Food and Beverage Environments
Food and Beverage Environments: Goal, Recommendation, Strategies, and Actions for Implementation
Goal: Create food and beverage environments that ensure that healthy food and beverage options are the routine, easy choice.
Recommendation 2: Governments and decision makers in the business community/private sector1 should make a concerted effort to reduce unhealthy food and beverage options2 and substantially increase healthier food and beverage options at affordable, competitive prices.
![]()
1The business community/private sector includes private employers and privately owned and/ or operated locations frequented by the public, such as movie theaters, shopping centers, sporting and entertainment venues, bowling alleys, and other recreational/entertainment facilities.
2Although there is no consensus on the definition of “unhealthy” foods/beverages, the term refers in this report to foods and beverages that are calorie-dense and low in naturally occurring nutrients. Such foods and beverages contribute little fiber and few essential nutrients and phytochemicals, but contain added fats, sweeteners, sodium, and other ingredients. Unhealthy foods and beverages displace the consumption of foods recommended in the Dietary Guidelines for Americans and may lead to the development of obesity.
Strategy 2-1: Adopt policies and implement practices to reduce overconsumption of sugar-sweetened beverages. Decision makers in the business community/private sector, in nongovernmental organizations, and at all levels of government should adopt comprehensive strategies to reduce overconsumption of sugar-sweetened beverages.3
For schools and other locations where children and adolescents are cared for, potential actions include
• prohibiting access to sugar-sweetened beverages;
• providing a variety of beverage options that are competitively priced and are recommended by and included in the Dietary Guidelines for Americans; and
• making clean, potable water available.
For the business community/private sector, nongovernmental organizations, and governments, potential actions include
• making clean, potable water readily available in public places, worksites, and recreation areas;
• making a variety of beverage options that are competitively priced readily available in public places, worksites, and recreation areas;
• implementing fiscal policies aimed at reducing overconsumption of sugar-sweetened beverages through (1) pricing and other incentives to make healthier beverage options recommended by the Dietary Guidelines for Americans more affordable and, for governments, (2) substantial and specific excise taxes on sugar-sweetened beverages (e.g., cents per ounce of liquid, cents per teaspoon of added sugar), with the revenues being dedicated to obesity prevention programs;
![]()
3Sugar-sweetened beverages are defined to include all beverages containing added caloric sweeteners, including, but not limited to, sugar- or otherwise calorically sweetened regular sodas, less than 100 percent fruit drinks, energy drinks, sports drinks, and ready-to-drink teas and coffees.
• supporting the work of community groups and coalitions to educate the public about the risks associated with overconsumption of sugar-sweetened beverages; and
• developing social marketing campaigns aimed at reducing overconsumption of sugar-sweetened beverages.
For the food and beverage industry, potential actions include
• developing and promoting a variety of beverage options for consumers, including a range of healthy beverage options, beverages with reduced sugar content, and smaller portion sizes (e.g., 8-ounce containers).
For health care providers, such as physicians, dentists, registered dietitians, and nurses, potential actions include
• performing routine screening regarding overconsumption of sugar-sweetened beverages and counseling on the health risks associated with consumption of these beverages.
Strategy 2-2: Increase the availability of lower-calorie and healthier food and beverage options for children in restaurants. Chain and quick-service restaurants should substantially reduce the number of calories served to children and substantially expand the number of affordable and competitively priced healthier options available for parents to choose from in their facilities.
Potential actions include
• developing a joint effort (modeled after the Healthy Weight Commitment initiative) to set a specific goal for substantially reducing the total annual calories served to children in these facilities; and
• ensuring that at least half of all children’s meals are consistent with the food and calorie guidelines of the Dietary Guidelines for Americans for moderately active 4- to 8-year-olds and are competitively priced.
Strategy 2-3: Utilize strong nutritional standards for all foods and beverages sold or provided through the government, and ensure that these healthy options are available in all places frequented by the public. Government agencies (federal, state, local, and school district) should ensure that all foods and beverages sold or provided through the government are aligned with the age-specific recommendations in the current Dietary Guidelines for Americans. The business community and the private sector operating venues frequented by the public should ensure that a variety of foods and beverages, including those recommended by the Dietary Guidelines for Americans, are sold or served at all times.
For government agencies, potential actions include
• the federal government expanding the healthy vending/concession guidelines to include all government-owned and/or -operated buildings, worksites, facilities,4 and other locations where foods and beverages are sold/served; and
• all state and local government-owned and -operated buildings, worksites, facilities, and other locations where foods and beverages are sold/served (including through vending machines and concession stands) adopting and implementing a healthy food and beverage vending/concession policy.
For the business community/private sector, potential actions include
• the business community and private-sector entities that operate places frequented by the public ensuring that a variety of food and beverage options are competitively priced and available for purchase and consumption in
![]()
4“Government-owned and -operated buildings, worksites, and facilities” is defined broadly to include not only places of work but, also, locations such as government-owned and/or -operated child care centers, hospitals, and other health care/assisted living facilities, military bases, correctional facilities, and educational institutions.
these places,5 including foods and beverages that are aligned with the recommendations of the Dietary Guidelines for Americans.
Strategy 2-4: Introduce, modify, and utilize health-promoting food and beverage retailing and distribution policies. States and localities should utilize financial incentives such as flexible financing or tax credits, streamlined permitting processes, and zoning strategies, as well as cross-sectoral collaborations (e.g., among industry, philanthropic organizations, government, and the community) to enhance the quality of local food environments, particularly in low-income communities. These efforts should include encouraging or attracting retailers and distributors of healthy food (e.g., supermarkets) to locate in under-served areas and limiting the concentration of unhealthy food venues (e.g., fast-food restaurants, convenience stores). Incentives should be linked to public health goals in ways that give priority to stores that also commit to health-promoting retail strategies (e.g., through placement, promotion, and pricing).
Potential actions include
• states creating cross-agency teams to analyze and streamline regulatory processes and create tax incentives for retailing of healthy foods in under-served neighborhoods;
• states and localities creating cross-sectoral collaborations among the food and beverage industry, philanthropy, the finance and banking sector, the real estate sector, and the community to develop private funding to facilitate the development of healthy food retailing in underserved areas; and
• localities utilizing incentive tools to attract retailing of healthy foods (e.g., supermarkets and grocery stores) to underserved neighborhoods, such as through flexible financing or tax credits, streamlined permitting processes, zoning strategies, grant and loan programs, small business/economic development programs, and other economic incentives.
![]()
5“Places frequented by the public” includes, but is not limited to, privately owned and/or operated locations frequented by the public such as movie theaters, shopping centers, sporting and entertainment venues, bowling alleys, and other recreational/entertainment facilities.
Strategy 2-5: Broaden the examination and development of U.S. agriculture policy and research to include implications for the American diet. Congress, the Administration, and federal agencies should examine the implications of U.S. agriculture policy for obesity, and should ensure that such policy includes understanding and implementing, as appropriate, an optimal mix of crops and farming methods for meeting the Dietary Guidelines for Americans.
Potential actions include
• the President appointing a Task Force on Agriculture Policy and Obesity Prevention to evaluate the evidence on the relationship between agriculture policies and the American diet, and to develop recommendations for policy options and future policy-related research, specifically on the impact of farm subsidies and the management of commodities on food prices, access, affordability, and consumption;
• Congress and the Administration establishing a process by which federal food, agriculture, and health officials would review and report on the possible implications of U.S. agriculture policy for obesity prevention to ensure that this issue will be fully taken into account when policy makers consider the Farm Bill;
• Congress and the U.S. Department of Agriculture (USDA) developing policy options for promoting increased domestic production of foods recommended for a healthy diet that are generally underconsumed, including fruits and vegetables and dairy products, by reviewing incentives and disincentives that exist in current policy;
• as part of its agricultural research agenda, USDA exploring the optimal mix of crops and farming methods for meeting the current Dietary Guidelines for Americans, including an examination of the possible impact of smaller-scale agriculture, of regional agricultural product distribution chains, and of various agricultural models from small to large scale, as well as other efforts to ensure a sustainable, sufficient, and affordable supply of fresh fruits and vegetables; and
• Congress and the Administration ensuring that there is adequate public funding for agricultural research and extension so that the research agenda can include a greater focus on supporting the production of foods Americans need to consume in greater quantities according to the Dietary Guidelines for Americans.
The 2010 Dietary Guidelines for Americans provide science-based recommendations that Americans aim to maintain energy balance so as to achieve and sustain a healthy weight; emphasize nutrient-dense foods and beverages in their diets; and reduce their intake of excess calories, such as those attributable to added sugars and solid fats (as described in Appendix B) (HHS/USDA, 2010). To achieve these dietary goals, the guidelines identify specific foods to increase and others to reduce (Box 6-1).
Among the consumer behaviors that the Dietary Guidelines suggest to help Americans achieve these goals are to (HHS/USDA, 2010)
• consume foods and drinks to meet, not exceed, calorie needs;
• limit calorie intake from solid fats and added sugars;
• increase intake of fruits, vegetables, and whole grains;
• increase intake of fat-free or low-fat milk and milk products and replace higher-fat milk and milk products with lower-fat options;
• choose water, fat-free milk, 100 percent fruit juice, or unsweetened tea or coffee as drinks instead of sugar-sweetened beverages;
• choose a variety of foods from protein sources;
• consume fewer foods and beverages high in solid fats, added sugars (including sugar-sweetened beverages), and sodium;
• reduce intake of refined grains;
• reduce portion sizes; and
• cook and eat more meals at home rather than eating out and, when eating out, consider choosing healthier options.
Nutrients that the Dietary Guidelines direct Americans to reduce, such as trans and saturated fatty acids, sodium, and added sugars, are often added to foods during processing. Processing also may result in an increase in caloric density and the removal of beneficial nutrients, such as fiber (Ludwig, 2011). While processing of many foods in this way is intended in part to increase their palatability, some have suggested that it has unintended consequences, in that some of the biological mechanisms that help us monitor and control the consumption of calories are bypassed. The result is said to be an “addictive consumption” of food that leads to dependence, with physiological symptoms upon withdrawal (Blumenthal and Gold, 2010; Garber and Lustig, 2011; Gearhardt et al., 2011; Ifland et al., 2009; Lenoir et al., 2007). While this line of reasoning is speculative, it is likely that
BOX 6-1
Dietary Guidelines Recommendations for Foods to Increase and to Reduce
Foods and Nutrients to Increase
• Increase vegetable and fruit intake.
• Eat a variety of vegetables, especially dark-green and red and orange vegetables and beans and peas.
• Consume at least half of all grains as whole grains. Increase whole-grain intake by replacing refined grains with whole grains.
• Increase intake of fat-free or low-fat milk and milk products, such as milk, yogurt, cheese, or fortified soy beverages.
• Choose a variety of protein foods, which include seafood, lean meat and poultry, eggs, beans and peas, soy products, and unsalted nuts and seeds.
• Increase the amount and variety of seafood consumed by choosing seafood in place of some meat and poultry.
• Replace protein foods that are higher in solid fats* with choices that are lower in solid fats and calories and/or are sources of oils.
• Use oils to replace solid fats* where possible.
• Choose foods that provide more potassium, dietary fiber, calcium, and vitamin D, which are nutrients of concern in American diets. These foods include vegetables, fruits, whole grains, and milk and milk products.
![]()
*Fats with a high content of saturated and/or trans fatty acids, which are usually solid at room temperature. Common examples of solid fats include butter, beef fat, lard, shortening, coconut oil, palm oil, and milk fat, which is solid at room temperature but is suspended in fluid milk by homogenization (HHS/UDSA, 2010).
Foods to Reduce
• Reduce daily sodium intake to less than 2,300 milligrams (mg) and further reduce intake to 1,500 mg among persons who are 51 and older and those of any age who are black or have hypertension, diabetes, or chronic kidney disease. The 1,500 mg recommendation applies to about half of the U.S. population, including children and the majority of adults.
• Consume less than 10 percent of calories from saturated fatty acids by replacing them with monounsaturated and polyunsaturated fatty acids.
• Consume less than 300 mg per day of dietary cholesterol.
• Keep trans fatty acid consumption as low as possible by limiting foods that contain synthetic sources of trans fats, such as partially hydrogenated oils, and by limiting other solid fats.
• Reduce the intake of calories from solid fats and added sugars.
• Limit the consumption of foods that contain refined grains, especially refined grain foods that contain solid fats, added sugars, and sodium.
• If alcohol is consumed, it should be consumed in moderation—up to one drink per day for women and two drinks per day for men—and only by adults of legal drinking age.
SOURCE: HHS/USDA, 2010.
reductions in the degree of processing would result in diets more likely to meet the Dietary Guidelines.
At present, solid fats and added sugars represent approximately 35 percent of calories consumed by Americans—children, adolescents, adults, and older adults, and both males and females—and contribute significantly to excess calorie intake without contributing significantly to overall nutrient adequacy. In an eating pattern within calorie limits, calories from solid fats and added sugars are more likely to contribute to weight gain than calories from other food sources. Furthermore, as solid fats and added sugars increase in the diet, it becomes difficult for individuals to meet nutrient needs while staying within calorie limits. Most Americans can accommodate only 5-15 percent of calories from solid fats and added sugars in an eating pattern that meets nutrient needs within calorie limits (USDA/HHS, 2010).
The amount of calories consumed should vary based on a person’s age, sex, and physical activity level (see Chapter 5 for recommendations related to physical activity). Table 6-1 summarizes estimated daily calorie needs by age, sex, and activity level. Most Americans consume too many calories on a daily basis given their age, sex, and activity level, and the calories they consume are often high in added sugars and solid fats rather than the items recommended by the Dietary Guidelines (Figure 6-1).
Governments and decision makers in the business community/private sector6 should make a concerted effort to reduce unhealthy food and beverage options7 and substantially increase healthier food and beverage options at affordable, competitive prices.
Food and beverage environments are one of the five critical areas for accelerating progress in obesity prevention identified by the committee (Figure 6-2). Increasing access to healthy food and beverage options and decreasing consumption of solid fats and added sugars are important steps toward achieving energy
![]()
6 The business community/private sector includes private employers and privately owned and/or operated locations frequented by the public, such as movie theaters, shopping centers, sporting and entertainment venues, bowling alleys, and other recreational/entertainment facilities.
7 Although there is no consensus on the definition of “unhealthy” foods/beverages, the term refers in this report to foods and beverages that are calorie-dense and low in naturally occurring nutrients. Such foods and beverages contribute little fiber and few essential nutrients and phytochemicals, but contain added fats, sweeteners, sodium, and other ingredients. Unhealthy foods and beverages displace the consumption of foods recommended in the Dietary Guidelines for Americans and may lead to the development of obesity.
TABLE 6-1 Estimated Calorie Needs per Day by Age, Sex, and Physical Activity Levela
| Physical Activity Levelb | |||||
| Sex | Age (years) | Sedentary | Moderately Active | Active | |
| Child (female and male) | 2-3 | 1,000-1,200c | 1,000-1,400c | 1,000-1,400c | |
| Femaled | 4-8 | 1,200-1,400 | 1,400-1,600 | 1,400-1,800 | |
| 9-13 | 1,400-1,600 | 1,600-2,000 | 1,800-2,200 | ||
| 14-18 | 1,800 | 2,000 | 2,400 | ||
| 19-30 | 1,800-2,000 | 2,000-2,200 | 2,400 | ||
| 31-50 | 1,800 | 2,000 | 2,200 | ||
| 51+ | 1,600 | 1,800 | 2,000-2,200 | ||
| Male | 4-8 | 1,200-1,400 | 1,400-1,600 | 1,600-2,000 | |
| 9-13 | 1,600-2,000 | 1,800-2,200 | 2,000-2,600 | ||
| 14-18 | 2,000-2,400 | 2,400-2,800 | 2,800-3,200 | ||
| 19-30 | 2,400-2,600 | 2,600-2,800 | 3,000 | ||
| 31-50 | 2,200-2,400 | 2,400-2,600 | 2,800-3,000 | ||
| 51+ | 2,000-2,200 | 2,200-2,400 | 2,400-2,800 | ||
NOTE: Estimates are rounded to the nearest 200 calories. An individual’s calorie needs may be higher or lower than these average estimates.
aBased on estimated energy requirement (EER) equations, using reference heights (average) and reference weights (healthy) for each age/gender group. For children and adolescents, reference height and weight vary. For adults, the reference man is 5 feet, 10 inches tall and weighs 154 pounds. The reference woman is 5 feet, 4 inches tall and weighs 126 pounds. EER equations are from IOM (2002).
bSedentary means a lifestyle that includes only the light physical activity associated with typical day-to-day life. Moderately active means a lifestyle that includes physical activity equivalent to walking about 1.5 to 3 miles per day at 3 to 4 miles per hour, in addition to the light physical activity associated with typical day-to-day life. Active means a lifestyle that includes physical activity equivalent to walking more than 3 miles per day at 3 to 4 miles per hour, in addition to the light physical activity associated with typical day-to-day life.
cThe calorie ranges shown are to accommodate needs of different ages within the group. For children and adolescents, more calories are needed at older ages. For adults, fewer calories are needed at older ages.
dEstimates for females do not include women who are pregnant or breastfeeding.
SOURCE: HHS/USDA, 2010.
balance when implemented together with adequate levels of physical activity (Chapter 5). The eating patterns of Americans cannot be changed in isolation. Major changes in the nation’s food system and food and eating environments have occurred in recent decades, driven by technological advances; U.S. food and agriculture policies; population growth; and economic, social, and lifestyle changes (Story et al., 2008). Food now is readily available and accessible in many settings throughout the day. The current U.S. food supply contains a large amount
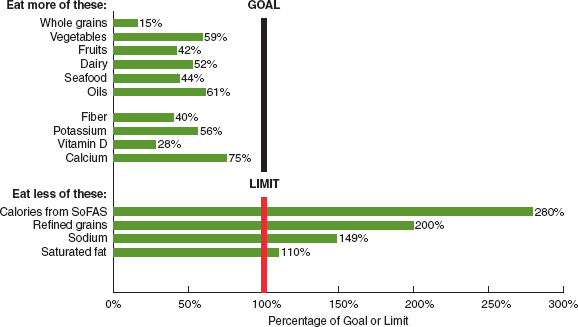
FIGURE 6-1 Comparison of typical American diets with Dietary Guidelines for Americans.
NOTE: SoFAS = solid fats and added sugars.
SOURCE: HHS/USDA, 2010.
of energy-dense foods, many of which consist of refined grains and foods high in fats and/or sugars and low in nutrients. Many of these foods are often available in increasingly large portion sizes at relatively low prices (Story et al., 2008). Americans also are eating out more often and consuming more calories away from home than ever before (Keystone Forum, 2006), and families are eating fewer meals together (Neumark-Sztainer et al., 2003). In addition, the school food environment is radically different than it was a few decades ago, with many schools now offering and promoting high-calorie, low-nutrition foods throughout the school day (Fox et al., 2009). Food marketing aimed at children using multiple channels, such as digital media, has increased dramatically as well (RWJF, 2011). Finally, an exodus of grocery stores and an influx of fast-food restaurants in lower-income urban areas have contributed to income and racial/ethnic disparities in access to healthier foods (IOM, 2005). Together, these environmental changes have influenced what, where, and how much Americans eat and have played a large role in the current obesity epidemic (IOM, 2009).
To change American’s eating patterns, a sustained, systematic and comprehensive approach is required that empowers consumers to make healthy choices;
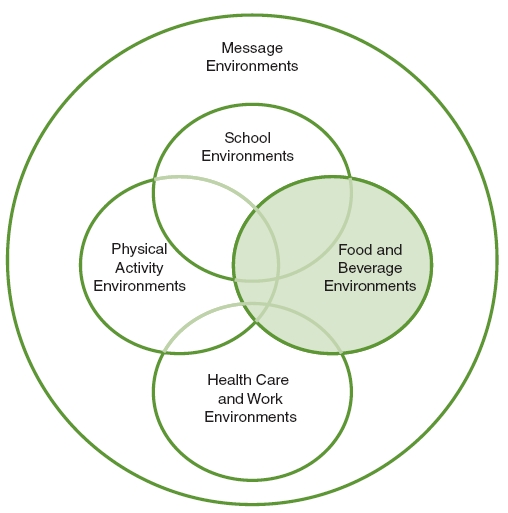
FIGURE 6-2 Five areas of focus of the Committee on Accelerating Progress in Obesity Prevention.
NOTE: The area addressed in this chapter is highlighted.
that gives them a variety of affordable, healthy options from which to choose; that promotes consistent messages about the importance of healthy eating in concert with daily physical activity; that makes healthy food options readily available and accessible; and that cuts across all sectors of society—from government, to schools, to restaurants and privately run places of public access, to health care settings, to farming. Absent a multifaceted approach, the nation will be no better off in 2022 than it is in 2012. The time for change is now. The committee recommends making the healthy option the routine, readily available, and affordable option and provides five strategies and potential actions for implementing this recommendation. These strategies and actions are detailed in the remainder of this chapter. Indicators for measuring progress toward the implementation of
each strategy, organized according to the scheme presented in Chapter 4 (primary, process, foundational) are presented in a box following the discussion of each strategy.
