3
Elements of a Health Impact Assessment
Chapter 2 established the rationale for examining the potential effects of decisions on health and health disparities and highlighted health impact assessment (HIA) as a potential tool for assessing the health implications of various decisions. This chapter describes the types, structure, and content of HIAs and summarizes the HIA process, methodologic approaches, and variations in practice. It is informed by a review of U.S. and international HIA literature and guidelines (see Appendixes A and E) and by the experience of committee members and others who provided input during the committee process. On the basis of its review, the committee synthesized the information from guidance, practice, and literature to propose criteria that define an HIA and draw several conclusions regarding HIA practice. As discussed in this chapter, HIAs have been used for a wide variety of applications and at all levels of government (local, state, tribal, and federal) and have been conducted with varied resources over different schedules. The committee does not intend that the definition and criteria proposed in this chapter be considered rigid requirements but rather that they reflect an ideal of practice, deviation from which may occur but should be based on clear and well-articulated needs and rationale.
Before discussing the various elements of HIA, it is important to understand the context in which HIA is undertaken in the United States. As described in Appendix A, there are few laws in the United States that specifically require HIA, although many—such as the National Environmental Policy Act (NEPA)—require a consideration of health that can be accomplished through HIA. Most HIAs in the United States are therefore undertaken outside the formal decision-making process by organizations (such as nonprofit community-based groups), universities, or health departments that do not have decision-making authority over the proposals being addressed. Although less common to date, HIAs are also sometimes conducted by a decision-making agency, such as a metropolitan planning organization or a federal agency complying with NEPA. The decision to initiate an HIA is often made ad hoc when public-health advocates recognize that the proposal may have important health implications that
would not otherwise be recognized or addressed. There are often not clear lines of authority between the team conducting the HIA and the decision-maker. The health effects that are included, the data sources and methods that are used, and the recommendations that are made are therefore determined by the HIA practitioners rather than according to a legal or regulatory standard (Wernham 2011). Thus, the assessment phase is separated from the management phase, as recommended elsewhere (NRC 1983). The fact, however, that the team conducting the HIA is aware of the decision context allows the assessment to be decision-relevant.
CATEGORIES OF HEALTH IMPACT ASSESSMENT
Scholars point to a remarkable consistency in the basic elements that are generally included in descriptions of HIA (Mindell et al. 2008). In practice, however, there is some inconsistency in how HIAs are conducted—for example, how stakeholders are engaged and how data are collected and analyzed—and in the structure and content of the final work products of an HIA. The diversity of practice owes partly to the fact that HIAs are undertaken for a wide array of policy-making that spans many sectors, levels of government, types of proposal (policies, plans, programs, and projects), and degrees of complexity. The variability in the practice has evolved in the absence of widely accepted practice standards or formal regulatory or procedural requirements for HIA outside NEPA and related state laws (see Appendix A). However, it appears to be increasingly accepted that HIA is carried out to inform the decision rather than to evaluate the impacts after the decision is made, and there is general agreement on the procedural steps of HIA (Harris-Roxas and Harris 2011).
HIA practice is often defined in terms of several categories. According to effort, complexity, and duration, HIAs are often described as rapid, intermediate, or comprehensive. Rapid HIAs may be completed in a short time (weeks to months), are often focused on smaller and less complex proposals, and generally involve primarily literature review and descriptive or qualitative analysis. The phrase desktop HIA has also been used to refer to a rapid HIA that entails little or no public engagement. Another variation, rapid-appraisal HIA, has been described and in some texts includes explicit public engagement through an initial half-day workshop for stakeholders (Parry and Stevens 2001; Mindell et al. 2003; ICMM 2010). Intermediate HIAs require more time and resources and involve more complex pathways, more stakeholder engagement, and a more detailed analysis but include little collection of new data. Comprehensive HIAs are most commonly differentiated from rapid and intermediate HIAs by the scope of potential impacts and the need for collection of new primary data. They can take longer than a year to complete.
HIAs are also differentiated according to whether they are integrated into an environmental impact assessment or done independently. Another categorization is based on the breadth of the HIA and distinguishes HIAs that have a tight
focus—such as ones that use a narrow definition of health and emphasize quantification—from HIAs that have a broader, holistic focus shaped by the social determinants of health (Kemm 2001). Others have proposed categorizing HIAs as participatory (emphasizing shared governance, public participation, and a focus on socioeconomic and environmental determinants), quantitative or analytic (concentrating on the methods and rigor of the analysis), or procedural (drawing on elements of the other two approaches but emphasizing the procedural steps required and often undertaken within a specified administrative or regulatory context) (Cole and Fielding 2007).
In practice, the categories are rarely used consistently, and a single HIA often encompasses a blend of various approaches to stakeholder engagement and participation, analytic methods, and interactions with the formal decision-making process. For example, desktop HIAs may consider indirect stakeholder input through review of public comments submitted outside the HIA process, comprehensive HIAs may have relatively little stakeholder engagement, and rapid-appraisal HIAs of smaller-scale proposals may involve collection of some new data to inform the analysis. The various categories of HIAs, although useful for describing distinct themes in the field, do not necessarily represent consistently distinct strains of practice. Instead, it appears that the specific methods and approaches used in a single HIA often evolve within the basic framework described above and develop as a pragmatic response to context. Influences on practice include the timeline, resources and skills available to the HIA team, the factors being considered and the data available for analysis, and the legal and regulatory context of the decision-making process. That description is consistent with the earlier characterizations of HIA as a combination of procedures, methods, and tools (WHO 1999; Quigley et al. 2006).
The committee notes that the diversity of approaches and decision contexts imposes challenges for determining the resources required for conducting an HIA. For example, although rapid HIAs are small-scale, low-cost investigations, comprehensive HIAs that require new primary data collection can take longer than a year to complete and require substantially more resources. Information on costs of HIAs would be valuable in determining whether an HIA can be undertaken with the resources available and could inform the screening process as described below. However, the committee notes that no published studies in the United States have attempted to quantify the costs of undertaking an HIA across a variety of settings. Such information would be useful for informing future implementation.
DEFINITION OF HEALTH IMPACT ASSESSMENT
The committee proposes on the basis of its review the following adaptation of the current working definition of the International Association of Impact Assessment (Quigley et al. 2006) as a technical definition of HIA:
HIA is a systematic process that uses an array of data sources and analytic methods and considers input from stakeholders to determine the potential effects of a proposed policy, plan, program, or project on the health of a population and the distribution of the effects within the population. HIA provides recommendations on monitoring and managing those effects.
That definition reflects the committee’s finding that the involvement of stakeholders—although the approaches used vary from little or no involvement to robust engagement and participation at every step—has consistently been described as a core element of HIA practice and should be considered essential to it. Although rapid or desktop HIAs may not involve stakeholders or consider their input, this often (although not uniformly) reflects a pragmatic response to limitations, such as the timeframe for the decision or resources available to the HIA team, rather than an optimal practice. The definition also notes that recommendations should incorporate monitoring, which is essential for effective continuing management as a decision is implemented.
WHO CONDUCTS HEALTH IMPACT ASSESSMENTS?
HIAs can be conducted by a variety of agencies, organizations, or individuals. A decision-making body—such as a department of planning or transportation—can conduct an HIA to inform its own decision. It is also common for local, state, or tribal health departments to undertake an HIA to inform another agency’s decision-making. University researchers have conducted HIAs, and community-based organizations have conducted HIAs with technical assistance from public-health experts to inform officials who are deliberating on a legislative or administrative proposal. HIAs are also done by private consultants who are hired by a project proponent or decision-maker or by private-industry stakeholders.
Because the assessment of health effects depends on an in-depth understanding of changes that may affect health—such as changes in traffic flow, roadway design, air quality, or community revenue sources—HIAs are inherently multidisciplinary; public-health experts may lead the effort but must draw on resources and expertise from other disciplines. Thus, HIA teams may include not only health experts but professionals in other related disciplines, such as air or water quality or traffic modeling. As discussed in greater depth in the section on scoping, it is common to convene advisory or steering committees, which can include both technical and policy experts and representatives from stakeholder groups that have an interest in the decision outcome.
The training and credentials of HIA practitioners are variable, and there is no universally accepted standard for a level of training necessary to lead an HIA. In the United States, HIAs have commonly been undertaken by people who have an MPH or equivalent degree and have attended a brief (2- to 5-day) training
session. In this report, HIA practitioner refers to the person (or people) involved in conducting an HIA.
PROCESS FOR HEALTH IMPACT ASSESSMENT
The tasks or elements that are described as part of an HIA are fairly consistent in the peer-reviewed literature and guides reviewed by the committee. The grouping of the elements in discrete stages or steps of an HIA is less consistent; some guides list as few as five steps, and others describe as many as nine (Quigley et al. 2006; Bhatia 2010; ICMM 2010). The committee selected a six-step framework as a clear way to organize and describe the critical elements of an HIA. The steps can be described as follows:
(1) Screening determines whether a proposal is likely to have health effects and whether the HIA will provide information useful to the stakeholders and decision-makers.
(2) Scoping establishes the scope of health effects that will be included in the HIA, the populations affected, the HIA team, sources of data, methods to be used, and alternatives to be considered.
(3) Assessment involves a two-step process that first describes the baseline health status of the affected population and then assesses potential impacts.
(4) Recommendations suggest design alternatives that could be implemented to improve health or actions that could be taken to manage the health effects, if any, that are identified.
(5) Reporting documents and presents the findings and recommendations to stakeholders and decision-makers.
(6) Monitoring and evaluation are variably grouped and described. Monitoring can include monitoring of the adoption and implementation of HIA recommendations or monitoring of changes in health or health determinants. Evaluation can address the process, impact, or outcomes of an HIA.
The following sections provide an overview of the process of conducting an HIA. For each step, the committee describes the basic purpose, objectives, and practice elements; summarizes the main outputs; and presents conclusions regarding pertinent issues raised. Major issues and challenges for HIA development and practice are considered in Chapter 4. The reader will notice that some of the committee’s descriptions and characterizations overlap with those of other guides; the similarities highlight the consistencies in the field.
Screening
Screening establishes the need for and value of conducting an HIA. Because HIAs can address decisions that range from small, localized programs or projects to national policies, screening ensures that HIA is used judiciously and
when it is most likely to be valuable. Given the volume and breadth of decisions at the local, state, tribal, and federal levels that can potentially affect health in some way, one of the challenges for HIA practice is to determine which proposals to screen. In the absence of mandates or formal procedures, topics for screening are often chosen on the basis of the interests of a group wishing to use HIA as opposed to a structured, strategic selection process.1
More structured approaches have also been used. In some cases, collaboration between a health department and other agencies has resulted in the identification of appropriate proposals for screening. In other cases, all proposals in selected agencies or sectors have been screened by local governments (SFCC 1998; Lester et al. 1999; Roscam Abbing 2004). For example, the San Francisco Department of Public Health routinely screens major projects and plans to ensure adequate analysis and mitigation of environmental health impacts. In Alaska, all large natural-resources development proposals are now screened for the need for HIA in a new program begun by the state health department.
Screening involves making an initial rapid judgment of whether an HIA is likely to be feasible and valuable. The central considerations include whether the proposal in question might cause important changes in health, whether health is already a major focus of the decision-making process, whether the legal framework provides an opportunity for health to be factored into the decision, and whether data, staff, resources, and time are adequate to complete a successful HIA in time to provide useful input into the decision-making process (that is, can information be provided within the timeline for the decision). Another consideration is whether the proposal is likely to place a disproportionate burden of risk on vulnerable populations in the affected community; screening proposals on this basis helps to ensure that the HIA addresses the risk factors that underlie observed disparities in the rates of illness among various populations.
A variety of screening tools and algorithms are commonly used (Cole et al. 2005; PHAC 2005; Harris et al. 2007; Bhatia 2010). Some use pertinent screening questions, such as the ones noted, and apply a sequential yes-no query to each (Cole et al. 2005). Some provide a checklist of factors to consider and often focus on health determinants that might be affected by the proposal. Some decisions to conduct HIA may depend on a specific statutory requirement or mandated procedure. For example, in the context of NEPA, the lead federal agency must consider “the degree to which the proposed action affects public health or safety” to determine whether a proposal is likely to have “significant” effects and therefore require an environmental impact statement (40 CFR
_________________
1Under NEPA, a federal agency must determine whether a federal environmental decision is likely to have significant effects, and if so, the level of analysis required (40 C.F.R. Section 1508.27). Because the degree to which the proposed action affects public health or safety is one factor considered, this process could be considered the equivalent of the screening step of an HIA. In practice, however, explicit consideration of health has been rare (Steinemann 2000; Cole et al. 2004; Bhatia and Wernham 2008).
1508.27). Ultimately, regardless of the specific tool used, the decision to conduct HIA in most cases relies on the practitioner’s or decision-maker’s judgment regarding the likelihood of impacts, the time and resources available, and the likelihood that the information produced by the HIA will be a valuable aid to decision-making.
