Many Americans believe that the United States has one of the best healthcare systems in the world and that consequently Americans enjoy better health than most of the world’s populations. The data, however, do not support that belief. In fact, the United States is ranked 32nd in the world in life expectancy even though it is ranked third in total expenditures on health care as a percentage of gross domestic product (GDP). Clearly, good health is determined by more than money spent on the health-care system. In fact, a growing body of research indicates that living conditions—including such factors as housing quality, exposure to pollution, and access to healthy and affordable foods and safe places to exercise—have a greater effect on health. That research highlights the importance of considering health in developing policies, programs, plans, and projects, including ones that may not appear at first to have an obvious relationship to health.
Health impact assessment (HIA) has arisen as an especially promising way to factor health considerations into the decision-making process. It has been defined in various ways but essentially is a structured process that uses scientific data, professional expertise, and stakeholder input to identify and evaluate public-health consequences of proposals and suggests actions that could be taken to minimize adverse health impacts and optimize beneficial ones. HIA has been used throughout the world to evaluate the potential health consequences of a wide array of proposals that span many sectors and levels of government. International organizations, such as the World Health Organization and multilateral development banks, have also contributed to the development and evolution of HIA, and countries and organizations have both developed their own guidance on conducting HIA.
Although HIA has not been used widely by decision-makers in the United States, its use has steadily increased over the last 10 years. Local, state, and tribal health departments have conducted HIAs to inform decision-making in other agencies; community-based organizations have conducted HIAs with input from public-health experts to inform officials who are deliberating on legislative or administrative proposals; planning and transportation departments have conducted HIAs to inform their own decisions; and private consultants have con-
ducted HIAs for industry to determine the potential health consequences of various projects. Given the potential health benefits of HIA, the Robert Wood Johnson Foundation, the National Institute of Environmental Health Sciences, the California Endowment, and the Centers for Disease Control and Prevention asked the National Research Council (NRC) to develop a framework, terminology, and guidance for conducting HIA of proposed policies, programs, and projects at the federal, state, tribal, and local levels, including the private sector. As a result of that request, NRC convened the Committee on Health Impact Assessment, which prepared this report.
THE NEED FOR HEALTH-INFORMED DECISION-MAKING
The U.S. population clearly has not reached its full health potential despite major medical advances and large expenditures on health care. Almost 50% of adults suffer from at least one chronic illness, and obesity, which contributes to many health conditions, has grown to epidemic proportions in children and adults. Poor health has implications not only for the quality and duration of life but for the economy. Health-care spending accounted for 7% of U.S. GDP in 1970, accounted for 16% of GDP in 2008, and is projected to account for almost 20% by 2019. Poor health also results in reduced participation in and productivity of the labor force. Thus, the consequences of chronic illness are huge in suffering and monetary and business costs.
Many scientists, policy-makers, and others recognize that health is determined by multiple factors, including factors that shape the conditions in which people are born, grow, live, work, and age. Policies and programs that have historically not been recognized as related to health are now known or thought to have important health consequences. For example, public health has been linked to housing policies that determine the quality and location of housing developments, to transportation policies that affect the availability of public transportation, to urban planning policies that determine land use and street connectivity, to agricultural policies that influence the availability of various types of food, and to economic-development policies that affect the location of businesses and industry. The recognition that health is shaped by a broad array of factors emphasizes the importance of understanding the possible health consequences of decision-making. In fact, it can be argued that major improvements in public health cannot be achieved without considering the root causes of ill health. Indeed, it has been argued that major health problems, such as the obesity epidemic and its associated health and monetary costs, are essentially unintended consequences of various social and policy factors related, for example, to the mass production and distribution of energy-dense foods and the engineering of physical activity out of daily life through changes in how transportation is organized and how neighborhoods are designed and built.
