Financing Mission-Critical Investments in Public Health Capacity Development
INTRODUCTION
The Institute of Medicine (IOM) committee on Public Health Strategies to Improve Health is charged with examining ways to strengthen the public health system in three separate but related areas: measurement, the law, and funding. The committee commissioned this paper to inform its deliberations regarding optimal mechanisms for financing the governmental public health infrastructure in a manner that will best support the needs of the public during and after health care reform. Based on guidance from the committee, this paper seeks to
• identify and describe priority investments in public health capacity that promise to strengthen the ability of state and local public health agencies to adopt an ecologically oriented, population-based approach to disease prevention and health promotion that addresses the broad socioenvironmental determinants of health;
• explore the extent to which categorical financing mechanisms have influenced the capacity deficits observed in these mission-critical areas; and
• examine the funding sources that have been successfully used by innovative public health agencies at the state and local level to finance these capacity-development priorities.
DEFINITIONS AND METHODS
For the purposes of this effort, the term capacity conveys a deliberately broad and flexible concept—the various attributes that enable the governmental public health infrastructure to pursue its mission of promoting physical and mental health and preventing disease, injury, and disability. As described in the committee’s first report, For the Public’s Health: The Role of Measurement in Action and Accountability, the governmental public health infrastructure comprises public health agencies at local, state, and federal levels and represents a relatively small—yet integral—component of the overall health system (see Figure C-1). This infrastructure is composed of three major components: (1) the public health workforce, (2) data and information systems, and (3) organizational capabilities to assess and respond to public health needs (Baker et al., 2005).
Capacities lie at the heart of the logic model the committee has developed to illustrate the series of steps linking inputs to outcomes in population health and represent the critical link between resources and processes (see Figure C-2). As such, the term capacity may be used to signify system attributes necessary to successfully implement particular actions in order to achieve particular goals (optimal capacity), or the term may be used to describe the manner in which resources are actually deployed and aligned (existing capacity). This paper focuses specifically on capacity within governmental public health agencies at the state and local level, while recogniz-
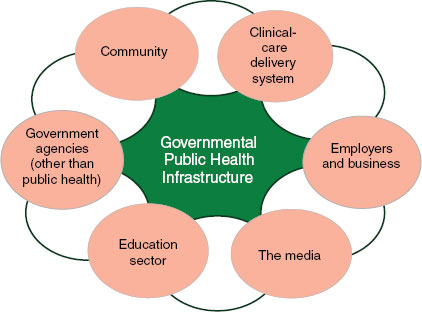
FIGURE C-1 The health system.
SOURCE: IOM, 2011.
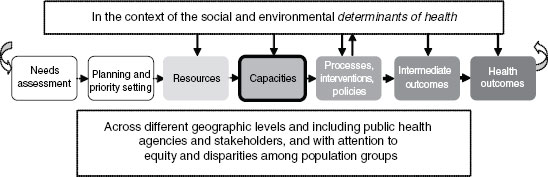
FIGURE C-2 Logic model.
SOURCE: IOM, 2011.
ing the broader systemic context in which these public-sector organizations operate. In light of the interstitial role played by governmental public health, the specific capacities needed for optimal performance of public-sector agencies are somewhat contingent on the nature and contributions of other health system partners, as well as population health needs.
The term capacity-development needs or capacity deficits represent those attributes of optimal capacity determined to be inadequate in, or missing from, the existing capacity. The evidence base surrounding both the definition of optimal public health capacity and documentation of existing capacity levels is extremely limited (Beitsch et al., 2006; Bhandari et al., 2010; Erwin, 2008; Mays et al., 2009; Scutchfield et al., 2004, 2009). Therefore capacity-development needs are most commonly identified through subjective assessments by public health practitioners and other experts. These needs are often characterized by insufficient resources (human, technological, or financial); inadequate capabilities, tools, or methods; or deficits in the scale, scope, or intensity of the activities through which these inputs are applied.
The content of this paper is based on telephone interviews with members of a committee workgroup1 and other public health leaders,2 as well as an extensive literature review. Findings based purely on the views of the public health leaders interviewed are clearly identified as expert opinion or perceptions. Respondents were selected based on their broad expertise in public health agency capacity, performance, and financing, as well as their experiences implementing innovative practices. Many interview respondents were directly identified by workgroup members, and additional respondents were identified during initial interviews with these public health leaders.
______________
1Leslie Beitsch, David Fleming, Glen Mays, David Ross, and Steven Teutsch.
2A complete list of interview respondents can be found following the reference list.
Limitations in the scale and scope of this effort prevented a more inclusive sample of respondents; therefore, respondents selected were not intended to be representative of public health officials nationally. However, efforts were made to ensure geographic diversity and a mix of perspectives across local and state agencies. Interviews were conducted by either the author or Alina Baciu (IOM Study Director) using a semistructured protocol, and each averaged approximately 1 hour in duration. Background materials (e.g., information on respondent’s organization, published research) were reviewed prior to the interviews in order to customize questions and prepare tailored probes.
Preparatory interviews with workgroup members identified a draft set of mission-critical capacity-development priorities that were shared with other interview respondents in order to stimulate discussion. Respondents were asked to (1) comment on and suggest revisions to the capacity-development priorities identified in the discussion draft, (2) describe the effect of categorical funding on capacity development in these areas, (3) identify financing strategies that have been used successfully to build these capacities, and (4) share insights on alternative financing strategies that could be used to support these capacities in the future. Respondents were not asked to rank or prioritize among the capacity-development needs identified, but to the extent that particular issues were consistently highlighted or emphasized, these concerns are noted in the following narrative.
Results from the interviews and literature review were synthesized to develop the findings summarized in the remainder of this paper. These findings are organized in three main areas
• Capacity-Development Priorities,
• Impact of Categorical Funding on Gaps in Mission-Critical Capacities, and
• Strategies for Financing Mission-Critical Capacities.
CAPACITY-DEVELOPMENT PRIORITIES
Addressing public health capacity-development needs has the potential to catalyze and accelerate broader reform in the health system. Because the governmental public health infrastructure serves as the nexus of the entire health system, deficits in the mission-critical capacities of state and local agencies are likely to have a rate-limiting effect on systemwide effectiveness and efficiency. Conversely, strengthening these capacities can create a pace-setting effect for overall improvements in health system performance.
The following identifies capacity-development priorities for state and local public health agencies based on the expert opinion of committee
members and input from other leaders in public health, as well as supporting evidence drawn from a review of the literature. These priorities are not intended to represent an exhaustive compilation of all capacity gaps within the field of public health. Rather, this summary is meant to highlight a mission-critical subset of public health capacities that appear to be (1) necessary for mounting an effective response to the broad determinants of health, (2) underdeveloped in many, if not most, state and local health agencies, and (3) difficult to develop adequately given the current level and structure of public health funding.
The capacity-development priorities described below are informed by and grounded in the
• Core functions and 10 essential services of public health,
• Operational Definition of a Local Health Department developed by the National Association of County and City Health Officials (NACCHO),
• State and local public health practice standards established by the Public Health Accreditation Board (PHAB),
• Core competencies for public health professionals established by the Council on Linkages between Academia and Public Health Practice, and
• Priority Areas for Improvement of Quality in Public Health identified by the U.S. Department of Health and Human Services.
These references broadly define the general functions, services, capacities, competencies, and quality improvements needed to support public health practice (Council on Linkages, 2010; Honoré and Scott, 2010; NACCHO, 2005; PHAB, 2009; Public Health Functions Steering Committee, 1995).
In contrast to these inclusive frameworks, the capacity-development priorities identified here are intended to emphasize specific high-yield opportunities for strategic investments in public health capacity. In essence, the priorities described in this paper highlight those aspects of the governmental public health infrastructure believed to be particularly nascent, fragile, or efficacious.
Mission-critical capacity-development needs appear pronounced in five general areas or domains
• Surveillance and epidemiology,
• Community health improvement planning,
• Partnership development,
• Policy decision support, and
• Public communications.
In general, interview respondents expressed a high degree of consensus regarding these capacity-development priorities. However, individual respondents often focused their remarks on specific aspects of these investment opportunities depending on the respondent’s unique experiences and areas of expertise. The few issues characterized by explicitly divergent viewpoints are noted in the following narrative.
Surveillance and Epidemiology
Surveillance and epidemiology are the foundation of public health practice, and deficits in this capacity domain can fundamentally undermine the effectiveness of governmental public health agencies. The type and magnitude of these capacity deficits appear to vary among states and localities depending on the specific public health surveillance systems, analytic tools, and epidemiologic workforce deployed in each jurisdiction (CSTE, 2009b). Despite these variations, the public health leaders interviewed for this paper strongly concurred that capacity-development needs related to surveillance and epidemiology are widespread and represent significant opportunities for improving performance at both the state and local level.
As described more fully in For the Public’s Health: The Role of Measurement in Action and Accountability (IOM, 2011), existing public health information systems and related analytic activities do not adequately support decision makers confronting important choices regarding the health of their communities. Although public health agencies at all levels of government engage in a broad variety of valuable activities to collect, analyze, and disseminate health information, these efforts often have limited relevance for decision makers seeking to intervene at the community level owing to critical deficiencies in the accuracy, breadth, and timeliness of information (Livingood et al., 2010; Luck et al., 2006).
Respondents believed that additional investments are critically needed to enhance governmental public health’s capacity to perform the following
• Conduct timely, community-level surveillance on disability, injury, behavioral health risks, and chronic diseases (including mental and oral health).
• Monitor the accessibility and quality of health care services.
• Measure important community characteristics, such as environmental health risks (e.g., infectious disease vectors, air and water quality) and other contextual factors that contribute to population health outcomes (e.g., community walkability, liquor store outlet density, and access to healthy foods).
These perceived gaps in surveillance and epidemiology capacity reflect limitations that have been widely documented in the peer-reviewed and grey literature (Ali et al., 2007; ASPHL, 2007; CDC, 2006, 2010; CSTE, 2009b; Malvitz et al., 2009; Mokdad, 2009).
Taken collectively, research findings and respondent perceptions yield generally consistent conclusions regarding the need for additional investments in surveillance and epidemiology capacity to address the deficits identified. Specific capacity-development needs vary somewhat depending on surveillance topic and jurisdiction. In general, investment opportunities include improvements to existing surveillance systems, the design and implementation of innovative surveillance methods, and workforce development.
Improved Relevance and Timeliness of Existing Surveillance Systems
With the exceptions of reportable disease surveillance for specific communicable diseases and disease registries for a limited number of conditions, public health surveillance is heavily reliant on either sample-based population surveys (e.g., Behavioral Risk Factor Surveillance System [BRFSS]) or administrative databases (e.g., vital statistics, hospital discharge data) that are not primarily designed for surveillance purposes (Love et al., 2008; Mokdad, 2009). Survey data are typically not valid at the community level and usually cannot be used to monitor racial and ethnic disparities or geographic variation within communities. Administrative data often lack relevant content and may be extremely dated. In both cases, the usefulness of these surveillance data sources could be improved through modifications in data variables, improved adherence to coding conventions, and enhanced data collection methods.
Some states and communities have invested in enhancements to existing population health surveys and conducted community-specific survey efforts in order to develop valid, timely community-level estimates for a wide range of noncommunicable conditions and risk factors. These investments have included additions to survey instruments and increased sample sizes for BRFSS or other population health surveys (Drewnowski et al., 2007; Livingood et al., 2010). Others have proposed the use of improved small-area estimation techniques to develop community-level data (Congdon, 2009, 2010; Zhang et al., 2011).
Addressing deficiencies within administrative datasets raises somewhat different challenges. A wide variety of data sources administered by state health agencies (e.g., claims data for public health insurance programs, hospital discharge databases, emergency department data, vital statistics, and disease and immunization registries) can be used to monitor rates of disease, injury, and health care utilization. However, access to these datasets
for public health surveillance purposes is often hindered by organizational and financial barriers. When these datasets can be accessed, data are often at least 1 to 2 years out of date upon release (Friedman, 2007).
In a survey of state chronic disease epidemiologists conducted by the Council of State and Territorial Epidemiologists (CSTE), a substantial number of respondents reported problems in gaining access to Medicare and Medicaid claims data (97 percent and 82 percent of states, respectively), state emergency department data (56 percent of states), hospital discharge data (59 percent of states), and state mortality data (63 percent of states). For those state chronic disease epidemiologists able to gain access to these health datasets, problems regarding data timeliness were frequently reported. Timely access to mortality data from state vital statistics systems appears particularly problematic (CSTE, 2009a). Interview respondents noted that local health officials face similar (and perhaps more daunting) challenges in accessing health datasets maintained by state health agencies.
Anecdotal accounts suggest that sources of nonhealth data that could be used to monitor environmental risks and other community characteristics related to health (e.g., traffic accident reports, liquor store license records) may be even more inaccessible than traditional health datasets. Whereas most health data are in electronic formats, data from other potentially relevant sources may not be digitized or stored in a manner that facilitates analysis. Also, state and local health officials are generally less familiar with these potential datasets and may not be experienced in the procedures needed to obtain and analyze this information. Additional training may be needed to help public health officials identify and access these potential sources of environmental and contextual surveillance data.
Streamlined data reporting, processing, and release protocols, as well as improved intergovernmental coordination, could reduce the time lags and access barriers observed in the use of administrative datasets for surveillance purposes. Wider adoption of data standards and coding conventions (such as geocoding data with spatial references, accurate and complete inclusion of external cause of injury codes) could further enhance the analytic applications of administrative data at the community level and facilitate linkages across datasets (CSTE, 2009b,c; Grigg et al., 2006; Krieger et al., 2002; Miner et al., 2005; Miranda et al., 2005).
Accelerated Development of Interoperable
Public Health Information Systems
Public health surveillance is highly dependent on information reported by the clinical care delivery system. Yet public health surveillance systems have not adequately adapted to technological advances in the way that clinical health information is collected, processed, and stored (Public Health
Data Standards Consortium, 2007). Progress has been made in public health informatics, such as increased electronic reporting of communicable diseases and improved integration of child health data (CSTE, 2009b; Fehrenbach et al., 2004; Overhage et al., 2008; Public Health Informatics Institute, 2003). However, many public health information systems continue to rely on antiqued, “stove-piped” mechanisms to both collect data from health care providers and to store data for analytic use (Public Health Data Standards Consortium, 2007; Staes et al., 2009). For example, CSTE reports that 47 percent of states have not yet implemented fully automated electronic laboratory reporting for reportable infectious diseases, and 59 percent have not developed web-based reporting for physicians and other providers (CSTE, 2009b).
