Our quality of life is turned upside down with each new challenge as the disorder progresses.
–Lisa Soeby
In the beginning of William’s journey in life people would say seizures aren’t a big deal, people live with them every day. It was tough to not get angry because it is just like cancer or other diseases that attack people’s bodies. William’s brain was being attacked and for many they couldn’t see that or know what the early mortality rates in epilepsy patients are. I hope we could educate the public better, because the right education teaches more tolerance and sensitivity.
–Tiernae Buttars
Characterized by seizures that are unpredictable in frequency, epilepsy is a common neurological disorder that affects people of all ages, with onset most often occurring in childhood and older adulthood. Epilepsy is a spectrum of disorders—the epilepsies—with a range of severities, widely differing seizure types and causes, and varying impacts on individuals and their families. Beyond actually living with epilepsy, its seizures, and coexisting health conditions, the challenges facing the millions of people living with epilepsy include having access to high-quality health care; learning about and coordinating health care and educational, vocational, independent living, and other community services; and dealing with stigma and common public misunderstandings. Epilepsy imposes an immense burden on individuals, families, and society. Estimates1 are that
_______________
1The committee used the prevalence and incidence ranges from Hirtz and colleagues (2007) and applied them to a U.S. population number of 313,000,000. (The U.S. Census population
• 2.2 million people in the United States and more than 65 million people worldwide have epilepsy;
• 150,000 new cases of epilepsy are diagnosed in the United States annually;
• 1 in 26 people in the United States will develop epilepsy at some point in their lifetime;
• children and older adults are the fastest-growing segments of the population with new cases of epilepsy;
• risk of death increases for people with epilepsy, with an estimated 10 years of life lost for people whose epilepsy has a known cause and 2 years lost for people with epilepsy from an unknown cause;
• the number of people with epilepsy who die of sudden unexpected death in epilepsy (SUDEP) varies from 1 of every 10,000 newly diagnosed to 9 of every 1,000 candidates for epilepsy surgery; and
• the annual direct medical care cost of epilepsy in the United States is $9.6 billion.2 This does not consider community service costs or indirect costs from losses in quality of life and productivity (these indirect costs are estimated to constitute the majority of the cost burden of epilepsy).3
Throughout the report, the committee emphasizes the ways in which epilepsy is a spectrum disorder. Epilepsy comprises more than 25 syndromes and many types of seizures that vary in severity. Additionally, people who have epilepsy span a spectrum that includes men and women of all ages and of all socioeconomic backgrounds and races/ethnicities, who live in all areas of the United States and across the globe. The impacts on physical health and quality of life encompass a spectrum as well, with individuals experiencing different health outcomes and having a range of activities of daily living that may be affected, including driving, academic achievement, social interactions, and employment. For some people, epilepsy is a childhood disorder that goes into remission (although the seizures may have lifelong consequences), while for others it is a lifelong burden or a condition that develops later in life or in response to an injury or other health condition. These many complexities of the epilepsies make it a challenging health condition to convey to the general public to promote understanding
_______________
estimate for January 30, 2012, was 312,933,845; www.census.gov/main/www/popclock.html.) In the paper by Hirtz and colleagues (2007) the median for incidence, based on the four studies of all age groups, was 48 per 100,000; median prevalence rate for all age groups was 7.1 per 1,000.
2Data are in 2004 dollars. As discussed later in this chapter and in Chapter 4, estimates of the cost burden of epilepsy vary widely and more data are needed on the use of health care services and on indirect costs.
3Begley et al., 2000; Gaitatzis et al., 2004; Hauser et al., 1980; Hesdorffer et al., 2011; Hirtz et al., 2007; Thurman, 2011; Thurman et al., 2011; Tomson et al., 2008; Yoon et al., 2009.
and alleviate stigma. This report aims to provide evidence and impetus for actions that will improve the lives of people with epilepsy and their families.
In 2010, the Institute of Medicine (IOM) was asked to examine the public health dimensions of the epilepsies with a focus on four areas:
• public health surveillance and data collection and integration;
• population and public health research;
• health policy, health care, and human services; and
• education for providers, people with epilepsy and their families, and the public.
The committee’s statement of task (Box 1-1) details the request for realistic priorities and recommendations in these four areas. The committee was asked not to examine biomedical research priorities because the Epilepsy Research Benchmarks, developed in 2000, continue to be updated by the National Institute of Neurological Disorders and Stroke (NINDS) and collaborating agencies and organizations (NINDS, 2007a,b, 2010).
To accomplish its task the IOM convened the Committee on the Public Health Dimensions of the Epilepsies, comprised of 17 members with expertise in epilepsy care, health services research, epidemiology, public health surveillance, mental health services, health care services and delivery, health literacy, public health, education, and communications. The IOM study had 24 sponsors: 12 federal agencies and 12 nonprofit organizations (Box 1-1). Vision 20-20, a coalition that includes many of the nonprofit organizations and federal agencies that sponsored the study, focuses on epilepsy research, care, services, education, and advocacy efforts.
The committee held five meetings and two public workshops during the course of its work (Appendix A). Throughout the study, many people with epilepsy and their family members and colleagues, as well as study sponsors and other organizations and individuals, provided compelling testimony to the committee about their concerns, burdens, joys, and challenges. The quotes throughout the report highlight some of the issues raised in testimony presented at the workshops and in e-mails to the committee.4 In addition to the meetings and workshops, a comprehensive review of the scientific literature and other available evidence formed a critically important part of the committee’s efforts. The committee’s work also benefited from information provided by sponsoring organizations, health systems,
_______________
4Public testimony and other materials submitted to the committee are available by request through the National Academies’ Public Access Records Office.
Statement of Task
An ad hoc committee will conduct a study and prepare a report to recommend priorities in public health, health care and human services, and health literacy and public awareness for the epilepsies and to propose strategies to address these priorities. The committee will focus its work on the following four topic areas:
• Public Health Surveillance, Collection, and Data Integration: Examine how existing or new surveillance systems could support a more accurate assessment of the public health burden of the epilepsies for patients and their families.
• Population and Public Health Research: Identify what research questions or areas of focus should be priorities for future epidemiological and population health studies on the epilepsies that may inform the development of interventions or preventive strategies.
• Health Policy, Health Care, and Human Services: Identify what constitutes adequate care and access to health and human services for people with epilepsy; what can be done to improve the consistency and quality of care for persons with epilepsy; what gaps and needs for improvement exist. Discussion is needed on maximizing community inclusion and personal outcomes for persons with epilepsies (e.g., changes in public health and health services policies and practices or community- and family-based support programs).
• Patient, Provider, and Public Education: Define what needs exist to improve the education and training of health and other professionals who treat or support persons with epilepsy. Additionally, explore how public education and awareness campaigns could best be used to increase patient and public literacy, reduce stigma, and improve community support and participation for people with epilepsy.
professional organizations, and others on specific topics (e.g., health education programs, health services use). Underpinning all its work was the committee’s desire to set forth practical, action-oriented goals to improve the health and well-being of people with epilepsy and their families.
This report provides the committee’s findings, research priorities, and recommendations and documents the evidence base. The report was written for a broad audience, including people with epilepsy; family members; health care and human services providers; local, state, and national policy makers; researchers; and foundations and nonprofit organizations.
Organization of the Report
The report covers the breadth of the statement of task. The current inadequacy of surveillance data on the epilepsies, methodologic consider-
Recommendations should be made for potential and realistic solutions and should, to the extent possible, prioritize the needs to be addressed taking into account the relative urgency of the identified needs, feasibility of implementing solutions, and considerations of time and cost. The recommendations should have a domestic focus, yet can identify major international issues. The committee should not focus on biomedical research priorities, such as those included in the 2007 Epilepsy Research Benchmarks so as to not duplicate this existing effort within the epilepsy research community to identify and monitor biomedical research needs.
