2
Indicators Related to Continuous HIV
Care and Access to Supportive Services
This chapter addresses the committee’s charge to “provide recommendations for the most critical data and indicators to gauge the impact of the National HIV/AIDS Strategy (NHAS) and the Patient Protection and Affordable Care Act (ACA) in improving HIV/AIDS care” in the United States (statement of task). The chapter presents the committee’s choice of core and additional indicators related to continuous HIV care and access to supportive services, such as housing, for people living with HIV/AIDS (PLWHA); the process by which the committee identified and prioritized the indicators; the committee’s rationale for selecting each indicator; and the data (elements) needed to measure the indicators. The committee recognizes the importance of efforts to increase access to HIV testing and the number of HIV-infected individuals who are aware of their serostatus (IOM, 2010, 2011b,c), as well as the need to reduce the transmission of HIV through efforts to reduce risk behaviors among all persons. Based on its statement of task, however, the committee focused its attention on linkage and access to and provision of appropriate HIV care and related supportive services for people already diagnosed with HIV/AIDS.1
__________________
1Although the committee did not focus on indicators specifically related to reducing the transmission of HIV by people in care for HIV (e.g., condom use), some indicators, such as those related to undetectable viral load, also promote transmission reduction. Preliminary results from a large HIV Prevention Trials Network randomized clinical trial (HPTN 052) indicate that early use of antiretroviral therapy (ART) in PLWHA reduces sexual transmission of HIV to an uninfected partner by 96 percent (Cohen et al., 2011). Likewise, the committee did specifically address the use of ART to reduce mother-to-child transmission in pregnant women with HIV as part of the prenatal care provided to HIV-infected pregnant women.
The chapter also discusses different types of data relevant to patient care and their usefulness for evaluating the continuity (and quality) of HIV care and access to supportive services. The relative merits of each type of data are discussed, as well as whether the differences among data types (in particular claims data and clinical data) “encompass gaps in measures for HIV care” (statement of task question 1b). The chapter ends with the committee’s conclusions and recommendations for “the most critical data and indicators for gauging the impact of the National HIV/AIDS Strategy (ONAP, 2010) and the Patient Protection and Affordable Care Act [P.L. 111-148] in improving HIV/AIDS care.”
The Institute of Medicine (IOM) letter report Leading Health Indicators for Healthy People 2020 (IOM, 2011d, p. 8) defined the term “indicator” as “a measurement” and “leading health indicators” as “quantitative expressions of health-related concepts that reflect major public health concerns.” For the purposes of the present report, indicators of HIV care and access to supportive services are defined as quantitative expressions (measurements) pertaining to the state of HIV care and the availability of supportive services for PLWHA (and subgroups thereof) in the United States. “Core indicators” are those indicators deemed by the committee to be fundamental both to assessing the extent to which persons diagnosed with HIV are connected to appropriate medical care, are maintained in care over time, and have access to needed supportive services in the United States and to gauging the impact of the NHAS and the ACA in improving HIV/AIDS care.
Indicators may include process measures and outcome measures. Process measures pertain to processes of care, such as regular visits for routine care, lab tests and screening performed, and therapies initiated. Outcome measures pertain to the actual health outcomes or status of patients. Mortality and morbidity are ultimate outcome measures for tracking access to quality HIV care for people diagnosed with HIV. Intermediate outcome measures include CD4+ T-cell counts (CD4 counts) and plasma HIV RNA levels (viral loads), which reflect disease progression and infectivity. Process measures are important indicators of quality of care and treatments received, which research has shown are directly associated with good clinical outcomes (Kitahata, 1996; Kitahata et al., 2000, 2003; Landon et al., 2005). For example, regular monitoring of CD4 counts implies good-quality HIV care, with the expectation of good outcomes.
Indicators often are defined in terms of a percentage, proportion, or other relative measure and are not synonymous with the data elements
necessary to assess them. Multiple data elements may be required to generate an indicator. For example, “the proportion of PLWHA in the United States who have a CD4+ cell count above X” is an indicator, while the data needed to assess that indicator are CD4 counts (specifically the number of people with a CD4+ cell count above X) and the total number of HIV-infected individuals in the United States.
Background
A number of important sets of performance measures (Horberg et al., 2010), health objectives (HHS, 2010), and indicators (PEPFAR, 2009) related to HIV screening and care have been developed or revised in recent years. The NHAS also identifies several specific targets, in addition to its three general goals of “reducing the number of people who become infected with HIV; increasing access to care and optimizing health outcomes for people living with HIV; and reducing HIV-related health disparities” (ONAP, 2010, p. 1). These sources provide a basis for the committee’s development of a set of indicators for measuring HIV care and access to mental health, substance abuse, and supportive services in the United States (Appendix Table 2-1).2
HIV Care Quality Measures
Michael Horberg and colleagues (2010) describe the development of a set of 17 performance measures for HIV care (Table 2-1), most of which have been endorsed by the National Quality Forum (NQF), a nonprofit organization that sets national consensus standards on performance in health care (see NQF, 2011a).
The measures represent a consensus among members of a working group of experts convened by the National Committee for Quality Assurance, in conjunction with the Health Resources and Services Administration (HRSA), the Physician Consortium for Performance Improvement of the American Medical Association, and the HIV Medicine Association of the Infectious Diseases Society of America. The effort to produce a single set of
__________________
2All indicators considered by the committee are population-aggregated individual measures, such as the proportion linked to care within 3 months of diagnosis and mortality rate. The committee recognizes the importance of system-level indicators, such as the structural dimensions of system comprehensiveness, capacity, integration, and accessibility described in the Health Resources and Services Administration (HRSA) System Assessment Project (Conviser, 2007). System-level indicators are important because they are related to getting diagnosed individuals linked to, engaged in, and retained in care. However, the committee understood its charge to be recommendations for indicators to measure the quality as well as the continuity of HIV care received by PLWHA in the United States.
TABLE 2-1 HIV Care Quality Measures
|
|
|||
| Measure | Level of Care Impacteda |
Level of Evidenceb | |
|
|
|||
| Process of care | |||
|
1. Retention in care (seen at least twice annually at least 60 days apart) |
P | Level II and QM | |
|
2. CD4+ cell count measurement (measured at least twice annually) |
P | Level II and QM | |
| Screening | |||
|
3. Gonorrhea/chlamydia screening (at least once) |
P | Level II | |
|
4. Syphilis screening (annually) |
P | Level II and QM | |
|
5. Injection drug use screening (annually) |
P | Level II | |
|
6. High-risk sexual behavior screening (annually) |
P | Level I and QM | |
|
7. Tuberculosis screening (at least once) |
P | Level I and QM | |
|
8. Hepatitis B screening (at least once) |
P | Level III and QM | |
|
9. Hepatitis C screening (at least once) |
P | Level III and QM | |
| Immunization | |||
|
10. Influenza immunization (annually) |
B | Level III | |
|
11. Pneumococcal immunization (at least once) |
B | Level II and QM | |
|
12. Hepatitis B vaccination first dose received (if appropriate) |
P | Level II and QM | |
|
13. Hepatitis B vaccination series completed (if appropriate) |
S | Level II and QM | |
| Prophylactic therapy | |||
|
14. PCP prophylaxis if CD4+ cell count <200 cells/µL |
B | Level I and QM | |
| ART prescription | |||
|
15. Appropriately prescribed ART |
P | Level I and QM | |
| Viral control (at least 6 months post-ART initiation) | |||
|
16. Achieving maximal viral control if prescribed ART |
S | Level II and QM | |
|
17. Achieving maximal viral control if prescribed ART or treatment plan documentation if maximal viral control not achieved |
P | Level II and QM | |
|
|
|||
NOTE: ART, antiretroviral therapy; PCP, Pneumocystis jiroveci pneumonia.
aLevels of care are as follows: P, physician; S, system; B, both.
bLevels of evidence are as follows: I, evidence from ≥1 randomized controlled trial; II, evidence from ≥1 clinical trial, multiple cohort studies, or multiple times series or dramatic results of uncontrolled experiments; III, expert opinion only; QM, previous quality measure data indicating gaps in care.
SOURCE: Adapted from Horberg et al., 2010, Table 1.
national performance standards for HIV care was precipitated by a proliferation of HIV performance measures developed by different bodies over a number of years (Horberg et al., 2010)3 and heeds the call from the 2004 IOM report Measuring What Matters: Allocations, Planning, and Quality Assessment for the Ryan White CARE Act for a standard set of quality measures that are applicable across the range of delivery systems (IOM, 2004). Most of the performance measures endorsed by NQF are process measures. Research has shown that patients who receive more routine office visits; appropriate initiation and prescription of antiretroviral therapy (ART); and appropriate screenings, prophylaxis, and immunizations have better outcomes than those who do not (Kitahata, 1996; Kitahata et al., 2000, 2003; Landon et al., 2005).4 However, other factors (e.g., untreated non-HIV comorbidities, including mental illness; contextual factors such as food and/or housing insecurity) can result in poorer outcomes even under conditions of the most expert care and perfect treatment adherence. For this reason, outcome measures (e.g., the results of CD4 counts, mortality) are more definitive markers of successful management of HIV disease, although even with outcome indicators there are numerous factors that can affect HIV quality care and may not be able to be assessed. In addition, despite their usefulness, outcome measures generally are more difficult to obtain than process measures, although the increasing use of electronic health records (EHRs) has significantly advanced the collection of health outcomes data.
Taken together, process measures and outcome measures provide a strong basis for the development of associated HIV care indicators and are important for assessing the impact of the NHAS and ACA in improving HIV/AIDS care in the United States. With appropriate care and treatment, HIV is a chronic disease with long disease progression time. Policies that improve HIV care may have an immediate impact on some process indicators (such as frequency of CD4 testing), but a delayed impact on certain outcome indicators (particularly mortality and secondary infections). The goal of any public health intervention is to improve outcomes, but process indicators can provide early feedback about whether the policy guiding
__________________
3See, e.g., New York State Department of Health AIDS Institute, HIV Quality of Care Program, (NYSDHAI, 2011); Veterans Health Administration, HIV-QUERI (Bozzette et al., 2000); Kaiser Permanente (Horberg et al., 2011); Ryan White Program, HRSA, HIV/AIDS Bureau, HIVQUAL (HRSA, 2011a,b).
4Studies such as these suggest that provider experience in caring for PLWHA improves quality of care and patient outcomes. As the number of individuals with HIV who are in care continues to increase, and with the evolution of HIV as a chronic condition, there will be a continued need for HIV care to move away from infectious disease (HIV) specialists toward nonspecialist primary care providers who have experience in treating HIV patients (IOM, 2011c).
that intervention works. This may be especially important for particular subpopulations of PLWHA, for whom conditions may moderate the effect of a given intervention. For example, a particular group might be linked to care sooner and receive more quality care, but have less change in mortality (compared to other groups) due to chronic housing and social service needs or even different sets of HIV-related risk environments or risk clusters.
Process indicators also can provide insights into why a policy is or is not working. If mortality remains the same despite improvements in certain areas (e.g., linking people to care, routine CD4 testing, appropriate ART initiation), the collection of additional process indicators may highlight other areas that need to be addressed (e.g., screening and immunization for certain coinfections).
Healthy People 2020 Objectives
Healthy People 2020 is the most recent incarnation of an initiative begun more than 30 years ago to identify data-based objectives for improving health among Americans (HHS, 2011a). Healthy People 2020 identifies 18 objectives relating to HIV: 14 relate to HIV prevention, testing, and diagnosis, and 4 relate to health care, survival, and death following diagnosis (HHS, 2010). In keeping with the committee’s focus on HIV care following diagnosis, three of the latter four objectives (HIV.9, HIV.10, and HIV.12), in addition to one pertaining to mother-to-child transmission (HIV.8), served as a basis for associated HIV care indicators (see Box 2-1).
PEPFAR Indicators
Indicators developed by the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) provided another basis for the indicators recommended by the committee. Originally authorized by the U.S. Congress in 2003 and reauthorized in 2008, PEPFAR is an unprecedented federal government investment to address the HIV/AIDS epidemic around the world. Now a cornerstone of President Obama’s Global Health Initiative, PEPFAR provides support for national programs and strategies in more than 85 host countries to treat adults and children currently living with HIV/AIDS and to reduce the transmission of HIV (PEPFAR, 2011). PEPFAR has developed a set of essential reported indicators to gather information for planning, monitoring, and management purposes (PEPFAR, 2009).
The PEPFAR indicators that pertain to the treatment of PLWHA and the provision of supportive services, such as food assistance, also provided a basis for the committee’s development of core indicators related to continuous care and access to supportive services for PLWHA in the United States (Box 2-2).
BOX 2-1
Healthy People 2020 Summary of Objectives: HIV
Diagnosis of HIV Infection and AIDS
[HIV-1–HIV-7]
HIV-8. Reduce the number of perinatally acquired HIV and AIDS cases
Death, Survival and Medical Healthcare After Diagnosis of HIV Infection and AIDS
HIV-9. Increase the proportion of new HIV infections diagnosed before progression to AIDS
HIV-10. Increase the proportion of HIV-infected adolescents and adults who receive HIV care and treatment consistent with current standards
HIV-11. Increase the proportion of persons surviving more than 3 years after a diagnosis with AIDS
HIV-12. Reduce deaths from HIV infection
SOURCE: HHS, 2010.
NHAS Goals
As discussed in Chapter 1, the NHAS lists three primary goals: (1) reduction of HIV transmission; (2) increased access to care and optimized health outcomes for PLWHA; and (3) reduction of HIV-related health disparities (ONAP, 2010, p. 1). Within these three general goals, the NHAS identifies a number of specific measurable objectives to be met by 2015. Of particular interest for the committee’s work are the specific targets pertaining to increased access to HIV care, improved health outcomes, and reduced HIV-related health disparities.
The NHAS (ONAP, 2010, p. 21) lists three targets regarding increased access to care:
• Increase the proportion of newly diagnosed patients linked to clinical care within 3 months of their HIV diagnosis from 65 to 85 percent.
• Increase the proportion of Ryan White HIV/AIDS Program clients who are in continuous care (at least two visits for routine HIV
medical care in 12 months at least 3 months apart) from 73 to 80 percent.
• Increase the percentage of Ryan White HIV/AIDS Program clients with permanent housing from 82 to 86 percent. (This serves as a measurable proxy of [ONAP’s] efforts to expand access to [U.S.] Department of Housing and Urban Development [HUD] and other housing supports to all needy people living with HIV.)
Although the NHAS does not specify it explicitly, the text makes clear that the continuous care target for Ryan White clients serves as a measurable proxy of efforts to ensure that all diagnosed HIV-infected persons are maintained in care (ONAP, 2010, pp. 23-25).
The NHAS (ONAP, 2010, p. 31) also lists three targets in support of the goal of reducing HIV-related health disparities:
BOX 2-2
PEPFAR Essential Reported Indicators
Prevention
P1.2.D Number of HIV-positive pregnant women who received antiretrovirals to reduce risk of mother-to-child transmission
Care
C2.1.D Number of HIV-positive adults and children receiving a minimum of one clinical service
C2.4.D Percentage of HIV-positive patients who were screened for tuberculosis (TB) in HIV care or treatment settings
C2.5.D Percentage of HIV-positive patients in HIV care or treatment (pre-ART or ART) who started TB treatment
C5.1.D Number of eligible clients who received food and/or other nutrition services
Treatment
T1.2.D Number of adults and children with advanced HIV infection receiving ART [CURRENT]
SOURCE: Adapted from PEPFAR, 2009, Table 1.
- Increase the proportion of HIV-diagnosed gay and bisexual men with undetectable viral load by 20 percent.
- Increase the proportion of HIV-diagnosed blacks with undetectable viral load by 20 percent.
- Increase the proportion of HIV-diagnosed Latinos with undetectable viral load by 20 percent.
As discussed in more detail later, these six specific strategy targets provided the basis for several of the indicators recommended by the committee. Since the issue of continuity of care clearly is not limited to Ryan White HIV/AIDS Program clients, the continuity-of-care indicator identified by the committee is directed toward the general population of PLWHA but can also be applied to Ryan White HIV/AIDS Program clients or any other subpopulation. The same is true for the indicators relating to permanent housing and undetectable viral load.
Selection of Indicators of HIV Care and Access to Supportive Services
In addition to the HIV-related performance measures, health objectives, indicators, and NHAS goals discussed in the preceding sections, the committee’s selection of core indicators “to gauge the impact of the National HIV/AIDS Strategy and the Patient Protection and Affordable Care Act in improving HIV/AIDS care” (statement of task) was informed by the identification of two overarching goals for the provision of HIV care: (1) to optimize health outcomes for PLWHA and (2) to reduce the risk of transmitting the virus to others. These goals of HIV care are best achieved through full engagement of PLWHA in clinical HIV care, as depicted in Figures 2-1 and 2-2.
Primary barriers to optimal outcomes for PLWHA include late diagnosis, delayed linkage to care, poor retention in care, delayed initiation of ART, and poor adherence to ART (i.e., discontinuing or intermittent ART), as well as untreated non-HIV comorbidities and unmet basic needs (Castilla et al., 2002; Gardner et al., 2011; Justice, 2006; Lo et al., 2002). Figure 2-3 shows the number of people lost to care at various points along the care continuum. Identification of benchmarks and points at which diagnosed PLWHA are lost along the continuum of engagement in HIV care from diagnosis to death served as a basis for the committee’s selection of process and outcome indicators of quality clinical HIV care. Throughout its deliberations, the committee, in keeping with its charge to recommend indicators that “capture the care experiences of people living with HIV without substantial new investments” and mindful of the need not to increase reporting burden unduly, sought to balance the numerous facets of quality HIV care against the need for parsimony in its selection of core indicators;
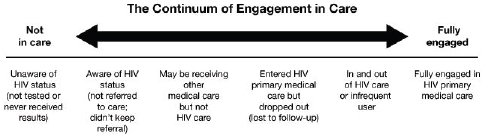
FIGURE 2-1 Continuum of engagement in care.
SOURCE: Cheever, 2007.
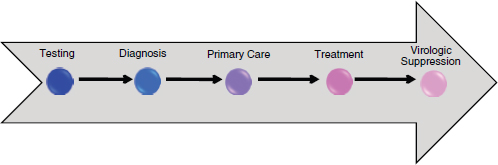
FIGURE 2-2 Continuum of HIV care arrow.
SOURCE: Adapted from Das, 2011.
hence, the core indicators reflect more general aspects of clinical HIV care, while more specific aspects are included in the additional indicators. In addition, the committee was specifically asked to address indicators related to access to supportive services, such as housing. Consideration of significant mediators of continuous engagement and optimal health outcomes in HIV care, including receipt of needed mental health and substance abuse services, homelessness and housing instability, food insecurity, and lack of transportation needed to access medical and supportive services, informed the committee’s selection of core and additional indicators in these areas.
A recent series of IOM reports discusses policies, facilitators, and barriers surrounding expanded HIV testing and access to care (IOM, 2010, 2011b,c). The present report focuses on adults who have been diagnosed with HIV and on indicators pertaining to the provision of HIV care and supportive services from diagnosis forward. Although the indicators for clinical HIV care and mental health and substance abuse are targeted toward adults, they apply to adolescents (.13 years) as well. There are tens of thousands of new diagnoses annually among the group of individuals
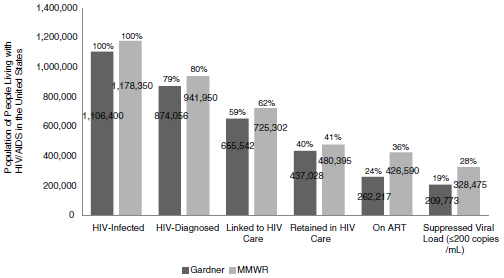
FIGURE 2-3 Engagement in HIV care cascade.
SOURCE: Adapted from CDC, 2011c; Gardner et al., 2011.
13 and older, with the highest rates between the ages of 20 and 49 years (CDC, 2012, Table 1a).5 In contrast, the use of ART to reduce or prevent perinatal transmission of the virus has resulted in a relatively small number of newly diagnosed pediatric HIV cases in the United States each year. In 2008, 218 children under the age of 13 were diagnosed with HIV; by 2010, the number had dropped to 185 (CDC, 2012, Table 1a).
Although some of the indicators, such as screening for sexually transmitted infections (STIs) and mental health and substance use disorders, generally do not apply to children under the age of 13, others, such as mortality rate, apply equally to all ages; indicators that reflect treatment guidelines apply to children as well, once they are adapted to reflect pediatric guidelines for HIV care (HHS, 2011e).
The indicators crafted by the committee reflect the current science and guidelines for the practice of HIV care at the time of writing. Although the specific details of the indicators (e.g., threshold CD4+ cell counts) may evolve over time as the science and practice of HIV care changes, the prin-
__________________
5Although there is a low rate of new HIV diagnoses among 13- to 14-year-olds (CDC, 2012, Table 1a), adolescents 13 and older fall within the same treatment guidelines as adults (HHS, 2011d) and therefore are included in the group. In addition, the current Centers for Disease Control and Prevention HIV screening guidelines also focus on individuals age 13 and older (Branson et al., 2006).
ciples embodied in the indicators (e.g., early diagnosis, linkage and retention in care, timely initiation of ART) continue to pertain.6
Core Indicators Related to Clinical HIV Care
Diagnosis
The first benchmark along the continuum of HIV care is diagnosis. Although the number of persons diagnosed with HIV earlier in the course of their infection has increased (CDC, 2009), there is evidence that many PLWHA continue to be diagnosed late. For example, the Centers for Disease Control and Prevention (CDC) estimates that in 2009 32 percent of all HIV cases reported by 46 states with confidential name-based reporting received a diagnosis of AIDS less than 12 months after their initial HIV diagnosis (CDC, 2012, Table 10a). CDC also estimates that approximately 20 percent of PLWHA in the United States are unaware that they have HIV (CDC, 2011a,b),7 putting them at risk for being diagnosed late, by which time symptoms may have already developed and treatment may not be as effective. Given the importance of care and treatment for improving health outcomes, timely diagnosis is a crucial first step in the provision of quality HIV care. In addition, research shows that individuals who are aware that they have HIV are less likely to transmit the virus to others (Pinkerton et al., 2008).
At the time of HIV diagnosis, patients should be evaluated to assess the stage of the disease and establish a baseline to help determine management plans and goals (HHS, 2011d, p. 4), including the need for mental health and substance abuse treatment and supportive services. Newly diagnosed patients also should receive recommended testing and screening, including CD4 and viral load testing, screening for concurrent infections and antiretroviral (ARV) drug resistance, and routine laboratory tests (Aberg et al., 2009, p. 662, Table 5; HHS, 2011d, p. 4; Kaplan et al., 2009).
__________________
6The committee considered guidelines for HIV treatment in its development of the indicators for clinical HIV care, including the U.S. Department of Health and Human Services Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents, dated October 14, 2011, that were current at the time the report went to press (HHS, 2011d). A revised version of the Guidelines was issued March 27, 2012, and readers may wish to take account of the revised Guidelines when considering the indicators.
7Michael Campsmith and colleagues (2010) used an extended back-calculation approach based on the number of HIV diagnoses by calendar year and disease severity (i.e., whether the individual received an AIDS diagnosis in the same calendar year as the HIV diagnosis) to estimate the total number of infections (known diagnosed cases plus estimated undiagnosed cases). They then subtracted the estimated number of deaths (obtained from national HIV/AIDS surveillance data) to arrive at an estimated prevalence of undiagnosed cases (232,700 95% CI = 221,200-244,200).
CD4 count at diagnosis provides a baseline against which subsequent tests can be compared. Along with the presence or absence of an AIDS defining illness, it serves as an indicator of the health status of the individual at HIV diagnosis. Higher CD4 counts at diagnosis indicate better health status and a shorter time between infection and diagnosis. Early diagnosis results in better health outcomes and decreased likelihood of viral transmission.
The committee recommends the following indicator as a measure of the health status of individuals at diagnosis and the timeliness of diagnosis.
• Proportion of people newly diagnosed with HIV with a CD4+ cell count >200 cells/mm3 and without a clinical diagnosis of AIDS
The indicator also can be used as a measure of the success of testing efforts within a population: an increase in the rate of early diagnosis indicates more successful testing efforts. Aggregate measures, such as median CD4 counts at diagnosis, also may be used to track the success of expanded testing efforts within a given population, with higher median CD4 counts being indicative of more people being tested sooner following infection.
