Informing Investment in Health
Public health leaders have sufficient information to take action in important sectors of population health. However, the public health system at all levels of government requires better information about the level of resources expended and how they are being used, what system characteristics are most closely linked with achieving desired outcomes, and what methods are most effective and efficient in improving population health. In this chapter, the committee first discusses the administrative changes needed to support the uniform collection and reporting of public health financial information (revenues and expenditures). Better information will help government officials to make evidence-based management decisions to generate and allocate resources for public health activities that maximize population health gains and minimize the costs of treating preventable diseases and injuries. And improved information will allow leaders of public health agencies to make better management decisions about organizing, staffing, and implementing public health activities that maximize the efficiency, reach, and effects of their operations. Research is also needed to generate objective information about the costs and outcomes of public health activities—information that would facilitate assessments of the comparative effectiveness of public health and social interventions and medical approaches, and allow decision makers in government and the private sector to identify better ways of allocating limited resources across the spectrum of health-related investment (Teutsch and Fielding, 2011b).
A NEED FOR FINANCIAL ANALYSIS AND RESEARCH
As mentioned in Chapter 1 and discussed in more detail in Chapter 4, the information available about public health funding has considerable limitations. Many governmental public health programs were established in response to specific health threats or as results of new interventions, such as the creation of a specific vaccine or the implementation of new smoking interventions to reduce cancer deaths. The collection of public health program activities has become what a governmental public health department does. But in many locales, public health departments have not been allowed the “luxury” of organizing activities into a coherent whole in which essential capabilities exist to support all programs or in which funding from one program is leveraged in a systematic manner to benefit other programs. The combination of that historical circumstance in funding, a lack of national standards in recording and reporting funding and expenditure data, and variations in the definitions of public health challenges any attempt to obtain accurate expenditure estimates.
Because financial information on public health is difficult to obtain at all levels of government, there is considerable uncertainty about current investment in public health activities in the United States and about the sources of revenue for this investment and the relative contributions of federal, state, local, and private bodies. It is also unclear what those sources purchase in terms of the spectrum of public health activities and infrastructure, how resources are allocated among different geographic areas and population groups, and, perhaps most important, how investment compares with the outcomes of public health activities. Poor financial information systems can breed poor performance because a lack of data and measurement makes it more difficult to evaluate, manage, and improve (Kaplan and Porter, 2011). Without better financial information, policymakers cannot assess the value realized from public health spending, nor can they clearly identify the health and economic consequences of underinvestment. Public health managers are unable to link cost data to their organizational structures, staffing patterns, and service delivery models. This limits their ability to enhance the productivity and efficiency of their operations. Because of a lack of adequate financial information, effective and efficient public health departments go unrewarded, and inefficient agencies face few incentives to improve (Honoré and Costich, 2009; Honoré et al., 2007).
In the United States, the Centers for Medicare and Medicaid Services Office of the Actuary develops the annual National Health Expenditure Accounts (NHEA) on the basis of data from federal and state governments and international standards. Some limitations of the NHEA, including definitional and methodological issues (Sensenig, 2011), are discussed in Chapter 4. Ballinger (2007) and Sensenig (2007, 2011) have shown that NHEA in Canada and the United States, respectively, do not usefully reflect the level of spending on public health, because there are no uniform,
universally accepted definitions of public health activity across levels of government (or internationally). The Association of State and Territorial Health Officials (ASTHO) and the National Association of County and City Health Officials (NACCHO) attempt to bridge that gap by conducting periodic surveys and other kinds of data collection to measure and understand public health department revenues and expenditures at the state and local levels, respectively (see, for example, ASTHO and NACCHO 2011 profiles of state and local public health departments). The value of the data on state and local governmental public health revenues is greatly limited by the lack of a uniform chart of accounts used among health departments, which makes it impossible for health department personnel around the United States to report data on expenditures consistently (Gans et al., 2007). In addition, the variation in scope of work among public health agencies and the fragmented and idiosyncratic1 nature of public health funding make it infeasible for the national associations to collect granular data on program-specific revenues and expenditures. Although knowing the level of funding by funding sources is a key to understanding the outcomes of investments in governmental public health programs, NACCHO found that “collecting these data nationally seems unrealistic given the difficulty of some [local health departments] in providing accurate data even on total revenues and expenditures” (NACCHO, 2011, p. 91).
Charts of Accounts
Honoré and colleagues observed that “[p]ublic health lacks an operational framework for basic levels of financial analysis and research” (2007, p. 121). The key element of such a framework is a standardized chart of accounts to enable public health to gather uniform data and conduct comparisons between jurisdictions. Charts of accounts are accounting records that organizations—including nonprofit organizations, health care entities, and universities—use to track expenditures and revenue (Honoré et al., 2007; see also University of Minnesota, 2010; Urban Institute National Center for Charitable Statistics, 2009). Charts of accounts generally match the financial structure of an organization and use categories or classifications for each type of expenditure. The information on a chart of accounts gives an organization an overview of financial activities and can be used for such purposes as fund accounting, reporting or demonstrating accountability to funders and stakeholders, development of financial reports, management, comparative analysis, and benchmarking. The lack of a uniform chart of accounts is a crucial gap for public health services research, in which a clear
______________
1One reason for this is that there has never been a consistent federal funding stream for public health infrastructure as there has been for hospital infrastructure (the Hill–Burton Act of 1946 aimed to strengthen the nation’s hospitals and to reach a specific ratio of hospital beds per population) and for the National Institutes of Health biomedical research enterprise.
understanding of the effectiveness and efficiency of investment in programs, personnel, and interventions is a necessity. The adoption of a uniform chart of accounts would enable public health departments at all levels to better ensure accountability for resources and outcomes. Accountability would be facilitated through uniform reporting of revenue and expenditures, and ultimately through establishing how financial inputs and outputs are associated with long-term outcomes.
The financial accounting systems used by public health agencies are highly idiosyncratic, varying from one jurisdiction to another, and they are generally fashioned on a local or state government’s template rather than being customized to meet the needs of public health departments.2 They are designed for budget management and fund accounting rather than for overall financial and program management, that is, understanding the linkages between resources, processes, outputs, and outcomes (see Figure 3-1, a logic model first introduced in the committee’s report For the Public’s Health: The Role of Measurement in Action and Accountability and out-lining the steps to population health improvement from inputs to outcomes3). Thus, there
______________
2Several states have undertaken efforts to develop charts of accounts. Florida has a comprehensive public health dataset and has begun to develop a chart of accounts (Honoré, 2011). It has begun to tackle the difficult issues of definitions (What is core public health? What are clinical care services “alone”?) and has developed a financial information reporting system. The system can be used to compare staffing, workload, population, budget, and full-time employees and can provide revenues and expenditures by program. It can measure revenue per capita, expenditure per capita, and the ratio of revenue to expenditures. This program is still in its testing phase but aims to be used at the state and local levels (Dillion, 2010). According to a state health official, objectives include enabling comparisons among jurisdictions and informing “sound business decisions relative to public health.” Georgia has also begun to develop local charts of accounts for its local governments that include some aspects of public health (categories include maternal and child health services, adult health services, health centers, and general clinics). However, each jurisdiction can adapt the template to its needs, and it is not a comprehensive uniform chart of accounts for public health. Other states have begun comprehensive cost analyses as part of a broader process of thinking about revenues, expenditures, and outcomes (Honoré, 2011).