Accordingly, systematic assessment of the health consequences of policies, programs, plans, and projects is critically important for protecting and
promoting public health; as indicated, lack of assessment can have many unexpected adverse health (and economic) consequences. One striking example is development of the transportation infrastructure in the United States. In 1956, Congress passed the Interstate Highway Act, which resulted in a transportation infrastructure focused on road-building and private automobile use and has shaped land-use patterns throughout the country. The emphasis on motorized transportation has been associated with more driving, less physical activity, higher rates of obesity, higher rates of air pollution, and transportation injuries and fatalities. A partial accounting of the costs of health outcomes wholly or partly associated with transportation indicates that the costs could be as great as $400 billion annually. No one can know how much the costs could have been reduced if health had been integrated into the decision-making. Without a systematic assessment, the health-related effects and their costs to individuals and society are hidden or invisible products of transportation-related decisions.
Several approaches, methods, or tools could be used to incorporate aspects of health into decision-making, but HIA holds particular promise because of its applicability to a broad array of policies, programs, plans, and projects; its consideration of adverse and beneficial health effects; its ability to consider and incorporate various types of evidence; and its engagement of communities and stakeholders in a deliberative process. The following sections define and describe the elements of HIA, the challenges to its practice, and the approaches to advancing it and integrating it into today’s decision-making processes.
DEFINING HEALTH IMPACT ASSESSMENT AND ITS ELEMENTS
On the basis of its review of HIA definitions, practice, published guidance, and peer-reviewed literature, the committee recommends the following technical definition of HIA, which is adapted from the definition of the International Association for Impact Assessment:
HIA is a systematic process that uses an array of data sources and analytic methods and considers input from stakeholders to determine the potential effects of a proposed policy, plan, program, or project on the health of a population and the distribution of those effects within the population. HIA provides recommendations on monitoring and managing those effects.
The committee emphasizes that HIA is conducted to inform a decision-making process and is intended to be concluded and communicated in advance of a decision so that the information that it yields can be used to shape a final proposal in such a way that adverse effects are minimized and beneficial ones are optimized. The committee acknowledges that other assessment methods may share some features with HIA, but they do not meet the definition and description of HIA that the committee provides in the present report.
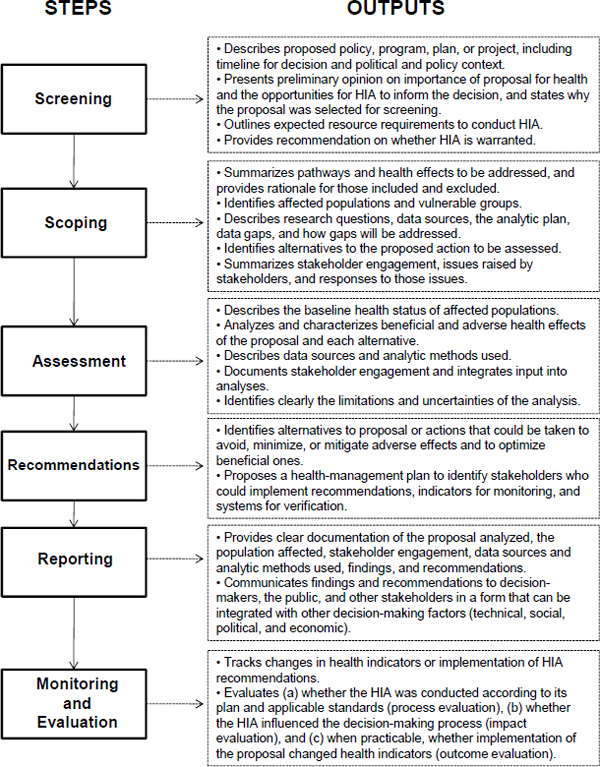
The committee found remarkable consistency regarding the basic elements that are generally included in descriptions of HIA, although they may be organized differently in the stages or steps that are outlined. The committee recommends a six-step framework as the clearest way to organize and describe the elements of HIA. The steps and their outputs are illustrated in Figure S-1; the committee’s conclusions regarding each step are provided below.
