3
Conducting Research on the Health Status of LGBT Populations
As background for the review of existing research on sexual- and gender-minority health in Chapters 4, 5, and 6, the present chapter reviews research challenges associated with the study of LGBT populations, the research methods and data sources used in studying these populations, and best-practice principles for conducting research on the health of LGBT people. The final section presents a summary of key findings and research opportunities.
RESEARCH CHALLENGES
Three important challenges confront researchers attempting to gather valid and reliable data for describing LGBT populations and assessing their health: (1) operationally defining and measuring sexual orientation and gender identity, (2) overcoming the reluctance of some LGBT individuals to identify themselves to researchers, and (3) obtaining high-quality samples of relatively small populations. In addition, as emphasized in Chapter 1, although the acronym “LGBT” is applied to lesbians, gay men, bisexual men and women, and transgender people, these groups are distinct, and they also comprise subgroups based on race, ethnicity, geographic location, socioeconomic status, age, and other factors. These variations have implications for health research, including the need to obtain sample sizes that are large enough to understand differences among subgroups.
Operationally Defining and Measuring Sexual Orientation and Gender Identity
Many social, cultural, and behavioral phenomena pose measurement challenges to researchers. For example, multiple operational definitions have been used to assess education (Smith, 1995), political ideology (Knight, 1999), religiosity and religious fundamentalism (Hall et al., 2008; Kellstedt and Smidt, 1996), and race and ethnicity (NRC, 2004; Stephan and Stephan, 2000). Similarly, researchers who study LGBT populations face the challenges of defining sexual orientation and gender identity and developing procedures for operationalizing these constructs.
As explained in Chapter 2, sexual orientation is typically defined and measured in terms of three dimensions—behavior, attraction, and identity. Ideally, which of these dimensions is used in research is informed by a particular study’s research goals. For example, a study of HIV risk in gay men would appropriately focus on sexual behavior, whereas a study of experiences with hate crimes or housing discrimination might focus on sexual orientation identity (Herek et al., 2010). Although most adults exhibit consistency across the three dimensions (e.g., they are exclusively heterosexual or homosexual in their sexual behavior, attractions, and self-labeled identity), some do not. Whether a particular study categorizes the latter individuals as lesbian, gay, homosexual, bisexual, heterosexual, or something else will depend on which specific dimension of sexual orientation is measured in that study. In a study that measures sexual orientation in terms of same-sex attraction or sexual behavior with a same-sex partner, for example, the sample may include some participants who do not label themselves as lesbian, gay, or bisexual.
Not only do studies vary in which facet of sexual orientation they measure, but they also can differ in how they define each of the three dimensions operationally. The current lack of standardized measures contributes to the variability of population estimates and can make comparisons across studies difficult. For example, if two studies defined sexual orientation operationally in terms of sexual behavior but used different time frames for screening participants (e.g., if one study used the criterion of any same-sex sexual behavior during the past 12 months, whereas the other used any same-sex sexual behavior since age 18), they might reach different conclusions about the target population. Moreover, the samples obtained for both studies would exclude individuals who were not sexually active during the specified time period even if they experienced same-sex attractions or self-identified as lesbian, gay, or bisexual. This variability in the criteria for operationally defining sexual orientation may produce what appear to be inconsistent findings across studies. Although it may appear obvious, it is important to make the point that researchers should carefully evaluate the
appropriateness of their operational definition(s) of sexual orientation in light of the research question their study addresses and clearly explain their measurement procedures when reporting their results.
Similar definitional and measurement variability can be observed across studies of transgender populations. No uniformly accepted best measures of gender variance and gender nonconformity currently exist. One common approach is simply to ask participants whether they are transgender (e.g., Almeida et al., 2009), and, in some studies, whether they further self-identify as female-to-male or male-to-female. This question often follows immediately a question about sexual orientation. However, Buchting and colleagues (2008) have proposed combining the two questions by asking respondents: “Do you consider yourself to be one or more of the following: (a) Straight, (b) Gay or Lesbian, (c) Bisexual, (d) Transgender.”
Because some gender-variant people do not use “transgender” to identify themselves, and some nontransgender individuals may not fully understand the term, simply asking individuals whether they are transgender may lead to underreporting and false positives (SMART, 2009). To address these concerns, some studies have provided respondents with a definition of “transgender” to increase the validity of responses (e.g., Massachusetts Department of Public Health, 2007). Conron and colleagues (2008) report the results of cognitive interviewing with a small nonprobability sample (n = 30) that included transgender youth. Using a question that combined biological sex and gender—asking respondents whether they were “female,” “male,” “transgender, female-to-male,” “transgender, male-to-female,” or “transgender (not exclusively male or female)”—they found that most transgender youth were able to choose a response option they felt was appropriate. However, the authors recommend further testing with slight modifications to the question (Conron et al., 2008). In addition, questions about gender transitioning have been included in several studies (Grant et al., 2010; Nemoto et al., 2005; Xavier et al., 2007).
Measuring the sexual orientation of transgender people poses special challenges because some respondents may answer questions about sexual orientation in terms of birth sex (their own or their partner’s), whereas others may respond in terms of gender identity, and still others may find it difficult to answer in terms of a male–female dichotomy (e.g., Austin et al., 2007; Garofalo et al., 2006). Some HIV studies have included questions about the respondent’s sexual behavior with males, females, transgender men, and transgender women.
While a number of effective measures of sexual orientation and gender identity have been developed, there remains a need for methodological research to determine the best ways to identify lesbian, gay, bisexual, and transgender people in health research. And while the most appropriate measures of sexual orientation and gender identity vary according to a
particular study’s research goals, standardization of measures in federally funded surveys would help improve knowledge about LGBT health because it would allow for the comparison and combination of data across studies.
Overcoming the Reluctance to Identify as LGBT to Researchers
Researchers studying sensitive topics must deal routinely with the reluctance of some participants to disclose accurate information about themselves. A topic may be sensitive because respondents perceive it as intruding on their privacy, because it raises concerns about the possible repercussions of disclosure to others, or because it triggers social desirability concerns (i.e., the desire to “look good” to others). Examples of sensitive topics include income, illegal activities, sexual practices, and membership in a stigmatized group. When confronted with a question about a sensitive topic, respondents may decline to answer or may intentionally give an inaccurate response. In some cases, respondents may decide not to participate in the study at all, thereby reducing the overall response rate and possibly making the sample less representative of the larger population. All of these outcomes have important implications for data quality (Lee, 1993; Tourangeau and Yan, 2007; Tourangeau et al., 2000).
Because they wish to avoid stigma and discrimination and are concerned about their privacy, some individuals are reluctant to disclose their membership in a sexual- or gender-minority group. McFarland and Caceres (2001), for example, describing the factors that lead to underestimation of HIV infection and risk among men who have sex with men, note that stigma and discrimination result in marginalization of these men, which in turn engenders suspicion toward government institutions, researchers, and service providers. Consequently, they argue, many men who have sex with men are unwilling or reluctant to participate in research studies.
As with research on other sensitive topics, challenges include nonparticipation and item nonresponse (which occurs when a respondent provides some of the requested information, but certain questions are left unanswered, or certain responses are inadequate for use). Nonparticipation and nonresponse threaten the generalizability of research data to the extent that those who do not disclose their sexual orientation or transgender identity accurately, or decline to participate altogether, differ in relevant ways from those who do disclose and participate.
A primary strategy to foster disclosure and reduce nonresponse is for researchers to establish a bond of trust with members of the target population. As with other populations, sexual and gender minorities are more likely to entrust researchers with sensitive information about themselves to the extent that they perceive the researchers to be professional, competent, and sensitive to their concerns about privacy (see, generally, Dillman et
al., 2009). In addition, sexual- and gender-minority participants are more likely to trust researchers who evidence knowledge and sensitivity about their community and culture, characteristics commonly understood to be components of cultural competence.
As an adjunct to cultural competence, a number of techniques have been used to improve response rates to questions relating to sensitive topics. Modes of data collection that foster participants’ sense of confidentiality or anonymity may yield higher rates of disclosure. For example, research participants may be more willing to disclose same-sex behavior or attractions when they provide their responses via computer rather than in a face-to-face interview (Villarroel et al., 2006; for a review, see Gribble et al., 1999). Collecting data in a private setting and taking steps to establish rapport before asking questions about sensitive topics may also increase respondents’ willingness to disclose sensitive information. Variations in the wording and format of questions, as well as use of terminology that is familiar to the participant, have shown some success in eliciting responses (Catania et al., 1996).
Respondents may be more willing to disclose sensitive information about themselves when their participation is anonymous. If anonymity is not possible, understanding that their responses are confidential may increase the extent of participants’ self-disclosure. Although it would not be required, a certificate of confidentiality from the National Institutes of Health (NIH) could be helpful in this regard (NIH, 2011).
Obtaining High-Quality Samples of Relatively Small Populations
As documented below and in subsequent chapters, numerous studies of sexual and gender minorities that have relied on nonprobability samples have yielded important information about and insights into LGBT life and health. If the goal of a study is to provide estimates that can be generalized with confidence to the entire LGBT population, however, the use of probability-based methods is necessary. Obtaining a probability sample of a relatively small population, such as a racial, ethnic, religious, sexual, or gender minority, requires considerably more resources than are required for sampling the population as a whole. This is the case because a large number of potential participants must be screened to obtain a sample of minority group members large enough for statistical analysis. Still more resources are required to collect samples that permit study of subpopulations within these groups, such as socioeconomic, age, and geographic groupings, and comparisons of respondents according to health-related characteristics.
Lacking such resources, relatively few studies designed specifically to examine LGBT individuals have been able to utilize large probability samples. There are, however, some exceptions. In the Urban Men’s Health
Study, Catania and colleagues (2001) used a complex, two-stage sampling procedure in New York, Los Angeles, San Francisco, and Chicago to obtain a probability sample of men who have sex with men (n = 2,881) (see also Blair, 1999). Herek and colleagues used the Knowledge Networks panel to obtain a national probability sample of self-identified lesbian, gay, and bisexual adults (n = 662) (Herek, 2009; Herek et al., 2010). Knowledge Networks creates a panel using random-digit dialing to generate a national probability sample and administers an online survey to the panel. Internet access and the appropriate equipment are provided for those panel members who lack them.
Other researchers have conducted secondary analyses of health data collected from surveys of large national samples that included at least one question about respondents’ sexual behavior (e.g., Cochran and Mays, 2000), sexual attraction (e.g., Consolacion et al., 2004), or sexual orientation identity (e.g., Cochran et al., 2003, 2007; Hatzenbuehler et al., 2009, 2010; Mays and Cochran, 2001; McLaughlin et al., 2010). The findings from many of these studies are discussed in later chapters of this report.
In addition to the data sets used in these secondary analyses, numerous other government and academic surveys routinely use large national probability samples to collect extensive data on the health of Americans. However, relatively few of these surveys have included measures of variables related to sexual orientation or gender identity. Consequently, many of the data sources widely used by health researchers do not yield insights into LGBT populations. As discussed later in this chapter, this situation can be remedied by routinely including measures of sexual orientation and gender identity in these surveys.
U.S. census data have also been used to obtain information about the LGBT population (Black et al., 2000; Gates, 2007; Rosenfeld, 2010), but the available information is limited. Since 1990, the census has reported data for same-sex partners who live in the same household, provided that one of them is designated the householder and both report their gender and relationship status on the household roster. However, an unknown number of same-sex partners who do not meet these conditions are not identified. Moreover, because census respondents’ sexual orientation is not ascertained, lesbians, gay men, and bisexual adults who are not cohabiting in a same-sex relationship remain invisible in the data. Nor can transgender people be identified in census data. It should be noted that adding content to the census requires the approval of the U.S. Office of Management and Budget and, ultimately, the Congress.
A third approach to obtaining a national probability sample with a sufficient number of sexual- and gender-minority respondents involves combining data across studies. For ongoing studies that recruit new probability samples on a regular basis, it can be possible to combine sexual- and
gender-minority respondents across years to produce a sample that is sufficiently large for analysis, provided that the studies all include comparable measures of key variables. Combining data from eight waves of the General Social Survey with data from the National Health and Social Life Survey (NHSLS) and the Chicago Health and Social Life Survey, for example, Wienke and Hill (2009) compared the well-being of partnered gay men and lesbians (n = 282) with that of single gay men and lesbians (n = 59) and married, cohabiting, dating, and single heterosexuals (sample sizes ranged from 614 to 6,734).
Combining data from multiple samples can be helpful in researching groups (like sexual and gender minorities) that represent a small domain in part of a larger survey. Because the numbers of these small groups often are not sufficiently large for analysis, combining data from multiple samples allows researchers to generate more accurate estimates. However, this method poses a variety of analytical challenges, and statistical methods for improving the estimation and analysis of small domains continue to be developed (Rao, 2003). These methods usually require assumptions about the statistical models employed and additional information related to the estimates the researcher wants to produce. For application to LGBT health research, these measures require the implementation and use of consistent measures to identify LGBT populations.
Raghunathan and colleagues (2007) provide an example that, although not involving LGBT populations, combines information from two data sets to improve the efficiency of county-level estimates. The authors use a statistical modeling approach—combining data from the Behavioral Risk Factor Surveillance System (BRFSS), a telephone survey conducted by state agencies, and the National Health Interview Survey (NHIS), an area probability sample surveyed through face-to-face interviews—to improve county-level prevalence rates of cancer risk factors that were developed from one survey alone. In a case study using data from the NHIS and the National Nursing Home Survey, Schenker and colleagues (2002) provide an example that illustrates the benefits of combining estimates from complementary surveys and discuss the analytic issues involved in doing so. Schenker and Raghunathan (2007) review four studies conducted by the National Center for Health Statistics that combine information from multiple surveys to improve various measures of health. In another example, Elliott and colleagues (2009) recognized that estimates of health care disparities in small racial/ethnic groups are often lacking in precision because of the small sample sizes involved. They developed an application of the Kalman filter (a recursive algorithm originally used in engineering applications; see Kalman, 1960) to use the available data more efficiently. By applying the Kalman filter to 8 years of data from the NHIS, they demonstrated how estimates for small populations could be improved by combining estimates from
multiple years. In many cases, this method improved precision to an extent that would be similar to what would be achieved by doubling the sample size of the yearly data. When this method is used, the LGBT populations in the data sets that are statistically combined must be identified.