Linkage to and Continuity of Care
Timely linkage to care following diagnosis is the second benchmark in HIV care. Currently only 64 to 77 percent of individuals newly diagnosed with HIV are linked to HIV care within 3 to 4 months of diagnosis (see CDC, 2011c; Gardner et al., 2011; Marks et al., 2010; Torian and Wiewel, 2011). A study of time-limited case management intervention focused on linkage to HIV care demonstrated improved linkage to care over the standard-of-care arm, which received only passive referral to a local HIV care provider in addition to information about HIV and local care resources (Gardner et al., 2005). The more quickly newly diagnosed individuals enter HIV care, the better their health outcomes are apt to be. ART may be initiated more promptly, with an attendant reduction in viral load, which leads to improved health outcomes and a reduction in HIV transmission. In addition, prompt receipt of prevention services, such as screening and treatment for STIs and mental health and substance use disorders, risk reduction counseling and behavioral interventions, assistance with partner notification, and housing assistance and other supportive services, is important for reducing transmission of the virus and improving health outcomes among PLWHA (CDC, 2010b; Crepaz, et al., 2006; Kamb et al., 1998; Shain et al., 1999; Weinhardt et al., 1999; Wolitski et al., 2005). The NHAS sets a target of linkage to care within 3 months of diagnosis (ONAP, 2010, p. 21), as does CDC’s HIV Prevention Strategic Plan (CDC,
2007). Although newly diagnosed PLWHA ideally would be linked to care within 1 month of diagnosis, the 3-month time frame is more realistic and dovetails with existing literature and public health goals.
Given the importance of timely linkage to HIV care in optimizing health outcomes of PLWHA and in reducing transmission of the virus, the committee recommends the following core indicator.
• Proportion of people newly diagnosed with HIV who are linked to clinical care for HIV within 3 months of diagnosis
Retention in or continuity of care is another key aspect of engagement in HIV care. As previously noted, regular office visits for ongoing care, appropriate initiation and monitoring of ART, and monitoring of CD4 and viral load levels, as well as provision of recommended screening, prophylaxis, and treatment for comorbid conditions, are important for ensuring optimal health outcomes for HIV-infected individuals. Missed visits during the first year of care are associated with an increasing risk of death as the number of missed visits increases (Giordano et al., 2007; Mugavero et al., 2009; Park et al., 2007). Given that approximately 50 percent of diagnosed PLWHA are not engaged in regular care (CDC, 2011c; Gardner et al., 2011; Giordano et al., 2007), increasing the proportion of diagnosed HIV-infected individuals in continuous care is important to the success of the NHAS.
Measuring continuity of care requires specifying what constitutes appropriate ongoing care. However, clinical care guidelines may not be consistent and may also evolve over time to reflect updates in clinical practice. HIV Care Quality Measures recommend HIV-infected patients be seen at least twice within a 12-month period, at least 60 days apart, and receive CD4 testing at least once every 6 months (Horberg et al., 2010). With regard to Ryan White HIV/AIDS Program clients, the NHAS defines continuous care as at least two visits within a 12-month period at least 3 months apart (ONAP, 2010, p. 21).
Regular HIV-related laboratory tests, such as CD4 and viral load testing, provide evidence of continuity of clinical HIV care (Perkins et al., 2008). U.S. Department of Health and Human Services (HHS) guidelines recommend CD4 and viral load testing every 3 to 6 months prior to initiating ART and extend the interval to every 6 to 12 months in clinically stable patients with a suppressed viral load on ART (HHS, 2011d, p. i). Although not directly representative of office visits, because patients may have office visits in addition to those associated with laboratory testing or receive laboratory testing independent of an office visit, regular monitoring of patients’ CD4 and viral load levels can serve as proxies for care visits when evaluating continuity of care.
The committee recommends the following core indicator for tracking retention in HIV care.
• Proportion of people with diagnosed HIV infection who are in continuous care (two or more visits for routine HIV medical care in the preceding 12 months at least 3 months apart)
Improvements in linkage to and retention in care are particularly important for a number of subpopulations of PLWHA that are at heightened risk for delayed entry into and poor retention in care, although the at-risk groups do not reflect consistent racial, ethnic, or sex differences (CHAIN Fact Sheet, 2004; Dennis et al., 2011; Meditz et al., 2011; Mugavero et al., 2007), because the individuals affected often vary with local resources and considerations. However, groups of particular concern, including homeless and unstably housed individuals, HIV-infected adolescents, those living in rural areas of the South, and some racial or ethnic minorities, are often burdened with a set of complex social factors such as a lack of resources (Denning and DiNenno, 2010); fears about their HIV status being revealed and the resultant stigma and discrimination (Sayles et al., 2009); or distrust of the medical system (Bogart et al., 2010; Whetten et al., 2006a).
Quality of HIV Care
Quality of HIV care is distinct from continuity of care, since a patient might be seen regularly but not receive quality HIV care—that is, care in accordance with accepted practice guidelines or measures. A number of the indicators identified by the committee could serve to measure quality of care as well as linkage to and continuity of care. For example, regular monitoring of patients’ CD4 and viral load levels (discussed in the previous section) can provide information about their continuity of care, as well as about the quality of their HIV care. The core indicators that relate to quality of care and health outcomes are presented in the following discussion.
CD4 and Viral Load Testing As process measures, CD4 and viral load testing in accordance with recommended guidelines not only demonstrate continuity of care but also are acceptable indicators of quality HIV care. Regular CD4 testing improves health outcomes in PLWHA by permitting providers to monitor individuals’ immune function, determine when to initiate ART, assess immunologic response to ART, and assess the need for initiation or discontinuation of prophylaxis for opportunistic infections (OIs) (HHS, 2011d, p. 7). Regular viral load testing is also important for monitoring clinical progression of the disease, particularly therapeutic response in individuals on ART (HHS, 2011d, p. 9). Decreased viral load, or
undetectable viral load in individuals on ART, is associated with improved health outcomes and reduced transmission of the virus.
The appropriate number and intervals for “regular” CD4 and viral load testing vary with the health status and needs of each individual. HHS Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents recommend testing every 3 to 6 months, with additional testing at the time of ART initiation or modification (HHS, 2011d, pp. 6-10).8 The interval between tests may be increased to every 6 to 12 months for clinically stable individuals on ART with viral suppression. For the purpose of tracking the impact of the NHAS and the ACA on HIV care in the United States, the committee chose to define regular testing as two or more tests in the preceding 12 months. Although the committee recognizes that one test per year could serve as a minimum standard to identify individuals who clearly have fallen out of care, in most cases it would be inappropriate to consider this frequency of testing to be indicative of optimal treatment.
Accordingly the committee recommends the following core indicators for regular CD4 and viral load testing.
- Proportion of people with diagnosed HIV infection who received two or more CD4 tests in the preceding 12 months
- Proportion of people with diagnosed HIV infection who received two or more viral load tests in the preceding 12 months
ART Initiation and Adherence Appropriate initiation of ART, the third benchmark of quality HIV care, is crucial to increased longevity and reduced morbidity among PLWHA and important for reducing transmission of the virus to others (HHS, 2011d). For this reason, a significant measure of the quality of HIV care is the proportion of PLWHA who are started on the correct drug regimen at the appropriate time. Although approximately 77 to 80 percent of individuals being treated with ART have an undetectable viral load, many PLWHA are not on ART (CDC, 2011c; Gardner et al., 2011). According to estimates, only 24 to 36 percent of PLWHA are receiving ART and only 19 to 28 percent of PLWHA overall have an undetectable viral load (CDC, 2011c; Gardner et al., 2011). As indicated in Figure 2-3, the gap lies in undetected cases of HIV infection, inadequate linkage to and retention in care for those who are diagnosed, and delayed or absent initiation of ART.
The current HHS Guidelines (HHS, 2011d, p. 27) specify that indi-
__________________
8The Guidelines also recommend viral load testing 2 to 8 weeks following ART initiation or modification and, if needed, every 4 to 8 weeks thereafter until suppression to <200 copies/mL (HHS 2011d, p. 6).
viduals with a CD4+ cell count below 350 cells/mm3 or those who have a history of an AIDS-defining illness should be started on ART. The Guide lines further recommend that ART be initiated in people whose CD4+ cell counts are between 350 and 500 cells/mm3, but the HHS panel was divided on whether to recommend ART for patients with CD4+ cell counts greater than 500 cells/mm3. In formulating a core indicator for initiation of ART, the committee followed the HHS panel’s recommended threshold of 500 cells/mm3.
• Proportion of people with diagnosed HIV infection and a measured CD4+ cell count <500 cells/mm3 who are not on ART
Initial results from the HIV Treatment Prevention Network’s HPTN 052 clinical trial funded by the National Institutes of Health indicate that early initiation of ART in PLWHA reduces sexual transmission of HIV in serostatus-discordant couples by 96 percent (Cohen et al., 2011). In an August 2011 letter to HHS Secretary Kathleen Sebelius, the Presidential Advisory Council on HIV/AIDS (PACHA) emphasized the importance of these “treatment as prevention” findings, stating that “HHS-supported HIV clinical treatment guidelines must be revised to reflect these findings” (PACHA, 2011). If HHS were to revise its guidelines according to PACHA’s recommendation, the committee would support similar revision of its ART-initiation indicator. Movement toward universal treatment for PLWHA has begun. The San Francisco and, more recently, New York City departments of health now recommend initiation of ART regardless of individuals’ CD4 count (Charlebois et al., 2011; NYC DOHMH, 2011). If a policy of universal treatment becomes widespread, a more appropriate indicator of ART initiation would be the time from diagnosis to ART initiation.
With the advent of more potent antiretroviral drugs, the goal of ART is durable virologic suppression, the fourth benchmark of quality HIV care. Adherence to a prescribed antiretroviral drug regimen is an important factor in successful treatment with ART. Failure to take antiretroviral medications as prescribed not only decreases the drugs’ effectiveness in reducing individuals’ viral load but also may increase the risk of HIV transmission to others and may lead to the emergence of ARV-resistant strains of the virus, undermining the durability of the present drug regimens. People on ART may fail to take their drugs as prescribed for a variety of reasons, including inability to pay for the medications, undesirable side effects, serious mental illness, lack of food, stigma, and forgetfulness. It is important to work with nonadherent patients to identify and address the causes of nonadherence (Cooperman et al., 2012; de Bruin et al., 2010; Henderson et al., 2011; HHS, 2011d, pp. 122-125; Reisner et al., 2009; Simoni et al., 2006, 2010).
Although adequate adherence is an important factor in achieving viral
suppression, viral suppression itself is the most important outcome measure for successful ART. HIV-infected individuals with a viral load below the level of detection experience significantly improved health outcomes (HHS, 2011d, p. 9). In addition, as reinforced by the results of the HPTN 052 clinical trial, individuals with virologic suppression are much less likely to infect others (Cohen et al., 2011). Current estimates indicate that 13 to 20 percent of individuals on ART still have a detectable viral load (CDC, 2011c; Gardner et al., 2011). Imperfect viral load suppression among treated individuals motivates the committee’s identification of the following core indicator of successful treatment with ART.
• Proportion of people with diagnosed HIV infection who have been on ART for 12 or more months and have a viral load below the level of detection
This indicator serves not only as a measure of the status of the epidemic in terms of optimal health outcomes and decreased risk of HIV transmission but also as a surrogate measure of treatment adherence and the prescription of effective drug regimens. An alternate indicator would be the time from diagnosis to virologic suppression.
Additional Outcome Indicators In aggregate, CD4 and viral load test results provide information about the status of the epidemic nationally or in specific subpopulations or geographic areas. Although virologic suppression is the primary outcome indicator for individuals on ART, the committee recommends two additional outcome indicators for monitoring the provision of quality HIV care to PLWHA.
Maintaining a CD4+ cell count ≥350 cells/mm3 reduces the risk of complicating OIs and cancers among PLWHA (HHS, 2011d, pp. 28-31). Since 64 to 76 percent of PLWHA currently are not on ART (CDC, 2011c; Gardner et al., 2011), the following indicator serves as an outcome measure for this group, as well as for those who are on ART, but have not achieved virologic suppression.
• Proportion of people with diagnosed HIV infection in continuous care for 12 or more months and with a CD4+ cell count ≥350 cells/mm3
If a large number of previously undiagnosed individuals with late-stage HIV disease entered care, the CD4+ cell count ≥350 cells/mm3 indicator might drop, suggesting poor system performance. However, this change could be interpreted correctly in the full context of all the indicators.
Mortality rate is the ultimate outcome measure for people diagnosed
with HIV infection and serves as another aggregate-level measure of HIV care. Mortality among PLWHA should be inversely related to the quality of overall care delivered. To avoid the difficulties inherent in identifying and reporting which deaths among PLWHA resulted directly or indirectly from HIV infection, the committee recommends the use of all-cause mortality in the following indicator.
• All-cause mortality rate among people with diagnosed HIV infection
Taken together, the committee recommends the preceding indicators as core indicators related to continuous and quality clinical care for PLWHA. Core indicators pertaining to mental health, substance abuse, and supportive services, such as housing, that affect the health outcomes of PLWHA are discussed in the following section.
Core Indicators Related to Mental Health,
Substance Abuse, and Supportive Services
A number of factors, including mental health symptoms and disorders, substance abuse, lack of well-being, and poor quality of life, as well as difficulty securing and maintaining basic needs of housing, food, and access and transportation to medical care and supportive services, have been shown to have a significant, negative impact on the health status and health outcomes of PLWHA (see, e.g., Conviser and Pounds, 2002a,b; Gaynes et al., 2007; Kidder et al., 2007; Leaver et al., 2007; Lo et al., 2002; Pence, 2009; Royal et al., 2009; Stall et al., 2003; Weiser et al., 2009a,b). The committee identified screening and treatment for mental health and substance use disorders, as well as access to needed housing, food, and transportation assistance, to be sufficiently important facilitators of improved health outcomes for PLWHA to recommend as indicators of HIV care. Obtaining data to estimate these indicators, especially those pertaining to supportive services, poses challenges different from those that attend the clinical HIV care indicators, nevertheless they are amenable to objective quantification.
Mental Health and Substance Abuse
Substantial evidence indicates that mental health symptoms and disorders, including neurocognitive disorders, and substance use disorders are significantly increased in people with HIV (see Hinkin et al., 2002; Lansky et al., 2009; Milloy et al., 2010; Owe-Larsson et al., 2009; WHO, 2008), and these disorders affect treatment adherence to antiretroviral medications (Ettenhofer et al., 2009; Hinkin et al., 2002; Tucker et al., 2003; Waldrop-Valverde et al., 2006) and continuity of care, secondary transmission, and
overall health outcomes (Samet et al., 2007; Ulett et al., 2009; Zaller et al., 2007). For this reason, screening HIV-infected patients for mental health and substance use symptoms and disorders is essential to providing care that will lead to the best health outcomes.
“Mental health disorders” refers to a broad range of conditions that might affect treatment and health outcomes for PLWHA, including anxiety and mood (e.g., depression) disorders, psychoses, and subthreshold conditions (i.e., mental conditions not meeting full diagnostic criteria for mental disorders). Mental health symptoms refer to conditions of psychological distress, which may be acute or chronic and are known to be related to negative health outcomes. Moderate to severe depression is particularly prevalent among PLWHA and is associated with failure to access ART, failure to adhere to ART, increased morbidity and mortality, and potentially increased HIV-related risk behavior (Crepaz and Marks, 2002; Horberg et al., 2008; Kalichman, 2000; Kumar and Encinosa, 2010; Penzak et al., 2000). The prevalence of HIV-associated neurocognitive disorders is greater than 50 percent, and perhaps higher in older HIV patients (Valcour et al., 2011), making age-specific analysis of relevant indicators particularly informative. Even mild symptomatic cognitive impairment is associated with non–central nervous system (non–CNS) morbidity and overall HIV mortality (Vivithanaporn et al., 2010). Early detection and treatment of depression, psychological distress, and cognitive impairment among PLWHA are important because they often negatively impact daily routine functioning and the ability to efficaciously adhere to medication routines. In addition, symptomatic impairment, whether mild neurocognitive disorder or asymptomatic neurocognitive impairment, has been linked to all-cause mortality (Valcour et al., 2011). More serious HIV-related neurocognitive disorders can result in dementia, which can also impede good health outcomes without necessary interventions.
Mental health disorders and symptoms can be associated with HIV in two ways: first, individuals with mental health disorders may be at greater risk for acquiring, as well as transmitting, HIV; second, HIV-infected individuals are at greater risk for developing neurocognitive disorders. In addition, HIV-infected patients, as they live longer and age, increasingly have high rates of medical comorbidity associated with the normal aging process as well as side effects from their ART (Bisson et al., 2003; Goulet et al., 2007). There is evidence as well that mental health and neurocognitive disorders are increased among older PLWHA (Justice et al., 2004; Valcour et al., 2011), making screening especially important for this subpopulation. Although some HIV-related cognitive disorders have decreased in incidence or severity with the use of ART, the overall prevalence is increased among older PLWHA.
With evidence mounting that mental health and neurocognitive disor-
ders are common in spite of ART, screening for depression and other mental health disorders as well as changes in cognition and the accompanying functional impairments may be an important factor in achieving sufficiently high adherence rates to maintain undetectable viral load and immunologic competency. Since many medical comorbidities, such as hepatitis C (and other) infection in the central nervous system (CNS), endocrine disorders, advanced cerebrovascular disease, and medications, can cause cognitive changes, the screening for medical causes of cognitive dysfunction is also imperative in order to maximize health outcomes. Although complete mental health and neuropsychological testing often are not clinically available outside of academic HIV treatment centers, a number of user-friendly screening tools are available for use in the clinic to help identify patients who should be referred to specialty services or for more extensive evaluation. Basic screening tools include the nine-item Patient Health Questionnaire (PHQ-9) for depression (Pfizer, 2011), the Modified HIV Dementia Scale (AETC, 2011, Figure 1) and the culture neutral International Dementia Scale (Sacktor et al., 2005, Figure 1), the Montreal Cognitive Assessment scale (MoCA, 2011), and the Exit 25 for severe cognitive disorders (UTHSC, 2011).
Unhealthy substance abuse or misuse behaviors, such as chronic and heavy intake of alcohol and illicit drug use, particularly injection drug use, are significantly related to the acquisition of HIV infection and for some PLWHA serve as a way to cope with and manage HIV-related symptoms (Brion et al., 2011). Heavy and chronic abuse of alcohol and other substances is also significantly related to increased risk of acquiring new HIV infections, since they can impair judgment and reduce inhibitions, potentially resulting in unsafe sex and other HIV-related transmission risk behaviors. Substance abuse is also linked with poorer health outcomes for HIV-infected individuals (Carrico, 2011), complicates health care outcomes, and decreases adherence to ART regimens. In a prospective cohort study of 140 HIV-infected patients at a county hospital HIV clinic during the year following initiation of highly active antiretroviral therapy (HAART), Carol Golin and colleagues (2002) found that nearly all of the patients’ adherence levels were suboptimal and that interventions that assessed and treated substance abuse and incorporated assistance with antiretroviral adherence were more likely to result in optimal care levels. Not only can substance use negatively affect treatment adherence and hence outcomes (Tucker et al., 2003); the use of certain substances, such methamphetamine, also has been shown to increase HIV viral replication in animal models (Gavrilin et al., 2002) and to increase neuronal damage and cognition impairment in humans (Langford et al., 2003; Rippeth et al., 2004). Judith Cook and colleagues (2008) found that the use of crack cocaine was associated with a faster progression of HIV.
Recent studies have found that multidisciplinary approaches to care that address psychiatric conditions and substance abuse and its sequelae, such as hepatitis C coinfection, resulted in improved access to and retention in care and better uptake rates of initiation of ART (Litwin et al., 2005; Palepu et al., 2006; Sherer et al., 2002). Screening, Brief Intervention, and Referral to Treatment (SBIRT) and Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) are user-friendly screening tools that permit early diagnosis and intervention in alcohol and drug use disorders in HIV and other health care settings (Babor et al., 2007; Humeniuk et al., 2008; SAMHSA, 2011). Other tools such as the Alcohol Use Disorders Identification Test (AUDIT) or CAGE (an acronym derived from its four questions that stands for “cut down,” “annoyed,” “guilty,” and “eye-opener”) questions also can be used to screen for alcohol dependency (NIAAA, 2005). Use of such tools in conjunction with a complete alcohol and drug history, including over-the-counter and alternative medicines as well as illicit drugs, is vital for increasing optimal antiretroviral treatment, reducing secondary HIV transmission, elucidating cognitive changes, and identifying individuals who might benefit from specialized adjunct treatment in addition to the management of their HIV disease.
The committee recommends two core indicators relating to mental health and substance abuse.
- Proportion of people with diagnosed HIV infection and mental health disorder who are referred for mental health services and receive these services within 60 days
- Proportion of people with diagnosed HIV infection and substance use disorder who are referred for substance abuse services and receive these services within 60 days
Studies have shown that referrals for mental health and substance abuse services that can be accessed in a short period of time after they have been recommended have some of the best outcomes and high levels of patient satisfaction (Kowal et al., 2011). In cities such as Baltimore and San Francisco, treatment on demand for substance use has been instituted to reduce the human and economic harm associated with alcohol and illicit drug use and to increase the benefits of better treatment (Drug Strategies, 2000; Friedmann et al., 2003; Sears et al., 2009). Detroit found that treatment on demand reduced homicides and larceny and resulted in high rates of patient satisfaction (Trent, 2004). The committee considered receipt of specialty mental health and substance abuse services within 30 days of referral, with urgent cases being seen as soon as possible, to reflect optimal care because it is anticipated that individuals with sufficiently severe mental health or substance use disorders to merit referral should receive those
services in a short window of time to reduce the likelihood of suboptimal adherence to ART and to decrease the risk for secondary transmission of HIV infection (and preventable new infections). However, the committee concluded that receipt of specialty services within 60 days was more realistic given the current limited capacity of many providers to see new patients within a shorter time frame.
Housing, Food Security, and Transportation
Assessment of food and housing needs and referral to appropriate services are essential to improving HIV care, improving health outcomes, and reducing health disparities among the HIV-infected population (Anema et al., 2009; McMahon et al., 2011; Reily et al., 2011; Weiser et al., 2009a,b). Studies suggest that as many as half of all persons diagnosed with HIV in the United States will face homelessness or experience an unstable housing situation at some point over the course of their illness (Aidala et al., 2007; Song, 1999). Estimates indicate that 140,000 PLWHA currently are in need of housing assistance (NAHC, 2012). Needs assessments have found that rates of food insecurity and nutritional needs range from 20 to more than 50 percent among samples of PLWHA in medical care or social service settings, with rates higher among PLWHA who are not in care.
For the purpose of this report, “housing instability” refers to homelessness, imminent risk of homelessness, and unstable housing as defined for reporting in HUD’s Homeless Management Information Systems (HMIS), which are used by all jurisdictions receiving HUD funding to address homelessness and risk of homelessness (HUD, 2010). The broad distinction is between persons who have stable, permanent housing in the community and individuals or families who lack the resources or support networks to retain or obtain permanent housing. Guidance is provided for classifying housing status in four categories: literally homeless (e.g., lack a regular nighttime residence, staying in an emergency shelter);9imminently losing housing (e.g., being evicted or being discharged from an institution with no housing options identified); unstably housed and at-risk of losing housing (e.g., temporarily doubled up with others, moving frequently for economic reasons); and stably housed (HUD, 2010, pp. 54-56). HUD currently is taking the lead in interagency efforts to develop a common vocabulary of homelessness and to standardize housing status questions among several
__________________
9This category is based on the McKinney-Vento Homeless Assistance Act (42 U.S.C. 11302, Sec. 103) definition of homelessness, as amended by the Homeless Emergency Assistance and Rapid Transition to Housing (HEARTH) Act of 2009 (P.L. 111-22, div. B, Sec. 1003). HUD issued its final rule for the definition of homelessness on December 5, 2011 (Federal Register 76[233]:75944-76019).
federal agencies, including HHS (e.g., Centers for Medicare and Medicaid Services, HRSA) and the Department of Veterans Affairs.
“Food insecurity” refers to the U.S. Department of Agriculture (USDA) definition as “limited or uncertain availability of nutritionally adequate and safe foods or limited or uncertain ability to acquire acceptable foods in socially acceptable ways” (ERS, 2009, citing Anderson, 1990). Since 2006, the USDA has applied four classifications to the range of food (in)security. High food security means “no reported indications of food-access problems or limitations”; marginal food security means “one or two reported indications—typically of anxiety over food sufficiency or shortage of food in the house [with] little or no indication of changes in diets or food intake”; low food security means “reports of reduced quality, variety, or desirability of diet [with] little or no indications of reduced food intake”; and very low food security means “reports of multiple indications of disrupted eating patterns and reduced food intake” (ERS, 2011). Persons who are classified with low and very low food security are considered food insecure (ERS, 2011).
Housing instability, food insecurity, and other supportive service needs affect HIV outcomes in direct and indirect ways. Lack of shelter or severely inadequate housing increases exposure to infectious agents, allergens, and neurotoxins that compromise health (Shaw, 2004). Poor nutrition affects the ability to maintain healthy body weight and increases the risk or complicates the management of other chronic diseases such as heart disease, diabetes, and cancer. In addition, some ARVs need to be taken with food, and diarrhea, which is often associated with homelessness, is associated with underabsorbtion of ARVs (Brantley et al., 2003; Bushen et al., 2004; Dillingham et al., 2011).
As the NHAS points out, persons who face daily challenges meeting their basic needs for housing and food are much less likely to maintain a stable HIV treatment regimen (ONAP, 2010, p. 28). Housing instability is one of the major factors limiting access to and maintenance in HIV care and adherence to treatments (Aidala et al., 2007; Ghose et al., 2011; Kidder et al., 2007; Leaver et al., 2007). Persons who are food insecure are also less likely to be in care, stay in care, or be adherent to treatment than their counterparts whose food and nutrition needs are met (Anema et al., 2009; Ashman et al., 2002; Riley et al., 2011).