Broader dissemination of electronic health records (EHR) and significant investments in health information technology by hospitals and other health care facilities offer promising opportunities to strengthen public health surveillance (Birkhead, 2010; Cossman et al., 2008; Klompas and Yokoe, 2009; Lazarus et al., 2009; Magruder et al., 2004). Meaningful use criteria established by the EHR Incentive program sponsored by the Centers for Medicare and Medicaid Services (CMS) create additional incentives for the electronic exchange of public health information (Blavin and Ormond, 2011). However, state and local public health agencies have struggled to adapt public health surveillance systems to leverage these advances in health information technology and do not appear to have the capacity necessary to shape the development of EHRs in clinical settings to optimize their potential for surveillance purposes.
Capacity developments needed to accelerate the design and implementation of innovative public health surveillance methods include augmenting the number and skills of public health workers with specialized expertise in health informatics; investing in the design and implementation of new, interoperable public health information systems; and expanding the use of mobile communication technologies to facilitate electronic data capture and transfer (Kukafka et al., 2007; Magruder et al., 2005; Turner et al., 2008; Yasnoff et al., 2001). Several interview respondents indicated that the financial cost of these capacity improvements has hindered development in this area. Information systems development represents a significant investment with costs associated with design, capital acquisition, training, and lost productivity during transition from the legacy system. Similarly, the labor market for skilled informatics personnel is highly competitive, resulting in salary levels that cannot typically be offered in public health agencies.
Interview respondents noted, however, that both organizational and financial barriers block the development of more rational, sophisticated public health information systems. The business case for informatics developments may be difficult to justify given that the benefits of these investments
are likely to accrue to organizational units that are not directly responsible for maintaining surveillance systems and are unlikely to bear the costs of upgrades. Several respondents also raised concerns that the policies and procedures imposed by centralized agencies within state government responsible for overseeing information systems often slow or prevent innovation by public health agencies. Absent a dedicated source of funding to catalyze public health information systems development, these organizational barriers can be difficult to overcome.
Increased Number and Competencies of Epidemiologists
Workforce deficiencies related to epidemiology capacity compound the surveillance-related capacity-development needs described above. CSTE estimates that approximately 1,500 additional epidemiologists are needed nationwide for optimal surveillance and epidemiology capacity in all program areas at the state level (CSTE, 2009b). In addition to the need for more staff dedicated to epidemiological analyses, CSTE cites the need for more extensive training of epidemiology personnel,3 expanded consultative support for epidemiology at the state level to meet local needs, increased use of analytic tools (such as cluster detection software and geographic information systems), and better coordination of epidemiology resources across program areas.
Categorical funding appears to encourage a distributed model for epidemiology capacity wherein states embed epidemiology capacity within discrete programs, rather than developing a centralized epidemiology unit to serve as a cross-cutting resource. Program-based epidemiology personnel often dedicate only a portion of their time to epidemiology activities and typically have limited epidemiological training and expertise. This type of distributed model may deter integrated analyses and can hinder the development of more sophisticated epidemiology capacity if robust coordinating mechanisms are not implemented (CSTE, 2009b; Duffy and Siegel, 2009).
Although similar epidemiology workforce requirements are not available for local health agencies, NACCHO reports that a minority of local health departments engages in surveillance and epidemiology activities for noninfectious diseases. Agencies serving populations under 100,000 rarely employ professionals occupationally classified as epidemiologists (NACCHO, 2009).4
______________
3Respondents noted that substantial on-the-job training is often needed for new staff (even those with academic training in epidemiology) owing to inadequate experience in descriptive epidemiology, practical surveillance, and investigation techniques.
4Staff classified as epidemiologists may not have graduate level training in epidemiology.
COMMUNITY HEALTH IMPROVEMENT PLANNING
For surveillance and epidemiology capacity to have a meaningful effect on population health outcomes, the information gleaned through these activities must be interpreted and translated into actionable interventions. Historically this decision making and response has occurred within programmatic silos and has sometimes resulted in a failure to intervene, duplication of efforts across programs, or a suboptimal alignment of public health resources relative to community need. Comprehensive community health improvement planning is widely viewed as a more effective approach to the assessment of health needs across a broad range of outcomes and detriments and the allocation of resources to address these needs.
Community health improvement planning has been conceptualized and implemented in a variety of ways. Typically these strategic planning activities include at least three distinct phases: the completion of a community health assessment,5 the identification of health priorities, and the development of an action plan to respond to priorities identified (Jacobs and Elligers, 2009). The evidence base regarding the optimal nature and scale of investments in each of these phases is underdeveloped (Friedman and Parrish, 2009; Myers and Stoto, 2006). However, the need for some level of capacity in community health assessment and related health improvement planning is widely recognized. Because these activities are often viewed as fundamental elements of public health practice, PHAB will not consider a health agency for national accreditation if the organization has not developed a community health assessment, a community health improvement plan, and an agency strategic plan.
The public health leaders interviewed for this paper believe that additional capacity development is needed to ensure that community health improvement planning efforts are effective in improving community health outcomes. Deficits were observed in all three stages of community health improvement planning identified above, with development needs cited related to public health agencies’ capacity to
• conduct comprehensive community health assessments (CHAs),
• facilitate participatory priority setting involving multiple stakeholders, and
• identify cost-effective, community-based interventions to prevent disease, injury, and disability.
These perceived gaps in capacity for community health improvement
______________
5While a variety of formal definitions have been developed, the term community health assessment typically refers to a systemic effort to collect, analyze, and disseminate information on the health of a community (Friedman, 2010; Myers and Stoto, 2006).
planning are supported by findings in the literature. However, the status of, and development needs related to, community health assessment activities have been more extensively documented than those regarding the latter stages of the planning process.
Over the past two decades, many states have enacted policies that mandate the completion of community health assessments by local health agencies, and a variety of trainings and tools have been developed to assist these efforts.6 These activities have supported the implementation of community health assessments throughout the country and facilitated the use of health data in planning and policy development. In 2008, NACCHO found that the majority of local health agencies led or contributed to a collaborative process to conduct a community health assessment at some point within the prior 3-year period (NACCHO, 2009).
Yet, despite this progress, substantial opportunities exist for expanding the implementation of community assessments. A significant proportion of local health agencies (37 percent) report that no community assessment had been conducted for the jurisdictions served within the 3 years prior to 2008, and 31 percent did not have plans to conduct a community health assessment in the immediate future.7 Agencies serving populations of less than 25,000 were most likely (47 percent) to report the absence of a community health assessment. Among local health agencies that have completed assessments, variations exist with respect to methods used, reflecting varying levels of quality, scope, and utility (Stoto et al., 2009).
Most CHAs are designed to support the development of community health improvement plans, and the vast majority of community health improvements plans (92 percent) are based on formal community health assessments (NACCHO, 2009). While CHAs provide an objective fact base for priority setting, ultimately this information must be assessed and interpreted through a subjective process to establish community health improvement priorities. Public health agencies have the potential to play a leadership role in this priority setting process, but capacity deficits may limit the extent and effect of public-sector contributions.
Some studies indicate that the involvement of governmental public health agencies in community health improvement planning tends to diminish as the processes moves from assessment to priority setting and action planning (Abarca et al., 2009; Fielding et al., 1999). These findings suggest that the latter stages of planning fall outside the “comfort zone” of many governmental public health agencies. Other researchers have found that
______________
6Such as MAPP (Mobilizing for Action through Planning and Partnerships), APEX (Assessment Protocol for Excellence in Public Health), CDC’s Assessment Initiative, and NACCHO’s CHA/CHIP (Community Health Assessment/Community Health Improvement Plan) project.
7Within the next 3 years.
community assessments that focus narrowly on specific health issues or populations are somewhat more likely to be viewed as impactful than more comprehensive efforts (Spice and Snyder, 2009). This finding may reflect, in part, the challenges of interpreting a diverse array of community health indicators and prioritizing among different types of disease threats and vulnerable populations.
Capacity-development investments that promise to advance the implementation and broaden the impact of community health improvement planning include dedicating resources to support all phases of these planning efforts, improving the scope and integration of surveillance data in CHAs, enhancing leadership skills to facilitate priority setting and conflict resolution, and improving awareness and adoption of evidence-based practices.
Dedicated Resources in Terms of Both Financing and Staff Time Availability
Community health assessment and related planning activities are time intensive and demand a significant staffing commitment (Abarca et al., 2009; Curtis, 2002; Paul-Shaheen et al., 1997). One study found that on average, CHAs require nearly 12 person-months of personnel time and cost over $60,000 to complete (Fielding et al., 1999). The establishment of dedicated units adequately staffed by personnel with analytic, policy, and technical expertise appears to promote the successful completion of CHAs (Paul-Shaheen et al., 1997). Conversely, lack of time, insufficient funding, and low levels of interest have been reported as the most significant barriers preventing the completion of community health assessment and planning (Curtis, 2002).
Although private-sector, community-based organizations frequently contribute significant amounts of both paid and in-kind staff resources to community health improvement planning, local and state health agencies often play pivotal roles (Fielding et al., 1999; NACCHO, 2009). CHAs typically rely on datasets maintained by the state health agencies, and planning efforts commonly depend on local health agencies to coordinate and mediate diverse community interests (see Box C-1). Absent the active engagement of governmental public health, efforts initiated solely by private-sector stakeholders may result in duplicative efforts and the creation of multiple (possibly conflicting) assessments and plans for a given community.
Recent, substantial reductions in the public health workforce may hinder a robust public-sector coordinating role in community health assessments sponsored by hospitals and other private entities (ASTHO, 2011; NACCHO, 2011). These staffing constraints within state and local health agencies decrease the likelihood that actionable health improvement plans will emerge from these assessment efforts.
BOX C-1
Role of Hospitals in Community Health Assessments
Not-for-profit hospitals are often active collaborators on community health assessments as state law in multiple jurisdictions requires tax-exempt hospitals to complete such assessments. The Patient Protection and Affordable Care Act creates a similar national mandate beginning in 2012 and promises to significantly increase hospitals’ investments in community health assessments. While these private-sector efforts promise to support improvements in the reach and quality of community health assessments, this growth may increase, rather than diminish, the need for additional public-sector involvement. Many state and local health agencies are working proactively to ensure appropriate public–private partnerships. For example, the Kansas Hospital Association and the Kansas Association of Local Health Directors have issued a joint resolution encouraging collaborative partnerships for community health assessments.
Improved Ability to Integrate Information from a Wide Variety of Sources
The breadth and depth of CHAs vary, and this variation is undoubtedly influenced by differences in epidemiology and surveillance capacity described in the preceding section of this paper. Community health assessments typically include indicators of health status, risk behaviors, and access to health care and other services. Measures regarding environmental health (e.g., air quality) and other community characteristics that influence population health (e.g., walkability, access to healthy food, local public health capacity, and health care provider supply) are featured in some CHAs, but the range of “contextual” indicators included may differ significantly across assessments (Myers and Stoto, 2006).
Ideally, CHAs provide a comprehensive understanding of community health status, the various factors that contribute to the health outcomes observed, and community perceptions of priority needs (Irani et al., 2006; Spice and Snyder, 2009). Developing this broad perspective requires the use of indicators drawn from a wide variety of datasets (e.g., BRFSS, hospital discharge data, vital statistics), linking records across datasets, epidemiological analyses to identify relationships between and among different data variables, and surveys to elicit community input. The data gathering and analytic challenges associated with these integrative efforts represent major barriers to successful community health assessments (Byrne et al., 2002; Stoto et al., 2009).
Many states have developed data warehouses, web-based query systems, training and technical assistance resources, and other mechanisms to improve the ability of local health agencies to access and use a wide array of
datasets for CHAs (Asaro et al., 2001; Friedman and Parrish, 2006; Love and Shah, 2006; Rooney and Thompson, 2009).8 Despite this progress, additional capacity enhancements are needed to enhance data dissemination tools (e.g., better trend analyses, benchmark support), improve the timeliness of available data, expand epidemiology-support capacity provided at the state level, and augment the analytic skills of local health officials (Friedman and Parrish, 2006; Love and Shah, 2006).
Improved Community Outreach and Engagement
Ideally, CHAs provide an initial basis for broad community involvement and sets the stage for the active participation of community residents and partner organizations throughout the course of the community health improvement planning process (CDC, 2010; Jacobs and Elligers, 2009). Significant community outreach, local data collection to assess perceived community health needs, and a participatory assessment process facilitate the engagement of residents and other stakeholders in the community health assessment (Cheadle et al., 2008; Kegler et al., 2009; Keller et al., 2002; Parker et al., 2003; Running et al., 2007; Spice and Snyder, 2009). These interactive activities also increase the staff time commitments and other costs associated with conducting CHAs and may demand an orientation and set of skills not commonly found within public health agencies. Additional investments are needed to identify effective techniques for outreach and engagement, disseminate this evidence, and train public health personnel in the application of these methods.
Enhanced Leadership and Communication Skills to Support Priority Setting
Priority setting requires a special set of skills and competencies related to the interactive nature of group facilitation and consensus building. The literature surrounding these capacity requirements is less robust than that pertaining to community assessment, which may further substantiate the extent to which community priority setting falls outside of conventional public health practice.
Public health lacks clear, widely accepted criteria for prioritizing community health needs (Michaelis, 2002). A variety of factors may be considered when establishing community health priorities, including the number of people affected, severity of the problem, perceived urgency of issue, efficacy
______________
8Since 1992, funding through CDC’s Assessment Initiative has supported 19 states (Arkansas, Florida, Illinois, Iowa, Maine, Massachusetts, Minnesota, Missouri, New Hampshire, New Mexico, New York, North Carolina, Ohio, Oregon, Rhode Island, Texas, Utah, Virginia, and Washington) to improve state and local capacity for conducting community health assessments.
of interventions, political will to address health threats identified, and the cost, feasibility, and sustainability of response efforts (Anderson et al., 2005; Finison, 2007). Priority setting is an inherently value laden and subjective activity. Facilitating a prioritization process that engages a broad variety of stakeholders with diverse interests and perspectives will almost certainly lead to some degree of conflict and disagreement.
