The Geriatric Mental Health and
Substance Use Workforce
Abstract: The geriatric mental health and substance use (MH/SU) workforce is a loosely defined set of providers who assess, diagnose, treat, manage, and care for older adults who have or are at risk for MH/SU conditions. Members of this workforce have shifting and overlapping roles, as older adults may see many types of health providers to deal with their complex array of physical and mental health concerns. Current education and training for most health care providers do not cover the skills and competencies necessary to provide adequate care for older adults who need MH/SU care. Geriatric MH/SU specialists, who are the most highly trained to handle complex MH/SU cases, are in very short supply. Direct care workers, peer support providers, and consumers and their families are playing increasingly vital roles in the MH/SU workforce. Training for these groups is less systematic and thus more difficult to analyze. Though the challenges facing the geriatric MH/SU workforce are numerous and complex, many stakeholders have initiated efforts to build and strengthen the workforce, with various degrees of success.
This chapter addresses the Institute of Medicine (IOM) committee’s most fundamental challenge: to assess the capacity and competence of the mental health and substance use (MH/SU) workforce to meet the needs of the rapidly growing older population. Yet, this workforce is not easy
to define, document, or examine. The term “workforce” often connotes a cohesive, definable group of professionals, paraprofessionals, and others who are employed with a common purpose. However, the geriatric MH/SU workforce is more aptly described as a de facto group (Robiner, 2006) of diverse professionals and others who care for older adults in a wide variety of settings under many different working conditions. Some members of the MH/SU workforce are highly trained individuals with advanced graduate training while others have associate’s or bachelor’s degrees, high school diplomas, or less formal education (Hoge et al., 2007). Each profession has its own history, unique educational requirements and curriculum, career path, certification and licensure requirements, earning potential, and employment options, though these may vary significantly within some professions. In addition, the MH/SU workforce is blurred by the ambiguous boundaries among the numerous professions. Mental health providers, such as psychiatrists and psychologists, advanced practice nurses and physician assistants, and counselors and social workers, often have overlapping roles and scopes of practice, which may differ by state.
Many researchers have described the difficulties in trying to ascertain the nature, location, qualifications, and size of the MH/SU workforce for patients of any age (Hoge et al., 2007; IOM, 2006; Robiner, 2006). Focusing on the workforce with specific skills who are providing geriatric MH/SU services is even more of a challenge. The committee discussed these challenges at its first meeting and addressed two questions: first, how to define the geriatric MH/SU workforce and, second, how to estimate workforce demands and supply. These decisions are explained below. The chapter then presents a review of the key sectors of the workforce. The following sections will describe some of the primary challenges in improving the geriatric MH/SU workforce and include relevant efforts that have been implemented to strengthen the workforce.
DEFINING THE GERIATRIC MH/SU WORKFORCE1
Older adults are diagnosed and treated for MH/SU conditions by an array of providers in a wide variety of settings, including primary care offices, hospitals, individuals’ homes, long-term care facilities, and specialty settings (both outpatient and residential), which makes defining the “geriatric MH/SU workforce” difficult. The committee focused on those who provide services specifically in the diagnosis, treatment, care,
____________
1 This report uses the term “geriatric MH/SU workforce” to refer to the full range of personnel providing services to older adults with mental health and substance use conditions.
BOX 3-1
Geriatric Mental Health and Substance Abuse
Workforce Professions
• Physicians
° Primary care physicians
° Psychiatrists
• Nurses
° Licensed practical nurses
° Registered nurses (RNs)
° Advanced practice RNs
• Physician assistants
• Psychologists
• Social workers
• Marriage and family therapists
• Counselors
• Pharmacists
• Occupational therapists
• Peer support specialists
• Community health workers
• Direct care workers
• Family and other unpaid caregivers
and management of MH/SU conditions in the geriatric population. This includes primary care providers, MH/SU professionals, and professionals providing other types of therapies for MH/SU conditions, direct care workers (DCWs), community providers, and family caregivers, as listed in Box 3-1. Many other groups also work closely with older adults and are integral to the overall health and well-being of this population. Their role in identifying MH/SU symptoms and referring older adults to appropriate services is vitally important, but will not be discussed in this review.
ESTIMATING WORKFORCE SUPPLY AND DEMAND
Questions about demand/need and their relationship to supply emerge naturally in any discussion of workforce issues. At first blush, it might seem straightforward to translate data on illness prevalence into estimates of service need and then, in turn, to estimates of required workforce supply. Throughout the history of health care, however, such efforts
have been fraught with methodological challenges and serious questions about the validity of estimates that have been generated.
A previous IOM committee, which focused on the provision of psychosocial services to cancer patients, grappled with this issue and drew the following conclusions:
Ideally, one might want to estimate carefully the level of need for these services and then attempt to predict accurately the necessary workforce supply to meet that need. However, experts in health care workforce issues note decades of failure of efforts to estimate the size, composition, and distribution of the nation’s health care workforce. … Even in countries with centrally managed, universal health care systems, progress in medical technology and changes in the organization of care can create large forecasting errors. Predicting workforce supply in the United States is further complicated by the fact that demand for services is not tightly controlled, and the distribution of the workforce is neither controlled nor actively shaped through reimbursement mechanisms. … To complicate the matter, data on health professions are not collected in a routine, standardized fashion across the multiple disciplines … and the dramatic growth in selected disciplines, such as clinical psychology and counseling, has reshaped the composition of the health care workforce. Another limitation on a forecasting effort is that the same function (e.g., care coordination, case management, or patient navigation) may be carried out by different types of professionals, paraprofessionals, or volunteers in different organizations or systems. Thus, workforce needs are heavily influenced at the local level by the assignment of functions to providers. For these and other reasons … the development of estimates of the overall workforce capacity required to meet psychosocial health needs through modeling or other methods was not a feasible activity for this study. (IOM, 2008a, pp. 287-288)
Data on the geriatric MH/SU workforce is even more elusive because the majority of workers who provide services to the geriatric population do not have recognized credentials in this specialty, and are thus more difficult to count, track, and analyze. The committee used information from professional organizations, government agencies such as the Bureau of Labor Statistics (BLS) and the Health Resources and Services Administration (HRSA), and other sources to obtain estimates of the existing workforce. However, the committee chose not to make predictions of workforce capacity or demands because the data to inform these estimates are severely lacking.
REVIEW OF THE GERIATRIC MH/SU WORKFORCE
This portion of the chapter will provide an overview of the main professions that comprise the geriatric MH/SU workforce. Each section will
describe the general scope of the profession, the nature of the profession’s work with older adults and patients or clients with MH/SU conditions, and workforce characteristics. Required training and competency in geriatric MH/SU will be discussed briefly for each group. Detailed requirements for each profession in the areas of older adult care, mental health, substance use, co-occurring MH/SU conditions, and geriatric MH/SU are listed in Appendix C.
Overview on Accreditation, Licensure, Examination, and Certification
A wide variety of organizations and entities, at both the national and state levels, play a role in setting standards and requirements for the education and training of health care providers. Accreditation, licensure, examination, and certification are the primary processes used to ensure quality training and minimum competencies for a provider. The process, structure, and requirements for each vary among professions. However, there are some commonalities, and they will be described generally here. The entities responsible for accreditation, licensure, examination, and certification for each profession are listed in Table 3-1.
Accreditation is the primary process by which higher education institutions and programs ensure quality to the public. Accreditation is carried out by private, nonprofit organizations. Institutions, specific programs, or freestanding schools (e.g., schools of medicine) may be accredited. While accreditation is voluntary, it is often used as an indicator of academic quality, and may be a condition of federal and state funding or professional licensure. Accreditation bodies are held accountable by receiving recognition from the Council for Higher Education Accreditation (non-governmental) or the U.S. Department of Education (Eaton, 2011).
Licensure is state regulated and required for individual practitioners. Where a profession is licensed, it is illegal for an individual to practice without a license (Hartigan, 2011). State licensing boards establish scopes of practice, minimum standards for education and training, examination requirements, and standards for professional behavior and ethics (NCSBN, 2011b).
Examination is a process that is typically required for licensure. Because state licensing boards are the primary user of exam scores, many licensing exams are created by nonprofit associations of state licensing boards, such as the Association of Social Work Boards and the National Coalition of State Boards of Nursing. Most professions use the same exam nationwide to ensure consistency and to improve the portability of credentials across state lines. However, individual state boards may have different criteria for passing.
| Workforce Sector | Accreditation | Licensure | Licensure Examination | Certification (Voluntary Credentialing) |
| Social work | Council on Social Work Education | State boards of social work, behavioral health professionals | Association of Social Work Boards (bachelor’s, master’s, advanced generalist, and clinical social work licensure examinations) | National Association of Social Workers |
| Marriage and family therapists(MFTs) | Commission on Accreditation for Marriage and Family Therapy Education | State boards of MFT, counseling, or behavioral health professionals | Association of Marriage and Family Therapy Regulatory Boards (AMFTRB Examination in Marriage and Family Therapy) | None |
| Counselors | Council for the Accreditation of Counseling and Related Educational Programs; Council on Rehabilitation Education | State boards of counseling, or behavioral health professionals | National Board for Certified Counselors (National Counselor Examination, National Clinical Mental Health Counseling Examination, Examination for Master’s Addiction Counseling); Commission on | National Board for Certified Counselors; Commission on Rehabilitation Counselor Certification |
| Nursing: Registered nurses (RNs) | State boards of nursing; Commission on Collegiate Nursing Education (voluntary); National League of Nursing Accrediting Commission (voluntary) | State boards of nursing | National Council of State Boards of Nursing (National Council Licensure Examination for Registered Nurses) | American Nurses Credentialing Center |
| Nursing: Advanced practice RNs | State boards of nursing; Commission on Collegiate Nursing Education (voluntary); National League of Nursing Accrediting Commission (voluntary) | State boards of nursing | None | American Nurses Credentialing Center; American Academy of Nurse Practitioners; American Association of Critical-Care Nurses Certification Corporation |
| Physician assistants (PAs) | Accreditation Review Commission on Education for the Physician Assistant | State PA or medical boards | National Commission on Certification of Physician Assistants (PA National Certifying Exam) | National Commission on Certification of Physician Assistants |
| Psychology | American Psychological Association Commission on Accreditation | State boards of psychology | Association of State and Provincial Psychology Boards (Examination for Professional Practice in Psychology) | Association Board of Professional Psychology |
| Social work | Council on Social Work Education | State boards of social work, behavioral health professionals | Association of Social Work Boards (bachelor’s, master’s, advanced generalist, and clinical social work licensure examinations) | National Association of Social Workers |
| Marriage and family therapists (MFTs) | Commission on Accreditation for Marriage and Family Therapy Education | State boards of MFT, counseling, or behavioral health professionals | Association of Marriage and Family Therapy Regulatory Boards (AMFTRB Examination in Marriage and Family Therapy) | None |
| Counselors | Council for the Accreditation of Counseling and Related Educational Programs; Council on Rehabilitation Education | State boards of counseling, or behavioral health professionals | National Board for Certified Counselors (National Counselor Examination, National Clinical Mental Health Counseling Examination, Examination for Master’s Addiction Counseling); Commission on | National Board for Certified Counselors; Commission on Rehabilitation Counselor Certification |
| Rehabilitation Counselor Certification (Certified Rehabilitation Counselor Examination) | ||||
| Pharmacists | Accreditation Council for Pharmacy Education; American Society of Health System Pharmacists (residency programs) | State boards of pharmacy | National Association of Boards of Pharmacy (North American Pharmacist Licensure Examination, Multistate Pharmacy Jurisprudence Examination); state boards of pharmacy (may have separate state jurisprudence examination) | Board of Pharmacy Specialties; Commission for Certification in Geriatric Pharmacy |
| Occupational therapists | Accreditation Council for Occupational Therapy Education | State boards of occupational therapy | National Board for Certification in Occupational Therapy (NBCOT Certification Examination) | National Board for Certification in Occupational Therapy, American Occupational Therapy Association |
| Direct care workers, certified nurse assistants | State boards of nursing or departments of public health; Medicare- or Medicaid-qualified nursing homes must follow federal requirements for minimum training | State boards of nursing or departments of public health | Evaluation developed by state regulatory body; some states use National Council of State Boards of Nursing program (National Nurse Aide Assessment Program) Medicare- or Medicaid-qualified nursing homes must follow federal requirements for evaluation |
None |
| Home health aides | State boards of nursing, departments of public health; Medicare- or Medicaid-qualified home health agencies must follow federal requirements for minimum training | Some states do not credential home health aides; where credentialing exists, it is regulated by state boards of nursing or departments of public health | Evaluation requirements established by state regulatory body Medicare- or Medicaid-qualified home health agencies must follow federal requirements for evaluation |
None |
| Personal and home care aides | Most states do not regulate personal and home care aide training programs | Most states do not credential personal or home care aides; federal legislation requires states to establish personnel qualifications for Medicaid-funded personal care services, but does not establish specific standards | Most states do not require evaluation or examination of personal or home care aides | National Association for Home Care and Hospice (Home Care Aide Certification); Direct Care Alliance (Personal Care and Support Credential); CertifiedCare (Basic Caregiving, Advanced Health and Safety, and Alzheimer’s- Dementia Specialist Certification) |
SOURCES: 42 C.F.R. Parts 483 and 484, State Medicaid Manual(Chapter 4, Section 4480, paragraph E).
Unlike licensure, certification is a voluntary, nongovernmental process that allows practitioners to publicly attest that they have met the professional competence standards of specific credentialing organizations (ACA, 2012). Certification is often used to document competency in a specialty or subspecialty, such as psychiatry or geriatric psychiatry. Certification may require examination as well. While certification is a voluntary credential in most professions, in some contexts, certification is required in order to practice. For example, certified nursing assistants and certified substance abuse counselors must obtain certification to practice in these roles, and the certification is regulated by a government entity (CSAT, 2005; Maryland Board of Nursing, 2010).
Physicians
This section will focus on primary care physicians, psychiatrists, and geriatric specialists, although it is recognized that physicians of numerous specialties play an important role in the care of older adults with MH/SU disorders. The nature of our health care system often renders physicians as the principals in patient care within ambulatory, inpatient, and long-term care settings. Thus, for many episodes of patient care, a specialist physician (e.g., cardiologist, oncologist, emergency medicine physician) without specific training in MH/SU disorders may be the first-contact provider of care for older adults with MH/SU disorders. These specialist providers, who clearly play a role in the care of older adults with MH/SU, are not included in the discussion below. Furthermore, when referring to physicians, the term is meant to encompass both medical doctors (MDs) and doctors of osteopathic medicine (DOs), including foreign medical graduates.
Undergraduate Medical Education
Every state licensing board requires physicians to graduate from an accredited 4-year medical school program and to pass either the U.S. Medical Licensing Exam or the Comprehensive Osteopathic Licensure Examination in order to practice. Allopathic programs are required to include clinical experience in psychiatry (Liaison Committee on Medical Education, 2011); on average, psychiatry clerkships last 7 weeks (Barzansky and Etzel, 2001). However, the extent of medical students’ specific exposure to geriatric mental health is not well documented. Medical licensing examinations assess general knowledge of early identification, diagnosis, and treatment of mental disorders and substance-related disorders, and the normal physical and mental changes associated with aging (Federation of
State Medical Boards of the United States and National Board of Medical Examiners, 2011; NBOME, 2011).
Primary Care Physicians
Primary care physicians2 are trained to provide comprehensive and continuous care for patients without limitation to diagnosis, organ system, or problem origins. They often serve as the first point of entry into the health system, and assist individuals in navigating other health services as needed (AAFP, 2011). In 2008, there were an estimated 208,000 general internal medicine or family medicine physicians—the principal primary care medical specialties—in the United States (AAMC, 2008).
Few details are available on the geriatric MH/SU content of postgraduate primary care education. In a 2008 survey, about 50 percent of family medicine and 29 percent of internal medicine residency program directors reported that their programs required fewer than 12 days of clinical geriatrics during the entire 3-year residency training period (GWPSC, 2009a,b,c). Family medicine residency directors indicated that their programs also required some training in geriatric psychiatry.
Geriatricians There were about 7,500 certified geriatricians in 2011 (ABFM, 2011; ABIM, 2011; AOA, 2010). Geriatricians are physicians who complete 1 to 3 years of geriatric fellowship after a 3-year residency in internal medicine or family practice. Geriatric fellowships typically require didactic and clinical experience in geriatric psychiatry, including knowledge of depressive, psychotic, anxiety, personality, and substance disorders and treatment options as well as the assessment of physical and mental status in older adults (ACGME, 2006, 2007; AOA, 2011b).
Opportunities to train in geriatrics appear to far exceed demand for training slots. In the 2011-2012 academic year, 362 fellows held 149 accredited geriatric fellowships (ACGME, 2012). Since 2000, 25 to 46 percent of geriatric fellowship positions have not been filled (GWPSC, 2010a). In 2009-2010, the American Osteopathic Association had 12 accredited geriatric fellowship programs with 46 positions available; only 2 were filled (GWPSC, 2010b).