Whether via physiological or psychosocial mechanisms, homelessness or unstable housing is associated with lower CD4 counts, higher viral loads, and higher rates of comorbidities among PLWHA, controlling for a wide range of individual and medical care variables (Clements-Nolle et al., 2008; Kidder et al., 2007; Knowlton et al., 2006; LeGrand et al., 2010). Homelessness has been an independent predictor of mortality in all studies that have investigated the impact of housing status on the survival of
HIV-infected persons (Lieb et al., 2002; McMahon et al., 2011; Riley et al., 2005a,b; Schwarcz et al., 2009; Walley et al., 2008). Food insecurity also is associated with poor clinical outcomes and higher mortality in the United States, as well as in low-resource countries (Campa et al., 2005; Hendricks and Gorbach, 2009; Kalichman et al., 2010; McMahon et al., 2011; Vogenthaler et al., 2010; Weiser et al., 2009a,b).
However, research has also shown that addressing the need for housing and other supportive services is both effective and cost-effective for improving health care access and health outcomes of HIV-infected people. A systematic review of 17 housing-related studies (Leaver et al., 2007) found a significant positive association between increased housing stability and better health-related outcomes, including connection to HIV medical care and adherence to treatment. In a randomized trial commissioned by the CDC and HUD, provision of rental assistance was associated with reduced emergency room use and improved mental health and clinical health outcomes for HIV-infected clients (Wolitski et al., 2010). Food and nutrition programs have improved adherence to and the effectiveness of HIV medications among food-insecure patients. Nonmedical supportive services including food assistance can serve to attract clients who need other services and can facilitate their entry into and maintenance in HIV medical care (see Ashman et al., 2002; Conover and Whetten-Goldstein, 2002; Conviser, 2007; Conviser and Pounds, 2002a,b; Messeri et al., 2002).
Another crucial supportive service for many PLWHA is transportation. Lack of reliable transportation has long been recognized as limiting access to and utilization of medical care, especially the use of prevention services and medical monitoring of chronic conditions (see, e.g., Arcury et al., 2005; Baldwin et al., 2004; Littenberg et al., 2006; Valet et al., 2009). Lack of transportation is a major barrier to regular and timely health care visits for PLWHA as well, especially in rural areas where distances to providers are often very long and public transportation is absent (Conover and Whetten-Goldstein, 2002; HRSA, 2009; Napravnik et al., 2006; Reif et al., 2005; Sarnquist et al., 2011; Stewart et al., 2011).
In rural areas, particularly in the southern United States, which accounts for almost 70 percent of all rural cases of HIV, transportation can be a significant barrier to care, including quality HIV-related medical services (Arcury et al., 2005; Cohn et al., 2001; HRSA, 2009; Kempf et al., 2010). HIV care providers can be as much as 2 hours away in rural West Virginia and as much as 200 miles away in parts of Montana (NRHA, 2006). Long travel hours, inclement weather, and lack of travel resources may be critical issues for PLWHA in rural areas and need to be addressed for these individuals to achieve timely linkage to and continuity of care (Krawczyk et al., 2006b; Weis et al., 2010). Transportation concerns are especially important in southern states because the greatest number of new infections in African
Americans, particularly women, is occurring there (Mays et al., 2011). Studies of HIV in the South have indicated the need for transportation, particularly since some individuals seek care further from their neighborhoods in order to avoid stigma and discrimination (Mays et al., 2011; Reif et al., 2005; Vermund et al., 2010).
Transportation issues often pose barriers to appropriate care for PLWHA in urban areas as well. Services research in Boston (Lo et al., 2002), Chicago (Kenagy et al., 2003), Detroit (Andersen et al., 2007), Minneapolis–St. Paul (Othieno, 2007), New York City (Halkitis et al., 2008; Messeri et al., 2002), and several multisite studies covering diverse geographic areas (Ashman et al., 2002; Cunningham et al., 1999; Rumptz et al., 2007) has shown that transportation needs are consistently associated with failure to keep scheduled medical appointments and generally worse engagement with HIV primary care. Medicaid beneficiaries and Ryan White HIV/AIDS Program clients may be eligible for transportation assistance for medical visits. However, costs are seldom fully covered and there are other medical transportation barriers as well. Public transportation may have restricted coverage and times of operation, require long walks or some other form of transport to bus stops or transit stations, and have long wait times in potentially inclement weather. Transportation services for medically fragile or wheelchair-bound individuals may be limited, and clients often face scheduling challenges. Reliance on social networks for help with transportation to HIV care or services may be closed to PLWHA due to stigma and fear of disclosure associated with visits for HIV care or services (HRSA, 2009).
Routine assessment of transportation needs and provision of transportation assistance are effective for promoting timely entry into care and retention in care for persons living with HIV (Ashman et al., 2002; Chin et al., 2009; Conover and Whetten-Goldstein, 2002; Messeri et al., 2002; Rumptz et al., 2007). Transportation assistance also facilitates appropriate follow-through and use of mental health and substance abuse services (Whetten et al., 2006b). Because their transportation needs tend to be greater, assistance with transportation shows greater impact on medical care outcomes among HIV-infected women, ethnic minorities, and recently incarcerated individuals (Andersen et al., 2007; Burks et al., 2011; Halkitis et al., 2010; Kenagy et al., 2003; Sarnquist et al., 2011; Scheyett et al., 2010). Medical and social service providers recognize transportation assistance as an effective mechanism for promoting retention in care for PLWHA (Amico, 2011).
Given the importance of adequate housing, food, and transportation to the health outcomes of PLWHA, the committee identified three core indicators related to access to services that promote housing stability, food security, and transportation. Tracking the proportion of PLWHA who
require assistance to meet their needs in these areas provides information about whether available services are meeting those needs. The committee recommends the following indicators.
- Proportion of people with diagnosed HIV infection who were homeless or temporarily or unstably housed at least once in the preceding 12 months
- Proportion of people with diagnosed HIV infection who experienced food or nutrition insecurity at least once in the preceding 12 months
- Proportion of people with diagnosed HIV infection who had an unmet need for transportation services to facilitate access to medical care and related services at least once in the preceding 12 months
Additional Indicators Related to Clinical HIV Care
In addition to the core indicators for HIV care, the committee identified a number of additional indicators, based on other, more granular, process measures, that provide a comprehensive measure of the quality of HIV care (Appendix Table 2-1).
Testing and Screening for Concurrent Infections
In addition to CD4 and viral load testing, individuals newly diagnosed with HIV should receive a complete medical workup (Aberg et al., 2009; HHS, 2011d), including testing for tuberculosis (TB); STIs, in particular, syphilis, as well as gonorrhea and chlamydia (by nucleic acid amplification test); and hepatitis B and C. Testing for these concurrent infections is important because HIV-infected individuals may be more likely to transmit HIV and other STIs to others and because comorbid conditions are more likely to affect the health of PLWHA. For this reason, the committee identified the following additional indicators pertaining to testing and screening.
- Proportion of people with diagnosed HIV infection who have had a documented tuberculosis screening test with results interpreted at least once since HIV diagnosis
- Proportion of people with diagnosed HIV infection who have had documented chlamydia, gonorrhea, and syphilis screenings at least once in the preceding 12 months
- Proportion of people with HIV infection who have had hepatitis B screening performed at least once since HIV diagnosis or for whom there is documented immunity
- Proportion of people with diagnosed HIV infection who have had hepatitis C screening performed at least once in the preceding 12 months.
The time frame specified for repeat testing or screening varies among diseases and the risk of infection. STI screening is recommended annually for sexually active individuals. Hepatitis B screening is recommended only once since diagnosis because immunity is conferred either by previous infection or by vaccination subsequent to a negative screening test, precluding the need for repeat screening. Routine testing or screening should continue to be administered at appropriate intervals in accordance with recommended treatment guidelines (CDC, 2010b) and recognized performance measures (Horberg et al., 2010; NQF, 2011b).
PLWHA also should receive recommended screening and routine primary care in accordance with accepted practice guidelines (see, e.g., Aberg et al., 2009). In particular, quality HIV care should include monitoring for a number of co-occurring, chronic medical conditions associated with HIV infection or treatment, including hyperlipidemia, diabetes, osteoporosis, renal disease, cancers, and depression. PLWHA are at increased risk for such conditions, and as HIV-infected individuals live longer, screening, monitoring, and treatment of these chronic conditions have become increasingly important elements of HIV care. Although the committee recognizes the importance of screening, monitoring, and treating such conditions in the provision of quality HIV care, it did not include indicators related to these practices, since the number of co-occurring conditions made specification of indicators for every condition impracticable and the practice guidelines for the conditions are the same for individuals with and without HIV. Oral health is another important aspect of care for PLWHA. Oral problems can be caused by either a weakened immune system or by certain types of ART, resulting in discomfort; potential difficulty with eating, maintenance of good nutrition, and adherence to ART; and potential psychosocial problems (Chapple and Hamburger, 2000; Coulter et al., 2002; NYSDHAI, 2001). Appendix Table 2-3 lists some of the co-occurring conditions most commonly associated with HIV, along with their etiologic cofactors and references to published guidelines for optimal management.
Immunizations and Prophylaxis
Appropriate immunizations and prophylaxis are other important elements of quality HIV care. The effect of HIV infection on the immune system places PLWHA at greater risk for serious complications of seasonal influenza, pneumococcal pneumonia, and the occurrence of OIs, including pneumocystis pneumonia, TB, and viral hepatitis. Immunosuppression in
PLWHA increases susceptibility to OIs, which not only increase morbidity and mortality among PLWHA but also may cause an increase in HIV viral load, thereby further weakening the immune system (Lawn et al., 2001). Although the use of ART greatly reduces the risk of acquiring OIs (Candiani et al., 2007; Kaplan et al., 2000; Ledergerber et al., 1999), PLWHA should receive appropriate immunizations and prophylactic measures in accordance with recommended guidelines to maximally protect individuals against OIs and their sequelae (Aberg et al., 2009; Kaplan et al., 2000, 2009). Because of the large number of OIs, the committee chose not to develop indicators specific to OI prophylaxis, opting instead to emphasize the importance of following established guidelines for the management of OIs (Kaplan et al., 2009).
The committee did, however, identify the following indicators pertaining to recommended immunizations for PLWHA (HHS, 2009; Horberg et al., 2010; Kaplan et al., 2009, p. 77).
- Proportion of people with diagnosed HIV infection who have received an influenza immunization during the preceding 12 months
- Proportion of people with diagnosed HIV infection who have received a pneumococcal immunization at least once since HIV diagnosis
- Proportion of people with diagnosed HIV infection who have received a hepatitis B vaccination, or who have documented immunity
The need for revaccination varies with the effectiveness of the vaccine at preventing future infection.
Additional Indicators for ART Initiation
In addition to providing guidance for initiating ART based on CD4 count (one of the core indicators recommended by the committee), HHS Guidelines specify that ART should be initiated in patients with HIV-associated nephropathy and in patients coinfected with hepatitis B virus (HBV) when treatment for HBV is indicated (HHS, 2011d, pp. 27, 30).10 The Guidelines also recommend initiation of ART in patients with active TB within 2 to 4 weeks of starting treatment for TB for patients with CD4+ cell counts ≤500 cells/mm3, and 8 weeks for those with CD4+ cell counts >500 cells/mm3 (HHS 2011d, p. 118).
The Guidelines further specify that combination ART should be initiated in pregnant women with HIV (regardless of CD4 count) to help
__________________
10Guidance for initiation of ART in response to hepatitis C coinfection is more ambiguous (HHS, 2011d, pp. 114-116; Kaplan et al., 2009, p. 89; Shafran, 2007).
prevent mother-to-child transmission of HIV (HHS, 2011d, pp. 27, 32; 2011f, p. 8). In conjunction with caesarian instead of vaginal delivery and avoidance of breastfeeding, the use of ART during pregnancy has reduced the rate of perinatal HIV transmission from 25-30 percent to less than 2 percent (CDC, 2006).
In keeping with the HHS Guidelines, the committee identified the following additional indicators for the initiation of ART.
- Proportion of people with diagnosed HIV infection and HIV-associated nephropathy, hepatitis B (when treatment is indicted), or active tuberculosis who are not on ART
- Proportion of pregnant women with diagnosed HIV infection who are not on ART
ARV Resistance Testing
The HHS Guidelines also indicate that ARV drug resistance testing should be performed prior to the initiation of ART, or if previously performed, repeat testing should be considered (HHS, 2011d, p. 11). A 2006 study showed that 15 percent of individuals newly diagnosed with HIV experience antiretroviral drug resistance (Wheeler et al., 2010), which is one barrier to effective treatment. Drug resistance testing prior to the initiation of ART helps to determine the appropriate treatment regimen and therefore improves health outcomes and reduces viral transmission. HHS Guidelines (HHS, 2011d, p. 42) list additional factors that influence selection of individual ART regimens, including the presence or absence of
comorbid conditions (e.g., cardiovascular disease, chemical dependency, liver disease, psychiatric disease, renal diseases, or tuberculosis); potential adverse drug effects; potential drug interactions with other medications; pregnancy or pregnancy potential; … gender and pretreatment CD4 count if considering nevirapine (NVP); HLA-B*5701 testing if considering abacavir (ABC); coreceptor tropism assay if considering maraviroc (MVC); patient adherence potential; and convenience (e.g., pill burden, dosing frequency, and food and fluid considerations).
Since the decision about which ART regimen is appropriate varies among patients and would be impossible to quantify and because new therapies may be developed, the best measure of whether appropriate therapy has been prescribed is the individual’s response to it. Nevertheless, the importance of ARV drug resistance testing as a first step in selecting an ART regimen led the committee to identify the following indicator of quality HIV care.
• Proportion of ART-naïve people with diagnosed HIV infection who receive drug resistance testing (genotypic) prior to ART initiation
Additional Indicators Related to Mental Health,
Substance Abuse, and Supportive Services
Unlike the additional clinical HIV care indicators, which supplement the core indicators by tracking other important aspects of HIV care, the additional indicators for mental health, substance abuse, and supportive services are directly related to the core indicators in that they track identification of PLWHA who have a need for those services through annual screening.
- Proportion of people with diagnosed HIV infection who were screened for mental health disorders at least once during the preceding 12 months
- Proportion of people with diagnosed HIV infection who were screened for substance use disorders at least once during the preceding 12 months
- Proportion of people with diagnosed HIV infection who were assessed for need for housing at least once during the preceding 12 months
- Proportion of people with diagnosed HIV infection who were assessed for need for food or nutrition at least once during the preceding 12 months
- Proportion of people with diagnosed HIV infection who were assessed for need for transportation at least once during the preceding 12 months
Summing Up
Taken together, the core and additional indicators for clinical HIV care and mental health, substance abuse, and supportive services identified by the committee provide a means for assessing the impact of public health policies across the HIV care continuum. Figure 2-4 shows the continuum of care arrow depicted in Figure 2-2 with the indicators mapped to it.
Appendix Table 2-2 also maps the indicators (and the related data elements) to the continuum of care and indicates which indicators relate to outcome measures, process measures, or both. Appendix Table 2-1 provides a summary of the indicators, including the data elements (and proxy/alternative data elements) needed to estimate them and a brief rationale for each.
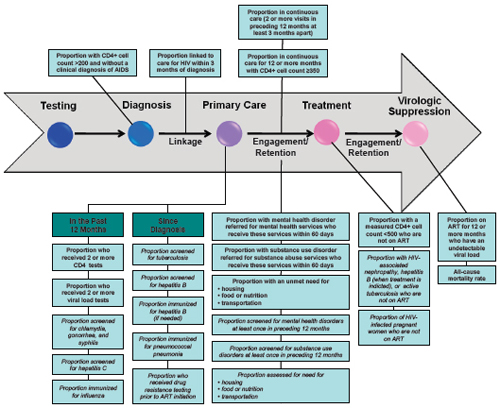
FIGURE 2-4 Continuum of HIV care arrow mapped to indicators for HIV care and supportive services.
SOURCE: Adapted from Das, 2011.
NOTE: Indicators written in bold text correspond to the committee’s recommended core indicators; the indicators written in italics correspond to the additional indicators identified by the committee.
As indicated by the NHAS targets (Box 1-1), subpopulations of PLWHA, including Ryan White HIV/AIDS Program clients, black Americans, Latinos, and gay and bisexual men, are of particular interest when evaluating HIV care. Other important subpopulations include additional vulnerable populations of race and ethnicity, sex and gender, age, lower socioeconomic status, high mobility, and those in certain geographic areas. Significant disparities exist among racial, ethnic, and sexual minorities with respect to HIV risk, incidence, and access to and continuity of care and treatment (Espinoza et al., 2008; Gebo et al., 2005; Hall et al., 2008; Mays et al., 2011; Prejean et al., 2008, 2011; Robison et al., 2008). Several studies report differences in the quality of care received by racial and ethnic minorities compared to whites (Garland et al., 2010; Korthuis et al., 2008). Differences exist in the care experiences of these groups, including differences in access to health care services; differences in the presentation of health care information and advice as a function of patient-provider interactions; and perceived bias and discrimination, although the mechanisms of how these work are not well understood (Baicker et al., 2004; Cooper-Patrick et al., 1999; Doescher et al., 2001; Johnson et al., 2004a,b; Schneider et al., 2002). Blacks are more likely to receive care from health care facilities that have fewer clinical resources and to have longer travel times to care; they also are less likely to see the same provider in follow-up care visits (Doescher et al., 2001; Probst et al., 2007). In studies comparing the care experiences of African Americans and whites, African Americans rate their care visits as less participatory and more dominated by their provider (Johnson et al., 2004b).
In addition to race and ethnicity, an individual’s country of origin and citizenship status are factors that may be related to HIV-related disparities. For example, in 2006, almost one-quarter of all new HIV infections in Latinos living in the United States were among Puerto Ricans. This finding may indicate a higher risk of HIV for Puerto Ricans or higher rates of HIV detection. Puerto Ricans may have had higher rates of testing secondary to higher rates of health insurance and access to health care when compared to other subpopulations of Latinos (Garland et al., 2010). Latinos from Mexico and Central America have been found to have higher rates of late diagnosis of HIV infection (Garland et al., 2010). Research has shown that foreign-born or unacculturated Latinos are less likely to have been tested for HIV, not only because of less access to health care but also due to a lack of knowledge about HIV as a disease (Chen et al., 2010).
Evidence also suggests that culturally and linguistically specific care increased adherence to treatment among Latinos, which then significantly improved CD4 counts and decreased viral loads (Oh et al., 2009; Silverberg
et al., 2009; Sullivan et al., 2007). Good results with adherence have been noted with urban foreign-born Latinos from Mexico and Central America when culturally appropriate care was delivered by bicultural and bilingual health care staff (Enriquez et al., 2008). It therefore appears that knowledge of linguistic and cultural differences among subpopulations of PLWHA can make a difference in the design of appropriate care approaches that can aid in adherence.
Age, sex, and geographic location are other demographic characteristics associated with disparities in HIV care. Studies have reported disparities in the receipt of HAART by age (Agwu et al., 2011; Wohl et al., 2011). Women, racial minorities, and people without private health insurance are less likely to keep an initial appointment for HIV care and therefore are less likely to establish care (Mugavero et al., 2007). Another study suggests that although white women with HIV began ART sooner than other groups, there is some evidence that women tended to have a higher incidence of HIV-related and AIDS-defining illnesses than men, with nonwhite women experiencing higher morbidity than those in other groups (Meditz et al., 2011). The study also showed a correlation between geographic location (southern United States) and higher morbidity. There is some evidence that the socioeconomic position of nonwhite women in the South is a determinant of increased morbidity in that group (Aziz and Smith, 2011; Meditz et al., 2011).
To the extent that lower socioeconomic status plays a role in racial, ethnic, and gender disparities in access to HIV care and better outcomes, implementation of the ACA may be expected to reduce disparities by increasing access to health care within certain of those subpopulations. Medicaid provides coverage for 47 percent of PLWHA estimated to be receiving regular medical care, making it the largest single source of coverage for HIV care in the United States (Kates, 2011). By raising the income threshold to qualify for Medicaid coverage to 133 percent of the federal poverty level, the ACA will significantly increase access to Medicaid, with an anticipated increase in health care utilization and improved health outcomes (Finkelstein et al., 2011). However, undocumented and recent immigrants will remain ineligible for Medicaid coverage, which may increase health disparities by citizenship.
All of the indicators identified by the committee for tracking clinical HIV care and mental health, substance abuse, and supportive services can be applied to specific subpopulations of PLWHA to evaluate and track disparities among those groups. For example, several indicators and subpopulations are specifically targeted in the NHAS under the primary goal of reducing HIV-related disparities and health inequities (ONAP, 2010, p. 1). The NHAS specifies targets for increasing the proportion of PLWHA with an undetectable viral load among black Americans, Latinos, and gay
and bisexual men by 2015 (ONAP, 2010, p. 31; see also Box 1-1). Indicators specific to these NHAS targets can be generated by applying the relevant core indicator identified by the committee—that is, the proportion of people with diagnosed HIV infection who have been on ART for 12 or more months and have a viral load below the level of detection—to these subpopulations.
- Proportion of black Americans with diagnosed HIV infection who have been on ART for 12 or more months and have a viral load below the level of detection
- Proportion of Latinos with diagnosed HIV infection who have been on ART for 12 or more months and have a viral load below the level of detection
- Proportion of gay and bisexual men with diagnosed HIV infection who have been on ART for 12 or more months and have a viral load below the level of detection
Other indicators, such as a continuity-of-care indicator—that is, the proportion of people with diagnosed HIV infection who are in continuous care (two or more visits for routine HIV medical care in the preceding 12 months at least 3 months apart)—could be applied to these and other subpopulations of interest. For example, applying the continuity-of-care indicator to the population of Ryan White HIV/AIDS Program clients would generate the information to track the NHAS target of increasing “the proportion of Ryan White HIV/AIDS Program clients who are in care (at least 2 visits for routine HIV medical care in 12 months at least 3 months apart) from 73% to 80%” by 2015 (ONAP, 2010, p. 21). Similarly, applications of the committee-identified indicators to different racial or ethnic, foreign-born, gender, and socioeconomic subpopulations would be of interest as well.
Access to quality HIV care also varies based on geographic area of residence, in terms of rural, urban, and suburban populations and region of the country (South, Northeast, Midwest, etc.) (Krawczyk et al., 2006a,b; Reif et al., 2005). People in rural areas, for example, have a more difficult time accessing appropriate HIV care. Barriers to accessing HIV care for people in rural areas include greater stigma regarding HIV infection; increased fear of HIV status being disclosed; reduced availability of local HIV-knowledgeable providers; and difficulty traveling to obtain HIV care elsewhere (Heckman et al., 1998; Mays et al., 2011; Ohl et al., 2010; Reif et al., 2005; Schur et al., 2002; Vermund et al., 2010). Barriers to accessing quality HIV care can result in poorer health outcomes for PLWHA in rural areas. A recent study of individuals initiating HIV care within the Veterans Health Administration (VHA) found that delayed entry into care
accounted for higher mortality among PLWHA in rural areas compared to those in urban areas, although, once in care, care utilization was equivalent between the two groups (Ohl et al., 2010). PLWHA in the southern United States also have been shown to be less apt to initiate treatment than those from other regions of the country. Lower socioeconomic status may play a role in these differences (Krawczyk et al., 2006a,b; Meditz et al., 2011; Weis et al., 2010).
Indicators for tracking health disparities in rural areas (and different geographic regions) can be derived from those identified by the committee. Examples of such indicators include the following:
- Proportion of people living in rural areas and newly diagnosed with HIV who are linked to clinical care for HIV within 3 months of diagnosis
- Proportion of people with diagnosed HIV infection who are living in rural areas and have been on ART for 12 or more months and have a viral load below the level of detection
- Proportion of people with diagnosed HIV infection who are living in rural areas who are in continuous care (two or more visits for routine HIV medical care in the preceding 12 months at least 3 months apart)
Equivalent framing of any of the other indicators pertaining to HIV care and needed services in terms of different subpopulations of PLWHA would help to inform both the evaluation and the impact of policies on disparities in those areas as well.
DATA ELEMENTS TO GAUGE THE IMPACT OF THE NHAS AND THE ACA
The committee identified three general groups of data elements for gauging the impact of the NHAS and the ACA in improving HIV care. Although the data elements identified include those needed to estimate the previously discussed indicators that capture the care experiences of PLWHA, the lists are not identical. The committee recognized some data elements, such as stigma, discrimination, and patient satisfaction with care, to be important but did not recommend related indicators because of the difficulties in defining, objectively quantifying, and measuring those elements.11 The three groups of data identified by the committee are health
__________________
11Although obtaining data to estimate indicators for housing, food, and transportation poses challenges, those needs are objectively quantifiable using standardized definitions such as those provided in the text. By contrast, experiences of stigma, discrimination, and satisfaction with care are not quantifiable in the same way.
care data, including data on diagnoses, test results, and health care service utilization; data pertaining to access to housing, food, and transportation; and demographic data, which, as in the case of zip code, can provide information regarding risk environment, permitting those areas to be targeted in terms of linkage of care, STI services, and the like. Health care data inform indicators related to linkage to and continuity of care, as well as quality of care. Data pertaining to supportive services inform indicators related to access to those services. Demographic and other personal data inform indicators related to payer sources and disparities (racial, ethnic, and sexual minorities; geographic) in HIV-related health care.
