Health is influenced by an array of factors, including social, genetic, environmental, and other factors that cut across a number of different sectors. Improving the health of populations therefore will require a collaborative, intersectoral effort that involves public and private organizations and individuals. At the same time, both health problems and community needs, resources, and circumstances vary among localities, so no single approach to combating health problems can be applied.
Primary care and public health are uniquely positioned to play critical roles in tackling the complex health problems that exist both nationally and locally. They share a similar goal of health improvement and can build on this shared platform to catalyze intersectoral partnerships designed to bring about sustained improvements in population health. In addition, they have strong ties at the community level and can leverage their positions to link community organizations and resources. Thus, the integration of primary care and public health holds great promise as a way to improve the health of society. The purpose of this report is to explore how this promise can be realized.
It is well documented that the nation’s health system is expensive and does not translate into excellent outcomes for all (AHRQ, 2011; United Health Foundation, 2011). The opportunity currently exists to shift the system in significant ways to improve on this situation. Investments in the current model of health care are not focused in the most effective way.
While these patterns of investment have produced what is arguably the best biomedical research and specialty care system in the world, the nation has failed to balance its investments in primary care, public health, prevention, and the broader determinants of health, a problem clearly demonstrated by its low rankings in overall health status. McGinnis and Foege (1993) estimated that nearly half of all U.S. deaths that occurred in 1990 were attributable to behavioral and environmental factors. It has repeatedly been shown that such factors have a substantial influence on health outcomes, yet the current health system devotes most of its resources to treating disease and much less to the underlying causes of illness (CDC, 1992; Miller et al., 2012). Financial incentives and a medical culture focused overly on acute care and heroic cures encourage giving most attention to individuals who are already sick rather than promoting an effective balance of treatment and personal and community-based prevention. As a result, the current health system is inadequately equipped to provide critical health promotion and preventive services.
A number of relatively new developments have converged to create opportunities for improving the nation’s health. First, there is growing recognition that the status quo is unacceptable. The unsustainable rise in health care costs has created an urgent need for innovative ways to deliver health care more efficiently. This imperative has been evident not only in the activities of government health organizations but also in the private sector. As purchasers of health care, many employers have been exploring ways to reduce the growth in these costs. A recent survey by Towers Watson and National Business Group on Health (2010) found that many employers are incentivizing a number of healthy lifestyle activities for their employees, including weight management, smoking cessation, and screenings. The concern about health care expenditures has opened the door for innovative approaches to improving health and health care.
Adding momentum to the recognition that the status quo is unacceptable, health research continues to clarify the importance of social and environmental determinants of health (Marmot and Wilkinson, 2006; McMichael, 1999) and the limitations of the acute care medical system in addressing prevention and care needs in chronic illness. At the same time, the science with respect to primary prevention has grown and developed (The New York Academy of Medicine, 2009). As a result of these factors, a shift in the way health is approached in the United States is taking place.
Another development is the increased availability of health-related data. Advances in data collection techniques and health informatics have presented an opportunity to facilitate the utilization and sharing of data among health professionals. Recent endeavors have begun to capitalize on these opportunities. For instance, the Health Information Technology for Economic and Clinical Health (HITECH) Act encourages the collection
and use of patient-level data through electronic health records.1 In addition to improvements in how data are collected and used, more data sets are becoming available for widespread use. And the Health Data Initiative, led by the Department of Health and Human Services (HHS), has made a wide array of health-related data available to the public (HHS, 2011b). These newly available data are providing communities, health care providers, and researchers with an unprecedented opportunity to access and analyze information that can aid in understanding and addressing community-level health concerns. The new opportunities presented by these data give primary care and public health a solid foundation upon which they can initiate integration.
Finally, and most important, the recent national focus on health care reform and the adoption of the Patient Protection and Affordable Care Act (ACA) present an overarching opportunity to change the way health care is organized and delivered. The ACA is discussed in more detail later in the report.
The convergence of these opportunities makes this a pivotal time to achieve sustainable improvements in population health. When discussing the term “population health,” the committee chose to adopt Kindig and Stoddart’s definition (2003, p. 381): “the health outcomes of a group of individuals, including the distribution of such outcomes within the group.” In this report, population health is viewed as an ultimate goal toward which the strategies and reforms discussed in subsequent chapters would move the health system.
THE PATH TO IMPROVING POPULATION HEALTH
Improving population health will require activities in three domains: (1) efforts to address social and environmental conditions that are the primary determinants of health, (2) health care services directed to individuals, and (3) public health activities operating at the population level to address health behaviors and exposures. There is abundant evidence for the benefit and value of activities in each of these domains for achieving the aim of better and more equitable population health (Andrulis, 1998; Commission on Social Determinants of Health, 2008; WHO, 2003).
A clear challenge for achieving improved population health is generating an appropriate balance in investment across and within these three domains, clarifying the appropriate roles and tasks for stakeholders in each domain, and improving the integration of activities at the interfaces among the domains. It is in this context that primary care and public health have
_________________
1American Recovery and Reinvestment Act of 2009 (ARRA), HR1, Section 13001, 111th Cong. (February 17, 2009).
critical roles. Their integration can not only improve the efficiency and effectiveness of each of their functions but also lead to collaboration with other entities that will assist in the improvement of population health. Integration of primary care and public health can serve as a catalyst for cooperation across the entire health system, connecting key stakeholders in communities nationwide.
To discuss the integration of primary care and public health, it is necessary to understand what these terms mean broadly and how they are used in this report.
Primary Care
In 1996, the IOM Committee on the Future of Primary Care defined primary care as “the provision of integrated, accessible health care services by clinicians who are accountable for addressing a large majority of personal health care needs, developing a sustained partnership with patients, and practicing in the context of family and community” (IOM, 1996, p. 1). The committee emphasized that “primary” means care that is first and fundamental, and declared that primary care is not a specialty or a discipline but an essential function in health care systems. The inclusion of the words “integrated,” “sustained partnership,” and “context of family and community” reflects a prominent population perspective, as well as a responsibility to connect with other actors in the health system.
Also embedded in the 1996 report is the inextricable link between mental health and primary care. A paper commissioned for that report, and included as an appendix, asserts that “a sensible vision of primary health care must have mental health care woven into its fabric” (IOM, 1996, p. 285). Primary care providers address a broad range of health issues to which mental health concerns are integral. Mental, behavioral, and physical health are so closely entwined that they must be considered in conjunction with one another. While the nature and role of primary care have been debated and studied at length, it is generally recognized that primary care has the four key features listed in Box 1-1.
The importance of primary care is well known and researched. In their review of the literature, Starfield and colleagues (2005) found that areas with the highest numbers of primary care providers have the best health outcomes; people who consistently receive care from a primary care provider have better health outcomes than those who do not; and the characteristics themselves of primary care are associated with good health. Additionally, primary care was found to be associated with a reduction of
BOX 1-1
Four Key Features of Primary Care
• It is person-rather than disease-focused. This focus entails sustained relationships between patients and providers in primary care practices over time, often referred to as continuity.