Public health leaders interviewed for this paper identified a number of underdeveloped capacities related to priority setting in the context of community health improvement planning, including the need for improved leadership skills related to conflict mediation and group facilitation, more and better models for communicating community health assessment findings in actionable formats that can be easily understood by a lay audience, and additional evaluation and research related to effective methods for priority setting in a community context.
Increased Awareness and Adoption of Evidence-Based Practices
The ultimate purpose of community health improvement planning is to identify, select, and plan for the implementation of interventions that can effectively address community health priorities. These decisions should be based on the best available evidence regarding health detriments and effective public health practice. However, a variety of barriers hinder evidence-based decision making in community health planning (Braveman et al., 2011). The evidence base for effective public health practices is growing, but remains limited, particularly with respect to effective community-based interventions (Anderson et al., 2005). Suboptimal use of available evidence by public health practitioners further undermines the inclusion of effective inventions in community health plans (Brownson et al., 2009).
Evidence-based practice guidelines (such as those identified in CDC’s Guide to Community Preventive Services) and systematic evidence reviews (such as those developed by the Cochrane Collaboration and the Canadian Institutes of Health Research) support the dissemination of research findings to public health practitioners. However, available tools and resources do not fully support the information needs of state and local officials (LaPelle et al., 2006; Rockoff et al., 2007; Twose et al., 2008).
LaPelle et al. (2006) identified a continuum of information resources required to support evidence-based public health practice, including (1) early reports on newly identified health risks and preventive behaviors; (2) early reports on emerging practices and programs; (3) information on evaluated new interventions known to be effective; (4) syntheses of knowledge on established public health threats and practices; (5) published research reports, including meta-analyses and systematic reviews as found in peer-reviewed journals; and (6) evidence-based guidelines. For all these types of
information resources, concerns have been raised related to ease of access by public health practitioners and inadequate customization of existing search and retrieval tools for public health purposes.
Researchers have suggested numerous proposals to improve access to information regarding evidence based public health practices including expanded access to full-text journal articles, automated notifications regarding new research findings, greater standardization of public health-related keywords, tailored search filters, better access to relevant research from other disciplines (e.g., urban planning), and streamlined mechanisms for searching the grey literature produced by credible sources (such as professional associations) (LaPelle et al., 2006). Several interview respondents voiced similar concerns about the need for better information retrieval mechanisms and also noted that more training and consultative assistance may be required to help public health workers select appropriate evidence-based practices.
Additional analytic support may be needed to assist local health officials in appropriately targeting interventions to address the specific manner in which community health risks are exhibited. The evidence base surrounding the various factors that influence health outcomes and practitioners’ awareness of this evidence are strong relative to evidence regarding the effectiveness of interventions. However, most noncommunicable diseases have a complex etiology, and the relative contribution of discrete causal factors is likely to vary across communities, as well as across population groups within communities. Second-order “drill down” analyses may be needed to determine which evidence-based interventions are likely to yield the greatest health improvements and where these interventions should be implemented.
Partnership Building
Community health improvement plans often feature ecologically oriented public health interventions that must be implemented through intersectoral partnerships. Traditionally, state and local public health agencies have focused on the implementation of disease prevention and health promotion activities that these agencies have direct responsibility and operational control over (e.g., lead abatement, vector control, sanitation, food service inspections, and health education). Transforming the primary prevention role of state and local public health agencies to one that mobilizes multiple community stakeholders in order to facilitate broad societal change will require significant investments in partnership-building capacities. State and local public health agencies are being called on to cultivate strong relationships with a variety of health system partners, including
• clinical care providers (e.g., physicians, hospitals, laboratories, pharmacies, and insurers),
• child care providers,
• primary and secondary schools,
• colleges and universities,
• businesses,
• community-based organizations,
• media organizations,
• other government agencies,
• public health agencies in other jurisdictions (local-local; state-state),
• public health agencies in other levels of government (federalstate-local),
• governance bodies, and
• intra-agency partners (e.g., coordination of multiple programs, divisions within state and local health agencies).
Local health agencies do engage in a variety of collaborative relationships, although the nature and strength of these relationships appear to vary by jurisdiction and partner type (Cheadle et al., 2008; Lovelace, 2000; Mays and Scutchfield, 2010; NACCHO, 2009; Zahner, 2005). Strong partnerships with schools, health care providers, nonprofit community organizations, and state health agencies appear most common. Some partnerships represent bi-lateral coordination of routine activities (which are sometimes mandated by law), while others represent voluntary collaborative initiatives involving multiple stakeholders. Local health agencies may play a central role in these collaborative networks or may act in a supportive capacity (Kassler and Goldsberry, 2005; Mays and Scutchfield, 2010; Wholey et al., 2009).
A limited but growing evidence base supports the belief that community partnerships improve the reach and performance of governmental public health agencies, facilitate system change, reduce health risks, and improve health outcomes (Cheadle et al., 2008; Mays and Scutchfield, 2010; Roussos and Fawcett, 2000; Scutchfield et al., 2004). Effective partnerships are characterized by committed leadership, high frequency of interaction, clear definition and high concordance of goals, adaptability to change, and ability to communicate value and benefits to the community (Bazzoli et al., 2003; Cheadle et al., 2008; Easterling, 2003; Lovelace, 2000; Roussos and Fawcett, 2000). However, significant investments of time and resources are required to create and sustain effective collaboration (Mays and Scutchfield, 2010; Woolf et al., 2011).
Interview respondents cited a variety of capacity deficits that currently limit the ability of state and local health agencies to build effective partnerships, including the capacity to
• assess the interests, priorities, culture, and operating processes of partner organizations,
• adapt and coordinate programmatic activities to seamlessly interface with partner organizations and advance cross-cutting, strategic goals,
• provide training, technical assistance, and other forms of support to partners,
• implement and sustain collaborative interventions involving multiple stakeholders (including individual citizens and grassroots organizations), and
• encourage financial contributions to fund community health improvement plan implementation and galvanize support for investments in the governmental public health infrastructure.
Priority opportunities for capacity development in this domain include improved leadership skills and commitment, enhanced communication and coordination with strategic partners, improved ability to align agency activities with community health improvement goals, and increased clarity and accountability regarding partner roles and contributions.
Improved Leadership and Commitment to Collaboration
Leadership commitment and skills have been consistently identified as key predictors of success in collaborative endeavors. Agency directors and senior management staff influence the nature and quality of interorganizational relationships directly through their personal interactions and engagement with potential partners and indirectly through the way the value and importance of collaboration is conveyed to the broader agency. In many traditional organizational structures, building external relationships (with governance bodies and strategic partners) is often seen as a primary responsibility of leadership personnel. Agency leaders frequently serve as the “public face” of state and local health departments, presenting at governance functions, participating in intergovernmental cabinets and workgroups, serving as the main liaison to private-sector groups, and engaging with media outlets. These interactions can profoundly shape the tenor and tone of partnerships and are deeply affected by leaders’ convictions regarding both the appropriate role of governmental public health in addressing the broad determinants of health and the usefulness of partner contributions. The nature and effectiveness of partnerships are also influenced by the interpersonal skills, communication abilities, and tolerance for risk further exhibited by public health leadership.
While direct leadership roles are critical in cultivating collaborative relationships, indirect influences may have even farther reaching, longer-term effects on agency capacity. Because the time and attentions of leadership staff are finite, collaborative partnerships are best advanced if more broadly supported through agency policies and operations. Agency
culture regarding the perceived need for and benefits of collaboration is shaped over time by the attitudes and behaviors of agency leadership as expressed by informal and formal management practices and policies (e.g., staff meeting agendas, performance review procedures, and promotion criteria). Relative to unilateral activities, collaborative efforts require greater investments of staff time to support communication, coordination, and negotiations with external organizations. Staff are unlikely to assume these short-term costs without strong leadership commitment to the long-term vision of a more efficient and effective health system and some form of reward or recognition for their efforts to be supportive partners (Mays and Scutchfield, 2010).
In addressing capacity-development needs related to leadership, interview respondents cited the need for more leadership-development opportunities, peer-to-peer sharing about promising approaches to partnership development, and more formal evaluations of the communication mechanisms and management techniques that foster a collaborative culture. However, several respondents also raised more fundamental concerns that prevailing salary levels combined with limited autonomy in resource allocation decisions may discourage the retention and recruitment of high-caliber leaders capable of building constructive relationships with health system partners. Short tenures of agency directors, particularly at the state level, were also cited as a barrier to the development of stable partnerships. Some respondents felt that structural changes in compensation, budgetary authority, and employment terms would be necessary to attract and retain innovative public leaders capable of establishing and sustaining strategic partnerships.
Interview respondents generally concurred that while the vision of a collaborative, ecologically oriented health system is widespread among local and state health officials, current leadership capacity to advance this model is highly variable. A few respondents were somewhat more pessimistic and expressed concern that leaders in many public health agencies have not yet embraced a more expansive, collaborative role.
Limited political support for public health efforts to promote social and environmental change was cited as a major factor discouraging public health leaders from pursuing innovative forms of partnership (Libbey and Miyahara, 2011). Several respondents indicated that additional evidence regarding the feasibility and effectiveness of collaborative partnerships would be needed to increase policymakers’ support for public health officials implementing or considering these interventions. Some respondents suggested that concrete financial incentives for collaboration would encourage public health leaders, policymakers, and partner organizations to invest in these strategic relationships (Mays and Scutchfield, 2010).
Enhanced Communication and Coordination with Strategic Partners
Although leadership commitment and involvement were seen as essential to establishing an organizational culture conducive to collaborative partnerships, interview respondents also identified a range of structural characteristics and operating practices that appear to influence the effectiveness of communication and coordination with health system partners. Several respondents noted the level of staff time and skill involved in engaging partners and cited the need for personnel who are explicitly tasked with coordinating strategic relationships and are trained for and evaluated on these duties.
A dedicated liaison or partner relations function may facilitate regular interaction with partner organizations, enhance efforts to monitor the implementation of strategic plans, and promote the active identification and mediation of any conflicts or problems that may arise. Liaisons are likely to be most effective in translating public health objectives, identifying mutually efficient processes, and resolving unproductive tensions if they understand the various ways the agency interacts with the partner organization, have some level of authority to shape these interactions, and are highly familiar with the business practices and operating procedures of partner organizations. Ideally, partner liaisons have had prior professional experience working in these settings and maintain close relationships with their former colleagues.
Liaisons may also be effective in minimizing problems associated with intra-agency fragmentation. Public health agencies can devolve into information silos with limited coordination across programs (Merrill et al., 2008). Absent proactive management, such fragmentation can significantly increase the burden experienced by partners and decrease the coherence and productivity of collaborative relationships. Many partnerships are complex and reflect relationships with and among a variety of programmatic areas. In addition to undermining trust and goodwill through inefficiencies, intra-agency fragmentation can also erode the cumulative effect of the various routine interactions that occur at the program level, particularly if these programmatic interactions fail to align with broader strategic goals.
Improved Flexibility to Align Agency Activities with Community Health Improvement Goals
Achieving meaningful improvements in community health will typically require health system partners to change their operating practices in some way—conducting existing activities more effectively, taking on new roles and responsibilities, or discontinuing practices that fail to contribute to improvements in community health. Each of these options represents dif-
ficult strategic decisions with concrete implications for staffing levels and skill mix, management practices, and capital needs. Ideally such strategic realignments are made in a coordinated fashion with a systemic perspective of the relative strengths and weaknesses of all health system partners.
To optimize partner contributions and model collaborative action, local and state health agencies may need to revisit their own strategic position within the broader health system and restructure governmental activities and service offerings accordingly. Interview respondents raised concerns regarding the ability of state and local health agencies to significantly reorient their operational activities in order to support strategic goals. Categorical funding appears to limit public health officials’ flexibility in resource allocation decisions and reduces the availability of “venture capital” that could be used to develop new activities or services in response to unmet needs (Baum et al., 2011). For example, several respondents noted that local public health agencies could be playing a stronger role in providing training and technical assistance to health system partners (e.g., facilitating quality-improvement efforts in clinical settings, informing policy development in nonhealth sectors, providing health consultations to schools and child care facilities).
Similar concerns were voiced regarding the ability of public health agencies to relinquish or transfer certain operational responsibilities to partners who might be better positioned to carry out these activities. For example, implementation of health reform has reopened a longstanding debate in the field of public health regarding the appropriate role of governmental public health agencies in the delivery of clinical services. Some argue that the direct provision of clinical services distracts governmental public health agencies from their core mission of promoting population health and may engender pernicious competitive tensions with private-sector providers. Others believe that public health agencies cannot relinquish their clinical service responsibilities because the private-sector health care delivery system fails to provide adequate access to care (Keane et al., 2003).
Although relatively few local health agencies provide comprehensive primary care, the vast majority offer some type of clinical or personal care service (e.g., immunizations, case management, Women, Infants, and Children [WIC] services, family planning, TB treatment) (NACCHO, 2009). A substantial proportion of local health department budgets are devoted to these personal services, although the extent of this commitment depends on the nature and range of services provided (Brooks et al., 2009; Plough, 2004; Santerre, 2009). The scope of personal services provided by local health departments also significantly influences total funding levels and accounts for much of the wide variation in revenue per capita observed among agencies (Mays and Smith, 2009).
As discussed earlier in this paper, public health agencies generally lack the ability to assess access to care and, apart from the direct provision of
services, appear to have limited legal authority or operational capacity to assure access (CSTE, 2009b; Keane et al., 2003; Scutchfield et al., 2004). Demands on governmental public health agencies for clinical services are unlikely to decrease substantially in the short term (Meyer and Weiselberg, 2009). However, as reforms (such as Medicaid eligibility changes and the formation of accountable care organizations and state-based insurance exchanges) continue to evolve and mature it will be critically important for public health agencies to improve their ability to monitor access and carefully consider the benefits and disadvantages of transferring responsibility for personal care services to private-sector providers. If officials determine that community health interests are best served by a given public health agency’s continued involvement in personal services, improvements in third-party billing capabilities may be required.
Despite the importance and visibility of public health agencies’ role in the direct provision of clinical services, interview respondents did not focus narrowly on these issues. The perceived need to realign roles and responsibilities relative to the clinical sector was typically framed around broader questions related to how public health agencies could better support clinical providers in the development of a patient-centered, prevention-oriented system of care. Concerns were raised regarding limitations in expertise, resources, and expectations that could prevent public health agencies from taking a proactive role in delivery system reform.