Because any actions taken on the basis of HIA recommendations need to be implemented within a specific legal and policy context, screening needs to establish a clear description of the decision-making process and context. It should also identify the points at which there is an opportunity for information from the HIA to influence decisions. Mapping out the timeline for the decision-making process can be helpful, and for large and complex programs and projects, identifying the agencies involved and their jurisdictions is important. Such programs and projects involve many agencies and entities that have authority over some aspect of planning and implementation. For example, the planning of the Atlanta Beltline, as described later in this chapter, involved the regional planning commission, local legislative bodies, state and federal environmental regulators, and private developers. It is also useful to assess the political context of the proposal to be assessed and consider, for example, the major political drivers of the proposal, the arguments made by political supporters and those opposed to the proposal, and any economic or technical constraints that limit the alternatives that can be considered.
Public concerns are a common trigger for a decision to screen, and the degree of concern or controversy about a proposal may be one of the factors weighed in the decision to undertake an HIA. For example, the Massachusetts Department of Public Health responded to citizen concerns regarding a proposed power plant by considering whether HIA would be an appropriate way to address them (McAuliffe 2009). The committee notes that public involvement is important in screening; information provided by stakeholders may provide insight into the potential effects of a proposal under consideration that contribute to the final determination of whether an HIA is warranted and likely to be useful.
Screening is often not well documented, and it is often not clear from an HIA report what factors were considered in making the decision to do an HIA. Moreover, because there is generally no written record of HIAs that stop at screening, still less is known about the reasons that have led to decisions not to proceed with HIA. Box 3-1 provides an example of how screening on a proposal for a residential housing program was conducted. It includes the information that was taken into account and the final output of the screening process, which was a decision on whether to commission and proceed with an HIA.
Outputs of Screening
Screening should result in a simple statement that includes the following:
• A description of the proposed policy, program, plan, or project that will be the focus of the HIA, including the timeline for the decision and intervention points at which HIA information will be used.
• A statement of why the proposal was selected for screening.
• A preliminary opinion regarding the potential importance of the proposal for health.
• The expected resource requirements of the HIA and the ability of the HIA team to meet them.
• A description of the political and policy context of the decision and an analysis of the opportunities to influence decision-making or otherwise make health-oriented changes.
BOX 3-1 Screening: HIA of a Residential Housing Program
The Crossings is a proposed housing development in Los Angeles that will provide 450 units in a newly rezoned residential area that needs affordable housing. A local community-based organization worked with a housing developer on the proposal and site plan. They expressed “interest in developing The Crossings in a way that will address local community needs for affordable housing and for other community assets that are safe, healthy, and supportive” (p. Intro-1).
In 2009, an HIA was conducted to ensure that health impacts were considered in the design and development of The Crossings and in the broader policies that affected redevelopment in the area. The HIA report describes the screening process but does not provide great detail about it.
The HIA notes that the area within which The Crossings is proposed to be built has the following characteristics:
• A growing population of families that have children.
• Dilapidated housing conditions.
• Prevalence of overcrowding.
• A lack of access to needed goods and services.
The HIA notes that the residential area is inhabited by a vulnerable population, that the built environment is of low quality, that the development will potentially have important health implications for residents in the local and surrounding communities, and that there is a strong commitment shown by the community and the developer to integrate health considerations into the planning process. It was concluded during the screening phase that an HIA would add value to project outcomes. An HIA would identify health assets, health liabilities, and health-promoting mitigations related to the proposed development project. The facts that resources were available and that timelines were appropriate were also relevant to the decision to conduct an HIA.
Source: Adapted from Heller et al. 2009.
• A screening recommendation—for example, no further action required; no HIA, but health advice and input to be offered in an alternative way; or proceed with HIA.
Committee Conclusions Regarding Screening
Screening is essential for high-quality HIA. Poorly selected proposals may result in HIAs that add little new information and consume considerable time and resources of the HIA team to complete and of recipients to review. HIA should not be assumed to be the best approach to every health-policy question but should instead be seen as part of a spectrum of public-health and policy-oriented approaches, some of which will be more appropriate than others, depending on the specific application. Although the reasons and objectives for HIA are often not articulated at the outset of screening, establishing well-defined objectives will focus the screening process on determining whether HIA is likely to be an effective approach for achieving them.
Any approach to determining which proposals will be screened should demonstrate a consistent rationale; should document the rationale in the HIA report; and should take account of public input. Screening should also consider whether a proposal conforms with applicable standards, policies, or laws relevant to health inasmuch as there is a wide variety of them that bear directly or indirectly on health. For example, U.S. priorities for improving public health are expressed in the Healthy People 2020 Program of the U.S. Department of Health and Human Services (DHHS 2010). Some laws—such as NEPA, state environmental-policy acts, and various local zoning ordinances—may establish protection of health as a requirement or priority. The programs and policies, however, may not provide any guidance on how health should be considered (see, for example, Pub. L 91-190, 42 U.S.C. 4321-4347 [1970]; EC 2001). Furthermore, some policies may focus on determinants of health—for example, economic development, transportation, or housing—rather than explicitly mentioning health. In each case, it is important to determine how the standards, policies, programs, and laws bear on how health is factored into a proposal.
The committee concludes that the following are the most important factors to consider in determining whether to do an HIA:
• The potential for substantial adverse or beneficial health effects and the potential to make changes in the proposal that could result in an improved health risk-benefit profile.
• The potential for HIA-based information to alter a decision or help a decision-maker discriminate among decision options.
• The potential for irreversible or catastrophic effects (including effects of low likelihood).
• The potential for health effects to place a disproportionate burden on or substantially benefit vulnerable populations.
• Public concern or controversy regarding health effects of the proposed decision.
• The opportunity to bring health information into a decision-making process that may otherwise not include this information.
• The potential for the HIA to be completed in the time allotted and with the resources available.
Ultimately, the HIA report should provide a rational and consistent explanation of how proposals are selected for screening. That explanation is particularly important when public funds are to be used for an HIA because the public may want to understand the basis for allocating sparse public resources. Given the breadth of decisions that are likely to warrant consideration, the approach taken will vary on the basis of who is initiating the HIA, the capacity and authority of the agency or entity undertaking it, and the objectives for contemplating an HIA.
Scoping
Scoping establishes the boundaries of the HIA and identifies the health effects to be evaluated, the populations affected, the HIA team, sources of data, methods to be used, and any alternatives to be assessed. Well-executed scoping saves time, work, and resources in the later stages of the HIA (Harris et al. 2007). The choice of what to evaluate will reflect the specific social, political, and policy context of the decision; the needs, interests, and questions of stakeholders and decision-makers; and the health status of the affected population.
Potential Health Effects
Determining the potential health effects to include in the HIA and proposing hypothetical causal pathways are the central tasks of scoping. Scoping considers input from many sources, including preliminary literature searches, public input, and professional or expert opinion in fields relevant to the proposal. Because it will often not be practical or possible to address all direct and indirect health effects that appear theoretically possible, it is important to select issues carefully.2 Setting priorities considers pathways that appear most important from a public-health perspective and considers issues that have been raised prominently by stakeholders. Questions that are important from a public-health perspective might include the severity of the health effect, the size and likelihood of the effect, and the potential of the effect to exacerbate health disparities. In practice, some HIAs have focused on a specific health end point, such as obesity, or
_________________
2Identifying high-priority issues has been addressed in numerous contexts outside HIA, including human-health and ecologic risk assessment (see, for example, EPA 1989, 1992; NRC 1996, 2009).
health concerns related to a single impact of the proposal, such as the health effects of air pollutants, most likely without using a systematic approach that considered and eliminated other impacts (see, for example, Kuo et al. 2009; Castro et al. 2010).
Iteration during scoping and between scoping and assessment often results in additional changes in the final list of issues included in the HIA. During scoping, the HIA team may produce an initial list, refine it on the basis of stakeholder input, and then make it final through research and analysis in the assessment phase. In other cases, the initial scope is generated by stakeholders and then refined through research and input from advisory or steering committees.
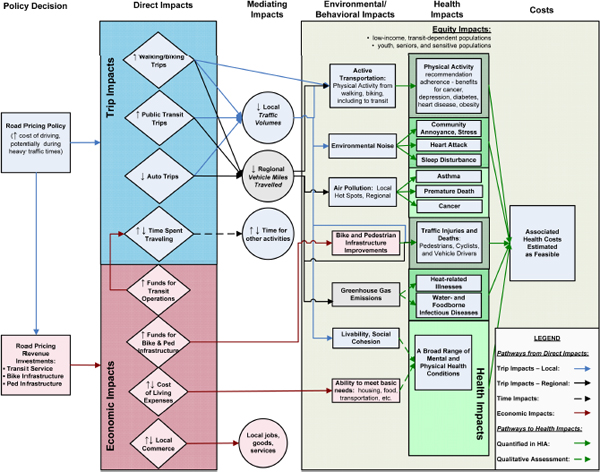
Several approaches for scoping are available. One approach uses a logic framework that maps out the causal pathways by which health effects might occur (see Figure 3-1). In general, this approach describes effects directly related to the proposal (such as changes in air emissions) and traces them to health determinants (such as air quality) and finally to health outcomes (such as asthma). The first step in the framework is typically a determinant of health, such as air pollution, traffic, employment, or noise. Logic frameworks can be used as part of stakeholder engagement to develop a shared understanding of how a project will develop and the outcomes that can be expected (Cave and Curtis 2001a,b; Cave et al. 2001). Another method of scoping is to develop a table that facilitates a systematic and rapid appraisal of all the potential ways in which a proposal might affect health (see Table 3-1). In this approach, the aspects of a proposal that may affect health are listed and considered in major categories of health and illness.
Box 3-2 provides an example of scoping for the HIA of a proposed development in Atlanta. The health issues were identified by determining the populations that would be affected and then considering how they would be affected. A variety of information was used to inform the process
Establishing Who Might Be Affected
Scoping identifies those likely to be affected by the proposed policy, project, program, or plan. The process may include identifying communities and geographic regions; demographic, economic, racial, and ethnic groups; and vulnerable populations, such as children, elderly people, disabled people, low-income people, racial and ethnic minorities, and people who have pre-existing health conditions. The process of describing pre-existing health issues, health disparities, and influences on health may also begin during scoping, although the full characterization of baseline health status generally takes place during assessment.
TABLE 3-1 Example of a Table Used for Systematic Scoping
| Potentially Affected Areas | Health Category | ||||
| Chronic Disease | Infectious Disease | Injury | Nutrition | Well-being or Psychosocial | |
| Environment • Air quality • Water quality • Soil • Other |
|||||
| Economy • Personal (income, employment; can include occupational risk) • Revenue or expense to local, state, or tribal government (support for or drain on services, infrastructure) |
|||||
| Infrastructure • Need for new roads and transit, water, or sanitation systems • Demand on existing infrastructure |
|||||
| Services • New services as a direct result of proposal • Drain on existing services resulting from proposed action |
|||||
| Demographics • Community composition • Traffic volume • Residential or commercial use patterns |
|||||
| Other | |||||
BOX 3-2 Scoping: Atlanta BeltLine HIA
As described by Ross (2007, p. 9), “the Atlanta BeltLine is a transit, trails, parks, and redevelopment project that uses a 22-mile loop of largely abandoned freight rail line that lies between two and four miles from the city center” and affects about 45 neighborhoods. In 2005, an HIA was conducted by a multidisciplinary team. The goal was to incorporate health considerations into the decision-making process “by predicting health consequences, informing decision makers and the public about health impacts, and providing realistic recommendations to prevent or mitigate negative health outcomes” (p. 9).
One of the first steps in identifying the parameters of the assessment was to establish an understanding of the BeltLine, a complex project that had been evolving for several years and was expected to be constructed over a 30-year period. The HIA team needed an authoritative description on which to base its assessment. The Atlanta Development Authority’s BeltLine Redevelopment Plan (November 2005) was identified as a coherent and publicly accepted vision that had been approved by local elected officials (ADA 2005). The source of public funding for the project was the Tax Allocation District (TAD), and only within the district’s boundaries could funding be collected and bond money spent. A variety of planning and zoning, funding, and environmental regulatory decisions were required for the BeltLine’s various components to be developed.
The HIA team was assisted by an advisory committee, but it appears that the committee was not involved in the scoping. The HIA report states that scoping was done by the HIA team and involved desk-based research and a web and postal survey. The scoping phase was used to identify the parameters of the assessment, the affected and most vulnerable populations, and potential key health effects. The final HIA report describes each factor (see below) and presents the results of the scoping. The entire decision-making process is appropriately not described in the final report; however, the reader is not told whether the HIA team prepared a scoping report or whether it presented the findings of the scoping stage.
