Socioeconomic Success and Health in Later Life: Evidence from the Indonesia Family Life Survey1
Firman Witoelar, John Strauss, and Bondan Sikoki
Indonesia has been undergoing a health and nutrition transition over the past 20 years and more. Overall, health of the population has been improving, as indicated by a continuing rise in attained adult heights for men and women over the entire 20th century (heights of both men and women increased by about 1 cm per decade over this period, Strauss and Thomas, 1995; Strauss et al., 2004). In Indonesia, infectious diseases caused 72% of all deaths in 1980; by 1992, noninfectious conditions caused more than half of the country’s deaths (Indonesian Public Health Association, 1993). As part of the reason for the increase in deaths from chronic conditions, body mass indices (BMIs) have been rising for middle-aged people and the elderly, as has been noted more generally in Asia (see, for example, Monteiro et al., 2004; Popkin, 1994; Strauss and Thomas, 2008; Strauss et al., 2004). In Indonesia, body mass among the aged population has been rising rapidly, especially for women, as has waist circumference. On the other hand, hemoglobin levels have also been rising, though from low levels, leading to improved health. Yet, other health measures have been fairly steady as shown in the Indonesia Family Life Survey (IFLS),
____________
1 An earlier version of this chapter was presented at the annual meetings of the Population Association of America, April 2009, Detroit, Michigan, and the World Congress of the International Union for the Scientific Study of Population, October 2009, Marrakesh, Morocco. We thank Paul Heaton, James P. Smith, and other participants of the RAND Labor and Population Workshop for their very helpful comments. All errors are ours. Witoelar gratefully acknowledges the financial support of the World Bank’s Research Support Budget. The views expressed here do not necessarily reflect those of the World Bank and of its member countries.
including the prevalence of hypertension. In terms of measures of health outcomes, while some trends seem upwards, specifically the movement out of undernutrition and communicable diseases, there seems at the same time to have been a movement toward more risk factors that are likely to lead to future chronic problems, but not universally so. Related to this, other symptoms, such as low levels of HDL cholesterol, are very high, especially for men, and the extremely high rate of current male smoking does not yet show a downward trend (Witoelar, Strauss, and Sikoki, 2009).
The backdrop of these important health and nutrition transitions is a country where the formal social safety system is still in its infancy and policies and programs that are designed to address specific challenges brought about by an aging population are still lacking.2,3 As in many developing countries in the region, elderly in Indonesia mostly rely on children and family networks for old-age support, either through co-residency or transfers (Cameron and Cobb-Clark, 2008). With the elderly population becoming more exposed to risk of chronic and noncommunicable diseases, the issues of elderly care are becoming increasingly important.4 Understanding the socioeconomic status (SES) correlates of elderly health outcomes will help to improve knowledge that could be useful in designing health as well as social programs to improve the well-being of the elderly in Indonesia.
In this chapter, we document the health and nutrition transition that the elderly population in Indonesia has undergone in the 15 years between 1993 and 2008, using the four full waves of the Indonesia Family Life Survey (IFLS).5 This period spans a period of rapid economic growth from 1993 to 1997, a major financial crisis starting at the end of 1997 going through 1998 and 1999, and a major economic expansion starting in 2000, continuing through early 2008. IFLS is uniquely suited to look at changes over time, both for age groups and for birth cohorts in Indonesia, as it is a panel survey covering most of the country. Indonesia, like other developing countries in Asia and Latin America, has been aging rapidly. In 1980, only 3.4% of the population was aged 65 and older; by 2010, it was projected to be 6.1%, and by 2040, 14.7% (Kinsella and He, 2009). The population aged 65 and older is projected to double between 2000 and 2020 and again by 2040. We examine the IFLS sample 45 years and older
____________
2 An important bill on social safety nets was passed in October 2004 (Law no 40/2004). It includes a number of provisions that are important for elderly such as pensions, old-age savings, and health coverage, but has yet to be implemented.
3 See Abikusno (2009) for a review of past and recent laws and government policies related to elderly in Indonesia.
4 Van Eeuwijk (2006) argues that the epidemiological health transition has necessitated a shift from a “cure” to “care” paradigm in healthcare delivery in urban areas in Indonesia.
5 IFLS1 was fielded in 1993, IFLS2 in 1997, IFLS3 in 2000, and IFLS4 in 2007-2008
in each of the four waves, pretending that we have a series of independent cross-sections. Age 45 is chosen because it corresponds to early retirement age in Indonesia and is the age cutoff used in the new Health and Retirement Study type surveys being done in Asia.6
We focus in this chapter on examining changes over time for a series of health outcomes and behaviors, mainly using biomarkers. The health outcomes that we focus on are body mass index (BMI), waist circumference (a measure of body fat, given BMI), blood hemoglobin, total and HDL cholesterol levels, hypertension, cognition measured by word recall, and an index of depression (the short CES-D).7 This is a much broader set of health indicators than is usually analyzed, in large part because such a rich set of health data is not usually available in broad-purposed socioeconomic surveys.
In addition to looking at trends in IFLS, we examine the correlations between these health outcomes and behaviors, and a series of SES variables: own education and the log of household per-capita expenditure (pce). In all cases, we examine the data separately for men and women and include age, period, and cohort effects (normalized), as well as dummy variables for province and rural area, alone and interacted with year of survey.
We find that the nutrition transition has progressed strongly in Indonesia over the 15-year period 1993-2008. Large increases in overweight have occurred for both men and women aged 45 years and older. For women, a full 33% are now overweight and for men, 10 percentage points less. On the other side of the coin, underweight has dramatically decreased, although among the current older population, it is still a problem. Related to nutrition, blood hemoglobin has improved over this period, especially since 2000. However, levels of hemoglobin are still low by international standards. On the other hand, hypertension has been constant over the period since 1997, since IFLS has been measuring it.
We find strong, positive correlations between SES and good health outcomes in most cases except hypertension and cholesterol. We recognize that causality runs both ways. We allow for interactions between one SES variable—education—and age and find that education tends to suppress the negative impact of age on many health outcomes. For hypertension we have data not only on measured prevalence, but also on doctor
____________
6 These are the China Health and Retirement Longitudinal Study (CHARLS), Japanese Study of Aging and Retirement (JSTAR), Korean Longitudinal Study of Ageing (KLoSA), and Longitudinal Study of Aging in India (LASI).
7 We also examine the degree to which older Indonesians have difficulties with Activities of Daily Living and Instrumental Activities of Daily Living (ADLs and IADLS, respectively) and their self-reported general health status, as well as two important inputs for elderly health: smoking and physical activity. The results are available in Witoelar, Strauss, and Sikoki (2009).
diagnosis. We find a very high level of underdiagnosis of hypertension, which is strongly, negatively associated with SES for women, but not associated for men. Even among those who have been diagnosed, a large proportion claim not to be taking medications. We speculate that for other chronic health conditions, the degree of underdiagnosis is likely to also be quite high, suggesting the need for major health campaigns directed both at the general population and very specifically at doctors and other health providers.
DATA AND METHODOLOGY
The Indonesia Family Life Survey is a general-purpose survey designed to provide data for studying many different behaviors and outcomes. The survey contains a wealth of information collected at the individual and household levels, including indicators of economic and noneconomic well-being. In particular for this chapter, IFLS collects a rich set of information on health outcomes, in particular on many biomarkers.
IFLS is an ongoing longitudinal survey. The first wave, IFLS1, was conducted in 1993-1994. The survey sample represented about 83% of the Indonesian population living in 13 of the country’s 26 provinces.8 IFLS2 followed up with the same sample four years later, in 1997. IFLS2 ended in December 1997, just as the financial crisis was beginning, so it serves as an immediate baseline. IFLS3 was fielded on the full sample in 2000, three years after the crisis, and IFLS4 in 2007-2008, some 10 years after. Thus, IFLS from 1993 to 2008 provides a period of still-strong economic growth, followed by a major economic crash and recovery.
In this chapter, for some purposes we treat each year as though it were an independent cross-section, in order to explore how prevalence of different measures have evolved cross-sectionally for a particular age group, those aged 45 and older. For the regressions, though, we test pooling across years and then pool with some interactions after we fail to reject that SES coefficients are the same over the four waves. We do not employ dynamic models in this chapter and so do not use the panel nature directly; we will deal with these topics in another chapter.
One potential worry in a study like this over a 15-year period is sample
____________
8 Public-use files from IFLS1 are documented in six volumes under the series title The 1993 Indonesian Family Life Survey, DRU-1195/1-6-NICHD/AID, The RAND Corporation, December 1995. IFLS2 public-use files are documented in seven volumes under the series The Indonesia Family Life Survey, DRU-2238/1-7-NIA/NICHD, RAND, 2000. IFLS3 public-use files are documented in six volumes under the series The Third Wave of the Indonesia Family Life Survey (IFLS3), WR-144/1-NIA/NICHD. IFLS4 public-use files are documented in the six volumes under the series The Fourth Wave of the Indonesia Family Life Survey (IFLS4), WR-675/1-NIA/NICHD.
attrition. However, the attrition in IFLS is quite low. In IFLS1, 7,224 households were interviewed, and detailed individual-level data were collected from over 22,000 individuals. In IFLS2, 94.4% of IFLS1 households were re-contacted (interviewed or died). In IFLS3, the re-contact rate was 95.3% of IFLS1 dynasty households (any part of the original IFLS1 households). In IFLS4, the recontact rate of original IFLS1 dynasties was 93.6% (of course, the period between waves was seven years, not three). Among IFLS1 dynasties, 90.3% were either interviewed in all four waves or died. Of some 6,523 households, 6,329, or 87.6%, were actually interviewed in all four waves.9 These re-contact rates are as high as or higher than most longitudinal surveys in the United States and Europe. For the regressions, we do not weight, but for the descriptive tables we do weight, both for the sampling procedures (which oversampled urban areas and some outer provinces) and for attrition (see Strauss et al., 2009, for details of weighting). The weights provide the inverse probability that a household and individual were sampled and appeared in IFLS in each wave.