Other opportunities for strategic realignment were frequently cited, as respondents collectively referred to untapped promise in each of the potential partnerships identified above. In addition to calls for refocusing relationships with the clinical sector, respondents most commonly discussed needs related to strengthening collaboration among public health agencies. Many respondents indicated that relationships between public health agencies at the state and local levels could be improved and were at times adversarial rather than cooperative. States have established a variety of approaches to organizing public health activities and distributing operational responsibilities among state agencies, local health departments, and health system partners (Mays et al., 2010). Recognizing this diversity, respondents generally did not offer specific recommendations for intergovernmental realignment of responsibilities and resources, but they suggested that states and localities need to carefully reconsider existing structural conventions and coordination mechanisms.
Similarly, several respondents emphasized the need for improved regional collaboration among public agencies at the local level, particularly among agencies serving small populations. These small local health departments often have limited staff capacity and face efficiency challenges related to economies of small size (NACCHO, 2009). Research by Santerre (2009) has suggested that a population base of approximately 100,000 may rep-
resent the minimum size needed to support efficient operations. Currently, over three-quarters of local health departments serve populations smaller than this minimally efficient scale (NACCHO, 2009). Regional collaboration among local health departments may take many forms, including full organizational consolidation, shared services, and cooperative activities (Libbey and Miyahara, 2011).
Increased Clarity and Accountability Regarding Partner Roles and Contributions
Sustained implementation of community health improvement plans involving multiple stakeholders requires ongoing efforts to ensure responsible parties are fulfilling their respective commitments (Woolf et al., 2011). Clearly defined roles and measurable, incremental objectives coupled with public reporting and nonpunitive, transparent recognition of implementation obstacles appear to support the long-term success of collaborative initiatives. Public health officials are typically unaccustomed to ensuring accountability in a voluntary context and may lack the skills necessary to monitor and maintain progress toward established goals. Model action plans and accountability mechanisms, along with additional opportunities for training and peer-to-peer learning, may be needed to enhance public health agencies’ ability to monitor and sustain community partnerships.
Policy Decision Support
State and local public health agencies have the potential to play a stronger role in informing public policy decisions that influence community health outcomes—including policies focused specifically on public health and health care services, as well as those in other policy sectors (e.g., urban planning, transportation, criminal justice, education, and agriculture). As described in the National Prevention Strategy and a variety of other international and state-level plans that articulate a “health in all policies” framework, there is widespread recognition that policies made outside of the traditional health policy domain have a powerful impact on the health of communities (National Prevention Council, 2011; Rudolph et al., 2010; Ståhl et al., 2006; WHO, 2010).
Interview respondents noted several underdeveloped capacities that may hinder state and local health agencies’ ability inform the broad range of legislative, regulatory, and administrative policies that affect community health, including deficits in the capacity to
• identify policy change opportunities in nonhealth sectors,
• anticipate the information needs of policymakers,
• provide timely analytic support to policy deliberations in a wide variety of sectors,
• monitor the performance of public health agencies to both inform internal quality improvement policies and influence governance decisions related to public health authorities and funding, and
• increase public awareness of health-promoting policies.
A variety of capacity-development investments are needed to address these deficits. They are discussed in the following sections.
Improved Ability to Monitor Agency Performance and Implement Quality Improvement Processes
Robust performance assessment and related quality improvement (QI) efforts are viewed as key ingredients for improving community health, demonstrating accountability, and securing policy makers’ support for the governmental infrastructure. Although most state and local public health agencies engage in some type of performance monitoring and quality improvement, the nature and scope of these activities appear to vary substantially (Beitsch et al., 2010; Madamala et al., 2010). Inconsistent definitions of quality improvement in public health have hindered efforts to document the uptake of, and barriers to, metrics-based performance improvement processes (Beitsch et al., 2010; Leep et al., 2009; Riley et al., 2010).
Despite recent momentum to expand the use of QI techniques9 (both agency-wide and within individual program areas), interview respondents felt that additional investments are needed to increase the use and improve the consistency of performance monitoring and QI methods in public health agencies. While constraints related to funding and training were acknowledged as significant barriers to broader adoption of performance monitoring and QI, perceived needs related to the methods and information supporting performance measures were also cited. For example, modifications to existing public health information systems (such as time stamps on data in reportable disease surveillance records) may be needed to improve the usefulness of these systems for performance-monitoring purposes.
Efficiency and cost-effectiveness were also considered critical aspects of performance. Expanded use of financial measures in performance assessment and more consistent methods for documenting the financial status of public health agencies (e.g., financial ratios, recording resource allocations using a standard chart of accounts) were viewed as important to both establishing comparative benchmarks for public health finance and demon-
______________
9Such as NACCHO’s Accreditation and Quality Improvement Demonstration Site Project and the CDC’s National Public Health Improvement Initiative.
strating the cost-effectiveness of public health interventions (Costich et al., 2009; Honoré and Costich, 2009; Honoré and Schlechte, 2007; Honoré et al., 2004, 2007; Suarez et al., 2011).
Several respondents also noted that public health agencies often lack the analytic capacity necessary to develop and implement decision support tools that address financial management decisions. Honoré et al. (2010) have documented the benefits of integrating budgeting and strategic planning through formal, evidence-based decision analyses. Yet the structured application of cost-effectiveness analyses to resource allocation decisions is relatively rare in public health agencies (Baum et al., 2011).
Increased Participation in Practice-Based Research
Respondents raised concerns about the lack of a robust evidence base linking agency performance to community health outcomes (Bender and Halverson, 2010; Erwin et al., 2011). Policy support for public health is compromised by gaps in the evidence base related to both the cost-effectiveness of public health interventions and optimal approaches to the organization and management of public health agencies. Scientific study in these areas is commonly referred to as public health services and systems research (PHSSR) (Scutchfield et al., 2007). Although the field of PHSSR has grown considerably in recent years, myriad opportunities exist for additional scientific inquiry (Bales et al., 2011; Council on Linkages, 2005; Harris et al., 2011; Merrill et al., 2011).
Funding limitations have perhaps been the dominant factor hindering growth of PHSSR, but interview respondents also noted the need to promote academic partnerships in order to more actively engage public health agencies in practice-based research. Innovative efforts, such as the Public Health Practice-Based Research Networks Program funded by the Robert Wood Johnson Foundation, have incubated these types of research partnerships and demonstrate the potential of such collaboration. Yet a broad range of challenges, including constraints related to funding, personnel, cultural tensions, and ethical considerations, jeopardize broader implementation of practice-based research (Potter et al., 2006). Additional investments are needed to overcome these challenges to ensure that PHSSR addresses the practical information needs of public health officials and policymakers.
Increased Adoption and Further Development of Analytic Tools to Assess the Health Impact of Policies (Existing and Proposed) in a Wide Variety of Policy Sectors
Multiple mechanisms exist to ensure health effects are considered in the policies promulgated by nonhealth sectors, but health impact assessments
(HIAs) are emerging as a particularly pragmatic tool (Koivusalo, 2010; Wernham, 2011). Wernham defines a health impact assessment as a “structured process that brings together scientific data, public health expertise and principles, and stakeholder input to identify the potential health effects of a proposed policy, program, project or plan and to craft health-based recommendations” (Wernham, 2011, p. 947-948).
Although application of HIAs is growing, use of this analytic approach in the United States is not yet widespread (Wernham, 2011). Lack of funds and limited training opportunities have slowed the adoption of HIAs in conventional public health practice. Additional legal requirements and methodological development may also be required to ensure the spread and utility of HIAs (Dannenberg et al., 2006; Lhachimi et al., 2010; Rajotte et al., 2011). For example, continued development of accessible, reliable microsimulation models is needed to create standard tools for quantifying health impacts in both biological and economic terms (Lhachimi et al., 2010).
Public Communications
Communication capacity represents a specialized area of expertise, as well as a complex, evolving science. Corporations invest billions in marketing (typically ranging from 1 to 20 percent of revenues depending on industry) in order to persuade consumers to purchase goods and services (CMO Council, 2010). As a result, consumers are inundated by information emanating from an ever-expanding variety of media outlets. Public health messages must compete for attention in this crowded, highly stylized, and sophisticated information landscape.
Many public health practitioners have recognized the magnitude of this challenge and are increasingly using social marketing techniques to educate the public about health risks and promote healthy behaviors (Grier and Bryant, 2005). Social marketing borrows commercial marketing principles and methods to reach the public and influence behaviors in a manner that benefits individual and collective interests. Like commercial marketing, social marketing is a consumer-focused endeavor that includes a sophisticated approach to (1) audience segmentation; (2) market research to clarify the target audiences’ beliefs, values, and attitudes; (3) the cost/benefit trade-offs associated with the promoted behavior; (4) competing behaviors that the audience may prefer to the promoted behavior; and (5) the development of a comprehensive marketing strategy based on these considerations (Pirani and Reizes, 2005). Application of these principles in a public health context can significantly improve the effectiveness of public campaigns to increase awareness of health risks and behavioral norms (Brooks and Deshpande, 2003).
Despite the potential benefits of social marketing to the success of public health interventions, capacity in this area is perceived to be undervalued and
underresourced within public health agencies. Anecdotal accounts suggest that preparedness funding has helped to build media communication capabilities within state and local health agencies. However, these efforts have rarely supported broader development in the social marketing capacity need to promote behavior change.
Interview respondents described deficits related to public health agencies’ capacity to do the following
• Use mass media (both paid and earned) to increase public awareness of health risks and promote healthy behaviors.
• Leverage innovative mechanisms (such as social media, text messaging, and “message placement” in entertainment programming) to create synergistic, multimedia communication platforms.
• Conduct formative research to guide the development of comprehensive social marketing campaigns.
Investment priorities related to these underdeveloped areas are discussed in the following sections.
Expanded Support for Mass Media Communications
Funding for mass media communications appears extremely limited and constrains the ability of state and local agencies to develop comprehensive social marketing campaigns. CDC has invested in some highly effective, media-based social marketing efforts (such as the VERB campaign) and has developed a variety of technical assistance resources related to social marketing. However, federal grants offer very limited direct financial support to state and local agencies’ health communications and social marketing activities.
Mass media communications represent an extremely powerful—and potentially cost-prohibitive—component of social marketing (Randolph and Viswanath, 2004). A few respondents emphasized the high costs associated with media buys, particularly in highly competitive, urban media markets. Although respondents generally concurred that capacity for paid media communications is underdeveloped in state and local public health agencies, some expressed skepticism that political support for capacity development in this area could be mustered.
Improved Ability to Customize Health Messages to Specific Target Audiences
Despite funding limitations, public health agencies are increasingly using mass media to promote healthy behaviors, sometimes in partnership
with private-sector funders (Cousins et al., 2011; Grier and Bryant, 2005; Maibach et al., 2007). Unfortunately, such efforts may lack adequate investments in formative market research and message development, undermining the reach and effectiveness of public health campaigns (Grier and Bryant, 2005; Whittingham et al., 2008). Additional financial support appears needed for qualitative and quantitative market research, message testing, evaluation of social marketing interventions, and media consultation.
IMPACT OF CATEGORICAL FUNDING ON DEVELOPMENT OF MISSION-CRITICAL CAPACITIES
Most governmental public health agencies appear to be heavily reliant on categorical funding, although the degree of this dependence seems to vary across jurisdictions. Categorical financing mechanisms support important programmatic activities, but such funding also imposes restrictions on the use of funds and can constrain the potential for strategic investments. However, interview respondents expressed some differences of opinion regarding the extent to which categorical funding has limited investments in the capacity-development priorities described in the preceding section of this paper.
Respondents generally agreed that categorical funding discourages coordination across programs; fosters a fragmented, inefficient deployment of public health resources; perpetuates a narrow view of the role of public health agencies; and hinders adaptation to changing population health needs and scientific advancements. However, respondents did not express consistent views on the extent to which categorical funding actually prevents the development of cross-cutting, mission-critical capacities.
The various perceptions of interview respondents suggest that the degree to which categorical funding hinders capacity development in mission-critical areas is somewhat contingent on several intersecting factors including the attitudes of public health officials; the nature and rigidity of formal and informal categorical restrictions imposed at the federal, state, and local levels; and the burden associated with categorical program requirements and deliverables. These variables and their potential influence on capacity development are explored in more detail below. However, a more rigorous, systematic study of the categorical funding mechanisms used at all levels of government may be needed to test the validity of these impressions.
Leadership Attitudes
Most respondents believe that proactive public health leaders are able to overcome the barriers imposed by categorical mechanisms. Such leaders are reportedly able to find innovative ways to align categorical resources and
effectively manage agency activities to ensure coordination across program areas. Some respondents emphasized that categorical restrictions leading to program silos are more a function of perception than reality. Others indicated that the design and administration of categorical funding streams create a variety of management challenges that demand an extraordinary level of creativity to overcome. These respondents felt it was both unreasonable and unproductive to expect the average state or local health official to put forth this amount of proactive effort. Some commentators have suggested that the contortions required of public health officials to navigate categorical obstacles can border on misrepresentation and raise ethical concerns (St. Luke’s Health Initiative, 2002).
Some respondents emphasized that the ability of public health agencies to attract and retain high-caliber leaders is severely constrained by heavy reliance on categorical funding. Because health officials have very limited discretion in resource allocation and other managerial decisions, creative, innovative leaders are discouraged from accepting or continuing in leadership positions within public health agencies.
Nature of Categorical Restrictions
Differences in respondent views may also relate to variations in their personal experiences and differences in the mix of categorical programs encountered. Several respondents noted that the rigidity of categorical restrictions can vary significantly depending on funding mechanism and administering agency. For example, categorical funding provided by the U.S. Department of Agriculture (USDA) to state and local health agencies for information system development related to the WIC program was frequently cited as particularly restrictive. Respondents indicated that formal guidance explicitly prohibited agencies from using grant-funded computer hardware and software for purposes other than the support of WIC services.
It is worth noting that respondents held inconsistent views with respect to the limitations imposed by specific categorical programs administered by the federal government. For example, some respondents felt that CDC preparedness grants offered a practical model for how a categorical mechanism could allow, and even encourage, the development of cross-cutting capacities. Others indicated that federal restrictions related to preparedness funding have evolved since the program’s inception and became significantly more permissive and flexible over time.
Concerns were also raised that while the policies of some federal categorical grants might permit a reasonable level of shared functionality across programs, the policies of other federal categorical programs could hinder state and local officials from taking full advantage of such flexibility. For example, one federal grant might allow personnel employed in other pro-
gram areas to cross-train in order to expand agency capacity for a particular activity. However, the “host” program for those staff might prohibit the allocation of personnel time outside of that program area.
