Improving Health Literacy at the Community Level
NEW YORK CITY MAYOR’S INITIATIVE ON HEALTH LITERACY
Rima Rudd, M.S.P.H., Sc.D. Harvard School of Public Health
Rudd began her presentation by describing the New York City Health Literacy Initiative as a public health intervention where activities take place outside the healthcare system. Five or 6 years of research, including 3 or 4 years of experimentation and development, preceded the implementation of the initiative. The instruction developed through the initiative was eventually incorporated into the mandated continuing education programs offered statewide for adult educators. The materials for the training of teachers in adult education and the findings from evaluations have been sent to every state department of education in the country. The work has been replicated, adapted, and adopted in multiple states and around the world (e.g., England, Ireland, and Spain).
Within the New York City Mayor ’s Office of Adult Education, there are three areas focused on health literacy: health literacy and adult education; health literacy fellowships; and the health literacy campaigns Prevention and Detection, Be Active, and Nutrition.
Rudd confined her presentation to the first focus area, health literacy and adult education. The health literacy activities were carried out through a partnership of university collaborators from the Harvard School of Public Health and individuals from a practice agency, the Literacy Assistance Center (LAC) of New York. The LAC focuses on services
for adult education teachers, tutors, counselors, job developers, program managers, executive directors, students, researchers, funders, and policy makers. The LAC is the adult education resource for the State of New York and offers student information systems and technical support, a professional development center, a family literacy resource center, and published and online resources.
At the time the health literacy initiatives were being developed in New York, Rudd was a scholar and coinvestigator at the National Center for the Study of Adult Learning and Literacy (NCSALL). The individual scholars and universities comprised by NCSALL were focused on research related to adult learning and literacy. Rudd was the only investigator at NCSALL who conducted research focused on the intersection of health and literacy. Although the level of funding through the U.S. Department of Education was modest, it supported work for 12 years, from 1996 to 2008. The goal for NCSALL was to build and develop research within the adult education field and then translate research into practice.
Throughout her work with NCSALL, Rudd attempted to understand the expectations that health systems had for participating adults and the literacy skills of U.S. adults. She then examined the match (or mismatch) between the expectations and skills. Rudd collaborated with adult education researchers and practitioners, state directors of adult education, teachers and learners, and with representatives of the public health and medical care systems, such as researchers and practitioners in chronic disease specialties, dentistry, mental health, and environmental health. She engaged in a series of studies of health-related activities of adult education programs within states, in programs for adult educators, and in materials and programs for learners to identify the need for collaborative work. Furthermore, Rudd assembled a team of experts across the education and health fields to undergo a “deconstruction” process. This involved an analysis of health-related activities to break down activities (e.g., improving nutrition) into component tasks (e.g., reading food labels, figuring out portion size) and to understand the literacy-related skills people needed to accomplish the tasks as well as to use the tools and materials given to them.
Just before the publication of the 2004 IOM report on health literacy, the New York mayor ’s office was becoming interested in health literacy and decided to launch a health literacy initiative. The LAC and a number of stakeholders met. At the time, a team with representatives from medicine, nursing, nutrition, adult education, and public health were working to develop a program of study that would enhance the ability of adult educators to develop and teach health literacy skills. With support from NCSALL, the team was developing a series of training manuals for professionals in the adult education sector to help teachers integrate
health literacy skills into their programs. The content focus was on three critical issues related to disparities: access to care, managing any chronic disease, and participating in disease prevention and early detection activities. The training manuals were based on a “study circle” process that engages adult educators in collaborative work to examine research findings and then translate those findings into classroom activities.
A pilot site was needed to test the materials. The LAC was eager to pilot the materials and contribute to their development. New York City became the pilot site, and the work became part of the New York City Mayor ’s Health Literacy Initiative.
Research indicates that people who have limited literacy skills are in triple jeopardy because they have limited access to care, are less likely to participate in screening and disease prevention activities, and are less likely to manage a chronic disease. Consequently, they are seven to eight times more likely to die unnecessarily of a chronic disease. Thus, the focus of the study circles fit well with the population of interest to the LAC and to the City of New York.
Rudd noted that the health literacy study circle activities and materials were not meant to turn adult educators into health educators. Instead, the goal was to focus on the existing expertise of the adult educator and to integrate health-related examples and issues into the classroom with a focus on skills the adult education teacher already teaches. The educators were eager to use health as a context for their teaching because of its relevance to students’ lives and to the high interest adult learners have in health-related issues and topics. However, the educators were not particularly interested in teaching health.
The Study Circle Guidebook was piloted and improved through this collaborative relationship with the LAC. The LAC staff, experienced in professional development and program implementation, offered in-depth reviews from seasoned experts, venues for facilitator reflections and suggestions, and opportunities to tap into the perceptions and suggestions of participating teachers. The collaboration identified and raised funding for further collaborative work. Three Health Literacy Study Circle Facilitator Guide manuals were developed and disseminated.
Financial support for the initiative was inadequate, Rudd said. The director of the LAC was asked to launch the Health Literacy Initiative; however, there was no financial support from the mayor ’s office. NCSALL resources for the pilot test of their health literacy materials were used for the project. Subsequently, the LAC raised funds for the collaborative work. The LAC and Rudd formed a relationship built on mutual respect and excitement for the undertaking. Rudd turned to the LAC for their literacy expertise, and the LAC turned to Rudd because it knew the interaction would allow the LAC to hone and further develop understanding
of adult learners’ health literacy as well as teaching techniques, lesson plans, syllabus development, curriculum design, and evaluation methods.