Screening establishes the need for and value of conducting an HIA and is essential for high-quality HIA practice. The committee concludes that the following factors are the most important to consider in determining whether to conduct an HIA: the potential for substantial adverse or beneficial health effects or irreversible or catastrophic effects, even if the effects have a low likelihood; the ability of information from the HIA to alter a decision or help a decision-maker to discriminate among options; the possibility that a disproportionate burden of the health effects is placed on vulnerable populations; the existence of public concern or controversy regarding health effects of a proposal; the opportunity to incorporate health information into a decision-making process that may not otherwise include such information; and the ability of the HIA team to complete the assessment within the time and with the resources available.
Scoping identifies the populations that might be affected, determines which health effects will be evaluated in the HIA, identifies research questions and develops plans to address them, identifies the data and methods to be used and alternatives to be assessed, and establishes the HIA team and a plan for stakeholder participation throughout the HIA process. The credibility of an HIA and its relevance to the decision-making process rest on a systematic evaluation of the full array of potential effects—risks, benefits, and tradeoffs—rather than on a narrow consideration of a subset of issues predetermined by a team’s research interests or regulatory requirements. However, to ensure judicious use of resources, the HIA should ultimately focus on the health effects of greatest potential importance. The committee notes that it is appropriate to include issues that are the subject of community concern even if they appear unlikely to be substantiated by further analysis; such an analysis can provide reassurance to communities even if the eventual conclusions do not support their concerns.
Assessment is a process that involves describing the baseline health status of the affected populations and then characterizing the expected effects on health (and its determinants) of the proposal and each alternative under consideration relative to the baseline and each other. In light of the various policies, programs, plans, and projects that are the subject of HIAs, a broad array of data and analytic methods are used to evaluate the potential effects. Often, complete information is not available, and expert judgment plays an important role in the HIA. Whatever approach is taken, an explicit statement of data sources, methods, assumptions, and uncertainty is essential. The committee notes that uncertainty does not negate the value of information. Even when the evidence of an effect is uncertain, describing the potential causal pathways that are based on a
Recommendations identify alternatives to the proposal or specific actions that could be taken to avoid, minimize, or mitigate adverse effects or to take advantage of opportunities for a proposal to improve health. Relatively little attention has been paid to the formulation of effective, actionable recommendations, and the committee offers three points for consideration. First, community input is essential for proposals that could have localized effects because it helps to ensure that specific aspects of living conditions and community design that may not be obvious to outside researchers are considered, and it maximizes the probability that the affected community will accept the conclusions and recommendations of the assessment. Second, recommendations are effective only if they are adopted by a decision-maker and implemented. The chances that the recommendations are adopted and implemented will increase if measures are drafted to address identified public-health risks; recognize feasibility issues, practical challenges, and other concerns possibly raised by the decision-maker during the HIA process; and fulfill the requirements of the legal and policy framework governing the decision. Third, recommendations should include the elements of a health-management plan that identifies appropriate indicators for monitoring, an entity with authority or ability to implement each measure, and a mechanism for verifying implementation and compliance. In practice, the HIA team will be asking a decision-maker to consider the findings and recommendations; ultimately, the decision-maker must balance health considerations with the many other technical, social, political, and economic concerns that bear on the proposal.
Reporting is the communication of findings and recommendations to decision-makers, the public, and other stakeholders. At present, there is little uniformity in the content of an HIA report. The committee recommends that, at a minimum, the written HIA report describe the proposed action or policy and alternatives that are the subject of the HIA, document the data sources and analytic methods used, identify the people consulted during the HIA process, and provide a clear, concise, and easily understood description of the process, findings, and recommendations. Furthermore, the reports should be made publicly available. A well-designed dissemination strategy is critical for the success of an HIA, and continuing efforts to inform decision-makers and stakeholders of the findings and recommendations are essential. However, efforts to support health-based recommendations must be carefully distinguished from biased efforts to promote a specific alternative on the basis of a skewed comparison of favorable and unfavorable aspects of a proposal or a predetermined political agenda. Undue bias in an HIA will likely compromise its credibility and efficacy.