Significant variations were also observed in state policies related to categorical funds provided to local agencies. Some states appear to be more restrictive than others based on several factors including the extent to which categorical mechanisms are used to distribute state funds, the rigidity of limitations defined for state categorical programs, the extent to which the state is reliant on federal categorical programs, and the manner in which federal guidance is interpreted and, in turn, conveyed to local agencies. These state-level variations appear to result in significant differences in the way that categorical restrictions are perceived at the local level.
Other respondents observed that some of the more explicitly restrictive language limiting resource sharing across programs is often imposed by project staff within federal and state agencies and is not embedded in statute or regulation. Explicit restrictions may be incorporated into formal grant guidance or contractual agreements, but less formal program management practices may also constrain the use of program funds. For example, contentious negotiations surrounding the establishment of agreements and contracts, as well as a difficult history of expenditure disallowances after a grant has been awarded, may dissuade public health agencies from investing categorical funds in cross-cutting capacities that could benefit other program areas.
Burden of Categorical Program Requirements
Categorical funding may also undermine the development of mission-critical capacities in more subtle, indirect ways owing to the programmatic, management, and reporting burdens associated with these funding streams. For example, some respondents indicated that the deliverables required for some categorical programs require a level of investment that exceeds the resources awarded for those purposes, requiring grantees to deplete more flexible sources of state or local funding in order to support categorical objectives. Other program requirements, such as the mandated establishment of program-specific community advisory boards and assessments, can conflict or interfere with broader community health planning efforts. Some respondents indicated that the timing and nature of these program-specific requirements often create insurmountable obstacles to integrated community outreach and planning.
The consuming demands of program-specific activities, along with extensive financial reporting requirements related to staff time allocations and other categorical program costs, also contribute to the formation of intra-agency silos (Slonim et al., 2007). The divisive influence of categori-
cal funding creates significant management challenges and discourages the development of centralized or shared functional capacity capable of serving broad organizational needs (ASTHO, 2009). The negative impact of this fragmentation appears particularly acute in highly specialized functional areas (e.g., informatics, communications, and epidemiology) that require significant expertise and often demand more highly compensated personnel. Individual programs often lack sufficient funding to support these functions independently, yet the organizational cultures and management practices that have evolved in response to categorical incentives frequently deter a more efficient pooling of resources to develop adequate capacity in these areas.
FINANCING STRATEGIES USED TO BUILD MISSION-CRITICAL CAPACITIES
Agencies that have made progress building mission-critical capacities in the priority areas described above appear to use a wide variety of funding sources to support these investments, including
• flexible funds from local government,
• flexible funds from state government,
• cross-subsidization from reimbursement- and fee-based services,
• categorical program funds, and
• private-sector grants from philanthropic organizations, health system partners, and corporate foundations.
In most instances, capacity development relied on two or more of these various funding sources. However, few clear patterns emerged regarding the financing strategies most commonly pursued or the relative importance of each type of funding source. The lack of a clear typology for these financing strategies likely reflects the diverse fiscal policies that characterize public health finance across the nation, differences in the nature and level of the development investments described by interview respondents, and, to some degree, limitations in the qualitative methods used to gather information for this paper.
Relatively few respondents had made substantial investments in all of the mission-critical capacity-development needs identified, and most focused their remarks on strategies used to finance development in one or two major capacity domains. To the extent that capacity-development investments had been made in multiple areas, respondents typically described their financing strategies in broad terms and were not asked to supply detailed budgets or revenue allocations for specific activities. Because of the informal qualitative nature of these interviews, it is difficult to form conclusions.
Interview respondents typically used the terms “piecing,” “stitching,” “cobbling,” or “crocheting” funding together to support capacity development in cross-cutting mission-critical areas. These capacities are viewed as investment priorities by innovative leaders who “find ways” to fund their development—in whatever manner is most feasible given the idiosyncratic funding opportunities and obstacles experienced. In light of these variations, the following narrative provides a general description of each major type of funding source used to build mission-critical capacities and summarizes salient issues regarding the perceived availability and usefulness of each. To the extent clear differences of opinion were expressed by respondents, alternative perspectives are noted.
Flexible Funds from Local Government
Funds provided to local health departments by local governments were frequently cited as an important source of flexible dollars that can be invested in mission-critical capacities. Relative to state and federal funding sources, local health officials appear to have more discretion over the use of local funds and may be able to use this flexibility to address priority capacity-development needs. However, respondents cautioned that the usefulness of local funding to enhance public health capacity and performance is likely contingent on the level of local funding available, the extent to which categorical restrictions are imposed by local governance bodies, and the motivation of local health officials to make strategic investments. These issues have not been studied widely.
Although the evidence base is limited, research findings support the notion that the availability of funding from local sources may be a particularly important predictor of local health departments’ ability to perform the essential services of public health. A sample-based study conducted by Honoré et al. (2004) revealed a positive association between self-assessed agency performance and the per capita amount of local tax revenue dedicated to public health, yet found no significant correlation between performance and total per capita public health funding. The authors postulated that “the ability to determine the use of revenues at the local level is a factor to increasing performance” (Honoré et al., 2004, p. 449). This conclusion is consistent with findings of other researchers who have demonstrated that agency performance is positively associated with the presence of a local board of health if that board has policy-making authority (Bhandari et al., 2010). Strong financial support from local government also appears to improve the likelihood that a local health agency will attract state and federal funds (Bernet, 2007). But this causal relationship is not clearly established; it is also possible that state and federal funding encourage local investments.
Nationally, the level of locally financed funding for local health departments has not been fully documented. In 2008, local health departments received an average of 25 percent of total funding from local government sources, and expenditures averaged $64 per capita, suggesting that local funds provided approximately $16 per capita.10 However, the contribution of locally financed funds varies widely by state, ranging from 61 percent of total spending (New Jersey) to 2 percent of total funding (South Carolina) (NACCHO, 2009). These differences in the proportion of local agency budgets derived from local funding sources are difficult to interpret in light of wide variations in agencies’ total per capita spending (Mays and Smith, 2009). More specific data on per capita spending of local funds by local health departments have not been reported publicly.
The extent to which local public health funds are restricted to specific categorical purposes is somewhat unclear, as the nature and prevalence of locally imposed categorical restrictions have not been well studied. Respondents believed that the flexibility of local funding is highly variable across jurisdictions and may depend, in part, on the financing mechanism used to distribute local tax dollars. Like most activities of local government, local funding for public health is largely drawn from property taxes (Honoré et al., 2011). Funding levels may be determined through either (1) an annual appropriations process during which general fund dollars are allocated by a governing body (such as a county board of commissioners) for public health and other local government purposes, or (2) a dedicated property tax that levies a legally specified tax millage rate against assessed property values to raise revenues expressly for public health agency operations.
Although the relative merits of these alternative mechanisms are not well established, dedicated taxes are often perceived as a more stable, flexible financing strategy than yearly budget negotiations. Revenues raised through dedicated taxes are subject to fluctuation owing to changes in local property values,11 and local policy makers may impose conditions on a public health agency’s use of dedicated revenues. However, resource allocations established through a yearly, politically charged budget process are likely to be even less predictable and more restrictive than those determined through a dedicated millage rate.
The adoption of dedicated property taxes for public health, the millage rates applied for these purposes, and the impact of these policies have not been fully documented.12 Limited evidence indicates that dedicated public
______________
10Assumes revenues are roughly equal to expenditures.
11These fluctuations tend to be modest and somewhat predictable as assessed property values are less volatile than market prices (Lutz et al., 2011).
12Local governments have the authority to levy dedicated taxes for public health in approximately 10 states, but the extent to which these authorities have been exercised in these states is unclear (Personal communication with Peggy Honoré, June 30, 2011).
health tax mechanisms are associated with improved community health outcomes except in low-income communities (Honoré et al., 2011). Honoré and colleagues suggest that policy debates surrounding the establishment or retention of a dedicated local tax can provide a powerful opportunity for engaging the public in the role and contributions of the governmental public health infrastructure (Honoré et al., 2011). Respondents echoed the recommendations of these researchers in advocating for additional scientific study to explore the causal relationships between local funding policies and the capacity and performance of public health agencies.
Despite the positive effect local funding appears to have on capacity development, an overreliance on local funds can be detrimental to community health and public health performance. As demonstrated by recent budget cuts, the fiscal solvency of local government is very sensitive to economic downturns owing in part to prohibitions against deficit spending (CBO, 2010). Politically based resource allocation decisions often disregarded evidence from objective analyses in response to budgetary pressure (Honoré et al., 2010). Funding for public health purposes (both appropriated and dedicated) may be particularly vulnerable to cuts given limitations in policy makers’ understanding of population-based services (Berk & Associates, 2006; Libbey and Miyahara, 2011). Perhaps more importantly, a community’s health needs and financial resources are often asymmetric, further validating the need for the diversification of revenue streams beyond local sources (Honoré et al., 2011).
Flexible Funds from State Government
The nature of community health promotion inherently involves interventions focused at the local level, but this focus does not diminish the potential role for investment by state government. Several interview respondents indicated that state funds have been used to build the capacity of state health agencies, particularly in development related to innovative surveillance and epidemiology capabilities. State-sponsored training, technical assistance, and analytic support designed to strengthen and augment local capacity were also referenced as valuable resources to address capacity-development priorities.
Respondents with current or prior experience working in local health agencies generally acknowledged the broad systemic benefits of investments in state health agency capacity, but they often focused their remarks on the usefulness of direct financial support from state government. Several respondents indicated that state funding had been used to build local capacity in mission-critical areas, using both categorical and noncategorical funds.
Several states use terms like base funding, core services, or general aid to describe certain contractual or grant mechanisms used to distribute funds to
local health departments. The nature of these generic funding mechanisms appears to vary widely. In a few states (e.g., Washington,13 New York, and Florida) these general mechanisms provide flexible, noncategorical funds that local officials may use to deliver core services (Livingood et al., 2011; NYSACHO, 2001; Washington State Department of Health, 2008). In other states, “base” funding mechanisms may be used to bundle federal categorical dollars with associated categorical restrictions and programmatic requirements applied to the use of these dollars. Mechanisms financed solely or primarily with state general fund dollars may be less restrictive than those funded by state and federal categorical programs, but these issues have not been well studied.
The provision of noncategorical funds by state government to local health departments does not appear to be widespread, and the funding levels offered may be modest. However, even when funds are limited and do not fully cover related capacity-development costs, flexible state dollars may assist local health departments in securing other sources of flexible funding. State funding may cultivate some level of foundational capacity that can then be leveraged to attract competitive grants offered by the federal government and the private sector. This “seeding” effect appears most evident in localities that have benefited from long-standing, flexible core support from states.
Flexible state funding also has the potential to encourage local investments in local health departments. In some cases, states may require local governments to provide matching funds in order to draw-down state dollars. Although opinions were mixed regarding the merits of local match requirements, some respondents indicated that these types of mandates can protect local funds from budget cuts as local policymakers seek to avoid sacrificing revenue from external sources.
Respondents cautioned, however, that that noncategorical support provided to local health departments by state government has been significantly reduced in recent years due to both the fiscal pressures facing states and increased adoption of performance-based budgeting. These anecdotal reports are difficult to document nationally given limited information regarding state investments in local health agencies specifically and in public health more broadly. The complexity and variability of financial relationships between state and local governments compound the challenges of fully characterizing the nature and availability of flexible public health funding provided by states to localities. The extent to which local health departments actually use flexible state funding to develop the mission-critical capacities identified in this paper is also unclear.
______________
13In Washington flexible funding is distributed to local health departments through three mechanisms financed by the state’s General Fund that together provided approximately $84 million in the 2007-2009 biennium period.
The proportion of state-financed investments expended at the local level and the extent to which these funds are offered through noncategorical mechanisms are not well documented. NACCHO reports significant variations in local health departments’ reliance on state funding. Nationwide, approximately 20 percent of local health department revenue was derived from state sources in 2008 (excluding federal pass-through), reflecting roughly $13 per capita in state-financed expenditures by local health departments. State-specific contributions ranged from median levels of 55 percent in Pennsylvania14 to 5 percent in neighboring Ohio. However, revenue sources used to finance state aid may not be transparent to local health officials, suggesting that revenue attributed to state sources may be overestimated.
Numerous issues surrounding state financing for public health are not well documented, including
• the level of resources invested by states in the public health infrastructure,
• the proportion of state investments distributed respectively to local health departments, state agencies, and private-sector organizations,
• the nature of the mechanisms used to distribute these funds,
• the source of revenue used to fund these investments, and
• the financing mechanisms used to generate these revenues.
Preliminary data from the ASTHO 2010 Profile indicates that in 2009 state health agencies’ total expenditures averaged $98 per capita in 2009, and approximately 40 percent of total agency revenues were derived from state general funds or other state-financed funds15 (Sellers, 2011). Taken together these data suggest that state governments contributed an average of roughly $39 per capita to state and local public health activities in 2009.
Interview respondents generally agreed that public health capacity at both the state and local level would benefit from additional funding from states, particularly in states that currently contribute minimal revenue to public health efforts. Significant variation in state support for public health is widely acknowledged, but available evidence lacks precision regarding the nature, magnitude, cause, and effect of these differences. The Trust for America’s Health (TFAH) reports that in fiscal years 2009-2010, state contributions16 ranged from $3.40 per capita in Nevada to $171.30 in Hawaii
______________
14Most county health departments in Pennsylvania are fully funded by the state and offer limited services. Only 10 local jurisdictions (six county, four municipal) have established independent local health departments. Also, NACCHO notes low response rates from local health units in Pennsylvania, raising questions about data accuracy for this state.
15Federal funds represented 45 percent of total state health agency revenues in FY 2009.
16TFAH estimates the median value of state government investment in public health (excluding federal pass-through) at $30.61 per capita in FY 2009-2010.
(TFAH, 2011). Despite efforts by TFAH to minimize inconsistencies resulting from state-level variability in both organizational structure and financial reporting, data limitations17 undermine the comparability of per capita state spending estimates. While data artifacts compromise the accuracy of state-specific estimates, it is not likely that these structural factors fully account for the wide disparities observed in state revenue devoted to public health.
