Multiple factors may affect recovery after traumatic brain injury (TBI), including the individual’s severity of injury; access and response to treatment; age, preexisting environmental, genetic, or medical complications; or conditions co-occurring with the primary condition. It is important to note that recovery is not one dimensional. Practitioners and researchers measure outcomes in various ways, ranging from mortality to ability to return to preinjury employment status. However, TBI survivors themselves and their families are likely more interested in quality-of-life outcomes, such as reintegration into the community, successful return to work or school, and functional capacity in everyday life.
Previous chapters have addressed severity of TBI and other injury-related factors affecting outcome. This chapter describes the premorbid conditions (e.g., learning disabilities or psychiatric conditions), comorbidities (e.g., stress-related psychiatric disorders or somatic symptoms), and contextual factors (i.e., social environmental) affecting cognitive and functional recovery from TBI. The following sections are not intended to be an exhaustive review of all possible associated conditions; rather this synthesis of the literature focuses on those factors that the committee determined were most relevant for this report—those that may interfere with an individual’s response to rehabilitation following TBI, including cognitive rehabilitation therapy (CRT). These issues are discussed within the context of both civilian and military populations. Figure 3-1 shows the environmental, personal, or medical factors that may affect recovery.
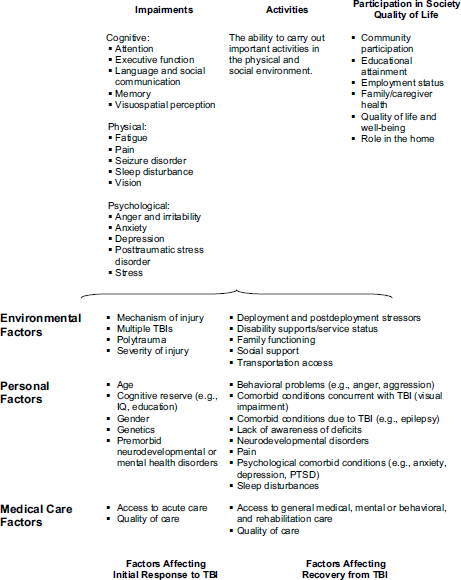
FIGURE 3-1 Factors affecting initial response to TBI and recovery from TBI.
Individuals who sustain TBI may have preexisting conditions, as well as diverse cognitive, medical, genetic, and environmental backgrounds that potentially moderate the effects of injury. Each of these elements (independently and collectively) along with the heterogeneity of TBI can affect an
individual’s initial response to trauma and subsequent response to treatment. Gaps in knowledge exist regarding the effects of preexisting conditions on outcome following TBI, and it is often difficult to differentiate the effects of preinjury factors from those related to the injury itself or the postinjury environment. Preinjury conditions, such as attention deficit hyperactivity disorder (ADHD), learning disabilities, or mild forms of syndromes on the autism spectrum (e.g., Asperger’s), may also affect an individual’s cognitive deficits after a TBI, as well an individual’s ability to acknowledge an injury, seek screening or treatment, understand a diagnosis and subsequent treatment plans, and set appropriate goals for treatment success.
Preinjury depression may affect the manifestation of various TBI-related effects. In a study of TBI by Bombardier et al. (2010), a prior history of depression among patients correlated with higher post-TBI rates of major depressive disorder. Although screening attempts to prevent individuals with most major affective disorders from military service, instances of bipolar disorder, schizophrenia, or substance use disorder (SUD), among others, may go undiagnosed. Corrigan et al. (2003) demonstrate that about half of the civilian subjects in TBI Model Systems, a national data repository of information about the acute and postacute care of individuals with TBI, had preinjury SUD. Emotional disturbance and ongoing substance abuse can also affect a survivor’s capacity to cognitively engage in and potentially benefit from even a well-designed cognitive rehabilitation program.
Other preexisting factors may contribute to poor outcomes following TBI, including a lack of social support systems and environmental factors. Socioeconomic status (SES) is an environmental factor that can affect cognitive, behavioral, and functional outcomes. Socioeconomic status is associated with low education status or low IQ. But the relationship between low SES and a worse outcome may be due to the limited resources available to the individual and the family, including access to high-quality rehabilitation and availability of family members to act as caregivers. If an individual from low SES suffers a TBI in the military, that person may be afforded the opportunity for continued treatment and care due to his service, which may otherwise be unavailable. However, due to work restrictions or other responsibilities, that person’s family or other caregivers may not be able to provide the support system and care the person needs after hospitalization and during a structured rehabilitation program.