Affected populations: As the TAD constituted only a portion of the city that would be directly affected, the HIA team created the HIA study area by placing a 0.5-mile buffer around the BeltLine TAD. The HIA study area was divided into five planning areas, and census (2000) and mortality data were used to analyze the population profiles. Variations were found in race, age, employment status, poverty, car ownership, and mortality. It was not possible to derive mortality rates for demographic subgroups. Behavioral Risk Factor Surveillance System data were used for the county and the state and stratified by race.
Most vulnerable populations: Less information was provided about this step. The most vulnerable populations were identified as people of low economic status, children, older adults, renters, and the carless. Calculations were conducted to develop a vulnerability score. The top 10% of the census tracts within the study area were then identified as locations of the most vulnerable populations.
Key health effects: Issues were identified through analysis of newspaper coverage; outreach to such groups as local officials, members of the public, and businesses; development of a logic framework; and a survey of people living, working, or attending school near the BeltLine. The HIA team identified the following critical issues that could affect the health of the study area population: access and social equity, physical activity, safety, social capital, and environment (including air quality, noise, and water management).
Source: Adapted from Ross 2007.
The HIA Team, Advisory Bodies, and Stakeholder Involvement
Scoping also determines who will be part of the HIA team and establishes a plan for technical oversight and review, stakeholder participation and involvement, and involvement of and interaction with decision-makers. Commonly, a core team is responsible for the bulk of writing and analysis. In some cases, the team may draw on outside consultants who have expertise in a specific health issue or method. Furthermore, HIA teams commonly rely on analyses by such experts as traffic-safety engineers or air-quality analysts who provide information on the links between the proposal and changes in health determinants.
Advisory, steering, and technical oversight committees are also commonly convened during scoping. Membership is variable but may include representatives of affected communities or community-based organizations, industrial proponents or business groups, public-health experts, officials involved in the decision-making process, and others who have a stake in the outcome. The committees may be convened for several purposes, including providing technical guidance or peer review, ensuring adequate and fair representation of diverse interests and priorities among stakeholders, communicating the results of the HIA to decision-makers, and developing recommendations that address community needs and are compatible with the specific legal requirements of the decision-making process.
Public and stakeholder participation during scoping can serve several important purposes, such as providing local knowledge regarding existing conditions and potential impacts, introducing alternatives or mitigation measures that stakeholders would endorse as effective ways to address key concerns, and allowing representative participation in shaping the terms of the HIA by groups affected by the proposal. Scoping also establishes a plan for stakeholder participation in later phases of the HIA. The early and central role of stakeholder identification and participation is analogous to the guidance provided in the report published by the Presidential/Congressional Commission on Risk Assessment and Risk Management (1997).
The approaches taken for stakeholder involvement vary widely. The variation partly reflects the wide array of applications of HIA; for example, it is not necessary or feasible to use the same approaches to involve stakeholders for a local project and for a high-level state or national policy. That issue is discussed at greater length in Chapter 4.
Data Sources and Methods
Scoping identifies appropriate data sources for the analysis and should also identify important data gaps. In some cases, the timeline and available resources will prevent collection of new data to address gaps that are identified. In others, scoping may identify studies that can be carried out by the HIA team or
studies that can be carried out by experts involved in some other aspect of the planning, permitting, or review process (such as air-quality or traffic-safety analysis). Scoping also establishes a plan for the analytic methods that will be used during the assessment phase. The specific methods used in assessment are discussed in depth in the next section.
Alternatives
Another issue that should be addressed in scoping is identifying alternatives to the proposed action. The cornerstone of an assessment that is conducted to comply with NEPA is the presentation of a set of reasonable alternatives to the proposed action; the assessment then considers the impacts of the proposed action and the alternatives. Assessing alternatives in parallel with the proposal can aid decision-making by highlighting tradeoffs and actions that can be taken to achieve the desired outcome while minimizing harms. Because HIA in the United States is often undertaken outside a formal legal mandate, it has not consistently included alternatives assessment. The committee concludes that when alternatives to the proposal being assessed are under consideration, the HIA team should assess the impacts of each alternative. Because developing an alternative (such as suggesting an alternate route for a proposed highway) involves many considerations that may be outside the purview and expertise of an HIA team, the committee recognizes that it may not be practical to expect the HIA team to develop alternatives independently. However, where practical, the HIA team should aim to evaluate a variety of alternatives or, minimally, to identify the characteristics of proposed actions that would be health-protective or detrimental to health. For example, although an HIA may not be able to incorporate engineering or economic specifications for alternate routes for a proposed highway, it could discuss factors that would influence health outcomes, such as indicating that a desirable route would be, for example, 100 m from any school or elderly facility or would not be proximate to high-population-density areas with a number of vulnerable people. It would then fall to the decision-makers to determine routes that met those criteria.
Outputs of Scoping
On the basis of its review of current guidance and practice, the committee recommends that scoping should result in a framework for the HIA and a written project plan that includes the following:
• An initial brief summary of the pathways through which health could be affected and the health effects to be addressed, including a rationale for how the effects were chosen and an account of any potential health effects that were considered but were not selected and why. Any logic models or scoping tables that were completed should also be included.
• Identification of the population and vulnerable groups—such as children, the elderly, racial or ethnic minorities, low-income people, and communities—that are likely to be affected.
• A description of the research questions, data sources, methods to be used, and any alternatives to be assessed.
• Identification of apparent data gaps and of data collection that could be undertaken to address the gaps or a rationale for not undertaking data collection.
• A summary of how stakeholders were engaged, the main issues that the stakeholders raised, and how they will be addressed or why they will not be addressed.
Committee Conclusions Regarding Scoping
The credibility and relevance of HIA to the decision-making process rest on a balanced and complete examination of the health risks, benefits, and tradeoffs presented by the project, policy, program, or plan being assessed. For that reason, it is important that scoping begin with a systematic consideration of all potential effects rather than limiting consideration to a subset of issues predetermined by the team’s research interests or regulatory requirements. Conversely, to have the greatest relevance as an informational and planning document and to ensure judicious use of resources, the HIA should ultimately focus on the health effects of greatest potential importance. Therefore, scoping should be thought of as a two-part process that starts with a systematic effort to identify all potentially important effects and that continues with selection of the most important and well-substantiated effects for further analysis at later stages.
Characteristics unique to the affected community may not be obvious to HIA practitioners who are outside the community. Stakeholders, however, may have insights into local conditions and potential solutions for addressing concerns raised by the proposal under consideration. Scoping should therefore entail a deliberative process that involves engagement of stakeholders. Review of literature and a consideration of the social, economic, and political context of the eventual decision are also important. In selecting the analytic methods that will be used, the HIA practitioner should consider not only technical limitations but what type of information will be most useful to decision-makers.
Finally, it is appropriate to include issues that are the subject of community concern even if they seem unlikely to be substantiated by further analysis. An HIA does not have to accept community concern uncritically. If the HIA is based on a thorough analysis, provides complete information so that community members are able to critique the analysis, and is conducted openly, it may provide reassurance to affected communities even if the conclusions do not support the community’s concerns.
Assessment
The assessment phase includes two tasks. The first is to create a profile of the population affected, which includes information on the demographics, baseline health status, and social, economic, and environmental conditions that are important to health. The second task is to analyze and characterize effects on health and its determinants for the proposal and for any alternatives under consideration relative to the baseline and to each other. As part of the assessment phase, a set of specific indicators that can be used to describe the baseline and potential changes in health status or health determinants should be developed. The committee notes that a variety of qualitative and quantitative approaches are often used to generate predictions, but regardless of the methods used, most available guidance emphasizes the importance of considering diverse forms of evidence, a consistent and unbiased approach to selecting and interpreting evidence, and a clear and transparent description of the analytic approach (WHO 1999; Mindell et al. 2008; Fredsgaard et al. 2009; Bhatia et al. 2010).
Given the broad scope of HIA practice settings, applications, and data sources, the committee chose not to develop specific standards or criteria for what constitutes “adequate” evidence or analysis for HIA. Other groups have developed “standard” approaches to promote and evaluate practice quality, including the quality of analysis (see, for example, Fredsgaard et al. 2009; Bhatia et al. 2010). Instead, the committee focused its review on the characterization of effects and the use of evidence, although several recommendations to improve the quality of analysis are discussed in Chapter 4.
Baseline Profile
The baseline profile characterizes the health status of affected populations and includes trends and factors (social, economic, and environmental) known to affect health. Assessing the baseline health status of the affected population provides a reference point with which the predicted changes in health status may be compared; it identifies any groups that could be more vulnerable than the general population to the impacts of the proposal; and it provides an understanding of the factors that are responsible for determining health in the affected communities, and this, in turn, allows for a better understanding of how any changes in those factors may affect health. In general, the baseline profile focuses on health issues and health determinants that may be affected by the proposal rather than on attempting to provide a complete assessment of community health.
Various sources of population-health statistics at the national, state, and local levels are available. But few data may be available on the geographic scale of some decisions addressed in an HIA, such as decisions related to projects that would affect a rural area or a single neighborhood. Moreover, disease rates in small populations can vary substantially, and it may not be possible to calculate
them reliably. In such cases, HIAs often rely on data on a larger region and consider whether the characteristics of the larger population can be generalized to the affected community.
Sources of information used in a baseline profile might include census data, hospital-discharge records, disease registries, and population and behavior surveys, such as the Behavioral Risk Factor Surveillance Survey, in which information is collected on different geographic scales. The baseline profile also generally draws on data that describe the social, economic, and environmental conditions important to health, such as labor or housing reports, environmental impact assessments, and gray or unpublished data specific to the decision context.
Developing a robust characterization of baseline health status and the social, economic, and environmental conditions important to health is a challenging aspect of HIA practice. In many cases, a complete and accurate description of health and its determinants in the affected community may not be possible. Some HIAs rely on proxy measures when rates of specific diseases are not available or are too small to calculate. For example, rather than providing an estimate of lung-cancer rates in a small community, an HIA might identify smoking rates and important sources of airborne pollutants in the community’s airshed. The committee notes that any limitations, incomplete data, and uncertainty in the baseline analysis should be clearly stated. New surveys to address data gaps or questions specific to the proposal in question are also common in comprehensive HIAs.
Characterization of Effects
Regardless of whether effects are quantified, the assessment stage should include a characterization of each effect to the greatest extent. Different HIA guides vary somewhat as to the specific descriptors that should be used, and practice is highly variable. The core issues that are commonly addressed are as follows:
• Nature—describes the effect and the causal pathway.
• Direction—indicates whether the effect is adverse or beneficial. In some cases, the direction of the effect may be unclear, or conflicting influences on a given health outcome may be identified (Harris et al. 2007).
• Intensity—indicates the severity of the effect (for example, fatal, disabling, or no disability).
• Magnitude—refers to the expected size of the effect and can be described by the number of people affected or by expected changes in the frequency or prevalence of symptoms, illness, or injury.
• Distribution—delineates the spatial and temporal boundaries of the effect and identifies various groups or communities that are likely to bear differential effects. This factor is important for ensuring that health equity is addressed.
Groups can be defined by age, sex, ethnicity, socioeconomic position, locational disadvantage, and health status or disability (Harris et al. 2007). Recognizing and addressing the effects of a proposal on health equity (or health disparities) between various groups has been seen as a core task of HIA, although HIA practice has sometimes been criticized for a lack of attention to health equity (Scott-Samuel 1996; WHO 1999; Harris et al. 2007).
• Timing and duration—indicates at what point of the proposed activity (such as construction vs operation of a new power plant) the effect will occur, how long it will last, and how rapidly the changes will occur; also discusses whether effects are reversible or permanent.
• Likelihood—refers to the chance or probability that the effect will occur.
• Confidence or certainty—characterizes the effect according to level of confidence or certainty in the prediction; that characterization is based on the strength of the evidence as described below.
Some HIA guides recommend using a matrix, such as those shown in Tables 3-2 and 3-3, to characterize effects (Harris et al. 2007; ICMM 2010). A matrix can be a useful way to organize a qualitative analysis and to convey results in a manner that is easy to understand, but a matrix may also be misinterpreted as being more objective than a simple description. It is important to note that a matrix does not explain how evidence was used to reach conclusions. A clear explanation should be provided with the characterization of effects that indicates the evidence used to develop the matrix and any limitations, data gaps, and uncertainties.
The committee notes that in addition to characterizing effects, HIAs may provide conclusions on the significance—or societal importance—of the effects, although this has been rare in U.S. practice. Assignment of significance rests on the characterization of an effect as described above, but judgments regarding what constitutes a significant impact are ultimately determined partly on the basis of social and political values.