3In its first report on population health measurement, “the committee adapted a simple structure–process–outcome logic model (Donabedian, 1988) to illustrate both the sequence of steps between inputs and outputs in population health and the multiple categories for measurement” (IOM, 2011, pp. 50-51). The figure was originally provided to help in thinking about the types of data and indicators available and needed at each step in the process. The figure ranges from resources and capabilities to intermediate outcomes and indicators and distal outcomes. The “determinants of health” box in the figure “is intended to refer largely to determinants that can be modified by the actions of various agencies and organizations in the health system” (IOM, 2011, p. 51). “Arrows between the determinants of health and many of the boxes represent the feedback loops between determinants and system inputs or outputs. For example, broader societal values and priorities influence the availability of resources for population health activities. Population health interventions, such as policy changes, are often designed to influence particular determinants of health. After evaluation and research to assess the effectiveness of an intervention on a given determinant, the intervention may be modified or replaced” (IOM, 2011, p. 51).
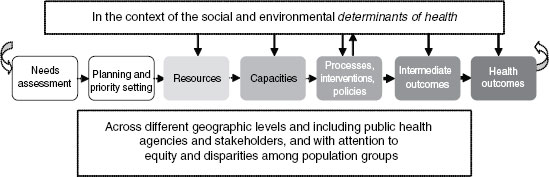
FIGURE 3-1 Logic model: from inputs to outputs and outcomes.
SOURCE: IOM, 2011.
is a dearth of comprehensive and consistent financial data on the nation’s health departments. A standard chart of accounts would ensure that expenditures were recorded consistently among jurisdictions and would support management, permit comparisons between jurisdictions, and allow more accurate estimates of public health spending by states, regions, and the nation. A uniform chart of accounts would also provide a reliable basis for studying how variability in use of resources leads to differences in processes and interventions and how they lead to differences in outputs. It would help local health departments to make more informed decisions on allocating their resources. The minimum package of public health services introduced in Chapter 2 to ensure a standard level of capacity in all jurisdictions could also serve as a framework for developing a chart of accounts, that is, preparing sets of accounts for each domain of foundational capabilities and each basic program. Steps toward creating a unified chart of accounts would include
• Studying the accounting structures now in place.
• Building a model chart of accounts.
• Comparing the model with existing accounting practices used by local and state agencies.
• Examining how well accounting structures accommodate funding flows.
Once it were developed and endorsed, the Department of Health and Human Services (HHS) could require use of a chart of accounts for reporting as a condition of receipt of federal funds, as is the case with the Medicare Cost Report that all health care providers must submit.4
______________
4See, for example, Hospital Cost Report (CMS, 2012).
The characteristics of a useful chart of accounts include
• A mutually exclusive set of expense accounts to ensure that program expenses are not double-counted.
• A uniform record that captures all work activity that creates expenses.
• Sufficient detail to link resources to specific processes that affect intermediate and final outcomes.
• The management information needed to enable improvement of performance of public health systems on a local, statewide, and national basis.
A chart of accounts also needs to support management accounting of a specified set of items, beginning with the minimum package of services consisting of foundational capability domains and required programs; fund accounting; and financial reporting. And a process will be needed to ensure that the public health chart of accounts is not static but evolves to suit the financial reporting and management needs of the field.
Uniform charts of accounts have been used successfully in other sectors, including medical care and education. Examples in the medical care sector include those used by the Healthcare Financial Management Association (HFMA) and charts of accounts for hospitals (Nowicki and Berger, 2006). In the education sector, the National Center for Education Statistics Common Core of Data surveys administered to school districts and schools leads to the publication of an annual report on school revenues and expenditures. Financial reporting standards and frameworks also guide colleges and universities (Honoré et al., 2007).
Charts of accounts are linked with what Honoré and colleagues describe as “exemplary practices” used in the clinical care and educational sectors (2007). These practices include (1) uniform classifications for expenses and revenues, (2) infrastructures for electronic data reporting, (3) standardized system-wide financial analysis practices, (4) extensive reporting of financial results, and (5) professional associations for the accounting workforce. Implementation of these practices in some fields has been driven by private sector market forces that demand accountability, whereas in other fields it has evolved as a result of statutory mandates and stakeholder demands for information (Honoré et al., 2007, p. 125).
Over the last several years, NACCHO and the University of Southern Mississippi have partnered to develop a Web-based Public Health Uniform Data System for local health departments (a project funded by the Robert Wood Johnson Foundation). The system, projected to be available in 2012, is expected to have the capacity to collect data and provide immediate feedback to health departments on financial and operational performance,
benchmarking, program sustainability, and other measures. Its purpose is to make available a uniform set of account definitions to promote the collection and analysis of valid, reliable, and uniform public health data. It will be the closest thing yet to a uniform chart of public health accounts.5 The committee views the HHS and NACCHO effort as a step in the right direction. However, the committee notes that the type of classification described in the draft template appears to be based on the array of expense categories that are typically seen in health departments and does not appear to create mutually exclusive expense accounts as typical charts of accounts do. Additional work is needed to develop charts of accounts that fully meet the needs of public health departments.
Adopting a uniform chart of accounts in all public health departments will not be easy or rapid. An ideal chart of accounts would assign expenditure codes to a hierarchic cascade of activities that begins with the broad functions and the minimum package of public health services. Each broad category would divide into more granular categories, which would eventually lead to codes that describe discrete tasks associated with the broad category.
Several barriers potentially stand in the way of adoption of a uniform chart of accounts. For example, the committee acknowledges that it will be difficult to assign a uniform accounting code structure that all health departments would be required to adopt. However, if agreement can be reached on the highest levels of accounting aggregation, health departments could reshape their existing charts of accounts to align with the highest levels of definitions. In time, health departments could progressively refine their subcodes to comport with the national model chart of accounts. In the interval before an agency reaches complete compliance with the model chart of accounts, it could submit data to a nationally operated information utility that would translate local codes into nationally compliant codes. For example, a purpose of health information exchange organizations is to take health care encounter data encoded in a hospital or provider office idiosyncratically and translate them to nationally standardized codes that can be interpreted and used by other health care organizations. A similar translation process could serve as a transitional step for public health accounting data and lead to the development of a structure to which each public health department would “map,” for example, its way of coding. The cost of adoption of a chart of accounts is another barrier. It includes investment needed to familiarize health department personnel with new systems and the cost of implementing a new infrastructure, which could be substantial.