Monitoring and evaluation can be characterized by several activities. Monitoring can consist of tracking the adoption and implementation of HIA recommendations or tracking changes in health indicators (health outcomes or health determinants) as a new policy, program, plan, or project is implemented. Evaluation can be process evaluation (evaluation of whether the HIA was conducted according to its plan of action and applicable standards), impact evaluation (evaluation of whether the HIA influenced the decision-making process), or
outcome evaluation (evaluation of whether implementation of the proposal changes health outcomes or health determinants). Few HIA evaluation data have been published in the United States or elsewhere, and it is not reasonable to expect that decision-makers will adopt HIA widely in the absence of evidence of its effectiveness and value. Consequently, the committee concludes that the lack of attention to evaluation is a barrier that will need to be overcome if HIA is to be advanced in the United States and notes that unbiased evaluation of its effectiveness and value will require participation of evaluators independent of the HIA team, stakeholders, decision-makers, and fiscal sponsors.
The committee emphasizes that the definitions and criteria recommended here should not be considered rigid requirements but rather reflect an ideal of practice. Given the broad array of applications and the resources and time available for HIA, deviations are expected, but they should be justified by a clear and well-articulated rationale. The committee also notes that HIA should not be assumed to be the best approach to every health-policy question but should be seen as part of a spectrum of public-health and policy-oriented approaches; the most appropriate will depend on the situation and decision-making context.
CHALLENGES AHEAD FOR HEALTH IMPACT ASSESSMENT
The committee identified several challenges for the successful emergence, development, and practice of HIA. Many are related to various aspects of HIA practice and are noted below with the committee’s suggestions for possible resolutions.
Defining health and the boundaries for HIA. As noted above, there is a growing consensus that individual health and public health are shaped by genetic, behavioral, social, economic, and environmental factors. Therefore, the committee concludes that HIA practice should not be restricted by a narrow definition of health or restricted to any particular policy sector (for example, education, urban planning, or finance), level of government (federal, state, tribal, or local), type of proposal (policy, program, project, or plan), or specific health outcome or issue (for example, asthma or obesity). There is no evidence to suggest that HIA is more important, appropriate, or effective in any particular decision context. On the contrary, HIA may be useful in a broad array of decision contexts, including many decision types to which it has not yet been applied. Accordingly, HIA should be focused on applications that present the greatest opportunity to protect or promote health and to raise awareness of the health consequences of decision-making. Because there are few legal mandates for HIA in the United States, it is most often conducted as a voluntary practice. As such, it will be difficult to ensure that decisions that could have the greatest impact on health are selected for evaluation. Thus, the current ad hoc approach to conducting HIA may result in less useful applications. The committee concludes that any future policies, standards, or regulations for HIA should include explicit criteria for identifying and screening candidate decisions and rules for providing
oversight for the HIA process; such criteria and rules would promote the utility, validity, and sustainability of HIA practice.
Balancing the need to provide timely, valid information with the realities of varying data quality. HIA must provide evidence-based findings and recommendations within the practical realities and timelines of the decision-making process; however, HIA practitioners often face substantial challenges regarding data availability and quality.1 The committee offers three strategies to maximize the validity of findings and recommendations in light of data constraints. First, one should consider diverse types of evidence and use expertise from multiple disciplines. Second, one should critically evaluate the data quality and select the evidence and analytic methods that are the strongest from among those available for a particular decision and context. There are no uniform standards for evaluating all potential evidence used in HIA, given the diverse applications and heterogeneity of data; in the future, criteria for data quality could be developed to characterize the relative strength of evidence and the nature and magnitude of uncertainties. Third, a strategy for assessing, acknowledging, and managing uncertainties is essential for ensuring the credibility of HIA findings and recommendations.
Producing quantitative estimates of health effects. Many expect HIA to produce quantitative estimates of health effects. Quantitative estimates of health effects have a number of desirable properties: they provide an indication of the magnitude of health effects, they can be easily compared with existing numerical criteria or thresholds that define the significance of particular effects, they allow one to make more direct comparisons among alternatives, and they provide inputs for economic valuation. They can be produced when there has been sufficient empirical research on relationships between particular determinants and health outcomes. Relying exclusively on quantitative estimation in HIA, however, presents some drawbacks. First, quantification has high information requirements. Given the breadth of health effects potentially considered in HIA, the sparse data available to support quantitative approaches, and the variability in practitioner capacity, it would be challenging or impossible for all HIAs to predict all potentially important health effects quantitatively. Second, because quantification can be resource-intensive, it may require more time than is practical, given the timeline for decision-making. Third, quantitative estimates may create an unwarranted impression of objectivity, precision, and importance and lead a reader to give credence to quantified results even if assumptions used in the analysis were based on subjective choices. Overall, however, quantitative estimates of health effects have value and should be provided when the data and resources allow and when they are responsive to decision-makers’ and stakeholders’ information needs.