These materials were all developed with a theoretical base in pedagogy and participatory engagement. The processes were based on the pedagogy of Malcolm Knowles and of Paulo Freire. Participants in the study circle engage in an analytic process of discovery, creativity, and group analysis. This process, called Praxis, comes out of Paulo Freire’s work. People engage in analysis, gather insights, determine options for putting learning into action, take action, and then come back to the table for reanalysis. The framework for the specific activities within each session was based on Bandura’s model of efficacy building and included the facilitator ’s modeling of possible teaching techniques. Thereafter, the theory of diffusion of innovation was applied to disseminate materials within and throughout the adult education system in every state.
The activities for teachers participating in the study circle mirrored some of the processes undertaken by the initial research team to analyze the expectations for adults’ actions related to each area of health disparity. Teachers participating in the study circle identified various health activities and then identified the tasks embedded in an activity as well as the tools needed to accomplish each task. Finally, the teachers identified the literacy skills needed by their students. For example, teachers examined an activity such as taking medicine and were able to identify about 20 different tasks, including going to the pharmacy to obtain the medicine, talking with health professionals, reading and recognizing the name of the medicine, differentiating medicine A from medicine B, reading instructions, and knowing when the medicine goes out of date and needs to be renewed. For every task, they then examined tools needed to accomplish the tasks (e.g., the medicine label), and the literacy skills needed to use each of those tools were identified. Literacy teachers teach reading, speaking and listening skills, as well as numeracy. This deconstruction process was the core of the work and resonated with the teachers.
Teachers participating in the study circle were provided with sample lesson plans (in week 2) that they used or modified in trials with their students. They then developed and tried lesson plans of their own, shared their experiences with fellow participants, and together developed syllabi and evaluation plans. Teachers met for half days, 5 times, with 2 weeks in between. The 2-week break was used to develop lessons and experiment within their classrooms. Study circles are based on the concept of research to practice. Teachers come together, learn about the research that has been done, analyze the relevance of the findings to their own practice, and work together to find ways to apply that research to their practice. The guidebook design is illustrated below (Box 5-1).
Each section of the guidebook includes a booklet that the trainer can
- Overview, planning, and facilitation tips
- Overview and prep for session 1
- Session 1: Intro to health literacy and [topic]
- Session 2: Identifying tasks and underlying skills, sample lessons
- Session 3: Integrating health literacy skills into instruction
- Session 4: Planning lessons, units, and evaluations
- Session 5: Developing strategies for success with loose-leaf readings, examples, and handouts
SOURCE: Rudd, 2010.
bring to the training session. It also includes a loose-leaf section with background readings and a comprehensive set of materials that facilitators can replicate for distribution to the participating teachers. Every session is structured the same way. For each session there are notes to facilitators, suggestions for introductory activities, tips on helping participants engage in discussion and analysis, examples of classroom planning tools, closure activities for the session, an evaluation exercise for the session, and an analysis of group discussion methods used in the session that the teachers could then use in their own classrooms. Every training activity was viewed as a modeling opportunity. The facilitator is modeling teaching techniques that the teachers could use in the classroom.
During the first 2 years of the New York City Mayor ’s Health Literacy Initiative more than 200 teachers were trained, reaching 50,000 adult learners in New York City. An outside group conducted a rigorous first-year evaluation to ensure that programs had shared lessons and expanded expertise, educators built skills, and learners had enhanced skills. In addition, the pilot led to the development of a richer set of materials that were then published. The program and its materials were disseminated through train-the-trainer programs led by the LAC in New York City, in New York State, and then to states around the country. Materials were sent at no cost to every department of education in the country and posted online. The materials have also been used internationally. In addition, relationships were formed within neighborhoods in New York City between adult education programs and local hospitals based on a navigation activity embedded in the access-to-care study circle. One hospital in particular moved ahead to call for community-wide participation in a hospital visit for an introduction to, and overview of, the hospitals’
services—an activity that generated wide media coverage. This event also enhanced the reputation of the hospital within the community.
There have been some new more recent developments. For example, partnerships have been formed between health literacy programs and local libraries, hospitals, and hospital groups. In addition, training capacity has been expanded and train-the-trainer programs have taken place in many places throughout the country. Participants of the early study circles went on to facilitate the study circles with other adult education centers.
Partnerships are built on respectful engagements, not through the idea that “I’m going to ask you to do something that I need to have done,” but instead, coming together to meet each other ’s needs and with respect for each partner ’s area of expertise and with a goal of serving each other ’s needs. Participatory approaches are needed, Rudd said, so that trainees have the power and the ability to share insights and introduce changes to the process and products. It is important to pay attention to both content and process and to build on the strengths of all partners.
It is important to understand that health literacy is an intersection of skills and demands, Rudd said. Health literacy is not a characteristic of individuals—something that one has, or does not have. Instead, it is composed of skills that can be built. However, while educators can help build these skills, professionals in public health or medicine do not have the capability, the mission, or the time to increase the public’s health literacy. Instead, those in health fields need to be attentive to the demand side of the equation. Health providers have a responsibility to remove literacy-related barriers to information and to care. There is ample evidence of the skills of the public. The expectations of healthcare providers must be realistic and activities (e.g., talk, materials, processes) must be in line with people’s needs. It is critically important to improve health providers’ communication skills.