As an example of how sets of accounts are developed, all immunization-
______________
5Personal Communication, Peggy Honoré, December 1, 2011. For more information, see http://publichealthfinance.org/research-and-analysis/2292.
related activities would be grouped in a set of immunization accounts. The generic “immunization” can be separated into codes for “routine vaccine clinic administration,” “routine vaccine supply management,” “emergency mass immunization clinic,” and so on. During an influenza pandemic or other emergency mass immunization event, the codes for those activities would be linked to the “emergency preparedness” set of accounts. Staff conducting immunization activities would recognize the work as vaccination clinic work, and administrators may also need to define it as a component of a specific emergency response. A thorough chart of accounts would categorize program expenses to show actual expenditures involved in doing the work and offer the flexibility of associating expenses to lines of revenue (such as insurance or Medicaid reimbursement for vaccinations administered or funding from Section 317 of the Public Health Services Act, which provides support for vaccines and vaccination infrastructure). Once standard definitions and a uniform chart of accounts have been adopted, it will be possible to capture reliable specific data on public health spending patterns in existing federal surveys, such as the U.S. Census Bureau’s periodic Census of Governments, which is the primary source of data used in NHEA. That survey currently asks state and local governments to report their public health expenditures in one large lump-sum category that is poorly defined. The Census Bureau could ask governments for much more detailed reporting on public health expenditures if it were assured that governments would provide this information in a consistent format. Table 3-1 shows a sample portion of a hypothetical and highly simplified chart of accounts.
Recommendation 5: The committee recommends that a technical expert panel be established through collaboration among government agencies and organizations6 that have pertinent expertise to develop a model chart of accounts for use by public health agencies at all levels to enable better tracking of funding related to programmatic outputs and outcomes across agencies.
The adoption of a uniform chart of accounts could be made a Public Health Accreditation Board (PHAB) requirement in addition to being made a prerequisite for federal and state funding. The process of developing a chart of accounts needs to take place with consideration of the broader management needs of public health departments and the more difficult work of measuring and accounting for nonclinical services.
______________
6Agencies and organizations would include HHS, public health departments, ASTHO, NACCHO, PHAB, and the National Association of State Budget Officers.
TABLE 3-1 Excerpt of a Hypothetical, Highly Simplified Public Health Chart of Accounts
| Account Category (Programs) | Account Code | Account Title | Definition/Linked to |
| Immunization | All funds spent on immunizations | ||
| 3000 | Routine vaccine clinic administration | ||
| 3010 | Routine vaccine supply management | ||
| 3020 | Emergency mass immunization clinic | Linked to preparedness category | |
| 3030 | Communication on immunization | ||
| Environmental Health | |||
| 6000 | Healthy Homes and Lead Hazard Prevention Program | Linked to prevention programs category | |
| 6000.1 | Public service announcements | ||
| 6000.2 | Staff training | ||
| 6010 | Compliance and enforcement, Air | ||
| 6010.1 | Outreach and education | ||
| 6010.2 | Permits | ||
| 6020 | Compliance and enforcement, Water | ||
| Chronic Disease | |||
| 9000 | Asthma | Linked to environmental health | |
| Obesity Prevention and Control | Linked to chronic disease category | ||
| 9010.1 | Data collection, obesity (all ages) | Linked to data collection category | |
| 9010.2 | Program evaluation, obesity | Linked to research and data collection categories | |
| 9010.3 | Mass media campaigns and social marketing | Linked to communication | |
| 9010.4 | Nutrition education and counseling | Linked to general education and counseling | |
| Account Category (Programs) | Account Code | Account Title | Definition/Linked to |
| 9010.5 | Physical education and counseling | Linked to general education and counseling | |
| 9010.6 | Restaurant menu labeling inspection and enforcement | ||
| 9010.7 | Planning | ||
| 9010.8 | Policy development | ||
| Asthma | |||
| 9020.1 | Data collection, asthma (all ages) | ||
| 9020.2 | Program evaluation, asthma | ||
| Account Category (Administrative) | |||
| Workforce | 1000 | Total salaries | |
| 1010 | Total liability days for unused vacation | ||
| 1020 | Total fringe benefits | ||
| 1030 | Professional development | ||
| Infrastructure | |||
| 2000 | Utilities | ||
| 2010 | Computers | ||
| 2010.1 | Information technology support | ||
DATA AND INFORMATION TO SUPPORT PRACTICE
This section discusses the research and evaluation needed to inform and support evidence-based and best practices in the funding of public health. Research, for example prevention-effectiveness and comparative-effectiveness research, and evaluation are relevant to funding because they inform the continuum of public health practice, including decisions about what population-based interventions are funded, and the field’s knowledge about what works best in public health financing, administration, and organization (PHSSR, 2012). The committee outlines below the thin evidence base that supports many areas of public health practice, the funding imbalances and the siloed nature of health research and development, and some specific needs.
The Evidence Base
The committee has noted before that the evidence base on the effectiveness of health interventions is growing, but it remains particularly sparse with respect to population-based interventions. The work of the Centers for Disease Control and Prevention Task Force on Community Preventive Services has led the way in establishing the effectiveness of interventions, but there are areas where much remains to be done to show what is effective.7 Health systems research, including public health services and systems research, is an expanding field (AcademyHealth, 2012; RWJF, 2012). However, efforts to improve population health are hampered by the many uncertainties and evidence gaps concerning how to promote health and prevent disease and disability on a populationwide basis.
The nation’s local, state, and federal public health agencies—with their peers and partners in the private and public sectors—constitute a vast but diffuse delivery system charged, to greater or smaller degrees, with implementing public health and prevention strategies (Teutsch and Fielding, 2011a). But evidence on the most effective and efficient ways of organizing, financing, and deploying the strategies through the delivery system is inadequate (Coffman, 2003/2004; IOM, 2011). Public health leaders have few research-tested guidelines, protocols, and decision supports to inform their choices about funding, staffing, and managing public health activities. Similarly, policy leaders have relatively little empirical guidance on the most effective ways to exercise taxing, spending, and regulatory authorities for the public’s health. The dearth of evidence promotes wide variation in public health practices among communities, creating missed opportunities for improving population health, waste and inefficiencies in resource use, and inequities in health protection (Culyer and Lomas, 2006). The scientific fields of prevention research and, more recently, public health services and systems research (PHSSR) have mobilized to address those information needs and build the evidence needed for improved decisionmaking in public health practice. Thacker and colleagues (2005, p. 227) found that “[i]n addition to the relatively young state of the field, there is little funding for population-based effectiveness research in public health compared with basic and patient-oriented clinical research. This situation might reflect the analytic challenges of this kind of research or the absence of societal commitment to invest resources in such research.” Expanded investments in the applied fields of research are needed to produce information with which policy officials and public health professionals can drive improvements in
______________
7The Cochrane Collaboration, the Campbell Collaboration, and others are building the evidence base of systematic reviews of population-based interventions (Sweet and Moynihan, 2007).
the nation’s public health system (see Recommendation 6 toward the end of this chapter).