STRATEGIES AND ACTIONS FOR IMPLEMENTATION
Decision makers in the business community/private sector, in nongovernmental organizations, and at all levels of government should adopt comprehensive strategies to reduce overconsumption of sugar-sweetened beverages.8
For schools and other locations where children and adolescents are cared for, potential actions include
• prohibiting access to sugar-sweetened beverages;
• providing a variety of beverage options that are competitively priced and are recommended by and included in the Dietary Guidelines for Americans; and
• making clean, potable water available.
For the business community/private sector, nongovernmental organizations, and governments, potential actions include
• making clean, potable water readily available in public places, worksites, and recreation areas;
• making a variety of beverage options that are competitively priced readily available in public places, worksites, and recreation areas;
• implementing fiscal policies aimed at reducing overconsumption of sugar-sweetened beverages through (1) pricing and other incentives to make healthier beverage options recommended by the Dietary Guidelines for Americans more affordable and, for governments, (2) substantial and specific excise taxes on sugar-sweetened beverages (e.g., cents per ounce of
![]()
8 Sugar-sweetened beverages are defined to include all beverages containing added caloric sweeteners, including, but not limited to, sugar- or otherwise calorically sweetened regular sodas, less than 100 percent fruit drinks, energy drinks, sports drinks, and ready-to-drink teas and coffees.
liquid, cents per teaspoon of added sugar), with the revenues being dedicated to obesity prevention programs;
• supporting the work of community groups and coalitions to educate the public about the risks associated with overconsumption of sugar-sweetened beverages; and
• developing social marketing campaigns aimed at reducing overconsumption of sugar-sweetened beverages.
For the food and beverage industry, potential actions include
• developing and promoting a variety of beverage options for consumers, including a range of healthy beverage options, beverages with reduced sugar content, and smaller portion sizes (e.g., 8-ounce containers).
For health care providers such as physicians, dentists, registered dietitians, and nurses, potential actions include
• performing routine screening regarding overconsumption of sugar-sweetened beverages and counseling on the health risks associated with consumption of these beverages.
Context
Consumption of sugar-sweetened beverages is the single largest contributor of calories and added sugars to the American diet (HHS/USDA, 2010; NCI, 2010b; Welsh et al., 2011). Such beverages also displace healthier, more nutrient-dense beverages such as milk, 100 percent fruit juice, and water (Woodward-Lopez et al., 2010).
According to National Health and Nutrition Examination Survey (NHANES) 2005-2006 dietary intake data, sugar-sweetened beverages represent the largest share of calories in the diets of all individuals aged 2 and above9—more calories than are contributed by any other food category, including grain-based desserts, yeast breads, and chicken and chicken mixed dishes. Using the same NHANES data, Reedy and Krebs-Smith (2010) show that for children and adolescents aged
![]()
9 This figure is calculated by summing all persons’ mean intake of energy (in kilocalories) from two categories—soda/energy/sports drinks (114 kcal) and fruit drinks (36 kcal)—to obtain 150 kcal, which is a higher proportion of total calories than that represented by any other food group. This is likely a conservative estimate, because it does not include calories from other sugar-sweetened beverages, such as sweetened, ready-to-drink teas and coffee drinks (NCI, 2010b).
2-18, sugar-sweetened beverages were the largest contributor—22 percent—to empty calorie intake (that is, calories from solid fat and added sugars).
On a given day, one-half of the U.S. population aged 2 and older consumes sugared drinks (excluding ready-to-drink sugar-sweetened teas and coffees) (Ogden et al., 2011). According to NHANES data for 2005-2008, 25 percent of Americans drink more than one sugared drink daily (200 kcal/day), 20 percent consume one to four such drinks a day (200-566 kcal/day), and 5 percent drink more than four such drinks daily (567 kcal/day) (Ogden et al., 2011).
Consumption of sugar-sweetened beverages is not limited to particular segments of the U.S. population, although certain groups are more likely to consume them than others. According to Ogden and colleagues (2011), males are more likely than females to consume sugared drinks, with males aged 2-19 most likely to do so (70 percent) on a given day and females aged 20 and older least likely to do so (40 percent). At the same time, sugared drinks represent a greater percentage of daily caloric intake for certain racial/ethnic groups (Ogden et al., 2011). Sugared drink consumption represents 8.5 percent of total daily kilocalories for non-Hispanic black children and adolescents aged 2-19 as compared with 7.7 percent and 7.4 percent of total daily kilocalories for non-Hispanic whites and Mexican American children and adolescents, respectively (Ogden et al., 2011). For Americans aged 20 and over, the racial/ethnic disparity in sugared drink consumption is even greater—8.6 percent of total daily kilocalories consumed by non-Hispanic blacks were from sugared drinks as compared with 5.3 and 8.2 percent for non-Hispanic whites and Mexican Americans aged 20 and over, respectively (Ogden et al., 2011). Consumption of sugared drinks also is lower among higher-income than lower-income persons, with such differences being particularly noticeable among adults aged 20 and over (Ogden et al., 2011).
Of particular concern are the added sugars attributable to excess consumption of sugar-sweetened beverages overall. According to NHANES 2005-2006 dietary intake data, sugar-sweetened beverages are the largest contributor to added sugars in the diets of all individuals aged 2 and above.10 While added sugar intake has declined for Americans aged 2 and older, largely because of reduced consumption of regular sodas, added sugar intakes continue to exceed dietary recommendations, and rates of consumption of energy drinks as a source of added sugars have increased significantly over the past decade (Welsh et al., 2011). If people are to
![]()
10 This figure is calculated by summing all persons’ mean intake of added sugars (in teaspoons) from two categories—soda/energy/sports drinks (35.7 tsp) and fruit drinks (10.5 tsp)—which yields a higher proportion of added sugars than that represented by any other food group (NCI, 2010a).
meet the Dietary Guidelines for Americans’ recommended food pattern/caloric intake for their age, sex, and activity level, they must minimize their intakes of all solid fats and added sugars. While the maximum recommended limits for solid fats and added sugars vary by age, sex, and level of physical activity, these limits are intended to reflect intakes of both solid fats and added sugars. Yet in most cases, more than half of the recommended calories from solid fats and added sugars being consumed are from sugared drinks; in many cases, more than two-thirds of the recommended calories from solid fats and added sugars are attributable to sugared drink consumption (Figure 6-3). In other words, Americans’ current rates of sugared drink consumption leave very little room in their diet for any additional solid fats and added sugars, and in some cases (e.g., males aged 6-8 and 12-13), they exceed the daily recommendations for solid fats and added sugars with their sugared drink consumption alone. As the Keystone Forum11 (2006) notes in its recommendations for preventing weight gain and obesity, several dietary factors contribute to the development of obesity (a detail that the Forum participants recognized), “and one of those factors is excess caloric intake. A decrease in caloric beverage consumption is just one of many necessary strategies in the effort to reduce obesity.”
Evidence
Despite the complexity of the etiology of obesity and the difficulty of quantifying relative contributions to the obesity epidemic, researchers have found strong associations between intake of sugar-sweetened beverages and weight gain. Although the exact mechanisms of how sugar-sweetened beverages contribute to obesity are not fully known, their link to obesity is stronger than that observed for any other food or beverage, as described in the 2010 Dietary Guidelines for Americans advisory report (DGAC, 2010). Woodward-Lopez and colleagues (2010) found that sugar-sweetened beverages account for at least 20 percent of the increases in weight in the United States from 1977 to 2007. Others have concluded that liquid calories supplied approximately half of the 150- to 300-calorie increase in daily energy intake observed over the past 30 years (Johnson et al., 2009), concomitant with no apparent change in physical activity (Briefel and Johnson, 2004; Nielsen et al., 2002). Additional evidence supporting the reduction of sugar-sweetened beverages in order to promote energy balance is predicated on evidence suggesting that liquid calories from sweet, energy-dense beverages are poorly compensated for by reduced
![]()
11 The Keystone Forum of the Keystone Center is a nonprofit public policy and dispute resolution organization that brought together participants from industry, government, civic organizations, and academia.
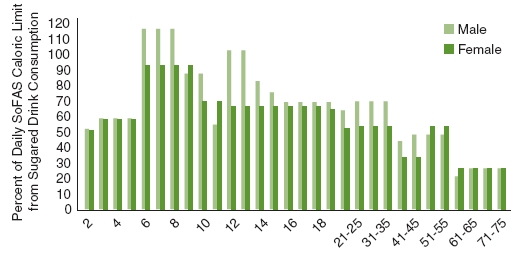
FIGURE 6-3 Percentage of daily caloric limit of solid fats and added sugars from sugared drink consumption for given ages, assuming moderate activity level.
NOTES: Moderate physical activity is defined as a lifestyle that includes physical activity equivalent to walking about 1.5-3 miles per day at 3-4 miles per hour, in addition to the light physical activity associated with typical day-to-day life (HHS/USDA, 2010, p. 78). The definition of sugared drinks is based on that used in Ogden et al. (2011) and Reedy and Krebs-Smith (2010). Sugared drinks include fruit drinks, sodas, energy drinks, sports drinks, and sweetened bottled waters. Sugared drinks in this analysis do not include sweetened teas or flavored milks, nor do they include 100 percent fruit juices or diet drinks. The percentage of daily limit of solid fats and added sugars attributable to sugared drinks was computed by dividing the average daily caloric intake of sugar drinks from Ogden et al. (2011) by the maximum calories from solid fats and added sugars for the given age/sex, assuming a moderate physical activity level, from the Dietary Guidelines for Americans (HHS/USDA, 2010). Note that some of the age categories do not directly correspond to the age categories reported in Ogden et al. (2011). In these cases, the calories were assigned based on the earlier year in the age range (e.g., 19-20 reflects the calories for 12- to 19-year-olds, whereas 21-25 reflects the calories for 20- to 39-year-olds from Ogden et al. [2011]).
SoFAS = solid fats and added sugars.
SOURCE: Computed based on Dietary Guidelines for Americans, Appendix 7 (HHS/USDA, 2010; Ogden et al., 2011).
dietary intake from other sources (Bellisle and Rolland-Cachera, 2001; DiMeglio and Mattes, 2000; Mattes, 1996; Popkin and Duffey, 2010).
The 2010 Dietary Guidelines Advisory Committee (DGAC) concluded that for adults, “limited evidence shows that intake of SSBs [sugar-sweetened beverages] is linked to higher energy intake … a moderate body of epidemiologic evidence suggests that greater consumption of SSBs is associated with increased body weight in adults, and a moderate body of evidence suggests that under isocaloric controlled
conditions, added sugars, including sugar-sweetened beverages, are no more likely to cause weight gain than any other source of energy” (DGAC, 2010, p. 301). The 2010 DGAC found a more robust link between sugar-sweetened beverages and childhood adiposity, concluding that “strong evidence supports the conclusion that greater intake of SSBs is associated with increased adiposity in children.” The DGAC recommended a “greatly reduced” intake of sugar-sweetened beverages to prevent excess weight among children, noting that consumption should also be discouraged because of the need to replace empty calories with nutrient-rich energy for optimal growth and development (DGAC, 2010, p. 12).
The contributions of the consumption of sugar-sweetened beverages to childhood obesity also will likely lead to greater future prevalence of adult obesity. The established habitual nature of consumption of these beverages suggests that their consumption is likely to persist into adulthood, further increasing the risk for obesity (Popkin and Duffey, 2010).
Because 100 percent fruit juice is suggested as an alternative to sugar-sweetened beverages and there may be concern that its calorie content will promote obesity, the committee cites the DGAC report, which states: “limited and inconsistent evidence suggests that for most children, intake of 100 percent fruit juice is not associated with increased adiposity when consumed in amounts that are appropriate for age and energy needs of the child.” The report also notes, however, that intake of 100 percent fruit juice has been prospectively associated with increased adiposity in children who are overweight or obese (DGAC, 2010). Furthermore, the report explains that although 100 percent fruit juice provides nutrients and can be part of a healthy diet when consumed in moderation,12 it lacks dietary fiber and can contribute extra calories when consumed in excess; thus, the majority of fruit servings should come from whole fruits.
Implementation
Recognizing the trends described above, a number of prior Institute of Medicine (IOM) committees have recommended strategies aimed at reducing consumption of and exposure to sugar-sweetened beverages, as well as encouraging consumption of healthier beverages. Nutrition Standards for Foods in Schools: Leading the Way Toward Healthier Youth (IOM, 2007a) recommends that beverages provide no more than 35 percent of calories from total sugars per packaged portion, with the
![]()
12 The American Academy of Pediatrics (AAP) recommends not introducing 100 percent fruit juice into the diet before 6 months of age, and recommends daily upper limits of 4-6 ounces for children aged 1-6 and 8-12 ounces for older children, up to age 18 (AAP Committee on Nutrition, 2001).
exception of 100 percent fruit juices and 100 percent vegetable juices without added sugars and unflavored nonfat and lowfat milk. The same report also recommends that sports drinks be available in schools only for student-athletes participating in vigorous-intensity sports for at least 1 hour. Likewise, the IOM (2009) has recommended that local governments ensure that publicly run entities promote healthy beverages. It has also recommended that restaurants promote healthier options, such as by serving nonfat milk instead of soda in children’s meals (IOM, 2006b, 2009); that food, beverage, restaurant, retail, and marketing industry trade associations improve the availability and selection of healthful beverages accessible at eye level and reach in grocery stores and retail environments (IOM, 2006b); that the media promote healthful beverages (IOM, 2006b); that industry shift product portfolios and advertising and marketing emphasis toward beverages substantially lower in total calories and added sugars and higher in nutrient content (IOM, 2006b); and that caregivers of young children (birth to 4 years) build skills to foster the selection of healthful beverages (IOM, 2006b).
Likewise, a number of medical, public health, scientific, policy-making, nonprofit, and consensus-building bodies have specifically identified reduced consumption of sugar-sweetened beverages and/or excess caloric intake associated with such consumption as key issues requiring a societal response that involves not only governments but also, just as important, schools, industry, food service providers, and medical care providers. The Dietary Guidelines for Americans (HHS/USDA, 2010), the American Academy of Pediatrics in association with the American Heart Association (Gidding et al., 2006), and the American Medical Association (AMA, 2007) all recommend reducing intake of sugar-sweetened beverages because they are the leading contributor to excess sugar consumption in the American diet. And the Centers for Disease Control and Prevention (CDC) (2010) has identified seven recommended strategies for reducing consumption of sugar-sweetened beverages that are aligned with actions outlined above by the committee. The following discussion briefly summarizes the evidence, positions, and, where available, implementation experiences related to the overall strategy of reducing consumption of sugar-sweetened beverages.
Access to sugar-sweetened beverages in public places and schools The U.S. Surgeon General (2010), the Department of Health and Human Services (National Prevention Council, 2011), the National Governors Association (Mulheron and Vonasek, 2009), the National Association of Local Boards of Health (2010), CDC (Khan et al., 2009), the Alliance for a Healthier Generation (2006), the American
Dental Association (2005), and the American Academy of Pediatric Dentistry (AAPD, 2010) all recommend a range of strategies for reducing consumption of sugar-sweetened beverages. These strategies include eliminating or restricting access to sugar-sweetened beverages, including those sold through vending machines and in schools, child care/early learning centers, and other government facilities and public places and increasing access to healthier options, such as bottled water and non- or low-fat milk. Likewise, given the wide availability of sugar-sweetened beverages in workplaces, schools, recreation facilities, entertainment venues, and other places frequented by the public, a number of organizations have recognized the need to ensure that Americans have sufficient alternatives to such beverages available, and have identified specific strategies to that end. The Keystone Forum (2006, p. 11) specifically called upon food service providers to “develop, make available, and promote beverage options that help consumers to reduce caloric intake,” including through smaller portion sizes and a range of low-calorie13 and zero-calorie beverage choices, increased selections of low-fat and nonfat milk beverages, and pricing strategies that make smaller sizes and lower-calorie options more appealing. Although the beverage industry has sold sugar-sweetened beverages with smaller portion sizes (e.g., 7.5 ounce cans) for some time, they are not priced favorably (CSPI, 2010), nor are they marketed to encourage consumers to choose them in lieu of the larger options (e.g., 12 ounce cans, 20 ounce bottles).
Given the relationship between consumption of sugar-sweetened beverages and child and adolescent overweight and obesity, most policy interventions to date have focused on the elementary and, to a lesser extent, secondary school environments. In 2006, the Alliance for a Healthier Generation (an alliance between the William J. Clinton Foundation and the American Heart Association) brokered an agreement with three major beverage firms to limit access to sugar-sweetened beverages in schools. The resulting School Beverage Guidelines limit portion sizes of and set standards for the calorie and nutrient content of beverages sold in schools; the restrictions are tighter in elementary and middle schools than in high schools. An industry report following implementation of the guidelines indicated an 88 percent reduction in beverage calories shipped to schools by the middle of the 2009-2010 school year (ABA, 2010). Independent researchers reported that based on a nationally representative mail-back survey, high-calorie beverages and beverages not allowed by national guidelines were still available in
![]()
13 Because its charge was to focus specifically on strategies for accelerating progress in obesity prevention, the committee did not deliberate on the effects of low-calorie, artificially sweetened beverages on population health and did not take a position on this issue.
elementary schools during the 2008-2009 school year. They noted that beverages in schools may be obtained from school stores or vending machines that are outside of formal contracts with beverage suppliers (Turner and Chaloupka, 2010). Additionally, concern has been expressed about the less restrictive guidelines for high schools, where intake of sugar-sweetened beverages occurs more frequently than in other schools; about the lack of nonindustry evaluation funding; and about the fact that the guidelines fail to address other beverages, such as calorie-dense sports drinks, diet drinks (for which brand marketing continues to be offered), and new drink categories such as energy drinks (Sharma et al., 2010).
Levy and colleagues (2011) reviewed the literature on school nutrition policies directed at consumption of sugar-sweetened beverages by children and adolescents, finding that policies limiting the availability of such beverages and improving food offerings in school lunches generally have been associated with reduced consumption of these beverages. In middle schools, restricting access can reduce the percentage of students consuming sugar-sweetened beverages by 25 percent and the energy they consume by 30 percent. In high schools, 30 percent reductions in energy intake were observed among student buyers of sugar-sweetened beverages when access policies were in place.
Briefel and colleagues (2009a,b), Levy and colleagues (2011), and Taber and colleagues (2011) conclude that restrictions on in-school access to sugar-sweetened beverages reduce in-school consumption, and that reduced intake of such beverages in schools is unlikely to be offset by increased consumption outside of schools. Recent experience in Boston public schools confirms that students do not compensate for reduced access to sugar-sweetened beverages by buying those beverages outside of school (Cradock et al., 2011) (see Box 6-2).
Access to water Recognizing that if governments, employers, schools, public places, and other locations encouraged reduced consumption of sugar-sweetened beverages, consumers would need alternative options readily available, the IOM (2007a, 2009), the National Association of County and City Health Officials (NACCHO, 2010), the Department of Health and Human Services (HHS/USDA, 2010), and CDC (Khan et al., 2009) all recommend increasing the availability of safe, free drinking water and healthier beverages such as non-fat/low-fat milk and 100 percent juices in schools and other places where beverages are sold and served. Increasing water intake may help limit excess weight gain among children, adolescents, and adults (Daniels and Popkin, 2010; Dennis et al., 2010; Stookey et al., 2007, 2008). Replacing sugar-sweetened beverages with water is associated
with reductions in total energy intake for children and adolescents (Wang et al., 2009), and installing water fountains in public places and facilities can increase water intake and prevent and reduce overweight and obesity (Muckelbauer et al., 2009). The Healthy, Hunger-Free Kids Act of 201014 requires schools participating in federally funded child nutrition programs to make water available during meal periods at no cost to students, and mandates that child care facilities provide free water throughout the day. After a survey revealed that 40 percent of responding California school districts reported lack of access to free drinking water in cafeterias for students, a state law was implemented requiring schools to make free, fresh drinking water available during meals (California Food Policy Advocates, 2011).