• It provides a point of first contact for whatever people might consider a health or health care problem. In properly organized health care systems, primary care ensures access to needed services.
• It is comprehensive. By definition, it can encompass any problem. Many problems in primary care are ambiguous and defy precise diagnosis. Nonetheless, primary care meets a large majority of patient needs without referral.
• It coordinates care. Primary care adopts mechanisms that facilitate the transfer of information about health needs and health care over time. Highly personalized solutions to patients’ problems can be implemented when sustained relationships permit deeper knowledge and understanding of individuals’ habits, preferences, and goals.
SOURCE: Starfield and Horder, 2007.
health disparities both in the United States and among international populations (Starfield et al., 2005).
Primary care is the foundation of the U.S. health system. In the United States, more individuals receive care in primary care settings than in any other setting of formal health care. On average, primary care settings see 11 percent of the entire population each month, compared with 1.3 percent for emergency departments and 0.07 percent for academic medical center hospitals (Green et al., 2001). Of interest, these proportions have not changed substantially since the 1950s and 1960s despite the stunning progress of medical knowledge, new technology, and expansion of health services (White et al., 1961).
The primary care system in the United States comprises both private providers and those supported by government agencies, such as the Veterans Health Administration and the Health Resources and Services Administration (HRSA). HRSA-supported health centers serve nearly 20 million patients a year (HRSA, 2011) and provide a safety net for society’s most vulnerable populations. Although most primary care is delivered through the private sector, both private and government-supported primary care share common features. For example, in its policy paper on primary care, the National Business Group on Health, which represents more than 300 large employers providing health care coverage for 55 million people, asserts that primary care should be the key to efficiency, effectiveness,
and quality improvement in the nation’s health system (National Business Group on Health, 2010). Both sectors also share the same challenges.
As a whole, primary care currently is facing a workforce shortage. The primary care workforce remains a relatively small proportion of the overall workforce compared with other health fields (Bodenheimer et al., 2009; Canadian Labour and Business Centre, 2003; European Observatory on Health Systems and Policies, 2006). During the last decade, the proportion of primary care providers fell from nearly a third to now less than a fourth of the output of the graduate medical education system (COGME, 2010; Phillips et al., 2011; Salsberg et al., 2008). This decline goes beyond physicians to include nurse practitioners and physician assistants as well (HRSA, 2010; Jones, 2007). Primary care also faces a chronic problem of relative shortage due to workforce maldistribution (Zhang et al., 2008). Regional shortages have seen little improvement despite federal and state loan repayment programs and the rapid growth of safety net clinics over the last decade (GAO, 2003).
In addition to workforce shortages, the increase in chronic diseases has posed challenges for primary care and served to motivate its transformation. Chronic diseases are linked to a number of unhealthy behaviors, such as lack of physical activity, poor nutrition, and tobacco use, but primary care often has struggled to address these behaviors adequately. In recognition of the difficulties associated with treating chronic diseases, the Chronic Care Model (Wagner et al., 2001) was implemented. This initiative emphasized a systematic and more efficient means of improving chronic care management for individual patients (Coleman et al., 2009). In its fullest expression, the Chronic Care Model contained six critical elements—community resources and policies, health care organization, self-management support, delivery system design, decision support, and clinical information systems—and effectively bridged patient care across the practice setting, the delivery system, and the broader community (Bodenheimer et al., 2002)
The success of the Chronic Care Model in revitalizing the management of patients with chronic conditions by relying on an interdisciplinary primary care team with aligned objectives and methodology generated interest in redesigning the entire practice of primary care. This interest in reinventing primary care led in turn to interest in the “medical home,” a model first proposed in the 1960s for providing care for children with special needs (Rosenthal, 2008). In the last few years, intensive activity has focused on implementing the “patient-centered medical home,” spurred by funding and research supported by the Centers for Medicare & Medicaid Services (CMS), the Commonwealth Fund, HRSA, and a number of other groups. These efforts are aimed at stimulating new models of care delivery, with primary care teams at the core of the delivery structure.
A fully realized patient-centered medical home encompasses the principle
that individual patients are members of a broader community, and that activity within the construct of individual clinical encounters includes links that can be leveraged to generate wellness and prevention beyond the individual patient. A systematic approach to population health, called community-oriented primary care (COPC), is employed in other health systems and has previously been studied by the Institute of Medicine (IOM, 1984). This approach to primary care helped launch the community health center movement in the United States and is still used in some communities. COPC, which is discussed in more detail later in the chapter, offers a model of primary care that more fully embraces public health. There is already some evidence that the foundational relationship between patient and primary care provider can generate dividends for the broader community. Several integrated service delivery networks, such as the Geisinger Health System, Group Health Cooperative of Puget Sound, and HealthPartners, are providing early evidence that accountable care for patient panels and populations can reduce mortality, costs, and unnecessary utilization, and in some cases can improve the fiscal health of hospitals as well (Flottemesch et al., 2011; Grumbach and Grundy, 2010; IOM, 2010).
Primary care is well positioned to work with public health on improving the health of local populations. The research networks of major primary care provider groups could assist in this effort. Some of primary care’s major concerns include factors that are not present in a clinical setting, such as circumstances at the onset of illness, predisposing factors that increase the risk of death and disease, and precipitating factors that lead people to seek care (White, 2000). One of its strengths is that primary care often holds a position of trust in communities and is able to leverage that position in addressing community concerns. This community relationship is exemplified by health centers and other primary care delivery systems, particularly those that use a community-oriented approach. Thus, primary care is working in areas that largely overlap with public health and is strategically placed at the interface of people in communities and the rest of the health care system.
Public Health
Public health is a dynamic field that continues to evolve to meet the needs of society. While the concept of modern public health emerged in response to the conditions that resulted from industrialization and the subsequent rise in infectious diseases (Rosen, 1993), the issues confronting public health look very different today. Although the primary focus of public health has shifted from infectious to chronic diseases, which are more prevalent in today’s society, its emphasis has remained on improving conditions where people spend their lives outside of health care settings.
While it is generally recognized that a critical component of public health is the services provided under the legal authority of government through health departments, articulating broadly what public health is and does is no easy task.
A number of key reports published over the last few decades have presented a vision for public health. The 1988 IOM report The Future of Public Health provides two critical definitions. The first is the mission of public health, defined as “fulfilling society’s interest in assuring conditions in which people can be healthy” (IOM, 1988, p. 140). The second is the substance of public health, defined as “organized community efforts aimed at the prevention of disease and promotion of health. It links many disciplines and rests upon the scientific core of epidemiology” (IOM, 1988, p. 41). Although the report emphasizes the importance of government health agencies and argues that strengthening the role of health departments would be crucial in moving public health forward in the future, its overall conception of public health is much broader, involving the private sector, community organizations, public–private partnerships, and others.
