inconsistencies in measuring both exposures and outcomes also can affect research findings. Studies use different measures for food insecurity and for weight. Some analyses look at the full population, others look only at middle- and low-income households, and others are restricted to very low income households. “We’re trying to tease out only the direct effect of food insecurity when we have this wonderful multidimensional construct that’s capturing probably more than just the food security status in households,” Laraia said.
The conceptual framework of research in this area needs to be better defined and thought through, said Laraia. Perhaps the focus should be on visceral fat instead of BMI or obesity. Categories of obesity and moderators of food insecurity such as dieting need to be considered more carefully. Dieting can be very stressful, as shown both psychologically and from animal and human studies, so dieting itself causes a stress response.
With regard to stress, research should focus on critical periods of growth and development, especially during adolescence and in girls, said Laraia. The aging population and diet-sensitive chronic disease are other important issues. Finally, she recommended that the interaction between food insecurity and the food environment be explored.
Types of Research Studies Needed
A very large proportion of the evidence for both children and adults comes from cross-sectional studies, observed Rafael Pérez-Escamilla, professor of epidemiology and public health at Yale School of Public Health. He agreed with Gundersen that little progress can be expected if more of the same studies are funded. However, prospective, retrospective, experimental, and other types of studies also have the potential to advance knowledge.
Longitudinal Studies
Longitudinal studies are needed to better characterize and understand what happens over the course of the month in low-income households enrolled in food assistance programs, said Pérez-Escamilla. Key questions to be addressed are: Do food purchasing and eating behaviors change during the month? Are these changes explained by the level of food assistance benefits? Do eating behaviors lead to weight cycling during the month?
Longitudinal studies also are needed to understand if maternal depression or infant feeding parenting styles modify the relationship between food insecurity and childhood obesity. As shown by the work of Bronte-Tinkew et al. (2007), complex statistical approaches based on sound theoretical frameworks such as structural equation modeling are needed to disentangle the direct and indirect pathways by which food insecurity may influence childhood obesity. In the research on food insecurity and obesity, it is crucial to model interactive effects to identify key effect modifiers. “Some of the most interesting findings that illustrate the complexity of the pathways that may make these relationships come from those studies that have bothered to look at effect modification,” said Pérez-Escamilla. “This information can provide the evidence base for the design of effective interventions targeting different subgroups.” Examples of key potential effect modifiers are participation in food assistance programs, caregiver stress or depression, social supports, family structure, and child age and gender.
As an example of effect modification, Pérez-Escamilla cited findings from Canada suggesting that birth weight may modify the relationship between food insufficiency and the likelihood of childhood obesity later in life (Dubois et al., 2006). Babies with low birth weight were several times more likely to develop childhood obesity if they lived in a food-insecure household, whereas there was no relationship if a baby was born with a normal birth weight. Babies born heavier than expected for their gestational age also had an increased risk for obesity, though not as high as babies with low birth weight.
Retrospective Studies
Retrospective studies can answer a different set of questions. How do food insecurity experiences early in life shape longer-term eating behaviors? Do such experiences transfer to the next generation? Are caregivers who were food insecure more likely to overfeed their children? Does acculturation modify the relationship between food insecurity and obesity? Does food insecurity modify the relationship between acculturation and obesity? Acculturation is a complex, dynamic, and time-dependent process,
Pérez-Escamilla observed. Methodological advances have yielded ways to measure acculturative changes based on retrospective life history questionnaires, whereas longitudinal studies would take decades to yield similar results.
Experimental Studies
Experimental studies can help answer at least some counterfactual questions, discussed earlier in this chapter. Will reductions of food insecurity lead to decreases in obesity? How can food-insecure households be made food secure? The design of these studies is ethical, Pérez-Escamilla pointed out, because it is not known whether programs such as SNAP have a mitigating, exacerbating, or no effect on the development of obesity among low-income individuals. On the other hand, it would be unethical to probe the other side of the counterfactual, because it would be unethical to make food-secure households food insecure to determine whether obesity increases.