RESEARCH METHODS
In all empirical research, each component of the study design must be based on consideration of specific characteristics of the population being studied if effective methods for data gathering are to be developed. For LGBT studies, researchers must identify and select the most effective methods to compensate for the unique research challenges discussed above. This section reviews sampling issues, including the utility of probability and nonprobability sampling for generating study populations for LGBT health research, and describes quantitative and qualitative analytic methods used in LGBT research.
Research studies are designed to describe population characteristics, explore unanswered questions, or test hypotheses in order to validate previous findings or investigate areas that have not been fully explored. The applicability of research findings is directly related to the study design and the ability of the research team to identify an adequate sample for analysis. The manner in which the data collection methodology, the measurement design, and sample selection methods and subject recruitment are assembled into a coherent study design determines the relevance and generalizability of the findings.
Internal and external validity are important considerations for evaluating the relevance of LGBT research findings. Internal validity means that the measures of all variables are reliable, there is justification for linkages of relationships between independent and dependent variables, and other extraneous variables that are not logically associated are ruled out. External validity denotes the generalizability of study results beyond the specific study setting. These issues are discussed throughout the chapter.
Sampling Challenges
Careful sampling requires a precise definition of the target population of the study. The target population is the set of elements about which information is wanted and parameter estimates are required (OMB, 2001). For example, the target population could be all LGBT persons in the United States or in a state, community, or other geographic area. If members of the target population are selected into the sample by a random, unbiased mechanism such that every person in the target population has a known chance of being selected into the study, the resultant study sample can be
used to draw inferences and generalize about the target population, and the sample thus generated is “representative” of the target population. After the desired target population for a study has been specified, selection of a sample requires identifying or developing a sampling frame or list of elements in the target population. The completeness of the sampling frame relative to the target population and the methods by which individual units are selected or identified for the study sample determine the limits of statistical inference and generalizability for the study results. Typically, researchers obtain study samples by selecting participants from a geographically defined population or a list of individuals who share a common characteristic, such as inclusion in a membership list of professionals. As discussed above, a variety of factors create challenges for generating samples that are representative of LGBT populations.
Recently, alternative models have been developed to identify a target population by starting with the community of interest and identifying samples that mirror characteristics of that community. A probability-based mechanism may or may not be used for selecting the study sample. For LGBT studies, both probability and nonprobability sampling methods have been used.
Probability Sampling
Probability sampling identifies a well-defined target population and sampling frame and uses a probabilistic method of selection to obtain a sample that is representative of the target population (Kalton, 2009). Although probability sampling can be expensive and the statistical methods employed can be complicated, the ensuing data lead to findings that can be generalized to the target population. If the target population were the nation’s LGBT populations, the sampling frame had characteristics such that it was possible to identify all LGBT people, and a probability mechanism were defined that gave everyone in the sampling frame an equal chance of being selected, then the findings could be generalized to LGBT populations in the United States—within the scope of the study measures and subject to limitations of sampling and nonsampling error. Probability-based sampling methods rely on the assumption that a list of all eligible units of the target population can be constructed and that all units will have a known probability of selection.
Many approaches to obtaining a probability-based sample of a population ensure that valid inferences can be drawn. Kalton (2009) describes a number of such approaches for obtaining valid samples for subpopulations. When an existing sampling frame can identify whether an individual is a member of a subpopulation, drawing a sample of a specified size can be accomplished in a straightforward way. On the other hand, in many
applications, individuals cannot be identified prior to selection of the sample. In such cases, major challenges exist within the probability-based framework. The approaches Kalton describes can be costly, as several require extensive screening to identify the subpopulation(s) of interest or can rely on a number of assumptions to permit valid inferences.
A common practice is to draw a large sample of the general population and then screen potential participants for inclusion in the study based on criteria that define the study’s target population. With populations such as LGBT individuals, ineligible participants must be identified and eliminated from the study during the data collection process. This process is often implemented with a series of screening questions administered at the time the interviewer first contacts the household person. For example, the previously mentioned Urban Men’s Health Study used telephone screening, along with other techniques, to obtain a probability sample of men who were gay or bisexual or reported having sex with men and who resided in New York, Chicago, Los Angeles, and San Francisco (Blair, 1999; Catania et al., 2001). To compare the yield of population-based methods for health needs assessments, Meyer and colleagues (2002) and Bowen and colleagues (2004) conducted paired surveys in Jamaica Plain, Massachusetts, using random-digit dialing and household area probability sampling in the same census tracts. Percentages of women who identified as sexual minorities were similar across the two sampling methods.
Another method, known as disproportionate stratification, can be effective for identifying small study populations. This method identifies areas where the target population is more highly concentrated and then samples a higher fraction of units within those areas. Disproportionate sampling may be an effective screening strategy for LGBT populations while ensuring that population estimates are possible. For example:
-
Boehmer and colleagues (2010) used disproportionate sampling to select geographic units in census areas with a higher prevalence of lesbians and bisexual women.
-
The 2003 California LGBT Tobacco Survey used disproportionate stratification in its random-digit dialing sampling design. The survey used areas identified by the 2000 decennial census as having a high proportion of unmarried same-sex partners and applied a weighting scheme to make the sample representative of the lesbian and gay population of California (Carpenter and Gates, 2008).
-
Sampling using multiple sampling frames takes advantage of more than one partial listing of the target population to create a probability sample; care must be taken to remove duplicate listings of individuals when using this method. Aaron and colleagues (2003) used capture recapture methods with multiple lists and elimina-
-
tion of duplicates to estimate the lesbian population in Allegheny County, Pennsylvania.
-
Network or multiplicity sampling uses sampled persons as proxy respondents for persons who are “linked” to them in a specific way, for example, as a family member (Sirken, 2004). An assumption required for this method is that all members of the linkage must know or be willing to report the rare population status of those linked to them (Kalton, 2009).
Probability sampling has seen limited use in the study of LGBT health. As explained above, the relatively small size of LGBT populations, the lack of research funding, and the sensitivity of questions relating to sexual behavior and gender expression have been barriers to effective probability sampling. Despite these challenges, some researchers have used probability samples for LGBT research. In addition to the examples cited earlier (Catania et al., 2001; Herek et al., 2010), the NHSLS, described in the previous chapter (Laumann et al., 1994), used multistage sampling to create a probability sample of U.S. households. Although sexual and gender minorities were not specifically targeted for the study, questions about sexual orientation were included in the survey instrument. Similarly, the federally sponsored National Survey of Family Growth (NSFG) does not specifically target LGBT people but does include questions about sexual orientation identity, behavior, and attraction (Mosher et al., 2005). A further example is the National Survey of Sexual Health and Behavior (Herbenick et al., 2010), which was based on data from an online survey using a cross-sectional sample of U.S. adolescents and adults participating in a Knowledge Networks panel and reported data on the sexual orientation and behavior of participants. Another study using a probability sample of self-identified lesbian, gay, and bisexual participants in the Knowledge Networks panel reported extensive data on demographic, psychological, and social commonalities and differences across sexual orientation subgroups (Herek et al., 2010). Illustrative examples of the study designs and sexual orientation measures used in some of these studies are shown in Box 3-1.
Sexual orientation and gender identity measures have also been included in state-level health surveys of probability-based samples, allowing some comparisons with heterosexual counterparts. The Massachusetts Department of Public Health has incorporated these measures into its Behavioral Risk Factor Surveillance System surveys since 2001 (transgender identity question added in 2010). Conron and colleagues (2010) aggregated 2001–2008 data from the Massachusetts Behavioral Risk Factor Surveillance System surveys to examine patterns in self-reported health by sexual orientation identity. The California Health Interview Survey (CHIS), conducted every 2 years, is a population-based random-digit dialing telephone
|
BOX 3-1 Examples of Probability Sample Studies with Sexual Orientation Measures National Survey of Family Growth (NSFG) Personal interviews were conducted with the civilian noninstitutionalized population to collect data on factors influencing pregnancy and women’s health in the United States. Sexual orientation questions were asked and answered by audio computer-assisted self-interview.* A national sample of adult men and women aged 15-44 was interviewed. In 2002, 12,751 interviews were completed (4,928 men and 7,643 women). Asked of women and men: Do you think of yourself as: Heterosexual, Homosexual, Bisexual, or something else? Men were asked about oral and anal sex with another man; women were asked whether they had ever had any sexual experience of any kind with another female. Men and women were asked whether they were sexually attracted to males, females, or both. National Health and Social Life Survey (NHSLS) The NHSLS was designed to be a representative and current survey of adult sexual behavior in the United States. The goals of the study were to describe the distribution of sexual practices in the general population and to examine the changes in these practices under current conditions. Multistage household sampling was used to develop an area probability sample of households; 3,432 adult respondents were included. Identity Question: Do you think of yourself as … (1) heterosexual (2) homosexual (3) bisexual (4) or something else? (Specify) [Volunteered responses: (5) normal/straight (6) don’t know] Key Behavior Questions: Now thinking about the time since your 18th birthday and during the time before you started living with [(S)pouse/(C)ohabitant], how many people, including men and women, did you begin having sex with, even if only one time? (If one) Was this partner a male or female? (If two or more) How many of these partners were…(a) male? (b) female? Now I would like to ask you some questions about sexual experiences with (SAME SEX AS R[espondent]; males/females) after you were 12 or 13, that is, after puberty. How old were you the first time that you had sex with a [male/female]? Have your sex partners in the last {12 months/5 years} been … exclusively male; both male and female; female? Now thinking about the time since your 18th birthday (including the recent past you’ve already told us about) how many {female/male} partners have you had sex with? |
|
Attraction Questions: On a scale of 1 to 4, where 1 is very appealing and 4 is not at all appealing, how would you rate each of these activities: … (b) having sex with someone of the same sex. FEMALE ONLY: In general, you are sexually attracted to (1) only men (2) mostly men (3) both men and women (4) mostly women (5) only women. MALE ONLY: In general, you are sexually attracted to (1) only women (2) mostly women (3) both women and men (4) mostly men (5) only men. |
survey of a sample of more than 42,000 California adults. In 2001 and 2003, the CHIS included questions about sexual orientation identity and gender (male/female) of recent sex partners. Data from the CHIS have been used to examine LGBT health issues, including obesity and body weight (Carpenter, 2003; Deputy and Boehmer, 2010) and smoking (Tang et al., 2004). The California Quality of Life Survey, a population-based health survey of adult Californians conducted in 2004–2005 (n = 2,272 adults), employed a sampling frame that was created from a subset of adults first interviewed in the 2003 CHIS and included an oversample of sexual-minority adults. These data have been used to examine physical health status, psychological distress, and mental health status in different sexual orientation groups (Cochran and Mays, 2007, 2009). These studies and others make use of survey vehicles designed for the general population to capture information about sexual and gender minorities that has localized relevance for priority setting at the state and substate levels. Illustrative examples of the study designs and sexual orientation measures of state-level probability-based studies are shown in Box 3-2.
The ability of researchers to draw valid inferences with probability samples hinges on three key elements: proper item design (i.e., questions that elicit the desired information from respondents), acceptably high completion rates,1 and sufficiently large samples. Thus, for example, the NHSLS was carefully designed to elicit information on sensitive issues, and the
|
BOX 3-2 Examples of State-Level Probability Sample Studies with LGBT Measures Massachusetts Behavioral Risk Factor Surveillance System (MA BRFSS) The Centers for Disease Control and Prevention’s (CDC) Behavioral Risk Factor Surveillance System requires all states to implement annual random-digit dialing surveys of community-residing adults to gather information about a wide range of health-related behaviors. The primary focus has been on behaviors that are linked with the leading causes of death—heart disease, cancer, stroke, diabetes, and injury—and other important health issues. These behaviors include (1) not getting enough physical activity; (2) being overweight; (3) not using seatbelts; (4) using tobacco and alcohol; and (5) not getting preventive medical care that can save lives, such as flu shots, mammograms, Pap smears, and colorectal cancer screening tests. Although the inclusion of questions about sexual orientation and gender conformity is not required, six states and two urban areas have added such questions. Massachusetts has included sexual orientation measures since 2000 and began to include a transgender question in 2010. Questions in 2009 MA BRFSS Do you consider yourself to be: heterosexual or straight, homosexual or (if respondent is male read “gay”; else if female, read “lesbian”), bisexual or other? Do you consider yourself to be transgender? During the past 12 months, have you had sex with only males, only females, or with both males and females? The last time you had sex, was your partner male or female? California Health Interview Survey (CHIS) The CHIS is the nation’s largest state health survey. A random-digit dialing telephone survey conducted every 2 years on a wide range of health topics, the CHIS yields a detailed picture of the health and health care needs of California’s large and diverse population. More than 50,000 Californians—including adults, teenagers, and children— are surveyed by the CHIS. Participants in the CHIS are chosen at random, and the sample is extensive enough to be statistically representative of California’s diverse population. The CHIS is especially known for its difficult-to-find data on ethnic subgroups. CHIS telephone surveys are conducted in all 58 counties of California. The CHIS may also conduct oversampling and small-area estimates of certain counties, such as Los Angeles and San Diego. The CHIS is conducted by the University of California, Los Angeles (UCLA) Center for Health Policy Research in collaboration with the California Department of Public Health and Department of Health Care Services. Questions in 2001 This next question is about your sexual orientation and I want to remind you again that your answers are completely confidential. Are you gay, (lesbian), or bisexual? Questions in 2003 In the past 12 months, have your sexual partners been male, female, or both male and female? Do you think of yourself as straight or heterosexual, as gay (lesbian) or homosexual, or bisexual (IF NEEDED SAY: “Straight or Heterosexual people have sex with, or are primarily attracted to people of the opposite sex, Gay (and Lesbian) people have sex with or are primarily attracted to people of the same sex, and Bisexuals have sex with or are attracted to people of both sexes.”) |
completion rate was close to 80 percent. The design team initially hoped to sample 20,000 individuals for the study, but, as noted in the previous chapter, received funding sufficient to complete a sample of only 3,432. The total number of women who reported nonheterosexual behavior, attraction, or identity was 150 (8.6 percent of the total), and the comparable number for men was 143 (10.1 percent). The consequence is that estimates for these key subpopulations are not precise; that is, they have relatively large margins of error. Thus, the sample is useful, but far from ideal, for the purpose of studying LGB populations, and it does not permit meaningful analysis of subgroups defined by race/ethnicity, age, and other sociodemographic characteristics. The study included no measure of gender identity.