To look at the associations of SES and health outcomes under a multivariate context, we run a set of regressions. The specification, which is used for all health outcomes analyzed in this chapter, is as follows. In results not shown, we first test for pooling across waves, for those health outcomes that we have data for multiple waves. We find that the age, schooling, and pce coefficients are not significantly different across years although the province/rural-urban dummies are (results are available upon request). Consequently, we pool the data across rounds of the survey (IFLS1, 2, 3, and 4), but allow for interactions between year dummies and the province/rural-urban dummies. These interactions will capture community/time differences in prices, healthcare availability and quality, and health conditions. The sample for each regression consists of adults who are aged 45 and older at the time of the survey, and for whom the physical measurements (or other measures) are available. Estimation for males and females are done separately. We use ordinary least squares for continuous dependent variables and linear probability (LP) model for binary dependent variables. LP model estimates are consistent for estimating average partial effects of the regressors, which is what we are interested in. Robust standard errors of the regression coefficients are computed, which also allow for clustering at the community level. By using robust standard errors for the linear probability regressions, we ensure that these standard error estimates are consistent.
Table 13-1 shows means and standard deviations from the IFLS4 data for our covariates. We create dummy variables for age indicating whether an individual is aged 55 and older, 65 and older, and 75 and older. In this
____________
9 See Thomas et al. (forthcoming) for a more detailed discussion of IFLS attrition rates.
TABLE 13-1 Descriptive Statistics of the Socioeconomic Variables, 2007
| Male (N = 4,014) | Female (N = 4,629) | |||
| Variable | Mean | Std. Dev | Mean | Std. Dev |
| Age (yrs) | 57.94 | 10.465 | 58.47 | 10.786 |
| Age (dummy vars.): | ||||
| 45-54 | 0.466 | 0.499 | 0.455 | 0.498 |
| 55-64 | 0.272 | 0.445 | 0.261 | 0.439 |
| 65-74 | 0.178 | 0.383 | 0.191 | 0.393 |
| 75+ | 0.084 | 0.277 | 0.093 | 0.291 |
| Years of education (yrs) | 6.046 | 4.661 | 4.015 | 4.273 |
| School completion (dummy vars.) | ||||
| No schooling | 0.150 | 0.357 | 0.337 | 0.473 |
| Some primary school | 0.281 | 0.450 | 0.290 | 0.454 |
| Completed primary school | 0.276 | 0.447 | 0.206 | 0.405 |
| Completed junior high | 0.293 | 0.455 | 0.167 | 0.373 |
| Monthly pce (Rp) | 562,568 | 834,740 | 590,319 | 1,064,606 |
| Residence (dummy vars.) | ||||
| Rural | 0.503 | 0.500 | 0.492 | 0.500 |
| Province | ||||
| North Sumatra | 0.055 | 0.229 | 0.061 | 0.239 |
| West Sumatra | 0.049 | 0.216 | 0.055 | 0.229 |
| South Sumatra | 0.047 | 0.211 | 0.045 | 0.208 |
| Lampung | 0.044 | 0.205 | 0.036 | 0.187 |
| Jakarta | 0.064 | 0.245 | 0.060 | 0.238 |
| West Java | 0.166 | 0.372 | 0.157 | 0.364 |
| Central Java | 0.138 | 0.345 | 0.145 | 0.352 |
| Yogyakarta | 0.072 | 0.259 | 0.074 | 0.261 |
| East Java | 0.155 | 0.362 | 0.162 | 0.369 |
| Bali | 0.054 | 0.226 | 0.054 | 0.226 |
| West Nusa Tenggara | 0.059 | 0.236 | 0.058 | 0.234 |
| South Kalimantan | 0.047 | 0.211 | 0.040 | 0.195 |
| South Sulawesi | 0.049 | 0.215 | 0.052 | 0.223 |
SOURCE: Data from IFLS4.
way, the coefficients on the dummy variables indicate the marginal change from the next lowest age group (not from the omitted group) of being in the reference group. Similarly, for education, the dummy coefficients show the marginal change over the next lowest education group: We use a dummy variable for having at least some primary education, completed primary school or more, and completed junior high school or more. For per capita expenditures (pce), we take logs and then use a linear spline with a knot at the median of log pce.10 For health measures that we have
____________
10 The coefficient on the second log pce variable we report is the change in the coefficient from the slope to the left of the knot point.
data on from more than one wave, we include dummy variables if the observations are from 1997 and after (if 1993 observations are available), 2000 and after, or 2007, and, as stated, interaction of these period effects with province and province-rural dummies. For the few health variables that we only have data for 2007-2008, we just include the province and province-rural dummies. Also for measures that data exist for multiple waves, we use five-year birth cohort dummy variables.11,12 It is, of course, not possible to separately identify age, cohort, and period effects without untestable assumptions made. In our case, we aggregate ages into 10-year intervals and birth cohorts into five-year groups.13 Because we are pooling the four waves for each age group, we have several birth-year cohorts, helping identification.
Nevertheless, we are not so interested in the age, cohort, or year effects as we are in the SES coefficients. However, if we left out age and/or birth cohort variables, we would bias the education coefficients positively, as the estimated education impacts would then also capture cohort effects. This would arise because younger birth cohorts have more schooling and also faced better health conditions when they were babies and in the fetus, compared to older cohorts. There is an accumulation of evidence now that better health conditions when young are associated with better health in old age (for instance, Barker, 1994; Gluckman and Hanson, 2005; and Strauss and Thomas, 2008, for an economist’s perspective).
We have to be careful not to interpret the SES coefficients from these regressions as causal (Strauss and Thomas, 1995, 1998, 2008). Causality runs in both directions between SES and health outcomes. However, we add one variable that can help some in this regard, an interaction between years of education and de-meaned age. Using de-meaned age is helpful for interpretation because then the coefficients on the education dummies show the differentials at the sample mean age. The interaction coefficient then shows how that differential changes with age differences compared to the mean age. What we are looking for is whether education mitigates the powerful negative influence of aging on our health outcomes. If it does, then this is more consistent with a causal interpreta-
____________
11 The birth-year cohort dummy variables included are as follows: -1928, 1929-1933, 1934-1938, 1939-1943, 1944-1948, 1949-1953, 1954-1958, with 1959-1963 omitted as the base.
12 For health measures that we only have data from 2007, of course, we do not use either year or birth cohort dummies, but we still use the age dummies. For these cases, the age dummies must be interpreted with even more caution, since it is not possible to disentangle age from birth cohort from time effects.
13 The year dummy variables are aged 55 and older, 65 and older, 75 and older, with 45 and older omitted as the base.
tion of our education coefficients.14,15 Studies of child height have shown that mother’s education has its largest impact on heights when the child is less than three years (Barrera, 1990; Thomas, Strauss, and Henriques, 1990, 1991). This is thought to be the period during which children are most vulnerable to infection from dirty water and ill-prepared food, so that mother’s schooling might well have its biggest impact during that period. Among the mechanisms for this enhanced impact is thought to be an allocative efficiency effect of mother’s schooling, knowing, or being better at acquiring information regarding what inputs are better and safer for children, such as boiling water. A similar argument might be applied to our measures of health, which are largely general; at older ages, people are more susceptible to problems, hence one’s own schooling may have a larger allocative impact at these ages (though possibly from affecting health inputs and behaviors from years earlier).
RESULTS
Physical Measurement:
Anthropometry, Hemoglobin Level, and Hypertension BMI
We first look at a number of biomarkers: BMI, waist circumference, blood hemoglobin levels, and hypertension.16 BMI, which is weight (in kg)
____________
14 While this interaction coefficient could also represent a nonlinear effect of schooling, the fact that we enter schooling with level dummies protects us in part against this potential confounding effect.
15 Another empirical strategy we could have taken would be to include household fixed effects. That would have captured all factors at the household level, but still would not have addressed the issue of unobserved individual factors. Household fixed effects would have required there to be multiple men aged 45 and older within the same household and likewise for adult women. We examined the cell sizes for our samples, using as our definition of household, the “dynastic” 1993 households (that is combining all households that split from a given 1993 household into one household). We found that an average dynastic household contained 1.1 adult male or adult female members aged 45 and older. In the case of CES-D, for example, we had 3,900 individual men in our sample and 3,683 dynasties. That means we only had 217 individuals from multiple member households, and it is this group that would be used to estimate the SES coefficients. We judged that this was too small a group from which to reliably get estimates. This case is typical. For health outcomes that we measure over time, like BMI, we have numerous persons for whom we have multiple measures over waves. We thus could have used individual fixed effects in that case, but that should be part of a dynamic analysis, which is a different research exercise than this chapter.
