As homes increasingly become the places for health care delivery and self-management, the intertwined effects of multiple environments (physical, social/cultural, community, and policy) on the well-being of care recipients and caregivers are more visible (Wahl et al., 2009). Managing health care at home is a challenge confronted by many people, including older persons, children, and younger adults with disabilities, who are especially vulnerable to their environments. This is also true for people with low incomes, multiple chronic illnesses, limited social supports, and health disparities as well as those who live in unsafe neighborhoods or poor-quality housing. A majority of vulnerable individuals do not receive effective health care for their chronic illnesses and live in housing that does not support their independence or functioning.
Without accessible and supportive housing, the options for delivery of health care in the home are limited. This chapter discusses the environmental factors that impact health care at home, with the intent of exploring how residents, health professionals, and policy makers can work together to improve environments that support better health. The lens of human factors considers the relationships among individuals, the tasks they perform, and the environment, offering a systems perspective to understand how the home environment can better support health care.
The environment for home-based health care is multilayered (see Figure 3-1). It includes the physical attributes of the home; social and cultural influences, such as social activity and personal values; community and municipality characteristics; and health/social service policy and governmental regulations. This chapter discusses the attributes of different envi-
ronments as they apply to health care in the home. The family vignettes in Boxes 6-1 and 6-2 serve to illustrate many of the points made.
PHYSICAL ENVIRONMENTS
In contrast to more structured settings, such as hospitals, nursing homes, or doctors’ offices, the physical environments of homes are more uncontrolled, dynamic, personal, and diverse (Gitlin, 2003; Siebert, 2009). These locations therefore pose novel challenges to providing direct health care and using health technology and equipment. Homes vary widely in their location, size, condition, and physical characteristics (see Table 6-1). Each of these factors affects provision of care and how health technologies are used. Home environments can either help or hinder the ability of individuals to perform physical functions, carry out personal care tasks, or use health technologies. Individuals and families also differ in their willingness to change the home environment to facilitate health care, their preferences for where they perform basic activities of daily living, and their willingness to use health technologies (Albert, 2010). As each home is unique, solutions that may be suitable for one individual, family caregiver, and home may not be appropriate or effective for others.
Housing in the United States
The United States is characterized by great diversity of residential locations, housing types and conditions, and cultural, neighborhood, and health policy influences. These variations have important implications for the provision of health care in the home.
According to 2010 U.S. census data, approximately 244 million persons in the United States live in urban and suburban areas, and 65 million live in rural areas (U.S. Census Bureau, 2010). These locations have different capacities to support the health needs of individuals due to the varying availability of public transit, housing options, and health care services. Moreover, the types of housing vary considerably: nearly 79 million are detached single-family homes, 5 million are duplexes, 28 million are multifamily units, and 9 million are mobile homes (American Community Survey, 2008).
In these different settings, older adults make up a large proportion of the 133 million U.S. residents with one or more chronic illnesses (Wu and Green, 2000). Nearly 86 percent of the more than 37 million people over age 65 have chronic illness (Centers for Disease Control and Prevention, 2008), but many older adults reside in older homes that are not well suited to their changing needs (Gill et al., 1999; Commission on Affordable
TABLE 6-1 Environmental Factors That Affect Medical Care and Life at Home
| Physical Environment | Types of homes (detached single-family house, duplex, townhouse, apartment, mobile home) |
| Age and condition | |
| Layout including location of bathrooms and bedrooms | |
| Accessibility in, out, and around the home | |
| Supportive features | |
| Communications/Internet access | |
| Adequacy of utilities | |
| Presence of children and animals | |
| Social Environment | Immediate family |
| Extended family | |
| Friends | |
| Religious affiliates | |
| Colleagues | |
| Cultural community | |
| Neighborhood community | |
| Clubs/associations | |
| Charitable activities | |
| Leisure activities | |
| Community Environment | Safety conditions |
| Weather conditions | |
| Presence and condition of streets and sidewalks | |
| Presence and condition of parks and recreation opportunities | |
| Presence and condition of meeting centers/locations | |
| Availability of goods and services | |
| Availability of public transportation | |
| Health Policy Environment | Housing policies |
| Zoning policies | |
| Building codes | |
| Social services policies | |
| Medical insurance company policies | |
| Medicare policies | |
| Medicaid policies | |
| Health care and long-term care reimbursement policies |
Housing and Health Facility Needs for Seniors in the 21st Century, 2002; Donald, 2009).
Housing Conditions
Too many individuals live in housing that may adversely affect their health and the delivery of care. For example, over 6 million households (about 5 percent of the total) live in housing that has moderate or severe physical problems related to heating, plumbing, and electrical deficiencies (U.S. Department of Housing and Urban Development, 2009, p. 389). Such problems are more prevalent in homes of low-income persons who are also at risk of exposure to lead paint, vermin and pest infestations, water leakage, and lack of air conditioning. These issues pose an especially serious risk to vulnerable populations, such as children with asthma, older adults with cognitive or physical impairments, and individuals with chronic diseases or disabilities, who are more susceptible to toxic exposures, respiratory problems, infections, and dehydration or hypothermia (U.S. Department of Housing and Urban Development, 2009). Moreover, such physical hazards impact the ability to install and use life-sustaining health devices.
Housing Barriers
The physical layout of homes can put individuals at greater risk of accidents, make daily living activities more difficult to perform, and even necessitate moving to a different home, assisted living, or nursing home (Fänge and Iwarsson, 2003; Iwarsson, 2005; Lau et al., 2007; Stark, 2008). For example, an older adult with mobility difficulties living in a three-story home may begin to experience difficulty navigating its stairs. An older adult who uses a diuretic living in a home with a bathroom only on the second floor may become nonadherent due to lack of easy access to the bathroom.
The role of the physical environment in accidents such as falls is of significant concern for persons with disabilities and those who are frail. One study of outpatients with lower limb amputations found that 58 percent of individuals with unilateral amputations and 27 percent of those with bilateral amputations reported at least 1 fall in the previous 12 months. Among people with unilateral amputations, 12 percent of falls were related to the prosthesis alone, 22 percent were related to the environment alone, and 48 percent were a result of intrinsic patient-related factors (Kulkarni et al., 1996). Older adults are also at increased risk for falls. Environmental factors, implicated in 40 to 50 percent of falls of older persons, include slippery surfaces, inadequate lighting, loose or deep pile or worn carpet, staircases without an appropriate railing, badly arranged furniture,
and poorly designed bathrooms (Clemson, Cumming, and Roland, 1996; Pynoos et al., 2006).
The spatial layout of a home can even hinder performance of activities of daily living. Insufficient space can make it difficult for caregivers to provide assistance and can hinder placement of medical devices (Sanford, 2010). Narrow staircases and small rooms illustrated in the vignette (see Box 6-1) are typical in that they were not designed for persons with disabilities, let alone for the delivery of health care or use of health technologies.
Home Modifications
The way in which individuals adapt to changing functional ability at home tends to follow a hierarchy of choices (see Figure 6-1). Individuals, particularly older adults, initially respond to functional difficulties by modifying their behaviors in the home, often reducing the frequency of an activity or taking more time to accomplish a particular task. If this does not work, they then adopt the use of an assistive device. When these strategies are no longer effective, individuals may choose to modify their home or use a combination of behavioral and environmental modifications along with personal care assistance when other strategies no longer are effective (Norburn et al., 1995).
At any of these stages, telehealth technologies can be employed. Telehealth is the delivery of health care services or information via telecommunications technologies. Often is it used to link care recipients and caregivers to external health care providers, but it can also be used for communications between care recipients and caregivers. Today, telehealth can include a telephone call, an e-mail, an online course, remote monitoring, and an online portal to store and send information. In the future, the presence of telehealth technologies will rise dramatically as they become more affordable and readily integrated into users’ lifestyles. More devices will be smaller, wireless, and embedded and/or integrated with other devices and systems. More robotic tools and sophisticated software will be available to enable automatic surveillance and decision support.