Rudd’s final point focused on the partnership process. The project did not involve one partner in the analytic process and the other in an implementation process. Instead, both partners were engaged in the rigorous development of creative and malleable products and processes that could be replicated, adapted, and adopted.
Cynthia Solomon FollowMe, Inc.
Solomon began her presentation by describing the motivation behind her involvement in health literacy. As the mother of a child with very complex medical needs (including 18 brain surgeries and 30 hospital-
izations) and no easy way to track his care, she began to develop and promote personal health records (PHR), especially for vulnerable populations. Her company’s product, MiVIA, is a web-based, patient-owned electronic PHR originally designed for low-income, migrant, agricultural workers. It was well suited to this population as migrants are mobile and when seeking care, access many clinics and health systems. Since its early use in 2003, it has been adapted to meet the needs of anyone with a medical condition, including the homeless, and people with special needs. The tools and resources within the MiVIA PHR help bridge health systems, promote health literacy, facilitate continuity of care, and engage and empower patients to become active care partners, Solomon said. MiVIA ensures security and privacy and is compliant with federal law (i.e., the Health Insurance Portability and Accountability Act [HIPAA] of 1996 [P.L. 104-191]).
The role of the MiVIA PHR is to engage patients by providing them with a place to store and share their medical information. It is also a tool to teach consumers patients’ rights, roles and responsibilities, how to interact with the healthcare system, and how to work with providers as a partner in care. The MiVIA PHR helps reduce the digital divide and provides access to health and community services, clinics, libraries, English as Second Language (ESL) programs, and peer-to-peer communications.
One of the keys to the success of MiVIA has been the role of the promotores de salud. These Spanish-speaking, community-based, lay workers provide enrollment assistance and training in the use of MiVIA. They also provide cultural and social support, and they check in with clients on their use of MiVIA. There are more than 5,000 MiVIA members in Sonoma County, California.
The training of the promotores includes using computers, accessing programs, Internet navigation, and how to enter information into the PHR. The need for privacy and security is highlighted. The training in work groups can be intense, and trainees are encouraged to return for a MiVIA review. The repetition helps the clients gain comfort and confidence.
As of 2010, MiVIA had expanded to six states with 24,000 users. The program serves diverse populations and projects. For example, hospital systems are using MiVIA for their mobile medical units and migrant education. Likewise, county governments use MiVIA for clients that attend their mobile health units. It has provided a low-cost health information exchange system. Community partnerships are being expanded. Solomon pointed out that MiVIA maximizes existing resources.
The addition of audio and video learning tools has enhanced the product. As part of its Effective Healthcare Project, AHRQ developed a series of six 1-minute videos with Ileana Gonzalez, an AHRQ expert who
has practiced medicine in her native Nicaragua. Topics include understanding medications, osteoporosis, gestational diabetes, and when to use the emergency department.
Health literacy gains can be realized with the prudent use of computers, the Internet, e-health, and PHRs, said Solomon. For example, colleagues at the University of California, Davis, Department of Adolescent Medicine worked to develop a product similar to MiVIA for homeless adolescents aging out of foster care. Working with teens in a homeless shelter in Sacramento, California, a personal health information system website was developed, www.healthshack.info. The front page of the site is maintained by the youths themselves. The site incorporates a blog, video, mobile texting, and social networking sites such as Facebook and Twitter. These components were necessary for their communication and for training. Solomon described how at the outset of the collaboration, the teens involved would not make eye contact with the MiVIA staff. They did not feel they had a place in this world of importance. However, they were key developers of HealthShack, and today they are youth ambassadors who travel all over the country to educate others.
Another PHR, Follow My Heart, was designed to meet the needs of patients with congenital heart disease. This product was physician inspired and promotes the development of a physician-patient partnership.
Each of the products developed have incorporated what is called granular consent tools. Inside the PHR, the record holder can give permission for certain individuals to access physical health, but not mental health information. Or the record holder could decide to give a mental health provider sole access to sensitive information.
Solomon itemized lessons learned from her 10 years of experience. First, it is important to understand what the consumer needs. Make no assumptions. Second, people do not like to be labeled (example: migrants, homeless, at-risk, vulnerable). Third, it is crucial to build trust through peer-to-peer outreach before deployment. Fourth, it is critical to partner with organizations that speak the same language and share and understand the same culture as the end user. Finally, consumers need to have a sense of ownership and control with assurances of privacy and consent over the use of their health information.
Solomon made several recommendations. It is important, she said to strategically place language-appropriate health information materials in electronic format, including audio and video media. Furthermore, one needs to support and fund health information technology collaborations and inclusion of community-based organizations and agencies that have direct responsibility for underserved populations—it is crucial to have funds at the local level. Solomon recommended that local and state governments promote consumer engagement in health information technol-
ogy by introducing technology through culturally appropriate efforts and organizations.
PHRs and other consumer tools should be customized to specific populations addressing the cultural issues and providing information using a nonthreatening, nonjudgmental approach, Solomon said. It is important to provide limited (3–5 years) funding for job training for community-based programs such as the promotores, health ambassadors, and health advocate programs in doing peer-to-peer outreach and education.