The following section provides an introduction to the primary types of health care, supportive services, and demographic data and lays the foundation for the later discussion of the data elements necessary for assessing each of the indicators identified by the committee.
Types of Data
The health, service utilization, and demographic data elements needed to assess the indicators are found in several general data types, including claims data, clinical data, surveillance and vital records data, and survey or interview data. Relevant data may be used for financial, legal, or epidemiologic purposes, such as billing third-party payers, certifying birth or death, and disease tracking to establish public health interventions, as well as the provision of individual patient care.
Claims Data
Claims data, also known as billing data, are records of interactions between patients and various parts of the health care system designed to solicit reimbursement from private or public third-party payers (e.g., private health insurance, Medicare, Medicaid). These data include patient-identifiable demographic data (e.g., patient address, sex, date of birth), diagnosis and procedure codes, claims for laboratory tests and other types of studies, and some claims for prescription drugs.
There are numerous advantages to the use of claims data for health care research and the evaluation of performance measures (Ferver et al., 2009; Jollis et al., 1993). They represent a large quantity of data that is relatively easy and inexpensive to obtain. The large amount of data is especially useful for compiling information on rare conditions and may facilitate the identification of trends or practices that would otherwise be missed. Some claims data systems include demographic information, such as income level and employment status, that is not generally available from other health care data systems. Claims data also are, or easily can be made, anonymous and hence can be used without patient authorization. The anonymity of the
data also make claims data particularly good source of data pertaining to sensitive diagnoses such as HIV/AIDS or mental illness. Claims data also are available electronically, which facilitates their use for research.
Claims data have a number of disadvantages as well. One major disadvantage is that claims data are designed for billing and not for use in health care research (Ferver et al., 2009; Jollis et al., 1993). Only the data necessary to file the claim are captured, which leaves the data lacking in sufficient clinical detail to be maximally useful in research on health outcomes for example. There is a single International Classification of Diseases, Ninth Revision (ICD-9) code for prostate cancer, for example, which indicates the diagnosis but provides no information as to the stage of the disease at the time of diagnosis or treatment (see, e.g., West et al., 2010). Likewise, claims data cannot directly provide information on disease progression, treatment failure, or treatment intention (e.g., therapeutic or palliative) (Jollis et al., 1993). With respect to HIV, for example, claims data may provide reasonable information on how many CD4 and viral load tests are performed in a given period, but they will not provide information on the results of those tests and so are not of use in identifying treatment failure or tracking the effect of various therapeutic interventions on CD4 counts and viral load over time. For chronic conditions the “date of onset” may be listed as the date of service at each subsequent visit or the visit may be attributed to one medical problem (diagnosis) when several in fact are present. Similarly, several procedures may be “bundled” into a single claim (Ferver et al., 2009).
Since the purpose of claims data is to generate reimbursement, there is a financial disincentive to capture any data that are not directly related to that end (Ferver et al., 2009). If itemizing diagnoses or procedures will not increase the amount of reimbursement, there is no incentive to do so; indeed, the additional reporting time required creates a disincentive. This may be especially problematic for patients with multiple comorbid conditions, including HIV. Similarly, data on procedures not submitted for reimbursement may not be captured. For example, data on HIV testing may be underrepresented if the test kits are paid for by a health department. Conversely, there is an increased incentive to include tests and procedures that can be reimbursed, which also must be taken into account when interpreting the data.
Another significant disadvantage of using claims data for research is how labor intensive it can be to analyze the data. It often requires someone with strong training in data management to perform the necessary recoding and data manipulation. For example, the rows of data may be patient records and some patients have multiple records (rows). Extensive recoding is needed to reformat the data into the patient or episode level. In addition, it may be necessary to use sample records (e.g., rather than analyzing all Medicaid records) because it would be too computationally taxing to run
all of the data. Again, this type of sampling requires someone with very strong technical skills.
Other disadvantages arise with claims data as well. Coding inaccuracies of various types may render the data problematic for research purposes. Not only may typographical coding errors occur, but misunderstandings about diagnoses and incorrect or misreported diagnoses also may occur. In addition, questionable billing practices can lead to inaccurate coding or “upcoding” in order to increase reimbursement in certain cases (Ferver et al., 2009). All of these factors are potentially problematic for the use of claims data to generate estimates of the percentage of individuals with a specific condition or receiving certain tests or procedures.
Clinical Data
Clinical data are collected for or pertain directly to the health and welfare of individual patients. The primary source of clinical data is individuals’ personal health records compiled by health care providers during the course of caring for those individuals. Health records include information on individuals’ health status, findings from physical examinations, and information on individuals’ medical history. The records also document diagnoses, tests or studies that are ordered and the results, diagnostic and therapeutic procedures, medications prescribed, when medication was administered (for inpatients), information on allergies or side effects, and the like. Health records also may contain information concerning consultations and referrals. Health records commonly include certain demographic information, such as address, date of birth, sex, and insurance status. However, certain types of demographic information, including race and ethnicity, gender identity, and sexual orientation, may not be recorded at all; may be based on provider observation rather than patient self-report; or may be reported or recorded in different ways, making it difficult to code uniformly. In addition, medical records generally do not include information on individuals’ socioeconomic position (e.g., income, wealth, education) (Krieger, 1992).
Medical records provide more detailed information, such as laboratory test and treatment results, than that available through claims data and hence are preferable for use in health care research, especially research focusing on quality of care and health outcomes. In addition, clinical data are apt to give a more accurate picture than claims data of patients’ health status (Roos et al., 1991; Tang et al., 2007).
Although medical records may provide more detailed and comprehensive information about the health care received by specific individuals, they also have a number of disadvantages from a research perspective. One problem lies in the accuracy and completeness of the health record. Clini-
cians vary not only in their accuracy regarding diagnoses but also in the accuracy and completeness of the information they elicit and record from a patient’s medical history and physical examination (Roos et al., 1991). Nevertheless, there is good reason to believe that the accuracy and comprehensiveness of the clinical information are greater than found in claims data (Roos et al., 1991).
Other difficulties involve the extraction of pertinent data from patient health records and the challenge of linking individual-level data across providers for patients with multiple providers (e.g., primary care provider, HIV specialist, mental health provider). This process can be labor intensive, expensive, and time consuming, which makes claims data an attractive surrogate for medical records data in health care research. The increased use of EHRs, especially following enactment of the Health Information Technology for Economic and Clinical Health (HITECH) Act, as part of the American Recovery and Reinvestment Act of 2009 (P.L. 111-5), has simplified the process of data extraction, although challenges remain for extraction as well as for data linking and system interoperability across providers. Integrated care systems with comprehensive EHRs, such as Kaiser Permanente (KP) and the VHA, avoid these challenges to a certain extent. EHRs can pose other difficulties as well, such as system failures, decreased interdisciplinary communication, and overreliance on checkboxes (in lieu of critical thinking) (NIH, NCRR, 2006).
Despite such potential drawbacks, EHRs also can improve the quality of documentation, increase the accuracy of shared information, and improve patient safety (e.g., through checking for possible drug interactions) (Tang et al., 2007). Use of EHR data for quality measurement also reduces provider burden by reusing clinical data already being entered as part of patient care (Tang et al., 2007). However, providers’ notes remain as “free text” that needs to be combed to find pertinent pieces of clinical information. This information extraction may be done manually, adding time and expense to the project as well as potentially introducing inaccuracies from errors during the extraction process. In some cases, it also is possible to mechanize the extraction of data from free text.
Pharmacy records are a source of data on prescriptions that have been filled. Although claims data may also provide this information, pharmacy data are available even when patients lack prescription drug coverage. Although filling a prescription does not ensure that the medication actually is being taken or taken as directed, there is some correlation between refill data and treatment adherence (Pladevall et al., 2004). As is the case with claims data, the extraction of person-level (rather than record-level) data is technically difficult. People may visit multiple pharmacies, which would make it difficult to compile data at the patient level. In addition, there is apt to be variation in the use and interoperability of electronic record systems.
The challenges may be mitigated, but not eliminated, for pharmacies that are integrated into health care systems such as KP or the VHA.
Surveillance and Vital Records Data
Disease registries and surveillance systems, such as the CDC’s National HIV Surveillance System (NHSS), a population-based registry of individuals diagnosed with HIV in the United States (CDC, 2010a), are useful sources of certain health and demographic data. Such population-based registries serve epidemiologic and public health functions, permitting the tracking of a disease’s prevalence and incidence over time and within specified geographic areas. Disease registries and surveillance systems include demographic and health data relevant to their function, including, for example, disease diagnosis and staging, risk factors, individual’s name, address, age, sex, and race and ethnicity. In addition, some HIV surveillance systems include selected clinical test results and drug treatment information. Since the NHSS and state and local HIV surveillance systems as a group are inclusive of the majority of individuals diagnosed with HIV in the United States and contain a wealth of information relevant to HIV care, they are important sources of data on PLWHA.
Vital records, which include information on births and deaths, are another source of data. Of particular interest for HIV care are mortality data on PLWHA. Although vital records systems may have developed procedures for uniform reporting on cause of death, challenges to the accuracy of cause of death information persist. Whether the proximate cause of death is attributable to a secondary or tertiary cause of interest, such as HIV, may be subject to diagnostic or reporting errors or not recorded at all. For this reason, all-cause mortality may provide a more accurate measure of mortality with in a population diagnosed with a particular disease.
Survey and Interview Data
Surveys or interviews are additional sources of data that can be used to evaluate health care quality and outcomes. Well-designed surveys can be used to help track and identify trends in health insurance, health services, hospitalizations, cost, access, and quality of care; to capture patients’ experiences with their health care services; and to evaluate the ability of the nation’s health system to meet the public’s health needs (NCHS, 2012). In addition, they can be used as tools in clinical care to assist providers in delivering needed health services and as quality measurement tools to assess clinical performance (Kass-Bartelmes, 2002).
There are a number of advantages to using surveys for data collection (Marsden and Wright, 2010). A well-designed sampling scheme allows data
gathering on a good cross-sectional snapshot of all residents, including those who are not in care (i.e., those who are by definition excluded from clinical and administrative data sets). Surveys also permit collection of data on indicators or variables that are not recorded in claims, clinical, surveillance, or other types of data (e.g., barriers to accessing care) and systematic assessment of data elements that providers may not uniformly report (e.g., socioeconomic position, educational attainment) for all patients. Questions can be tailored to fit information needs (e.g., a consistent measure of homelessness, food security, or education, rather than relying on the different ways in which clinicians may collect that information in their clinical records). In addition, interviews can elicit qualitative data about complex issues that are hard to quantify objectively, such as stigma, discrimination, or reasons some subpopulations are less likely to access care. New surveys can be fielded to collect data on emerging issues, and long-term trends can be assessed using panel data.
There are disadvantages to the use of surveys and interviews as well (Marsden and Wright, 2010). Losses to follow-up and nonresponse, which may be more common among hard-to-reach populations such as those who are homeless or unstably housed or struggling with mental health or drug use problems, may introduce bias and compromise the representativeness of results. In addition, it may be difficult to collect accurate self-reported data for a variety of reasons, including forgetfulness and reluctance to disclose sensitive information (although some survey modes such as computer-assisted questionnaires may help in that regard). Finally, primary data collection can be costly and labor intensive, although there are ways to make it less so (e.g., adding modules to existing surveys such as the National Health and Nutrition Examination Survey, contracting with companies that have existing sample pools).
Summary
The differences between clinical data such as test results and claims data can result in gaps in measures of HIV care. Claims data provide information about the number of PLWHA who are in care and the frequency with which they are seen, although it may not always be possible to gauge whether a visit for an unrelated health concern also included HIV care, nor are claims data designed to measure care quality. Claims data also can yield information about what tests and other procedures are being provided to an individual and the frequency with which they are being done. However, claims data provide no information on the results or outcomes of the tests or procedures. Similarly claims data or pharmacy records may provide information about whether prescriptions for ART medications are being
filled and at what interval, but such information serves only as a proxy for data on treatment adherence.
Claims data provide important, although potentially incomplete, information about quality of HIV care with regard to continuity of care (frequency of visits), provision of appropriate screening and monitoring (types and frequency of laboratory tests), and, to a certain extent, timely initiation and prescription of appropriate ART (medical and pharmacy records). Such data are important for assessing whether PLWHA are receiving quality HIV care. Other factors, such as substance use, mental health disorders, housing instability, and food insecurity, can negatively affect health outcomes even when individuals receive and adhere to quality HIV care and treatment. For this reason, clinical data pertaining to health outcomes, such as lower viral loads and higher CD4 counts, are important for tracking the overall success of HIV care in improving health outcomes for PLWHA and controlling the epidemic. Such clinical data (e.g., CD4 count results) also are currently needed to supplement other types of data when assessing the timeliness of ART initiation.
Data from surveys and interviews can fill additional data gaps by providing information on hard-to-reach populations, such as homeless individuals and PLWHA who are not in care, and permitting collection of data not routinely collected by health care providers, such as need for and access to supportive services and subjective experiences of stigma and discrimination and satisfaction with care providers.
For these reasons, different types of data (e.g., claims, clinical, surveillance, survey) are needed to estimate the core indicators related to continuous, quality clinical HIV care and access to mental health, substance abuse, and supportive services for people living with HIV and hence to assess the impact of the NHAS and the ACA in terms of improving care for PLWHA. Because the data needed to estimate the indicators identified by the committee are likely to come from different sources, attention to the use of consistent definitions (e.g., homelessness, food insecurity, race, ethnicity, gender) in the collection of data is important.
Data Elements for Assessing Indicators
Appendix Table 2-1 lists the data elements needed to estimate each of the indicators identified by the committee. Many of the data elements are used to estimate more than one indicator, making the total number of required data elements fewer than it might initially appear. In some cases, suitable proxies may exist that can be substituted for the specified data elements when they cannot be obtained from a specific data system of interest. The following sections discuss the data elements in groups pertaining to their use.
Denominators
All of the indicators rely on the population of PLWHA or a subpopulation thereof (e.g., a clinical marker of some type, such as ART or pregnancy status) for their denominators. The goal is to select as comprehensive and nationally representative a population of PLWHA as possible when assessing indicators for the full population of PLWHA in the United States. Discussion of the current availability of nationally representative data for the population of PLWHA in the United States follows in Chapter 3. Similarly, when assessing indicators for specific subpopulations of PLWHA, the goal, again, is to begin with as comprehensive and nationally representative a population as possible and then to apply the limiting element, such as race or ethnicity, to the group.
As noted, blacks, Latinos, gay and bisexual men, and Ryan White HIV/AIDS Program clients are subpopulations specifically identified in NHAS targets. Additional subpopulations of interest include other racial and ethnic groups, women, individuals living in rural areas or different geographic areas, individuals of varying socioeconomic position or levels of acculturation, and individuals with different payer status. Demographic data needed to assess the application of indicators to such subpopulations include race and ethnicity; gender identity; sexual orientation; zip code or other identifier for current geographic area of residence; payer status (e.g., private, Medicaid, Medicare, VA, Ryan White HIV/AIDS Program); socioeconomic position; and level of acculturation (e.g., primary language spoken). These data can be collected, based on individual self-report, in clinical records, surveys, and administrative records for claims or program eligibility records.
One difficulty faced in evaluating, tracking, and reporting on the quality of the care and treatment of these subpopulations is the lack of data collected on a number of these demographic characteristics. Although data systems relating to HIV care generally capture data on age, sex assigned at birth, and certain information on race and ethnicity and current area of residence, many fewer capture complete information on payer status, sexual minority status, gender identity, nativity status, and primary language preferred.
It is important that complete data on both race and ethnicity be collected not only to evaluate and track health disparities but also because of the essential role they play in clinical care decisions. For example, Latinos, African Americans, American Indians, and some subpopulations of Asian and Pacific Islanders are at higher risk for diabetes and its complications than are whites, raising concerns about the use of some ARVs with higher associations of metabolic syndromes. In a small study of 43 ART-naïve Latinos, Latinos were found to have greater unfavorable changes in metabolic
parameters and body composition in response to ART initiation than either blacks or whites (Gibert et al., 2009). Also since some Latinos present late in the course of the HIV disease continuum, they are more likely to have OIs related to their countries of origin (Garland, 2010).
Standardization of the collection of data on race and ethnicity is important to permit the collection and sharing of this information across federal agencies and other bodies. In 1997, the Office of Management and Budget (OMB) issued revised minimum standards for the collection of race and ethnicity data, specifying five racial (American Indian or Alaska Native, Asian, black or African American, Native Hawaiian or other Pacific Islander, and white) and two ethnic (Hispanic or Latino; not Hispanic or Latino) categories in an effort to increase standardization of race and ethnicity data in administrative reporting and statistical activities within federal agencies (OMB, 1977, 1997b). In addition, OMB encourages the collection of more granular data on ethnicity when they can be aggregated back to the minimum categories (OMB, 1997a). This effort has improved the collection of such data within many health information systems, but not all nonfederal data collection activities use these categories (IOM, 2009) or even require the collection of data on race and ethnicity. In addition, there may be differences in the way these data are collected. For example, race may be collected by providers based on their observations, which can differ from a patient’s description of his or her race. Furthermore, OMB does not specify standardized collection of more granular data, for example, pertaining to country of origin, which is important for clinical decision making and nuanced monitoring of health disparities.
In response to Section 4302 of the ACA, new HHS guidance on data collection standards for race, ethnicity, sex, primary language, and disability status, effective October 31, 2011, set minimum standards for the collection of such data in population-based health surveys conducted or sponsored by HHS (HHS, 2011g). The HHS data standards mandate the collection of more granular data on race and ethnicity as specified in the guidance, as well as the collection of data on “biologic sex” and English proficiency as a measure of primary language. The guidance also recommends the wording for collection of data on the specific language spoken at home should an agency wish to collect such data.12
HHS is also in the process of developing a national progression plan to integrate the collection of data on sexual orientation and gender identity into its national surveys (HHS, 2011c,g) and to collect data on socioeconomic status. Collection of standardized demographic data on gender
__________________
12The guidance includes a data standard for the collection of disability status, which might apply to PLWHA in cases when the disease process results in one or more of the disabling conditions specified.
identity and sexual orientation is important to track access to, and quality of, HIV care among sexual minority subpopulations of PLWHA—for example, by estimating the proportion of gay and bisexual men with an undetectable viral load as specified in the NHAS (ONAP, 2010, p. 31). A 2011 IOM report assessing the current state of knowledge about the health of lesbian, gay, bisexual, and transgender people provides working definitions of gender identity and sexual orientation (IOM, 2011a, pp. 25-29). “Gender identity refers to a person’s basic sense of being a man or boy, a woman or girl, or another gender (e.g., transgender, bigender, or gender queer—a rejection of the traditional binary classification of gender)” (IOM, 2011a, p. 25). “[S]exual orientation refers to an enduring pattern of or disposition to experience sexual or romantic desires for, and relationships with, people of one’s same sex, the other sex, or both sexes” (i.e., homosexual, heterosexual, bisexual) (IOM, 2011a, p. 27). Although useful and important, these categories will not capture the group of MSM who do not self-identify as homosexual or bisexual or gender different. For this reason, the collection of data on sex of sexual partner(s) is also important.
Minimizing the burden of data collection is an important consideration, but it must be balanced against the importance of the information for clinical decision making and the evaluation and monitoring of treatment and care, which may differ in quality based on many of the aforementioned demographic data elements. The committee supports the HHS efforts to increase the scope and granularity of demographic data collected in national population-based health surveys and recommends that the expanded data collection standards be extended to all HHS-sponsored data collection activities to the extent practicable.
Although OMB and HHS standards apply to federal data collection, private health insurance plans vary in their collection of these data. KP, discussed in more detail in Chapter 3, collects data on race and ethnicity and sexual orientation. Although the data are incomplete, KP is actively working to complete the missing data (KP response to IOM request for information, March 30, 2011). The Ingenix Normative Health Information Database®, which includes claims from private commercial insurance plans, self-funded employer group health plans, and Medicare Advantage plans, also contains data on race and ethnicity, but the data are incomplete. These data are available for 50 to 94 percent of private commercial and self-funded employer group beneficiaries, depending on plan, but no information on race and ethnicity is available for Medicare Advantage plans. Ingenix does not capture data on sexual orientation (Ingenix response to IOM request for information, April 27, 2011). The HealthCore Integrated Research Database (HIRD®), which includes longitudinal administrative claims data representing commercially insured members of 15 Blue Cross Blue Shield health plans across the United States, does not contain data on
race and ethnicity or sexual orientation. Although the HIV/AIDS epidemic has disproportionately affected traditionally disadvantaged and vulnerable populations, who are generally covered by public insurance, the reduction in work disability with the advent of ART makes employer-based insurance an increasingly relevant source of information on PLWHA. As such, the routine collection of standardized data on race and ethnicity, as well as sexual orientation and gender identity, by private insurers would facilitate their usefulness for tracking changes in access to and the provision of HIV care.
Core Indicators for Clinical HIV Care
The data elements required to assess the core indicators for clinical HIV care are date of HIV diagnosis, date of first visit for HIV care, dates of subsequent routine HIV care visits, dates and results of ongoing CD4 and viral load tests, date of diagnosis of AIDS or AIDS-defining condition (if applicable), dates of ART initiation and ongoing prescription or dispensing of drugs, and date of death. Most of these data are available through surveillance or claims data systems, although some clinical data might have to be obtained from patient medical records.
The date of first visit for HIV care may be difficult to obtain. Claims data capture office visits for HIV care if they are coded as such, but data sources generally only capture the date an individual was first seen for HIV care within a given system, not the first-ever date of HIV care (see Chapter 3 for additional discussion). Individuals’ medical records may contain the approximate date of first HIV care, but the information is apt to be incomplete, and the process of mining it is time consuming.
The date of first CD4 and viral load tests may be used as a proxy for the date of first visit for HIV care. One difficulty with this approach arises when the tests are not recorded on the same date that the first appointment occurred. For the purpose of measuring linkage to care, however, the difference of a day or two between the date of the first visit and the test date is seldom important. A more significant problem occurs when the tests are ordered at the time of diagnosis. In this case, the first CD4 or viral load test date is less likely to reflect linkage to care. Although the date of first visit for HIV, as well as lab test dates, can be obtained from claims data, the lab test dates also are available from surveillance data, which may make them preferable since most of the other data elements required to assess the core indicators can be obtained from surveillance data as well (see Chapter 3).
As indicated in Chapter 3, a number of data systems collect information for a specified reporting period. In such cases, yes/no documentation of CD4 or viral load tests, use of ART, or diagnosis of AIDS within the reporting period can be used if specific test, prescription, or diagnosis dates
are not available. Documentation of CD4 or viral load tests also may serve as a proxy for HIV care visits to indicate continuity of care.
Outside of medical records, in particular EHRs, obtaining data on ART initiation is challenging, because it requires linking evidence of ART prescription or dispensing with CD4 test results. When specific dates for CD4 counts and ART prescription or dispensing are not available, some combination of results using the most recent CD4 test within the reporting period and yes/no documentation of whether the individual is on ART within the reporting period can be used.
Additional Indicators for Clinical HIV Care
Assessment of the additional indicators for HIV care requires a number of the same data elements needed to assess the core HIV care indicators: date of HIV diagnosis, CD4 test results at diagnosis or first visit for HIV care, date of ART initiation, and dates of ART prescription or dispensing. Data elements that are specific to the additional HIV care indicators include dates and results of TB tests; dates of chlamydia, gonorrhea, and syphilis screenings; date of hepatitis B screening or date of documented immunity; dates of hepatitis C tests; dates of influenza immunizations; date of pneumococcal immunization; and date of hepatitis B vaccination or date of documented immunity. Test or screening and immunization dates (or a close proxy) may be obtained from either clinical or claims databases. The information needed is documented evidence that the specified screenings and immunizations took place after HIV diagnosis and, where relevant, at the appropriate intervals. Clinical data on TB test results and documentation of hepatitis B immunity would have to be obtained from medical records or, in the case of TB, possible linkage with public health surveillance systems.
Other data elements needed to assess additional indicators relating to ART include dates of drug resistance testing, diagnosis or test results for HIV-related nephropathy, and pregnancy test results (or documentation of pregnancy). Dates or evidence of drug resistance testing may be obtained from claims databases, but diagnosis of nephropathy and documentation of pregnancy are not available from claims data. Yes/no documentation of these conditions may be obtained from other administrative data systems, as well as from EHRs or other medical records. Evidence of concurrent ART usage is needed as well to evaluate the relevant indicators.