When behavioral modifications include reducing the frequency of self-care, individuals are at risk for negative health effects, including depression, health problems, and functional decline (Wrosch, Schulz, and Heckhausen, 2002). A supportive home environment can compensate for a person’s impaired functional capacity. Home modifications can enhance accessibility and minimize barriers of conventional housing, particularly for persons with impaired ambulation (Schaie et al., 2003; Gitlin, 2007). In addition, it appears that home modifications, when used in conjunction with exercise and medical risk assessment, can reduce the risk of falls among older adults (Pynoos, Steinman, and Nguyen, 2010).
BOX 6-1
The Johnson Family
Sam Johnson is a 38-year-old veteran who lost his hearing and both legs after stepping on a land mine in Iraq. He arrived home recently to the small two-story rowhouse he shares with his wife, Barbara, and their 8-year-old son, Aaron. Barbara assists her husband with activities of daily living in the evenings and on weekends when she is home from her job and Sam’s home health aide is unavailable. Sam spends the majority of his time in their second-floor bedroom because he doesn’t like going up and down the stairs on his artificial limbs. At times, he uses a wheelchair for mobility, but he keeps it on the first floor. He’s glad that he cannot hear the doorbell, because it gives him an excuse not to struggle with the stairs.
Sam’s rowhouse was built in 1946. It has 4 steps up to the front door and 12 more on a narrow stairway with handrails leading to a second floor with two bedrooms and a small bathroom with a toilet, bathtub, and sink. The house is dimly lit, and the staircase has a light switch only at the bottom. Sam has fallen on his way to the bathroom at night a couple of times since he came home.
Barbara, tired from her caregiving duties, has little time to herself as she tries to manage her own anxiety, hypertension, and chronic back pain, along with her husband’s needs. She is concerned about keeping everything straight, especially regarding their different medication schedules, and fears making errors. She struggles to communicate with Sam due to his hearing loss and often writes notes to make sure he understands what she’s saying to him.
Modifications to their home, adoption of available technologies, and some training could make this family’s life easier. It could be advantageous to set up a room on the first floor as Sam’s bedroom and add a small first-floor bathroom. Installing a light in the bedroom that flashes when someone rings the doorbell (which he cannot hear) would alert him that he has a visitor. A lift chair to help him transfer from sitting to standing would also be helpful. Although it would help to install a walk-in (i.e., curbless) shower so caregivers could safely help Sam bathe, such a change would depend on available space and funds.
Sam receives an array of support through the U.S. Department of Veterans Affairs (VA), such as monthly disability compensation for him and his dependents (averaging $2,932 per month), health care through the VA hospitals and health care system, and funds for home modifications.
_____________
SOURCE: Research experience of committee member Sara J. Czaja.
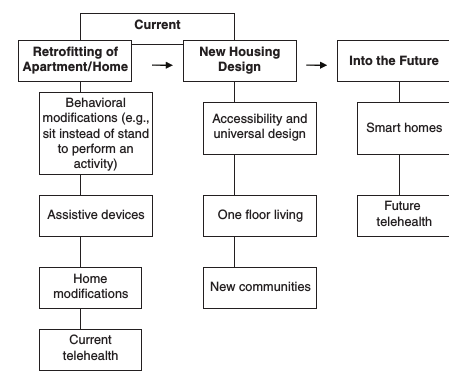
FIGURE 6-1 Continuum of housing modification options.
SOURCE: Adapted from Gitlin (2007).
Home modifications may include removing hazards; adding special features, such as grab bars, stair lifts, and ramps; and rearranging furnishings to create clear pathways. In addition, spaces can be renovated and the purpose of a room may be modified to accommodate a person with mobility limitations who cannot climb stairs or needs constant supervision (Pynoos et al., 1987). Many care recipients benefit from both low-cost home modifications and training in their use to enable them to engage in their daily activities more safely and efficiently (Gitlin and Corcoran, 2000; Gitlin et al., 2009).
Cognitive deficits affect over 5.3 million older persons, adding a layer of complexity to health care in the home (Hebert et al., 2003; Alzheimer’s Association, 2010). Because persons with cognitive impairments have diminished capacity in problem solving, decision making, and recognizing environmental cues, they have special environmental needs (Olsen, Ehrenkrantz, and Hutchings, 1993) and interventions. For example, as
dementia can affect depth perception, it is important to keep objects out of pathways to prevent people from falling. Night lights that automatically turn on at dusk could make it easier and safer to navigate the home during the evening. Likewise, large labels can help compensate for limited vision to help identify objects and use them appropriately. Devices that monitor people’s movements or detect a fall, alarms that indicate a door has opened, and safety alert bracelets may improve the safety of persons with dementia and provide reassurance to caregivers.
A survey by the American Association of Retired Persons (2000) of people over age 45 found that a substantial percentage of respondents had made the following home modifications:
- Installing light switches at the top and bottom of stairs (24 percent),
- Adding handrails on stairs (17 percent),
- Making changes to live on a first floor (14 percent),
- Widening doorways (9 percent),
- Adding a ramp or stair lift (4 percent).
Bathroom modifications were more likely to be made in the homes of older persons (ages 75 and over), the population with the greatest need (Freedman, 2011).
Although there is an array of home modification products on the market, there is no single place to purchase them all. Building supply stores carry a limited range of products, such as single-lever handles, “comfort” height toilets, handheld showers, grab bars, and hand rails. Medical supply and drug stores tend to focus on assistive devices (e.g., reachers, raised toilet seats) rather than home modifications. A growing number of specialized home modification firms have evolved that offer a variety of products (e.g., grab bars in different materials, stair lifts, curbless showers, easy access bathtubs) and a number of websites provide access to a range of products. For example, AbleData, a website maintained by the National Institute on Disability and Rehabilitation Research (NIDRR), features a product listing to help locate product manufacturers or distributors.1 Occupational therapists who specialize in home assessments are particularly skilled at helping to identify what will work for a particular individual and how to install home modifications to maximize an individual’s abilities.
A systematic home assessment by a trained occupational or physical therapist can help identify potential problems and solutions in the home
_____________
1The AbleData database of assistive technology contains objective information on almost 40,000 assistive products. For each product, the database includes a detailed description of the product’s functions and features, price information (when available), and contact information for the product’s manufacturer and/or distributors.
environment. A home assessment can also help caregivers provide better care, simplify tasks, and effectively use such assistive devices as a tub bench or lift chair (Pynoos et al., 1997). A home assessment prior to a person’s discharge from the hospital can also facilitate the transition to home and possibly minimize functional decline that can have a role in hospital readmissions (van Haastregt et al., 2000; Stuck et al., 2002).
There is a large unmet need for home modifications. About 1 million older persons have unmet needs for home modifications due to such factors as costs, their own inability to make changes, and lack of skilled installers. People are also reluctant to make some changes because they do not like their appearance (American Association of Retired Persons, 2000). Renters in particular may hesitate to make modifications because, even though the Fair Housing Amendments Act of 1998 gives them the right, they fear objections from their landlords or that they may have to take them out when they move (Newman and Mezrich, 1997; Pynoos et al., 2008).
Health-Related Technologies in the Home
A wide range of technology solutions is available to assist care recipients and caregivers in the home in order to make the environment more assistive and inclusive. Solutions that facilitate bedside care include adjustable beds that change position and height, pressure-relieving bed surfaces (e.g., gel mattress, low-air-loss mattress), lift devices (to facilitate transferring from one surface to another and reduce risk of caregiver injury), and seating devices to relieve pressure and prevent contractures.