Psychiatrists
Psychiatrists are physicians who specialize in the prevention, diagnosis, and treatment of mental, addictive, and emotional disorders upon
____________
2 The term “primary care physician” is used throughout this report to refer to general internal medicine or family medicine physicians.
completion of a 4-year residency program (ACGME, 2009). Psychiatric residencies include some contact with older adults with mental health or substance use conditions. Allopathic residencies specifically require 1 month in both geriatric psychiatry and substance use, including patients with dual diagnoses (ACGME, 2009). The osteopathic psychiatric residency also includes geriatric experience in psychiatric disorders and substance abuse problems for an unspecified time period (Ross and Goldner, 2009).
Geriatric psychiatrists Geriatric psychiatrists specialize in the treatment and diagnosis of mental health conditions in older adults. They work with older adults, families and caregivers, and other health professionals to address co-occurring medical conditions, medication management, family concerns, and social or environmental issues specific to older adults (Geriatric Mental Health Foundation, 2012). Subspecialization in geriatric psychiatry requires a 1-year fellowship after residency (ACGME, 2003b). Although the fellowships in geriatric psychiatry have been available since 1991, few psychiatrists have pursued additional training, and interest in the subspecialty appears to be waning. In the most recent academic year (2011-2012), there were 58 geriatric psychiatry fellows nationwide (ACGME, 2012). Since 2006, less than half of the available geriatric psychiatry fellowships have been filled (GWPSC, 2010b).
Psychiatrists who subspecialize in geriatric psychiatry have the option to become board certified in geriatric psychiatry. Since 1991, when the credential was introduced, 3,067 psychiatrists have been certified in geriatric psychiatry (ABPN, 2010a). Certification must be renewed after 10 years (ABPN, 2007). As of 2010, 1,382 geriatric certificates were still active (ABPN, 2010b).
Addiction psychiatrists Psychiatrists also have the option to subspecialize in addiction psychiatry. The 1-year fellowships include training in geriatrics and may offer some experience with the diagnosis and care of older adults with substance use conditions (ACGME, 2003a; AOA, 2011a). The American Board of Psychiatry and Neurology has awarded 2,102 certificates in addiction psychiatry since 1993 (ABPN, 2010a). Only 40 percent of them have been maintained (ABPN, 2010b).
Nurses
Nursing is a multilevel profession focused primarily on caring for and dealing with individual responses to health problems (ANA, 2011). This section will focus on licensed practical nurses (LPNs), registered nurses (RNs), and advanced practice registered nurses (APRNs). Certified nursing
assistants (CNAs) will be discussed in the direct care worker section below.
A new role—the clinical nurse leader (CNL)—has recently been added to nursing master’s-level education. Nurses in this role are viewed as “advanced generalists.” The first CNL certification exams were offered in December 2008 (AACN Commission on Nurse Certification, 2011; CNC, 2011).
Licensed Practical Nurses3
LPNs are nurses who care for people under the direction of RNs and physicians. The role of the LPN varies by state and by job setting; most often LPNs provide basic patient care such as recording vital signs, dressing wounds, assisting with bathing and dressing, and collecting health histories. Experienced LPNs may supervise nursing assistants and aides and help physicians and RNs perform tests and procedures. In some states, LPNs are permitted to administer prescribed medicines (Lafer and Moss, 2007). Nursing homes employ the largest number of LPNs, followed by hospitals, physician offices, home health services, and community care facilities for the elderly (BLS, 2011).
There were more than 730,000 LPNs in the United States in 2010 (BLS, 2010). LPN training is obtained through 12- to 18-month programs in vocational/technical schools or community colleges. The programs are accredited by state boards of nursing with varying levels of coordination with national accrediting bodies (NCSBN, 2004). There is a national licensing exam that tests knowledge in geriatric and psychiatric care, including identifying symptoms of mental health and substance abuse problems, supporting patients in seeking and receiving treatment, and providing care for the special needs of older adults (NCSBN, 2011a). Whether the exam includes competencies in geriatric MH/SU is unclear.
Registered Nurses
The vast majority of nurses—more than 3 million in 2008—are registered nurses (HRSA, 2010). RNs are trained to treat, educate, and support patients in a variety of health care settings. RNs work more independently than LPNs and have the added responsibilities of developing and adjusting plans of care and supervising other nursing staff. Most RNs (62 percent) work in hospital settings; nearly 12 percent (190,000) of hospital-based RNs report spending the majority of their time with older adults. About 5 percent of hospital-based nurses work primarily
____________
3 In some states, LPNs are referred to as licensed vocational nurses, or LVNs.
in psychiatry and mental health (HRSA, 2010). RNs are also commonly employed by nursing facilities, home health agencies, physician offices, schools, and public health clinics. One in four RNs in nonhospital settings (240,000) report that their time is predominantly devoted to geriatric patients (HRSA, 2010).
To achieve the RN title, an individual must complete a nursing program—either a 4-year bachelor’s degree program (BSN), a 2-year associate degree program (ADN), or a 3-year diploma program. All three routes lead to the same license (Center to Champion Nursing in America, 2010). An estimated 45 percent of RNs have 2-year degrees (HRSA, 2010). However, interest in bachelor’s-level training is growing. Between 1980 to 2008, the percentage of RNs with bachelor’s degrees doubled from 17 to 34 percent (HRSA, 2010). Baccalaureate students receive more training in population health, leadership, and the translation of research into practice. RN programs are accredited by state boards of nursing. Two national groups offer voluntary accreditation (NCSBN, 2004). One requires baccalaureate programs to provide clinical experience with the frail elderly, including depression and other mental disorders (AACN, 2008), while the other does not specify standards for geriatric MH/SU curricula.
RNs must pass a national licensure examination. The exam includes geriatric and psychiatric topics and tests candidates’ abilities in handling clients’ reactions to MH/SU diagnoses, support and monitoring of adherence to treatment plans, recognizing changes in mood and behavior, evaluating abnormal responses to aging, and tailoring care and patient education to older adults’ special needs (NCSBN, 2010a).
Nursing specialty certification RNs may specialize in gerontological nursing, adult psychiatric and mental health nursing, and family psychiatric and mental health nursing. Specialty certification requires an active RN license; 2 years of experience; 2,000 hours of clinical nursing experience in the specialty area; and 30 hours of continuing education in the specialty area. The gerontological exam assesses knowledge of tools and techniques for psychological assessment of older adults, and identification of risk factors for self-harm and variations from normal behavior (ANCC, 2010a). The psychiatric and mental health exam includes normal and abnormal mental changes across the life span and the use of age-appropriate assessment tools and techniques (ANCC, 2010b). An estimated 9,000 RNs are certified in gerontology; 19,000 are certified in psychiatric/mental health (HRSA, 2010). Certifications are valid for 5 years (ANCC, 2012).
Advanced Practice Registered Nurses
APRNs have master’s degrees or PhDs in nursing and work with a high level of independence. In most states, they have authority to diagnose, to order tests, and to refer patients in collaboration with or under physician supervision. In some states, APRNs can work and prescribe medications without physician oversight (Christian et al., 2007).
There were approximately 250,000 APRNs in the United States in 2008 (HRSA, 2010). Training and certification of APRNs are evolving. By 2015, all APRNs will be required to have a graduate degree, national certification, and licensure from a state board (NCSBN, 2010c). APRNs will be licensed and certified in specific areas of practice (nurse practitioner [NP], clinical nurse specialist, midwife, or anesthetist) and patient populations (family/individual, adult-gerontology, neonatal, pediatrics, women’s health/gender, or psychiatric-mental health). Adult-gerontology nurse practitioners may further focus on acute or primary care (NCSBN, 2011c). The required degree for APRNs will be a doctorate in nursing practice. There are currently 150 doctoral nursing programs, with 100 in development (AACN, 2004).
Advanced specialty nursing Few APRNs have specialty certification in gerontological or psychiatric/mental health nursing. Two percent are certified in gerontology (HRSA, 2010); of these, only half work full-time as a gerontological nurse practitioner (Kennedy Malone et al., 2008). Core competencies for primary care gerontology include diagnosing and treating mental disorders, assessing patients with comorbid physical and mental conditions, and discussing substance use with patients (AACN, 2010a,b). Four percent of APRNs are certified in psychiatric/mental health (HRSA, 2010). In 2004, more than a quarter of advanced practice psychiatric nurses reported working in the field for at least 30 years (Hanrahan and Hartley, 2008).
Physician Assistants
Physician assistants (PAs) are credentialed or licensed health care professionals who practice medicine under physician supervision. Most states allow PAs to work autonomously if communication with a physician is available (Hooker, 2006). PAs usually perform patient assessments, order and interpret diagnostic tests, develop diagnoses, establish and manage treatment plans, and prescribe and manage medications. They have prescription privileges nationwide (AAPA, 2010a).
PAs are typically employed in hospitals and physician offices (AAPA, 2010b), where they often care for older patients. However, fewer than 1 percent of PAs work in specialty geriatrics. Fewer than 5 percent of PAs
report working in nursing homes or other long-term care facilities; even fewer work in specialty psychiatry (1 percent) or addiction medicine (0.4 percent) (AAPA, 2010b).
The PA workforce has quadrupled in the past two decades, growing from just over 20,000 PAs in practice in 1991 to nearly 83,500 in 2010 (AAPA, 2010b; Morgan and Hooker, 2010). During the same period, the number of accredited PA training programs increased from 54 to 154 (ARCEPA, 2010b).
Through the 1990s most PA programs offered bachelor’s degrees as their highest credential. By 2009, nearly 90 percent offered master’s degrees (Physician Assistant Education Association, 2009). Accreditation curriculum standards include instruction on detection and treatment of substance abuse; palliative and end-of-life care; basic counseling and patient education; issues of death, dying, and loss; and psychiatric/behavioral conditions. Supervised clinical practice in care for the elderly and for behavioral and mental health conditions is also required (ARCEPA, 2010a). An earlier requirement for clinical experience in long-term care settings was dropped in 2010 (ARCEPA, 2010a).
PA programs are typically 27 months long. Graduates may opt for additional 12- to 24-month clinical postgraduate training, although most do not (Brugna et al., 2007). More than half of PA postgraduate programs focus on surgery, surgical specialties, critical care, or emergency medicine. In 2010, there were only two PA programs in psychiatry, and none in geriatrics or addiction medicine (Association of Postgraduate PA Programs, 2010).
Psychiatry Certification
As of 2011, PAs can obtain certificates of added qualifications in five areas. The psychiatry certificate requires an unrestricted PA license; general PA certification; 150 specialty-focused continuing medical education hours; at least 2,000 hours of PA practice in the specialty; attestation of skill and knowledge from a physician in the specialty; and a passing score on the psychiatry qualifying exam (NCCPA, 2009b). The psychiatry exam blueprint indicates that knowledge and skills in “age issues” may be tested (NCCPA, 2009a).
Pharmacists
Pharmacists are trained in the safe, effective, and appropriate use of medications (Council on Credentialing in Pharmacy, 2009). In community-based settings, pharmacists provide direct patient care by evaluating the appropriateness of prescriptions and providing counseling and education
to the patient on proper usage, side effects, and potential interactions. In institutional settings, pharmacists may play a role in medication selection and monitor medication distribution within the institution (Council on Credentialing in Pharmacy, 2009). In 2009, 54 percent of practicing pharmacists reported working in community settings (e.g., independent pharmacies, chains, or supermarkets); 27 percent in hospitals; 3 percent in nursing facilities or other long-term care settings; and 16 percent in other settings including industry and nonpatient care (Midwest Pharmacy Workforce Research Consortium, 2010).
Pharmacists must earn a doctor of pharmacy (PharmD) degree from an accredited program and pass exams as determined by their state (ACPE, 2011). Graduate pharmacy education typically takes 4 years to complete (AACP, 2010). Accreditation for pharmacy schools does not require training in mental health, substance use, or geriatrics. However, advanced practice experience in the last year of education must include primary, acute, chronic, and preventive care among patients of all ages in community pharmacy, hospital or health-system pharmacy, ambulatory care, and inpatient/acute care general medicine. In a 2007 survey of all accredited pharmacy schools, 100 percent of the 49 out of 91 schools that responded reported teaching about depression, schizophrenia, bipolar disorder, and generalized anxiety disorder. Eighty-one percent said they covered substance use disorders (Cates et al., 2007).
Graduates may do 1 or 2 years of residency to prepare them for clinical work or specialty fields (Council on Credentialing in Pharmacy, 2009). As of 2011, there were 12 geriatric and 23 psychiatric residency programs (ASHSP, 2011). In the 2011 residency match process, 9 out of 14 geriatric positions were filled; 26 of 31 psychiatric positions were filled (National Matching Services, 2011). Psychiatry residents are required to understand the clinical presentation, pharmacotherapeutic treatments, and monitoring parameters for therapeutic effects, adverse reactions, and toxicity of psychiatric disorders in the elderly (ASHSP, 2007).
Psychiatric Pharmacy
Pharmacists may obtain specialty certification in psychiatric pharmacy. The certification exam likewise covers psychiatric disorders and medications seen in the elderly and in long-term care settings (BPS, 2005). As of 2010 there were 627 board-certified psychiatric pharmacists in the United States (BPS, 2011). Psychiatric pharmacists work with other health professionals to develop optimal drug therapy plans for patients with psychiatric or neurologic disorders. They may conduct mental status examinations, interview patients, and analyze health history data to design or recommend treatment and monitoring strategies (BPS, 2005).
Geriatric Pharmacy
Geriatric pharmacists are often called consultant pharmacists. Certification as a geriatric pharmacist requires knowledge of psychiatric disorders, including depression and other mood disorders; schizophrenia and other psychotic disorders; sleep disturbances; anxiety disorders; behavioral disorders; and alcohol and drug abuse (CCGP, 2011). There are currently nearly 1,700 certified geriatric pharmacists; an estimated 36 percent are actively working in long-term care, 21 percent in hospital pharmacies.4
Psychologists
Professional psychologists provide an array of prevention, assessment, intervention, and consultation services designed to promote the behavioral health of individuals and populations. There are an estimated 93,000 clinically trained psychologists in the United States (APA, 2011a). Clinical psychology is the largest general provider specialty in this profession. Clinical psychologists assess, diagnose, prevent, and treat a wide variety of mental disorders and abnormal behaviors across the life span. Counseling psychology is another general provider specialty. Counseling psychologists focus more on development and personal functioning, and generally work on healthy aspects and strengths of the client (APA, 2011b,c). In the 2008 American Psychological Association (APA) Survey of Psychology Health Service Providers, 67 percent of psychologists reported graduating in clinical psychology, and 19 percent in counseling psychology. Practicing psychologists have reported that 9 percent of their practice time is dedicated to adult clients over the age of 65 (Michalski et al., 2010). While only 4.2 percent of licensed members of the APA identified geropsychology as a focus, 39 percent of all psychologists surveyed reported delivering services to adults over 65 during a sample week.
Psychologists are licensed by the professional board for psychology in the state in which they practice. To independently practice as a clinical or counseling psychologist, most states require a doctoral degree in psychology, postdoctoral experience, and passing of a licensing exam. Some states allow individuals with master’s degrees to practice as psychologist associates, psychologist assistants, or school psychologists (ASPPB, 2011b). Accreditation standards for doctoral, internship, and postdoctoral residency programs in clinical, counseling, and school psychology are not highly prescriptive about curriculum (APA Commission on Accreditation, 2009)
____________
4 T. Clark, Executive Director, Commission for Certification in Geriatric Pharmacy, personal communication, August 18, 2011.
.
Twelve percent of the psychology licensing exam is devoted to life span development, which includes psychosocial factors, individual and family development, and diseases/disorders that affect people across the life span. It is unclear how much is specifically related to older adults. The exam also covers comorbidity of mental illness with substance abuse and medical disorders, including rates of occurrence and age ranges affected (ASPPB, 2011a).
Geropsychology
Geropsychology applies the knowledge and methods of psychology to understanding and helping older persons and their families address behavioral health problems and achieve maximum potential during later life. The APA formally recognized geropsychology as a specialty area in 2010; it was previously designated as an area of professional proficiency (APA, 2011d; Hinrichsen, 2010). The American Board of Professional Psychology does not offer specialty certification in geropsychology (ABPP, 2012). Psychologists who identified as geropsychologists in the 2008 APA survey reported a broad range of work settings, including private practice (35.1 percent), nursing homes (16.3 percent), group private practices (11.7 percent), and Department of Veterans Affairs (VA) medical centers (7.9 percent) (Michalski et al., 2010). Few geropsychologists reported working in primary care offices or community health centers.
Specialized training in geropsychology may occur through graduate, internship, fellowship, and/or postlicensure continuing education (Hinrichsen et al., 2010; Karel et al., 2010b; Qualls et al., 2005a). Such training usually includes a didactic curriculum on normal versus illness-related aging experiences; orientation to the ethical and legal issues in geropsychology; supervised clinical experience with older adults in varied care settings; membership on an interprofessional team; and experiences designed to promote self-awareness regarding personal responses to aging and the diverse life histories of older adults.