Sponsors
Department of Health and Human Services sponsors: Administration on Developmental Disabilities, Center for Devices and Radiological Health (Food and Drug Administration [FDA]), Center for Drug Evaluation and Research (FDA), Eunice Kennedy Shriver National Institute of Child Health and Human Development (National Institutes of Health [NIH]), National Center for Chronic Disease Prevention and Health Promotion (Centers for Disease Control and Prevention [CDC]), National Center on Birth Defects and Developmental Disabilities (CDC), National Institute of Mental Health (NIH), National Institute of Neurological Disorders and Stroke (NIH), National Institute on Aging (NIH), Office of the Assistant Secretary for Health, Office of the Assistant Secretary for Planning and Evaluation, and Office on Women’s Health
Vision 20-20 nonprofit organization sponsors: American Epilepsy Society, Citizens United for Research in Epilepsy, Dravet.org, Epilepsy Foundation, Epilepsy Therapy Project, Finding A Cure for Epilepsy and Seizures, Hemispherectomy Foundation, International League Against Epilepsy, National Association of Epilepsy Centers, Preventing Teen Tragedy, Rasmussen’s Encephalitis Children’s Project, and Tuberous Sclerosis Alliance
ations, and potential data sources that could be used to build the knowledge base so as to better focus future efforts in health policy, research, and public health are discussed in Chapter 2. Chapter 3 looks at the epidemiologic research with a focus on risk factors, comorbidities, and outcomes of the epilepsies and the corresponding prevention strategies and research needs. Chapter 4 examines health care for people with epilepsy and highlights the actions needed to improve the quality, access, and value of care. Improving quality of care will necessitate enhancing the education and training of the range of health professionals involved; this topic is covered in Chapter 5. Because epilepsy can produce challenges that limit quality of life, the committee focuses on community resources and supporting human services and makes recommendations for improving quality of life in Chapter 6. For people with epilepsy and their family members, being informed about epilepsy is critically important, and opportunities for improving these educational efforts are explored in Chapter 7. Information needs
are then broadened in Chapter 8 to look at ways of raising awareness and overcoming the stigma and misperceptions often associated with epilepsy by communicating clearly with the public. Based on the evidence, findings, and conclusions discussed in the preceding chapters, the report concludes with the committee’s research priorities and recommendations in Chapter 9. In reading the report it is important to note that the concluding chapter draws together the evidence presented throughout the report and its common themes (see later discussion in this chapter) and puts forth the committee’s call for action from a wide range of government, nonprofit, community, and health professional organizations to improve the lives of people with epilepsy and their families.
To begin the report, this chapter provides an overview of epilepsy—a challenging task, given the complexity of the disorder and its varied impacts. The chapter begins with details on the extent and costs of epilepsy followed by an overview that discusses definitions and terminology and reviews types of seizures and epilepsy syndromes. A short synopsis of health care, quality of life, and education needs is followed by an overview of current biomedical research efforts and public health responses to epilepsy. The chapter ends by identifying several of the report’s cross-cutting themes.
EPILEPSY IS A FREQUENTLY OCCURRING AND COSTLY NEUROLOGICAL DISORDER
Incidence and Prevalence in the United States
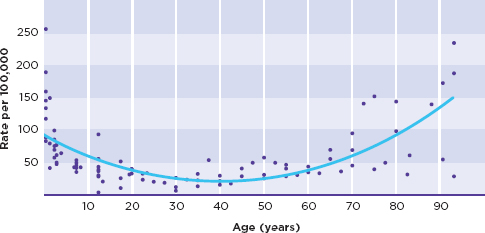
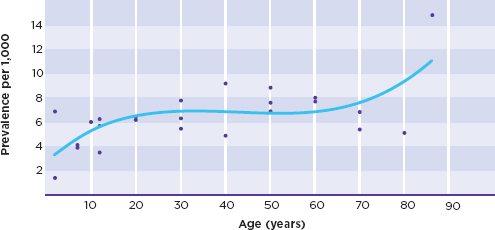
Epilepsy is the fourth most common neurological disorder in the United States after migraine, stroke, and Alzheimer’s disease (Hirtz et al., 2007). For many neurological disorders (such as Parkinson’s disease and Alzheimer’s disease), the number of new cases (incidence) is highest in older adults, while others (such as autism spectrum disorders and cerebral palsy) may be congenital or appear in early childhood (Table 1-1). For the epilepsies, the incidence is bimodal—highest in both young children and older adults (Figure 1-1a), although epilepsy may occur at any point in the life span, with the total number of people in the population who have epilepsy (prevalence) increasing with age (Figure 1-1b).
An estimated 1 in 100 people in the United States has had a single unprovoked seizure or has been diagnosed with epilepsy (NINDS, 2011c). It remains challenging to determine the total number of people with epilepsy in the United States and, in particular, the extent of the disorder in various subpopulations (e.g., by age, gender, race/ethnicity, socioeconomic status, geography). The 2.2 million prevalence estimate is most accurately viewed as approximating a midpoint in a wide potential range of 1.3 million to 2.8 million people with epilepsy (Hirtz et al., 2007; see also footnote 1). This
TABLE 1-1
Prevalence and Incidence of Common Neurological Diseases and Disorders
| Disease/Disorder | Estimated U.S. Prevalence (total number of cases) | Estimated Annual U.S. Incidence (number of new cases per year) | Age(s) of Peak Incidence |
| Migraine | 35,461,000 | — | — |
| Stroke | 2,956,000 | 541,000 | Older adults |
| Alzheimer′s disease | 2,459,000 | 468,000 | Older adults |
| Epilepsya | 2,200,000 | 150,000 | Children and older adults |
| Autism spectrum disorders | 500,000 individuals younger than 21 years | — | Children |
| Parkinson′s disease | 349,000 | 59,000 | 70 years and older |
| Multiple sclerosis | 266,000 | 12,000 | 30 years |
| Cerebral palsy | 207,000 | — | First year of life |
NOTES: The disorders listed in the table were selected by the authors of the Hirtz and colleagues (2007) study because they are neurological disorders across the life span that cause substantial morbidity and mortality.
a The epilepsy estimates are based on the calculations described in footnote 1; Hirtz and colleagues (2007) estimated 2,098,000 for epilepsy prevalence and 142,000 for incidence. Current estimates were not calculated for the other conditions since several are based on subpopulations (e.g., adults age 65 and older), and up-to-date general subpopulation denominators were not available.
SOURCE: Adapted from Hirtz et al., 2007. Reprinted with permission from Wolters Kluwer Health.
rather high degree of uncertainty exists because the population-based assessments of epilepsy prevalence are outdated and do not reflect the current size and diversity of the U.S. population (Chapters 2 and 3).
Cost of the Epilepsies in the United States
Epilepsy is a costly disorder in terms of its impact on individuals and their families, as well as on society. For example, seizures and seizure medications may affect cognitive ability—a concern for people at all ages, including young children whose brains and cognitive functions are still developing. For young and middle-aged adults, epilepsy can impact the ability to live and function independently, drive to and from school and work, maintain employment, have children, and participate in social life. For older adults, epilepsy may contribute to the health burden of other neurological disorders, such as stroke or dementia, and may hinder safety and independent living. These limitations can pose considerable economic, social, and emotional burdens on individuals with epilepsy and their families.
For society, the cost burden of epilepsy is a sum of direct health care costs (e.g., hospitalizations, health care visits), direct nonmedical costs (e.g., informal care, community services), and indirect costs due to lost productivity from unemployment, underemployment, and premature mortality. Indirect costs—the social costs resulting from effects on employment, productivity, and independent living—are considerably higher than direct medical costs for many types of epilepsy. Estimates of the annual economic burden of epilepsy in the United States range from $9.6 billion to $12.5 billion5 (Begley et al., 2000; Yoon et al., 2009). A significant percentage of the direct health costs of epilepsy is associated with the more severe forms of epilepsy and the unresponsiveness of some types of epilepsy to medications or other treatments (Begley et al., 2000).
Global Burden of Epilepsy
Epilepsy is estimated to affect more than 65 million people worldwide, with more than 80 percent of people with epilepsy living in developing countries (Ngugi et al., 2010; Thurman et al., 2011). This disproportionate burden is reflected in prevalence estimates that are at least twice as high in developing countries compared to developed countries (Ngugi et al., 2010). These markedly higher rates may be explained in part by larger numbers of cases caused by specific infectious diseases endemic in some developing nations (Ngugi et al., 2010). Further, as shown in Table 1-2, in terms of impact on disability and premature mortality, epilepsy ranks fifth among mental health, neurological, and substance-use disorders in low- and middle-income countries (Collins et al., 2011).
Although data are scant and developed using varying methodologies (Leonardi and Ustun, 2002), a number of consistently identified barriers to healthy living confront people with epilepsy globally, including inadequate infrastructure (e.g., health care services and workforce, rehabilitation programs, social supports), poor access to medications and other treatments, limited public knowledge and awareness, and stigma (Dua et al., 2006).
Generally, the availability of diagnostic services and community services for people with epilepsy varies, with lower-income countries having fewer services (Dua et al., 2006). The “treatment gap,” or the difference between the number of people who need treatment for epilepsy and the number who receive it, is significant. While the treatment gap is less than 10 percent in many high-income countries, it rises to more than 50 percent in middle-income countries and more than 75 percent in low-income countries (Meyer et al., 2010). Furthermore, variations are seen within countries, with rural
_______________
5The lower estimate is in 2004 dollars and is an estimate of direct costs (Yoon et al., 2009). The higher estimate is in 1995 dollars, 85 percent of which is attributable to indirect costs (Begley et al., 2000).