“Braided” Funding from Categorical Programs
As described in above, respondents indicated that categorical funds are being used to support the development of mission-critical capacities despite the challenges associated with these funding streams. The magnitude of these challenges appears to be strongly influenced by the degree to which an agency relies on categorical dollars, as well as the specific nature of the restrictions and requirements associated with those categorical programs. These dynamics appear to play out differently across jurisdictions.
Unfortunately, the scale and scope of this effort did not allow an in-depth exploration of these issues. The experiences of respondents may not be representative, and detailed information was not gathered regarding either the specific categorical funds leveraged or the management techniques used to coordinate across program areas. However, the interviews did yield some interesting observations that may be valuable in identifying issues for future study.
Some agencies have benefited from federal grants and cooperative agreements specifically focused on capacity development in the mission-critical areas identified, such as CDC’s Assessment Initiative and more recently the National Public Health Improvement Initiative. These types of targeted categorical programs are expressly designed to support capacity development in one or more of the priority areas identified. However, awards are often made on a competitive basis or, if non-competitive, offer limited financial support. Such programs focused on public health capacity development appear to represent a relatively small proportion of categorical funding.
More traditional programmatic funds, such as CDC’s Public Health Emergency Preparedness cooperative agreements and the Health Resources and Services Administration’s Rural Health Network Development grants, have also contributed to capacity development in mission-critical areas. Though focused more narrowly on specific programmatic goals, these
______________
17For example, Hawaii’s highly centralized public health structure (common to states with relatively compact geography) explains, in part, the high level of per capita funding reported as expenditures include investments at both the state and local level. Conversely, in other states detailed budgets are not publicly available so spending estimates are based solely on allocations from state General Funds (as noted in TFAH’s reports) and funding from alternative revenue sources (such as trusts established with tobacco settlement funds) may be excluded.
categorical funds support activities, such as partnership development and community outreach, which have a “spill-over” effect on other program areas and create a foundation for cross-cutting capacity. A wide variety of state and federal categorical programs appear to fund narrowly defined aspects of the mission-critical capacities identified. As described in the preceding section, the various activities of these funded programs can often be successfully coordinated to build more generalized cross-cutting capacity. Yet, numerous management challenges often hinder this type of integrated approach, and tactical shifts within categorical programs can undermine the sustainability of core capacities.
Respondents also expressed concerns that federal categorical programs largely target funds at the state level, and because of the modest size of these awards, limited amounts of federal categorical funding trickle down to local agencies. ASTHO reports that of the $14 billion in federal funds received by state health agencies in fiscal year 2009, approximately 60 percent was directly distributed to local and regional health departments (Sellers, 2011). However, this statistic is significantly influenced by WIC funding, which accounts for roughly half of federal funds provided to state health agencies.
Cross-Subsidization from Reimbursement-Based and Fee-Based Services
Respondents offered mixed perspectives regarding the extent to which revenues generated from reimbursement- and fee-based services support capacity development. Revenue generating activities include the provision of clinical services, regulatory functions (e.g., restaurant inspections), and record management services (e.g., birth certificates). Although no respondents suggested that this type of revenue was the sole or dominant contributor to mission-critical capacities, several respondents did indicate that excess revenues from other service areas were used to fund development efforts. Others indicated that fee- and reimbursement-based activities were barely self-sustaining or even dependent on other sources of resource and did not offer a viable source of funds for capacity development.
The amount of revenue available for intra-agency redistribution appears to be influenced by a variety of factors including the extent to which an agency engages in revenue-generating services, the payment rates associated with these services, the efficiency of service providers, and policies toward resource sharing among organizational units. Variation in these characteristics has not been well documented.
Approximately 11 percent of state health agency revenue and 26 percent of local health department revenue were derived from fee- and reimbursement-based activities in fiscal year 2009 (NACCHO, 2009; Sellers, 2011). For state agencies, fees and fines represented a larger proportion of total
revenue (7 percent) than reimbursement through Medicare and Medicaid (4 percent). For local health departments, reimbursement (15 percent) provided a larger proportion of revenue than fees (11 percent). However, these relative proportions vary widely by agency and are significantly influenced by the role a public health agency plays in health care service delivery.
Public health agencies’ ability to influence payment rates for revenue-generating services appears limited. Local health departments have little influence in setting reimbursement rates for Medicaid and Medicare. The adequacy of these reimbursement rates relative to costs is likely to vary among agencies. Theoretically local health departments exert more control over the payment rates associated with regulatory and other fee-based services. However, fees may be dictated by state law and, even if determined locally, are often constrained by political pressure from the regulated industries that bear the cost of public health fees. Rate increases intended to finance general capacity, rather than the direct costs of providing fee-based services, are likely to face especially vocal opposition.
A few respondents specifically commented on the usefulness of Medicaid Management Information Systems (MMIS) funding for developing interoperable public health information systems. CMS offers an enhanced match for MMIS improvements, and under certain conditions this funding may be used to develop public health information systems (Blavin and Ormond, 2011).
Private-Sector Grants from Philanthropic Organizations, Health System Partners, and Corporate Foundations
Most respondents cited the use and importance of private-sector funds in building mission-critical capacity, particularly during the early stages of development. The Turning Point Initiative, sponsored by the W.K. Kellogg Foundation and the Robert Wood Johnson Foundation (RWJF) was frequently acknowledged as an important catalyst for reorienting state and local public health agencies. Although funds are no longer being distributed through this philanthropic program, several respondents believe that these investments are yielding lasting capacity improvements that are now being sustained through the other financing mechanisms described above. Funding through the RWJF Multi-State Learning Collaborative was also credited as important source of revenue for stimulating further advances in capacity development.
Contributions of private-sector funders do not appear to be limited to large national health foundations. Respondents frequently cited support from smaller state, regional, and local philanthropies and also described both direct financial and in-kind support provided by health system partners. Support from hospitals was often cited as particularly important. As
the commissioned paper prepared by Sara Rosenbaum explores in additional detail, new community benefit requirements under federal law may be encouraging increased support for public health agencies by tax-exempt hospitals (see Appendix B).
Grants from locally based private-sector funders appear to represent ongoing sources of support for sustaining mission-critical capacity, as well as point-in-time investments to kick-start or accelerate specific development activities. The use of fiscal intermediaries, such as Public Health Institutes, was cited as a useful strategy for securing and using private-sector funds (ASTHO, 2009).
Policy Change Proposals
Based on their experiences using existing funding opportunities to finance capacity development in mission-critical areas, respondents were asked to share suggestions for policy changes that would enhance the ability of public health agencies to adopt an ecologically oriented, population-based approach to disease prevention and health promotion that addresses the broad socioenvironmental determinants of health. While suggestions varied somewhat by respondent, proposals tended to cluster around the need to do the following
• Create dedicated, stable funding for the development of mission-critical capacity. Many respondents indicated that existing funding streams, both categorical and noncategorical in nature, were insufficient to adequately support the development of mission-critical capacities in state and local agencies. Although most acknowledged the benefits of flexible financing, many questioned the political defensibility of noncategorical funding. Many respondents believed that categorical program expressly dedicated to capacity development offered a more viable option for investment and would allow for better accountability in both characterizing existing capacity levels and documenting progress made moving forward. A few respondents did advocate for flexible funding, arguing that a noncategorical approach would allow public health officials to adapt to changing needs and technologies. Some believed that funding for public health capacity development, whether categorical or flexible in nature, should be financed through a predictable, dedicated revenue stream (e.g., property tax mill rate, a motor vehicle excise tax, a tax on health insurance premiums, a tax on sweetened carbonated beverages, or another type of dedicated tax).
• Reduce barriers to cross-cutting capacity development in existing categorical programs. Many respondents indicated that changes in
• existing categorical programs were necessary to minimize the obstacles hindering the development of cross-cutting capacity. While most focused on reducing or eliminating categorical restrictions, others emphasized the need for explicit guidance encouraging the coordination of resources across programs and incentivizing the development of shared capacities. These respondents felt that clear guidance on permissible or preferred approaches to resource allocation would be necessary, given the long history of categorical restrictions. For example, some respondents suggested categorical programs should allow higher indirect cost rates in order to recognize and fund the core capacities upon which programmatic activities rely.
• Establish incentives that promote diversified funding for strategic investments. Many respondents indicated that increased support from local, state, federal, and private sources would be needed to build robust capacity in state and local health agencies. Several respondents suggested that financing policies should create incentives for additional investments by each of these stakeholder groups and promote a more efficient alignment of public health resources.
A few respondents focused specifically on the creation of either federal matching grants for state investment in local health department capacity or state matching grants for local investments in public health capacity. Proponents of matching grants suggested that these types of funding mechanisms would promote a shared commitment to capacity investments across multiple levels of government. Requiring local, state, and federal partners to have “skin in the game” was viewed as a necessary ingredient for diversifying funding, and perhaps more importantly, for establishing a shared vision regarding performance expectations and accountability processes. Respondents recognized that match-based funding would need to be carefully structured to both achieve these goals and protect against potential drawbacks. For example, some respondents suggested that match rates could be customized to accommodate the relative affluence of individual states or localities, and preferential rates could be used to create incentives for specific types of investments, regional collaboration, agency accreditation, or other desired practices.
CONCLUSION
A clear consensus emerged from the respondent interviews regarding the need for improved and expanded capacity in state and local health agencies related to surveillance and epidemiology, community health improvement
planning, partnership development, policy decision support, and public communication. Respondents indicated that additional investments are needed to increase the number and skills of the public health workforce (particularly for personnel with expertise in informatics, communications, financial management, epidemiology, and other analytic competencies), to develop interoperable surveillance systems, and to improve the evidence base surrounding public health interventions and management best practices.
Historically categorical funding mechanisms have created obstacles to the development of cross-cutting capacities and have often fostered a fragmented, inefficient alignment of public health resources. Categorical funding streams have also contributed to ossification within the governmental public health infrastructure, limiting agencies’ ability to use scientific advancements and adapt to evolving population health needs. Perhaps most importantly, the dominance of these restrictive funding mechanisms has perpetuated a narrow vision for the potential role and contributions of state and local public health agencies—implying that their mission is merely the sum of categorical parts, rather than a comprehensive, holistic strategy to prevent disease and promote health.
Despite these challenges, innovative public health leaders have successfully used categorical funding in tandem with more flexible funding from local, state, and private sources to build capacity in mission-critical areas. These exploratory findings suggest that diversified funding is needed to support strategic investments in public health capacity development. Additional study may be needed to fully characterize the existing portfolio of funding mechanisms currently supporting state and local agencies and to identify the optimal level, mix, and structure of financing needed to ensure adequate capacity development in mission-critical areas.
Respondents suggested that public health finance policy should be refocused to encourage additional investments across all levels of government and to promote a more efficient coordination of public health resources. Finance policies should reduce categorical restrictions that hinder the development of cross-cutting capacity, dedicate funds to capacity-development priorities, and create financial incentives for rational investments.
REFERENCES
Abarca, C., C. M. Grigg, J. A. Steele, L. Osgood, and H. Keating. 2009. Building and measuring infrastructure and capacity for community health assessment and health improvement planning in Florida. Journal of Public Health Management & Practice 15(1):54-58.
Ali, R., D. Wheitner, E. O. Talbott, and J. V. Zborowski. 2007. Connecting environmental health data to people and policy: Integrating information and mobilizing communities for environmental public health tracking. Journal of Community Health 32(5):357-374.
Anderson, L. M., R. C. Brownson, M. T. Fullilove, S. M. Teutsch, L. F. Novick, J. Fielding, and G. H. Land. 2005. Evidence-based public health policy and practice: Promises and limits. American Journal of Preventive Medicine (5 Suppl):226-230.
Asaro, P. V., G. H. Land, and J. W. Hales. 2001. Making public health data available to community-level decision makers—Goals, issues, and a case report. Journal of Public Health Management & Practice 7(5):58-63.
ASPHL (Alaska State Public Health Laboratory). 2007. State Environmental Health Laboratories: Capabilities and Capacity. Silver Spring, MD: ASPHL.
ASTHO (Association of State and Territorial Health Officials). 2009. State Perspectives on the Use of Fiscal Intermediaries. Washington, DC: ASTHO.
ASTHO. 2011. Budget Cuts Continue to Affect the Health of Americans: Update May 2011. Washington, DC: ASTHO.
Baker, E. L., M. A. Potter, D. L. Jones, S. L. Mercer, J. P. Cioffi, L. W. Green, P. K. Halverson, M. Y. Lichtveld, and D. W. Fleming. 2005. The public health infrastructure and our nation’s health. Annual Review of Public Health 26:303-318.
Bales, M. E., S. B. Johnson, J. W. Keeling, K. M. Carley, F. Kunkel, and J. A. Merrill. 2011. Evolution of coauthorship in public health services and systems research. American Journal of Preventive Medicine 41(1):112-117.
Baum, N. M., C. DesRoches, E. G. Campbell, and S. D. Goold. 2011. Resource allocation in public health practice: A national survey of local public health officials. Journal of Public Health Management & Practice 17(3):265-274.
Bazzoli, G. J., E. Casey, J. A. Alexander, D. A. Conrad, S. M. Shortell, S. Sofaer, R. Hasnain-Wynia, and A. P. Zukoski. 2003. Collaborative initiatives: Where the rubber meets the road in community partnerships. Medical Care Research Review 60(4 Suppl):S63-S94.
Beitsch, L. M., R. G. Brooks, M. Grigg, and N. Menachemi. 2006. Structure and functions of state public health agencies. American Journal of Public Health 96(1):167-172.
Beitsch, L. M., C. Leep, G. Shah, R. G. Brooks, and R. M. Pestronk. 2010. Quality improvement in local health departments: Results of the NACCHO 2008 survey. Journal of Public Health Management & Practice 16(1):49-54.
Bender, K., and P. K. Halverson. 2010. Quality improvement and accreditation: What might it look like? Journal of Public Health Management & Practice January/February 16(1):79-82.
Berk & Associates. 2006. Financing Local Public Health in Washington State: Challenges and Choices. Report to the Public Health Improvement Plan Finance Committee. Seattle, WA: Berk & Associates.
Bernet, P. 2007. Local public health agency funding: Money begets money. Journal of Public Health Management & Practice 13(2):188-193.
Bhandari, M. W., F. D. Scutchfield, R. Charnigo, M. C. Riddell, and G. P. Mays. 2010. New data, same story? Revisiting studies on the relationship of local public health systems characteristics to public health performance. Journal of Public Health Management & Practice 16(2):110-117.
