6
What Do We Still Need to Learn
About Reducing Health Disparities?
The following panel addressed social determinants of health disparities and ways to reduce health disparities, promote health equity, and move successful models to a larger scale. Each speaker was asked the question, “What do we still need to learn about reducing health disparities?”
Paula Braveman is a professor of family and community medicine and has published extensively on disparities in health and health care. She explained that her presentation had three main points, which are outlined in Box 6-1.
Research on Social Determinants of Health Disparities
First, not only is more research clearly needed, but also research that better conceptualizes the social determinants of health. Braveman offered some examples from the research effort behind the Robert Wood Johnson Foundation’s Commission to Build a Healthier America (http://www.commissiononhealth.org). Figure 6-1 shows national data on health strati-fied by the three largest racial and ethnic groups in the United States. Within each of these groups, the prevalence of self-reported poor or fair health is shown by family income level. These data show that as income goes up, self-reported health improves. This is true within each of the three racial/ ethnic groups.
BOX 6-1
Priorities for Health Disparities Research
• More—and better—research on the social determinants of health disparities
• More intervention research (based on promising hypotheses)—understanding pathways is not sufficient
• Multilevel, critical mass, studied longitudinally
• More translational research
• How to inform the public about health disparities
• How to get them to care
• How to create political will
SOURCE: Braveman (2010).
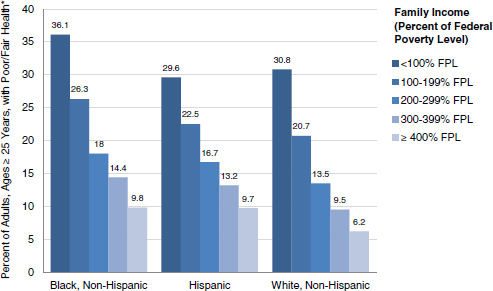
FIGURE 6-1 Income is linked with health regardless of racial or ethnic group. Differences in health status by income do not simply reflect differences by race or ethnicity; differences in health can be seen within each racial or ethnic group. Both income and racial or ethnic group matter.
*Age-adjusted.
SOURCE: RWJF (2009). Prepared for the Robert Wood Johnson Foundation by the Center on Social Disparities in Health at the University of California, San Francisco. © 2008 Robert Wood Johnson Foundation. www.commissiononhealth.org.
However, when the poorest group is compared with all other groups, it is clear that the size of the racial/ethnic disparities is much smaller than the size of the income disparities. It is not enough, then, to look at racial and ethnic differences; socioeconomic differences should also be considered. Braveman explained that without considering both, the long-term effects of the experience of racism are not captured.
Braveman noted that institutionalized racism, independent of socio-economic differences, also affects health. The effects of institutionalized racism may mean that a child born to an African American family is far more likely to grow up in a neighborhood with fewer opportunities and more adverse effects on health. Residential segregation systematically tracks certain racial and ethnic groups into worse living and working conditions. The effects of crime, toxic hazards, a lack of safe areas to play or exercise, a lack of access to healthy foods, and an environment filled with despair are all a part of an important potential pathway through which disparities are played out, Braveman said.
From a historical perspective, the focus on disparities in health care at the beginning of the disparities movement, Braveman explained, has had both positive and negative effects. One unfortunate outcome of this focus is that it has fed into racial and ethnic stereotypes and led to unfounded assumptions about the basis of racial and ethnic health disparities. For example, a common assumption is that disparities are based on the construct of “culture.” The problem with this construct is that it implies that culture is something that people freely choose.
More measurement work is needed, said Braveman, to enable the field to do a better job of tracing the pathways by which different social factors contribute to the creation of health disparities. A better understanding of those factors, how they operate, and how they perpetuate and exacerbate health disparities is needed.
