Consumer Health
Information Technology
in the Home
|
A GUIDE FOR |

NATIONAL RESEARCH COUNCIL
OF THE NATIONAL ACADEMIES
Every day, in households across the country, people engage in behavior to improve their current health states, recover from disease and injury, or cope with chronic, debilitating conditions. Innovative computer and information systems may help these people manage health concerns, monitor important indicators of their health, and communicate with their formal and informal caregivers. Designers and developers can help change the face of health care at home by creating appropriate consumer health information technology (IT) applications. This guide introduces designers and developers to the practical realities and complexities of managing health at home. It provides guidance and human factors design considerations that will help designers and developers create consumer health IT applications that are useful resources to achieve better health.
What is the purpose of this guide?
- To help designers and developers create consumer health IT applications that are easy to use by people with a wide range of life situations.
- To assist home health professionals in selecting tools to complement professional home health care services.

What is covered in this guide?
- An overview of health and health care at home, including who is involved and what they do;
- Encouragement to create new kinds of consumer health information technologies to help people reach their health goals; and
- Strategies to make consumer health information technologies more acceptable and useful to people with different life situations.
Who should use this guide?
- Software designers,
- Hardware and device designers,
- Product marketing teams,
- Information systems staff in health care organizations who want patients to make use of their portals, and
- Home health professionals responsible for selecting health tools for patients to use.
What are some examples of consumer health information technologies?
Examples range from common applications, such as
- In-home monitoring, disease management, and self-management systems;
- Online forums on health topics; and
- Telemedicine and health-related Websites;
to new tools for a health future, such as
- “Aware” refrigerators, which keep track of the food stored within, expiration dates, and nutritional guidelines and can also suggest menus or provide warnings about food allergies;
- Smartphones that deliver health-promoting text messages; and
- Mobile devices that track nutritional balance.
A simple way to think about human factors and health at home
Human factors is an engineering science dedicated to understanding and improving the way people use technology and other things in the environment. A graphical model created by Czaja and Nair for the National Research Council (2011) depicts the key elements of health at home and the human factors considerations related to each one. At the core are three circles, representing people engaged in tasks using certain kinds of equipment or technology. This triad is embedded in ever-expanding environments, beginning with the physical layout of the house, the social structure of people’s relationships with their friends and families, the community where they reside, and the health policy context, which influences the type of health services available and the presence (or absence) of funding for care, home-based technologies, and care personnel. As designers and developers create new consumer health information technologies for the home, they need to consider how each innovation will help a person doing related tasks in these environments.
As designers and developers create new consumer health information technologies for the home, they need to consider how each innovation will help a person doing related tasks in these environments.
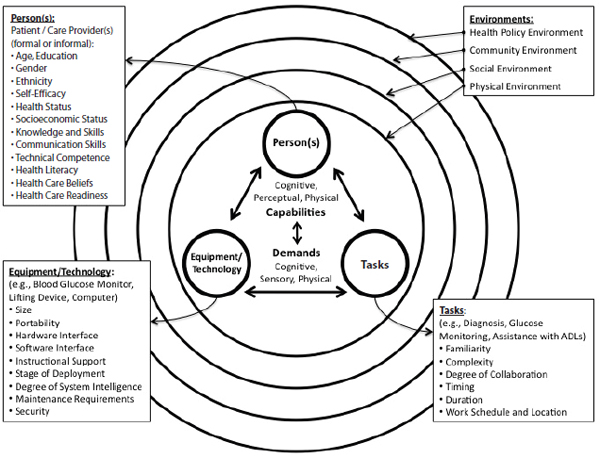
Figure: Model of Human Factors of Health Care in the Home
Source: National Research Council. (2011). Health Care Comes Home: The Human Factors. Committee on the Role of Human Factors in Home Health Care, Board on Human-Systems Integration. Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press. Adapted by Czaja, S.J., and Nair. S. from Czaja, S.J., Sharit, J., Charness, N., and Fisk, A.D. (2001). The Center for Research and Education on Aging and Technology Enhancement (CREATE): A program to enhance technology for older adults. Gerontechnology, 1, 50-59.
