“To Err Is Human”
“Crossing the Quality Chasm”
Together, the above phrases—titles of reports—catalyzed a revolution in American health care to ensure patient safety and improve quality of care. To Err Is Human estimated that 44,000-98,000 lives are lost in hospitals every year due to medical errors and led to the widespread recognition that health care is not as safe as it should be (IOM, 1999). With an emphasis on improving quality,1 better results were thought to be achievable (IOM, 2001).
Subsequent research further documented the deficiencies in the quality and safety of American health care. Early work found evidence-based practice is only followed 55 percent of the time (McGlynn et al., 2003), and ensuing studies have reconfirmed that medical errors continue to be prevalent, as more than 1.5 million preventable adverse drug events occur annually (IOM, 2006). Adverse events can result from almost any type of interaction with the care system, at any point during care delivery, and in all care settings. Events can be the result of human, technological, and systems errors and can be classified as errors of commission (a direct consequence of treatment) or errors of omission (failure to undertake an action that should have been completed). Specific to safety, there has been a tendency to assume that a focus on quality will of necessity result in improved safety.
![]()
1 The Institute of Medicine (IOM) identified six aims of quality improvement, stating that health care should be safe, effective, patient-centered, timely, efficient, and equitable (2001).
This assumption may have delayed awareness of the need for a robust framework focused on safety alone.
Perhaps more important, these studies brought to light the critical concept of systemness, which recognizes that health care is a collection of disparate fragmented parts with many individual actors, each seeking to do their best by the patient instead of health professionals within a comprehensive “system.” This lack of systems to improve coordination in part fostered the promulgation of poor-quality, unsafe health care. Although the attention to systems of care have increased greatly, many of the efforts in the 10 years since To Err Is Human and Crossing the Quality Chasm have focused on processes of care as a first step, with the end goal of creating a comprehensive system of high-quality and safe care. These studies and those in the next section focused on quality and safety in health care overall. This background is needed to understand the context for discussing patient safety related to health information technology (health IT).2
More than 10 years since these landmark patient safety reports, there is considerable controversy about how much improvement in safety has actually occurred. Clearly some progress has been made with respect to specific processes, such as high rates of prescribing beta-blockers at discharge to patients presenting with an acute myocardial infarction (Chassin et al., 2010), and significantly reduced surgical mortality rates (Neily et al., 2010). Nationwide efforts were undertaken to reduce the number of medical errors in all care settings, and campaigns were developed to increase awareness, reduce risk factors, and develop a framework for high-quality care.
Despite these efforts, quality improvement throughout much of the U.S. health care system is still proceeding at a glacial pace. The National Healthcare Quality Report by the Agency for Healthcare Research and Quality (AHRQ) revealed that while nearly two-thirds of 179 measures of health care quality did show improvement, the median annual rate of change was only 2.3 percent. Several quality measures relating to cancer screening and diabetes management actually worsened during this time (AHRQ, 2010).
In terms of safety, several new studies have recently been published suggesting
![]()
2 Health IT is a term that is used somewhat interchangeably with other terms such as health information systems, health information and communications technology, and informatics. The terms are not necessarily defined the same way; for example, informatics–defined as a scientific field that draws upon the information sciences and related technology to enhance the use of the knowledge base of the health sciences to improve the health of individuals and populations through care, basic biomedical and clinical research, education, management, and policy–is a broader field than health IT. This report employs the term health IT but recognizes these other, broader terms are also used.
that patients continued to experience high rates of safety problems during hospital stays. Indeed, one study found adverse events continue to occur in as many as one-third of hospital patients (Classen et al., 2011). These adverse events occur in hospitalized patients even in regions where there has been a heavy programmatic focus on improving patient safety in hospitals (Landrigan et al., 2010). Safety problems also plague Medicare beneficiaries—a study suggests that more than 27 percent of Medicare beneficiaries will experience an adverse event during their hospitalizations, with half of these patients suffering more severe adverse events (HHS, 2010a).
These patient safety problems are not just limited to inpatient care. To Err Is Human recognized that more patients could be harmed by errors in ambulatory settings because more medical care is delivered outside of hospitals than inside. A recent review of malpractice claims concluded that 52 percent of all paid malpractice claims for all physician services involved ambulatory services, and almost two-thirds of these claims involved a major injury or death (Bishop et al., 2011).