TABLE 1-2
Global Burden of Mental Health, Neurological, and Substance-Use (MNS) Disordersa
| Worldwide | High-Income Countriesb | Low- and Middle-Income Countries | ||||
| Rank No. | Cause | DALYsc (millions) | Cause | DALYs (millions) | Cause | DALYs (millions) |
| 1 | Unipolar depressive disorders | 65.5 | Unipolar depressive disorders | 10.0 | Unipolar depressive disorders | 55.5 |
| 2 | Alcohol-use disorders | 23.7 | Alzheimer’s and other dementi | 4.4 | Alcohol-use disorders | 19.5 |
| 3 | Schizophrenia | 16.8 | Alcohol-use disorders | 4.2 | Schizophrenia | 15.2 |
| 4 | Bipolar affective disorder | 14.4 | Drug-use disorders | 1.9 | Bipolar affective disorder | 12.9 |
| 5 | Alzheimer’s and other dementias | 11.2 | Schizophrenia | 1.6 | Epilepsy | 7.3 |
| 6 | Drug-use disorders | 8.4 | Bipolar affective disorder | 1.5 | Alzheimer’s and other dementias | 6.8 |
| 7 | Epilepsy | 7.9 | Migraine | 1.4 | Drug-use disorders | 6.5 |
| 8 | Migraine | 7.8 | Panic disorde | 0.8 | Migraine | 6.3 |
| 9 | Panic disorder | 7.0 | Insomnia (primary) | 0.8 | Panic disorder | 6.2 |
| 10 | Obsessive-compulsive disorder | 5.1 | Parkinson’s disease | 0.7 | Obsessive-compulsive disorder | 4.5 |
| 11 | Insomnia (primary) | 3.6 | Obsessive-compulsive disorder | 0.6 | Posttraumatic stress disorder | 3.0 |
| 12 | Posttraumatic stress disorder | 3.5 | Epilepsy | 0.5 | Insomnia (primary) | 2.9 |
| 13 | Parkinson’s disease | 1.7 | Posttraumatic stress disorder | 0.5 | Multiple sclerosis | 1.2 |
| 14 | Multiple sclerosis | 1.5 | Multiple sclerosis | 0.3 | Parkinson’s disease | 1.0 |
a Examples of MNS disorders under the purview of the Grand Challenges in Global Mental Health initiative.
b World Bank criteria for income (2009 gross national income per capita): low income is US$995 equivalent or less; middle income is $996-$12,195; high income is $12,196 or more
c A disability-adjusted life-year (DALY) is a unit for measuring the amount of health lost because of a disease or injury. It is calculated as the present value of the future years of disability-free life that are lost as a result of the premature deaths or disability occurring in a particular year.
SOURCE: Collins et al., 2011. Reprinted with permission from Macmillian Publishers, Ltd. Nature: http://www.nature.com/nature/index.html.
areas having a wider treatment gap than urban ones, which likely reflects some combination of inadequate access to services; stigma, negative beliefs, and discriminatory attitudes about epilepsy; and low health literacy (Ngugi et al., 2010). However, as described further below, stigma is universal: “[Everywhere in the world it is a hidden disease” (de Boer, 2010, p. 631).
While most people only see the seizures themselves, there is far more to epilepsy. Being proactive in treatment means not only taking daily medication, but also participating in activities, talking to doctors or therapists as necessary, actively participating in school, and thriving at work.
-Elizabeth Musick
The occurrence of two or more unprovoked seizures separated by at least 24 hours is the broad operational definition of epilepsy (ILAE, 1993), which the committee uses for the purposes of this report. Seizures6 are, in essence, symptoms of epilepsy, and epilepsy is the disorder. However, the details are much more complex.7 Seizures differ from person to person with respect to their cause and severity, the areas of the brain involved, the location(s) and functions of the body affected, the effectiveness of medications and other treatments, and many other factors. These large and significant differences are why epilepsy, as noted, is understood as a spectrum of disorders—the epilepsies. More than 25 epilepsy syndromes and other epilepsy disorders have been delineated (Berg et al., 2010). While epilepsy is a chronic disorder, some people with epilepsy, particularly children, go into remission (Berg et al., 2001; Callaghan et al., 2007; Choi et al., 2011; Sillanpää and Schmidt, 2006).
Individuals with epilepsy are at risk not only for seizures, but also for a myriad of comorbid health conditions (i.e., conditions that occur in persons with epilepsy more than would be expected by chance; Chapter 3). Often the comorbidities that accompany epilepsy outweigh the burden of the seizures themselves. Common comorbidities that occur in epilepsy include cognitive dysfunction, such as memory, attention, or concentration problems; mental health conditions, such as depression or anxiety; and somatic comorbidities, such as sleep disorders, migraines, or cardiovascular disease. Other health problems can occur as a result of ongoing seizures, the cause of the epilepsy, or problems associated with the treatment, such
_______________
6 An epilepsy seizure has been defined as a “transient occurrence of signs and/or symptoms due to abnormal excessive or synchronous neuronal activity in the brain” (Fisher et al., 2005, p. 470).
7This report does not provide an in-depth clinical description of the epilepsies; resources such as Ropper and Samuels (2009) and Bazil and Pedley (2009) can be consulted for additional information.
as fractures and other injuries, osteoporosis, reproductive problems, and even death. Several disorders are causally related to developing epilepsy. These include traumatic brain injury, brain tumor, stroke, central nervous system infection, autism spectrum disorders, Alzheimer’s disease, and genetic disorders (such as Rett syndrome and tuberous sclerosis complex, among others). Further, epilepsy is associated with substantially higher rates of mortality than experienced in the population as a whole (Chapter 3). Goals for epilepsy efforts focus on preventing seizures in people at risk, controlling seizures in those with epilepsy, eliminating side effects of treatments, and helping people with epilepsy and their families achieve a high quality of life.
Not all seizures or seizure-like events are epilepsy (Figure 1-2). One of the challenges for neurologists and other health care providers is to determine whether their patient is having seizures because of electrical activity in the brain and, if so, the seizures’ type and cause. For some seizures, such as febrile seizures, the cause and treatment may be relatively straightforward (AAP Subcommittee on Febrile Seizures, 2011), although even a single seizure can have health and quality of life implications. Many medical problems including migraines, cardiac problems, or sleep disorders can give rise to events that appear similar to seizures. These seizure-like events, including those with a psychological basis, are not caused by electrical disturbances in the brain, and identifying the cause and determining appropriate treatments may be challenging (Binder and Salinsky, 2007; Devinsky et al., 2011).
TERMINOLOGY, STIGMA, MISPERCEPTIONS, AND CULTURAL BELIEFS
A major challenge for people with epilepsy, as well as for the epilepsy field, has been the multitude of ways that epilepsy is perceived and, in many cases, misperceived. The unpredictable nature of seizures, the feelings of helplessness of those who witness them, and the centuries of misperceptions and misinformation about epilepsy have resulted in people with epilepsy being stigmatized and isolated. Baker and colleagues (2008), for example, found that 36 percent of students with epilepsy said that they had kept their epilepsy a secret, because they did not want to be treated differently (23 percent of their parents also did not disclose the diagnosis because they did not want their son or daughter to face the potential stigma). This type of internalized stigma (i.e., “felt” stigma) can reduce quality of life even when seizures are well controlled by medications or other treatments. In a history of epilepsy, Eadie and Bladin (2001) wrote, “It can be safely said that epilepsy has been one of the least understood and most maligned of medical conditions” (p. 230).
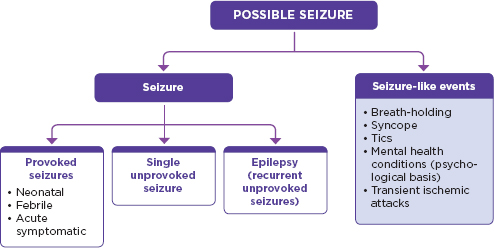
FIGURE 1-2
Seizures and seizure-like events
NOTES
• Neonatal seizures are seizures that occur in infants ≤ 4 weeks old (ILAE, 1993). While epilepsy can begin in the neonatal period, neonatal seizures are frequently reactive to an acute injury and often do not persist beyond a few days or weeks (Glass et al., 2011; Mizrahi and Clancy, 2000).
• Febrile seizures are seizures “occurring in childhood after age 1 month, associated with a febrile illness not caused by an infection of the CNS [central nervous system], without previous neonatal seizures or a previous unprovoked seizure, and not meeting criteria for other acute symptomatic seizures" (ILAE, 1993, p. 593).
• Acute symptomatic seizures are seizures “occurring in close temporal association with an acute systemic, metabolic, or toxic insult or in association with an acute CNS insult (infection, stroke, cranial trauma, ntracerebral hemorrhage, or acute alcohol intoxication or withdrawal)" (ILAE, 1993, p. 594)
• Single unprovoked seizures include a single cluster occurring within a 24-hour period or a single episode of status epilepticus (ILAE, 1993)
• Seizure-like events with a psychological basis are “events resembling epileptic seizures that are not caused by paroxysmal neuronal discharges or other physiologic problems, and are thought to be of psychological origin” (Salinsky et al., 2011, p. 945).