16 Heights were measured using a lightweight SECA aluminum height board, the SECA 214 portable stadiometer. Weights were measured using a portable digital scale, the CAMRY EB6171. Hemoglobin was measured using a small, hand-held meter, the Hemocue Hb301 analyzer. A finger prick was made using a lancet and a drop of blood inserted into the Hemocue microcuvette. Blood pressure was taken with a digital meter, the Omron HEM 712c meter. Total and HDL cholesterol were measured using a CardiochekPA meter. This meter measures over the range 100-400 for total cholesterol and 15-100 for HDL.
divided by height (in m) squared, provides a convenient summary of height and weight of adults. We use World Health Organization (WHO) standards whereby adults whose BMI is under 18.5 are considered undernourished and those whose BMI is 25 or greater are considered overweight. Extreme values of BMI are associated with elevated hypertension, diabetes, and other causes of mortality.
Figures 13-1a and 13-1b plot the cumulative distribution functions (CDF) of BMI for adult males and females aged 45 and older using data from IFLS1, 2, 3, and 4. The CDFs are shifted down for each year after 1993 for both men and women. The shift for 2007 from 2000 is especially large. The fact that the CDFs do not cross means that each successive year first order stochastically dominates the last. In the case of BMI, unlike income, stochastic dominance across the entire distribution does not have a clear welfare implication. On the one hand, undernourishment is unambiguously dropping, but on the other hand, overweight is unambiguously increasing. Table 13-2 shows the percentages of adults aged 45 and older who are undernourished and overweight in 2007. The percentage of adult males who are undernourished was around 17.5 in 2007. This number continues the decline from 28.3 in 1993 to 23.5 in 2000 (see Witoelar, Strauss, and Sikoki, 2009).17 The numbers are similar for women, with around 17.4% who were undernourished in 2007, compared to 29.7% in 1993. But what is more interesting has to do with the proportion of those overweight. In 2007, around 31% of elderly women have BMI 25 or over, more than double the fraction of 1993. Among elderly men in 2007, 17% are overweight, compared to 8.5% in 1993. Among the different age groups, it is the 45-54 age group who have both the lowest fraction of undernourished and the largest fraction of overweight.
The increase over the years and the substantial degree of overweight suggests that overnutrition and health conditions associated with it have become increasingly important in Indonesia. At the same time, under-nutrition has not entirely disappeared, though its magnitude among the aged has sharply dropped.
Holding BMI constant, greater waist circumference increases the risks of various cardiovascular diseases. For people who are overweight or obese, the risk of future mortality is higher if their waist circumference is greater than 120 cm for men or 88 cm for women. The CDF of waist circumference for both men and women shifted to the right between 2000 and 2007 (see Witoelar, Strauss, and Sikoki, 2009). Around 30% of women aged 45 and older in 2007 had waist circumferences that are greater than 88 cm compared to around 20% in 2000. This CDF does not control for BMI changes, so a lot of the increase in waist circumference may simply be
____________
17 Percentages of adults 45+ who are undernourished and overweight in all four survey waves of the IFLS are presented in Witoelar, Strauss, and Sikoki (2009).
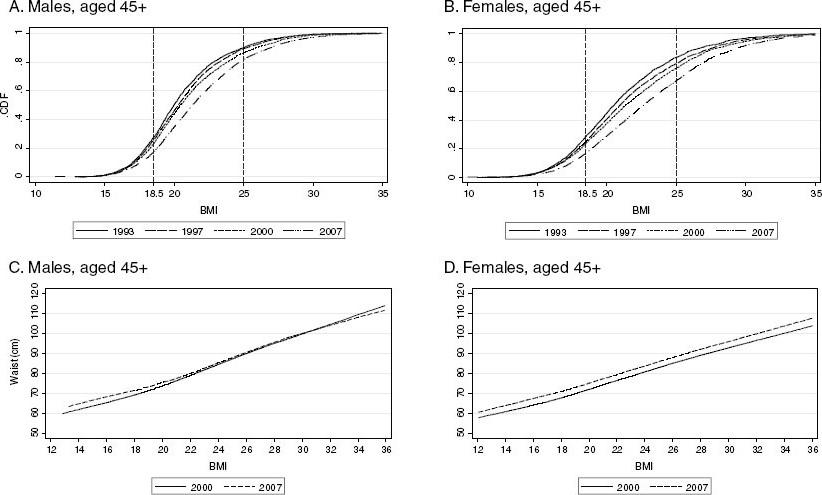
FIGURE 13-1 CDF of body mass index and waist circumference by body mass index, adults aged 45 and older.
SOURCE: Data from IFLS, Waves 1-4.
TABLE 13-2 Under/Overnutrition, Low Hemoglobin Level, High Total Cholesterol, and Low HDL Level Among 45+ in 2007
| Male | Female | |||
| % | # obs. | % | # obs. | |
| 45-54 years | ||||
| % undernourished | 9.46 | 1,870 | 9.39 | 2,106 |
| % overweight | 22.65 | 1,870 | 40.18 | 2,106 |
| % low blood hemoglobin | 17.72 | 1,869 | 28.08 | 2,091 |
| % high total cholesterol | 12.49 | 1,832 | 20.02 | 2,054 |
| % low HDL | 70.59 | 1,832 | 40.81 | 2,054 |
| 55-64 years | ||||
| % undernourished | 18.22 | 1,096 | 16.64 | 1,211 |
| % overweight | 17.26 | 1,096 | 30.57 | 1,211 |
| % low blood hemoglobin | 26.01 | 1,093 | 32.82 | 1,212 |
| % high total cholesterol | 12.66 | 1,071 | 26.00 | 1,204 |
| % low HDL | 64.79 | 1,071 | 36.25 | 1,204 |
| 65-74 years | ||||
| % undernourished | 27.95 | 713 | 29.57 | 878 |
| % overweight | 8.59 | 713 | 18.82 | 878 |
| % low blood hemoglobin | 40.86 | 728 | 40.25 | 886 |
| % high total cholesterol | 9.48 | 716 | 23.07 | 884 |
| % low HDL | 59.49 | 715 | 41.31 | 883 |
| 75+ years | ||||
| % undernourished | 38.05 | 338 | 33.60 | 438 |
| % overweight | 6.31 | 338 | 13.96 | 438 |
| % low blood hemoglobin | 52.24 | 350 | 50.06 | 461 |
| % high total cholesterol | 8.60 | 339 | 21.63 | 448 |
| % low HDL | 65.22 | 339 | 34.47 | 448 |
| All adults 45+ | ||||
| % undernourished | 17.54 | 4,017 | 17.40 | 4,633 |
| % overweight | 17.31 | 4,017 | 31.14 | 4,633 |
| % low blood hemoglobin | 27.12 | 4,040 | 33.81 | 4,650 |
| % high total cholesterol | 11.66 | 3,958 | 22.33 | 4,590 |
| % low HDL | 66.55 | 3,957 | 39.09 | 4,589 |
| Mean BMI | 21.75 | 4,017 | 22.90 | 4,633 |
| Mean blood hemoglobin | 13.99 | 4,040 | 12.42 | 4,650 |
| Mean total cholesterol | 178.16 | 3,958 | 198.46 | 4,590 |
| Mean HDL | 34.94 | 3,957 | 44.97 | 4,589 |
SOURCE: Data from IFLS4. Undernourished = BMI < 18.5, overweight = BMI ≥ 25, low blood hemoglobin = < 13.0 mg/dL (male) or < 12.0 mg/dL (female), high total cholesterol = (≥ 240 mg/dL, low HDL = < 40 mg/dL).
due to an increase in BMI, but not all. Figures 13-1c and 13-1d plot waist circumference against BMI for men and women in 2000 and 2007. For men at higher BMI levels, there is not much change in waist circumference, so that the upward shift in waist circumference for men between 2000 and 2007 is largely a result of increasing BMI. Not so for women, however, who have a shift up in mean waist circumference by BMI. In 2007 being over 188 cm in waist size is associated with a BMI of 26, instead of 28, which was the case in 2000.
Table 13-3 shows the regression results for BMI. Men who completed junior high or more are likely to have higher BMI than those with less schooling. For women, BMI seems to increase with education; this is true for those with some primary education compared to no schooling at all and for those with completed primary or more compared to some primary. However, having completed junior high or more does not have any additional effect (the marginal coefficient is slightly negative, but not significant). Thus the BMI-education gradient flattens out for women with junior high school (nine years) or more schooling, very similar to the effect found by Strauss and Thomas (2008). Education variables are jointly significant for both men and women. Pce variables turn out to be statistically significant and positive, similar to findings in previous studies that have found BMI is positively correlated with income. For both men and women, the results show that BMI decreases at old ages. In results not shown, BMIs are also lower for successively older birth cohorts.
One important result from this table is that the effect of education (as well as its interaction with age in the case of men) and pce are still significant even after we control for province and province-urban interactions, as well as province-urban-year interactions. The province-urban-year interactions are themselves also jointly statistically significant. This is an important finding that suggests that there is a degree of inequality of health outcomes among the elderly population even after we control for some regional characteristics, a theme that we will see again in some other health biomarkers.
The negative interaction coefficient on the age-schooling interaction for men can be interpreted as meaning that better educated men lose more BMI as they age compared to the less educated. This effect is small in magnitude, however. For a man 10 years older than the mean, 58, and with 10 years of schooling, BMI falls an additional .15. Note that for women, the interaction is close to zero and not significant, consistent with the flattening out of the BMI education gradient for women compared to men.