Figure 6-2 from the Karolinska Institute in Sweden (Burstrom et al., 2010) outlines a simple way to demonstrate how health inequities are created. Differential exposure is related to social position, and social position is reflected by racial/ethnic group. (Social position can also be reflected by sexual orientation, disability status, or any number of other characteristics that define the likelihood that an individual will experience discrimination on the basis of that social position.) Furthermore, social position determines the extent to which a person is exposed to either factors that promote health or factors that have adverse effects on health.
Differential vulnerability should also be considered; that is, social position also affects the extent to which a given level of exposure is likely to result in a given level of damage to health outcomes. For example, increasing knowledge about the physiology of stress—and, particularly, of chronic stress—demonstrates how experiences associated with a lower social position
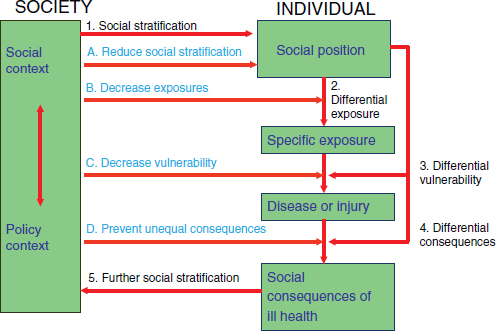
FIGURE 6-2 A way to demonstrate how health inequities are created.
SOURCE: Burstrom et al. (2010).
can result in physiological outcomes that create a greater vulnerability to negative health outcomes.
Disease, injury, and the differential consequences of being ill or physically disabled also affect social position and lead to further social stratification. Social stratification—that is, how people sort themselves into hierarchical groups according to characteristics like race or income—in turn affects access to more resources or more opportunities.
Figure 6-2 is also useful in that it indicates the potential points of intervention and puts social stratification, which most researchers do not include in their models, on the table, Braveman said. Most researchers, in fact, do not consider the ways in which the underlying differences in opportunities and resources can result in worse health outcomes.
Braveman noted that another feature of the model in Figure 6-2 is that it shows how disadvantages accumulate across a person’s life span and how they can accumulate across generations as well. The consequences of social stratification for the parents can determine the kind of neighborhood in which a child grows up, the influences to which that child is exposed, and even the quality of the schools in that neighborhood.
Poor school quality is one of the most important ways in which place
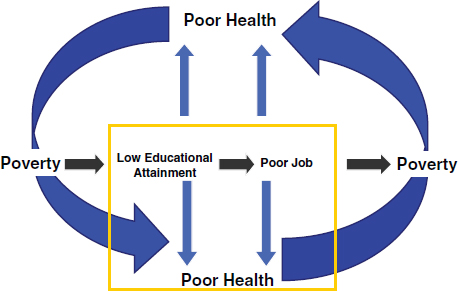
FIGURE 6-3 Vicious cycle of poverty and poor health.
SOURCE: Braveman (2010).
influences health. Figure 6-3 highlights the role of low educational attainment as a critical pathway to poor health. The role of racial segregation, for example, is one of the ways that people are systematically tracked into schools with lower levels of educational attainment. Lower levels of educational attainment, in turn, lead to lower wage earnings, poverty, and poor health outcomes. Although educational attainment influences health by several potential pathways, Figure 6-4 shows the pathway for which the knowledge base is the most limited (inside box).
In short, said Braveman, although more research is needed to better understand how social factors influence health disparities, more research on how to interrupt the pathways is needed. Furthermore, more research is needed to discern how these pathways play out with different populations and in different settings.
Research on Promising Interventions
Second, a massive expansion in intervention research is needed. Braveman noted that a number of promising hypotheses are ready to be tested in the field. Additionally, she said that “going to scale” is the next step because research has already demonstrated success on a small scale. A large body of research, in fact, demonstrates success at a small scale.