A major question in experimental studies is how to make food-insecure households food secure. For example, is it better to give families food, money, or both? “I am not sure that we really know how to do that. And without this knowledge, it is not possible to test the hypothesis that food insecurity leads to obesity based on experimental designs,” he noted.
Other Considerations for Designing Future Research
Choice of Variables
Most research in this area models obesity as a dependent variable and food insecurity as an independent variable. However, it is also possible that the opposite is true—that obesity leads to food insecurity, perhaps through pathways mediated by depression and chronic disease that limit work performance and the ability to generate a reasonable income. “To my knowledge, there are almost no studies that focus on answering questions related to this direction of the relationship,” said Pérez-Escamilla. If this hypothesis is confirmed, it would indicate that improving access not only to chronic disease management care but also to much-needed mental healthcare services could lead to improvements in food security for entire households.
Measuring Food Insecurity
Practically all studies reviewed have measured household food insecurity using experience-based scales or subscales. These scales have adequate
psychometric, predictive, and concurrent validity in diverse socioeconomic and cultural settings. They also capture information that goes above and beyond traditional poverty measures. Measures of food insecurity and poverty “are not the same,” emphasized Pérez-Escamilla. “If they were the same, we wouldn’t need to be meeting here today, because the relationship between poverty and obesity is fairly well established.”
There are several limitations to be considered with experience-based measures of household food insecurity. First, these measures provide a description of the situation of the household as a unit. They do not necessarily represent the food insecurity of the individuals living in a household. Thus, it is possible that the household food insecurity measure does not always capture accurately the food insecurity of individuals whose anthropometric or body composition data are modeled in regression analyses. Research is needed to better understand if and how food insecurity varies across individuals within a household, Pérez-Escamilla said. Also, he continued, measures of food insecurity need to be more standardized, with the use of similar scales and evidence-based cutoff points.
Some studies simply classify households as either food secure or food insecure, while others divide households into two or three different levels of food insecurity. “I suspect this is mostly [the result of] a post hoc decision after exploring the data [and identifying the ‘best’ food insecurity classification algorithm],” Pérez-Escamilla said.
THE NEED FOR ACTION
Regardless of whether food insecurity is causally linked with obesity, it has been consistently associated with lower dietary quality and especially with a lower consumption of fruits and vegetables. Food insecurity is likely to have many other negative consequences for human development, said Pérez-Escamilla (Dietary Guidelines Advisory Committee, 2010; Pérez-Escamilla, in press). Food insecurity is associated with negative psycho-emotional outcomes for children and adults, poor academic performance, and maternal stress and depression (Pérez-Escamilla, in press). Maternal stress has been associated with childhood obesity and high-energy-density diets characterized by low fruit and vegetable consumption; such diets correlate with both childhood and adult obesity. Given these observations, said Pérez-Escamilla, having a definitive answer to the question at the heart of the workshop is not essential to take action.
Nevertheless, the question being addressed at the workshop remains important because understanding potential pathways by which food insecurity influences obesity may provide opportunities for interventions, said Pérez-Escamilla. This, in turn, can have major implications for the design or redesign of food assistance and nutrition education programs. For example,
if research shows that dietary behaviors leading to obesity result from an abundance of food during some parts of the month but not others, then programs such as SNAP could reconsider the best timing for benefit distribution, he noted. Similarly, if studies confirm that lack of access to fruits and vegetables mediates a relationship between food insecurity and obesity, then programs such as SNAP and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) could continue to develop innovative ways of encouraging SNAP and WIC recipients to purchase more fruits and vegetables with their benefits. “This line of work can have an impact not only on the improvement of food assistance programs but also on the improvement of the vulnerable communities’ food systems as a whole,” Pérez-Escamilla said.