Core Indicators for Mental Health, Substance Abuse, and Supportive Services
Data elements for assessing the core indicators for mental health and substance abuse include dates of mental health screening, as well as dates
of diagnosis or referral and first visit for mental health services, and the equivalent dates for substance abuse screening, referral, and first visit for services. Referral dates for mental health and substance use disorders are not readily available outside of EHRs and other medical records, and dates of first treatment may be difficult to acquire because individuals may be referred to outside providers or the services may be “carved out” (i.e., fee-for-service, provided by a different managed care plan than the rest of the individual’s medical care, or paid out of pocket). Suitable proxies for estimating the relevant indicators include evidence of assessment for mental health or substance abuse disorders and any visits for treatment services during the same reporting period. Pharmacy data showing evidence of prescriptions relevant to the treatment of mental health or substance abuse disorders also may serve as a proxy for receipt of care for these conditions. As discussed in Chapter 4, privacy laws may pose particular challenges for obtaining data to estimate the core indicators for access to mental health and substance abuse services.
Data elements for assessing the core indicators for supportive services include housing and food security status (e.g., as previously defined) and need for transportation services to access medical care and related services. Obtaining data to estimate the indicators for supportive services is particularly challenging since most data systems related to HIV care do not capture this type of data and have no reporting requirement in these areas. Evidence of reported need for (or access to) housing, food, or transportation assistance during the reporting period can be used if information about housing instability, food insecurity, or unmet transportation need is not available. Surveys are promising vehicles for obtaining data to estimate the supportive services indicators.
Additional Indicators for Mental Health, Substance Abuse, and Supportive Services
The additional indicators pertaining to mental health, substance abuse, and supportive services for housing, food, and transportation assistance involve documentation of assessment of need for relevant treatment or supportive services. If assessment dates are not available, then yes/no documentation of assessment (e.g., within a specified reporting period) would be a suitable proxy.
Additional Data Elements of Interest
As previously noted, the committee identified several data elements that reflect important aspects of the care experiences of PLWHA but are not required to estimate the indicators related to continuous HIV care and ac-
cess to supportive services. These additional data elements include access to dental care, emergency department or inpatient use, sexual risk behaviors, and partner HIV status (see Appendix Table 3-2f).
Other data elements pertain to individuals’ experience of discrimination or stigma as PLWHA (Sengupta et al., 2011), individuals’ level of satisfaction with their HIV care experience, and individuals’ assessment of their health-related quality of life (HHS, 2011a,b). Such experiences are important to the success of treatment and health outcomes of PLWHA, since they can affect the willingness of individuals to enter and remain in care and adhere to ART (see, e.g., Valdiserri, 2002). They also may affect individuals’ mental state and the likelihood that they will initiate or continue substance use (Mays and Cochran, 2001).
Stigma and discrimination, along with numerous other factors (e.g., housing instability, food insecurity), are major sources of chronic stress, which can precipitate or exacerbate mental health and substance use disorders. Stress also can compromise immunological functioning and may alter the progression of HIV disease. Studies of HIV samples have confirmed the relevance of stress-influenced biomarkers in physiological mechanisms of HIV (Glover et al., 2010; Kopnisky et al., 2004; Kumar et al., 2003). For example, norepinephrine, a neurotransmitter of the autonomic nervous system released in response to stress, has been shown to accelerate HIV replication (Chipimo et al., 2011; Cole, 2008; Miles et al., 2011).
The NHAS highlights HIV stigma and discrimination, calling for a reduction of stigma and discrimination against PLWHA as one of its action steps (ONAP, 2010, p. 35). Data on subjective experiences such as these are difficult to quantify objectively, however, which complicates the collection and meaningful application of data in these areas. Surveys and interviews can be particularly effective collection tools for this type of data, which can be used to supplement data obtained from clinical and administrative sources.
CONCLUSIONS AND RECOMMENDATIONS
• Measures of continuous HIV care as well as access to and quality of care can be monitored by a limited number of core indicators. Primary challenges to optimal outcomes for PLWHA include late diagnosis, delayed linkage to care for HIV, poor retention in care, delayed initiation of ART, and poor adherence to ART (i.e., discontinuing or intermittent ART), as well as untreated non-HIV comorbidities and unmet basic needs. Core indicators can measure the extent to which these challenges are being addressed across the
care continuum and can be used to gauge the impact of the NHAS and the ACA in improving HIV/AIDS care in the United States.
Recommendation 2-1. The Department of Health and Human Services should use the following core indicators13 to assess the impact of the National HIV/AIDS Strategy and the Patient Protection and Affordable Care Act on improving HIV/AIDS care and access to supportive services for individuals with HIV:
Core Indicators for Clinical HIV Care
Proportion of people newly diagnosed with HIV with a CD4+ cell count >200 cells/mm3 and without a clinical diagnosis of AIDS
Proportion of people newly diagnosed with HIV who are linked to clinical care for HIV within 3 months of diagnosis
Proportion of people with diagnosed HIV infection who are in continuous care (two or more visits for routine HIV medical care in the preceding 12 months at least 3 months apart)
Proportion of people with diagnosed HIV infection who received two or more CD4 tests in the preceding 12 months
Proportion of people with diagnosed HIV infection who received two or more viral load tests in the preceding 12 months
Proportion of people with diagnosed HIV infection in continuous care for 12 or more months and with a CD4+ cell count ≥350 cells/mm3
Proportion of people with diagnosed HIV infection and a measured CD4+ cell count <500 cells/mm3 who are not on ART
Proportion of people with diagnosed HIV infection who have been on ART for 12 or more months and have a viral load below the level of detection
All-cause mortality rate among people diagnosed with HIV infection
__________________
13The rationale for each of the indicators is summarized in Appendix Table 2-1.
Core Indicators for Mental Health, Substance Abuse, and Supportive Services
Proportion of people with diagnosed HIV infection and mental health disorder who are referred for mental health services and receive these services within 60 days14
Proportion of people with diagnosed HIV infection and substance use disorder who are referred for substance abuse services and receive these services within 60 days15
Proportion of people with diagnosed HIV infection who were homeless or temporarily or unstably housed at least once in the preceding 12 months
Proportion of people with diagnosed HIV infection who experienced food or nutrition insecurity at least once in the preceding 12 months
Proportion of people with diagnosed HIV infection who had an unmet need for transportation services to facilitate access to medical care and related services at least once in the preceding 12 months
• The differences among clinical, claims, and other types of data can result in gaps in measures for HIV care. Both clinical and claims data are needed to provide a complete picture of the quality of HIV care. Data from surveys and interviews can fill additional data gaps by providing information on hard-to-reach populations, such as homeless individuals and PLWHA who are not in care, and permitting collection of data not routinely collected by health care providers, such as need for and access to supportive services, and data on subjective experiences, such as HIV stigma and discrimination. Various types of data are needed to estimate the core indicators related to continuous, quality HIV care and access to mental health, substance abuse, and supportive services for people living with HIV, and hence to assess the impact of NHAS and ACA on improving HIV/AIDS care.
• Demographic data are essential to fully understanding HIV care challenges especially among groups disproportionately affected
__________________
14Receipt of care within 30 days would reflect optimal care, but 60 days is more realistic given the current limited capacity of many providers to see new patients within a shorter time frame. Urgent cases should be seen as soon as possible.
15See footnote 14.
by the HIV epidemic. Many of these crucial data elements, such as gender identity, sexual orientation, sexual risk behaviors, geographic marker of residence, income, primary means of reimbursement for medical services, and level of acculturation as reflected in primary language, are not routinely collected. Other data elements such as race and ethnicity often are not collected with a sufficient level of detail to make nuanced distinctions among the health needs of different racial and ethnic groups. New HHS guidance, effective October 31, 2011, on minimum data collection standards for race, ethnicity, sex, primary language, and disability status mandates the collection of more granular data on race and ethnicity, as well as the collection of data on “biologic sex” and English proficiency as a measure of primary language. These standards apply to all national population health surveys sponsored or conducted by HHS. HHS is also in the process of developing a national progression plan to integrate the collection of data on sexual orientation and gender identity into HHS national surveys and to collect data on socioeconomic status.
Recommendation 2-2. The Department of Health and Human Services and the Office of Management and Budget should continue to expand the demographic data elements to be captured by federal data systems relevant to HIV care to permit calculation of the indicators for subgroups of the population of people with diagnosed HIV infection, including, but not limited to, the following:
Age
Race
Ethnicity
Sex (assigned at birth)
Gender identity (e.g., male, female, transgender [male-to-female, female-to-male], bigender, gender queer)
Sexual orientation (e.g., heterosexual, homosexual, bisexual)
Current geographic marker of residence (e.g., current address, zip code, partial zip code, census block)
Income or poverty level
Primary means of reimbursement for medical services (including Medicaid, Medicare, Ryan White HIV/AIDS Program, private insurance or health maintenance organization, no coverage)
In addition, HHS should, to the extent practicable, extend its expanded data collection standards beyond national population-based health surveys to all HHS-sponsored data collection activities.
Aberg, J. A., J. E. Kaplan, H. Libman, P. Emmanuel, J. R. Anderson, V. E. Stone, J. M. Oleske, J. S. Currier, and J. E. Gallant. 2009. Primary care guidelines for the management of persons infected with human immunodeficiency virus: 2009 update by the HIV Medicine Association of the Infectious Diseases Society of America. Clinical Infectious Diseases 49(5):651-681.
AETC (AIDS Education and Training Centers). 2011. HIV-Associated Dementia and Other Neurocognitive Disorders. http://www.aidsetc.org/aidsetc?page=cg-802_dementia (accessed December 16, 2011).
Agwu, A. L., J. A. Fleishman, P. T. Korthuis, G. K. Siberry, J. M. Ellen, A. H. Gaur, R. Rutstein, and K. A. Gebo. 2011. Disparities in antiretroviral treatment: A comparison of behaviorally-HIV-infected youth and adults in the HIV Research Network. Journal of Acquired Immune Deficiency Syndromes 58(1):100-107.
Aidala, A. A., G. Lee, D. M. Abramson, P. Messeri, and A. Siegler. 2007. Housing need, housing assistance, and connection to HIV medical care. AIDS and Behavior 11(6 Suppl):101-115.
Amico, K. R. 2011. Standard of care for antiretroviral therapy adherence and retention in care from the perspective of care providers attending the 5th International Conference on HIV Treatment Adherence. Journal of the International Association of Physicians in AIDS Care 10(5):291-296.
Andersen, M., E. Hockman, G. Smereck, J. Tinsley, D. Milfort, R. Wilcox, T. Smith, C. Connelly, L. Adams, and R. Thomas. 2007. Retaining women in HIV medical care. Journal of the Association of Nurses in AIDS Care 18(3):33-41.
Anderson, S. A. 1990. Core indicators of nutritional state for difficult to sample populations. Journal of Nutrition 120:1557S-1600S.
Anema, A., N. Vogenthaler, E. A. Frongillo, S. Kadiyala, and S. D. Weiser. 2009. Food insecurity and HIV/AIDS: Current knowledge, gaps, and research priorities. Current HIV/AIDS Reports 6(4):224-231.
Arcury, T. A., J. S. Preisser, W. M. Gesler, and J. M. Powers. 2005. Access to transportation and health care utilization in a rural region. Journal of Rural Health 21(1):31-38.
Ashman, J. J., R. Conviser, and M. B. Pounds. 2002. Associations between HIV-positive individuals’ receipt of ancillary services and medical care receipt and retention. AIDS Care 14(Suppl 1):S109-S118.
Aziz, M., and K. Y. Smith. 2011. Challenges and successes in linking HIV-infected women to care in the United States. Clinical Infectious Diseases 52(Suppl 2):S231-S237.
Babor, T. F., B. G. McRee, P. A. Kassebaum, P. L. Grimaldi, K. Ahmed, and J. Bray. 2007. Screening, brief intervention, and referral to treatment (SBIRT): Toward a public health approach to the management of substance abuse. Substance Abuse 28(3):7-30.
Baicker, K., A. Chandra, J. S. Skinner, and J. E. Wennberg. 2004. Who you are and where you live: How race and geography affect the treatment of Medicare beneficiaries. Health Affairs (Suppl Variation, October):VAR33-44, doi: 10.1377/hlthaff.var.33.
Baldwin, L., S. H. Taplin, H. Friedman, and R. Moe. 2004. Access to multidisciplinary cancer care: Is it linked to the use of breast-conserving surgery with radiation for early-stage breast carcinoma? American Cancer Society 100(4):701-709.
Bisson, G., R. Gross, V. Miller, I. Weller, A. Walker, on behalf of the Writing Group. 2003. Monitoring of long-term toxicities of HIV treatments: An international perspective. AIDS 17(17):2407-2417.
Bogart, L. M., G. Wagner, F. H. Galvan, and D. Banks. 2010. Conspiracy beliefs about HIV are related to antiretroviral treatment nonadherence among African American men with HIV. Journal of Acquired Immune Deficiency Syndromes 53(5):648-655.
Bozzette, S. A., B. Phillips, S. Asch, A. L. Gifford, L. Lenert, T. Menke, E. Ortiz, D. Owens, and L. Deyton. 2000. Quality Enhancement Research Initiative for human immunodeficiency virus/acquired immunodeficiency syndrome: Framework and plan. HIV-QUERI executive committee. Medical Care 38(6 Suppl 1):I60-I69.
Branson, B. M., H. H. Handsfield, M. A. Lampe, R. S. Janssen, A. W. Taylor, S. B. Lyss, and J. E. Clark. 2006. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. Morbidity and Mortality Weekly Report 55(RR14):1-17.
Brantley, R. K., K. R. Williams, T. M. Silva, M. Sistrom, N. M. Thielman, H. Ward, A. A. Lima, and R. L. Guerrant. 2003. AIDS-associated diarrhea and wasting in northeast Brazil is associated with subtherapeutic plasma levels of antiretroviral medications and with both bovine and human subtypes of Cryptosporidium parvum. Brazilian Journal Infectious Diseases 7(1):16-22.
Brion, J. M., C. D. Rose, P. K. Nicholas, R. Sloane, I. B. Corless, T. G. Lindgren, D. J. Wantland, J. K. Kemppainen, E. F. Sefcik, K. M. Nokes, K. M. Kirksey, L. Eller, M. J. Hamilton, W. L. Holzemer, C. J. Portillo, M. R. Mendez, L. M. Robinson, S. Moezzi, M. Rosa, S. Human, M. Maryland, J. Arudo, A. V. Ros, T. P. Nicholas, Y. Cuca, E. Huang, C. Bain, L. Tyer-Viola, S. M. Zang, M. Shannon, A. Peters-Lewis, and S. Willard. 2011. Unhealthy substance-use behaviors as symptom-related self-care in persons with HIV/AIDS. Nursing & Health Sciences 13(1):16-26.
Burks, D. J., R. Robbins, and J. P. Durtschi. 2011. American Indian gay, bisexual and two-spirit men: A rapid assessment of HIV/AIDS risk factors, barriers to prevention and culturally-sensitive intervention. Culture, Health & Sexuality 13(3):283-298.
Bushen, O. Y., J. A. Davenport, A. B. Lima, S. C. Piscitelli, A. J. Uzgiris, T. M. Silva, R. Leite, M. Kosek, R. A. Dillingham, A. Girao, A. A. Lima, and R. L. Guerrant. 2004. Diarrhea and reduced levels of antiretroviral drugs: Improvement with glutamine or alanyl-glutamine in a randomized controlled trial in northeast Brazil. Clinical Infectious Diseases 38(12):1764-1770.
Campa, A., Z. Yang, S. Lai, L. Xue, J. C. Phillips, S. Sales, J. B. Page, and M. K. Baum. 2005. HIV-related wasting in HIV-infected drug users in the era of highly active antiretroviral therapy. Clinical Infectious Diseases 41(8):1179-1185.
Campsmith, M. L., P. H. Rhodes, H. I. Hall, and T. A. Green. 2010. Undiagnosed HIV prevalence among adults and adolescents in the United States at the end of 2006. Journal of Acquired Immune Deficiency Syndromes 53(5):619-624.
Candiani, T. M., J. Pinto, C. A. Cardoso, I. R. Carvalho, A. C. Dias, M. Carneiro, and E. A. Goulart. 2007. Impact of highly active antiretroviral therapy (HAART) on the incidence of opportunistic infections, hospitalizations and mortality among children and adolescents living with HIV/AIDS in Belo Horizonte, Minas Gerais State, Brazil. Cadernos de Saude Publica 23(Suppl 3):S414-S423.
Carrico, A. W. 2011. Substance use and HIV disease progression in the HAART era: Implications for the primary prevention of HIV. Life Sciences 88(21-22):940-947.
Castilla, J., P. Sobrino, L. De La Fuente, I. Noguer, L. Guerra, and F. Parras. 2002. Late diagnosis of HIV infection in the era of highly active antiretroviral therapy: Consequences for AIDS incidence. AIDS 16(14):1945-1951.
CDC (Centers for Disease Control and Prevention). 2006. Achievements in public health: Reduction in perinatal transmission of HIV infection—United States, 1985-2005. Morbidity and Mortality Weekly Report 55(21):592-597.
CDC. 2007. Goals and objectives of the CDC HIV Prevention Strategic Plan: Extended through 2010. http://www.cdc.gov/hiv/resources/reports/psp/pdf/psp.pdf (accessed December 19, 2011).
CDC. 2009. Late HIV testing—34 states, 1996. Morbidity and Mortality Weekly Report 58(24):661-665.
CDC. 2010a. HIV Infection Reporting. http://www.cdc.gov/hiv/topics/surveillance/reporting.htm (accessed January 6, 2012).
CDC. 2010b. Sexually transmitted diseases treatment guidelines, 2010. Morbidity and Mortality Weekly Report 59(RR12):1-110.
CDC. 2011a. HIV in the United States. http://www.cdc.gov/hiv/resources/factsheets/PDF/us.pdf (accessed December 20, 2011).
CDC. 2011b. HIV surveillance—United States, 1981-2008. Morbidity and Mortality Weekly Report 60(21):689-729.
CDC. 2011c. Vital signs: HIV prevention through care and treatment—United States. Morbidity and Mortality Weekly Report 60(47):1618-1623.
CDC. 2012. Diagnoses of HIV infection and AIDS in the United States and dependent areas, 2010. HIV Surveillance Report. Volume 22. http://www.cdc.gov/hiv/surveillance/resources/reports/2010report/index.htm (accessed March 21, 2012).
CHAIN (Community Health Advisory & Information Network) Fact Sheet. 2004. Factors Associated with Delayed Care Seeking among HIV-Infected Individuals in New York City. http://www.nyhiv.com/pdfs/Delayed%20Entry%20Fact%20Sheet_v7.pdf (accessed December 15, 2011).
Chapple, I. L. C., and J. Hamburger. 2000. The significance of oral health in HIV disease. Sexually Transmitted Infections 76(4):236-243.
Charlebois, E. D., M. Das, T. C. Porco, and D. V. Havlir. 2011. The effect of expanded antiretroviral treatment strategies on the HIV epidemic among men who have sex with men in San Francisco. Clinical Infectious Diseases 52(8):1046-1049.
Cheever, L. W. 2007. Engaging HIV-infected patients in care: Their lives depend on it. Clinical Infectious Diseases 44(11):1500-1502.
Chen, N., E. Erbelding, H. C. Yeh, and K. Page. 2010. Predictors of HIV testing among Latinos in Baltimore City. Journal of Immigrant and Minority Health 12(6):867-874.
Chin, J. J., M. Botsko, E. Behar, and R. Finkelstein. 2009. More than ancillary: HIV social services, intermediate outcomes and quality of life. AIDS Care 21(10):1289-1297.
Chipimo, P., M. Tuba, and K. Fylkesnes. 2011. Conceptual models for mental distress among HIV-infected and uninfected individuals: A contribution to clinical practice and research in primary-health-care centers in Zambia. BMC Health Services Research 11(January):7 (12 pages).
Clements-Nolle, K., R. Marx, M. Pendo, E. Loughran, M. Estes, and M. Katz. 2008. Highly active antiretroviral therapy use and HIV transmission risk behaviors among individuals who are HIV infected and were recently released from jail. American Journal of Public Health 98(4):661-666.
Cohen, M. S., Y. Q. Chen, M. McCauley, T. Gamble, M. C. Hosseinipour, N. Kumarasamy, J. G. Hakim, J. Kumwenda, B. Grinsztein, J. H. S. Pilotto, S. V. Godbole, S. Mehendale, S. Charjvalertsak, B. R. Santos, K. H. Mayer, I. F. Hoffman, S. H. Eshelman, E. Piwowar-Manning, L. Wang, J. Makhema, L. A. Mills, G. de Bruyn, I. Sanne, J. Eron, J. Gallant, D. Havlir, S. Swindells, H. Ribaudo, V. Elharrar, D. Burns, T. E. Taha, K. Nielsen-Saines, D. Celentano, M. Essex, and T. R. Fleming. 2011. Prevention of HIV-1 infection with early antiretroviral therapy. New England Journal of Medicine 365:493-505.
Cohn, S.E., M. L. Berk, S. H. Berry, N. Duan, M. R. Frankel, J. D. Klein, M. M. McKinney, A. Rastegar, S. Smith, M. F. Shapiro, and S. A. Bozzette. 2001. The care of HIV-infected adults in rural areas of the United States. Journal of Acquired Immune Deficiency Syndromes 28(4):385-392.
Cole, S. W. 2008. Psychosocial influences on HIV-1 disease progression: Neural, endocrine, and virologic mechanisms. Psychosomatic Medicine 70(5):562-568.
Conover, C. J., and K. Whetten-Goldstein. 2002. The impact of ancillary services on primary care use and outcomes for HIV/AIDS patients with public insurance coverage. AIDS Care 14(Suppl 1):S59-S71.
Conviser, R. 2007. Catalyzing system changes to make HIV care more accessible. Journal of Health Care for the Poor and Underserved 18(3 Suppl):224-243.
Conviser, R., and M. B. Pounds. 2002a. Background for the studies on ancillary services and primary care use. AIDS Care 14(Suppl 1):S7-S14.
Conviser, R., and M. B. Pounds. 2002b. The role of ancillary services in client-centred systems of care. AIDS Care 14(Suppl 1):S119-S131.
Cook, J. A., J. K. Burke-Miller, M. H. Cohen, R. L. Cook, D. Vlahov, T. E. Wilson, E. T. Golub, R. M. Schwartz, A. A. Howard, C. Ponath, M. W. Plankey, A. M. Levine, and D. D. Grey. 2008. Crack cocaine, disease progression, and mortality in a multicenter cohort of HIV-1 positive women. AIDS 22(11):1355-1363.
Cooper-Patrick, L., J. J. Gallo, J. J. Gonzales, H. T. Vu, N. R. Powe, C. Nelson, and D. E. Ford. 1999. Race, gender, and partnership in the patient-physician relationship. Journal of the American Medical Association 282(6):583-589.
Cooperman, N. A., M. Heo, K. M. Berg, X. Li, A. H. Litwin, S. Nahvib, and J. H. Arnsten. 2012. Impact of adherence counseling dose on antiretroviral adherence and HIV viral load among HIV-infected methadone maintained drug users. AIDS Care:1-8. DOI:10.1080/09540121.2011.644231.
Coulter, I. D., K. C. Heslin, M. Marcus, R. D. Hays, J. Freed, C. Der-Martirosian, N. Guzmán-Becerra, W. E. Cunningham, R. M. Andersen, and M. F. Shapiro. 2002. Associations of self-reported oral health with physical and mental health in a nationally representative sample of HIV persons receiving medical care. Quality of Life Research 11(1):57-70.
Crepaz, N., and G. Marks. 2002. Towards an understanding of sexual risk behavior in people living with HIV: A review of social, psychological, and medical findings. AIDS 16(2):135-139.
Crepaz, N., C. M. Lyles, R. J. Wolitski, W. F. Passin, S. M. Rama, J. H. Herbst, D. W. Purcell, R. M. Malow, and R. Stall, for the HIV/AIDS Prevention Research Synthesis (PRS) Team. 2006. Do prevention interventions reduce HIV risk behaviours among people living with HIV? A meta-analytic review of controlled trials. AIDS 20(2):143-157.
Cunningham, W. E., R. M. Andersen, M. H. Katz, M. D. Stein, B. J. Turner, S. Crystal, S. Zierler, K. Kuromiya, S. C. Morton, P. St. Clair, S. A. Bozzette, and M. F. Shapiro. 1999. The impact of competing subsistence needs and barriers on access to medical care for persons with human immunodeficiency virus receiving care in the United States. Medical Care 37(12):1270-1281.
Das, M. 2011. Intensifying HIV Prevention in the Communities Where HIV Is Most Heavily Concentrated. PowerPoint presentation at the 2011 National HIV Prevention Conference, Atlanta, GA, August 15.
de Bruin, M., W. Viechtbauer, H. P. Schaalma, G. Kok, C. Abraham, and H. J. Hospers. 2010. Standard care impact on effects of highly active antiretroviral therapy adherence interventions: A meta-analysis of randomized controlled trials. Archives of Internal Medicine 170(3):240-250.
Denning, P., and E. DiNenno. 2010. Communities in Crisis: Is There a Generalized HIV Epidemic in Impoverished Urban Areas in the United States? Abstract WEPDD101 XVIII International AIDS Conference, Vienna, Austria, July 18-23. http://www.cdc.gov/hiv/topics/surveillance/resources/other/pdf/poverty_poster.pdf (accessed January 9, 2012).