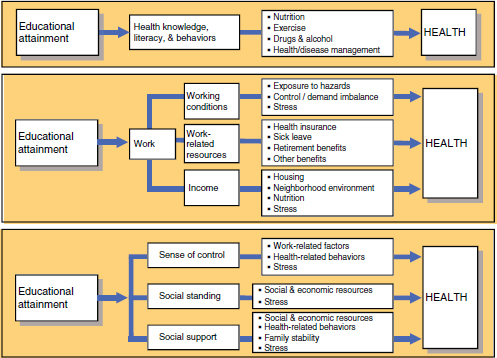
FIGURE 6-4 How could education affect health?
SOURCE: Braveman (2010).
Braveman also cautioned against the “silver bullet trap.” This is the expectation that a single intervention is enough. For example, knowledge about what really works to make schools better is one of the least developed areas. No single program will make a school better; what is needed is a multifaceted approach.
One challenge to conducting research on multifaceted interventions is to convince funding institutions and policy makers to take chances on this research, Braveman said. Because this research involves going at a problem from multiple directions and on multiple levels, it is necessarily messy and complex.
Translational Research
Finally, Braveman stated that more translational research that will translate the existing knowledge base into action is strongly needed. She said that the biggest barrier to reducing health disparities is not a lack of knowledge; rather, it is a lack of political will. Attention should be paid to translational research if reductions in health disparities are to be seen.
Ideas that seem radical in the United States are considered mainstream public health interventions by Europeans, she said; the basic level of social solidarity that exists in Europe is not present here. So how, then, can a greater level of social consensus be created in the United States? This lack of political will, Braveman concluded—not a lack of knowledge—is the biggest obstacle to ending health disparities.
Anne Beal is president of the Aetna Foundation, the independent and charitable arm of the Aetna Insurance Company. She is a physician who specializes in pediatrics and public health.
History of the Disparities Agenda
Beal began her comments by outlining the evolution of research on health disparities in the United States. Initially, the focus was on minority health, that is, the health of “those other people,” she said. The focus then shifted to acknowledgment of a gap between whites and people of color and finally to an interest in closing that gap. It is here that the language of health disparities was first used. The initial research on health disparities was descriptive in nature. It then became clear that disparities could be seen everywhere: in Medicare, Medicaid, health care access, and health care outcomes.
The next step was to look at questions of whether the data were adequate and whether the data were appropriate to capture the extent of disparities. This work was critically important, Beal said, and is reflected in federal legislation such as the Patient Protection and Affordable Care Act (ACA) of 2010. The law includes language around the need for high-quality data on race and ethnicity.
Once the data became available, the next step was to begin to look at the root causes of health disparities. One of the first findings to emerge, said Beal, was that where one lives and where one goes to receive health care are major drivers of health disparities. In other words, Beal said, “where you live makes a difference.” Just as the saying states that “all politics is local,” Beal said that “all disparities are local” as well. Although national data are useful for moving to an evidence-based action plan, what is needed are more localized and focused action plans.
The data on health care quality make it clear that providers who care for more racial/ethnic minority patients have more challenges with delivering high-quality care to those patients. This occurs in nursing homes, hospitals, and health plans. Obviously, challenges related to quality do not exist because a provider who has a large number of minority patients is a
bad provider; rather, something about the milieu in which those providers practice leads to challenges to delivering high-quality health care. Health disparities are thus actually an issue of health care quality; when measures of disparities are considered, those measures are, in fact, showing differences in the quality of care received. Beal said that it is impossible to “talk about quality without talking about quality for everyone.”
It is not a good use of our time and effort, Beal said, to focus on a particular factor such as health literacy, access to health care, or the patient-centered medical home. When health and wellness for people of color are considered, researchers need to look at all of those indicators; this type of research is complicated. This runs counter to the traditional bench research approach in which, ideally, one variable is changed and all other variables are controlled for.
Need for an Evidence-Based Action Plan
What is needed, said Beal, is what Paula Braveman called “intervention research,” that is, research that “tells us where to go in terms of next steps.” This is what Beal called an “evidence-based action plan.” Beal reiterated Braveman’s statement that research to describe disparities is not needed. What is needed is an evidence-based action plan for improving health care quality.