Important differences exist between the inpatient and ambulatory settings regarding patient safety, including the types of errors seen (IOM, 1999), the relative importance of patient responsibility for following through on care decisions, and the different organizational and regulatory structures in place (Gandhi and Lee, 2010). As a result, it cannot be assumed that interventions to improve hospital safety will be applicable in the ambulatory setting, which deserves focused attention of its own. In recognition of this, an expert consensus conference to establish an agenda for research in ambulatory patient safety recognized that knowledge of ambulatory patient safety was lacking (Hammons et al., 2001). A recent 10-year review of ambulatory patient safety literature concluded that some progress has been made in understanding ambulatory safety, major gaps remain, and virtually no experiments or demonstrations have been done that show how to improve it (Lorincz et al., 2011).
This new refocus on patient safety as a specific system priority is best exemplified by a new Department of Health and Human Services (HHS) initiative with a sole focus on patient safety. Policy makers have recently recognized the significant challenges in improving patient safety across the continuum of care and the lack of progress over the past decade. HHS recently announced a national initiative called the Partnership for Patients, aimed at reducing preventable hospital-acquired conditions and complications, that would result in about 1.8 million fewer injuries to patients and would save more than 60,000 lives over 3 years. The partnership also aims to reduce preventable complications during care transitions, thereby cutting hospital readmissions by 20 percent from 2010 levels (HHS, 2011). This may herald a new national focus on patient safety over the next decade in the United States.
As these findings indicate, the opportunity to continue to improve is great, with many tools yet to be developed and effectively implemented. In virtually every report on patient safety summarized above, health IT has been identified as a critical tool to both measure and improve patient safety. Yet despite the possibility that health IT can enhance the safety and effectiveness of care, the widespread adoption and safe use of health IT products is still relatively immature. Technical and organizational limitations exist that can make health IT difficult to use effectively to improve the safety and quality of care.
For the purposes of this report, health IT includes a broad range of products, including electronic health records (EHRs),3 patient engagement tools (e.g., personal health records), and health information exchanges; excluded is software for medical devices (e.g., software in an implantable cardioverter-defibrillator). The use of data support systems in health settings began as administrative tools to facilitate billing processes and other related transactions. More recently, health IT has evolved to EHRs and other forms of technology that engage not just in transactions and data storage but also decision support and the capacity for clinicians and patients to see the patient’s clinical progress and data more easily. Clinicians and health care systems can potentially benefit from studying populations of similar patients, leading to learning health care systems. Clinicians expect health IT to support delivery of high-quality care in several ways, including storing comprehensive health data, providing clinical decision support, facilitating communication, engaging patients, and reducing medical errors. In the near future, it is likely that patients, particularly those with chronic illnesses, will consistently use the Internet to track their own health through personal health records and handheld device applications. Current health IT products are still improving their capacity to increase communications and reduce errors by making the right thing to do easier to do. It is important that health IT maximize patient safety while minimizing harm.
Adoption of health IT has been slow and is not yet widespread in the United States. Although adoption rates have increased significantly over the past decade, only 50.7 percent of office-based physicians use any type of EHR, with 10.1 percent reporting use of a fully functional record (Hsiao et al., 2010) (see Figure 1-1).
![]()
3 In this report, electronic health record will be used as the desired term over electronic medical record because it is more inclusive of the way electronic records are being used currently. EHRs include clinical decision support tools, computerized provider order entry systems, and e-prescribing systems.
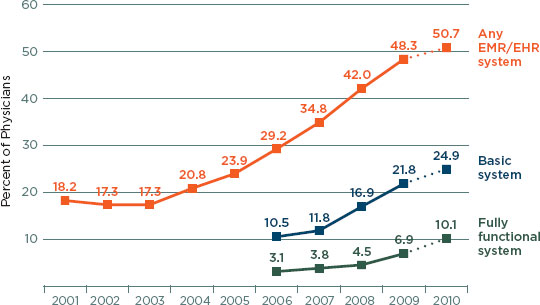
FIGURE 1-1
Percentage of office-based physicians with electronic medical records/electronic health records: United States, 2001-2009 and preliminary 2010.