Dennis, A. M., S. Napravnik, A. C. Sena, and J. J. Eron. 2011. Late entry to HIV care among Latinos compared with non-Latinos in a southeastern U.S. cohort. Clinical Infectious Diseases 53(5):480-487.
Dillingham, R., P. Leger, C. A. Beauharnais, E. Miller, A. Kashuba, S. Jennings, K. Dupnik, A. Samie, E. Eyma, R. Guerrant, J. Pape, and D. Fitzgerald. 2011. AIDS diarrhea and antiretroviral drug concentrations: A matched-pair cohort study in Port au Prince, Haiti. American Journal of Tropical Medicine and Hygiene 84(6):878-882.
Doescher, M. P., B. G. Saver, K. Fiscella, and P. Franks. 2001. Racial/ethnic inequities in continuity and site of care: Location, location, location. Health Services Research 36(6 Pt 2):78-89.
Drug Strategies. 2000. Smart Steps: Treating Baltimore’s Drug Problem. http://www.drugstrategies.com/pdf/baltimore.pdf (accessed May 17, 2012).
Enriquez, M., R. Farnan, A. L. Cheng, A. Almeida, D. Del Valle, M. Pulido-Parra, and G. Flores. 2008. Impact of a bilingual/bicultural care team on HIV-related health outcomes. Journal of the Association of Nurses in AIDS Care 19(4):295-301.
ERS (Economic Research Service, U.S. Department of Agriculture). 2009. Food Security in the United States: Measuring Household Food Security. http://www.ers.usda.gov/Briefing/FoodSecurity/measurement.htm (accessed August 3, 2011).
ERS. 2011. Food Security in the United States: Definitions of Hunger and Food Security. http://www.ers.usda.gov/Briefing/FoodSecurity/labels.htm (accessed August 3, 2009).
Espinoza, L., H. I. Hall, R. M. Selik, and X. Hu. 2008. Characteristics of HIV infection among Hispanics, United States, 2003-2006. Journal of Acquired Immune Deficiency Syndromes 49(1):94-101.
Ettenhofer, M. L., C. H. Hinkin, S. A. Castellon, R. Durvasula, J. Ullman, M. Lam, H. Myers, M. J. Wright, and J. Foley. 2009. Aging, neurocognition, and medication adherence in HIV infection. American Journal of Geriatric Psychiatry 17(4):281-290.
Ferver, K., B. Burton, and P. Jesilow. 2009. The use of claims data in healthcare research. Open Public Health Journal 2:11-24.
Finkelstein, A., S. Taubman, B. J. Wright, M. Bernstein, J. Gruber, J. P. Newhouse, H. Allen, K. Baicker, and the Oregon Health Study Group. 2011. The Oregon Health Insurance Experiment: Evidence from the First Year. National Bureau of Economic Research, Working paper 17190. Cambridge, MA. http://www.nber.org/papers/w17190 (accessed January 6, 2012).
Friedmann, P. D., S. C. Lemon, M. D. Stein, and T. A. D’Aunno. 2003. Accessibility of addiction treatment: Results from a national survey of outpatient substance abuse treatment organizations. Health Services Research 38(3):887-903.
Gardner, E. M., M. P. McLees, J. F. Steiner, C. Del Rio, and W. J. Burman. 2011. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clinical Infectious Diseases 52(6):793-800.
Gardner, L. I, L. R. Metsch, P. Anderson-Mahoney, A. M. Loughlin, C. del Rio, S. Strathdee, S. L. Sansom, H. A. Siegal, A. E. Greenberg, S. D. Holmberg, and the Antiretroviral Treatment Access Study (ARTAS) Study Group. 2005. Efficacy of a brief case management intervention to link recently diagnosed HIV-infected persons to care. AIDS 19(4):423-431.
Garland, J. M., A. S. Andrade, and K. R. Page. 2010. Unique aspects of the care of HIV-positive Latino patients living in the United States. Current HIV/AIDS Reports 7(3):107-116.
Gavrilin, M. A., L. E. Mathes, and M. Podell. 2002. Methamphetamine enhances cell-associated feline immunodeficiency virus replication in astrocytes. Journal of Neurovirology 8(3):240-249.
Gaynes, B. N., A. J. Rush, M. H. Trivedi, S. R. Wisniewski, G. K. Balasubramani, D. C. Spencer, T. Petersen, M. Klinkman, D. Warden, L. Nicholas, and M. Fava. 2007. Major depression symptoms in primary care and psychiatric care settings: A cross-sectional analysis. Annals of Family Medicine 5(2):126-134.
Gebo, K. A., J. A. Fleishman, R. Conviser, E. D. Reilly, P. T. Korthuis, R. D. Moore, J. Hellinger, P. Keiser, H. R. Rubin, L. Crane, F. J. Hellinger, and W. C. Mathews. 2005. Racial and gender disparities in receipt of highly active antiretroviral therapy persist in a multistate sample of HIV patients in 2001. Journal of Acquired Immune Deficiency Syndromes 38(1):96-103.
Ghose, T., D. T. Swendeman, and S. M. George. 2011. The role of brothels in reducing HIV risk in Sonagachi, India. Qualitative Health Research 21(5):587-600.
Gibert, C. L., J. C. Shlay, S. Sharma, G. Bartsch, G. Peng, and C. Grunfeld, for the Terry Beirn Community Programs for Clinical Research on AIDS and the International Network for Strategic Initiatives in Global HIV Trials. 2009. Racial differences in changes of metabolic parameters and body composition in antiretroviral therapy-naive persons initiating antiretroviral therapy. Journal of Acquired Immune Deficiency Syndromes 50(1):44-53.
Giordano, T. P., A. L. Gifford, A. C. White, Jr., M. E. Suarez-Almazor, L. Rabeneck, C. Hartman, L. I. Backus, L. A. Mole, and R. O. Morgan. 2007. Retention in care: A challenge to survival with HIV infection. Clinical Infectious Diseases 44(11):1493-1499.
Glover, D. A., E. F. Garcia-Aracena, P. Lester, E. Rice, and M. J. Rothram-Borus. 2010. Stress biomarkers as outcomes for HIV+ prevention: Participation, feasibility and findings among HIV+ Latina and African American mothers. AIDS and Behavior 14(2):339-350.
Golin, C. E., H. Liu, R. D. Hays, L. G. Miller, C. K. Beck, J. Ickovics, A. H. Kaplan, and N. S. Wenger. 2002. A prospective study of predictors of adherence to combination antiretroviral medication. Journal of General Internal Medicine 17(10):756-765.
Goulet, J. L., S. L. Fultz, D. Rimland, A. Butt, C. Gibert, M. Rodriguez-Barradas, K. Bryant, and A. C. Justice. 2007. Aging and infectious diseases: Do patterns of comorbidity vary by HIV status, age, and HIV severity? Clinical Infectious Diseases 45(12):1593-1601.
Halkitis, P., J. Palamar, and P. Mukherjee. 2008. Analysis of HIV medication adherence in relation to person and treatment characteristics using hierarchical linear modeling. AIDS Patient Care and STDs 22(4):323-335.
Halkitis, P. N., S. A. Kupprat, and P. P. Mukherjee. 2010. Longitudinal associations between case management and supportive services use among black and Latina HIV-positive women in New York City. Journal of Women’s Health 9(1):99-108.
Hall, H. I., R. Song, P. Rhodes, J. Prejean, Q. An, L. M. Lee, J. Karon, R. Brookmeyer, E. H. Kaplan, M. T. McKenna, and R. S. Janssen. 2008. Estimation of HIV incidence in the United States. Journal of the American Medical Association 300(5):520-529.
Heckman, T. G., A. M. Somlai, J. Peters, J. Walker, L. Otto-Salaj, C. A. Galdabini, and J. A. Kelly. 1998. Barriers to care among persons living with HIV/AIDS in urban and rural areas. AIDS Care 10(3):365-375.
Henderson, K. C., J. Hindman, S. C. Johnson, R. J. Valuck, and J. J. Kiser. 2011. Assessing the effectiveness of pharmacy-based adherence interventions on antiretroviral adherence in persons with HIV. AIDS Patient Care and STDs 25(4):221-228.
Hendricks, K., and S. Gorbach. 2009. Nutrition issues in chronic drug users living with HIV infection. NIDA Addiction Science and Clinical Practice 5(1):16-23.
HHS (U.S. Department of Health and Human Services). 2009. Recommended Immunizations for HIV Positive Adults. http://www.aidsinfo.nih.gov/contentfiles/Recommended_Immunizations_FS_en.pdf (accessed January 6, 2012).
HHS. 2010. Healthy People 2020 Summary of Objectives. http://www.healthypeople.gov/2020/topicsobjectives2020/pdfs/HIV.pdf (accessed December 20, 2011).
HHS. 2011a. About Healthy People. http://www.healthypeople.gov/2020/about/default.aspx (accessed December 19, 2011).
HHS. 2011b. Health-Related Quality of Life and Well-Being. http://www.healthypeople.gov/2020/about/QoLWBabout.aspx (accessed December 7, 2011).
HHS. 2011c. Improving Data Collection for the LGBT Community. http://www.healthcare.gov/news/factsheets/2011/06/lgbt06292011a.html (accessed December 6, 2011).
HHS. 2011d. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents. October 14. http://aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL002534.pdf (accessed January 6, 2012).
HHS. 2011e. Panel on Antiretroviral Therapy and Medical Management of HIV-Infected Children. Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infection. National Institutes of Health. http://aidsinfo.nih.gov/contentfiles/PediatricGuidelines.pdf (accessed January 6, 2012).
HHS. 2011f. Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission. Recommendations for Use of Antiretroviral Drugs in Pregnant HIV-1-Infected Women for Maternal Health and Interventions to Reduce Perinatal HIV Transmission in the United States. http://aidsinfo.nih.gov/ContentFiles/PerinatalGL.pdf (accessed January 6, 2012).
HHS. 2011g. U.S. Department of Health and Human Services Implementation Guidance on Data Collection Standards for Race, Ethnicity, Sex, Primary Language, and Disability Status. http://aspe.hhs.gov/datacncl/standards/ACA/4302/index.pdf (accessed December 6, 2011).
HHS. 2012. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents. March 27. http://aidsinfo.nih.gov/contentfiles/lvguidelines/adultandadolescentgl.pdf (accessed May 18, 2012).
Hinkin, C. H., S. A. Castellon, R. S. Durvasula, D. J. Hardy, M. N. Lam, K. I. Mason, D. Thrasher, M. B. Goetz, and M. Stefaniak. 2002. Medication adherence among HIV+ adults: Effects of cognitive dysfunction and regimen complexity. Neurology 59(12): 1944-1950.
Horberg, M. A., M. J. Silverberg, L. B. Hurley, W. J. Towner, D. B. Klein, S. Bersoff-Matcha, W. G. Weinberg, D. Antoniskis, M. Mogyoros, W. T. Dodge, R. Dobrinich, C. P. Quesenberry, and D. A. Kovach. 2008. Effects of depression and selective serotonin reuptake inhibitor use on adherence to highly active antiretroviral therapy and on clinical outcomes in HIV-infected populations. Journal of Acquired Immune Deficiency Syndromes 47(3):384-390.
Horberg, M. A., J. A. Aberg, L. W. Cheever, P. Renner, E. O’Brien Kaleba, and S. M. Asch. 2010. Development of national and multiagency HIV care quality measures. Clinical Infectious Diseases 51(6):732-738.
Horberg, M., L. Hurley, W. Towner, R. Gambatese, D. Klein, D. Antoniskis, W. Weinberg, P. Kadlecik, C. Remmers, R. Dobrinich, C. Quesenberry, M. Silverberg, and M. Johnson. 2011. HIV quality performance measures in a large integrated health care system. AIDS Patient Care and STDs 25(1):21-28.
HRSA (Health Resources and Services Administration). 2009. New Strategies for Rural Care. HRSA Care Action (April). http://hab.hrsa.gov/newspublications/careactionnewsletter/april2009.pdf (accessed December 20, 2011).
HRSA. 2011a. HAB HIV Performance Measures. http://hab.hrsa.gov/deliverhivaidscare/habperformmeasures.html (accessed December 6, 2011).
HRSA. 2011b. HIVQUAL Continuous Quality Program. http://hab.hrsa.gov/deliverhivaidscare/hivqual.html (accessed December 6, 2011).
HUD (U.S. Department of Housing and Urban Development). 2010. Homeless Management Information System (HMIS) Data Standards, Revised Notice. Office of Community Planning and Development, March. http://www.hudhre.info/documents/FinalHMISDataStandards_March2010.pdf (accessed December 9, 2011).
Humeniuk, R., V. Dennington, and R. Ali. 2008. World Health Organization ASSIST Phase III Study Group. The Effectiveness of a Brief Intervention for Ilicit Drugs Linked to the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) in Primary Health Care Settings: A Technical Report of Phase III Findings of the WHO Assist Randomized Control Trial. Geneva, Switzerland: World Health Organization.
IOM (Institute of Medicine). 2004. Measuring What Matters: Allocation, Planning, and Quality Assessment for the Ryan White Care Act. Washington, DC: The National Academies Press.
IOM. 2009. Race, Ethnicity, and Language Data: Standardization for Health Care Quality Improvement. Washington, DC: The National Academies Press.
IOM. 2010. HIV Screening and Access to Care: Exploring Barriers and Facilitators to Expanded HIV Testing. Washington, DC: The National Academies Press.
IOM. 2011a. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: The National Academies Press. IOM. 2011b. HIV Screening and Access to Care: Exploring the Impact of Policies on Access to and Provision of HIV Care. Washington, DC: The National Academies Press.
IOM. 2011c. HIV Screening and Access to Care: Health Care System Capacity for Increased HIV Testing and Provision of Care. Washington, DC: The National Academies Press.
IOM. 2011d. Leading Health Indicators for Healthy People 2020. Washington, DC: The National Academies Press.
Johnson, R. L., D. Roter, N. R. Powe, and L. A. Cooper. 2004a. Patient race/ethnicity and quality of patient-physician communication during medical visits. American Journal of Public Health 94(12):2084-2090.
Johnson, R. L., S. Saha, J. J. Arbelaez, M. C. Beach, and L. A. Cooper. 2004b. Racial and ethnic differences in patient perceptions of bias and cultural competence in health care. Journal of General Internal Medicine 19(2):101-110.
Jollis, J. G., M. Ancukiewicz, E. R. DeLong, D. B. Pryor, L. H. Muhlbaier, and D. B. Mark. 1993. Discordance of databases designed for claims payment versus clinical information systems. Implications for outcomes research. Annals of Internal Medicine 119(8):844-850.
Justice, A. C. 2006. Prioritizing primary care in HIV: Comorbidity, toxicity, and demography. Topics in HIV Medicine 14(5):159-163.
Justice, A. C., K. A. McGinnis, J. H. Atkinson, R. K. Heaton, C. Young, J. Sadek, T. Madenwald, J. T. Becker, J. Conigliaro, S. T. Brown, D. Rimland, S. Crystal, and M. Simberkoff. 2004. Psychiatric and neurocognitive disorders among HIV-positive and negative veterans in care: Veterans aging cohort five-site study. AIDS 18(Suppl 1):S49-S59.
Kalichman, S. 2000. HIV transmission risk behaviors of men and women living with HIV-AIDS: Prevalence, predictors, and emerging clinical interventions. Clinical Psychology: Science and Practice 7(1):32-47.
Kalichman, S. C., C. Cherry, C. Amaral, D. White, M. O. Kalichman, H. Pope, C. Swetsze, M. Jones, and R. Macy. 2010. Health and treatment implications of food insufficiency among people living with HIV/AIDS, Atlanta, Georgia. Journal of Urban Health 87(4):631-641.
Kamb, M. L., M. Fishbein, J. M. Douglas, Jr., F. Rhodes, J. Rogers, G. Bolan, J. Zenilman, T. Hoxworth, C. K. Malotte, M. Iatesta, C. Kent, A. Lentz, S. Graziano, R. H. Byers, and T. A. Peterman, for the Project RESPECT Study Group. 1998. Efficacy of risk-reduction counseling to prevent human immunodeficiency virus and sexually transmitted diseases: A randomized controlled trial. Journal of the American Medical Association 280(13):1161-1167.
Kaplan, J. E., D. Hanson, M. S. Dworkin, T. Frederick, J. Bertolli, M. L. Lindegren, S. Holmberg, and J. L. Jones. 2000. Epidemiology of human immunodeficiency virus-associated opportunistic infections in the United States in the era of highly active antiretroviral therapy. Clinical Infectious Diseases 30(Suppl 1):S5-S14.
Kaplan, J. E., C. Benson, K. H. Holmes, J. T. Brooks, A. Pau, and H. Masur. 2009. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: Recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Morbidity and Mortality Weekly Report 58(RR-4):1-207.
Kass-Bartelmes, B. L. 2002. AHRQ Tools and Resources for Better Health Care. Agency for Healthcare Research Quality. http://www.ahrq.gov/qual/tools/toolsria.htm (accessed January 6, 2012).
Kates, J. 2011. Medicaid and HIV: A National Analysis. Washington, DC: Henry J. Kaiser Family Foundation. http://www.kff.org/hivaids/upload/8218.pdf (accessed January 11, 2012).
Kempf, M. C., J. McLeod, A. K. Boehme, M. W. Walcott, L. Wright, P. Seal, W. E. Norton, J. E. Schumacher, M. Mugavero, and L. Moneyham. 2010. A qualitative study of the barriers and facilitators to retention-in-care among HIV-positive women in the rural southeastern United States: Implications for targeted interventions. AIDS Patient Care STDS 24(8):515-20.
Kenagy, G. P., N. L. Linsk, D. Bruce, R. Warnecke, A. Gordon, F. Wagaw, and A. Densham. 2003. Service utilization, service barriers, and gender among HIV-positive consumers in primary care. AIDS Patient Care and STDs 17(5):235-244.
Kidder, D. P., R. J. Wolitski, S. Royal, A. Aidala, C. Courtenay-Quirk, D. R. Holtgrave, D. Harre, E. Sumartojo, and R. Stall. 2007. Access to housing as a structural intervention for homeless and unstably housed people living with HIV: Rationale, methods, and implementation of the housing and health study. AIDS and Behavior 11(6 Suppl):149-161.
Kitahata, M. 1996. Physicians’ experience and survival in patients with AIDS. New England Journal of Medicine 335(5):349-351.
Kitahata, M. M., S. E. Van Rompaey, and A. W. Shields. 2000. Physician experience in the care of HIV-infected persons is associated with earlier adoption of new antiretroviral therapy. Journal of Acquired Immune Deficiency Syndromes 24(2):106-114.
Kitahata, M. M., S. E. Van Rompaey, P. W. Dillingham, T. D. Koepsell, R. A. Deyo, W. Dodge, and E. H. Wagner. 2003. Primary care delivery is associated with greater physician experience and improved survival among persons with AIDS. Journal of General Internal Medicine 18(2):95-103.
Knowlton, A., J. Arnsten, L. Eldred, J. Wilkinson, M. Gourevitch, S. Shade, K. Dowling, and D. Purcell. 2006. Individual, interpersonal, and structural correlates of effective HAART use among urban active injection drug users. Journal of Acquired Immune Deficiency Syndromes 41(4):486-492.
Kopnisky, K. L., D. M. Stoff, and D. M. Rausch. 2004. Workshop report: The effects of psychological variables on the progression of HIV-1 disease. Brain, Behavior, and Immunity 18(3):246-261.
Korthuis, P. T., S. Saha, J. A. Fleishman, M. M. McGrath, J. S. Josephs, R. D. Moore, K. A. Gebo, J. Hellinger, and M. C. Beach. 2008. Impact of patient race on patient experiences of access and communication in HIV care. Journal of General Internal Medicine 23(12):2046-2052.
Kowal, J., J. R. Swenson, T. D. Aubry, H. D. Marchand, and C. Macphee. 2011. Improving access to acute mental health services in a general hospital. Journal of Mental Health 20(1):5-14.
Krawczyk, C. S., E. Funkhouser, J. M. Kilby, and S. H. Vermund. 2006a. Delayed access to HIV diagnosis and care: Special concerns for the southern United States. AIDS Care 18(Suppl 1):S35-S44.
Krawczyk, C. S., E. Funkhouser, J. M. Kilby, R. A. Kaslow, A. K. Bey, and S. H. Vermund. 2006b. Factors associated with delayed initiation of HIV medical care among infected persons attending a southern HIV/AIDS clinic. Southern Medical Journal 99(5):472-481.
Krieger, N. 1992. Overcoming the absence of socioeconomic data in medical records: Validation and application of a census-based methodology. American Journal of Public Health 82(5):703-710.
Kumar, V., and W. Encinosa. 2010. Effects of HIV medication complexity and depression on adherence to HIV medication. The Patient: Patient-Centered Outcomes Research 3(1):59-69.
Kumar, M., A. M. Kumar, D. Waldrop, M. H. Antoni, and C. Eisdorfer. 2003. HIV-1 infection and its impact on the HPA axis, cytokines, and cognition. Stress 6(3):167-172.
Landon, B. E., I. B. Wilson, K. McInnes, M. B. Landrum, L. R. Hirschhorn, P. V. Marsden, and P. D. Cleary. 2005. Physician specialization and the quality of care for human immunodeficiency virus infection. Archives of Internal Medicine 165(10):1133-1139.
Langford, D., A. Adame, A. Grigorian, I. Grant, J. A. McCutchan, R. J. Ellis, T. D. Marcotte, and E. Masliah. 2003. Patterns of selective neuronal damage in methamphetamine-user AIDS patients. Journal of Acquired Immune Deficiency Syndromes 34(5):467-474.
Lansky, A., A. Drake, and H. T. Pham. 2009. HIV-associated behaviors among injecting-drug users—23 cities, United States, May 2005-February 2006. Morbidity and Mortality Weekly Report 58(13):329-332. (Reprinted in JAMA 302[4]:376-377.)
Lawn, S. D., S. T. Butera, and T. M. Folks. 2001. Contribution of immune activation to the pathogenesis and transmission of human immunodeficiency virus type 1 infection. Clinical Microbiology Reviews 14(4):753-777.
Leaver, C. A., G. Bargh, J. R. Dunn, and S. W. Hwang. 2007. The effects of housing status on health-related outcomes in people living with HIV: A systematic review of the literature. AIDS and Behavior 11(6 Suppl):85-100.
Ledergerber, B., M. Egger, M. Opravil, A. Telenti, B. Hirschel, M. Battegay, P. Vernazza, P. Sudre, M. Flepp, H. Furrer, P. Francioli, and R. Weber. 1999. Clinical progression and virological failure on highly active antiretroviral therapy in HIV-1 patients: A prospective cohort study. Swiss HIV Cohort Study. Lancet 353(9156):863-868.
LeGrand, A., Y. Yomb, M. Bourrelly, N. Lorente, and A. NKom. 2010. MSM law in francophone Africa and the fight against AIDS: The hypocrisy of certain countries. HIV/AIDS Policy and Law Review 14(3):13-17.
Lieb, S., R. G. Brooks, R. S. Hopkins, D. Thompson, L. K. Crockett, T. Liberti, A. A. Jani, J. P. Nadler, V. M. Virkud, K. C. West, and G. McLaughlin. 2002. Predicting death from HIV/AIDS: A case-control study from Florida public HIV/AIDS clinics. Journal of Acquired Immune Deficiency Syndromes 30(3):351-358.
Littenberg, B., K. Strauss, C. D. MacLean, and A. R. Troy. 2006. The use of insulin declines as patients live farther from their source of care: Results of a survey of adults with type 2 diabetes. BMC Public Health 6 (July):198 (8 pages).
Litwin, A. H., I. Soloway, and M. N. Gourevitch. 2005. Integrating services for injection drug users infected with hepatitis C virus with methadone maintenance treatment: Challenges and opportunities. Clinical Infectious Diseases 40(Suppl 5):S339-S345.
Lo, W., T. MacGovern, and J. Bradford. 2002. Association of ancillary services with primary care utilization and retention for patients with HIV/AIDS. AIDS Care 14(Suppl 1): S45-S57.
Marks, G., L. I. Gardner, J. Craw, and N. Crepaz. 2010. Entry and retention in medical care among HIV-diagnosed persons: A meta-analysis. AIDS 24(17):2665-2678.
Marsden, P. V., and J. D. Wright, eds. 2010. Handbook of Survey Research, 2nd Edition. Bingley, UK: Emerald Group Publishing Limited.
Mays, V. M., and S. D. Cochran. 2001. Mental health correlates of perceived discrimination among lesbian, gay, and bisexual adults in the United States. American Journal of Public Health 91(11):1869-1876.
Mays, V. M., R. Maas, J. Ricks, and S. D. Cochran. 2011. HIV and African American women in the South: Employing a population-level HIV prevention and interventions. In Handbook of Health Psychology, Second Edition, edited by A. Baum, T. Revenson, and J. Singer. London: Psychology Press.
McMahon, J., C. Wanke, N. Terrin, S. Skinner, and T. Knox. 2011. Poverty, hunger, education, and residential status impact survival in HIV. AIDS Behavior 15(7):1503-1511.
