2
People Involved in Health Care in the Home
The health care delivery system is rapidly changing, and individuals are assuming an increasing role in management of their own health. In this environment, individuals and their families are expected to perform a range of health care tasks and interact with a vast array of medical devices and technologies in residential settings. However, the population of people who receive and provide care is very diverse and possesses variable skills, resources, knowledge, and experiences. They also differ on a number of other characteristics, such as age, cultural and ethnic backgrounds, education, and living arrangements.
Management of health care at home presents numerous challenges, especially since the characteristics of individuals who engage in health care tasks and interact with health care systems and technologies vary so greatly. Ensuring that health care in the home is safe, efficient, effective, and responsive to individual needs requires identifying potential user groups who will be interacting with home health systems; understanding the capabilities/limitations, needs, and preferences of these populations; and matching these capabilities, needs, and preferences to the demands generated by health care and health management tasks, technologies, and the environments in which these tasks occur.
This chapter provides an overview of users—the people who receive and the people who provide health care in the home. We define the broad populations of interest and describe abilities and characteristics of each group relevant to the tasks that they are expected to perform.
We begin by broadly defining and briefly describing three groups of
TABLE 2-1 Types of People Involved in Health Care in the Home
| Category | Examples |
| Care Recipients | Infants |
| Children | |
| Adults | |
| Elders | |
| Informal Caregivers |
Care recipients themselves |
|
Immediate family members |
|
|
Extended family members |
|
|
Friends |
|
|
Neighbors |
|
|
Colleagues |
|
|
Other acquaintances |
|
| Formal Caregivers |
Home health aides, personal care attendants, social service aides |
|
Nurses |
|
|
Physicians |
|
|
Pharmacists |
|
|
Social workers |
|
|
Physical, occupational, vocational, respiratory, speech-language therapists |
|
|
Dieticians |
individuals who engage in health care in the home: people who receive care (recipients), people who are informal providers of care (informal caregivers), and people who are formal providers of care (formal caregivers) (see Table 2-1). One distinction between informal and formal caregivers is that informal caregivers are typically not paid for the care provided. In addition, formal caregivers are more likely to have health care training, although it is not always specific to the provision of care in the home. We describe abilities and characteristics of people relevant to the performance of health care tasks that are common across all three groups. We also describe circumstances (e.g., living arrangements) and qualifications (e.g., type of certification) that are unique to each group and how they may influence the performance of health care tasks in the home. The overarching goal is to demonstrate how an understanding of the characteristics and abilities of these people is critical to the design of safe and effective systems of health care in the home.
RECIPIENTS OF HEALTH CARE IN THE HOME
People involved in health care in the home range from young to old and include people who are well and those with a variety of medical con-
ditions, disabilities, and impairments. People who receive care vary in as many characteristics as the population at large, including culture/ethnicity, education, and socioeconomic status, as well as in physical abilities, such as strength and stamina, manual dexterity, visual acuity, cognition, health and technology literacy, and level of skill.
Almost everyone is involved in some type of health care activity at home. These activities include disease prevention and health maintenance activities (e.g., regular exercise, health information seeking) and management of acute ailments (e.g., colds, minor infections, injuries) and chronic diseases (e.g., diabetes, multiple sclerosis) and disabilities (e.g., vision, hearing, mobility or cognitive impairment). Everyone has the potential to become a recipient or provider of health care, and these roles can change over time.
One large population of people who receive care at home are those with chronic conditions, such as hypertension, asthma, diabetes, cancer, HIV/AIDS, chronic respiratory disease, neuromuscular disease, dementia, or emotional disorders. Currently, about 60 percent of the adult civilian noninstitutionalized population of the United States has at least one chronic condition, and people with chronic conditions incur approximately 75 percent of the nation’s health care expenditures (Centers for Disease Control and Prevention, 2009a). The Centers for Disease Control and Prevention (2009a) defines chronic diseases as “noncommunicable illnesses that are prolonged in duration, do not resolve spontaneously, and are rarely cured completely.” The five most costly chronic conditions in 2006 were heart conditions, cancer, trauma-related disorders, mental disorders, and asthma (Soni, 2009).
Although chronic conditions may be acquired at any point in the life course (e.g., those resulting from trauma-related injuries), some are more prevalent in various age groups. Examples are children on ventilators; children with diabetes or asthma who require insulin or inhaler treatments; adults with sleep apnea who use positive airway pressure equipment; people with renal failure who use home dialysis while waiting for or avoiding costly kidney transplantations; and middle-aged or older people with diabetes, arthritis, cardiovascular conditions, dementia, or AIDS who follow complex medication regimens.
The population of people involved in health care in the home also includes persons with physical, sensory/perceptual, cognitive, and emotional disabilities. According to the U.S. Census Bureau (Brault, 2008), approximately 49 million people in the United States over 15 years of age have some form of disability. This includes people who have long-lasting conditions that make it difficult to do routine activities, such as seeing, hearing, learning, remembering, walking, climbing stairs, dressing, bathing, leaving the home, or working at a job. The likelihood of having a dis-
ability and the likelihood the individual will need assistance increase with age, particularly after age 65 (Brault, 2008). Figure 2-1 illustrates how the percentage of people with disabilities increases with age, rising from 10 percent of 15-24-year-olds to 70 percent of those over age 80. As the population ages in coming decades, the number of people with disabilities may increase, although there is some evidence that disability rates may be declining (Freedman et al., 2007). Individuals with disabilities represent a significant population of people who engage in or receive care at home.
The population of people with disabilities includes large numbers of veterans who have served in U.S. military forces during conflicts including and since World War II. Approximately 2.6 million veterans were receiving disability compensation benefits in September 2007 (Economic Systems Inc., 2008). The types of disability observed in veteran populations tend to differ from those in the civilian population. Veterans’ disabilities are often musculoskeletal disorders (45 percent) and mental disorders that include posttraumatic stress disorder (15 percent). A high percentage of veterans have multiple disabilities (Economic Systems Inc., 2008), such as co-occurring musculoskeletal and hearing problems.
These prevalent types of disability have implications for home health care system design. Health care device manufacturers must design for ease
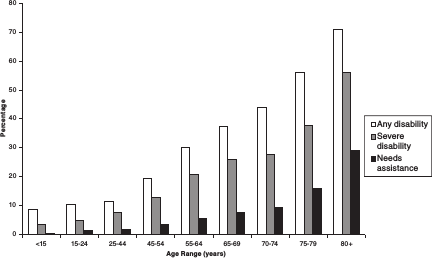
FIGURE 2-1 Percentage of disability prevalence and needs for assistance by age, 2005.
SOURCE: Brault (2008).
of manipulation (e.g., they must permit one-handed operation of devices similar to requirements for keyboard use in Section 508 of the Rehabilitation Act) and delivery of instruction through text rather than (or in addition to) voice (Charness, 2010). Similarly, for veteran populations, vision rather than hearing should often be the preferred channel for providing information about system states and warnings. The large numbers of veterans who experience cognitive problems due to head trauma or to multiple traumas, such as limb amputation coupled with head trauma, must also be recognized. These individuals may find it particularly difficult to interact with a variety of technologies and devices. They are also likely to need assistance with routine activities as well as emotional support for many years, given that many acquired these disabilities as young adults.
It is important to recognize that disability is associated with health care disparities. Data from the 2006 National Health Interview Survey show that disability and disability coupled with gender were predictive of lack of access to health care. Specifically, people with disabilities were two to three times less likely than those without disabilities to have access to health care. In addition, women with disabilities had less access to health care than either women without disabilities or men with disabilities (Smith, 2008).
CAREGIVERS
People who provide care to ill or disabled individuals in the home can be broadly categorized as either informal (e.g., family) or formal (e.g., professional) caregivers. Informal caregivers include individuals providing their own care as well as people who provide health-related assistance to individuals to whom they are related or otherwise associated. Informal caregivers typically do not receive financial compensation for the care they provide and are predominantly relatives, but they may include individuals’ friends, neighbors, or members of volunteer organizations. Informal caregivers are also referred to as family caregivers, lay caregivers, or simply family and friends who provide assistance by virtue of kinship, friendship, or altruism.1
In contrast, formal caregivers (sometimes referred to as professional caregivers2) have often had formal health care training and have some level of service delivery skill and education. However, some formal caregivers who provide care in the home have no formal health care training. Formal caregivers include physicians and physician assistants, nurses, nurse
_____________
1In places where research cited is specifically referring to family members who provide care, the term family caregiver is used.
2The committee decided to use the term formal caregivers in recognition of the fact that some family members or other informal providers of care are also professionals.
practitioners, social workers, physical, occupational and speech therapists, pharmacists, and home health aides.
Both informal and formal caregivers are also quite heterogeneous, varying widely in their skills, abilities, and attitudes.
CHARACTERISTICS AND ABILITIES
The person component of the home-based health care equation is complex, and understanding people’s abilities and characteristics is critical to the design and selection of safe, efficient, and effective care devices (Scherer et al., 2007) as well as the overall care system for the home. Performance of health care tasks places a variety of physical, cognitive, sensory/perceptual and emotional demands on people, whether they are caring for themselves
BOX 2-1
The Lopez Family
Ricardo Lopez, an 82-year-old retired teacher of Cuban descent, takes care of his wife Dolores, who in her mid-70s was diagnosed with Alzheimer’s disease, approximately 7 years ago. The couple lives in a small one-bedroom apartment in Florida, within walking distance of a small local grocery store and pharmacy. Ricardo speaks both English and Spanish, and Dolores used to speak Spanish. Two years ago, she stopped talking and is now only able to make sounds whenever she gets emotional. This is very difficult for Ricardo to deal with, as he feels he has lost the ability to communicate with his wife; he misses her voice and their long talks. Dolores also shows other signs of mental and physical deterioration, and she depends on Ricardo to help her with all activities of daily living, such as feeding herself, bathing, dressing, and getting into and out of the bed or chair.
Ricardo is consumed with all aspects of Dolores’s care and often neglects his own personal needs. He does not go to the doctor on a regular basis, because he does not have time or someone to take care of Dolores in his absence. He is in overall good health, but he has to monitor his blood pressure and diet.
Ricardo recently accepted the advice of a community social worker to have Dolores attend a day care program three times a week, which gives him some respite. Although getting her ready in the morning is very challenging, he does it because he feels that Dolores needs to be stimulated by engaging in social activities. She was a pianist and enjoys being around people and music.
or fulfilling the caregiver role. These demands can vary in complexity and the level of skill required. Health care tasks may also involve some type of equipment or technology, which presents its own set of demands, and may be performed in various environments that generate additional demands. (The family vignette in Box 2-1 illustrates some of this complexity.)
Cognitive abilities (e.g., memory, reasoning) and physical and motor functioning (which often decline with age) impact a person’s ability to read and comprehend medication instructions, access medications, comply with medication regimens, and use technologies and assistive devices. Physical capabilities affect whether a caregiver can safely assist with such tasks as patient lifting and bathing. Sensory/perceptual capabilities determine whether someone can read the display on a medical device, such as an infusion pump, or hear an alarm, such as on an apnea monitor. Other
During the time that Dolores is at day care, Ricardo can go to the grocery store and pharmacy and do household chores. Although he has no formal training, he says, he does his best to keep the house clean. He tries to organize all of his errands and tasks to be done before the weekend, because on Saturday and Sunday he does not have any help. He spends most of that time preparing the week’s meals for Dolores, with the idea that if he keeps her healthy, he can minimize the chances of her being hospitalized.