TABLE 13-3 Multivariate Regressions: BMI and Hemoglobin Levels
| BMI | Hemoglobin | |||||||
| Male | Female | Male | Female | |||||
| Coeff. | t-stat | Coeff. | t-stat | Coeff. | t-stat | Coeff. | t-stat | |
|
Age Group (dummy variables) |
||||||||
|
55 and older |
-0.0004 | [-0.004] | 0.1806 | [1.523] | -0.2742*** | [-2.738] | -0.0463 | [-0.836] |
|
65 and older |
-0.3004*** | [-2.651] | -0.0401 | [-0.291] | -0.2447*** | [-2.623] | -0.1418* | [-1.730] |
|
75 and older |
-0.4224*** | [-2.938] | -0.6853*** | [-4.152] | -0.3392*** | [-2.814] | -0.2890*** | [-3.544] |
|
Years of Education (dummy variables) |
||||||||
|
At least some primary |
0.2194** | [2.342] | 0.7537*** | [5.202] | 0.1072 | [1.455] | 0.1051** | [2.158] |
|
Completed primary school or more |
0.3443*** | [3.548] | 0.6045*** | [4.330] | 0.0140 | [0.221] | 0.1454*** | [2.912] |
|
Completed junior high or more |
1.0519*** | [8.106] | 0.0804 | [0.423] | 0.2614*** | [4.372] | 0.0194 | [0.218] |
|
Education × Age Interaction |
||||||||
|
Years of education × agea |
-0.0015* | [-1.754] | -0.0011 | [-0.841] | 0.0001 | [0.140] | 0.0019*** | [2.935] |
|
Per Capita Expenditures (splines)b |
||||||||
|
0 - median pce |
0.6904*** | [7.730] | 0.8015*** | [6.983] | 0.2712*** | [4.409] | 0.1244** | [2.425] |
|
> = median pce |
0.0996 | [0.669] | 0.0409 | [0.245] | -0.0606 | [-0.701] | -0.0591 | [-0.803] |
|
Year Dummy Variables |
||||||||
|
1997 and after |
-0.4722* | [-1.963] | -0.0677 | [-0.220] | ||||
|
2000 and after |
-0.1163 | [-0.543] | -0.4053 | [-1.570] | 0.2680** | [2.196] | 0.1544 | [0.945] |
|
2007 |
-0.2097 | [-0.630] | -0.2841 | [-0.987] | -0.4854*** | [-3.000] | 0.0375 | [0.243] |
|
Constant |
14.4015*** | [14.600] | 15.5432*** | [12.079] | 10.9429*** | [15.749] | 10.6710*** | [18.213] |
|
Observations |
12,836 | 14,735 | 10,305 | 11,853 | ||||
|
R-squared |
0.226 | 0.222 | 0.123 | 0.057 | ||||
|
Cohort Dummy Variables |
Yes | Yes | Yes | Yes | ||||
|
Province × Rural Dummy |
Yes | Yes | Yes | Yes | ||||
|
Variables + Province × Rural × |
||||||||
|
Year Interactions |
||||||||
| BMI | Hemoglobin | |||||||
| Male | Female | Male | Female | |||||
| Coeff. | t-stat | Coeff. | t-stat | Coeff. | t-stat | Coeff. | t-stat | |
| F-tests for joint significance: | F-stat | p(values) | F-stat | p(values) | F-stat | p(values) | F-stat | p(values) |
|
Age group dummy variables |
5.869 | 0.001 | 8.284 | 0.000 | 3.948 | 0.008 | 5.057 | 0.002 |
|
Education variables |
47.550 | 0.000 | 27.479 | 0.000 | 10.818 | 0.000 | 6.651 | 0.000 |
|
Educ. years + educ. age interactions |
41.392 | 0.000 | 21.542 | 0.000 | 8.220 | 0.000 | 6.635 | 0.000 |
|
Per capita expenditures |
82.506 | 0.000 | 78.482 | 0.000 | 30.996 | 0.000 | 6.474 | 0.002 |
|
Cohort dummy variables |
5.143 | 0.000 | 11.298 | 0.000 | 2.067 | 0.046 | 1.649 | 0.120 |
|
Year dummy variables |
1.963 | 0.119 | 1.292 | 0.277 | 5.154 | 0.006 | 0.639 | 0.528 |
|
Province x rural dummy variables |
4.626 | 0.000 | 6.787 | 0.000 | 4.182 | 0.000 | 4.208 | 0.000 |
|
Year x prov x rural variables interactions |
2.233 | 0.000 | 2.815 | 0.000 | 4.687 | 0.000 | 2.728 | 0.000 |
NOTES: The dependent variable for BMI regressions is the BMI; for hemoglobin, the hemoglobin level (g/dL). Blood hemoglobin level was not collected in 1993. t-statistics (in brackets) are based on standard errors that are robust to clustering at the community level. * denotes significant at 10%; ** significant at 5%; *** significant at 1%. The omitted group for age dummy variable is 45 and older, for education, “no schooling,” and for province, Jakarta. Birth-year cohort dummy variables included are as follows: -1928, 1929-1933, 1934-1938, 1939-1943, 1944-1948, 1949-1953, 1954-1958, with 1959-1963 omitted.
aThe interaction term is between years of education and the de-meaned age. Means of age in the BMI sample are 58.2 (male), 58.5 (female); in the hemoglobin sample: 58.3 (male), 58.8 (female).
bKnot point is at the median pce, coefficient represent change in the slope.
SOURCE: Data from IFLS, Waves 1-4.
Hemoglobin
Levels of hemoglobin in blood are of interest because low levels indicate problems of anemia, which can have various negative consequences. Iron deficiency is associated, for instance, with lower endurance for physical activity.18 For some types of employment, this deficiency may affect productivity significantly (see Thomas et al., 2008).
Figure 13-2 displays the CDF of blood hemoglobin levels for elderly for 1997, 2000, and 2007 (blood hemoglobin level was not collected in 1993).19 The vertical lines at 13.0 dL for males and 12.0 g/dL for females in Figure 13-2 show the thresholds that are used in previous studies.20 The figure shows the shift to the right from previous rounds for both men and women, indicating higher levels of blood hemoglobin levels in the population, and lower proportion of elderly who are below the thresholds. Indeed the proportion of elderly men with blood hemoglobin levels lower than the threshold of 13.0 g/dL has declined from 40.6 in 1997 to 27.12 in 2007. For women, the proportion below the threshold of 12.0 g/dL has declined from 41.9 to 33.8. Given what we know about what blood hemoglobin levels can tell us, this change shows an improvement in one dimension of health in Indonesia over the years. Even so, the 2007 levels are still high compared to what is found in industrial countries, consistent with much evidence that low hemoglobin levels exist in low-income countries (Tolentino and Friedman, 2007).
The regressions presented in Table 13-3 show that older age has a strong impact on lowering blood hemoglobin levels for both and women. There are no significant cohort effects for women, though there are for men, with older cohorts having lower hemoglobin levels. For men, having completed junior high school or more education is associated with higher levels of hemoglobin compared to those with less schooling. For women, having some primary schooling has a strong positive correlation and completed primary schooling even more so. The relationship flattens out with junior high school or more. Log pce has a strongly positive correlation with hemoglobin at low levels of income. The age-education interaction is strongly significant and positive for women, meaning that the negative association with age for women is weakened for those with more schooling. For a woman having completed primary school, with 6 years of schooling and 15 years older than mean age, the marginal impact of being over 75 is cut in half, a large impact.
____________
18 Hemoglobin levels may also be low if a person has an infection or for other reasons.
19 A validation study reported by Crimmins et al. (2011) shows that the Hemocue meter performs well compared to a gold standard of hemoglobin measured from venous blood.
20 Studies have also shown that the relationship between hemoglobin level and work capacity is nonlinear; higher level above the thresholds have no impact on work capacity; see for, instance, Thomas et al. (2008).
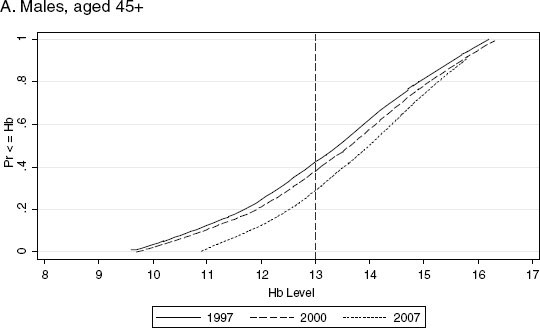

FIGURE 13-2 CDF of hemoglobin levels, adult aged 45 and older, 1997, 2000, and 2007.
SOURCE: Data from IFLS, Waves 2-4.
Cholesterol
Lipids, in particular high total cholesterol and low HDL, were measured, non-fasting, in IFLS4. Lipids are strongly correlated in the medical literature with cardiovascular risk (e.g., Kannel, Castelli, and Gordon, 1979). It is thus of considerable interest to explore their levels in a low-income country like Indonesia, and, as well, their associations with SES variables.21Table 13-2 shows the 2007 sample means and fractions above the threshold for total cholesterol and below for HDL, using standard WHO thresholds. For total cholesterol, high levels are not large, only 12% for men, but higher for women at 22%.22 However, the situation for low HDL is completely different. Levels below the threshold of 40 are large, especially for men, 67%, and 39% for women. Small fractions of high total cholesterol but large fractions of low HDL is a pattern that is being found in several low-income countries where it has been looked at (e.g., Crimmins et al., 2011; Gurven et al., 2009), including the Tsimane study of primitive Amazon Indians in Bolivia and the CHARLS study in China (Crimmins et al., 2011). Figure 13-3 plots the fraction above and below the thresholds of total and HDL cholesterol against age. One can see that there is little relationship for total cholesterol, with a small increasing tendency to have high total cholesterol for women until the mid-50s, when the curve flattens. For HDL there is some decline in the incidence of low levels with age.