One example that has seen real success in improving health care quality is in the checklist used in intensive care units. Use of a basic checklist to ensure that certain things are done and that patients are appropriately cared for led to significant reductions in the incidence of infections and pneumonia in patients (e.g., Berenholtz et al., 2004).
Unfortunately, Beal pointed out, it is not always easy to get quality-improvement research published. Quality-improvement research does not fit into the randomized controlled trial model. A new paradigm for assessing quality-improvement research is needed, as it does not have the same methodological rigor as bench research that uses the randomized controlled trial model.
For example, when children of color are admitted to the hospital with asthma, they are less likely than white children to be sent home with medications that control asthma. A number of strategies could be taken to address this issue: creation of guidelines to distribute to all staff, patient education, collaboration with pharmacies to ensure that each child is sent home with medications, and working with primary care providers to ensure that appropriate follow-up occurs. As a pediatrician, Beal said that she would keep doing all of these things until 100 percent of her patients were sent home with asthma-controlling medication. By consideration of the data for each of these steps, improvement can take place.
The research that is needed should be linked with a concerted communication plan to share the information from that research with those people who do not know that health disparities are a problem in this country. Health disparities are a national issue that affects the country’s economic stability and life expectancy rates for all groups, Beal stated. Furthermore, given the growing diversity of the U.S. population, this issue cannot be ignored.
One of the challenges to creating an evidence-based action plan is that it requires a fresh approach to research. One of the basic tenets of experimental research is the availability of a clear, concise, narrowly focused question to be answered. This kind of reductionist approach will not work when health disparities are addressed.
The reductionist approach also lends support to the idea that a “silver bullet” that can address disparities does exist. The reality is that to get to the root cause of disparities, it is not going to be just one factor. For example, poor health literacy perpetuates health disparities, as does a lack of access to care, a lack of access to a regular provider, and a lack of access to a medical home. No single factor can be considered to be the root cause of disparities.
It is also clear that although national data can provide a direction, local data are needed to determine an appropriate intervention. Beal used as an example the implementation of an intervention to address obesity in The Bronx, New York, versus one to address obesity in rural Mississippi. How an intervention gets implemented on the ground is going to be extremely different in these two locales. This means that everyone must be prepared for complexity.
Beal described a patient she once had, a young Latina, who was dealing with an unplanned pregnancy. She was already 2 months pregnant when she realized that she was pregnant. She then took another month to decide to keep the baby. At 3 months pregnant, she tried to go see a physician. The physician explained to her that she needed to have health insurance, so she had to apply for Medicaid. The young woman did apply for Medicaid, which took another 6 weeks to process. At this point, the young woman was 4.5 months pregnant. The next step was to find a provider who would accept Medicaid. By the time she found a health care provider who would accept Medicaid, she had to wait 6 weeks for an appointment. At 6 months pregnant, she was ready for her first prenatal visit. Several days before her appointment, the young woman went into labor and delivered triplets. The babies ended up doing well, because the mother was quite capable and had strong family support. Clearly, however, said Beal, this is an example of a disparity in access to health care.
What could have been done to help this mother? First, she could have been insured right from the start and provided with coverage that includes access to contraception. She could have had easier access to care. She could
have had easier access to Medicaid providers in her community; however, an inadequate number of providers were willing to accept Medicaid. A situation like this one would have needed several interventions to prevent a disparate outcome. Again, this research is not simple, and all involved need to be prepared for what is not going to be clean research.
Cultural Competence
Cultural competence is critically important, said Beal. Patients need to feel valued, and patients need to be able to talk with their providers. At the same time, this is not enough to eliminate disparities. Beal stated that “cultural competence is important in and of itself, but it is not the panacea, and it is not going to do all that we need to do to address disparities.”
As an example, she talked about her father, who has end-stage renal disease. He reported that he often feels that he is not treated with respect by the hospital staff (for example, they call him by his first name, which he does not find acceptable). Beal’s father also reports challenges with poor care coordination and challenges with payment for home care. This takes the policy discussions about health disparities back to the real world and out of the realm of policy discussions.