Who is the consumer who will use consumer health IT?
The purpose of consumer health IT applications is to improve people’s health and help them to act in ways that enhance their lives. To achieve this purpose, designers and developers should understand that there are many types of people involved in achieving health in everyday living:
- People who are well. These individuals engage in health practices in the home (e.g., eating well, scheduling regular health checkups, exercising) to maintain or improve their health state.
- People who are ill or managing complex diseases. Half of all households have a resident with a health problem (e.g., a soldier returning with an injury, a child born with a congenital limitation, a well-functioning individual who takes medications to control a chronic condition). These individuals are the most common users of many consumer health information technologies.
- Kids. Such technologies as games for health or interesting Websites can guide kids, sick or well, in the process of making healthy choices or help them keep track of complex medical regimens they need to sustain life.
- People with disabilities. Such technologies as talking computers or motion-sensitive faucets make everyday life easier for people with physical or cognitive limitations.
- People who are older. Today, 1 in 10 persons is over the age of 65; in 20 years, that number will grow to 1 in 8. Most older people have skills and strengths that can be enhanced by well-designed consumer health information technologies. Some individuals will use these applications alone, others with the help of caregivers.
Designers and developers should understand that there are many types of people involved in achieving health in everyday living.
Not all consumer health information technologies will be used by people in the categories identified above. Sometimes family, friends, or health professionals provide assistive care. Designers and developers should also keep these people in mind when creating new equipment and technologies:
- Informal caregivers. As many as 36 million family caregivers or friends help others manage their health and health care. Informal caregivers make meals, ensure on-time arrival to medical appointments, modify household layouts, and generally anticipate and act on the needs of the individual.
- Formal caregivers. Formal caregivers serve as the source of professional guidance and intervention. Individuals may travel to visit a formal caregiver in a hospital or clinic or may communicate with them remotely.
Each of these users (patient or caregiver) has characteristics (examples of which are provided in the circle diagram) that influence how they manage health and that therefore dictate how consumer health information technologies should be designed to support them.
What equipment and technologies are used in the home?
Technologies that help people understand and better manage health problems are fast becoming everyday objects in the home. Blood pressure meters and glucose monitors provide people with important information about their own health state and guide them toward healthy choices about medications and eating patterns. Many consumer health IT applications are developed for use with a computer, ranging from health-related Websites that help individuals better understand health conditions to game controllers and interfaces that engage people in exercise and mental challenges. High-tech devices that use complex networks of sensors and advanced appliances are also currently being built for home environments. For example, think of a carpet embedded with sensors that can tell if a person’s gait is normal or if he or she is becoming unsteady. Designers and developers will play a key role in designing technologies that are responsive to the environmental attributes listed in the circle diagram. In this guide we use the term “devices” to refer to the full range of IT developed for consumer use in the home – including web interfaces, special purpose tools like lifting devices, and computer systems.
Care should be taken to design equipment and echnologies that fit into the home environment and can be used by people in many situations.
Care should be taken to design equipment and technologies that fit into the home environment and can be used by people in many situations. Such equipment may consist of computers or devices with embedded computer processors. In considering usability, designers must be both clever and visionary in order to choose the right
- Size,
- Portability,
- Interfaces,
- Software functionality, and
- Hardware platform.
In addition, designers and developers have to plan for
- The amount of instruction the equipment requires,
- The level of maturity of the product,
- The extent to which instruction about how to manage the equipment is embedded in the equipment (system intelligence),
- The demands for maintenance, and
- The level of data security feasible in the system, because health information is highly confidential.

What tasks are conducted in the home?
Tasks include all of the activities in which people participate to maintain or improve health. Individuals engage in a number of everyday tasks (characterized by the attributes in the circle diagram) in addressing their health and health care, which may be supported by appropriate design of equipment and technologies:
- Self-monitoring. Self-monitoring includes paying attention to the cues of health in everyday living. This may be done informally (e.g., attending to one’s sensations while stretching in the morning) or systematically (e.g., monitoring blood glucose to ensure proper management of diabetes).