Relatively few opportunities are available for formal geropsychology training at the graduate level, with only 10-15 programs offering a special geropsychology track (Perry and Boccaccini, 2009; Qualls et al., 2005a). Many psychologists-in-training have their first opportunity to specialize in the care of older adults during the internship year, through intensive geropsychology rotations in settings that include VA medical centers, outpatient clinics, psychiatric hospitals, and rehabilitation hospitals. The 2011 Association of Psychology Postdoctoral and Internship Centers directory listed 86 accredited U.S. programs as providing a major rotation in geropsychology, and 223 programs as offering a minor rotation. Formal postdoctoral fellowship programs provide the most intensive, specialized
training in the field, typically through a year of full-time training after completion of the doctoral degree. In 2010, there were approximately 22 full-time fellowships in geropsychology. Continuing professional education opportunities in geropsychology are growing, but still limited (Karel et al., 2010b).
Social Workers
Social workers “assist individuals, groups, or communities to restore or enhance their capacity for social functioning, while creating societal conditions favorable to their goals” (NASW, 2011d, p. 1). They provide a wide array of services across the life span, helping people cope with and overcome challenges such as poverty, addiction, disability, and mental illness. Social workers play a large role in the care of older adults in nursing homes. Federal law requires that skilled nursing facilities provide medically related social services.5 Nursing homes with more than 120 beds are required to employ a full-time social worker with at least a bachelor’s degree in social work or “similar professional qualifications.” Facilities with 120 beds or fewer must still provide social services, but do not need to have a full-time social worker on staff (Social Work Policy Institute, 2010).
The United States has an estimated 642,000 social workers (BLS, 2009b). The Association of Social Work Boards (ASWB) offers licensing exams in five general categories of social work practice: associate’s, bachelor’s, master’s, advanced generalist, and clinical. Individual state licensing boards may offer licensing at some or all of these levels. Associate-level licensing is only offered in four states, for the titles of social work associate, assistant, or technician. The ASWB offers the same exam for associate’s- and bachelor’s-level candidates, though the passing score is lower for the former (ASWB, 2011).
Bachelor’s-level positions typically include outreach, case management, and resource linkage duties. At this level most states require a bachelor’s of social work (BSW) degree from an accredited program, and a passing score on the ASWB bachelor’s licensing exam. Some states will license individuals with non-BSW bachelor’s degrees if they have compensating work experience. Some states do not license bachelor’s-level social workers at all (ASWB, 2008). The licensing exam includes questions on mental health, substance use disorders, co-occurring conditions, and older adult behavior. It also covers the intersection of aging and MH/SU,
____________
5 42 C.F.R. § 483.15.
including the symptoms of mental illness across the life span and the effects of aging on specific interventions (ASWB, 2011).
A master’s in social work (MSW) is required for more advanced social work practice and management. Though the MSW is considered the terminal degree for social workers, about 2 percent of social workers have doctoral degrees (Whitaker et al., 2006). The ABSW master’s licensing exam covers aging processes and more advanced mental health topics, such as the DSM6 framework and intervention planning, though the content outline does not explicitly include MH/SU in the elderly. In states that license advanced generalists and clinical social workers, an MSW or doctorate is required, plus 2 years of postgraduate work experience. Advanced generalists are expected to have more developed training in supervision and leadership, research use, and administration. Clinical social workers apply the principles and goals of social work to the diagnosis, treatment, and prevention of mental and behavioral disorders. They are trained to provide psychotherapy to clients (NASW, 2005).
Mental Health and Substance Abuse Social Work
The 2006 National Association of Social Workers (NASW) workforce study estimates that 37 percent of social workers work in mental health, making it by far the largest practice area (Whitaker et al., 2006). Social workers also constitute the largest proportion of mental health providers in the United States. Social workers who practice in the fields of mental health and/or substance abuse typically assess and treat individuals in recovery from mental illness and/or substance abuse, and provide a bridge to needed services and resources in the community. These services may include outreach and engagement; assessment and service planning; case management; treatment with individuals, families, and groups; discharge planning; and program planning and implementation across home, community-based, and institutional settings.
The NASW offers voluntary credentials for specialty social work practice. Clinical social workers can apply for the Certified Clinical Alcohol, Tobacco, and Other Drug (ATOD) Social Worker credential. Social workers in this specialty area have advanced knowledge and skills in ATOD epidemiology, physiology, pharmacology, treatment, and policy issues. An MSW, 2 years of postgraduate experience, 180 hours of continuing education, a state license, and adherence to NASW standards are required
____________
6 DSM, or DSM-IV-TR, refers to the Diagnostic and Statistical Manual of Mental Disorders. During the course of this study, the Fourth Edition-Text Revision (DSM-IV-TR) was in use. A fifth edition is expected in 2013 (American Psychiatric Association, 2012).
(NASW, 2011b). All NASW specialty credentials must be renewed every 2 years.
Gerontological Social Work
Seventy-eight percent of social workers report working with older adults, and 9 percent report aging as their primary area of practice (Whitaker et al., 2006). Social workers who work with older adults may assist with advance care planning, loss and grief, independent living, and lifestyle adjustments, among many other issues that older adults may face. They also provide support for family caregivers of older adults.
Gerontology is one of two specialty credentials that the NASW offers at the BSW level. The credential requires a bachelor’s degree, 3 years of work experience with older adults, 20 hours of continuing education, a state license (passing licensing exam score or extra work experience and education may substitute), and adherence to NASW standards of practice (NASW, 2011e). NASW also offers credentials in gerontology for advanced social workers and clinical social workers, which require an MSW, 2 years of postgraduate experience, 20 (advanced) or 30 (clinical) hours of continuing education, a state license, and adherence to NASW standards (NASW, 2011a,c).
Marriage and Family Therapists
Marriage and family therapists (MFTs) diagnose and treat mental health and behavioral disorders within the context of marriage and family relationships. They provide psychotherapy to individuals, couples, or families, with emphasis on how relationships impact an individual’s behavior. Marriage and family therapy is meant to be brief, lasting 9 to 13 weeks, and oriented toward specific therapeutic goals (AAMFT, 2011b). BLS estimates that there were 33,050 MFTs in 2010 (BLS, 2012c).
All 50 states and the District of Columbia recognize and license MFTs (AAMFT, 2011a). Most states require a master’s or doctoral degree from an accredited MFT program, at least 2 years of postgraduate clinical experience, and successful completion of a licensing exam. Educational accreditation guidelines and the licensing exam content include elements on age diversity, life stages, and human development, but do not explicitly mention MH/SU care for older adults (Commission for Accreditation of Marriage and Family Therapy Education, 2005; Professional Examination Service, 2011).
Medicare does not cover mental health services provided by MFTs, thus limiting opportunities for MFTs to work with older adults. This exclusion from Medicare is inconsistent with other federal policy, since
marriage and family therapy is recognized as one of five core mental health professions (psychiatry, psychology, mental health nursing, clinical social work, and MFT) by HRSA’s Bureau of Health Professions in determining mental health provider shortage areas (AAMFT, 2006; HRSA, 2012).
Counselors
Counselors are trained to helped people accomplish mental health, wellness, education, and career goals. There are several types of counselors. The specialties most relevant to geriatric MH/SU are mental health, substance abuse, rehabilitation, gerontological, and pastoral counseling.
State licensure requirements for counselors vary greatly, and may differ by the type of counseling. Typically, one must obtain a master’s degree or higher to be a licensed professional counselor (LPC).7 BLS estimates there were more than 100,000 mental health counselors and nearly 78,000 substance use counselors in 2011. Estimates for the other counseling specialties were not identified.
Mental Health Counseling
Mental health counselors are trained to work with individuals, families, and groups to prevent, assess, and treat mental health, substance use, behavioral, and emotional disorders (BLS, 2009a). For mental health and addiction counseling programs, core curricula must include theories, strategies, and interventions for addiction, as well as individual and family development over the life span. Counselors should also have knowledge of screening and assessment for addictive disorders, and an understanding of the presentation and treatment of co-occurring mental health and substance use conditions (CACREP, 2010).
Addiction and Substance Abuse Counseling
Counselors specializing in addiction and substance abuse counseling are typically licensed by a state agency or board different from mental health counselors. State regulation of this profession is more widely varied than for other types of counselors or mental health providers. For example, North Dakota has only one licensed addiction counseling position, while California has at least nine credentials that can be obtained
____________
7 In some states, LPCs are referred to as licensed clinical professional counselors or licensed mental health counselors. Rehabilitation and pastoral counselors may have different licenses in some states.
in alcohol and drug counseling (CAADAC, 2011; North Dakota Board of Addiction Counseling Examiners, 2000). In many states, individuals can become certified or licensed as an addiction or substance abuse counselor with an associate’s degree or less (ATTC, 2011).
Gerontological Counseling
Accreditation for gerontological counseling programs was dropped in 2009 (CACREP, 2011). Certification in gerontological counseling has also been discontinued due to low levels of interest (Bobby and Urofsky, 2008).
Rehabilitation Counseling
Rehabilitation counselors are trained to work with people with physical, mental, developmental, cognitive, and emotional disorders. They engage in assessment, treatment planning, case management, and advocacy to assist clients in living as independently as possible (CRCC, 2011). Core curriculum requirements emphasize individual diversity, including aging issues, and the impact of disabilities across the life span. Psychiatric and substance abuse treatment and rehabilitation as well as the implications of co-occurring disabilities are also covered (CORE, 2010).
Pastoral Counseling
Pastoral counselors incorporate religious and spiritual elements into mental health counseling (AAPC, 2012). The profession of pastoral counseling is not regulated in most states, though some pastoral counselors may qualify as an LPC (AAPC, 2009).
Occupational Therapists
Occupational therapists (OTs) work with individuals with physical, mental, developmental, and cognitive conditions to help them improve their ability to perform daily living and vocational tasks. The most common sites of employment for OTs are hospitals, outpatient settings, schools, nursing facilities, and home health care services. BLS estimates that OTs held about 100,300 jobs in 2010 (BLS, 2012g).
OTs provide a wide variety of services to older adults. According to the American Occupational Therapy Association (AOTA) Workforce Survey in 2010, over 35 percent of the workforce serves those who are 65 and older, primarily in skilled nursing facilities. OTs work with
patients to improve mobility and independence in activities of daily living (ADLs), provide consultation on environmental modifications that promote safety and occupational functioning, work with a care team to address behavioral or cognitive challenges that may hinder functioning, and help patients and families with transitions home or to another facility (Washkowiak et al., 2010).
In the 2010 survey, 3 percent of respondents identified mental health as their primary work setting, including community mental health centers and outpatient psychiatric clinics (Washkowiak et al., 2010). In mental health settings, OTs may work with patients to develop coping strategies, identify and implement routines that promote wellness, and create individualized recovery and wellness plans (Champagne and Gray, 2011).
The practice of occupational therapy is regulated in all 50 states and the District of Columbia. Generally, an OT must hold a master’s or doctoral degree, complete required fieldwork, and pass an examination (AOTA, 2012b). OT students are trained to understand the occupational effects of mental health conditions, and to design and implement interventions that address these effects. Accreditation standards for both degrees require that curricula prepare students for practice with a wide variety of populations, including the elderly, in areas of physical and mental health. Curricula must also include content on developmental psychology across the life span, as well as abnormal psychology. Students must complete field work in at least one setting where psychological and social factors influence occupational ability. The required duration of field experience is not specified (ACOTE, 2012). Most states also regulate occupational therapy assistants (OTAs), who have associate’s degrees and provide rehabilitative services under the supervision of OTs (BLS, 2012h). OTA programs are accredited by the same body as OT programs, so curriculum standards are highly analogous, but less advanced (ACOTE, 2012).
Mental Health Certification
OTs specializing in mental health design and deliver services to patients with psychiatric conditions. Candidates for certification in mental health must demonstrate professional experience and competence in mental health across the life span, the impact of psychiatric conditions on occupational performance, and current biomedical and occupational therapy practices used to minimize the adverse effects of psychiatric conditions (AOTA, 2009). According to the AOTA, only nine OTs are certified in mental health (AOTA, 2012a).
Gerontology Certification
OTs specializing in gerontology work with older adults to minimize the impacts of disability and optimize participation in life activities. Certification in gerontology requires competence in aging-related physical, cognitive, and psychological changes, and their impact on occupational ability. There are 13 OTs certified in gerontology (AOTA, 2012a).
Direct Care Workers
Direct care workers (DCWs) are individuals who are paid to provide support to individuals with a wide range of health and human service needs. Next to family members, these workers provide the vast majority of services to elderly and younger people with disabilities. There is not a single, unified occupational title for DCWs in aging, physical disabilities, or behavioral health. Occupational titles vary within each sector and across sectors. In aging, there are generally three recognized job categories. Nursing assistants are employed in nursing homes and sometimes other residential settings such as assisted living. Home health aides are employed by Medicare- and/or Medicaid-certified home health agencies. Home care aides/personal care attendants are employed by agencies or hired directly by consumers and/or their families and are employed in a range of community-based settings, including individual homes and apartments, adult daycare centers, and residential settings. In behavioral health a broadly recognized occupational title to denote this type of work does not exist. Some are referred to as community mental health specialists; others work as psychiatric technicians or addiction counselors (noncertified). DCWs in behavioral health are employed in a range of settings, including psychiatric hospitals, outpatient clinics, small group homes, and other community-based settings.
There are currently no data on the actual number of DCWs who care for older adults with MH/SU conditions. In 2008, there were an estimated 1.47 million nursing assistants, 922,000 home health aides, and 817,000 home care/personal care aides providing services to people of all ages in institutional and community-based settings (PHI, 2011). BLS data indicate that 44,300 psychiatric aides were employed in institutional and community-based settings in 2008. The majority of nursing home residents are age 65 and over. Likewise, approximately 55 percent of those likely to receive services from a DCW in the community are age 65 and older.
Those serving the older adult population typically provide hands-on assistance with personal care and hygiene (e.g., bathing, dressing, and grooming); assistance with home skills such as meal preparation,
housekeeping, and laundry; assistance with health-related tasks such as medication management; and companionship and emotional support. The direct care workforce is dominated by females. Nine out of 10 workers employed in nursing homes, home health, and home care are women. A substantial proportion of these workers are nonwhite, ranging from 51 percent in nursing homes and personal care/home care to 58 percent in home health care. Furthermore, 20 to 25 percent of nursing home, home health, and home care aides are foreign born.
DCWs in behavioral health have a slightly different profile. MH/SU-specific settings employ more male DCWs, though women still make up two-thirds of DCWs employed in psychosocial rehabilitation and 70 percent of those employed in the addictions field (Hewitt et al., 2008). Behavioral health also has a higher proportion of white DCWs, with 70 percent in psychosocial rehabilitation and 70 to 90 percent in addiction centers. DCWs employed in the behavioral health sector are more highly educated than their peers in nursing home, home health, and home care, with a much larger proportion having more than a high school education.
Requirements for training are minimal and lack consistency across settings and states. In many cases, there are no requirements. Federal requirements exist for CNAs and home health aides employed by Medicare- or Medicaid-qualified nursing homes and home health agencies. Regulation of other DCWs, including home care or personal care workers employed by assisted living facilities, home care agencies, or private consumers, is determined by the states. Staff in these settings generally receive little or no training (Stone and Urban Institute Staff, 2011).
Federal law requires CNAs working in Medicare- or Medicaid-qualified nursing homes to complete a minimum of 75 hours of training, including 16 hours of supervised clinical practice. The basic training requirements include mental health as a required topic, but the federal regulations offer little guidance on what specifically must be taught. CNAs must also pass a state-approved exam, and become listed on the state nurse’s aide registry.8 The facility employing the CNA must do an annual performance review and provide a minimum of 12 hours of in-service education per year.9 State requirements for certification vary; many exceed the federal standards (National Clearinghouse on the Direct Care Workforce, 2004). Federal requirements for home health aides employed by Medicare- or Medicaid-qualified home health agencies are analogous to the CNA requirements.
Findings from a nationally representative sample of certified nursing
____________
8 42 C.F.R. § 483.152 (Requirements for States and Long Term Care Facilities).
9 42 C.F.R. § 483.75 (Requirements for States and Long Term Care Facilities).
assistants employed in nursing homes in 2004 found that a third felt their initial training did not prepare them well for their jobs; one in four reported that their continuing education training over the past 2 years had not been useful (Sengupta et al., 2010). A little over a fifth of the respondents indicated that they had no input into the topics that were included in their in-service training sessions. The study also identified several topics that DCWs would like in their initial training: working with abusive residents, giving dementia care, performing assistance with ADLs, communicating with coworkers, and managing time. Dementia care, communicating with residents, and working with supervisors were the most often mentioned topics to be included in continuing education. A number of studies have highlighted the lack of geriatric-specific education for these individuals (IOM, 2008b; Office of Inspector General, 2002).
DCWs may obtain voluntary credentials. The National Association for Home Care and Hospice (NAHC) offers voluntary Home Care Aide national certification, which consists of 75 hours of training, a skills demonstration assessed by an RN, and a written examination. NAHC certification has been offered since 1990.