The paradigm needs to be shifted from a deficit model of describing health disparities to an asset model that considers solutions, stated Beal. Rather than looking at a community’s disparities, look for a community with no disparities and study them. Those pockets of excellence need to be found and studied. Much as Elliot Fisher demonstrated with the Dartmouth Atlas (www.dartmouthatlas.org), it is essential to look for the communities with high-quality care and low levels of health disparities and to study those communities. Beal concluded by emphasizing several future needs: the need for a paradigm shift from health disparities to health equity, the need for an evidence-based action plan, and the need to be prepared for complexity.
Dennis Andrulis is a senior research scientist at the Texas Health Institute, where he conducts research with vulnerable populations on the topics of urban health, cultural competence, and language assistance. He was previously associate dean for research in the Drexel University School of Public Health. Andrulis began his comments by stating the three main themes for his presentation, which can be identified by the following questions:
• Where are the knowledge gaps?
• Where does cultural competence stand today?
• What are the next steps?
Knowledge Gaps
In discussing the knowledge gaps in the field of health disparities today, Andrulis acknowledged that research on the incidence and prevalence of health disparities has matured. However, although a base has been established, knowledge gaps persist. Andrulis explained that the knowledge gaps occur at three key levels: the individual, organizational, and community levels.
Individual Level
On the individual level, Andrulis said, although research and knowledge regarding the incidence and prevalence of health disparities-related conditions have matured in many ways, gaps persist in knowledge about why disparities in health outcomes have not narrowed more significantly. The persistence of these knowledge gaps, in turn, leads to three questions:
• Do historic or generational issues (such as poverty) that might change over time exist? He described some earlier research conducted in Prince George’s County, Maryland, that found that very high levels of chronic disease and mortality continue to exist there, even though it is one of the wealthiest counties with a predominantly African American population in the United States. In fact, the rates for many conditions or causes of mortality (for example, infant mortality, smoking, and irregular seat belt use) were similar to those seen in inner-city Washington, DC (Lurie et al., 2009).
• To what extent are current and intensifying concerns (such as overweight, obesity, and diabetes) mitigating efforts to reduce health disparities? In other words, are there contributing factors that are superseded by other emerging factors now coming to the fore? Efforts to reduce the effects of these emerging factors on chronic conditions could be mitigating progress in reducing health disparities.
• How and to what extent do race and culture-specific impediments to effective care and management (such as language, health literacy, and communication challenges) contribute to health disparities? This broad set of issues around race, culture, language, and cultural competence should be addressed.
Organizational Level
Health care reform, the ACA, has implications for reductions in health disparities through system incentives, such as reimbursement rates.
In responding to these system incentives, health care organizations can have an effect on reducing disparities. However, resistance to change to address diverse patient needs can intersect with new incentives to improve patient access and quality; therefore, it is critical to note the characteristics of low-performing health systems and compare them with the characteristics of high-performing health systems. Understanding the implications and impact of pay for performance should also be considered in the context of efforts to reduce health disparities. Andrulis noted both an opportunity and an obligation to engage these organizations more fully, directly, and in a measured way to address health disparities, as health care institutions play a key role in affecting institutional racism in the health care system.
Community Level
The influences of place and geography as contributors to health disparities have a very limited research base and several questions remain unanswered. For example, what are the community factors that contribute to and help perpetuate health disparities, aside from the usual suspects (for example, poverty and a lack of education)? What is the importance of each factor to an understanding of health disparities? What about the importance of the mix of factors in different communities?
What Is the Current Status of Cultural Competence?
Although knowledge about the role of cultural competence in access to and quality of health care is growing, more specific detail on the operationalization of cultural competence is needed, said Andrulis. In fact, the National Center on Minority Health and Health Disparities (NCMHD) has included cultural competence in its solicitations for proposals, indicating the importance of cultural competence among access and quality measures.