Table 13-4 reports the regressions. There is very little SES correlation with either the probability of having high total cholesterol or low HDL. There are pce correlations for men for total and for women for HDL. For men, having higher per capita household expenditure is associated with a higher chance of being above the threshold for total cholesterol, then the pce curve flattens out above the median. For women for HDL, having a higher pce is associated with a lower chance at being below the HDL threshold, but then flattens out above the median level of pce. For men’s HDL, however, we do not see any association with pce. There are also quite strong community effects that are found, though from the dummies we cannot say what exactly they represent; perhaps impacts of local food prices, through diets, but it could be through other mechanisms as well.
____________
21 Crimmins et al. (2011) report a validation study of the Cardiochek PA meter against venous blood for both total and HDL cholesterol. The results look quite similar. It is the case, however, that the distributions for Cardiochek PA samples are censored at the measurement bounds of the meter (see footnote 16). However, we define our dependent variables as the fraction above or below thresholds (≥ = 240 for total and <40 for HDL). These thresholds are within the measurement bounds of the meter, so this censoring should not matter for this chapter.
22 This same gender differential is found in the CHARLS data for China, see Crimmins et al. (2011).
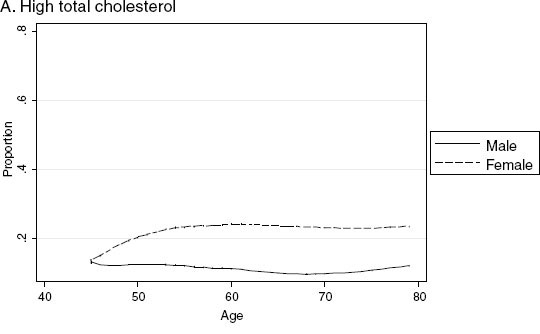
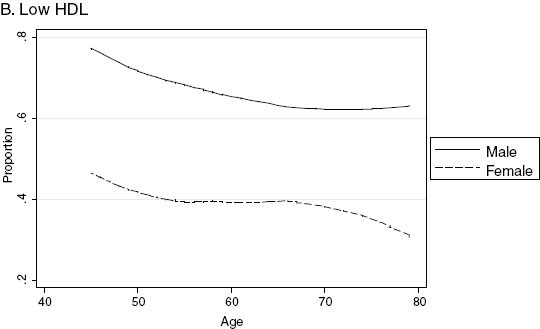
FIGURE 13-3 Proportion with high total cholesterol and low HDL, adults aged 45 and older, 2007.
SOURCE: Data from IFLS4.
TABLE 13-4 Multivariate Regressions: High Total Cholesterol and Low HDL Levels, Aged 45 and Older in 2007
| High Total Cholesterol | Low HDL | |||||||
| Male | Female | Male | Female | |||||
| Coeff. | t-stat | Coeff. | t-stat | Coeff. | t-stat | Coeff. | t-stat | |
|
Age Group (dummy variables) |
||||||||
|
55 and older |
0.0112 | [0.378] | -0.0082 | [-0.229] | 0.0375 | [0.920] | 0.0132 | [0.326] |
|
65 and older |
-0.0175 | [-0.643] | -0.0019 | [-0.050] | 0.0431 | [0.751] | 0.0275 | [0.636] |
|
75 and older |
-0.0022 | [-0.047] | -0.0209 | [-0.390] | 0.0110 | [0.162] | 0.0459 | [0.794] |
|
Years of Education (dummy variables) |
||||||||
|
At least some primary |
-0.0048 | [-0.367] | 0.0347* | [1.853] | 0.0285 | [1.186] | -0.0188 | [-0.857] |
|
Completed primary school or more |
0.0159 | [1.286] | -0.0006 | [-0.032] | -0.0320* | [-1.700] | 0.0238 | [1.153] |
|
Completed junior high or more |
0.0223 | [1.421] | 0.0230 | [0.997] | 0.0320 | [1.520] | -0.0022 | [-0.084] |
|
Education × Age Interaction |
||||||||
|
Years of education × agea |
-0.0001 | [-0.574] | -0.0001 | [-0.337] | 0.0001 | [0.309] | -0.0001 | [-0.568] |
| Per Capita Expenditures (splines)b | ||||||||
|
0 - median pce |
0.0438*** | [3.202] | 0.0218 | [1.161] | -0.0285 | [-1.104] | -0.0874*** | [-3.677] |
|
> = median pce |
-0.0372 | [-1.552] | -0.0072 | [-0.250] | 0.0344 | [0.954] | 0.1188*** | [3.467] |
|
Constant |
-0.4599*** | [-2.699] | -0.1567 | [-0.657] | 1.1763*** | [3.571] | 1.5265*** | [5.018] |
|
Observations |
3,960 | 4,591 | 3,958 | 4,589 | ||||
|
R-squared |
0.069 | 0.074 | 0.047 | 0.068 | ||||
|
Cohort Dummy Variables |
Yes | Yes | Yes | Yes | ||||
|
Province × Rural |
Yes | Yes | Yes | Yes | ||||
| High Total Cholesterol | Low HDL | |||||||
| Male | Female | Male | Female | |||||
| Coeff. | t-stat | Coeff. | t-stat | Coeff. | t-stat | Coeff. | t-stat | |
| F-tests for joint significance: | F-stat | p(values) | F-stat | p(values) | F-stat | p(values) | F-stat | p(values) |
|
Age group dummy variables |
0.185 | 0.907 | 0.063 | 0.979 | 0.521 | 0.668 | 0.357 | 0.784 |
|
Education variables |
1.838 | 0.139 | 2.289 | 0.078 | 1.437 | 0.231 | 0.526 | 0.664 |
|
Educ. vars + educ. age interactions |
1.572 | 0.180 | 1.868 | 0.115 | 1.096 | 0.358 | 0.571 | 0.684 |
|
Per capita expenditures |
6.692 | 0.001 | 1.736 | 0.177 | 0.610 | 0.544 | 6.908 | 0.001 |
|
Cohort dummy variables |
1.649 | 0.120 | 1.649 | 0.120 | 1.649 | 0.120 | 1.649 | 0.120 |
|
Year dummy variables |
0.639 | 0.528 | 0.639 | 0.528 | 0.639 | 0.528 | 0.639 | 0.528 |
|
Province × rural dummy variables |
6.756 | 0.000 | 8.508 | 0.000 | 4.386 | 0.000 | 8.971 | 0.000 |
NOTES: The dependent variable for high total cholesterol is 1 if individual has total cholesterol level > 240 mg/dL, 0 otherwise. The dependent variable for low HDL level is 1 if individual has HDL level < 40 mg/dL, 0 otherwise. Blood cholesterol levels were only measured in 2007. t-statistics (in brackets) are based on standard errors that are robust to clustering at the community level. * denotes significant at 10%; ** significant at 5%; *** significant at 1%. The omitted group for age dummy variable is 45 and older, for education, “no schooling,” and for province, Jakarta. Birth-year cohort dummy variables included are as follows: -1928, 1929-1933, 1934-1938, 1939-1943, 1944-1948, 1949-1953, 1954-1958, with 1959-1963 omitted.
aThe interaction term is between years of education and the de-meaned age. Means of age in the sample are 58.0 (male) and 58.6 (female).
bKnot point is at the median pce, coefficient represent change in the slope.
SOURCE: Data from IFLS4.
Hypertension
Along with BMI and waist circumference, blood pressure is a useful indicator of risk of coronary heart diseases. Blood pressure measures are available from IFLS2, 3, and 4.23Figure 13-4 plots the proportion of those who are hypertensive (those whose systolic is greater than or equal to 140 or diastolic is greater than or equal to 90) against age. For both men and women, there is a strong positive relationship between age and being hypertensive.
Looking at the levels of measured hypertension over the years in Table 13-5 Panel A, there seems to be little change. Among men aged 45 and older, around 44% had hypertension in 2007, the same percentage as in 1997. Similarly among women, 53% were hypertensive, and the number does not change much over the years. However, it is important to note that the percentage of those with hypertension is substantial, so clearly hypertension is a major health issue for the elderly.
A major public health issue, given the nutrition and health transitions that Indonesians are undergoing, is whether the health system, which is set up to focus on young children and mothers and infectious diseases, can adequately care for chronic disease among the elderly. Are the elderly being diagnosed and treated? In IFLS4 2007, the respondents were asked whether or not they had ever been diagnosed with hypertension by a modern medical provider. We take the union of those who answer yes and those whom we measured to have hypertension (of course, there is an overlap) to arrive at a sum of persons who have hypertension.24 We then tabulate the fraction of those who have hypertension who say they have been diagnosed, in Table 13-5 Panel B and show the bivariate relationship with level of education. Almost 75% of men and 62% of women are undiagnosed according to Table 13-5 Panel B. 25 By education level there is a drop in undiagnosed hypertension with higher education for both men and women; for women, the drop occurs for those with any schooling. Panel C shows among those who are report being diagnosed, what fraction are not taking
____________
23 In IFLS2 1997 and IFLS3 2000, blood pressure was measured only once. In IFLS4 2007, blood pressure was measured three times. For 2007, we use the average of the three measures for our analysis.