NOTES: Any EMR/EHR is a medical or health record system that is either all or partially electronic (excluding systems solely for billing). The 2010 data are preliminary estimates (as show by dotted lines), based only on the mail survey. Estimates through 2009 include additional physicians sampled from community health centers; prior 2008 combined estimates were revised to include those physicians (4). Estimates of basic and fully functional systems prior to 2006 could not be computed because some items were not collected in the survey. Fully functional systems are a subset of basic systems. Some of the increase in fully functional systems between 2009 and 2010 may be related to a change in survey instruments and definitions of fully functional systems between 2009 and 2010. Includes nonfederal, office-based physicians. Excludes radiologists, anesthesiologists, and pathologists.
SOURCE: Hsiao et al. (2010); CDC/NCHS, National Ambulatory Medical Care Survey.
With respect to hospitals, 11.9 percent of U.S. hospitals use comprehensive EHRs (Jha et al., 2010). Many barriers to adopting health IT exist, including the complexity of training needed to integrate systems into new patterns and clinical workflows, the cost of acquiring and maintaining health IT, and the lack of resources to overcome barriers to implementation. As a result, the current culture of care delivery is often not ready for widespread safer and more effective use of health IT.
In contrast to the United States, other countries have achieved much higher adoption rates of EHRs. Denmark has had fully electronic patient records for 10 years, and countries such as the Netherlands, Australia,
Singapore, and Canada also are much further along than the United States (see Chapter 2). These countries report both efficiencies in operation and reductions in prescription error rates. Problems associated with health IT reported overseas, most recently highlighted in the United Kingdom’s decision to end its National Programme for IT after spending £6.4 of the £11 billion allotted for the program, reflect complex issues of contracts, product capabilities, and vendor performance, not necessarily patient safety (Whalen, 2011).
A report by the President’s Council of Advisers on Science and Technology concluded that the full potential of health IT to improve the quality and cost of health care has not yet been realized. Many advances will be needed, from lifting barriers (e.g., eliminating the proprietary nature of products to promote interoperability, broadening the ways in which data are used, ensuring privacy and security) to more innovative and competitive health IT products (PCAST, 2010).
In an effort to improve health care, the U.S. government has invested and will continue to invest billions of dollars toward the meaningful use of effective health IT in the hopes of improving the quality of care, decreasing the cost of care through improved efficiency, and guiding clinicians to choose the most effective care interventions. In 2004, the Office of the National Coordinator for Health Information Technology (ONC) was established by executive order within the Office of the Secretary of HHS. It was created in statute by the Health Information Technology for Economic and Clinical Health (HITECH) Act, part of the American Recovery and Reinvestment Act of 2009. Working toward the goal of bringing EHRs to all Americans by 2014, the mission of the ONC is to both coordinate development of a national health IT infrastructure and support and promote meaningful use of EHRs. The ONC is supported directly and indirectly by several federal advisory bodies (ONC, 2011). Those directly involved include the following:
• The Health IT Policy Committee was provided for in the HITECH Act to make recommendations to the National Coordinator for Health IT toward development of a policy framework for a nationwide health information infrastructure.
• The Health IT Standards Committee was established at the same time as the Policy Committee for the purpose of making recommendations regarding standards and certification criteria for the electronic exchange and use of health IT to the National Coordinator.
• The National Committee on Vital and Health Statistics was established in 1949 to advise the Secretary of HHS in issues related to health data, statistics, and national information policy. Its National
Health Information Infrastructure report created the vision for the emerging system (NCVHS, 2001).
Indirectly, the ONC receives helpful advice from a number of groups, including the advisory groups for the National Library of Medicine, AHRQ, multiple Boards of Scientific Counselors of the Centers for Disease Control and Prevention, the Visiting Committee on Advanced Technology of the National Institute for Standards and Technology, and the multiple advisory committees of the Food and Drug Administration.
In collaboration with many private efforts and other public agencies, these groups have been instrumental in advancing the development of an initial framework for health IT. Although these efforts have been essential to advancing the state of health IT, much more work is needed before all Americans will have access to health IT-assisted care.
Development of health IT-assisted care is also being encouraged by the broader health policy environment. Safe, interoperable health IT is a foun- dational component of strategies such as accountable care organizations and the patient-centered medical home. The promise of these movements to reduce costs and improve patient outcomes assumes that high-quality patient data can be shared reliably and effectively among providers. These movements, among others, are likely to influence the speed of adoption and broaden the functions of health IT considerably (NCVHS, 2001). In contrast to these possible future uses, it is clear that current health IT implementations are often complex, cumbersome, and brittle in ways that may also have negative effects on clinician performance (AHRQ, 2009; HIMSS, 2009; PCAST, 2010).