Pricing strategies and fiscal policies At least three IOM committees have considered fiscal policies (taxes and incentives) to discourage consumption of unhealthy foods and beverages such as sugar-sweetened beverages or encourage consumption of healthier alternatives. Two committees (IOM, 2005, 2006b) concluded that evidence was insufficient to draw a definite conclusion or develop a strong recommendation either for or against imposing a tax on less healthful foods. In 2009, however, the IOM recommended that local governments “implement fiscal policies and local ordinances to discourage the consumption of calorie-dense, nutrient poor foods and beverages (e.g., taxes, incentives, land use and zoning regulations)” (IOM, 2009, p. 62). That committee highlighted “implement[ing] a tax strategy to discourage consumption of foods and beverages of minimal nutritional value, such as sugar-sweetened beverages” as an action with considerable promise, noting the growing interest in and broad reach of such a strategy (IOM, 2009, p. 63). One of the earlier IOM committees recommended that governments consider incentives, including tax incentives, to encourage and reward food, beverage, and restaurant companies that develop, provide, and promote healthier beverages for children and adolescents in the settings in which they typically consume beverages (IOM, 2006b). Likewise, the 2009 IOM report recommends creating incentive programs to enable small food store owners in underserved areas to carry healthier, affordable food items. That report also recommends offering incentives or subsidies to government programs and localities that provide healthy foods at competitive prices and limit calorie-dense, nutrient-poor foods.
Non-IOM reports also have recommended fiscal policies to discourage consumption of less healthy foods and beverages and encourage consumption of
![]()
14 Public Law 111-296, 111th Cong., 2d sess. (December 13, 2010), 124, 3183.
BOX 6-2
Case Study of the Impact of Boston Public Schools’ Policy on Consumption of Sugar-Sweetened Beverages
Boston Public Schools instituted a policy in 2004 restricting the sale of sugar-sweetened beverages (soft drinks, non-100 percent fruit and vegetable juices, and sports drinks) anywhere in school buildings or campuses. Concurrent activities included the introduction of nutrition-related curricula in elementary and middle schools, presentation of the policy to school administrators, and negotiation of new vending contracts to provide more healthful beverage options. Two years later, more than 2,000 students were surveyed to determine whether consumption of sugar-sweetened beverages declined after the policy was implemented (Cradock et al., 2011). The student body is diverse (37 percent black, 39 percent Hispanic, 13 percent white, and 9 percent Asian), and almost three-quarters of the students are eligible for free or reduced-price meals. On average, students reported consuming 1.71 servings of sugar-sweetened beverages in 2004 and 1.38 servings in 2006; servings of soda (–0.16), other sugar-sweetened beverages (–0.14), and total sugar-sweetened beverages (–0.30) declined during that period. The percentage of students reporting no consumption of these beverages rose from 4.5 percent in 2004 to 9.8 percent in 2006. During the same time (2004-2006), national data from the National Health and Nutrition Examination Survey showed no significant changes in adolescent consumption of sugar-sweetened beverages, ruling out the possibility that consumption decreased in general during this time. The study authors concluded that students did not compensate for reduced school access to sugar-sweetened beverages by buying
healthier alternatives. The California Legislature Task Force on Diabetes and Obesity (Greenwood et al., 2009) has recommended creating tax incentive programs to encourage employers to adopt workplace policies that make healthy eating easier for employees, as well as offering incentives to mobile carts within one-half mile of school campuses to offer healthy and restrict unhealthy foods. The Robert Wood Johnson Foundation Action Strategies Toolkit for state and local leaders (RWJF, 2009) encourages state and local policy makers, through financial or other incentives, to motivate restaurants to provide price reductions for healthier foods, and convenience stores and bodegas to provide affordable healthy
those beverages elsewhere, and that restricting their sale in schools may be a promising strategy for reducing unnecessary energy intake among adolescents.
This case study illustrates policies restricting access to sugar-sweetened beverages in schools coinciding with reductions in consumption of these beverages. Given that these beverages are a leading sources of calories in the diets of Americans aged 2-18,* this case study is illustrative of the potential impact of this implementation action for Strategy 2-1. The investigators did not examine sales or beverage substitution behaviors because these outcomes were beyond the scope of the study, which focused exclusively on sugar-sweetened beverage consumption patterns.
SOURCE: Cradock et al., 2011.
![]()
*This figure is calculated by summing 2- to 18-year-olds’ mean intake of energy (in kilocalories) from two categories—soda/energy/sports drinks (118 kcal) and fruit drinks (55 kcal)—to obtain 173 kcal, which is a higher proportion of total calories than that represented by any other food group for this age subgroup. Available http://riskfactor.cancer.gov/diet/foodsources/energy/table1b.html (accessed December 19, 2011).
options. CDC (Khan et al., 2009) has recommended that communities provide incentives for food retailers to locate in underserved areas and offer healthy food and beverage choices. CDC also has issued a series of strategies for reducing consumption of sugar-sweetened beverages. Finally, the White House Task Force on Childhood Obesity (2010) has recommended an analysis of the effect of state and local taxes on less healthy, energy-dense foods.
While available research on existing small sales taxes (ranging from 1.0 to 7.25 percent) (Bridging the Gap Program, 2011) finds little or no impact on consumption, body mass index (BMI), or obesity rates (Finkelstein et al., 2010; Kim
and Kawachi, 2006; Powell and Chriqui, 2011; Powell et al., 2009; Sturm et al., 2010), many believe that more sizable, nontrivial pricing interventions could have measurable effects on weight outcomes, particularly for children and adolescents, populations of low socioeconomic status, and those most at risk for overweight (Finkelstein et al., 2010; Powell and Chaloupka, 2009; Powell et al., 2009; Sturm et al., 2010). Although a number of state and local governments recently have attempted to enact sizable taxes on sugar-sweetened beverages (on the order of 1 cent per liquid ounce) (Rudd Center for Food Policy and Obesity, 2011), none have succeeded in doing so to date. The rationale for these proposals is grounded largely in the considerable body of evidence for the impact of food pricing on weight outcomes and in an emerging literature that examines the impact of taxes or price increases (amounting to a 10-20 percent price increase) on consumption of sugar-sweetened beverages and weight outcomes. Note that estimates of the impact of a tax on sugar-sweetened beverages will likely vary because of the length of the causal pathway between prices of these beverages and weight outcomes and the complexity of the variables involved in this pathway.
The effectiveness of a tax on sugar-sweetened beverages depends in part on the degree to which consumers change their food and beverage purchasing and consumption behavior in response to higher sugar-sweetened beverages prices (price elasticity). In a review that includes studies based on large survey data sets, Andreyeva and colleagues (2010) show that food consumption or expenditure is generally price sensitive. Smith and colleagues (2010) estimate that a 10 percent price increase for sweetened beverages would reduce grocery store purchases of these items by 12.6 percent, and also note that when taxes are large, estimated elasticities may underestimate actual consumer reactions. Another study (Wendt and Todd, 2011) reports that inflation-adjusted prices for carbonated drinks have fallen over the past 30 years and that responses to changes in price vary, particularly across income levels and BMI range. In the past, 10 percent higher prices for carbonated beverages were associated with a decrease in the average child’s BMI. The effect was significant for boys but not for girls. The effect also was greater for children in households with income below 200 percent of the federal poverty level, a finding that is not surprising because economic theory suggests that lower-income households are more price-responsive than their higher-income counterparts. The effect was larger for children with lower BMI, perhaps because these children are less likely to substitute caloric drinks (such as juice) (see the discussion below) or because their preferences for carbonated beverages are less entrenched, so their price sensitivity for these beverages is higher. Notwithstanding
available estimates, Smith and colleagues (2010) conclude that the literature lacks the demand elasticity estimates needed to fully examine the effect of a tax on sugar-sweetened beverages in practice.
A number of studies have predicted the effect of sizable taxes and/or price increases on consumption of sugar-sweetened beverages. According to one recent estimate, a 10 percent price increase for soft drinks would reduce their consumption by 8-10 percent (Andreyeva et al., 2010). Another analysis indicates that a penny-per-ounce tax would reduce per capita consumption of sugar-sweetened beverages by 24 percent and could reduce per capita calorie intake from such beverages by about 50 calories/day (approximately 5 pounds/year), assuming no substitution of other caloric beverages or foods (Andreyeva et al., 2011). Some of these same studies suggest that a 20 percent increase in the price of sugar-sweetened beverages or a penny-per-ounce tax could significantly reduce per capita calorie intake, translating to a reduction in body weight ranging from approximately 1.5 to 5.0 pounds a year, assuming no substitution of other caloric beverages (Andreyeva et al., 2011; Dharmasena and Capps, 2011; Smith et al., 2010). Chaloupka and colleagues (2011b) modeled a penny-per-ounce tax on sugar-sweetened beverages in the state of Illinois, showing that the frequency of consumption of such beverages (≥2 times/day) would fall sharply as a result of the tax. They estimated an overall 23.5 percent drop in consumption of sugar-sweetened beverages and an average weight reduction of 1.7 pounds annually based on the assumption that half of the calorie deficit from reduced consumption of such beverages would be offset by increases in energy intake from other sources. Wang and colleagues (2012) estimated that a penny-per-ounce sugar-sweetened beverages tax would reduce sugar-sweetened beverages consumption by 15 percent among adults aged 25-64, after factoring in the assumption that 40 percent of the calorie deficit from reduced sugar-sweetened beverages consumption would be compensated for by consumption of other caloric beverages (such as milk and juice) in equal measure. They also projected the sugar-sweetened beverages tax’s impact on downstream health benefits and medical costs savings over a 10-year period (2010-2020), finding that it could reduce new cases of type 2 diabetes by 2.6 percent and the prevalence of obesity by 1.5 percent. Over 10 years these reductions would result in 95,000 fewer coronary heart events, 8,000 fewer strokes, and 26,000 fewer premature deaths, avoiding more than $17 million in medical costs while generating approximately $13 billion in tax revenue.
The extent to which calories from nontaxed foods and caloric beverages are substituted for calories in taxed items is a key consideration when translating
tax-induced reductions in caloric intake into decreased body weight and obesity (Chaloupka et al., 2011b). The literature in this area is mixed. Fletcher and colleagues (2011b) maintain that substitution of other high-calorie drinks for soft drinks may blunt the effect of soft drink taxes on obesity; they cite the lack of evidence supporting the argument that if taxes are large enough, consumption of sugar-sweetened beverages will fall substantially. However, others have estimated only modest increases in calories from other caloric beverages and continue to observe a net caloric deficit when examining a hypothetical 20 percent price increase in sugar-sweetened beverages (Dharmasena and Capps, 2011; Smith et al., 2010). While those researching this topic agree almost universally that more research is needed, Fletcher and colleagues (2011a) point out that convincing evidence may not be available until a large tax is instituted in a state or locality. Despite the apparent lack of research examining substitution effects, analyses that examine weight outcomes are implicitly capturing the substitution that occurs, and a negative impact of taxing sugar-sweetened beverages on BMI and/or obesity prevalence indicates that full compensation from substitution of other calorie sources does not occur.
The committee considered the potential allegation that taxes on sugar-sweetened beverages are regressive, that is, that they would disproportionately affect low-income and minority consumers, who spend a larger proportion of their income on food than those with higher incomes and whites. Brownell and colleagues (2009) observe that taxes on such beverages may be most beneficial to the former populations because they are disproportionately affected by obesity, may consume more soft drinks than other populations, and may be more price sensitive—all supporting the argument that they may stand to benefit substantially from reduced consumption of sugar-sweetened beverages, especially if they are the focus of the obesity prevention programs funded by the taxes on these beverages. Furthermore, sugar-sweetened beverages are not an essential dietary component, and as explained above, hinder Americans from achieving dietary intakes aligned with the Dietary Guidelines for Americans. Finally, water, a no-cost alternative to sugar-sweetened beverages, is readily available (Brownell et al., 2009).
Even though predicted reductions in body weight resulting from a substantial tax on sugar-sweetened beverages may be relatively small or still must be tested in practice, the committee believes that fiscal policies such as incentivizing the purchase of healthier beverages or taxing sugar-sweetened beverages are one action that can be taken to reduce consumption of these beverages. The current evidence does not indicate that fiscal policies alone can solve the obesity problem. Rather, it
suggests that fiscal policies would act synergistically with other actions to reduce consumption of sugar-sweetened beverages, thereby advancing the achievement of a comprehensive obesity prevention strategy, particularly if the revenues from taxes on such beverages were directed toward obesity prevention programs, as recommended by the public health community (Brownell and Ludwig, 2011; Chaloupka et al., 2011a; Powell and Chriqui, 2011). The public also is more supportive of taxes on sugar-sweetened beverages if revenues will support activities to reduce obesity. A December 2008 poll found that 52 percent of New Yorkers supported a “soft drink tax,” and support increased to 72 percent when respondents were told the revenues would be earmarked to prevent obesity and to avoid service cuts in schools, health care, mass transit, or law enforcement (Citizens’ Committee for Children of New York, Inc., 2008). Likewise, a 2011 poll of 500 Massachusetts voters found that 69 percent would support a sales tax on soda if the revenues funded local schools or anti-obesity programs targeting children, but the sample was split nearly 50-50 if they were not told how the revenues would be used. The Rudd Center has compiled additional results from eight other polls demonstrating public support for a tax on sugar-sweetened beverages, particularly when the revenues would be earmarked for obesity prevention (Rudd Center for Food Policy and Obesity, 2010).
Social marketing campaigns Social marketing has been used to impact a variety of health and risk behaviors among children, adolescents, and adults. Because many health-based social marketing campaigns are insufficiently funded and not sustained over significant periods of time, assessing their effectiveness accurately is difficult (Randolph and Viswanath, 2004; Wakefield et al., 2010). However, evidence from carefully designed studies indicates that media campaigns can have a positive impact on health behaviors if they are carefully crafted, well tested, fully funded, highly targeted (in terms of audience and behavior), and sustained over a long period of time (Wakefield et al., 2010). Social marketing campaigns are discussed in greater detail in Chapter 7, under Strategy 3-1.
Social marketing campaigns aimed at reducing consumption of sugar-sweetened beverages are emerging rapidly and are encouraged by health professional organizations. For example, the American Academy of Pediatric Dentistry “encourages collaboration with other dental and medical organizations, governmental agencies, education officials, parent and consumer groups, and corporations to increase public awareness of the negative effects of frequent and/or inappropriate intake of sweetened drinks (carbonated and noncarbonated) and low nutrient dense snack
foods on infant, child, and adolescent oral health, nutrition, and general health” (AAPD, 2010, p. 56).
In 2011, a campaign titled “Life’s Sweeter with Fewer Sugary Drinks” debuted with the goal of decreasing average consumption of such drinks (regular soda, fruit drinks with less than 100 percent juice, sweetened teas, lemonade, energy drinks, and sports drinks) to approximately three cans per person per week by 2020 (CSPI, 2011). The campaign brings together health experts, civic organizations, youth groups, and others to meet this goal. It also encourages employers, hospitals, and government agencies to adopt policies designed to decrease soda consumption. The campaign has been embraced by the American Diabetes Association, the American Heart Association, the Center for Science in the Public Interest, and more than 100 local and national health organizations. At the same time, local and state governments from across the country—including Boston, New York City, Philadelphia, Seattle and King County, and the Rhode Island Department of Health, to name a few—have been developing and implementing social marketing campaigns aimed at reducing consumption of sugar-sweetened beverages.
Role of health care providers All health care providers should adopt standards of practice for prevention, screening, and counseling regarding overweight and obesity to help their patients achieve and maintain a healthy weight (see Chapter 8, Strategy 4-1). Given the linkage between consumption of sugar-sweetened beverages and obesity, particularly among children and adolescents, and the fact that these beverages are the leading source of added sugars in the American diet, health care providers such as physicians, dentists, registered dietitians, and nurses have a unique opportunity to screen and/or counsel patients on the risks associated with overconsumption of these beverages. The American Academy of Pediatrics (2011) calls for pediatricians to educate children, adolescents, and their parents about the linkage among consumption of sports drinks, excess caloric intake, and obesity and overweight, as well as dental erosion; to promote water as the principal source of hydration for children and adolescents; and to limit consumption of sports drinks to circumstances in which rapid replenishment of carbohydrates and/or electrolytes is necessary, such as during periods of prolonged, vigorous physical activity. Additionally, given the risk of dental caries associated with excessive sugar consumption, the AAP Section on Pediatric Dentistry and Oral Health (2008) recommends that pediatricians counsel parents and caregivers on the importance of reducing children’s exposure to added sugars in foods and bever-
ages, including limiting sugared drinks, avoiding carbonated beverages and juice drinks containing less than 100 percent juice, and encouraging children to drink only water and milk between meals.
In summary, sugar-sweetened beverages make a substantial contribution to the energy intake of Americans and are linked to increased weight gain/body weight, particularly in children. Moreover, availability of and exposure to such beverages are widespread in all sectors of society. Therefore, the committee believes an integrated, comprehensive approach will be needed to cause Americans to reduce consumption of these beverages as part of an effort to ensure a balanced diet that includes a variety of foods and beverages recommended in the Dietary Guidelines for Americans.
Indicators for Assessing Progress in Obesity Prevention for Strategy 2-1
Primary Indicator
• Reduction in energy intake from consumption of sugar-sweetened beverages.
Source for measuring indicator: NHANES
Process Indicators
• Reduction in consumption of sugar-sweetened beverages such that they account for a smaller proportion of solid fats and added sugars in the daily diet.
Source for measuring indicator: NHANES
• Adoption by states and school districts of policies that prohibit the sale of sugar-sweetened beverages in schools and require that schools offer a variety of no- or low-calorie beverage options that are favorably priced.
Sources for measuring indicator: CDC’s School Health Policies and Practices Survey and CLASS (NCI)
• Adoption by states and school districts of policies that require schools to provide access to free, clean, potable water throughout the school setting.
Source for measuring indicator: CDC’s School Health Policies and Practices Survey
Foundational Indicators
• USDA’s prohibition of the sale of sugar-sweetened beverages in schools as part of the competitive food and beverage regulations to be developed for the Healthy, Hunger-Free Kids Act of 2010.
Source for measuring indicator: USDA
• Reduction in energy intake from consumption of sugar-sweetened beverages among populations with higher rates of consumption of such beverages, including non-Hispanic blacks, Mexican Americans, and lower-income individuals.
Source for measuring indicator: NHANES
NOTE: CDC = Centers for Disease Control and Prevention; CLASS = Classification of Laws Associated with School Students; NCI = National Cancer Institute; NHANES = National Health and Nutrition Examination Survey; USDA = U.S. Department of Agriculture.
Chain and quick-service restaurants should substantially reduce the number of calories served to children and substantially expand the number of affordable and competitively priced healthier options available for parents to choose from in their facilities.
Potential actions include
• developing a joint effort (modeled after the Healthy Weight Commitment initiative) to set a specific goal for substantially reducing the total annual calories served to children in these facilities; and
• ensuring that at least half of all children’s meals are consistent with the food and calorie guidelines of the Dietary Guidelines for Americans for moderately active 4- to 8-year-olds and are competitively priced.
Context
On any given day, it is estimated that 30-40 percent of children and adolescents (aged 4-19) eat fast food (Bowman et al., 2004; Kant and Graubard, 2004; Paeratakul et al., 2003). Approximately one-third of calories consumed by all Americans (aged 2 and older) are consumed outside the home (ERS, 2004). Most quick-service and chain restaurants offer children’s meals. Limited research has addressed the nutritional profile of these meals. Relative to established expert guidelines (i.e., the Dietary Guidelines for Americans [HHS/USDA, 2010], Healthier School Challenge [FNS, 2011a], the Dietary Reference Intakes [IOM, 2006a], IOM school meal guidelines [IOM, 2007a]), however, two studies found that a majority of children’s meals at chain and fast-food restaurants exceed the recommended calories, are considered high in saturated fat and sodium, and offer limited healthful choices (Harris et al., 2010; Wootan et al., 2008). In 2007 only 3 percent of meals marketed to children at 10 popular quick-service restaurants met the current National School Lunch Guidelines (O’Donnell et al., 2008). The caloric content of meals studied ranged from 180 to 880 kcal (O’Donnell et al., 2008).
To date, much of the attention related to reducing childhood obesity has focused on marketing of foods and beverages to children and adolescents, especially items to be consumed in the home, such as cereals and snack foods. Voluntary initiatives (CFBAI, 2011; Healthy Weight Commitment Foundation, 2011) have sought to address such marketing through nutrition standards and have resulted in some product reformulation and the introduction of some healthier foods (Kraak et al., 2011). As of this writing, however, the membership of Children’s Food and Beverage Advertising Initiative (CFBAI) includes just two restaurants, and the Healthy Weight Commitment includes just one. Thus, this avenue offers substantial potential for accelerating progress in obesity prevention. Expectations are that by the end of 2015, food manufacturing companies will reduce annual calories by 1.5 trillion and sustain that level (Gable, 2011). An individual evaluation of the Healthy Weight Commitment began in 2010 to study calorie sources and eating pattern shifts (UNC Carolina Population Center, 2011). Such evaluation efforts present many opportunities and challenges, but clearly show that work is under way to measure progress.