Last summer Dolores was hospitalized for almost a month for problems with her digestive system. This was very stressful for Ricardo, as he had to travel to and from the hospital and often had to stay with Dolores overnight. He is thankful to have the support of friends and some of Dolores’s family members, such as her sisters and a niece. They don’t visit often but they do send home-cooked meals to help him.
Ricardo and Dolores do not have any children together, but Ricardo has a 58-year-old son who was recently hospitalized due to complications with a diabetic ulcer. Ricardo feels guilty that he is unable to visit his son as much as he would like, and he calls him every day to check up on him. Ricardo’s son recently gave him a computer, and Ricardo has learned how to look up information and keep in contact with old friends who live in Spain and Mexico. At night he spends a few hours chatting online and keeping up with the news. For him, this is time he dedicates to himself, and he wishes he could learn more about how to use the computer.
_____________
SOURCE: Client at the University of Miami Miller School of Medicine.
characteristics and abilities, such as education, language/communication proficiency, health status, health literacy, health self-efficacy, knowledge of specific health conditions and treatments, culture, autonomy, social participation, personality, motivation, attitudes/beliefs, and trust are all important to the performance of health care tasks. In addition to the personal capabilities mentioned above, relevant attributes also include caregivers’ skill level, technology literacy, attitude toward care recipients, coping ability, and ability to manage their workload.
Cognitive abilities influence a person’s ability to process, comprehend, and integrate health information and to decide on and execute the appropriate response. For some user groups, the complex cognitive demands associated with current health care tasks and equipment/technologies may exceed user capabilities. Normal aging is associated with declines in “fluid abilities such as reasoning, attentional capacity and working memory” (Fisk et al., 2009). However, cognitive declines are possible at all ages as a result of illness, head trauma, the side effects of medication, or the complications of stress, learning disabilities, or developmental disabilities. In addition, cognitive abilities may wax and wane over time due to the effects of fatigue, pain, drugs, or disease progression. Care recipients (and even caregivers to the extent that fatigue and their own health challenges affect them) can be competent at times and impaired at others.
Physical impairments may affect mobility and gross motor movements, such as shifting the body from one posture or location to another, and declines in strength and stamina are common among people with diminished health. Limitations in manual dexterity may affect a person’s ability to operate controls on equipment or open medication containers. Older adults often have slower walking speeds, and they may experience negative changes to the vestibular system that make balance less stable, increasing the risk of injury when caring for themselves (e.g., dressing, walking on uneven surfaces) or caring for others (e.g., helping a spouse move onto or off a bed or toilet) (Charness, 2010). Aging is often accompanied by decreases in ability to execute precise movements, which may make it difficult for older people to use small controls or use input devices, such as a keyboard, mouse, or touch screen. Chronic conditions, such as arthritis, may affect one’s ability to execute movements precisely, operate controls, open containers, or grasp objects. These limitations are even more pronounced for people who have limb tremor or movement initiation disorders (e.g., Parkinson’s disease).
Sensory/perceptual skills, critical to many tasks, are limited in many people. Recent data from the National Health Interview Survey indicate that, among adults ages 18 and older, about 15 percent have hearing impairments, 11 percent have some type of visual impairment, and 3.3 percent have combined vision and hearing impairments (U.S. Department of
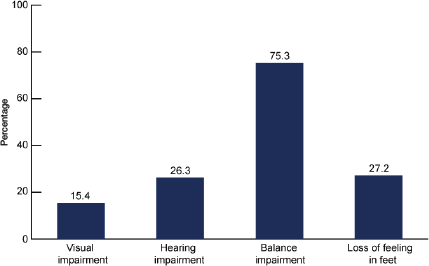
FIGURE 2-2 The prevalence of sensory impairments among people ages 70 and over, United States, 1999-2006.
SOURCE: Dillon et al. (2010).
Health and Human Services, 2009). These impairments, as well as additional impairments in balance and loss of feeling in feet, are more prevalent in older adults age 70 and over (see Figure 2-2). Declines in sensory abilities such as vision may make it difficult for people to read labels on medication containers or on controls of devices, and auditory declines may make alarm sensing and communication problematic.
Language and communications skills can have a profound impact on ability to access and implement care requirements and live independently at home. For many reasons, including the rise in non-English speakers,3 many people may not easily express themselves well, comprehend complex instructions, or be able to use a health care device when provided with written instructions. It is estimated that 93 million U.S. adults have English literacy skills that are categorized as “basic” and “below basic.” Rates of low literacy are higher among populations of lower socioeconomic status, older adults, and minorities (Kutner et al., 2006). Furthermore, for significant numbers of Americans, English language–only health care materials are inadequate. People with mental health problems are prone to
_____________
3Data from the 2000 U.S. census indicate that nearly 47 million people—or about 1 in 5 U.S. residents ages 5 and older—regularly speak a foreign language at home, representing an increase of 15 million people since 1990.
communication and language deficits, since, as a result of their conditions, they may have difficulties with memory, understanding, reasoning, talking, swallowing, and/or may have altered social skills and reduced nonverbal skills. Whether barriers such as weak language or cognitive skills can be surmounted by instructional materials that make greater use of symbols, diagrams, or video is not yet well understood (e.g., Morrell and Park, 1993).
The average age of the U.S. population is increasing because of relatively low birth rates coupled with declining death rates. Population projections indicate that by 2020, there will be an estimated 55 million people ages 65 and older and 6.6 million people ages 85 and older (Administration on Aging, 2009).
Older adults are more likely to have some type of disability. In addition, older adults experience increased activity limitations as they age as a result of chronic health conditions (see Figure 2-3). The older population is predominantly female (although this phenomenon is expected to be less
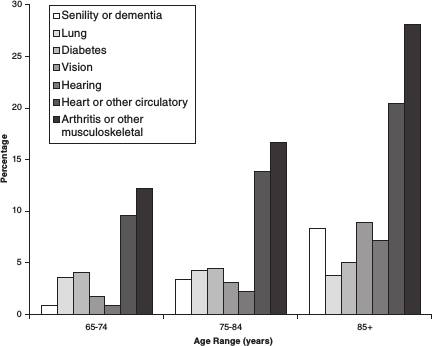
FIGURE 2-3 Older adults with limitations in activities.
SOURCE: Centers for Disease Control and Prevention (2009b).
pronounced in the future), and many of these women are likely to live alone.4 Older adults as a whole have low health literacy, and the current cohort of elders is less likely to be familiar with computers and the Internet (Jones and Fox, 2009). Generally, older adults are less comfortable about adopting new technologies than are younger adults and have lower computer self-efficacy and less comfort with computers than other age groups (Nair, Lee, and Czaja, 2005; Czaja et al., 2006).
Educational achievement has increased over the past 70 years in the United States. The percentage of the population ages 25 and older that has completed 4 years of high school has risen from less than 40 percent in 1940 to nearly 90 percent in 2003. The proportion of the population that has completed 4 or more years of college has increased sixfold from 5 to over 30 percent (Stoops, 2004). Higher educational attainment is generally associated with higher income, better health, and greater longevity. These educational increases bode well for the ability of future generations to cope with complex health care regimens and equipment. However, it is important to recognize that educational disparities exist in all age groups.
Attitudinal variables also affect a person’s performance of health care tasks. General attitudes toward health and health care have a strong influence on willingness to seek care and adherence to treatment protocols. Beliefs in one’s ability to successfully carry out health care protocols and beliefs about the effectiveness of these protocols have a strong impact on treatment adherence and willingness to adopt behavioral changes. Trust is another important consideration. In today’s world, this includes trust that one will have access to needed care, trust in caregivers, and trust in health care technologies. The distinction between distrust and overtrust should be recognized. Distrust, which can evolve from a number of attitudes including lack of confidence in knowledge or skills or concerns about privacy, can lead to the rejection of advice, use of an aid, or piece of technology. Conversely, overtrust can lead to complacency and failure to question or recognize malfunctions or misreadings under the presumption that equipment is working properly.
Ethnicity/Culture
Marked changes in the ethnic composition of the United States have occurred and are expected to continue over the coming decades. Overall, the Hispanic population is expected to double in size from 2000 to 2050, and the Asian population is projected to increase by 79 percent. Other ethnic minority groups, such as blacks and American Indians, will also
_____________
4In 2005, among people ages 85 and older, only 15 percent of women but 57 percent of men lived with their spouse (U.S. Census Bureau, 2007).
see moderate growth (Ortman and Guarmeri, 2009; U.S. Census Bureau, 2009). The older adult (ages 65+) minority populations are also projected to increase from 8.0 million in 2010 (20.1 percent of the elderly) to 12.9 million in 2020 (23.6 percent of the elderly) (Administration on Aging, 2009).
The prevalence of disease and disability and the risk factors, health behaviors, and access to and utilization of health services differ substantially by race and ethnicity as well as age. Many racial/ethnic minorities and individuals of lower socioeconomic status are less likely than whites and persons of higher socioeconomic status to have a usual source of care, to have access to quality care, and to engage in preventive health practices. These groups also tend to experience disproportionately some chronic illnesses and conditions, such as obesity, hypertension, and diabetes. For example, diabetes is more common among non-Hispanic blacks and Mexican Americans than among non-Hispanic whites (U.S. Department of Health and Human Services, 2010). There is also racial/ethnic variation in rates of disability (see Figure 2-4).
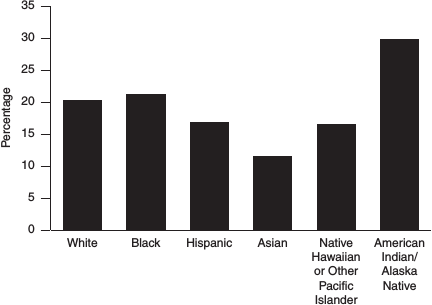
FIGURE 2-4 Disability rates among U.S. adults (≥ 18 years) by race and ethnicity, 2004-2006.
SOURCE: Centers for Disease Control and Prevention (2008).
With respect to technologies such as computers and the Internet, although use of these technologies by Hispanics and blacks is increasing, it still lags behind utilization rates of whites (Jones and Fox, 2009; Livingston, Parker, and Fox, 2009). This is important given the increased use of the Internet as a vehicle for delivery of health information and services.
For a racial/ethnic group whose primary means of communication is through a language other than English, translation of health materials originally written in English into a second language may be necessary. In this case, care should be taken to ensure that the translation is adequately performed and is sensitive to differences in culture (Taylor and Lurie, 2004). Lack of understanding of health documents or instructions may increase health disparities among racial/ethnic groups (U.S. Department of Health and Human Services, 2001).
Perceptions of power and cultural influences on attitudes about health and illness are also important to consider. Power differentials between care recipients and the health care system may be especially uncomfortable for minority racial and ethnic groups. Discomfort with this power difference arises from historical experiences and is reinforced by current practices (Valdez and Brennan, 2008). In addition, mental models about the nature of illness do not always transcend ethnic and racial boundaries. The majority population in the West believes in the use of allopathic medicine (i.e., that disease can be treated by drugs that have an antagonistic effect to the disease), but many cultures do not share this mental model. Mental models of illness vary among cultures and are informed by such factors as tradition, experiences, and religion (Valdez and Brennan, 2008).
Informal caregivers respond differently to the caregiving experience depending on their ethnic/cultural background. Implementing culturally competent interventions and care programs can help to overcome the cultural distance between caregivers, their care recipients, and associated communities and enhance health outcomes among diverse racial/ethnic groups (e.g., Gallagher-Thompson et al., 2003). These approaches include tailoring the language and images used in educational materials and brochures, becoming familiar with the histories and cultural norms of different populations, eliciting people’s health beliefs and the context in which they experience illness, and developing mutually agreeable treatment plans (Gallagher-Thompson et al., 2003).