R&D Funding: Imbalance and Silos
In Chapter 1, the committee discussed the imbalance in health system funding, which is directed at clinical care and is inadequate to support an effective public health infrastructure. Similarly, congressional research appropriations favor biomedical science. Funding for health-related research and development is skewed toward discovery of therapeutic interventions and elucidating basic pathophysiologic mechanisms as opposed to prevention strategies and especially population-based prevention (Cook-Deegen, 2011; Crow, 2011; Miller et al., 2008; Moses et al., 2005; Scrimshaw et al., 2001). Similarly, little is spent on delivery research. The Coalition for Health Services Research estimated that just 0.19 percent of total federal spending on health care services is spent on health services research (CHSR, 2009) and Moses and colleagues (2005) estimated that a mere 0.1 percent of total U.S. health expenditures goes to health services research. The meager funding available for public health research is structured similarly, although there has recently been increased attention from foundation and government funders. Substantial research investments are needed to help public health agencies to be more operationally efficient and programmatically effective.
The heavy orientation toward therapeutics that forms the basic structure of U.S. health research and development is only the broadest example of the boundaries that separate research pertinent to clinical care and therapeutics from research on population health. The nation’s health research enterprise is further segmented into silos that focus on specific disease processes and biomedical pathways, thereby reducing opportunities for research that examines cross-cutting social and environmental pathways and for research on prevention opportunities outside clinical care settings. One way to begin to break those silos would be to include population-based research in comparative effectiveness research (most of which is clinically oriented). The Affordable Care Act, 2010 (ACA) provisions calling for the establishment of the Patient-Centered Outcomes Research Institute (PCORI) excludes population-based preventive interventions from the institute’s purview.8 PHSSR researchers and others (e.g., Teutsch and Fielding, 2011a,b)
______________
8From PL 111-148, 124 STAT. 727 ‘‘(2) COMPARATIVE CLINICAL EFFECTIVENESS RESEARCH;
RESEARCH.
‘‘(A) IN GENERAL.—The terms ‘comparative clinical effectiveness research’ and ‘research’ mean research evaluating and comparing health outcomes and the clinical effectiveness, risks, and benefits of 2 or more medical treatments, services, and items described in subparagraph (B).
‘‘(B) MEDICAL TREATMENTS, SERVICES, AND ITEMS DESCRIBED.—The medical
have called for reconsideration. If, as the committee has observed in Chapter 1, public health is recognized as being on a continuum with clinical care, it follows that the preventive interventions being evaluated by PCORI ought to include the most broad-based types of interventions, that is, ones that aim to improve the health of entire populations. The committee concurs with the view that PCORI’s comparative effectiveness analyses ought to include population-based interventions. However, even if PCORI’s mission9 is not interpreted more broadly, the public health research enterprise must be extended to support comparing the effectiveness of population-based interventions. A cost-effectiveness literature that has compared clinical with population-based interventions has suggested greater efficiencies associated with such population-based interventions from water fluoridation, antismoking policies, and fortification of the food supply to prevent neural tube defects than are associated with clinical approaches to preventing related conditions (Gaziano et al., 2007; Grosse et al., 2007; Halpin et al., 2010; Kelly et al., 1996; Weintraub et al., 2011). The committee’s first report acknowledged the impact of social and environmental determinants of health—upstream determinants of health (such as urban planning and early childhood development and education)—on population-health outcomes (Garcia and White, 2006; Garcia et al., 2009; IOM, 2011; Karoly et al., 2005), and efforts of communities and foundations have begun to improve population health (e.g., Building a Healthier America funded by RWJF). Developing an understanding of where resources are best placed, whether clinical or population-based, is necessary for gaining value from investment in the health system.
Unmet Needs
Various public health research and development efforts are needed. The committee highlights here a subject that was first introduced by the committee in their report on data and measurement For the Public’s Health: The Role of Measurement in Action and Accountability (see Box 3-1 for pertinent recommendations from the report). In that report, the committee identified substantial deficits in the nation’s ability to collect and analyze
![]()
treatments, services, and items described in this subparagraph are health care interventions, protocols for treatment, care management, and delivery, procedures, medical devices, diagnostic tools, pharmaceuticals (including drugs and biologicals), integrative health practices, and any other strategies or items being used in the treatment, management, and diagnosis of, or prevention of illness or injury in, individuals.”
9In January 2012, PCORI released its draft research priorities for research that includes this: “Assessment of Prevention, Diagnosis, and Treatment Options. Research should focus on 1) clinical options with emphasis on patient preferences and decision-making, 2) biological, clinical, social, economic, and geographic factors that may affect patient outcomes” that are relevant to public health (PCORI, 2012, p. 4).
BOX 3-1
Research-Related Recommendations
from For the Public’s Health: The Role of
Measurement in Action and Accountability
Recommendation 1
The committee recommends that
a. The Secretary of Health and Human Services transform the mission of the National Center for Health Statistics to provide leadership to a renewed population health information system through enhanced coordination, new capacities, and better integration of the determinants of health.
b. That the National Prevention, Health Promotion, and Public Health Council include in its annual report to Congress on its national prevention and health-promotion strategy an update on the progress of the National Center for Health Statistics transformation.
Recommendation 2
The committee recommends that the Department of Health and Human Services support and implement the following to integrate, align, and standardize health data and health-outcome measurement at all geographic levels:
a. A core, standardized set of indicators that can be used to assess the health of communities.
b. A core, standardized set of health-outcome indicators for national, state, and local use.a
c. A summary measure of population health that can be used to estimate and track Health-Adjusted Life Expectancy for the United States.
Recommendation 6
The committee recommends that the Department of Health and Human Services coordinate the development and evaluation and advance the use of predictive and system-based simulation models to understand the health consequences of underlying determinants of health. HHS should also use modeling to assess intended and unintended outcomes associated with policy, funding, investment, and resource options.
data about the public’s health at national, state, and community levels. Those deficits constrain the volume, quality, and pace of research that can be conducted to discover effective prevention strategies and delivery system approaches. Producing the evidence needed for informed public health decision making will require investment in targeted strategies to improve
Recommendation 7
The committee recommends that the Department of Health and Human Services work with relevant federal, state, and local public-sector and private-sector partners and stakeholders to
1. Facilitate the development of a performance-measurement system that promotes accountability among governmental and private-sector organizations that have responsibilities for protecting and improving population health at local, state, and national levels. The system should include measures of the inputs contributed by those organizations (e.g., capabilities, resources, activities, and programs) and should allow tracking of impact on intermediate and population health outcomes.