In recent years, several fast-food and chain outlets have started developing healthier options for children’s meals. In 2006, for example, Disney began offering a healthier children’s meal as the default option at its theme parks (The Walt Disney Company, 2011). In 2011 the National Restaurant Association announced an initiative in which 19 chains, including Burger King, agreed to provide at least
one children’s meal option with no more than 600 calories (NRA, 2011). Also in 2011, McDonald’s announced that low-fat milk will be the default drink option with Happy Meals, apples will be included in every Happy Meal, and the portion of french fries offered with Happy Meals will be reduced, resulting in a 20 percent calorie reduction compared with the traditional Happy Meal (the company did not release the specific number of calories) (McDonald’s, 2011).
Although these developments sound encouraging, a recent analysis of the availability of healthy items on fast-food menus (as of January 2010) revealed that much more progress is needed (Harris et al., 2010). Just 12 of the 3,039 possible children’s meal combinations that were studied met nutrition criteria for preschoolers, while 15 met the criteria for older children and adolescents (Harris et al., 2010). Although almost all of the top quick-service chains offer at least one healthy side dish and nutritious beverages, very few of the main dish options qualify as nutritious (Harris et al., 2010). In sum, industry has begun to respond to the need to provide healthier options for parents, but given the magnitude of the health challenge posed by childhood obesity, much more needs to be done, and on a far more urgent basis. Industry must truly step up and take, as the IOM has recommended, a “transforming” leadership role (IOM, 2006b).
Evidence
The IOM and other observers have long recommended that fast-food and chain restaurants play a larger role in addressing obesity, particularly childhood obesity. One IOM report recommends that full-service and fast-food restaurants expand healthier food options (IOM, 2005), and another calls on restaurant trade associations to assume “transforming leadership roles” on behalf of healthful diets for children and adolescents (IOM, 2006b). Similarly, the White House Task Force on Childhood Obesity has recommended that the restaurant industry “develop or reformulate more healthful foods for children and young people” (White House Task Force on Childhood Obesity, 2010, p. 60). And the Healthy Eating, Active Living Convergence Partnership has recommended encouraging restaurants to provide healthy foods and beverages by “reformulating existing menu items, adding healthier menu items (e.g., fruits, vegetables, and whole grains), offering affordable and reasonably sized portions, [and] providing healthier combinations for meals,” and specifically suggested “making healthier items the standard for children’s meals” (Lee et al., 2008, p. 7).
Children and adolescents who eat more meals from restaurants (sit-down and fast-food) have higher caloric intakes and poorer diet quality (i.e., more fat
and sugar-sweetened beverages and less fruit, vegetables, and milk) (Befort et al., 2006; Boutelle et al., 2004; Bowman et al., 2004; French et al., 2001b; Lin et al., 1999; Paeratakul et al., 2003; Schmidt et al., 2005; Wiecha et al., 2006; Zoumas-Morse et al., 2001). Some studies have had mixed results regarding the association between frequency of eating out and higher BMI or body fatness; however, two longitudinal studies found that greater intake of fast food in adolescence is associated with an increase in body weight or BMI in young adulthood (Niemeier et al., 2006; Thompson et al., 2004). It has been reported that specific populations of children and adolescents consume higher amounts of fast food (males, non-Hispanic blacks, older adolescents, those with higher household incomes, and those who reside in the South) and that children, adolescents, and young adults consume more fast food than adults (Bowman et al., 2004; Paeratakul et al., 2003).
Implementation
Given the substantial number of calories consumed by children and adolescents away from home and particularly at quick-service and full-service restaurant chains, the committee believes this recommendation has the potential to accelerate progress in obesity prevention by effecting substantial reduction in the calories and fat consumed by children and adolescents. This recommendation may have the added benefit of reducing disparities in obesity rates for those young people who consume more food away from home—those who are male, non-Hispanic black, of higher household income, and older (i.e., adolescents).
Some companies have begun to make healthier options the default selection unless the customer requests otherwise, and other companies are beginning to offer healthier (lower-calorie) children’s meals. After Disney began offering a healthier children’s meal as the default option at its theme parks in 2006, more than 50 percent of customers stayed with the healthier choice (The Walt Disney Company, 2011). When McDonald’s began offering apple dippers on request as a substitute for french fries in Happy Meals, the chain reported that less than 11 percent of customers requested the apples instead of the fries (McDonald’s, 2011). In summer 2011, McDonald’s announced it would be including apples, a smaller portion of french fries, and 20 percent fewer calories overall in the “most popular” Happy Meals. In 2011, the National Restaurant Association announced that 19 large restaurant chains had agreed to provide at least one children’s meal option with no more than 600 calories (NRA, 2011).
These and other new restaurant industry efforts will need further evaluation to determine the impact of these new offerings on purchase requests and consumption patterns. The vast majority of children’s menu items in quick-service and chain outlets currently fail to meet the Dietary Guidelines for Americans (Harris et al., 2010); if they did so, a meaningful reduction in calories would result. The success of some outlets (for example, Disney) in making healthier children’s meals the default option indicates that many children and parents will make the healthier choice. At the same time, it must be noted that a majority of the food purchased for older children and adolescents in quick-service restaurants does not come from the available items on children’s menus (Harris et al., 2010). Instead, ordering from such menus for older children has declined, while purchases of items from value menus have increased. In particular, parents of elementary-age children are more likely to order items for their children from the regular menu than from the children’s menu (Harris et al., 2010). Therefore, it will be important to monitor the overall amount of calories consumed by children and adolescents in quick-service and chain restaurants to ensure that the unintended effect of shifting children’s choices to higher-calorie, less-nutritious menu items does not occur. A multiyear effort will be required in which industry leaders make a joint commitment to reformulating menus and substantially reducing calories in child and adolescent meal offerings.
In sum, a significant number of calories consumed by children and adolescents come from fast-food and chain restaurants. Offering healthier selections and lower-calorie options should result in a more opportunities for children and adolescents (and parents) to select these items, thus improving the quality of diets, reducing caloric intake, and likely reducing BMI or weight.
Indicators for Assessing Progress in Obesity Prevention for Strategy 2-2
Process Indicators
• Reduction in caloric intake by children and adolescents in chain and quick-service restaurants.
Source for measuring indicator: NPD Group (a consumer market research firm)
• Increase in the proportion of children’s meals offered by chain and quick-service restaurants that meet the Dietary Guidelines for Americans.
Source for measuring indicator: Update to study or similar to 2010 “Fast Food FACTS: Evaluating Fast Food Nutrition and Marketing to Youth” (Yale Rudd Center for Food Policy and Obesity)
• Increase in the proportion of restaurant outlets that offer a healthier option as the default menu choice.
Source needed for measurement of indicator.
• Increase in the proportion of purchased children’s meals that are labeled as “healthy.”
Source for measuring indicator: NPD Group (a consumer market research firm)
• Maintenance of or reduction in the percentage of adult meals, value meals, or à la carte items consumed by children and adolescents in chain or quick-service restaurants.
Source for measuring indicator: NPD Group (a consumer market research firm)
Foundational Indicators
• Increase in the proportion of chain and quick-service restaurants that join the Children’s Food and Beverage Advertising Initiative.
Source for measuring indicator: CFBAI
• Increase in the percentage of chain and quick-service restaurants that join the Healthy Weight Commitment.
Source for measuring indicator: HWC
• Increase in the proportion of chain and quick-service restaurants that commit to offering at least 50 percent of all children’s meals meeting the Dietary Guidelines for Americans.
Sources for measuring indicator: NRA and the associated press.
NOTE: CFBAI = Children’s Food and Beverage Advertising Initiative; HWC = Healthy Weight Commitment; NRA = National Restaurant Association.
Government agencies (federal, state, local, and school district) should ensure that all foods and beverages sold or provided through the government are aligned with the age-specific recommendations in the current Dietary Guidelines for Americans. The business community and the private sector operating venues frequented by the public should ensure that a variety of foods and beverages, including those recommended by the Dietary Guidelines for Americans, are sold or served at all times.
For government agencies, potential actions include
• the federal government expanding the healthy vending/concession guidelines to include all government-owned and/or -operated buildings, worksites, facilities,15 and other locations where foods and beverages are sold/served; and
• all state and local government-owned and -operated buildings, worksites, facilities, and other locations where foods and beverages are sold/served (including through vending machines and concession stands) adopting and implementing a healthy food and beverage vending/concession policy.
For the business community/private sector, potential actions include
• the business community and private-sector entities that operate places frequented by the public ensuring that a variety of food and beverage options are competitively priced and available for purchase and consumption in these places,16 including food and beverages that are aligned with the recommendations of the Dietary Guidelines for Americans.
![]()
15 “Government-owned and -operated buildings, worksites, and facilities” is defined broadly to include not only places of work but also locations such as government-owned and/or -operated child care centers, hospitals, and other health care/assisted living facilities, military bases, correctional facilities, and educational institutions.
16 “Places frequented by the public” includes, but is not limited to, privately owned and/or operated locations frequented by the public such as movie theaters, shopping centers, sporting and entertainment venues, bowling alleys, and other recreational/entertainment facilities.
Context
In 2010, 47.9 percent of all food spending, or more than $594 million, was for food consumed away from home (which includes food purchased by families and individuals for other-than-home consumption, expense-account meals, food furnished to employees, food furnished to inmates and patients, and food and cash donated to schools and institutions) (ERS, 2011a,b). Thus, attention must be paid to those places Americans frequent on a regular basis where they have ready access to food to ensure that they have a range of food options, including those that are healthy and affordably priced.
The food environment and points of access to that environment are vast. Outside of the home, Americans have access to food on a daily basis through government-run and/or -operated buildings and facilities, at work, at school and in child care settings, in recreational and entertainment settings, and in other locations (e.g., institutional facilities, military bases). Yet many of these locations are often overlooked as critical in affecting Americans’ access to healthy, affordable foods that are recommended by the Dietary Guidelines for Americans.
Evidence
To maintain energy balance and focus on nutrient-dense foods and beverages, Americans must have access to a wide range of foods and beverages and not be inundated predominantly with those options that the Dietary Guidelines recommend limiting. Given that foods consumed outside of the home represented approximately 34 percent of the energy intake of children and adolescents by 2006 (Poti and Popkin, 2011) and 47.9 percent of all food spending (ERS, 2011b), it is critical to focus on such foods, including those consumed in government-owned and -operated buildings, worksites, and facilities, as well as places owned and operated by private enterprise but frequented by the public.
There is a positive relationship between eating behaviors and access to healthy foods (Larson et al., 2009). Studies have found that individuals with access to a greater amount of healthy foods consume more fresh produce and other healthful items (Treuhaft and Karpyn, 2010). Increasing consumption of the foods and beverages recommended by the Dietary Guidelines will depend heavily upon their availability and affordability. In fact, a 2011 IOM workshop on hunger and obesity explained that the keys to maximizing the purchase of healthier food options are increased availability, reduced price, and promotion of healthier choices (IOM, 2011). The evidence is clear that decreasing the prices of healthy food items relative to less-healthy items is effective in promoting purchases of the healthier items
(Epstein et al., 2006, 2007; French, 2003; French et al., 1997, 2001a; Michels et al., 2008; Ni Mhurchu et al., 2010), and that higher beverage prices lead to reduced consumption (Powell and Chaloupka, 2009; Smith et al., 2010).
Implementation
Federal, state, and local government Federal, state, and local government agencies are providers of food and should not be overlooked as part of the food environment. Various government programs procure food for their own restaurant/food service operations or provide assistance to allow others to do so (IOM, 2010). These programs range from food purchases for public worksites, health care facilities, senior centers, and military bases to foods sold in vending machines in city parks and other public places. More than 19 million individuals are employed at the federal, state, and local levels of government (U.S. Census Bureau, 2007), and this figure does not include members of the public who frequent or reside in government-owned or operated buildings, worksites, or facilities. Further, more than 1,400,000 people are on active duty in the U.S. military worldwide (Defense Manpower Media Center, 2011); the most recent estimate indicates that the military purchases more than $800 million in food to feed these personnel (GAO, 2000). According to the U.S. Census Bureau, between 2005 and 2009 more than 2 million people resided in adult correctional facilities, more than 1.8 million in nursing facilities/skilled nursing facilities, and more than 2 million in college/ university housing (U.S. Census Bureau, 2011). Additionally, a number of federal programs use government funds for the purchase of food (GAO, 2000). The ability of these settings to institute public food standards may vary given their purpose, operating constraints, and reach (see Table 6-2).
Early child care and school settings also are key points of food access. More than 8 million children aged 3-5 were enrolled in early child care programs in 2009, and more than 55 million children and adolescents were projected to be enrolled in public and private secondary schools in 2010 (NCES, 2010, 2011). (See the discussion of school food standards in Chapter 9.)
Research has shown that changes in the workplace and child care settings (in addition to changes in the school setting addressed in Recommendation 5 [Chapter 9]) are effective in increasing the consumption of healthy options or in limiting access to unhealthy options. Strong evidence shows that worksite obesity prevention and control programs can reduce weight in employees and create habits that could be modeled at home. Some of these effective programs include interventions that improve access to healthy foods by changing cafeteria and
TABLE 6-2 Federal Agencies and Programs That Directly Purchase Foods or Use or Set Standards for Food Purchases
| Agency | Program |
| U.S. Department of Agriculture |
National School Lunch Program School Breakfast Program Supplemental Nutrition Assistance Program (SNAP) Summer Food Service Program Child and Adult Care Food Program Commodity Supplemental Food Program Food Distribution Program on Indian Reservations Nutrition Program for the Elderly The Emergency Food Assistance Program Food Assistance for Disaster Relief Fresh Fruit and Vegetable Program Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) Nutrition Services Incentive Program |
| Department of Defense |
Regular feeding of troops Fresh Fruit and Vegetable Program Defense Supply Center Philadelphia’s Subsistence Directorate (link between the Armed Forces and the food industry; provides subsistence for military personnel and federal agencies worldwide) |
| Department of Justice (Bureau of Prisons) | Subsistence program purchases food for prisons |
| Department of Veterans Affairs | Food purchases for Veterans Affairs facilities |
| Department of Labor |
Job Corps Center (provides training and employment for severely disadvantaged youths, generally in a residential setting) |
SOURCES: Defense Logistics Agency, 2011; FNS, 2011b; GAO, 2000.
vending machine options as part of a multicomponent program (Anderson et al., 2009). (See also the discussion of Strategy 4-3 in Chapter 8.) Likewise, research suggests that in child care settings, the nutritional quality of meals and snacks can be poor, and activity levels may be inadequate (see the discussion of Strategy 1-4 in Chapter 5) (Ball et al., 2008; Padget and Briley, 2005; Story et al., 2006). Furthermore, children model the behavior of adults (Pearson et al., 2009). Thus,
ensuring that publicly run worksites and child care centers are offering foods and beverages that are aligned with the Dietary Guidelines for Americans is essential to making the healthy choice the default choice (IOM, 2009; Ritchie et al., 2012).
Governments nationwide are in fact adopting and implementing nutrition standards to ensure the availability of a wide variety of foods and beverages, including those recommended by the Dietary Guidelines for Americans, in government-run or -regulated facilities and programs and applying those standards to food and beverage procurement and contracting (see Box 6-3). Such standards were recommended by a prior IOM committee and other experts (IOM, 2009, 2011). They build on the work done in schools nationwide to create healthy eating environments through state, district, and federal policies (the latter with the implementation of the Healthy, Hunger-Free Kids Act of 201017) that restrict fats, sugars, calories, and other items that the Dietary Guidelines recommend limiting (CDC, 2011; Chriqui et al., 2010; Trust for America’s Health and RWJF, 2011).
By instituting nutrition standards for all foods purchased with government dollars, local and state authorities can reduce the calories consumed by their residents across a variety of environments, model healthier eating, and potentially drive reformulation as companies respond to new product specifications. Furthermore, local and state governments can have considerable influence over a number of diverse food purchase and distribution locations. The introduction of nutrition standards is an area of increasing activity that offers an opportunity to influence diet at the population level. Beyond federal programs, state and local governments often are relatively large purchasers of food. They purchase or contract with restaurant/food service operators to supply the foods sold in employee cafeterias, schools and child care centers, public hospitals, senior centers, parks, and numerous other facilities (IOM, 2010).
Business community Foods are readily available in public places such as movie theaters, sports venues, and theme parks, to name a few, and attendance at these public places is not trivial. In 2010, more than 1.3 billion movie tickets were sold in the United States and Canada; 68 percent of all Americans and Canadians— or 222.7 million people—attended at least one movie in 2010 (Motion Picture Association of America, 2010). Furthermore, 339 million people attended theme parks during 2009, and 132 million attended professional sporting events such as Major League Baseball, National Football League, and National Basketball
![]()
17 Public Law 111-296 (December 13, 2010).
BOX 6-3
Government Nutrition Standards
A number of states, counties, and cities have adopted nutrition standards for the meals and snacks they serve or provide to clients, employees, and the public. The introduction of nutrition standards for snacks and drinks sold in vending machines located on government-owned or -operated property, most commonly schools and hospital systems, is another area of recent local government engagement. When nutrition standards for foods sold in machines are incorporated into vending machine contracts, government further supports normalizing the consumption of healthier foods (IOM, 2010).
Federal Worksites
The Department of Health and Human Services and the General Services Administration developed Health and Sustainability Guidelines for Federal Concessions and Vending Operations (CDC, 2011). The goal of these guidelines is to assist contractors in increasing the availability of healthy food and beverage options and maintaining sustainable practices at federal worksites.
New York City
In 2009, New York City adopted standards for meals/snacks purchased and served by city agencies to agency clients that include schools, senior centers, homeless shelters, child care centers, after-school programs, correctional facilities, public hospitals and parks, and other agency facilities and programs and for beverage vending machines (New York City Department of Health and Mental Hygiene, 2011). The beverage vending machine standards affect all machines on city property. Twelve city agencies purchase or serve food that is covered by the meal/snack standards. These standards and those for beverage vending machines are being adopted voluntary by some private hospitals, workplaces, and community organizations (personal communication, T. Farley, New York City Department of Health and Mental Hygiene, May 25, 2011).
Based on agency reports, the New York City Department of Health and Mental Hygiene estimates that the standards affect more than 260 million meals and snacks served each year by city agencies (New York City Department of Health and Mental Hygiene, 2011). Five (of the nine) city agencies that serve meals provide three meals a day to their clients, while the other four agencies serve one or two meals a day (personal communication, T. Farley, New York City Department of Health and Mental Hygiene, May 25, 2011). Some of the clients are seen every day (in day care and after school), while others are transient populations (the hospitalized, the homeless).
Since the adoption of the standards for meals/snacks in 2009, the New York City agency procurement practices and purchasing patterns have changed. The standards have been included in contracts with food suppliers and caterers. The result has been discontinuation of the purchase of some items (e.g., sugary drink mixes or items that require deep frying), the purchase of healthier alternative products (e.g., fruit packed in juice, not syrup), and the reformulation of some products to meet the standards (e.g., reducing the sodium in canned vegetables and reducing the sodium and fat in beef patties) (personal communication, T. Farley, New York City Department of Health and Mental Hygiene, May 25, 2011). Overall, implementation of the standards has resulted in the availability of more healthy options among the foods purchased and served by New York City agencies.
Massachusetts
In 2009, the Governor of Massachusetts issued an executive order mandating that all food purchased and sold by state agencies on state property conform to certain nutrition standards established by the public health department (Executive Order 509, 2009). Vending machines and other independent concessions are exempted. This order is aimed at food served to clients by state agencies and their vendors. These clients are dependent on the state for a package of services that
Association games—all venues where food is sold for immediate consumption and all hosting a captive audience or consumer base seeking a wide range of food and beverage options, including those recommended by the Dietary Guidelines for
includes the provision of food and beverages. The executive order applies to 9 of the state’s 58 agencies, responsible for approximately 110,980 meals each day (personal communication, Cynthia Taft Bayerl, Massachusetts Department of Public Health, August 24, 2011).
As of August 2011, the language of the executive order had been incorporated into a request for proposals for bakery products and catering to serve the nine affected agencies. As a result, the availability of healthy food choices has improved for these agencies. The larger agencies have larger food budgets, which allow them to balance the reduction in unhealthy food options (e.g., high-calorie foods and snacks) with the increased cost of healthy food options (e.g., whole-grain rather than white bread). The smaller agencies report the most difficulty in offering healthier foods. These agencies lack the buying power of the larger state agencies. Given their limited number of clients and storage space, these sites purchase smaller amounts of food at the local supermarket.
Public-service venues, vendings, and concessions are exempt from the executive order. However, they are encouraged to follow the state’s Healthy Meeting and Event Guide (Massachusetts Department of Public Health, 2007).
Delaware State Parks
In June 2010, Delaware State Parks adopted a “Munch Better” initiative that will provide healthy foods for sale and in vending machines. For the first year, the goal is for at least 75 percent of the food and beverage products sold by parks to be either a “Go” or a “Slow” food (i.e., no more than 25 percent will be a “Whoa” food). This initiative was developed through a partnership among the Division of Parks and Recreation, the Nemours Health and Prevention Services (which developed the food and beverage guidelines), and the Delaware Health and Social Services’ Division of Public Health (which will monitor progress) (Delaware State Parks, 2011).