The Direct Care Alliance (DCA) recently developed the Direct Care Alliance Personal Care and Support Credential for personal assistance workers who work with older adults (and people with disabilities) in home- and community-based settings. The DCA credential was developed with support from the Ford Foundation after extensive review of existing training programs and discussion with focus groups of direct care workers, consumers, and employers (Direct Care Alliance, 2011a). Workers earn the credential through a competency-based test. The exam covers interpersonal skills, personal care knowledge and skills, health-related knowledge and skills, and safety, but does not include MH/SU competencies (Direct Care Alliance, 2011b). The DCA began offering the exam in spring 2011 with the goal of credentialing 3,000 personal care workers by the end of the year (Direct Care Alliance, 2011b).
The National Alliance of Direct Support Professionals also offers a credentialing program, but the focus is not on an older client population (NADSP, 2011a,b). After demonstrating competence in providing specialized support to individuals with disabilities in community human services, trainees are certified as DSP-Specialists. The DSP-Specialists can obtain a specialty credential in four areas: positive behavioral support, health support, inclusion and supervision, and mentoring.
The U.S. Department of Labor registers apprenticeships in the following long-term care occupations: direct support specialist, CNA, home health aide, and health support specialist. The CNA and home health aide occupations are multilevel and allow for specialization. CNAs can advance from level 1, to advanced, to specialized CNA. Similarly, home
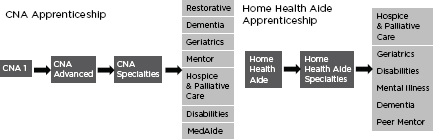
FIGURE 3-1
U.S. Department of Labor apprenticeships in long-term care occupations.
SOURCE: DOLETA Office of Apprenticeship, 2012.
health aides can advance to specialized care (Figure 3-1). CNAs and home health aides can both choose to specialize in geriatrics. Home health aides can specialize in disabilities and mental illness (DOLETA Office of Apprenticeship, 2012).
Apprenticeship programs combine workplace learning and related instruction and require DCWs to complete a specified number of hours of training and on-the-job skill implementation. In addition, apprenticeship standards require that DCWs receive a wage increase upon completion of the program. More than 50 employers have sponsored apprenticeships in the four long-term care occupations (DOLETA Office of Apprenticeship, 2012).
Peer Support Providers
In the context of mental health, a peer is someone who receives or has received MH/SU services and who self-identifies as a person with an MH/SU condition living in recovery. Peer providers may be called peer support specialists, certified peer specialists (CPSs), peer support technicians, peer counselors, peer or consumer advocates, recovery support specialists, recovery aides, client liaisons, or peer bridgers, among other titles. The variation in titles reflects the range of roles that peers may play. Peers may be employed to counsel or mentor others, provide crisis support, run drop-in centers within hospitals, create recovery-oriented programs and hobby groups, help people transition after hospital discharge, or provide other forms of support (Bluebird, 2008).
Integral to peer support is the concept of recovery, which the President’s New Freedom Commission on Mental Health defines as the process in which people are able to participate fully in their communities and live fulfilling and productive lives despite disability, which may include
the reduction or complete remission of symptoms (Hogan, 2003). Peer support providers are trained in a specific skill set to be role models for recovery and teach self-directed recovery tools. In a review of peer support best practices, the Defense Centers for Excellence for Psychological Health and Traumatic Brain Injury identified social support, experiential knowledge, trust, confidentiality, and easy access as the key elements that distinguish peer support (Money et al., 2011).
Peer support is increasingly being incorporated into treatment programs within mental health systems. However, analysis of the workforce in its entirety is difficult because of large variations in titles, employment status (paid versus volunteer), credentialing, work settings, and state efforts to document this workforce. No data are available on how many peer support providers work across all settings nationwide and how many provide services to older adults. The following information will discuss two groups of peer support providers for which the most data are available: those certified by state governments and those working in the Veterans Health Administration (VHA). In many settings and circumstances, peer support providers do not need state- or nationally recognized certification or training to work.
States have been able to reimburse peer support service through Medicaid since 2001. The Centers for Medicare & Medicaid Services (CMS) endorses peer support as an evidence-based model of care and issued guidance to state Medicaid directors in 2007 on Medicaid-funded peer support (CMS, 2007). Use of peer support requires supervision by a mental health professional (as defined by the state); care coordination within a comprehensive, individualized plan of care; and training and credentialing, including continuing education, that ensure providers have the competencies necessary to deliver peer support services (CMS, 2007). According to the 2010 survey of state Medicaid directors, 22 states have Medicaid reimbursement for certified peer specialist services, 8 plan to seek reimbursement in the next year, and 3 plan to establish reimbursement, but not within the next year (Daniels et al., 2011). In a 2009 survey of states with Medicaid reimbursement, 21 states reported employing a total of roughly 2,800 peer specialists (Daniels et al., 2010).
State requirements for certification vary greatly. Some states have developed their own training modules, while others have adopted well-established curricula such as the Georgia Certified Peer Specialist Training or the Recovery Opportunity Center Peer Employee Training (Johnson, 2008). In addition to didactic training, certification may require work experience. For example, Certified Recovery Support Specialists in Illinois must have 2,000 hours of paid work experience, while Pennsylvania and North Carolina require 3 months of supervised peer support work (Johnson, 2008).
BOX 3-2
Veterans Health Administration Peer Support Technician
Domains of Competency
1. Recovery principles
2. Peer support principles
3. Cultural competence
4. Communications skills
5. Group facilitation skills
6. Managing stigma
7. Comprehending the illness
8. Recovery tools
9. Professional development and workplace skills
10. Managing crisis and emergency situations
SOURCE: Veterans Health Administration, 2011.
The VHA embraces a recovery model of service, and has employed peer support technicians to work in seriously mentally ill (SMI) and substance use recovery since 2005. VA facilities are required to provide access to peer support services to all veterans with SMI, whether through an onsite program or through a community provider that has similar standards of quality. Peer support technicians must pass a competency test or obtain certification as a peer provider from a state or agency, and engage in 15 hours of continuing education annually. Competency domains are listed in Box 3-2. As of 2010 there were 237 peer support technicians, and an additional 139 volunteer peer support providers, in the VA system (O’Brien-Mazza and Chinman, 2011).
Community Health Workers
Community health workers (CHWs) are members of communities who work for pay or volunteer in association with the local health care system (HRSA, 2007). CHWs offer interpretation and translation services; provide culturally appropriate health education, counseling, and guidance; assist people in navigating care; advocate for individuals and community health needs; and may provide basic direct services such as first aid and blood pressure screening. CHWs may also be referred to as community health advisors, lay health advocates, outreach educators, community health representatives, peer health promoters, or peer health educators (Goodwin
and Tobler, 2008). Another common title is promotor or promotora. Promotores belong to and serve specific underserved minority populations. As respected members of these populations, promotores are in a unique position to build trust and to address unmet health needs in their communities. Programs that integrate promotores in their services focus on vulnerable segments of the population, such as migrant or farm worker families, or prominent health problems, such as HIV/AIDS or mental illness (Migrant Health Promotion, 2012). Promotores working in mental health may have roles similar to those of peer support providers, such as facilitating support groups and sharing experience in managing mental health issues (Rhett-Mariscal, 2008).
Because CHWs work under many titles, and may work for pay or as volunteers, precise estimates of the workforce are not available. In 2007 the Bureau of Health Professions completed a rigorous and comprehensive CHW workforce survey. The United States has an estimated 86,000 CHWs, with 20 percent concentrated in California and New York (HRSA, 2007). According to this survey, 27 percent of CHWs reported dealing with mental health and 29 percent worked in substance abuse.
Family Caregivers
The term “family caregiver” is broadly defined and refers to any relative, partner, friend, or neighbor who has a significant relationship with, and who provides a broad range of assistance for, an older adult or an adult with chronic or disabling condition(s). Family caregivers have been described as a “shadow workforce, acting as geriatric case managers, medical recordkeepers, paramedics, and patient advocates to fill dangerous gaps in a system that is uncoordinated, fragmented, bureaucratic, and often depersonalized” (Bookman and Harrington, 2007, p. 1005). There is no clear consensus about how large a public investment in institutional or home care is reasonable or what the true costs or benefits are of a community-based strategy that relies extensively on the time, skills, and financial resources of families. AARP’s report, Valuing the Invaluable: 2011 Update: The Contributions and Costs of Family Caregiving, states that in 2009, about 42.1 million U.S. family caregivers provided care to an adult with ADL limitations at any given point in time, and about 61.6 million provided care at some time during the year (Feinberg et al., 2011). The estimated economic value of their unpaid contributions was approximately $450 billion in 2009.
SHORTAGE OF GERIATRIC MH/SU PROVIDERS
The committee’s review of the geriatric MH/SU workforce makes apparent that the sheer number of providers entering, working in, and
remaining in the fields of primary care, geriatrics, mental health, substance use, and geriatric MH/SU is disconcertingly small. Because the shortage of primary care, geriatric specialty care, and MH/SU providers has been documented and analyzed extensively in other recent IOM reports (IOM, 2001, 2006, 2008b), this chapter focuses specifically on the shortage of geriatric MH/SU specialists. In this discussion, “geriatric MH/SU specialist” refers to providers with advanced training and expertise in working with older adults with mental health and/or substance use conditions.
Geriatric MH/SU specialists are an essential part of the interdisciplinary team, as they are the most experienced and best equipped to consult and provide care for SMIs and other complex conditions. With shifting models of care and the changing roles of different professions, it is not possible to estimate with great precision how many geriatric MH/SU specialists will be necessary to serve the geriatric population. However, the rate of specialized providers entering the workforce is dwarfed by the pace at which the population is growing. One key example is geriatric psychiatry (see Figure 3-2). The number of available fellowships in geriatric psychiatry increased in the late 1990s, but has remained relatively stagnant since then. From 1996 to 2011, the number of geriatric psychiatry fellows filling these slots decreased by 50 percent. This decline, juxtaposed with the predicted doubling of the geriatric population in the next 20 years (AOA, 2010), will make it increasingly difficult to meet the MH/SU needs of older adults.
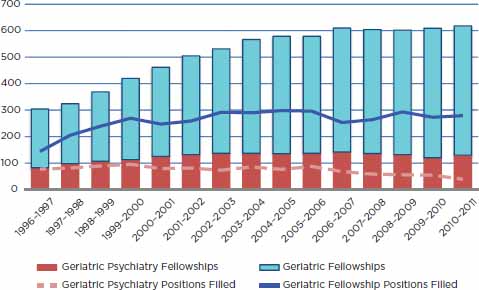
FIGURE 3-2
Comparison of geriatric fellowship and geriatric psychiatry fellowship growth.
SOURCE: Adapted from GWPSC, 2010b.
with the predicted doubling of the geriatric population in the next 20 years (AOA, 2010), will make it increasingly difficult to meet the MH/SU needs of older adults.
As discussed earlier in the chapter, assessing the precise shortage of geriatric MH/SU providers is not possible because of unclear definitions of the geriatric MH/SU workforce and because up-to-date, comprehensive data on the workforce do not exist across all professions. Estimating geriatric MH/SU specialists proves particularly difficult because only two types of mental health professionals may currently obtain specialty credentials in geriatrics: psychiatrists and clinical social workers. There are likely more providers who possess expertise in geriatric MH/SU who do not have formal credentials that indicate this. To estimate the “best case scenario,” Table 3-2 tallies the number of providers specially trained in MH/SU (regardless of the age of the patient population). Of these “general” MH/SU providers, it is unknown how many possess expertise in geriatric care. However, the committee’s review of professional health training and education suggests that the proportion is small.
RECRUITMENT OF GERIATRIC MH/SU SPECIALISTS
This section will describe some of the primary challenges that exist in the recruitment of potential geriatric MH/SU specialists: stigma against MH/SU and aging, lack of incentives to enter this specialty, limited opportunities for specialization, limited support and mentorship, and difficulty recruiting racial/ethnic minority students (Box 3-3). Many groups have recognized these challenges and developed and implemented various strategies to address them; their efforts will be highlighted below. Programs and initiatives highlighted in this section are meant to convey the various strategies adapted across different professions and patient populations. The list is by no means exhaustive, and inclusion in this report does not indicate a detailed review or endorsement by this committee. In some areas, many groups have taken the mantle to make improvements. Other areas have not received as much attention. The impact and potential for replication of these strategies will be discussed where evidence is available.
Stigma Associated with MH/SU and Aging
The enduring stigma associated with MH/SU and aging is a major barrier to growing the geriatric MH/SU workforce. Stigmatizing attitudes held by the general public regarding older adults and mental illness have long been recognized (HHS, 1999; IOM, 2006; World Psychiatric Association and World Health Organization, 2002). Additionally, working
TABLE 3-2
Estimated Number of Mental Health/Substance Use Specialists, 2011
| Psychiatrists | Psychologistsa | MH/SU Social Workers |
Psychiatric APRNsb |
Substance Abuse and Behavioral Health Counselors |
Mental Health Counselors |
Marriage and Family Therapists |
| 23,140 | 100,850 | 115,390 | 19,126 | 76,600 | 114,180 | 33,990 |
| TOTAL | 483,126 |
a Psychologists include clinical, counseling, and school psychologists.
b Estimate for psychiatric advanced practice registered nurses (APRNs) is drawn from the 2008 National Sample Survey of Registered Nurses. All other estimates are from the U.S. Bureau of Labor Statistics.
SOURCES: BLS, 2012b,c,d,e,f,g; HRSA, 2010.
BOX 3-3
Primary Challenges in the Recruitment of
Geriatric MH/SU Specialists
• Stigma against mental health and substance use (MH/SU) and aging
• Lack of financial incentives to practice in geriatric MH/SU
• Limited opportunities for specialization
• Inadequate early career support and mentorship
• Difficulty recruiting racial/ethnic minorities
in MH/SU carries its own stigma. A literature review by the World Psychiatric Association found that medical students widely view psychiatry as having low prestige, lacking a solid scientific foundation, and bringing low job satisfaction (Sartorius et al., 2010). Students also view careers dedicated to older adults negatively. A 2007 survey of high school students interested in pursuing nursing careers showed that 48 percent had no interest in specializing in geriatrics (Evercare, 2007). When MSW students from three large universities were asked in a 2004 survey which population they most desired to work with after graduation, the most popular answer was children, while the least popular choice was older adults (Cummings et al., 2005). As with psychiatry, students perceive working with older adults to be less glamorous and requiring less skill than working with other populations (Cummings et al., 2005). In combination, negative perceptions of mental illness and old age create a powerful barrier to recruiting more geriatric MH/SU providers.
While stigma is deeply rooted and not easily eradicated, some studies indicate that students’ negative perceptions of MH/SU and old age can be reduced through education and exposure to the stigmatized populations (Cummings et al., 2005; Happell, 2008; Happell and Roper, 2003; Koder and Helmes, 2008; Wallendal et al., 2009; Wood and Wahl, 2006). Contact with individuals with mental illnesses, as opposed to instruction or factual information, appears to be the most effective way to reduce stigmatizing attitudes (Couture and Penn, 2003). Therefore, facilitating clinical experiences and personal contact with older adults and individuals with MH/SU conditions may be one effective strategy to interest students in specializing in geriatric MH/SU.
Early Exposure
Many schools give students the option to work with older adults with MH/SU conditions, but the committee did not identify any programs that require students to interact with this population before choosing a specialty area. Medicine has some programs that come close to this by requiring contact with older adults and psychiatric patients. Accredited allopathic medical schools are required to have psychiatry clerkships (Liaison Committee on Medical Education, 2011), but there is no way to know whether students interact with geriatric patients during their rotations. Some medical schools have required geriatric clerkships for fourth-year medical students that include training in MH/SU assessment skills, but as with psychiatry clerkships, it is unclear if these skills are exercised with patients who actually have MH/SU conditions. A number of medical schools have implemented senior mentor programs, where medical students are paired with volunteer mentors over age 65 to meet periodically, discuss aging experiences, and develop personal connections. Evaluations of these programs have found improvements in geriatric competencies and attitudes toward aging, but the older adults in these programs are generally healthy and active, and may or may not have MH/SU conditions (Bernard et al., 2003; Corwin et al., 2006; Eleazer et al., 2006; Hoffman et al., 2006). The committee did not identify programs in other disciplines, such as nursing or social work, that have similar requirements for interacting with older adults and MH/SU consumers.
Lack of Financial Incentives for Practicing in Geriatric MH/SU
A number of factors can influence an individual’s choice to seek additional training in geriatric MH/SU. One of these factors is money, as students consider current costs of education and anticipate future returns on their training. Costs of education include tuition and other direct training costs, but most importantly the opportunity cost of the individual’s time to undertake the training. For example, a psychiatry resident’s opportunity cost for an extra year of geriatric fellowship is the income and experience the resident could have earned by going into practice immediately. While 1 year of practice lost does not seem like much, it is important to consider that the average amount of student debt of 2011 medical school graduates was $118,000, with nearly a third owing over $200,000 (AAMC, 2011). Enhanced competencies may make providers more effective in treating MH/SU conditions of older adults, but current health care payment systems do not recognize or reward the extra skills and knowledge. Psychiatry graduates are becoming less interested in subspecialization (Faulkner et al., 2011). Colenda and colleagues (2005) note that psychiatrists
with geriatric specialty training and general psychiatrists who see a substantial proportion of older adult patients have similar compensation, suggesting there is little reason to seek specialty credentialing.