Lieu et al. (2004) conducted research funded by The Commonwealth Fund on the effects of cultural competence–related policies and practices on outcomes of care for asthma in children and found that cultural competence did play a role in the more positive health outcomes. Although this finding is promising, little research that might flesh out the particular components of cultural competence that make a difference has followed. Much more needs to be done in this area.
Work in the area of standards development for cultural competence has also taken place. For example, the Joint Commission, the Office on Minority Health in HHS, and the National Quality Forum are all developing standards for interpreter qualifications as well as language and culture measures. Although movement in the area of cultural competence is clearly
happening, it is not clear where the movement toward the development of these standards will go next.
Specific Elements of a Cultural Competence Model
Perhaps the biggest knowledge gap in the implementation of cultural competence interventions and the creation of measures involves the specific elements of a cultural competence model. Andrulis asked what works, when, and how. Much work remains to be done in this area. Although practitioners who believe in the concept accept the concept, some skepticism about cultural competence remains.
A second knowledge gap is that little research on what constitutes effective training in cultural competence has taken place. Training should also be standardized, and this has not yet occurred. Again, a much larger literature around training in cultural competence needs to be created.
Finally, the importance of community engagement in the provision of culturally competent care is acknowledged but has not been fully explicated. For example, the Centers for Medicare and Medicaid Services (CMS) is working with quality-improvement organizations participating in diabetes management programs to require these organizations to engage communities and include community-based workers in their programs. Overall, however, much more work is needed in this area.
Next Steps
Andrulis closed his presentation with some suggestions about what needs to happen next in health disparities research. He outlined his suggestions in three separate areas.
First, research is needed to identify effective strategies for tailoring chronic disease and wellness management programs to diverse individuals. Clinical care models (and the components of those models) that might be adapted to the management of health and wellness for diverse populations have not been adequately reviewed or analyzed to date.
Self-management should also be considered a part of these models. What specific strategies of self-management will help diverse populations take charge of their health and wellness? What strategies will help diverse populations respond and adhere to treatment? Models of care management and wellness management should take into account issues around race, culture, literacy, and language. Development of an evidence base for the management of chronic diseases in diverse patients should also be a part of this process.
Second, provision of support for research and assessment activities that link health care organizations with efforts to reduce disparities is a
necessary next step. Organizations should conduct cultural audits of their activities and ensure that the consumer’s perceptions match the organization’s perceptions of their actions to reduce health disparities and improve cultural competence. A body of work is needed to determine whether it is possible to differentiate actions that work better from others that work less well.
The third area of research needed is the creation and testing of specific interventions that train and educate health care organizations and practitioners to use broader intersectoral strategies to promote health and prevent chronic illness. It is not enough to look at the health care system, because the health care system often serves as the funnel for other problems facing diverse populations (for example, domestic abuse, poor housing options, and homelessness). All of these systems should be considered together, and the barriers across systems should be broken down.
One potential strategy to promote intersectoral work is to change the ways that health care practitioners are rewarded. For example, a physician-practitioner advocate role could be formalized in a way that allows incentives for health care institutions to work with agencies beyond the health care clinic.
Andrulis proposed that the Institute of Medicine (IOM) undertake a comprehensive study to provide guidance about cultural competence to the health care field. With the enactment of health care reform, this would be a very helpful document, he suggested. The report should cover the following issues:
• Define what constitutes the field of cultural competence.
• Identify what data are needed to create an evidence base.
• Develop applicable measures of effectiveness.
• Establish the link between cultural competence and health care quality, cost, and effectiveness.
• Identify what constitutes effective diversity training and education.
• Clarify the role of cultural competence in achievement of prevention outcomes.
A federal strategy to promote intersectoral programs, initiatives, and policies should be created and formalized, Andrulis said. Interagency and community collaborations to promote prevention and health care goals should also be promoted at the state and local levels. Furthermore, the research base should be broadened to include successful demonstrations of collaborative initiatives between health care organizations and housing, transportation, and other relevant agencies with the goal of improving health.