Other studies have also examined subsets of sexual and gender minorities in LGBT populations using probability samples that were not designed to study those individuals. An example is the study of same-sex couples in the U.S. census. Questions were not designed for the purpose of learning about same-sex couples, but the data have well-known properties. The 2000 U.S. census long form (received by approximately one in every six households) is very large. Thus, inferences drawn have high internal validity for very specific population parameters and have high external validity for more general population parameters. See Box 3-3 for an example of an inference that can be drawn from U.S. census data.
Respondent-driven sampling. Respondent-driven sampling, a chain-referral method, attempts to create a sample based on the social networks of participants. It has been used to obtain samples of rare populations and is being used more frequently in LGBT research. Respondent-driven sampling is similar to snowball sampling, defined later in the chapter, in that a sample is developed by using referrals from initial recruiters (seeds) and existing participants, from which estimates can be made about the social patterns of the study population. Those estimates are then used in
|
BOX 3-3 Drawing an Inference from Census Data Using data from the 2000 U.S. census, Black and colleagues (2007) were able to report on home ownership among cohabitating same-sex couples. They report that 60.4 percent of cohabiting male couples and 61.7 percent of cohabiting female couples owned their home (or were paying a mortgage). By comparison, 75.0 percent of heterosexual couples owned their home or were paying a mortgage. These data appear to be consistent with those from other sources (Herek et al., 2010). |
conjunction with data generated by the study to draw inferences about the population as a whole.
Respondent-driven sampling is limited in that it relies on a number of assumptions to enable those generalizable inferences (Kalton, 2009). For example, a theory of respondent-driven sampling developed by Volz and Heckathorn (2008) assumes that respondents accurately report the number of people linked to them in their social network, that they recruit others at random, and that they have reciprocal relationships with those they recruit. Most probability sampling methods do not require such assumptions. As a result, respondent-driven sampling is applicable mainly in examining small domains where clear social networks exist (Kalton, 2009).
Reisner and colleagues (2010) examined data generated by 74 original seeds from four Massachusetts studies conducted between 2006 and 2008 that used respondent-driven sampling to reach high-risk men who have sex with men. Thirty-four percent of seeds generated two or more subsequent participants. Analysis of the data indicated that the size of a participant’s social network was not significantly associated with generating additional participants. Social network size is frequently considered in developing a respondent-driven sample of men who have sex with men, but this study suggests that social network size alone is insufficient to identify participants who will recruit other participants. Factors such as the strength of social network ties and the frequency of a study-specific health behavior may be important as well.
Time-location sampling. This sampling approach uses multiple stages of data collection to increase the likelihood of developing a representative sample of the target study population, focusing on key social and behavioral characteristics. With community involvement, personal interviews with community leaders and gatekeepers and focus groups are included in an ethnographic assessment to generate an exhaustive list of sites where members of the target population congregate. A sample of the sites is drawn randomly for data collection, and specific time intervals are established when attendees are recruited for study participation. This method, described as venue-based, time-space sampling, has been used for studies of gay men and is one of the two methods employed by geographic sites within Centers for Disease Control and Prevention’s (CDC’s) National HIV Behavioral Surveillance program (Gallagher et al., 2007).
The strengths of this method include community participation that may result in a more comprehensive roster of potential sites than might otherwise be obtained and reduce suspicion among the study population. Its effectiveness depends on how well the ethnographic assessment is conducted, as well as the comprehensiveness and stability of sites in the initial roster (sampling frame). If probability-based methods are used at each stage
of implementation, inferences about the target population are possible. The Community Intervention Trial for Youth relied on this method to evaluate the effects of a multicomponent, community-level intervention to promote safer sexual behavior among men aged 15–25 who reported having sex with other men. The researchers identified locations or venues attended by the target population and at what times (days and time periods). They selected venues and time periods randomly and then systematically sampled members of the target population at those venues during those time periods. The collection of data from these participants allowed the researchers to draw inferences about the target population (Muhib et al., 2001).
Nonprobability Sampling
For a variety of reasons, including a historical lack of the resources needed to obtain probability samples of sexual and gender minorities, the majority of studies addressing topics relevant to LGBT health have been conducted using nonprobability samples (Herek et al., 2010). A nonprobability sample is one in which all elements of the target population do not have a known, nonzero chance of being included. Consequently, in contrast to probability samples, the sampling error associated with population estimates derived from nonprobability samples cannot be computed, and the extent to which the sample represents the population from which it was drawn cannot be known. In the worst cases, nonprobability samples based on extremely biased assumptions about the population can lead to highly inaccurate conclusions, as when findings from studies of sexual minorities in prison and clinical samples were used during the early twentieth century to depict homosexuality as a pathological condition (Herek, 2010; Meyer and Wilson, 2009). In recent years, however, investigators have used increasingly sophisticated methods for obtaining large and diverse community-based nonprobability samples that have provided numerous insights into the health of sexual and gender minorities (Binson et al., 2007; Herek et al., 2010; Meyer and Wilson, 2009).
An array of strategies can be used to create nonprobability samples, the choice of which depends on the study’s research question, data collection methods, and available resources. For example, venues such as bars and clubs, community events and organizations, Internet listservs, and social networks have often been used to recruit LGBT study participants (Herek et al., 2010; Meyer and Wilson, 2009). The samples drawn from such venues are often referred to as convenience samples, although Meyer and Wilson (2009) observe that “for most nonprobability sampling procedures, ‘convenience’ is a misnomer; nonprobability sampling requires very careful consideration, design, and execution” (p. 26). Whereas some researchers distinguish convenience samples from other types of nonprobability
samples, the term often is used to refer generally to any type of nonprobability sample (Binson et al., 2007). Throughout this report, the committee attempts to characterize each study’s sample using the terminology employed by the authors, with the consequence that convenience sample is used to refer to nonprobability samples obtained through a variety of techniques. Similarly, the terms community sample and community-based study are used in this report to refer to nonprobability samples that are obtained from a specific locale, such as a city or neighborhood. The various techniques for collecting nonprobability samples of LGBT populations, each of which can be understood as incorporating “some level of systematic exclusion and inclusion criteria” into the task of obtaining participants (Binson et al., 2007, p. 406), include purposive sampling, quota sampling, and snowball sampling.
Purposive sampling involves selecting specific sample elements because the researcher has reason to believe they are likely to provide the most useful information about the topic to be researched. For example, a study may select HIV-infected individuals to study behaviors that can lead to an increased risk of infection. Or researchers conducting a school-based study of LGBT adolescent health may include a particular high school in the sample because they believe it will yield especially valuable information. Diamond (1998), for example, recruited 89 nonheterosexual women aged 16–23 to participate in a longitudinal study of sexual identity development among young women. Participants were recruited at lesbian, gay, and bisexual community events; at classes on gender and sexuality issues at a large private university; and from lesbian, gay, and bisexual student groups at various universities. Of the 89 original participants, 79 participated in successive follow-up interviews over a period of 10 years. Two-thirds of those participants changed their sexual identity labels, and half did so two or more times (Diamond, 2008). This study made an important contribution to the discussion of sexual fluidity among women.
Quota sampling involves selecting a set number of participants to fill preestablished categories as a means of increasing the sample’s variability or diversity (Binson et al., 2007). The researcher may begin by identifying the target number of sample elements in each of several categories (based on, for example, demographic groupings such as gender, race, and ethnicity). The goal may be to have a final sample in which the proportions of various key groups resemble the population from which the elements were drawn or to oversample relatively uncommon groups. Participants are then recruited to fill the various “quotas.” Kennamer and colleagues (2000) used quota sampling to develop a sample of more than 700 Caucasian and African American men who have sex with men in order to conduct a statewide survey of HIV-related knowledge, behaviors, and attitudes in Virginia. The purpose of this study was to provide information for public
health planning with respect to the HIV risks of men who have sex with men. As men who have sex with men were largely hidden, no population data were available from which to sample. Using population estimates from statewide and regional census information, the research team created target sizes for regional-level samples and used community and venue recruitment to identify participants. Additional efforts were made to recruit African American men who have sex with men, who tend to be underrepresented in surveys. The results assisted public health planners in determining regional allocations for HIV education and prevention programs. Although the study data would not be applicable to another state or geographic area, information about the methodology could be helpful to others considering such a study.
Snowball sampling relies on an initial core group of participants to recruit others into the study through their social networks; those individuals, in turn, may be asked to recruit additional participants from their networks, and so on (Binson et al., 2007; Meyer and Wilson, 2009). Sample development begins when members of the target population are identified and selected as seeds who will distribute surveys to or identify others who meet the study’s inclusion criteria. This method was used prominently in early studies of sexual and gender minorities and continues to be applied when previously unstudied population groups are engaged in research. Like respondent-driven sampling (discussed earlier in this chapter), snowball sampling is a chain-referral method. Unlike respondent-driven sampling, however, it does not involve the use of probabilistic procedures for sample selection.
Many studies of sexual and gender minorities with large nonprobability samples have used a combination of the above and related methods (e.g., Bell and Weinberg, 1978; Herek et al., 1999; Kennamer et al., 2000; Martin and Dean, 1990; Meyer et al., 2008; Morris and Rothblum, 1999). The National Lesbian Health Care Survey (NLHCS), for example, conducted in 1984–1985, developed a national study of self-identified lesbians across the United States (Solarz, 1999). A community effort throughout, the NLHCS used snowball sampling strategies by organizing groups of women across the country to distribute questionnaires to other lesbians. Notices about the survey were posted across the country in bookstores and other locations frequented by lesbians, and a study phone number was provided for those with questions or concerns. Women who self-identified as lesbians were eligible to participate (Bradford et al., 1993). Each questionnaire was numbered and coded to enable identification of the initial and secondary distributors, such that the researchers could track them from the original distribution location through a second and sometimes third handler. NLHCS data were the earliest to suggest that lesbians experienced higher-than-expected rates of sexual abuse and stress-related behaviors, such as
alcohol use and mental health support. The extent to which lesbians were open about their sexual orientation was associated with greater availability of mental health services (Bradford et al., 1993). At a time when lesbians were largely hidden, the study results provided a base of information from which successive studies employing more rigorous sampling methods could be developed.
Another creative use of sampling methods is demonstrated by studies that have recruited sexual- and gender-minority participants through various nonprobability methods and then asked sample members to recruit other participants who meet specific criteria. For example, Rothblum and Factor (2001) placed advertisements in local and national periodicals to recruit lesbians with at least one female sibling. Eligible women who responded to the ad were sent two copies of a questionnaire, one for them to complete and the other for their sister (the questionnaires did not indicate that the study focused on lesbians). Although the representativeness of the sample could not be known, the researchers were able to compare lesbians with heterosexual “controls” from highly similar backgrounds on multiple health variables. Similar sibling-control studies have been conducted with gay men and bisexuals (Rothblum et al., 2004) and with same-sex couples (Balsam et al., 2008).
The National Transgender Discrimination Survey (NTDS), conducted by the National Center for Transgender Equality and the National Gay and Lesbian Task Force, distributed online links to the survey site through a network of more than 800 transgender-serving and transgender-led advocacy and service organizations, support groups, listservs, and online social networks; 2,000 paper surveys were distributed to difficult-to-reach transgender and gender-nonconforming respondents, resulting in a total sample of 6,450 (Grant et al., 2010). Characteristics of this sample closely resembled a convergence of findings from a growing number of convenience studies conducted across the country, primarily in urban centers or at the state level. NTDS results pointed to critical concerns regarding unemployment and economic insecurity; employment challenges; and barriers to health care, such as a lack of health insurance and culturally competent providers (Grant et al., 2010).
Well-designed nonprobability studies have been useful for local and state-level health access initiatives. In 2004–2005, the Virginia Department of Health’s HIV Prevention Community Planning Group drew on findings from existing nonprobability transgender health surveys to develop the Virginia Transgender Health Initiative Survey (THIS). This policy-oriented health assessment study used focus groups to determine constructs for a statewide survey of transgender people and to gather information about regional differences that could affect survey distribution methods. A questionnaire was developed and distributed through community outreach efforts at
local and regional locations, including health care providers’ offices, LGBT events, and balls and house parties. It was also made available on a protected website. At a time when few transgender studies had been conducted, and none at the state level, it was critical for community representatives, experienced scientists, and public health officials to craft an approach that would be useful and accepted in the context within which they were working (Xavier et al., 2005, 2007). Study results were used to increase awareness of transgender health needs, resulting in expanded services throughout the public health system.
Even though the extent to which their findings accurately characterize the entire LGBT population is unknown, studies based on nonprobability samples have yielded valuable information for expanding the field of LGBT research and addressing health service gaps (see Box 3-4). In addition to providing general descriptive data for LGBT populations and subgroups, they have served to demonstrate the existence of phenomena; to test experimentally the effectiveness of various behavioral and medical interventions; to assess relationships among study variables; to identify differences among groups; and in general, to provide insights into the health-related challenges faced by LGBT populations.
In addition, in the absence of data from probability samples, researchers often develop approximations of population patterns when the findings from multiple methodologically rigorous studies with different nonprobability samples converge. During the 1990s and 2000s, for example, multiple studies using nonprobability samples suggested that lesbians were considerably more likely than gay men to report that they were in a committed relationship at the time of data collection (e.g., Kurdek, 2004). Data from the U.S. census and a national probability sample confirmed this pattern (Gates, 2009; Herek et al., 2010).
Data Collection: Quantitative and Qualitative Methods
In addition to selecting an appropriate sampling frame, a major methodological concern is choosing quantitative or qualitative data collection methods.
Quantitative Data Collection Methods
Quantitative data collection methods include traditional survey research, Internet/online surveys, randomized controlled trials (RCTs), longitudinal cohort studies, and use of patient-level data.