Americans (Motion Picture Association of America, 2010). Indeed, the business community has been improving the foods and beverages offered for sale at entertainment and sporting events (see Box 6-4 for examples).
BOX 6-4
Examples of Improved Food and Beverage Offerings at Entertainment and Sporting Events
Improvements in food and beverage offerings are not limited to government settings. Positive steps in this regard also are occurring in the business community through improvements in the foods and beverages offered for sale in public venues such as entertainment and sporting events. Two illustrative examples follow.
Movie Theaters
In March 2010, the chairman and CEO of Sony Pictures Entertainment, Michael Lynton, asked the nation’s theater owners to offer healthier snacks at their concession stands alongside the traditional candy, popcorn, and soda (James, 2010). In April 2011, AMC Theaters introduced AMC Smart MovieSnacks at all of its U.S. theaters for $7.00, compared with the roughly $10 cost of popcorn and a soda (AMC Entertainment, 2011; Carollo, 2011). The snack packs contain “the best of nutritious snack choices, yet still allow guests to indulge, albeit smartly, when snacking at the movies” (AMC Entertainment, 2011). They include
• Chiquita Fruit Chips consisting of 100 percent real fruit;
• Dasani purified water;
• Odwalla Bar Chocolate Chip Trail Mix with chocolate chips, rolled oats, peanuts, raisins, coconut, sunflower seeds, and Vitamins A, C, and E plus folic acid and calcium; and
• PopCorners—chip-like corn snacks that are air popped with real corn and all natural ingredients.
In sum, the committee believes that implementation of this strategy, in concert with the other strategies recommended in this chapter and in the report as a whole, represents an important step toward reducing the obesogenic environment in which Americans live, work, and play. Implementation of this strategy by
The new snack bundle has about 450 calories and 10 grams of fat (Carollo, 2011).
AMC’s initiative to improve access to more nutritious snacks at the movies included working with the Alliance for a Healthier Generation and testing hundreds of products with guest panelists. AMC modeled its Smart MovieSnacks on the Alliance’s school competitive food and beverage guidelines (AMC Entertainment, 2011).
Baseball Stadiums
At Dodger Stadium in Los Angeles, Kaiser Permanente has partnered with the stadium’s restaurant group to offer healthier options at “Healthy Plate” carts in three locations around the stadium. Menu items include “Curried Chicken Lettuce Wraps served with radish, cucumber, cottage cheese and cherry tomatoes; Spicy Shrimp Cocktail, a refreshing gazpacho-like dish; Fresh Fruit Salad using only fruits that are in season; Greek Salad made with basil, feta cheese, tomatoes and red onions with low-fat balsamic vinaigrette; assorted sushi including California rolls, spicy tuna rolls and cucumber rolls; and a turkey sandwich served on whole wheat with avocado. Gluten-free beer and snacks will also be available at the Kaiser Permanente Healthy Plate Carts” (Dodgers, 2010). With the original recipe, the curried chicken salad ($8.75) weighs in at 313 calories and 15 grams of fat per serving, but the ballpark serving will be a couple of ounces bigger and include a scoop of cottage cheese. The farmers’ market Greek salad ($8.75) has 130 calories and 11 grams of fat per serving, and the fruit and yogurt parfait ($5.25) with granola topping has 222 calories and 2 grams of fat (both per original recipes) (Stein, 2009).
governments and the business community would go a long way toward providing Americans with access to foods and beverages recommended by the Dietary Guidelines for Americans in places where they spend their work and leisure time.
Indicators for Assessing Progress in Obesity Prevention for Strategy 2-3
Primary Indicators
• Increase in the proportion of energy intake attributable to consumption of foods and beverages recommended by the Dietary Guidelines for Americans.
Source for measuring indicator: NHANES
• Reduction in energy intake associated with solid fats and added sugars.
Source for measuring indicator: NHANES
Process Indicators
• The federal government’s expansion of its healthy vending/concession guidelines to include all federal government-owned, -operated, and -occupied buildings, worksites, and facilities.
Sources for measuring indicator: GSA and HHS
• Increase in the proportion of states and municipalities that adopt and implement policies designed to ensure that foods/beverages sold and served in government-owned and -operated buildings, worksites, and facilities and other public places where foods and beverages are sold/served are aligned with the recommendations of the Dietary Guidelines for Americans.
Source needed for measurement of indicator.
• Increase in the proportion of public places where foods and beverages are sold that offer a range of affordable and healthy food and beverage options.
Source needed for measurement of indicator.
• Assurance of age-appropriate portion sizes and increase in quality of foods and beverages offered in government-owned and/or -operated child care programs.
Source for measuring indicator: USDA program monitoring/reporting for funded programs
Foundational Indicator
• Adoption of healthy vending and food/beverage standards by members of the business community selling foods/beverages for public consumption.
Source needed for measurement of indicator.
NOTE: GSA = U.S. General Services Administration; HHS = U.S. Department of Health and Human Services; NHANES = National Health and Nutrition Examination Survey; USDA = U.S. Department of Agriculture.
States and localities should utilize financial incentives such as flexible financing or tax credits, streamlined permitting processes, and zoning strategies, as well as cross-sectoral collaborations (e.g., among industry, philanthropic organizations, government, and the community) to enhance the quality of local food environments, particularly in low-income communities. These efforts should include encouraging or attracting retailers and distributors of healthy food (e.g., supermarkets) to locate in underserved areas and limiting the concentration of unhealthy food venues (e.g., fast-food restaurants, convenience stores). Incentives should be linked to public health goals in ways that give priority to stores that also commit to health-promoting retail strategies (e.g., through placement, promotion, and pricing).
Potential actions include
• states creating cross-agency teams to analyze and streamline regulatory processes and create tax incentives for retailing of healthy foods in underserved neighborhoods;
• states and localities creating cross-sectoral collaborations among the food and beverage industry, philanthropy, the finance and banking sector, the real estate sector, and the community to develop private funding to facilitate the development of healthy food retailing in underserved areas; and
• localities utilizing incentive tools to attract retailing of healthy foods (e.g., supermarkets and grocery stores) to underserved neighborhoods, such as through flexible financing or tax credits, streamlined permitting processes, zoning strategies, grant and loan programs, small business/economic development programs, and other economic incentives.
Context
As noted earlier, there is a positive relationship between access to healthy foods and eating behaviors (Larson et al., 2009; Treuhaft and Karpyn, 2010). Studies have found that individuals with access to a greater abundance of healthy foods consume more fresh produce and other healthful items (Lopez, 2007; Morland et al., 2006; Powell et al., 2007; Treuhaft and Karpyn, 2010). Yet many neighborhoods in the United States are without any type of grocery store or supermarket (Powell, 2009). Rural areas have fewer food retailers of any type than urban areas (controlling for population density) (Morton and Blanchard, 2007). Neighborhoods that are predominantly black, Hispanic, and low-income have disproportionately limited access and have seen the greatest decrease in the introduction of new food stores compared with predominantly Caucasian and higher-income neighborhoods (Powell, 2009; Treuhaft and Karpyn, 2010). Even when supermarkets are available in the former neighborhoods, healthier food items are less available (Krukowski et al., 2010; Treuhaft and Karpyn, 2010).
Additionally, greater access to convenience stores and fast-food restaurants, where healthy choices may not be readily available and may cost more, has been associated with a greater likelihood of lower dietary quality (Boone-Heinonen et al., 2011; Hickson et al., 2011; Larson et al., 2009). The availability of fast-food restaurants, convenience stores, and calorie-dense foods is greater in lower-income and minority neighborhoods (Baker et al., 2006; Larson et al., 2009).
Local food environments influence the choices made by children, families, and community members (IOM, 2009). Emerging evidence indicates that community strategies designed to reduce obesity by modifying the local food environment must take a comprehensive approach that is designed both to increase the availability of and access to healthy food options and to limit the concentration of and access to unhealthy food options (Boone-Heinonen et al., 2011). The relative balance of healthy and unhealthy food options may be more important than the presence or absence of any given food resource. Additionally, strategies that actively promote the selection and purchase of healthy food options (e.g., in-store
promotions/placement, favorable display locations) may be critical to optimizing the benefits of healthy food resources.
Evidence
Since 2005 a number of expert committees have recommended that communities improve access to healthy foods, particularly in low-income and underserved areas, through a variety of evidence-based strategies in order to improve healthy eating (IOM, 2005, 2009; Khan et al., 2009; Lee et al., 2008; RWJF, 2009; White House Task Force on Childhood Obesity, 2010). The IOM report Local Government Actions to Prevent Childhood Obesity (IOM, 2009), in addition to recommending strategies for improving access to healthy foods, recommends strategies designed to discourage unhealthy local foods and resources.
In general, these strategies are supported by research indicating that consuming a diet rich in fruits and vegetables (in conjunction with other behaviors) tends to be associated with reduced weight gain and lower prevalence of obesity (or weight gain); however, the relationship of fruit and vegetable intake and eating behaviors to adiposity (i.e., BMI) in children is not clear (Alinia et al., 2009; Jago et al., 2007; Kahn et al., 1997; Ledoux et al., 2010; Muller et al., 1999). Evidence as to whether the availability of a specific type of food resource is associated with dietary consumption patterns or obesity rates is mixed, although it appears to be stronger for low-income males (Boone-Heinonen et al., 2011). Still, research suggests that individuals with greater access to retail venues that sell healthy foods (e.g., supermarkets) and limited access to those where healthy choices may not be available and cost more (e.g., fast-food restaurants, convenience stores) tend to have a lower risk of obesity or reduced weight gain (Giskes et al., 2011; Jilcott et al., 2011; Larson et al., 2009; Lopez, 2007; Morland and Evenson, 2009; Morland et al., 2006; Powell et al., 2007). More specifically, greater access to supermarkets can positively influence fruit and vegetable intake, dietary intake, consumption patterns, and diet quality compared with limited access, and for adolescents has been associated with lower BMI (Auld and Powell, 2009; Mikkelsen and Chehimi, 2007; Morland et al., 2002; Powell et al., 2007, 2010; Rose and Richards, 2004; Zenk et al., 2005). For example, Supplemental Nutrition Assistance Program (SNAP) participants who do not shop at supermarkets purchase fewer fresh fruits and vegetables and less milk than those who shop at supermarkets (ERS, 2009).
Evidence is mixed, however, on the influence of the availability and proximity of supermarkets on dietary quality, fruit and vegetable intake, and prevalence of
obesity (Boone-Heinonen et al., 2011; Michimi and Wimberly, 2010). This mixed evidence suggests that the impact of supermarkets on food intake and obesity is mediated by what happens inside the store—other factors such as food prices and promotion/retailing practices. Access to affordable healthy foods does not necessarily mean that consumers will purchase and consume them. Building a store is the first step toward increasing availability of healthy foods, but complementary strategies to promote dietary behavior change must be included in such initiatives. Although research is limited, Glanz and Yaroch (2004) found that point-of-purchase information; reduced prices and coupons; increased availability, variety, and convenience; and promotion and advertising in supermarkets were moderately effective in influencing purchasing behavior. Major food retailers likewise have stated that in-store retailing practices are an essential influence on their customers’ purchasing decisions (Rogers, 2011; Thomas, 2011).
As noted earlier, poor food environments often include an abundance of fast-food restaurants and convenience stores selling high-calorie, high-fat meals at relatively low prices (Lewis et al., 2005), as is disproportionately the case in lower-income and minority neighborhoods. Fast-food consumption and availability are related among low-income individuals (Boone-Heinonen et al., 2011). Adolescents who live and attend school in areas with more fast-food restaurants and convenience stores than food outlets with healthier selections, such as grocery stores, are more likely to consume soda and fast food than those who live and attend school in areas with healthier food environments (Babey et al., 2011). For example, fast-food availability may contribute to greater energy intake in younger black Americans (Hickson et al., 2011).
Despite the growing evidence base linking the concentration of fast-food restaurants to the consumption of calorie-dense food, community-level strategies to limit access to or reduce the concentration of fast-food restaurants are limited. Moratoriums on such restaurants and other strategies designed to limit the concentration of certain restaurant types are relatively new and as yet unproven. Given the emerging evidence implicating the concentration of fast-food restaurants in unhealthy eating, such strategies may prove beneficial in enhancing the quality of local food environments, particularly in low-income communities.
Implementation
A number of efforts have been undertaken to support and implement the sentiment of this recommended strategy by developing programs, initiatives, and legislation through public and private partnerships. The introduction of super-
markets in neighborhoods where they are lacking has yielded some initial positive economic results (see Box 6-5 for an example of supermarket initiatives and support programs).
Given the disproportionate lack of access to affordable healthy foods for a large number of Americans, the use of financial incentives, zoning, and cross-sectoral collaborations can attract healthy food retailing and distribution (e.g., supermarkets) to underserviced areas and limit the concentration of unhealthy
BOX 6-5
Supermarket Programs, Initiatives, and Legislation
• The Food Trust’s Supermarket Campaigna
• Pennsylvania Fresh Food Financing Initiativeb
• Food Retail Expansion Support Health in New York Cityc
• New Orleans Fresh Food Retailer Initiatived
• Louisiana Healthy Food Retail Acte
• TransForm Baltimoref
• California FreshWorks Fundg
• Re/Store Nashvilleh
• Federal Incentive Programs (USDA, HHS, HUD, EPA, US Treasury)i
![]()
aThe Food Trust, 2011.
bThe Reinvestment Fund, 2010.
cNew York City Government, 2009.
dThe City of New Orleans, 2011.
eHealthy Food Retail Act 2009. No. 252, §1.
fTransForm Baltimore, 2011.
gCalifornia FreshWorks Fund, 2011.
hGet Out. Be Active., 2011.
iSummarized in ERS, 2009, p. 105.
food venues (e.g., fast food). Preliminary economic impact assessments of such initiatives have found that they have a significant impact on estate prices, employment, and earnings, and they are expected to significantly increase access to healthy foods for millions of households and communities that are currently underserved (The Reinvestment Fund, 2010; Treuhaft and Karpyn, 2010). Yet while a large number of initiatives and investments are already being implemented in some localities, it is clear that further work is needed to provide access to healthy foods for everyone. In 2011, leaders from major retailers, foundations, and small businesses announced commitments to provide access to healthy, affordable food for millions of people in underserved communities (Partnership for a Healthier America, 2011). As part of the retail industry’s focus on healthy food initiatives, some of these same retailers have reported undertaking large-scale efforts to encourage healthier food purchases by understanding their customers and meeting their needs through the use of pricing strategies (e.g., coupons, daily specials), simple labeling or endorsements of healthier food products, in-store cooking demonstrations and recipes, and reorganization of the supermarket itself (customers must walk through the produce area to get to other sections of the store) (Rogers, 2011; Thomas, 2011).
In sum, the committee believes this recommended strategy would likely have a direct effect on the availability and accessibility of healthy and unhealthy foods in targeted neighborhoods and could encourage consumers to purchase foods that would help them meet the Dietary Guidelines for Americans. In particular, this strategy has the potential to reduce disparities in obesity rates for consumers who have no or limited access to retailers of healthy foods (e.g., supermarkets) and are exposed to a large number of retailers of unhealthy food. These include residents of neighborhoods that are predominantly black, Hispanic, low-income, and rural, as well as individuals lacking transportation.
Indicators for Assessing Progress in Obesity Prevention for Strategy 2-4
Process Indicators
• Increase in the proportion of Americans who have access to a food retail outlet that sells a variety of foods recommended by the Dietary Guidelines for Americans.
Source needed for measurement of indicator.
• Adoption and achievement of the grocery industry standard of 3 square feet of retail space per capita by all grocery retailers.*
Source needed for measurement of indicator.
Foundational Indicator
• Development and implementation by municipal governments of incentive programs for new and/or existing food retailers to increase access to healthier food and beverage options in underserved areas.
Source needed for measurement of indicator.
![]()
*Three square feet of space per person is a measure of demand for grocery retail service in a defined area commonly used by grocery retailers (International Council of Shopping Centers, 2008).
Congress, the Administration, and federal agencies should examine the implications of U.S. agriculture policy for obesity, and should ensure that such policy includes understanding and implementing, as appropriate, an optimal mix of crops and farming methods for meeting the Dietary Guidelines for Americans.
Potential actions include
• the President appointing a Task Force on Agriculture Policy and Obesity Prevention to evaluate the evidence on the relationship between agriculture policies and the American diet, and to develop recommendations for policy options and future policy-related research, specifically on the impact of farm subsidies and the management of commodities on food prices, access, affordability, and consumption;
• Congress and the Administration establishing a process by which federal food, agriculture, and health officials would review and report on the possible implications of U.S. agriculture policy for obesity prevention to ensure that this issue will be fully taken into account when policy makers consider the Farm Bill;
• Congress and the U.S. Department of Agriculture (USDA) developing policy options for promoting increased domestic production of foods recommended for a healthy diet that are generally underconsumed, including fruits and vegetables and dairy products, by reviewing incentives and disincentives that exist in current policy;
• as part of its agricultural research agenda, USDA exploring the optimal mix of crops and farming methods for meeting the current Dietary Guidelines for Americans, including an examination of the possible impact of smaller-scale agriculture, of regional agricultural product distribution chains, and of various agricultural models from small to large scale, as well as other efforts to ensure a sustainable, sufficient, and affordable supply of fresh fruits and vegetables; and
• Congress and the Administration ensuring that there is adequate public funding for agricultural research and extension so that the research agenda can include a greater focus on supporting the production of foods Americans need to consume in greater quantities according to the Dietary Guidelines for Americans.
Context
U.S. agriculture policy is a complex system that has evolved over many decades. The impact that farm policy has on the nation’s food supply and diet reflects not only current policies but also the long history of agriculture policies. Whether and how farm policy is related to the obesity epidemic are questions research has only recently begun to explore, and a definitive evidence base has
not yet emerged. But a consensus does appear to be developing around two key points: first, blunt approaches such as eliminating farm subsidies are unlikely to offer a quick fix to the obesity epidemic; and second, there are real opportunities to adjust farm policies in meaningful ways to better support the nation’s changing food and nutrition needs.
The current farm system does not produce sufficient fruits and vegetables and dairy products to support a substantial increase in the availability of healthier food and beverage options at affordable, competitive prices. Indeed, even including imports, the supply of fresh fruits and vegetables would be inadequate if all Americans adopted a diet consistent with the Dietary Guidelines for Americans (Buzby et al., 2006). This imbalance is a result of decades of farm policies and will take time to address.
Because considerable time will be required for the changes to agriculture policy that could positively impact obesity prevention to be implemented and translate to weight outcomes, action must be taken now to move policy toward a constructive long-term approach. The committee believes the nation can no longer ignore the need to address the potential role of farm policies in preventing obesity. This means giving priority to ensuring that U.S. farm and trade policies promote healthy eating and do not undermine obesity prevention, and applying that perspective to the evaluation of current policies and the development of policy alternatives. American farmers can and should be important allies in the fight against obesity, but they will assume that role only if agriculture policies support them in doing so.
Evidence
The impact of U.S. agriculture policies on obesity has received increasing attention over the past decade. In particular, concern has been raised about the impact of farm subsidies, check-off programs, marketing orders, and land use rules. Relative to the role of other sectors in the causes of obesity, the contribution of U.S. agriculture policies has received less scholarly analysis. This is one reason the committee is recommending an acceleration of both agriculture- and policy-focused research and deliberation.
Previous IOM committees have made similar recommendations, but without delineating specific implementing actions. A 2005 IOM report suggests that government agencies at all levels need to reexamine their existing policies and initiatives that may hinder progress toward prevention of childhood obesity, including agriculture policies. It suggests that a review of agriculture policies could identify
unintended effects of U.S. agriculture subsidies on human health, noting that further investigation of the possible relationships among agriculture policies (such as corn subsidies and the production and use of high fructose corn syrup in the U.S. food supply), the obesity epidemic (Bray et al., 2004), and the marked increase in type 2 diabetes (Gross et al., 2004; Schulze et al., 2004) is warranted. Specifically, the report recommends that the federal government undertake an independent assessment of federal nutrition assistance programs and agriculture policies to ensure that they promote healthful dietary intake for all children and adolescents. It also recommends that policies and programs be revised as necessary to promote a U.S. food system that supports energy balance at a healthy weight.
In assessing progress made toward this recommendation, a 2007 IOM report notes that there have been limited analyses examining the relationships among U.S. food supply-related agricultural, industrial, and economic policies (or the environments resulting from these policies) and consumer demand-driven nutrition policies (e.g., dietary guidance) (IOM, 2007b; Tillotson, 2004). The report suggests that future efforts to improve the U.S. food and agriculture system will need to forge connections among health, food, and farm policies that support the 2005 Dietary Guidelines for Americans. It also identifies the Farm Bill as an opportunity to foster changes that both support healthier diets and strengthen agricultural economies. The Institute for Agriculture and Trade Policy has drawn similar conclusions (Schoonover and Muller, 2006).