- Self-care. Self-care activities are undertaken in collaboration with health professionals. These may include taking medication, exercising to maintain muscle strength, or preparing appropriate meals.
- Disease management. Disease management varies with the extent and severity of a health problem and may include following complex breathing treatments, changing bandages, monitoring for signs of infection, or operating household objects safely when confusion or dementia limits judgment. It requires close coordination with health professionals and many times also requires specialized equipment.
- Communication. Communication activities can range from informal, day-to-day conversations with a close family member to deliberate the next course of action, to coordination of complex care activities after a major accident. Communication with health providers, for example, sending a series of blood pressure readings to evaluate the effects of a new medicine, is also very important and could benefit from good design.
Homes differ in important ways from hospitals and clinics, placing special demands on designers and developers to incorporate appropriate features into their designs.
What are the relevant characteristics of the home and its environment?
Homes differ in important ways from hospitals and clinics, placing special demands on designers and developers to incorporate appropriate features into their designs.
- Types of homes vary. In the United States, about 79 million homes are detached single-family houses, 28 million are multifamily suites, 5 million are duplexes, and 9 million are mobile homes.
- Not everyone lives in a private home. Many people are transient because of their work or economic situation, and approximately 3.5 million people (including 1.35 million children) are likely to experience homelessness in their lifetime.
- Homes have characteristic living spaces. Living rooms often serve as common gathering spaces for family members and friends. Kitchens and dining rooms are locations for
meal preparation and sharing. Bedrooms and bathrooms are often considered the most private spaces of the home. Health-related activities can take place in any of these spaces, although they are more likely to be undertaken in the kitchen, bathrooms, and bedrooms. Designers therefore cannot count on an individual having a dedicated space in the home to use equipment or technology.
Given the large number of considerations that may affect appropriate design, designers must learn to balance these considerations as they progress through the design process.
The circle diagram depicts home spaces as a set of embedded environments. Note that the concentric circles in the model depict environments that not only influence people’s health state, but also can shape the technologies that help them manage their health and health care.
- Physical environment. The physical environment is the relatively immutable infrastructure of a house. Physical characteristics include electrical infrastructure, spaces for public or private activities, and communication capabilities, such as telephone, Internet and television services, and storage resources.
- Social environment. The social and cultural environments include the people who live in the home, as well as those who live elsewhere but are integral to the people living there, along with their ethnic, national, and religious identities. Social and cultural environments influence how health issues are addressed, who is in charge of health information, the extent to which managing health problems is a private matter or a shared interest, and attitudes toward health care technology and practitioners.
- Community environment. The community environment includes the neighborhood that surrounds a household, including such characteristics as the accessibility of health care delivery services, the availability of public transportation, and the safety of public spaces. The designation of a neighborhood as rural or urban brings along with it connotations of the technical infrastructure that can support technologies in the home. Accessibility and safety may drive how important such features as telemedicine are to an individual.
- Public policy environment. The public policy environment shapes the availability of the telecommunications infrastructure, privacy policies related to health data, and public support for health. Each of these may increase or diminish the self-reliance that home-dwellers must have and the reliance they would be willing to place on consumer health information technologies in the home. Policies that permit or prohibit payment for specific items by health care payers, such as Medicare, in part determine the market feasibility of a device or technology. This guide addresses human factors issues; public policy issues are not discussed here.
The following tables offer design guidance related to the dimensions of the user, the physical environment, and the social and community environments, which should be considered when creating consumer health information technologies. Considerations of the task being performed are interwoven into the guidance. Given the large number of considerations that may affect appropriate design, designers must learn to balance these considerations as they progress through the design process.

