Health care is coming home. For a number of reasons, health care is increasingly occurring in residential settings rather than in professional medical settings. This change in the locus of care needs to be seen in context. In this first decade of the 21st century, great attention is being devoted to U.S. society’s needs for access to health care and health care delivery. To date, however, there has been too little focus on the transition of care into the home. A wide range of procedures and therapies are now performed far from any medical facility, often with no health care professional on site, with highly variable results. Although each situation is unique, all are dependent on the people involved—the human factors.
Given converging trends of an aging population, an increasing human life span, medical technology migrating into the home, and design features of the home in contrast to health care institutions, it is important to gain an understanding of the most prevalent and serious threats to safety, the quality of care experienced, and the well-being of care recipients and caregivers. Developing a human factors approach to health care in the home that can accommodate the diversity, strengths, and limitations of humans, both as care recipients and caregivers, is critical to addressing these threats effectively.
Human factors focuses on the interactions between people and the other elements of a system, generally with the goal of optimizing safety and performance. Elements of the system may include tasks, technologies, and environments, as well as other people. The success of these interactions is dependent on the degree to which the physical, sensory, cognitive, and emotional capabilities of the people match the corresponding demands imposed
by elements of the system. If the individual is not sufficiently capable or the system’s demands are too high, then the tasks cannot be performed. In these situations, there are usually several solutions, the most appropriate of which will depend on the results of an analysis of the individual, the tasks, the technologies, and the environmental context. In some cases, tasks can be modified to reduce the demands on the individual; in others, the technology itself can be modified to augment the individual’s capabilities or simplify task execution. In still others, training to augment an individual’s skills is the most appropriate solution.
Members of the then-standing Committee on Human-Systems Integration1 at the National Research Council (NRC), a division of the National Academies, became interested in the topic of human factors and its role in improving health care in the home. The Agency for Healthcare Research and Quality at the U.S. Department of Health and Human Services agreed that the issues were worth exploring and agreed to fund this study.
To conduct the study, the NRC appointed the Committee on the Role of Human Factors in Home Health Care. This committee of 11 experts included physicians and nurses with knowledge of home health care and experts from various technological, social, and behavioral science disciplines. Members of the committee were selected following standard NRC procedures for committee formation that ensure individual member qualification and independence, as well as freedom from conflicts of interest and overall committee balance and diversity. Brief biographical sketches of the committee members are contained in the Appendix.
The charge to the committee is shown in Box 1-1. The committee’s overall objective was to gain a deeper understanding of (1) the role human factors can play in developing systems that address the relevant sensory, behavioral, and cognitive capabilities of care recipients and caregivers; (2) the nature of the care processes, procedures, and therapies increasingly occurring in the home; (3) the steady migration and use of medical equipment and technologies in the home environment; (4) the design of the physical home environment to facilitate the delivery of care; and (5) the impact of cultural, social, and community factors on home health care and healthy lifestyles.
This report, prepared by members of the committee, documents the current state of health care in the home and identifies existing problems and opportunities for the improvement of care through applying human factors knowledge and methods. Throughout our work, the committee was constantly reminded that delivery of health care in the home occurs in the larger context of the health care system and policies that impact that
_____________
1In December 2010, the Committee on Human-Systems Integration was reconstituted as the Board on Human-Systems Integration.
BOX 1-1
Charge to the Committee
An ad hoc study committee will examine the impact of human factors issues relevant to the safety and quality of home health care. The study will synthesize and analyze the research literature to gain an understanding of the human factors challenges relevant to sensory, behavioral, and cognitive capabilities of care recipients and caregivers and the increasing use of medical devices, equipment, and technologies in the home environment. The committee will develop a conceptual and methodological framework to guide the study; conduct a review of the existing research literature and sources of evidence; and describe its findings, conclusions, and recommendations regarding strategies, methodologies, and best practices of successful home care practices.
In addition to providing an overarching review and synthesis of the findings and consensus regarding the research evidence, the committee will
- identify and describe strategies, methodologies, best practices, and guidelines that can be used by designers, equipment manufacturers, home care providers and patients when preparing and configuring spaces, equipment, and tasks for home health care;
- identify existing and potential barriers and obstacles to successful implementation, including potential remedies;
- identify gaps in our current understanding, as well as suggest research efforts to remedy these gaps;
- provide an integrative framework for the various disciplines and stakeholders that need to collaborate for improved understanding; and
- provide recommendations or roadmap for a more programmatic approach to subsequent research, practice, and policy.
system. Decisions about reimbursable services, populations eligible for publicly funded health care, and providers qualified for reimbursement have a significant impact on the availability of this care. However, while the committee recognized the importance of these issues, thorough consideration of them was viewed as beyond the charge, which focused on a human factors perspective on health care in the home.