Evidence and Approaches
Characterization of health effects in HIA relies on qualitative and quantitative evidence. The wide array of evidence includes public testimony on local conditions and concerns, interviews with key informants, surveys, epidemiologic analysis (for example, observational cross-sectional surveys, longitudinal studies, and intervention or experimental studies), measurement of physical environmental conditions and modeling (for example, modeling of infectious-disease propagation or dispersion of noise and air pollutants), and expert opinion. In many cases, the first course of action is to gather information from published literature, unpublished reports, administrative data gathered for routine
TABLE 3-2 Example of a Matrix for Analyzing Health Effects
| Main Health Outcome or Health Determinant | Health Outcome or Health Determinant Sub-Category | What is the health impact? | Who benefits? Who is negatively affected? Who is unaffected? | Pathway of health impact | Magnitude/consequence of impact | Likelihood/probability of impact | Significance of impact (Magnitude x Likelihood) | Degree of Confidence of the impact occurring |
| Positive, negative, uncertain or no effect | Whole population, vulnerable group Heath equity Cumulative impacts | How does the impact occur | Low Medium High | Low (possible) Medium (probable) High (definite) | Low Medium High | Low Medium High | ||
| Health Outcome | ||||||||
| Infectious disease | ||||||||
| Chronic disease | ||||||||
| Nutritional disorders | ||||||||
| Injury | ||||||||
| Mental health and well-being | ||||||||
| Health Determinant | ||||||||
| Individual/family | ||||||||
| Physiological | ||||||||
| Behaviour | ||||||||
| Socio-economic circumstances | ||||||||
| Environmental | ||||||||
| Physical | ||||||||
| Social | ||||||||
| Economic | ||||||||
| Institutional | ||||||||
| Organization of health care | ||||||||
| Other institutions | ||||||||
| Policies | ||||||||
Source: ICMM 2010. Reprinted with permission; copyright 2010, International Council on Mining and Metals.
TABLE 3-3 Example of a Table for Rating Importance of Health Effects
| Magnitude of impact | Likelihood of Occurrence of a Health Impact | |||
| Low | Medium | High | ||
| Health impact rating | Description | Unlikely to occur | Likely to occur sometimes | Likely to occur often |
| 0 | None | No significance | No significance | No significance |
| 1 | Low | Very low significance | Low significance | Medium significance |
| 2 | Medium | Low significance | Medium significance | High significance |
| 3 | High | Medium significance | High significance | High significance |
Source: ICMM 2010. Reprinted with permission; copyright 2010, International Council on Mining and Metals.
monitoring purposes, and other available documents. Such reviews of the existing literature are common. The degree to which they are systematic varies, and some authors have suggested frameworks and guidance for conducting systematic reviews (Mindell et al. 2004, 2010). The available data, however, may not be sufficient, and the HIA team may make a decision to dedicate resources to collection of new data. The use of various types of evidence and approaches used to make predictions are discussed below. The committee notes that each approach for gathering and interpreting data may be conducted in ways that are more or less participatory, engaging stakeholders in shaping the research questions, interpreting the findings, and developing recommendations on the basis of the findings.
Qualitative evidence provides a context-specific view of people’s lives. Qualitative data can be gathered through, for example, focus groups, one-on-one interviews, surveys, individual meetings with stakeholder organizations, testimony in community meetings, Web-based or other written input, and running a stand or exhibition in a public place. Participatory approaches that actively engage stakeholders in the process can yield rich information and provide opportunities for stakeholders—including community members—to influence the questions asked and to participate in the interpretation of findings. The approaches can provide useful information on how people view the proposal, that is, how it is expected to affect them and potentially improve or harm their quality of life. A central tenet is that people’s experience offers an invaluable perspective on the potential effects of the proposal.
The selection of qualitative and descriptive approaches will be informed by the scale and size of the proposal, the profile of the affected population, and the uses of the resulting information. Qualitative approaches can more easily present the causal pathways in terms used by participants; this ensures that different voices are presented in the HIA and can increase the legitimacy and stakeholder’s ownership of the process and results. Box 3-3 provides an example of an assessment step that was based on interviews with people who were likely
to be affected by a decision and that considered their impressions of the effects that industrial activities were having and were likely to continue to have on individual, family, and community life. The committee notes that qualitative social sciences and participatory-action research provide fertile ground for innovative methods for HIA. However, it is important to note that the use of qualitative approaches in HIA should not be interpreted as implying a need for less analytic rigor. As for any other research method, qualitative analysis in HIA should use appropriate methods and a clear, rigorous research design.
BOX 3-3 Assessment: Northeast National Petroleum Reserve-Alaska
In 1998, the Bureau of Land Management (BLM) completed a Northeast National Petroleum Reserve-Alaska Integrated Activity Plan/Environmental Impact Statement (EIS). BLM later considered amending the EIS to make additional public lands available for oil and gas leasing in the original 4.6-million-acre planning area. The local North Slope Borough government—an agency that participated in preparing the EIS—conducted an HIA, which was integrated into the EIS report.
The HIA drew on public testimony, literature review, and accepted mechanisms of health and illness to establish the scope of health concerns that should be considered. A logic framework was produced to guide the assessment. The associations between expected disturbances and changes in health were then analyzed in more depth to look at the alternatives proposed for the expansion and at the cumulative effects of oil exploration and extraction. The HIA team identified the pathways in which the expansion would affect the lives of the primarily Iñupiat residents of the area. Activities directly or indirectly associated with oil and gas—including aircraft traffic, seismic exploration, influx of nonresident workers, and emissions and discharges—were identified, and pathways were analyzed to consider their impacts on such problems as diet-related chronic illnesses (for example, diabetes and hypertension), food insecurity, and social pathology (for example, assault, alcohol and drug abuse, and violence). Those pathways and others were evaluated by using public-health data, literature on analogous populations, knowledge about accepted mechanisms of health and disease, witness testimony, and the effects analysis of other resources.
The discussion described pathways by which Iñupiat health was likely to be affected. For example, under Alternative A, diabetes and metabolic disorders would be expected to increase if impacts on subsistence led to declining subsistence harvests (through declining populations of subsistence resources, displacement of resources that made hunting less successful, or displacement of hunters by oil activity and infrastructure). It identified which areas and villages were most likely to be affected and when. The assessment also highlighted several potential benefits, such as “funding for infrastructure and health care; increased employment and income; and continued funding of existing infrastructure” (BLM 2007, p. 500). Because the biologists on the EIS team were uncertain of the degree to which subsistence harvests might be favorably or adversely affected, the HIA did not attempt to make quantitative estimates of the probability or intensity of the impact.
Public-health professionals reviewed the results of the analysis. On the basis of the findings, the HIA recommended a series of public-health mitigation measures that were selected to maximize any favorable impacts and to minimize harms.
Source: Adapted from BLM 2007 and Wernham 2007.
Quantitative evidence can include routinely collected information, such as mortality and census data, that can inform the baseline assessment. It can also include information from social-science and epidemiologic studies regarding the strength of associations between the social and physical environment (such as air and water quality and economic impacts) and health outcomes—information essential in the quantitative prediction of health effects. A large and growing body of quantitative evidence is available; where specific additional information is needed and resources are available, HIA teams may collect new quantitative data in the course of conducting an assessment.
If there is a causal relationship between variables, a valid estimate of effect size, and data on how a decision will change the prevalence of a health-related factor (exposure), it is possible to make quantitative predictions of effects (Fehr 1999; Veerman et al. 2005; Bhatia and Seto 2011). Potential health effects have been estimated by using established approaches for quantitative analysis, such as the calculation of the fraction of disease rates in a population that can be attributed to the risk being analyzed and the application of available exposure-response functions to quantify cancer risk associated with incremental changes in exposure to carcinogens. Additional modeling approaches, such as system-dynamic modeling and agent-based models, are also promising and emerging tools that could have applications to health. Box 3-4 provides several examples of topics that have been addressed in HIA by using quantitative methods.
Outputs of Assessment
Assessment should result in a report that
• Describes the baseline health status of the affected population with appropriate indicators, including prevalent health problems, health disparities, and social, economic, and environmental factors that affect health. The baseline should be focused on the issues that are likely to be affected by the proposal.
• Analyzes beneficial and adverse health effects and characterizes the changes in the indicators selected, to the extent possible, in terms of nature, direction, intensity, magnitude, distribution in the population, timing and duration, and likelihood.
• Integrates stakeholder input into the analysis of effects.
• Describes data sources and analytic methods and methods used to engage stakeholders.
• Identifies limitations and uncertainties clearly.
Committee Conclusions Regarding Assessment
The selection of analytic methods for HIA is driven by the complex pathways and the multiple, sometimes conflicting, influences on any given health
outcome and is also affected by the decision-making context. Decision-making is rarely based solely on scientific evidence but instead takes into account an array of political, economic, technical, and practical considerations. Decisions are often based on incomplete information and must often be made within a specified time rather than waiting for more complete information. By necessity, therefore, impact assessment is a pragmatic exercise and reflects a balance between scientific rigor and professional judgment. Expert judgment is central to HIA but must be grounded in a solid foundation of scientific neutrality and accepted public-health principles. An explicit statement of data sources, methods, assumptions, and uncertainty is essential, but uncertainty does not negate the value of the information. Even when there is substantial uncertainty, an assessment can illuminate potential causal pathways that—even when there appear to be conflicting influences on a specific outcome—can point the way toward a flexible framework for monitoring and managing any impacts that might occur as the proposal is implemented.
Literature review provides much of the empiric evidence for most HIAs, and whenever possible, assessors should conduct a systematic review of the literature for any health effects and determinants identified as high-priority issues in scoping. Failing to undertake a systematic review may mean overlooking evidence that would lead an assessor to a different conclusion. In practice, not all HIAs have conducted systematic literature reviews or documented review methods. If it is not possible to undertake complete, systematic literature reviews for an effect analyzed in an HIA, HIA practitioners must be vigilant to avoid selective searching and consideration of only studies that confirm particular conclusions (Mindell et al. 2004). However the literature review is conducted, the methods should be clearly described in the report, and any studies with conflicting results acknowledged.
BOX 3-4 Examples of Health and Behavioral Effects That Have Been Addressed Quantitatively in HIA
The bulleted list below provides examples in which some health impacts or behavioral outcomes have been quantified. The committee notes that in any assessment, it would be difficult or impossible to quantify all potential health impacts.
• Cancer risk associated with exposure to hazardous chemicals.
• Shortened life expectancy associated with air pollution.
• Injuries and fatalities associated with changes in vehicle traffic or speeds.
• Physical activity associated with changes in pedestrian infrastructure.
• Alcohol-consumption effects of alcohol taxes.
• Cancer risk and changes in life expectancy associated with tobacco taxes.
• HIV-AIDS infection risk associated with oil-pipeline construction.
• Life expectancy and physical function associated with income.
Sources: Veerman et al. 2005 and Bhatia and Seto 2011.
The reliability and validity of predictions made in HIAs have often been questioned (Thomson 2008). That issue will probably continue to challenge the credibility of HIA practice in the eyes of some audiences and highlights the need for continued research and refinement of methods to improve its value to decision-makers (Petticrew et al. 2006). Issues surrounding uncertainty, literature review, and reliability and validity of predictions are discussed in greater depth in Chapter 4.
Recommendations
Recommendations identify specific actions that could be taken to avoid, minimize, or mitigate harmful effects identified during the course of the HIA or to take maximal advantage of opportunities for a proposal to improve health. Depending on the nature of the proposal being assessed and the specific impacts, recommendations can take various forms (see Box 3-5), such as the following:
• A major alternative to a proposal (for example, routing a proposed highway away from a vulnerable population or building a light-rail line rather than widening a road).
• Mitigation measures that address a specific impact identified in the HIA and are intended to minimize a potential harm (for example, a measure to reduce benzene emissions from gas wells near residential areas) or measures to maximize a potential benefit.
• Health-supportive measures that would generally support health but are not tied directly to a specific impact (for example, building a clinic in an under-served neighborhood that would be adversely affected by emissions from a new freeway).
• Adopting a position for or against a proposal (for example, support for or opposition to a legislative proposal).
An HIA, however, might not provide any recommendations; this could occur if the HIA failed to reveal any important health effects. In some cases, the lack of a recommendation may reflect a desire to avoid a perception that the HIA is a one-sided advocacy exercise, particularly when options for recommendations would involve adopting a position wholly supportive of or opposed to the proposal being assessed.
The development of recommendations should be guided by a consideration of any available evidence regarding effectiveness. Such evidence may come from a review of published literature on interventions to address the health outcomes of concern. Or, in some cases, there may be unpublished evaluations of measures that have been implemented in similar scenarios. However, because few studies have directly assessed the impact of the implementation of policies, plans, programs, or projects on health outcomes, there may be little direct evi-
dence available with which to predict a given measure’s effectiveness. In those cases, the HIA team may need to rely on established principles of health promotion and disease prevention to develop approaches to minimizing or mitigating the identified effects. The committee emphasizes that the effectiveness of recommendations depends not only on the scientific validity of the interventions identified but on their relevance to the affected community’s concerns and their applicability within the regulatory or legislative framework of the proposal being considered. Chapter 4 discusses the extent to which an HIA can ensure the implementation of recommendations.