GLOBAL IMPLICATIONS OF THE RELATIONSHIP BETWEEN FOOD INSECURITY AND OBESITY
Pérez-Escamilla observed that the theme of the workshop has global implications. For example, the Mexican conditional cash transfer program known as Oportunidades provides a stipend and complementary food for young children as long as families keep their children in school and bring them to receive immunizations and other primary healthcare services. The Mexican government is investing close to $3 billion annually in the program with the hope of improving the health and nutritional status of the most poor and food insecure in Mexico. Rigorous evaluations have shown that risk of stunting declines among certain subgroups of children as a result of exposure to Oportunidades (Fernald et al., 2009). However, the risk of obesity increases among caregivers (Fernald et al., 2008), illustrating the need to understand how food insecurity and federal nutrition assistance program participation affect different members of the same household. “This principle can be extended to SNAP,” said Pérez-Escamilla, and “to any type of food assistance program in the world.”
GROUP DISCUSSION
Moderator: Mary Story
During the group discussion period, points raised by participants included the following:
Influence of the Life Course
Several questions revolved around associations between food insecurity and obesity for specific age groups. Story pointed out that very few studies
have examined the association among the elderly, where she said that much more research is needed. Gundersen said that in the studies to which he has contributed, no relationship was found in adolescents. Pérez-Escamilla pointed out that the growth rate during infancy is an important predictor of childhood obesity risk and that there are major differences in the way breastfed babies grow. This observation raises several largely unresolved questions about the feeding of infants including the influence of food insecurity on exclusive breastfeeding and the introduction of complementary foods before the recommended 6 months of age. There are very few studies that examine food insecurity and breastfeeding behaviors, noted Pérez-Escamilla. One study in Africa demonstrated that women who are food insecure are less likely to breastfeed exclusively, in part because they have doubts about their ability to produce enough milk. This is an area of research where existing scales of food insecurity “don’t mean much,” unless we examine household food insecurity in relation to infant feeding practices, said Pérez-Escamilla.
Edward Frongillo, Jr., raised the issue of whether food insecurity in children predisposes them to greater risk of obesity later in life. The work that has looked at this question either prospectively or retrospectively is “extremely limited.” He also raised several additional issues regarding the standard measures of food insecurity and obesity. “Some of the basic assumptions that we have about what obesity even means in children are, I think, questionable.” For example, recent research on the so-called adiposity rebound—in which BMI increases after a low point in childhood—suggests that this phenomenon involves lean tissue rather than fat. “So this very basic idea—that we’re looking over patterns of changes in fatness as measured by BMI—is just wrong, most likely, in a developmental sense with children.”
Interpretations of Measures
Another consideration is whether “worry” over food supplies, which is the least severe measure of food security—that is, in a psychometric sense—may be one of the most important indicators of stress. “We’re going to have to be thoughtful about that,” said Frongillo.
Retrospective Studies
Gundersen responded that retrospective studies may help with some of these questions. For example, work with recent immigrants can indicate what they may have experienced in their home countries and how their experiences even 20 years ago may influence the food insecurity status of their adult children today.
Cautions in Modeling Data
Mark Nord raised a caution about the use of controls in modeling research. Good evidence demonstrates that food insecurity is related to stress and that stress is related to overweight, yet evidence also suggests that food insecurity is not related to overweight, Nord pointed out. Studies have to control for stress, because stress can have origins other than food insecurity, but in controlling for stress some of the most important possible pathways to obesity may be overlooked. “An important question is: How much of the stress is related to food insecurity? … Is it the kind of stress that matters? I don’t know that we have the answer to that at this point,” Nord said. Pérez-Escamilla responded that structural modeling can help address such questions, even if statisticians disagree on the mathematics behind such modeling. “Conceptually it forces us to have a reasonable theoretical model in place before we start collecting the data.”
Publication Bias
Valerie Tarasuk, citing her own research experiences, agreed that negative publication bias is an important factor. “The literature is only a small window on the findings, because some of us have walked away from negative effects,” she said.
Dieting
In response to a question from Elizabeth Dowler about how issues surrounding dieting to lose weight might relate to food insecurity, Laraia responded that very little research-based evidence is available on the subject. However, she also observed that because obesity is more prevalent than food insecurity, episodes of food insecurity may have a relationship to dieting during those episodes or during other parts of a person’s life. “Women might be confronted with that horrible cycle of not knowing where the next meal is, being stressed out, and also trying to possibly lose weight. It’s all enmeshed, and I’m not sure how we would begin to tease it out. We would need to start with a group of young women who are of normal weight and follow them prospectively, but that would take years, and I don’t know if that’s necessarily the right question. It is very complicated.”