24 This is the usual way in HRS-type data to calculate levels of hypertension (for example, see Gurven et al., 2009; Strauss et al., 2010).
25 In China, the same analysis has been done with the CHARLS pilot data (see Strauss et al., 2010). There the underdiagnosis rate is 45%. The fraction of those who are diagnosed who take medications is much higher, 75-80%. For Mexico the situation for hypertension is the same (Parker et al., 2010). Clearly, the health system in Indonesia has a major problem of healthcare for the elderly.
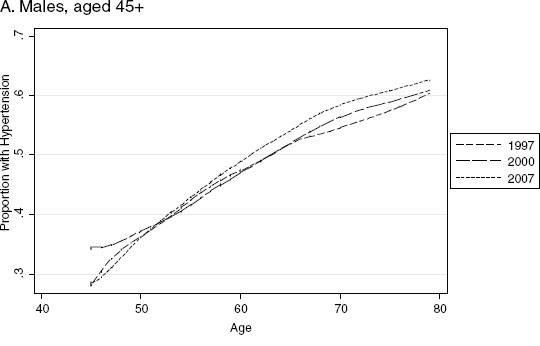
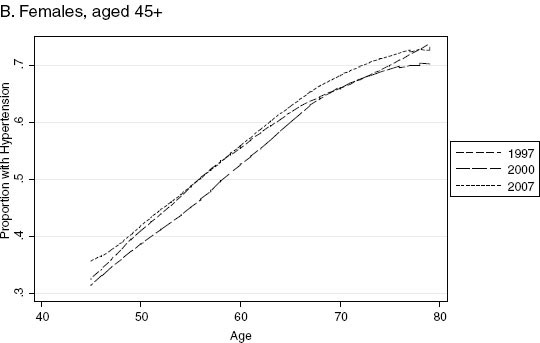
FIGURE 13-4 Proportion with hypertension by age, 1997, 2000, and 2007.
SOURCE: Data from IFLS, Waves 2-4.
TABLE 13-5 Hypertension, Underdiagnosis, and Medication Take Up, Age 45+
| PANEL A. Incidence of hypertension, diagnosis, and medication take up | ||||||
| Men | Women | |||||
| 1997 | 2000 | 2007 | 1997 | 2000 | 2007 | |
| Observations | 2856 | 3,477 | 4,044 | 3,307 | 3,631 | 4,674 |
| % measured as hypertensive | 43.8 | 44.2 | 44.2 | 52.6 | 49.6 | 52.7 |
| % not measured, but diagnosed | 6.5 | 11.6 | ||||
| as hypertensivea | ||||||
| Total hypertensive (%)b | 43.8 | 44.4 | 50.7 | 52.6 | 50 | 63.3 |
| PANEL B. Underdiagnosis of hypertension by completed education, adults 45+c | ||||||
| Education | 2007 | 2007 | ||||
| no schooling | 79.0 | 69.5 | ||||
| primary schooling | 74.4 | 58.2 | ||||
| junior high | 73.2 | 52.1 | ||||
| senior high + | 68.0 | 62.1 | ||||
| all adults 45+ | 73.6 | 62.1 | ||||
| PANEL C. Hypertensive and not taking medication, by completed education, aged 45+d | ||||||
| Education | 2007 | 2007 | ||||
| no schooling | 91.5 | 92.6 | ||||
| primary schooling | 89.1 | 89.3 | ||||
| junior high | 73.6 | 79.4 | ||||
| senior high + | 77.9 | 86.8 | ||||
| all adults 45+ | 85.0 | 89.2 | ||||
aDiagnosed” if answered “Yes” to the question “Has a doctor/nurse/paramedic ever told you that you have hypertension?” The question was only asked in 2007. Percentages of those diagnosed with hypertension are out of individuals aged 45+.
bPercentages are out of individuals 45+.
cPercentages are out of individuals 45+ who are measured and/or diagnosed to be hypertensive.
dPercentages are out of individuals 45+ who are diagnosed to be hypertensive.
SOURCE: Data from IFLS Waves 2-4.
medications for hypertension, and by level of schooling. A very high percentage of those diagnosed are not taking medications and the percentage is higher for women, 89%, than for men, 85%. Education level gradients exist, particularly for men.
The multivariate regressions presented in Table 13-6 confirm what we saw in Figure 13-4 that the probability of having hypertension increases with age, although the increase with birth cohort is even larger. For men, education levels are jointly significant, with higher levels of schooling
TABLE 13-6 Hypertension and Underdiagnosis of Hypertension: Linear Probability Models
| Hypertension | Underdiagnosis of hypertension | |||||||||||||||
| Male | Female | Male | Female | |||||||||||||
| Coeff. | t-stat | Coeff. | t-stat | Coeff. | t-stat | Coeff. | t-stat | |||||||||
| Age Group (dummy variables) | ||||||||||||||||
| 55 and older | 0.0478** | [2.434] | 0.0390** | [2.143] | -0.0290 | [-0.910] | 0.0310 | [1.152] | ||||||||
| 65 and older | 0.0257 | [1.230] | 0.0558*** | [3.115] | -0.0351 | [-1.111] | 0.0200 | [0.692] | ||||||||
| 75 and older | 0.0695*** | [2.634] | 0.0300 | [1.372] | -0.0259 | [-0.684] | -0.0289 | [-0.892] | ||||||||
| Years of Education (dummy variables) | ||||||||||||||||
| At least some primary | -0.0067 | [-0.385] | 0.0105 | [0.680] | -0.0144 | [-0.396] | -0.1249*** | [-4.704] | ||||||||
| Completed primary school or more | 0.0255* | [1.658] | -0.0018 | [-0.113] | -0.0213 | [-0.736] | 0.0287 | [1.030] | ||||||||
| Completed junior high or more | 0.0333** | [2.172] | -0.0060 | [-0.286] | -0.0358 | [-1.075] | 0.0298 | [0.872] | ||||||||
| Education × Age Interaction | ||||||||||||||||
| Years of education × agea | -0.0001 | [-0.984] | 0.0004*** | [2.984] | -0.0003 | [-1.334] | -0.0003 | [-1.250] | ||||||||
| Per Capita Expenditures (splines)b | ||||||||||||||||
| 0 - median pce | 0.0172 | [1.095] | 0.0371** | [2.540] | -0.0507 | [-1.342] | -0.0998*** | [-3.244] | ||||||||
| >= median pce | 0.0022 | [0.096] | -0.0285 | [-1.397] | 0.0263 | [0.484] | 0.0753* | [1.652] | ||||||||
| Year Dummy Variables | ||||||||||||||||
| 2000 and after | 0.0580 | [1.610] | 0.0385 | [1.068] | ||||||||||||
| 2007 | 0.1166*** | [2.674] | 0.0608 | [1.401] | ||||||||||||
| Constant | -0.0267 | [-0.147] | -0.1018 | [-0.610] | 1.3425*** | [2.802] | 1.7300*** | [4.411] | ||||||||
| Observations | 10,376 | 11,994 | 1,966 | 2,745 | ||||||||||||
| R-squared | 0.064 | 0.088 | 0.045 | 0.072 | ||||||||||||
| Cohort Dummy Variables | Yes | Yes | No | No | ||||||||||||
| Province × Rural Dummy Variables + | Yes | Yes | Province × | Province × | ||||||||||||
| Province × Rural × Year Interactions | rural | rural | ||||||||||||||
| F-tests for Joint Significance: | ||||||||
| Age group dummy variables | 3.447 | 0.017 | 3.630 | 0.013 | 1.163 | 0.323 | 0.988 | 0.398 |
| Education variables | 4.206 | 0.006 | 0.171 | 0.916 | 1.280 | 0.281 | 7.586 | 0.000 |
| Educ. years + educ. age interactions | 3.953 | 0.004 | 2.913 | 0.021 | 1.253 | 0.288 | 7.305 | 0.000 |
| Per capita expenditures | 2.569 | 0.078 | 4.424 | 0.012 | 1.891 | 0.152 | 8.253 | 0.000 |
| Cohort dummy variables | 7.374 | 0.000 | 4.417 | 0.000 | ||||
| Year dummy variables | 4.791 | 0.009 | 1.990 | 0.138 | ||||
| Province × rural dummy variables | 1.769 | 0.019 | 3.293 | 0.000 | 2.653 | 0.000 | 6.955 | 0.000 |
|
Year × prov × rural variables interactions |
1.979 | 0.000 | 2.682 | 0.000 | ||||
NOTES: The dependent variable for the hypertension regressions is whether the individual is hypertensive = 1, 0 otherwise; and for the underdiagnosis of hypertension, the dependent variable is 1 if the individual has ever been diagnosed with hypertension, 0 otherwise, conditional of being hypertensive. Blood pressure measurement was not collected in 1993, and question about diagnosis was only asked in 2007. t-statistics (in brackets) are based on standard errors that are robust to clustering at the community level. * denotes significant at 10%; ** significant at 5%; *** significant at 1%. The omitted group for age dummy variable is 45 and older, for education, “no schooling,” and for province, Jakarta. Birth-year cohort dummy variables included are as follows: -1928, 1929-1933, 1934-1938, 1939-1943, 1944-1948, 1949-1953, 1954-1958, with 1959-1963 omitted.
aThe interaction term is between years of education and the de-meaned age. Means of age in the hypertension sample are: 58.3 (male), 58.9 (female); in the underdiagnosis sample: 60.3 (male), 60.8 (female).
b Knot point is at the median pce, coefficient represent change in the slope.