HIA recommendations take various forms, and some examples are provided below. The committee is not endorsing the HIAs or the recommendations, but simply providing examples.
• Alternative to a proposal. As described in Box 3-3, the HIA of oil and gas leasing in the National Petroleum Reserve-Alaska raised concerns regarding the potential for adverse effects on the culture, well-being, and health of local residents because of the risk of disrupting the local fish and game on which the community depends for food. All three leasing alternatives presented in the environmental impact statement raised similar concerns. To address the concerns, the North Slope Borough suggested restrictions on leasing in a small percentage of the area. The final decision by the Bureau of Land Management reflected a consideration of those concerns and deferred leasing in the most critical fishing and hunting areas, which represented a small percentage of the total area available for leasing (BLM 2008).
• Mitigation measures. An HIA of rezoning from industrial to residential use in San Francisco—a plan that would add 30,000 households—identified health-related noise and air-quality issues for the proposed residential units. It recommended new standards for ventilation and acoustical protection for new development. As a result, the city adopted performance-based regulations to ensure indoor-air quality and noise protections for all new residential development (Bhatia and Wernham 2008).
• Mitigation and health-supportive measures. An HIA of proposed oil development in Sakhalin Island, Russia, concluded that a large influx of oil and gas workers from outside the region could increase the risk of sexually transmitted illnesses in workers and the community. The HIA proposed mitigation measures (such as restricting access to the work camp by local residents) and health-supportive measures (such as “supporting the health community in improving STD programme management”) (Balint et al. 2003).
• Adopting a position for or against a proposal. An HIA of proposed restrictions in the funding for the Massachusetts rental-voucher program for low-income residents found that the restrictions could be harmful to health and recommended against them (Child Health Impact Working Group 2005).
Recommendations are often developed throughout the HIA process. It is common for mitigation measures and design alternatives to be considered during scoping, to be refined as the assessment phase further characterizes the impacts and identifies their importance, and to be made final during the recommendations phase. The process is analogous to the approach in the new risk-based decision-making framework proposed in Science and Decisions (NRC 2009), in which the primary objective of risk assessment is to help decision-makers choose among risk-management options by providing information on health risks that can be considered in the context of economic, social, and other factors. Similarly, HIA recommendations concern measures that can be taken to protect or improve health, but ultimately the decision-makers must weigh those recommendations with the political, economic, social, and technical factors that are relevant to the decision. In some cases, recommendations are developed by a decision-maker in response to an HIA report (Quigley et al. 2006). As discussed later in this section, recommendations can also establish a foundation for monitoring, and the results of the monitoring may indicate that the management strategies need to be adapted to respond to the observed outcomes—a process known as adaptive management (Johnson 1999).
The Roles of the Public and Decision-Makers
Public input while recommendations are being developed helps to ensure that proposed measures are locally relevant, address context-specific factors that might render them more or less effective, and address public concerns and hopes. The success of recommendations ultimately depends on the public’s trust in and support of them. For example, in Alaska, one of the adverse impacts of a proposed mine expansion was the feared contamination of water and wildlife, and evidence suggested that a fear of contamination might lead communities to shy away from eating a traditional diet. To address that concern, monitoring of concentrations of selected contaminants in local fish was proposed as a mitigation measure. Community input on the proposal suggested that for the program to reassure community members effectively, the monitoring should be conducted by an independent third party, and there should be strong community oversight at each stage.
Because decision-makers must eventually translate health-based recommendations into actionable measures (for example, by modifying legislation, drafting regulations or permit conditions, instituting new zoning requirements, or encouraging voluntary activities), regular communication between the HIA team and the decision-makers is important for the success of a proposed recommendation (EPA 2009). As in the realm of health risk assessment, there remains a need to distinguish between the assessment and management phases to avoid manipulation of analytic components by decision-makers. However, Science and Decisions (NRC 2009) emphasizes that a detailed understanding of the decision context is necessary for analyses to be scoped appropriately and that the concep-
tual distinction between assessment and management should not be interpreted as a firewall that prevents communication between parties. Having transparency throughout the process and clearly delineating the roles and responsibilities among various parties will help to limit real and perceived bias. Mechanisms to limit bias in decision-relevant analyses further are discussed in Chapter 4.
Health-Management Plan
HIA guidance often points out the need for monitoring and continuing management and verification that mitigation measures are being implemented. A plan for continuous monitoring, adaptation of mitigation measures, and verification of performance—although not currently a uniform aspect of HIA practice—helps to ensure that measures are carried out and achieving their objectives. Such a plan is often referred to as a public-health management plan or a health-action plan (Quigley et al. 2006). Recommendations form the core of a health-management plan, but the plan also determines authority for and assigns responsibility for implementing each recommendation, establishes a monitoring plan, and creates or suggests mechanisms to verify that assigned responsibilities are being met. Monitoring focuses on measures that are likely to be sensitive and early indicators of change. Selection of appropriate indicators will be discussed at greater length below in the section “Monitoring and Evaluation.”
The health-management plan suggests which stakeholder agency or entity could take responsibility for implementing each recommendation. Recommendations may be implemented through regulatory mandates or voluntary actions by stakeholders. Industrial proponents, government decision-making agencies, local health departments, and independent organizations (such as universities and nongovernment organizations) may all be in a position to implement measures recommended in the HIA.
Management of the health effects of a proposal as it moves from planning into implementation should be a dynamic process in which monitoring results may drive continued adaptation of the health-management plan. As noted above, the iterative process is known as adaptive management in the field of environmental management.
Outputs of Recommendations
The recommendations should be provided in the final HIA report and should document available supporting evidence, stakeholder input, and a health-management plan, which should do the following:
• Discuss what entity has the authority or ability to implement each measure and document any commitments to do so.
• Propose appropriate indicators for monitoring.
• Propose a system to verify that measures are being implemented as planned.
If no recommendations are made in the HIA report, an explicit rationale should be provided for the decision not to include them.
Committee Conclusions Regarding Recommendations
Making recommendations is a well-accepted part of HIA practice, but relatively little attention has been paid to how they should be formulated. The committee notes three considerations that may be particularly important for producing effective, actionable recommendations. First, community input is essential especially for proposals that will affect the local community primarily. Community input during the development of recommendations can ensure that they address specific aspects of living conditions and community design that may not be obvious to an outside researcher, and it provides an opportunity to ensure that the recommendations address high-priority issues in a manner that is acceptable to the affected community.
Second, recommendations are effective only if they are adopted and implemented. Adoption of recommendations depends partly on the involvement of decision-makers in the HIA process (Elliot and Francis 2005; Davenport et al. 2006). A gulf may exist between an intervention that is sound from a public-health perspective and one that is acceptable and can be acted on within the relevant regulatory or legal framework. Drafting measures that address identified public-health risks and that fulfill the requirements of the legal framework governing a decision will increase the chances that HIA recommendations are implemented. Drafting measures that can be readily incorporated into statutes, regulations, zoning provisions, or permit conditions with little adaptation may also increase chances of implementation. Collaboration with decision-makers or consultation with experts familiar with the legal or regulatory context may be the most effective way to ensure that recommendations are pragmatic and can be practically incorporated into the decision-making process.
Third, recommendations should include the elements of a health-management plan, including a consideration of appropriate indicators for monitoring, identification of entities that have the authority or ability to implement each measure, and a mechanism for verifying implementation and compliance. That permits recommendations to form the basis of effective implementation and management rather than merely providing a static system without the capacity to adapt. The process of implementing recommendations should be transparent and should include opportunities for public participation in the decision process and clear mechanisms of accountability.
As a final note, it is important to remember the context in which HIAs are conducted when considering the recommendations phase. As discussed at the beginning of this chapter, HIAs in the United States are often conducted without
a formal legal mandate and by an agency or organization that does not have decision-making authority. In practice, therefore, the HIA team will be asking a decision-maker to consider the findings and recommendations. The decision-maker must ultimately balance health considerations with the many technical, social, political, and economic concerns that bear on the proposal. The use of the information by the decision-maker is discussed at greater length in Chapter 4 in the section “Managing Expectations.”
Reporting
Reporting is the communication of the findings and recommendations of an HIA to decision-makers, the public, and other stakeholders. It includes the production and dissemination of written materials that document the HIA process, methods, findings, recommendations, and limitations of the analysis; and it includes the public dissemination of results through other channels, such as meetings with the public, decision-makers, and other stakeholders. The information generated by the HIA process needs to be organized and presented in such a way that it can be readily understood by the intended audiences and present a compelling case for recommended actions. Box 3-6 shows how the results of an HIA of proposals to provide paid sick days to employees were presented clearly in a report with appropriate acknowledgement of the strengths and weaknesses of the evidence. It also shows how HIA results can be disseminated widely in different formats through a number of channels. For example, HIA reports can be disseminated in hard copy, in electronic format, at public meetings, to focus groups, or at different stages in the HIA process or policy cycle. The committee notes that effective dissemination requires consideration of barriers—including those associated with language, availability of child care, disability, access to transportation, disenfranchisement, or literacy—and that multiple approaches may be required for disseminating a single HIA so that all appropriate audiences can be reached. That issue is addressed again in Chapter 4.
In some cases, the HIA process allows a period for formal public comment on a draft of the HIA report. The final draft responds to public comments and incorporates necessary changes or new information. The process mirrors the one set out by NEPA for an environmental impact statement, but the practice is far more variable for HIA. In other cases, a draft may be submitted to an internal body, such as a steering group, whose comments are incorporated into a final public version.
In practice, however, reporting may occur at earlier stages of the HIA process and include public meetings; meetings with decision-makers, other stakeholders, and advisers; and dissemination of interim public reports, such as a scoping summary. HIA is meant to assist decision-makers, so although the act of reporting is a formal step in the HIA process, it is also in the interest of decision-makers and the HIA team to keep in constant communication throughout the HIA process so that emerging results can be incorporated into the policy, plan, program, or project.
BOX 3-6 Reporting: Legislation on Paid Sick Days
The National Partnership for Women and Families commissioned Human Impact Partners and researchers at the San Francisco Department of Public Health to conduct an HIA of the federal Health Families Act of 2009, which would guarantee workers access to paid sick leave. The research was funded by the Annie E. Casey Foundation as an initiative with the potential to encourage long-term strategies and partnerships to strengthen families and communities. Human Impact Partners then worked with groups in other states to extrapolate the findings of the national report to local jurisdictions to analyze the health effects of paid sick days.
The report of the Healthy Families Act HIA provides a clear description of the steps in the analytic process. The key findings are provided in the opening section of the report, and they are categorized according to the strength of the evidence as “highly likely,” “likely but less well-supported by the available evidence,” and “plausible, but not well-supported.” For example, according to the report, a requirement for paid sick days is highly likely to lead to more workers taking leave to recuperate from an illness, to receive preventive care, or to care for ill children and dependents. It is also highly likely to lead to “improved compliance with public-health guidance regarding seasonal influenza and community mitigation strategies for pandemic influenza.” In contrast, effects that are likely but less well supported include increased ambulatory or preventive primary care, fewer emergency-room visits by workers who are insured, and greater compliance with infection-control policies. Finally, effects that are plausible but are not supported by available evidence include fewer hospitalizations because workers are able to receive the preventive primary care needed to maintain good health.
The results of the HIA were presented in different formats; the full report was accompanied by a summary and fact sheets. The findings of the HIA were covered by newspapers and Web sites in California, Maine, Massachusetts, and New Hampshire; and the HIA researchers were interviewed on radio. The press coverage recognized the tension between the burden that this new requirement would place on businesses and how the health of employees and the wider community are affected by people who work while they are ill. Human Impact Partners noted that many—including labor groups and funders—used the HIAs to assess work and family issues. The HIAs also changed the debate in such a way that providing paid sick days for employees began to be presented as a public-health issue rather than a labor issue. For example, the chair of the California Assembly Labor Committee referred to the HIA and “asked the opposition to the bill if they condoned the spread of disease through restaurant workers.”
Sources: Adapted from Cook et al. 2009; Human Impact Partners 2009a,b; AECF 2011.
The quality of the report can be a criterion by which the quality of the process is judged; that is, How clearly does the final document present the results of the analysis? It is critical to arrange the information logically so that readers can navigate easily through the document, to provide a lay summary that
accurately describes the main findings and conclusions of the study, and to reference all data and sources accurately (Fredsgaard et al. 2009).