Survey research. Survey methods are commonly used in LGBT health studies and are particularly valuable for determining population demographic
|
BOX 3-4 Examples of the Use of Nonprobability Sample Surveys to Address Transgender Health National Transgender Discrimination Survey (NTDS) The NTDS gathered data from self-identified transgender or gender-nonconforming individuals in the first national effort to document discrimination found in previous small sample studies and anecdotal reports. A 6-month data collection effort online and with paper surveys generated a total sample of 6,450, distributed across the United States in a pattern that closely replicated that of same-sex households in the 1990 and 2000 census data. Whites and persons of color were represented in proportions similar to those in the 2007 American Community Survey (ACS): whites made up 75.1 percent of the ACS sample and 76 percent of the NTDS sample; 24.9 percent of the ACS sample and 24 percent of the NTDS sample, respectively, were people of color (combined racial and ethnic categories). Consistent with results of numerous earlier studies, 26 percent of respondents reported having lost their job because they were transgender or gender-nonconforming. Black (32 percent) and multiracial (37 percent) respondents were particularly hard hit. Harassment or mistreatment on the job was reported by 97 percent of respondents. Compared with the general population, 62 percent of whom had access to employer-based insurance, this was the case for only 40 percent of NTDS respondents. Other prominent concerns related to transgender status included poverty and housing instability. Describing transgender identification: “Transgender/gender non-conforming” describes people whose gender identity or expression is different, at least part of the time, from the sex assigned to them at birth.
Virginia Transgender Health Initiative Survey Focus groups were conducted to determine constructs for a statewide survey and to gather information about regional differences that could affect survey distribution methods. After considering various methods, including respondent-driven sampling, the statewide team decided on a mixed-method approach. A quantitative survey was available on a protected website and in paper-and-pencil form at local and regional locations, including health care providers’ offices, LGBT events, |
|
balls and house parties, community outreach venues, and transgender listservs. A $15 incentive was provided for completed surveys, using blank money orders sent to a name and location stated by the respondent. A total of 367 self-identified transgender individuals completed the survey. Across the state, 61 percent responded online, while 39 percent completed paper surveys. Characteristics of the subsamples differed by race/ethnicity, type of community (urban, suburban, rural), living alone or with others, home ownership, health insurance, and disclosure of gender nonconformity to primary care provider. If either method had been used alone, a distorted description of the target population would have resulted. Describing transgender identification: For the purposes of this study, we consider you to be transgender if you:
If you answered yes to all three of these questions, please continue. |
and sociocultural characteristics, assessing knowledge and opinions, assessing behavior and behavioral intentions, and gathering data to describe the distribution of health conditions among populations and subpopulations. When a survey is used to gather information about a target population, it is important to assess the quality of the survey data to determine how useful the data are for drawing inferences about that population. Defined sources of error can and do affect all studies involving data collection, and researchers must strive to minimize their impact on the study results. A classification of error sources in data collection systems provides a framework with which analysts can evaluate the limitations of their data.
Survey data are subject to (1) the error inherent in examining a portion of the population (as opposed to surveying every individual of that population) and (2) errors that occur as a result of data collection procedures. Theoretically, the quality of survey data can be assessed in terms of total survey error, which is a combination of those two general sources of error, known as sampling error (when probability sampling methods are used) and nonsampling error (Biemer, 2010).
When a probability-based sample is used, sampling error refers to the error that occurs when the researcher draws a sample of a population using a probability-based mechanism rather than surveying every member of that population (Biemer, 2010; OMB, 2001). The sampling error associated with an estimate is a measure of the estimate’s precision. Sampling error occurs by chance and is based on the random selection scheme used. The amount of expected variance due to sampling decreases as the size of the sample increases.
Nonsampling error refers to error that originates in the limitations of the data collection methods and procedures used in a study. This type of error may occur through a number of data collection mechanisms and is not easily quantified. Nonsampling error can be divided into four major categories: coverage error, nonresponse error, measurement error, and processing error (Biemer, 2010; OMB, 2001). See Table 3-1 for examples of these sources of error.
Coverage error occurs when members of the target population are excluded from the frame population, when members outside of the target
TABLE 3-1 Sources of Nonsampling Error in Survey Research
|
Coverage Error |
Associated with differences between the target population (a set of characteristics defining the population to be studied) and the sampling frame population. Example: In a random-digit dialing survey that sampled only land lines, lesbians with cell phones but not land lines would be excluded. |
|
Nonresponse Error |
Occurs when study participants fail to answer survey questions, either completely or in part. Example: Questions relating to sexual behavior or gender nonconformity are at risk for nonresponse because of participants’ reluctance to reveal information about such private behavior. |
|
Measurement Error |
Relates to the logistics of data collection—the influence of how and in what settings questions are asked—and comes from four major sources: the questionnaire, the data collection method, the interviewer (if used), and the respondent. Because of the unpredictable nature of these factors, measurement error has the most potential to reduce data quality. Example: When sensitive questions are included, a private setting can facilitate accurate reporting. |
|
Processing Error |
Occurs in the handling and use of information generated through the data collection process. Example: Quality control measures are not routinely carried out, or not all errors that are found are corrected. |
population are included in the frame population, and when members of the target population are included in the sampling frame more than once (OMB, 2001). In the case of random-digit dialing telephone surveys, for example, low-income individuals and those living in rural areas may be disproportionately excluded as they are more likely to live in a household without a telephone line (Galesic et al., 2006). More recently, the exclusion of households without a land-line telephone has exacerbated the coverage error of random-digit dialing surveys and resulted in the need to include a cell phone sampling frame in addition to the land-line telephone sampling frame.
Nonresponse error takes two forms. Unit nonresponse refers to cases in which a particular sampling unit (e.g., household, person, business) fails to respond to all parts of a questionnaire. Item nonresponse occurs when a respondent provides some of the requested information but leaves certain questions unanswered or provides responses that are inadequate for use. Nonresponse errors can result in biased survey estimates if there are relevant differences between those who respond to a questionnaire (or a particular question) and those who do not. Item nonresponse can be a significant factor for questions that are sensitive in nature.
Measurement error relates to the processes involved in data collection. These processes include the questionnaire design, important for receiving an accurate response; question wording or survey instructions, which if ambiguous lead to incorrect responses; and the way the questionnaire is formatted. Data collection methods have been shown to influence responses; for example, in-person interviews may generate more accurate information than telephone interviews, while reporting on sensitive topics may be improved when the interview takes place over the telephone because of the anonymity of the interviewee. Interviewers vary in how they ask questions and administer the interview, affecting respondents’ answers. Respondents can also be a source of error: they may differ in their comprehension of questions and in their memory of past events; they also may provide incorrect responses to questions, intentionally or unintentionally.
Processing error stems from inconsistencies or oversight during the handling and use of data generated through the data collection process (OMB, 2001). Such errors may take place when survey-generated data are transformed into published statistical results; when responses to survey questions are recorded incorrectly; and during data entry, when collected data are transferred to an electronic medium. More complicated errors can arise in applying mathematical algorithms to survey data in order to account for other sources of error; imputation, for example, is sometimes used for generating values to replace missing or erroneous data to facilitate analysis (Brick and Kalton, 1996; Kalton and Kasprzyk, 1986). Such errors can also occur in population-based studies in which probability-based
sample designs apply sampling weights to account for frame coverage, nonresponse, and sampling probabilities. Errors can occur in modifying data in these ways and can affect the results of the study.
Internet/online surveys. Internet surveys have numerous advantages over traditional survey methods. Data collection and coding can be completed rapidly over a large geographic area at a relatively low cost per survey. Because they are computer-based, moreover, Internet surveys allow for many capabilities not readily available with paper questionnaires, such as complex skip patterns, branching, and the inclusion of video and audio (e.g., Dillman et al., 2009). And the anonymity and accessibility of the Internet make it a particularly good medium for conducting sexuality research among otherwise underrepresented populations (Mustanski, 2001).
As a data collection mode, the Internet can be used with probability or nonprobability samples, depending on the existence of a sampling frame and the use of a probability-based method of sample selection (Couper, 2000). In organizational settings where Internet access is provided, such as academic and health care institutions, a sampling frame of research participants may be generated using personnel records, and members of the sample may be asked to complete a questionnaire online. Other methods, such as random-digit dialing, can also be used to obtain a probability sample for an Internet study if Web access is ensured for all. For example, Knowledge Networks has used random-digit dialing techniques to recruit members of an ongoing panel; Internet access and equipment are provided to panel members who lack them.
Most Internet studies, however, rely on nonprobability samples recruited through a variety of means. Samples recruited from the Internet are subject to bias because those without Internet access are excluded. In addition, the characteristics of individuals more likely to respond to Internet surveys could differ from those of the general population (Rosser et al., 2009). For instance, Internet survey participants may be more likely than respondents recruited in other venues to seek sexual partners online (Bolding et al., 2007). On the other hand, given that survey data gathered online reflect only the individuals who complete the survey, the data obtained may not reflect the complete population of individuals using the Internet to seek sexual partners. Studies of Web surveys conducted among men who have sex with men in the United States and the United Kingdom also have found that certain variables were associated with higher rates of questionnaire noncompletion in online sexuality research; these variables include nonwhite ethnicity, less openness about sexual orientation, self-identifying as heterosexual or bisexual, and in some cases younger age (Evans et al., 2008; Ross et al., 2004).
As with other nonprobability sampling methods, Internet-based research with samples of volunteers faces some special challenges related to the in-
ternal validity of the data. Verifying participants’ identities can be difficult, raising concern about the honesty of responses and the possibility of multiple submissions from the same respondent. (It should be noted that similar problems arise in studies that distribute paper questionnaires throughout a community, such as in newspapers or magazines.) A number of solutions have been proposed for this problem, including directly asking participants not to respond more than once, collecting e-mails or Internet Protocol (IP) addresses, and placing tracking “cookies” (units of information stored by a user’s Web browser) on the computers of individuals who have responded (Reips, 2000). While these strategies offer partial solutions, the collection of e-mail and IP addresses and the use of cookies also raise other methodological and ethical concerns (Mustanski, 2001; Riggle et al., 2005).
With the increasingly widespread use of Internet and mobile phone technology, it is worth noting that emerging technologies can play a role not only in recruitment of study participants but also in many other areas of research (e.g., surveillance, interventions, clinical trials). Technologies such as text messaging, e-mailing, web-based interventions, and geographic information systems are currently being used to identify and reach at-risk populations and offer promising opportunities for future studies (for example, see Bowen et al., 2008; Carpenter et al., 2010; Geanuracos et al., 2007).
Randomized controlled trials. Since the work of Fisher (1925) was published, it has been recognized that randomization lends credibility to estimates of causal relationships that cannot be matched by other research designs. RCTs measure an intervention’s effect by randomly assigning individuals (or groups of individuals) to an intervention group or a control group. In health research, RCTs typically are used to assess the efficacy of a behavioral or clinical intervention, such as in a drug trial, or participation in a risk reduction program.
While RCTs, at their best, can have high internal validity, concerns invariably remain with regard to external validity. For example, a particular AIDS treatment that is found to be effective in an RCT conducted with middle-aged white men in the United States might be less effective for other subpopulations. An RCT of the efficacy of a behavioral intervention to prevent the acquisition of HIV among men who have sex with men in six U.S. cities over a period of 48 months, known colloquially as the EXPLORE study, used HIV infection as the primary efficacy outcome (HIV Prevention Trials Network, 2011). In a sample of 4,295 participants, 39.7 percent reported having a history of childhood sexual abuse (Mimiaga et al., 2009). In prior studies, rates of childhood sexual abuse reported by men who have sex with men ranged from 11 to 37 percent (Brennan et al., 2007), while the rate of such abuse among the general population of men had been estimated at 5 to 10 percent (Finkelhor, 1994). Analysis of data
from EXPLORE showed that childhood sexual abuse was highly associated with HIV risk-taking behavior and infection among men who have sex with men who participated in the study.
Even when RCTs are impractical, their basic principles can be extended to other research. Suppose one wants to evaluate the effectiveness of a community-based training program designed to help LGBT high school dropouts transition to employment. Researchers clearly cannot establish credible estimates of a “treatment” (completion of the program) by comparing subsequent employment rates of program participants with those of nonparticipants. After all, youths with high motivation are more likely to stay with the program than youths with low motivation. Researchers might, however, credibly estimate the impact of the program by comparing employment rates of youths in neighborhoods where the program was made available (the “treatment” group) with those of youths in otherwise comparable neighborhoods that had no training program (the “control” group). Such credible program evaluations are important for understanding the treatment effects of social programs, and can be conducted even when the “treatment” choice (the neighborhood choice for the employment program) is not randomly assigned as in a proper RCT.
CDC’s Diffusion of Effective Behavioral Interventions (DEBI) program is an example of how RCTs are being used to determine the most effective of two or more community-level or population-specific interventions. DEBI is a national-level strategy to provide high-quality training and ongoing technical assistance to state and community HIV/sexually transmitted infection (STI) program staff for selected evidence-based prevention interventions that focus on HIV, other STIs, and viral hepatitis. Initiated in 1999, the program includes evidence-based behavioral interventions identified in the 2009 Compendium of Evidence-Based HIV Prevention Interventions, which were evaluated through a series of efficacy reviews, many of which involved RCTs (CDC, 2009). Development of a model for adapting evidence-based prevention interventions to groups not initially studied was initiated in 2004 (McKleroy et al., 2006). This effort supported increased funding for adapting and culturally tailoring evidence-based prevention interventions initially designed for gay men for use with other affected population groups.
Implementation of the DEBI program has been critically reviewed in the context of dissemination and technology transfer. Dworkin and colleagues (2008) emphasize the importance of adaptation and dissemination as a participatory process and conclude that additional strategies are needed to ensure that the experience and assistance of community stakeholders are effectively represented.
The view of RCTs as the gold standard for measuring an intervention’s impact extends across many diverse fields of human inquiry, such as educa-
tion, welfare and employment, medicine, and psychology. The impact of an intervention can be evaluated only for populations participating in these trials. A letter to the New England Journal of Medicine suggests that sexual minorities have, at times, been explicitly excluded from such trials (Egleston et al., 2010). There is a need for peer-reviewed research to explore this topic further. The inclusion of LGBT participants in efficacy trials of treatment interventions would help ensure that the needs of these populations are reflected in such research.