Person
Understanding who is using health IT devices
| Users’ varying abilities | Types of varying abilities | Reasons for varying abilities | Effects of varying abilities | Design considerations to meet users’ varying abilities |
|
Cognitive abilities |
• Reasoning, decisionmaking, memory function, attention capacity • Reading and language comprehension • Numeracy skills • Health and technology literacy |
• Age (e.g., older adults, children) • Education • Head trauma • Disease (e.g., Alzheimer’s disease) • Illness (e.g., dementia) • Side effects of medication • Stress • Learning disabilities • Developmental disabilities |
• Reduced ability to process, comprehend, and integrate health information • Difficulties with decisionmaking • Difficulties with executing the appropriate response • Difficulties with learning and remembering step-by-step procedures • Reduced ability to comprehend instructions • Increased need for assistance |
• Devices should be designed to facilitate appropriate automatic responses by taking advantage of affordances (cues built into the device) and appropriate mapping (relationship between control and resulting action) • Devices should provide feedback to users and be tolerant of user error • Interfaces should be consistent throughout a single device and across devices • Content should be presented as simply as possible |
| Users’ varying abilities | Types of varying abilities | Reasons for varying abilities | Effects of varying abilities | Design considerations to meet users’ varying abilities |
|
Physical abilities |
• Strength (amount of weight user can lift) • Reach (how high, low, or far) • Flexibility • Finger dexterity (gripping) • Mobility (e.g., walking with or without assistance, in wheelchair) • Stamina (physical exertion) |
• Age (e.g., older adults, children) • Disease (e.g., arthritis) • Injury • Limb tremor • Movement initiation disorders (e.g., Parkinson’s disease) • Genetic abnormality • Limb amputation |
• Reduced gross motor movements (reaching, shifting the body) • Difficulties with moving from one location to another • Declines in strength and stamina • Difficulties in lifting or moving heavy equipment • Reduced ability to grip objects or open containers • Reduced walking speeds • Reduced stability and balance • Reduced ability to execute movements precisely or operate controls |
• Devices should require minimum physical effort • Devices should be operable from a neutral body position • Devices should require minimal force, repetitive action, and sustained physical effort for operation • Devices should be customizable to accommodate variations in anthropometric measurements, such as height, reach, and grip size, and ranges of motion, such as finger dexterity, neck movement, and walking distance • Devices that are meant to be portable should be lightweight, easy to disconnect/disassemble, and easy to grasp |
|
Sensory or perceptual abilities |
• Visual • Auditory • Tactile • Olfactory |
• Age • Injury • Illness • Disease • Environmental factors (e.g., noise from highway or neighbors, glare from sunlight) |
• Difficulties seeing or reading content • Difficulties hearing alarms or instructions • Difficulties distinguishing among smaller buttons |
• Devices should be customizable to account for diverse sensory and perceptual abilities (e.g., volume controls, font size, line spacing) • Devices should be flexible and use redundancies (e.g., visual, auditory, tactile signals) so that people with different abilities and needs can use them properly and effectively |

Physical Environment
Understanding the home where health IT devices are being used
| Varying physical environmental aspects of the home | Types of varying physical environmental aspects | Reasons for varying physical environmental aspects | Effects of varying physical environmental aspects | Design considerations to meet the varying physical environmental aspects of users |
|
Layout of the home |
• Space to use devices, store recordings, and dispose of trash • Clean storage space for the device and its attachments • Width of doors and hallways • Height of cabinets • Electricity (outlet location, voltage, i.e., 110 vs. 220) |
• Age of home • Size of home (square footage) • Design of home (e.g., ranch, two-story) • Floor plan (proximity of different types of living spaces) • Cleanliness of home • Socioeconomic status of family |
• Increased crowdedness • Reduced space for device placement and device storage • Devices may be placed out of reach • Increased likelihood of electrical shortages • Devices may be used in unintended locations |
• Employ layout templates to help users choose space wisely • Provide storage containers for the device and its attachments to reduce space requirements during storage • Create devices that are durable, waterproof, easily cleaned • Minimize the power demand of devices through the use of long-acting batteries or chargers • Recognize that many homes lack grounded outlets and design packaging labels that alert consumers to the need for grounding |
| Varying physical environmental aspects of the home | Types of varying physical environmental aspects | Reasons for varying physical environmental aspects | Effects of varying physical environmental aspects | Design considerations to meet the varying physical environmental aspects of users |