Comorbidities are conditions that occur in addition to the primary insult, injury, or disease. Comorbidities can occur by chance (i.e., two or more conditions occurring simultaneously, with one condition not the direct origin of the other), or by causal association (Valderas et al. 2009). Causal
conditions may be linked in one of two ways: by direct causation, where one disease or injury results in another disorder, e.g., when TBI leads to memory impairment or epilepsy, or by associated risk factors, where the environment or agents leading to one condition also may manifest in another, e.g., sustaining a TBI and broken femur in the same explosion (Valderas et al. 2009). Co-occurring conditions have also been explained by selection bias, meaning those who seek treatment may be more likely to have more than one disease or adverse health condition (Valderas et al. 2009).
Comorbidities of TBI may include behavioral, psychiatric, physical, or cognitive disorders. These are generally causal associations—either due to direct causation or associated risk factors. Just as cognitive and psychiatric disorders can occur as preexisting conditions, they are also the most common comorbidities following injury, particularly in the long term. For example, TBI has been shown to be associated with the premature onset of neurodegenerative diseases, including dementia (Kiraly and Kiraly 2007). Common comorbidities include depression, anxiety disorders (e.g., PTSD), and SUD, all discussed further in this chapter.
These comorbidities may also be differentially reflected in civilian and military populations due to the nature of deployment, prolonged battle, or other challenging war zone conditions experienced by members of the military. In severe TBI in civilian populations, behavioral disturbances including irritability, disinhibition, aggression, and lack of insight or awareness pose a burden to caregivers and a challenge for rehabilitation clinicians. Meanwhile, the most commonly reported comorbidities among military populations include depression and anxiety disorders. Of these, posttraumatic stress disorder (PTSD) has been reported in 43 percent of service members who sustained blast-related mild TBI associated with alteration of consciousness (Hoge et al. 2008). Mental health disorders can affect soldiers’ and veterans’ quality of life, ability to engage in social activities or employment, and capacity to resume satisfying lives within their families and communities (Sandberg et al. 2009). Additionally, mental health disorders may have direct effect on neuropsycological functioning. They also have the potential to interfere with recognition of the need for treatment or the ability to actively engage in therapies like CRT.
Depression
Depression is defined by symptoms including sadness, apathy, negative thoughts, low energy, cognitive distortions, inability to enjoy everyday activities, and suicidal ideation (APA 2000). Depression is a common and disabling mood disorder that can significantly diminish an individual’s quality of life. Studies have found that the rate of depression post-TBI is nearly eight times higher than the general population’s rate (53.1 versus
6.7 percent) (Bombardier et al. 2010). Furthermore, depression may also develop indirectly years after an injury as a result of the effects of TBI and maladaptive readjustment (Moldover et al. 2004).
Anxiety Disorders
According to a growing body of literature, anxiety disorders (e.g., Generalized Anxiety Disorder, PTSD, and others) can develop after mild, moderate, or severe TBI (Bryant et al. 2010; Zatzick and Grossman 2011). Furthermore, as anxiety disorders are a common preinjury condition, occurring in 29 percent of the general population (Kessler et al. 2005), it has been suggested that they continue to exacerbate issues postinjury (Moore et al. 2006). Anxiety disorders have been documented as co-occurring with TBI to varying degrees in many studies. Virtually all types of anxiety disorders have been documented individuals who have experienced mild TBI, including Generalized Anxiety Disorder at 3 to 28 percent, panic disorder at 4 to 17 percent, and obsessive-compulsive disorder at 2 to 15 percent (Moore et al. 2006).
Posttraumatic Stress Disorder
Individuals diagnosed with PTSD reexperience unwanted and disturbing memories associated with a trauma. To cope, these individuals avoid thinking about the event or experience psychic numbness, often vacillating between emotional numbing and distress in response to reexperiencing symptoms. PTSD is also characterized by increased arousal, which may manifest as hypervigilance, irritability, impaired concentration, exaggerated startle response, and sleep disturbance (Sayer et al. 2009). Sleep issues, cognitive problems, or emotional issues associated with PTSD may negatively impact one’s ability to cope with effects of TBI (Lew et al. 2009). The prevalence of PTSD as a comorbid condition is higher in military TBI than in civilian TBI. Furthermore, a lack of research exists concerning how comorbid PTSD affects veterans and service members who have sustained mild, blast-related TBI.
A Rand report released in 2008 included survey results on previously deployed service members with TBI from Operation Enduring Freedom (OEF) in Afghanistan, and Operation Iraqi Freedom (OIF) in Iraq (Adamson et al. 2008). The report found that one-third of study participants “met criteria for probable PTSD” (Adamson et al. 2008). This strong association between TBI with PTSD was also reflected in a study of recently returned infantry soldiers, which shows that 43.9 percent of the infantry soldiers experienced PTSD symptoms after a loss of consciousness due to TBI, compared to 27.3 percent after an altered mental state, 16.2 percent
with other injuries, and 9.1 percent with no reported injuries (Hoge et al. 2008). Civilians may also experience PTSD associated with TBI, due to terrifying circumstances that may lead to an injury, such as a motor vehicle accident or assault. Studies have reported varying frequencies of connection between TBI and comorbid PTSD, ranging from 20 percent of individuals (Bryant and Harvey 1999) to 84 percent (Feinstein et al. 2000). While the relationship between PTSD and TBI severity has not yet been well studied, TBI severity appears to have a role in PTSD diagnosis. In civilians and military members, the prevalence of PTSD is higher in patients with milder injuries (Adamson et al. 2008; Hoge et al. 2008). Patients with more severe TBI show less risk of developing symptoms consistent with a PTSD diagnosis (Zatzick et al. 2010), possibly due to more prolonged periods of unconsciousness following the trauma.