In 2002, the IOM released The Future of the Public’s Health in the 21st Century, which reinforces the idea that public health’s broad mission of ensuring healthy communities requires interactions among a number of health-influencing actors, such as communities, businesses, the media, governmental public health, and the health care delivery system (IOM, 2002). The report notes that health departments are not alone in carrying out the essential public health services listed in Box 1-2. Figure 1-1 depicts
BOX 1-2
Essential Public Health Services
• Monitor health status to identify community health problems.
• Diagnose and investigate health problems and health hazards in the community.
• Inform, educate, and empower people about health issues.
• Mobilize community partnerships to identify and solve health problems.
• Develop policies and plans that support individual and community health efforts.
• Enforce laws and regulations that protect health and ensure safety.
• Link people to needed personal health services, and assure the provision of health care when otherwise unavailable.
• Assure a competent public health and personal health care workforce.
• Evaluate effectiveness, accessibility, and quality of personal and populationbased health services.
• Research for new insights and innovative solutions to health problems.
SOURCE: Public Health Functions Steering Committee, 1994.
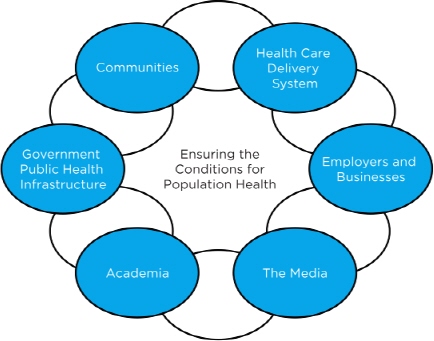
FIGURE 1-1 The intersectoral public health system.
SOURCE: IOM, 2002.
an interconnected system of sectors that influence a population’s health, with government public health being one of several actors (IOM, 2002).
More recently, the IOM published two in a series of reports called For the Public’s Health, looking at public health in the context of measurement and law (IOM, 2011a,b). A third report, on financing, was published in 2012 (IOM, 2012). These reports provide an opportunity to revisit public health in light of changes in health status in the United States since the IOM’s 1988 report was published. For example, obesity tripled among children and doubled among adults between 1980 and 2008 (CDC, 2011). Recognizing the complex nature of health challenges facing society today, the IOM committee responsible for the report on measurement noted that it is the “complex interactions of multiple sectors that contribute to the production and maintenance of the health of Americans” (IOM, 2011b, p. 21). The prevention of disease, which is a pillar of public health’s work, requires the engagement of all segments of a community. For instance, combating the rise in obesity requires encouraging individuals to improve their
diet and increase physical activity. These efforts require multiple partners, such as schools, employers, urban planners, and policy makers. These various stakeholders may provide one or more of the essential public health services. For example, a community-based organization may implement a health outreach campaign to educate people about health issues, or a public–private partnership may be engaged to mobilize the community to solve a particular health problem.
Traditionally, public health has worked with systems, policy, and the environment to reduce the burden of infectious disease. Improvements in sanitation, food preparation, and water treatment are successful examples of this work. To address more current concerns, public health has turned its attention to fighting chronic disease. Community-based interventions undertaken by public health for the prevention of chronic diseases have proven to be effective (The New York Academy of Medicine, 2009). In addition, some research suggests that making system, policy, and environmental changes may be effective; for example, French and colleagues (2004) found that an intervention aimed at the school environment resulted in students purchasing healthier foods. In general, the field would benefit from additional efforts to evaluate the effectiveness of these interventions in terms of implementation and outcomes.
Public health faces a number of challenges, including insufficient funding to fulfill its mission, a shrinking workforce, and inadequate investments in health information technology (HIT). In its report on public health funding, the Trust for America’s Health found that public health funding had been reduced at the federal, state, and local levels (ASTHO, 2011; NACCHO, 2011; Trust for America’s Health, 2011). Not surprisingly, a reduction in the public health workforce has also been documented (ASTHO, 2011; NACCHO, 2011; Trust for America’s Health, 2011). Another concern for public health is the lack of investment, relative to the health delivery system, in HIT. This disparity is exemplified by the distribution of HIT funding in the American Recovery and Reinvestment Act of 2009, which designated $17.2 billon of the total $19.2 billion appropriated for HIT for incentives to be paid to physicians and hospitals to promote the use of electronic health records (Steinbrook, 2009). This lack of investment could pose challenges for public health in managing population-level data.
Despite these challenges, public health today continues to meet the changing needs of communities. It encompasses a diverse group of public and private stakeholders (including the health care delivery system) working in a variety of ways to contribute to the health of society. Uniquely positioned among these stakeholders is governmental public health. Because health departments are legally tasked with providing the essential public health services, they are required to work with all sectors of the community.
This allows them to serve as a catalyst for engaging multiple stakeholders to confront community health problems. In addition, their assessment and assurance functions put them in close contact with the community and in touch with its health needs. Public health defined broadly is much more than governmental public health, yet health departments play a fundamental role in creating healthy communities.
Integration
Integration is an imprecise term that encompasses a wide variety of definitions. Accordingly, the committee decided it would be too limiting and not helpful to use a narrow definition. For this report, integration of primary care and public health is defined as the linkage of programs and activities to promote overall efficiency and effectiveness and achieve gains in population health. Because integration can take many forms, the committee chose to think conceptually about the variables that influence integration, which include the level at which it takes place, the partners involved, the actions entailed, and the degree to which integration occurs.
Levels
Integration can take place on many different levels. For this report, two major levels—the agency and local community levels—are addressed. The agency level refers to HRSA, the Centers for Disease Control and Prevention (CDC), and other federal agencies. Integration at this level involves largely joint efforts among the leadership of these agencies, as well as the appropriate programmatic staff working together.
At the local level, integration efforts are responsive to local health needs and relate to local resources and partners available and willing to work together. While innovative actions are being taken at the local level, many of which are improving the health of local populations, the committee attempted to distinguish clearly between which of these initiatives involve primary care–public health integration and which are innovative but do not necessarily involve integration. The other variables discussed below were used to make this distinction. It should also be noted that at one extreme, either primary care or public health can adopt approaches typical of the other, thereby integrating these functions within an organization. For example, some public health departments deliver primary care. This report, however, focuses on more formal integration efforts between local primary care and public health organizations.
Partners
At the agency level, most primary care–public health linkages in this report refer to HRSA and CDC working directly together, although there are some cases in which it would be beneficial for HRSA and CDC to work jointly with other federal agencies. In some cases, it would also make sense to partner with national provider and public health groups. Thus, the partners for the agency level are HRSA; CDC; and, as available and willing, other federal agencies and national groups.