Synthesizing conclusions on dissimilar health effects. Given that HIA analyzes multiple health effects, a practical challenge is synthesizing and presenting results on dissimilar health effects in a manner that is intelligible and useful to
_________________
1In this report, the term HIA practitioners refers to the people conducting the HIA.
decision-makers and stakeholders. Although summary measures have not been commonly used in HIA practice, they can be used to translate estimated effects on disparate health outcomes into a single comparable unit, such as quality-adjusted life years, disability-adjusted life years, and healthy-years equivalent. Calculating summary measures, however, requires assumptions and weighting schemes that need to be recognized and explained, and summary measures may not allow the integration of all health effects. Therefore, if summary measures are used, the committee recommends that effects—including those excluded from the summary measure—be described and characterized separately with regard to magnitude and significance in a way that allows users to judge their cumulative nature. The relative value of dissimilar health effects can then be considered explicitly or implicitly in the decision-making process.
Engaging stakeholders. Ensuring that stakeholders are able to participate effectively in the HIA process is widely described as an essential element of practice, although stakeholders often are not engaged or are only minimally engaged in the process. That discrepancy can be attributed to several factors, including the time and resources available; the methods, guidance, and standards used to conduct HIA; the importance that the practitioner or sponsor places on stakeholder participation; and a view that stakeholder participation may interfere with or impede progress. However, stakeholder participation is critical for the quality and effectiveness of the HIA. It helps to identify important issues; focus the HIA scope; highlight local conditions, health issues, and potential effects that may not be obvious to practitioners from outside the community; and ensure that recommendations are realistic and practical. Thus, whenever possible, strategies for stakeholder participation should extend beyond some minimal effort and address barriers and challenges to participation.
Ensuring the quality and credibility of HIA. Although HIA is different from primary scientific research, the committee concludes that several aspects of the HIA process could benefit from peer review. Peer review could highlight overlooked issues, identify opportunities to improve data or methods, and increase the legitimacy of conclusions and their acceptance and utility in the decision-making process. A formal peer-review process would need to overcome several obstacles, such as the possible difficulties in assembling the multidisciplinary team that would be needed to perform the review, the substantial delays that could occur in the process, and the current lack of agreed-on evaluation criteria. However, HIA is often conducted on proposals that are contested among polarized and disparate interests and stakeholders, and accusations of bias can arise. Independent peer review could help to ensure that the process by which HIA is conducted and the conclusions and recommendations produced are as impartial, credible, and scientifically valid as possible. The committee notes, however, that some flexibility in the peer-review process would be necessary particularly for cases in which an HIA must be completed rapidly to be relevant to the decision that it is intended to inform.
Managing expectations. HIA clearly is intended to inform decisions and ultimately to shape policy, programs, plans, and projects so that adverse health
effects are minimized and potential health benefits are optimized. The hope is that identifying valid information on a decision’s harms or benefits to health will motivate decision-makers to take protective actions. However, health typically is only one factor in the decision-making process; practical factors—such as cost, feasibility, and regulatory authority—also play a prominent role. And improved knowledge alone cannot necessarily change the ideology, interests, and attitudes of decision-makers. Thus, it is not reasonable to consider HIA successful only if it changes decisions. Furthermore, looking at HIA only as a mechanism for advocacy will compromise the support for and legitimacy of the practice.