Substance Use Disorders
Substance use disorders commonly occur among adults who have experienced a TBI. Substance abuse and dependence after TBI can complicate individuals’ efforts to successfully recover from their injury, particularly in the areas of employment and social reintegration. A cross-sectional study of substance abuse program participants reported that 10 to 20 percent of individuals with TBI, with no preinjury substance abuse issues, were substance abusers after their injuries (Corrigan et al. 1995). Other studies reveal a different story, possibly due to differences in study design or patient populations. For example, several longitudinal studies of individuals with no preinjury history of substance abuse rarely develop alcohol or drug use problems after TBI (Bombardier et al. 2003; Kreutzer et al. 1996; Ponsford et al. 2007). These studies report that less than 10 percent of participants became substance abusers after TBI.
SUDs can be both a cause and effect of TBI. Alcohol and illicit drug use in civilian populations represents a risk factor for TBI, primarily through accidents or acts of violence. However, service members deployed in OEF and OIF have limited access to alcohol and illicit drugs; thus, use of these substances at the time of injury is uncommon (Warden 2006). However, substance use as a comorbid condition with TBI has been associated with military discharge. Compared with all those discharged from the military, people with mild TBI were more than two times as likely to be discharged for alcohol, drugs, or criminal convictions, and people with moderate TBI were about five times more likely to be discharged for alcohol or drug problems (Ommaya et al. 1996). Patients with more severe brain injuries who were substance abusers preinjury may have a period of abstinence in the immediate postinjury period, but many survivors return to preinjury use levels at 2 years from injury (Corrigan et al. 1995).
Other Comorbid Conditions
Other conditions associated with TBI that may adversely affect treatment success, especially when the injury is more severe, include lack of awareness, agitation, aggression, disinhibition, and apathy (Ciurli et al. 2011; Flashman and McAllister 2002; Kim 2002). Other comorbid conditions particularly relevant to service members are those commonly associated with blast injuries, which can include physical injuries to the musculoskeletal system (including amputation and fracture), soft tissue, oral/maxillofacial areas, auditory, and visual systems (Sayer et al. 2009). Fatigue, pain, and sleep disturbance are especially common conditions in service members or veterans who experience TBI, and these conditions are likely to affect an individual’s participation in rehabilitation (DVBIC 2010).
Fatigue
Fatigue is a common complicating condition following TBI and is prevalent even months following injury (Belmont et al. 2006; Lundin et al. 2006a, 2006b; Ziino and Ponsford 2005). Fatigue is generally defined as a feeling of physical or mental exhaustion, tiredness, or weakness. It is highly interrelated with other conditions, such as sleep disturbance or depression, but these are often patient-specific correlations. Furthermore, after TBI, physical fatigue is more prevalent and severe than fatigue based on depression, pain, or sleep disturbance (Cantor et al. 2008). Fatigue may deter a person’s active participation in rehabilitation activities, and therefore, may mediate response to CRT; however, these connections have not been studied extensively.
Pain
The co-occurrence of TBI and pain is common and may arise from cognitive and physical trauma often experienced with more severe injuries, or changes in brain functioning that affect sensory and motor functioning and, perhaps, perception of pain stimuli (Sherman et al. 2006). Following TBI, frequently reported locations of pain include the head, back, legs, and shoulders. Headaches alone are one of the most common symptoms after TBI, affecting more than 30 percent of the population and often continuing long after injury (Model Systems Knowledge Translation Center 2011). Pain, including headaches, may be referred to as chronic if it persists for an extended period of time (i.e., 3 to 6 months or more). Chronic pain is often associated with other problems, including functional disability, psychological distress, litigation/compensation issues, and family discord and vocational issues (Lew et al. 2009). A recent metaanalysis considering only
veteran populations with TBI found a 43.1 percent prevalence of reported pain (Nampiaparampil 2008). In addition, pain and PTSD are often intertwined, as a chronic pain flare-up may generate PTSD-related thoughts and PTSD symptoms such as hyperarousal may increase pain intensity (Lew et al. 2009).