INTERSECTION OF PATIENT SAFETY AND HEALTH IT
Health IT is not one specific product that, once implemented, can automatically result in highly safe and effective health care. It encompasses a technical system of computers, software, and devices that operate in the context of a larger sociotechnical system—a collection of hardware and software working in concert within an organization that includes people, processes, and workflow. It is widely believed that, when designed and used appropriately, health IT can help create an ecosystem of safer care while also producing a variety of benefits such as reductions in administrative costs, improved clinical performance, and better communication between patients and caregivers. In this view, it can be a positive, transformative force for delivering health care. However, the assumption that the aforementioned benefits are highly correlated with health IT has not been adequately tested, and there are some indications that the features needed to acquire one benefit may actually frustrate efforts to achieve another.
In particular, there is a growing concern that health IT designs that maximize the potential for administrative and economic benefit may be creating new paths to failure. Reports of health IT becoming a distraction or cause of miscommunication raise the possibility that health IT may cause harm if it is poorly designed, implemented, or applied. Poorly designed, implemented, or applied, health IT can create new hazards in the already complex delivery of health care, requiring health care professionals to work around brittle software, adding steps needed to accomplish tasks, or presenting data in a nonintuitive format that can introduce risks that may lead to harm. Risks to patient safety also arise as a result of great heterogeneity in health IT products. As health IT products have become more intimately involved in the delivery of care, the potential for health IT-induced medical error, harm, or death has increased significantly. Examples of health IT-induced harm that can result in serious injury and death include dosing errors, failing to detect fatal illnesses, and delaying treatment due to poor human-computer interactions or loss of data (Aleccia, 2011; Associated Press, 2009; Graham and Dizikes, 2011; Schulte and Schwartz, 2010; Silver and Hamill, 2011; U.S. News, 2011).
The portfolio of research on health IT has included little regarding the general impact of health IT on safety of clinical care. The evidence in the literature about the impact of health IT on patient safety is mixed but shows that the challenges facing safer health care and safer use of health IT involve the people and clinical implementation as much as the technology. The literature does reflect improvements in some areas in well-established health care institutions, notably medication administration through use of computerized prescribing and bar-coding systems. But the evidence of health IT’s impact on patient safety beyond medication safety and across the health care system is lacking. Although evidence suggests improvements in safety can be made, some studies have found health IT to have no effect on patient safety, and case reports such as those cited above show that it can also contribute to harm.
Advanced technology can create some new paths to failure at the same time that it blocks others. These new forms of failure are often hard to anticipate and may go unnoticed or be misidentified until the introduction of the new technology is well advanced. The resulting shift in the locus of failure can make the evaluation of the impact of technology on safety difficult, especially if the contribution of technology to the new forms of failure is not appreciated (Woods et al., 2010). Given the large investments being made in health IT, there is a great need to ensure that the new technology is actually improving safety of care.
The ONC’s Health IT Policy Committee held a hearing on patient safety and health IT in February 2010 and recommended the ONC “commission a formal study to thoroughly evaluate health IT patient safety concerns, and to recommend additional actions and strategies to address those concerns” (HHS, 2010b). In September 2010, the ONC asked the Institute of Medicine (IOM) to make recommendations about how public and private actors can maximize the safety of health IT-assisted care (see Box 1-1). In response, the IOM established the Committee on Patient Safety and Health Information Technology.
The committee’s report comes at a point in time characterized by a number of rather dramatic changes relating to health care in addition to major national health insurance and financial reforms. First, the HITECH legislation provides substantial incentives to accelerate the adoption of EHR systems. Second, there is an ongoing movement away from the historical
BOX 1-1
Statement of Task
An ad hoc committee will review the available evidence and the experience from the field on how the use of health information technology affects the safety of patient care and will make recommendations concerning how public and private actors can maximize the safety of health IT-assisted health care services. The committee will produce a report that will be both comprehensive and specific in terms of recommended options and opportunities for public and private interventions that may improve the safety of care that incorporates the use of electronic health records (EHRs) and other forms of health IT.