There are, however, numerous barriers, challenges, and realities in the use of health information technology to advance health literacy. There is lack of funding for community-based organizations wanting to adopt innovative health information technology. Another limiting factor is the private sector has no interest in providing support until there is a demonstration of significant revenue streams or opportunities to sell aggregate data. For true system transformation to take place, financial support is needed at the grassroots level, Solomon said.
Having an impact on vulnerable populations in terms of health literacy might require implementing disruptive technologies that serve the consumer, Solomon said. This will promote cost savings to the payer system and redirect funding back to the providers and communities serving these populations.
Ariella Herman, Ph.D., M.S. University of California, Los Angeles
One million children and families are served every year by Head Start. Services include education and comprehensive health and family services. The program serves families with multiple ethnic, language, and literacy challenges. The Health Care Institute (HCI) at UCLA’s Anderson School of Management has had a long-standing relationship with the Head Start program. Twenty years ago, a training program designed for Head Start directors was implemented. To date, the HCI Management Fellows program has trained over 1,200 Head Start directors and managers.
In 2000, Herman surveyed participating Head Start directors about barriers to good health among Head Start participants. Poor health literacy and poor program attendance were identified as obstacles to better health outcomes for families participating in Head Start (Herman, 2000).
BOX 5-2
Goals of the HCI Health Literacy Program
- Provide a strategic model for agencies serving families and their young children to successfully implement health literacy education programs.
- Build a better future for vulnerable children by providing their parents with skills and knowledge to
- enable them to become better caregivers by improving healthcare knowledge and skills,
- empower them in health decision making, and
- enhance their self-esteem and confidence in dealing with health issues.
SOURCE: Herman, 2010.
In response to these findings, HCI identified health literacy within Head Start as its primary research focus. Its mission is to help agencies work with young children and their families to provide culturally sensitive, low literacy, health education programs. The goals of the HCI health literacy program are in Box 5-2.
In 2001, Herman engaged with Head Start agencies and planned a health literacy intervention. The key tool that emerged is the Health Improvement Project, shown in Figures 5-1 and 5-2. The first step of the project involves training the trainer, in this case Head Start staff. Teams from Head Start agencies experience 2 days of instruction from faculty from the Anderson School of Management. The training provides staff with skills to effectively market their program within their agency, to their families, and to their communities. The topic of motivation, both staff motivation and parent motivation, is emphasized. Mock training sessions are held where trainees role-play being Head Start parents. Over time, the project also brought in Head Start directors that had been through the program to share with new trainees examples of successes and failures.
Following training, each agency team goes back to their local setting and begins to implement the plan for training. A few months later, the parents whose children attend Head Start participate in a 3-hour training session. Participation has been very good; nationally, about 85 percent of parents attend the session. After the parent training, three home visits are made. This contact with the families helps reinforce both the messages from the training and positive behavioral changes. A graduation ceremony acknowledges parent participation in the training. Data are collected to monitor program effectiveness, including self-assessments of knowledge and behavior, and tracking of health behaviors and outcomes
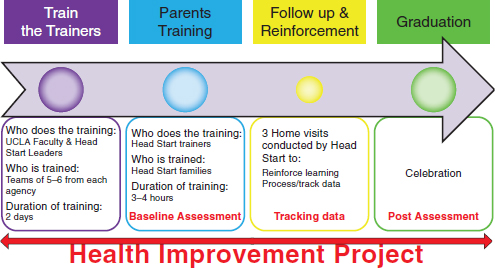
FIGURE 5-1 HCI health improvement project.
SOURCE: Herman, 2010.
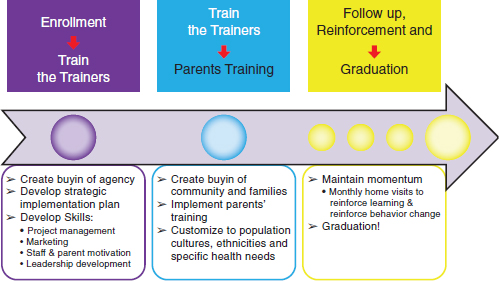
FIGURE 5-2 HCI strategic implementation.
SOURCE: Hermann, 2010.
(e.g., emergency room visits, clinic visits, school days missed, workdays missed) (Figure 5-1). The entire program rolls out in alignment with the school year, from the beginning of planning to the final graduation event. As shown in Figure 5-2, the strategic implementation of this project occurs in three phases: from the enrollment until the train-the-trainer; from the train-the-trainer until the parent training; from the follow-up until the graduation.
An important lesson learned, Herman said, is the need for the agency to create buy-in from Head Start staff, realizing that staff are overworked. A strategic implementation plan is needed to identify how the Head Start agency will accomplish its goals. For example, how will the agency approach the community to get in-kind support? Bringing the community to the training is one way to inspire the community. An example of community engagement is bringing medical residents from a local hospital to participate in the training so they interact with their patients and develop a relationship.
To motivate a poor family to come for parent training one must remove all the barriers, which means providing transportation, childcare, a meal, and creating excitement. To create excitement for parents and motivate their involvement, Head Start staff has to feel excited about the program.
Another lesson learned from collaboration with the Head Start agencies is that the program must be customized. For example, one cannot simply translate materials from one language to another and expect the program to be equally effective in the other language. To reach a particular ethnic group, any program needs to be adapted to that group’s specific language and cultural needs. Herman described how one parent training event was conducted in seven languages simultaneously.