Longitudinal cohort studies. Longitudinal studies are often used in psychology to study developmental trends across the life span, in education to assess the outcomes of education or training, in sociology to study life events throughout lifetimes or generations, or in economics to study behavioral and attitudinal data on social and economic issues (Kasprzyk et al., 1989; Lynn, 2009). Unlike cross-sectional studies, longitudinal studies track the same analytic units, usually individuals, over time. Therefore, analyses of unit-level changes and analyses of the frequency, timing, or duration of specific events are of interest. The advantages of such studies are discussed by Lynn (2009). By providing repeated measures on the same characteristics and following the same individuals, these studies can observe changes more accurately than other approaches and develop an extensive set of analytic variables. One of the challenges with longitudinal studies is recruitment. LGBT participants are members of small populations and not always easy to identify. Another challenge is retention of participants. Since studies span a number of years, participants may move, lose interest, or otherwise become unreachable by researchers. In medicine, the design is used to uncover predictors of certain diseases. Results from longitudinal cohort studies have made a significant contribution to the understanding of LGB health concerns. Longitudinal designs may be employed with probability as well as nonprobability samples, the data may be qualitative or quantitative, and data collection can utilize any of the methods discussed in this chapter. Some examples of longitudinal cohort studies are presented in Box 3-5.
The Nurses’ Health Study (NHS), initiated in 1976 by Dr. Frank Speizer, and the NHSII, initiated in 1989 by Dr. Walter Willett, are the most definitive long-term epidemiological studies conducted to date on older women’s health. Married registered nurses who were aged 30–55 in 1976, who lived in the 11 most populous states, and whose nursing boards agreed to supply the researchers with their members’ names and addresses were enrolled in the cohort if they responded to the baseline questionnaire. Approximately 122,000 nurses out of the 170,000 who received the questionnaire by mail responded. For the NHSII, the target population was women aged 25–42 in 1989. Over time, additional questions have been added, most notably a dietary assessment added to the original NHS in 1980. Sexual orientation
|
BOX 3-5 Examples of Longitudinal Cohort Studies Nurses’ Health Study, initiated in 1976, and Nurses’ Health Study II, initiated in 1989 Cohort participation has been carefully maintained. Deaths, usually reported by kin or by postal authorities, have been followed up. Where possible and permitted, in cases suggestive of cardiovascular disease or coronary heart disease, the follow-up has gone beyond examining death certificates to include gathering available documentation from autopsy reports and other records. Mortality follow-up has been better than 98 percent. The core NHS sample consisted of 121,700 female registered nurses. In 1995, when sexual orientation was measured, the sample size was 90,823. Sexual Orientation Question Whether or not you are currently sexually active, what is your sexual orientation or identity? (Please choose one answer). Heterosexual; Lesbian, gay or homosexual; Bisexual; None of these; Prefer not to answer. Growing Up Today Study (GUTS) GUTS is a longitudinal cohort study of adolescent girls and boys living throughout the United States. Study participants were recruited in 1996 from among NHSII participants who reported having at least one child aged 9–14. Sexual orientation was captured in 1999 with a sample size of 16,800. Sexual Orientation Question Which one of the following best describes your feelings? (1) Completely heterosexual (attracted to persons of the opposite sex); (2) mostly heterosexual; (3) bisexual (equally attracted to men and women); (4) mostly homosexual; (5) completely homosexual (gay/lesbian, attracted to persons of the same sex); and (6) not sure. SOURCES: Channing Laboratory, 2011a,b. |
was not assessed at study initiation but was added in 1995 in the NHSII (Case et al., 2004).
Corliss and colleagues (2008) analyzed data on 13,450 youth who had been followed for 7 or more years in the Growing Up Today Study (GUTS), a community-based prospective cohort study of adolescent girls and boys living throughout the United States. The researchers recruited 16,882 study participants in 1996 by identifying NHSII participants who reported having at least one child aged 9–14. A mail survey was used to collect data.
Use of patient-level data. Coupled with national health care reform initiatives, the growing awareness of health disparities among LGBT people
and concerns about barriers to their care have generated increased attention to the importance of identifying sexual and gender minorities within patient populations. Although the rationale for collecting these data may be increasingly clear, the best ways to do so have not yet been clarified. Organizations that focus on services for LGBT people typically utilize information about sexual orientation entered within the patient’s record by the physician; the physician may not be required to check a category that will become part of the patient’s enduring record. Thus, disclosure is kept between patient and provider, and it is up to the patient to determine whether to share this information.
Gathering data about patients’ sexual orientation and/or transgender identity has been a subject of considerable interest for at least a decade. In 2001–2002, an urban federally qualified health center with a specific focus on serving the LGBT community conducted a pilot study in which patients were asked at intake to complete a voluntary one-page survey that included sexual orientation and gender identity questions (Barrett et al., 2002). Respondent demographics closely matched those of the overall patient population. Information from this study was valuable for organizational management and development, leading to an ongoing discussion about the best way to gather this information on a routine basis without endangering the privacy of patients. With recent improvements in database design and the expectation that such data will be increasingly important for tracking services to this population, the health center has added sexual orientation measures to the standard patient-registration form. To identify transgender patients, the question “Do you identify as a transgender person?” was added 3 years ago, following the legal sex question with “male” or “female” options.
In 2010, the Joint Commission on Accreditation of Healthcare Organizations published the monograph Advancing Effective Communication, Cultural Competence, and Patient- and Family-Centered Care: A Roadmap for Hospitals to help hospitals integrate the concepts of effective communication and patient-centered care into their organizations. This monograph contains several recommendations specific to LGBT populations and identifies best practices and processes that can assist hospitals in meeting the needs of their LGBT patients (The Joint Commission, 2010). New accreditation requirements have been developed to assess hospital performance, including two that are specifically relevant to the care of LGBT people: the first addressing the patient’s right to choose his or her support individuals; the second addressing prohibition of discrimination, encompassing that based on personal characteristics, including “sexual orientation and gender identity or expression.” These new requirements will count toward a hospital’s accreditation decision beginning July 1, 2011 (The Joint Commission, 2011).
As awareness of the health-related needs of LGBT people grows, it is reasonable to expect that opportunities for collecting patient-level data for these populations will continue to emerge. For example, the Agency for Healthcare Research and Quality’s Practice Based Research Networks could be one way to collect, analyze, and disseminate data on LGBT health. It is also reasonable to expect that the inclusion of sexual- and gender-minority measures in databases will increase. Consistent with the overall thrust of this chapter, it will be important for standard measures to be developed and implemented according to procedures that have been tested and found effective for ensuring privacy and confidentiality at all levels of health care organizations, including education of patients and their support persons, as well as providers and administrators. The use of patient-level data holds great potential for yielding a better understanding of the health status and health-related needs of LGBT people and how these differ from those of other groups in the U.S. population.
Qualitative Methods
Qualitative research methods can bring unique strengths to efforts to understand LGBT health. Examples of qualitative research include one-on-one interviews, focus groups, and cognitive interviews. Qualitative studies cannot be used to assess the characteristics of an entire population, but they do allow for a more detailed account of individuals’ experiences as members of LGBT populations (Binson et al., 2007). These accounts can help a researcher identify hypotheses that could be tested in another study and lay the groundwork for future research. This type of perspective is ordinarily unavailable from sample survey based research. In addition, qualitative research can assist in developing quantitative instruments for studying LGBT populations. Qualitative methods are particularly well suited to
-
explore understudied areas of inquiry, social settings, behaviors, or groups;
-
build knowledge of key issues to refine elements of research designs for subsequent quantitative study;
-
understand thought processes, experiences, or meanings of phenomena;
-
describe and explain complexity and situational context in lived experience; and
-
generate novel understandings and formulate explanations of patterns of human experience.
In studies of LGBT health, qualitative research is particularly relevant in exploring and explaining meanings of sexual- and gender-minority status
in specific, local, and historical contexts of lived experience. Qualitative methods, both on their own and in conjunction with quantitative methods, are essential tools for understanding LGBT health.
One-on-one interviews. One-on-one interviews can vary from structured interviews typically used by survey researchers to less structured interviews that tend to be used by researchers who collect qualitative data (Bates et al., 2008). In structured interviews, the interviewer follows scripted questions, with no deviations from a set order; in semistructured interviews, the interviewer initiates questions and probes in response to the participant’s answers, and questions may be reordered; and unstructured interviews are like a free-flowing conversation, with no set order to any questions—the interviewer may answer questions and make clarifications and may add or delete questions between interviews. Qualitative interviews are a good choice when the research aims are to shed new light on puzzling questions, identify variables and frame hypotheses for future survey research, and unravel complex events and events that evolve over time. Jarama and colleagues (2007) used random-digit dialing to recruit a probability sample of black women to undergo personal interviews conducted by trained peers. The purpose of the interviews was to have participants describe in their own words their perceptions of HIV risks and how they were taught to think and behave about sexuality. Each of the interviews was guided by a common set of questions; while some interviews followed the questions in order, others took their own direction, circling back to cover questions that were not answered in order. Peer interviewers had been carefully trained to ensure that study data would be collected from each interview and in a manner that respected the flow of each participant’s thought process and mode of expression.
Focus groups. Focus groups are often used as one component of a mixed-methods study in which the goal is to obtain quantitative data on a target population. During the first phase of the Virginia Transgender Health Initiative Study, for example, regional focus groups were conducted to inform the content of a phase two statewide survey of self-identified transgender residents. A team of facilitators including transgender researchers and community advocates was trained to conduct the interviews, which were developed in conjunction with a statewide task force created to guide and support the initiative. Results were disseminated to communities, and after feedback was received from community and professional audiences, the focus group findings were used in developing a conceptual framework and questions for the phase two statewide quantitative survey (Xavier and Bradford, 2005; Xavier et al., 2007). In another example, the Census Bureau recently used 18 focus groups distributed over seven locations to help develop a better
understanding of how gay and lesbian couples think about and report their relationship and marital status (Bates et al., 2010).
Cognitive interviews. The cognitive interviewing approach to evaluating sources of response error in survey questionnaires was developed during the 1980s through an interdisciplinary effort involving survey methodologists and psychologists (NRC, 1984). This approach has the following general features (Willis, 2004):
-
It focuses mainly on the questionnaire rather than on the entire survey administration process. That is, the focus is on survey questions, as opposed to administrative procedures such as computer-administered personal interviewing, mentioned earlier in this chapter.
-
It focuses explicitly on the cognitive processes that respondents use to answer survey questions. Therefore, covert processes that are normally hidden, as well as overt, observable processes, are studied.
-
For the conduct of the cognitive interview, volunteer subjects are recruited and are interviewed either in a laboratory environment or in some other private location. (In this application, the term “subject” refers to an individual who is tested through a cognitive interviewing procedure, and “respondent” defines someone who is interviewed in a fielded survey.)
-
The recruitment of subjects targets persons with specific characteristics of interest (for example, the elderly, those who have used illicit drugs in the past 12 months, teenagers who have used chewing tobacco).
Clark and colleagues (2005) used cognitive interviews of a sample of 40 women to evaluate survey questions designed to measure sexual orientation and gender expression. Results of the interviews helped identify questions that may have been confusing to respondents and specific terms that needed additional clarification. Cognitive interviews are currently being used by the National Center for Health Statistics to develop and test measures for including LGBT questions on federal surveys.
DATA SOURCES
The relative lack of population-based data presents the greatest challenge to describing the health status and health-related needs of LGBT people. Although recommendations have been made for some time about collecting data on sexual and gender minorities (Westoff, 1973), only a limited number of publicly funded probability sample studies include measures
of sexual orientation, and none measure gender identity. In 2000, Healthy People, the nation’s health promotion and disease prevention program (HHS, 2000), included people defined by sexual orientation as a population group experiencing health disparities. At that time, only two federally funded data sets (the National Health and Nutrition Examination Survey and the National Household Survey on Drug Abuse) included measures of sexual orientation. Secondary analysis of these data sets was prominent in calling attention to significant differences in reported rates of mental health and substance abuse between LGB people and heterosexuals (Cochran and Mays, 2000; Cochran et al., 2000, 2004). In the past decade, sexual orientation measures have been included in additional federally funded surveys. Recurring federally funded surveys that include LGB measures are listed and their properties described in Table 3-2.
Not surprisingly, the limited number of studies that have used probability samples and rigorous methods and focused on sexual and gender minorities has contributed to the lack of an extensive published literature on LGBT health. A Medline database review of literature published during 1980–1999 found that only 0.1 percent of articles over this 20-year period had focused on LGBT people or same-sex behavior or attraction (Boehmer, 2002). This percentage is based on the contents of the entire Medline database; the study identified 3,777 articles that met its inclusion criteria. Most of these articles were focused on HIV/AIDS, substance abuse, and mental health to the exclusion of other topics (Gay and Lesbian Medical Association and LGBT Health Experts, 2010). Since 2008, the Center for Population Research in LGBT Health has maintained a publicly accessible bibliography of published literature on LGBT health, including journal articles, books, and reports published since 1990 and indexed in PubMed. As of this writing, the programmed search has yielded 12,928 journal articles. A chart of the number of publications meeting search criteria suggests an increase in annual scholarly output in LGBT health research, particularly in the last decade; when charted as a ratio of all PubMed2 journal articles, however, growth in scholarly output in LGBT health appears to have been slower and more uneven (Figure 3-1).