Epilepsy was recognized as early as circa 1050 B.C.E. in Babylon, and Hippocratic writings talk about epilepsy as a disorder of the brain as early as circa 400 B.C.E. (Eadie and Bladin, 2001; Epilepsy.com, 2011c; Reynolds and Kinnier Wilson, 2008; Temkin, 1971). Throughout the centuries, associations of seizures with mental health conditions, witchcraft, and demonic or divine possession have resulted in terminology with negative and sensationalized connotations and led to cultural and societal beliefs, perceptions, and stereotypes about epilepsy that can be difficult to modify. For example, although depictions in the movies of characters with epilepsy are becoming more realistic, examples of characters with seizures being portrayed as violent or dangerous still persist, as do inaccurate and misleading depictions in print media (Baxendale, 2003; Krauss et al., 2000).
Some cultural beliefs include misperceptions that the person with epilepsy is being punished for sins, has a lack of spiritual faith, is taking illegal drugs, or is possessed by spirits (Sirven et al., 2005; Szaflarski et al., 2006). As a consequence, people with epilepsy and their families may be faced with a lack of social support from extended family members, feelings of parental guilt, social isolation, embarrassment and fear (particularly connected with having a seizure in public), and discrimination. Although efforts are being made to correct these misconceptions and to better inform people about the epilepsies, doing so remains a challenge (Chapter 8). Awareness and sensitivity to individual and cultural beliefs about epilepsy and about medicine and health care (including traditional healing techniques in some cultures) are key considerations for efficient and effective interactions between health professionals and individuals with epilepsy.
Epilepsy-related terminology is complex. Historically, terms to describe the disorder have included “the sacred disease” and “falling sickness,” and, until recently, seizures have been termed “fits” and “spells.” The committee considered the terminology to be used throughout this report carefully. As noted above, epilepsy is a spectrum of disorders—ranging from severe, life-threatening, and disabling disorders to ones that are much more benign and sometimes transient. Therefore, the term “epilepsies” is more descriptive of the spectrum. The plural use of the term, however, can be cumbersome as in “people with the epilepsies.” In this report, for the sake of clarity, the committee generally uses the singular “epilepsy,” except when it is important to remind readers of the considerable spectrum of disability that the epilepsies represent. The report does not use the term “seizure disorders” because, as discussed above, there are a number of conditions that result in seizures that are not epilepsy.
The epilepsy field has moved away from the use of the term “epileptics” and toward the phrase “people with epilepsy,” just as other general terms such as “the disabled,” “the elderly,” and “the homeless” have been replaced with the phrases “people with disabilities,” “older adults,” and “homeless individuals.” Because the term “epileptic” has a pejorative connotation, the committee believes it should be discontinued. To paraphrase a 16-year-old with epilepsy, “Epilepsy is what I have, not who I am” (Clark, 2011). Throughout the report the committee suggests using more precise— and less negative terms—such as “seizure medications” (to replace “anti-epileptic drugs”), epilepsy seizures (to replace “epileptic seizures”), and “seizure-like events with a psychological basis” (rather than psychogenic, non-epileptic seizures).
Types of Seizures and Syndromes
Although much remains to be learned about the neuroscience of the epilepsies and the causes of specific types of epilepsy, generally seizures are caused by excessive and hypersynchronized neuron discharges in the brain (McNamara, 1994; Pitkanen and Lukasiuk, 2011). These discharges can involve widespread areas of the brain simultaneously or be focused in one specific area. The effects of seizures on a person’s health and well-being depend on the location and extent of the nerve cells involved; as a result, seizures can range from mild (such as a momentary loss of awareness) to severe (such as body convulsions).
Defining and categorizing the multiple types of epilepsy can be difficult. In 1964, the International League Against Epilepsy (ILAE) developed a classification system for epilepsy seizures and syndromes that continues to be updated (Arnautova and Nesmeianova, 1964; Berg et al., 2010). Because of the complex and disparate nature of where and to what extent the brain is affected by seizures, the epilepsies can be categorized according to multiple dimensions:
• Seizure type—Seizures are classified into two major categories: (1) focal seizures that originate in a network of neurons limited to one hemisphere of the brain and (2) generalized seizures that originate in a network of neurons that is distributed to both brain hemispheres (Berg et al., 2010). Seizures also can be categorized as of unknown type. Box 1-2 provides an overview of seizure types.
• Syndromes—Berg and colleagues (2010) recently defined a syndrome as “a complex of clinical features, signs, and symptoms that together define a distinctive, recognizable clinical disorder” (p. 681). Often, a syndrome is characterized by the typical age of onset, specific characteristics of the electroencephalogram (EEG), and seizure types. Table 1-3 provides an overview of a few of the many epilepsy syndromes.
As described by Engel (2001), in addition to seizure type and syndrome, other dimensions used to characterize the epilepsies can include the specific etiology (cause), the extent of impairment, and general descriptions of the seizure(s).
Most seizures last from fractions of a second to less than a minute and end on their own without intervention. However, sometimes a seizure does not stop spontaneously. Status epilepticus is usually defined as a prolonged seizure or series of seizures without full recovery of consciousness
Focal seizures originate within a network of neurons limited to one hemisphere of the brain, and the signs and resulting symptoms depend on precisely where the disruptions in brain activity occur. Focal seizures may have motor, sensory, autonomic, or other symptoms (e.g., hallucinations, deja vu). Focal seizures are often categorized as
• those without impairment of consciousness or awareness or
• those with impairment of consciousness or awareness.
Generalized seizures originate within a network of neurons that is distributed to both hemispheres of the brain and vary considerably in their clinical features, from subtle alterations in consciousness to body convulsions. Generalized seizures are categorized as the following:
• Tonic-clonica seizures—A generalized tonic-clonic (previously called grand mal) seizure is a severe type of seizure that starts with a sudden loss of consciousness and generalized stiffening of the body (tonic phase) followed by contraction of the muscles (clonic phase).
• Absence seizures—Often common in childhood, absence (previously called petit mal) seizures are generally brief lapses in awareness. Some clonic motor activity may occur.
• Myoclonic seizures—Characterized by sudden and brief muscular contractions, myoclonic seizures may involve any group of muscles and can resemble tremors.
• Clonic seizures—These seizures consist of alternating successions of contractions and partial relaxations of a muscle.
• Tonic seizures—These brief seizures involve a sudden onset of increased muscle tone.
• Atonic seizures—Characterized by a sudden loss of muscle tone, atonic seizures begin suddenly and cause the individual, if standing, to fall quickly to the floor.
_____________
aThe term tonic describes the prolonged muscular contraction. The term clonic describes the rapid alternating succession of contractions and partial relaxations of a muscle.
SOURCES: Bazil and Pedley, 2009; Berg et al., 2010; Ropper and Samuels, 2009.
in between (Bazil and Pedley, 2009). In clinical care this generally involves seizures lasting longer than 5 minutes. Status epilepticus can occur in individuals who do not have a prior history of seizures. Status epilepticus is a neurological emergency and can be fatal.
In the past two decades, awareness has been raised about high rates of SUDEP; people with epilepsy have a more than 20 times higher rate of sudden death than does the general population (Ficker et al., 1998). Little
TABLE 1-3
Examples of Epilepsy Syndromes with Differing Severities
| Syndrome | Description | Disease Course |
| Benign rolandic epilepsya (benign childhood epilepsy with centrotemporal spikes) | Infrequent seizures in children typically occurring at night, generally affecting the facial muscles, may be accompanied by tonic-clonic seizures | Average age of onset is 6 to 8 years, seizures go into remission without treatment, usually stopping by age 15 years |
| Childhood and juvenile absence epilepsy | Commonly involves brief (about 10 seconds) staring episodes or times of seeming to be absent | Childhood absence epilepsy has an onset between ages 4 and 10 years, and the majority of absence seizures stop by mid-adolescence. Juvenile absence epilepsy may evolve into juvenile myoclonic epilepsy, which may require lifelong treatment with medications |
| Juvenile myoclonic epilepsy | Involves absence seizures, myoclonic seizures, and generalized tonic-clonic seizures; often characterized by myoclonic jerks that occur when waking up | Onset usually between ages 5 and 16 years, seizures may improve after the fourth decade of life. Seizures are generally well controlled with medications |
| Temporal lobe epilepsy | Seizures include focal seizures with or without out impairment of consciousness, including auras | May start in childhood, but most common in adolescence or early adulthood. Varying responses to medications; however, seizures that arise from one temporal lobe respond well to surgery |
| Dravet syndrome | Begins with frequent febrile seizures with later myoclonic seizures; often children have poor development of language and motor skills | Genetic disorder with onset typically during the first year of life; degree of cognitive impairment may stabilize or improve slightly with age depending on the frequency of the seizures |
| Lennox-Gastaut syndrome | Involves multiple types of seizures including tonic and atonic seizures; children often have impaired intellectual functioning and developmental delays | Accounts for approximately 2 to 5 percent of childhood epilepsies; difficult to control with medications |
aAlso termed “rolandic epilepsy.”