Other low-tech assistive devices include grab bars, raised toilet seats, and clocks or telephones with large numerals (Gitlin et al., 2005, 2009, 2010). In addition, simple monitoring devices, such as intercoms or cell phones, can facilitate communication. There are also innovations in remote health monitoring that may help caregivers by providing mechanisms for monitoring safety and well-being. In cases involving persons with early-stage dementia, the technologies that are likely to be most useful are passive and do not require learning new procedures or practices. These include motion monitors that send alerts for people at risk of falling, video monitoring for activities and well-being, and interactive telehealth systems that encourage communication among care recipients, informal caregivers and formal caregivers. Although these technologies are promising, strong evidence is not yet available for the effectiveness of any particular remote monitoring technologies in achieving specific health outcomes. These approaches warrant further development and testing.
Although telehealth technologies and assistive devices may alleviate the burden of care (Gitlin, Winter, and Dennis, 2010), there are significant environmental challenges to their effective use. These include physical
aspects of the home (e.g., narrow hallways and staircases) that may hinder installation of assistive devices, lack of reliable electricity, and absence of Internet connections. Some technologies may be too costly, and the lack of reimbursement could require families to pay for them out of pocket. Any personal discomfort with technologies or devices in general could also reduce their use.
The Home as a Work Environment
The home can be a challenging environment for both residents and their formal caregivers, such as registered nurses, physical therapists, occupational therapists, physicians, or personal care aides (Piersol and Ehrlich, 2009).
Environmental conditions that can affect self-management and provision of health care in the home include lighting conditions; noise levels and room acoustics; temperature and humidity levels; air and water quality; electrical capacity and outlets; spatial layout and privacy; sanitation; the overall condition of the home (e.g., windows or doors that do not open or shut, falling ceilings, inadequate plumbing); and accessibility. Poor heating and air conditioning can place individuals at risk of heatstroke or hypothermia. Finally, a home may have broken windows or locks or unsafe walls and leaky roofs (Gershon et al., 2008). Rooms may be physically crowded or cluttered, making it difficult for the person providing or receiving care to maneuver within the space. Injuries to one or both parties may occur during transfers in confined spaces with few physical supports and no room for a lift device. Carpeting or stairs may hinder medical device or mobility aid maneuverability. The home may not be clean, increasing the risk of infection or disease. The household may be busy with other residents and activities, providing distractions that may confuse people while they engage in health-related activities.
Conditions may especially make it difficult to use electronic devices. For example, the lighting level may be low, making it hard to see people or device displays and controls. The noise levels may be high, making it difficult to hear people or device prompts and alarms. The temperature may be very high (e.g., in Florida) or very low (e.g., in Alaska), which can affect people or equipment. The humidity may be very high (e.g., in Louisiana), which can cause condensation, or very low (e.g., in Arizona), which can produce static electricity. Children, unauthorized users, pets, or vermin in the home can also put them at risk (e.g., playing with syringes), cause damage to devices (e.g., chewing on tubing), or change device settings, which may not be noticed before the unit is used again.
SOCIAL AND CULTURAL ENVIRONMENTS
Table 6-1 provides examples of social and cultural networks and activities. These networks provide support as well as prevailing attitudes about health care, and activities provide a sense of well-being and self-worth.
Care recipients’ mental outlook and physical health benefit from outdoor activity (National Institute on Aging, 2001; World Health Organization, 2002; Kai, Anderson, and Lau, 2003; Li et al., 2006). Enabling care recipients to participate in meaningful activities may reduce their apathy, boredom, and risk of depression (Gitlin et al., 2008, 2009). In addition, enabling family members who find themselves as informal caregivers to engage in meaningful activities and to take care of their own health can help them provide care for a longer period of time. For example, the ability to obtain formal daily supportive services for care recipients would also allow informal caregivers time to attend to their own needs. The availability of instruction on proper care techniques, such as how to assist with transfer in and out of the bed, would help informal caregivers reduce their own risk of injury (Sörensen et al., 2002; Pinquart and Sörensen, 2006).
Health care in the home is not only influenced by the availability and capability of social networks. It is also influenced by varying attitudes toward health care by different cultural and ethnic groups. Cultural beliefs about health affect how people cope with illness and maintain home care regimens. In a broad sense, the kind of health care a person receives at home depends on the meaning of “home” to them. This includes whether they are motivated to adapt their home and manage serious illness or disability in the community. Families differ in their willingness to reorganize living spaces to accommodate an ill family member (Albert, 1990) and in their tolerance for disorder and strategies for managing it (Rubinstein, 1990). People also differ in their attitudes about using medical technology, such as home infusion therapy or lift devices. For example, some people do not want their homes turned into what they perceive as a hospital, while others are willing to accept various devices and technology that would help them to function better and socialize.
Personal values also play a role in end-of-life care at home. For example, some people consider a peaceful death at home as the preferred outcome. For others, experiencing a loved one’s death in the home is stressful or uncomfortable. These beliefs determine the nature of care delivered in the final days of life (Kagawa-Singer, 2001).
COMMUNITY ENVIRONMENTS
Table 6-1 illustrates community environmental factors that can play an important role in whether care recipients can live independently and manage their health care at home (Golant, 2006, 2007). Poor neighborhood conditions are linked to higher rates of depression, worse chronic illness, and poor access to formal care staff (Bowling and Stafford, 2007; Beard et al., 2009). The local community can influence whether care recipients can carry out daily living tasks, participate in social activities, and engage in healthy behaviors, such as walking safely in their neighborhood and shopping for healthy foods. Neighborhoods can be ill suited to outdoor activity when, for example, sidewalks and intersections are lined with hazards and debris and the traffic signals are too short to allow time for care recipients to cross the street safely (Li et al., 2006). Many communities lack adequate public transit or pay only limited attention to sidewalk and street crossing maintenance. Many neighborhoods in suburban areas do not have sidewalks at all.
Community features vary widely, including land use patterns/development density, road conditions, street and pedestrian connection systems, street safety (e.g., separation from traffic, crossings), street design (e.g., furniture, trees, lighting), sidewalk maintenance and amenities (e.g., benches, street lights, width, snow, cracks), and accessibility features (e.g., curb cuts) to promote mobility, activity, and health (Sallis and Owen, 1999; Ewing, Schieber, and Zegger, 2003; Frank, Engelke, and Schmid, 2003; Frumkin, 2003; Roper et al., 2003; Saelens, Sallis, and Frank, 2003; Boslaugh et al., 2004; Fisher, Tzamaras, and Scherer, 2004; Frank et al., 2005; Suminski et al., 2005).
Access to reliable utilities and phone service also varies by community. Intermittent access to electrical power, telephone service, or cell-phone reception can make it challenging for formal caregivers to contact individuals, make appointments, and help them properly manage their own health. Neighborhoods can also influence whether caregivers feel safe (Gershon et al., 2008).
These concerns have led some localities to focus on developing more livable communities for persons of all ages and abilities (Alley et al., 2007). The Indiana AdvantAge Initiative has created a list of components of an elder-friendly community and a set of 33 indicators of elder-friendliness (Oberlink and Stafford, 2009). The Atlanta Regional Commission has undertaken a broad approach through its Lifelong Communities planning process, intended to promote housing and transportation options, encourage healthy lifestyles, and expand information and access (Lawler and Berger, 2009).
HEALTH POLICY ENVIRONMENTS
Table 6-1 identifies policies that can influence the state and quality of health care services and technologies in the home. Inadequate incentives contribute to shortages of primary care physicians, nurses, occupational and physical therapists, and personal care aides in general and in home care in particular (Institute of Medicine, 2008). Though new mobile diagnostic devices and health information technologies are emerging, currently little reimbursement is provided for these tools.