Assessing the Impact of Various Stressors
Frongillo observed that one way to use experimentation in exploring the relationship between obesity and food insecurity is to take advantage
of perturbations in existing systems. For example, in work he has done in Bangladesh, a program was instituted to alleviate poverty among women in an extremely poor population. Researchers looked at four potential forms of stress on these women: food insecurity, domestic violence, workload, and a lack of social support. The research showed that food insecurity was by far the dominant mediator between the alleviation of poverty and improvement in women’s well-being.
Laraia responded to this observation by pointing to the possibility that abuse early in life is connected to food insecurity and weight outcomes later in life. Various stressors are highly correlated with anxiety and depression, so it becomes hard to separate causative factors. The dieting issue is also important, she said, especially because dieting can cause a biological stress response.
Episodic Nature of Food Insecurity
John Cook asked about measures of food insecurity that look back over the previous month rather than the previous year. Conditions can change considerably over the course of a year, and food insecurity tends to occur in spells. The episodic nature of food insecurity could be a complicating or exacerbating factor with regard to nutrition and nutritional health. In general, he said, “obesity is an extremely complicated phenomenon, and if there are associations between food insecurity and obesity, they are way more complex than I ever dreamed they could be. I don’t really dismiss the idea that there are important relationships … even when the predominance of research strongly suggests there aren’t.”
Diet Quality
In response to a question from Marlene Schwartz about diet quality and obesity, Laraia said that the literature does not point to much of an association, although this may be a consequence of how diet is measured. Diet quality usually is measured through food records or recall covering the past few days, but short-term records, even if accurate, can be misleading. “We probably need to be using the 30-day retrospective food security scale and the 3 days of food recall.” Also, the food propensity questionnaire being used in NHANES can capture much more information about diet.
Pérez-Escamilla said that he had a different take on this issue. He has been involved with the adaptation and validation of the U.S. food security measure in different parts of the world, and especially in Latin America, and one of the validation criteria used in addition to poverty is how well the measure correlates with the intake of healthful, nutritious foods such as fruits and vegetables. Using simple and short food frequency question-
naires, he and his colleagues have found in extensive data from Brazil that the measure consistently correlates with fruit and vegetable intake—the more severe the level of household food insecurity, the greater is the reduction in the likelihood that the household consumes fruits and vegetables on a daily basis. Some data from the United States point in the same direction, along with research indicating that food-insecure households are less likely to have access to healthful diets.
Adam Drewnowski, who has conducted some of that research, said that the data on diet quality when stratified by socioeconomic status show two things. First, there is a social gradient for the consumption of certain nutrients and for some food groups. Lower cost grains, fats, and sweets are overconsumed by lower-income groups, and soft drinks are very much overconsumed by the lowest-income groups. By contrast, more fruits and vegetables are consumed by higher-income groups. Even within food categories there are social gradients, so that the consumption of whole fruit is associated with upper-income groups whereas juices are consumed by lower-income groups. This socioeconomic gradient in food consumption patterns is partly explained by the cost of different foods, but other factors, such as taste, convenience, and habit, may also exert an effect.
Christine Olson agreed that the food group least available in food-insecure households is fruits and vegetables. The 24-hour recall of food eaten by adults in food-insecure households includes less fruits and vegetables. Also the nutrients associated with fruits and vegetables are lower in circulating blood levels in adults who live in food-insecure households. The evidence linking insufficient fruits and vegetables and food insecurity is “really strong,” said Olson.
Gundersen observed that questions about diet are critically important in health outcomes regardless of any effect on obesity. “I would like to see a workshop on understanding the relationship between food insecurity and nutrient intakes, because that, to me, is the core issue. If you improve people’s nutrition, that has benefits, even if they still may be obese or not obese.”
REFERENCES
Adam, T. C., and E. S. Epel. 2007. Stress, eating and the reward system. Physiology and Behavior 91(4):449-458.