Transparency of HIA
HIAs in the private sector are increasingly common, pursuant to internal corporate guidelines or requirements of lending banks, such as the International Finance Corporation and World Bank (see Appendix A for further discussion) (Birley 2005; IPIECA/OGP 2005; McHugh et al 2006; ICMM 2010; IFC 2007, 2010).3 Few, however, are made public. Disclosure requirements and practices vary considerably among development lenders and private-sector proponents. The World Bank and International Finance Corporation have policies governing the disclosure of information, and although the policies differ, both provide for withholding or excluding documents that might contain proprietary information or information whose disclosure could damage a client or lender’s financial, political, or legal interests (Halifax Initiative Coalition 2006; IFC 2006, 2010; McHugh et al. 2006; World Bank 2010). For private corporations undertaking an HIA, the decision of whether to make an HIA public and what to disclose may be governed by internal corporate policies, by the standards of lenders supporting the project, or by a government that has jurisdiction over the project (McHugh et al. 2006). A number of corporations and professional associations, such as the International Committee on Mining and Metals and the International Association of Oil and Gas Producers, have guidance for HIA, but relatively few completed industry-led HIAs or environmental, social, and health impact assessments are available on the Internet or on public Web sites that catalog HIA activity.
A related issue is incomplete disclosure—such as disclosure of only summary information without data or analysis, disclosure only by electronic media in communities unlikely to have access, and English-only reports. Incomplete disclosure may substantially limit access to complete information regarding the process, data sources, methods, and findings of an HIA for those who will be affected by the proposal being assessed (McHugh et al. 2006).
Failure to disclose HIA results and incomplete disclosure are not restricted to industry. Public agencies might not disclose or might redact or otherwise limit disclosure of information. Similarly, HIAs sponsored by private nonprofit organizations may not have requirements for disclosure inasmuch as most U.S. HIAs are not done under a legal mandate that requires disclosure. However, many HIA reports are available from public agencies, universities, and nonprofit organizations, and the committee found few examples of HIAs led or commis-
_________________
3The committee is referring here to HIAs sponsored or led by private-sector entities that are not part of any formal government process, such as a permitting or regulatory requirement. HIAs conducted as part of a formal government process are generally subject to disclosure and freedom-of-information requirements.
sioned by the private sector that were available. Given that HIA led by the private sector appears to be a rapidly increasing practice, the issue of availability bears further consideration.
Outputs of Reporting
The final HIA report should document the following:
• The nature of the proposal being assessed, including alternatives that were included in the analysis.
• The population, subgroups, vulnerable populations, and stakeholders likely to be affected and how they were involved in the HIA process.
• Data sources and analytic tools used.
• Findings of each stage of the HIA and a summary of outputs at the end of each stage.
In addition to a final report, stand-alone executive summaries or fact sheets can help to disseminate and communicate the findings and recommendations of an HIA to various key audiences.
Committee Conclusions Regarding Reporting
Across the field, there is little uniformity in the content of written HIA reports. The committee finds that an HIA report should at least describe the proposal and alternatives that are the subject of the HIA, the data sources and analytic methods used, the groups and individuals that were consulted in the course of the HIA, the process and findings of each step of the HIA, and the overall conclusions and recommendations. The HIA conclusions and recommendations should be presented in a manner that is clear and easily understood.
The committee recommends that HIAs be publicly released and disseminated. Although little has been written on the reasons for keeping HIA information confidential, the committee recognizes that there may be reasons for organizations conducting HIAs to decide not to disclose the results. For example, there may be concerns about risks to a proponent’s reputation or to the viability and public acceptance of a proposed project if a report discloses important unmitigated adverse impacts or potential impacts that are uncertain or for which strong evidence does not exist. There could also be concerns that disclosure of such information would lead to litigation. Furthermore, impact assessments, including HIAs, may rely on proprietary business information whose disclosure is legally barred or could damage a proponent’s business edge or competitiveness.
Notwithstanding those considerations, the committee considers the public disclosure of HIAs to be an important ideal of practice but recognizes that it may not be realistic to expect widespread disclosure in the absence of requirements or incentives for it. However, the committee notes that there are several benefits
of disclosure for industry, policy-makers, and the affected communities. First, disclosure informs affected communities and individuals and possibly other stakeholders, such as government agencies and officials, of possible effects on their health and well-being, a core objective of HIA. Second, it allows findings to be reviewed and improved. Third, it informs government agencies and officials of potential changes in demand for services, such as health care, emergency response, and public safety; this can facilitate an appropriate response. Fourth, disclosure of potential impacts may benefit industry by reducing the risk of litigation and by reducing tort liability by fulfilling requirements to warn those potentially responsible and potentially affected before the effects occur. Fifth, transparent reporting of possible environmental and health impacts has proved in many studies to lead to risk reduction because it motivates changes, such as improved pollution controls, on the part of industry and governments (Wolf 1996; Bennear and Olmstead 2008; Vaccaro and Madsen 2009). Sixth, because many established environmental risk factors are found at higher concentrations in vulnerable communities, disclosure of risks may be an important way to reduce health disparities and address concerns about environmental justice (Miranda et al. 2008). Seventh, disclosure allows people to take voluntary actions to avoid risk (Neidell 2009). For those reasons, the committee concludes that HIAs—including, to the extent practical, the data used for the analysis, analytic methods, assumptions, findings, uncertainties, data gaps, and recommendations—should be made public.
A well-designed dissemination strategy is critical for the success of an HIA. The dissemination strategy should be developed in a systematic manner, should consider what groups need or will rely on the information (including stakeholders and decision-makers), and should determine the most effective ways to present the information to these groups, taking into account any barriers or challenges.
Simply producing and disseminating a report may not be sufficient to secure adoption and implementation of HIA recommendations. Robust and continuing efforts to inform decision-makers of the findings and recommendations of the HIA and efforts by HIA practitioners and other stakeholders to champion choices that will benefit health can be an essential part of an effective HIA. Available studies suggest that efforts to involve and inform decision-makers throughout the HIA process and a strong relationship between the HIA team and decision-makers are often critical for the HIA’s effectiveness (Veerman et al. 2005; Morgan 2011). It is critical for the credibility of the HIA that the measures or outcomes being promoted are grounded in full and transparent consideration of the evidence that supports and does not support the issue in question. Efforts to support health-based recommendations must be carefully distinguished from biased efforts to promote a specific outcome or measure on the basis of an incomplete or inaccurately weighted comparison of favorable and unfavorable aspects of a proposal or of a predetermined political agenda. The committee recognizes that undue bias in an HIA may compromise its credibility and efficacy.
Monitoring and Evaluation
Monitoring and evaluation are often, although variably, described as the final stage of HIA (see Appendix E). Some have suggested that evaluation should be considered as outside the HIA process itself because of the need for an independent and objective perspective, particularly for impact evaluation (Bhatia et al. 2009). Several types of evaluation may be conducted on an HIA, including the following:
• Process evaluation. Considers whether the HIA was carried out according to the plan of action and applicable standards.
• Impact evaluation. Seeks to understand the impact of the HIA itself on the decision-making process or on other factors outside the specific decision being considered.
• Outcome evaluation. Focuses on the changes in health status or health indicators resulting from implementation of the proposal.
In practice, most HIAs do not include process, impact, or outcome evaluation; this has been attributed to a lack of interest, time, and resources in the case of process and impact evaluation and to the length of time (often many years) required for observing changes related to implementation. The discussion below briefly provides definitions and key features of HIA monitoring and evaluation.
Monitoring
As previously described in the section on “Recommendations,” monitoring can refer to tracking changes in health indicators as a new project or policy is implemented and has been defined as outcome monitoring. Indicators may be health outcomes in some cases, whereas health determinants may be more appropriate in others. For example, if a traffic-calming infrastructure was installed on a street that had a high rate of pedestrian injury, it may be appropriate to monitor injury rates directly because changes would be expected as soon as the installation was complete. In contrast, the effect of decisions on some health outcomes (such as cancer or obesity) may take years to occur and may have multiple contributing factors. In those cases, it may be more appropriate to monitor exposures—such as environmental concentrations of a carcinogen or the availability of safe walking corridors—that are linked to the outcome of interest by public-health evidence.
Process Evaluation
Process evaluation assesses the design and execution of the HIA in light of its intended purpose and plan of action and applicable practice standards. Proc-
ess evaluation can range from a simple self-assessment that is undertaken at the end of an HIA and focuses on a few variables that are relatively simple to describe, track, or measure—such as the methods used, degree of certainty of predictions, and approach to stakeholder engagement—to a more comprehensive case study that seeks to evaluate the HIA process holistically. Observing and documenting the HIA process—such as methods of engaging stakeholders and interacting with decision-makers and approaches to addressing analytic challenges—and interviewing participants and stakeholders are the main methods of process evaluation.
Impact Evaluation
Impact evaluation attempts to judge whether the HIA influenced the decision-making process, that is, whether and to what degree the recommendations were adopted and implemented and how the HIA influenced the decision-making process. It can also assess whether the HIA had other important effects, such as building new collaborations among agencies, ensuring that stakeholder perspectives were considered, and increasing awareness of previously unrecognized health considerations. In some cases, the impact of the HIA on a decision is clear-cut. For example, in the Alaskan oil and gas HIA mentioned in Box 3-3, the HIA team drafted recommendations in collaboration with the decision-maker, the Bureau of Land Management, which formally adopted the recommendations as mitigation measures.
In other cases, it may not be possible to attribute a particular decision to the influence of an HIA (Wismar et al. 2007). For example, in Oregon, an independent health-oriented nonprofit organization conducted an HIA of a series of proposals to reduce vehicle miles traveled in a bill intended to reduce greenhouse-gas emissions (UPH 2009). The enacted legislation is consistent with some of the recommendations of the HIA, but there were no data to evaluate whether those drafting the legislation were influenced by the recommendations; there were no interviews with legislators over the course of the legislative process (Human Impact Partners 2010). Observations that might indicate some influence of the HIA include discussion about HIA by legislators debating a proposal. In that case, a robust evaluation method, such as interviews conducted with decision-makers before and after the HIA, could provide the data needed to gauge the effect on decisions.
Impact evaluation can also help to determine an HIA’s effectiveness relative to the objectives set out during screening and scoping. In most cases, influencing decisions to protect or promote health is a central objective but by no means the sole outcome of value. As discussed above, additional benefits may include, for example (Wismar et al. 2007; Harris-Roxas and Harris 2011),
• Alerting decision-makers to the more general need to focus on health in future decisions.
• Developing new cross-disciplinary and interagency collaborations.
• Identifying data gaps and questions for future research.
• Establishing a foundation for appropriate monitoring.
• Ensuring that the public has accurate and complete information on adverse and beneficial effects.
• Developing new forecasting methods.
• Improving relationships and collaboration between stakeholders.
Outcome Evaluation
Whereas HIA aims to predict the effects of a decision before it occurs, outcome evaluation assesses whether the implementation of a decision has actual effects on health or health determinants (Parry and Kemm 2005). Outcome evaluation requires a suitable research design, ideally an appropriate comparison group, and data from the monitoring of health outcomes or of changes in health determinants as described above. The committee notes that outcome evaluation considers the effects of the whole decision, including changes made as a result of HIA recommendations. Thus, it is generally not possible to attribute outcomes specifically to HIA recommendations because they are implemented with the decision.
Evaluation of whether a decision has changed specific health outcomes may often be difficult or impossible because of the complex and multifactorial causal pathways involved in many health outcomes, the length of time from implementation of a decision to observable changes in health indicators, and the lack of suitable comparison groups (Quigley and Taylor 2004; Parry and Kemm 2005). However, in some cases, the relationships between the implemented decision and health determinants may be more direct and measurable. Because of the timeframe of proposal implementation and effects on health, outcome evaluation often requires a long-term research commitment. The committee notes that outcome evaluation of policy experiments is a field independent of HIA, and many large-scale social interventions—such as Head Start and Moving to Opportunity—have been subject to outcome evaluation that has included consideration of health or health determinants (Leventhal and Brooks-Gunn 2003; Schweinhart et al. 2005; Frank et al. 2006; Jagannathan et al. 2010). There are, however, no current examples of HIAs in the United States that include outcome evaluation as described here.
Outputs of Monitoring and Evaluation
Monitoring should provide information that allows one to conduct the evaluations noted above. An evaluation plan should have been developed early in the HIA process to guide selection of the appropriate methods for conducting
evaluations. An evaluation report should be produced at the conclusion of the HIA that includes the following:
• An evaluation of the HIA process against the HIA plan and applicable standards and consideration of whether the process used was appropriate given the decision-making context, needs, objectives, and resources available (a process evaluation).
• A description of the HIA’s impact on decision-making (to the extent that salient decisions have occurred by that time) as measured by an accounting of HIA recommendations that were adopted and an evaluation of available evidence that suggests whether and how the HIA played a role in decisions or contributed to changes in decision-makers’ knowledge, attitudes, or positions.
• A discussion of whether the HIA achieved its initial objectives.
• Acknowledgement of plans for future outcome evaluation or discussion of limitations that prevent such an evaluation.