Partners at the local level include a primary care entity (often as part of a larger organized delivery system), a public health entity, and the community. Often, other stakeholders are involved at the local level as well. For this report, the committee conceived of a primary care entity as any entity whose main purpose is the delivery of primary care, but the report also considers larger organized systems that contain entities with this purpose. These could include a solo practice, a group practice, primary care providers affiliated with a health care system, primary care providers affiliated with a university system, a HRSA-supported health center, or other community health centers. The committee was more selective in its choice of public health partners. While many entities provide public health services (including academic health centers and community-based organizations), health departments are legally responsible for provision of the essential public health services. Given that the committee’s statement of task explicitly mentions local health departments, the report emphasizes them over other entities in integration efforts. Finally, community participation, which could be facilitated through advisory boards, surveys, or community assessments undertaken by health departments, is critical to any integration efforts at the local level.
In addition to primary care and public health entities, other groups working at the community level are striving for population health improvements. These may include business groups, community-based organizations, public–private partnerships, academic health centers, faith-based groups, or other community-level entities. These groups can play many roles. For example, they may act as neutral conveners, able to link primary care and public health in a balanced way. They may also provide shared resources, such as community health workers, IT support staff, or case managers—resources that neither primary care nor public health may be able to support, but that could be beneficial in linking the two. Thus for the purposes of this report, linkages created at the community level must consist of a primary care partner, a public health partner (preferably a health department), and the community itself. However, other stakeholders working in the community may and often should be involved as well.
Actions
How the above partners integrate will differ depending on which partners are involved, the level at which the integration is occurring, and the local situation. At a minimum, each partner should be committed to a shared goal of improved population health and be willing and able to contribute to achieving that goal. The contribution may range from ideas and planning assistance, to financial or human resources, to goods or a physical space, but ideally will include a shared vision for an ongoing and sustainable relationship and a continual dialogue that goes beyond a single project. The contributions of each partner may not always be equal. And the action need not always be challenging; taking on easy tasks to start is as valid as tackling more complex problems. It is the shared recognition that success is not possible without each of the partners that is key.
Degree
As stated above, integration can have different meanings for different people. To some, it has a negative connotation, implying that one entity is subsumed by another, stronger entity. To others, integration has a positive connotation, suggesting a seamless flow between two entities. The committee recognized that integration occurs along a continuum (see Figure 1-2). At one end of this continuum is isolation, with primary care and public health entities working completely separately. At the other end is merger, with one combined entity replacing the formerly separate entities. By using the term “integration,” the committee is not advocating for a complete merger, nor does it see the benefit of isolation. Rather, the committee believes there are degrees of integration—ranging from mutual awareness, to cooperation, to collaboration, to partnership—that can be used to achieve better health. With mutual awareness, primary care and public health are informed about each other and each other’s activities. Cooperation denotes some sharing of resources, such as space, data, or personnel. Collaboration is more intense and involves joint planning and execution, with both entities
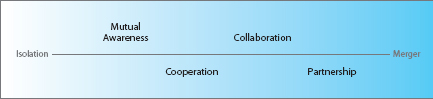
working together to coordinate at multiple points to carry out a combined effort. Partnership implies integration on a programmatic level, with two entities working so closely together that there is no separation from the end user’s perspective; there are, in fact, two parties, but their degree of integration is so great that the effect is nearly seamless. The discussion of integration in this report encompasses all of these degrees. Each community is different, and not all will be able to achieve true partnership. In some communities, achieving mutual awareness will be a significant step forward. However, it is useful to be aware of this continuum and strive for greater integration when possible.
BENEFITS AND CHALLENGES OF INTEGRATION
Primary care and public health have complementary functions and a common goal of ensuring a healthier population. However, they presently operate largely independently with distinct governance and funding streams, and each approaches this goal differently. Table 1-1, based on a table that highlights the differences between medicine and public health (Fineberg, 2011), provides an overview of these different perspectives.
While their perspectives and approaches may differ, in many ways primary care and public health align neatly. By working together, primary care and public health can each achieve their own goals and simultaneously have a greater impact on the health of populations than either of them would have working independently. For example, public health’s ties to community resources can provide support in areas of patient care that are typically difficult for primary care to handle on its own, such as prevention, health promotion, and the management of chronic disease. A primary care practitioner caring for significant numbers of people with asthma can work with local public health agencies to identify geographic areas in the community where poor housing stock or environmental risks can be addressed through combined action with other local stakeholders to remove or reduce asthma risks and ultimately decrease unnecessary use and expense in the health care system. And the incorporation of data from frontline health care providers into public health systems can enable more accurate and timely assessments of health issues, such as infectious disease outbreaks or diseases related to environmental exposures, as well as chronic disease trends in communities that might suggest areas for public health interventions.
These examples illustrate why primary care and public health should and how they could integrate. The evidence base supporting integration is not robust. Few studies have specifically examined integration and gauged its impact on health or process outcomes. In Chapter 2, some examples of integration taking place in local communities around the United States
TABLE 1-1 Perspectives of Medicine and Public Health
|
Medicine |
Public Health |
|
Primary focus on individual |
Primary focus on population |
|
Personal service ethic, conditioned by awareness of social responsibilities |
Public service ethic, tempered by concerns for the individual |
|
Emphasis on diagnosis and treatment, care for the whole patient |
Emphasis on prevention, health promotion for the whole community |
|
Medical paradigm places predominant emphasis on medical care |
Public health paradigm employs a spectrum of interventions aimed at the environment, human behavior and lifestyle, and medical care |
|
Well-established profession with sharp public image |
Multiple professional identities with diffuse public image |
|
Biologic sciences central, stimulated by needs of patients; move between laboratory and bedside |
Biologic sciences central, stimulated by major threats to health of populations; move between laboratory and field |
|
Clinical sciences an essential part of professional training |
Clinical sciences peripheral to professional training |
|
Rooted mainly in the private sector |
Rooted mainly in the public sector |
SOURCE: Based on Fineberg, 2011.
are presented; cases in which improved outcomes have been reported are highlighted.
It has long been asserted that public health and primary care should be viewed as “two interacting and mutually supportive components” of a health system designed to improve the health of populations (Welton et al., 1997, p. 262). There is vast potential for alignment between the two sectors. Each has knowledge, resources, and skills that can be used to assist the other in carrying out its roles. To quote the 1996 IOM report Primary Care: America’s Health in a New Era, “the population-based functions of public health and the primary care services delivered to individuals are complementary functions, and strengthening the relationship should be the focus of action in both arenas” (pp. 131-132).
Benefits of Integration
As mentioned above, there have been few formal analyses of the efficacy of primary care and public health integration. However, evidence indicates that some advantages can be realized through integration.
A recent literature review of primary care and public health collaborations conducted in Canada found that these efforts resulted in improved
health outcomes, improved workforce outcomes, and benefits at the patient and population levels (Martin-Misener et al., 2009), but that these examples are not widespread. Lasker and the Committee on Medicine and Public Health (1997) conducted a review of more than 400 instances of medicine and public health collaboration and noted a number of benefits that arose from such endeavors. Specifically, the authors found that collaboration benefited clinicians by providing population-based information relevant to their practices, enhancing their capacity to address behaviors and the underlying causes of illness, and generating better quality assurance standards and performance measures. Public health entities received support for their role in carrying out population-based strategies, including the collection of individual-level data for surveillance purposes, the dissemination of health education and key health promotion messages, and cooperation for the assurance of quality medical care for all members of a community.