If issues related to power mismatch, mental models of illness, and language barriers are not addressed, racial/ethnic groups may refuse to follow health care procedures or use medical equipment or may fail to act when they do not understand health care tasks well. As a result, disparities in health status and health outcomes and rates of health care utilization could continue or increase (Valdez and Brennan, 2008).
Health Literacy
Currently, nearly half the U.S. population has difficulty understanding and using health information. Particularly vulnerable populations include elderly individuals, minority populations, people with chronic mental or physical health conditions, and people of lower socioeconomic status. Low health literacy has vast implications for home-based health care, having been linked to higher rates of hospitalization and use of expensive emergency services as well as lower use of preventive services (e.g., Baker et al., 2002).
Health literacy is defined in Healthy People 2010 as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” (U.S. Department of Health and Human Services, 2000, vol. 1, pp. 11-20). Health literacy includes the ability to understand instructions on prescription drug bottles and wording on appointment slips, medical education brochures, instructions and communications from doctors, medical consent forms, and health insurance plans, among others. Health literacy requires reading, listening, analytical and decision-making skills, and the ability to apply these skills to health situations.
Individuals and their family members at home often confront complex information and treatment decisions. They have to engage in such tasks as finding relevant health information, evaluating that health information for credibility and quality, analyzing relative risks and benefits of recommended treatment or health behaviors, calculating dosages, and interpreting test results. In order to accomplish these tasks, individuals need to be visually literate (able to understand graphs or other visual information), numerically or computationally literate (able to calculate or reason numerically), and analytically literate (able to integrate and apply relevant information). Oral language skills are important as well, as they enable individuals and their caregivers to articulate health concerns, describe symptoms and responses to treatment, ask pertinent questions, and understand spoken medical advice or treatment instructions. In an age of shared responsibility between consumers and providers of health care, individuals need strong decision-making skills. With the development of the Internet as a source of health information, health literacy has begun to include the ability to use a computer, search the Internet, and evaluate websites (U.S. Department of Health and Human Services, 2000).
INFORMAL CAREGIVERS
Rosalyn Carter is often quoted for her observation that there are only four types of people in the world: “those who have been caregivers; those
who currently are caregivers; those who will be caregivers; and those who will need caregivers” (Carter, 1997). It follows that informal caregivers represent a broad and diverse group of individuals and are therefore difficult to characterize (see Table 2-1). Informal caregivers span the spectrum of age and are heterogeneous across multiple dimensions that include their relationship to and geographical proximity to the people for whom they provide care and the nature, duration, and intensity of the assistance they provide. They also vary in their level of competence and skill, their motivations for providing assistance, and the attitudes they bring to their role.
Prevalence of Informal Caregiving
Estimates of the number of informal caregivers in the United States vary widely across surveys. At one extreme is an estimate that 28.5 percent of the U.S. adult population, or 65.7 million people, provide unpaid care to an adult or child with special health care needs (National Alliance for Caregiving and American Association of Retired Persons, 2009). This figure is similar to the estimated 59 million adults with a disability in the United States found in the Behavioral Risk Factor Surveillance System survey (Centers for Disease Control and Prevention, 2006). A smaller estimate, reported by the Survey of Income and Program Participation, is that 28.8 million caregivers assist persons ages 15 and older with personal everyday needs (National Family Caregivers Association and Family Caregiver Alliance, 2006). A review of eight nationally representative surveys found published estimates ranging in magnitude from 2.7 to 36.1 million informal caregivers providing care to older disabled adults (Giovanetti and Wolff, 2010). Most prevalence estimates of caregivers from national surveys reflect ongoing assistance related to chronic disability. Intermittent episodes of caregiving are not well represented and are less well understood.
Children typically experience multiple acute illnesses that require assistance from adults, and children who have chronic disabilities require intensive and sometimes long-term support from their parents or other caregivers. The 2005-2006 National Survey of Children with Special Health Care Needs estimates that 13.9 percent of children under age 18 have special health care needs, defined in terms of use of services, therapies, counseling, or medications, or have functional limitations that persist for at least a year (U.S. Department of Health and Human Services, Health Resources and Services Administration, and Maternal and Child Health Bureau, 2008).
In some cases, grandparents have primary responsibility for the care of children. According to data from the 2000 U.S. census, 2.4 million individuals over age 30 were grandparent caregivers, defined as people who had primary responsibility for coresident grandchildren younger than age 18. The prevalence was particularly high among blacks (4.3 percent of the
population age 30 or older) and American Indians and Alaska Natives (4.5 percent), compared with Hispanics (2.9 percent) and whites (1.1 percent, Simmons and Dye, 2003).
Recently it has also been recognized that some informal caregivers are children. One recent survey estimated that as many as 1.4 million children in the United States between the ages of 8 and 18 provide care for an older adult (Levine et al., 2005).
Because most surveys of caregivers are restricted to individuals who provide hands-on assistance with chronic illness and disability, gaps exist in knowledge of the numbers of other caregivers, such as individuals who assist from a distance or during time-limited episodes or who provide care to individuals at the end of life. In addition, recent events have resulted in unanticipated caregiving challenges, as veterans return from ongoing wars with multiple, interacting injuries or multiple traumas. The need for sustained caregiving for veterans is potentially immense, and the nature of the challenges for their informal caregivers is poorly understood.
Personal Characteristics
It is not surprising that the attributes of caregivers vary across surveys, given the wide variability in estimates of their numbers and the definitions employed. However, most data suggest that caregivers to older adults are typically female and are spouses or adult children of the people for whom they provide care and who either reside with or live in close proximity (e.g., National Alliance for Caregiving and American Association of Retired Persons, 2009). Approximately one-third to one-half of family caregivers to older adults are employed; employment rates are higher among caregivers who are adult children than for spouses, and higher among secondary caregivers than among those taking primary responsibility (Spillman and Pezzin, 2000). There is some evidence that blacks and Hispanics are more likely to be engaged in caregiving than are whites (Roth et al., 2009). As a group, caregivers are more likely to be of lower socioeconomic status (National Association for Caregiving and American Association of Retired Persons, 2004). The limited available information regarding child caregivers suggests that they also are more likely to come from households with lower incomes, less likely to reside in a two-parent home, and more likely to experience depression and anxiety when compared with their noncaregiving counterparts (Levine et al., 2005).
Roles and Responsibilities
Informal caregivers are involved in a wide range of household, personal care, and medically oriented tasks. The role that is perhaps most widely rec-
ognized is in assisting with personal care (activities of daily living, or ADLs: typically eating, dressing, bathing, transferring, toileting) and conducting household tasks (instrumental activities of daily living, or IADLs, such as shopping, transportation, meal preparation, money management, light housework, and laundry). Data from the National Long Term Care Survey and its Informal Caregivers Survey indicate that caregivers commonly assist with the full range of these tasks. In one study, primary caregivers helped chronically disabled older adults with shopping and/or transportation (85.3 percent), household tasks (77.7 percent), finances (49.4 percent), personal care and nursing (48.5 percent), and indoor mobility (35.1 percent) (Wolff and Kasper, 2006). These tasks commonly characterize long-term assistance provided to an older adult with a physical or cognitive disability.
In a 2009 survey conducted by the National Alliance for Caregiving (NAC) and the American Association of Retired Persons (AARP), the most common tasks performed by caregivers to children with special health care needs were reported as (National Alliance for Caregiving and American Association of Retired Persons, 2009)
- monitoring and reporting on condition severity (e.g., with school or government agencies, 85 percent),
- ensuring that people understand how to interact with and handle their child (84 percent),
- advocating for their child (72 percent),
- providing treatments and therapies (65 percent),
- administering medications or injections (64 percent),
- assisting with physical therapies/treatments (44 percent),
- preparing special diets (40 percent), and
- arranging paid services (39 percent).
Informal caregivers’ involvement in health care delivery processes has been less systematically studied but is no less important. A substantial 43-53 percent of family caregivers perform medically oriented tasks in facilitating wound care, injections, equipment, or medication administration (Donelan, Hill, and Hoffman, 2002; Wolff and Kasper, 2006). Family caregivers who provide assistance to individuals with cognitive impairments, such as Alzheimer’s, are widely acknowledged as taking responsibility for the full range of health care activities, including medical decision making. Caregivers commonly accompany care recipients to medical appointments and are actively engaged in medical communications (Schilling et al., 2002; Clayman et al., 2005; Wolff and Roter, 2008). The complexity of identifying and gaining access to health and social service support options that might be useful to family caregivers is daunting, even to experienced health professionals cast into the family caregiving role
(Kane, Preister, and Totten, 2005). The average informal caregiver faces significant challenges in optimizing formal support services to minimize the burdens of caregiving.
Ability to Provide Care
In addition to the range of physical, sensory, emotional, cognitive, perceptual, and intellectual attributes described earlier, several considerations affect informal caregivers’ ability to provide care. Family dynamics and history, competing life demands, and available financial and social resources collectively influence the context of assistance and caregivers’ motivation and capacity to provide high-quality care. The geographic proximity of informal caregivers to the person for whom they provide care is another important consideration. One study of living arrangements found that 24 percent of caregivers lived in the same house, 42 percent lived within 20 minutes, 19 percent lived between 20 and 60 minutes away, 5 percent lived 1 to 2 hours away, and 10 percent lived more than 2 hours away from the individual’s home (National Alliance for Caregiving and American Association of Retired Persons, 2004). Geographic proximity affects the need to travel and the magnitude of psychological burdens experienced by caregivers, as well as their ability to supervise ongoing health-related activities, such as medication management.
The extent to which informal caregivers are prepared for the roles they assume varies considerably, but, for many people, preparation is minimal. According to one national survey, nearly one in five family caregivers who assist with medication management and one in three who assist with changing dressings or bandages received no instruction from a health care professional regarding how to perform these tasks (Donelan, Hill, and Hoffman, 2002). Caregivers’ ability to cope with the challenges of caregiving in chronic illness may be enhanced by skills training designed to help prepare them to monitor the care recipient’s behavior and progression of the disease and to provide appropriate assistance in response. One recent randomized clinical trial demonstrated the efficacy of a caregiver psychoeducational intervention on quality of life in multiple domains among white, black, and Hispanic caregivers of care recipients with dementia (Belle et al., 2006). Other intervention studies have shown that environmental modifications (Gitlin et al., 2009) and caregiver counseling (Mittelman et al., 2007) can reduce caregiver burden and delay institutionalization of the care recipient. Recognition that caregivers and care recipients reciprocally affect each other has led to the development of interventions that simultaneously target both caregiver and care recipient, with the aim of showing that dual treatment approaches are superior to treatments that focus on the caregiver only (Schulz et al., 2009). Intervention studies indicate that education and
training can be valuable tools in enhancing caregiver functioning, but they have not yet been widely implemented in residential settings.
Monitoring of caregiver performance is a neglected area among both researchers and clinicians. With few exceptions (e.g., Gitlin et al., 2003), intervention studies that provide skills training to caregivers rarely assess the extent to which the intended skills are effectively implemented outside the treatment sessions, whether the learned skills are useful for newly emerging caregiver challenges, or how long skills learned as part of an intervention are used after the intervention is terminated. Similarly, clinicians who educate caregivers about care provision rarely assess the quality or appropriateness of caregiving outside the training session. For some types of care, care recipient status may be used as a proxy for caregiver performance, but this does not guarantee that the care provided by the caregiver was delivered as intended (Schulz and Tompkins, 2010). The costs of skills training and education for family members are covered during episodes of functional treatment for the care recipient (Gitlin et al., 2010); however, support for informal caregivers who themselves need assistance and support in order to continue to care for impaired family members is not reimbursed.