Adams, E. J., L. Grummer-Strawn, and G. Chavez. 2003. Food insecurity is associated with increased risk of obesity in California women. Journal of Nutrition 133(4):1070-1074.
Anderson, S. A. 1990. Core indicators of nutritional state for difficult-to-sample populations. Journal of Nutrition 120(11S):1557-1600. Report by the Life Sciences Research Office, Federation of American Societies for Experimental Biology, for the American Institute of Nutrition.
Basiotis, P., and M. Lino. 2002. Food insufficiency and prevalence of overweight among adult women. Family Economics and Nutrition Review 15(2):55-57.
Bhargava, A., D. Jolliffe, and L. L. Howard. 2008. Socio-economic, behavioural and environmental factors predicted body weights and household food insecurity scores in the Early Childhood Longitudinal Study-Kindergarten. British Journal of Nutrition 100(2):438-444.
Briefel, R., and C. E. Woteki. 1992. Development of the food sufficiency questions for the third National Health and Nutrition Examination Survey. Journal of Nutrition Education 24:24S-28S.
Bronte-Tinkew, J., M. Zaslow, R. Capps, A. Horowitz, and M. McNamara. 2007. Food insecurity works through depression, parenting, and infant feeding to influence overweight and health in toddlers. Journal of Nutrition 137(9):2160-2165.
Casey, P. H., K. Szeto, S. Lensing, M. Bogle, and J. Weber. 2001. Children in food-insufficient, low-income families: Prevalence, health, and nutrition status. Archives of Pediatrics and Adolescent Medicine 155(4):508-514.
Chilton, M., and S. Booth. 2007. Hunger of the body and hunger of the mind: African American women’s perceptions of food insecurity, health and violence. Journal of Nutrition Education and Behavior 39(3):116-125.
Cook, J. T., D. A. Frank, S. M. Levenson, N. B. Neault, T. C. Heeren, M. M. Black, C. Berkowitz, P. H. Casey, A. F. Meyers, D. B. Cutts, and M. Chilton. 2006. Child food insecurity increases risks posed by household food insecurity to young children’s health. Journal of Nutrition 136(4):1073-1076.
Coplan, J. D., E. L. P. Smith, M. Altemus, S. J. Mathew, T. Perera, J. G. Kral, J. M. Gorman, M. J. Owens, C. B. Nemeroff, and L. A. Rosenblum. 2006. Maternal-infant response to variable foraging demand in nonhuman primates: Effects of timing of stressor on cerebrospinal fluid corticotropin-releasing factor and circulating glucocorticoid concentrations. Annals of the New York Academy of Sciences 1071:525-533.
Crossman, A., D. Anne Sullivan, and M. Benin. 2006. The family environment and Ameri can adolescents’ risk of obesity as young adults. Social Science and Medicine 63(9):2255-2267.
DePolt, R. A., R. A. Moffitt, and D. C. Ribar. 2009. Food stamps, temporary assistance for needy families and food hardships in three American cities. Pacific Economic Review 14(4):445-473.
Dietary Guidelines Advisory Committee. 2010. Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans, 2010, to the Secretary of Agriculture and the Secretary of Health and Human Services. Washington, DC: U.S. Department of Agriculture, Agricultural Research Service.
Dixon, L. B., M. A. Winkleby, and K. L. Radimer. 2001. Dietary intakes and serum nutrients differ between adults from food-insufficient and food-sufficient families: Third National Health and Nutrition Examination Survey, 1988-1994. Journal of Nutrition 131(4):1232-1246.
Drewnowski, A., and S. E. Specter. 2004. Poverty and obesity: The role of energy density and energy costs. American Journal of Clinical Nutrition 79(1):6-16.
Dubois, L., A. Farmer, M. Girard, and M. Porcherie. 2006. Family food insufficiency is related to overweight among preschoolers. Social Science and Medicine 63(6):1503-1516.