International health organizations likewise have called on member nations to step up efforts to ensure consistency between farm and health policies. The World Health Organization’s (WHO’s) Global Strategy on Diet, Physical Activity, and Health (WHO, 2004, p. 8) states that “national food and agriculture policies should be consistent with the promotion and protection of public health” and directs member states to consider “healthy nutrition” in their agriculture policies. The International Obesity Task Force recommends a three-pronged strategy: include nutritional criteria in agriculture policies, undertake health impact assessments of such policies, and provide support for agriculture programs aimed at meeting WHO’s dietary guidelines (Hawkes, 2007). The International Assessment of Agricultural Knowledge, Science and Technology for Development considers “improving nutrition and human health” as one of the goals in its framework for making decisions on international agriculture policies (McIntyre et al., 2009). The Chicago Council on Global Affairs and the UK Government Office of Science provided further support on connecting future farm policies with obesity (Foresight, 2011; The Chicago Council on Global Affairs, 2011).
Documenting the relationship between specific agriculture policies and public health outcomes is difficult because as noted, there is likely to be a time lag between agricultural cause and dietary effect (Hawkes, 2007), and a number of variables could mask or amplify the causal relationships (Muller et al., 2009). U.S. agriculture policy includes a complex set of programs that affect production costs, production, commodity prices, and farm incomes. Furthermore, farm outputs often go through several processing steps before reaching consumers, making it difficult to quantify the effect of a given policy on obesity. Consequently, the effects of agriculture policies on dietary intake and obesity are not well understood (Alston et al., 2006).
Implementation
Farm subsidies Existing examinations of the issues outlined above are limited, and researchers have reached differing conclusions. Some in the health professions believe that agriculture policies—particularly farm subsidies—have decreased the price of obesogenic foods, presumably leading to overconsumption of these foods and thereby contributing to the increase in obesity prevalence (e.g., Pollan, 2003; Schoonover and Muller, 2006; Tillotson, 2003). Others, including some in the agricultural economics community, conclude that farm subsidies bear little responsibility for lower food prices, increased consumption of obesogenic foods, and increased obesity prevalence (e.g., Alston et al., 2006, 2008; Miller and Coble, 2008; Schaffer et al., 2007).
Some analysts argue that farm subsidies have contributed to obesity because they decrease the prices of corn, soybeans, and other commodity crops. Food processors therefore can purchase these commodities at lower prices and thus are encouraged to use them as ingredients. Such ingredients (e.g., high fructose corn syrup and partially hydrogenated vegetable oils) often are found in low-nutrient, energy-dense (obesogenic) foods. The reasoning continues that because of the low input costs, such foods can be sold at low prices that encourage consumers to purchase and consume more of these foods, contributing to weight gain (Schaffer et al., 2007; Schoonover and Muller, 2006; Wallinga et al., 2009). Cawley and Kirwan (2011) use estimates and assumptions about the relationships among subsidies, food prices, and BMI to estimate that agriculture subsidies increase youth BMI by 0.08 percent. They also point out that the USDA’s commodity distribution program donates agriculture commodities to schools and maintain that in most cases, these commodities—cheese, milk, beef, pork, and oils—are energy dense. They estimate that the risk of obesity among children and adolescents who con-
sume school lunches is raised by 0.14 percentage points because of the commodity distribution program.
Wallinga and colleagues (2009) suggest that the relatively low prices for obesogenic foods have caused them to proliferate in the U.S. diet and have placed healthier foods, such as fruits and vegetables, at a competitive disadvantage. They also speculate that low commodity prices help maintain high profit margins on foods that make liberal use of these commodity inputs, consequently driving interest in the marketing of these foods.
Taking a different perspective, a number of papers and presentations on this topic were developed as part of a 4-year project undertaken by the University of California, Davis and Iowa State University, funded under a National Research Initiative Grant from the USDA National Institute for Food and Agriculture.18 The project team concluded that U.S. farm subsidy programs—namely, price and income supports for commodities—have had negligible effects on commodity prices and that eliminating or reversing commodity subsidy policies would be unlikely to affect consumer dietary behaviors such that obesity rates would be meaningfully reduced (Alston, 2010; Alston et al., 2006, 2007, 2008). First, they cite evidence that subsidies have had mixed and only modest effects on the availability and prices of commodities, particularly those that are ingredients in obesogenic foods. Second, they report that the magnitude of the effect of changes in commodity prices on retail prices depends on the cost share of the commodity in retail prices. Because food commodities represent about 20 percent of the current cost of food in the United States (and less for products such as soda and meals away from home), changes in the prices of commodities used in high-calorie foods may not translate into perceptible changes in the price of high-calorie food products. Cawley and Kirwan (2011) concur that the cost of farm commodities typically represents a small percentage of food’s retail price. Furthermore, Alston and colleagues (2006, 2008; Alston, 2010) maintain that even if subsidy policies affect food prices, food consumption patterns are relatively unresponsive to changes in market prices.
Production of foods recommended for a healthy diet While the evidence regarding the relationship between subsidies and obesity is mixed, what is clearer is that the current agriculture system fails to produce the mix and quantity of foods necessary for Americans to consume diets recommended by the Dietary Guidelines for Americans. A 2006 Economic Research Service report examining the implications for U.S. agriculture if Americans consumed the recommended fruits, vegetables,
![]()
18 See http://aic.ucdavis.edu/obesity/papers.htm (accessed October 19, 2011).
and whole grains concludes that an additional 7.4 million acres of cropland would need to be harvested per year, and that meeting the dairy guidelines would require the production of an additional 108 billion pounds of dairy products domestically (Buzby et al., 2006).
Buzby and colleagues (2006) found that the average American is eating too much food made with refined grains, but would need to increase whole-grain consumption by more than 200 percent to meet the recommendations of the Dietary Guidelines for Americans (see Figure 6-1 earlier in this chapter). Overall, this means that Americans would need to reduce consumption of total grains by 27 percent. Because it takes less raw wheat to produce a whole-grain product than a similar refined-grain product, the overall drop in demand could translate to 5.6 million fewer acres of wheat each year. Additionally, Buzby and colleagues (2006) point out that an increase in dairy demand (of roughly 65 percent) would likely require an increase in the number of dairy cows, an increase in the volume of feed grains needed, and possibly an increase in the acreage devoted to dairy production. Still, producers of whole grains and dairy have existing mechanisms in place to aid in the availability and affordability of these products. Whole grains are a commodity crop, which provides price and income support, and dairy has an organized pricing, marketing, and support system (and can be subsidized) (Manchester and Blayney, 2001).
However, fruit and vegetable consumption is influenced by several factors, including domestic production, convenience, cost, palatability and personal preference, the desire to cultivate a healthy lifestyle, and the availability and diversity of products procured through trade (Pollack, 2001). Their consumption is positively correlated with income, as well as per capita supply. In the current agriculture policy environment, farmers may be dissuaded from producing fruits and vegetables for a number of reasons, including planting restrictions under commodity programs, financial concerns (e.g., difficulty accessing credit or securing sufficient crop insurance, higher risk, high startup costs, higher production costs), complex production practices, the need for specialized equipment and sufficient labor for harvesting, and agronomic constraints (e.g., limited season, water) (Johnson et al., 2006; Krueger et al., 2010).
Most harvested cropland in the United States is enrolled in the primary commodity payment program, which makes price and income support payments to farmers in proportion to the acreage on which traditional program crops (wheat, feed grains, cotton, rice, oilseeds) are grown. In general, farmers are prohibited from planting and harvesting fruits and vegetables on acres enrolled in the com-
modity payment program. An Economic Research Service analysis found that eliminating planting restrictions would likely have a small market effect, but could have a significant effect on individual producers depending on the costs and returns for producing a particular crop, which vary across regions and over time (Johnson et al., 2006).
Farmers may be deterred from producing fruits and vegetables because of the relative difficulty (compared with other crops) of obtaining loan approval to plant them (Krueger et al., 2010). USDA has collected a body of data on historical yields and prices for the covered commodity crops grown on restricted acres. Such data do not exist for fruits and vegetables, making it difficult for farmers of those crops to project their income in order to obtain loan approval, while the federal government and private entities can more confidently offer loans and financing to producers of commodity crops that are supported by more data.
Price and yield data also are used to determine insurance coverage, which fruit and vegetable farmers rely on to protect against losses. Many fruit and vegetable crops are highly sensitive to weather perturbations, and crop insurance is the primary tool for managing climate-related risks. The lack of data is a factor in the lack of individual crop insurance policies for many fruits and vegetables, leaving farmers to rely on catastrophic coverage under the Non-insured Crop Disaster Assistance Program, which covers about 28 percent of the value of a total loss (Krueger et al., 2010). In an Institute for Agriculture and Trade Policy webinar19 about the challenges to growing healthy foods, fruit and vegetable farmers stated that it was difficult to obtain insurance for growing fruits and vegetables, in part because banks are increasingly risk-averse and perceive those crops to be relatively risky. Krueger and colleagues (2010) offer policy change recommendations designed to remedy the dearth of crop price and yield data.
Local food systems Although local food systems remain a small share of total U.S. agriculture sales, interest has increased in these systems as part of food and agriculture policy. In relation to obesity prevention, the benefits of local food markets remain largely unstudied. In a recent review of local food systems, USDA’s Economic Research Service cites a number of potential benefits, including reducing safety risks, developing social capital, improving environmental quality, reducing energy use, and fostering local economic development. It is unclear what direct role local food systems have in consumer or dietary choices as opposed to
![]()
19 See http://healthyfoodaction.org/?q=hero/what-it-takes-grow-healthy-food-views-farm (accessed December 12, 2011).
availability and access in general (Martinez et al., 2010). Additionally, the precise role of local food systems in improving food security in areas with limited access to fresh foods is difficult to assess (Martinez et al., 2010). Furthermore, prices of local foods depend on the market dynamics in particular locations and may be comparable to or lower or higher than prices of other products or in other markets (Pirog and McCann, 2009).
Agricultural research Cawley and Kirwan (2011, p. 8) maintain that publicly funded agricultural research is “the agricultural policy with potentially the greatest impact on food prices and consumption.” According to Alston and colleagues (2006, 2008), agricultural research and development (R&D) policies are a reason that farm commodity prices have fallen so substantially. Agricultural R&D contributes to lower production and processing costs, increasing farm productivity and thereby making agricultural commodities much less expensive and more abundant than they would otherwise be. One study (Miller and Coble, 2007) that econometrically modeled farm productivity showed that agricultural technology gains have increased food affordability across food groups. Faulkner and colleagues (2010) concur that agricultural R&D has had an impact on consumption and obesity through increased agricultural output and lower farm commodity prices. Alston and Okrent (2009) conclude that compared with farm subsidies, public agricultural research policy has had much larger long-term effects on food prices and consumption.
In summary, this strategy and the associated potential implementing actions address a gap in the current arsenal of obesity prevention strategies. According to Muller and colleagues (2009), food and agriculture issues usually are discussed in silos, without consideration of their effect on public health or other aspects of the food system. Lock and colleagues (2010) note that neither sector considers the complex interactions among agritrade, food consumption patterns, health, and development. This strategy encourages stakeholders to view food and agriculture issues from a broader perspective as the foundation of the nation’s food supply, which in turn impacts consumption behaviors and energy intake. The reach of this strategy is broad and would affect every American.
Indicators for Assessing Progress in Obesity Prevention for Strategy 2-5
Foundational Indicators
• Encouragement and promotion of increased consumption of fresh fruits and vegetables by policy makers, other governmental decision makers, and the business community through competitive pricing and increased availability and production to enable all Americans to consume the amounts of fruits and vegetables recommended by the Dietary Guidelines for Americans.
Source needed for measurement of indicator.
• Formation of a task force to examine the relationships between U.S. agriculture policy and obesity prevention.
Source needed for measurement of indicator.
• Issuance of a government report on the obesity-related implications of the Farm Bill.
Source needed for measurement of indicator.
• Occurrence of congressional hearings on the relationship between U.S. agriculture policy and obesity to inform future agriculture policy.
Source needed for measurement of indicator.
• Establishment of a process for obesity-related review of the Farm Bill.
Source needed for measurement of indicator.
• Introduction of legislative and regulatory policies to increase domestic production of fruits and vegetables.
Source needed for measurement of indicator.
• Maintenance of or increases in funding budgets for USDA research and Land Grant universities.
Source needed for measurement of indicator.
NOTE: USDA = U.S. Department of Agriculture.
INTEGRATION OF STRATEGIES FOR ACCELERATING PROGRESS IN OBESITY PREVENTION
The strategies included in this chapter have one goal: to make the healthy option the routine and affordable option. Increasing access to healthy food and beverage options recommended by the Dietary Guidelines for Americans (HHS/USDA, 2010) and decreasing consumption of solid fats and added sugars (e.g., sugar-sweetened beverages), in particular, are critical steps toward achieving energy balance when implemented in concert with achieving recommended levels of physical activity (Chapter 5). However, adherence to the food patterns recommended by the Dietary Guidelines for Americans is no easy task and will take time. The current obesogenic environment provides unhealthy options that are often more affordable and available than healthy options. For this situation to change, a concerted effort will be required on the part of governments, industry, restaurants and other food service providers, schools and child care providers, and members of the business community/private sector operating places frequented by the public to change the types of foods and beverages sold or offered to consumers such that they provide a range of competitively priced options.
Governments, in particular, have a critical role to play in this effort. Through their policy-making authority, governments (at all levels) can incentivize the purchase of healthier food and beverage options or impose taxes on unhealthy options (e.g., sugar-sweetened beverages). State and local governments also can remove regulatory barriers to and create incentives for retailing of healthy foods, particularly in underserved neighborhoods without ready access to healthy food options. Governments should support the work of community groups and coalitions in their efforts to create healthy food environments in the nation’s communities. And the federal government should examine the extent to which U.S. farm policy can support production of the optimal mix of crops and the farming methods necessary to meet the food patterns recommended in the Dietary Guidelines for Americans.
In short, the strategies presented in this chapter are intended to support the evidence-based recommendations included in the Dietary Guidelines for Americans. Taken in isolation, the individual strategies included in this chapter likely will be insufficient to accelerate progress in obesity prevention. Taken together, however, in concert with comparable changes in physical activity levels, in school environments, in messaging, in health care and worksite environments, and in critical community supports, these strategies can go a long way toward helping Americans meet the food patterns recommended by the Dietary Guidelines for Americans and, in turn, accelerate progress in obesity prevention.
AAP (American Academy of Pediatrics). 2011. Sports drinks and energy drinks for children and adolescents: Are they appropriate? Pediatrics 127(6):1182-1189.
AAP Committee on Nutrition. 2001. The use and misuse of fruit juice in pediatrics. Pediatrics 107(5):1210-1213.
AAP Section on Pediatric Dentistry and Oral Health. 2008. Preventive oral health intervention for pediatricians. Pediatrics 122(6):1387-1394.
AAPD (American Academy of Pediatric Dentistry). 2010. Policy on vending machines in schools. Reference Manual: Oral Health Policies 33(6):55-56.
ABA (American Beverage Association). 2010. Alliances school beverage guidelines final progress report. http://www.ameribev.org/files/240_School%20Beverage%20Guidelines%20Final%20Progress%20Report.pdf (accessed December 5, 2011).
Alinia, S., O. Hels, and I. Tetens. 2009. The potential association between fruit intake and body weight—a review. Obesity Reviews 10(6):639-647.
Alliance for a Healthier Generation. 2006. School beverage and competitive foods guidelines. http://www.healthiergeneration.org/companies.aspx?id=5691 (accessed October 19, 2011).
Alston, J. M. 2010. Farm subsidies, agricultural R&D, and obesity. Presented at the Workshop on Farm and Food Policy and Obesity, May 21-22, 2010, Davis, CA.
Alston, J. M, and A. Okrent. 2009. Farm commodity policy and obesity. Paper presented at Pre-Conference Workshop, Diet and Obesity: Role of Prices and Policies, August 16, 2009, Beijing, China.
Alston, J. M., D. A. Sumner, and S. A. Vosti. 2006. Are agricultural policies making us fat? Likely links between agricultural policies and human nutrition and obesity, and their policy implications. Review of Agricultural Economics 28(3):313-322.
Alston, J. M., J. C. Beghin, H. H. Jensen, L. Kaiser, D. A. Sumner, and S. A. Vosti. 2007. Effects of agricultural policies on human nutrition and obesity. Paper presented at USDA-NRI Human Nutrition and Obesity Project Directors’ Workshop, June 26-28, 2007, Washington, DC.
Alston, J. M., D. A. Sumner, and S. A. Vosti. 2008. Farm subsidies and obesity in the United States: National evidence and international comparisons. Food Policy 33(6):470-479.
AMA (American Medical Association). 2007. Childhood obesity: American Medical Association policy and guidelines. http://www.ama-assn.org/ama1/pub/upload/mm/433/ama-policies-childhood-obesity.pdf (accessed November 13, 2011).
AMC Entertainment. 2011. AMC Theatres® raises the curtain on AMC smart movie snacks & trade. http://www.investor.amctheaters.com/releasedetail.cfm?ReleaseID=561642 (accessed September 16, 2011).
American Dental Association. 2005. Food marketing to kids workshop—comment (project no. P034519). http://ada.org/sections/advocacy/pdfs/nutrition_letter_ftc.pdf (accessed October 21, 2011).
Anderson, L. M., T. A. Quinn, K. Glanz, G. Ramirez, L. C. Kahwati, D. B. Johnson, L. R. Buchanan, W. R. Archer, S. Chattopadhyay, G. P. Kalra, and D. L. Katz. 2009. The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: A systematic review. American Journal of Preventive Medicine 37(4):340-357.
Andreyeva, T., M. W. Long, and K. D. Brownell. 2010. The impact of food prices on consumption: A systematic review of research on the price elasticity of demand for food. American Journal of Public Health 100(2):216-222.
Andreyeva, T., F. J. Chaloupka, and K. D. Brownell. 2011. Estimating the potential of taxes on sugar-sweetened beverages to reduce consumption and generate revenue. Preventive Medicine 52(6):413-416.
Auld, M. C., and L. M. Powell. 2009. Economics of food energy density and adolescent body weight. Economica 76(304):719-740.
Babey, S. H., J. Wolstein, and A. L. Diamant. 2011. Food environments near home and school related to consumption of soda and fast food. Policy Brief UCLA Center for Health Policy Research (PB2011-6):1-8.
Baker, E. A., M. Schootman, E. Barnidge, and C. Kelly. 2006. The role of race and poverty in access to foods that enable individuals to adhere to dietary guidelines. Preventing Chronic Disease 3(3):A76.
Ball, S. C., S. E. Benjamin, and D. S. Ward. 2008. Dietary intakes in North Carolina child-care centers: Are children meeting current recommendations? Journal of the American Dietetic Association 108(4):718-721.
Befort, C., H. Kaur, N. Nollen, D. K. Sullivan, N. Nazir, W. S. Choi, L. Hornberger, and J. S. Ahluwalia. 2006. Fruit, vegetable, and fat intake among non-Hispanic black and non-Hispanic white adolescents: Associations with home availability and food consumption settings. Journal of the American Dietetic Association 106(3):367-373.
Bellisle, F., and M. F. Rolland-Cachera. 2001. How sugar-containing drinks might increase adiposity in children. Lancet 357(9255):490-491.
Blumenthal, D. M., and M. S. Gold. 2010. Neurobiology of food addiction. Current Opinion in Clinical Nutrition & Metabolic Care 13(4):359.
Boone-Heinonen, J., P. Gordon-Larsen, C. I. Kiefe, J. M. Shikany, C. E. Lewis, and B. M. Popkin. 2011. Fast food restaurants and food stores: Longitudinal associations with diet in young to middle-aged adults: The CARDIA study. Archives of Internal Medicine 171(13):1162-1170.
Boutelle, K. N., J. A. Fulkerson, D. Neumark-Sztainer, M. Story, and S. A. French. 2004. Fast food for family meals: Relationships with parent and adolescent food intake, home food availability and weight status. Public Health Nutrition 10:16-23.
Bowman, S. A., S. L. Gortmaker, C. B. Ebbeling, M. A. Pereira, and D. S. Ludwig. 2004. Effects of fast-food consumption on energy intake and diet quality among children in a national household survey. Pediatrics 113(1 Pt 1):112-118.
Bray, G. A., S. J. Nielsen, and B. M. Popkin. 2004. Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity. American Journal of Clinical Nutrition 79(4):537-543.