Beyond the benefits to providers and public health entities, it stands to reason that society gains from integration as well. Integration can improve the efficiencies and harness the capabilities of primary care and public health and their respective workforces to focus on common problems. By joining forces, primary care and public health are better able to meet the nation’s goal of improved population health. Unfortunately, however, integration is no easy task.
Challenges of Integration
Aligning primary care and public health to work together and with other partners in pursuit of the shared goal of improved population health is challenging. A number of trends reinforce the fragmented nature of the current health system, including a history of segregation between primary care and public health, a lack of financial resources and incentives, and an inflexible regulatory system (Baker et al., 2005; IOM, 1988, 2002, 2003, 2011b).
In the early 20th century, despite years spent as related and overlapping areas (Brandt and Gardner, 2000; Duffy, 1979), public health began to establish itself as a profession independent of medicine. This fissure can be traced to a number of factors, most notably the decision to create public health schools separate from medical schools and the rise of the biomedical model.
In 1915, the Welch-Rose Report, authored by William Welch and Wycliffe Rose of the Johns Hopkins School of Medicine, described a research-focused approach to public health education. Based on this report, the Rockefeller Foundation, with which Welch was affiliated, began to focus its philanthropic efforts on public health, and in 1916, the Johns Hopkins School of Hygiene and Public Health was established with financial support
from the foundation. By 1947, 10 schools of public health had been established, separating public health education from the more narrowly focused and uniform medical curriculum. As public health professionals and educators argued for more independence from medicine in universities and government, public health became viewed by medical professionals as an economic competitor that was largely encroaching on matters believed to be best resolved through the care and treatment provided by medical professionals to individual patients (Brandt and Gardner, 2000).
In addition to this separation, the biomedical model of disease emerged from a greater understanding of germ theory and bacteriology. This model conceived of disease as something separate from any social causes. As the objective biomedical model gained prominence, a natural consequence was the uncoupling of medical care from public health, which was viewed as being marred by politics and social matters. This view led to a decline in spending on and attention to public health relative to medical care that persists today (Brandt and Gardner, 2000).
After decades of separation, both primary care and public health have hard-won identities, achievements, and cultures that they prize. Revising these identities and adapting to each other’s cultures in order to integrate their efforts can be experienced as a loss. Both sectors tend to view themselves as neglected and underappreciated. Both primary care and public health are fragmented within themselves, sometimes struggling to coordinate and align efforts internally, much less with each other. Both have dedicated advocacy groups that stake out territory and defend it against encroachment by alternative interests.
This historical divide is further cemented by a lack of financial investment in both primary care and public health. In this environment, the creation of financial incentives and supporting linkages between primary care and public health is not easy to accomplish or sustain. Payment structures within the delivery system reward disease treatment rather than prevention, pay for volume rather than value, and incentivize specialty care and procedural interventions over primary care. Moreover, primary care and public health both receive a relatively small proportion of the expenditures devoted to health in the United States (as discussed in more detail in Chapter 4). Frequently, they find themselves competing with each other for resources insufficient for either, much less both. Primary care and public health at their best result in nonevents, often at moments distant in time, for individuals and populations, making success somewhat invisible to others. This invisibility often hinders both sectors from attracting funders willing to invest in improvement efforts.
Furthermore, both primary care and public health operate under inflexible regulatory policies and funding restrictions that may preclude or hamper shared action. Neither is accountable to the other, and there is no
shared space where primary care and public health come together routinely and automatically to identify problems and opportunities, plan together, coordinate their work, and undertake joint efforts. In terms of informatics and data collection, primary care and public health often lack interoperable information systems both within the delivery system and between the delivery and public health systems. This internal fragmentation and external siloing often means that even when entities are willing to integrate, they lack the infrastructure to do so.
These challenges notwithstanding, the committee believes that the potential benefits of greater integration of primary care and public health are sufficiently promising to merit action now, taking these challenges into account. The call to better integrate primary care and public health is not new. The National Commission on Community Health Services, in a report known as “The Folsom Report” (1966), raised this issue half a century ago by calling for a more comprehensive model of health including both primary care and public health elements; Kerr White’s Healing the Schism revisited this idea in 1991 (White, 1991). While examples of long-term, successful models of integration are not abundant, there appears to be an interest in communities in bringing primary care and public health together to improve population health (see Box 1-3 and Chapter 2). However, the sustainability and scalability of models of integration have been lacking. The key task now is to focus on the challenge of sustainable implementation of community-based models of primary care and public health integration. Critical elements for this task are providing sustained resources and incentives for these models and supporting the infrastructure necessary to weave together the diverse stakeholders across multiple sectors that must participate in their implementation.
BOX 1-3
Interest in Collaboration
A willingness to collaborate is evident among diverse health disciplines. In 2011, the National Committee on Vital and Health Statistics focused on communities as learning health systems and explored a convenience sample of contemporary examples of local efforts in multiple states to use data to identify and monitor local health needs and problems. Many examples were readily identified and studied in sufficient detail to conclude that, even without formal programs and sufficient infrastructure, these efforts were successful and demonstrated widespread interest in collaboration among community leaders, clinicians, public health departments at various political levels, and academicians to identify local health and health care concerns and new, collaborative ways of responding to them (HHS, 2011a).
Previous examples of integration of primary care and public health can be found both in the United States and abroad.
Efforts in the United States
Some prior initiatives have focused on bridging the gap between primary care and public health and the community. For example, efforts have been made in some areas within the United States to adopt COPC models. COPC has been defined as a continual process by which primary health care teams provide care to a defined community on the basis of its assessed health needs through the integration in practice of primary care and public health (IOM, 1984). It is a dynamic, interdisciplinary model for planning, implementing, and evaluating primary care, health promotion, and disease prevention in the community that generally has appealed to practitioners working in underresourced areas with limited access to health care services. The application of COPC in the United States has not been widespread. A recent systematic review found that most articles about COPC did not adhere strictly to the model as originally described (Thomas, 2008). Even with modified models, however, a number of COPC initiatives have been found to generate notable improvements in the delivery of primary care (Merzel and D’Afflitti, 2003; Pickens et al., 2002). COPC models have been implemented internationally as well, with some success (Epstein et al., 2002; Iliffe and Lenihan, 2003).
In 1994 the American Medical Association and the American Public Health Association created the Medicine and Public Health Initiative. This effort began with a task force that met for 2 years and outlined shared agendas in several areas. The task force developed seven major recommendations for collaboration between primary care and public health: (1) engaging the community, (2) changing the education process, (3) creating joint research efforts, (4) devising a shared view of health and illness, (5) working together in health care provision, (6) jointly developing health care assessment measures, and (7) translating initiative ideas into action (Beitsch et al., 2005, p. 150). Other activities of note included a national congress in 1996, the development of a grant program funded by the Robert Wood Johnson Foundation (Cooperative Actions for Health Program, 2001), and a monograph of examples of collaboration (Lasker and the Committee on Medicine and Public Health, 1997).While the initiative was successful in promoting and showcasing efforts at the local level, commitment at the state and national levels ultimately faltered (Beitsch et al., 2005).