Eicher-Miller, H. A., A. C. Mason, C. M. Weaver, G. P. McCabe, and C. J. Boushey. 2009. Food insecurity is associated with iron deficiency anemia in U.S. adolescents. American Journal of Clinical Nutrition 90(5):1358-1371.
FAO (Food and Agriculture Organization of the United Nations). 1996. Rome Declaration on World Food Security and World Food Summit Plan of Action.
Fernald, L. C. H., P. J. Gertler, and X. Hou. 2008. Cash component of conditional cash transfer program is associated with higher body mass index and blood pressure in adults. Journal of Nutrition 138(11):2250-2257.
Fernald, L. C., P. J. Gertler, and L. M. Neufeld. 2009. 10-year effect of Oportunidades, Mexico’s conditional cash transfer programme, on child growth, cognition, language, and behaviour: A longitudinal follow-up study. The Lancet 374(9706):1997-2005.
Garasky, S., S. D. Stewart, C. Gundersen, B. J. Lohman, and J. C. Eisenmann. 2009. Family stressors and child obesity. Social Science Research 38(4):755-766.
Gibson, L. Y., S. M. Byrne, E. A. Davis, E. Blair, P. Jacoby, and S. R. Zubrick. 2007. The role of family and maternal factors in childhood obesity. Medical Journal of Australia 186(11):591-595.
Gundersen, C., and B. Kreider. 2009. Bounding the effects of food insecurity on children’s health outcomes. Journal of Health Economics 28(5):971-983.
Gundersen, C., and V. Oliveira. 2001. The food stamp program and food insufficiency. American Journal of Agricultural Economics 83(4):875-887.
Gundersen, C., B. J. Lohman, S. Garasky, S. Stewart, and J. Eisenmann. 2008. Food security, maternal stressors, and overweight among low-income U.S. children: Results from the National Health and Nutrition Examination Survey (1999-2002). Pediatrics 122(3).
Gundersen, C., S. Garasky, and B. J. Lohman. 2009a. Food insecurity is not associated with childhood obesity as assessed using multiple measures of obesity. Journal of Nutrition 139(6):1173-1178.
Gundersen, C., D. Jolliffe, and L. Tiehen. 2009b. The challenge of program evaluation: When increasing program participation decreases the relative well-being of participants. Food Policy 34(4):367-376.
Hamilton, W., J. Cook, W. Thompson, L. Buron, E. Frongillo, C. Olson, and C. Wehler. 1997. Household Food Security in the United States in 1995: Summary Report of the Food Security Measurement Project. Alexandria, VA: Office of Analysis, Nutrition, and Evaluation, Food and Nutrition Service, U.S. Department of Agriculture.
Hanson, K. L., J. Sobal, and E. A. Frongillo. 2007. Gender and marital status clarify associations between food insecurity and body weight. Journal of Nutrition 137(6):1460-1465.
Hernandez, D. C., and A. Jacknowitz. 2009. Transient, but not persistent, adult food insecurity influences toddler development. Journal of Nutrition 139(8):1517-1524.
Jones, S. J., and E. A. Frongillo. 2006. The modifying effects of food stamp program participation on the relation between food insecurity and weight change in women. Journal of Nutrition 136(4):1091-1094.
Jones, S. J., and E. A. Frongillo. 2007. Food insecurity and subsequent weight gain in women. Public Health Nutrition 10(2):145-151.
Jyoti, D. F., E. A. Frongillo, and S. J. Jones. 2005. Food insecurity affects school children’s academic performance, weight gain, and social skills. Journal of Nutrition 135(12): 2831-2839.
Kaiser, L. L., M. S. Townsend, H. R. Melgar-Quiñonez, M. L. Fujii, and P. B. Crawford. 2004. Choice of instrument influences relations between food insecurity and obesity in Latino women. The American Journal of Clinical Nutrition 80(5):1372-1378.
Kaufman, D., M. A. Banerji, I. Shorman, E. L. P. Smith, J. D. Coplan, L. A. Rosenblum, and J. G. Kral. 2007. Early-life stress and the development of obesity and insulin resistance in juvenile bonnet macaques. Diabetes 56(5):1382-1386.