Bridging the Gap Program. 2011. State sales taxes on regular, sugar-sweetened soda and snacks, 1997-2011. http://www.bridgingthegapresearch.org (accessed December 6, 2011).
Briefel, R. R., and C. L. Johnson. 2004. Secular trends in dietary intake in the United States. Annual Review of Nutrition 24:401-431.
Briefel, R. R., M. K. Crepinsek, C. Cabili, A. Wilson, and P. M. Gleason. 2009a. School food environments and practices affect dietary behaviors of U.S. public school children. Journal of the American Dietetic Association 109(2):S91-S107.
Briefel, R. R., A. Wilson, and P. M. Gleason. 2009b. Consumption of low-nutrient, energy-dense foods and beverages at school, home, and other locations among school lunch participants and nonparticipants. Journal of the American Dietetic Association 109(2):579-590.
Brownell, K. D., and D. S. Ludwig. 2011. The supplemental nutrition assistance program, soda, and USDA policy: Who benefits? Journal of the American Medical Association 306(12):1370-1371.
Brownell, K. D., T. Farley, W. C. Willett, B. M. Popkin, F. J. Chaloupka, J. W. Thompson, and D. S. Ludwig. 2009. The public health and economic benefits of taxing sugar-sweetened beverages. New England Journal of Medicine 361(16):1599-1605.
Buzby, J. C., H. F. Wells, and G. Vocke. 2006. Possible implications for U.S. agriculture from adoption of select dietary guidelines. Economic Research Report No. 31. Washington, DC: USDA, ERS.
California Food Policy Advocates. 2011. Why water? http://www.waterinschools.org/whywater.shtml (accessed October 18, 2011).
California FreshWorks Fund. 2011. Freshworks. http://www.cafreshworks.com/ (accessed October 21, 2011).
Carollo, K. 2011. Movie theatres to sell healthy snacks. http://abcnews.go.com/Health/movie-theatres-sell-healthy-snack-pack-amc-sells/story?id=13311986 (accessed September 16,2011).
Cawley, J., and B. Kirwan. 2011. Agricultural policy and childhood obesity. In Handbook of the social science of obesity, edited by J. Cawley. New York: Oxford University Press.
CDC (Centers for Disease Control and Prevention). 2010. The CDC guide to strategies for reducing consumption of sugar-sweetened beverages. http://www.cdph.ca.gov/SiteCollectionDocuments/StratstoReduce_Sugar_Sweetened_Bevs.pdf (accessed November 13,2011).
CDC. 2011. Health and sustainability guidelines for federal concessions and vending operations. http://www.cdc.gov/chronicdisease/resources/guidelines/food-service-guidelines.htm (accessed October 19, 2011).
CFBAI (Children’s Food and Beverage Advertising Initiative). 2011. Category-specific uniform nutrition criteria. http://www.bbb.org/us/storage/16/documents/cfbai/CFBAI-Category-Specific-Uniform-Nutrition-Criteria.pdf (accessed August 9, 2011).
Chaloupka, F. J., L. M. Powell, and J. F. Chriqui. 2011a. Sugar-sweetened beverages and obesity prevention: Policy recommendations. Journal of Policy Analysis and Management 30(3):662-664.
Chaloupka, F. J., Y. C. Wang, L. M. Powell, T. Andreyeva, J. F. Chriqui, and L. M. Rimkus. 2011b. Estimating the potential impact of sugar-sweetened and other beverage excise taxes in Illinois. Report to the Illinois State Legislature.
Chriqui, J. F., L. Schneider, F. J. Chaloupka, C. Gourdet, A. Bruursema, K. Ide, and O. Pugach. 2010. School district wellness policies: Evaluating progress and potential for improving children’s health three years after the federal mandate: School years 2006-07, 2007-08 and 2008-09, volume 2. Chicago, IL: Bridging the Gap Program, Health Policy Center, Institute for Health Research and Policy, University of Illinois.
Citizens’ Committee for Children of New York, Inc. 2008. Public opinion poll conducted by Beck Research, LLC. Voter preferences for closing the New York State budget gap. http://www.cccnewyork.org/publications/12-12-08CCCPoll.pdf (accessed July 6, 2011).
Cradock, A. L., A. McHugh, H. Mont-Ferguson, L. Grant, J. L. Barrett, C. Wang, and S. L. Gortmaker. 2011. Effect of school district policy change on consumption of sugar-sweetened beverages among high school students, Boston, Massachusetts, 2004-2006. Preventing Chronic Disease 8(4):A74.
CSPI (Center for Science in the Public Interest). 2010. Coke to fleece America by charging more for less, says CSPI. http://www.cspinet.org/new/201001291.html (accessed October 28, 2011).
CSPI. 2011. Life’s sweeter with fewer sugary drinks. http://www.aapd.org/media/Policies_Guidelines/P_VendingMachines.pdf (accessed September 21, 2011).
Daniels, M. C., and B. M. Popkin. 2010. Impact of water intake on energy intake and weight status: A systematic review. Nutrition Reviews 68(9):505-521.
Defense Logistics Agency. 2011. Subsistence. http://www.dscp.dla.mil/subs/ (accessed October 19, 2011).
Defense Manpower Media Center. 2011. Active duty military personnel strengths by regional area and by country (309a). http://media.hotnews.ro/media_serverl/document-2011-05-11-8614257-0-numarul-total-soldati-americani-desfasuratinivel-mondial.pdf (accessed October 19, 2011).
Delaware State Parks. 2011. Healthy eating initiative. http://www.destateparks.com/general_info/healthy-eating.asp (accessed October 21, 2011).
Dennis, E. A., A. L. Dengo, D. L. Comber, K. D. Flack, J. Savla, K. P. Davy, and B. M. Davy. 2010. Water consumption increases weight loss during a hypocaloric diet intervention in middle-aged and older adults. Obesity 18(2):300-307.
DGAC (Dietary Guidelines Advisory Committee). 2010. Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans, 2010, to the Secretary of Agriculture and the Secretary of Health and Human Services. Washington, DC: USDA, ERS.
Dharmasena, S., and O. Capps. 2011. Intended and unintended consequences of a proposed national tax on sugar-sweetened beverages to combat the U.S. obesity problem. Health Economics.
DiMeglio, D. P., and R. D. Mattes. 2000. Liquid versus solid carbohydrate: Effects on food intake and body weight. International Journal of Obesity 24(6):794-800.
Dodgers. 2010. Dodgers and Levy Restaurants to unveil new menus at Dodger Stadium on opening day. The Picante Dog will be reintroduced this season. http://mlb.mlb.com/news/press_releases/press_release.jsp?ymd=20100409&content_id=9174090&vkey=pr_la&fext=.jsp&c_id=la (accessed September 16, 2011).
Epstein, L. H., E. A. Handley, K. K. Dearing, D. D. Cho, J. N. Roemmich, R. A. Paluch, S. Raja, Y. Pak, and B. Spring. 2006. Purchases of food in youth: Influence of price and income. Psychological Science 17(1):82-89.
Epstein, L. H., K. K. Dearing, R. A. Paluch, J. N. Roemmich, and D. Cho. 2007. Price and maternal obesity influence purchasing of low- and high-energy-dense foods. American Journal of Clinical Nutrition 86(4):914-922.
ERS (Economic Research Service). 2004. Diet quality and food consumption: Daily food consumption at different locations: All individuals ages 2 and older. http://www.ers.usda.gov/briefing/DietQuality/data/foods/table5.htm (accessed December 12, 2011).
ERS. 2009. Access to affordable and nutritious food: Measuring and understanding food deserts and their consequences. Report to Congress. Washington, DC: ERS.
ERS. 2011a. Food CPI and expenditures: Table 3t—food away from home: Total expenditures. http://www.ers.usda.gov/Briefing/CPIFoodAndExpenditures/Data/Expenditures_Tables/table3.htm (accessed October 19, 2011).
ERS. 2011b. Food CPI and expenditures: Table 10—food away from home as a share of food expenditures. http://www.ers.usda.gov/Briefing/CPIFoodAndExpenditures/Data/Expenditures_tables/table10.htm (accessed October 19, 2011).
Faulkner, G., P. Grootendorst, V. H. Nguyen, R. Ferrence, R. Mendelson, P. Donnelly, and K. Arbour-Nicitopoulos. 2010. Economic policy, obesity and health: A scoping review. Final report submitted to the Heart and Stroke Foundation of Canada. Toronto, Ontario: Exercise Psychology Unit.
Finkelstein, E. A., C. Zhen, J. Nonnemaker, and J. E. Todd. 2010. Impact of targeted beverage taxes on higher- and lower-income households. Archives of Internal Medicine 170(22) :2028-2034.
Fletcher, J. M., D. E. Frisvold, and N. Tefft. 2011a. Are soft drink taxes an effective mechanism for reducing obesity? Journal of Policy Analysis and Management 30(3):65 5-662.
Fletcher, J. M., D. E. Frisvold, and N. Tefft. 2011b. The proof is in the pudding: Response to Chaloupka, Powell, and Chriqui. Journal of Policy Analysis and Management 30(3):664-665.
FNS (Food and Nutrition Service). 2011a. Healthier U.S. school challenge. http://www.fns.usda.gov/tn/healthierus/index.html (accessed November 13, 2011).
FNS. 2011b. Nutrition assistance programs. http://www.fns.usda.gov/fns/ (accessed October 19, 2011).
Foresight. 2011. The future of food and farming. Final project report. London: The Government Office for Science.
Fox, M. K., A. Gordon, R. Nogales, and A. Wilson. 2009. Availability and consumption of competitive foods in the U.S. public schools. Journal of the American Dietetic Association 109(2):S57-S66.
French, S. A. 2003. Pricing effects on food choices. Journal of Nutrition 133(3):841S-843S.
French, S. A., R. W. Jeffery, M. Story, P. Hannan, and M. P. Snyder. 1997. A pricing strategy to promote low-fat snack choices through vending machines. American Journal of Public Health 87(5):849-851.
French, S. A., R. W. Jeffery, M. Story, K. K. Breitlow, J. S. Baxter, P. Hannan, and M. P. Snyder. 2001a. Pricing and promotion effects on low-fat vending snack purchases: The CHIPS Study. American Journal of Public Health 91(1):112-117.
French, S. A., M. Story, D. Neumark-Sztainer, J. A. Fulkerson, and P. Hannan. 2001b. Fast food restaurant use among adolescents: Associations with nutrient intake, food choices and behavioral and psychosocial variables. International Journal of Obesity and Related Metabolic Disorders 25(12):1823-1833.
Gable, L. 2011. Healthy Weight Commitment Foundation triples membership in first year, launches program in all of its priority areas. http://www.healthyweightcommit.org/news/healthy_weight_commitment_foundation_triples_membership_in_first_year/ (accessed January 30, 2012).
GAO (Government Accountability Office). 2000. Food and commodities: Federal purchases and major regulations that potentially affect prices paid. Washington, DC: GAO.
Garber, A. K., and R. H. Lustig. 2011. Is fast food addictive? Current Drug Abuse Reviews 4(3):146-162.
Gearhardt, A. N., S. Yokum, P. T. Orr, E. Stice, W. R. Corbin, and K. D. Brownell. 2011. Neural correlates of food addiction. Archives of General Psychiatry 68(8):808-816.
Get Out. Be Active. 2011. Re/store Nashville. http://nashville.getoutbeactive.com/2011/02/21/restore-nashville/ (accessed October 21, 2011).
Gidding, S. S., B. A. Dennison, L. L. Birch, S. R. Daniels, M. W. Gillman, A. H. Lichtenstein, K. T. Rattay, J. Steinberger, N. Stettler, and L. Van Horn. 2006. Dietary recommendations for children and adolescents: A guide for practitioners. Pediatrics 117(2):544-559.
Giskes, K., F. van Lenthe, M. Avendano-Pabon, and J. Brug. 2011. A systematic review of environmental factors and obesogenic dietary intakes among adults: Are we getting closer to understanding obesogenic environments? Obesity Reviews 12(5):e95-e106.
Glanz, K., and A. L. Yaroch. 2004. Strategies for increasing fruit and vegetable intake in grocery stores and communities: Policy, pricing, and environmental change. Preventive Medicine 39(Suppl. 2):S75-S80.
Greenwood, M. R. C., P. B. Crawford, and R. M. Ortiz. 2009. Legislative Task Force on Diabetes and Obesity: Report to the California legislature. Santa Clara, CA: Offices of Santa Clara County Supervisors.
Gross, L. S., L. Li, E. S. Ford, and S. Liu. 2004. Increased consumption of refined carbohydrates and the epidemic of type 2 diabetes in the United States: An ecologic assessment. American Journal of Clinical Nutrition 79(5):774-779.
Harris, J. L., M. B. Schwartz, K. D. Brownell, V. Sarda, A. Ustjanauskas, M. Javadizadeh, M. Weinberg, C. Munsell, S. Speers, E. Bukofzer, A. Cheyne, P. Gonzalez, J. Reshetnyak, H. Agnew, and P. Ohri-Vachaspati. 2010. Fast food facts: Evaluating fast food nutrition and marketing to youth. New Haven, CT: Yale Rudd Center for Food Policy and Obesity.
Hawkes, C. 2007. Promoting healthy diets and tackling obesity and diet-related chronic diseases: What are the agricultural policy levers? Food and Nutrition Bulletin 28(Suppl. 2):S312-S322.
Healthy Weight Commitment Foundation. 2011. Healthy Weight Commitment Foundation 2010 annual report. Washington, DC: Healthy Weight Commitment Foundation.
HHS/USDA (U.S. Department of Health and Human Services/U.S. Department of Agriculture). 2010. Dietary Guidelines for Americans. Washington, DC: U.S. Government Printing Office.
Hickson, D., A. Diez Roux, A. Smith, K. Tucker, L. Gore, L. Zhang, and S. Wyatt. 2011. Associations of fast food restaurant availability with dietary intake and weight among African Americans in the Jackson Heart Study, 2000-2004. American Journal of Public Health 101(Suppl.):S301-S309.
Ifland, J. R., H. G. Preuss, M. T. Marcus, K. M. Rourke, W. C. Taylor, K. Burau, W. S. Jacobs, W. Kadish, and G. Manso. 2009. Refined food addiction: A classic substance use disorder. Medical Hypotheses 72(5):518-526
International Council of Shopping Centers. 2008. Inside site selection: Retailers’ search for strategic business locations. http://www.icsc.org/srch/government/briefs/200805_insidesite.pdf (accessed January 3, 2012).
IOM (Institute of Medicine). 2002. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Washington, DC: The National Academies Press.
IOM. 2005. Preventing childhood obesity: Health in the balance, edited by J. P. Koplan, C. T. Liverman, and V. A. Kraak. Washington, DC: The National Academies Press.
IOM. 2006a. Dietary reference intakes: The essential guide to nutrient requirements. Washington, DC: The National Academies Press.
IOM. 2006b. Food marketing to children and youth: Threat or opportunity?, edited by J. M. McGinnis, J. Gootman, and V. I. Kraak. Washington, DC: The National Academies Press.
IOM. 2007a. Nutrition standards for foods in schools: Leading the way toward healthier youth. Washington, DC: The National Academies Press.
IOM. 2007b. Progress in preventing childhood obesity: How do we measure up? Washington, DC: The National Academies Press.
IOM. 2009. Local government actions to prevent childhood obesity. Washington, DC: The National Academies Press.
IOM. 2010. Strategies to reduce sodium intake in the United States. Washington, DC: The National Academies Press.
IOM. 2011. Hunger and obesity: Understanding a food insecurity paradigm: Workshop summary, edited by L. M. Troy, E. A. Miller, and S. Olson. Washington, DC: The National Academies Press.
Jago, R., T. Baranowski, J. C. Baranowski, K. W. Cullen, and D. Thompson. 2007. Distance to food stores and adolescent male fruit and vegetable consumption: Mediation effects. International Journal of Behavioral Nutrition and Physical Activity 4:35.
James, A. 2010. Forget popcorn; executive demands healthy treats at movie theatres. http://www.popeater.com/2010/03/17/healthy-food-movie-theater/ (accessed September 16, 2011).
Jilcott, S. B., T. Keyserling, T. Crawford, J. T. McGuirt, and A. S. Ammerman. 2011. Examining associations among obesity and per capita farmers’ markets, grocery stores/supermarkets, and supercenters in US counties. Journal of the American Dietetic Association 111(4):567-572.
Johnson, D., B. Krissoff, E. Young, L. Hoffman, G. Lucier, and V. Breneman. 2006. Eliminating fruit and vegetable planting restrictions: How would markets be affected? Economic Research Report No. 40. Washington, DC: USDA, ERS.
Johnson, R. K., L. J. Appel, M. Brands, B. V. Howard, M. Lefevre, R. H. Lustig, F. Sacks, A. Steffen, and J. Wylie-Rosett. 2009. Dietary sugars intake and cardiovascular health: A scientific statement from the American Heart Association. Circulation 120:1011-1020.
Kahn, H. S., L. M. Tatham, C. Rodriguez, E. E. Calle, M. J. Thun, and C. W. Heath, Jr. 1997. Stable behaviors associated with adults’ 10-year change in body mass index and likelihood of gain at the waist. American Journal of Public Health 87(5):747-754.
Kant, A. K., and B. I. Graubard. 2004. Eating out in America, 1987-2000: Trends and nutritional correlates. Preventive Medicine 38(2):243-249.
Keystone Forum. 2006. The Keystone Forum on away-from home foods: Opportunities for preventing weight gain and obesity. Washington, DC: The Keystone Center.
Khan, L. K., K. Sobush, D. Keener, K. Goodman, A. Lowry, J. Kakietek, and S. Zaro. 2009. Recommended community strategies and measurements to prevent obesity in the United States. Morbidity and Mortality Weekly Report 58(RR-7):1-26.
Kim, D., and I. Kawachi. 2006. Food taxation and pricing strategies to “thin out” the obesity epidemic. American Journal of Preventive Medicine 30(5):430-437.
Kraak, V. I., M. Story, E. A. Wartella, and J. Ginter. 2011. Industry progress to market a healthful diet to American children and adolescents. American Journal of Preventive Medicine 41(3):322-333.
Krueger, J. E., K. R. Krub, and L. A. Hayes. 2010. Planting the seeds for public health: How the farm bill can help farmers to produce and distribute healthy foods. St. Paul, MN: Farmers’ Legal Action Group, Inc.
Krukowski, R. A., D. S. West, J. Harvey-Berino, and T. Elaine Prewitt. 2010. Neighborhood impact on healthy food availability and pricing in food stores. Journal of Community Health 35(3):315-320.
Larson, N. I., M. T. Story, and M. C. Nelson. 2009. Neighborhood environments: Disparities in access to healthy foods in the U.S. American Journal of Preventive Medicine 36(1):74-81.
Ledoux, T. A., M. D. Hingle, and T. Baranowski. 2010. Relationship of fruit and vegetable intake with adiposity: A systematic review. Obesity Reviews 12(5):e143-e150.
Lee, V., L. Mikkelsen, J. Srikantharajah, and L. Cohen. 2008. Promising strategies for creating healthy eating and active living environments. Oakland, CA: Prevention Institute, Healthy Eating Active Living Convergence Partnership, and PolicyLink.
Lenoir, M., F. Serre, L. Cantin, and S. H. Ahmed. 2007. Intense sweetness surpasses cocaine reward. PLoS One 2(8):e698.
Levy, D. T., K. B. Friend, and Y. C. Wang. 2011. A review of the literature on policies directed at the youth consumption of sugar-sweetened beverages. Advances in Nutrition: An International Review Journal 2(2):182S-200S.
Lewis, L. B., D. C. Sloane, L. M. Nascimento, A. L. Diamant, J. J. Guinyard, A. K. Yancey, and G. Flynn. 2005. African Americans’ access to healthy food options in south Los Angeles restaurants. American Journal of Public Health 95(4):668-673.
Lin, B. H., J. Guthrie, and E. Frazao. 1999. Away-from-home foods increasingly important to quality of American diet. Washington, DC: ERS.
Lock, K., R. D. D. Smith, A. D. Dangour, M. Keogh-Brown, G. Pigatto, C. Hawkes, R. M. Fisberg, and Z. Chalabi. 2010. Health, agricultural, and economic effects of adoption of healthy diet recommendations. The Lancet 376(9753):1699-1709.
Lopez, R. P. 2007. Neighborhood risk factors for obesity. Obesity (Silver Spring) 15(8):2111-2119.
Ludwig, D. S. 2011. Technology, diet, and the burden of chronic disease. Journal of the American Medical Association 305(13):1352-1353.
Manchester, A. C., and D. P. Blayney. 2001. Milk pricing in the United States. Agriculture information bulletin no. 761. Washington, DC: USDA, ERS.
Martinez, S., M. Hand, M. Da Pra, S. Pollack, K. Ralston, T. Smith, S. Vogel, S. Clark, L. Lohr, S. Low, and C. Newman. 2010. Local food systems: Concepts, impacts, and issues. Report no# 97. Washington, DC: USDA, ERS.