Not only do financial disincentives detract students from pursuing geriatric MH/SU, but they can also influence credentialed specialists to stop practicing in their subspecialty if they can earn more in general practice. As of 2010, fewer than half of the certificates in geriatric psychiatry earned since 1991 have been maintained (ABPN, 2010a,b). The attrition of trained geriatric providers is an ongoing threat to the general geriatric workforce (IOM, 2008b).
Loan Forgiveness and Scholarships
Providing monetary compensation through loan forgiveness or scholarships is one strategy to defray the most immediate opportunity cost of extra training. Linking training subsidies to service obligations may also potentially mitigate some attrition. South Carolina’s Geriatric Loan Forgiveness Program and California’s Mental Health Social Work Stipend Program are examples of how financial incentives can build and retain the geriatric MH/SU workforce to meet local needs.
In 2005 the South Carolina legislature approved the nation’s first geriatric loan forgiveness program (South Carolina Lieutenant Governor’s Office on Aging, 2011a). The state offers loan repayment for geriatricians or geriatric psychiatrists in exchange for a commitment to practice in South Carolina for 5 years. Physicians must become board certified in a geriatric subspecialty within the first year of the practice, agree to accept Medicare and Medicaid reimbursement, and accept patients regardless of ability to pay. The penalty for not meeting these conditions is substantial. Noncompliant participants must pay the state three times the total reimbursement plus interest at the prime rate plus 10 percent. Applicants are required to sign a statement of intent to continue working in the state after the 5-year commitment. Priority is given to South Carolina natives (those who were born in the state and continue to reside there, or those who have lived in-state for at least 15 years) and those who complete fellowships in South Carolina (South Carolina Lieutenant Governor’s Office on Aging, 2011b). Since 2005, 16 physicians have received loan repayment through this program (South Carolina Lieutenant Governor’s Office on Aging, 2011a), increasing the state’s number of geriatric specialists from 30 to 46 (AARP South Carolina, 2010). Using South Carolina as a model, the American Geriatrics Society has created a toolkit for its other state affiliates to advocate for similar programs in their states (AGS, 2011).
California offers financial support to geriatric social work trainees in its Mental Health Social Work Stipend Program (CalSWEC-Mental
Health). MSW students at 18 participating social work schools may receive a stipend of $18,500 in their second year of training in exchange for a 1-year commitment to working in the state’s community mental health system after graduation. Two of the primary goals of this program are to increase the number of social workers trained in geriatrics, and to create a more culturally competent and diverse social work workforce. From 2005 to 2010, nearly 1,000 students participated in this program; over 50 percent identified themselves as racial/ethnic minorities (CalSWEC, 2011a). Data from 2006 to 2008 show that 55 percent of the students were bilingual (Sirojudin and Jacob, 2009).
Core competencies and teaching resources in community mental health were developed for participating schools, including curricular modules on Specialized Mental Health Interventions with Older Adults, and Co-occurring Disorders (CalSWEC, 2011b). The original cohort was tracked for 2 years after completion of their commitment; 94 percent were still employed in the community mental health system (Sirojudin and Jacob, 2009). A quality-improvement study and 5-year outcomes study are in development (CalSWEC, 2011a). The program is funded by the California Mental Health Services Act of 2005, which approved a new 1 percent tax on income over $1 million to enhance community mental health services. The program has also received support from local foundations.
Limited Opportunities for Specialization in Geriatric MH/SU
The number of specially trained geriatric mental health providers is small in part because there are few ways to pursue specialization in this area. Opportunities are limited for advanced training and for recognition of expertise. As stated earlier, only two mental health professions offer certification in geriatrics: psychiatry and social work. Psychologists, psychiatric nurses, MFTs, mental health counselors, and substance use counselors do not have the option to become certified in older adult care. Though many providers without specialty credentials may have clinical expertise from working with older populations, certification and other modes of formal recognition can ensure more systematic advanced training and bring more widespread attention to the focus area.
Advanced Training Programs
As presented earlier, geriatric psychiatry fellowships have had increasingly high levels of vacancy in recent years. However, this lack of demand for advanced training is not apparent in all mental health professions. Clinical psychology programs that collect admissions data for specific concentrations report that application for the aging track outnumber
available slots by a 6:1 ratio on average (Qualls et al., 2005b). Some prime training opportunities have been eliminated because of waning financial support from outside grants. HRSA’s Bureau of Health Professions (BHP) Graduate Psychology Education (GPE) grants were established in 2002 to fund training for psychologists specializing in integrated care for underserved populations. In 2003, BHP added dedicated funding for geropsychology under the GPE Program. Seven awards totaling $1.8 million were granted, each for a period of 3 years. With GPE funding, psychology departments and training sites were able to create and expand geropsychology training programs. In 2006, GPE funding was cut by over 50 percent, and the geropsychology grants were discontinued (APA, 2012b). Many programs that received funds were negatively impacted when the grants were not renewed. The University of South Florida, University of Illinois at Chicago, and University of Rochester cut the geropsychology training programs they developed with the GPE grant dollars (APA, 2012a; Clay, 2006).
National Certification
Several mental health disciplines have spearheaded efforts to create geriatric certification. The counseling field identified the need for a gerontological counseling specialty beginning in the 1970s. In recognition of the dearth of counselor preparation in serving older adults, the American Counseling Association sought and received five grants from the Administration on Aging to develop aging curriculum and competencies. In the early 1990s, the Council for Accreditation of Counseling and Related Education Programs (CACREP) adopted accreditation standards for gerontological counseling programs, and the National Board of Certified Counselors began to certify gerontological counselors (Meyers, 1995). However, as noted earlier, both program accreditation and certification in gerontological counseling have been discontinued due to lack of interest and participation. In 1995, Myers predicted that without strong national leadership and advocacy, support for counseling programs through the accreditation process, and the development of continuing education opportunities, specialty gerontological counseling would not survive (Meyers, 1995).
While geropsychiatric nursing has been an active field for some time, leaders in the area are now developing a plan for a Geropsychiatric Nursing (GPN) Specialist Certificate Program which, if funded, will define the scope and preparation for specialty practice and credentialing at the graduate/ postgraduate level in line with the new APRN Consensus Model (APRN Consensus Work Group and the National Council of State Boards of Nursing APRN Advisory Committee, 2008). Currently APRNs who prepared
in many different fields find themselves working in areas broadly construed as “geropsych,” such as dementia clinics, nursing homes, primary care settings, geropsychiatric and neurological services, acute care, home care, and so on. Over time, many of these APRNs have developed clinical expertise in a specific focus area, but few have had systematic training in GPN and, thus, have gaps in their knowledge and skill base. The proposed GPN Specialist Certificate Program will address these gaps by developing a model graduate/postgraduate certificate program in geropsychiatric nursing that can serve to further prepare graduates from a range of fields, such as psychiatric-mental health, adult gero primary and acute care, family health, and women’s health, for expert mental health practice with older adults. Expected outcomes include (1) a confirmed set of core GPN competencies, (2) four to six Web-based modules covering core GPN competencies for delivery as academic credit or continuing education, (3) a design for a precepted clinical laboratory experience, (4) a gap analysis procedure to facilitate individualization of the curriculum for each learner, (5) an examination to assess learner mastery of core competencies upon completion of the program, and (6) a development plan for national certification in concert with the American Nurses Credentialing Center and/or other relevant bodies.
Lack of Support and Mentorship
Supporting students and graduates who show an interest in geriatric MH/SU early in their education and career is one strategy to develop professionals dedicated to this specialty area. In the 2011 Association of American Medical Colleges (AAMC) survey of medical school graduates, 77 percent of graduates said their role models had moderate or strong influence on their choice of specialty. Interacting and receiving individualized attention from faculty, professionals, and mentors can show students the variety of opportunities that exist in geriatric MH/SU, and guide them in succeeding in this field. Although most medical schools now have an academic geriatric program, geriatric faculty are devoted primarily to clinical practice, research, and graduate education (Warshaw et al., 2002). Less than 8 percent of geriatric faculty spent time on medical student education. Only 29 percent of baccalaureate nursing programs have a faculty member certified in geriatrics (IOM, 2011).
Early Career Support and Mentorship Programs
Initiatives such as the Geriatric Mental Health Foundation (GMHF) Scholars Fund and the Geriatric Social Work Initiative (GSWI)/John A. Hartford Foundation programs, strive to encourage students and early-
career professionals who are interested in aging to orient their careers toward the older adult population by providing financial assistance and mentorship.
The American Association of Geriatric Psychiatrists (AAGP) created the GMHF Scholars Fund to attract medical students and psychiatry residents to the specialty via mentorship and education. The program provides free AAGP membership, one-on-one mentorship, a structured Scholars Program at the AAGP annual meeting, and travel expenses to attend the annual meeting. For medical students, the Scholars Program is designed to build interest in geriatric psychiatry by presenting various options for clinical and research opportunities available in medical school and residencies. Psychiatry residents go through a different program that offers more detail about the practice of geriatric psychiatry, and showcases geriatric fellowship opportunities. The Scholars Fund is supported by donations and grants. The program received over $50,000 for the 2012 cycle, $35,000 in 2011, and $18,000 in 2010 (AAGP, 2011). The current budget can support about 20 scholars. GMHF reports that nearly 75 percent of scholars go on to specialized geriatric fellowships (AAGP, 2011).
GSWI of the John A. Hartford Foundation collaborates with social work programs, organizations, and other funders around the country to prepare social workers to improve the care and well-being of older adults and their families. In 2005, the Foundation, in collaboration with the Gerontological Society of America (GSA), began a predissertation award program for doctoral students in social work. The objectives of the program were to expose students to gerontological social work research and to encourage them to advance the field of gerontological social work practice. The award provided travel expenses and registration to the GSA Annual Meeting, sessions at the GSA meeting on research and grant writing, free membership in GSA and the Association for Gerontology Education in Social Work, and networking opportunities with Hartford Doctoral Fellows and Hartford Faculty Scholars. The Hartford Foundation encouraged predissertation awardees to apply for the Hartford Doctoral Fellows program in the next phase of their academic career. The doctoral fellows program granted students up to $50,000 over 2 years to complete a dissertation related to social work and older adults, and provides additional professional development opportunities. Eighty predissertation awards were given out from 2005 to 2009 (Geriatric Social Work Initiative, 2012). The Association for Gerontology Education in Social Work adopted the program and funded 20 students from 2010 to 2011, with plans to fund 10 more in 2012 (AGESW, 2011).
Early career programs geared toward encouraging new scholars in the field of geriatric social work have also included the Doctoral Fellows Program in Geriatric Social Work and the Geriatric Social Work Scholars program, both sponsored by the John A. Hartford Foundation and GSA.
The programs fostered an intellectually stimulating, mutually supportive network of peers and colleagues involved in research and teaching in geriatric social work. Based on the integrated components of mentoring, career development, and networking, these programs have sponsored 117 faculty scholars and 104 doctoral fellows, but were recently discontinued due to financial constraints.
Difficulty Recruiting Minorities to Geriatric MH/SU
One study of medical students found that white students were three times as likely to indicate interest in geriatrics than minority peers (Voogt et al., 2008). Furthermore, fewer African American, Hispanic, and Native American students earn college and graduate degrees than their white peers (Aud et al., 2012), potentially limiting the pipeline of minority students for geriatric MH/SU specialties.
The committee did not identify any programs that specifically recruit minority students to geriatric MH/SU practice, although many initiatives recruit minority students to MH/SU professions in general. For example, in FY 2011 the Substance Abuse and Mental Health Services Administration provided $4.7 million in minority fellowship program grants to the American Nurses Association, American Psychiatric Association, American Psychological Association, Council on Social Work Education, and American Association for Marriage and Family Therapy to use over 3 years (SAMHSA, 2011b). The purpose of the minority fellowship programs is to increase the number of culturally competent and diverse MH/SU providers prepared to serve disadvantaged populations (SAMHSA, 2011a). For example, in social work the Council on Social Work Education Mental Health/Substance Abuse Fellowship Program has existed since the early 1970s, and is designed to increase the number of racial and ethnic minorities with doctoral degrees in social work education who can provide leadership in the planning and evaluation of culturally competent mental health and substance abuse programs.
One program previously existed to recruit minority researchers to this field. From 2003 to 2008, the National Institute of Mental Health operated the Institute for Research Minority Training on Mental Health and Aging to engage more minority early investigators in geriatric MH/SU research. Over 5 years, the program trained 10 participants. However, the program could not secure funding necessary to continue (Bartels et al., 2010).
INADEQUATE PREPARATION OF THE
GERIATRIC MH/SU WORKFORCE
While geriatric MH/SU specialists are critical in caring for older adults with MH/SU, the more broadly defined geriatric MH/SU work-
force has far greater contact with older adults who have or may be at risk for MH/SU conditions. Aside from geriatric MH/SU specialists, the remainder of the geriatric MH/SU workforce is somewhat arbitrarily defined. However, the committee believes that all professions that provide services to older adults for the assessment, diagnosis, treatment, management, or care of MH/SU conditions are part of the geriatric MH/SU workforce and should be prepared for this role.
The review of the workforce found many gaps in geriatric MH/SU training across most professions. As is evident from examining the table of required competencies in Appendix C, most providers who are not geriatric MH/SU specialists are required to have little knowledge or experiential training in mental health or substance use as related to older adults. Few students are explicitly required to understand the presentation or treatment of comorbid MH/SU conditions. Some professions barely require any learning in MH/SU or aging in general.
TRAINING THE GERIATRIC MH/SU WORKFORCE
General providers at all levels should be aware of the signs and symptoms of MH/SU conditions and be able to respond appropriately within their level of training and scope of practice. However, few professions have mandated curricular standards related to MH/SU in geriatric patients. Although curricula exist, clarity is needed in how and to what extent the concepts are applied in the classroom or in practical training. The prevalence of co-occurring conditions in the elderly and the shift toward collaborative models of care make interprofessional training essential to overall training in geriatric MH/SU care. The increasing racial, ethnic, and linguistic diversity of the geriatric population also makes cultural competence imperative. To what extent these aspects of care are being integrated into training and education is also unclear. These key areas of training are summarized in Box 3-4.
BOX 3-4
Key Areas for Improving Training
• Integrating geriatric mental health and substance use competencies into education for all health professionals
• Training for existing providers
• Training in cultural competency
• Interprofessional training
Several professional groups, schools, and other entities have developed or are working to develop tools to improve geriatric MH/SU skills and competencies in the nonspecialist workforce. These efforts are described in this section. As stated in the earlier discussion on recruitment, inclusion of an initiative in this chapter does not represent an endorsement from the committee because evidence to support the effectiveness or analyze the outcomes is often not available.
Integrating Geriatric MH/SU Competencies into
Education for All Health Professionals
The development and integration of core competencies in health care education and training have increased with the recognition that critical skills, knowledge, and attitudes must be more precisely defined for more consistent advancement of the field. Significant efforts have been made to develop geriatric MH/SU competencies and to integrate these competencies into education and training programs.
The Geropsychiatric Nursing Collaborative (GPNC) started in 2008 with funding from the John A. Hartford Foundation (AAN, 2010). Its goal is to improve the quality of mental health care provided to older adults by enhancing the knowledge and skills of nurses. One of the GPNC’s primary goals is to develop geropsychiatric core competencies for entry-level and advanced practice nurses. The competencies were developed to enhance current nursing curriculum for both generalist and specialist nurses. The GPNC created competency enhancements for the following audiences: entry-level nurses, gerontological clinical nurse specialists (CNSs), gerontological NPs, older adult care CNSs (CNSs who care for older adults, but are not specialized), older adult care NPs (NPs who care for older adults, but are not specialized), psychiatric mental health CNSs, and psychiatric mental health NPs. All competency enhancements cover key concepts in assessment, management, approach to older adults, and nursing roles (Box 3-5). The competency enhancements have been endorsed by 12 other nursing organizations. The GPNC posted these competency sets, along with other geriatric nursing resources, on the Portal of Online Geriatric Education (POGOe) website.10 Deans of every school of nursing were notified about these new resources (Beck et al., 2011).
Professional geropsychology has adopted a competency-based model of training, the Pikes Peak Model for Training in Professional Geropsychology (Knight et al., 2009). It delineates attitude, knowledge, and skill competencies for geropsychology practice and acknowledges that there are multiple pathways to geropsychology competence. The Pikes Peak
____________
10 See http://www.pogoe.org.
BOX 3-5
Geropsychiatric Nursing Key Concepts
I. Assessment
a. Normal aging: biopsychosocial theories
b. Appropriate instruments/clinical evaluation tools
c. Adapted assessment procedures
d. Atypical presentations, co-occurring illness, psychiatric manifestations, medical conditions
e. Common disorders
f. Comprehensive assessments
g. Stressors affecting mental health
II. Management
a. Care transitions
b. Behavioral, environmental, and pharmacological interventions and communication for behaviors
c. Pharmacotherapeutics
d. Referrals
e. Influences from decisional capacity, health literacy
f. Patient/family/peer education: mental and physical health interactions
g. Ethical/legal and socioeconomic factors
Model builds on the APA Guidelines for Psychological Practice with Older Adults (APA, 2004) by laying out more specific goals for training. The competencies are aspirational in nature and are intended to guide entry-level psychologists with specialized practice with older adults. The Council of Professional Geropsychology Training Programs created the Pikes Peak Geropsychology Knowledge and Skill Assessment Tool for supervisors to assess trainees or for psychologists who wish to do a self-assessment (Karel et al., 2010a). The assessment tool rates the psychologist as novice, intermediate, advanced, proficient, or expert in each of the competencies outlined in the Pikes Peak Model. The tool enables supervisors and learners to identify strengths, areas for growth, and goals for training and education.