Meditz, A. L., S. MaWhinney, A. Allshouse, W. Feser, M. Markowitz, S. Little, R. Hecht, E. S. Daar, A. C. Collier, J. Margolick, J. M. Kilby, J. P. Routy, B. Conway, J. Kaldor, J. Levy, R. Schooley, D. A. Cooper, M. Altfeld, D. Richman, and E. Connick. 2011. Sex, race, and geographic region influence clinical outcomes following primary HIV-1 infection. Journal of Infectious Diseases 203(4):442-451.
Messeri, P. A., D. M. Abramson, A. A. Aidala, F. Lee, and G. Lee. 2002. The impact of ancillary HIV services on engagement in medical care in New York City. AIDS Care 14(Suppl 1):S15-S29.
Miles, M. S., M. R. Isler, B. B. Banks, S. Sengupta, and G. Corbie-Smith. 2011. Silent endurance and profound loneliness: Socioemotional suffering in African Americans living with HIV in the rural south. Qualitative Health Research 21(4):489-501.
Milloy, M. J., T. Kerr, R. Zhang, M. Tyndall, J. Montaner, and E. Wood. 2010. Inability to access addiction treatment and risk of HIV infection among injection drug users recruited from a supervised injection facility. Journal of Public Health 32(3):342-349.
MoCA (Montreal Cognitive Assessment). 2011. The Montreal Cognitive Assessment. http://www.mocatest.org/ (accessed December 16, 2011).
Mugavero, M. J., C. Castellano, D. Edelman, and C. Hicks. 2007. Late diagnosis of HIV infection: The role of age and sex. American Journal of Medicine 120(4):370-373.
Mugavero, M. J., H. Y. Lin, J. H. Willig, A. O. Westfall, K. B. Ulett, J. S. Routman, S. Abroms, J. L. Raper, M. S. Saag, and J. J. Allison. 2009. Missed visits and mortality among patients establishing initial outpatient HIV treatment. Clinical Infectious Diseases 48(2):248-256.
NAHC (National AIDS Housing Coalition). 2012. HOPWA 2013 Budget Request: NAHC Recommends $380 Million. http://nationalaidshousing.org/PDF/2013HOPWANeedPaper.pdf (accessed January 9, 2012).
Napravnik, S., J. J. Eron, Jr., R. G. McKaig, A. D. Heine, P. Menezes, and E. Quinlivan. 2006. Factors associated with fewer visits for HIV primary care at a tertiary care center in the Southeastern U.S. AIDS Care 18(Suppl 1):S45-S50.
NCHS (National Center for Health Statistics). 2012. About Health Care Surveys. http://www.cdc.gov/nchs/dhcs/about_dhcs.htm (accessed June 7, 2012).
NIAAA (National Institute on Alcohol Abuse and Alcoholism). 2005. Screening for alcohol and alcohol related problems. Alcohol Alert, no. 65. http://pubs.niaaa.nih.gov/publications/aa65/AA65.htm (accessed January 6, 2012).
NIH, NCRR (National Institutes of Health, National Center for Research Resources). 2006. Electronic Health Records Overview. McLean, VA: MITRE Corporation. http://www.ncrr.nih.gov/publications/informatics/ehr.pdf (accessed January 6, 2012).
NQF (National Quality Forum). 2011a. About NQF. http://www.qualityforum.org/About_NQF/About_NQF.aspx (accessed January 6, 2012).
NQF. 2011b. NQF Endorsed Standards. http://www.qualityforum.org/Measures_List.aspx?#k=HIV&p=2&s=n&so=a (accessed January 6, 2012).
NRHA (National Rural Health Association). 2006. Rural HIV care. http://199.237.254.34/opporty/pdf/HIV_Transportation.pdf (accessed January 5, 2012).
NYC DOHMH (New York City Department of Health and Mental Hygiene). 2011. 2011 Advisory #27: Health Department Releases New HIV Treatment Recommendations. http://www.nyc.gov/html/doh/downloads/pdf/cd/2011/11md27.pdf (accessed May 15, 2012).
NYSDHAI (New York State Department of Health AIDS Institute). 2001. HIV and Oral Health: General Principles. http://www.hivguidelines.org/clinical-guidelines/hiv-and-oral-health/general-principles/ (accessed January 6, 2012).
NYSDHAI. 2011. New York State Quality of Care Program. http://www.hivguidelines.org/quality-of-care/nys-hiv-quality-of-care-program/ (accessed January 6, 2012).
Oh, D. L., F. Sarafian, A. Silvestre, T. Brown, L. Jacobson, S. Badri, and R. Detels. 2009. Evaluation of adherence and factors affecting adherence to combination antiretroviral therapy among white, Hispanic, and black men in the MACS cohort. Journal of Acquired Immune Deficiency Syndromes 52(2):290-293.
Ohl, M., J. Tate, M. Duggal, M. Skanderson, M. Scotch, P. Kaboli, M. Vaughan-Sarrazin, and A. Justice. 2010. Rural residence is associated with delayed care entry and increased mortality among veterans with human immunodeficiency virus infection. Medical Care 48(12):1064-1070.
OMB (Office of Management and Budget). 1977. Statistical Policy Directive No. 15, Race and Ethnic Standards for Federal Statistics and Administrative Reporting. http://wonder.cdc.gov/wonder/help/populations/bridged-race/Directive15.html (accessed August 11, 2011).
OMB. 1997a. Recommendations from the Interagency Committee for the Review of the Racial and Ethnic Standards to the Office of Management and Budget concerning changes to the standards for the classification of federal data on race and ethnicity. Federal Register (3110-01):36873-36946.
OMB. 1997b. Revisions to the standards for the classification of federal data on race and ethnicity. Federal Register 62:58781-58790.
ONAP (Office of National AIDS Policy). 2010. National HIV/AIDS Strategy for the United States. http://www.whitehouse.gov/sites/default/files/uploads/NHAS.pdf (accessed January 6, 2012).
Othieno, J. 2007. Twin cities care system assessment: Process, findings, and recommendations. Journal of Health Care for the Poor and Underserved 18(3 Suppl):189-213.
Owe-Larsson, M. B., L. Säll, E. Salamon, and C. Allgulander. 2009. HIV infection and psychiatric illness. African Journal of Psychiatry 12(2):115-128.
PACHA (Presidential Advisory Council on HIV/AIDS). 2011. Letter to HHS Secretary Kathleen Sebelius (August 8). http://aids.gov/federal-resources/policies/pacha/meetings/august-2011/august-2011-pacha-letter-secretary.pdf, (accessed January 6, 2012).
Palepu, A., D. M. Cheng, T. Kim, D. Nunes, J. Vidaver, J. Alperen, R. Saitz, and J. H. Samet. 2006. Substance abuse treatment and receipt of liver specialty care among persons coinfected with HIV/HCV who have alcohol problems. Journal of Substance Abuse Treatment 31(4):411-417.
Park, W. B., P. G. Choe, S. H. Kim, J. H. Jo, J. H. Bang, H. B. Kim, N. J. Kim, M. Oh, and K. W. Choe. 2007. One-year adherence to clinic visits after highly active antiretroviral therapy: A predictor of clinical progress in HIV patients. Journal of Internal Medicine 261(3):268-275.
Pence, B. W. 2009. The impact of mental health and traumatic life experiences on antiretroviral treatment outcomes for people living with HIV/AIDS. Journal Antimicrobial Chemotherapy 63(4):636-640.
Penzak, S. R., Y. S. Reddy, and S. R. Grimsley. 2000. Depression in patients with HIV infection. HIV Update 57.
PEPFAR (U.S. President’s Emergency Plan for AIDS Relief). 2009. Next Generation Indicators Reference Guide. http://www.pepfar.gov/documents/organization/81097.pdf (accessed December 15, 2011).
PEPFAR. 2011. About PEPFAR. http://www.pepfar.gov/about/index.htm (accessed December 15, 2011).
Perkins, D., B. E. Meyerson, D. Klinkenberg, and B. T. Laffoon. 2008. Assessing HIV care and unmet need: Eight data bases and a bit of perseverance. AIDS Care 20(3):318-326. Pfizer. 2011. Welcome to the Patient Health Questionnaire (PHQ) Screeners. http://www.phqscreeners.com/ (accessed December 15, 2011).
Pinkerton, S. D., D. R. Holtgrave, and C. L. Galletly. 2008. Infections prevented by increasing HIV serostatus awareness in the United States, 2001 to 2004. Journal of Acquired Immune Deficiency Syndromes 47(3):354-357.
Pladevall, M., L. K. Williams, L. A. Potts, G. Divine, H. Xi, and J. E. Lafata. 2004. Clinical outcomes and adherence to medications measured by claims data in patients with diabetes. Diabetes Care 27(12):2800-2805.
Prejean, J., R. Song, Q. An, and H. I. Hall. 2008. Subpopulation estimates from the HIV incidence surveillance system—United States, 2006. Morbidity and Mortality Weekly Report 57(36):985-989. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5736a1.htm (accessed December 20, 2011).
Prejean, J., R. Song, A. Hernandez, R. Ziebell, T. Green, F. Walker, L. S. Lin, Q. An, J. Mermin, A. Lansky, and H. I. Hall. 2011. Estimated HIV incidence in the United States, 2006-2009. PLoS One 6(8):e17502.
Probst, J. C., S. B. Laditka, J. Y. Wang, and A. O. Johnson. 2007. Effects of residence and race on burden of travel for care: Cross sectional analysis of the 2001 U.S. National Household Travel Survey. BMC Health Services Research 7 (March):40 (13 pages).
Reif, S., C. E. Golin, and S. R. Smith. 2005. Barriers to accessing HIV/AIDS care in North Carolina: Rural and urban differences. AIDS Care 17(5):558-565.
Reisner, S. L., M. J. Mimiaga, M. Skeer, B. Perkovich, C. V. Johnson, and S. A. Safren. 2009. A review of HIV antiretroviral adherence and intervention studies among HIV-infected youth. Topics in HIV Medicine 17(1):14-25.
Riley, E. D., D. R. Bangsberg, D. Guzman, S. Perry, and A. R. Moss. 2005a. Antiretroviral therapy, hepatitis C virus, and AIDS mortality among San Francisco’s homeless and marginally housed. Journal of Acquired Immune Deficiency Syndromes 38(2):191-195.
Riley, E. D., A. R. Moss, R. A. Clark, S. L. Monk, and D. R. Bangsberg. 2005b. Cash benefits are associated with lower risk behavior among the homeless and marginally housed in San Francisco. Journal of Urban Health 82(1):142-150.
Riley, E. D., K. Moore, J. L. Sorensen, J. P. Tulsky, D. R. Bangsberg, and T. B. Neilands. 2011. Basic subsistence needs and overall health among human immunodeficiency virus-infected homeless and unstably housed women. American Journal of Epidemiology 174(5):515-522.
Rippeth, J. D., R. K. Heaton, C. L. Carey, T. D. Marcotte, D. J. Moore, R. Gonzalez, T. Wolfson, and I. Grant. 2004. Methamphetamine dependence increases risk of neuropsychological impairment in HIV infected persons. Journal of the International Neuropsychological Society 10(1):1-14.
Robison, L. S., A. O. Westfall, M. J. Mugavero, M. C. Kempf, S. R. Cole, J. J. Allison, J. H. Willig, J. L. Raper, C. M. Wilcox, and M. S. Saag. 2008. Short-term discontinuation of HAART regimens more common in vulnerable patient populations. AIDS Research and Human Retroviruses 24(11):1347-1355.
Roos, L. L., S. M. Sharp, and M. M. Cohen. 1991. Comparing clinical information with claims data: Some similarities and differences. Journal of Clinical Epidemiology 44(9):881-888.
Royal, S. W., D. P. Kidder, S. Patrabansh, R. J. Wolitski, D. R. Holtgrave, A. Aidala, S. Pals, and R. Stalle. 2009. Factors associated with adherence to highly active antiretroviral therapy in homeless or unstably housed adults living with HIV. AIDS Care 21(4): 448-455.
Rumptz, M. H., C. Tobias, S. Rajabiun, J. Bradford, H. Cabral, R. Young, and W. E. Cunningham. 2007. Factors associated with engaging socially marginalized HIV-positive persons in primary care. AIDS Patient Care and STDs 21(Suppl 1):S30-S39.
Sacktor, N. C., M. Wong, N. Nakasujja, R. L. Skolasky, O. A. Selnes, S. Musisi, K. Robertson, J. C. McArthur, A. Ronald, and E. Katabira. 2005. The international HIV dementia scale: A new rapid screening test for HIV dementia. AIDS 19(13):1367-1374.
Samet, J. H., A. Y. Walley, and C. Bridden. 2007. Illicit drugs, alcohol, and addiction in human immunodeficiency virus. Panminerva Medica 49(2):67-77.
SAMHSA (Substance Abuse and Mental Health Services Administration). 2011. Screening, Brief Intervention, and Referral to Treatment (SBIRT). http://www.samhsa.gov/prevention/SBIRT/index.aspx (accessed November 21, 2011).
Sarnquist, C. C., S. Soni, H. Hwang, B. B. Topol, S. Mutima, and Y. A. Maldonado. 2011. Rural HIV-infected women’s access to medical care: Ongoing needs in California. AIDS Care 23(7):792-796.
Sayles, J. N., M. D. Wong, J. J. Kinsler, D. Martins, and W. E. Cunningham. 2009. The association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. Journal of General Internal Medicine 24(10):1101-1108.
Scheyett, A., S. Parker, C. Golin, B. White, C. P. Davis, and D. Wohl. 2010. HIV-infected prison inmates: Depression and implications for release back to communities. AIDS and Behavior 14(2):300-307.
Schneider, E. C., A. M. Zaslavsky, and A. M. Epstein. 2002. Racial disparities in the quality of care for enrollees in Medicare managed care. Journal of the American Medical Association 287(10):1288-1294.
Schur, C. L., M. L. Berk, J. R. Dunbar, M. F. Shapiro, S. E. Cohn, and S. A. Bozzette. 2002. Where to seek care: An examination of people in rural areas with HIV/AIDS. Journal of Rural Health 18(2):337-347.
Schwarcz, S. K., L. C. Hsu, E. Vittinghoff, A. Vu, J. D. Bamberger, and M. H. Katz. 2009. Impact of housing on the survival of persons with AIDS. BMC Public Health 9 (July):220 (18 pages).
Sears, C., T. Davis, J. Guydish, and A. Gleghorn. 2009. Investigating the effects of San Francisco’s Treatment on Demand Initiative on a publicly-funded substance abuse treatment system: A time series analysis. Journal of Psychoactive Drugs 41(3):297-304.
Sengupta, S., B. Banks, D. Jonas, M. S. Miles, and G. C. Smith. 2011. HIV interventions to reduce HIV/AIDS stigma: A systematic review. AIDS and Behavior 15(6):1075-1087.
Shafran, S. D. 2007. Early initiation of antiretroviral therapy: The current best way to reduce liver-related deaths in HIV/hepatitis C virus-coinfected patients. Journal of Acquired Immune Deficiency Syndromes 44(5):551-556.
Shain, R. N., J. M. Piper, E. R. Newton, S. T. Perdue, R. Ramos, J. D. Champion, and F. A. Guerra. 1999. A randomized, controlled trial of a behavioral intervention to prevent sexually transmitted disease among minority women. New England Journal of Medicine 340(2):93-100.
Shaw, M. 2004. Housing and public health. Annual Review of Public Health 25 (April):397-418.
Sherer, R., K. Stieglitz, J. Narra, J. Jasek, L. Green, B. Moore, S. Shott, and M. Cohen. 2002. HIV multidisciplinary teams work: Support services improve access to and retention in HIV primary care. AIDS Care 14(Suppl 1):S31-S44.
Silverberg, M. J., W. Leyden, C. P. Quesenberry, and M. A. Horberg. 2009. Race/ethnicity and risk of AIDS and death among HIV-infected patients with access to care. Journal of General Internal Medicine 24(9):1065-1072.
Simoni, J. M., C. R. Pearson, D. W. Pantalone, G. Marks, and N. Crepaz. 2006. Efficacy of interventions in improving Highly Active Antiretroviral Therapy adherence and HIV-1 RNA viral load: A meta-analytic review of randomized controlled trials. Journal of Acquired Immune Deficiency Syndromes 43(Suppl 1):S23-S35.
Simoni, J. M., K. R. Amico, L. Smith, and K. Nelson. 2010. Antiretroviral adherence interventions: Translating research findings to the real world clinic. Current HIV/AIDS Reports 7(1):44-51.
Song, J. 1999. HIV/AIDS & Homelessness: Recommendations for Clinical Practice and Public Policy. Nashville, TN: Health Care for the Homeless Clinicians’ Network, National Health Care for the Homeless Council. http://www.nhchc.org/wp-content/uploads/2011/10/AIDS-Homelessness.pdf (accessed January 9, 2012).
Stall, R., T. C. Mills, J. Williamson, T. Hart, G. Greenwood, J. Paul, L. Pollack, D. Binson, D. Osmond, and J. A. Catania. 2003. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. American Journal of Public Health 93(6):939-942.
Stewart, K. E., M. M. Phillips, J. F. Walker, S. A. Harvey, and A. Porter. 2011. Social services utilization and need among a community sample of persons living with HIV in the rural south. AIDS Care 23(3):340-347.
Sullivan, P. S., M. L. Campsmith, G. V. Nakamura, E. B. Begley, J. Schulden, and A. K. Nakashima. 2007. Patient and regimen characteristics associated with self-reported nonadherence to antiretroviral therapy. PLoS One 2(6):e552 (6 pages).
Tang, P. C., M. Ralston, M. F. Arrigotti, L. Qureshi, and J. Graham. 2007. Comparison of methodologies for calculating quality measures based on administrative data versus clinical data from an electronic health record system: Implications for performance measures. Journal of the American Medical Informatics Association 14(1):10-15.
Torian, L. V., and E. W. Wiewel. 2011. Continuity of HIV-related medical care, New York City, 2005-2009: Do patients who initiate care stay in care? AIDS Patient Care and STDs 25(2):79-88.
Trent, C. R. 2004. Treatment on Demand: A Public Policy Initiative of the City of Detroit. Workshop, September 27-28, Detroit, MI.
Tucker, J. S., M. A. Burnam, C. D. Sherbourne, F.-Y. Kung, and A. L. Gifford. 2003. Substance use and mental health correlates of nonadherence to antiretroviral medications in a sample of patients with human immunodeficiency virus infection. American Journal of Medicine 114(7):573-580.
Ulett, K. B., J. H. Willig, H.-Y. Lin, J. S. Routman, S. Abroms, J. Allison, A. Chatham, J. L. Raper, M. S. Saag, and M. J. Mugavero. 2009. The therapeutic implications of timely linkage and early retention in HIV care. AIDS Patient Care and STDs 23(1):41-49.
UTHSC (University of Texas Health Science Center). 2011. The Executive Interview (Exit 25). http://www.dementia-assessment.com.au/frontotemporal/EXIT25_Executive_Interview.pdf (accessed December 16, 2011).
Valcour, V., R. Paul, S. Chiao, L. A. Wendelken, and B. Miller. 2011. Screening for cognitive impairment in human immunodeficiency virus. Clinical Infectious Diseases 53(8):836-842.
Valdiserri, R. O. 2002. HIV/AIDS stigma: An impediment to public health. American Journal of Public Health 92(3):341-342.
Valet, R. S., T. T. Perry, and T. V. Hartert. 2009. Rural health disparities in asthma care and outcomes. Journal of Allergy and Clinical Immunology 123(6):1220-1225.
Vermund, S. H., S. L. Hodder, J. E. Justman, B. A. Koblin, T. D. Mastro, K. H. Mayer, D. P. Wheeler, and W. M. El-Sadr. 2010. Addressing research priorities for prevention of HIV infection in the United States. Clinical Infectious Diseases 50(Suppl 3):S149-S155.
Vivithanaporn, P., G. Heo, J. Gamble, H. B. Krentz, A. Hoke, M. J. Gill, and C. Power. 2010. Neurologic disease burden in treated HIV/AIDS predicts survival: A population-based study. Neurology 75(13):1150-1158.
Vogenthaler, N. S., C. Hadley, S. J. Lewis, A. E. Rodriguez, L. R. Metsch, and C. del Rio. 2010. Food insufficiency among HIV-infected crack-cocaine users in Atlanta and Miami. Public Health Nutrition 13(9):1478-1484.
Waldrop-Valverde, D., R. L. Ownby, F. L. Wilkie, A. Mack, M. Kumar, and L. Metsch. 2006. Neurocognitive aspects of medication adherence in HIV-positive injecting drug users. AIDS and Behavior 10(3):287-297.
Walley, A. Y., D. M. Cheng, H. Libman, D. Nunes, C. R. Horsburgh, Jr., R. Saitz, and J. H. Samet. 2008. Recent drug use, homelessness and increased short-term mortality in HIV-infected persons with alcohol problems. AIDS 22(3):415-420.
Weinhardt, L. S., M. P. Carey, B. T. Johnson, and N. L. Bickman. 1999. Effects of HIV counseling and testing on sexual risk behavior: A meta-analytic review of published research, 1985-1997. American Journal of Public Health 89(9):1397-1405.
Weis, K. E., A. D. Liese, J. Hussey, J. J. Gibson, and W. A. Duffus. 2010. Associations of rural residence with timing of HIV diagnosis and stage of disease at diagnosis, South Carolina 2001-2005. Journal of Rural Health 26(2):105-112.
Weiser, S. D., D. R. Bangsberg, S. Kegeles, K. Ragland, M. B. Kushel, and E. A. Frongillo. 2009a. Food insecurity among homeless and marginally housed individuals living with HIV/AIDS in San Francisco. AIDS and Behavior 13(5):841-848.
Weiser, S. D., E. A. Frongillo, K. Ragland, R. S. Hogg, E. D. Riley, and D. R. Bangsberg. 2009b. Food insecurity is associated with incomplete HIV RNA suppression among homeless and marginally housed HIV-infected individuals in San Francisco. Journal of General Internal Medicine 24(1):14-20.
West, J., Y. Khan, D. M. Murray, and K. B. Stevenson. 2010. Assessing specific secondary ICD-9-CM codes as potential predictors of surgical site infections. American Journal of Infection Control 38(9):701-705.
Wheeler, W. H., R. A. Ziebell, H. Zabina, D. Pieniazek, J. Prejean, U. R. Bodnar, K. C. Mahle, W. Heneine, J. A. Johnson, and H. I. Hall. 2010. Prevalence of transmitted drug resistance associated mutations and HIV-1 subtypes in new HIV-1 diagnoses, U.S.—2006. AIDS 24(8):1203-1212.
Whetten, K., J. Leserman, R. Whetten, J. Ostermann, N. Thielman, M. Swartz, and D. Stangl. 2006a. Exploring lack of trust in care providers and the government as a barrier to health service use. American Journal of Public Health 96(4):716-721.
Whetten, R., K. Whetten, B. W. Pence, S. Reif, C. Conover, and S. Bouis. 2006b. Does distance affect utilization of substance abuse and mental health services in the presence of transportation services? AIDS Care 18(Suppl 1):27-34.
WHO (World Health Organization). 2008. HIV/AIDS and Mental Health (EB124/6). Report by the Secretariat. http://www.who.int/gb/ebwha/pdf_files/EB124/B124_6-en.pdf (accessed January 6, 2012).
Wohl, A. R., W. H. Garland, J. Wu, C. W. Au, A. Boger, R. Dierst-Davies, J. Carter, F. Carpio, and W. Jordan. 2011. A youth-focused case management intervention to engage and retain young gay men of color in HIV care. AIDS Care 23(8):988-997.
Wolitski, R. J., R. S. Janssen, I. M. Onorato, D. W. Purcell, and N. Crepaz. 2005. An overview of prevention with people living with HIV. In Positive Prevention: Reducing HIV Transmission Among People Living with HIV/AIDS, edited by Seth Kalichman. New York: Kluwer Academic/Plenum Publishers. Pp. 1-28.
Wolitski, R. J., D. P. Kidder, S. L. Pals, S. Royal, A. Aidala, R. Stall, D. R. Holtgrave, D. Harre, and C. Courtenay-Quirk. 2010. Randomized trial of the effects of housing assistance on the health and risk behaviors of homeless and unstably housed people living with HIV. AIDS and Behavior 14(3):493-503.
Zaller, N., F. S. Gillani, and J. D. Rich. 2007. A model of integrated primary care for HIV-positive patients with underlying substance use and mental illness. AIDS Care 19(9):1128-1133.