THE RISE OF HOME HEALTH CARE
A number of factors are driving the migration of health care practice from professional facilities to the home and, as a result, significantly increasing the numbers of people who must provide health care in the home:
- The costs of providing health care at formal medical facilities are increasing. Advanced medical technologies and procedures, as well as the training of medical professionals to employ them, can be very expensive.
- Hospitals are discharging patients, including premature infants, sooner into home care, sometimes with complex care regimens.
- The U.S. population is aging (see Figure 1-1), and consequently the demand is growing for various health services (particularly related to conditions associated with aging). At the same time, people are focusing increasingly on overall wellness and quality of life, even into advanced age.
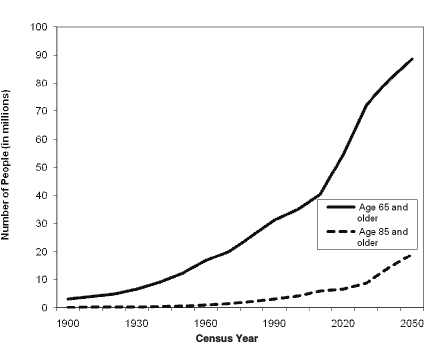
FIGURE 1-1 Projected increase in the older population by 2050.
SOURCE: Administration on Aging (2009).
- The prevalence of chronic conditions across the entire age spectrum is growing (particularly conditions related to obesity, such as diabetes), and growing along with it is the demand for health care. More people are living longer with increasingly complex medical and social needs.
- Larger numbers of veterans are surviving military conflicts and returning home to live with disabilities.
- People who may have had a rapidly fatal illness years ago, such as a heart attack or AIDS, are instead now living with longer chronic illnesses, such as congestive heart failure or HIV.
- Some types of health care professionals are in short supply, which shifts the burden of some types of care onto lay caregivers to fill the gap.
- Consumers want to be independent in their health management and are seeking more home-based services.
- Innovations in information technology, along with consumer demands for more health care quality and personal independence, are shifting the focus from health care providers, procedures, and prescriptions onto consumers and how they can manage care at home (Yogesan et al., 2009). Health care tasks managed at home range from health maintenance and disease prevention activities (regular exercise, good nutrition, healthy behaviors, wellness through ongoing monitoring) and self-care (adherence to medication and other therapeutic regimens) to the use of complex medical devices (e.g., home dialysis, ventilators) and end-of-life care.
Bringing health care to people in their homes can have significant benefits—reduced costs, added convenience (particularly for frail, elderly people who have difficulty getting to a doctor’s office), and improved well-being, to name a few. For example, the Washington Hospital Center in Washington, DC, has been providing house calls for more than a decade and now serves approximately 600 care recipients. Their staff has found that the program returns significant financial savings. The codirector of the program, George Taler, in acknowledgment of a recent survey of home-based primary care sites (Edes et al., 2010), reported that similar house call programs have reduced expected hospitalizations among this group by almost two-thirds. Jim Pyles, a lawyer and member of the board of directors of the American Academy of Home Care Physicians, commented, “We found that you could afford to treat a patient for a whole year at home by avoiding just one hospitalization” (Andrews, 2010).
The rise of home health care, as well as the services and technologies to provide such care, show promise to make health and medical care more effective and efficient, allowing people to heal or age “in place,” live more
independently, and avoid more expensive institutional care. However, the range of home settings and health and medical needs leaves much to be considered.
THE DIVERSITY OF HOME HEALTH CARE
Overall, health care that occurs at home is a complex experience, involving various types of individuals, tasks, technologies, and environments.
- The people involved in health care in the home include people receiving care, who may care for themselves, and those providing care, who may be professional or lay caregivers, family or friends, or some combination. These individuals have a wide range of personal and health literacy skills, social needs, and economic and social resources. People have different perceptions of the power differential between care recipient and the health care system, different cultural views about health and illness, and different language capabilities and preferences. All of these can affect the form and quality of health care received. The majority of people providing care in the home (care recipients themselves, families, and direct-care workers) vary widely in their training and generally have very limited formal training or credentialing; direct-care workers may be employed by families outside the formal health care system and be involved in reimbursement without oversight.
- The tasks involved in home-based health care include activities for maintaining health, activities associated with episodic care (e.g., in response to illness or injury) or chronic care, or activities to support the end of life. The medical conditions involved may be simple and involve little time and no medical equipment, or they may be very complex and consume many hours every day and require the use of complicated devices.
- The devices and technologies for health care in the home cover a vast range, from simple first aid tools to respiratory equipment, and from meters and monitors to computer equipment and software associated with interconnected electronic systems. Some of this equipment was designed only for professional use but is finding its way into the home nevertheless. A particular concern for health care that occurs outside medical facilities is the use of “legacy” (outdated) equipment, which may not have technical support available or even come with instructions; if instructions are available, they generally were not written for lay users.