A final ingredient of success, Herman said, is keeping the community engaged to maintain momentum, year after year. One might call this ingredient the L.O.V.E. principle: Listening, Observing, Valuing, and Encouraging. This principle is applied to all levels of the program—the management team, the Head Start staff, the teachers, and the parents. The logic model used is to involve staff, children, and parents in the program in order to have an impact on knowledge, behavior, and sustainability.
Herman described some of the outcomes of the Head Start health literacy program. Before the intervention, when asked, “When your child is sick, where do you first go for help?” more than two-thirds (68.9 percent) of parent participants replied that they would seek help from a doctor. Following the intervention, the percentage of parents reporting a doctor as the first source of help declined to 32.6 percent (Table 5-1). The intervention prompted participants to increasingly rely first on printed low-literacy health materials for help.
TABLE 5-1 Parents’ Sources of Help When a Child Is Sick
|
|
||
| Source | Preintervention (%) | Postintervention (%) |
|
|
||
| Book | 4.7 | 47.6 |
| Doctor | 68.9 | 32.6 |
| Emergency room | 4.4 | 0 |
|
|
||
SOURCE: Herman and Mayer, 2004.
The increased reliance on books and on skills learned in the sessions reduced unneeded utilization of healthcare resources. There was a 42 percent decline in number of doctor visits, a 29 percent decline in school days missed, and a 42 percent decline in workdays missed when these events were tracked over the first 8 years of the program. Emergency room visits also declined (Herman and Mayer, 2004).
Based on these changes in healthcare service use, a conservative calculation of cost savings was computed. Assuming $80 for a doctor visit and $320 for an emergency visit, there is $554 savings in healthcare costs per family trained per year. The average cost of this program is $100. This estimate did not take into consideration many other qualitative outcomes and benefits of the program. The program and, in particular, the use of the health reference book led to an increase in parental awareness of health warning signs, a better understanding of common childhood illnesses, and quicker responses to early signs of illness. Parents were also empowered to appropriately use the healthcare system. Figure 5-3 presents an overview of the program’s model, impacts, and outcomes.
Research is linked to practice in two ways, Herman said. The first linkage is through effective implementation that involves building capacity, developing leadership, providing tools for strategic project management and replication, and enhancing community outreach. The second linkage is through health promotion that involves using materials that are culturally sensitive and understandable, offering a portfolio of health topics, teaching health skills, and addressing health decision making. Modules have been developed on common childhood illness, oral health, obesity, prenatal education, and how to read over-the-counter medication labels.
The program has trained 45,000 families, 1,150 trainers, and 189 agencies in 45 states, in seven languages, and has adapted the program for successful implementation in 10 ethnic groups. This year, the program moved beyond Head Start and has provided programs within two school districts. The program has corporate and public financial support.
There is one module that addresses obesity and diabetes prevention. This module educates staff, parents, and children. The program has succeeded in improving children’s nutrition knowledge, eating behavior,
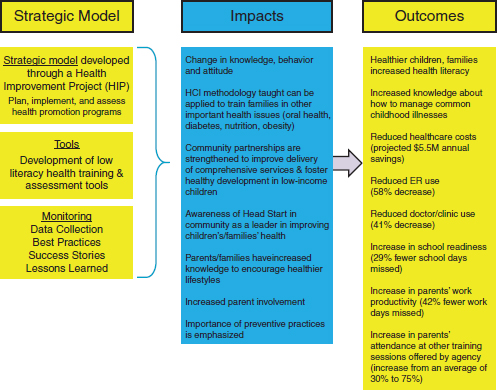
FIGURE 5-3 Overview of the Head Start intervention.
SOURCE: Herman, 2010.
physical activity, and body mass index (BMI). Children were taken to a farmers market and then that experience was used to teach math and science. Parents’ BMI improved also, and there was a link between the BMI change of the children relative to the parents. This example illustrates how such a trilevel early intervention can prompt changes within a whole community.
Herman expressed her desire to reach the entire Head Start community. Focusing on prevention and early education is critical, she said. Parents can become the strongest advocates for children if they are given appropriate tools. To be effective, programs must be designed to understand local needs and to motivate members of the community. Entire communities must be engaged. HCI has learned that what is communicated and how communication occurs matters. Appropriate tools need to be provided in a respectful and culturally sensitive way. Parents need to be allowed to assume the primary role of decision making in the care of their children.
Herman concluded by summarizing HCI’s vision. That vision is to
- expand reach to all vulnerable families to help reduce health literacy in the nation;
- approach the problem from a population perspective with scalable programs;
- focus on prevention;
- recognize parents are key to advocating for the health and wellbeing of their families;
- empower families with knowledge, tools, resources, and self-efficacy/self-confidence so they can actively participate in health decisions;
- engage families to achieve sustainable adoption of healthy lifestyle choices; and
- work with communities to develop social capital.
Empowered families can make a difference, Herman said. They can change communities, and they will lead to a healthier nation.
Ellen Beck, M.D. University of California, San Diego
Beck recounted a lesson learned early in her career while directing a health education program for the elderly. She had been somewhat discouraged in trying to teach medical students how to consistently take a medical history, so she decided she would teach elderly patients how to give a medical history. This was a success, and the patients reported how much they enjoyed walking into the doctor ’s office and speaking to their doctor using what they had learned, “I told him my chief complaint, and then I went on to my history of present illness, and then I gave him my past medical history.” This is just one example of the potential benefits of teaching patients to learn to speak in their doctor ’s language.