“Health IT-assisted care” means health care and services that incorporate and take advantage of health information technologies and health information exchange for the purpose of improving the processes and outcomes of health care services. Health IT-assisted care includes care supported by and involving EHRs, clinical decision support, computerized provider order entry, health information exchange, patient engagement technologies, and other health information technology used in clinical care.
The committee will (1) summarize existing knowledge of the effects of health IT on patient safety; (2) make recommendations to HHS regarding specific actions that federal agencies should take to maximize the safety of health IT-assisted care; and (3) make recommendations concerning how private actors can promote the safety of health IT-assisted care, and how the federal government can assist private actors in this regard.
model of physician autonomy to one focused on adherence to evidence-based guidelines and best practices that promote safe, high-quality care. Finally, the practice of medicine is inexorably moving from being based primarily upon knowledge of organs and organ systems to being based upon genomics and proteomics, which has major implications for data management capabilities. The aggregate impact of these tectonic shifts beneath health care and its related technologies and treatments is one that requires development of more complex yet reliable systems to assure high performance in the midst of great baseline challenges to achieving excellent outcomes.
Scope
In his statement to the committee, David Blumenthal, the then-National Coordinator, asked the committee to consider the full range of activities available in developing recommendations to assure the safety of health IT-assisted care (Blumenthal, 2010). The statement of task defines health IT very broadly and includes multiple types of technologies used in the delivery of health care services. The committee considered all stakeholders as having important roles in improving patient safety with respect to health IT. This includes patients and their families, health professionals, health care delivery organizations (ranging from small physician offices to large hospital systems), health IT vendors, accrediting agencies, professional societies, insurance companies, and the government.
Controversy exists regarding the impact of both the introduction of health IT and the use of health IT on patient safety. Proponents argue that published literature from trials generally support the claim that health IT can reduce particular types of failure, improve quality and safety, and reduce costs. Critics point to reports of health IT failures. This report does not attempt to resolve the controversy; instead it seeks to assess some of the important issues surrounding health IT and its introduction and to indicate the activities most likely to bring the potential value of health IT to the U.S. health care system. Therefore, while the committee recognizes that both risks and benefits are associated with health IT, it interpreted its charge as making health IT-assisted care safer so that the nation is in a better position to realize the potential benefits of health IT.
The committee did not examine a number of issues related to health IT, including whether health IT should be implemented, access to health IT products, medical liability, privacy, security, and standards. These are critical for the ONC to address in order to achieve its mission of having widespread use of EHRs by 2014. Similarly, the validity and use of information from common Internet sites applied to specific patient situations during delivery of care is also important in the changing health care delivery environment but was not considered in the scope of this report. The committee
also did not consider recommendations to address the broader issues associated with health care safety. This report focuses on patient safety as it relates to health IT and the delivery of care and will therefore concentrate on the aspects of health IT directly pertaining to safety.
Methods
To address the statement of task, the committee conducted a wide- ranging evaluation of the literature to gather evidence about patient safety and health IT (see Appendix B) and received input in a variety of forums. Over the course of this 12-month study, the committee met in person three times. The committee also benefited by engaging with the public during two workshops where it received statements from various stakeholder organizations. Additionally, the committee solicited input from the public and specifically the EHR vendor community.4 Public comments included both statements about how a health IT product had improved the safety of an organization as well as instances of harm. Vendors described various processes adopted to both receive and handle customer-submitted reports of patient safety issues, some appointing a formal team to guide follow- on actions. However, when asked about the volume and types of adverse events related to their EHR products, vendor responses ranged from 0 to 40 events per year, although none provided a full list of problematic events and potential patient safety concerns (IOM, 2011). The committee considered all these statements over the course of its deliberations and weighed them against the literature and its expertise. Given the committee’s limited ability to verify statements from the public and vendors, it did not systematically weigh these statements.
RECOMMENDATIONS FROM PREVIOUS IOM REPORTS REGARDING HEALTH IT
For more than two decades, the IOM and the National Academy of Sciences have recognized health IT as a central component of a safe, high- quality health care system. The first uses of computers for medical information and records were primarily for reporting the results of laboratory tests and for administrative purposes, particularly billing. It was only later that they began to be used for a wider array of clinical uses, in particular as a supplement to or replacement for paper for holding medical record data. The growth of computing technology led the IOM to form a committee in
![]()
4 In this report, the term vendor is used to mean companies that design, make, and sell health IT products. In many industries the terms developers and manufacturers are also used, but in health IT, vendor is generally the preferred term.