Since the Medicine and Public Health Initiative, other, more limited efforts to catalogue and analyze integration initiatives on the ground have
been undertaken in the United States. These include a review of public–private partnerships that brought together service delivery networks and coalitions of stakeholders focused on public health and community planning (Bazzoli, 1997), an examination of how organizational characteristics and market conditions contribute to collaborations between either community hospitals or community health centers and public health agencies (Halverson et al., 2000), and the American Medical Association’s analysis of effective clinical partnerships between primary care practices and public health agencies (Sloane et al., 2009). While these initiatives point to an enduring interest in integration, they were not part of a sustained effort to promote integration, and none alleviated a steady and persistent relative neglect of both primary care and public health.
International Efforts
There has been some international recognition of the need to coordinate primary care and public health efforts. In 2003, at a primary care strategic planning meeting held to assess the status of health improvement since the Declaration of Alma Ata (WHO, 1978), the World Health Organization noted that “the emphasis placed on community participation and intersectoral collaboration is especially appropriate now, when so many health issues … cannot be effectively addressed by health systems working in isolation” (WHO, 2003, p. 16). The ensuing report on that meeting recommended the strengthening of public health functions in primary health care settings. Likewise, a number of countries have made efforts to implement the integration of primary care and public health. A restructuring of the National Health Service in England placed public health professionals in Primary Care Trusts in an attempt to change the way primary care operates (The NHS Confederation, 2004). In 2000, New Zealand announced changes to its health care system that established District Health Boards with responsibility for both primary care and public health (New Zealand Ministry of Health, 2000). Attempts to reform public health currently are under way in Canada, where a 2005 workshop called for the Public Health Agency of Canada to develop stronger collaboration between primary care and public health (Rachlis, 2009). In addition, McMaster University in Ontario initiated a research program to explore the potential for collaboration between primary care and public health and the extent to which such collaborative partnerships currently exist (StrengthenPHC, 2011).
This study originated in a joint request from HRSA and CDC. With the passage of the ACA, these two agencies, further described in Appendix A,
have a unique opportunity to ensure that the provisions they are charged with implementing line up in a way that promotes population health and contributes to an enhanced health system with increased access, improved quality, and reduced costs. These agencies asked the IOM to convene the Committee on Integrating Primary Care and Public Health, whose 17 members include experts in primary health care, state and local public health, service integration, health disparities, HIT, health care finance, health care policy, public health law, workforce education and training, organization management, and child health. Biographical sketches of the committee members are presented in Appendix D.
In clarifying the committee’s charge at its first meeting, the sponsors reiterated their interest in receiving practical, actionable recommendations that could assist both agencies in establishing linkages with each other and with other relevant agencies. Box 1-4 presents the committee’s statement of task. Funding for the study was provided by HRSA, CDC, and the United Health Foundation.
In conducting the study, the committee held six open and two closed meetings. The open meetings were held in Washington, DC, and Irvine, California, and included 34 presentations. Four of the open meetings were focused on HRSA and CDC and their work in the areas of maternal and child health, cardiovascular disease prevention, and colorectal cancer screening. The agendas for the open meetings can be found in Appendix C. Members of the general public made comments at the open meetings and submitted documents to the committee. The committee also reviewed the published literature, held discussions with HRSA and CDC, and commissioned papers on relevant topics. Finally, a number of consultants assisted the committee; they are listed at the front of the report.
While cardiovascular disease prevention was identified as a required area for the study, the committee’s statement of task (Box 1-4) included selecting one or two additional areas. The committee selected maternal and child health (further refined to focus on maternal, infant, and early childhood home visiting) and colorectal cancer screening to complement cardiovascular disease prevention. These three areas flow across the life course and include elements of mental and behavioral health, while also reflecting many of the issues related to health disparities.
This report is organized into five chapters. Chapter 2 summarizes the committee’s literature review, presents a set of principles identified by the committee as necessary for the integration of primary care and public health, and highlights examples from around the country of innovative integration programs. Chapter 3 focuses on the Maternal, Infant, and
The Health Resources and Services Administration (HRSA) and the Centers for Disease Control and Prevention (CDC) have requested that the Institute of Medicine convene a committee of experts to examine ways to better integrate public health and primary care to assure healthy communities. The committee’s work would ultimately result in an evidence-based, integrated model and other recommendations that would help achieve successful linkages between public health and primary care. As part of its work, the committee will address the following questions:
1. What does the evidence report as the best methods to improve population health and/or reduce health disparities through integrating or connecting public health and primary care?
A. What are the models and factors that promote and sustain effective integration and connection between public health and primary care?
B. What are the gaps in evidence?
2. What are the best examples of effective public health and primary care integration and connection that address:
A. Demonstrated, shared accountability for population health improvement
B. Optimizing the integration of the public health and primary care workforce
C. Collaborative governance, financing, and care coordination models including optimizing reimbursement to health departments for clinical and case management (particularly STDs and TB models)
D. Effective use of health information technology (explore the possible role of health departments as data hubs)
a. This should include non-patient specific reporting of notifiable conditions and health department notification of primary care providers regarding key community health challenges
b. This should include patient specific information on
i. TB, HIV, HBV perinatal immunization—coordination of care and follow-up to improve outcomes
ii. Primary care systems and public health departments as potential hubs (neutral brokers for the community)
iii. Sentinel surveillance systems (e.g., autism, birth defects)
Early Childhood Home Visiting Program, the Million Hearts initiative, and colorectal cancer screening as examples of how HRSA and CDC can foster and support integration. Chapter 4 describes the policy and funding levers that can promote integration. Finally, Chapter 5 offers conclusions and recommendations. In addition, the report contains four appendixes.
c. This should include recommendations on the barriers and steps to make significant progress on exchanging electronic health record generated information
E. Promotion of integration for the goal of achieving high quality primary care and public health
3. How can HRSA and CDC use Affordable Care Act provisions (e.g., community transformation grants, prevention strategy, quality strategy, community health center expansion, National Health Services Corps, and other workforce programs) to promote integration of public health and primary care?
4. How can HRSA-supported primary care systems (e.g., Federally Qualified Health Centers, Rural Health Clinics, Ryan White Clinics) and state and local public health departments effectively integrate and coordinate to improve cardiovascular disease prevention (which would include obesity, tobacco use, aspirin use, blood pressure and cholesterol management)
A. One to two additional topics based on Committee input that address issues relevant to health disparities or specific populations
a. These should be chosen from among immunization, TB control, STD control, asthma management, falls prevention, behavioral health, SBIRT (screening, brief intervention, and referral to treatment), cancer screening, diabetes mellitus prevention and care, and family planning
5. Within each care area, the committee should address potential actions, needs, or barriers regarding:
A. Science
B. Finance
C. Governance
D. Health information technology
E. Delivery system and practice
F. Policy
G. Workforce education and training
6. What actions should CDC and HRSA take to promote these changes?
The committee should engage relevant stakeholders and perform a comprehensive literature review that includes international experiences, to identify promising practices and gaps in integrating public health and primary care.