BEST-PRACTICE PRINCIPLES ASSOCIATED WITH SAMPLE SURVEY AND RESEARCH STUDIES
Scientific and methodological challenges exist in the design and implementation of most sample surveys and research studies. This is
TABLE 3-2 Recurring Federally Funded Surveys That Include LGB Measures
|
Name/Study Website |
Sexual Orientation/ Gender Identity Measures |
Periodicity |
Sample Size |
Data Collection Mode |
Topic Areas |
|
American Community Survey |
Same-sex partner household |
Annually |
2009: 2,064,000 households |
Vary from year to year; for more information about subjects covered: census.gov/acs/www/data_documentation/pums_documentation/ |
|
|
Behavioral Risk Factor Surveillance Systemd |
Varies by state; states have included identity, behavior, transgender identity |
Annually |
Varies by state |
Telephone (CATI) |
Health risk behaviors, preventive health practices, and health care access related primarily to chronic disease and injury |
|
Current Population Survey |
Same-sex partner household |
Monthly |
2010: 97,263 households |
Personal visits (CAPI), telephone (CATI) |
Work status, earnings, hours of work, and other employment indicators; supplemental questions on diverse topics such as expectation of family size, tobacco use, computer use, and voting patterns are sometimes added |
|
General Social Survey |
Identity, behavior, same-sex partner household |
Annually; sexual orientation only in 2008 |
2008: 2,000 individuals |
Personal visits (CAPI) |
Includes a standard “core” of demographic, behavioral, and attitudinal questions, plus topics of special interest |
|
National Epidemiologic Survey of Alcohol and Related Conditions |
Identity, behavior, attraction |
Wave 1: 2001–2002; Wave 2: 2004–2005 (longitudinal) |
43,100 individuals |
Personal visits (CAPI) |
Alcohol and drug use; alcohol and drug abuse and dependence; associated psychiatric and other medical comorbidities |
|
National Health and Nutrition Examination Survey |
Identity, behavior |
Annually |
2007–2008: 10,149 individuals |
Personal visits (CAPI), health examination |
Disease and chronic conditions, health risk factors, smoking, alcohol consumption, sexual practices, drug use, physical fitness and activity, weight, dietary intake, and reproductive health |
|
National Health Interview Survey |
Same-sex partner household |
Annually |
2009: 33,856 households |
Personal visits (CAPI) |
Demographics, health status and limitations, injuries, health care access and utilization, health behaviors, health insurance, and income and assets |
|
National Household Survey on Drug Abuse |
Behavior |
Annually; sexual orientation assessed only in 1996 |
1996: 18,300 individuals |
Personal visits (SAQ until 1999, ACASIe thereafter) |
Use of illicit drugs, alcohol, and tobacco; substance abuse treatment history; illegal activities; mental health; access to care; driving behavior; and demographics |
|
National Survey of Family Growth |
Identity, behavior, attraction |
7 cycles collected since 1973; only the 2002 cycle included sexual orientation |
2002: 12,600 individuals |
Personal visits (including CAPI, ACASI, and interviewer observations) |
Schooling, family background, marriage and divorce, fertility, family planning, sex education, sexual history, sexually transmitted diseases (STDs)/AIDS, and demographics |
|
United States Census |
Same-sex partner household |
Decennially |
2000: 115.9 million households |
Mail (SAQ), personal visit follow-up |
Age, sex, race, household relationships, tenure; the American Community Survey replaced the “long form” on the census |
|
Name/Study Website |
Sexual Orientation/ Gender Identity Measures |
Periodicity |
Sample Size |
Data Collection Mode |
Topic Areas |
|
Youth Risk Behavior Surveillance Systemf |
Varies; states have included identity, behavior, attraction, transgender identity |
Biennially |
Varies |
SAQ |
Adolescent health risk behaviors, including behaviors that contribute to unintentional injuries and violence, tobacco use, alcohol and other drug use, sexual behaviors that contribute to unintended pregnancy and STDs, unhealthy dietary behaviors, and physical inactivity |
|
NOTES: a SAQ = self-administered questionnaire. b CATI = computer-assisted telephone interview. c CAPI = computer-assisted personal interview. d Locations that have historically measured sexual-minority status include Arkansas, California, Colorado, Connecticut, Georgia (Fulton County), Massachusetts, New York City, North Dakota, Ohio, Oregon, San Francisco, Vermont, Washington, and Wisconsin. e ACASI = audio computer-assisted self-interview. f Locations that have historically measured sexual-minority status include Boston, Chicago, Connecticut, Delaware, Hawaii, Illinois, Los Angeles, Maine, Massachusetts, Milwaukee, North Dakota, New Hampshire, New York City, Rhode Island, San Diego, San Francisco, Seattle, Vermont, Washington (DC), and Wisconsin. The Oregon Healthy Teens Survey and Minnesota Student Survey are similar surveys. |
|||||
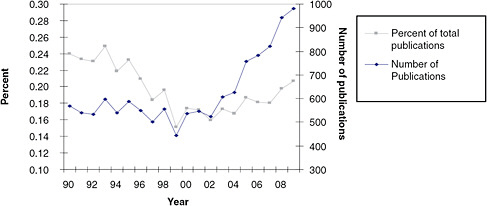
FIGURE 3-1 Publications in LGBT health indexed in PubMed.
SOURCE: Center for Population Research in LGBT Health (http://www.icpsr.umich.edu/icpsrweb/FENWAY/findings/index.jsp).
particularly true of studies of relatively small populations on topics construed by the respondent to be of a sensitive nature. Health research studies of LGBT populations are often viewed in this way. Methodological challenges, however, can be overcome when careful attention is paid to scientific rigor and respectful involvement of individuals who represent the target population. Scientific rigor includes incorporating and monitoring culturally competent study designs, such as the use of appropriate measures to identify participants and implementation processes adapted to unique characteristics of the study population. Respectful involvement of the study population, in this case LGBT people, refers to the involvement of individuals and community representatives in the research process, from decisions about the study purpose and methods, to ongoing consultation and data gathering, to dissemination of results (Minkler and Wallerstein, 2002).
The use of professionally accepted best practices that ensure scientific rigor in the design, conduct, and analysis of sample surveys and research studies is critical to the general acceptance of the results. As noted earlier in this report, the lack of demographic, economic, and health-related information on LGBT populations and their racial/ethnic subgroups makes it difficult to discuss health policy options intelligently. Identifying and adopting best practices for a sample survey or research study helps ensure that discussions about health policy do not become confounded with discussions about the nature of the data and the sample survey/study used to collect the data. Several textbooks concerned with methods for conducting sample surveys provide good examples of the issues a researcher must address to conduct such a survey with scientific rigor (Biemer and Lyberg,
2003; Czaja and Blair, 1996; Groves et al., 2004). These sources describe the key elements of sample surveys and design and implementation issues, sources of error, and ways of minimizing and controlling error. The American Association for Public Opinion Research (AAPOR), an association of survey methodologists, statisticians, and social science researchers, has identified best practices for its members to follow on its website (AAPOR, 2010). These practices, identified by a committee of survey methodologists, represent a valuable and thoughtful way to approach collecting information by means of a rigorous sample survey.
The principles relied upon to design and conduct scientifically rigorous sample surveys are critical as well to successful research studies, particularly community-based participatory research studies, in which scientific rigor and strong research community collaboration are critical. The contributions of such studies to research on LGBT and other minority and underserved populations have been acknowledged by numerous public agencies and private organizations (Buchting et al., 2008; SMART, 2009), including institutes within NIH that have allocated funding for this type of study with certain populations, including those defined by sexual orientation. For example, reviewing approaches to HIV surveillance, McFarland and Caceres (2001) emphasize the importance of ongoing formative research and alliances with key organizations and actors in communities of men who have sex with men to develop study measures and guide appropriate use of data.
Listed below are some general principles related to best practices for sample surveys and research studies. The intent is not to identify individual design decisions, such as the data collection mode, the reference period, or an appropriate sample or study design, as “best” since individual study goals, circumstances, and available resources will vary.
-
Identify specific goals for the study—for example, to develop estimates with which to describe a population or certain relationships, or to study the effects of experimental treatments. If a community-based study, develop partnerships and collaborate actively on the study goals with representatives of the study population within the community.
-
Identify and describe the study’s target population.
-
Identify or develop a sampling frame from which to select members of the target population for the study.
-
Determine and implement an appropriate method for drawing a probability-based sample to represent the target population or a recruitment strategy for the study population in a nonprobability design.
-
If the study will analyze the effects of a program or intervention, identify and implement an appropriate experimental design.
-
Determine a data collection mode consistent with the nature of the study.
-
Identify and develop the concepts to be measured, and, as appropriate, use cognitive interviews, focus groups, or expert panels to review draft questionnaires; for community-based research, developing a thorough knowledge of the local community, its culture, and its health-related needs is particularly important.
-
If appropriate for the study, identify sponsors, respected community leaders, or interested parties who support the study, and develop materials for the respondents that enable them to understand the reasons for the study, its potential benefits, and the need for their participation.
-
Pretest questionnaires on a sample of the study population.
-
If interviewers are being used to conduct the study, ensure that they receive sufficient training.
-
Develop procedures to maximize the data collection response rate, subject to availability of funds.
-
Develop and implement data processing and editing specifications to ensure that data are consistent and outlier data are minimized.
-
Develop and implement appropriate statistical methods to weight the data (if a probability sample) and to calculate variances for sample estimates.
-
Use statistical methods appropriate to the analysis.
-
Provide sufficient documentation on the survey, data collection, and statistical methods used (including response rates) to permit an independent reviewer to assess the quality of the data collection and analysis.
-
Ensure the privacy and confidentiality of survey responses.
-
Disseminate the results of the survey or research study widely, and in the case of community-based research, do so through meetings and presentations to the community and through partnership communication channels.
SUMMARY OF KEY FINDINGS AND RESEARCH OPPORTUNITIES
Findings
This chapter has addressed the challenges as well as the methodological issues associated with conducting research on LGBT populations and subpopulations. This discussion should provide a foundation for the review of
the state of knowledge regarding LGBT health across the life course in the following chapters. Key findings presented in this chapter are listed below.
Research Challenges
A number of challenges are associated with conducting research on the health status of LGBT populations:
-
The lack of standardized measures in federally funded surveys— Sexual orientation and gender nonconformity are multifaceted concepts, and a variety of methods have been used to identify them for research purposes.
-
Small populations—Since LGBT populations represent a relatively small proportion of the U.S. population, creating a sufficiently large sample to provide reliable estimates of these populations requires considerable resources. A further challenge arises in obtaining a probability sample of LGBT participants that includes sufficient numbers of representatives of population subgroups, such as racial-and ethnic-minority individuals, to permit meaningful analyses.
-
Barriers to identification as LGBT—Because of concerns about stigma and privacy, individuals may be reluctant to answer research questions about their same-sex sexual behavior or gender nonconformity.
Sampling
-
Probability sampling allows findings based on the data to be generalized to the study’s target population with a known margin of error. Some methods make it possible to improve the precision of estimates for small populations by combining two or more data sets. Although probability sampling is not used frequently in the study of LGBT health, some studies have obtained probability samples of LGBT participants, while others (such as federal health surveys and the U.S. census) have examined subsets of sexual and gender minorities using probability samples not designed specifically to study those individuals.
-
The majority of studies addressing topics relevant to LGBT health have been conducted using nonprobability samples. Even though the extent to which their findings accurately characterize the entirety of LGBT populations is unknown, studies based on nonprobability samples have yielded valuable information. In addition to providing general descriptive data for LGBT populations and subgroups, they have served to demonstrate the existence of certain phenomena, to test experimentally the effectiveness of various be-
-
havioral and medical interventions, to assess relationships among variables, to identify differences among groups, and in general, to provide insights into the health-related challenges faced by LGBT people. In addition, in the absence of data from probability samples, researchers often develop approximations of population patterns when the findings from multiple methodologically rigorous studies with different nonprobability samples converge.
Methods
-
Quantitative data can be collected through a variety of methods, including survey research, RCTs, longitudinal cohort studies, and patient-level data. Of these methods, survey research is particularly common in LGBT health studies, especially as a way to generate demographic data. There are four main sources of error associated with survey research: coverage, nonresponse, measurement, and processing errors (Table 3-1).
-
RCTs measure an intervention’s effects by randomly assigning individuals (or groups of individuals) to an intervention or control group. While these trials are considered the gold standard for measuring an intervention’s impact, the results may not be generalizable to groups other than those who participated in the trials.
-
Longitudinal cohort studies track individuals over time, allowing researchers to observe changes more accurately than is otherwise possible. The NHS and NHSII are examples of longitudinal cohort studies that have made significant contributions to understanding health.
-
Research on LGBT populations using patient-level data is evolving, with discussion ongoing about how to collect sexual orientation and gender identity data in databases.
-
Qualitative data can be collected through a variety of methods, including one-on-one interviews, focus groups, and cognitive interviews. These methods can be especially useful for generating hypotheses and laying the groundwork for future research.
Research Opportunities
A number of issues related to studying the health status of LGBT populations would benefit from additional research:
-
Federally funded surveys do not measure sexual orientation or gender expression in a uniform and consistent way, limiting the ability to compare data across these surveys.
-
The majority of LGBT literature relies exclusively on LGBT respondents, making it difficult to compare characteristics of LGBT populations with those of the entire U.S. population.
-
Research into better methods for recruiting and retaining participants in longitudinal studies is needed.
-
While valuable research has been conducted despite the limitations of available data sources, more national data must be collected if we are to fully understand the health needs of U.S. LGBT populations.
-
Even if LGBT populations can be identified through national surveys, since these populations represent a relatively small proportion of the U.S. population, estimates will be relatively imprecise unless resources are available with which to collect large oversamples of LGBT individuals. Research is necessary on ways to improve the quality and understand the limitations of estimates obtained by combining independent data sets, or by combining direct sample-based estimates with model-based estimates derived from supplemental but related data.
-
Guidelines need to be developed for maximizing the utility of available data through such mechanisms as aggregating data sets over time, adding supplemental samples or oversampling LGBT individuals for ongoing studies, and developing standards for recoding measures across multiple studies to achieve nationally representative data sets.
REFERENCES
AAPOR (American Association for Public Opinion Research). 2010. Best practices. https://www.aapor.org/Best_Practices.htm (accessed October 22, 2010).
Aaron, D. J., Y. F. Chang, N. Markovic, and R. E. LaPorte. 2003. Estimating the lesbian population: A capture-recapture approach. Journal of Epidemiology & Community Health 57(3):207–209.
Almeida, J., R. M. Johnson, H. L. Corliss, B. E. Molnar, and D. Azrael. 2009. Emotional distress among LGBT youth: The influence of perceived discrimination based on sexual orientation. Journal of Youth & Adolescence 38(7):1001–1014.