1989 to examine this development and make recommendations relating to the future of computers in record keeping. The report of this committee was entitled The Computer-Based Patient Record: An Essential Technology for Health Care and it explained the contrast to the traditional paper-based medical record. Lawrence Weed had described his problem-oriented medical record in 1969 and it was being developed in a computer-based format in a system known as the problem-oriented medical information system (PROMIS). The IOM report made a number of important conceptual contributions well ahead of the maturation of the technology and its uses in health care by focusing first on the patient, making it clear that patient- centeredness was primary, and that the key was not who was entering the information into the record. Clearly, it denoted that the record was based upon a computer and not on paper. The subtitle focused upon health care, not medical, nursing, public health, or any other subcategory relating to health-related activities for which a record was kept. In that sense, it was not envisioning an electronic medical record, but a record for medical care as well as any care relating to health at that time.
Finally, The Computer-Based Patient Record identified a list of 12 functions that a record should properly serve. The committee’s vision was very clear in the context of both its perspective and its functionalities. The report was also limited in the sense that computer-based personal health records and computer-based public health records have changed dramatically since the time of its publication. The report reflected its time with a focus upon the record as used in medical environments, but not solely for medicine or medical care in the narrowest sense. It set a vision for nationwide computer-based patient records and called for electronic records to be standard in care delivery and detailed primary and secondary uses of electronic records (IOM, 1991). A later effort concluded that development of robust data was critical to attaining this vision, requiring the creation of data standards and collection of data for regional and national patient- record efforts (IOM, 1994).
However, progress toward these goals was too slow (IOM, 2001), leading to the continued recognition that health IT is essential to reengineering the health care system (IOM, 2001, 2003, 2004b; NAE and IOM, 2005). Recommendations identified ways health IT could be advanced and included the following:
• A renewed call for comprehensive national data standards to be established and disseminated by the federal government for the definition, collection, coding, and exchange of data (IOM, 2001, 2004b);
• A series of demonstration projects to develop a health IT infrastructure—particularly in the areas of communication, access
to patient information, knowledge management, and decision support—that would take place at the community, state, multistate, and regional levels (IOM, 2003);
• Industry and government collaboration at a national level, for example with the development of public-private partnerships (IOM, 2004a; NAE and IOM, 2005); and
• Large federal investments to support the development of a national health information infrastructure to improve patient safety and health care delivery (IOM, 2002, 2004b; NAE and IOM, 2005).
In 2003, the IOM reported that emerging competencies for the future include knowledge, skills, and attitudes relating to (1) practice in teams, (2) use of evidence-based knowledge, (3) continuously improving quality, (4) patient-centered care, and (5) employing informatics. Education and training must go beyond simply educating current clinicians on how to use a specific EHR product. For safe delivery of health care in the future, health professionals need to know how to work in complex systems. Understanding health IT within the context of contemporary health reforms and challenges for improving safety and outcomes will be critical (IOM, 2004a).
Upon recognizing that many types of health IT exist to address many different purposes, and can vary by setting of care, the IOM examined specific components of health IT (IOM, 2004b). Particular emphasis was placed on EHRs and reduction of medication errors. To help move the field forward, the IOM described an EHR system as a system that “encompasses (1) longitudinal collection of electronic health information for and about persons, (2) electronic access to person- and population-level information by authorized users, (3) provision of knowledge and decision support systems, and (4) support for efficient processes for health care delivery” (IOM, 2004b). It identified eight key functionalities for EHR systems: health information and data, results management, order entry management, decision support, electronic communication and connectivity, patient support, administrative processes, and reporting and population health management.
In an effort to emphasize the importance of preventing medication errors, the effective use of technologies to reduce medication errors was the focus of a different IOM committee. Agencies within HHS were identified as actors to establish standards affecting drug-related health information technologies, such as development of a common drug nomenclature to be used in all clinical IT systems, specifications for alert mechanisms and intelligent prompting, and optimum design of user interfaces for the clinical environment. These recommendations were made to address patients’ unique characteristics and needs while also recognizing providers’ individual prescribing, ordering, and error patterns (IOM, 2006).