Detrimental Effects of Caregiving
Caregiving can be challenging for both people who provide care and people who receive it. For people who require it, receiving assistance from others may challenge their sense of independence; in some cases, the assumption of new roles and responsibilities within the family may result in conflict. One study of people ages 65 and older with physical disabilities whose spouses were their caregivers found that nearly 40 percent reported emotional distress from receiving the assistance, 50 percent reported being helped with activities unnecessarily, and 28 percent reported that they did not receive the help they needed (Newsom and Schulz, 1998).
Informal caregivers may experience a range of health and emotional morbidities associated with providing care. Studies have found that about two-thirds of all caregivers report stress or strain associated with the caregiving role (Schulz et al., 1997; Roth et al., 2009). Although relatively few studies have focused on the association between caregiving and health habits, researchers have found evidence for impaired health behaviors among caregivers engaged in heavy-duty caregiving (Schulz et al., 1997; Burton et al., 2003; Lee et al., 2003; Matthews et al., 2004). For some individuals, the experience of caregiving is sufficiently demanding that it may compromise their health and result in elevated stress hormones, physical illness, and psychological distress (Pinquart and Sörensen, 2003; Vitaliano, Zhang, and Scanlan, 2003). Measures of negative psychological effects, such as depression, stress, and burden, have been found to be
more consistent than physical measures in indicating adverse consequences (Schulz et al., 1995, 1997; Teri et al., 1997; Marks, Lambert, and Choi, 2002; Pinquart and Sörensen, 2003).
Effects associated with caregiving are influenced by a range of contextual and personal characteristics, such as caregivers’ age, socioeconomic status, and the availability of informal support: caregivers who are younger and have more economic and interpersonal resources report better health than do older caregivers, individuals of low socioeconomic status, and those with small support networks (Vitaliano et al., 2003). Some reviews suggest that the psychological effects of caregiving may be greater than the physical health effects, regardless of whether they are measured by self-report instruments or such measures as stress hormone levels (Vitaliano et al., 2003; Pinquart and Sörensen, 2007).
Although uncommon, elder abuse is by nature difficult to study and believed to be underdetected (Cooper, Selwood, and Livingston, 2009). Abusive arrangements have been shown to be more likely to occur among older adults who are physically dependent and cognitively impaired (Beach et al., 2005; Cooper, Selwood, and Livingston, 2009). One recent study of spousal caregivers in three U.S. communities found depression to be a risk factor for potentially harmful caregiver behaviors, which were defined as psychological (e.g., screaming, threatening with nursing home placement) and physical mistreatment of the care recipient (e.g., withholding food, hitting or slapping, shaking; Beach et al., 2005). Initial and intermittent assessment of caregivers would be beneficial, but little guidance regarding candidate assessment and situation intervention is available.
Interventions designed to diminish caregiver burden generally include education and training to help the caregiver understand the nature of a particular disease, its symptoms, and its progression. This type of information is often complemented with referral resources that provide additional information and services relevant to a particular health condition.
The effects of caregiving may extend to negative economic consequences. Middle-aged women at the peak of their earning power provide the majority of care to older disabled relatives (see Schulz and Martire, 2009, for a review), so caregiving may be combined with employment, childrearing, or both (Spillman and Pezzin, 2000). The increasing participation of women in the labor force, along with the increasing demand for care, raises important questions regarding how effectively and at what cost caregiving and employment may be combined. Caregiving may impose fairly significant burdens due to out-of-pocket costs (Covinsky et al., 1994). The most recent survey of caregivers by the NAC and AARP found that more than 6 in 10 informal caregivers with other jobs had made work accommodations that increased in proportion to the level of care needed by the person for whom they provided care (see Table 2-2).
TABLE 2-2 Work-Related Adjustments by Level of Burden (Base = Caregivers employed while caregiver)
Q41-Q47. IF WORKING WHILE A CAREGIVER: In your experience as both a worker and a caregiver did you ever:
|
|
||||||
| Total | Level 1 | Level 2 | Level 3 | Level 4 | Level 5 | |
|
|
||||||
| In late, leave early, etc. | 57% | 40% | 51% | 63% | 75% | 83% |
| Took leave of absence | 17% | 8% | 17% | 14% | 22% | 41% |
| Went from full time to part time | 10% | 3% | 7% | 9% | 15% | 37% |
| Gave up work entirely | 6% | 1% | 3% | 4% | 4% | 35% |
| Lost any job benefits | 5% | 2% | 2% | 5% | 9% | 15% |
| Turned down promotion | 4% | 2% | 3% | 5% | 6% | 14% |
| Chose early retirement | 3% | 1% | 1% | 2% | 3% | 12% |
| None of the above | 38% | 57% | 44% | 31% | 21% | 8% |
|
|
||||||
Base: 935 caregivers in the United States.
NOTE: The five levels refer to the level of burden of caregiving duties, based on the amount of time per week caregiver takes care of recipient and number and types of activities performed. Level 1 indicates lowest caregiving intensity, and Level 5 indicates the highest.
SOURCE: National Alliance for Caregiving and American Association of Retired Persons (2004, Table 9). Used by permission.
Evidence of health and economic consequences associated with caregiving suggests that it is an important public health issue in the United States (Talley and Crews, 2007). Recognition of these facts and the knowledge that caregivers represent a major national health resource resulted in the creation of the National Family Caregiver Support Program (Section 371 of the Older Americans Act) in 2001. This program, administered by the Administration on Aging, makes a range of services available to caregivers through Area Agencies on Aging and Aging and Disability Resource Centers. Services include information and assistance to caregiver services, counseling, support groups and training, respite care, and supplemental services. The program represents an important step in its explicit recognition of family caregivers. However, program funding has been fairly stable at a modest $150 million per year, and many advocates for caregivers feel that existing programs fall far short of what is needed (Riggs, 2003-2004).
FORMAL CAREGIVERS
Health professionals are defined here as individuals who receive compensation to provide health-related technical and supportive services. They include distinct groups that are certified and credentialed for their roles by virtue of education and training: physicians; nurses; physical, speech-language, and occupational therapists; social workers; dieticians; and pharmacists (see Table 2-3). Health professionals also include direct-care
TABLE 2-3 Types of Health Professionals Involved in Health Care Delivery in the Home, Ordered by Estimated 2018 Size of Workforce in the Home
|
|
|||||
| Type of Provider | Estimated Total Quantity (000s) | Estimated Quantity in Homes (000s) | Mean Earnings ($) | ||
| 2008 | 2018 | Overall | In-Home Care | ||
|
|
|||||
| Home health aide | 920 | 1,400 | Most | 9.84/hour | 9.70/hour |
| Home aide/personal attendant | 820 | 1,200 | Most | 9.22/hour | 7.94/hour |
| Registered nurse | 2,600 | 3,200 | 130 | 62,450/year | 58,740/year |
| Licensed practical nurse | 750 | 900 | 40 | 39,000/year | 39,000/year |
| Social service assistant | 352 | 432 | Many | 27,280/year | ? |
| Physician (primary care) | 661 | 806 | Few | 186,044/year | ? |
| Pharmacist | 270 | 316 | Few | 106,410/year | ? |
| Physical therapist | 186 | 242 | Few | 72,790/year | 77,630/year |
| Social work | 139 | 170 | Few | 46,650/year | 46,930/year |
| Speech therapists | 119 | 141 | Few | 62,930/year | 77,030/year |
| Respiratory therapists | 106 | 128 | Few | 52,200/year | ? |
| Occupational therapists | 105 | 131 | Few | 66,780/year | 74,510/year |
| Dietician | 60 | 66 | Few | 50,590/year | ? |
|
|
|||||
SOURCE: Bureau of Labor Statistics (2010a).
workers, who may be hired independently by individuals or their families or employed by home health, hospice, or other community-based agencies and who typically possess less formal education, certification, or credentialing: home care aides or personal care attendants, social service aides, or companions. In addition to providing direct health care services, health professionals supervise and educate individuals and families and provide technically skilled and supportive assistance that is unavailable or to augment assistance from families and friends.
Definitive estimates of the numbers of health professionals who deliver health care in the home do not exist. This workforce is difficult to quantify for several reasons. First, these professionals are remunerated by multiple funding streams, and they may be paid directly by care recipients or their families. Second, credentialing and licensure span numerous professional and paraprofessional organizations and typically vary by state. Third, since health care professionals may be employed in the home directly by individuals or families, their titles and job responsibilities may, at times, be poorly defined. The home health workforce that is certified and credentialed is composed primarily of nurses (registered nurses and licensed practical nurses). However, the dominant workers who provide health care in the home are home health aides, home aides/personal assistants, and social service assistants (see Tables 2-3 and 2-4).
Types of Professionals Providing Health Care in the Home
Direct-care workers who are employed in the home may be broadly categorized as home health aides and personal care aides or home care aides. These health professionals commonly assist with personal care activities, such as bathing, dressing, and performing daily tasks. They may also assist with food preparation or health care activities, such as wound care. These professional caregivers are believed to interact more than any others with individuals receiving care in the home; according to the Paraprofessional Health Care Institute (2010), they deliver 8 of every 10 hours of paid long-term services received in the home. About 88 percent of home care aides are women, which is even higher than their prevalence among informal caregivers (Yamada, 2002). Despite being the linchpin of health care in the home, direct-care workers have limited training, education, and credentialing requirements and may receive minimal or no oversight.