III. Approach to Older Adults
a. Age-related adaptations
b. Age/culturally appropriate interventions and communications
c. Recognition of personal and societal biases
d. Sensitivity in end-of-life care
IV. Role
a. Promotion of safety and risk factor reduction
b. Knowledge of geriatric mental health/illness
c. Lifelong learning
d. Policy/advocacy
e. Research participation/use
f. Quality-improvement initiatives
g. Interdisciplinarity
h. Delivery systems
i. Service barriers
SOURCE: POGOe, 2010.
Disseminating Training Resources
Once core competencies are identified, the challenge remains of integrating the skills and knowledge into classes and training courses. Some professions are developing and disseminating tools that instructors can use to infuse geriatric MH/SU into their curriculum. The geriatric MH/SU teaching tools from the Council on Social Work Education (CSWE) and the Hartford Institute for Geriatric Nursing are evidence based, free, and include supporting materials to simplify the use of them. The NASW also offers professional development courses on aging, substance abuse, and related topics online, including webinars, for a cost or free of charge (NASW, 2012).
The CSWE Gero-ed Center, funded by the John A. Hartford Foundation, was created with the mission of promoting gerontological competencies in social work. The Gero Innovations Grant (GIG) was one part of the
Master’s Advanced Curriculum Project, which ran from 2007 to 2010 with the goal of enhancing advanced specialty training in older adult health, mental health, and substance abuse. From 2007 to 2009, the GIG provided funding to 14 MSW programs to develop and evaluate teaching tools and strategies for social work in gerontological health, mental health, and substance abuse. All but one of the grantees developed teaching modules related to mental health or substance use. The teaching modules cover diverse topics, including depression, anxiety, paranoia, mental health in older Latinos, polypharmacy, mental health in skilled nursing facilities, informal sources of mental health care in Native American traditions, and co-occurring MH/SU conditions. All of the modules are posted on the CSWE Gero-Ed Center website,11 along with supporting materials such as lecture slides, videos, instructor scripts, course reading lists, vignettes, and case studies.
The Hartford Institute for Geriatric Nursing at the New York University College of Nursing has created a series of guides to best practices and assessment tools relevant to the care of geriatric patients. The “Try This” series has several tools related to MH/SU, including the Geriatric Depression Scale in English and Spanish, alcohol use screening and assessment, and the Horowitz Impact of Event Scale for posttraumatic stress. There are other tools that are not specifically related to MH/SU, but that are highly relevant to caring for older patients with MH/SU conditions, such as the Beers Criteria for Potentially Inappropriate Medication Use in the Elderly, the Transitional Care Model criteria for hospital discharge screening for high-risk older adults, and the Preparedness for Caregiving Scale. The assessments are intended to be simple, requiring less than 20 minutes to administer. The material is contained within a two-page brief, with background information on the issue; an explanation of the assessment’s validity, strengths, and limitations; and a list of additional resources. Most assessments in the series are also accompanied by a longer “How to Try This” article from the American Journal of Nursing that provides case studies for more nuanced instruction, and a video that demonstrates how to administer the tool. The entire series is available for free on the Web,12 and may be reproduced for educational purposes without fee.
Integrating Geriatric MH/SU Competencies in Education
The GeriEd Program at the Albert Einstein College of Medicine (AECOM) is one program that uses classroom and clinical lessons to
____________
11 See http://www.cswe.org/CentersInitiatives/GeroEdCenter.aspx.
expose undergraduate medical students to geriatric issues, including MH/SU, before they choose a specialty. The first- and second-year curricula weave geriatric content into small-group lectures and workshops on the patient. In the first year, 15 to 20 students are assigned to a geriatric practicum to begin learning clinical interviewing skills. The geriatric program, which has been offered since 2002, focuses on the mental status exam, social and functional history, and palliative care. Students work in multidisciplinary teams across various clinical settings, including outpatient, home care, and long-term care. The clinical experiences are paired with group sessions that cover topics such as depression, dementia, and chronic illness. Students in the geriatric program can continue their learning by monitoring community-dwelling patients on an ongoing basis. In the third and fourth year, all students are required to do a 2-week clerkship in geriatrics, which includes training in assessing and managing depression. This clerkship has been required at AECOM since 1995 (Ehrlich and Jacobs, 2004).
AECOM received a $100,000 grant in 2001 from the AAMC and the Hartford Foundation to fully integrate geriatric content into relevant areas throughout undergraduate medical education. From 2006 to 2010, the Donald W. Reynolds Foundation gave AECOM nearly $2 million toward the innovative integration of geriatrics into training activities. The AAMC/Hartford Foundation and the Reynolds Foundation grant programs each gave similar awards to 39 other medical schools (AAMC, 2003; Donald W. Reynolds Foundation, 2011).
Training the Existing Health Care Workforce
in Geriatric MH/SU Issues
While improving formal education is crucial to improving the workforce’s competence in geriatric MH/SU, there is a large existing workforce that must be trained as well. Strengthening the geriatric MH/SU workforce requires reaching providers of all types throughout their careers. This can be done through several methods, including in-service training and continuing education.
In-Service Training
One example of geriatric mental health in-service training is a program called Training in the Assessment of Depression (TRIAD). TRIAD is a brief intervention that improves the ability of home care nurses to identify depression symptoms in older adults and make appropriate referrals. This intervention was developed by Bruce and colleagues (2007) in collaboration with three home care agencies, and tested in a randomized
controlled trial with 53 home care RNs. The intervention used the depression portion of the Outcome and Assessment Information Set (OASIS) because this information is already required by Medicare and would not overburden the workload of nurses. OASIS requires nurses to document signs of depressions, but does not provide guidance on identifying symptoms. The intervention trained nurses in observing behavioral and nonverbal signs that could indicate depression, understanding conditions that can complicate depression assessment, and asking follow-up questions to determine the persistence and severity of symptoms. The training took place over two sessions, totaling 4.5 hours, and included didactic instruction, role playing, and watching demonstration videos. Bruce and colleagues found that training increased the rate of depression referrals, without increasing false-positive referrals, and that referred patients had better clinical outcomes than patients who were not referred.
To disseminate this training, TRIAD has been adapted into a Web-based learning module, called Depression Recognition and Assessment in Older Homecare Patients (Weill Medical College of Cornell University, 2004). It includes training on identifying and assessing depression, recognizing and handling suicide ideation, and making a referral. Users may also download Weill Cornell’s Depression Screening Toolkit (Weill Cornell Homecare Research Partnership, 2004).
Continuing Education
Most licensed professions require practitioners to receive continuing education each year to build competency and promote professional growth. For providers who may have received little training or education in school about geriatric MH/SU, continuing education is one possible way to gain this knowledge. Boston University’s Institute for Geriatric Social Work has numerous online training courses that provide continuing education credits for social workers. Topics include geriatric assessment, mental health and aging, substance abuse, compulsive hoarding, suicide prevention, among many others relevant to geriatric MH/SU. Social workers can take these online training courses to earn a certificate in Mental Health and Aging, which requires six courses (Boston University Institute for Geriatric Social Work, 2011).
University of Washington also offers several types of continuing education opportunities related to geriatric MH/SU. For example, existing providers may enroll in courses such as diagnosing and treating older adults with chronic mental illnesses, mood and thought disorders in older adults, and the psychology of aging. The courses are generally held weekly over an academic quarter, in a downtown classroom. Providers may also pursue a certificate in geriatric mental health by enrolling
in a five-course program that lasts 12 to 24 months. The University of Washington geriatric MH/SU continuing education programs are geared toward an array of professionals, including social workers, mental health counselors, marriage and family therapists, and psychologists (University of Washington Professional and Continuing Education, 2012).
Training in Cultural Competency
The Stanford Geriatric Education Center (SGEC), a collaborative project from Stanford University School of Medicine, San Jose State University, Community Health Partnership, and Santa Clara County Mental Health Department, specializes in developing and providing multidisciplinary training in geriatric care for ethnic minorities. The SGEC offers training through several different media. It holds monthly webinars on clinical ethnogeriatric topics, including depression and mental health, which physicians, nurses, psychologists, social workers, or MFTs may use for continuing education credit. The SGEC also offers a 10-module curriculum for teaching culturally appropriate depression and dementia care for older adults at risk for diabetes. Instructors may download a handbook and Power Point slides for each module. The curriculum provides in-depth discussions of depression, dementia, and diabetes in African Americans, American Indians, Chinese Americans, Filipino Americans, Hmong Americans, Japanese Americans, and Mexican Americans. The SGEC and OnLok Senior Health, a local senior service organization, developed Diversity, Healing, and Health Care, a unique Web-based resource for clinicians who see older patients from diverse backgrounds. The website is a quick-reference source on ethnicity, religion, and age, so that clinicians can have a baseline context for interacting with patients. Information includes greetings and introductions in various languages, cultural attitudes about illness and disability, religious customs at time of death, and major cohort life events (see Table 3-3).
Interprofessional Training
Competencies in interdisciplinary care have been developed and endorsed by many professional education groups, including the Accreditation Council for Graduate Medical Education, American Association of Colleges of Nursing, American Geriatrics Society, American Psychological Association, American Society of Consultant Pharmacists, and Council on Social Work Education, among other professional groups. The Interprofessional Education Collaborative, a joint effort among schools of allopathic and osteopathic medicine, nursing, dentistry, pharmacy, and public health, recently published core competencies for interprofessional
TABLE 3-3
Example of a Cultural Competence Tool: Korean American Life Cohort Events
| Years | Historical Events Experienced by Korean American Elders | Current Age of Older Adult | |||
| 55-65 Years | 65-75 Years | 75-85 Years | 85+ Years | ||
| Life Stage at Time of Event | |||||
| 1980-present | Increased fractionalization among Koreans Post–Rodney King decision focuses on Korean Americans Number of women continues to outnumber men Continued population influx: 1980 population was 354,600; 1990 population exceeded 800,000 |
Young adults, middle aged | Middle aged, Young-old | Young-old, old | Old |
| 1970s | Influx of Koreans after the Immigration and Nationality Act of 1965 Women continue to outnumber men, 10:7 Educated, middle-class immigrants Stereotypes: liquor store operators and green grocers Korean towns emerge in urban areas |
Adolescents, young adults | Young adults, middle aged | Middle aged, young-old | Young-old, old |
| 1940-1960 | Slow move out of Chinatowns Awareness of war brides and orphans as fallout from Korean War Population change, more women to men, 10:7 1950-1953 Korean War; war brides and war orphans |
Children, adolescents | Adolescents, young adults | Young adults, middle aged | Middle aged, young-old |
| 1920-1940 | Lived in rural areas and Chinatowns Lumped with Asian groups as “Oriental” Some families, and small communities in Hawaii and California Population was 4 men for each woman 1924 Immigration Act stops picture brides |
Children | Children, adolescents | Adolescents, young adults | Young adults, middle aged |
| 1900-1920 | Laborers moved to West Coast of United States 1906—beginning of picture brides Immigrants were 10 men for each woman 1902—immigration to Hawaii |
— | Children | Children, adolescents | Adolescents, young adults |
| Pre-1900 | Limited information about immigration to the United States is available; numbers of immigrants few or none | — | — | Children | Children, adolescents |
SOURCE: Adapted from Stanford Geriatric Education Center, 2004.
education, delineating what this concept means in practice and what this training should accomplish (Interprofessional Education Collaborative Expert Panel, 2011).
Geropsychology training emphasizes interdisciplinary practice and competence in providing a broad range of services to older adults (Karel et al., 2010b). These include (1) assessment of psychological, intellectual, cognitive, functional, personality, emotional, and decision-making capacity; (2) psychological, psycho-educational, behavioral, cognitive rehabilitation, and pain management interventions, end-of-life care, and grief work; (3) consultation to primary care providers, long-term care settings, health and social service agencies, family members and primary caregivers, and attorneys and other legal system personnel; and (4) supervision and management of direct caregivers, interdisciplinary teams, programs, and agencies caring for the elderly.
In response to the 2008 IOM report Retooling for an Aging America: Building the Health Care Workforce, 21 health care provider organizations formed a coalition called the Partnership for Health in Aging (PHA). The PHA created Multidisciplinary Competencies in the Care of Older Adults at the Completion of the Entry-Level Health Professional Degree (Partnership for Health in Aging, 2010), which identified 23 competencies within 6 domains as essential for the following health professionals: physicians, dentists, nurses, occupational therapists, pharmacists, physical therapists, physician assistants, psychologists, and social workers. The competency domains are health promotion and safety, evaluation and assessment, care planning and coordination across the care spectrum (including end-of-life care), interdisciplinary and team care, caregiver support, and health care system and benefits. This effort did not address competency-based training for DCWs, but the domain of interdisciplinary and team care states that upon completion of the entry-level degree, health professionals should know and be able to demonstrate how to “communicate and collaborate with older adults, their caregivers, other health care professionals, and direct care workers to incorporate discipline-specific information into overall team care planning and implementation” (Partnership for Health in Aging, 2010, p. 2). The competencies are not centered on mental health in aging, but this interdisciplinary effort is a step toward improving geriatric MH/SU care because older adults with MH/SU conditions often see a constellation of providers because of other health concerns. Mental health is included in three of the six domains, in reference to health interventions, appropriate assessment, and advanced care planning.
The Geriatric Education Centers (GECs), funded through grants from HRSA, are collaborative arrangements that bring different health professionals together for training in geriatric care. To receive a grant, a GEC must offer interdisciplinary education that involves at least four
health professions. The disciplines may include allopathic or osteopathic medicine, dentistry, optometry, podiatry, pharmacy, nursing, physician assistant practice, chiropractic, clinical psychology, health administration, allied health professions, professional counseling, and social work.
PROMOTING THE ROLE OF DIRECT CARE
WORKERS IN GERIATRIC MH/SU CARE
DCWs are involved in the care of many older adults with MH/SU conditions. The demand for direct care services is growing with the aging population, yet the growth of this workforce is not keeping pace (Stone and Urban Institute Staff, 2011). The low professional status of DCWs and limited opportunities for growth in this field make it difficult to attract and retain a quality workforce. Most professions are recognized through credentials, such as certificates, licenses, and degrees, that verify an individual has received training and is able to perform the duties required of the profession. As discussed in the review of the direct care workforce, credentialing for direct care workers is limited. Recognition and growth of this profession will require a higher, more consistent level of training. Currently there are few advancement opportunities, or incentives to invest in such opportunities, for DCWs who excel in their work or wish to get more training in their profession. This section will discuss strategies for training DCWs and promoting their role in geriatric MH/SU care.
Training in Geriatric MH/SU
DCWs who have received special training in working with older adults and others with MH/SU disorders have been shown to provide better care for clients with these conditions. However, few direct care workers receive such training in the normal course of employment. Analysis of human capital investment, based on Becker (1962) and the stream of literature that followed this seminal work, suggests that employers do not benefit from providing general training that is transferrable to other settings because trained workers could leave for higher pay elsewhere. A result of this low investment in training is that employers do not have an incentive to increase wages or benefits in order to retain workers.
The lack of training at the organizational level is undoubtedly reinforced by the lack of national standards for this occupation. National requirements for training only exist for certain types of DCWs in specific settings, leaving a great number of DCWs for whom no consistent standards apply. Where standards exist, training requirements for DCWs tend to be minimal in hours and in content, with little included on MH/SU issues. While some groups, such as the Direct Care Alliance, the Paraprofessional
Healthcare Institute (PHI), and the National Association for Home Care and Hospice, have created DCW training programs, there are few initiatives to improve older adult MH/SU care training, even though DCWs play a prominent role in long-term care and home care, where older adults are primary recipients of services.
In 2010 the state of Alaska formed a public-private collaborative to address the challenge of training DCWs. It created the Alaskan Core Competencies for Direct Care Workers in Health and Human Services, a set of competencies relevant across diverse health care sectors that include long-term care, mental health, addictions, developmental disabilities, and traumatic brain injury. The competencies can be used to develop training content for initial or continuing education, update existing curricula, or assess employee competencies. To assist organizations in using the competencies, a companion toolkit for assessing worker competencies was released in 2011. A curriculum for the competencies has been piloted with DCWs, including those from long-term care, and is scheduled for release in 2012.
This initiative has been funded by the Alaska Mental Health Trust Authority and the Alaska Department of Health and Social Services. The competencies, assessment tools, and curriculum have been developed by the Western Interstate Commission for Higher Education Mental Health Program and the Annapolis Coalition on the Behavioral Health Workforce, with oversight from a committee of Alaskans. A project description and the work products are available for review at http://www.annapolis coalition.org/core_competencies.aspx.