Medicare was created in 1965, and at that time care recipients predominantly experienced time-limited acute illness; over the years, hospital stays have shortened and care recipients are returning home in need of more complex care, including a wide range of medical and nursing services. There is a mismatch, however, between current reimbursement policy, which rewards volume of services in the inpatient and subspecialty environment, and the need for home-based care of those with multiple chronic illnesses and disabilities. For example, some care recipients must choose between paying $150 for a round-trip wheelchair van ride to a doctor’s office or not seeing the doctor at all.
At home, care recipients are in need of primary care teams trained to evaluate their homes and coordinate all needed medical, social, and housing services. This would require payment incentives to fund providers who coordinate care across settings and time.2 Also, informal caregivers would benefit from services that increase their skills in managing the complex health conditions and functional disabilities of their care recipients. These services require payment mechanisms to support their delivery (Gitlin, Jacobs, and Vause-Earland, 2010).
Growing populations of frail elders, younger adults with disabilities, disabled veterans, and children with special health care needs require care coordination in the home and community (Bodenheimer, 2008; Administration on Aging, 2009; Vincent and Velkoff, 2010). A wide range of experts has concluded that care coordination for high-need individuals has a positive effect on health care outcomes and costs of care (Chen et al., 2000; Brown et al., 2007; Administration on Aging, 2009; National Advisory Board, 2009; Vincent and Velkoff, 2010). Their research has shown that the key elements to improve care and reduce costs are (a) involvement of primary care physicians, (b) a focus on high-risk beneficiaries, (c) well-trained teams that execute customized plans of care, (d) frequent in-person contact in the home, and (e) specific incentives for good results and savings. Other
_____________
2The Patient Centered Medical Home (PCMH) is one model for providing comprehensive primary care and is generally institutionalized in a health care setting that facilitates partnerships between individual care recipients and their personal physicians and, when appropriate, formal caregivers in the home and the care recipient’s family.
studies have shown benefits of home-based primary care that includes these elements for high-need populations (Counsell et al., 2007; Edes, 2010).
Current fee-for-service payments from Medicare and Medicaid, however, discourage coordination of care (Davis, 2007; Bodenheimer, 2008). This payment policy has led to fragmented care, increasing costs per beneficiary, and a projection that the Medicare Trust Fund will be empty by 2029 (Social Security and Medicare Board of Trustees, 2010). Recent research has shown that fee-for-service methods lead to “supply-sensitive” care, wherein the density of hospital beds and subspecialists drive costs of care (Dartmouth Atlas of Health Care, 2008).
To support comprehensive home-based health care, policy makers need to promote innovations that challenge the status quo, such as mobile primary care teams (Christensen, Bohmer, and Kenagy, 2000). This would have the benefits of better coordinated care in the home, improved access for care recipients and families, and lower overall costs. The Patient Protection and Affordable Care Act (PPACA) includes elements that could promote care coordination at home for high-need populations. These include the Medicare Center for Innovation, the Medicare Shared Savings Program, and the Independence at Home Act.
Several related ongoing innovative programs in Medicaid, such as 1915(c) Home and Community-Based Waivers and 1915(j) Cash and Counseling (Doty, Mahoney, and Sciegaj, 2010), are intended to keep people in the community and out of institutional settings. Cash and Counseling allows participants to manage a fixed monetary allowance that can be used for employing outside service providers, friends, or family members to provide care. In addition, it can be used for services not generally covered by Medicaid such as transportation, rehabilitation, procurement of assistive technology, and installation of home modifications.
Although no federal program covers the cost of or finances home modifications, a range of public and private financing sources are available, including loans available to individuals as well as programs supported by housing, health, and social service sectors. Resources vary considerably and may depend on such factors as where a person lives, income/assets, type of housing (e.g., rented/owned), and specific problems or health conditions. The U.S. Department of Veterans Affairs has several programs to assist disabled veterans and service members with home modifications. For example, the Specially Adapted Housing (SAH) Grant Program is designed to provide barrier-free living environments that support independent living in a newly constructed home or one that is modified to meet their adaptive needs. The program provides up to $63,000 and serves permanently disabled veterans with such problems as loss or loss of use of both lower extremities and blindness (U.S. Department of Veterans Affairs, 2010). A separate program, the Special Home Adaptation (SHA) Grant Program,
targets veterans and service members with permanent disabilities, such as blindness in both eyes or loss of use of both hands and extremities below the elbows. This program provides up to $12,756 to modify an existing home to meet adaptive needs, such as assistance with mobility (U.S. Department of Veterans Affairs, 2010).
Other care recipients, like Mrs. Harper in Box 6-2, have fewer support options and might have to piece together resources to implement home modifications. The U.S. Department of Housing and Urban Development Community Development Block Grant funds and Administration on Aging Title III funds have often been used by local communities for home modification programs for low-income persons. In addition, Medicaid waiver programs intended to keep low-income persons in the community often cover environmental modifications. Many such programs, however, operate with
BOX 6-2
The Harper Family
Mrs. Harper, an 86-year-old woman with multiple chronic conditions, including early-stage dementia, depression, low vision, and severe rheumatoid arthritis, depends on her granddaughter Susan for some of her care. Susan lives in the suburbs 24 miles away from her grandmother, who lives alone in a mobile home. The mobile home has six steps up to the front door, which prevent her from getting out of the house. The home’s hallways are narrow and the bathroom, typical of such homes, is very small.
Mrs. Harper needs assistance getting into and out of the bathtub, but limited space makes it hard for someone to assist her. Previously active and socially engaged, she now spends most of her time sitting in a recliner in her living room. With little to occupy her, she has become depressed and lost muscle strength due to inactivity.
The addition of an outside stair lift would give her better access into and out of the house, and her bathroom needs modification. At a minimum, grab bars should be added, taking into account that they need to be specially secured because her bathing area has fiberglass surfacing. Until she can modify the bathroom or obtain outside help, she might take a sponge bath instead of using the bathtub. Mrs. Harper could also benefit from single-lever or motion sensor–activated faucets, anti-scald devices on plumbing fixtures, and nonslip flooring to reduce fall risk.
_____________
SOURCE: Clinical experience of committee member Eric DeJonge.
caps on expenditures (often less than $1,000), serve defined geographic areas, pay for a limited range of modifications, and require eligibility related to income and need. Existing private long-term care insurance policies often have allowances for home modifications, but they also may have caps and eligibility requirements. Medicare is not a viable option for home modification funding, as it pays for only medically necessary durable medical equipment and supplies, not for changes to the physical environment (Pynoos and Nishita, 2003). It is possible for a person to count medically related home modifications as a medical deduction if their total expenditures for health care reach at least 7.5 percent of their income. Finally, although the recently adopted long-term care insurance program (the Community Living Assistance Services and Supports Act, known as the CLASS Act) included in the Patient Protection and Affordable Care Act will pay eligible persons a daily amount that they can use for care and home adaptations, it is not yet clear how payment for expensive modifications will be covered.
Under Medicare, in order to obtain the services of an occupational therapist for a home assessment and treatment, a referral is needed from a physician, and coverage for a limited number of visits is restricted to individuals with functional decline or safety concerns (Pynoos et al., 1987, 1997, 1998; Pynoos, 1993; Gitlin et al., 2010). A home assessment for home modifications by occupational therapists is also available through some state programs, but they, too, are highly restricted. Consequently, given the patchwork of resources, it is estimated that three-quarters of older persons pay for home modifications out of pocket (LaPlante et al., 1992).
FUTURE ENVIRONMENTAL TRENDS
Physical Housing Modifications
Home modification interventions occur along a continuum. As shown in Figure 6-1, the current approach involves introducing modifications into conventional homes and developing products that fit preexisting specifications. The main barriers for retrofitting conventional homes are insufficient resources for paying for modifications and installing assistive products. Future trends include building new homes with accessibility features, creating healthy communities, and developing smart homes.