Sleep Disturbance
Diagnosed sleep disorders following TBI include excessive daytime sleepiness, hypersomnia, insomnia, and parasomnia and circadian rhythm alterations, such as delayed sleep phase syndrome and irregular sleep–wake pattern (Ayalon et al. 2007; Baumann et al. 2007). Previous research has shown that among brain-injured adults, sleep disturbance causes daytime sleepiness, fatigue, poorer levels of overall functioning (Verma et al. 2007), and a lack of necessary quality sleep. For patients recovering from TBI, lack of quality sleep can exacerbate symptoms such as pain, irritability, and cognitive deficits (Ouellet and Morin 2007).
Insomnia is common following TBI and has been reported in frequencies from 3 to 84 percent of TBI patients (Zeitzer et al. 2009). The cause of insomnia following TBI can be direct (e.g., secondary to neural damage), indirect (e.g., secondary to depression), or unrelated, though still present. Population-based studies indicate that insomnia occurs in approximately 40 percent of individuals with TBI of any severity and is often the most prevalent somatic complaint (Schwab et al. 2007). Sleep apnea (i.e., sleep-disordered breathing), a prevalent disorder in the general population, has been reported to be present in about half of the U.S. Department of Veterans Affairs (VA) TBI patient population (Zeitzer et al. 2009).
Treatment Options for Pre- and Comorbid Conditions
Many treatment options are available for the preinjury conditions and comorbidities described in this chapter. Of particular concern is these factors’ potential influence on or interference with CRT. In addressing the needs of the whole person for optimal outcome, the presence of pre- or comorbid conditions requires optimal coordination of treatments to address psychiatric or physical conditions in addition to cognitive impairments. Treatment coordination may include sequential versus concurrent treatment, or separate versus integrated approaches. For example, addressing PTSD symptoms first may enhance later response to CRT interventions for attention deficits, because the individual will be less distracted by psychological symptoms during rehabilitation. Likewise, one study showed improved cognitive function in patients treated for major depressive disorder (Herrera-Guzmán et al. 2010). Although the study did not include TBI
participants, the relationship between treatment for psychological disorders and cognitive function may warrant future study.
Medications are commonly prescribed to treat a range of physical or psychological symptoms. Medications that have a sedating effect or other adverse effect on cognition may affect the individual’s attention and ability to participate in CRT. However, a lack of extensive data exists on this issue. In addition to pharmacologic treatment, cognitive behavioral therapy, a form of psychotherapy, is commonly used to treat psychological conditions such as depression or PTSD (Foa et al. 2009). A previous Institute of Medicine (IOM) report evaluating PTSD interventions found sufficient evidence to support the effectiveness of exposure-based interventions, of which cognitive behavioral therapy is one (IOM 2008). As described in Chapter 4, cognitive behavioral therapy is distinct from CRT in both the target of the intervention and the specific intervention components. Cognitive behavioral therapy for PTSD typically consists of four basic components: psychoeducation, imaginal or in vivo exposure to the trauma or feared stimuli, reappraisal of distorted beliefs and thoughts, and anxiety management training (Harvey et al. 2003). Cognitive behavioral therapy interventions are designated as a first-line strategy for mental health specialty treatment of PTSD within the VA/Department of Defense (DoD) Clinical Practice Guidelines for Management of Posttraumatic Stress (VA/DoD 2010) and by several other professional and scientific organizations.
In addition to preexisting and comorbid conditions, relevant contextual factors (e.g., social environment) may influence the path to recovery from TBI. Social and family support can influence treatment outcome. In addition, compensation and disability status or application (e.g., through workman’s compensation, disability insurance, or litigation) have been shown to create patterns of symptom reporting among TBI populations. Finally, contextual conditions such as deployment and subsequent return home are important for military populations.
Family and Social Support
Family members and significant others play a key role in the recovery of adults with TBI. A key social-environmental factor that can affect the recovery process and outcome is family functioning, as families are often partners in the rehabilitation process and can play a role in goal planning and generalization of skills and knowledge to the home setting (Levack et al. 2009). Successful rehabilitation requires family cooperation in a variety of areas such as transportation, finances, leisure, and emotional support
(Jacobs 1988). From a health care systems perspective, family members or caregivers provide a large portion of the care needed to help adults with TBI function on a daily basis. Family functioning has been associated with greater improvement in people with TBI, including improvement in overall disability, level of functioning, and employability. On the other hand, family stress and unhealthy family communication and roles can hinder the rehabilitation process (Sander et al. 2002). Holistic approaches to CRT often include some family interventions, which could include educational, skill-building, and psychological support components. The results of the few family-intervention studies, while mixed in their conclusions, have reported such benefits to families as a greater number of needs being met, a perception of fewer obstacles to receiving services posttreatment (Kreutzer et al. 2009), improvement in psychological distress (Brown et al. 1999; Sinnakraruppan and Williams 1991), reduced burden, improved satisfaction with caregiving, and increased perception of caregiving competency (Albert et al. 2002). However, use of effective problem solving and coping strategies by the family was related to lower levels of depression for the person with TBI (Leach et al. 1994).