Austin, S. B., K. Conron, A. Patel, and N. Freedner. 2007. Making sense of sexual orientation measures: Findings from a cognitive processing study with adolescents on health survey questions. Journal of LGBT Health Research 3(1):55–65.
Balsam, K. F., T. P. Beauchaine, E. D. Rothblum, and S. E. Solomon. 2008. Three-year follow-up of same-sex couples who had civil unions in Vermont, same-sex couples not in civil unions, and heterosexual married couples. Developmental Psychology 44(1):102–116.
Barrett, K., J. Bradford, and J. Ellis. 2002. Using mapping to facilitate development of a health care infrastructure. Redlands, CA: ESRI Newsletter.
Bates, C., C. Droste, L. Cuba, and J. Swingle. 2008. One-on-one interviews: A qualitative assessment approach. Crawfordsville, IN: Center in Inquiry in the Liberal Arts at Wabash College.
Bates, N., T. J. Demaio, C. Robins, and W. Hicks. 2010. Classifying relationship and marital status among same-sex couples. Paper read at Proceedings of the Section on Survey Research Methods, July 31–August 10, 2010, Vancouver, British Columbia, Canada.
Bell, A. P., and T. S. Weinberg. 1978. Homosexualities: A study of diversity among men and women. New York: Simon and Schuster.
Biemer, P. P. 2010. Overview of design issues: Total survey error. In Handbook on survey research (2nd ed.), edited by P. V. Mardsen and J. D. Wright. Bingley, UK: Emerald Group Publishing Limited. Pp. 27–57.
Biemer, P. P., and L. Lyberg. 2003. Introduction to survey quality. Hoboken, NJ: Wiley & Sons, Inc.
Binson, D., J. Blair, D.M. Huebner, and W.J. Woods. 2007. Sampling in surveys of lesbian, gay, and bisexual people. In The health of sexual minorities, edited by I. H. Meyer and M. E. Northridge. New York: Springer. Pp. 375–418.
Black, D. A., G. Gates, S. G. Sanders, and L. J. Taylor. 2000. Demographics of the gay and lesbian population in the United States: Evidence from available systematic data sources. Demography 37(2):139–154.
Black, D. A., S. G. Sanders, and L. J. Taylor. 2007. The economics of lesbian and gay families. The Journal of Economic Perspectives 21:53–70.
Blair, J. 1999. A probability sample of gay urban males: The use of two-phase adaptive sampling. Journal of Sex Research 36(1):39–44.
Boehmer, U. 2002. Twenty years of public health research: Inclusion of lesbian, gay, bisexual, and transgender populations. American Journal of Public Health 92(7):1125–1130.
Boehmer, U., M. Clark, M. Glickman, A. Timm, M. Sullivan, J. Bradford, and D. J. Bowen. 2010. Using cancer registry data for recruitment of sexual minority women: Successes and limitations. Journal of Women’s Health 19(7):1289–1297.
Bolding, G., M. Davis, G. Hart, L. Sherr, and J. Elford. 2007. Where young MSM meet their first sexual partner: The role of the Internet. AIDS & Behavior 11(4):522–526.
Bowen, A. M., M. L. Williams, C. M. Daniel, and S. Clayton. 2008. Internet based HIV prevention research targeting rural MSM: Feasibility, acceptability, and preliminary efficacy. Journal of Behavioral Medicine 31(6):463–477.
Bowen, D. J., J. B. Bradford, D. Powers, P. McMorrow, R. Linde, B. C. Murphy, J. Han, and J. Ellis. 2004. Comparing women of differing sexual orientations using population-based sampling. Women & Health 40(3):19–34.
Bradford, J., C. Ryan, and E. D. Rothblum. 1993. National Lesbian Health Care Survey: Implications for mental health care. Journal of Consulting & Clinical Psychology 62(2):228–242.
Brennan, D. J., W. L. Hellerstedt, M. W. Ross, and S. L. Welles. 2007. History of childhood sexual abuse and HIV risk behaviors in homosexual and bisexual men. American Journal of Public Health 97(6):1107–1112.
Brick, J. M., and G. Kalton. 1996. Handling missing data in survey research. Statistical Methods in Medical Research 5(3):215–238.
Buchting, F. O., Scout, P. Fagan, M. Pien, and A. Rose. 2008. Lesbians, gays, bisexuals, and transgenders of color sampling methodology. Scotts Valley, CA: ETR Associates.
Carpenter, C. 2003. Sexual orientation and body weight: Evidence from multiple surveys. Gender Issues 21(3):60–74.
Carpenter, C., and G. J. Gates. 2008. Gay and lesbian partnership: Evidence from California. Demography 45(3):573–590.
Carpenter, K., S. Stoner, A. Mikko, L. Dhanak, and J. Parsons. 2010. Efficacy of a web-based intervention to reduce sexual risk in men who have sex with men. AIDS and Behavior 14(3):549–557.
Case, P., S. B. Austin, D. J. Hunter, J. E. Manson, S. Malspeis, W. C. Willett, and D. Spiegelman. 2004. Sexual orientation, health risk factors, and physical functioning in the Nurses’ Health Study II. Journal of Women’s Health 13(9):1033–1047.
Catania, J. A., D. Binson, J. Canchola, L. M. Pollack, W. Hauck, and T. J. Coates. 1996. Effects of interviewer gender, interviewer choice, and item wording on responses to questions concerning sexual behavior. Public Opinion Quarterly 60(3):345–375.
Catania, J. A., D. Osmond, R. D. Stall, L. Pollack, J. P. Paul, S. Blower, D. Binson, J. A. Canchola, T. C. Mills, L. Fisher, K. H. Choi, T. Porco, C. Turner, J. Blair, J. Henne, L. L. Bye, and T. J. Coates. 2001. The continuing HIV epidemic among men who have sex with men. American Journal of Public Health 91(6):907–914.
CDC (Centers for Disease Control and Prevention). 2009. 2009 compendium of evidence-based HIV prevention interventions. http://www.cdc.gov/hiv/topics/research/prs/evidence-based-interventions.htm (accessed October 27, 2010).
Channing Laboratory. 2011a. Growing Up Today Study (GUTS). http://nhs2survey.org/gutsweb/?page_id=2 (accessed March 7, 2011).
Channing Laboratory. 2011b. The Nurses’ Health Study. http://www.channing.harvard.edu/nhs/ (accessed March 3, 2011).
Clark, M. A., G. Armstrong, and L. Bonacore. 2005. Measuring sexual orientation and gender expression among middle-aged and older women in a cancer screening study. Journal of Cancer Education 20(2):108–112.
Cochran, S. D., and V. M. Mays. 2000. Lifetime prevalence of suicide symptoms and affective disorders among men reporting same-sex sexual partners: Results from NHANES III. American Journal of Public Health 90(4):573–578.
Cochran, S. D., and V. M. Mays. 2007. Physical health complaints among lesbians, gay men, and bisexual and homosexually experienced heterosexual individuals: Results from the California Quality of Life Survey. American Journal of Public Health 97(11):2048–2055.
Cochran, S. D., and V. M. Mays. 2009. Burden of psychiatric morbidity among lesbian, gay, and bisexual individuals in the California Quality of Life Survey. Journal of Abnormal Psychology 118(3):647–658.
Cochran, S. D., C. Keenan, C. Schober, and V. M. Mays. 2000. Estimates of alcohol use and clinical treatment needs among homosexually active men and women in the U.S. population. Journal of Consulting and Clinical Psychology 68(6):1062–1071.
Cochran, S. D., J. G. Sullivan, and V. M. Mays. 2003. Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. Journal of Consulting and Clinical Psychology 71(1):53–61.
Cochran, S. D., D. Ackerman, V. M. Mays, and M. W. Ross. 2004. Prevalence of non-medical drug use and dependence among homosexually active men and women in the US population. Addiction 99(8):989–998.
Cochran, S. D., V. M. Mays, M. Alegria, A. N. Ortega, and D. Takeuchi. 2007. Mental health and substance use disorders among Latino and Asian American lesbian, gay, and bisexual adults. Journal of Consulting and Clinical Psychology 75(5):785–794.
Conron, K. J., Scout, and S. B. Austin. 2008. “Everyone has a right to, like, check their box:” Findings on a measure of gender identity from a cognitive testing study with adolescents. Journal of LGBT Health Research 4(1):1–9.
Conron, K. J., M. J. Mimiaga, and S. J. Landers. 2010. A population-based study of sexual orientation identity and gender differences in adult health. American Journal of Public Health 100(10):1953–1960.
Consolacion, T. B., S. T. Russell, and S. Sue. 2004. Sex, race/ethnicity, and romantic attractions: Multiple minority status adolescents and mental health. Cultural Diversity & Ethnic Minority Psychology 10(3):200–214.
Corliss, H. L., M. Rosario, D. Wypij, L. B. Fisher, and S. B. Austin. 2008. Sexual orientation disparities in longitudinal alcohol use patterns among adolescents: Findings from the Growing Up Today Study. Archives of Pediatrics & Adolescent Medicine 162(11):1071–1078.
Couper, M. P. 2000. Web surveys: A review of issues and approaches. Public Opinion Quarterly 64(4):464–494.
Czaja, R., and J. Blair, eds. 1996. Designing surveys: A guide to decisions and procedures. Thousand Oaks, CA: Pine Forge Press.
Deputy, N. P., and U. Boehmer. 2010. Determinants of body weight among men of different sexual orientation. Preventive Medicine 51(2):129–131.
Diamond, L. M. 1998. Development of sexual orientation among adolescent and young adult women. Developmental Psychology 34(5):1085.
Diamond, L. M. 2008. Female bisexuality from adolescence to adulthood: Results from a 10-year longitudinal study. Developmental Psychology 44(1):5–14.
Dillman, D. A., J. D. Smyth, and L. M. Christian. 2009. Internet, mail, and mixed-mode surveys: The tailored design method (3rd ed.). Hoboken, NJ: John Wiley & Sons, Inc.
Dworkin, S. L., R. M. Pinto, J. Hunter, B. Rapkin, and R. H. Remien. 2008. Keeping the spirit of community partnerships alive in the scale up of HIV/AIDS prevention: Critical reflections on the roll out of DEBI (Diffusion of Effective Behavioral Interventions). American Journal of Community Psychology 42(1–2):51–59.
Egleston, B. L., R. L. Dunbrack, Jr., and M. J. Hall. 2010. Clinical trials that explicitly exclude gay and lesbian patients. New England Journal of Medicine 362(11):1054–1055.
Elliott, M. N., D. F. McCaffrey, B. K. Finch, D. J. Klein, N. Orr, M. K. Beckett, and N. Lurie. 2009. Improving disparity estimates for rare racial/ethnic groups with trend estimation and Kalman filtering: An application to the National Health Interview Survey. Health Services Research 44(5 Pt. 1):1622–1639.
Evans, A. R., R. D. Wiggins, G. Bolding, and J. Elford. 2008. Characteristics of gay and bisexual men who drop out of a web survey of sexual behaviour in the UK. AIDS & Behavior 12(6):957–963.
Finkelhor, D. 1994. Current information on the scope and nature of child sexual abuse. Future Child 4(2):31–53.
Fisher, R. A. 1925. Statistical methods for research workers. London: Oliver and Boyd.
Galesic, M., R. Tourangeau, and M. Casper. 2006. Complementing random digit dial telephone surveys with other approaches to collecting data. American Journal of Preventive Medicine 31(5):437–443.
Gallagher, K. M., P. S. Sullivan, A. Lansky, and I. M. Onorato. 2007. Behavioral surveillance among people at risk for HIV infection in the U.S.: The National HIV Behavioral Surveillance System. Public Health Reports 122(Suppl. 1):32–38.
Garofalo, R., J. Deleon, E. Osmer, M. Doll, and G. W. Harper. 2006. Overlooked, misunderstood and at-risk: Exploring the lives and HIV risk of ethnic minority male-to-female transgender youth. Journal of Adolescent Health 38(3):230–236.
Gates, G. 2007. Geographic trends among same-sex couples in the U.S. Census and the American Community Survey. Los Angeles, CA: The Williams Institute.
Gates, G. 2009. Same-sex spouses and unmarried partners in the American Community Survey, 2008. Los Angeles, CA: The Williams Institute.
Gay and Lesbian Medical Association and LGBT Health Experts. 2010. Healthy People 2010 companion document for lesbian, gay, bisexual, and transgender (LGBT) health. San Francisco, CA: Gay and Lesbian Medical Association.
Geanuracos, C. G., S. D. Cunningham, G. Weiss, D. Forte, L. M. Reid, and J. M. Ellen. 2007. Use of geographic information systems for planning HIV prevention interventions for high-risk youths. American Journal of Public Health 97(11):1974–1981.
Grant, J. M., L. A. Mottet, J. Tanis, D. Min, J. L. Herman, J. Harrison, and M. Keisling. 2010. National Transgender Discrimination Survey Report on Health and Health Care. Washington, DC: National Center for Transgender Equality and the National Gay and Lesbian Task Force.
Gribble, J. N., H. G. Miller, S. M. Rogers, and C. F. Turner. 1999. Interview mode and measurement of sexual behaviors: Methodological issues. Journal of Sex Research 36(1):16–24.
Groves, R. M., F. J. Fowler, M. P. Couper, J. M. Lepkowski, E. Singer, and R. Tourangeau. 2004. Survey methodology. New York: John Wiley & Sons, Inc.
Hall, D., K. Meador, and H. Koenig. 2008. Measuring religiousness in health research: Review and critique. Journal of Religion and Health 47(2):134–163.
Hatzenbuehler, M. L., K. M. Keyes, and D. S. Hasin. 2009. State-level policies and psychiatric morbidity in lesbian, gay, and bisexual populations. American Journal of Public Health 99(12):2275–2281.
Hatzenbuehler, M. L., K. A. McLaughlin, K. M. Keyes, and D. S. Hasin. 2010. The impact of institutional discrimination on psychiatric disorders in lesbian, gay, and bisexual populations: A prospective study. American Journal of Public Health 100(3):452–459.
Herbenick, D., M. Reece, V. Schick, S. A. Sanders, B. Dodge, and J. D. Fortenberry. 2010. Sexual behavior in the United States: Results from a national probability sample of men and women ages 14–94. The Journal of Sexual Medicine 7:255–265.