2. Support the implementation of the performance measurement system by
a. Educating and securing the acceptance of the system by policymakers and partners.
b. Establishing data-collection mechanisms needed to construct accountability measures at appropriate intervals at local, state, and national levels.
c. Encouraging early adoption of the system by key government and nongovernmental public health organizations and use of the system for performance reporting, quality improvement, planning, and policy development.
d. Assessing and developing the necessary health-system capacity (e.g., personnel, training, technical resources, and organizational structures) for broader adoption of the framework, including specific strategies for steps to address nonperformance by accountable agencies and organizations.
aThe conception of a community may differ from one context to another, and it could range from a neighborhood to a county. Local decisionmakers may include mayors, boards of supervisors, and public health officials. The notion of “local” may also vary (from census tract or ZIP code to city or county), depending on planning or research objectives and many other factors (IOM, 2011). NOTE: Recommendations 3, 4, and 5 of the report are not related to research and are not included here. SOURCE: IOM, 2011.
NOTE: Recommendations 3, 4, and 5 of the report are not related to research and are not included here.
SOURCE: IOM, 2011.
the nation’s public health data, measurement, and analytic capacities, as articulated in the committee’s report (IOM, 2011). The committee recommended strengthening the National Center for Health Statistics (NCHS) as part of a broader effort to transform the nation’s population health information system. NCHS, which is a core component of the U.S. popu-
lation health information system, conducts some of the nation’s primary surveys on population health, including the Health Interview Survey and the National Health and Nutrition Examination Survey. However, the agency’s role has been seriously limited by funding constraints, and the committee believes that NCHS can play a broader leadership role in the population health information system by expanding its analytic capabilities, its research activities, its ability to collaborate with those who use its data, and its ability to help to modernize and integrate the system. Doing so would increase the usefulness of NCHS data and facilitate and guide the “translation” of data into information and knowledge that decisionmakers and communities can use.
Public health organizations receive inadequate research support to address the leading causes of premature death and disease in American communities. Considerable uncertainty remains in the policy and practice domains about the array of public health services that every community should offer, the level of investment required to provide those services, and the health and economic benefits that can be expected from the investment over various timeframes—including the potential for downstream offsets in medical care spending. The nation’s current public health knowledge and capabilities are inadequate to address some of the most pressing threats to population health, such as those related to obesity and social determinants of health. Where evidence-based strategies are lacking, the development of new knowledge and efficacious public health strategies is imperative. It takes a strong research infrastructure to produce the evidence needed for optimizing the nation’s portfolio of investment in public health and the nation’s health expenditures on health in general, but, as noted by an earlier Institute of Medicine (IOM) committee (IOM, 2003), there is still little infrastructure and support for this type of research.
The Guide to Community Preventive Services provides evidence-based recommendations and identifies important gaps in knowledge regarding the effectiveness of interventions and thus contributes to a research agenda (TFCPS et al., 2005). On the service delivery side, a research agenda for public health services research has recently been developed (PHSSR, 2011). More and better evidence is needed to inform policy and managerial decisions about resource allocation in public health and to ensure accountability for current and future investment in the public health system.
Types of Research Needed
The discovery of new and better prevention strategies and delivery system approaches requires a continuum of research activities, including
• Descriptive research to understand the distribution of population health measures at national, state, and community levels; to detect variation in health measures among communities; and to detect changes in health measures.
• Epidemiologic and etiologic research to identify causal mechanisms and pathways that determine population health and explain why health varies among communities and why it changes.
• Efficacy trials and effectiveness studies to identify the prevention strategies (programs, policies, and interventions) that improve population health.
• Economic studies to determine the cost, efficiency, cost effectiveness, and economic impact of prevention strategies (such as those for obesity) and thus to inform the decisions of policymakers, communities, and individuals.
• Dissemination and implementation research to determine the best ways to organize, finance, and deliver effective prevention strategies to population groups that can benefit.
• Comparative effectiveness research and priority-setting studies to determine which prevention strategies work best in which community and institutional settings and in which population groups.
In addition to those traditional scientific approaches to learning what works, the public health field needs to seek knowledge from newly emerging avenues of inquiry, including the application of behavioral economics principles and complex systems analysis to study how environmental, social, and economic conditions and patterns of interaction combine to influence population health (see Box 3-2 for an example). Research in public health also needs to embrace “realistic” methods of inquiry that rely on cumulative, rapid-cycle learning from experience and that are designed to elucidate how complex, multicomponent public health strategies and prevention interventions interact with different social, environmental, and institutional contexts to produce community-level outcomes. The nontraditional approaches, termed realistic evaluation by Pawlson and Tilley in the social research literature and called the science of improvement by Berwick in the clinical research literature, offer methods that “are not compromises in learning how to improve; they are superior” (Berwick, 2008, p. 1183; Pawson and Tilley, 1997).
A strong infrastructure is needed to support each part of the research continuum described above. Specific needs include
• Robust data collection at state and community levels.
• Methods for constructing meaningful indicator sets—valid, reliable, sensitive, specific, and actionable.
• Infrastructure for accessing and linking with new and diverse sources of data relevant to population health, including electronic health data, place-based data sources (such as the food environment and the physical environment), and commercial data on purchasing, consumption, travel, work, and recreational behavior (also discussed in IOM, 2011).
• Research on analytic methods and a variety of techniques, including complex system modeling, structural equation modeling, and qualitative methods to shed light on causal mechanisms and the effectiveness of interventions.
• Training and development for the public health research workforce.
According to a social scientist (Coffman, 2003/2004, p. 7), evaluation and research can be contrasted as follows: Evaluation “determines the merit, worth, or value of things” through a process that “identifies relevant values or standards that apply to what is being evaluated, performs empirical investigation using techniques from the social sciences, and then integrates conclusions with the standards into an overall evaluation or set of evaluations.” Research does not seek to formulate evaluative conclusions but rather “is restricted to empirical (rather than evaluative) research, and bases
BOX 3-2
Obesity and Information Needs
In the case of obesity, little is known about the types of population-based interventions that can stem the tide of obesity that is leading to diabetes and other costly health conditions. As discussed in Chapter 1, complex adaptive systems are involved in causing obesity, and action on multiple levels is needed to solve this serious public health problem (Bar-Yam, 2006; Leischow and Milstein, 2006; Leischow et al., 2008). There are many gaps in public health knowledge about obesity. For example, although it is understood that obesity is in part the result of preventable risky behavior, such as inactivity and poor nutrition, there is not enough knowledge to guide the selection of interventions or combinations thereof. Is adding a supermarket a key requirement? What types of school-based interventions work? What about increasing the walkability of neighborhoods, and what elements of the built environment make the most difference? What combination of sidewalks, traffic lights, crosswalks, and bicycle and walking paths is needed? Little is known about how to select the best metrics to show improvement or to define what combination of individual-based and population-based interventions would make a difference. Food-environment data are becoming available, city planners are increasingly versed in public health, and several HHS agencies are targeting obesity, including through the study of policy interventions, but more research is needed, as is funding to support it.