Disability Status or Compensation-Seeking Behavior
Compensation-seeking behavior or litigation has been shown to impact recovery rates and symptom patterns. The majority of studies on this topic indicate that TBI survivors actively engaged in litigation report more postconcussional symptoms (versus nonlitigants). Compensation seekers or litigants experience longer-lasting symptoms, which may result in delayed work return and higher levels of psychological stress (possibly due to the injury, unresolved financial issues, or both) (Blanchard et al. 1998; Cook 1972; Feinstein et al. 2001; Miller 2001; Paniak et al. 2002; Wood and Rutterford 2006).
Deployment and Postdeployment Factors
In a war zone, individuals are exposed to a number of factors that can influence physical and emotional health. Among the most salient of these exposures are physical trauma and psychological stressors or trauma. Physical trauma can lead not only to TBI, but also to other bodily injuries. Psychological trauma can result in a broad array of adverse outcomes including, but not limited to, PTSD and depression. Moreover, physical trauma can be associated with adverse psychological consequences, and psychological trauma can have physical symptoms. War-zone stress exposures may be particularly potent, as they are not typically limited to a single trauma. The co-occurrence of trauma to multiple body systems is
often referred to as polytrauma (see Chapter 2 for more details on poly-trauma). Furthermore, physically traumatic events are often embedded within a larger context, including exposure to psychological trauma, and service members are exposed to these types of recurring and relentless life-threatening events for extended periods of time (Vasterling et al. 2009).
In addition to direct combat exposure, stressors unique to military personnel within a war zone include episodes of extreme fear, exposure to the terrifying consequences of contemporary warfare, the lack of contemporary amenities and the comforts of daily life, and periods of boredom (King et al. 2008). Concerns about events at home may increase stress levels for deployed service members, and difficulties experienced during the transition from the war zone to home life may also increase the level of psychological distress (Vasterling et al. 2010). Combining TBI with repeated exposure to extreme stress and prolonged displacement from family, home, and community can cause interactive psychiatric and neurological disorders. Although most service members readjust successfully to their predeployment lives, an estimated 26 percent of troops develop postdeployment mental health conditions such as depression and anxiety disorders (Adamson et al. 2008). A 2006 survey assessed the health of more than 200,000 active duty service members and veterans from the Army and Marine Corps (Hoge et al. 2006). The study found that approximately 20 percent of active duty service members screened positive for one mental health condition, and 31 percent of veterans had at least one outpatient mental health care visit within the first year after returning home from Iraq or Afghanistan (Hoge et al. 2006). According to a recent report screening service members returning from combat, among those that screened positive for TBI, 33.8 percent screened positive for PTSD and 31.8 percent screened positive for depression (Adamson et al. 2008). Many of these deployment and postdeployment factors have the potential to influence the success of rehabilitation.
The factors described in this chapter may moderate an individual’s response to CRT. Furthermore, preinjury conditions, comorbidities, or environmental features may differ between civilian and military populations with TBI. Preinjury depression and anxiety disorders may be present and contribute to persistent symptoms for anyone with TBI. However, more severe preinjury psychiatric disorders or substance abuse may be more common in civilians due to screening procedures used by the military. Depression is a common comorbid condition in both civilian and military TBI. In contrast, PTSD is far more prevalent after blast-related TBI, and service members are more frequently exposed to blasts than civilians. Although social support and other environmental factors should be considered in
both civilian and military situations, the stressors associated with combat and deployment are typically more adverse than what is experienced in civilian life.
Unfortunately, published literature evaluating how these factors may affect response to CRT is sparse. Clinical trials of CRT have not consistently reported the frequency of these conditions among study participants, nor have these studies consistently controlled for conditions that could ostensibly interfere with treatment response. Even with limitations in knowledge, rehabilitation professionals must consider these potential conditions when planning treatment programs for patients with TBI. Likewise, future research on the benefit of CRT interventions for TBI may plan for these issues, which may benefit continued development and understanding of CRT and its ability to treat whole-person functioning. Chapter 14 of this report includes specific directions regarding these issues.
Adamson, D. M., M. A. Burnam, R. M. Burns, L. B. Caldarone, R. A. Cox, E. D’Amico, C. Diaz, C. Eibner, G. Fisher, T. C. Helmus, T. Tanielian, B. R. Karney, B. Kilmer, G. N. Marshall, L. T. Martin, L. S. Meredith, K. N. Metscher, K. C. Osilla, R. L. Pacula, R. Ramchand, J. S. Ringel, T. L. Schell, J. M. Sollinger, L. H. Jaycox, M. E. Vaiana, K. M. Williams, and M. R. Yochelson. 2008. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Edited by T. Tanielian and L. H. Jaycox. Santa Monica: RAND Corporation.
Albert, S. M., A. Im, L. Brenner, M. Smith, and R. Waxman. 2002. Effect of a social work liaison program on family caregivers to people with brain injury. Journal of Head Trauma Rehabilitation 17(2):175–189.