Home health aides employed by Medicare-certified home health and hospice agencies are required to have at least 75 hours of classroom and practical training and to pass a competency test covering 12 subject areas that include communication skills, reading and recording vital signs, infec-
TABLE 2-4 Roles of Health Professionals Relevant to Health Care in the Home
| Type of Provider | Types of Job Responsibilities | Standards for Education, Licensure/Accreditation |
| Home health aide | Assist with personal care activities (e.g., bathing, dressing, negotiating daily tasks), light housekeeping, and health care activities, such as wound care, reading and recording vital signs, medications. Supervised by RNs or other home care professionals. | No high school diploma; 75-hour training program and state-competency evaluation if working for Medicare-Medicaid certified agency |
| Home aide/personal attendant | Assist with personal care activities (e.g., bathing, dressing, negotiating daily tasks), household tasks. May assist with food preparation or health care activities, such as wound care. | No high school diploma required; no certification |
| Registered nurse (RN) | Provide skilled care, perform diagnostic tests and analyze results, operate medical equipment, administer treatments and medications, help establish treatment plans, supervise licensed practical nurses and other direct-care workers. Instruct care recipients and families how to perform self-care tasks. RNs may also be involved in coordinating care. | National Council Licensure Exam (NCLEX-RN); accredited program graduate (2-4 years duration beyond high school); state requirements vary |
| Licensed practical nurse (LPN) | Deliver routine care (e.g., administration of medication, wound care, and taking vital signs), collect samples for testing, perform routine laboratory tests, and may prepare injections, monitor catheters, dress wounds, and assist with hygiene and personal care. Supervised by RNs. | National Council Licensure Exam (NCLEX-PN); state-approved training program graduate (1-year duration beyond high school); state requirements vary |
| Type of Provider | Types of Job Responsibilities | Standards for Education, Licensure/Accreditation |
| Advanced practical nurse | Utilize expanded skills, experience and knowledge in assessment, planning, implementation, diagnosis, and evaluation of care required. Few practice in the home setting. | Qualifications of a registered nurse plus trained at the graduate level and required to attain at least a master’s degree |
| Social service assistant | Help determine eligibility, obtain access, and monitor use of social service programs. | High school diploma; no standard training or certification |
| Physician | Diagnose and treat injuries and disease, oversee care. Examine patients; obtain medical histories; order, perform, and interpret diagnostic tests; counsel care recipients on lifestyle and self-care activities. Few physicians practice in the home but they are most often responsible for initiation of health care services, prescription medications, and health care procedures. Home health care is initiated with physician prescription; home health care recipients must be under care of a physician. | Medical school (4 years) from accredited program in addition to bachelor degree; 3-8 year internship/residency; U.S. Medical Licensing Examination (USMLE) and board certification from American Board of Medical Specialists |
| Pharmacist | Dispense prescription drug medications, counsel care recipients and their families on use of prescription drugs and over-the-counter medications, advise physicians about medication therapy. Some pharmacists advise care recipients, provide specialized services related to specific conditions or diseases, assist with billing to third-party payers. | Doctor of pharmacy (4 years) from approved program in addition to bachelor degree; North American Pharmacist Licensure Exam (NAPLEX); other exams vary by state |
| Type of Provider | Types of Job Responsibilities | Standards for Education, Licensure/Accreditation |
| Physical therapist | Promote mobility and restoration or maintenance of functioning by engaging care recipients in a range of activities, such as therapeutic exercise, functional training, and teach them to use assistive and adaptive devices and equipment. Jobs may be physically demanding. | Graduate of an accredited postbaccalaureate program plus state requirements that typically include licensure examination |
| Social worker (medical/public health) | Help care recipients cope with and solve life issues by providing psychosocial support or assessing, coordinating, and monitoring services. | Bachelor degree; state licens varies but typically includes supervised experience |
| Speech therapist | Assess, diagnose, and treat disorders related to swallowing, voice, speech, language fluency, and communication. Help care recipients to make sounds, increase their written or oral communication, with alternative communication methods, such as the use of automated devices or sign language. May help care recipients to swallow without choking or inhaling food by strengthening muscles or relying on compensatory strategies. | Graduate of an accredited postbaccalaureate program; national certification examination; state licensure varies but typically includes 300-375 hours of supervised clinical experience and 9 months experience |
| Respiratory therapist | Evaluate and treat breathing and cardiopulmonary disorders. Respiratory therapists typically treat care recipients with oxygen, chest physiotherapy, aerosol medications, or ventilators. Those employed by home health agencies inspect and maintain equipment, educate care recipients in the use of medications and equipment. Supervised by physicians. | Associate degree from accredited program, plus certification exam; licensure varies by state |
| Type of Provider | Types of Job Responsibilities | Standards for Education, Licensure/Accreditation |
| Occupational therapist | Help care recipients with mental, physical, or emotional deficits to compensate for loss of functioning, with the goal of maximizing independence, productivity, and quality of life. Help them develop, recover, and maintain their ability and skills using a range of techniques, computer programs, and adaptive or assistive devices. | Graduate of an accredited postbaccalaureate program plus national certification examination; state licensure requirements vary |
| Dietician | Plan food and nutrition programs, promote health with recommended dietary modifications, and evaluate and counsel individuals. Few dieticians practice in the home, but success of dietary treatment regimens hinge on care recipients’ and families’ adherence and implementation in the home environment. | Bachelor degree; state licensure requirements vary but may include certification exam; continuing education required |
SOURCE: Bureau of Labor Statistics (2010b).
tion control, body functions, and basic nutrition, among others.5 Some states require more training, but approximately half of all states require no more than the minimum (Institute of Medicine, 2008); home health aides are allowed to work up to 4 months before completing this training. Home health aides are supervised by registered nurses or speech, occupational, or physical therapists, who are also involved in care.
Personal and home care aides are typically employed and supervised by individuals and families who are also responsible for deciding whether the worker adequately demonstrates basic competencies; they are not typically supervised by licensed health care professionals (e.g., nurses or therapists). Although some states require training and certification for personal and home care aides, the extent of such requirements is highly variable (U.S. Department of Health and Human Services, 2006). Some states impose
_____________
5See Home Health Aide Training. 2006. 42 C.F.R 484.36.
no training or credentialing requirements on personal and home care attendants.
Nurses constitute the largest single occupation involved in the provision and oversight of skilled health care in the home. Two broad categories of nurses commonly practice in the home: registered nurses and licensed practical nurses. Although advanced practice nurses are important to the nursing workforce, they much less frequently practice in the home setting. The education, training, and certification required to practice, as well as the scope of practice, vary considerably across these three categories of nurses, as shown in Table 2-4. Of the three categories, licensed practical nurses have the most limited scope of practice and are supervised by registered nurses or advanced practice nurses.
Registered nurses, in an effort to ensure quality of clinical care, record medical histories and symptoms, perform diagnostic tests and analyze results, operate medical equipment, administer treatments and medications, and help establish treatment plans. Registered nurses also supervise licensed practical nurses and other direct-care workers and play an important educational role by instructing care recipients and families how to perform self-care tasks. Registered nurses may also be involved in coordinating care.
Licensed practical nurses provide direct care, such as administration of medication, wound care, and measurement of vital signs, such as height, weight, and blood pressure. They may also collect samples for testing, perform routine laboratory tests, prepare injections, monitor catheters, dress wounds, and assist with hygiene and personal care. Licensed practical nurses may help educate care recipients and their family members in following a treatment plan.
The presence of advanced practice nurses in the home lags behind other practice settings. Reasons for this disparity include lack of a well-defined role for advanced practice nurses in the home (Milone-Nuzzo and Pike, 2001), restrictive reimbursement mechanisms, and regulatory challenges pertaining to the scope of practice for advanced practice nurses in home care.6 Although limited, empirical studies that have examined the impact of advanced practice nurses suggest beneficial effects for the cost and quality of care provided in the home to specific patient populations, as well as for postacute patients transitioning from the hospital back to the community (Brooten et al., 1986, 2001, 2002; Naylor et al., 1999).
Aside from nurses and direct-care workers, few other health professionals practice in the home (see Table 2-3). Nevertheless, the involvement of
_____________
6See, for example, interpretive guidelines such as Medicare Home Health Conditions of Participation and Guidance to Surveyors (http://cms.gov/manuals/Downloads/som107ap_b_hha.pdf [March 31, 2011]) that clarify 42 CFR Part 484, Conditions of Participation for home health agencies.
several types of health care providers—notably therapists, physicians, and pharmacists—merits comment, in that their involvement has substantive relevance to the quality of health care delivered in the home. For example, physical, occupational, and speech therapists have been valuable members of home care teams for decades. Importantly, physicians typically oversee, monitor, and adjust care recipients’ overall plan of care; Medicare stipulates that home health care recipients must be “under the care of a physician.” Likewise, although few pharmacists practice in the home, many of them provide medical devices and supplies that are used in the home, and they offer training, albeit usually informal.
Unfortunately, adverse complications of prescription drug underuse, overuse, and misuse are common (Gurwitz et al., 2003). A greater degree of coordination between pharmacists and physicians and a focus on educating care recipients have been shown to improve outcomes, such as successful glucose control among diabetics (Rothman et al., 2003). Yet with rare exceptions, most physicians and pharmacists do not have broad exposure to home environments. House call programs, under which very frail older adults receive primary care in their homes and care coordination across all treatment settings, are one such exception. Care coordination is provided by a physician- or nurse practitioner–directed team of health care professionals with geriatrics training who make in-home visits and are available around the clock to carry out plans of care tailored to the beneficiary’s individual needs (Andrews, 2010).
Recruitment and Retention
The hiring of direct-care workers independently by individuals or their families has been described as a huge, private pay “grey market” operating off the books (Seavey, 2007). These providers may be identified through an informal network of friends, family members, churches, and other social groups that are either aware of people looking for employment or have had positive personal experience with an individual whom they refer. The dilemma this presents is that prospective employers (the individuals needing care or family members) may not know if the worker’s training and experience matches their needs and may be unable to conduct an appropriate background check or otherwise confirm credentials and trustworthiness.
A number of factors challenge retention and recruitment of direct-care workers. As shown in Table 2-3, the mean hourly wage of home health aides and personal and home care aides in 2008 was $9.70/hour and $7.94/hour, respectively (Bureau of Labor Statistics, 2010a), the lowest wage earned among all categories of health professionals presented. Although some direct-care workers (25 percent) have completed some
college (Wright, 2005), a substantial proportion have not received a high school diploma (Montgomery et al., 2005; Seavey, 2007). Given low wages and low levels of educational attainment, it is not surprising that many direct-care providers in all settings are among the working poor (U.S. Department of Health and Human Services, Health Resources and Service Administration, and Maternal and Child Health Bureau, 2004). They are more likely than other workers to live in poverty, to rely on food stamps, and to lack health insurance (U.S. Government Accounting Office, 2001). As many as one in four direct-care workers are single parents of dependent children (Wright, 2005; Smith and Baughman, 2007).
Several other factors impede recruitment and retention of direct-care workers, including perceptions of lack of respect, lack of control over the workplace, and limited opportunities for professional growth that contribute to low job satisfaction (Parsons et al., 2003; Castle et al., 2007). Although exact estimates vary widely, direct-care worker turnover rates are extremely high, ranging from 40 to 75 percent per year (Paraprofessional Health Care Institute, 2005; Lacey and McNoldy, 2007). Direct-care work often is physically demanding. Job-related injury rates are high, with reported workplace injuries among direct-care workers that result in time away from work four times the average rate of all occupations (Bureau of Labor Statistics, 2007). Since many direct-care workers are employed outside the formal health care system, workplace injury reporting may fall outside existing surveillance systems, raising the likelihood of underestimates.
Lack of training or commitment to long-term career success has the potential to detract from the caring attitude and knowledgeable care essential for direct-care workers to deliver optimal care. For example, since most direct-care workers are female, there may be an assumption that they can expertly perform such tasks as shopping for and preparing healthy foods for restricted diets, although they may have never learned or personally experienced either. Perhaps more problematic is that without guidelines for practice, unsupervised direct-care workers may practice beyond their scope, inadvertently endangering the individuals in their care due to their insufficient knowledge or skill in identifying emerging health crises, making appropriate clinical decisions, or knowing when to summon assistance. A lack of professional supervision may likewise endanger direct-care workers whose actions (or inaction) may result in occupation-related illness or injury. Furthermore, they may not be aware of how to handle on-the-job injury or to collect workers’ compensation if they are injured in the work setting (Institute of Medicine, 2008).
There is a well-documented shortage of nurses, and evidence suggests that home care nurses are among the least satisfied with their profession (Sochalski, 2004). In one article, input into decision making and
freedom to make important health care and work decisions were consistently highly ranked in relation to job satisfaction (Flynn, 2003; Flynn, Carryer, and Budge, 2005). Commonly cited reasons for possibly leaving their jobs include burdensome paperwork, excessive workload, and lack of role in organizational decision making (Smith-Stoner, 2004; Ellenbecker and Byleckie, 2005; Ellenbecker, Boylan, and Samia, 2006). Features of the work environment central to job satisfaction among home care nurses include design of the work hours, job structure, opportunities for career advancement, and access to continuing education and professional development (Cushman et al., 2001; Kimball and O’Neill, 2002). Flynn and Deatrick (2003) found that insufficient time with and access to front-line managers was a significant contributor to stress and job dissatisfaction in home care nurses.
Professional Practice Issues
Relative to health professionals employed in traditional clinical environments, those who practice in the home have greater independence and autonomy. Control over practice decisions, flexibility, and independence (clinical autonomy) have been reported to be key driving forces in attracting and keeping nurses in home health care (Anthony and Miline-Nuzzo, 2005; Tullai-McGuinness, Madigan, and Anthony, 2005) and are likely to be relevant issues for all health care professionals who practice in the home.