The Student-Run Free Clinic Project (SRFCP), founded in 1997 by a group of University of California, San Diego (UCSD) medical students, outstanding community partners, and Beck, engage in health literacy-related work. The project serves a variety of diverse patients and partners. For example, an older African-American couple who marched with Martin Luther King from Selma to Montgomery helped start one of the free clinic sites, at Baker Elementary School, that serves the surrounding community. A Hispanic member of the community, and former patient of the clinic, first volunteered and is now employed as the project’s lead
health promoter (promotora). A formerly homeless man has become one of the project’s street homeless health promoters.
There are now four sites. Two are located in churches that have a long-standing history of providing services to the underserved. Two other sites are located in inner-city elementary schools.
The free clinic project can be considered a safety net for the safety net. San Diego has very limited health services for the poor and uninsured, and many individuals fall through the cracks. For example, a U.S. citizen living in San Diego, who cannot afford health insurance, and thus is in need of county health services must earn less than $1,490 a month to receive such services. In addition, the individual must have a disease that might lead to serious complications, disability, or death. Finally, the person has to sign a lien against any future property to cover healthcare expenditures.
The SRFCP provides continuous, comprehensive, high-quality, outpatient health care to 2,000 people who are without access to care. If a prospective client is eligible for insurance or healthcare elsewhere, such as at a community health center, the SRFCP helps the individual access those services. The SRFCP serves a demographically and socially diverse population, 51 percent Latino, 30 percent Caucasian, and 25 percent street homeless. Most patients (over 85 percent) have at least one serious chronic illness, most commonly, hypertension, diabetes, hyperlipidemia, asthma, or depression.
The clinic has adopted a core philosophy that is taught, modeled, and expected throughout all activities. The components of this philosophy are patient empowerment, humanistic care, transdisciplinary care, and an understanding that the community is the teacher. Trainees are also taught the behaviors associated with these key principles and are evaluated in terms of their adherence to these principles. The SRFCP provides training for students of medicine, pharmacy, acupuncture, dentistry, social work, and law.
Empowerment means creating an environment in which a person can take charge of his or her life and achieve health and well-being. The clinic sponsors a Spanish language empowerment group (formerly called a support group). Beck shared a few personal experiences from the groups. One patient who had been a member of the group for 3 years said,
When I first came to the group, I was carrying a lot on my shoulders, and I let everything out. I cried a lot. And since then, everybody in the group has helped me to think, to defend myself, to move forward without fear. Everything I hear here I share with my family, and they also are changing. I was in the hospital recently, and they gave me a lot of support. I want this group to continue and want to invite a lot of people so they can listen and learn not to have fear and to move forward. This is my home, and I want to share it with everybody.
Another patient who had been a member of the empowerment group for 4 years said,
Before coming to this group, I did not know how to control my temper, and I did not know how to speak with my children or my husband. Now I feel like a different person. I know how to control my temper. I know how to speak to my children. Now I know how to get along with myself better. Before, I didn’t value myself. I didn’t take time for myself. I feel much better about myself. Thanks to all of you. For me, this group is like a family, something beautiful that happened in my life, this experience, this support … Ojalá! I wish I can continue to come and to share.
Many of the SRFCP’s patients have become volunteers, and they help with the day-to-day clinic functioning. There is a rule that if you attend an empowerment group, it must be as a member and not in the role of a volunteer or professional. The groups are usually conducted in Spanish.
The underlying philosophy of the clinic is humanistic, based on work by Carl Rogers, the founder of humanistic psychology, and the person who coined the phrases, “client-centered,” “person-centered,” and “patient-centered.” Rogers said that the essential qualities of all successful encounters, and especially the therapeutic encounter, required the three elements of empathy, congruence, and respect (Zimring, 1994). Thus, the students are taught and the faculty models that in every client encounter, the SRFCP providers are expected to demonstrate empathy, respect, and congruence. Empathy is a sense of what the patient might be feeling; respect is shown to all in all contexts. Students are taught that they may not respect what a person has done, but they can still show respect to the person as a human being, and that all human beings deserve to be treated with respect. Congruence is self-awareness on the part of the provider, an awareness of what is being experienced and felt in the moment and how that awareness affects the patient encounter. One of the clinic’s goals is to dispel hierarchies, stereotypes, and interprofessional prejudices. The clinic philosophy is taught through examples, role modeling, weekly reflection sessions, community building, writing, and didactic sessions that cover topics such as health promotion, health education, working with interpreters, and social resources.
Of the 122 medical students in the first year class at UCSD, 105 students choose to take an intensive elective in order to work at the SRFCP. Throughout first and second year, there are another 70 students who continue to work at the SRFCP as they learn to take on administrative and clinical roles under the supervision of faculty. Some students participate in the clinic during their third year, and 80 fourth-year students elect one of two 4-week clerkships, one in family medicine, and one in undeserved medicine, both of which include intensive experience in the SRFCP. Many
of the fourth-year students will be pursuing specialty residencies, for example, radiology, pathology, and anesthesiology, and yet they elect to gain experience at the free clinic. The clinic also offers training to students of pharmacy, dentistry, acupuncture, social work, and law.