|
Services to the home |
• Telephone service (e.g., landline, mobile) • Internet connection (wired, wireless, speed) |
• User’s technological literacy • User’s technological self-efficacy • Location of home • Socioeconomic status of family |
• Reduced use of devices that require telephone or Internet services • Slowed interaction with devices that require Internet connection |
• Devices should be useable both online and offline • Devices should be designed in different ways to transfer data from home to health care system (e.g., design devices to be compatible with home printers) • Devices should contain content that can be downloaded both with and without graphics or in simpler formats for people with slow Internet connections • Devices should contain redundancies in the ways in which interactions can take place (e.g., email, chat, phone) |
|
Devices in the home |
• Proximity to other devices • Reliance on the presence of other devices • Connectivity to or compatibility with other devices |
• Space in the home • Number of other devices in the home • Types (and brands) of devices in the home • Age of devices • Socioeconomic status of family |
• Reduced compatibility with other devices • Cluttering of devices • Devices can malfunction • Missing needed devices due to lack of space or access • Reduced use of devices that rely on other devices |
• Devices should be designed to require minimal storage and space • Devices should be designed to be used independently of other devices when possible • Devices should be designed to be compatible with different brands and models of other devices • Product information should include the necessary technical requirements |
| Varying physical environmental aspects of the home | Types of varying physical environmental aspects | Reasons for varying physical environmental aspects | Effects of varying physical environmental aspects | Design considerations to meet the varying physical environmental aspects of users |
|
Home environment |
• Temperature • Humidity • Air quality • Adequate lighting • Environmental hazards (e.g., water, open flames) • Clutter |
• Location of home • Cleanliness of home • Preferences of homeowner • Socioeconomic status of family |
• Devices can malfunction • Devices can be harder to use • Devices can create other hazards |
• Devices should be designed to withstand a wide range of environmental conditions (e.g., incorporate backlighting) • Incorporate protection for devices (e.g., covers, filters, surge protectors) to protect from dust, grease, particulates, fumes, water, and open flames |

Social and Community Environments
Understanding the social and community environments in which health information technologies are being used
| Varying physical environmental aspects of the home | Types of varying physical environmental aspects | Reasons for varying physical environmental aspects | Effects of varying physical environmental aspects | Design considerations to meet the varying physical environmental aspects of users |
|
Nonusers in the home |
• Children • Adults • Aging adults • Pets • Caregivers • Other individuals with limiting cognitive, physical, or perceptual abilities |
• Different family structures • Visitors • Caregiving • Preferences of home owner |
• Choking hazards • Tripping hazards • Electrical hazards • User may feel self-conscious or embarrassed • May cause user to withdraw from socializing in home • Reduced user privacy |
• Devices should be designed to be portable for both private and shared use and easy storage • Devices should be cordless or have minimal cord exposure • Devices should build in fail-safe options (e.g., immediate cutoff of power when device is immersed in liquid) • Devices should be sold with appropriate storage and casings for small parts and fragile hardware • Devices should contain stands that are sturdy and not easily toppled • Devices should be inconspicuous and blend into the rest of the home • Devices should allow for both private and shared use (e.g., screens with the option of being visible only from specific angles) |
| Varying physical environmental aspects of the home | Types of varying physical environmental aspects | Reasons for varying physical environmental aspects | Effects of varying physical environmental aspects | Design considerations to meet the varying physical environmental aspects of users |
|
Family dynamics |
• Stress • Cohesion • Power structure • Communication patterns |
• Illness • Disability • Competing demands • Age of family development |
• Lack of social support • Stigma and shame • Expectations for privacy • Burden of caregiving |
• Devices should provide easy-to-use control over privacy settings • Devices’ menus and choices should be simplified • Devices should offer a variety of interaction and communication modes • Devices should be lightweight and portable |
|
Other responsibilities |
• User as caregiver for others • Work • Child care • Driving |
• Different family structures • Caregiving obligations for parents, children, neighbors, family, friends • Household obligations (e.g., mortgage, rent, bills) • Cost of health care • Location of caregiving activities • Location of home • Proximity to health care system |