Accessibility and Universal Design
New homes and housing developments can be built to contain a minimum set of accessibility features. The Fair Housing Amendments Act of 1998 (FHAA) has a set of standards and guidelines that require such features in multiunit and townhouses with four or more units. However,
single-family housing and smaller townhouses—in which the majority of U.S. residents live—are exempt from the FHAA. In order to provide a minimum level of accessibility in housing not subject to FHAA, 17 states and 30 cities in the United States have passed what are called “visitability” codes, which currently apply to 30,000 homes (Nishita et al., 2007; Maisel, Smith, and Steinfeld, 2008). These codes add very little to costs but result in housing that accommodates visitors with disabilities (for example, ensuring no-step entrances) and also allows “aging in place” for individuals who experience mobility impairments. The International Code Council (ICC) and the American National Standards Institute (ANSI), which respectively focus on building codes and accessibility, have both endorsed voluntary accessibility standards (i.e. ICC/ANSI A117.1, Accessible and Usable Buildings and Facilities). These standards could facilitate more jurisdictions to pass such visitability codes and encourage legislative consistency throughout the country.
Universal design is a broader concept than visitability or accessibility, as it is intended to create residential settings that work for everyone regardless of size, age, or ability. The “universal” in universal design signifies that design features of a home should enhance the lives of young families with children, persons who are middle aged, and older persons who want to age in place. Instead of a special approach to accommodate disabilities, universal design is based on a set of seven principles: (1) equitable use, (2) flexible use, (3) simple and intuitive use, (4) perceptible information, (5) tolerance for error, (6) low physical effort, and (7) size and space for approach and use (Steinfeld and Shea, 2001; Story, 2001; Young and Pace, 2001). Homes based on these principles, sometimes also referred to as inclusive or lifetime housing, are intended to be residential in appearance and the design features integrated and virtually invisible (Center for Inclusive Design and Environmental Access, 2010). For example, fully realized homes with universal design could include such features as a no-step path to a no-step entry, doorways that are at least 34-inches wide, at least one accessible full bathroom on the main floor, kitchen countertops and cabinetry that allow a person to work in the kitchen in a seated position, nonglare surfaces, a curbless shower in the bathroom, anti-scald faucet devices to avoid burns, nonslip flooring, variable height counters, doors and faucets with single-lever handles, and a bedroom on the main floor. Such features can help persons and their caregivers carry out everyday tasks and prevent serious and costly accidents (e.g., falls, burns). Moreover, because it avoids the costs and inconveniences of home modifications (e.g., ramps, lifts, bathroom remodels), universal design is aligned with the overall goal of sustainability. In the long run, implementing universal design in more homes will result in housing that suits the long-term needs of more residents, provides more housing choices for persons with chronic conditions and disabilities,
and causes less forced relocation of residents to more costly settings, such as nursing homes.
Currently, few housing codes require universal design, and builders and architects are not designing most homes according to its principles. This is due to lack of knowledge about the concept, perceived low demand, and concern about costs. However, surveys indicate that there is an increasing demand for such features (American Association of Retired Persons, 2003), and they are considered beneficial.
A third approach is to develop new housing options that can be created within an existing unit (e.g., by converting a garage into a living space), constructed as a temporary or permanent extension of a house or built as a free-standing unit in the backyard (Kunkle, 2010) to accommodate a person with a chronic condition or disabilities. Although impractical in some cases, such solutions could work in communities in which the zoning codes allow for such changes and lots are large enough to accommodate them. New homes could also be designed to include “mother-in-law suites” or first-floor master or guest bedrooms.
New Communities
Complementary efforts are focusing on creating healthy neighborhoods and communities. For example, planned communities with restricted access are increasing in number. Almost 9 million residents lived in this type of setting in 1997 (Cannuscio, Block, and Kawachi, 2003); this trend began in Florida and California and is likely to increase in coming years in major metropolitan areas, with more people living in communities that have community centers (e.g., exercise facilities, convenience stores), social networking opportunities, and basic services, such as home repair and gardening. There is no guarantee, however, that they will include an array of housing options (including those that are affordable) nor homes that allow for aging in place or that meet the needs of persons with disabilities. However, it is encouraging that some builders, such as those in the planned community of Irvine, California, have provided prospective buyers with brochures and information about universal design features that can be included in homes to be constructed.
Another housing trend is the rise of naturally occurring retirement communities (NORCs) throughout the United States. These communities may be vertical (typically apartment buildings or condominiums) or horizontal and have large concentrations of older persons. Although not initially planned for older persons, over time the residents of these communities have aged and now need supportive services and home modifications to remain in their homes. Because of economies of scale, such neighborhoods present a natural setting for developing comprehensive home-based services
(Vladeck, 2004; Enguidanos et al., 2010) to provide a social supportive safety net for vulnerable populations.
Smart Homes
Although not necessarily an essential feature of universal design, the “smart house” concept involves a home that is outfitted for telehealth services and other computer-based technologies to support people, including those with cognitive impairments (Sanford, 2010). As described in Chapter 5, existing technologies include motion detectors for tracking an individual’s movement through key areas of the home (i.e., kitchen, bathroom, bedroom) and alerting designated responders about a fall, sensors that detect if a person has left the house, and health monitoring systems that operate in conjunction with each other and allow information to be transmitted to health care providers, caregivers, or selected family members.
Sophisticated technologies are increasingly being constructed into homes worldwide (Chan et al., 2009). Over the last decade and a half, a number of demonstration smart homes have been built by universities (e.g., Georgia Institute of Technology, University of Florida) to test such new technologies. In addition, several homes have been developed, such as the Eskaton National Demonstration Home just outside Sacramento, California, that integrate smart home technology, health monitoring, and “green” house features. Researchers from five countries (Finland, Ireland, Lithuania, Norway, and the United Kingdom) joined their efforts for the ENABLE project (Cash, 2003), which promotes the well-being of people with early dementia with several features, such as a locator for lost objects, a temperature monitor, and an automatic bedroom light. In Toulouse, France, the PROSAFE project is using a set of infrared motion sensors to support automatic recognition of resident activity and of possible falls (Chan et al., 1999).
Advances in robotics, artificial intelligence, and machine learning are enabling development of automated systems capable of inferring (through motion detectors, camera vision, and infrared, sonar, and laser sensors) what a person is doing at home and providing physical or cognitive assistance when needed or desired (Nugent et al., 2008; Chan et al., 2009). Examples include wearable, installed, or mobile robotic systems that work cooperatively with people who are otherwise unable to function safely and independently without help from others. Many of these emerging quality-of-life technologies are still in the proof-of-concept stage or undergoing usability testing of prototypes in small-sample laboratory or field trials and are far from having demonstrated efficacy or being commercially available. Despite concerns about cost, privacy, and the potential for reducing human contact that have been expressed by older adults and persons with disabilities (Matthews et al., 2010), many potential users indicate that
they would be willing to use these types of context-aware and responsive technologies (Beach et al., 2009), especially if doing so would enable them to live in the residential environment of their choosing (Beach et al., 2009, 2010).
Changes in Health Policy
Federal and state health policy reforms are moving from volume-based reimbursement to paying more for clinical and financial results. In the 2010 Patient Protection and Affordable Care Act (PPACA), there are several elements, such as the Medicare Center for Innovation, Accountable Care Organizations (ACOs), the Independence at Home (IAH) Demonstration Program, and the Transitional Care Program, that change reimbursement to promote better care in lower cost settings. Several of these initiatives propose to “share savings” with the most effective providers. The Medicaid Health Home Program (Section 2703, PPACA) also seeks to build better community-based care and lessen the state and federal costs of dual-eligible persons. The budgetary imperative of unsustainable Medicare and Medicaid costs is driving such reimbursement incentives to monitor and deliver care in the home. This includes more human services (such as home health aides, nursing, and medical staff), better mobile technology, and more intensive coordination of care. These efforts will be buttressed by the CLASS Act, as noted earlier also part of the PPACA, that will build a reserve of funds for long-term care services to assist younger persons with disabilities and older persons who are frail. Delivery of daily supportive services, complex medical care, and mobile technology can lower costs and improve the experience of people who are living at home. In order for such policy efforts to succeed, however, home-based health care needs to overcome the challenges noted in this and other chapters and demonstrate practical and safe care in a lower-cost setting.