Integrating HIA into environmental impact assessment (EIA). The U.S. National Environmental Policy Act (NEPA) and some related state laws explicitly require the identification and analysis of health effects when EIA is conducted. EIA, however, has traditionally included at most only a cursory analysis of health effects. Some argue that health analysis should be integrated into EIA because NEPA and related state laws provide a mechanism for achieving the same substantive goals as HIA. Others contend that EIA has become too rigid to accommodate a comprehensive health analysis and that attention should be focused on the independent practice of HIA. The committee emphasizes that the appropriate assessment of direct, indirect, and cumulative health effects in EIA under NEPA is a matter of law and not discretion, and recent efforts have successfully integrated the HIA framework into EIA. Thus, where legal standards under NEPA or applicable state EIA laws require an integrated analysis of health effects, one should be conducted with the same procedures that would be used to assess any other required factor. Because the steps and approaches of HIA and EIA are compatible, HIA offers an appropriate way to meet the requirement for health analysis under NEPA and related state laws. Although there are some substantive challenges to overcome, the committee concludes that improving the integration of health into EIA practice under NEPA and related state laws is needed and would advance the goal of improving public health.
ADVANCING HEALTH IMPACT ASSESSMENT
Substantial improvements in public health will require a focused effort to recognize and address the health consequences of decisions made at all levels and in all sectors of government. As noted, HIA is a particularly promising approach for integrating health implications into decision-making. International experience and the limited (but growing) experience in the United States provide important clues as to what is needed most to advance HIA.
Societal awareness of and education in HIA. First, the common belief that our health depends only on genetic predisposition, health care, and personal choice is impeding the improvement of public health. Policy-makers and the public need to be educated in the many factors that can affect health, the importance of considering them in all decision-making, and the role that HIA can play in the decision-making process. An education campaign will be necessary to
secure the resources that will be needed for the development of HIA practice. Second, few U.S. academic institutions offer formal education in HIA. Consequently, there are few professionally trained HIA practitioners in the country, and there is little agreement among them as to what constitutes good practice. High-quality education and training will be vital for the advancement of HIA in the United States. Third, continuing education of HIA professionals, policy-makers, and the public will be important for improving the quality of HIA practice in this country. The committee notes that a professional association or society could facilitate continuing education and develop, monitor, and facilitate standards of professional education and practice in HIA.
Structures and policies to support HIA. First, substantial interagency collaboration at the local, state, and federal levels is necessary to conduct HIA of policies, programs, plans, and projects, especially those emanating from nonhealth sectors, such as transportation, finance, urban planning, education, and agriculture. Such collaboration is essential, given the resource-constrained environments in which makers of public policy and other officials often work. The committee offers several suggestions for promoting interagency collaboration in the present report. Second, systematic use of HIA ultimately will depend on the adoption of policies and legal mandates to integrate health considerations into decision-making. As noted above, NEPA requires the analysis of health effects when EIA is conducted, but the spirit of the requirement needs to be reinvigorated and strengthened. Explicit guidance demonstrating how health considerations could be incorporated into NEPA would be beneficial. The committee emphasizes that policies and legislation outside the context of NEPA will most likely be needed to facilitate the use of HIA.
Research on and scholarship in HIA. First, few evaluations of HIA effectiveness have been conducted in the United States, especially because it has emerged so recently. Because conducting HIA will probably require the investment of substantial public and private resources, research is needed to document HIA practices and their effectiveness in influencing decision-making processes and promoting public health. Second, the quality of HIA could be substantially improved if there were better evidence on the relationship of “distal” factors to health outcomes. For example, research on how health is affected by federal, state, and local policies and actions traditionally considered to be unrelated to health—such as transportation, agriculture, education, housing, financial, and immigration policies—would be extremely beneficial.
The recognition that health is affected by much more than medical care, personal choice and behavior, and genetic predisposition is fundamental for the development and implementation of strategies to improve public health. However, the mere promulgation of a legal requirement to consider health would most likely not result in the health improvements that the United States needs. A tool, method, or approach is needed to facilitate the integration of health into decision-making. HIA is particularly promising in light of its broad applicability, its focus on adverse and beneficial health effects, its ability to incorporate various types of evidence, and its emphasis on stakeholder participation.