• Increased workload and stress that can affect device use • Devices may be used in locations other than the home • Devices may be used in transit |
• Devices should require minimal time and effort for use • Devices should be lightweight and portable with long battery life • Devices should be inconspicuous for use in communal settings • Devices should be durable to withstand use on the go |
| Varying physical environmental aspects of the home | Types of varying physical environmental aspects | Reasons for varying physical environmental aspects | Effects of varying physical environmental aspects | Design considerations to meet the varying physical environmental aspects of users |
|
Resources |
• Health insurance • Access to home care • Access to informal caregivers • Access to transportation • Access to device training • Access to device technical support |
• Location of home • Socioeconomic status of family • Different family structures • Location of neighbors, family, friends • Public transportation options • Distance of home to health care facilities • Telephone and Internet connections to home |
• Missing needed device • Reduced help with heath care activities • Lack of device use assistance • Reduced relationship with health care providers • Difficulties with device use • Negative attitude toward device use |
• Devices should be easily portable with long battery life • Provide compatible training (e.g., hands-on, verbal instructions, written instructions) • Provide effective technical support through different media • Devices should be designed to facilitate use by taking advantage of affordances (cues built into the device) and appropriate mapping (relationship between control and resulting action) • Devices should be tolerant of user error |

Why is culture important?
Consumer health information technologies for the home should be designed to appropriately reflect the cultural context in which they will be integrated. Although “culture” is a broad term, in this guide it refers primarily to behaviors and beliefs that are shaped by identification with a racial, ethnic, nationalistic, or religious group. Cultural influences of this nature are embedded in the user and the user’s physical, social, and community environments. They shape design dimensions that include type of technology, content, functionality, interface, and related decisions, such as where in the home the technology may be used. Cultural considerations affecting design dimensions are incorporated in the discussion of users, physical environment, and social and community environment. It is important to remember that there are often differences within cultural groups as well as between them; it is therefore important to understand the specific users for which a technology is being designed and to avoid stereotyping.
Users
Language. In the United States, 47 million people do not speak English as their first language. The content and interface of a technology designed for the home must therefore reflect the appropriate language of its intended users. This requires moving beyond simple translation to ensuring that the idioms, metaphors, and concepts used in the content and interface of the technology are appropriate.
Mental model of illness. Not all cultural groups espouse the beliefs of conventional Western medicine. The content of health information technologies designed for the home must be sensitive to different beliefs about the causes and treatments of illnesses. Similarly, not all cultural groups embrace all technologies as a partner in treatment or management. The type of technologies with which a tool is coupled should comport with the intended user’s cultural beliefs.
Trust and power. Some cultural groups distrust the medical establishment. This distrust is born of historical events and is sustained by current practices and the persistence of racial and ethnic health care disparities. Consequently, it is particularly important that technology designed for individuals identifying with these groups is transparent (i.e., it should be clear who is seeing and using the patient’s information) and that its content has collaborative, not paternalistic, overtones.

Physical Environment
Use of physical space. Cultural beliefs may influence how individuals use or share living spaces in a home. Such beliefs may shape, for example, what spaces are perceived as communal and private or the type of behaviors that are appropriate in each space (e.g., a bedroom also used for prayer may not be appropriate for certain health management tasks). In such cases, the use of portable devices may be appropriate, since they can be moved for use in appropriate locations.
Social and Community Environment
Care management. Cultural groups may differ as to how they expect their family, friends, neighbors, and other community members to be involved in their health and health management (e.g., who acts as a caregiver, what are the roles of formal and informal caregivers, how caregivers are expected to respond to the caregiving experience). Such differences should be accounted for when determining, for example, how to construct privacy and security options, how to facilitate such actions as delegating or sharing decisionmaking, and how to construct training options.