SOURCES: Epilepsy.com, 2011a,b,d,e,f,g; NINDS, 2011b.
is known about the causes of SUDEP, although rates are higher in people with seizures that are refractory8 (Tomson et al., 2005; Chapter 3).
Health Care
Epilepsy is typically diagnosed by self-report of seizures (or report by family members) and the patient’s medical history, since it is unusual for the health care provider to actually observe a seizure during an office visit. Whereas some seizures, such as generalized tonic-clonic seizures, are relatively easy to diagnose, other types, such as absence or focal seizures, may be more challenging. As noted above, a number of medical problems can mimic epilepsy seizures. Tests such as the EEG and magnetic resonance imaging often provide support for the diagnosis (Chapter 4). Continuous video-EEG monitoring over several days is an option that provides an opportunity to record a seizure and is typically used to confirm the diagnosis, determine seizure type, and inform decisions about whether surgery is a viable treatment option.
The major medically based approaches to seizure treatment are medications, medical devices, and surgery. Additionally, other treatments, including behavioral and dietary approaches, may be used. Epilepsy treatment is often highly effective in reducing or eliminating seizures. However, most treatments are used to suppress seizures and do not cure the disorder. In a study of newly diagnosed people with epilepsy, using both older and more recently introduced seizure medications, up to 63 percent of individuals became seizure free during treatment (Kwan and Brodie, 2000); seizures in approximately half of patients were controlled with the first seizure medication tried. When a second drug was necessary, an additional 13 percent became seizure-free. However, among those whose seizures persisted after treatment with two epilepsy medications, only an additional 4 percent controlled their seizures through subsequent medication trials. For many people with epilepsy, concerns about medications include the effectiveness of the medications in seizure control, side effects, dosing schedules, and high costs (Fisher et al., 2000b). In a community-based survey, only 68 percent of people with epilepsy were very satisfied with their current seizure medication (Fisher et al., 2000b). While relatively few individuals with epilepsy are candidates for surgery in which brain tissue involved in the origin of the seizure is removed, this is a therapy that reduces or eliminates seizures for some individuals. Medical devices are also an effective treatment option for some people with epilepsy (Chapter 4). An important consideration regarding health care for people with epilepsy is the need to
_______________
8Refractory epilepsy is defined as the failure to control seizures after two seizure medications (whether as monotherapies or in combination) have been appropriately chosen and used (Chapter 4) (Kwan et al., 2010).
use a whole-patient approach—not only trying to eliminate or alleviate the seizures but also treating comorbid health conditions—which will necessitate coordinated care among a number of health professionals.
Although there is wide variation in experiences, individuals with new-onset seizures are often first seen in an emergency room or by a primary care provider (Chapter 4). Depending on the availability of neurologists, the primary care provider’s expertise, the type or severity of initial seizure(s), and initial findings on examination, patients may be referred to a general neurologist for further evaluation, diagnosis, and treatment. Epilepsy specialists (epileptologists9) provide specialty care and are generally a part of an epilepsy center, which has the expertise and facilities to provide thorough patient assessments and, if indicated, surgical and device consultations and treatment, as well as connections to other health professionals (detailed below), as needed. Clinical practice guidelines and recommendations from professional organizations suggest that when the diagnosis is in question, or seizure control is not achieved after (1) a trial of two or three appropriate seizure medications or (2) 1 year of care with a general neurologist, patients should be referred to an epileptologist or epilepsy center (Cross et al., 2006; Labiner et al., 2010). Whether and when patients actually receive such a referral vary greatly (as do other aspects of health services for epilepsy; see Appendix B). Chapter 4 emphasizes the need to ensure a more timely referral process. Some patients are not referred to an epilepsy center for surgical consultation until 15 or more years after initial diagnosis and years of living with uncontrolled seizures (Haneef et al., 2010). Currently, 166 health care facilities—located in 42 states, the District of Columbia, and Puerto Rico—identify themselves as epilepsy centers (NAEC, 2012) (see also Appendix C).
Over the continuum of care from diagnosis to treatment and management, people with epilepsy may encounter a variety of health professionals, including an array of physicians (e.g., neurologists, epileptologists, psychiatrists, neurosurgeons, primary care physicians), nurses, psychologists and counselors, pharmacists, emergency medical technicians and first responders, electroneurodiagnostic technologists, physical and occupational therapists, community health workers, and direct care workers, who play a variety of roles in their health care (Appendix D provides an overview of these roles and the relevant professional boards and organizations). To ensure that people with epilepsy and their families have access to high-quality, patient-centered, coordinated care, the health care workforce’s knowledge base and skills in diagnosing, treating, supporting, referring, and gener-
_______________
9Neurologists with concentrated training in epilepsy are designated as epileptologists. A new subspecialty board certification in epileptology is being created by the American Board of Psychiatry and Neurology. A board-certification examination for epileptologists will be offered for the first time in 2013 (Chapter 5).
ally working with people with epilepsy need to be enhanced. As discussed in Chapter 5, health professionals need current knowledge about many aspects of the epilepsies: seizure recognition and diagnosis; prevention strategies and treatment options; associated comorbidities, risks, and safety concerns; necessary social services; psychosocial and quality-of-life factors; and countering stigma. The specific types and depth of knowledge required vary across professions, depending on the roles, responsibilities, and scope of practice of the professionals and the specific settings in which they work.
Quality of Life and Community Services
Living with epilepsy is about seizures but also much more. Beyond the seizures, comorbid health conditions and epilepsy-related limitations can have an impact on many aspects of health and quality of life. Living with epilepsy, particularly refractory epilepsy, can involve challenges in school, uncertainties about social and employment situations, limitations on driving, and questions about independent living.
In a U.S. community-based survey that received responses primarily from adults with epilepsy, respondents noted that the major problems they experienced due to having epilepsy included limitations on daily activities, stigma, family concerns, and fear of the seizures (Fisher et al., 2000a). Survey respondents had median household incomes less than the general population, and unemployment among people with epilepsy who were able to work was five times higher than the national rate at the time. Side effects of seizure medications were a problem for many; the most common concerns noted were cognitive problems and impacts on energy level, school performance, motor skills coordination, having children, and sexual function (Fisher et al., 2000b). Similarly, in focus groups of people with epilepsy in South Carolina, many participants said they had to change life plans due to having epilepsy (Sample et al., 2006). These and similar surveys reinforce well-documented challenges for many people with epilepsy that extend beyond medical care. The need to treat the whole person and family often requires a network of professionals and agencies across a variety of health care and community settings (Chapters 4 and 6).
Educating People with Epilepsy and Their Families
Much is being done and more is needed to educate people with epilepsy and their families about the disorder, the range of treatment options, and the array of community services that might be helpful to achieve optimal self-management10 (Chapter 7). Access to information about topics such as
_______________
10Self-management for epilepsy includes the information and resources that people with epilepsy and their families need to develop skills and behaviors that enable them to actively
diagnosis, prognosis, treatment, strategies for injury prevention and healthy living, employment rights and protections, and self-management skills can increase the individual’s (and family’s) sense of empowerment, promote adaptation to the disorder, and enhance overall quality of life (Couldridge et al., 2001).
Because of the complexity of epilepsy and the varied cultural perceptions connected to the disorder, both health literacy and attention to cultural considerations are particularly relevant. Health literacy is understood as “the degree to which individuals have the capacity to obtain, communicate, process, and understand basic health information and services needed to make appropriate health decisions” (Ratzan and Parker, 2000, p. vi). Nearly 9 out of every 10 adults in the United States have limited health literacy (many have limited general literacy as well), and although limited health literacy is widespread and not specific to any sociodemographic group, it disproportionately affects certain population subgroups, including people in lower socioeconomic groups, racial/ethnic minorities, people with disabilities, and older adults (Grabois et al., 1999; Kutner et al., 2006; ODPHP, 2010). Kutner and colleagues (2006) found that only 12 percent of English-speaking U.S. adults have “proficient” health literacy skills. Ensuring that health information is conveyed in ways that are understandable and take into account cultural considerations is key to making sure that all people with epilepsy have the tools to understand and deal with their disorder and attain optimal quality of life. Health literacy is not solely attributable to the characteristics of the individual but also reflects the efforts of the health care and educational systems, and much can be done to provide information that is easily and well understood.