The Affordable Care Act authorized, and Congress appropriated funds for a 2-year demonstration in core competency training for personal and home care aides (the Personal and Home Care Aide State Training Program or PHCAST).13 Six states—California, Iowa, Maine, Massachusetts, Michigan, and North Carolina—were awarded funds to develop and evaluate core competencies, pilot training curricula, and certification programs for personal and home care aides. Although, the grantees are not required to include core competencies in MH/SU, Maine’s program includes the development of a specialized training track to help prepare individuals to become mental health rehabilitation technicians. Michigan’s program includes in-service continuing education training that focuses on critical topics, including the management of behavior issues in people with dementia.
____________
13 Public Law 111-148.
Professional Recognition of Competency in Geriatric MH/SU Care
As discussed in the review of the DCW workforce, there are currently few ways for DCWs to earn recognition for their skill, competency, and experience. DCWs are typically paid low entry wages that do not rise substantially with experience, either with tenure in one job or tenure in the occupation. Squillace and colleagues found “years of experience do not translate into higher wages; CNAs with 10 or more years of experience averaged just $2/hr more than aides who started working in the field less than 1 year ago” (Squillace et al., 2009, p. 185).
DCWs do not have a strong incentive to seek extra training, knowledge, or skills because their training and experience are often not certified at all. Where certification exists, it represents a very minimal standard rather than a level of achievement, such as in the case of the 75 hours of experience mandated for certified nursing assistants working in Medicare-and Medicaid-certified nursing homes. Additional training for DCWs is rarely available except through special grants and initiatives (Eaton et al., 2001; Harmuth and Konrad, 2010; Wilson et al., 2003). With basic training and recognition being so rarely obtained, recognition of competence in a specialty area such as MH/SU is even further off.
The state of California has had a well-established workforce of licensed MH/SU DCWs, called psychiatric technicians, for decades, and demonstrates a successful movement in professionalization of a historically devalued occupation. Psychiatric technicians are licensed by the Board of Vocational Nursing and Psychiatric Technicians, and are considered to be of similar skill level to LVNs. As of 2008 there are approximately 14,000 psychiatric technicians in California. They are employed by hospitals, correctional facilities, psychiatric emergency response teams, residential treatment programs, and many other settings where psychiatric services are needed. The state accredits psychiatric technician education programs and requires 576 hours of didactic learning and 954 hours of supervised clinical experience. Curriculum must include learning in gerontological nursing. Psychiatric technicians must complete 30 hours of continuing education every 2 years to maintain licensure.
The professional recognition of psychiatric technicians emerged from advocacy efforts of psychiatric “attendants” and “aides” from state mental institutions who organized into the California Society of Psychiatric Technicians in 1950. In 1951, California added psychiatric technician as a state civil service classification, which created specific minimum requirements for entry into the field. Because more psychiatric technicians were emerging in settings that were not run by the state, California created an exam that could be used to establish the eligibility of any psychiatric technician. This development eventually led the state to develop a professional license for this occupation in 1970. The California Association of
Psychiatric Technicians, which serves both as a union for state employees and as a professional organization for all psychiatric technicians, has since advocated for additional advancements in the profession. In 1989, legislation passed requiring continuing education and license renewal for psychiatric technicians. Since 1998, psychiatric technicians have been allowed to draw blood and administer hypodermic injections after receiving additional training. California is one of three states to license psychiatric technicians. The others are Colorado and Kansas. Arkansas licensed psychiatric technicians at one time, but stopped in 2009.
Several states offer DCW development initiatives, some of which include opportunities for specific training in working with older adults with MH/SU conditions. For example, the state of Iowa created a Direct Care Workforce Advisory Council that is mandated with collecting data on the DCW workforce, implementing a HRSA grant-funded pilot training and credentialing program, and making recommendations for advancing this workforce. The Council has recommended a structure of core training, advanced training, and specialty endorsement, with each level conferring an additional level of credentialing. Specialty endorsements would be created by experts in the subject area and approved by the state. Proposed areas of specialization include MH/SU-related areas, including Alzheimer’s/dementia, mental health, positive behavior support, and psychiatric care. As of March 2012, Iowa is proposing legislation to license DCWs. The legislation follows the recommendations of the Advisory Council and would require the development of statewide curriculum standards and licensing requirements, with opportunities for advancement and specialization (Ozga, 2012).
EMPOWERING OLDER ADULTS AND THEIR FAMILIES
On a day-to-day basis, consumers and families carry far more responsibility for older adult MH/SU care than any professional group. Family caregiving, self-care, and peer support play a large role in the health and well-being of older adults with MH/SU conditions, whether these activities are formally organized or not. Supporting consumers in being active participants in their health is a critical aspect of patient-centered care (see Box 3-6). The President’s New Freedom Commission report, the Surgeon General’s report on mental health, and the IOM’s Improving the Quality of Health Care for Mental and Substance-Use Conditions report have all called for more consumer and family involvement in the process of care in order to improve outcomes and experiences for both consumers and families (Hogan, 2003; IOM, 2006; SAMHSA, 1999).
BOX 3-6
Rules for Patient-Centered Care
Customization based on patient needs and values: The system of care should be designed to meet the most common types of needs, but have the capability to respond to individual patient choices and preferences.
The patient as the source of control: Patients should be given the necessary information and the opportunity to exercise the degree of control they choose over health care decisions that affect them. The health system should be able to accommodate differences in patient preferences and encourage shared decision making.
Shared knowledge and the free flow of information: Patients should have unfettered access to their own medical information and to clinical knowledge. Clinicians and patients should communicate effectively and share information.
The need for transparency: The health care system should make available to patients and their families information that allows them to make informed decisions when selecting a health plan, hospital, or clinical practice, or choosing among alternative treatments. This should include information describing the system’s performance on safety, evidence-based practice, and patient satisfaction.
Anticipation of needs: The health system should anticipate patient needs, rather than simply reacting to events.
SOURCE: IOM, 2001.
Expanding Peer-Led Support Programs for Older Adults
The demand for more consumer-led, recovery-oriented services has increased in past decades and continues to grow, and evidence supporting the benefits of these services is emerging.14 However, information on the availability and impact of MH/SU peer support for older adults is sparse, although some noteworthy programs provide consumer-oriented, peerled
____________
14 See Box 4-1 (in Chapter 4) for a description of recent trends in peer support.
MH/SU support to older adults, including programs associated with larger establishments like Alcoholics Anonymous (AA) and the VHA.
Seniors in Sobriety (SIS) is a coalition of AA members who are concerned with spreading the message of sobriety to older adult alcoholics (SIS, 2012). SIS, originally called Sober over Sixty, began in 1990 in southeastern New York (SIS, 2012). The reach of SIS has grown, as more communities recognize the unique concerns of older adult alcoholics. According to the 2004 AA Membership Survey, 16 percent of AA members are over age 60, and 23 percent are ages 51 through 60 (Alcoholics Anonymous, 2008). Communities in Hawaii, mid-southern California, and Arizona have established standing Cooperation with the Elder Community committees to work on service and outreach to older adult alcoholics. Nearly 30 groups across 11 states and one Canadian province have started AA meetings for seniors in places of worship, senior centers, retirement homes, and other senior-oriented settings.
Vet-to-Vet is a peer-led support program for veterans with serious mental illnesses. Vet-to-Vet follows a consumer-professional partnership model, where groups are separate from formal VA medical services, but peer leaders work in close consultation with mental health professionals (Resnick et al., 2004). Many Vet-to-Vet groups are physically located at VA centers to maximize accessibility for participants and to facilitate consultation between consumer providers and mental health professionals, though the program has been adopted in non-VA community settings as well (Barber et al., 2008). A 2008 nationwide survey of Vet-to-Vet participants from 38 sites found that over 40 percent of participants were black or Latino, and 90 percent were men (Barber et al., 2008). While Vet-to-Vet is inclusive of all veterans and does not target older adults, the average age of participants is 53 (Barber et al., 2008). In a study of Vet-to-Vet attendance indicators, Resnick found that older age, more negative attitudes toward recovery, and lower levels of functioning were positively correlated with more frequent attendance, suggesting that this peer support model reaches veterans who may otherwise not typically access peer support services (Resnick, 2010).
Providing Physical, Financial, and Psychosocial Support for Families
Few family caregivers are trained to take on these roles even though the burden can be heavy. Family caregivers are at high risk for depression. A study of over 5,500 caregivers of people with dementia found that 32 percent met criteria for depression. Caregivers of people with behavioral disturbances, such as angry or aggressive behavior, and those who spent more time caregiving were more likely to experience depression (Covinsky et al., 2003). Caregiving also can cause financial strain when
individuals quit their job or reduce their hours to fulfill their caregiving duties. Approximately 42 percent have less than $50,000 in household income. Caregivers also tend to have family obligations outside of tending to their sick relative. The majority are married, and more than one-third have children or grandchildren under age 18 in the household (National Alliance for Caregiving and AARP, 2009). Data on caregivers who specifically care for older adults with MH/SU conditions are limited.
Training and education for family caregivers and providing a supportive environment to talk have shown encouraging results. In a review of family psychoeducation as an intervention for serious mental illnesses, McFarlane et al. (2003) found more than 30 randomized trials with positive outcomes for patient recovery and family well-being. While more research is needed to explore the efficacy of different modes of psychoeducation delivery, McFarlane and colleagues concluded that support, information, guidance, and sharing of burden are the most critical aspects of family education. The CMS Leadership Summit on the Direct Care Workforce and Family Caregivers recommends that training for family caregivers should be flexible, optional, accessible, “just in time,” self-paced, and customized to meet the needs of individual caregivers and people receiving care (Direct Service Workforce Resource Center, 2011).
Many state organizations and local affiliates of the National Alliance for Mental Illness (NAMI) have adapted programs or started other programs to meet the needs of their communities’ consumers and families. NAMI New Hampshire (NAMI NH) created a program specifically for older adults with mental illness, their families and caregivers, called Side-by-Side for Independent Living (NAMI New Hampshire, 2012). Side-by-Side is an educational workshop series with nine parts: (1) meeting caregiver needs, (2) navigating the health system, (3) depression and suicide, (4) mental health issues, (5) substance abuse and misuse, (6) understanding dementia, (7) challenging behaviors, (8) legal issues, and (9) wellness and healthy living. Each session consists of 1 hour of educational material and 1 hour of discussion. NAMI NH has partnered with hospitals, senior centers, assisted living facilities, community mental health centers, and adult day programs to bring Side-by-Side to groups most likely to benefit from this information. In some communities, NAMI NH has partnered with major employers to offer workshops onsite during lunch hour to reach caregivers who may not be able to attend classes at other times. Training can be offered as a series or as individual modules to maximize flexibility and meet specific needs. In evaluations of the program, 95 percent of over 400 program participants reported being more aware of supports related to mental illness in older adults, and/or for caregiver issues (NAMI New Hampshire, 2010).
Taking time away from caregiving is critical for family caregivers.
Since 2009, the U.S. Administration on Aging has provided funding to 24 states to implement State Lifespan Respite Programs, which are designed to help families find respite providers and access respite payment resources (AoA, 2010).
Addressing the Needs of Diverse Populations
Providing culturally competent care is critical to reaching older adults with MH/SU conditions. In the case of depressive illness, older minorities with depression report higher impairment levels and are more persistently ill than non-Hispanic, white older adults (Brown et al., 1996; Williams et al., 2007), yet they also report decreased rates of mental health care (Alegria et al., 2008). For example, among Medicare beneficiaries, Latinos are approximately only half as likely as others to receive treatment for depression and are the least likely to be treated using psychotherapy (Crystal et al., 2003).
The diverse needs of the family caregiver mirror those of the consumer. Some studies have shown that caregiver depression rates may differ among racial groups. For example, African American caregivers report lower levels of burden than white caregivers (Janevic and Connell, 2001), while Hispanic caregivers experience high levels of depression and burden (Magaña et al., 2007; Pinquart and Sorensen, 2005). Differences in level of burden may be due to specific cultural values, their influences on how stress is perceived, and what coping techniques are employed, as well as issues related to perception of burden within and among subgroups of family caregivers (Adams et al., 2002; Aranda and Knight, 1997; Knight and Sayegh, 2010). Effectively reaching caregivers from diverse populations requires understanding of these specific cultural norms and developing culturally and linguistically relevant services (Aranda et al., 2003; Chadiha et al., 2006).
Engaging older consumers and families from minority populations is a unique challenge that is currently not widely addressed. One exemplary effort is from the Union of Pan Asian Communities (UPAC), a human services organization in San Diego that offers an array of support opportunities for older adults with MH/SU conditions. UPAC operates a counseling and treatment center for monolingual and limited English-proficient Asian and Pacific Islander adults and older adults with mental illness. The center focuses on helping individuals and their families to better understand the effects of posttraumatic stress, depression, and social isolation. Most clients are immigrants and refugees who face other challenges such as lack of access to health care and community resources, previous or ongoing trauma, past incarceration, and alcohol, drug, or gambling addictions. Another of UPAC’s major programs, Elderly Multicultural
Access and Support Services (EMASS), has helped over 800 Filipino, Latino, African American, and Somali clients learn about and discuss mental health issues through culturally tailored “Good Mental Health” forums and other activities. Focus groups run by the Health Services Research Center of the University of California, San Diego, found that EMASS participants reported an increased knowledge of prevention and early intervention for mental health problems, and a relief of mental health symptoms, including depression and anxiety (Union of Pan Asian Communities, 2011). In addition to these services, UPAC operates the East Wind Club House, which provides peer-led socialization and rehabilitation activities to approximately 180 chronically ill Southeast Asian adults and older adults with mental disabilities. It is the first program of this kind in California. UPAC also partners with other community organizations to provide multicultural peer and family support at the San Diego County Psychiatric Hospital. This program specifically staffs Older Adult Family Support Specialists (Montrose Counseling Center, 2012b).
Along with ethnic and racial minority populations, lesbian, gay, bisexual, and transgender (LGBT) older adults are also often disenfranchised as MH/SU consumers (Hunter, 2005). The Montrose Counseling Center in Houston is dedicated to providing affordable mental health services to the local LGBT community. Montrose launched the Seniors Preparing for Rainbow Years (SPRY) program in 2005 specifically to meet the needs of older adults. SPRY holds weekly men’s and women’s peer support groups, sponsors social activities, and provides professional counseling and case management. Montrose has launched a community campaign that encourages anyone to become an advocate for LGBT seniors. Advocates receive a 1-day training to recognize signs of depression, suicide risk, and substance abuse in LGBT seniors. Advocates are trained in QPR (Question, Persuade, and Refer) to connect older adults to SPRY services (Montrose Counseling Center, 2012a).
The committee’s finding on the current state of the geriatric MH/SU workforce are summarized in Box 3-7. The barriers to building an adequately sized, well-trained geriatric MH/SU workforce are numerous and complex. Recent efforts to augment training show that even when provided opportunities to specialize in geriatric MH/SU, students often do not choose to pursue them. This could be because financial returns for specializing in geriatric MH/SU are relatively unfavorable. However, money does not always override negative perceptions of MH/SU and aging, or professional influences to enter more “prestigious” specialties. These observations underscore the importance of simultaneously providing
BOX 3-7
Findings on the Geriatric Mental Health and Substance Use
(MH/SU) Workforce
Defining the Geriatric MH/SU Workforce
a. The geriatric MH/SU workforce is made up of many types of providers. Workforce roles are often poorly defined and overlapping.
Estimating Workforce Supply and Demand
b. Standardized workforce data that are trended over the time required to make accurate predictions of workforce supply and demand are not available.
Shortage of Geriatric MH/SU Providers
c. The workforce prepared to care for geriatric MH/SU is inadequate in sheer numbers, with the growth of the population threatening to exacerbate this.
Recruiting Geriatric MH/SU Providers
d. Across all health professions, relatively few opportunities exist for specialization in geriatric MH/SU. There is little support or mentorship available for those who do pursue specialization.
e. Financial incentives are not in place to encourage geriatric MH/SU providers to enter and stay in this field.
Inadequate Preparation of the Geriatric MH/SU Workforce
f. Professional training in geriatric MH/SU is inconsistent and not well documented because national standards and requirements in these areas are minimal and vague. MH/SU specialists have little required training in geriatrics; geriatric specialists have little
more training opportunities, guidance, mentorship, positive experiences, and financial incentives. Building up one of these components without considering the others will not solve the workforce crisis at hand.
Training general health care professionals and direct care workers is pivotal to improving the workforce because they are the most likely to have contact with older adults with MH/SU conditions. The extent to which training and education are provided for these groups is not well documented. Relatively few standards ensure that formal training programs include competencies in addressing MH/SU conditions in older adults. Also essential to training are skills in cultural competence and interprofessional collaboration to meet the complex needs of older adults.
required training in MH/SU; and most general providers do not have extensive requirements in either area.