Massachusetts Department of Public Health. 2007. Healthy meeting and event guide. http://www.mass.gov/Eeohhs2/docs/dph/com_health/nutrition_phys_activity/healthy_meeting_event_guide.pdf (accessed December 1, 2011).
Mattes, R. D. 1996. Dietary compensation by humans for supplemental energy provided as ethanol or carbohydrate in fluids. Physiology and Behavior 59(1):179-187.
McDonald’s. 2011. McDonald’s announces commitments to offer improved nutrition choices. http://www.aboutmcdonalds.com/mcd/media_center/recent_news/corporate/commitments_to_offer_improved_nutrition_choices.html (accessed August 10, 2011).
Mclntyre, B. D., H. R. Herren, J. Wakhungu, and R. T. Watson. 2009. Agriculture at a crossroads. Washington, DC: International assessment of agriculture knowledge, science, and technology for development. http://www.agassessment.org/reports/IAASTD/EN/Agriculture%20at%20a%20Crossroads_Global%20Report%20(English).pdf (accessed December 12, 2011).
Michels, K. B., B. R. Bloom, P. Riccardi, B. A. Rosner, and W. C. Willett. 2008. A study of the importance of education and cost incentives on individual food choices at the Harvard School of Public Health cafeteria. Journal of the American College of Nutrition 27(1):6-11.
Michimi, A., and M. C. Wimberly. 2010. Associations of supermarket accessibility with obesity and fruit and vegetable consumption in the conterminous United States. International Journal of Health Geographics 9:49.
Mikkelsen, L., and S. Chehimi. 2007. The links between the neighborhood food environment and childhood nutrition. Princeton, NJ: RWJF.
Miller, J. C., and K. H. Coble. 2007. Cheap food policy: Fact or rhetoric? Food Policy 32(1):98-111.
Miller, J. C., and K. H. Coble. 2008. An international comparison of the effect of government agricultural support on food budget shares. Journal of Agricultural and Applied Economics 40(2):551-558.
Morland, K. B., and K. R. Evenson. 2009. Obesity prevalence and the local food environment. Health Place 15(2):491-495.
Morland, K. B., S. Wing, and A. Diez Roux. 2002. The contextual effect of the local food environment on residents’ diets: The atherosclerosis risk in communities study. American Journal of Public Health 92(11):1761-1767.
Morland, K. B., A. V. Diez Roux, and S. Wing. 2006. Supermarkets, other food stores, and obesity: The atherosclerosis risk in communities study. American Journal of Preventive Medicine 30(4):333-339.
Morton, L. W., and T. C. Blanchard. 2007. Starved for access: Life in rural America’s food deserts. Rural Realities 1(4).
Motion Picture Association of America. 2010. Theatrical market statistics. http://www.mpaa.org/Resources/93bbebl6-0e4d-4b7e-b085-3f41c459f9ac.pdf (accessed December 1,2011).
Muckelbauer, R., L. Libuda, K. Clausen, A. M. Toschke, T. Reinehr, and M. Kersting. 2009. Promotion and provision of drinking water in schools for overweight prevention: Randomized, controlled cluster trial. Pediatrics 123(4):e661-e667.
Mulheron, J., and K. Vonasek. 2009. Shaping a healthier generation: Successful state strategies to prevent childhood obesity. Washington, DC: National Governors Association, Center for Best Practices.
Muller, M. J., I. Koertzinger, M. Mast, K. Langnase, and A. Grund. 1999. Physical activity and diet in 5 to 7 years old children. Public Health Nutrition 2(3A):443-444.
Muller, M., A. Tagtow, S. L. Roberts, and M. Erin. 2009. Aligning food systems policies to advance public health. Journal of Hunger and Environmental Nutrition 4(3-4):225-240.
NACCHO (National Association of County and City Health Officials). 2010. Statement of policy, comprehensive obesity prevention. Washington, DC: NACCHO.
National Association of Local Boards of Health. 2010. Position statement: Nutrition, physical activity and obesity. Washington, DC: National Association of Local Boards of Health.
National Prevention Council. 2011. National prevention strategy. America’s plan for better health and wellness. Rockville, MD: Office of the Surgeon General, HHS.
NCES (National Center for Education Statistics). 2010. Table 52. Enrollment of 3-, 4-, and 5-year-old children in preprimary programs, by level of program, control of program, and attendance status: Selected years, 1965 through 2009. http://nces.ed.gov/programs/digest/d10/tables/dt10_052.asp (accessed October 19, 2011).
NCES. 2011. Fast facts. http://nces.ed.gov/fastfacts/display.asp?id=65 (accessed October 19, 2011).
NCI (National Cancer Institute). 2010a. Mean intake of added sugars & percentage contribution of various foods among U.S. population, by age, NHANES 2005-2006. http://riskfactor.cancer.gov/diet/foodsources/added_sugars/table5a.html (accessed December 19, 2011).
NCI. 2010b. Mean intake of energy and mean contribution (kcal) of various foods among U.S. population, by age, NHANES 2005-06. http://riskfactor.cancer.gov/diet/foodsources/energy/table1b.html (accessed December 19, 2011).
Neumark-Sztainer, D., P. J. Hannan, M. Story, J. Croll, and C. Perry. 2003. Family meal patterns: Associations with sociodemographic characteristics and improved dietary intake among adolescents. Journal of the American Dietetic Association 103(3):317-322.
New York City Department of Health and Mental Hygiene. 2011. New York City food standards. http://www.nyc.gov/html/doh/html/cardio/cardio-vend-nutrition-standard.shtml (accessed October 19, 2011).
New York City Government. 2009. Food retail expansion to support health. http://www.nyc.gov/html/misc/html/2009/fresh.shtml (accessed December 1, 2011).
Ni Mhurchu, C., T. Blakely, Y. Jiang, H. C. Eyles, and A. Rodgers. 2010. Effects of price discounts and tailored nutrition education on supermarket purchases: A randomized controlled trial. American Journal of Clinical Nutrition 91(3):736-747.
Nielsen, S. J., A. M. Siega-Riz, and B. M. Popkin. 2002. Trends in energy intake in US between 1977 and 1996: Similar shifts seen across age groups. Obesity Research 10(5):370-378.
Niemeier, H. M., H. A. Raynor, E. E. Lloyd-Richardson, M. L. Rogers, and R. R. Wing. 2006. Fast food consumption and breakfast skipping: Predictors of weight gain from adolescence to adulthood in a nationally representative sample. Journal of Adolescent Health 39(6):842-849.
NRA (National Restaurant Association). 2011. Kids Live Well: About. http://www.restaurant.org/foodhealthyliving/kidslivewell/about/ (accessed August 10, 2011).
O’Donnell, S. I., S. L. Hoerr, J. A. Mendoza, and E. T. Goh. 2008. Nutrient quality of fast food kids meals. American Journal of Clinical Nutrition 88(5):1388-1395.
Ogden, C. L., B. K. Kit, M. D. Carroll, and S. Park. 2011. Consumption of sugar drinks in the United States, 2005-2008. Data brief no. 71. Hyattsville, MD: National Center for Health Statistics.
Padget, A., and M. E. Briley. 2005. Dietary intakes at child-care centers in central Texas fail to meet food guide pyramid recommendations. Journal of the American Dietetic Association 105(5):790-793.
Paeratakul, S., D. P. Ferdinand, C. M. Champagne, D. H. Ryan, and G. A. Bray. 2003. Fast-food consumption among US adults and children: Dietary and nutrient intake profile. Journal of the American Dietetic Association 103(10):1332-1338.
Partnership for a Healthier America. 2011. News and information. http://www.ahealthieramerica.org/#!/news-and-information (accessed October 19, 2011).
Pearson, N., A. Timperio, J. Salmon, D. Crawford, and S. J. Biddle. 2009. Family influences on children’s physical activity and fruit and vegetable consumption. The International Journal of Behavioral Nutrition and Physical Activity 6:34.
Pirog, R., and N. McCann. 2009. Is local food more expensive? A consumer price perspective on local and non-local foods purchased in Iowa. Ames, IA: Leopold Center for Sustainable Agriculture.
Pollack, S. 2001. Consumer demand for fruit and vegetables: The US example. In Changing structure of global food consumption and trade, edited by A. Regmi. Washington, DC: USDA, ERS. Pp. 49-54.
Pollan, M. 2003. The (agri)cultural contradictions of obesity. The New York Times, October 12.
Popkin, B. M., and K. J. Duffey. 2010. Sugar and artificial sweeteners: Seeking the sweet truth. In Nutrition and health: Nutrition guide for physicians, edited by T. Wilson, G. A. Bray, N. J. Temple, and M. B. Struble. New York: Humana Press.
Poti, J. M., and B. M. Popkin. 2011. Trends in energy intake among U.S. children by eating location and food source, 1977-2006. Journal of the American Dietetic Association 111(8):1156-1164.
Powell, L. M. 2009. Fast food costs and adolescent body mass index: Evidence from panel data. Journal of Health Economics 28(5):963-970.
Powell, L. M., and F. J. Chaloupka. 2009. Food prices and obesity: Evidence and policy implications for taxes and subsidies. Milbank Quarterly 87(1):229-257.
Powell, L. M., and J. F. Chriqui. 2011. Food taxes and subsidies: Evidence and policies for obesity prevention. In The Oxford handbook of the social science of obesity, edited by J. Cawley. Pp. 639-664.
Powell, L. M., M. C. Auld, F. J. Chaloupka, P. M. O’Malley, and L. D. Johnston. 2007. Associations between access to food stores and adolescent body mass index. American Journal of Preventive Medicine 33(Suppl. 4):S301-S307.
Powell, L. M., J. Chriqui, and F. J. Chaloupka. 2009. Associations between state-level soda taxes and adolescent body mass index. Journal of Adolescent Health 45(Suppl. 3):S57-S63.
Powell, L. M., E. Han, and F. J. Chaloupka. 2010. Economic contextual factors, food consumption, and obesity among U.S. adolescents. Journal of Nutrition 140(6):1175-1180.
Randolph, W., and K. Viswanath. 2004. Lessons learned from public health mass media campaigns: Marketing health in a crowded media world. Annual Review of Public Health 25:419-437.
Reedy, J., and S. M. Krebs-Smith. 2010. Dietary sources of energy, solid fats, and added sugars among children and adolescents in the United States. Journal of the American Dietetic Association 110(10):1477-1484.
Ritchie, L. D., S. Whaley, K. Hecht, K. Chandran, M. Boyle, P. Spector, S. Samuels, and P. Crawford. 2012. Participation in the Child and Adult Care Food Program is associated with more nutritious foods and beverages in childcare. Childhood Obesity. In press.
Rogers, K. 2011. Accelerating progress in obesity prevention. Presented at the Farm and Food Policy: Relationship to Obesity Prevention, May 19, 2011, Washington, DC.
Rose, D., and R. Richards. 2004. Food store access and household fruit and vegetable use among participants in the US food stamp program. Public Health Nutrition 7(8):1081-1088.
Rudd Center for Food Policy and Obesity. 2010. Public opinion data. http://www.yaleruddcenter.org/what_we_do.aspx?id=273 (accessed July 19, 2011).
Rudd Center for Food Policy and Obesity. 2011. Sugar-sweetened beverage taxes and sugar intake: Policy statements, endorsements, and recommendations. New Haven, CT: Yale University Rudd Center on Food Policy and Obesity Prevention.
RWJF (Robert Wood Johnson Foundation). 2009. Action strategies toolkit: A guide for local and state leaders working to create healthy communities and prevent childhood obesity. Princeton, NJ: RWJF.
RWJF. 2011. Summary of food marketing research roundtable. Presented at the RWJF Food Marketing Research Roundtable, April 4-5, 2011, Washington, DC.
Schaffer, H., D. B. Hunt, and D. E. Ray. 2007. US agricultural commodity policy and its relationship to obesity. Background paper developed for the Wingspread Conference on Childhood Obesity, Healthy Eating & Agriculture Policy. Knoxville, TN: Agricultural Policy Analysis Center, University of Lennessee.
Schmidt, M., S. G. Affenito, R. Striegel-Moore, P. R. Khoury, B. Barton, P. Crawford, S. Kronsberg, G. Schreiber, E. Obarzanek, and S. Daniels. 2005. Fast-food intake and diet quality in black and white girls: The National Heart, Lung, and Blood Institute Growth and Health Study. Archives of Pediatrics and Adolescent Medicine 159(7):626-631.
Schoonover, H., and M. Muller. 2006. Food without thought: How U.S. farm policy contributes to obesity. Minneapolis, MN: The Institute for Agriculture and Trade Policy.
Schulze, M. B., J. E. Manson, D. S. Ludwig, G. A. Colditz, M. J. Stampfer, W. C. Willett, and F. B. Hu. 2004. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. Journal of the American Medical Association 292(8):927-934.
Sharma, L. L., S. P. Teret, and K. D. Brownell. 2010. The food industry and self-regulation: Standards to promote success and to avoid public health failures. American Journal of Public Health 100(2):240-246.
Smith, T. A., B. Lin, and J. Lee. 2010. Taxing caloric sweetened beverages: Potential effects on beverage consumption, calorie intake, and obesity. Economic Research Report No. 100. Washington, DC: USDA, ERS.
Stein, J. 2009. A Dodger Dog with a side of yogurt? http://articles.latimes.com/2009/apr/12/science/sci-stadiumfare12 (accessed December 1, 2011).
Stookey, J. D., F. Constant, C. D. Gardner, and B. M. Popkin. 2007. Replacing sweetened caloric beverages with drinking water is associated with lower energy intake. Obesity 15(12):3013-3022.
Stookey, J. D., F. Constant, B. M. Popkin, and C. D. Gardner. 2008. Drinking water is associated with weight loss in overweight dieting women independent of diet and activity. Obesity 16(11):2481-2488.
Story, M., K. M. Kaphingst, and S. French. 2006. The role of child care settings in obesity prevention. Future of Children 16(1):143-168.
Story, M., K. M. Kaphingst, R. Robinson-O’Brien, and K. Glanz. 2008. Creating healthy food and eating environments: Policy and environmental approaches. Annual Review of Public Health 29:253-272.
Sturm, R., L. M. Powell, J. F. Chriqui, and F. J. Chaloupka. 2010. Soda taxes, soft drink consumption, and children’s body mass index. Health Affairs 29(5):1052-1058.
Taber, D. R., J. F. Chriqui, L. M. Powell, and F. J. Chaloupka. 2011. Banning all sugar-sweetened beverages in middle schools: Reduction of in-school access and purchasing but not overall consumption. Archives of Pediatrics and Adolescent Medicine [epub ahead of print].
The Chicago Council on Global Affairs. 2011. Bringing agriculture to the table. Chicago, IL: The Council on Global Affairs.
The City of New Orleans. 2011. Fresh food retailer initiative. http://www.nola.gov/HOME/FreshFoodRetailersInitiative (accessed December 12, 2011).
The Food Trust. 2011. Supermarket campaign. http://www.thefoodtrust.org/php/programs/super.market.campaign.php (accessed July 15, 2011).
The Reinvestment Fund. 2010. Pennsylvania fresh food financing initiative. http://www.trfund.com/resource/downloads/Fresh_Food_Financing_Initiative_Comprehensive.pdf (accessed November 13, 2011).
The Walt Disney Company. 2011. Promoting healthy lifestyles. http://corporate.disney.go.com/citizenship2010/familyentertainment/overview/promotinghealthylifestyles/ (accessed January 27, 2012).
Thomas, A. 2011. Healthier food initiative. Presented at the Farm and Food Policy: Relationship to Obesity Prevention, May 19, 2011, Washington, DC.
Thompson, O., C. Ballew, K. Resnicow, A. Must, L. G. Bandini, H. Cyr, and W. H. Dietz. 2004. Food purchased away from home as a predictor of change in BMI Z-score among girls. International Journal of Obesity 28:282-289.
Tillotson, J. E. 2003. Pandemic obesity: Agriculture’s cheap food policy is a bad bargain. Nutrition Today 38:186.
Tillotson, J. E. 2004. America’s obesity: Conflicting public policies, industrial economic development, and unintended human consequences. Annual Review of Nutrition 24(1):617-643.
TransForm Baltimore. 2011. Transform Baltimore: The zoning code rewrite. http://www.transformbaltimore.net/portal/ (accessed October 21, 2011).
Treuhaft, S., and A. Karpyn. 2010. The grocery gap: Who has access to healthy food and why it matters. Oakland, CA and Philadelphia, PA: PolicyLink and The Food Trust.
Trust for America’s Health and RWJF. 2011. F. as in fat: How obesity threatens America’s future, edited by J. Levi, L. M. Segal, R. St. Laurent and D. Kohn. Washington, DC: Trust for America’s Health.
Turner, L., and F. J. Chaloupka. 2010. Wide availability of high-calorie beverages in U.S. elementary schools. Archives of Pediatrics and Adolescent Medicine 165(3):223-228.
UNC Carolina Population Center. 2011. Evaluation of food industry initiatives to reduce obesity. http://www.cpc.unc.edu/projects/nutrans/policy/food-industry-eval (accessed January 3, 2012).
U.S. Census Bureau. 2007. Census of government employment. Table 1. Summary of public employment and payrolls by type of government: March 2007. http://www2.census.gov/govs/apes/emp_compendium.pdf (accessed October 21, 2011).
U.S. Census Bureau. 2011. S2601b. Characteristics of the group quarters population by group quarters type data set: 2005-2009 American community survey 5-year estimates. http://factfindescensus.gov/servlet/STTable?_bm=y8c-geo_id=01000US8c-qr_name=ACS_2009_5YR_G00_S2601B&-ds_name=ACS_2009_5YR_G00_8c-redoLog=false (accessed October 19, 2011).
U.S. Surgeon General. 2010. The Surgeon General’s vision for a healthy and fit nation. Washington, DC: HHS.
Wakefield, M. A., B. Loken, and R. C. Hornik. 2010. Use of mass media campaigns to change health behaviour. The Lancet 376(9748):1261-1271.
Wallinga, D., H. Schoonover, and M. Muller. 2009. Considering the contribution of US agricultural policy to the obesity epidemic: Overview and opportunities. Journal of Hunger and Environmental Nutrition 4(1):3-19.
Wang, Y. C., D. S. Ludwig, K. Sonneville, and S. L. Gortmaker. 2009. Impact of change in sweetened caloric beverage consumption on energy intake among children and adolescents. Archives of Pediatrics and Adolescent Medicine 163(4):336-343.
Wang, Y. C., P. Coxson, Y.-M. Shen, L. Goldman, and K. Bibbins-Domingo. 2012. A penny-per-ounce tax on sugar-sweetened beverages would cut health and cost burdens of diabetes. Health Affairs 31(1):199-207.
Welsh, J. A., A. J. Sharma, L. Grellinger, and M. B. Vos. 2011. Consumption of added sugars is decreasing in the United States. American Journal of Clinical Nutrition 94(3):726-734
Wendt, M., and J. E. Todd. 2011. The effect of food and beverage prices on children’s weights. Economic Research Report No. 118. Washington, DC: USDA, ERS.
White House Task Force on Childhood Obesity. 2010. Solving the problem of childhood obesity within a generation: White House Task Force on Childhood Obesity report to the President. Washington, DC: Executive Office of the President of the United States.
WHO (World Health Organization). 2004. Global strategy on diet, physical activity, and health. Geneva, Switzerland: WHO.
Wiecha, J. L., D. Finkelstein, P. J. Troped, M. Fragala, and K. E. Peterson. 2006. School vending machine use and fast-food restaurant use are associated with sugar-sweetened beverage intake in youth. Journal of the American Dietetic Association 106(10):1624-1630.
Woodward-Lopez, G., J. Kao, and L. Ritchie. 2010. To what extent have sweetened beverages contributed to the obesity epidemic? Public Health Nutrition 1-11.
Wootan, M. G., A. Batada, and E. Marchlewicz. 2008. Kids meals. Obesity on the menu. Washington, DC: Center for Science in the Public Interest.
Zenk, S. N., A. J. Schulz, B. A. Israel, S. A. James, S. Bao, and M. L. Wilson. 2005. Neighborhood racial composition, neighborhood poverty, and the spatial accessibility of supermarkets in metropolitan Detroit. American Journal of Public Health 95(4):660-667.
Zoumas-Morse, C., C. L. Rock, E. J. Sobo, and M. L. Neuhouser. 2001. Children’s patterns of macronutrient intake and associations with restaurant and home eating. Journal of the American Dietetic Association 101(8):923-925.


















































