BOX 3-3
Examples of Where Research and Evaluation Can Help
Considerable uncertainty remains in the policy and practice communities about the basic package of critical public health services that are needed in every community, the level of investment that is required to support the availability of the package of services, and the health and economic benefits that can be expected from the investment and over what timeframe, including the potential for downstream savings in medical care spending.
More and better evidence is needed to inform policy and managerial decisions about resource allocation in public health and to ensure accountability for current and future investment in the public health system. Implementing a standard chart of accounts as recommended in this chapter is a prerequisite.
The nation’s current public health knowledge and capabilities must be strengthened to address some of the most pressing threats to population health, such as those related to obesity and the effects of the social determinants of health. Where evidence-based strategies are lacking, the discovery of new knowledge and efficacious public health strategies is imperative. A robust research infrastructure is required to produce the evidence needed for optimizing the nation’s portfolio of investment in public health, but, as noted in the 2003 IOM report, there is still little infrastructure and support for this type of research. Research on public health services and systems is still in its adolescence (Scutchfield and Ingram, 2011).
its conclusions only on factual results—that is, observed, measured, or calculated data” (Coffman, 2003/2004). In the field of public health, research has several different purposes: on a practice level,10 to demonstrate the effectiveness and comparative effectiveness of population-based interventions; and on an administrative or management level, to inform the organization, administration, and financing of public health department activities. At each level, the committee has identified gaps in the knowledge available to inform decision making. That is pertinent to a report on funding both because of the need for research funding and because of the need for additional research on public health administration and financing (for example, research on the optimal size of a health department, discussed above; see also Box 3-3).
Not enough is known about how health departments can become learning organizations and acquire an adaptive systems perspective that would enable them to function productively in the self-organizing partnerships that
______________
10Much public health research is not practice-oriented, such as etiologic research, behavioral science, and laboratory science; but little research is aimed at closing the gap between research and practice, for example, research useful to those in the field who need to implement the best intervention for a given issue (Glasgow and Emmons, 2007).
are becoming the norm, as opposed to the traditional management setting (Leischow et al., 2008).
Translation of Research for Decisionmaking and Action
Building the research infrastructure that the committee proposes will allow policymakers to make informed resource allocation decisions that are based on societal or community values and on estimated health and economic impacts of prevention and public health strategies (including use by the National Prevention, Health Promotion, and Public Health Council as recommended in Chapter 2). It will help to develop evidence-based implementation strategies, guidelines, protocols, and checklists for use by the public health practice community. The evidence can be used to establish and update accreditation standards and performance expectations for public health agencies as accreditation becomes more widely adopted by public health agencies. Finally, the information that is generated would be used to support rapid-cycle innovation, quality improvement, and learning by public health agency administrators.
Cycle time in learning what works in public health needs to be reduced through research and development designed to “fail fast and often” to produce a steady stream of innovative results that do work well. Policymakers and public health decision makers need to be able to learn what works in public health, for what population, in what contexts, and at what cost. Whereas “steady-state” industries devote 2-3 percent to research and development, pharmaceutical, biotechnology and medical technology, and software industries all spend about 15 percent of their budgets on these endeavors (Cutler, 2011). Public health is most similar to industries that face pressures to grow, adapt, and improve and that rely heavily on research and development investments to generate the innovations that sustain them. Yet, of every $100 in federal health research spending, less than $1 is devoted to research on how to deliver (and finance) interventions, and most of that small amount is spent on delivery system research focused on medical care and only a minuscule portion on public health systems and services research (Woolf, 2007, 2008).
Public health has not been able to innovate, adapt, and respond quickly enough to contemporary health threats—particularly those associated with chronic disease. If it maintains a steady-state approach, public health and the larger health system will not be able to contain the rising health consequences and costs of chronic disease or address the changing needs of population health. With respect to large-scale chronic disease prevention, there are some good ideas but not a lot of evidence on whether and how they can be implemented effectively populationwide. Given the economic magnitude of the population health problem (75 percent of the nation’s $2.6 trillion
annual health care expenditures are due to chronic disease [CDC, 2011]), it seems prudent to invest in the research and development needed to learn how to avoid the preventable elements of that cost. For example, 15 percent of the current NHEA estimate of total federal public health spending ($11.5 billion) would be $1.7 billion. That amount, if devoted to public health research and development, would equal less than 0.1 percent of what the United States spends each year on health care for chronic disease treatment. If such an investment led to interventions that had only a modest impact on the growth of costs related to chronic disease, such as lowering the growth in cost by 1 percent as suggested by Roehrig and Rousseau (2011), it would yield a saving of more than $11 for every $1 invested—a highly favorable return on investment. The “value of information” associated with learning what works in public health seems to be very high according to its cost-saving potential.
The field must find ways to reach more of the populations that are at great risk for preventable disease and injury and must seek out new and more effective prevention strategies. The committee believes that knowing what works in population health is critical for the future of our nation, and the rate of spending on research and development in public health needs to be similar to that in the industries mentioned above—perhaps up to 15 percent of total public health expenditures. Funding of research, development, and dissemination in public health must be seen as a critical investment in the nation’s economic growth and competitiveness.
The ACA authorized a program of research related to many of the issues raised in this chapter (Section 4301, “Research on Optimizing the Delivery of Public Health Services”), but funding and infrastructure development for this program are not yet available. The committee recommends steps to achieve the needed research infrastructure.
Recommendation 6: The committee recommends that Congress direct the Department of Health and Human Services to develop a robust research infrastructure for establishing the effectiveness and value of public health and prevention strategies, mechanisms for effective implementation of these strategies, the health and economic outcomes derived from this investment, and the comparative effectiveness and impact of this investment. The infrastructure should include
• A dedicated stream of funding for research and evaluation.
• A national research agenda.
• Development of data systems and measures to capture research-quality information on key elements of public health delivery, including program implementation costs.
• Development and validation of methodologies for comparing the benefits and costs of alternative strategies to improve population health.
The recommended research infrastructure would be shared among three HHS agencies—the National Institutes of Health, the Agency for Healthcare Research and Quality, and the Centers for Disease Control and Prevention—and a national research agenda needs to include a priority-ordered list of topics to be addressed by the research. Development of data systems and measures to capture research-quality information (and training of needed staff) is needed at the national, state, and community levels and would include information on expenditures, workforce size and composition, and the volume, intensity, and mix of activities produced.11
There are many data systems for studying medical care delivery, such as the Medical Expenditure Panel Survey, the Healthcare Cost and Utilization Project with its National Inpatient Sample, and the National Ambulatory Medical Care Survey. Analogous data systems for public health delivery are needed. The development and validation of methods to improve population health need to include strategies from outside the health sector. The current research paradigm—randomized clinical trials as the gold standard for intervention research—needs to be expanded to include other empirical study designs and the use of modeling and microsimulation for comparing treatment strategies with prevention strategies, including strategies aimed at underlying determinants of health and combinations of strategies. As discussed in the committee’s report on measurement, system dynamics and other types of modeling are useful in a context of great complexity, such as one in which health problems are caused by multiple, interacting factors and requiring action by multiple stakeholders on many dimensions (see, for example, Homer and Hirsch, 2006; Homer et al., 2007, 2010; Jones et al., 2006; Leischow and Milstein, 2006; Leischow et al., 2008; Milstein, 2008; Milstein et al., 2011). Enhancing the research capacity of public health departments is consistent with the idea of public health departments as knowledge organizations described in Chapter 2.