APA (American Psychiatric Association). 2000. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association.
Ayalon, L., K. Borodkin, L. Dishon, H. Kanety, and Y. Dagan. 2007. Circadian rhythm sleep disorders following mild traumatic brain injury. Neurology 68(14):1136–1140.
Baumann, C. R., E. Werth, R. Stocker, S. Ludwig, and C. L. Bassetti. 2007. Sleep-wake disturbances 6 months after traumatic brain injury: A prospective study. Brain 130(7):1873–1883.
Belmont, A., N. Agar, C. Hugeron, B. Gallais, and P. Azouvi. 2006. Fatigue and traumatic brain injury. Annales de Réadaptation et de Médecine Physique 49(6):283–288, 370–374.
Blanchard, E. B., E. J. Hickling, A. E. Taylor, T. C. Buckley, W. R. Loos, and J. Walsh. 1998. Effects of litigation settlements on posttraumatic stress symptoms in motor vehicle accident victims. Journal of Traumatic Stress 11(2):337–354.
Bombardier, C. H., J. R. Fann, N. R. Temkin, P. C. Esselman, J. Barber, and S. S. Dikmen. 2010. Rates of major depressive disorder and clinical outcomes following traumatic brain injury. Journal of the American Medical Association 303(19):1938–1945.
Brown, R., K. Pain, C. Berwald, P. Hirschi, R. Delehanty, and H. Miller. 1999. Distance education and caregiver support groups: Comparison of traditional and telephone groups. Journal of Head Trauma Rehabilitation 14(3):257–268.
Bryant, R. A., and A. G. Harvey. 1999. Postconcussive symptoms and posttraumatic stress disorder after mild traumatic brain injury. Journal of Nervous & Mental Disease 187(5):302–305.
Bryant, R. A., M. L. O’Donnell, M. Creamer, A. C. McFarlane, C. R. Clark, and D. Silove. 2010. The psychiatric sequelae of traumatic injury. American Journal of Psychiatry 167(3):312–320.
Cantor, J. B., T. Ashman, W. Gordon, A. Ginsberg, C. Engmann, M. Egan, L. Spielman, M. Dijkers, and S. Flanagan. 2008. Fatigue after traumatic brain injury and its impact on participation and quality of life. Journal of Head Trauma Rehabilitation 23(1):41–51.
Ciurli, P., R. Formisano, U. Bivona, A. Cantagallo, and P. Angelelli. 2011. Neuropsychiatric disorders in persons with severe traumatic brain injury: Prevalence, phenomenology, and relationship with demographic, clinical, and functional features. Journal of Head Trauma Rehabilitation 26(2):116–126.
Cook, J. B. 1972. The post-concussional syndrome and factors influencing recovery after minor head injury admitted to hospital. Scandinavian Journal of Rehabilitation Medicine 4(1):27–30.
Corrigan, J. D., G. L. Lamb-Hart, and E. Rust. 1995. A programme of intervention for substance abuse following traumatic brain injury. Brain Injury 9(3):221–236.
Corrigan, J. D., J. A. Bogner, G. L. Lamb-Hart, and N. Sivak-Sears. 2003. Problematic Substance Use Identified in the TBI Model Systems National Dataset. The Ohio State University.
DVBIC (Defense and Veterans Brain Injury Center). 2010. Mild Traumatic Brain Injury Pocket Guide.
Feinstein, A., S. Hershkop, A. Jardine, and D. Ouchterlony. 2000. The prevalence and neuropsychiatric correlates of posttraumatic stress symptoms following mild traumatic brain injury. Brain and Cognition 44(1):78–82.
Feinstein, A., D. Ouchterlony, J. Somerville, and A. Jardine. 2001. The effects of litigation on symptom expression: A prospective study following mild traumatic brain injury. Medicine, Science & the Law 41(2):116–121.
Flashman, L. A., and T. W. McAllister. 2002. Lack of awareness and its impact in traumatic brain injury. NeuroRehabilitation 17(4):285–296.
Foa, E. B., T. M. Keane, M. J. Friedman, and J. A. Cohen, eds. 2009. Effective Treatments for PTSD: Practice Guidelines from the International Society for Traumatic Stress Studies. 2nd ed. New York, NY: The Guilford Press.
Harvey, M., B. Hood, A. North, and I. H. Robertson. 2003. The effects of visuomotor feedback training on the recovery of hemispatial neglect symptoms: Assessment of a 2-week and follow-up intervention. Neuropsychologia 41(8):886–893.