However, with this autonomy comes the potential for social and professional isolation from peers. Delivering health care in the home requires independence and critical thinking to solve problems as they arise, and other clinicians often are not available to provide advice or assistance. Health professionals are susceptible to compassion fatigue, but they rarely have access to peer support or emotional guidance because of the autonomous nature of their practice (Abendroth and Flannery, 2006). Electronic record-keeping, telecommunication, and agency policies may further limit in-person interactions and impede collegiality. This problem may be seen as an opportunity for good user-centered design of electronic networks to alleviate some of the isolation among formal caregivers working in homes.
Because health care professionals are usually educated in, and typically practice in, institutional or ambulatory health care settings, they may lack familiarity with issues encountered in the home. This disconnect between health care professionals who practice in the home and their counterparts raises the potential for communication breakdown and conflict that may detract from quality of care and safety and may exacerbate professionals’ feelings of isolation, lack of support, and misunderstanding. From a professional practice standpoint, there is less opportunity for supervision, and it is more difficult to build in quality controls.
Given extensive autonomy and independence, it is paradoxical that health professionals who practice in the home often struggle with a lack of professional identity (Humphrey and Milone-Nuzzo, 2009). Unlike their colleagues in other settings, most professionals who practice in the home do not have active professional organizations. Few professional organizations impose certification exams or standards for employment that are specific to the home environment. For health care professionals in other settings, professional organizations serve as a mechanism for career development and advancement, along with commensurate salary increases. These benefits are largely unavailable for professionals working in the home environment. Lack of formal credentialing, in combination with logistical challenges associated with supervision in the home, raises the potential for quality of care to be compromised.
Occupational Hazards
The home is, in many ways, more challenging as a workplace than formal ambulatory or institutional health care environments designed and constructed for health care delivery. The physical environment is much more varied and may include logistical or physical impediments, and even hazards, for the administration of health care. Health professionals may encounter distractions, hazardous household conditions, physical discomfort from carrying equipment, heavy lifting, travel requirements, and even violence in neighborhoods and homes (Markkanen et al., 2007).
Although environmental issues are broadly relevant to everyone involved in health care in the home (and are discussed in detail in Chapter 6), several issues are unique to health care professionals. Health care professionals who practice in the home are more susceptible to a range of injuries and hazards because, unlike medical facilities, the home environment is more variable and generally not designed for the delivery of health care services. For example, although such tasks as lifting, pushing, and pulling are often performed by health care professionals, in the home they have less human assistance, usually no ergonomically designed equipment, and the environment is typically less appropriate (e.g., small spaces, crowded rooms) than in institutional health care facilities. Consequently, tasks may be performed in awkward positions or involve more strain and exertion—and may thereby result in injury. Formal caregivers whose jobs involve substantial time on personal care tasks, such as transferring, bathing, and dressing, have been found to incur among the highest rates of musculoskeletal injuries (Orr, 1997; Pohjonen, Punakallio, and Louhevaara, 1998; Galinsky, Waters, and Malit, 2001).
Health care professionals who practice in the home work primarily out of their cars or use public transportation and have no formal work-
station (Markkanen et al., 2007). Most agencies provide “trunk kits” to professional staff that include extra supplies, protective equipment, and other items in order to reduce the need to return to the office to retrieve something necessary to complete an expected or unexpected visit. Because they repeatedly get into and out of the car (or other vehicle), often carrying equipment and supplies, these individuals are at risk for discomfort in and injury to the neck, lower back, shoulders, and hips (Sitzman, Pett, and Bloswick, 2002; Askew and Walker, 2008). The average home health care bag was found to weigh approximately 20 pounds in one study (Lee et al., 2006). Another study found that 60 percent of home care nurses experience discomfort from transporting their nursing bag (Sitzman, 2005). In addition to their bags, health professionals often must transport medical devices and technologies and various supplies, as well as paperwork, teaching materials, references such as a drug compendium, and anything else needed for an efficient and effective visit. Although these professionals are encouraged to complete all documentation in the home during the visit, this is not always possible and can necessitate writing, making phone calls, and using other technology in the uncomfortable conditions of an automobile.
Occupational hazards associated with provision of health care in the home extend well beyond physical stresses. For example, a report by the National Institute for Occupational Safety and Health details a broad range of issues that may be encountered in the delivery of health care in the home. In addition to musculoskeletal disorders, caregivers are exposed to blood-borne pathogens and needlestick injuries, various chemicals, unsanitary environments, violence and firearms, animals, weather-related hazards such as ice-covered sidewalks, and vehicular injuries related to long commutes to the worksite (Centers for Disease Control and Prevention, 2010).
COMMUNICATION BETWEEN FORMAL AND INFORMAL CAREGIVERS
The ability of professional caregivers to engage with family members, understand their strengths, respect their cultural norms and values, and foster their competence as informal caregivers is a critical dimension of practice. Because the typical home health care visit is one hour or less (Madigan, 2007), it is incumbent upon home health care professionals to be skilled at preparing family members to function effectively in their absence. Teaching is such an important aspect of providing home care that Medicare considers teaching as a skilled service—one that can be done only by a licensed health care professional. Despite the practical importance of establishing a productive partnership with care recipients and their informal caregivers, most formal caregivers are exposed to limited, if any, formal educational curriculum addressing effective strategies to include families in
health decision making, prepare them to facilitate use of medical or adaptive technologies, or evaluate and support family caregivers’ needs related to care provision (Reinhard et al., 2008; Yaffe and Jacobs, 2008).
The partnership between care recipients, families, and health care providers is not always positive. For example, family members of hospitalized patients often receive insufficient information and perceive lack of respect from hospital-based health professionals (Azoulay et al., 2000; Heyland et al., 2002; Teno et al., 2004).
One study of home health care recipients found that communication between clinicians and informal caregivers was not adequate around the discharge process (the termination of home health services). Nearly 40 percent of these informal caregivers reported learning that the home care services would end around the time of the last visit by the formal caregiver (Levine et al., 2006). This gave the family no time to prepare for the transition.
Cultural competence is important, as professional caregivers and care recipients are often from different backgrounds and may differ in expectations and preferences. The health care professional must respect, acknowledge, and address care recipients’ and families’ preferences and beliefs so as to effectively garner their support in adhering to their treatments (Lowe and Archibald, 2009; Teal and Street, 2009).
An exemplary effort to further best practices for health care professionals to support informal caregivers is a partnership—funded by the John A. Hartford Foundation and the Jacob and Valeria Langeloth Foundation, among the AARP Foundation, the American Journal of Nursing, the Council on Social Work Education, the Family Caregiver Alliance, and the Rutgers Center for State Health Policy—to advance competencies in this area specifically for nurses and social workers (Kelly, Reinhard, and Brooks-Danso, 2008). The effort outlines nursing and social work–specific competencies in six domains: (1) cultural competence and appreciation for diversity in people’s attitudes and values; (2) communication—respect and compassion for both care recipients and their family caregivers; (3) assessment of family knowledge, skills, and needs; (4) intervention planning and implementation; (5) education; and (6) interdisciplinary teamwork (Damron-Rodriguez, 2008). This model could serve for other professional groups, including direct-care workers, physicians, and pharmacists.
Communication is important between caregivers in the home and primary care providers. Caregivers would like to have more regular communication with the care recipient’s primary care provider (Fairchild et al., 2002). Given the complex health conditions of many people receiving health care in the home, coordination of health care services across settings and providers of care is important (Bodenheimer, 2008). Such coordination may be possible with developments in communications systems, medical
technologies, and training. As we detail in the next chapters, human factors can play an increasingly important role in ensuring that systems, technologies, and training are all accessible to and usable by diverse populations.
REFERENCES
Abendroth, M., and Flannery, J. (2006). Predicting the risk of compassion fatigue: A study of hospice nurses. Journal of Hospice and Palliative Nursing, 8(6), 346-356.
Administration on Aging. (2009). A profile of older Americans. Available: http://www.aoa.gov/AoARoot/Aging_Statistics/Profile/2009/2.aspx [July 2010].
Andrews, M. (2010, September 13). House calls ready to go national. Los Angeles Times. Available: http://articles.latimes.com/2010/sep/13/health/la-he-house-calls-20100913 [April 2011].
Anthony, A., and Milone-Nuzzo, P. (2005). Factors attracting and keeping nurses in home care. Home Healthcare Nurse, 23(6), 372-377.
Askew, R., and Walker, J.T. (2008). Ergonomics for home care providers. Home Healthcare Nurse, 26(7), 412-417.
Azoulay, E., Chevret, S., Leleu G., Pochard, F., Barboteu, M., Adrie, C., Canoui, P., Le Gall, J.R., and Schlemmer, B. (2000). Half the families of intensive care unit patients experience inadequate communication with physicians. Critical Care Medicine, 28, 3044-3049.
Baker, D.W., Gazmararian, J.A., Williams, M.V., Scott, T., Parker, R.M., Green, D., Ren, J., and Peel, J. (2002). Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. American Journal of Public Health, 92, 1278-1283.
Beach, S.R., Schulz, R., Williamson, G.M., Miller, L.S., Weiner, M.F., and Lance, C.E. (2005). Risk factors for potentially harmful informal caregiver behavior. Journal of the American Geriatrics Society, 53(2), 255-261.
Belle, S.H., Burgio, L., Burns, R., et al. (2006). Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: A randomized, controlled trial. Annals of Internal Medicine, 145(10), 727-738.
Bodenheimer T. (2008). Coordinating care: A perilous journey through the health care system. New England Journal of Medicine, 358, 1064-1071.
Brault, M.W. (2008). Americans with disabilities: 2005 household economic reports, current population reports. Washington, DC: U.S. Census Bureau. Available: http://www.census.gov/prod/2008pubs/p70-117.pdf [April 2011].
Brooten, D., Kumar, S., Brown, L., et al. (1986). A randomized clinical trial of early discharge and home follow-up of very low birthweight infants. New England Journal of Medicine, 315, 934-939.
Brooten, D., Youngblut, J.M., Brown, L., et al. (2001). A randomized trial of nurse specialist home care for women with high risk pregnancies: Outcomes and costs. American Journal of Managed Care, 7, 793-803.
Brooten, D., Naylor, M.D., York, R., et al. (2002). Lessons learned from testing the quality cost model of advanced practice nursing (APN) transitional care. Journal of Nursing Scholarship, 334, 369-375.
Bureau of Labor Statistics. (2007). Nonfatal occupational injuries and illnesses requiring days away from work. Washington, DC: Author.
Bureau of Labor Statistics. (2010a). May 2009 national occupational employment and wage estimates United States, 2010. Available: http://www.bls.gov/oes/current/oes_nat.htm [March 31, 2011].
Bureau of Labor Statistics. (2010b). Occupational handbook, 2010-2011 edition. Available: http://www.bls.gov/oco [March 31, 2011].
Burton, L.C., Zdaniuk, B., Schulz, R., Jackson, S., and Hirsch, C. (2003). Transitions in spousal caregiving. Gerontologist, 43(2), 230-241.
Carter, R. (1997, February 13). Remarks, as Honorary Chair of the Last Acts. Available: http://gos.sbc.edu/c/carter.html [April 2011].
Castle, N.G., Enberg, J., Anderson R., and Men, A. (2007). Job satisfaction of nurse aides in nursing homes: Intent-to-leave and turnover. The Gerontologist, 47(2), 193-204.
Centers for Disease Control and Prevention. (2006). Disability and health state chartbook: Profiles of health for adults with disabilities (LCCN: 2006-238868). Atlanta, GA: Author. Available: http://www.cdc.gov/ncbddd/disabilityandhealth/chartbook/ [April 2011].