This guide is designed to provide designers and developers of consumer health IT with insights about the home environment in which their devices will be used. The tables contained in the body of the guide and the checklist that follows may be used during multiple points in the design process, including both needs assessment and evaluation. The guide should supplement and shape rather than replace home visits conducted by designers and developers.

DESIGN CONSIDERATION CHECKLIST
The checklist below can be used by designers and developers to design and redesign equipment and technology to better meet users’ needs and to better fit into the physical, social, and community environments in which health behaviors are performed.
| Design Considerations to Meet Users’ Varying Abilities | Complete? (Yes: |
| Cognitive Abilities | |
| Device is designed to facilitate appropriate automatic responses by taking advantage of affordances (cues built into the device) and appropriate mapping (relationship between control and resulting action) | |
| Device provides feedback to users and is tolerant of user error | |
| Device interfaces are consistent throughout a single device and across devices | |
| Content is presented as simply as possible (e.g., elementary reading level) | |
| Physical Abilities | |
| Device requires minimal physical effort | |
| Device is operable from a neutral body position | |
| Device requires minimal force, repetitive action, and sustained physical effort for operation | |
| Device is customizable to accommodate variations in anthropometric measurements, such as height, reach, and grip size, and ranges of motion, such as finger dexterity, neck movement, and walking distance | |
| Device is portable, lightweight, easy to disconnect/disassemble, and easy to grasp | |
| Sensory or Perceptual Abilities | |
| Device is customizable to account for diverse sensory and perceptual abilities (e.g., volume controls, font size, line spacing) | |
| Device is flexible and uses redundancies (e.g., visual, auditory, tactile signals) so that people with different abilities and needs can use it properly and effectively | |
| Design Considerations to Meet Users’ Varying Abilities | Complete? (Yes: |
| Layout of the Home | |
| Product contains layout templates to help users choose space wisely | |
| Device includes storage containers for the device and its attachments to reduce space requirements when not in use | |
| Device is durable, waterproof, and easily cleaned | |
| Device minimizes power demand through the use of long-acting batteries or chargers | |
| Device contains packing labels that alert consumers to the need for grounded outlets when needed for its operation | |
| Services to the Home | |
| Device is useable both online and offline | |
| Device is designed to facilitate different ways of transferring data from the home to the health care system (e.g., a device designed to be compatible with home printers) | |
| Device contains content that can be downloaded both with and without graphics or in simpler formats for people with slow Internet connections | |
| Device contains redundancies in the ways in which interactions can take place (e.g., email, chat, phone) | |
| Devices in the Home | |
| Device requires minimal storage and space | |
| Device is usable independent of other devices when possible | |
| Device is compatible with different brands and models of other devices | |
| Product information includes necessary technical requirements | |
| Home Environment | |
| Device is designed to withstand a wide range of environmental conditions (e.g., incorporates backlighting) | |
| Device contains protection (e.g., covers, filters, surge protectors) to protect from dust, grease, particulates, fumes, water, open flames, etc. | |
| Design Considerations to Meet Users’ Varying Abilities | Complete? (Yes: |
| Nonusers in the Home | |
| Device is designed for both private and shared use | |
| Device is cordless/has minimal cord exposure | |
| Device has built-in fail-safe options (e.g., immediate cutoff of power when device is immersed in liquid) | |
| Device is sold with appropriate storage and casings for small parts and fragile hardware | |
| Device contains stands that are sturdy and not easily toppled | |
| Device is inconspicuous and blends into the rest of the home | |
| Device allows for both private and shared use (e.g., screens with the option of being visible only from specific angles) | |