Students rotating through the free clinic project learn to teach. Incorporating health literacy into clinical practice requires teaching skills. Fellows in Underserved Health Care teach the fourth-year medical students, and the fourth-year medical students learn to coach first-year students. The senior and junior students see patients together under the supervision of primary care clinicians, most of whom have extensive experience at the SRFCP. An adult health education model is used to teach the medical students how to incorporate health education and health promotion into their practice.
Beck attributed the positive medical outcomes (Table 5-2) of 182 diabetic patients seen at the free clinic and then assessed after receiving care at the free clinic for 1 year to the sense of community, the trust of the patients, the time taken by the students to interact with the patients, and the overall philosophy of care. Students are instrumental in helping patients take charge of their health.
Another program started through the free clinic is a comprehensive wellness program at an inner-city elementary school, Golden Avenue Elementary in the Lemon Grove School District. The program addresses the needs of children, teachers, parents, and the environment. The intervention involves providing access to care for the parents. There are community gardens and a mural program, which involves the community
TABLE 5-2 Outcomes of 182 Diabetic Patients Seen at the UCSD Free Clinic and Assessed at 1 Year
|
|
||
| Test | Test Completed Within the Last Year (%) | Percent with Test Result |
|
|
||
| Blood pressure | 100 | 46% < 130/80 77% < 140/90 |
| Hemoglobin A1C | 99 | Mean HA1C value = 8.26% |
| Low-density lipoprotein (LDL) | 93 | 70% < 100 86% < 130 |
| Triglyceride (TG) | 88 | — |
| High-density lipoprotein (HDL) | 88 | — |
| Microalbumin | 80 | — |
|
|
||
SOURCE: Marrone et al., 2010.
and improves the environment. For teachers, the focus of the intervention is professional renewal. There is a wellness curriculum for the children that involves creative expression (e.g., art, dance, and theater) as well as nutrition and exercise. In addition, the children themselves increase their health literacy and act as health literacy advocates by becoming junior health promoters and participating in an after school prehealth profession program called, “Blue Band-Aid” brigade. The classes provide activities to increase the children’s knowledge and skills related to common health issues.
Several health literacy and empowerment methods are used at the SRFCP, Beck said. When clinic providers use the teach-back method, they do not simply ask the patient to repeat information that the provider has discussed. They often ask the patient to pretend that he or she is the doctor and to teach the provider what the provider just taught them. Free clinic providers also learn to ask patients about barriers that may be preventing them from taking charge of their lives and their health. Providers then work with the patient to reduce those barriers. Trainees learn to write personal prescriptions for patients about their sources of strength to overcome barriers. Providers also learn to work with their clients to address client concerns about using fear management tools. During their encounters with patients, providers consider social determinants of health, such as income and social environments. These activities, in addition to learning to build trust, address stigma, and improve knowledge, are all essential ingredients of health literacy training. Beck emphasized the importance of not only working with clients on their health literacy, but also acting to improve clinician health literacy.
Community health workers who interact primarily with the Hispanic community, called promotores, come to the medical school to teach students. They are introduced as wise community members, health promoters who have a role at the free clinic, especially in developing and maintaining community trust and partnership. The promotores are available during clinic hours to help problem solve and consult. They also cofacilitate the clinic’s empowerment group. The free clinic’s community partners (e.g., hosts at each site, social workers) are involved in the weekly reflection sessions at the SRFCP.
Student-perceived self-efficacy relates to caring for traditionally underserved patients. Self-efficacy improved dramatically as measured before and after the students’ first free clinic elective.1 Students also reported an increased interest in primary care and increased interest in
_____________
1Beck said this finding comes from an independent study project involving 431 medical students who took the free clinic elective in 2001.
working with underserved populations following their exposure to the clinic.
A 1- to 2-year UCSD Fellowship in Underserved Health Care has enrolled six medical fellows, two dental fellows, and one acupuncture fellow. This fellowship occurs after residency training and is for health professionals interested in devoting their career to underserved health care. The fellows help direct the free clinic and complete a research project and training. Of these fellows, eight of nine were student free clinic leaders who returned after residency to help run the free clinic project. All now devote their careers to working with the underserved.
Beck has also worked to develop a national faculty training program entitled Addressing the Health Needs of the Underserved. Since 1999 this program has enrolled 135 faculty from 30 states. One-quarter of them are from underrepresented minorities in the health professions. The three areas of focus of the training program are faculty development skills, community partnerships and programs, and personal and professional renewal. Overall confidence of trainees in essential knowledge relevant to care of underserved populations increased markedly when measured before and after the training program. For example, improvements were noted in student confidence about creating student curricula related to underserved communities, designing a student- or resident-run free clinic, and developing an educational component or experience that addressed issues of culture and race (Beck et al., 2008). An outcomes study performed after the first 53 participants of the program had completed the program demonstrated that participants had started many student-run free clinics, developed curricula, written their first grants, and assumed new leadership roles.
Beck outlined key lessons learned from her experiences. She emphasized the importance of a sense of ownership by all participants in the SRFCP and other training programs that she has been involved with. The medical students succeed at this work when they have a sense of ownership and when the health literacy work is relevant to their ability to perceive themselves as a future good doctor. If the patient has a sense of ownership and the student has ownership, things work. Beck indicated that in her experience, role modeling and coaching are among the most effective teaching tools. Students need to be taught to be teachers. They also need to learn that patients and the community are truly the teachers. Community member involvement is essential in all aspects of training, teaching, and role modeling. Students need to be oriented to this type of humanistic, empowering transdisciplinary philosophy and to have specific expectations for performance made clear to them.