Committee Conclusions Regarding Monitoring and Evaluation
Few HIA evaluation data have been published in the United States and relatively few elsewhere. The committee notes that some guides consider evaluation not as a step of HIA but rather as an independent practice that supports the development of the field (see Appendix E). Although completed HIA reports are readily available, peer-reviewed or gray literature that discusses the impacts of specific HIAs is still rare. Evaluation is important for the quality of individual HIAs and for the success of the HIA field as a whole. It is not reasonable to expect decision-makers to adopt HIA widely in the absence of evidence of its effectiveness and value. Consequently, the committee concludes that the lack of attention to evaluation is a barrier that will need to be overcome if HIA practice is to be advanced in the United States.
Evaluation can be thought of in two useful and complementary ways: self-evaluation of the HIA process and impacts and independent external evaluation. Self-evaluation performed by the HIA team—for example, against a set of process objectives or practice criteria—serves quality-assurance aims and can produce insights that will improve the field. Self-evaluation should be considered a valuable step of the HIA process. It may lack the objectivity and rigor of an external evaluation conducted by an experienced evaluator, but it is important because it contributes to a database that informs other efforts in the field and provides basic information about the applications of HIA, the methods and strategies used by HIA practitioners, and the success of and challenges to its use. In contrast, independent evaluation can yield unbiased insights about an HIA from the perspectives of stakeholders and decision-makers, can contribute to a more robust external peer review, and can provide rich information regarding the strengths, weaknesses, and most effective methods and approaches in the field.
The characteristics and approaches of evaluation should be chosen to fit the time, resources, and data available to the HIA team. Building evaluation into the plans for an HIA early in the process may support and reinforce a more deliberate and careful approach to designing and implementing the HIA itself. Although HIA may not always include or provide resources for independent evaluation, more in-depth, independent evaluation will generate more robust conclusions about HIA’s effectiveness and best practices in the field and should be given high priority. The committee considers self-evaluation and independent evaluation to be essential for moving the field ahead.
Outcome evaluation will continue to be challenging, but it can generate useful information in well-selected cases. Monitoring outcomes can in some cases help to test the validity of predictions and inform future analytic methods. Although there are many potential benefits of undertaking an HIA, one common objective is to inform decisions to promote changes that support improvements in health determinants or health outcomes. For that reason, it is important for the field to define the circumstances under which outcome evaluation may be practicable. Outcome evaluation should be undertaken when available resources and data will allow reasonable judgments regarding the association between the implementation of decisions and observed changes in health outcomes or health determinants.
SUMMARY: WHAT CRITERIA DEFINE A HEALTH IMPACT ASSESSMENT?
This chapter has described HIA categories, defined HIA, discussed current HIA practice, noted variations in practice, and provided the committee’s conclusions regarding each step of the HIA process. The discussion recognizes that the practice of HIA varies because it is adapted for use in different decision-making contexts. The variability also reflects a lack of clear criteria that define HIA as a distinct field. On the basis of its review of available literature, HIA guides, and practice standards, the committee has synthesized the key criteria that define HIA and that set it apart from related approaches to public-health practice and policy. Not all HIAs will meet all proposed criteria, but the criteria are intended to describe typical practice. Although deviation from the criteria may occur, a valid and clearly articulated rationale for such deviation should be described when the HIA is reported.
• Health impact assessment is conducted to inform a decision-making process and is intended to be concluded and communicated in advance of the decision that is being assessed.
• It develops the scope of health effects for analysis through systematic consideration of all factors associated with the proposed action that have a potential to influence health, and it narrows the scope to effects that are judged most important for health.
• It identifies a baseline that describes the health status of populations that will be affected by the decision.
• It characterizes health effects according to their nature, direction, intensity, magnitude, distribution, timing and duration, and likelihood.
• It uses the best available evidence to analyze effects on health and health disparities.
• It solicits and responds to input from stakeholders throughout all stages of the process and includes publicly available and accessible documentation of processes, products, and sponsors.
• It recommends measures, in the context of the proposed action, to protect and promote health and reduce health disparities.
• It follows a systematic process that includes screening, scoping, assessment, recommendations, reporting, and monitoring and evaluation.
AECF (Annie E. Casey Foundation). 2011. About the Annie E. Casey Foundation, Baltimore, Maryland March 2011[online]. Available: http://www.aecf.org/~/media/Pubs/Other/A/AboutCasey/031111_88952_Aboutcasey.pdf [accessed May 13, 2011].
ADA (Atlanta Development Authority). 2005. Atlanta BeltLine Redevelopment Plan. Atlanta Development Authority. November 2005 [online]. Available: http://www.atlantada.com/media/CoverandTableofContents.pdf [accessed Jan. 24, 2011].
Balint, J., P. Boelens, and M. Debello. 2003. Pp. 97-116 in Health Impact Assessment: SEIC (Sakhalin Energy Investment Company) Phase 2 Development. World Health Organization [online]. Available: http://www.who.int/hia/examples/energy/en/HIA_Chps13_18.pdf [accessed July 29, 2011].
Bennear, L.S., and S.M. Olmstead. 2008. The impacts of “right-to-know:” Information disclosure and the violation of drinking water standards. J. Environ. Econ. Manage. 56(2):117-130.
Bhatia, R. 2010. A Guide for Health Impact Assessment. California Department of Public Health. October 2010 [online]. Available: http://www.cdph.ca.gov/pubsforms/Guidelines/Documents/HIA%20Guide%20FINAL%2010-19-10.pdf [accessed Apr. 22, 2011].
Bhatia, R., and E. Seto. 2011. Quantitative estimation in Health Impact Assessment: Opportunities and challenges. Environ. Impact Assess. Rev. 31(3):301-309.
Bhatia, R., and A. Wernham. 2008. Integrating human health into environmental impact assessment: An unrealized opportunity for environmental health and justice. Environ. Health Perspect. 116(8): 991-1000.
Bhatia, R., L. Farhang, M. Gaydos, K. Gilhuly, B. Harris-Roxas, J. Heller, M. Lee, J. McLaughlin, M. Orenstein, E. Seto, L. St. Pierre, A.L. Tamburrini, A. Wernham, and M. Wier. 2009. Practice Standards for Health Impact Assessment (HIA), Version 1. North American HIA Practice Standards Working Group, Oakland, CA. April 2009 [online]. Available: http://www.habitatcorp.com/whats_new/HIA_Practice_Standards_040709_V1.pdf [accessed May 17, 2011].
Bhatia, R., J. Branscomb, L. Farhang, M. Lee, M. Orenstein, and M. Richardson. 2010. Minimum Elements and Practice Standards for Health Impact Assessment (HIA), Version 2. North American HIA Practice Standards Working Group, Oakland, CA.
November 2010 [online]. Available: http://www.sfphes.org/HIA_Tools/HIA_Practice_Standards.pdf [accessed May 23, 2011].
Birley, M. 2005. Health Impact Assessment in multinationals: A case study of the Royal Dutch/Shell Group. Environ. Impact Assess. Rev. 25(7-8):702-713.
BLM (Bureau of Land Management). 2007. Northeast National Petroleum Reserve-Alaska (NPR-A) Draft Supplemental Integrated Activity Plan/Environmental Impact Statement (IAP/EIS). U.S. Department of the Interior, the Bureau of Land Management [online]. Available: http://www.blm.gov/ak/st/en/prog/planning/npra_general/ne_npra/northeast_npr-a_draft.html [accessed Nov. 30, 2010].
BLM (Bureau of Land Management). 2008. Northeast National Petroleum Reserve-Alaska, Supplemental Integrated Activity Plan, Record of Decision. U.S. Department of the Interior, the Bureau of Land Management [online]. Available: http://www.blm.gov/pgdata/etc/medialib/blm/ak/aktest/planning/ne_npra_final_supplement.Par.91580.File.dat/ne_npra_supp_iap_rod2008.pdf. [accessed July 29, 2011].
Castro, A., L. Chen, B. Edison, J. Huang, K. Mitha, M. Orkin, Z. Tejani, D. Tu, L. Wells, and J. Yeh. 2010. Santa Monica Airport Health Impact Assessment (HIA): A Health-Directed Summary of the Issues Facing the Community near the Santa Monica Airport. UCLA Community Health and Advocacy Training Program. February 2010 [online]. Available: http://www.hiaguide.org/sites/default/files/SM_Airport_Health_Impact_Assessment.pdf [accessed May 16, 2011].
Cave, B., and S. Curtis. 2001a. Developing a practical guide to assess the potential health impact of urban regeneration schemes. Promot. Educ. 8(1):12-16.
Cave, B., and S. Curtis. 2001b. Health Impact Assessment for Regeneration Projects, Vols. I and III. Breaking the Cycle, East London and the City Health Action Zone and Queen Mary, University of London, London [online]. Available: http://www.bcahealth.co.uk/links-internal.html [accessed May 16, 2011].
Cave, B., S. Curtis, A. Coutts, and M. Aviles. 2001. Health Impact Assessment for Regeneration Projects. Vol. II. Selected Evidence Base. Breaking the Cycle, East London and the City Health Action Zone and Queen Mary, University of London, London [online]. Available: http://www.bcahealth.co.uk/links-internal.html [accessed May 16, 2011].
Child Health Impact Working Group. 2005. Affordable Housing and Child Health: A Child Health Impact Assessment of the Massachusetts Rental Voucher Program. Child Health Impact Working Group, Boston, MA. June 2005 [online]. Available: http://www.healthimpactproject.org/resources/document/massachusetts-rentalvoucher-program.pdf [accessed July 29, 2011].
Cole, B.L., and J.E. Fielding. 2007. Health impact assessment: A tool to help policy makers understand health beyond health care. Annu. Rev. Public Health 28:393-412.
Cole, B.L., M. Wilhelm, P.V. Long, J.E. Fielding, G. Kominski, and H. Morgenstern. 2004. Prospects for health impact assessment in the United States: New and improved environmental impact assessment or something different? J. Health Polit. Policy Law 29(6):1153-1186.
Cole, B.L., R. Shimkhada, J.E. Fielding, G. Kominski, and H. Morgenstern. 2005. Methodologies for realizing the potential of health impact assessment. Am. J. Prev. Med. 28(4):382-389.
Cook, W.K., J. Heller, R. Bhatia, and L. Farhang. 2009. A Health Impact Assessment of the Healthy Families Act of 2009. Human Impact Partners and San Francisco Department of Public Health. June 2009 [online]. Available: http://www.humanimpact.org/component/jdownloads/finish/5/68 [accessed May 16, 2011].
Davenport, C., J. Mathers, and J. Parry. 2006. Use of health impact assessment in incorporating health considerations in decision making. J. Epidemiol. Community Health 60(3):196-201.
DHHS (U.S. Department of Health and Human Services). 2010. Healthy People. Office of Disease Prevention and Health Promotion, U.S. Department of Health and Human Services [online]. Available: http://www.healthypeople.gov/2010/ [accessed May 17, 2011].
EC (European Communities). 2001. Directive 2001/42/EC of the European Parliament and of the Council of 27 June 2001 on the assessment of the effects of certain plans and programmes on the environment. O.J. Eur. Comm. L 197:30-37.
Elliott, E., and S. Francis. 2005. Making effective links to decision-making: Key challenges for health impact assessment. Environ. Impact Assess. Rev. 25(7-8):747-757.
EPA (U.S. Environmental Protection Agency). 1989. Risk Assessment Guidance for Superfund, Vol. 1. Human Health Evaluation Manual Part A. EPA/540/1-89/002. Office of Emergency and Remedial Response, U.S. Environmental Protection Agency, Washington, DC. December 1989 [online]. Available: http://rais.ornl.gov/documents/HHEMA.pdf [accessed June 8, 2011].
EPA (U.S. Environmental Protection Agency). 1992. Framework for Ecological Risk Assessment. EPA/63-R-92/001. Risk Assessment Forum, U.S. Environmental Protection Agency, Washington, DC. February 1992.
EPA (U.S. Environmental Protection Agency). 2009. Red Dog Mine Extension Aqqaluk Project. Final Supplemental Environmental Impact Statement. Prepared for U.S. Environmental Protection Agency, Seattle, WA, by Tetra Tech, Inc., Anchorage, AK. October 2009 [online]. Available: http://www.reddogseis.com/Docs/Final/Front_Matter.pdf [accessed Nov. 30, 2010].
Fehr, R. 1999. Environmental health impact assessment: Evaluation of a 10 step model. Epidemiology 10(5):618-625.
Frank, D.A., N.B. Neault, A. Skalicky, J.T. Cook, J.D. Wilson, S. Levenson, A.F. Meyers, T. Heeren, D.B. Cutts, P.H. Casey, M.M. Black, and C. Berkowitz. 2006. Heat or eat: The Low Income Home Energy Assistance Program and nutritional and health risks among children less than 3 years of age. Pediatrics 118(5):e1293-e1302.