REFERENCES
Administration on Aging. (2009). A profile of older Americans. Available: http://www.aoa.gov/AoARoot/Aging_Statistics/Profile/2009/2.aspx [July 2010].
Albert, S.M. (1990). The dependent elderly, home health care, and strategies of household adaptation In J.F. Gubrium and A. Sankar (Eds.), The home care experience: Ethnography and policy. Thousand Oaks, CA: Sage.
Albert, S.M. (2010). Impact of cultural, social, and community environments on home care. In National Research Council, The role of human factors in home health care: Workshop summary (pp. 247-274). S. Olson, Rapporteur. Committee on the Role of Human Factors in Home Health Care. Committee on Human-Systems Integration, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press.
Alley, D., Liebig, P., Pynoos, J., Banerjee, T. and Choi, I.H. (2007). Creating elder-friendly communities. Journal of Gerontological Social Work, 49(1), 1-18.
Alzheimer’s Association. (2010). Alzheimer’s disease facts and figures. Available: http://www.alz.org/documents_custom/report_alzfactsfigures2010.pdf [March 31, 2011].
American Association of Retired Persons. (2000). Fixing to stay: A national survey of housing and home modification issues. Washington, DC: Author.
American Association of Retired Persons. (2003). These four walls: Americans 45+ talk about home and community. Washington, DC: Author.
American Community Survey. (2008). Physical housing characteristics for occupied housing units data set: 2005-2007 American Community Survey 3-year estimates. Washington DC: U.S. Census Bureau.
Beach, S., Schulz, R., Downs, J., Matthews, J., Barron, B., and Seelman, K.. (2009). Disability, age, and informational privacy attitudes in quality of life technology applications: Results from a national web survey. ACM Transactions on Accessible Computing, 2(1), 1-21.
Beach, S., Shultz, R., Seelman, K., Cooper, R.A., and Teodorski, E. (2010). Trade-offs and tipping points in the acceptance of quality of life technology: Results from a survey of manual and power wheelchair users. Paper presented at the International Symposium on Quality of Life Technology, June 28-29, Las Vegas, NV.
Beard, J.R., Cerda, M., Blaney, S., Ahern, J., Vlahov, D., and Galea, S. (2009). Neighborhood characteristics and change in depressive symptoms among older residents of New York City. American Journal of Public Health, 99, 1-7.
Bodenheimer, T. (2008). Coordinating care: A perilous journey through the health care system. New England Journal of Medicine, 358, 1064-1071.
Boslaugh, S.E., Luke, D.A., Brownson, R.C., Naleid K.S., and Kreuter M.W. (2004). Perceptions of neighborhood environment for physical activity: Is it “who you are” or “where you live”? Journal of Urban Health, 81(4), 671-681.
Bowling, A., and Stafford, M. (2007). How do objective and subjective assessments of neighborhood influence social and physical functioning in older age? Findings from a British survey of aging. Social Sciences and Medicine, 64, 2533-2549.
Brown, R., Peikes, D., Chen, A., Ng, J., Schore, J., and Soh, C. (2007). Evaluation of the Medicare coordinated care demonstration: Findings for the first two years. Princeton, NJ: Mathematica Policy Research. Available: http://www.mathematica-mpr.com/publications/pdfs/mccdfirsttwoyrs.pdf [March 31, 2011].
Cannuscio, C., Block, J., and Kawachi, I. (2003). Social capital and successful aging: The role of senior housing. Annals of Internal Medicine, 139(5 II), 395-399.
Cash, M. (2003). Assistive technology and people with dementia. Reviews in Clinical Gerontology, 13, 313-319.
Center for Inclusive Design and Environmental Access. (2010). Inclusive housing: A pattern book. New York: W.W. Norton.
Centers for Disease Control and Prevention. (2008). Percent of U.S. adults 55 and over with chronic conditions. Available: http://www.cdc.gov/nccdphp/overview.htm [July 2010].
Chan, M., Bocquet, H., Campo, E., Val, T., and Pous, J. (1999). Alarm communication network to help carers of the elderly for safety purposes: A survey of a project. International Journal of Rehabilitation Research, 22, 131-136.
Chan, M., Campo, E., Estève, D., and Fourniols, J.Y. (2009). Smart homes: Current features and future perspectives. Maturitas, 64(2), 90-97.
Chen, A., Brown, R., Archibald, N., Aliotta, S., and Fox, P.D. (2000). Best practices in coordinated care. Princeton, NJ: Mathematica Policy Research. Available: http://www.mathematica-mpr.com/pdfs/bestsum.pdf [March 31, 2011].
Christensen, C., Bohmer, R., and Kenagy, J. (2000). Will disruptive innovations cure health care? Harvard Business Review, 78(5), 102-112.
Clemson, L., Cumming, R.G., and Roland, M. (1996). Case-control study of hazards in the home and risk of falls and hip fractures. Age and Ageing, 25(2), 97.
Commission on Affordable Housing and Health Facility Needs for Seniors in the 21st Century. (2002). A quiet crisis in America: A report to Congress by the Commission on Affordable Housing and Health Facility Needs for Seniors in the 21st Century. Washington, DC: Author.
Counsell, S.R., Callahan, C.M., Clark, D.O., et al. (2007). Geriatric care management for low-income seniors—a randomized controlled trial. Journal of the American Medical Association, 298(22), 2623-2633.
Dartmouth Atlas of Health Care. (2008). Executive summary. Available: http://www.dartmouthatlas.org [July 2010].
Davis, K. (2007). Paying for care episodes and care coordination. New England Journal of Medicine, 356, 1166-1168.
Donald, I.P. (2009). Housing and health care for older people. Age and Ageing, 38(4), 364-367.
Doty, P., Mahoney, K.J., and Sciegaj, M. (2010). New state strategies to meet long-term care needs. Health Affairs, 29(1), 49-56.
Edes, T. (2010). Financial savings of home-based primary care for frail veterans with chronic disabling disease. Paper session, May 13, presented at the annual meeting of the American Geriatrics Society, Washington, DC. Abstract available: http://onlinelibrary.wiley.com/doi/10.1111/j.1532-5415.2010.02850.x/pdf [April 2011].
Enguidanos, S., Pynoos, J., Siciliano, M., Diepenbrock, L., and Alexman, S. (2010). Integrating community services within a NORC: The Park La Brea experience. Cityscape: A Journal of Policy Development and Research, 12(2), 29.
Ewing, R., Schieber, R.A., and Zegeer, C.V. (2003). Urban sprawl as a risk factor in motor vehicle occupant and pedestrian fatalities. American Journal of Public Health, 93(9), 1541-1545.
Fänge, A., and Iwarsson, S. (2003). Accessibility and usability in housing: Construct validity and implications for research and practice. Disability and Rehabilitation, 25(23), 1316-1325.
Fisher, Jr., A.H., Tzamaras, G.P., and Scherer, J.E. (2004). American Podiatric Medical Association best walking city competition, 2003. Journal of the American Podiatric Medical Association, 94(2), 211-215.
Frank, L., Engelke, P.O., and Schmid, T.L. (2003). Health and community: The impact of the built environment on physical activity. Washington, DC: Island Press.