Herek, G. M. 2009. Hate crimes and stigma-related experiences among sexual minority adults in the United States: Prevalence estimates from a national probability sample. Journal of Interpersonal Violence 24(1):54–74.
Herek, G. M. 2010. Sexual orientation differences as deficits: Science and stigma in the history of American psychology. Perspectives on Psychological Science 5.
Herek, G. M., J. R. Gillis, and J. C. Cogan. 1999. Psychological sequelae of hate-crime victimization among lesbian, gay, and bisexual adults. Journal of Consulting and Clinical Psychology 67(6):945–951.
Herek, G. M., A. Norton, T. Allen, and C. Sims. 2010. Demographic, psychological, and social characteristics of self-identified lesbian, gay, and bisexual adults in a US probability sample. Sexuality Research and Social Policy 7(3):176–200.
HHS (U.S. Department of Health and Human Services). 2000. Healthy People 2010: Understanding and improving health. Washington, DC: HHS.
HIV Prevention Trials Network. 2011. Explore: A randomized clinical trial of the efficacy of a behavioral intervention to prevent acquisition of HIV among men who have sex with men (MSM). http://www.hptn.org/research_studies/hivnet015.asp (accessed March 7, 2011).
Holbrook, A. L., J. A. Krosnick, and A. Pfent. 2008. The causes and consequences of response rates in surveys by the news media and government contractor survey research firms. In Advances in telephone survey methodology, edited by C. T. J. Lepkowski, J. M. Brick, E. de Leeuw, L. Japec, P. J. Lavrakas, M. W. Link, and R. L. Sangster. New York: John Wiley & Sons, Inc. Pp. 499–528.
Jarama, S. L., F. Z. Belgrave, J. Bradford, M. Young, and J. A. Honnold. 2007. Family, cultural and gender role aspects in the context of HIV risk among African American women of unidentified HIV status: An exploratory qualitative study. AIDS Care: Psychological and Socio-medical Aspects of AIDS/HIV 19(3):307–317.
The Joint Commission. 2010. Advancing effective communication, cultural competence, and patient- and family-centered care: A roadmap for hospitals. Oakbrook Terrace, IL: The Joint Commission.
The Joint Commission. 2011. Joint Commission Perspectives 31 (3). Oakbrook Terrace, IL: The Joint Commission.
Kalman, R. E. 1960. A new approach to linear filtering and prediction problems. Transactions of the ASME—Journal of Basic Engineering 82 (Series D):35–45.
Kalton, G. 2009. Methods for oversampling rare subpopulations in social surveys. Survey Methodology 35(2):125–141.
Kalton, G., and D. Kasprzyk. 1986. The treatment of missing survey data. Survey Methodology 12(1):1–16.
Kasprzyk, D., G. Duncan, G. Kalton, and M. P. Singh, eds. 1989. Panel surveys. New York: John Wiley & Sons, Inc.
Keeter, S., C. Miller, A. Kohut, R. M. Groves, and S. Presser. 2000. Consequences of reducing nonresponse in a national telephone survey. Public Opinion Quarterly 64(2):125–148.
Kellstedt, L. A., and C. E. Smidt. 1996. Measuring fundamentalism: An analysis of different operational strategies. In Religion and the culture wars: Dispatches from the front, edited by J. C. Green, J. L. Guth, C. E. Smidt, and L. A. Kellstedt. Lanham, MD: Rowman & Littlefield. Pp. 193–218.
Kennamer, J. D., J. Honnold, J. Bradford, and M. Hendricks. 2000. Differences in disclosure of sexuality among African American and white gay/bisexual men: Implications for HIV/ AIDS prevention. AIDS Education & Prevention 12(6):519–531.
Knight, K. 1999. Liberalism and conservatism. In Measures of political attitudes, Vol. 2, edited by J. P. Robinson, P. R. Shaver, and L. S. Wrightsman. San Diego, CA: Academic Press. Pp. 59–158.
Kurdek, L. A. 2004. Are gay and lesbian cohabiting couples really different from heterosexual married couples? Journal of Marriage and the Family 66(4):880–900.
Laumann, E. O., R. T. Michael, and J. H. Gagnon. 1994. A political history of the national sex survey of adults. Family Planning Perspectives 26(1):34–38.
Lee, R. M. 1993. Doing research on sensitive topics. Thousand Oaks, CA: SAGE Publications.
Lynn, P. 2009. Methodology of longitudinal surveys. New York: John Wiley & Sons, Inc.
Martin, J. L., and L. Dean. 1990. Developing a community sample of gay men for an epidemiologic study of AIDS. American Behavioral Scientist 33(5):546–561.
Massachusetts Department of Public Health. 2007. Behavioral Risk Factor Survey 2007 Questionnaire. Boston, MA: Massachusetts Department of Public Health.
Mays, V. M., and S. D. Cochran. 2001. Mental health correlates of perceived discrimination among lesbian, gay, and bisexual adults in the United States. American Journal of Public Health 91(11):1869–1876.
McFarland, W., and C. F. Caceres. 2001. HIV surveillance among men who have sex with men. AIDS 15(Suppl. 3):S23–S32.
McKleroy, V. S., J. S. Galbraith, B. Cummings, P. Jones, C. Harshbarger, C. Collins, D. Gelaude, and J. W. Carey. 2006. Adapting evidence-based behavioral interventions for new settings and target populations. AIDS Education & Prevention 18:59–73.
McLaughlin, K. A., M. L. Hatzenbuehler, and K. M. Keyes. 2010. Responses to discrimination and psychiatric disorders among black, Hispanic, female, and lesbian, gay, and bisexual individuals. American Journal of Public Health 100(8):1477–1484.
Meyer, I. H., and P. A. Wilson. 2009. Sampling lesbian, gay, and bisexual populations. Journal of Counseling Psychology 56(1):23–31.
Meyer, I. H., L. Rossano, J. M. Ellis, and J. Bradford. 2002. A brief telephone interview to identify lesbian and bisexual women in random digit dialing sampling. Journal of Sex Research 39(2):139–144.
Meyer, I. H., S. Schwartz, and D. M. Frost. 2008. Social patterning of stress and coping: Does disadvantaged social statuses confer more stress and fewer coping resources? Social Science & Medicine 67(3):368–379.
Mimiaga, M. J., E. Noonan, D. Donnell, S. A. Safren, K. C. Koenen, S. Gortmaker, C. O’Cleirigh, M. A. Chesney, T. J. Coates, B. A. Koblin, and K. H. Mayer. 2009. Childhood sexual abuse is highly associated with HIV risk-taking behavior and infection among MSM in the EXPLORE study. Journal of Acquired Immune Deficiency Syndromes: JAIDS 51(3):340–348.
Minkler, M., and N. Wallerstein, eds. 2002. Community-based participatory research for health. New York: Jossey-Bass.
Morris, J. F., and E. D. Rothblum. 1999. Who fills out a “lesbian” questionnaire? The interrelationship of sexual orientation, years “out,” disclosure of sexual orientation, sexual experience with women, and participation in the lesbian community. Psychology of Women Quarterly 23(3):537–557.
Mosher, W. D., A. Chandra, and J. Jones. 2005. Sexual behavior and selected health measures: Men and women 15–44 years of age, United States, 2002. Advanced Data (362):1–55.
Muhib, F. B., L. S. Lin, A. Stueve, R. L. Miller, W. L. Ford, W. D. Johnson, and P. J. Smith. 2001. A venue-based method for sampling hard-to-reach populations. Public Health Reports 116(Suppl. 1):216–222.
Mustanski, B. S. 2001. Getting wired: Exploiting the Internet for the collection of valid sexuality data. Journal of Sex Research 38(4):292–301.
Nemoto, T., D. Operario, and J. Keatley. 2005. Health and social services for male-to-female transgender persons of color in San Francisco. In Transgender health and HIV prevention: Needs assessment studies from transgender communities across the United States, edited by W. Bockting and E. Avery. New York: The Haworth Medical Press. Pp. 5–19.
NIH (National Institutes of Health). 2011. Certificates of confidentiality: Background information. http://grants.nih.gov/grants/policy/coc/background.htm (accessed February 9, 2011).
NRC (National Research Council). 1984. Cognitive aspects of survey methodology: Building a bridge between disciplines. Washington, DC: National Academy Press.
NRC. 2004. Understanding racial and ethnic differences in health in late life: A research agenda. Washington, DC: The National Academies Press.
OMB (Office of Management and Budget). 2001. Statistical policy working paper 31: Measuring and reporting sources of error in surveys. Washington, DC: Federal Committee on Statistical Methodology.
Raghuhathan, T. E., D. Xie, N. Schenker, V. L. Parsons, W. W. Davis, K. W. Dodd, and E. J. Feuer. 2007. Combining information from two surveys to estimate county-level prevalence rates of cancer risk factors and screening. Journal of the American Statistical Association 102(478):474–486.
Rao, J. N. K. 2003. Small area estimation. New York: John Wiley & Sons, Inc.
Reips, U. 2000. The web experiment method: Advantages, disadvantages, and solutions. In Psychological experiments on the Internet, edited by M. H. Birnbaum. San Diego, CA: Academic Press. Pp. 89–117.
Reisner, S. L., M. J. Mimiaga, C. V. Johnson, S. Bland, P. Case, S. A. Safren, and K. H. Mayer. 2010. What makes a respondent-driven sampling “seed” productive? Example of finding at-risk Massachusetts men who have sex with men. Journal of Urban Health 87(3):467–479.
Riggle, E. D., S. S. Rostosky, and C. Reedy. 2005. Online surveys for BGLT research: Issues and techniques. Journal of Homosexuality 49(2):1–21.
Rosenfeld, M. J. 2010. Nontraditional families and childhood progress through school. Demography 47(3):755–775.
Ross, M. W., B. R. S. Rosser, and J. Stanton. 2004. Beliefs about cybersex and Internet-mediated sex of Latino men who have Internet sex with men: Relationships with sexual practices in cybersex and in real life. AIDS Care 16(8):1002–1011.
Rosser, B. R. S., M. H. Miner, W. O. Bockting, M. W. Ross, J. Konstan, L. Gurak, J. Stanton, W. Edwards, S. Jacoby, A. Carballo-Dieguez, R. Mazin, and E. Coleman. 2009. HIV risk and the Internet: Results of the Men’s Internet Sex (MINTS) Study. AIDS & Behavior 13(4):746–756.
Rothblum, E. D., and R. Factor. 2001. Lesbians and their sisters as a control group: Demographic and mental health factors. Psychological Science 12(1):63–69.
Rothblum, E. D., K. F. Balsam, and R. M. Mickey. 2004. Brothers and sisters of lesbians, gay men, and bisexuals as a demographic comparison group: An innovative research methodology to examine social change. Journal of Applied Behavioral Science 40(3):283–301.
Schenker, N., and T. E. Raghunathan. 2007. Combining information from multiple surveys to enhance estimation of measures of health. Statistics in Medicine 26(8):1802–1811.
Schenker, N., J. F. Gentleman, D. Rose, E. Hing, and I. M. Shimizu. 2002. Combining estimates from complementary surveys: A case study using prevalence estimates from national health surveys of households and nursing homes. Public Health Reports 117(4):393–407.
Sirken, M. G. 2004. Network sample surveys of rare and elusive populations: A historical review paper read at Symposium 2004: Innovative Methods for Surveying Difficult-to-Reach Populations.
SMART (Self-Monitoring, Analysis, and Reporting Technology). 2009. Best practices for asking questions about sexual orientation on surveys. Los Angeles, CA: The Williams Institute.
Smith, T. W. 1995. Some aspects of measuring education. Social Science Research 24(3):215–242.
Solarz, A. 1999. Lesbian health care issues. Exploring options for expanding research and delivering care. AWHONN Lifelines 3(5):13–14.
Stephan, C. W., and W. G. Stephan. 2000. The measurement of racial and ethnic identity. International Journal of Intercultural Relations 24(5):541–552.
Tang, H., G. L. Greenwood, D. W. Cowling, J. C. Lloyd, A. G. Roeseler, and D. G. Bal. 2004. Cigarette smoking among lesbians, gays, and bisexuals: How serious a problem? (United States). Cancer Causes & Control 15(8):797–803.
Tourangeau, R., and T. Yan. 2007. Sensitive questions in surveys. Psychological Bulletin 133(5):859–883.
Tourangeau, R., L. J. Rips, and K. A. Rasinski. 2000. The psychology of survey response. Cambridge, England: Cambridge University Press.
Villarroel, M. A., C. F. Turner, E. Eggleston, A. Al-Tayyib, S. M. Rogers, A. M. Roman, P. C. Cooley, and H. Gordek. 2006. Same-gender sex in the United States: Impact of T-ACASI on prevalence estimates. Public Opinion Quarterly 70(2):166–196.
Volz, E., and D. Heckathorn. 2008. Probability based estimation theory for respondent driven sampling. Journal of Official Statistics 24(1):79–97.
Westoff, C. F. 1973. The commission on population growth and the American future: Its origins, operations, and aftermath. Population Index 39(4):491–507.
Wienke, C., and G. J. Hill. 2009. Does the “marriage benefit” extend to partners in gay and lesbian relationships? Evidence from a random sample of sexually active adults. Journal of Family Issues 30(2):259–289.
Willis, G. B. 2004. Cognitive interviewing revisited: A useful technique, in theory? Methods for testing and evaluating survey questionnaires. Hoboken, NJ: John Wiley & Sons, Inc.
Xavier, J. M., and J. Bradford. 2005. Transgender health access in Virginia: Focus group report. Richmond, VA: Virginia Department of Health.
Xavier, J. M., M. Bobbin, B. Singer, and E. Budd. 2005. A needs assessment of transgendered people of color living in Washington, DC. International Journal of Transgenderism 8(2/3):31–47.
Xavier, J. M., J. Bradford, and J. Honnold. 2007. The health, health-related needs, and life-course experiences of transgender Virginians. Richmond, VA: Virginia Department of Health.




















