On the basis of what is known about what public health agencies can and cannot afford to do and in light of the imbalance in national spending on clinical care and on population-based health services, the committee believes that the nation does not invest sufficiently in public health. The information available, however, does not allow the committee to determine with any precision what proportion of the nation’s health spending is needed to support population-based public health efforts. Improvements in the
______________
11This research model should reflect a desire for real progress by using traditional and nontraditional methods.
tracking of revenues and expenditures in public health and the enhancements in research and evaluation described in this chapter would no doubt inform the determination of public health funding needs, but a national effort is needed to begin to ascertain this and to make recommendations for an optimal balance. As the minimum package of public health services is established and the resources required to deliver them are ascertained, the public health field will gain a deeper understanding of the relative values of public health and clinical services. That understanding will inform investment in the public health system and the appropriate allocation between clinical care and population health.
Defining the minimum package of public health services will require the attention of a dedicated group that is knowledgeable about public health and population-based prevention, the economic impact of public health activities, and the value that could be realized by investment in clinical, nonclinical, and population-based efforts.
Recommendation 7: Expert panels should be convened by the National Prevention, Health Promotion, and Public Health Council to determine
• The components and cost of the minimum package of public health services at local and state and the cost of main federal functions.
• The proportions of federal health spending that need to be invested in the medical care and public health systems.
The information developed by the panels should be included in the council’s annual report to Congress.
Public health is dynamic, and there are always new challenges and the need to maintain progress in meeting old challenges. The recommended expert panels would anticipate future needs and capacities and adapt to changing circumstances.
This chapter has described two kinds of efforts needed to revitalize the public health infrastructure by clarifying how public health funding is used: standardizing financial information, which will require the development and adoption of a uniform chart of accounts, and expanding public health research to improve public health effectiveness and make the best use of resources. Earlier in this report, the committee described categories of public health knowledge that are adequate to inform action. Research and tools for disciplined management (given performance objectives and real world resource constraints) are needed to help public health professionals to do
their work better and more efficiently and to identify effective strategies and appropriate interventions. At the national level, expert guidance will fulfill two purposes: describing the governmental public health services that every community needs and determining the magnitude of funding necessary to accomplish them.
AcademyHealth. 2012. Public Health Services and Systems Research, 2003-2011. http://www.academyhealth.org/files/FileDownloads/HSRProjUpdate2012.pdf (December 12, 2011).
Ballinger, G. 2007. Refining estimates of public health spending as measured in national health expenditure accounts: The Canadian experience. Journal of Public Health Management & Practice 13(2):115-120.
Bar-Yam, Y. 2006. Improving the effectiveness of health care and public health: A multiscale complex systems analysis. American Journal of Public Health 96(3):459-466.
Berwick, D. M. 2008. The science of improvement. Journal of the American Medical Association 299(10):1182-1184.
CDC (Centers for Disease Control and Prevention). 2011. Rising Health Care Costs Are Unsustainable. http://www.cdc.gov/workplacehealthpromotion/businesscase/reasons/rising.html (January 27, 2012).
CHSR (Coalition for Health Services Research). 2009. Federal Funding for Health Services Research: Nominal Spending Increases Does Not Compensate for Years of Real Declines. Washington, DC: Academy Health.
CMS (Centers for Medicare and Medicaid Services). 2012. Hospital Cost Report. Washington, DC: CMS.
Coffman, J. 2003/2004. Michael Scriven on the differences between evaluation and social science research. Harvard Family Research Project 9(4):7.
Cook-Deegen, R. 2011. Boosting health services research. Science 333:1384-1385.
Crow, M. M. 2011. A radical restructure is the only way to solve the systemic problems of the world’s biggest funder of biomedical research. Nature 471:569-571.
Culyer, A. J., and J. Lomas. 2006. Deliberative processes and evidence-informed decision making in healthcare: Do they work and how might we know? Evidence & Policy: A Journal of Research, Debate and Practice 2(3):357-371.
Cutler, D. 2011 (March 3). Transcript, Eighth Meeting of the IOM Committee on Public Health Strategies to Improve Public Health. Washington, DC: IOM.
Donabedian, A. 1988. The quality of care: How can it be assessed? Journal of the American Medical Association 260 (12):1743-1748.
Dillion, A. 2010. Viewing Public Health Financial Information from a Different Perspective: Financial Ratio Analysis in Florida County Health Departments. http://www.publichealthsystems.org/media/file/Dillon2D.pdf (December 12, 2011).
Gans, D. N., N. F. Piland, and P. A. Honoré. 2007. Developing a chart of accounts: Historical perspective of the medical group management association. Journal of Public Health Management & Practice 13(2):130-132.
Garcia, R., and A. White. 2006. Healthy Parks, Schools, and Communities: Mapping Green Access and Equity for the Los Angeles Region. Los Angeles, CA: The City Project.
Garcia, R., Z. Rawson, M. Yellott, and C. Zaldana. 2009. Economic Stimulus, Green Space, and Equal Justice: Policy Report. Los Angeles, CA: The City Project.
Gaziano, T. A., G. Galea, and K. S. Reddy. 2007. Scaling up interventions for chronic disease prevention: The evidence. The Lancet 370:1939-1946.
Glasgow, R. E., and K. M. Emmons. 2007. How can we increase translation of research into practice? Types of evidence needed. Annual Review of Public Health 28:413-433.
Grosse, S. D., S. M. Teutsch, and A. C. Haddix. 2007. Lessons from cost-effectiveness research for United States public health policy. Annual Review of Public Health 28(1):365-391.
Halpin, H. A., M. M. Morales-Suarez-Varela, and J. M. Martin-Moreno. 2010. Chronic disease prevention and the new public health. Public Health Reviews 32(1):120-154.
Homer, J. B., and G. B. Hirsch. 2006. System dynamics modeling for public health: Background and opportunities. American Journal of Public Health 96(3):452-458.
Homer, J., G. Hirsch, and B. Milstein. 2007. Chronic illness in a complex health economy: The perils and promises of downstream and upstream reforms. System Dynamics Review 23(2-3):313-343.
Homer, J., B. Milstein, K. Wile, J. Trogdon, P. Huang, D. Labarthe, and D. Orenstein. 2010. Simulating and evaluating local interventions to improve cardiovascular health. Preventing Chronic Disease Public Health Research, Practice and Policy 7(1). http://www.cdc.gov/pcd/issues/2010/jan/08_0231.htm (January 3, 2012).