Biomedical Research on Epilepsy
This report comes at a time when the number of new discoveries about the brain and its associated disorders is increasing rapidly, and innovative tools and approaches continue to be developed and refined that can allow researchers to examine the mechanisms of a range of neurological disorders. As a result, improved treatments and, ultimately, preventive measures and cures may become possible. Although it is not within the purview of this report to examine the biomedical research agenda, it is important to acknowledge that recent biomedical research advances in epilepsy include improving the understanding of the mechanisms of
_______________
participate in patient-centered care; it is “the sum total of steps taken and processes used by a person to control seizures and manage the effects of having a seizure disorder” (DiIorio, 1997, p. 214). The committee adopted the concept of “optimal self-management,” recognizing that it represents a wide range of possibilities toward autonomy and independence and that what is optimal for one person may be beyond the capacity of another (Chapter 7).
epileptogenesis; identifying clinical and genetic correlations of epilepsy; exploring and refining prevention and treatment options; and improving technologies for imaging.
The NINDS, in collaboration with many professional and voluntary epilepsy organizations and stakeholders, held two Curing Epilepsy Conferences that developed and updated the Epilepsy Research Benchmarks (NINDS, 2007b, 2010). The first, held in 2000, developed benchmarks for a research agenda to cure epilepsy. A follow-up conference in 2007 demonstrated many biomedical advances toward this goal, identified critical areas needing further attention, and focused new attention on the comorbidities that complicate epilepsy. The benchmarks continue to be updated to reflect progress in epilepsy-related research (NINDS, 2010). Key areas of focus in the benchmarks, and in National Institutes of Health (NIH) research initiatives in general, are in translating basic research into practical applications and comparative effectiveness studies to identify effective interventions (NIH, 2011a,b).
The level of epilepsy research funding at the NIH in fiscal year 2011 was estimated to be $134 million (Meador et al., 2011).11 An analysis by Meador and colleagues (2011) found that epilepsy—the third most prevalent of the six neurological diseases examined—gets less funding than the other disorders when adjusted for prevalence (comparisons ranged from 1.7 times as much funding for stroke to 61.1 times as much for amyotrophic lateral sclerosis). To date, treatment of epilepsy has been focused on suppressing seizures rather than curing the disorder. With further research it is hoped that symptomatic treatment will be replaced with curative treatment and with prevention strategies.
Mobilizing the Public Health Response to Epilepsy
A number of organizations are working on research, programs, and policies to improve health and human services for people with epilepsy and their families, as well as being active in promoting prevention, education, and awareness of epilepsy. Many of the recent public health efforts focused on epilepsy, particularly in the United States, draw from the initiatives and priorities put forth by the 1978 U.S. Commission for the Control of Epilepsy and Its Consequences (U.S. Commission for the Control of Epilepsy and Its Consequences, 1978) and the Living Well with Epilepsy conferences held in 1997 and 2003 (AES et al., 2004; CDC et al., 1997). Sponsored by the Centers for Disease Control and Prevention, the Epilepsy Foundation, the American Epilepsy Society, the National Association of Chronic Disease Directors, and the National Association of Epilepsy Centers, the Living
_______________
11Actual spending in fiscal year 2011 was $152 million (NIH, 2012).
Well conferences spearheaded the development of a public health agenda for the epilepsies and resulted in a set of recommendations and goals that a range of research, public policy, community service, and advocacy efforts have since pursued.
The following collaborative public health initiatives highlight coordinated efforts that are under way. Other examples are provided throughout the report of the many organizations and individuals working to prevent, treat, and cure epilepsy and its comorbidities:
• The Vision 20-20 coalition was formed in 2004 and originally brought together five nonprofit organizations and one federal agency focused on epilepsy research. Initially the organizations shared progress on their own initiatives and funding resources and explored areas for collaboration. As of January 2012, 22 organizations and 3 federal agencies are part of the coalition and work through joint meetings and subgroups to develop and promote a “common message” that can be used to support efforts in epilepsy prevention, health care, research, and public awareness (Personal communication, Margaret Jacobs, American Epilepsy Society, January 5, 2012).
• The U.S. Department of Health and Human Services has organized an Interagency Collaborative to Advance Research in Epilepsy with membership from 20 federal agencies, as well as from research and advocacy groups (NINDS, 2011a). Vision 20-20 representatives are also invited to participate in the interagency working group.
• Globally, the ILAE, the International Bureau of Epilepsy, and the World Health Organization have led efforts, including the Global Campaign Against Epilepsy: Out of the Shadows, to increase public awareness and education about epilepsy and eliminate the barriers and stigma often associated with it (WHO, 2011). The campaign supports public and professional education and awareness, identifies service gaps and supports demonstration projects for national and regional areas, and promotes involvement of government and public health departments to target the needs of people with epilepsy (ILAE, 2011b; WHO, 2011).
• The Pan American Health Organization (PAHO) recently endorsed a Strategy and Plan of Action on Epilepsy (PAHO, 2011). This resolution encourages the more than 35 member nations of PAHO to develop national programs for epilepsy. Similar efforts by European Union nations in 2011 resulted in a Written Declaration on Epilepsy that urges research, policy assessment, and equitable services relevant to epilepsy (ILAE, 2011a).
Throughout this report several cross-cutting themes are highlighted by the committee:
• Epilepsy is a common and a complex neurological disorder. Epilepsy is not a single disorder but rather a spectrum of disorders— the epilepsies. Further, epilepsy is more than seizures and may be accompanied by a range of associated comorbid health conditions that can have significant health and quality-of-life implications. Some people with epilepsy have lives that are essentially unchanged, while others’ health and well-being are severely affected, and for some people, epilepsy is fatal. Communicating this range of outcomes and meeting the spectrum of needs are major challenges faced by the epilepsy field.
• Epilepsy often affects quality of life. For many individuals with epilepsy and their family members, living with epilepsy means challenges in school and work, social functioning and relationship dynamics, limits on driving, and daily worries about the possibility of seizures.
• A whole-patient perspective is needed. Because the effects of epilepsy go beyond health concerns and seizures, a whole-patient, patient-centered perspective is needed that provides people with epilepsy, their families, and caregivers with a coordinated, individual-specific approach to health care, mental health care, educational opportunities, and community services and promotes optimal self-management and quality of life.
• Effective treatments are available for many types of epilepsies, but timely referrals and access to those treatments fall short. For many people with epilepsy, seizures can be effectively reduced or eliminated by medications, surgery, devices, and dietary or other therapies. However, in the United States, referrals to epileptologists and epilepsy centers for surgical consultations can take 15 years or more.
• Data are lacking that could improve epilepsy care. Accurate, timely data on the extent and consequences of epilepsy and comorbid conditions and on health care and community services use and outcomes are sorely needed to make improvements in epilepsy prevention; diagnosis; health care access, quality, and value; and community services.
• Many health professionals need to be better informed about epilepsy. Improvements in epilepsy care can be made only if the quality and quantity of education about epilepsy for health care
professionals are improved dramatically through undergraduate and graduate levels and lifelong learning programs.
• Education efforts for people with epilepsy and their families need to be thorough and sensitive to health literacy and cultural considerations. Across the continuum from initial diagnosis through ongoing treatments and services, people with epilepsy and their families need to be aware of the disorder’s potential risks, including SUDEP, and the range of treatments and services available. Information must be conveyed in ways that are easily understandable and relevant to specific age groups and cultures.
• The stigma associated with epilepsy needs to be eliminated. The long history of epilepsy is full of examples of discrimination and secrecy due to misinformation and lack of understanding by the general public. Since stigma can have a detrimental effect on people with epilepsy, continued and sustained efforts are needed to raise public awareness and convey what epilepsy is and what it is not, as well as the basic messages embodied in these themes.
AAP (American Academy of Pediatrics) Subcommittee on Febrile Seizures. 2011. Febrile seizures: Guideline for the neurodiagnostic evaluation of the child with a simple febrile seizure. Pediatrics 127(2):389-394.
AES (American Epilepsy Society), CDC (Centers for Disease Control and Prevention), Chronic Disease Directors, Epilepsy Foundation, and NAEC (National Association of Epilepsy Centers). 2004. Living Well with Epilepsy. II: Report of the 2003 National Conference on Public Health and Epilepsy: Priorities for a public health agenda on epilepsy. http://www.cdc.gov/epilepsy/pdfs/living_well_2003.pdf (accessed February 2, 2012).
Arnautova, E. N., and T. N. Nesmeianova. 1964. A proposed international classification of epileptic seizures. Epilepsia 5:297-306.
Baker, G. A., E. Hargis, M. M.-S. Hsih, H. Mounfield, A. Arzimanoglou, T. Glauser, J. Pellock, S. Lund, and the International Bureau for Epilepsy. 2008. Perceived impact of epilepsy in teenagers and young adults: An international survey. Epilepsy and Behavior 12(3):395-401.