SOURCE: Data from IFLS, Waves 2-4.
associated with a great likelihood of being hypertensive. Pce on the other hand is not significantly related to hypertension for men. For women, it is pce and not education levels that is significantly related to hypertension, with higher pce being associated with higher chances of having hypertension. For underdiagnosis of hypertension, the regression results suggest that among women with hypertension, having some primary education reduces the probability of being underdiagnosed compared to those with no schooling, although having higher levels of schooling show no additional effects. The education variables are jointly significant for both women and men. On the other hand, pce is significant at under 1% for women. The higher per capita expenditure, the lower is underdiagnosis, so underdiagnosis is larger for lower income and uneducated people, particularly women.
Cognition: Word Recall
Cognition has been found to be an important issue among the elderly (see McArdle, Fisher, and Kadlec, 2007). We use immediate and delayed word recall as one of the cognitive measures, namely the episodic memory measure. In IFLS4, like the U.S. Health and Retirement Study (HRS), respondents are read a list of 10 simple nouns, and they are immediately asked to repeat as many as they can, in any order. After answering unrelated questions on morbidity, maybe 10 minutes later, the respondents are then asked again to repeat as many words as they can. We use the average number of correctly immediate and delayed recalled words as our memory measure (McArdle, Smith, and Willis, 2009).
On average, elderly men are able to recall 2.9 words, and elderly women are able to recall 3.2 words. Figure 13-5a shows a strong negative binary relationship between the number of words recalled and age. Note that in the top panel, the line for men is higher than that of women. This is partly due to the fact that at any given age, men on average are better educated than women. Along the same lines, part of the reason that the lines coincide is that for any given years of education, men are typically older than women. The multivariate analysis, presented in Table 13-7, sheds more light on these associations.
The regressions show a strong negative relationship between age and memory for men and women. A strong, positive relationship between education and memory is also evident, with a negative coefficient on the age-schooling interaction term for men, suggesting that education reinforces the negative effects of aging on memory in this case. The pce variables are jointly significant, positively correlated with word recall, with the effect at low levels of pce for men and at high levels for women.
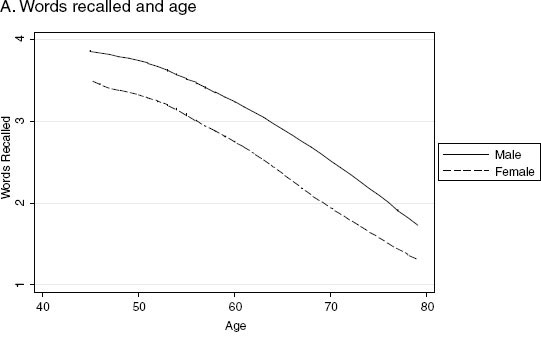
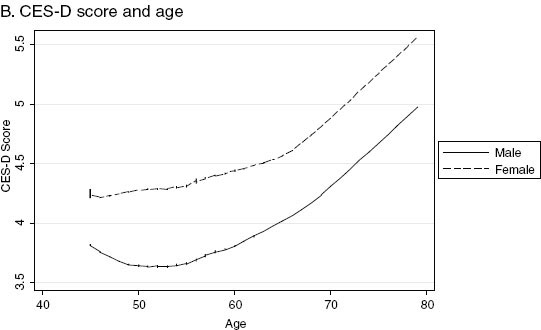
FIGURE 13-5 Words recalled and CES-D 10 (2007), adults aged 45 and older.
SOURCE: Data from IFLS4.
TABLE 13-7 Multivariate Regressions: Number of Words Recalled and the CES-D 10 Score
| Word Recall | CES-D 10 | |||||||
| Male | Female | Male | Female | |||||
| Coeff. | t-stat | Coeff. | t-stat | Coeff. | t-stat | Coeff. | t-stat | |
| Age Group (dummy variables) | ||||||||
|
55 and older |
-0.2597*** | [-3.530] | -0.2800*** | [-4.455] | 0.1468 | [1.105] | 0.0425 | [0.292] |
|
65 and older |
-0.4163*** | [-4.962] | -0.4913*** | [-6.805] | 0.5017*** | [2.997] | 0.2468 | [1.452] |
|
75 and older |
-0.6090*** | [-5.560] | -0.3392*** | [-3.262] | 0.5974** | [2.387] | 0.7027*** | [3.020] |
| Years of Education (dummy variables) | ||||||||
|
At least some primary |
0.4525*** | [4.724] | 0.5753*** | [8.541] | -0.3082* | [-1.743] | -0.3000** | [-2.165] |
|
Completed primary school or |
0.5900*** | [7.949] | 0.7014*** | [9.822] | -0.1542 | [-1.152] | -0.3948*** | [-2.758] |
|
Completed junior high or more |
0.5740*** | [7.873] | 0.5622*** | [6.850] | -0.5087*** | [-3.529] | -0.6314*** | [-3.623] |
| Education × Age Interaction | ||||||||
|
Years of education × agea |
-0.0019*** | [-3.338] | -0.0008 | [-1.203] | -0.0015 | [-1.373] | -0.0005 | [-0.356] |
| Per Capita Expenditures (splines)b | ||||||||
|
0 - median pce |
0.2001** | [2.536] | 0.0360 | [0.495] | -0.2731 | [-1.589] | -0.2583 | [-1.371] |
|
> = median pce |
0.0135 | [0.119] | 0.2082** | [1.992] | -0.0684 | [-0.269] | 0.0423 | [0.162] |
| Constant | 0.1745 | [0.175] | 2.1664** | [2.361] | 8.3122*** | [3.822] | 8.2205*** | [3.421] |
| Observations | 3,748 | 4,063 | 3,900 | 4,399 | ||||
| R-squared | 0.283 | 0.315 | 0.066 | 0.068 | ||||
| Province × Rural | Yes | Yes | Yes | Yes | ||||
| F-tests for Joint Significance: | ||||||||
|
Age group dummy variables |
43.322 | 0.000 | 50.164 | 0.000 | 7.318 | 0.000 | 6.522 | 0.000 |
|
Education variables |
104.477 | 0.000 | 169.400 | 0.000 | 11.726 | 0.000 | 21.114 | 0.000 |
|
Educ. years + educ. age interactions |
83.455 | 0.000 | 137.819 | 0.000 | 9.220 | 0.000 | 15.859 | 0.000 |
|
Per capita expenditures |
13.403 | 0.000 | 10.295 | 0.000 | 7.236 | 0.001 | 2.950 | 0.053 |
|
Province × rural dummy variables |
5.347 | 0.000 | 5.761 | 0.000 | 5.998 | 0.000 | 9.180 | 0.000 |
NOTES: The dependent variable for the word recall regression is the average number of the words recalled from the immediate and delayed recalls. Word recall question module was only administered in 2007. The dependent variable for the CES-D regression is the CES-D10 score. The score is computed in the way suggested by the Stanford group that created the CES-D, using numbers from 0 for rarely to 3 for most of the time, for negative questions such as “do you feel sad.” For positive questions, such as “do you feel happy,” the scoring is reversed from 0 for most of the time to 3 for rarely (see text). CESD-10 module was only asked in 2007. t-statistics (in brackets) are based on standard errors that are robust to clustering at the community level. * denotes significant at 10%; ** significant at 5%; *** significant at 1%. The omitted group for age dummy variable is 45 and older, for education, “no schooling,” and for province, Jakarta.
aThe interaction term is between years of education and the de-meaned age. Means of age in the word recall sample are 56.9 (male), 56.7 (female); and in the CES-D sample: 57.3 (male), 57.4 (female).
bKnot point is at the median pce, coefficient represent change in the slope.
SOURCE: Data from IFLS4.
CES-D 10 Score
As a measure of mental health, the respondents were administered a self-reported depression scale from the short version of the CES-D scale, one of the major international scales of depression used in general populations. Higher scores on the CES-D scale indicate a higher likelihood of having major depression.26 Some recent studies have failed to find a relationship between depression and education or income (see Das et al., 2007, for example); however, other studies have found such correlations. (Patel and Kleinman, 2003, surveyed several studies that do find negative correlations between depression and SES.) For Indonesia, Friedman and Thomas (2008) find that the economic crisis fueled depression indicators, especially for the more vulnerable population.27
Figure 13-5b displays the relationships between CES-D scores and age. For both elderly men and elderly women, CES-D scores increase with age and are higher for women. The mean CES-D scores among people aged 45 and older are 3.3 for men and 3.8 for women.
The regressions using CES-D as dependent variable (Table 13-7) show that even in a multivariate setting, age has a strong positive correlation with CES-D scores. The education variables are jointly statistically significant for both men and women, with the more schooling, the lower the CES-D scores. The age-schooling interactions are not significant. The pce variables, while not individually significant, are jointly significant (at 10% or lower) and show a negative association between pce and CES-D scores.28
CONCLUSIONS
Indonesia has undergone major changes in multiple dimensions since the Indonesia Family Life Survey was first fielded in 1993. Among these changes has been moving along the health and nutrition transition. IFLS is very well suited to examine those changes.