Frank, L.D., Schmid, T.L., Sallis, J.F., Chapman, J., and Saelen, B.E. (2005). Linking objectively measured physical activity with objectively measured urban form: Findings from SMARTRAQ. American Journal of Preventive Medicine, 28(2 Suppl. 2), 117-125.
Freedman, V.A. (2011). Disability, functioning, and aging. In R. Binstock and L. George (Eds.), Handbook of aging and the social sciences (7th ed.). Ann Arbor, MI: Institute for Social Research.
Frumkin, H. (2003). Healthy places: Exploring the evidence. American Journal of Public Health, 93(9), 1451-1456.
Gershon, R., Pogorzelska, M., Qureshi, K., et al. (2008). Home health care patients and safety hazards in the home: Preliminary findings. In Agency for Healthcare Research and Quality, Advances in patient safety: New directions and alternative approaches (vol. 1, pp. 407-422). Rockville, MD: Agency for Healthcare Research and Quality. Available: http://www.ncbi.nlm.nih.gov/books/NBK43619/ [April 2011].
Gill, T.M., Williams, C.S., Robison, J.T., and Tinetti, M.E. (1999). A population-based study of environmental hazards in the homes of older persons. American Journal of Public Health, 89(4), 553-556.
Gitlin, L.N. (2003). Conducting research on home environments: Lessons learned and new directions. The Gerontologist, 43(5), 628-637.
Gitlin, L.N. (2007). The impact of housing on quality of life: Does the home environment matter now and into the future? In H.-W. Wahl and C. Tesch-Romer (Eds.), New dynamics in old age: Individual, environmental, and societal perspectives. Amityville, NY: Baywood.
Gitlin, L.N., and Corcoran, M. (2000). Making homes safer: Environmental adaptations for people with dementia. Alzheimer’s Care Today, 1(1), 50-58.
Gitlin, L.N., Hauck, W., Dennis, M., and Winter, L. (2005). Maintenance of effects of the home environmental skill-building program for family caregivers and individuals with Alzheimer’s disease and related disorders. Journals of Gerontology Series A: Biological and Medical Sciences, 60(3), 368.
Gitlin, L.N., Winter, L., Burke, J., Cherrett, N., Dennis, M.P., and Hauck, W.W. (2008). Tailored activities to manage neuropsychiatric behaviors in persons with dementia and reduce caregiver burden: A randomized pilot study. The American Journal of Geriatric Psychiatry, 16(3), 229.
Gitlin, L.N., Hauck, W., Dennis, M.P., Winter, L., Hodgson, N., and Schinfeld, S. (2009). Long-term effect on mortality of a home intervention that reduces functional difficulties in older adults: Results from a randomized trial. Journal of the American Geriatrics Society, 57(3), 476-481.
Gitlin, L.N., Jacobs, M., and Vause-Earland, T. (2010). Translation of a dementia caregiver intervention for delivery in homecare as a reimbursable medicare service: Outcomes and lessons learned. Gerontologist, 50(6), 847-854.
Gitlin, L.N., Winter, L., and Dennis, M.P. (2010). Assistive devices to help manage behavioral symptoms of dementia: What do caregivers use and find helpful? (special issue in honor of Dr. Fozzard). Gerontechnology, 9(3), 408-414.
Gitlin, L.N., Winter, L., Dennis, M.P., Hodgson, N., and Hauck, W.W. (2010). Targeting and managing behavioral symptoms in individuals with dementia: A randomized trial of a nonpharmacologic intervention. Journal of the American Geriatrics Society, 58(8), 1465-1474.
Golant, S. (2006). Supportive housing for frail, low-income older adults: Identifying need and allocating resources. Generations, 29(4), 37-43.
Golant, S.M. (2007). Low-income elderly homeowners in very old dwellings: The need for public policy debate. Journal of Aging & Social Policy, 20(1), 1-28.
Hebert, L.E., Scherr, P.A., Bienias, J.L., Bennett, D.A., and Evans, D.A. (2003). Alzheimer’s disease in the U.S. population: Prevalence estimates using the 2000 census. Archives of Neurology, 60, 1119-1122.
Institute of Medicine. (2008). Retooling for an aging America: Building the health care workforce. Committee on the Future Health Care Workforce for Older Americans. Board on Health Care Services. Washington, DC: The National Academies Press.
International Code Council and American National Standards Institute. (2004). ICC/ANSI A117.1: Accessible and usable buildings and facilities. Available: http://www.phfa.org/forms/architects/a117_1_2003.pdf [April 2011].
Iwarsson, S. (2005). A long-term perspective on person-environment fit and ADL dependence among older Swedish adults. Gerontologist, 45(3), 327-336.
Kagawa-Singer, M. (2001). Negotiating cross-cultural issues at the end of life. Journal of the American Medical Association, 286, 2993-3001.
Kai, M.C., Anderson, M., and Lau, E.M.C. (2003). Exercise interventions: Defusing the world’s osteoporosis time bomb. Bulletin of the World Health Organization, 81, 827-830.
Kulkarni, J., Wright, S., Toole, C., Morris, J., and Hirons, R. (1996). Falls in patients with lower limb amputations: Prevalence and contributing factors. Physiotherapy, 82(2), 130-136.
Kunkle, F. (2010). Virginia launching portable housing for aging relatives. The Washington Post, B01.
LaPlante, M.P., Hendershot, G.E., and Moss, A.J. (1992). Assistive technology devices and home accessibility features: Prevalence, payment, need, and trends. Advance Data, No. 217. Hyattsville, MD: U.S. Department of Health and Human Services. Available: http://www.eric.ed.gov/PDFS/ED351814.pdf [April 2011].
Lau, D.T., Scandrett, K.G., Jarzebowski, M., Holman, K., and Emanuel, L. (2007). Health-related safety: A framework to address barriers to aging in place. Gerontologist, 47(6), 830-837.
Lawler, K., and Berger, C. (2009). Lifelong communities: Re-imagining the Atlanta region from the ground up. Generations, 33(2), 76-78.
Li, W., Keegan, T., Sternfeld, B., Sidney, S., Quesenberry, C.P., Jr., and Kelsey, J.L. (2006). Outdoor falls among middle-aged and older adults: A neglected public health problem. American Journal of Public Health, 96(7), 1192.
Maisel, J., Smith, E., and Steinfeld, E. (2008). Increasing home access: Designing for visitability. Washington, DC: American Association of Retired Persons. Available: http://assets.aarp.org/rgcenter/il/2008_14_access.pdf [March 31, 2011].
Matthews, J.T., Beach, S.R., Downs, J., de Bruin, W.B., Mecca, L.P., and Schulz, R. (2010). Preferences and concerns for quality of life technology among older adults and persons with disabilities: National survey results. Technology and Disability, 22(1-2), 5-15.
National Advisory Board. (2009). Declaration for independence. Available: http://www.redorbit.com/news/health/1682745/national_advisory_board_issues_declaration_for_independence_a_calltoaction_in/index.html [March 31, 2011].
National Institute on Aging. (2001). Exercises: A guide from National Institute on Aging. Washington, DC: U.S. Department of Health and Human Services. Available: http://www.nia.nih.gov/NR/rdonlyres/25C76114-D120-4960-946A-3F576B528BBD/0/ExerciseGuideComplete.pdf [April 2011].
Newman, S.J., and Mezrich, M.N. (1997). Implications of the 1988 Fair Housing Act for the frail elderly. In S. Lanspery and J. Hyde (Eds.), Staying put: Adapting the places instead of the people (pp. 237-252). Amityville, NY: Baywood.
Nishita, C., Liebig, P., Pynoos, J., Perelman, L., and Spegal, K. (2007). Promoting basic accessibility in the home: Analyzing patterns in the diffusion of visitability legislation. Journal of Disability Policy Studies, 18(1), 2.