Kirkpatrick, S. I., L. McIntyre, and M. L. Potestio. 2010. Child hunger and long-term adverse consequences for health. Archives of Pediatrics and Adolescent Medicine 164(8):754-762.
Koch, F. S., A. Sepa, and J. Ludvigsson. 2008. Psychological stress and obesity. Journal of Pediatrics 153(6).
Kuo, L. E., J. B. Kitlinska, J. U. Tilan, L. Li, S. B. Baker, M. D. Johnson, E. W. Lee, M. S. Burnett, S. T. Fricke, R. Kvetnansky, H. Herzog, and Z. Zukowska. 2007. Neuropeptide Y acts directly in the periphery on fat tissue and mediates stress-induced obesity and metabolic syndrome. Nature Medicine 13(7):803-811.
Laraia, B. A. 2010. Food insecurity and obesity among adults. Presented at the Institute of Medicine Workshop on Understanding the Relationship Between Food Insecurity and Obesity, November 16, Washington, DC.
Laraia, B. A., A. M. Siega-Riz, and K. R. Evenson. 2004. Self-reported overweight and obesity are not associated with concern about enough food among adults in New York and Louisiana. Preventive Medicine 38(2):175-181.
Laraia, B. A., A. M. Siega-Riz, C. Gundersen, and N. Dole. 2006. Psychosocial factors and socioeconomic indicators are associated with household food insecurity among pregnant women. Journal of Nutrition 136(1):177-182.
Larson, N., and M. Story. 2010. Food insecurity and risk for obesity among children and families: Is there a relationship? A research synthesis. Princeton, NJ, and Minneapolis, MN: Robert Wood Johnson Foundation Healthy Eating Research.
Lohman, B. J., S. Stewart, C. Gundersen, S. Garasky, and J. C. Eisenmann. 2009. Adolescent overweight and obesity: Links to food insecurity and individual, maternal, and family stressors. Journal of Adolescent Health 45(3):230-237.
Lyons, A. A., J. Park, and C. H. Nelson. 2007. Food insecurity and obesity: A comparison of self-reported and measured height and weight. American Journal of Public Health 98(4):751-757.
Miech, R. A., S. K. Kumanyika, N. Stettler, B. G. Link, J. C. Phelan, and V. W. Chang. 2006. Trends in the association of poverty with overweight among US adolescents, 1971-2004. Journal of the American Medical Association 295(20):2385-2393.
Nord, M., and A. M. Golla. 2009. Does SNAP decrease food insecurity? Untangling the self-selection effect. Economic Research Report No. 85. Washington, DC: Economic Research Service.
Nord, M., A. Coleman-Jensen, M. Andrews, and S. Carlson. 2010. Household food security in the United States, 2009. Economic Research Report No. 108. Washington, DC: Economic Research Service.
NRC (National Research Council). 2006. Food insecurity and hunger in the United States: An assessment of the measure. Edited by G. S. Wunderlich and J. L. Norwood. Washington, DC: The National Academies Press.
Olson, C. M. 1999. Nutrition and health outcomes associated with food insecurity and hunger. Journal of Nutrition 129(2 Suppl.).
Olson, C. M., and M. S. Strawderman. 2008. The relationship between food insecurity and obesity in rural childbearing women. Journal of Rural Health 24(1):60-66.
Pérez-Escamilla, R. In press. Food insecurity and hunger in children: Impact on physical and psycho-emotional development. In Modern Nutrition in Health and Disease. 11th ed, edited by C. A. Ross, B. Caballero, R. J. Cousins, K. L. Tucker, and T. R. Ziegler. Baltimore, MD: Lippincott Williams & Wilkins.
Phipps, S. A., P. S. Burton, L. S. Osberg, and L. N. Lethbridge. 2006. Poverty and the extent of child obesity in Canada, Norway and the United States. Obesity Reviews 7(1):5-12.
Rose-Jacobs, R., M. M. Black, P. H. Casey, J. T. Cook, D. B. Cutts, M. Chilton, T. Heeren, S. M. Levenson, A. F. Meyers, and D. A. Frank. 2008. Household food insecurity: Associations with at-risk infant and toddler development. Pediatrics 121(1):65-72.