Honoré, P. A. 2011 (March 3). Financing Mechanisms & Models for a Public Health System of Accounts. Presentation to the IOM Committee on Public Health Strategies to Improve Public Health. Washington, DC: IOM.
Honoré, P. A., and J. F. Costich. 2009. Public health financial management competencies. Journal of Public Health Management & Practice 15(4):311-318.
Honoré, P. A., R. L. Clarke, D. M. Mead, and S. M. Menditto. 2007. Creating financial transparency in public health: Examining best practices of system partners. Journal of Public Health Management & Practice 13(2):121-129.
IOM (Institute of Medicine). 2003. The governmental public health infrastructure. In The Future of the Public’s Health. Washington, DC: The National Academies Press. Pp. 96-177.
IOM. 2011. For the Public’s Health: The Role of Measurement in Action and Accountability. Washington, DC: The National Academies Press.
Jones, A. P., J. B. Homer, D. L. Murphy, J. D. K. Essien, B. Milstein, and D. A. Seville. 2006. Understanding diabetes population dynamics through simulation modeling and experimentation. American Journal of Public Health 96(3):488-494.
Kaplan, R. S., and M. E. Porter. 2011. How to solve the cost crisis in health care. Harvard Business Review 89(9):47-64.
Karoly, L. A., M. R. Kilburn, and J. S. Cannon. 2005. Early Childhood Interventions: Proven Results, Future Promise. Santa Monica, CA: RAND.
Kelly, A. E., A. C. Haddix, K. S. Scanlon, C. G. Helmick, and J. Mulinare. 1996. Cost effectiveness of strategies to prevent neural tube defects. In Cost Effectiveness in Health and Medicine. New York: Oxford University Press. Pp. 312-349.
Leischow, S. J., and B. Milstein. 2006. Systems thinking and modeling for public health practice. American Journal of Public Health 96(3):403-405.
Leischow, S. J., A. Best, W. M. Trochim, P. I. Clark, R. S. Gallagher, S. E. Marcus, and E. Matthews. 2008. Systems thinking to improve the public’s health. American Journal of Preventative Medicine 35(2 Suppl):s196-s203.
Miller, G., C. Roehrig, P. Hughes-Cromwick, and C. Lake. 2008. Quantifying national spending on wellenss and prevention. In Beyond Health Insurance: Public Policy to Improve Health Advances in Health Economics and Health Services Research. Vol. 19. Pp. 1-24.
Milstein, B. 2008. Hygeia’s Constellation: Navigating Health Futures in a Dynamic and Democratic World. Atlanta, GA: CDC, Syndemics Prevention Network.
Milstein, B., J. Homer, P. Briss, D. Burton, and T. Pechacek. 2011. Why behavioral and environmental interventions are needed to improve health at lower cost. Health Affairs 30(5):823-832.
Moses, H., E. R. Dorsey, D. H. M. Matheson, and S. O. Thier. 2005. Financial anatomy of biomedical research. Journal of the American Medical Association 294(11):1333-1342.
NACCHO (National Association of City and County Health Officials). 2011. 2010 National Profile of Local Health Departments. Washington, DC: NACCHO.
Nowicki, M., and S. H. Berger. 2006. HFMA’s Introduction to Hospital Accounting, Fifth Edition. Chicago, IL: Health Administratio Press.
Pawson, R., and N. Tilley. 1997. Realistic Evaluation. London, England: Sage Publications Ltd.
PCORI (Patient-Centered Outcomes Research Institute). 2012. Draft National Priorities for Research and Research Agenda (Version 1). Washington, DC: PCORI.
PHSSR (Public Health Services and Systems Reserch). 2011. Public Health Services and Systems Research: Setting the Research Agenda. Lexington, Kentucky: PHSSR.
PHSSR. 2012. PHSSR Research Agenda. http://www.publichealthsystems.org/cphssr/Research/PHSSR_Research_Agenda (December 12, 2011).
Roehrig, C. S., and D. M. Rousseau. 2011. The growth in cost per case explains far more of US health spending increases than rising disease prevalence. Health Affairs 30( 9):1657-1663.
RWJF (Robert Wood Johnson Foundation). 2012. Public Health Services and Systems Research: Building Evidence for Decision-Making. http://www.rwjf.org/files/applications/cfp/cfp_phssr2012.pdf (April 2, 1012).
Scrimshaw S. C., White L., Koplan J. 2001. The meaning and value of prevention research. Public Health Reports 116(Suppl. 1):4-9.
Scutchfield, F. D., and R. Ingram. 2011. Issue Brief: Setting the Agenda for Public Health Services & Systems Research. Lexington, Kentucky: National Coordinating Center for Public Health Services & Systems Research.
Sensenig, A. L. 2007. Refining estimates of public health spending as measured in National Health Expenditures Accounts: The United States experience. Journal of Public Health Management Practice 13 (2):103-14.
Sensenig, A. L. 2011 (March 3). Measuring Spending on Public Health Activity in National Health Accounts. Presentation to the IOM Committee on Public Health Strategies to Improve Public Health. Washington, DC: IOM.
Sweet and Moynihan, 2007. Improving Population Health: The Uses of Systematic Reviews. New York: Milbank Memorial Fund and CDC.
Teutsch, S. M., and J. E. Fielding. 2011a. Applying comparative effectiveness research to public and population health initiatives. Health Affairs 30(2):349-355.
Teutsch, S. M., and J. E. Fielding. 2011b. Comparative effectiveness—looking under the lamppost. Journal of the American Medical Association 305(21):2225-2226.
TFCPS (Task Force on Community Preventive Services), S. Zara, P. A. Briss, and K. W. Harris, eds. 2005. The Guide to Community Preventive Services. What Works to Promote Health? New York: Oxford University Press.
Thacker, S. B., R. M. Ikeda, K. E. Gieseker, A. B. Mendelsohn, S. H. Saydah, C. W. Curry, and J. W. Yuan. 2005. The evidence base for public health informing policy at the Centers for Disease Control and Prevention. American Journal of Preventive Medicine 29(3):227-233.
University of Minnesota. 2010. Charts of Accounts. Minneapolis: Regents of the University of Minnesota.
Urban Institute National Center for Charitable Statistics. 2009. Unified Charts of Accounts. http://nccs.urban.org/projects/ucoa.cfm (December 29, 2011).
Weintraub, W. S., S. R. Daniels, L. E. Burke, B. A. Franklin, D. C. Goff, L. L. Hayman, D. Lloyd-Jones, D. K. Pandey, E. J. Sanchez, A. P. Schram, and L. P. Whitsel. 2011. Value of primordial and primary prevention for cardiovascular disease. Circulation 124(8):967-990.
Woolf, S. H. 2007. Potential health and economic consequences of misplaced priorities. Journal of the American Medical Association 297(5):523-526.
Woolf, S. H. 2008. The meaning of translational research and why it matters. Journal of the American Medical Association 299(2):211-213.


