Appendix A provides a broad description of HRSA and CDC. Appendix B offers an overview of HRSA-supported primary care systems and health departments. Appendix C contains the committee meeting agendas. Finally, Appendix D contains the committee biosketches.
AHRQ (Agency for Healthcare Research and Quality). 2011. 2010 national healthcare quality report. Rockville, MD: AHRQ.
Andrulis, D. P. 1998. Access to care is the centerpiece in the elimination of socioeconomic disparities in health. Annals of Internal Medicine 129(5):412-416.
ASTHO (Association of State and Territorial Health Officials). 2011. Budget cuts continue to affect the health of Americans: Update May 2011. Arlington, VA: ASTHO.
Baker, E. L., M. A. Potter, D. L. Jones, S. L. Mercer, J. P. Cioffi, L. W. Green, P. K. Halverson, M. Y. Lichtveld, and D. W. Fleming. 2005. The public health infrastructure and our nation’s health. Annual Review of Public Health 26(1):303-318.
Bazzoli, G. J. 1997. Public-private collaboration in health and human service delivery: Evidence from community partnerships. Milbank Quarterly 75(4):533-561.
Beitsch, L. M., R. G. Brooks, J. H. Glasser, and Y. D. Coble. 2005. The medicine and public health initiative: Ten years later. American Journal of Preventive Medicine 29(2):149-153.
Bodenheimer, T., E. H. Wagner, and K. Grumbach. 2002. Improving primary care for patients with chronic illness. Journal of the American Medical Association 288(14):1775-1779.
Bodenheimer, T., K. Grumbach, and R. Berenson. 2009. Health care 2009: A lifeline for primary care. The New England Journal of Medicine 36(26):2693-2696.
Brandt, A. M., and M. Gardner. 2000. Antagonism and accommodation: Interpreting the relationship between public health and medicine in the United States during the 20th century. American Journal of Public Health 90(5):707-715.
Canadian Labour and Business Centre. 2003. Physician workforce in Canada: Literature review and gap analysis. Ottawa, ON: A Physician Human Resource Strategy for Canada: Task Force Two.
CDC (Centers for Disease Control and Prevention). 1992. Effectiveness in disease and injury prevention estimated national spending on prevention—United States, 1988. Morbidity and Mortality Weekly Reports 41(29):529-531.
CDC. 2011. Obesity: Halting the epidemic by making health easier. Atlanta, GA: CDC.
COGME (Council on Graduate Medical Education). 2010. Council on Graduate Medical Education 20th report: Advancing primary care. Hyattsville, MD: COGME.
Coleman, K., B. T. Austin, C. Brach, and E. H. Wagner. 2009. Evidence on the chronic care model in the new millennium. Health Affairs 28(1):75-85.
Commission on Social Determinants of Health. 2008. Closing the gap in a generation: Health equity through action on the social determinants of health. Geneva, Switzerland: WHO.
Cooperative Actions for Health Program. 2001. Lessons learned in medicine and public health collaboration. Chicago, IL: American Medical Association and Washington, DC: American Public Health Association.
Duffy, J. 1979. The American medical profession and public health: From support to ambivalence. Bulletin of the History of Medicine 53(Spring):1-22.
Epstein, L., J. Gofin, R. Gofin, and Y. Neumark. 2002. The Jerusalem experience: Three decades of service, research, and training in community-oriented primary care. American Journal of Public Health 92(11):1717-1721.
European Observatory on Health Systems and Policies. 2006. The health care workforce in Europe learning from experience. Trowbridge, Wilts: European Observatory on Health Systems and Policies.
Fineberg, H. V. 2011. Public health and medicine. American Journal of Preventive Medicine 41(4):S149-S151.
Flottemesch, T. J., P. Fontaine, S. E. Asche, and L. I. Solberg. 2011. Relationship of clinic medical home scores to health care costs. The Journal of Ambulatory Care Management 34(1):78-89.
French, S. A., M. Sory, J. A. Fulkerson, and P. Hannan. 2004. An environmental intervention to promote lower-fat food choices in secondary schools: Outcomes of the tacos study. American Journal of Public Health 94(9):1507-1512.
GAO (General Accounting Office). 2003. Physician workforce: Physician supply increased in metropolitan and nonmetropolitan areas but geographic disparities persisted. Washington, DC: GAO.
Gostin, L. O., P. D. Jacobson, K. L. Record, and L. E. Hardcastle. 2011. Restoring health to public reform: Integrating medicine and public health to advance the population’s wellbeing. Pennsylvania Law Review 159:1777-1823.
Green, L. A., G. E. Fryer, B. P. Yawn, D. Lanier, and S. M. Dovey. 2001. The ecology of medical care revisited. New England Journal of Medicine 344(26):2021-2025.
Grumbach, K., and P. Grundy. 2010. Outcomes of implementing patient centered medical home interventions: A review of the evidence from prospective evaluation studies in the United States. Washington, DC: Patient Centered Primary Care Collaborative.
Halverson, P. K., G. P. Mays, and A. D. Kaluzny. 2000. Working together? Organizational and market determinants of collaboration between public health and medical care providers. American Journal of Public Health 90(12):1913-1916.
HHS (Department of Health and Human Services). 2011a. The community as a learning system for health: Using local data to improve local health. Hyattsville, MD: HHS.
HHS. 2011b. Health data initiative. http://www.hhs.gov/open/initiatives/hdi/index.html (accessed September 22, 2011).
HRSA (Health Resources and Services Administration). 2010. The registered nurse population: Findings from the 2008 national sample survey of registered nurses. Hyattsville, MD: HHS.
HRSA. 2011. Uniform Data System 2010 National Data. Hyattsville, MD: HHS.
Iliffe, S., and P. Lenihan. 2003. Integrating primary care and public health: Learning from the community oriented primary care model. International Journal of Health Services 33(1):85-98.
IOM (Institute of Medicine). 1984. Community oriented primary care: A practical assessment. Vol. 1. Washington, DC: National Academy Press.
IOM. 1988. The future of public health. Washington, DC: National Academy Press.
IOM. 1996. Primary care: America’s health in a new era. Washington, DC: National Academy Press.
IOM. 2002. The future of the public’s health in the 21st century. Washington, DC: The National Academies Press.
IOM. 2003. Who will keep the public healthy? Educating public health professionals for the 21st century. Washington, DC: The National Academies Press.
IOM. 2010. The healthcare imperative: Lowering costs and improving outcomes: Workshop series summary. Washington, DC: The National Academies Press.