- The environments of health care delivered in the home, with few exceptions, are not designed for this use and often contain numerous
barriers, such as stairs that block a wheelchair user, low lighting that makes device controls difficult to see, or insufficient electrical supply for power-hungry medical equipment. If the home does not have Internet access, the occupants lack connectivity to enable any type of telehealth activity (e.g., data transfer, remote monitoring, information seeking). Each physical home environment resides within its respective social environment of family, friends, or colleagues, which is affected by the community environments of neighborhood and town and by the health policy environment defined by the presiding health and social service organizations and governmental bodies.
Although each situation is unique, all of these factors—the people, tasks, technologies, and environments—affect the safety and quality of the health care that occurs in the home.
The factors involved in health care outside formal medical facilities are dynamic and often uncontrolled and unpredictable. The health status of the care recipient may improve or decline; the identity, technical qualifications, and personal capabilities of the caregivers or professional medical providers may change. The tasks required, or the particular medical issue involved, or the device being used, or the environment(s) in which the task is performed may be modified in response to any kind of stimulus, including changes in the care recipient’s health condition. The physical, social, community, and health policy environments may shift in any number of ways.
The reorientation of the culture of health care to the home setting, as well as the range of individuals, tasks, technologies, and environments involved in home health care, heightens the importance of human factors. Care recipients and other caregivers, now expected to perform procedures previously executed only by trained professionals, bring a range of knowledge, capabilities, environments, and subsequent interactions to health care. Numerous issues arise in home settings that are not often considered in institutional-based practice. This report aims to shed light on those issues and the opportunities to improve care through application of human factors.
THE REPORT
In conducting our work, the committee determined it appropriate to restrict our focus to health care that occurs in residential environments. Although health care is also conducted in many other community settings, such as schools, workplaces, senior centers, day care centers, and while traveling, the committee decided that investigating those locations was beyond the scope of what we could accomplish. Similarly, we decided that investigating the circumstances of people who are homeless or are undocumented was also beyond the study scope.
We found it useful to subdivide caregivers into two groups: “informal” caregivers, who include unpaid laypersons (often family or friends), and “formal” caregivers, who include paid and trained professionals. These types of caregivers are described further in Chapter 2. We are using these terms to contrast informal, unpaid caregiving with formal, paid caregiving, as was done in the workshop report prepared for Phase I of this study (National Research Council, 2010).
Chapter 2 also describes the growing population of people who receive care. This chapter details the diversity of both care recipients and caregivers. The range of abilities and characteristics as well as cultural experiences presented demonstrates the importance of a human factors focus to the design of safe and effective health care in the home. In this chapter, as well as in Chapters 4, 5, and 6, we include family vignettes, drawn from the clinical or research experience of committee members, to illustrate and personalize the important points in the chapter for the readers.
Chapter 3 defines human factors by providing an overview of human factors tools and methods and their potential application. Chapter 4 considers the wide range of tasks and their demands relevant to health care in the home. It also introduces methods of analyzing home health tasks.
Chapter 5 takes a look at the technologies increasingly entering the home. We found it useful to subdivide technologies into two categories: (1) standalone devices and equipment and (2) information technologies, while recognizing the expanding interconnections between these categories. Some technologies were designed for medical purposes, and other technologies on the market or in development for different uses are being adapted for health care applications.
Chapter 6 examines the factors in multiple environments (physical, social/cultural, community, and policy) that impact home health care. This chapter aims to raise awareness of attributes of different environments as well as the challenges and benefits of bringing health care into the home.
Chapter 7 summarizes the committee’s findings regarding the status of the various components of health care in the home and presents our recommendations for addressing the most evident needs through application of human factors knowledge and methods.
REFERENCES
Administration on Aging. (2009). Projected future growth of the older population. Available: http://www.aoa.gov/AoARoot/Aging_Statistics/future_growth/future_growth.aspx [March 29, 2011].
Andrews, M. (2010, July 13, 2010). House calls: An old idea that may make a comeback. The Washington Post, p. E2.
Edes, T., Kinosian, B., Davis, D., and Hossain, M. (2010, May). Financial savings of home-based primary care for frail veterans with chronic disabling disease. Presentation at American Geriatrics Society Annual Scientific Meeting (Orlando, FL).
National Research Council. (2010). The role of human factors in home health care: Workshop summary. S. Olson, Rapporteur. Committee on the Role of Human Factors in Home Health Care. Committee on Human-Systems Integration, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press.
Yogesan, K., Bos, L., Brett, P., and Gibbons, M.C. (2009). Handbook of digital homecare. Series in Biomedical Engineering. Berlin: Springer.