Finally, although CLAS (Culturally and Linguistically Appropriate Services)
standards are in place, demonstrations and evaluations of programs implementing these and other relevant standards should be conducted. It is important to begin to measure the effects of these standards.
William Vega, describing himself as “having been a gardener in the vineyard of cultural competence,” commented that cultural competence is a heterogeneous concept. This makes it difficult to standardize measures and then link them to a specific form of training. Vega explained that because supervisors and chief executive Officers set and sustain policies, they should be willing to experiment. And as they experiment, those in leadership roles should be aware of the complexity of measuring cultural competence and the tentative nature of the process that Anne Beal described and have the willingness to go the distance in order to achieve cultural competence. Andrulis responded that leadership should play a key role and that leadership is where the process should begin. At the same time, building cultural competence within an organization among an array of practitioners might assist with sustainability. The recognition that every organization has strengths and assets and the tying of those assets to the measurement of cultural competence can lead to a strategy to build on those assets.
Valerie Welsh, the performance improvement evaluation Officer at OMH (Office of Minority Health), described research looking at public awareness of health disparities over time. She reported that although the general public’s awareness of health disparities has increased, the increase has been relatively modest. Awareness of health insurance disparities is higher, and African Americans are more aware of health disparities than are other racial/ethnic groups. The public has a very low level of awareness of health disparities affecting Asian Americans, even among Asian Americans themselves. Welsh said that increasing awareness is the first step in trying to address the problem. Awareness of disparities is markedly higher among physicians than among the general public; nonetheless, physicians too underestimate the degree of the disparities in many areas.
OMH released a strategic framework addressing health disparities in 2008. Welsh said that as the framework was being created, the Office found much research about the nature of the problem of health disparities and on the contributing and causal factors. In particular, more Americans are aware that disparities in health insurance coverage exist. However, what was not found was research identifying the specific outcomes at the individual, societal, and systems levels. This raised questions of how those outcomes should be measured so that methodologically sound evaluations of interventions designed to ameliorate those factors can be conducted.
Welsh noted that the research community could be doing a better job of identifying and testing measures of intervention outcomes.
Berenholtz, S. M., P. J. Pronovost, P. A. Lipsett, D. Hobson, K. Earsing, J. E. Farley, S. Milanovich, E. Garrett-Mayer, B. D. Winters, H. R. Rubin, T. Dorman, and T. M. Perl. 2004. Eliminating catheter-related bloodstream infections in the intensive care unit. Critical Care Medicine 32(10):2014-2020.
Braveman, P. 2010. Priorities for Health Disparities Research. Center on Social Disparities in Health, University of California, San Francisco. Presentation at the IOM Workshop: Ten Years Later: How Far Have We Come in Reducing Health Disparities? Washington, DC.
Burstrom, B., M. Whitehead, S. Clayton, S. Fritzell, F. Vannoni, and G. Costa. 2010. Health inequalities between lone and couple mothers and policy under different welfare regimes—The example of Italy, Sweden and Britain. Social Science & Medicine 70(6):912-920.
Lieu, T. A., J. A. Finkelstein, P. Lozano, A. M. Capra, F. W. Chi, N. Jensvold, C. P. Quesenberry, and H. J. Farber. 2004. Cultural competence policies and other predictors of asthma care quality for Medicaid-insured children. Pediatrics 114(1):e102-e110.
Lurie, N., K. M. Harris, R. A. Shih, T. Ruder, A. Price, L. G. Margin, J. Acosta, and J. C. Blanchard. 2009. Assessing Health and Health Care in Prince George’s County. Arlington, VA: RAND.
RWJF (Robert Wood Johnson Foundation), Commission to Build a Healthier America. 2009. Issue Brief 5: Race and Socioeconomic Factors. Princeton, NJ: Robert Wood Johnson Foundation.
