Baxendale, S. 2003. Epilepsy at the movies: Possession to presidential assassination. Lancet Neurology 2(12):764-770.
Bazil, C. W., and T. A. Pedley. 2009. Epilepsy. In Merritt’s neurology. 12th ed., edited by L. P. Rowland and T. P. Pedley. Philadelphia, PA: Lippincott Williams and Wilkins. Pp. 927-948.
Begley, C. E., M. Famulari, J. F. Annegers, D. R. Lairson, T. F. Reynolds, S. Coan, S. Dubinsky, M. E. Newmark, C. Leibson, E. L. So, and W. A. Rocca. 2000. The cost of epilepsy in the United States: An estimate from population-based clinical and survey data. Epilepsia 41(3):342-351.
Berg, A. T., S. Shinnar, S. R. Levy, F. M. Testa, S. Smith-Rapaport, B. Beckerman, and N. Ebrahimi. 2001. Two-year remission and subsequent relapse in children with newly diagnosed epilepsy. Epilepsia 42(12):1553-1562.
Berg, A. T., S. F. Berkovic, M. J. Brodie, J. Buchhalter, J. H. Cross, W. van Emde Boas, J. Engel, J. French, T. A. Glauser, G. W. Mathern, S. L. Moshe, D. Nordli, P. Plouin, and I. E. Scheffer. 2010. Revised terminology and concepts for organization of seizures and epilepsies: Report of the ILAE Commission on Classification and Terminology, 2005-2009. Epilepsia 51(4):676-685.
Binder, L. M., and M. C. Salinsky. 2007. Psychogenic nonepileptic seizures. Neuropsychology Review 17(4):405-412.
Callaghan, B. C., K. Anand, D. Hesdorffer, W. A. Hauser, and J. A. French. 2007. Likelihood of seizure remission in an adult population with refractory epilepsy. Annals of Neurology 62(4):382-389.
CDC (Centers for Disease Control and Prevention), AES, Epilepsy Foundation, and NAEC. 1997. Living Well with Epilepsy: Report of the 1997 National Conference on Public Health and Epilepsy. http://www.cdc.gov/epilepsy/pdfs/living_well_1997.pdf (accessed February 2, 2012).
Choi, H., G. A. Heiman, H. Munger Clary, M. Etienne, S. R. Resor, and W. A. Hauser. 2011. Seizure remission in adults with long-standing intractable epilepsy: An extended follow-up. Epilepsy Research 93(2-3):115-119.
Clark, S. E. 2011. It’s not who I am. http://www.itsnotwhoiam.com/uploads/Home_Page_Letter.pdf (accessed December 13, 2011).
Collins, P. Y., V. Patel, S. S. Joestl, D. March, T. R. Insel, A. S. Daar, W. Anderson, M. A. Dhansay, A. Phillips, S. Shurin, M. Walport, W. Ewart, S. J. Savill, I. A. Bordin, E. J. Costello, M. Durkin, C. Fairburn, R. I. Glass, W. Hall, Y. Huang, S. E. Hyman, K. Jamison, S. Kaaya, S. Kapur, A. Kleinman, A. Ogunniyi, A. Otero-Ojeda, M. M. Poo, V. Ravindranath, B. J. Sahakian, S. Saxena, P. A. Singer, and D. J. Stein. 2011. Grand challenges in global mental health. Nature 475(7354):27-30.
Couldridge, L., S. Kendall, and A. March. 2001. “A systematic overview—A decade of research.” The information and counselling needs of people with epilepsy. Seizure 10(8): 605-614.
Cross, J. H., P. Jayakar, D. Nordli, O. Delalande, M. Duchowny, H. G. Wieser, R. Guerrini, and G. W. Mathern. 2006. Proposed criteria for referral and evaluation of children for epilepsy surgery: Recommendations of the Subcommission for Pediatric Epilepsy Surgery. Epilepsia 47(6):952-959.
de Boer, H. M. 2010. Epilepsy stigma: Moving from a global problem to global solutions. Seizure 19(10):630-636.
Devinsky, O., D. Gazzola, and W. C. Lafrance, Jr. 2011. Differentiating between nonepileptic and epileptic seizures. Nature Reviews Neuroscience 7:210-220.
DiIorio, C. 1997. Epilepsy self-management. In Handbook of health behavior research II: Provider determinants. New York: Plenum Press. Pp. 213-230.
Dua, T., H. M. de Boer, L. L. Prilipko, and S. Saxena. 2006. Epilepsy care in the world: Results of an ILAE/IBE/WHO Global Campaign Against Epilepsy survey. Epilepsia 47(7):1225-1231.
Eadie, M. J., and P. F. Bladin. 2001. A disease once sacred: A history of the medical understanding of epilepsy. Eastleigh, UK: John Libbey and Company.
Engel, J., Jr. 2001. A proposed diagnostic scheme for people with epileptic seizures and with epilepsy: Report of the ILAE Task Force on Classification and Terminology. Epilepsia 42(6):796-803.
Epilepsy.com. 2011a. Benign rolandic epilepsy. http://www.epilepsy.com/epilepsy/epilepsy_benignrolandic (accessed October 19, 2011).
———. 2011b. Childhood absence epilepsy. http://www.epilepsy.com/EPILEPSY/epilepsy_childhoodabsence (accessed February 10, 2012).
———. 2011c. History of epilepsy. http://www.epilepsy.com/Epilepsy/history (accessed October 19, 2011).
———. 2011d. Juvenile absence epilepsy. http://www.epilepsy.com/EPILEPSY/epilepsy_juvenileabsence (accessed February 10, 2012).
———. 2011e. Juvenile myoclonic epilepsy. http://www.epilepsy.com/epilepsy/newsletter/May11_OnMyMind (accessed October 19, 2011).
———. 2011f. Lennox-Gastaut syndrome. http://www.epilepsy.com/EPILEPSY/epilepsy_lennoxgastaut (accessed October 19, 2011).
———. 2011g. Temporal lobe epilepsy. http://www.epilepsy.com/epilepsy/newsletter/apr11_onmymind (accessed October 19, 2011).
Ficker, D. M., E. L. So, W. K. Shen, J. F. Annegers, P. C. O’Brien, G. D. Cascino, and P. G. Belau. 1998. Population-based study of the incidence of sudden unexplained death in epilepsy. Neurology 51(5):1270-1274.
Fisher, R. S., B. G. Vickrey, P. Gibson, B. Hermann, P. Penovich, A. Scherer, and S. Walker. 2000a. The impact of epilepsy from the patient’s perspective. I: Descriptions and subjective perceptions. Epilepsy Research 41(1):39-51.
———. 2000b. The impact of epilepsy from the patient’s perspective. II: Views about therapy and health care. Epilepsy Research 41(1):53-61.
Fisher, R. S., W. van Emde Boas, W. Blume, C. Elger, P. Genton, P. Lee, and J. Engel, Jr. 2005. Epileptic seizures and epilepsy: Definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia 46(4):470-472.
Gaitatzis, A., A. L. Johnson, D. W. Chadwick, S. D. Shorvon, and J. W. Sander. 2004. Life expectancy in people with newly diagnosed epilepsy. Brain 127(Pt. 11):2427-2432.
Glass, H.C., K. J. Hong, E. E. Rogers, R. J. Jeremy, S. L. Bonifacio, J. E. Sullivan, A. J. Barkovich, and D. M. Ferriero. 2011. Risk factors for epilepsy in children with neonatal encephalopathy. Pediatric Research 70:535-540.
Grabois, E. W., M. A. Nosek, and C. D. Rossi. 1999. Accessibility of primary care physicians’ offices for people with disabilities. An analysis of compliance with the Americans with Disabilities Act. Archives of Family Medicine 8(1):44-51.
Haneef, Z., J. Stern, S. Dewar, and J. Engel, Jr. 2010. Referral pattern for epilepsy surgery after evidence-based recommendations: A retrospective study. Neurology 75(8):699-704.
Hauser, W. A., J. F. Annegers, and L. R. Elveback. 1980. Mortality in patients with epilepsy. Epilepsia 21(4):399-412.
Hesdorffer, D. C., G. Logroscino, E. K. T. Benn, N. Katri, G. Cascino, and W. A. Hauser. 2011. Estimating risk for developing epilepsy: A population-based study in Rochester, Minnesota. Neurology 76(1):23-27.
Hirtz, D., D. J. Thurman, K. Gwinn-Hardy, M. Mohamed, A. R. Chaudhuri, and R. Zalutsky. 2007. How common are the “common” neurologic disorders? Neurology 68(5):326-337.
ILAE (International League Against Epilepsy). 1993. Guidelines for epidemiologic studies on epilepsy. Commission on Epidemiology and Prognosis, International League Against Epilepsy. Epilepsia 34(4):592-596.