Centers for Disease Control and Prevention. (2008). Racial/ethnic disparities in self-rated health status among adults with and without disabilities: United States, 2004-2006. Morbidity and Mortality Weekly Report, 57(39), 1069-1073.
Centers for Disease Control and Prevention. (2009a). Chronic disease prevention and health promotion. Available: http://www.cdc.gov/chronicdisease/resources/publications/AAG/chronic.htm [July 2009].
Centers for Disease Control and Prevention. (2009b). National health interview survey, 2003-2007, table 1. Frequency distributions of number of limitations in activities of daily living (ADLs) by age: United States, 2003-2007. Hyattsville, MD: U.S. Department of Health and Human Services.
Centers for Disease Control and Prevention. (2010). NIOSH hazard review: Occupational hazards in home healthcare. Washington DC: National Institute for Occupational Safety and Health. Available: http://www.cdc.gov/niosh/docs/2010-125/pdfs/2010-125.pdf [April 2011].
Charness, N. (2010). The health care challenge: Matching care to people in their home environments. In National Research Council, The role of human factors in home health care: Workshop summary (pp. 73-117). S. Olson, Rapporteur. Committee on the Role of Human Factors in Home Healthcare. Committee on Human-Systems Integration, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press.
Clayman, M., Roter, D., Wissow, L., and Bandeen-Roche, K. (2005). Autonomy-related behaviors of patient companions and their effect on decision-making activity in geriatric primary care visits. Social Science and Medicine, 60(7), 1583-1591.
Cooper, C., Selwood, A., and Livingston, G. (2009). Knowledge, detection, and reporting of abuse by health and social care professionals: A systematic review. American Journal of Geriatric Psychiatry, 17(10), 826-838.
Covinsky, K.E., Goldman, L., Cook, E.F., et al. (1994). The impact of serious illness on patients’ families. Journal of the American Medical Association, 272(23), 1839-1844.
Cushman, M.J., Ellenbecker, C.H., Wilson, D.L., et al. (2001). Home healthcare nurses: Why they leave and why they stay. Caring, 20(10), 62-67.
Czaja, S.J., Charness, N., Fisk, A.D., et al. (2006). Factors predicting the use of technology: Findings from the Center for Research and Education on Aging and Technology Enhancement (CREATE). Psychology & Aging, 21, 333-352.
Damron-Rodriguez J. (2008). Developing competence for nurses and social workers: Quiz 46. American Journal of Nursing, 108, 40-46.
Dillon, C.F., Gu, Q., Hoffman, H.J., and Ko, C-W. (2010). Vision, hearing, balance, and sensory impairment in Americans aged 70 years and over: United States, 1999-2006. NCHS Data Brief, Number 31. Available: http://www.cdc.gov/nchs/data/databriefs/db31.pdf [April 2011].
Donelan, K., Hill, C., and Hoffman, C. (2002). Challenged to care: Informal caregivers in a changing health system. Health Affairs (Millwood), 21(4), 222-231.
Economic Systems Inc. (2008). A study of compensation payments for service-connected disabilities: Volume I, executive report. Falls Church, VA: U.S. Department of Veterans Affairs.
Ellenbecker, C.H., and Byleckie, J.J. (2005). Home healthcare nurses’ job satisfaction scale: Refinement and psychometric testing. Journal of Advanced Nursing, 52(1), 70-78.
Ellenbecker, C.H., Boylan, L.N., and Samia, L. (2006). What home healthcare nurses are saying about their jobs. Home Healthcare Nurse, 24(5), 315-324.
Fairchild, D.G., Hogan, J., Smith, R., et al. (2002). Survey of primary care physicians and home care clinicians: An assessment of communication and collaboration. Journal of General Internal Medicine, 17(4), 253-257.
Fisk, A.D., Rogers, W.A., Charness, N., Czaja, S., and Sharit, J. (2009). Designing for older adults: Principles and creative human factors approaches (2nd ed.). Boca Raton, FL: CRC Press.
Flynn, L. (2003). Agency characteristics most valued by home care nurses: Findings of a nationwide study. Home Healthcare Nurse, 21(12), 812-817.
Flynn, L., and Deatrick, J.A. (2003). Home care nurses’ descriptions of important agency attributes. Journal of Nursing Scholarship, 35(4), 385-390.
Flynn, L., Carryer, J., and Budge, C. (2005). Organizational attributes valued by hospital, home care, and district nurses in the United States and New Zealand. Journal of Nursing Scholarship, 37(1), 67-72.
Freedman, V.A., Schoeni, R.F., Martin, L.G., and Cornman, J.C. (2007). Chronic conditions and the decline in late-life disability. Demography, 44(3), 459-477.
Galinsky, T., Waters, T., and Malit, B. (2001). Overexertion injuries in home health care workers and the need for ergonomics. Home Health Care Services Quarterly, 20(3), 57-73.
Gallagher-Thompson, D., Haley, W., Guy, D., et al. (2003). Tailoring psychological interventions for ethnically diverse dementia caregivers. Clinical Psychology: Science and Practice, 10(4), 423-438.
Giovanetti, E.R., and Wolff, J.L. (2010). Cross-survey differences in national estimates of numbers of caregivers to disabled older adults. Milbank Quarterly, 88(3), 310-349.
Gitlin, L.N., Winter, L., Corcoran, M., and Hauck, W. (2003). Effects of the home environmental skill-building program on the caregiver-care recipient dyad: 6-month outcomes from the Philadelphia reach initiative. Gerontologist, 43(4), 532.
Gitlin, L.N., Hauck, W., Dennis, M.P., et al. (2009). Long-term effect on mortality of a home intervention that reduces functional difficulties in older adults: Results from a randomized trial. Journal of the American Geriatrics Society, 57(3), 476-481.
Gitlin, L.N., Winter, L., Dennis, M.P., et al. (2010). Targeting and managing behavioral symptoms in individuals with dementia: A randomized trial of a nonpharmacological intervention. Journal of the American Geriatrics Society, 58(8), 1465-1474.
Gurwitz, J., Field, T., Harrold, L.R., Rothschild, J.M., Debellis, K., Seger, A.C., Fish, L.S., Garber, L., Kelleher, M., and Bates, D.W. (2003). Incidence and preventability of adverse drug events among older persons in the ambulatory setting. Journal of the American Medical Association, 289(9), 1107-1116.
Heyland, D., Rocker, G., Dodek, P., Kutsogiannis, D.J., Konopad, E., Cook, D.J., Peters, S., Tranmer, J.E., and Callaghan, C.H. (2002). Family satisfaction with care in the intensive care unit: Results of a multiple center study. Critical Care Medicine, 30, 1413-1418.
Humprey, C.J., and Milone-Nuzzo, P. (2009). Characteristics of formal caregivers. Presentation to the Committee on the Role of Human Factors in Home Healthcare, Session 1: People Who Receive and Provide Home Healthcare, October 1, National Academy of Sciences, Washington, DC.
Institute of Medicine. (2008). Retooling for an aging America: Building the health care workforce. Committee on the Future Health Care Workforce for Older Americans. Board on Health Care Services. Washington, DC: The National Academies Press.
Jones, S., and Fox, S. (2009). Pew Internet Project data memo, re: Generations online in 2009. Available: http://www.pewinternet.org/~/media//Files/Reports/2009/PIP_Generations_2009.pdf [March 31, 2011].
Kane, R., Preister, R., and Totten, A.M. (2005). Meeting the challenge of chronic illness. Baltimore, MD: Johns Hopkins University Press.
Kelly, K., Reinhard, S.C., and Brooks-Danso, A. (2008). Professional partners supporting family caregivers. American Journal of Nursing, 108(9), 6-12.
Kimball, B., and O’Neill, E. (2002). Health care’s human crisis: The American nursing shortage. Princeton, NJ: Robert Wood Johnson Foundation. Available: https://folio.iupui.edu/bitstream/handle/10244/471/NursingReport.pdf?sequence=2 [April 2011].
Kutner, M.A., Greenberg, E., Jin, Y., and Paulsen, C. (2006). The health literacy of America’s adults: Results from the 2003 National Assessment of Adult Literacy. Washington, DC: National Center for Education Statistics.
Lacey, L., and McNoldy, T.P. (2007). Turnover rates in North Carolina home health and hospice agencies. North Carolina Center for Nursing-Quick Facts. Available: http://www.hwic.org/pdf/homehealth_turnover.pdf [March 31, 2011].
Lee, E.J., Haddock, M., Yu, S., Back, C., and Yassi, A. (2006). Developing and evaluating a nursing bag system for home care nurses using a participatory ergonomics approach. Home Healthcare Nurse, 24(9), 591-597.
Lee, S., Colditz, G.A., Berkman, L.F., and Kawachi, I. (2003). Caregiving and risk of coronary heart disease in U.S. women—A prospective study. American Journal of Preventive Medicine, 24(2), 113-119.
Levine, C., Hunt, G.G., Halper, D., Hart, A.Y., Lautz, J., and Gould, D.A. (2005). Young adult caregivers: A first look at an unstudied population. American Journal of Public Health, 95(11), 2071-2075.
Levine, C., Albert, S. M., Hokenstad, A., Halper, D.E., Hart, A.Y., and Gould, D.A. (2006). “This case is closed”: Family caregivers and the termination of home health care services for stroke patients. Milbank Quarterly, 84(2), 305-331.
Livingston, G., Parker, K., and Fox, S. (2009). Latinos online, 2006-2008: Narrowing the gap. Washington DC: Pew Hispanic Center, Pew Research Center.
Lowe, J., and Archibald, C. (2009). Cultural diversity: The intention of nursing. Nursing Forum, 44(1), 11-18.
Madigan, E.A. (2007). A description of adverse events in home healthcare. Home Healthcare Nurse, 25(3), 191-197.
Markkanen, P., Quinn, M., Gallign, C., Chalupka, S., Davis, L, and Laramie, A. (2007). There’s no place like home: A qualitative study of the working conditions of home health care providers. Journal of Occupational and Environmental Medicine, 49(3), 327-337.
Marks, N.F., Lambert, J.D., and Choi, H. (2002). Transitions to caregiving, gender, and psychological well-being: A prospective U.S. national study. Journal of Marriage and Family, 64(3), 657-667.
Matthews, J.T., Dunbar-Jacob, J., Sereika, S., Schulz, R., and McDowell, B.J. (2004). Preventive health practices: Comparison of family caregivers 50 and older. Journal of Gerontological Nursing, 30(2), 46-54.
Milone-Nuzzo, P., and Pike, A. (2001). Advanced practice nurses in home care: Is there a role? Journal of Home Health Management and Practice, 13(5), 349-355.
Mittelman, M.S., Roth, D.L., Clay, O.J., and Haley, W.E. (2007). Preserving health of Alzheimer caregivers: Impact of a spouse caregiver intervention. American Journal of Geriatric Psychiatry, 15(9), 780-789.
Montgomery, R.J.V., Holley, L., Deichert, J., and Kosloski, K. (2005). A profile of home care workers from the 2000 census: How it changes what we know. Gerontologist, 45(5), 593-600.
Morrell, R.W., and Park, D.C. (1993). The effects of age, illustrations, and task variables on the performance of procedural assembly tasks. Psychology and Aging, 8(3), 389-399.
Nair, S.N., Lee, C.C., and Czaja, S.J. (2005). Older adults and attitudes towards computers: Have they changed with recent advances in technology? Proceedings of the 49th Annual Meeting of the Human Factors and Ergonomics Society (pp. 154-157), Orlando, FL.
National Alliance for Caregiving and American Association of Retired Persons. (2004). Caregiving in the U.S. 2004. Washington, DC: Author.