Despite the efforts made over the past few decades, a recent report by the National Research Council (NRC, 2009) concluded that the current investment in health IT is inadequate to fully realize the positive effects IT can have to make health care more effective. If the promise of a high- performing health care system is to be achieved, future efforts will need to emphasize cognitive support for health care providers and patients, such as enhanced decision making and problem solving, which will require an interdisciplinary approach. In essence, the report sought to refocus attention to humans and away from technology as a simple solution.
This report consists of seven chapters, of which this introduction is the first. The committee evaluates the current state of health IT in Chapter 2 and offers a systems approach for health IT safety in Chapter 3. Chapter 4 highlights opportunities to improve safety from the perspectives of both manufacturers and users of health IT. The role of patients and their families is explored in Chapter 5. The responsibilities of the private and public sectors are explored in Chapter 6. Finally, the committee offers a future research agenda for health IT safety in Chapter 7.
AHRQ (Agency for Healthcare Research and Quality). 2009. Electronic health record usability: Evaluation and use case framework. Rockville, MD: AHRQ.
AHRQ. 2010. National healthcare quality report. Rockville, MD: AHRQ.
Aleccia, J. 2011. Nurse’s suicide highlights twin tragedies of medical errors. MSNBC.com. http://www.msnbc.msn.com/id/43529641/ns/health-health_care/t7nurses-suicide-highlights-twin-tragedies-medical-errors/#.Tph_EHI2Y9Y (accessed October 14, 2011).
Associated Press. 2009. Veterans given wrong drug doses due to glitch. MSNBC.com. http://www.msnbc.msn.com/id/28655104/#.Tph-b3I2Y9Z (accessed October 14, 2011).
Bishop, T. F., A. K. Ryan, and L. P. Casalino. 2011. Paid malpractice claims for adverse events in inpatient and outpatient settings. Journal of the American Medical Association 305(23):2427-2431.
Blumenthal, D. 2010. Statement to IOM Committee on Patient Safety and Health Information Technology. Statement read at the Workshop of the IOM Committee on Patient Safety and Health Information Technology, Washington, DC.
Chassin, M. R., J. M. Loeb, S. P. Schmaltz, and R. M. Wachter. 2010. Accountability measures—using measurement to promote quality improvement. New England Journal of Medicine 363(7):683-688.
Classen, D. C., R. Resar, F. Griffin, F. Federico, T. Frankel, N. Kimmel, J. C. Whittington, A. Frankel, A. Seger, and B. C. James. 2011. “Global trigger tool” shows that adverse events in hospitals may be ten times greater than previously measured. Health Affairs 30(4):581-589.
Gandhi, T. K., and T. H. Lee. 2010. Patient safety beyond the hospital. New England Journal of Medicine 363(11):1001-1003.
Graham, J., and C. Dizikes. 2011. Baby’s death spotlights safety risks linked to computerized systems. Los Angeles Times. http://www.latimes.com/health/ct-met-technology- errors-20110627,0,2158183.story (accessed June 29, 2011).
Hammons, T., N. F. Piland, S. D. Small, M. J. Hatlie, H. R. Burstin. 2001. An agenda for research in ambulatory patient safety: Conference synthesis. Rockville, MD: Agency for Healthcare Research and Quality.
HHS (Department of Health and Human Services). 2010a. Adverse events in hospitals: National incidence among Medicare beneficiaries. Washington, DC: HHS.
HHS. 2010b. Letter to the National Coordinator for Health Information Technology providing recommendations on the topic of patient safety. Washington, DC: HHS.
HHS. 2011. News release: Partnership for patients to improve care and lower costs for Americans. Washington, DC: HHS.
HIMSS (Healthcare Information and Management Systems Society). 2009. Defining and testing EMR usability: Principles and proposed methods of EMR usability evaluation and rating. http://www.himss.org/content/files/HIMSS_DefiningandTestingEMRUsability.pdf (accessed April 25, 2011).
Hsiao, C.-J., E. Hing, T. C. Socey, and B. Cai. 2010. Electronic medical record/electronic health record systems of office-based physicians: United States, 2009, and preliminary 2010 state estimates. Atlanta, GA: CDC.
IOM (Institute of Medicine). 1991. The computer-based patient record: An essential technology for health care. Washington, DC: National Academy Press.
IOM. 1994. Health data in the information age: Use, disclosure, and privacy. Washington, DC: National Academy Press.