Overall there have been significant changes in health outcomes among elderly Indonesians over the 15-year period of IFLS. Much of the change
____________
26 The answers for CES-D are on a four-scale metric, from rarely, to some days (1-2 days), to occasionally (3-4 days), to most of the time (5-7 days). We score these answers in the way suggested by the Stanford group that created the CES-D, using numbers from 0 for rarely to 3 for most of the time, for negative questions such as “do you feel sad.” For positive questions, such as “do you feel happy,” the scoring is reversed from 0 for most of the time to 3 for rarely.
27 They also use IFLS data, from 1993 and 2000. Unfortunately the depression scale that IFLS had been using was not as widely used as the CES-D scale, so we switched scales in 2007 to be more comparable to other international surveys, especially the HRS-type surveys. This means that in this chapter, we can only use the CES-D scale for one year, 2007
28 Similar results are again found in the CHARLS data for China (see Strauss et al., 2011).
can be seen as improvements, such as the movement out of undernutrition and communicable disease as well as the increasing levels of hemoglobin, which, however, are still at low levels compared to high-income countries. On the other hand, other changes, such as the increase in overweight and waist circumference, especially among women, and continuing high levels of hypertension and high levels of low HDL cholesterol seem to be inadequately addressed by the health system. These conditions indicate that the elderly population in Indonesia is increasingly exposed to higher risk factors that are correlated with chronic problems such as cardiovascular diseases and diabetes.
This is quite interesting because this period has seen major gyrations in economic activity, including strong growth from 1993 to 1996, a major economic collapse from late 1997 to 1998, and a strong recovery from 2000 to 2007. The financial crisis may have slowed the nutrition transition, and some of our evidence is consistent with that conjecture.
The relationship between health and SES at different stages in the life cycle is always difficult to disentangle. IFLS enables us to provide some important findings that contribute to our understanding of the relationships. In this chapter we examine correlations between SES and many health outcomes and behaviors for the elderly. Past work has usually been limited to just a small number of health outcomes and has not usually examined the elderly. To the extent that controlling for time, community, and their interactions account for differences in prices, healthcare availability, and quality in the communities over time, the significant correlations that still exist between SES and many of the health outcomes indicate a substantial degree of inequality of health among the elderly population. We find positive correlations between SES and most of the good health outcomes and that education tends to suppress the negative impacts of age on some health outcomes.
Of some importance, we find a very large rate of underdiagnosis for hypertension, the one chronic disease of the elderly for which we have data. These rates are differential by SES for women, with lower SES women having a greater chance of being undiagnosed. This is very likely true for other chronic conditions that we could not calculate. This lack of diagnosis indicates that the Indonesian health system, like most others in low-income countries, is still not set up to adequately care for chronic conditions of the elderly.
REFERENCES
Abikusno, N. (2009). Evaluation and implementation of ageing-related policies in Indonesia. In Older Persons in Southeast Asia: An Emerging Asset, E.N. Arifin and A. Ananta (Eds.). Singapore: ISEAS.
Barker, D. (1994). Mothers, Babies, and Health in Later Life. London: BMJ Publishing.
Barrera, A. (1990). The role of mother’s schooling and its interaction with public health programs in child health production. Journal of Development Economics 32(1):69-92.
Cameron, L.A., and D. Cobb-Clark (2008). Do co-residency and financial transfers from the children reduce the need for elderly parents to works in developing countries? Journal of Population Economics 21:1,007-1,033.
Crimmins, E., J. Hu, P. Hu, W. Huang, J. Kim, Y. Shi, J. Strauss, L. Zhang, and Y. Zhao. (2011). CHARLS Pilot: Blood-based Biomarker Documentation. Peking University, China Center for Economic Research.
Das, J., Q.-T. Do, J. Friedman, D. McKenzie, and K. Scott. (2007). Mental health and poverty in developing countries. Social Science and Medicine 65(3):467-480.
Friedman, J., and D. Thomas (2008). Psychological health, before, during and after an economic crisis: Results from Indonesia 1993-2000. World Bank Economic Review 23(1):57-76.
Gluckman, P., and M. Hanson (2005). The Fetal Matrix: Evolution, Development and Disease. Cambridge: Cambridge University Press.
Gurven, M., H. Kaplan, J. Winking, D.E. Rodriguez, S. Vasunilashorn, J.-K. Kim, C. Finch, and E. Crimmins. (2009). Inflammation and infection do not promote arterial aging and cardiovascular disease risk factors among lean horticulturalists. PLoS One 4(8):e6590. doi: 10.1371/journal.pone.0006590.
Indonesia Family Life Survey, Wave 1. (1994). Available: http://www.rand.org/labor/FLS/IFLS.html.
Indonesia Family Life Survey, Wave 2. (1997). Available: http://www.rand.org/labor/FLS/IFLS.html.
Indonesia Family Life Survey, Wave 3. (2000). Available: http://www.rand.org/labor/FLS/IFLS/ifls3.html.
Indonesia Family Life Survey, Wave 4. (2008). Available: http://www.rand.org/labor/FLS/IFLS/ifls4.html.
Indonesian Public Health Association. (1993). Analysis of the Health Transition in Indonesia: Implications for Health Policy. Jakarta: Indonesian Public Health Association.
Kannel, W.B., W.P. Castelli, and T. Gordon. (1979). Cholesterol in the prediction of atherosclerotic disease. New perspectives based on the Framingham study. Annals of Internal Medicine 90(1):85-91.
Kinsella, K., and W. He (2009). An Aging World: 2008. U.S. Census Bureau, International Population Reports, PS95/09-1. Washington, DC: U.S. Government Printing Office.
McArdle, J., G. Fisher, and K. Kadlec. (2007). Latent variable analysis of age trends in tests of cognitive ability in the Health and Retirement Survey, 1992-2004. Psychology and Aging 22(3):525-545.
McArdle, J., J.P. Smith, and R. Willis. (2009). Cognition and Economic Outcomes in the Health and Retirement Survey, manuscript, RAND Corporation, Santa Monica, CA.
Monteiro, C., E. Moura, W. Conde, and B. Popkin (2004). Socioeconomic status and obesity in adult populations of developing countries. Bulletin of the World Health Organization 82(12):940-946.
Parker, S., G. Teruel, and L. Rubalcava. (2010). Perceptions and Knowledge of Underlying Health Conditions in Mexico. Paper presented at the Population Association of America Annual Meetings, Dallas, Texas.
Patel, V., and A. Kleinman. (2003). Poverty and common mental disorders in developing countries. Bulletin of the World Health Organization 81(8):609-615.
Popkin, B. (1994). The nutrition transition in low-income countries: An emerging crisis. Nutrition Reviews 52(9):285-298.
Strauss, J., and D. Thomas (1995). Human resources: Empirical modeling of household and family decisions. In Handbook of Development Economics, Volume 3A, J.R. Behrman and T.N. Srinivasan (Eds.). Amsterdam: North Holland Press.
Strauss, J., and D. Thomas (1998). Health, nutrition and economic development. Journal of Economic Literature 36(3):766-817.
Strauss, J., and D. Thomas. (2008). Health over the life course. In Handbook of Development Economics, Volume 4, T.P. Schultz and J. Strauss (Eds.). Amsterdam: North Holland Press.
Strauss, J., K. Beegle, A. Dwiyanto, Y. Herawati, D. Pattinasarany, E. Satriawan, B. Sikoki, Sukamdi, and F. Witoelar. (2004). Indonesian Living Standards Before and After the Financial Crisis. Singapore: Institute for Southeast Asian Studies.
Strauss, J., F. Witoelar, B. Sikoki, and A.M. Wattie. (2009). User’s Guide for the Indonesia Family Life Survey, Wave 4: Volume 2. Working Paper WR-675/2-NIA/NICHD, Labor and Population Program. Santa Monica, CA: RAND Corporation.
Strauss, J., X. Lei, A. Park, Y. Shen, J.P. Smith, Z. Yang, and Y. Zhao. (2010). Health outcomes and socio-economic status among the elderly in China: Evidence from the CHARLS Pilot. Journal of Population Ageing 3(3):111-142.
Thomas, D., J. Strauss, and M.-H. Henriques. (1990). Child survival, height for age and household characteristics in Brazil. Journal of Development Economics 33(2):197-234.
Thomas, D., J. Strauss, and M.-H. Henriques. (1991). How does mother’s education affect child height? Journal of Human Resources 26(2):183-211.
Thomas, D., E. Frankenberg, J. Friedman, J.-P. Habicht, M. Hakimi, N. Ingwersen, Jaswadi, N. Jones, C. McKelvey, G. Pelto, B. Sikoki, T. Seeman, J.P. Smith, C. Sumantri, W. Suriastini, and S. Wilopo. (2008). Causal effect of health on social and economic prosperity: Experimental evidence, manuscript, Department of Economics, Duke University.
Tolentino, K., and J.F. Friedman. (2007). An update on anemia in less developed countries. American Journal of Tropical Medicine and Hygiene 77(1):44-51.
van Eeuwijk, P. (2006). Old age vulnerability, ill-health and care support in urban areas of Indonesia. Ageing and Society 26(1):61-80.
Witoelar, F., J. Strauss, and B. Sikoki. (2009). Socioeconomic Success and Health in Later Life: Evidence from the Indonesia Family Life Survey. RAND Labor and Population Working Paper No. WR-704. Santa Monica, CA: RAND Corporation.

