Seligman, H. K., and D. Schillinger. 2010. Hunger and socioeconomic disparities in chronic disease. New England Journal of Medicine 363(1):6-9.
Seligman, H. K., B. A. Laraia, and M. B. Kushel. 2010. Food insecurity is associated with chronic disease among low-income NHANES participants. Journal of Nutrition 140(2): 304-310.
Shrewsbury, V., and J. Wardle. 2008. Socioeconomic status and adiposity in childhood: A systematic review of cross-sectional studies 1990-2005. Obesity 16(2):275-284.
Singh, G. K., M. D. Kogan, P. C. Van Dyck, and M. Siahpush. 2008. Racial/ethnic, socioeconomic, and behavioral determinants of childhood and adolescent obesity in the United States: Analyzing independent and joint associations. Annals of Epidemiology 18(9):682-695.
Skalicky, A., A. F. Meyers, W. G. Adams, Z. Yang, J. T. Cook, and D. A. Frank. 2006. Child food insecurity and iron-deficiency anemia in low-income infants and toddlers in the United States. Maternal and Child Health Journal:1-9.
Slack, K. S., and J. Yoo. 2005. Food hardship and child behavior problems among low-income children. Social Service Review 79(3):511-536.
Stenhammar, C., G. M. Olsson, S. Bahmanyar, A. L. Hulting, B. Wettergren, B. Edlund, and S. M. Montgomery. 2010. Family stress and BMI in young children. Acta Paediatrica, International Journal of Paediatrics 99(8):1205-1212.
Sweeting, H., C. Wright, and H. Minnis. 2005. Psychosocial correlates of adolescent obesity, “slimming down” and “becoming obese.” Journal of Adolescent Health 37(5).
Townsend, M. S., J. Peerson, B. Love, C. Achterberg, and S. P. Murphy. 2001. Food insecurity is positively related to overweight in women. Journal of Nutrition 131(6):1738-1745.
Van Hook, J., and K. S. Balistreri. 2006. Ineligible parents, eligible children: Food Stamps receipt, allotments, and food insecurity among children of immigrants. Social Science Research 35(1):228-251.
Van Jaarsveld, C. H. M., J. A. Fidler, A. Steptoe, D. Boniface, and J. Wardle. 2009. Perceived stress and weight gain in adolescence: A longitudinal analysis. Obesity 17(12): 2155-2161.
VanEenwyk, J., and J. Sabel. 2003. Self-reported concern about food security associated with obesity—Washington, 1995-1999. Morbidity and Mortality Weekly Report 52(35): 840-842.
Vozoris, N. T., and V. S. Tarasuk. 2003. Household food insufficiency is associated with poorer health. Journal of Nutrition 133(1):120-126.
Whitaker, R. C., and A. Sarin. 2007. Change in food security status and change in weight are not associated in urban women with preschool children. Journal of Nutrition 137(9): 2134-2139.
Whitaker, R. C., S. M. Phillips, and S. M. Orzol. 2006. Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics 118(3):e859-868.
Wilde, P. E., and J. N. Peterman. 2006. Individual weight change is associated with household food security status. Journal of Nutrition 136(5):1395-1400.
Yoo, J. P., K. S. Slack, and J. L. Holl. 2009. Material hardship and the physical health of school-aged children in low-income households. American Journal of Public Health 99(5):829-836.
Zaslow, M., J. Bronte-Tinkew, R. Capps, A. Horowitz, K. A. Moore, and D. Weinstein. 2009. Food security during infancy: Implications for attachment and mental proficiency in toddlerhood. Maternal and Child Health Journal 13(1):66-80.
Zeller, M. H., J. Reiter-Purtill, A. C. Modi, J. Gutzwiller, K. Vannatta, and W. H. Davies. 2007. Controlled study of critical parent and family factors in the obesigenic environment. Obesity 15(1):126-136.


