IOM. 2011a. For the public’s health: Revitalizing law and policy to meet new challenges. Washington, DC: The National Academies Press.
IOM. 2011b. For the public’s health: The role of measurement in action and accountability. Washington, DC: The National Academies Press.
IOM. 2012. For the public’s health: Investing in a healthier future. Washington, DC: The National Academies Press.
Jones, P. E. 2007. Physician assistant education in the United States. Academic Medicine 82(9):882-887.
Kindig, D., and G. Stoddart. 2003. What is population health? American Journal of Public Health 93(3):380-383.
Lasker, R. D., and the Committee on Medicine and Public Health. 1997. Medicine and public health: The power of collaboration. New York: The New York Academy of Medicine.
Marmot, M. G., and R. G. Wilkinson. 2006. Social determinants of health. New York: Oxford University Press.
Martin-Misener, R., R. Valaitis, and The Strengthening Public Health Care Through Primary Care and Public Health Collaboration Research Team. 2009. A scoping literature review of collaboration between primary care and public health: A report to the Canadian Health Services Research Foundation. Hamilton, ON: StrengthenPHC.
McGinnis, J. M., and W. H. Foege. 1993. Actual causes of death in the United States. Journal of the American Medical Association 270(18):2207-2212.
McMichael, A. J. 1999. Prisoners of the proximate: Loosening the constraints on epidemiology in an age of change. American Journal of Epidemiology 149(10):887-897.
Merzel, C., and J. D’Afflitti. 2003. Reconsidering community-based health promotion: Promise, performance, and potential. American Journal of Public Health 93(4):557-574.
Miller, G., C. Roehrig, P. Hughes-Cromwick, and A. Turner. 2012. What is currently spent on prevention as compared to treatment? In Prevention vs. Treatment: What’s the right balance?, edited by H. S. Faust, and P. T. Menzel. New York: Oxford University Press. Pp. 37-55.
NACCHO (National Association of County and City Health Officials). 2011. Local health department job losses and program cuts: Findings from the July 2011 survey. Washington, DC: NACHHO.
National Association of Community Health Centers. 2009. Primary care access: An essential building block of health reform. Bethesda, MD: National Association of Community Health Centers.
National Business Group on Health. 2010. The health care delivery system should focus on primary care. Washington, DC: National Business Group on Health.
National Commission on Community Health Services. 1966. Health is a community affair: Report. Cambridge, MA: Harvard University Press.
The New York Academy of Medicine. 2009. A compendium of proven community-based prevention programs. New York: The New York Academy of Medicine.
New Zealand Ministry of Health. 2000. The New Zealand health strategy. Wellington, New Zealand: Ministry of Health.
The NHS Confederation. 2004. Making a difference: How primary care trusts are transforming the NHS. London: NHS Confederation.
Noncommunicable Diseases and Mental Health Evidence and Information for Policy World Health Organization. 2003. Primary health care: A framework for future strategic directions. Geneva, Switzerland: WHO.
Phillips, R. L., S. C. Petterson, and A. W. Bazemore. 2011. Primary care physician workforce and outcomes. Journal of the American Medical Association 306(11):1201-1202.
Pickens, S., P. Boumbulian, R. J. Anderson, S. Ross, and S. Phillips. 2002. Community-oriented primary care in action: A Dallas story. American Journal of Public Health 92(11): 1728-1732.
Public Health Functions Steering Committee. 1994. Public health in America: Vision, mission, and essential services. Washington, DC: Office of Disease Prevention and Health Promotion.
Rachlis, M. 2009. Public health and primary health care collaboration: A paper prepared for the public health agency of Canada. http://www.michaelrachlis.com/publications.php.
Rosen, G. 1993. A history of public health: Expanded edition. Baltimore, MD: The Johns Hopkins University Press.
Rosenthal, T. C. 2008. The medical home: Growing evidence to support a new approach to primary care. The Journal of the American Board of Family Medicine 21(5):427-440.
Salsberg, E., P. H. Rockey, K. L. Rivers, S. E. Brotherton, and G. R. Jackson. 2008. US residency training before and after the 1997 balanced budget act. Journal of the American Medical Association 300(10):1174-1180.
Sloane, P. D., J. Bates, M. Gadon, C. Irmiter, and K. Donahue. 2009. Effective clinical partnerships between primary care medical practices and public health agencies. Chicago, IL: American Medical Association.
Starfield, B., and J. Horder. 2007. Interpersonal continuity: Old and new perspectives. British Journal of General Practice 57(540):527-529.
Starfield, B., L. Shi, and J. Macinko. 2005. Contribution of primary care to health systems and health. Milbank Quarterly 83(3):457-502.
Steinbrook, R. 2009. Health care and the American Recovery and Reinvestment Act. New England Journal of Medicine 360(11):1057-1060.
StrengthenPHC. 2011. Strengthening primary health care through primary care and public health collaboration: About the project. http://strengthenphc.mcmaster.ca/ (accessed January 4, 2012).
Thomas, G. 2008. A systematic review of COPC: Evidence for effectiveness. Journal of Health Care for the Poor and Underserved 19(3):963-980.
Towers Watson and National Business Group on Health. 2010. Raising the Bar on Health Care: Moving Beyond Incremental Change. New York: Towers Watson.
Trust for America’s Health. 2011. Investing in America’s health: A state-by-state look at public health funding and key health facts. Washington, DC: Trust for America’s Health.
United Health Foundation. 2011. America’s health rankings: A call to action for individuals and their communities. St. Paul, MN: United Health Foundation.
Wagner, E., B. Austin, C. Davis, M. Hindmarsh, J. Schaefer, and A. Bonomi. 2001. Improving chronic illness care: Translating evidence into action. Health Affairs 20(6):64-78.
Welton, W. E., T. A. Kantner, and S. M. Katz. 1997. Developing tomorrow’s integrated community health systems: A leadership challenge for public health and primary care. Milbank Quarterly 75(9184684):261-288.
White, K. L. 1991. Healing the schism: Epidemiology, medicine, and the public’s health; with foreword by Halfdan Mahler, Frontiers of primary care. New York: Spinger-Verlag.
White, K. L. 2000. Fundamental research at primary care level. The Lancet 355(9218): 1904-1906.
White, K. L., T. F. Williams, and B. G. Greenberg. 1961. Ecology of medical care. New England Journal of Medicine 265(18):885-892.
WHO (World Health Organization). 1978. Declaration of Alma-Ata: International conference on primary health care, Alma-Ata, USSR, 6-12 September 1978. Paper presented at the International Conference on Primary Health Care.
WHO. 2003. Social determinants of health: The solid facts. Copenhagen, Denmark: WHO.
Zhang, X., R. L. Phillips Jr, A. W. Bazemore, M. S. Dodoo, S. M. Petterson, I. Xierali, and L. A. Green. 2008. Physician distribution and access: Workforce priorities. American Family Physician 15(77):1378.




