National Alliance for Caregiving and American Association of Retired Persons. (2009). Caregiving in the U.S. 2009. Available: http://www.caregiving.org/data/Caregiving_in_the_US_2009_full_report.pdf [March 31, 2011].
National Family Caregivers Association and Family Caregiver Alliance. (2006). Prevalence, hours and economic value of family caregiving, updated state-by-state analysis of 2004 national estimates. Kensington, MD: Author.
Naylor, M.D., Brooten, D., Campbell, R., Jacobsen, B.S., Mezey, M.D., Pauly, M.V., and Schwartz, J.S. (1999). Comprehensive discharge planning and home follow-up of hospitalized elders. Journal of the American Medical Association, 281(7), 613.
Newsom, J.T., and Schulz, R. (1998). Caregiving from the recipient’s perspective: Negative reactions to being helped. Health Psychology, 17(2), 172-181.
Orr, G.B. (1997). Ergonomics programs for health care organizations. Occupational Medicine, 12(4), 687-700.
Ortman, J., and Guarneri, C. (2009). United States population projections: 2000 to 2050. Washington, DC: U.S. Census Bureau. Available: http://www.census.gov/population/www/projections/analytical-document09.pdf.
Paraprofessional Healthcare Institute. (2005). Role of training in improving recruitment and retention of direct care workers in long-term care. Bronx, NY: Author.
Paraprofessional Healthcare Institute. (2010). Direct-care workers at a glance. Available: http://phinational.org/policy/about-the-workforce/at-a-glance/ [March 31, 2011].
Parsons, S.K., Simmons, W.P., Penn, K., and Furlough, M. (2003). Determinants of satisfaction and turnover among nursing assistants. The results of a statewide survey. Journal of Gerontological Nursing, 29(3), 51-58.
Pinquart, M., and Sörensen, S. (2003). Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychology & Aging, 18(2), 250-267.
Pinquart, M., and Sörensen, S. (2007). Correlates of physical health of informal caregivers: A meta-analysis. Journals of Gerontology Series B: Psychological Sciences & Social Sciences, 62B(2), 126-137.
Pohjonen, T., Punakallio, A., and Louhevaara, V. (1998). Participatory ergonomics for reducing load and strain in home care work. International Journal of Industrial Ergonomics, 21, 345-352.
Reinhard, S., Brooks-Danso, A., Kelly, K., and Mason, D.J. (2008). How are you doing? American Journal of Nursing, 108(9 Suppl), 4-5.
Riggs, J.A. (2003-2004). A family caregiver policy agenda for the twenty-first century. Generations, 27(4), 68-73.
Roth, D.L., Perkins, M., Wadley, V.G., Temple, E.M., and Haley, W.E. (2009). Family caregiving and emotional strain: Associations with quality of life in a large national sample of middle-aged and older adults. Quality of Life Research, 18(6), 679-688.
Rothman R, Malone, R., Bryant B., Horlen C., and Pignone M. (2003). Pharmacist-led, primary care-based disease management improves hemoglobin A1c in high-risk patients with diabetes. American Journal of Medical Quality, 18(2), 51-58.
Scherer, M., Jutai, J., Fuhrer, M., Demers, L., and Deruyter, F. (2007). A framework for modelling the selection of assistive technology devices (ATDs). Disability and Rehabilitation Assistive Technology, 2(1), 1-8.
Schilling, L., Scatena, L., Steiner, J., Albertson, G.A., Lin, C.T., Cyran, L., Ware, L., and Anderson, R.J. (2002). The third person in the room: Frequency, role, and influence of companions during primary care medical encounters. Journal of Family Practice, 51(8), 685-690.
Schulz, R., and Martire, L.M. (2009). Caregiving and employment. In S.J. Czaja and J. Sharit (Eds.), Aging and work: Issues and implications in a changing landscape. Baltimore, MD: Johns Hopkins University Press.
Schulz, R., and Tompkins, C.A. (2010). Informal caregivers in the United States: Prevalence, characteristics, and ability to provide care. In National Research Council, The role of human factors in home health care: Workshop summary (pp. 118-144). S. Olson, Rapporteur. Committee on the Role of Human Factors in Home Health Care. Committee on Human-Systems Integration, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press.
Schulz, R., O’Brien, A.T., Bookwala, J., and Fleissner, K. (1995). Psychiatric and physical morbidity effects of dementia caregiving: Prevalence, correlates, and causes. The Gerontologist, 35(6), 771-791.
Schulz, R., Newsom, J., Mittelmark, M., Burton, L., Hirsch, C., and Jackson, S. (1997). Health effects of caregiving: The caregiver health effects study: An ancillary study of the cardiovascular health study. Annals of Behavioral Medicine, 19(2), 110-116.
Schulz, R., Czaja, S.J., Lustig, A., Zdaniuk, B., Martire, L.M., and Perdomo, D. (2009). Improving the quality of life of caregivers of persons with spinal cord injury: A randomized controlled trial. Rehabilitation Psychology, 54(1), 1-15.
Seavey, D. (2007). Written statement before the Subcommittee on Workforce Protections, Committee on Education and Labor, U.S. House of Representatives hearing on “H.R. 3582: The Fair Home Health Care Act.” Available: http://www.directcareclearinghouse.org/download/Seavey%20Written%20Statement%20FINAL%20Oct%2007.pdf [April 2011].
Simmons, T., and Dye, J.L. (2003). Grandparents living with grandchildren: 2000. Census 2000 brief. Washington, DC: Economics and Statistics Administration.
Sitzman, K. (2005). Bag and supply transport tips. Home Healthcare Nurse, 23(1), 49.
Sitzman, K.L., Pett, M.A., and Bloswick, D.S. (2002). An exploratory study of nurse bag use by home visiting nurses. Home Healthcare Nurse, 20(4), 237-243.
Smith, D.L. (2008). Disparities in health care access for women with disabilities in the United States from the 2006 National Health Interview Survey. Disability and Health Journal, 1(2), 79-88.
Smith, K., and Baughman, R. (2007). Caring for America’s aging population: A profile of the direct care workforce. Monthly Labor Review, 130(9), 20-26.
Smith-Stoner, M. (2004). Home care nurses’ perceptions of agency and supervisory characteristics: Working in the rain. Home Healthcare Nurse, 22(8), 536-546.
Sochalski, J. (2004). Building a home healthcare workforce to meet the quality imperative. Journal for Healthcare Quality, 26(3), 19-23.
Soni, A. (2009). The five most costly children’s conditions, 2006 estimates for the U.S. civilian noninstitutionalized children, ages 0-17. Statistical brief, AHRQ #242. Rockville, MD: Agency for Healthcare Research and Quality.
Spillman, B., and Pezzin, L. (2000). Potential and active family caregivers: Changing networks and the “sandwich” generation. Milbank Quarterly, 78(3), 347-374.
Stoops, N. (2004). Educational attainment in the United States: 2003. Washington, DC: U.S. Census Bureau.
Talley, R.C., and Crews, J.E. (2007). Framing the public health of caregiving. American Journal of Public Health, 97(2), 224-228.
Taylor, S., and Lurie, N. (2004). The role of culturally competent communication in reducing ethnic and racial healthcare disparities. American Journal of Managed Care, 10, SP1-SP4.
Teal, C.R., and Street, R.L. (2009). Critical elements of culturally competent communication in the medical encounter: A review and model. Social Science and Medicine, 68(3), 533-543.
Teri, L., Logsdon, R.G., Uomoto, J., and McCurry, S.M. (1997). Behavioral treatment of depression in dementia patients: A controlled clinical trial. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences, 52B(4), P159-P166.
Teno, J.M., Clarridge, B.R., Casey, V., Welch, L.C., Wetle, T., Shield, R., and Mor, V. (2004). Family perspectives on end-of-life care at the last place of care. Journal of the American Medical Association, 291, 88-93.
Tullai-McGuinness, S., Madigan, E.A., and Anthony, M.K. (2005). Exercise of autonomous home care practice: The relationship with nurse characteristics. Home Healthcare Nurse, 23(6), 378-384.
U.S. Census Bureau. (2007). Statistical abstract of the United States: 2007. Washington, DC: Author.
U.S. Census Bureau. (2009). Statistical abstract of the United States: 2009. Washington, DC: Author.
U.S. Department of Health and Human Services. (2000). Healthy people 2010 volume 1. Washington, DC: U.S. Government Printing Office.
U.S. Department of Health and Human Services. (2001). Quick guide to health literacy. Available: http://www.health.gov/communication/literacy/quickguide/ [March 31, 2011].
U.S. Department of Health and Human Services. (2006). States’ requirements for Medicaid-funded personal care service attendants. (OEI-07-05-00250, revised December 2006). Available: http://oig.hhs.gov/oei/reports/oei-07-05-00250.pdf [April 2011].
U.S. Department of Health and Human Services. (2009). Summary health statistics for U.S. adults: National health interview survey, 2008. Hyattsville, MD: National Center for Health Statistics. Available: http://www.cdc.gov/nchs/data/series/sr_10/sr10_242.pdf [March 31, 2011].
U.S. Department of Health and Human Services. (2010). Summary health statistics for U.S. adults: National Health Interview Survey, 2009. Series 10, No. 249, Vital Health and Statistics. Available: http://www.cdc.gov/nchs/data/series/sr_10/sr10_249.pdf [April 2011].
U.S. Department of Health and Human Services, Health Resources and Services Administration, and Maternal and Child Health Bureau. (2004). Nursing aides, home health aides, and related health care occupations: National and local shortages and associated data needs. Washington, DC: National Center for Health Workforce Analyses, Bureau of Health Professions, Health Resources, and Services Administration. Available: http://bhpr.hrsa.gov/healthworkforce/reports/nursinghomeaid/nursinghome.htm [March 31, 2011].
U.S. Department of Health and Human Services, Health Resources and Services Administration, and Maternal and Child Health Bureau. (2008). The National Survey of Children with Special Health Care Needs chartbook 2005-2006. Available: http://mchb.hrsa.gov/cshcn05/ [May 3, 2010].
U.S. Government Accounting Office. (2001). Nursing workforce: Recruitment and retention of nurses and nurse aids is a growing concern. Testimony before the Committee on Health, Education, Labor and Pensions, U.S. Senate. Available: http://www.gao.gov/new.items/d01750t.pdf [April 2011].
Valdez, R., and Brennan, P. (2008). Medical informatics. New York: Springer.
Vitaliano, P.P., Zhang, J., and Scanlan, J.M. (2003). Is caregiving hazardous to one’s physical health? A meta-analysis. Psychological Bulletin, 129(6), 946-972.
Wolff, J., and Roter, D. (2008). Hidden in plain sight: Medical visit companions as a quality of care resource for vulnerable older adults. Archives of Internal Medicine, 168(13), 1409-1415.
Wolff, J.L., and Kasper, J.D. (2006). Caregivers of frail elders: Updating a national profile. Gerontologist, 46(3), 344-356.
Wright, B. (2005). Direct care workers in long-term care. Research report. Washington DC: AARP Public Policy Institute. Available: http://www.governor.wa.gov/ltctf/workgroup/20070912/DirectCareWorkersinLTC_AARP_052005.pdf [April 2011].
Yaffe, M., and Jacobs, B. (2008). Education about family caregiving: Advocating family physician involvement. Canadian Family Physician, 54(10), 1355-1364.
Yamada, Y. (2002). Profile of home care aides, nursing home aides, and hospital aides: Historical changes and data recommendations. Gerontologist, 42(2), 199-206.










