| Family Dynamics | |
| Device provides easy-to-use control over privacy settings | |
| Device menus and choices are simplified | |
| Device offers a variety of interaction and communication modes | |
| Device is lightweight and portable | |
| Other Responsibilities | |
| Device requires minimal time and effort for use | |
| Device is inconspicuous for use in communal settings | |
| Device is durable to withstand use on the go | |
| Resources | |
| Device comes with compatible training (e.g., hands-on, verbal instructions, written instructions) | |
| Device comes with effective technical support through different media | |
| Device is designed to facilitate use by taking advantage of affordances (cues built into the device) and appropriate mapping (relationship between control and resulting action) | |
RELEVANT RESOURCES AND LINKS TO RESOURCES AVAILABLE ONLINE
Agency for Healthcare Research and Quality
http://www.ahrq.gov/
American Medical Informatics Association
http://www.amia.org/
Association for Computing Machinery Special Interest Group on Computer Human Interaction
http://www.sigchi.org/
Environmental Protection Agency
http://www.epa.gov/
Healthcare Information Technology Standards Panel
http://www.hitsp.org/
Home Care Technology Association of America
http://www.hctaa.org/
Human Factors and Ergonomics Society
http://www.hfes.org/
International Electrotechnical Commission
http://www.iec.ch/
National Association for Homecare & Hospice
http://www.nahc.org/
National Institute of Standards and Technology
http://www.nist.gov/
University of Wisconsin–Madison Trace Center
http://trace.wisc.edu/
COMMITTEE ON THE ROLE OF HUMAN FACTORS IN HOME HEALTH CARE
David H. Wegman (Chair), Department of Work Environment, University of Massachusetts, Lowell; Sara J. Czaja, Department of Psychiatry and Behavioral Sciences, Center on Aging, University of Miami Miller School of Medicine; K. Eric DeJonge, Washington Hospital Center, Washington, DC; Daryle Jean Gardner-Bonneau, Bonneau & Associates, Portage, Michigan; Michael Christopher Gibbons, Johns Hopkins Urban Health Institute, Johns Hopkins University Center for Community Health; Laura N. Gitlin, Johns Hopkins School of Nursing; Judith Tabolt Matthews, Department of Health and Community Systems, University of Pittsburgh School of Nursing; Misha Pavel, Division of Biomedical Engineering, Department of Science and Engineering, Oregon Health and Science University; P. Hunter Peckham, Donnell Institute of Biomedical Engineering and Orthopaedics, Case Western Reserve University (resigned March 2010); Jon Pynoos, Ethel Percy Andrus Gerontology Center, Davis School of Gerontology, University of Southern California; Robert M. Schumacher, User Centric, Inc., Oakbrook Terrace, Illinois; Mary D. Weick-Brady, Food and Drug Administration, Rockville, Maryland (resigned April 2010); and Jennifer L. Wolff, School of Public Health and School of Medicine, Johns Hopkins University.
This booklet is based on the National Research Council report Health Care Comes Home: The Human Factors (2011) and its complementary workshop summary The Role of Human Factors in Home Health Care (2010), produced by the Committee on the Role of Human Factors in Home Health Care, under the auspices of the Board on Human-Systems Integration. It was written by Patricia Flatley Brennan, R.N., Ph.D., F.A.A.N.; Rupa Valdez, Ph.D. candidate, M.S.I.E.; and Joy Rodriguez, Ph.D. candidate, M.S.I.E, all from the University of Wisconsin–Madison. Reports are available from the National Academies Press at (888) 624-8373 or (202) 334-3313 (in the Washington, DC, metropolitan area) or via the NAP Website at www.nap.edu.
Funding for this project was provided under contract number HHSP23320042509XI, task order HHSP233200800004T, with the Agency for Healthcare Research and Quality (AHRQ), U.S. Department of Health and Human Services.
![]()
The opinions expressed in this document are those of the authors and do not reflect the official position of AHRQ or the U.S. Department of Health and Human Services.
Copyright © 2011 by the National Academy of Sciences. All rights reserved.
A PDF of this work is available free to download for your personal use at
|
THE NATIONAL ACADEMIES™ Advisers to the Nation on Science, Engineering, and Medicine The nation turns to the National Academies—National |
