Birkhead, G. S., and HHS. 2010. Achieving Population Health Through Meaningful Use: How Do Governmental Public Health Agencies View the Process to Date? HIT Policy Committee Meaningful Use Workgroup. Washington, DC: HHS, Office of the National Coordinator for Health Information Technology.
Blavin, F., and B. Ormond. 2011. HITECH, Meaningful Use, and Public Health: Funding Opportunities for State Immunization Registries. Washington, DC: Urban Institute.
Braveman, P. A., S. A. Egerter, S. H. Woolf, and J. S. Marks. 2011. When do we know enough to recommend action on the social determinants of health? American Journal of Preventive Medicine 40(1 Suppl 1):S58-S66.
Brooks, R., and S. Deshpande. 2003. Social Marketing and Public Health Lessons from the Field. Seattle, WA: Turning Point National Program Office at the University of Washington.
Brooks, R. G., L. M. Beitsch, P. Street, and A. Chukmaitov. 2009. Aligning public health financing with essential public health service functions and National Public Health Performance Standards. Journal of Public Health Management & Practice 15(4):299-306.
Brownson, R. C., J. E. Fielding, and C. M. Maylahn. 2009. Evidence-based public health: A fundamental concept for public health practice. Annual Review of Public Health 30:175-201.
Byrne, C., J. B. Crucetti, M. G. Medvesky, M. D. Miller, S. J. Pirani, and P. R. Irani. 2002. The process to develop a meaningful community health assessment in New York State. Journal of Public Health Management & Practice 8(4):45-53.
CBO (Congressional Budget Office). 2010. Fiscal Stress Faced by Local Governments. Washington, DC: CBO.
CDC (Centers for Disease Control and Prevention). 2006. Recommendations for Future Efforts in Community Health Promotion. Atlanta, GA: CDC.
CDC. 2010. Community Health Assessment and Group Evaluation (CHANGE): Building a Foundation of Knowledge to Prioritize Community Health Needs. Atlanta, GA: CDC.
Cheadle, A., C. Hsu, P. M. Schwartz, D. Pearson, H. P. Greenwald, W. L. Beery, G. Flores, and M. C. Casey. 2008. Involving local health departments in community health partnerships: Evaluation results from the Partnership for the Public’s Health Initiative. Journal of Urban Health 85(2):162-177.
CMO (Chief Marketing Officer) Council. 2010. State of Marketing: Outlook, Intentions and Investments for 2010. Palo Alto, CA: CMO Council.
Congdon, P. 2009. A multilevel model for cardiovascular disease prevalence in the U.S. and its application to micro area prevalence estimates. International Journal of Health Geographics 8:6.
Congdon, P. 2010. A multilevel model for comorbid outcomes: Obesity and diabetes in the United States. International Journal of Environmental Research and Public Health 7(2):333-352.
Cossman, R. E., J. S. Cossman, W. L. James, T. Blanchard, R. K. Thomas, L. G. Pol, A. G. Cosby, and D. M. Mirvis. 2008. Evaluating heart disease prescriptions-filled as a proxy for heart disease prevalence rates. Journal of Health Human Services Administration 30(4):503-528.
Costich, J. F., P. A. Honoré, and F. D. Scutchfield. 2009. Public health financial management needs: Report of a national survey. Journal of Public Health Management & Practice 15(4):307-310.
Council on Linkages. 2005. Public Health Systems Research: Summary of Research Needs. Council on Linkages between Academia and Public Health Practice. Washington, DC: Public Health Foundation.
Council on Linkages. 2010. Core Competencies for Public Health Professionals. Council on Linkages Between Academia and Public Health Practice. Washington, DC: Public Health Foundation.
Cousins, J. M., S. M. Langer, L. K. Rhew, and C. Thomas. 2011. The role of state health departments in supporting community-based obesity prevention. Preventing Chronic Disease 8(4):A87. http://www.cdc.gov/pcd/issues/2011/jul/10_0181.htm (accessed August 12, 2011).
CSTE (Council of State and Territorial Epidemiologists). 2009a. National Assessment of Epidemiology Capacity: Supplemental Report on Chronic Disease Epidemiology Capacity. Atlanta, GA: CSTE.
CSTE. 2009b. National Assessment of Epidemiology Capacity. Atlanta, GA: CSTE.
CSTE. 2009c. State Injury Indicators Report, Fourth Edition—2005 Data. Atlanta, GA: CSTE.
Curtis, D. C. 2002. Evaluation of community health assessment in Kansas. Journal of Public Health Management & Practice 8(4):20-25.
Dannenberg, A. L., R. Bhatia, B. L. Cole, C. Dora, J. E. Fielding, K. Kraft, D. McClymont-Peace, J. Mindell, C. Onyekere, J. A. Roberts, C. L. Ross, C. D. Rutt, A. Scott-Samuel, and H. H. Tilson. 2006. Growing the field of health impact assessment in the United States: An agenda for research and practice. American Journal of Public Health 96(2):262-270.
Drewnowski, A., C. D. Rehm, and D. Solet. 2007. Disparities in obesity rates: Analysis by ZIP code area. Social Science & Medicine 65(12):2458-2463.
Duffy, R. E., and P. Z. Siegel. 2009. Increasing chronic disease epidemiology capacity without increasing workforce: A success story in Ohio. Journal of Public Health Management & Practice 15(2):123-126.
Easterling, D. 2003. What have we learned about community partnerships? Medical Care Research and Review 60(4 Suppl):S161-S166.
Erwin, P. C. 2008. The performance of local health departments: A review of the literature. Journal of Public Health Management & Practice 14(2):E9-E18.
Erwin, P. C., S. B. Greene, G. P. Mays, T. C. Ricketts, and M. V. Davis. 2011. The association of changes in local health department resources with changes in state-level health outcomes. American Journal of Public Health 101(4):609-615.
Fehrenbach, S. N., J. C. Kelly, and C. Vu. 2004. Integration of child health information systems: Current state and local health department efforts. Journal of Public Health Management and Practice Suppl(Nov):S30-S35.
Fielding, J. E., C. E. Sutherland, and N. Halfon. 1999. Community health report cards. Results of a national survey. American Journal of Preventive Medicine 17(1):79-86.
Finison, L. J. 2007. Community Health Data Scan for Connecticut. New Britain: Connecticut Health Foundation.
Friedman, D. J. 2007. Assessing Changes in the Vital Records and Statistics Infrastructure. Silver Spring, MD: National Association for Public Health Statistics and Information Systems.
Friedman, D. J., and R. G. Parrish, 2nd. 2006. Characteristics, desired functionalities, and datasets of state web-based data query systems. Journal of Public Health Management & Practice 12(2):119-129.
Friedman, D. J., and R. G. Parrish. 2009. Is community health assessment worthwhile? Journal of Public Health Management & Practice 15(1):3-9.
Friedman, D. J., and R. G. Parrish. 2010. The population health record: Concepts, definition, design, and implementation. Journal of the American Medical Informatics Association 17:359-366.
Grier, S., and C. A. Bryant. 2005. Social marketing in public health. Annual Review of Public Health 26:319-339.
Grigg, M., B. Alfred, C. Keller, and J. A. Steele. 2006. Implementation of an Internet-based geographic information system: The Florida experience. Journal of Public Health Management & Practice 12(2):139-145.
Harris, J. K., K. E. Beatty, J. D. Lecy, J. M. Cyr, and R. M. Shapiro, 2nd. 2011. Mapping the multidisciplinary field of public health services and systems research. American Journal of Preventive Medicine 41(1):105-111.
Honoré, P. A., and J. F. Costich. 2009. Public health financial management competencies. Journal of Public Health Management & Practice 15(4):311-318.
Honoré, P. A., and T. Schlechte. 2007. State public health agency expenditures: Categorizing and comparing to performance levels. Journal of Public Health Management & Practice 13(2):156-162.
Honoré, P. A., and W. Scott. 2010. Priority Areas for Improvement of Quality in Public Health. Washington, DC: HHS.
Honoré, P. A., E. J. Simoes, W. J. Jones, and R. Moonesinghe. 2004. Practices in public health finance: An investigation of jurisdiction funding patterns and performance. Journal of Public Health Management & Practice 10(5):444-450.
Honoré, P. A., R. L. Clarke, D. M. Mead, and S. M. Menditto. 2007. Creating financial transparency in public health: Examining best practices of system partners. Journal of Public Health Management & Practice 13(2):121-129.
Honoré, P. A., P. J. Fos, T. Smith, M. Riley, and K. Kramarz. 2010. Decision science: A scientific approach to enhance public health budgeting. Journal of Public Health Management & Practice 16(2):98-103.
Honoré, P. A., P. J. Fos, X. Wang, and R. Moonesinghe. 2011. The effects on population health status of using dedicated property taxes to fund local public health agencies. BMC Public Health 11(1):471-480.
IOM (Institute of Medicine). 2011. For the Public’s Health: The Role of Measurement in Action and Accountability. Washington, DC: The National Academies Press.
Irani, P., C. Bohn, C. Halasan, M. Landen, and D. McCusker. 2006. Community health assessment: Driving the need for current, easily accessible population health data. Journal of Public Health Management & Practice 12(2):113-118.
Jacobs, L. M., and J. J. Elligers. 2009. The MAPP approach: Using community health status assessment for performance improvement. Journal of Public Health Management & Practice 15(1):79-81.
Kassler, W. J., and Y. P. Goldsberry. 2005. The New Hampshire public health network: Creating local public health infrastructure through community-driven partnerships. Journal of Public Health Management & Practice 11(2):150-157.
Keane, C., J. Marx, and E. Ricci. 2003. Local health departments’ mission to the uninsured. Journal of Public Health Management & Practice 24(2):130-149.
Kegler, M. C., J. E. Painter, J. M. Twiss, R. Aronson, and B. L. Norton. 2009. Evaluation findings on community participation in the California Healthy Cities and Communities program. Health Promotion International 24(4):300-310.
Keller, L. O., M. A. Schaffer, B. Lia-Hoagberg, and S. Strohschein. 2002. Assessment, program planning, and evaluation in population-based public health practice. Journal of Public Health Management & Practice 8(5):30-43.
Klompas, M., and D. S. Yokoe. 2009. Automated surveillance of health care-associated infections. Clinical Infectious Diseases 48(9):1268-1275.
Koivusalo, M. 2010. The state of Health in All Policies (HiAP) in the European Union: Potential and pitfalls. Journal of Epidemiology and Community Health 64(6):500-503.
Krieger, N., J. T. Chen, P. D. Waterman, M. J. Soobader, S. V. Subramanian, and R. Carson. 2002. Geocoding and monitoring of U.S. socioeconomic inequalities in mortality and cancer incidence: Does the choice of area-based measure and geographic level matter? The Public Health Disparities Geocoding Project. American Journal of Epidemiology 156(5):471-482.
Kukafka, R., J. S. Ancker, C. Chan, J. Chelico, S. Khan, S. Mortoti, K. Natarajan, K. Presley, and K. Stephens. 2007. Redesigning electronic health record systems to support public health. Journal of Biomedical Informatics 40(4):398-409.
LaPelle, N. R., R. Luckmann, E. H. Simpson, and E. R. Martin. 2006. Identifying strategies to improve access to credible and relevant information for public health professionals: A qualitative study. BMC Public Health 6:89-102.
Lazarus, R., M. Klompas, F. X. Campion, S. J. McNabb, X. Hou, J. Daniel, G. Haney, A. DeMaria, L. Lenert, and R. Platt. 2009. Electronic support for public health: Validated case finding and reporting for notifiable diseases using electronic medical data. Journal of the American Medical Informatics Association 16(1):18-24.
Leep, C., L. M. Beitsch, G. Gorenflo, J. Solomon, and R. G. Brooks. 2009. Quality improvement in local health departments: Progress, pitfalls, and potential. Journal of Public Health Management & Practice 15(6):494-502.
Lhachimi, S. K., W. J. Nusselder, H. C. Boshuizen, and J. P. Mackenbach. 2010. Standard tool for quantification in health impact assessment: A review. American Journal of Preventive Medicine 38(1):78-84.
Libbey, P., and B. Miyahara. 2011. Cross-Jurisdictional Relationships in Local Public Health: Preliminary Summary of an Environmental Scan. Princeton, NJ: RWJF.
Livingood, W. C., L. Razaila, E. Reuter, R. Filipowicz, R. C. Butterfield, K. Lukens-Bull, L. Edwards, C. Palacio, and D. L. Wood. 2010. Using multiple sources of data to assess the prevalence of diabetes at the subcounty level, Duval County, Florida, 2007. Preventing Chronic Disease 7(5):A108.
Livingood, W. C., M. Morris, B. Sorensen, K. Chapman, L. Rivera, P. Street, L. M. Beitsch, S. Coughlin, N. Winterbauer, C. Iusan, and D. Wood. 2011. Funding of Essential Services for Local Public Health. Paper read at PHSSR Keeneland Conference, April 12-14, Lexington, Kentucky. http://www.cdc.gov/pcd/issues/2010/sep/09_0197.htm (accessed August 12, 2011).
Love, D., and G. H. Shah. 2006. Reflections on organizational issues in developing, implementing, and maintaining state web-based data query systems. Journal of Public Health Management & Practice 12(2):184-188.
Love, D., B. Rudolph, and G. H. Shah. 2008. Lessons learned in using hospital discharge data for state and national public health surveillance: Implications for Centers for Disease Control and Prevention tracking program. Journal of Public Health Management & Practice 14(6):533-542.
Lovelace, K. 2000. External collaboration and performance: North Carolina local public health departments, 1996. Public Health Reports 115(4):350-357.
Luck, J., C. Chang, E. R. Brown, and J. Lumpkin. 2006. Using local health information to promote public health. Health Affairs 25(4):979-991.
Lutz, B., R. Molloy, and H. Shan. 2011. The housing crisis and state and local government tax revenue: Five channels. Regional Science and Urban Economics 41(4):306-319.
Madamala, K., K. Sellers, J. Pearsol, M. Dickey, and P. E. Jarris. 2010. State landscape in public health planning and quality improvement: Results of the ASTHO survey. Journal of Public Health Management & Practice 16(1):32-38.
Magruder, S. F., S. H. Lewis, A. Najmi, and E. Florio. 2004. Progress in understanding and using over-the-counter pharmaceuticals for syndromic surveillance. Morbidity and Mortality Weekly Report 53(Suppl):117-122.