IOM. 1999. To err is human: Building a safer health system. Washington, DC: National Academy Press.
IOM. 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
IOM. 2002. Leadership by example: Coordinating government roles in improving health care quality. Washington, DC: The National Academies Press.
IOM. 2003. Fostering rapid advances in health care: Learning from system demonstrations. Washington, DC: The National Academies Press.
IOM. 2004a. 1st annual Crossing the Quality Chasm Summit: A focus on communities. Washington, DC: The National Academies Press.
IOM. 2004b. Patient safety: Achieving a new standard for care. Washington, DC: The National Academies Press.
IOM. 2006. Preventing medication errors: Quality Chasm Series. Washington, DC: The National Academies Press.
IOM. 2011 (unpublished). Vendor responses—summary. Washington, DC: IOM.
Jha, A. K., C. M. DesRoches, P. D. Kralovec, and M. S. Joshi. 2010. A progress report on electronic health records in U.S. hospitals. Health Affairs 29(10):1951-1957.
Landrigan, C. P., G. J. Parry, C. B. Bones, A. D. Hackbarth, D. A. Goldmann, and P. J. Sharek. 2010. Temporal trends in rates of patient harm resulting from medical care. New England Journal of Medicine 363(22):2124-2134.
Lorincz, C. Y., E. Drazen, P. E. Sokol, K. V. Neerukonda, J. Metzger, M. C. Toepp, L. Maul, D. C. Classen, M. K. Wynia. 2011. Research in ambulatory patient safety 2000-2010: A 10-year review. Chicago, IL: American Medical Association.
McGlynn, E. A., S. M. Asch, J. Adams, J. Keesey, J. Hicks, A. DeCristofaro, and E. A. Kerr. 2003. The quality of health care delivered to adults in the United States. New England Journal of Medicine 348(26):2635-2645.
NAE (National Academy of Engineering) and IOM. 2005. Building a better delivery system: A new engineering/health care parternship. Washington, DC: The National Academies Press.
NCVHS (National Committee on Vital and Health Statistics). 2001. Information for health: A strategy for building the National Health Information Infrastructure. Washington, DC: NCVHS.
Neily, J., P. D. Mills, Y. Young-Xu, B. T. Carney, P. West, D. H. Berger, L. M. Mazzia, D. E. Paull, and J. P. Bagian. 2010. Association between implementation of a medical team training program and surgical mortality. Journal of the American Medical Association 304(15):1693-1700.
NRC (National Research Council). 2009. Computational technology for effective health care: Immediate steps and strategic directions. Washington, DC: The National Academies Press.
ONC (Office of the National Coordinator for Health IT). 2011. Federal advisory committees (FACAs). http://healthit.hhs.gov/portal/server.pt/community/healthit_hhs_gov federal_ advisory_committees_(facas)/1149#top (accessed February 4, 2011).
PCAST (President’s Council of Advisors on Science and Technology). 2010. Realizing the full potential of health information technology to improve healthcare for Americans: The path forward. http://www.whitehouse.gov/sites/default/files/microsites/ostp/pcast-health- it-report.pdf (accessed May 18, 2011).
Schulte, F., and E. Schwartz. 2010. As doctors shift to electronic health systems, signs of harm emerge. Huffington Post Investigative Fund. http://huffpostfund.org/stories/2010/04/ doctors-shift-electronic-health-systems-signs-harm-emerge (accessed October 13, 2010).
Silver, J. D., and S. D. Hamill. 20111. Doctor, nurse disciplined by UPMC in kidney transplant case. Post-Gazette.com. http://www.post-gazette.com/pg/11147/1149429-114-0.stm#ixzz1amZZEw6Y (accessed October 14, 2011).
U.S. News. 2011. E-prescribing doesn’t slash errors, study finds. U.S. News and World Report. http://health.usnews.com/health-news/family-health/articles/2011/06/30/e-prescribing- doesnt-slash-errors--study-finds (accessed October 14, 2011).
Whalen, J. 2011. U.K. ends health-service IT upgrade. Wall Street Journal. http://online.wsj.com/article/SB20001424053111904563904576587054273647780.html (accessed October 12, 2011).
Woods, D., S. Dekker, R. Cook, L. Johannesen, and N. Sarter. 2010. Behind human error, 2nd ed. Burlington, VT: Ashgate Publishing.
