Norburn, J.E., Bernard, S.L., Konrad, T.R., et al. (1995). Self-care and assistance from others in coping with functional status limitations among national sample of older adults. Journal of Gerontology Social Sciences, 50B, S101-S109.
Nugent, C.D., Finlay, D.D., Fiorini, P., Tsumaki, Y., and Prassler, E. (2008). Editorial home automation as a means of independent living. IEEE Automation Science and Engineering, 5(1), 1-9.
Oberlink, M., and Stafford, P. (2009). The Indiana advantage initiative: Measuring community elder-friendliness and planning for the future. Generations, 33(2), 91-94.
Olsen, R.V., Ehrenkrantz, E., and Hutchings, B. (1993). Homes that help: Advice from caregivers for creating a supportive home. Newark, NJ: New Jersey Institute of Technology.
Piersol, C.V., and Ehrlich, P.L. (2009). Occupational therapy in home health care. Austin, TX: PRO-ED.
Pinquart, M., and Sörensen, S. (2006). Helping caregivers of persons with dementia: Which interventions work and how large are the effects? International Psychogeriatrics, 18, 577-595.
Pynoos, J. (1993). Towards a national policy on home modification. Technology and Disability, 2(4), 1-8.
Pynoos, J., and Nishita, C. (2003). The cost and financing of home modifications in the United States. Journal of Disability Policy Studies, 14, 68-73.
Pynoos, J., Cohen, E., Davis, L., and Bernhardt, S. (1987). Home modifications: Improvements that extend independence. In V. Regnier and J. Pynoos (Eds.), Housing the aged: Design directives and policy considerations (pp. 277-303). New York: Elsevier.
Pynoos, J., Angelleli, J., Tabbarah, M., and Demiere, M. (1998). Improving the delivery of home modifications. Technology and Disability, 8(1/2), 3-14.
Pynoos, J., Liebig, P., Overton, J., and Calvert, E. (1997). The delivery of home modification and repair services. In S. Lanspery and J. Hyde (Eds.), Staying put: Adapting the places instead of the people (pp. 173-192). Amityville, NY: Baywood.
Pynoos, J., Rose, D., Rubenstein, L., Choi, I.H., and Sabata, D. (2006). Evidence-based interventions in fall prevention. Home Health Care Services Quarterly, 25(1), 55-73.
Pynoos, J., Nishita, C., Cicero, C., and Caraviello, R. (2008). Aging in place, housing, and the law. Elder Law Journal, 16, 77-107.
Pynoos, J., Steinman, B.A., and Nguyen, A.Q. (2010). Environmental assessment and modification as fall-prevention strategies for older adults. Clinics in Geriatric Medicine, 26(4), 633-644.
Roper, P., Green, F., Tziotis, M., and Veith, G. (2003). Revision of Austroads safety barriers guidelines. In Proceedings-Conference of the Australian Road Research Board (vol. 21, pp. 2107-2119). Melbourne, Australia: ARRB Transport Research.
Rubinstein, R.L. (1990). The home environments of older people: A description of the psychosocial processes linking person to place. Journal of Gerontology, 44, S45-S53.
Saelens, B.E., Sallis, J.F., and Frank, L.D. (2003). Environmental correlates of walking and cycling: Findings from the transportation, urban design, and planning literatures. Annals of Allergy Asthma & Immunology, 25(2), 80-91.
Sallis, J.F., and Owen, N. (1999). Physical activity and behavioral medicine. Thousand Oaks, CA: Sage.
Sanford, J. (2010). The physical environment and home healthcare. In National Research Council, The role of human factors in home health care: Workshop summary (pp. 201-246). S. Olson, Rapporteur. Committee on the Role of Human Factors in Home Health Care. Committee on Human-Systems Integration, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press.
Schaie, K.W., Wahl, H.-W., Mollenkopf, H., and Oswald, F. (2003). Aging independently: Living arrangements and mobility. New York: Springer.
Siebert, S. (2009). The clinic called home. In C.V. Piersol and P.L. Ehrlich (Eds.), Occupational therapy in home health care. Austin, TX: PRO-ED.
Social Security and Medicare Board of Trustees. (2009). A summary of the 2009 annual reports. Available: http://www.ssa.gov/OACT/TRSUM/index.html [March 31, 2011].
Sörensen, S., Pinquart, M., Habil, D., and Duberstein, P. (2002). How effective are interventions with caregivers? An updated meta-analysis. Gerontologist, 42, 356-372.
Stark, S. (2008). Removing environmental barriers in the homes of older adults with disabilities improves occupational performance. In W.W. Dunn (Ed.), Bringing evidence into everyday practice: Practical strategies for healthcare professionals (pp. 267). Thorofare, NJ: SLACK.
Steinfeld, E., and Shea, S. (2001). Fair housing: Toward universal design in multifamily housing. In W.F.E. Preiser and E. Ostroff (Eds.), Universal design handbook (Chapter 35). New York: McGraw-Hill.
Story, M. F. (2001). Principles of universal design. In W.F.E. Preiser and E. Ostroff (Eds.), Universal design handbook (Chapter 10). New York: McGraw-Hill.
Stuck, A.E., Egger, M., Hammer, A., Minder, C.E., and Beck, J.C. (2002). Home visits to prevent nursing home admission and functional decline in elderly people: Systematic review and meta-regression analysis. Journal of the American Medical Association, 287, 1022-1028.
Suminski, R.R., Poston, W.S.C., Petosa, R.L., Stevens, E., and Kazenmoyer, L.M. (2005). Features of the neighborhood environment and walking by U.S. adults. American Journal of Preventive Medicine, 28(2), 149-155.
U.S. Census Bureau. (2010). American fact finder: Urban and rural. Available: http://factfinder.census.gov [March 31, 2011].
U.S. Department of Housing and Urban Development. (2009). Leading our nation to healthier homes: The healthy homes strategic plan. Washington, DC: Author.
U.S. Department of Veterans Affairs. (2010). VA pamphlet 26-69-1: Questions on specially adapted housing and special housing adaptations (online version). Washington DC: Author. Available: http://www.questmobilitysolutions.com/resources/veterans/part2_va_pamphlet_26_jrd_edits_doc_rev_11052009.pdf [April 2011].
van Haastregt, J.C.M., Diederiks, J.P.M., van Rossum, E., deWitte, L.P., and Crebolder, H.F.J.M. (2000). Effects of preventive home visits to elderly people living in the community: A systematic review. British Medical Journal, 320, 754-758.
Vincent, G., and Velkoff, V. (2010). The next four decades, the older population in the United States: 2010 to 2050. Available: http://www.aoa.gov/AoARoot/Aging_Statistics/future_growth/DOCS/p25-1138.pdf [July 12, 2010].
Vladeck, F. (2004). A good place to grow old: New York’s model for NORC supportive service programs, a special report from the United Hospital Fund. New York: United Hospital Fund.
Wahl, H.W., Fänge, A., Oswald, F., Gitlin, L., and Iwarsson, S. (2009). The home environment and disability-related outcomes in aging individuals: What is the empirical evidence? Gerontologist, 49(3), 355-367.
World Health Organization. (2002). Active aging: A policy framework. Geneva, Switzerland: Author.
Wrosch, C., Schulz, R., and Heckhausen, J. (2002). Health stresses and depressive symptomatology in the elderly: The importance of health engagement control strategies. Health Psychology, 21, 340-348.
Wu, S.Y., and Green, A. (2000). Projection of chronic illness prevalence and cost inflation. Santa Monica, CA: RAND Health.
Young, L.C., and Pace, R.J. (2001). Fair housing: Toward universal design in multifamily housing. In W.F.E. Preiser and E. Ostroff (Eds.), Universal design handbook (Chapter 34). New York: McGraw-Hill.


