APPENDIX TABLE 2-1 follows on next page
|
Core Indicators for Clinical HIV Care |
|||
| Indicator | Data Elements Needed | Proxy/Alternative Data Elements | Rationale |
| Proportion of people newly diagnosed with HIV with a CD4+ cell count >200 cells/mm3 and without a clinical diagnosis of AIDS | • Date of HIV diagnosis • CD4 test results at diagnosis/first visit for HIV care • No diagnosis of AIDS or AIDS-defining illness (e.g., OIs) |
Reported rates of cases newly diagnosed with HIV and a CD4+ cell count >200 cells/mm3 and no clinical diagnosis of AIDS within time period can be used if specific CD4 test dates and results are not available. | Early diagnosis improves health outcomes and reduces transmission of the virus to others. |
| Proportion of people newly diagnosed with HIV who are linked to clinical care for HIV within 3 months of diagnosis | • Date of HIV diagnosis • Date of first visit for HIV care |
Date of first/second CD4 or viral load test can be used if date of first visit for HIV care is not available. | Timely linkage to clinical HIV care for PLWHA who are newly diagnosed improves individual health outcomes and reduces transmission of the virus to others. |
| Proportion of people with diagnosed HIV infection who are in continuous care (two or more visits for routine HIV medical care in the preceding 12 months at least 3 months apart) | • Dates of routine HIV-care visits | Dates of CD4 or viral load tests can be used if dates of visits for routine HIV care are not available. | PLWHA who are in continuous HIV care experience better health outcomes, including decreased mortality, and are less apt to transmit the virus to others. |
| Proportion of people with diagnosed HIV infection who received two or more CD4 tests in the preceding 12 months | • Dates of CD4 tests | Yes/no documentation of CD4 tests within 12-month reporting period can be used if specific dates of CD4 tests are not available. | Regular CD4 testing improves health outcomes in PLWHA by permitting providers to monitor individuals’ immune function; determine when to start antiretroviral therapy (ART) |
|
in untreated patients; assess immunologic response to ART, and assess the need for initiation or discontinuation of prophylaxis for opportunistic infections. |
|||
| Proportion of people with diagnosed HIV infection who received two or more viral load tests in the preceding 12 months | • Dates of viral load tests | Yes/no documentation of viral load tests within 12-month reporting period can be used if specific dates of viral load tests are not available. | Regular viral load (plasma HIV RNA) testing is important for monitoring clinical progression of the disease and therapeutic response in individuals on ART. Decreased viral load, and undetectable viral load in individuals on ART, is associated with improved health outcomes and reduced transmission of the virus. |
| Proportion of people with diagnosed HIV infection in continuous care for 12 or more months and with a CD4+ cell count >350 cells/mm3 | • Dates of routine HIV-care visits • Dates of CD4 tests • Results of at least one CD4 test within time period specified |
Dates of CD4 or viral load tests can be used if dates of visits for routine HIV care are not available. | Achieving and maintaining a CD4+ cell count ≥350 cells/mm3 reduces the risk of complicating opportunistic infections and cancers. |
| Proportion of people with diagnosed HIV infection and a measured CD4+ cell count <500 cells/mm3 who are not on ART* | • Dates of CD4 tests • Results of CD4 tests • Dates of ART prescription or dispensing |
Results from most recent CD4 test within reporting period can be used if specific dates of tests not available. Yes/no documentation of whether on ART can be used if prescription/ dispensing dates are not available. | Appropriate initiation of ART improves health outcomes and reduces transmission of the virus to others. |
*In contrast to the other indicators, the estimate for this indicator should decrease with improved access to care and supportive services.
| Indicator | Data Elements Needed | Proxy/Alternative Data Elements | Rationale |
| Proportion of people with diagnosed HIV infection who have been on ART for 12 or more months and have a viral load below the level of detection | • Dates of ART prescription or dispensing • Dates of viral load tests • Results of viral load tests |
Results from most recent viral load test within reporting period can be used if specific dates of tests not available. Yes/no documentation of whether on ART can be used if prescription or dispensing dates are not available. Rates of undetectable viral load among all persons diagnosed with HIV infection can be used as system level indicator. | With the advent of more potent antiretroviral drugs, the goal of ART is durable virologic suppression. An undetectable viral load improves health outcomes for PLWHA and reduces transmission of the virus. |
| All-cause mortality rate among people diagnosed with HIV infection* | • Date of death | Mortality rate within states or jurisdiction | Mortality is the ultimate outcome measure for assessing HIV/AIDS care among PLWHA. Mortality should be inversely related to the quality of overall care delivered. |
| Core Indicators for Mental Health, Substance Abuse, and Supportive Services | |||
| Indicator | Data Elements Needed | Proxy/Alternative Data Elements | Rationale |
|
|
|||
| Proportion of people with diagnosed HIV infection and mental health disorder who are referred for mental health services and receive these services within 60 daysa | • Date of diagnosis or evidence of mental health disorder • Date of mental health referral • Date of first visit for mental health services |
Evidence of mental health assessment and any visits for mental health services during the same reporting period can be used if specific dates of mental health referral and mental health visits are not available. | Untreated mental health disorders can negatively affect maintenance in care, adherence to treatment, and health outcomes for PLWHA, reducing treatment effectiveness and increasing risk of transmitting the virus to others. |
| Proportion of people with diagnosed HIV infection and substance use disorder who are referred for substance abuse services and receive these services within 60 daysb | • Date of diagnosis or evidence of substance use disorder • Date of referral for substance abuse services • Date of first visit for substance abuse services |
Evidence of substance use assessment and any visits for substance abuse services during the same reporting period can be used if specific dates of substance abuse referral and substance abuse visits are not available. | Untreated substance use disorders can negatively affect maintenance in care, adherence to treatment, and health outcomes for PLWHA, reducing treatment effectiveness and increasing risk of transmitting the virus to others. |
| Proportion of people with diagnosed HIV infection who were homeless or temporarily or unstably housedc at least once in the preceding 12 months* | • Housing status | Evidence of reported need for housing assistance during the reporting period can be used if information about housing status is not available. | Housing instability can negatively affect maintenance in care, adherence to treatment, and health outcomes for PLWHA, reducing treatment effectiveness and increasing risk of transmitting the virus to others. |
*In contrast to the other indicators, the estimate for this indicator should decrease with improved access to care and supportive services.
aReceipt of services within 30 days would be the ideal for optimal care, and more urgent cases should be seen sooner.
bSee footnote a above.
cThe U.S. Department of Housing and Urban Development’s Homeless Management Information System (HMIS) Data Standards provides guidance for classifying housing status in four categories: literally homeless (e.g., lack a regular nighttime residence, staying in an emergency shelter), following the McKinney-Vento Homeless Assistance Act (42 U.S.C. 11302, Sec. 103) definition of homelessness, as amended by the Homeless Emergency Assistance and Rapid Transition to Housing (HEARTH) Act of 2009 (P.L. 111-22, div. B, Sec. 1003); imminently losing housing (e.g., being evicted or being discharged from an institution with no housing options identified); unstably housed and at-risk of losing housing (e.g., temporarily doubled up with others, moving frequently for economic reasons), and stably housed(http://www.hudhre.info/documents/FinalHMISDataStandards_March2010.pdf, accessed March 12, 2012).
| Indicator | Data Elements Needed | Proxy/Alternative Data Elements | Rationale |
| Proportion of people with diagnosed HIV infection who experienced food or nutrition insecurityd at least once in the preceding 12 months* | • Food security status | Evidence of reported need for food assistance during the reporting period can be used if information about food security status is not available. | Food insecurity can negatively affect maintenance in care, adherence to treatment, and health outcomes for PLWHA, reducing treatment effectiveness and increasing risk of transmitting the virus to others. Poor nutrition affects absorption of medications and can contribute to diet-sensitive comorbidities. |
| Proportion of people with diagnosed HIV infection who had an unmet need for transportation services to facilitate access to medical care and related services at least once in the preceding 12 months* | • Transportation need | Evidence of reported need for transportation assistance during the reporting period can be used if information about access to transportation is not available. | Unmet need for transportation to access clinical HIV care and related services can negatively affect treatment access, service utilization, and health outcomes for PLWHA, reducing treatment effectiveness and increasing risk of transmitting the virus to others. |
| Additional Indicators for Clinical HIV Care | |||
| Indicator | Data Elements Needed | Proxy/Alternative Data Elements | Rationale |
| Proportion of people with diagnosed HIV infection who have had a documented tuberculosis (TB) screening test with results interpreted at least once since HIV diagnosis | • Date of HIV diagnosis/treatment or documentation of infection prior to test • Date and results of TB screening |
Yes/no documentation of TB test and results in medical record or yes/no documentation of TB test results within reporting period can be used if specific dates of HIV diagnosis and TB screening are not available. | All PLWHA with diagnosed active tuberculosis should receive ART to improve health outcomes. Screening for TB permits earlier diagnosis and initiation or ART. |
| Proportion of people with diagnosed HIV infection who have had documented chlamydia, gonorrhea, and syphilis screenings at least once in the preceding 12 months | • Date of chlamydia, gonorrhea, and syphilis screenings | Yes/no documentation of chlamydia, gonorrhea, or syphilis screening within reporting period can be used if specific dates of screening tests are not available. | Infection with co-occurring sexually transmitted infections (STIs) increases the risk of transmitting HIV to others. Screening for STIs permits earlier diagnosis and risk reduction. |
| Proportion of people with diagnosed HIV infection who have had hepatitis B screening performed at least once since HIV diagnosis or for whom there is documented immunity | • Date of hepatitis B screening or date of documented immunity | Yes/no documentation of hepatitis B screening within reporting period or documented immunity can be used if specific dates of HIV diagnosis and hepatitis B assessment are not available. | Individuals coinfected with HIV and hepatitis B virus are at greater risk for developing chronic hepatitis and for accelerated liver damage and serious liver-related morbidity and mortality. Early detection of hepatitis B coinfection permits earlier treatment and improved outcomes. Individuals who are screened and negative for immunity should be vaccinated, eliminating the need for repeated screening. |
| Proportion of people with diagnosed HIV infection who have had hepatitis C screening performed at least once in the preceding 12 months | • Date of hepatitis C screening | Yes/no documentation of hepatitis C screening within reporting period can be used if specific dates of screening tests are not available. | HIV and hepatitis C coinfection is associated with accelerated liver damage. Early detection of cooccurring hepatitis C coinfection permits earlier treatment and improved outcomes. |
*In contrast to the other indicators, the estimate for this indicator should decrease with improved access to care and supportive services.
dAccording to the U.S. Department of Agriculture, households with high food security have “no reported indications of food-access problems or limitations”; households with marginal food security have “one or two reported indications-typically of anxiety over food sufficiency or shortage of food in the house [with] little or no indication of changes in diets or food intake”; households with low food security have “reports of reduced quality, variety, or desirability of diet [with] little or no indications of reduced food intake”; and households with very low food security have “reports of multiple indications of disrupted eating patterns and reduced food intake.” The lower two levels-low and very low food security-refer to food insecurity (http://www.ers.usda.gov/briefing/foodsecurity/labels.htm#cnstat, accessed February 3, 2012).
| Indicator | Data Elements Needed | Proxy/Alternative Data Elements | Rationale |
| Proportion of people with diagnosed HIV infection who have received an influenza immunization during the preceding 12 months | • Date of influenza immunization | Yes/no documentation of influenza immunization within reporting period can be used if specific date of influenza immunization is not available. | HIV-infected individuals are considered to be at greater risk for serious influenza-related complications. CDC recommends annual prophylactic vaccination (inactive) for influenza. |
| Proportion of people with diagnosed HIV infection who have received a pneumococcal immunization at least once since HIV diagnosis | • Date of HIV diagnosis/treatment or documentation of infection prior to immunization • Date of pneumococcal immunization |
Yes/no documentation of pneumococcal immunization in medical record or yes/no documentation of pneumococcal immunization within reporting period can be used if specific dates of HIV diagnosis and pneumococcal immunization are not available. | HIV-infected individuals are considered to be at greater risk for contracting and developing serious complications from pneumococcal pneumonia. CDC recommends prophylactic vaccination as soon as possible following diagnosis, followed by a one-time revaccination 5 years later. |
| Proportion of people with diagnosed HIV infection who have received a hepatitis B vaccination, or who have documented immunity | • Date of hepatitis vaccine/date of documented immunity | Yes/no documentation of hepatitis B vaccination or documented immunity can be used if specific dates of HIV diagnosis and hepatitis B vaccination are not available. | HIV and hepatitis B coinfection is associated with accelerated liver damage and the development of chronic hepatitis and serious liver-related morbidity and mortality. CDC recommends prophylactic vaccination against hepatitis B for susceptible individuals with HIV. |
| Proportion of ART-naïve people with diagnosed HIV infection who receive drug resistance testing (genotypic) prior to ART initiation | • Date of drug resistance testing • Date of ART initiation |
Documentation of drug resistance testing for persons receiving ART can be used if dates of drug resistance testing and/or ART initiation are not available. | Drug resistance testing prior to the initiation of ART permits the identification of the appropriate treatment regimen and therefore improves health outcomes and reduces viral transmission. |
| Proportion of people with diagnosed HIV infection and HIV-associated nephropathy, hepatitis B (when treatment is indicted), or active TB, who are not on ART* | • Diagnosis or test results for HIVassociated nephropathy, hepatitis B, and TB • ART status (whether on ART or ART prescription/dispensing dates) |
Number of people with any of these conditions who are not on ART can be used if information about all three conditions is not available. | HHS recommends that HIV-infected individuals with HIV-associated nephropathy, hepatitis B virus coinfection (when treatment is indicated), or active TB receive ART to improve health outcomes. |
| Proportion of pregnant women with diagnosed HIV infection who are not on ART* | • Pregnancy status • ART status (whether on ART or ART prescription/dispensing dates) |
Number of births during reporting period to women not on ART can be used if complete information about pregnancy status is not available. | Use of combination ART in HIV positive pregnant women significantly reduces mother-to-child transmission of the virus. |
| Additional Indicators for Mental Health, Substance Abuse, and Supportive Services | |||
| Indicator | Data Elements Needed | Proxy/Alternative Data Elements | Rationale |
| Proportion of people with diagnosed HIV infection who were screened for mental health disorders at least once during the preceding 12 months | • Date of mental health screening | Yes/no evidence of screening for mental health disorders or referral for treatment during reporting period can be used if dates of mental health screening are not available. | Undiagnosed, and therefore untreated, mental health disorders can negatively affect adherence to treatment and health outcomes for PLWHA and increase their risk of transmitting the virus to others. |
*In contrast to the other indicators, the estimate for this indicator should decrease with improved access to care and supportive services.
| Indicator | Data Elements Needed | Proxy/Alternative Data Elements | Rationale |
| Proportion of people with diagnosed HIV infection who were screened for substance use disorders at least once during the preceding 12 months | • Date of screening for substance use | Yes/no evidence of screening for substance use disorders or referral for treatment during reporting period can be used if dates of substance use screening are not available. | Undiagnosed, and therefore untreated, substance use disorders can negatively affect adherence to treatment and health outcomes for PLWHA and increase the risk of transmitting the virus to others. |
| Proportion of people with diagnosed HIV infection who were assessed for need for housing at least once during the preceding 12 months | • Date of housing needs assessment | Yes/no evidence of housing assessment or referral for housing assistance during reporting period can be used if dates of housing assessment are not available. | Assessment of housing stability is important because housing instability can negatively affect adherence to treatment and health outcomes for PLWHA and increase the risk of transmitting the virus to others. |
| Proportion of people with diagnosed HIV infection who were assessed for need for food or nutrition at least once during the preceding 12 months | • Date of food security assessment | Yes/no evidence of food security assessment or referral for food or meal assistance during reporting period can be used if specific dates of assessment are not available. | Assessment of food security is important because food insecurity can negatively affect adherence to treatment; effectiveness of treatment, including ART; and health outcomes for PLWHA and increase the risk of transmitting the virus to others. |
| Proportion of people with diagnosed HIV infection who were assessed for need for transportation at least once during the preceding 12 months | • Date of transportation needs assessment | Yes/no evidence of assessment for transportation need or referral for transportation services during reporting period can be used if specific dates of assessment are not available. | Assessment of transportation need is important because an unmet need for transportation to access clinical HIV care and related services can negatively affect treatment access and health outcomes for PLWHA and increase the risk of transmitting the virus to others. |
|
|
|||
APPENDIX TABLE 2-2 follows on next page
| Diagnosis | Linkage | Engagement & Retention | Primary Care |
|
Indicators and Type (Process/Outcome) |
|||
|
• Process/Outcome |
• Process | • Process/Outcome | • Process |
|
• Proportion with a CD4+ cell count >200 cells/mm3 and without a clinical diagnosis of AIDS |
• Proportion linked to care for HIV within 3 months of diagnosis | • Proportion in continuous care (two or more visits in the preceding 12 months at least 3 months apart) • Proportion in continuous care for 12 or more months with CD4+ cell count ≥350 cells/mm3 |
In the preceding 12 months: • Proportion who received two or more CD4 tests • Proportion who received two or more viral load • Proportion screened for chlamydia, gonorrhea, and syphilis • Proportion screened for hepatitis C • Proportion immunized for influenza Since diagnosis: • Proportion screened for tuberculosis • Proportion screened for hepatitis B • Proportion immunized for hepatitis B (if needed) • Proportion immunized for pneumococcal pneumonia • Proportion who received drug resistance testing (genotypic) prior to ART initiation |
NOTE: The committee’s recommended core indicators are written in bold text.
| Treatment | Virologic Suppression | Mediators | Disparities |
|
|
|||
| • Process | • Outcome | • Process/Outcome | • Process/Outcome |
| • Proportion with a measured CD4+ cell count <500 cells/mm3 who are not on ART | • Proportion on ART for 12 or more months who have an undetectable viral load | • Proportion with mental health disorder referred for mental health services who received these services within 60 days | • All indicators related to diagnosis, linkage, engagement and retention, primary care, treatment, and virologic suppression, stratified by subpopulation |
| • Proportion with HIV-associated nephropathy, hepatitis B (when treatment is indicated), or active tuberculosis who are not on ART | • All-cause mortality rate | • Proportion with substance use disorder referred for substance abuse services who receive these services within 60 days | • All mediators, stratified by subpopulation |
| • Proportion of HIV infected pregnant women who are not on ART | • Proportion with an unmet need for • housing • food • transportation In the preceding 12 months: • Proportion screened for mental health disorders • Proportion screened for substance use disorders • Proportion assessed for need for • housing • food • transportation |
• All mediators, stratified by subpopulation | |
|
|
|||
| Diagnosis | Linkage | Engagement & Retention | Primary Care |
| Data Elements | |||
|
• Date of HIV diagnosis |
• Date of HIV diagnosis | • Dates of routine HIV-care visits | • Dates of CD4 tests |
|
• CD4 test results at diagnosis/first visit for HIV care |
• Date of first visit for HIV care (or proxy of first or second CD4 or viral load test date) | • Dates of CD4 tests | • Dates of viral load tests |
|
• Diagnosis of AIDS or AIDS-defining illness (e.g., OIs) |
• Results of at least one CD4 test within time period specified | • Date of HIV diagnosis/treatment or documentation of infection | |
| • Dates of chlamydia, gonorrhea, and syphilis screenings | |||
| • Date of hepatitis C screening | |||
| • Date and results of tuberculosis screening | |||
| • Date hepatitis B screening or date of documented immunity | |||
| • Date of influenza immunization | |||
| • Date of pneumococcal immunization | |||
| • Date of hepatitis vaccine/date of documented immunity | |||
| • Date of drug resistance testing | |||
| • Date of ART initiation | |||
| Treatment | Virologic Suppression | Mediators | Disparities |
|
|
|||
|
• Dates of CD4 tests • Results of CD4 tests • Dates of ART prescription or dispensing • Diagnosis or test results for HIV-associated nephropathy, hepatitis B, and tuberculosis • Pregnancy status |
• Dates of ART prescription or dispensing • Dates of viral load tests • Results of viral load tests • Date of death |
• Date of diagnosis or evidence of mental health disorder • Date of referral for mental health services • Date of first visit for mental health services • Date of diagnosis or evidence of substance use disorder • Date of referral for substance abuse services • Date of first visit for substance abuse services • Housing status • Food security status • Transportation need • Date of mental health screening • Dates of screening for substance use • Dates of housing, food security, and transportation needs assessment |
• All data elements for indicators and mediators • Additional data elements pertaining to subpopulations: |
| Condition | Etiological Cofactors | Guidance for Optimal Management |
| Cervical/anal dysplasia | Human papillomavirus (HPV); HIV* |
• Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents (http://www.aidsinfo.nih.gov/contentfles/Adult_OI.pdf) |
| Chronic obstructive pulmonary disease | Cigarette smoking |
• Chronic obstructive pulmonary disease and HIV (http://www.hiv.va.gov/provider/manual-primary-care/copd.asp) |
| Diabetes | HIV*; highly active antiretroviral therapy (HAART)*; diet; genetics; exercise |
• Clinical Practice Recommendations (http://care.diabetesjournals.org/content/31/Supplement_1.toc) |
| Hepatoma | Hepatitis B virus; hepatitis C virus |
• European AIDS Clinical Society (EACS) Guidelines for the Clinical Management and Treatment of Chronic Hepatitis B and C Coinfection in HIV Infected Adults (http://onlinelibrary.wiley.com/doi/10.1111/j.1468-1293.2007.00535.x/pdf) • EASL Clinical Practice Guidelines: Management of Chronic Hepatitis B (http://www.easl.eu/assets/application/fles/b73c0da3c52fa1d_fle.pdf) • Care of Patients with Chronic Hepatitis B and HIV Co-Infection: Recommendations from an HIV-HBV International Panel (www.hem-aids.ru/system/fles/attachments/1659/aids_aids_pdf_183.pdf) |
| Hyperlipidemia | HIV; HAART; diet; genetics; exercise |
• Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (ATP III Final Report) (http://www.nhlbi.nih.gov/guidelines/cholesterol/atp3_rpt.htm) • Guidelines for the Evaluation and Management of Dyslipidemia in Human Immunodefciency Virus (HIV)-Infected Adults Receiving Antiretroviral Therapy: Recommendations of the HIV Medicine Association of the Infectious Diseases Society of America and the Adult AIDS Clinical Trials Group (http://cid.oxfordjournals.org/content/37/5/613.full) |
| Condition | Etiological Cofactors | Guidance for Optimal Management | |
| Osteoporosis | HIV*; HAART*,**; lack of sun exposure; genetics; diet; substance use |
• Primary Care Guidelines for the Management of Persons Infected with Human Immunodefciency Virus: 2009 Update by the HIV Medicine Association of the Infectious Diseases Society of America (http://cid.oxfordjournals.org/content/49/5/651.full) |
|
| Renal disease | Hypertension; HAART**; HIV |
• Guidelines for the Management of Chronic Kidney Disease in HIV-Infected Patients (http://cid.oxfordjournals.org/content/40/11/1559.full) |
|
| Hypogonadism | Advanced HIV disease |
• Primary Care Guidelines for the Management of Persons Infected with Human Immunodefciency Virus: 2009 Update by the HIV Medicine Association of the Infectious Diseases Society of America (http://cid.oxfordjournals.org/content/49/5/651.full) |
|
| Hepatitis | Chronic hepatitis B or C; antiretroviral hepatotoxicity |
• Primary Care Guidelines for the Management of Persons Infected with Human Immunodefciency Virus: 2009 Update by the HIV Medicine Association of the Infectious Diseases Society of America (http://cid.oxfordjournals.org/content/49/5/651.full) • European AIDS Clinical Society (EACS) Guidelines for the Management and Treatment of Chronic Hepatitis B and C Coinfection in HIV-Infected Adults (http://onlinelibrary.wiley.com/doi/10.1111/j.1468-1293.2007.00535.x/pdf) |
|
| Sexually transmitted infections | Syphilis; gonorrhea; chlamydia; herpes simplex; enteric infections (via fecal contact) |
• Sexually Transmitted Diseases Treatment Guidelines, 2010 (http://www.cdc.gov/std/treatment/2010/STD-Treatment-2010-RR5912.pdf) |
|
| Tuberculosis and other opportunistic infections | HIV-associated immunodefciency |
• Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents (http://www.aidsinfo.nih.gov/contentfles/Adult_OI.pdf) |
|
| Condition | Etiological Cofactors | Guidance for Optimal Management | |
| Mental health disorders | Anxiety, depression, post-traumatic stress; stigma; discrimination |
• HIV and Mental Health (http://www.hivguidelines.org/clinical-guidelines/hiv-and-mental-health/) • Mental Health Disorders Among Substance-Using HIV-Infected Patients (http://www.hivguidelines.org/clinical-guidelines/hiv-and-substance-use/mental-health-disorders-among-substance-using-hiv-infected-patients/) |
|
| Substance use disorders | Anxiety, depression, post-traumatic stress; stigma; discrimination |
• HIV and Substance Use (http://www.hivguidelines.org/clinical-guidelines/hiv-and-substance-use/) • Mental Health Disorders Among Substance-Using HIV-Infected Patients (http://www.hivguidelines.org/clinical-guidelines/hiv-and-substance-use/mental-health-disorders-among-substance-using-hiv-infected-patients/) |
|
| Oral health | Candida; oral hairy leukoplakia; herpes simplex |
• HIV and Oral Health (http://www.hivguidelines.org/clinical-guidelines/hiv-and-oral-health/) |
|
* Connection between condition and cofactor not proven.
** Tenofovir most commonly associated with this finding.
























































