———. 2011a. European Union written declaration on epilepsy is approved. http://www.ilae.org/visitors/initiatives/EuropeanDeclaration2011.cfm (accessed January 9, 2012).
———. 2011b. Global outreach. http://www.ilae.org/Visitors/Archive/GlobalCampaign.cfm (accessed December 13, 2011).
Krauss, G. L., S. Gondek, A. Krumholz, S. Paul, and F. Shen. 2000. “The scarlet E”: The presentation of epilepsy in the English language print media. Neurology 54(10):1894-1898.
Kutner, M., E. Greenberg, Y. Jin, and C. Paulsen. 2006. The health literacy of America’s adults: Results from the 2003 National Assessment of Adult Literacy (NCES 2006-483). Washington, DC: National Center for Education Statistics.
Kwan, P., and M. J. Brodie. 2000. Early identification of refractory epilepsy. New England Journal of Medicine 342(5):314-319.
Kwan, P., A. Arzimanoglou, A. T. Berg, M. J. Brodie, W. A. Hauser, G. Mathern, S. L. Moshe, E. Perucca, S. Wiebe, and J. French. 2010. Definition of drug resistant epilepsy: Consensus proposal by the Ad Hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia 51(6):1069-1077.
Labiner, D. M., A. I. Bagic, S. T. Herman, N. B. Fountain, T. S. Walczak, and R. J. Gumnit. 2010. Essential services, personnel, and facilities in specialized epilepsy centers: Revised 2010 guidelines. Epilepsia 51(11):2322-2333.
Leonardi, M., and T. B. Ustun. 2002. The global burden of epilepsy. Epilepsia 43(Suppl. 6):21-25.
McNamara, J. O. 1994. Cellular and molecular basis of epilepsy. Journal of Neuroscience 14(6):3413-3425.
Meador, K. J., J. French, D. W. Loring, and P. B. Pennell. 2011. Disparities in NIH funding for epilepsy research. Neurology 77(13):1305-1307.
Meyer, A.-C., T. Dua, J. Ma, S. Saxena, and G. Birbeck. 2010. Global disparities in the epilepsy treatment gap: A systematic review. Bulletin of the World Health Organization 88(4):260-266.
Mizrahi, E. M., and R. R. Clancy. 2000. Neonatal seizures: Early-onset seizure syndromes and their consequences for development. Mental Retardation and Developmental Disabilities Research Reviews 6(4):229-241.
NAEC (National Assocciation of Epilepsy Centers). 2012. Epilepsy centers. http://www.naeclocator.org/locator/resultsall.asp (accessed January 5, 2012).
Ngugi, A. K., C. Bottomley, I. Kleinschmidt, J. W. Sander, and C. R. Newton. 2010. Estimation of the burden of active and life-time epilepsy: A meta-analytic approach. Epilepsia 51(5):883-890.
NIH (National Institutes of Health). 2011a. Comparative effectiveness research. http://www.nlm.nih.gov/hsrinfo/cer.html (accessed December 13, 2011).
———. 2011b. Translational research. http://commonfund.nih.gov/clinicalresearch/overview-translational.aspx (accessed December 13, 2011).
———. 2012. Estimates of funding for various research, condition, and disease categories. http://report.nih.gov/categorical_spending.aspx (accessed March 26, 2012).
NINDS (National Institute of Neurological Disorders and Stroke). 2007a. Curing epilepsy: The promise of research. http://www.ninds.nih.gov/disorders/epilepsy/Curing_Epilepsy_Brochure.pdf (accessed November 23, 2010).
———. 2007b. Update to NINDS epilepsy research benchmarks. http://www.ninds.nih.gov/research/epilepsyweb/epilepsy_benchmarks_guide_2007.pdf (accessed November 23, 2010).
———. 2010. 2010 epilepsy research benchmarks progress update (2007-2009). http://www.ninds.nih.gov/research/epilepsyweb/2010_benchmarks.pdf (accessed November 23, 2010).
———. 2011a. ICARE: Interagency Collaborative to Advance Research in Epilepsy. http://www.ninds.nih.gov/research/epilepsyweb/researchers/ICARE/index.htm (accessed December 13, 2011).
———. 2011b. NINDS Dravet syndrome information page. http://www.ninds.nih.gov/disorders/dravet_syndrome/dravet_syndrome.htm (accessed October 19, 2011).
———. 2011c. Seizures and epilepsy: Hope through research. http://www.ninds.nih.gov/disorders/epilepsy/detail_epilepsy.htm (accessed October 19, 2011).
ODPHP (Office of Disease Prevention and Health Promotion). 2010. National action plan to improve health literacy. Washington, DC: HHS.
PAHO (Pan American Health Organization). 2011. Strategy and plan of action on epilepsy. http://www.ilae-epilepsy.org/visitors/news/documents/PAHOEpilepsyStrategyEnglish.pdf (accessed December 13, 2011).
Pitkanen, A., and K. Lukasiuk. 2011. Mechanisms of epileptogenesis and potential treatment targets. Lancet Neurology 10(2):173-186.
Ratzan, S. C., and R. M. Parker. 2000. Introduction. In National Library of Medicine current bibliographies in medicine 2000-1: Health literacy. Bethesda, MD: National Institutes of Health.
Reynolds, E. H., and J. V. Kinnier Wilson. 2008. Psychoses of epilepsy in Babylon: The oldest account of the disorder. Epilepsia 49(9):1488-1490.
Ropper, A., and M. Samuels. 2009. Epilepsy and other seizure disorders. In Adams and Victor’s principles of neurology. 9th ed. New York: McGraw-Hill. Pp. 304-338.
Salinsky, M., D. Spencer, E. Boudreau, and F. Ferguson. 2011. Psychogenic nonepileptic seizures in U.S. veterans. Neurology 77(10):945-950.
Sample, P. L., P. L. Ferguson, J. L. Wagner, E. E. Pickelsimer, and A. W. Selassie. 2006. Experiences of persons with epilepsy and their families as they look for medical and community care: A focus group study from South Carolina. Epilepsy and Behavior 9(4):649-662.
Sillanpää, M., and D. Schmidt. 2006. Natural history of treated childhood-onset epilepsy: Prospective, long-term population-based study. Brain 129(Pt. 3):617-624.
Sirven, J. I., R. A. Lopez, B. Vazquez, and P. Van Haverbeke. 2005. Qué es la epilepsia? Attitudes and knowledge of epilepsy by Spanish-speaking adults in the United States. Epilepsy and Behavior 7(2):259-265.
Szaflarski, M., J. P. Szaflarski, M. D. Privitera, D. M. Ficker, and R. D. Horner. 2006. Racial/ethnic disparities in the treatment of epilepsy: What do we know? What do we need to know? Epilepsy and Behavior 9(2):243-264.
Temkin, O. 1971. The falling sickness: A history of epilepsy from the Greeks to the beginnings of modern neurology. 2nd ed. Baltimore, MD: Johns Hopkins University Press.
Thurman, D. 2011. Epidemiologic research and surveillance of the epilepsies: A systems-level perspective. PowerPoint presented at the IOM Meeting on Public Health Dimensions of the Epilepsies, Washington, DC, January 10. http://iom.edu/~/media/Files/Activity%20Files/Disease/Epilepsy/Thurman%202.pdf (accessed October 19, 2011).
Thurman, D. J., E. Beghi, C. E. Begley, A. T. Berg, J. R. Buchhalter, D. Ding, D. C. Hesdorffer, W. A. Hauser, L. Kazis, R. Kobau, B. Kroner, D. Labiner, K. Liow, G. Logroscino, M. T. Medina, C. R. Newton, K. Parko, A. Paschal, P.-M. Preux, J. W. Sander, A. Selassie, W. Theodore, T. Tomson, and S. Wiebe. 2011. Standards for epidemiologic studies and surveillance of epilepsy. Epilepsia 52(Suppl. 7):2-26.
Tomson, T., T. Walczak, M. Sillanpää, and J. W. A. S. Sander. 2005. Sudden unexpected death in epilepsy: A review of incidence and risk factors. Epilepsia 46(Suppl. 11):54-61.
Tomson, T., L. Nashef, and P. Ryvlin. 2008. Sudden unexpected death in epilepsy: Current knowledge and future directions. Lancet Neurology 7(11):1021-1031.
U.S. Commission for the Control of Epilepsy and Its Consequences. 1978. Plan for nationwide action on epilepsy. Bethesda, MD: U.S. Department of Health, Education and Welfare.
WHO (World Health Organization). 2011. Global Campaign Against Epilepsy: Out of the shadows. http://www.who.int/mental_health/management/globalepilepsycampaign/en/index.html (accessed October 19, 2011).
Yoon, D., K. D. Frick, D. A. Carr, and J. K. Austin. 2009. Economic impact of epilepsy in the United States. Epilepsia 50(10):2186-2191.