Lack of health literacy is an injustice, Beck said. As Martin Luther King said, “Injustice anywhere is a threat to justice everywhere.” She
encouraged the group to continue to address this injustice and, together, to discover creative ways to intervene and change the status quo.
Roundtable member, Will Ross, remarked on the success of the interventions described during the workshop and pointed out that some of the success can be traced to the fact that the interventions are based on good public health theory. He pointed out that the theories of diffusion of innovation, community-based planning, and constructs from social cognitive theory are not normally taught in health professional schools. These constructs have been well interwoven into the interventions described during the workshop. Ross mentioned the difficulty of taking a large issue like health literacy and implementing interventions to improve it within the community. In his view health literacy needs to be better integrated into health professional curriculums so core skills are acquired related to behavioral health theory and community planning.
Rudd responded and reiterated the importance of a theory-based approach to health literacy. Of critical importance also is the need for respect for clients and partners, she said. Adult learners, parents, farm workers, and others who might attend health literacy programs need to be treated with a level of respect and dignity so they recognize themselves as empowered agents, and not as subjects.
Beck added that from a medical school education perspective, students should be taught behavioral and social sciences once they have been directly involved in clinical care. Ideally the teaching is concurrent with these clinical experiences. Otherwise, the material is not perceived as relevant. These disciplines become more relevant after the student has had experiences, such as the death of a patient, or being in the emergency room and unable to communicate with a family. Students often learn best when they encounter cases that are challenging and when they are not sure of the best approach or how to cope with their reactions.
Conrad Person, Johnson & Johnson, asked the panel what companies that manufacture health products should be considering making their products more accessible to people. He pointed out that many resources are expended to develop materials that are meant to facilitate the use of products and enhance their effectiveness. These materials, however, do not always meet the needs of people with poor health literacy.
Solomon responded that companies could help sponsor health literacy projects that would lead to video and audio tools on some of the e-learning applications, both for electronic medical records and personal health records. In addition, companies could sponsor some educational programs in the area of medication management. Assisting people with
financial support so they could take advantage of some of these tools would also be very helpful, especially in the e-learning arena.
Roundtable chair Isham observed that some advantaged segments of the population tend to overuse commercial products and disadvantaged populations underuse certain products. Companies such as Johnson & Johnson are particularly rich in skills and talents in terms of market segmentation and being able to target particular audiences. There is tremendous social purpose that can be aligned with their economic objectives in terms of more carefully trying to address these disparities. The challenge is to make that alignment work both for the private companies as well as those populations.
Beck added that ideally, a product could be designed like some of the newer thermometers. A button on the packaging could be pushed and instructions in either English or Spanish could be selected and provide information in simple terms on how to use the product. As more people are learning how to navigate the Internet, instructions could be made available online. Solomon suggested a technological intervention that might be helpful: having patients able to pass the bar code on a product over a small machine that would either provide voice instruction or print out instructions in the language of choice.
Jan French, Los Angeles Best Babies Network, leads healthcare improvement collaboratives focused on prenatal and postpartum care in Los Angeles [LA] County. She asked Herman about leveraging resources within communities and at the state and national levels. French mentioned a local resource, the First 5 LA program,2 and on the federal level, she noted the Promise Neighborhoods Initiative of the Department of Education3 and the Patient Protection and Affordable Care Act expansion of home visitation programs to disseminate programs that work.4 Herman responded by describing programs that the HCI is involved with in LA
_____________
2This organization was created by California voters to invest tobacco tax revenues in programs to improve the lives of children in LA County, from prenatal care through interventions for children up to age 5 (http://www.first5la.org/, accessed February 16, 2011).
3Promise Neighborhoods provides grant funding to support nonprofit organizations and institutions of higher education to significantly improve the educational and developmental outcomes of children in distressed communities, including rural and tribal communities (http://www2.ed.gov/programs/promiseneighborhoods/index.html, accessed February 16, 2011).
4The act provides funding for the Maternal, Infant, and Early Childhood Home Visiting Program. The program relies on evidence-based home-visiting strategies that help families create a nurturing environment for young children and connect to a range of services, including health, early education, and early intervention. The Health Resources and Services Administration (HRSA) administers the program in collaboration with the Administration for Children and Families (ACF) (http://www.hrsa.gov/about/news/pressreleases/2010/100610.html, accessed February 16, 2011).
County. HCI has worked with five Early Head Start programs, seven Head Start programs, and two school districts in LA County. In terms of leveraging, Herman mentioned the importance of emphasizing community partnerships in training programs.
Shannon Alvarado of Lenox School district in LA County discussed her work with Herman. Following a train-the-trainer session in 2010, 120 parents in the school district attended an education program. The Lennox School district occupies a 1.3 square mile area near the L. airport. Most of the children in the district qualify for free or reduced lunches. The parents have used the course materials. A second cycle of parent training took place in early 2011. The work within the school district was highlighted in an article published in the Los Angeles Times in October 2010.5 Ms. Alvarado described the excitement of parents as they learned how to take charge of their children’s health.
_____________
5See http://articles.latimes.com/2010/oct/20/local/la-me-head-start-20101020, accessed February 16, 2011.
