Fredsgaard, M.W., B. Cave, and A. Bond. 2009. A Review Package for Health Impact Assessment Reports of Development Projects. Leeds, UK: Ben Cave Associates Ltd [online]. Available: http://www.bcahealth.co.uk/pdf/hia_review_package.pdf.
Halifax Initiative Coalition. 2006. One Step Forward, One Step Back: An Analysis of the IFC’s Sustainability Policy, Performance Standards and Disclosure. Ottawa, Canada: Halifax Initiative Coalition [online]. Available: http://www.ifc.org/ifcext/policyreview.nsf/AttachmentsByTitle/HalifaxReport/$FILE/IFC-Analysis-HI-Final.pdf [accessed Feb. 3, 2011].
Harris, P., B. Harris-Roxas, E. Harris, and L. Kemp. 2007. Health Impact Assessment: A Practical Guide. Sidney, Australia: Centre for Health Equity Training, Research and Evaluation, the University of New South Wales. August 2007 [online]. Available: http://www.hiaconnect.edu.au/files/Health_Impact_Assessment_A_Practical_Guide.pdf [accessed May 9, 2011].
Harris-Roxas, B., and E. Harris. 2011. Differing forms, differing purposes: A typology of health impact assessment. Environ. Impact Assess. Rev. 31(4):396-403.
Heller, J., J. Lucky, and W.K. Cook. 2009. Crossings at 29th St. / San Pedro St. Area Health Impact Assessment. Human Impact Partners, Oakland, California [online].
Available: http://www.hiaguide.org/sites/default/files/Crossings_LA_29thSt_HIA_FullReport.pdf [accessed May 17, 2011].
Human Impact Partners. 2009a. Newsroom: Paid Sick Days HIAs. Human Impact Partners [online]. Available: http://www.humanimpact.org/press [accessed May 16, 2011].
Human Impact Partners. 2009b. Past Projects: Paid Sick Days Legislation. Human Impact Partners [online]. Available: http://www.humanimpact.org/past-projects [accessed May 16, 2011].
Human Impact Partners. 2010. Past Projects: Vehicle Miles Traveled Legislation. Human Impact Partners [online]. Available: http://www.humanimpact.org/past-projects [accessed May 24, 2011].
ICMM (International Council on Mining and Metals). 2010. Good Practice Guidance on Health Impact Assessment. London, UK: International Council on Mining and Metals [online]. Available: http://www.icmm.com/page/35457/good-practice-guidance-on-health-impact-assessment [accessed May 16, 2011].
IFC (International Finance Corporation). 2006. Policy on Disclosure of Information. International Finance Corporation. April 30, 2006 [online]. Available: http://www.ifc.org/ifcext/enviro.nsf/AttachmentsByTitle/pol_Disclosure2006/$FILE/Disclosure2006.pdf [accessed May 17, 2011].
IFC (International Finance Corporation). 2007. Guidance Note 4. Community Health, Safety and Security. International Finance Corporation. July 31, 2007 [online]. Available: http://www.ifc.org/ifcext/sustainability.nsf/AttachmentsByTitle/pol_GuidanceNote2007_4/$FILE/2007+Updated+Guidance+Note_4.pdf [accessed Feb. 3, 2011].
IFC (International Finance Corporation). 2010. International Finance Corporation Performance Standard 4 – Rev -0.1. Community Health, Safety, and Security. International Finance Corporation. April 14, 2010 [online]. Available: http://www.ifc.org/ifcext/policyreview.nsf/AttachmentsByTitle/Phase2_PS4_English_clean/$FILE/CODE_Progress+Report_AnnexB_PS4_Clean.pdf [accessed Feb. 3, 2011].
IPIECA/OGP (International Petroleum Industry Environmental Conservation Association and International Association of Oil and Gas Producers). 2005. A Guide to Health Impact Assessments in the Oil and Gas Industry. International Petroleum Industry Environmental Conservation Association, and International Association of Oil and Gas Producers [online]. Available: http://www.hiaconnect.edu.au/files/HIA_in_OG.pdf [accessed May 17, 2011].
Jagannathan, R., M.J. Camasso, and U. Sambamoorthi. 2010. Experimental evidence of welfare reform impact on clinical anxiety and depression levels among poor women. Soc. Sci. Med. 71(1):152-160.
Johnson, B.L. 1999. The role of adaptive management as an operational approach for resource management agencies. Conserv. Ecol. 3(2):8 [online]. Available: http://www.ecologyandsociety.org/vol3/iss2/art8/ [accessed May 24, 2011].
Kemm, J. 2001. Health impact assessment: A tool for healthy public policy. Health Promot. Int. 16(1): 79-85.
Kuo, T., C.J. Jarosz, P. Simon, and J.E. Fielding. 2009. Menu labeling as a potential strategy for combating the obesity epidemic: A health impact assessment. Am. J. Public Health 99(9):1680-1686.
Lester, C., S. Hayes, S. Griffiths, G. Lowe, and S. Hopkins. 1999. Implementing a strategy to address health inequalities: A health authority approach. Public Health Med. 1(3):90-93.
Leventhal, T., and J. Brooks-Gunn. 2003.Moving to opportunity: An experimental study of neighborhood effects on mental health. Am J Public Health 93(9):1576-1582.
McAuliffe, M. 2009. Developers of Proposed Springfield Biomass Plant tell Public Health Council: “Nothing Less Than the Best”. The Republican, December 2, 2009. MassLive.com [online]. Available: http://www.masslive.com/news/index.ssf/2009/12/developers_of_proposed_springf.html [accessed May 19, 2011].
McHugh, S, S. Maruca, J. Lilien, and A. Manning. 2006. Environmental, Social and Health Impact Assessment (ESHIA) Process. Paper No. 98224-MS. SPE International Health, Safety & Environment Conference, 2-4 April 2006, Abu Dhabi, UAE. Society of Petroleum Engineers.
Mindell, J., E. Ison, and M. Joffe. 2003. A glossary for health impact assessment. J. Epidemiol. Community Health 57(9):647-651.
Mindell, J., A. Boaz, M. Joffe, S. Curtis, and M. Birley. 2004. Enhancing the evidence base for health impact assessment. J. Epidemiol. Community Health 58(7):546-551.
Mindell, J.S., A. Boltong, and I. Forde. 2008. A review of health impact assessment frameworks. Public Health 122(11):1177-1187.
Mindell, J., J. Biddulph, L. Taylor, K. Lock, A. Boaz, M. Joffe, and S. Curtis. 2010. Improving the use of evidence in health impact assessment. Bull. World Health Organ. 88(7):543-550.
Miranda, M.L., M.H. Keating, and S.E. Edwards. 2008. Environmental justice implications of reduced reporting requirements of the Toxics Release Inventory Burden Reduction Rule. Environ. Sci. Technol. 42(15):5407-5414.
Morgan, R.K. 2011. Health and impact assessment: Are we seeing closer integration? Environ. Impact Assess. Rev. 31(4):404-411.
Neidell, M. 2009. Information, avoidance behavior, and health: The effect of ozone on asthma hospitalizations. J. Human Res. 44(2):450-478.
NRC (National Research Council). 1983. Risk Assessment in the Federal Government: Managing the Process. Washington, DC: National Academy Press.
NRC (National Research Council). 1996. Understanding Risk: Informing Decisions in a Democratic Society. Washington, DC: National Academy Press.
NRC (National Research Council). 2009. Science and Decisions: Advancing Risk Assessment. Washington, DC: National Academies Press.
Parry, J., and A. Stevens. 2001. Prospective health impact assessment: Pitfalls, problems, and possible ways forward. BMJ 323(7322):1177-1182.
Parry, J.M., and J.R. Kemm. 2005. Criteria for use in the evaluation of health impact assessments. Public Health 119(12):1122-1129.
Petticrew, M., S. Cummins, L. Sparks, and A. Findlay. 2006. Validating health impact assessment: Prediction is difficult (especially about the future). Environ. Impact Assess. Rev. 27(1):101-107.
PHAC (Public Health Advisory Committee). 2005. A Guide to Health Impact Assessment: A Policy Tool for New Zealand, 2nd Ed. Wellington, New Zealand: PHAC [online]. Available: http://www.phac.health.govt.nz/moh.nsf/pagescm/764/$File/guidetohia.pdf [accessed May 9, 2011].
Presidential/Congressional Commission on Risk Assessment and Risk Management. 1997. Framework for Environmental Health Risk Management – Final Report, Vol. 1. [online]. Available: http://www.riskworld.com/nreports/1997/risk-rpt/pdf/EPAJAN.pdf [accessed July 28, 2011].
Quigley, R.J., and L.C. Taylor. 2004. Evaluating health impact assessment. Public Health. 118(8):544-552.
Quigley, R., L. den Broeder, P. Furu, A. Bond, B. Cave, and R. Bos. 2006. Health Impact Assessment: International Best Practice Principles. Special Publication Series No. 5. Fargo: International Association for Impact Assessment. September 2006 [online]. Available: http://www.iaia.org/publicdocuments/special-publications/SP5.pdf [accessed May 6, 2011].
Roscam Abbing, E.W. 2004. HIA and national policy in the Netherlands. Pp. 177-189 in Health impact Assessment: Concepts, Theory, Techniques and Applications, J. Kemm, J. Parry, and S. Palmer, eds. Oxford: Oxford University Press.
Ross, C.L. 2007. Atlanta Beltline: Health Impact Assessment. Center for Quality Growth and Regional Development, Georgia Institite of Technology, Atlanta, GA [online]. Available: http://www.healthimpactproject.org/resources/document/Atlanta-Beltline.pdf [accessed May 18, 2011].
Schweinhart, L.J., J. Montie, Z. Xiang, W.S. Barnett, C.R. Belfield, and M. Nores. 2005. Lifetime Effects: The High/Scope Perry Preschool Study through Age 40. Ypsilanti, MI: High/Scope Press.
Scott-Samuel, A. 1996. Health impact assessment. BMJ 313(7051):183-184.
SFCC (Federation of Swedish County Councils). 1998. Focusing on Health: How Can the Health Impact of Policy Decisions be Assessed? Federation of Swedish County Councils, Stockholm, Sweden [online]. Available: http://www.lf.se/hkb/engelskversion/general.htm.
SFDPH (San Francisco Department of Public Health). 2011. Assessing the Health Impacts of Road Pricing Policy Proposals. Program on Health Equity and Sustainability, San Francisco Department of Public Health [online]. Available: http://www.sfphes.org/HIA_Road_Pricing.htm [accessed July 8, 2011].
Steinemann, A. 2000. Rethinking human health impact assessment. Environ. Impact Assess. Rev. 20(6):627-645.
Thomson, H. 2008. HIA forecast: Cloudy with sunny spells later? Eur. J. Public Health 18(5):436-438.
UPH (Upstream Public Health). 2009. Health Impact Assessment on Policies Reducing Vehicle Miles Traveled in Oregon Metropolitan Areas. Upstream Public Health [online]. Available: http://www.upstreampublichealth.org/publications?type=reports [accessed June 13, 2011].
Vaccaro, A., and P. Madsen. 2009. Corporate dynamic transparency: The new ICT-driven ethics? Ethics Inform. Technol. 11(2):113-122.
Veerman, J., J. Barendregt, and J. Mackenback. 2005. Quantitative health impact assessment: Current practice and future directions. J. Epidemiol. Community Health. 59(5):361-370.
Wernham, A. 2007. Inupiat health and proposed Alaskan oil development: Results of the first Integrated Health Impact Assessment/Environmental Impact Statement of proposed oil development on Alaska’s North Slope. EcoHealth 4(4):500-513.
Wernham, A. 2011. Health impact assessments are needed in decision making about environmental and land-use policy. Health Aff. 30(5):947-956.
WHO (World Health Organization). 1999. Health Impact Assessment: Main Concepts and Suggested Approaches-the Gothenburg Consensus Paper. Brussels: European Centre for Health Policy, WHO Regional Office for Europe.
Wismar, M., J. Blau, K. Ernst, and J. Figueras. 2007. The effectiveness of Health Impact Assessment: Scope and Limitations of Supporting Decision-Making in Europe.
Copenhagen: World Health Organization [online]. Available: http://www.euro.who.int/__data/assets/pdf_file/0003/98283/E90794.pdf [accessed May 18, 2011].
Wolf, S. 1996. Fear and loathing about the public right to know: The surprising success of the emergency planning and community Right-to-Know Act. J. Land Use Environ. Law 11(2)217-325.
World Bank. 2010. The World Bank Policy on Access to Information. Document No. 54873. World Bank. July 1, 2010 [online]. Available: http://www-wds.worldbank.org/external/default/WDSContentServer/WDSP/IB/2010/06/03/000112742_20100603084843/Rendered/PDF/548730Access0I1y0Statement01Final1.pdf [accessed May 18, 2011].