Herrera-Guzmán I., E. Gudayol-Ferré, J. E. Herrera-Abarca, D. Herrera-Guzmán, P. Montelongo-Pedraza, F. Padrós Blázquez, M. Peró-Cebollero, and J. Guàrdia-Olmos. 2010. Major Depressive Disorder in recovery and neuropsychological functioning: Effects of selective serotonin reuptake inhibitor and dual inhibitor depression treatments on residual cognitive deficits in patients with Major Depressive Disorder in recovery. Journal of Affective Disorders 123(1–3):341–350.
Hoge, C. W., J. L. Auchterlonie, and C. S. Milliken. 2006. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. Journal of the American Medical Association 295(9):1023–1032.
Hoge, C. W., D. McGurk, J. L. Thomas, A. L. Cox, C. C. Engel, and C. A. Castro. 2008. Mild traumatic brain injury in U.S. soldiers returning from Iraq. New England Journal of Medicine 358(5):453–463.
IOM (Institute of Medicine). 2008. Treatment of Posttraumatic Stress Disorder: An Assessment of the Evidence. Washington, DC: The National Academies Press.
Jacobs, H. E. 1988. The Los Angeles head injury survey: Procedures and initial findings. Archives of Physical Medicine and Rehabilitation 69:425–431.
Kessler, R. C., N. Brandenburg, M. Lane, P. Roy-Byrne, P. D. Stang, D. J. Stein, and H. U. Wittchen. 2005. Rethinking the duration requirement for generalized anxiety disorder: Evidence from the National Comorbidity Survey Replication. Psychological Medicine 35(7):1073–1082.
Kim, E. 2002. Agitation, aggression, and disinhibition syndromes after traumatic brain injury. NeuroRehabilitation 17(4):297–310.
King, L. A., D. W. King, E. E. Bolton, J. A. Knight, and D. S. Vogt. 2008. Risk factors for mental, physical, and functional health in Gulf War veterans. Journal of Rehabilitation Research & Development 45(3):395–407.
Kiraly, M., and S. J. Kiraly. 2007. Traumatic brain injury and delayed sequelae: A review—traumatic brain injury and mild traumatic brain injury (concussion) are precursors to later-onset brain disorders, including early-onset dementia. Scientific World Journal 7:1768–1776.
Kreutzer, J., A. D. Witol, A. M. Sander, D. X. Cifu, J. H. Marwitz, and R. Delmonico. 1996. A prospective longitudinal multicenter analysis of alcohol use patterns among persons with traumatic brain injury. Journal of Head Trauma Rehabilitation 11(5):58–69.
Kreutzer, J. S., T. M. Stejskal, J. M. Ketchum, J. H. Marwitz, L. A. Taylor, and J. C. Menzel. 2009. A preliminary investigation of the brain injury family intervention: Impact on family members. Brain Injury 23(6):535–547.
Leach, L. R., R. G. Frank, D. E. Bouman, and J. Farmer. 1994. Family functioning, social support and depression after traumatic brain injury. Brain Injury 8(7):599–606.
Levack, W. M. M., R. J. Siegert, S. G. Dean, and K. M. McPherson. 2009. Goal planning for adults with acquired brain injury: How clinicians talk about involving family. Brain Injury 23(3):192–202.
Lew, H. L., J. D. Otis, C. Tun, R. D. Kerns, M. E. Clark, and D. X. Cifu. 2009. Prevalence of chronic pain, posttraumatic stress disorder, and persistent postconcussive symptoms in OIF/OEF veterans: Polytrauma clinical triad. Journal of Rehabilitation Research & Development 46(6):697–702.
Lundin, A., C. de Boussard, G. Edman, and J. Borg. 2006a. Symptoms and disability until 3 months after mild TBI. Brain Injury 20(8):799–806.
———. 2006b. Symptoms and disability until 3 months after mild TBI. Brain Injury 20(8):799–806.
Miller, L. 2001. Not just malingering: Syndrome diagnosis in traumatic brain injury litigation. NeuroRehabilitation 16(2):109–122.
Model Systems Knowledge Translation Center. 2011. Headaches After Traumatic Brain Injury. http://msktc.washington.edu/tbi/factsheets/headaches.asp (accessed July 13, 2011).
Moldover, J. E., K. B. Goldberg, and M. F. Prout. 2004. Depression after traumatic brain injury: A review of evidence for clinical heterogeneity. Neuropsychology Review 14(3):143–154.
Moore, E. L., L. Terryberry-Spohr, and D. A. Hope. 2006. Mild traumatic brain injury and anxiety sequelae: A review of the literature. Brain Injury 20(2):117–132.
Nampiaparampil, D. E. 2008. Prevalence of chronic pain after traumatic brain injury: A systematic review. Journal of the American Medical Association 300(6):711–719.
Ommaya, A. K., A. M. Salazar, A. L. Dannenberg, A. B. Chervinsky, and K. Schwab. 1996. Outcome after traumatic brain injury in the U.S. military medical system. Journal of Trauma-Injury Infection & Critical Care 41(6):972–975.