Magruder, C., M. Burke, N. E. Hann, and J. A. Ludovic. 2005. Using information technology to improve the public health system. Journal of Public Health Management & Practice 11(2):123-130.
Maibach, E. W., L. C. Abroms, and M. Marosits. 2007. Communication and marketing as tools to cultivate the public’s health: A proposed “people and places” framework. BMC Public Health 7:88.
Malvitz, D. M., L. K. Barker, and K. R. Phipps. 2009. Development and status of the National Oral Health Surveillance System. Preventing Chronic Disease 6(2):A66. http://www.cdc.gov/pcd/issues/2009/apr/08_0108.htm (accessed August 12, 2011).
Mays, G. P., and F. D. Scutchfield. 2010. Improving public health system performance through multiorganizational partnerships. Preventing Chronic Disease 7(6):A116. http://www.cdc.gov/pcd/issues/2010/nov/10_0088 (accessed March 1, 2011).
Mays, G. P., and S. A. Smith. 2009. Geographic variation in public health spending: Correlates and consequences. Health Services Research 44(5 Pt 2):1796-1817.
Mays, G. P., S. A. Smith, R. C. Ingram, L. J. Racster, C. D. Lamberth, and E. S. Lovely. 2009. Public health delivery systems: Evidence, uncertainty, and emerging research needs. American Journal Preventive Medicine 36(3):256-265.
Mays, G. P., F. D. Scutchfield, M. W. Bhandari, and S. A. Smith. 2010. Understanding the organization of public health delivery systems: An empirical typology. Milbank Quarterly 88(1):81-111.
Merrill, J., M. Caldwell, M. L. Rockoff, K. Gebbie, K. M. Carley, and S. Bakken. 2008. Findings from an organizational network analysis to support local public health management. Journal of Urban Health 85(4):572-584.
Merrill, J. A., J. W. Keeling, R. V. Wilson, and T. V. Chen. 2011. Growth of a scientific community of practice public health services and systems research. American Journal of Preventive Medicine 41(1):100-104.
Meyer, J., and L. Weiselberg. 2009. County and City Health Departments: The Need for Sustainable Funding and the Potential Effect of Health Care Reform on Their Operations. Princeton, NJ: RWJF and NACCHO.
Michaelis, A. P. 2002. Priority-setting ethics in public health. Journal of Public Health Policy 23(4):399-412.
Miner, J. W., A. White, A. E. Lubenow, and S. Palmer. 2005. Geocoding and social marketing in Alabama’s cancer prevention programs. Preventing Chronic Disease 2(Spec no):A17. http://www.cdc.gov/pcd/issues/2005/nov/05_0073.htm (accessed August 12, 2011).
Miranda, M. L., J. M. Silva, M. A. Overstreet Galeano, J. P. Brown, D. S. Campbell, E. Coley, C. S. Cowan, D. Harvell, J. Lassiter, J. L. Parks, and W. Sandele. 2005. Building geographic information system capacity in local health departments: Lessons from a North Carolina project. American Journal of Public Health 95(12):2180-2185.
Mokdad, A. H. 2009. The Behavioral Risk Factors Surveillance System: Past, present, and future. Annual Review of Public Health 30:43-54.
Myers, S., and M. Stoto. 2006. Criteria for Assessing the Usefulness of Community Health Assessments: A Review of the Literature. Santa Monica, CA: RAND.
NACCHO (National Association of County and City Health Officials). 2005. Operational Definition of a Functional Local Health Department. Washington, DC: NACCHO.
NACCHO. 2009. 2008 National Profile of Local Health Departments. Washington, DC: NACCHO.
NACCHO. 2011. Local Health Department Job Losses and Program Cuts: State-Level Tables from the 2010 National Profile Study. Washington, DC: NACCHO.
National Prevention Council. 2011. National Prevention Strategy. Washington, DC: National Prevention Council.
NYSACHO (New York State Association of County Health Officials). 2001. Preserve Article Six State Aid and State Grant Funding for Local Public Health Activities. Albany: NYSACHO.
Overhage, J. M., S. Grannis, and C. J. McDonald. 2008. A comparison of the completeness and timeliness of automated electronic laboratory reporting and spontaneous reporting of notifiable conditions. American Journal of Public Health 98(2):344-350.
Parker, E., L. H. Margolis, E. Eng, and C. Henriquez-Roldan. 2003. Assessing the capacity of health departments to engage in community-based participatory public health. American Journal of Public Health 93(3):472-476.
Paul-Shaheen, P. A., B. A. Schillo, G. E. Beane, and E. F. Kleinau. 1997. The challenge of developing community profiles for use in community health assessment: Lessons from Michigan’s experience. Journal of Public Health Management & Practice 3(3):16-28.
PHAB (Public Health Accreditation Board). 2009. Proposed Local Standards and Measures: For PHAB Beta Test. Alexandria, VA: PHAB.
Pirani, S., and T. Reizes. 2005. The Turning Point Social Marketing National Excellence Collaborative: Integrating social marketing into routine public health practice. Journal of Public Health Management & Practice 11(2):131-138.
Plough, A. 2004. Understanding the financing and functions of metropolitan health departments: A key to improved public health response. Journal of Public Health Management & Practice 10(5):421-427.
Potter, M. A., B. E. Quill, G. S. Aglipay, E. Anderson, L. Rowitz, L. U. Smith, J. Telfair, and C. Whittaker. 2006. Demonstrating Excellence in Practice-Based Research for Public Health. Washington, DC: Association of Schools of Public Health.
Public Health Data Standards Consortium. 2007. Building a Roadmap for Health Information Systems Interoperability for Public Health: Public Health Uses of Electronic Health Record Data. Baltimore, MD: Public Health Data Standards Consortium.
Public Health Functions Steering Committee. 1995. Public Health in America. http://www.health.gov/phfunctions/public.htm (March 17, 2012).
Public Health Informatics Institute. 2003. Integration of Newborn Screening and Genetic Service Systems with Other Maternal & Child Health Systems: A Sourcebook for Planning and Development. Decatur, GA: Public Health Informatics Institute.
Rajotte, B. R., C. L. Ross, C. O. Ekechi, and V. N. Cadet. 2011. Health in All Policies: Addressing the legal and policy foundations of Health Impact Assessment. Journal of Law, Medicine & Ethics 39(Suppl 1):27-29.
Randolph, W., and K. Viswanath. 2004. Lessons learned from public health mass media campaigns: Marketing health in a crowded media world. Annual Review of Public Health 25:419-437.
Riley, W. J., J. W. Moran, L. C. Corso, L. M. Beitsch, R. Bialek, and A. Cofsky. 2010. Defining quality improvement in public health. Journal of Public Health Management & Practice 16(1):5-7.
Rockoff, M. L., D. J. Cunningham, M. T. Ascher, and J. Merrill. 2007. Information outreach to a local public health department: A case study in collaboration. Journal of the Medical Library Association 95(3):355-357.
Rooney, B. L., and J. E. Thompson. 2009. The value of a web-based interactive regional health scorecard in setting public health priorities. Wisconsin Medical Journal 108(8):403-406.
Roussos, S. T., and S. B. Fawcett. 2000. A review of collaborative partnerships as a strategy for improving community health. Annual Review of Public Health 21:369-402.
Rudolph, L., A. Sisson, J. Caplan, L. Dillon, K. Ben-Moshe, M. Mohammadi, S. Sattelmeyer, and M. Walker. 2010. Health in All Policies Task Force: Report to the Strategic Growth Council. Sacramento: California Department of Public Health and University of California, San Francisco.
Running, A., K. Martin, and L. W. Tolle. 2007. An innovative model for conducting a participatory community health assessment. Journal of Community Health Nursing 24(4):203-213.
Santerre, R. E. 2009. Jurisdiction size and local public health spending. Health Services Research 44(6):2148-2166.
Scutchfield, F. D., E. A. Knight, A. V. Kelly, M. W. Bhandari, and I. P. Vasilescu. 2004. Local public health agency capacity and its relationship to public health system performance. Journal of Public Health Management & Practice 10(3):204-215.
Scutchfield, F. D., J. S. Marks, D. J. Perez, and G. P. Mays. 2007. Public health services and systems research. American Journal of Preventive Medicine 33(2):169-171.
Scutchfield, F. D., M. W. Bhandari, N. A. Lawhorn, C. D. Lamberth, and R. C. Ingram. 2009. Public health performance. American Journal of Preventive Medicine 36(3):266-272.
Sellers, K. 2011. State Public Health Finance: Results of the ASTHO 2010 Profile Survey. Washington, DC: ASTHO.
Slonim, A. B., C. Callaghan, L. Daily, B. A. Leonard, F. C. Wheeler, C. W. Gollmar, and W. F. Young. 2007. Recommendations for integration of chronic disease programs: Are your programs linked? Preventing Chronic Disease 4(2):A34. http://www.cdc.gov/pcd/issues/2007/apr/06_0163.htm (accessed August, 12, 2011).
Spice, C., and K. Snyder. 2009. Reviewing self-reported impacts of community health assessment in local health jurisdictions. Journal of Public Health Management & Practice 15(1):18-23.
St. Luke’s Health Initiative. 2002. Building a Public Health Movement in Arizona. Phoenix, AZ: SLHI.
Staes, C. J., W. Xu, S. D. LeFevre, R. C. Price, S. P. Narus, A. Gundlapalli, R. Rolfs, B. Nangle, M. Samore, and J. C. Facelli. 2009. A case for using grid architecture for state public health informatics: The Utah perspective. BMC Medical Informatics and Decision Making 9:32-41.
Ståhl, T., M. Wismar, E. Ollila, E. Lahtinen, and K. Leppo. 2006. Health in All Policies: Prospects and Potentials. Brussels, Belgium: European Observatory on Health Systems and Policies.
Stoto, M. A., S. G. Straus, C. Bohn, and P. Irani. 2009. A web-based tool for assessing and improving the usefulness of community health assessments. Journal of Public Health Management & Practice 15(1):10-17.
Suarez, V., C. Lesneski, and D. Denison. 2011. Making the case for using financial indicators in local public health agencies. American Journal of Public Health 101(3):419-425.
TFAH (Trust for America’s Health). 2011. Investing in America’s Health: A State-by-State Look at Public Health Funding and Key Facts. Washington, DC: TFAH.
Turner, A. M., J. Ramey, and S. Lee. 2008. Connecting public health IT systems with enacted work: Report of an ethnographic study. AMIA Annual Symposium Proceedings, 2008:737-741.
Twose, C., P. Swartz, E. Bunker, N. K. Roderer, and K. B. Oliver. 2008. Public health practitioners’ information access and use patterns in the Maryland (USA) public health departments of Anne Arundel and Wicomico Counties. Health Information & Libraries Journal 25(1):13-22.
Washington State Department of Health. 2008. 2008 Public Health Improvement Plan: Building Strength and Performance. Olympia: Washington State Department of Health.
Wernham, A. 2011. Health impact assessments are needed in decision making about environmental and land-use policy. Health Affairs 30(5):947-956.
Whittingham, J., R. A. Ruiter, F. Zimbile, and G. Kok. 2008. Experimental pretesting of public health campaigns: A case study. Journal of Health Communication 13(3):216-229.
WHO (World Health Organization). 2010. Adelaide Statement on Health in All Policies. Geneva, Switzerland: WHO.
Wholey, D. R., W. Gregg, and I. Moscovice. 2009. Public health systems: A social networks perspective. Health Services Research 44(5 Pt 2):1842-1862.
Woolf, S. H., M. M. Dekker, F. R. Byrne, and W. D. Miller. 2011. Citizen-centered health promotion: Building collaborations to facilitate healthy living. American Journal of Preventive Medicine 40(1 Suppl 1):S38-S47.
Yasnoff, W. A., M. J. Overhage, B. L. Humphreys, M. LaVenture, K. W. Goodman, L. Gatewood, D. A. Ross, J. Reid, E. W. Hammond, D. Dwyer, S. M. Huff, I. Gotham, R. Kukafka, J. W. Loonsk, and M. M. Wagner. 2001. A national agenda for public health informatics. Journal of Public Health Management and Practice 7(6):1-21.
Zahner, S. J. 2005. Local public health system partnerships. Public Health Reports 120(1):76-83.
Zhang, Z., L. Zhang, A. Penman, and W. May. 2011. Using small-area estimation method to calculate county-level prevalence of obesity in Mississippi, 2007-2009. Preventing Chronic Disease 8(4):A85.
ADDENDUM: INTERVIEW RESPONDENTS
|
Name and Title |
Organization/Prior Experience |
|
Susan Allan, Director |
Northwest Center for Public Health Practice, former Public Health Director, State of Oregon; and |
|
Health Director, Arlington County, Virginia |
|
|
Kaye Bender, President |
Public Health Accreditation Board |
|
Bobbie Berkowitz, Dean |
Columbia School of Nursing, former Deputy Director, WA State Department of Health; and Chief of Public Health Nursing, Seattle & King County Public Health |
|
Gus Birkhead, Deputy Commissioner |
Office of Public Health, NY State Department of Health |
|
Leah Devlin |
Former Director, NC Division of Public Health |
|
Paul Halverson, Director |
Arkansas Department of Health |
|
Peggy Honoré, Director |
Public Health System, Finance, and Quality Program, OASH, HHS |
|
Paul Kuehnert, Director |
Kane County (IL) Department of Health |
|
Pat Libbey |
University of WA School of Public Health, former NACCHO Director |
|
Pat McConnon |
Council of State and Territorial Epidemiologists |
|
Michael Meit |
Walsh Center for Rural Analysis/NORC |
|
Tom Milne |
Milne and Associates, former Director of NACCHO |
|
Bruce Miyahara |
Miyahara and Associates, former Director WA State Department of Health; and Director Seattle & King County Public Health |
|
Herminia Palacios, Executive Director |
Harris County Public Health & Environmental Services, Texas |
|
Bobby Pestronk, Executive Director |
NACCHO, former director Genesee County Health Department (Flint, MI) |
|
Phred Pilkington, Director |
Cabarrus Health Alliance (NC) |
|
Doug Scutchfield |
University of Kentucky School of Public Health |
|
Kathy Vincent |
Former Staff Assistant to the State Health Officer, Alabama Department of Public Health |




















