Ouellet, M. C., and C. M. Morin. 2007. Efficacy of cognitive-behavioral therapy for insomnia associated with traumatic brain injury: A single-case experimental design. Archives of Physical Medicine and Rehabilitation 88(12):1581–1592.
Paniak, C., S. Reynolds, G. Toller-Lobe, A. Melnyk, J. Nagy, and D. Schmidt. 2002. A longitudinal study of the relationship between financial compensation and symptoms after treated mild traumatic brain injury. Journal of Clinical and Experimental Neuropsychology 24(2):187–193.
Ponsford, J., R. Whelan-Goodinson, and A. Bahar-Fuchs. 2007. Alcohol and drug use following traumatic brain injury: A prospective study. Brain Injury 21(13–14):1385–1392.
Sandberg, M. A., S. S. Bush, and T. Martin. 2009. Beyond diagnosis: Understanding the healthcare challenges of injured veterans through the application of the international classification of function, disability and health (ICF). The Clinical Neuropsychologist 23(8):1416–1432.
Sander, A. M., J. S. Caroselli, W. M. High Jr., C. Becker, L. Neese, and R. Scheibel. 2002. Relationship of family functioning to progress in a post-acute rehabilitation programme following traumatic brain injury. Brain Injury 16(8):649–657.
Sayer, N. A., D. X. Cifu, S. McNamee, C. E. Chiros, B. J. Sigford, S. Scott, and H. L. Lew. 2009. Rehabilitation needs of combat-injured service members admitted to the VA polytrauma rehabilitation centers: The role of PM&R in the care of wounded warriors. PM&R 1(1):23–28.
Schwab, K. A., B. Ivins, G. Cramer, W. Johnson, M. Sluss-Tiller, K. Kiley, W. Lux, and D. Warden. 2007. Screening for traumatic brain injury in troops returning from deployment in Afghanistan and Iraq: Initial investigation of the usefulness of a short screening tool for traumatic brain injury. Journal of Head Trauma Rehabilitation 22(6):377–389.
Sherman, K. B., M. Goldberg, and K. R. Bell. 2006. Traumatic brain injury and pain. Physical Medicine and Rehabilitation Clinics of North America 17(2):473–490, viii.
Sinnakaruppan, I., and D. M. Williams. 2001. Family carers and the adult head-injured: A critical review of carers’ needs. Brain Injury 15(8):653–672.
VA/DoD (U.S. Department of Veteran’s Affairs/U.S. Department of Defense). 2010. VA/DoD Clinical Practice Guidelines for Management of Post-Traumatic Stress.
Valderas, J. M., B. Starfield, B. Sibbald, C. Salisbury, and M. Roland. 2009. Defining co-morbidity: Implications for understanding health and health services. Annals of Family Medicine 7(4):357–363.
Vasterling, J. J., M. Verfaellie, and K. D. Sullivan. 2009. Mild traumatic brain injury and post-traumatic stress disorder in returning veterans: Perspectives from cognitive neuroscience. Clinical Psychology Review 29(8):674–684.
Vasterling, J. J., S. P. Proctor, M. J. Friedman, C. W. Hoge, T. Heeren, L. A. King, and D. W. King. 2010. PTSD symptom increases in Iraq-deployed soldiers: Comparison with non-deployed soldiers and associations with baseline symptoms, deployment experiences, and postdeployment stress. Journal of Traumatic Stress 23(1):41–51.
Verma, A., V. Anand, and N. P. Verma. 2007. Sleep disorders in chronic traumatic brain injury. Journal of Clinical Sleep Medicine 3(4):357–362.
Warden, D. 2006. Military TBI during the Iraq and Afghanistan wars. Journal of Head Trauma Rehabilitation 21(5):398–402.
Wood, R. L., and N. A. Rutterford. 2006. The effect of litigation on long term cognitive and psychosocial outcome after severe brain injury. Archives of Clinical Neuropsychology 21(3):239–246.
Zatzick, D. F., and D. C. Grossman. 2011. Association between traumatic injury and psychiatric disorders and medication prescription to youths aged 10–19. Psychiatric Services 62(3):264–271.
Zatzick, D. F., F. P. Rivara, G. J. Jurkovich, C. W. Hoge, J. Wang, M. Y. Fan, J. Russo, S. G. Trusz, A. Nathens, and E. J. Mackenzie. 2010. Multisite investigation of traumatic brain injuries, posttraumatic stress disorder, and self-reported health and cognitive impairments. Archives of General Psychiatry 67(12):1291–1300.
Zeitzer, J. M., L. Friedman, and R. O’Hara. 2009. Insomnia in the context of traumatic brain injury. Journal of Rehabilitation Research & Development 46(6):827–836.
Ziino, C., and J. Ponsford. 2005. Measurement and prediction of subjective fatigue following traumatic brain injury. Journal of the International Neuropsychological Society 11(4):416–425.
