Training the Geriatric MH/SU Workforce
g. Many professions have made progress on geriatric MH/SU competency development and workforce development, though these efforts are often done in silos where their dissemination and impact are not easily measured.
h. Innovations in geriatric MH/SU workforce development are often vulnerable to grant cuts, and many promising programs end without adequate documentation or evaluation to assist future development.
Strengthening the Role of Direct Care Workers (DCWs) in Geriatric MH/SU Care
i. Complex factors, including poor working conditions, low wages, lack of training, and limited opportunities for advancement, deter the development of a stable DCW workforce.
j. DCWs have the most contact with older adult patients, yet do not have adequate training in geriatrics or MH/SU, and virtually never get trained in both.
Empowering Older Adults and Their Families
k. There is a growing emphasis on peer support and self-care, including for older adult populations.
l. Family members play a major role as caregivers, but receive little support and training for caring for older adults with any medical conditions, including MH/SU conditions.
However, the evidence base to determine what modes of training are most effective in geriatric MH/SU is largely insufficient.
Consumers and their families are often overlooked members of the workforce, though this is changing with an increasing number of initiatives to hire consumers and family members as paid providers. Even for those not formally entering the workforce, opportunities for education and support are growing. Whether these initiatives are specifically reaching older MH/SU consumers and their caregivers has not been thoroughly evaluated. The degree to which existing education and support programs are culturally sensitive and accessible to minority populations is also unknown.
AACN (American Association of Colleges of Nursing). 2004. AACN adopts a new vision for the future of nursing education and practice. http://www.aacn.nche.edu/news/articles/2004/dnp-release (accessed October 12, 2011).
———. 2008. The essentials of baccalaureate education for professional nursing practice. Washington, DC: AACN.
———. 2010a. Adult-gerontology clinical nurse specialist competencies. http://www.aacn.nche.edu/education-resources/competencies-older-adults (accessed October 13, 2011).
———. 2010b. Adult-gerontology primary care nurse practitioner competencies. http://www.aacn.nche.edu/education-resources/competencies-older-adults (accessed October 13, 2011).
AACN Commission on Nurse Certification. 2011. History of CNL certification. http://www.aacn.nche.edu/leading-initiatives/cnl/cnl-certification/pdf/History.pdf (accessed October 13, 2011).
AACP (American Association of Colleges of Pharmacy). 2010. Pharmacy school admission requirements, 2011-2012. Alexandria, VA: AACP.
AAFP (American Academy of Family Physicians). 2011. Primary care. http://www.aafp.org/online/en/home/policy/policies/p/primarycare.html#Parsys0004 (accessed September 29, 2011).
AAGP (American Association of Geriatric Psychiatry). 2011. Scholars fund. http://www.aagponline.org/index.php?submenu=forstudents_submenu&src=gendocs&ref=ScholarsProgram&category=forstudents_submenu&link=ScholarsProgram (accessed April 2, 2012).
AAMC (Association of American Medical Colleges). 2003. Geriatrics instruction in the medical school curriculum. Analysis in brief. Washington, DC: AAMC.
———. 2008. Physician specialty data. https://www.aamc.org/download/47352/data/specialtydata.pdf (accessed December 5, 2011).
———. 2011. Medical school graduate questionnaire: 2011 all schools summary report. Washington, DC: AAMC.
AAMFT (American Association for Marriage and Family Therapy). 2006. Medicare coverage of marriage and family therapists. http://www.cpca.org/cpca/assets/File/Policy-and-Advocacy/Legislative/Marriage-Family-Therapists/AAMFTMedicareFactSheet.pdf (accessed March 28, 2012).
———. 2011a. MFT licensing boards. http://www.aamft.org/iMIS15/AAMFT/Directories/MFT_Licensing_Boards/Content/Directories/MFT_Licensing_Boards.aspx?hkey=b1033df3-6882-491e-87fd-a75c2f7be070 (accessed October 21, 2011).
———. 2011b. Qualifications and FAQs. http://www.aamft.org/imis15/Content/About_AAMFT/Qualifications.aspx (accessed October 20, 2011).
AAN (American Academy of Nursing). 2010. Geropsychiatric nursing collaborative. http://www.aannet.org/i4a/pages/index.cfm?pageid=3833 (accessed November 21, 2011).
AAPA (American Academy of Physician Assistants). 2010a. PA facts. Alexandria, VA: AAPA.
———. 2010b. Physician assistant census report: Results from the 2010 AAPA census. Alexandria, VA: AAPA.
AAPC (American Association of Pastoral Counselors). 2009. State licensing for pastoral counselors. http://www.aapc.org/membership/licensing.aspx (accessed March 29, 2012).
———. 2012. About us. http://www.aapc.org/about-us.aspx? (accessed April 12, 2012).
AARP South Carolina. 2010. Loan forgiveness program for geriatric physicians. http://www.aarp.org/health/doctors-hospitals/info-09-2010/loan_forgiveness_sc.html (accessed December 22, 2011).
ABFM (American Board of Family Medicine). 2011. Diplomate statistics. https://www.the abfm.org/about/stats.aspx (accessed October 3, 2011).
ABIM (American Board of Internal Medicine). 2011. Candidates certified—all candidates. Philadelphia. http://www.abim.org/pdf/data-candidates-certified/all-candidates.pdf (accessed December 5, 2011).
ABPN (American Board of Psychiatry and Neurology). 2007. Frequently asked questions. http://www.abpn.com/faqs.html (accessed October 3, 2011).
———. 2010a. Initial certification statistics. http://www.abpn.com/cert_statistics.html (accessed October 4, 2011).
———. 2010b. Maintenance of certification statistics. http://www.abpn.com/moc_statistics.html (accessed October 4, 2011).
ABPP (American Board of Professional Psychology). 2012. Member specialty boards. http://www.abpp.org/i4a/pages/index.cfm?pageid=3286 (accessed April 12, 2012).
ACA (American Counseling Association). 2012. Licensure & certification. http://www.counseling.org/counselors/LicensureAndCert.aspx (accessed January 23, 2012).
ACGME (Accreditation Council for Graduate Medical Education). 2003a. ACGME program requirements for graduate medical education in addiction psychiatry. http://www.acgme.org/acWebsite/downloads/RRC_progReq/401pr703_u105.pdf (accessed April 23, 2010).
———. 2003b. ACGME program requirements for graduate medical education in geriatric psychiatry. http://www.acgme.org/acWebsite/downloads/RRC_progReq/407pr703_u105.pdf (accessed April 23, 2010).
———. 2006. ACGME program requirements for graduate medical education in geriatric medicine. http://www.acgme.org/acWebsite/downloads/RRC_progReq/125pr0706.pdf (accessed April 23, 2010).
———. 2007. ACGME program requirements for graduate medical education in geriatric medicine. http://www.acgme.org/acWebsite/downloads/RRC_progReq/151pr707_ims.pdf (accessed December 5, 2011).
———. 2009. ACGME program requirements for graduate medical education in psychiatry. http://www.acgme.org/acWebsite/downloads/RRC_progReq/400_psychiatry_07012007_u04122008.pdf (accessed December 5, 2011).
———. 2012. Number of accredited programs for the current academic year (2011-2012). http://www.acgme.org/adspublic/ (accessed January 19, 2011).
ACOTE (Accreditation Council for Occupational Therapy Education). 2012. 2011 Accreditation Council for Occupational Therapy Education standards and interpretive guide. Bethesda, MD: AOTA.
ACPE (Accreditation Council for Pharmacy Education). 2011. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. Chicago: ACPE.
Adams, B. M., M. P. Aranda, B. J. Kemp, and K. Takagi. 2002. Ethnic and gender differences in appraisal, coping and social support: A comparison of white-American, African-American, Japanese-American and Mexican-American spousal caregivers of persons with dementia. Journal of Clinical Geropsychology 8(4):279-301.
AGESW (Association for Gerontology Education in Social Work). 2011. Pre-dissertation initiative. http://agesw.org/about-agesw/pre-dissertation-initiative (accessed April 6, 2012).
AGS (American Geriatrics Society). 2011. State loan forgiveness toolkit. http://www.american geriatrics.org/ags_state_affiliates/state_affiliate_handbook/loan_forgiveness_toolkit/ (accessed December 22, 2011).
Alcoholics Anonymous. 2008. Alcoholics Anonymous 2007 membership survey. http://www.aa.org/pdf/products/p-48_07survey.pdf (accessed April 12, 2012).
Alegria, M., P. Chatterji, K. Wells, Z. Cao, C. N. Chen, D. Takeuchi, J. Jackson, and X. L. Meng. 2008. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatric Services 59(11):1264-1272.
ANA (American Nurses Association). 2011. What is nursing? http://www.nursingworld.org/EspeciallyForYou/StudentNurses/WhatisNursing.aspx (accessed October 6, 2011).
ANCC (American Nurses Credentialing Center). 2010a. Gerontological nursing board certification test content outline. http://www.nursecredentialing.org/GeroNurse-TCO2012.aspx (accessed October 12, 2011).
———. 2010b. Psychiatric and mental health nursing board certification test content outline. http://www.nursecredentialing.org/PsychNurse-TCO2012.aspx (accessed October 12, 2011).
———. 2012. Renew your nursing certification. http://www.nursecredentialing.org/RenewCertification.aspx (accessed January 5, 2012).
AoA (Administraton on Aging). 2010. Older Americans 2010: Key indicators of well-being. http://www.agingstats.gov/Main_Site/Data/2010_Documents/docs/Introduction.pdf (accessed April 12, 2012).
AOA (American Osteopathic Association). 2010. Osteopathic medical profession report. Chicago: AOA.
———. 2011a. Basic standards for fellowship training in addiction medicine in osteopathic family medicine and manipulative treatment. http://www.osteopathic.org/inside-aoa/accreditation/postdoctoral-training-approval/postdoctoral-training-standards/Documents/basic-standards-for-fellowship-training-in-addiction-medicine-family-practice.pdf (accessed December 5, 2011).
———. 2011b. Basic standards for fellowship training in geriatrics in osteopathic family medicine and manipulative treatment. http://www.osteopathic.org/inside-aoa/accreditation/postdoctoral-training-approval/postdoctoral-training-standards/Documents/basic-standards-for-fellowship-training-in-geriatrics-osteopathic-family-practice.pdf (accessed December 5, 2011).
AOTA (American Occupational Therapy Association). 2009. AOTA board certified in mental health candidate handbook. Bethesda, MD: AOTA.
———. 2012a. Board certified and specialty certified practitioners. http://aota.org/Practitioners/ProfDev/Certification/certified.aspx (accessed March 30, 2012).
———. 2012b. How to get a license. http://www.aota.org/Practitioners/Licensure/HowTo.aspx (accessed March 29, 2012).
APA (American Psychiatric Association). 2000. Diagnostic and statistical manual of mental disorders: DSM-IV-TR, 4th ed. Washington, DC: American Psychiatric Association.
APA (American Psychological Association). 2004. Guidelines for psychological practice with older adults. American Psychologist 59(4):236-260.
———. 2011a. Frequently asked questions. http://www.apa.org/workforce/about/faq.aspx#I.6 (accessed October 13, 2011).
———. 2011b. Public description of clinical psychology. http://www.apa.org/ed/graduate/specialize/clinical.aspx (accessed October 14, 2011).
———. 2011c. Public description of counseling psychology. http://www.apa.org/ed/graduate/specialize/counseling.aspx (accessed October 14, 2011).
———. 2011d. Recognized specialties and proficiencies in professional psychology. http://www.apa.org/ed/graduate/specialize/recognized.aspx (accessed October 13, 2011).
———. 2012a. Effects of cuts in funding for the graduate psychology education program in urban communities. http://www.apa.org/about/gr/issues/gpe/urban.aspx (accessed April 5, 2012).
———. 2012b. FY 2011 congressional appropriations request: Strengthen the graduate psychology education program. http://www.apa.org/about/gr/education/advocacy/2010/gpe-2011.aspx (accessed April 5, 2012).
APA Commission on Accreditation. 2009. Guidelines and principles for accreditation of programs in professional psychology. Washington, DC: American Psychological Association.
APRN Consensus Work Group and the National Council of State Boards of Nursing APRN Advisory Committee. 2008. Consensus model for APRN regulation: Licensure, accreditation, certification and education. https://www.ncsbn.org/Consensus_Model_for_APRN_Regulation_July_2008.pdf (accessed April 12, 2012).
Aranda, M. P., and B. G. Knight. 1997. The influence of ethnicity and culture on the caregiver stress and coping process: A sociocultural review and analysis. Gerontologist 37(3):342-354.
Aranda, M. P., V. M. Villa, L. Trejo, R. Ramirez, and M. Ranney. 2003. El Portal Latino Alzheimer’s Project: Model program for Latino caregivers of Alzheimer’s disease-affected people. Social Work 48(2):259-271.
ARCEPA (Accreditation Review Commission on Education for the Physician Assistant). 2010a. Accreditation standards for physician assistant education, 4th ed. http://www.arc-pa.org/acc_standards/ (accessed December 5, 2011).
———. 2010b. Accredited programs over time. http://www.arc-pa.org/documents/AccreditedProgamsOverTimegraphasof9.2010.pdf (accessed December 5, 2011).
ASHSP (American Society of Health-System Pharmacists). 2007. Required educational outcomes, goals, and objectives for postgraduate year two (PGY2) pharmacy residencies in psychiatry. http://www.ashp.org/DocLibrary/Accreditation/PGY1-Goals-Objectives.aspx (accessed December 5, 2011).
———. 2011. Online residency directory. http://accred.ashp.org/aps/pages/directory/residencyProgramSearch.aspx#1 (accessed September 26, 2011).
ASPPB (Association of State and Provincial Psychology Boards). 2011a. ASPPB information for EPPP candidates: Examination for Professional Practice in Psychology (EPPP). http://www.asppb.net/files/public/IFC.pdf (accessed October 14, 2011).
———. 2011b. Degree level requirements for licensure by jurisdiction. http://www.asppb.org/HandbookPublic/Reports/default.aspx?ReportType=DegreeLevelLiscensure (accessed October 14, 2011).
Association of Postgraduate PA Programs. 2010. APPAP programs by specialty. http://www.appap.org/LinkClick.aspx?fileticket=FqFcRIQsEF4%3d&tabid=58 (accessed December 5, 2011).
ASWB (Association of Social Work Boards). 2008. Social work laws & regulations database. https://www.datapathdesign.com/ASWB/Laws/Prod/cgi-bin/LawWebRpts2DLL.dll/EXEC/0/0es979v0m3bmaa16a5vok02j02ck (accessed December 5, 2011).
———. 2011. ASWB examination candidate handbook. http://www.aswb.org/pdfs/handbook.pdf (accessed December 5, 2011).
ATTC (Addiction Technology Transfer Center). 2011. Licensing and certification requirements. http://www.attcnetwork.org/find/certinfo/index.asp (accessed October 20, 2011).
Aud, S., M. A. Fox, and A. Kewal Ramani. 2012. Status and trends in the education of racial and ethnic groups. NCES 2010-015. U.S. Department of Education, National Center for Education Statistics. Washington, DC: U.S. Government Printing Office.
Barber, J. A., R. A. Rosenheck, M. Armstrong, and S. G. Resnick. 2008. Monitoring the dissemination of peer support in the VA health care system. Journal of Community Mental Health 44:441-443.
Bartels, S. J., B. D. Lebowitz, C. F. Reynolds III, M. L. Bruce, M. Halpain, W. E. Faison, and P. D. Kirwin. 2010. Programs for developing the pipeline of early-career geriatric mental health researchers: Outcomes and implications for other fields. Academic Medicine 85(1):26-35.
Barzansky, B., and S. I. Etzel. 2001. Educational programs in U.S. medical schools, 2000-2001. Journal of the American Medical Association 286(9):1049-1055.
Beck, C., K. C. Buckwalter, P. M. Dudzik, and L. K. Evans. 2011. Filling the void in geriatric mental health: The Geropsychiatric Nursing Collaborative as a model for change. Nursing Outlook 59(4):236-241.
Becker, G. S. 1962. Investment in human capital: A theoretical analysis. Journal of Political Economy 70(5 Part 2):9-49.
Bernard, M. A., W. J. McAuley, J. A. Belzer, and K. S. Neal. 2003. An evaluation of a low intensity intervention to introduce medical students to healthy older people. Journal of the American Geriatrics Society 51(3):419-423.
BLS (U.S. Bureau of Labor Statistics). 2009a. Occupational outlook handbook, 2010-11 edition, counselors. http://www.bls.gov/oco/ocos067.htm (accessed March 28, 2012).
———. 2009b. Occupational outlook handbook, social workers. http://www.bls.gov/oco/ocos060.htm (accessed October 19, 2011).
———. 2010. Occupational employment and wages, May 2009. 29-2061 Licensed practical and licensed vocational nurses. http://www.bls.gov/oes/current/oes292061.htm (accessed January 19, 2012).
———. 2011. Occupational employment and wages, May 2010. 29-2061 Licensed practical and licensed vocational nurses. http://www.bls.gov/oes/current/oes292061.htm (accessed October 10, 2011).
———. 2012a. Occupational employment and wages, May 2011. 19-3031 Clinical, counseling, and school psychologists. http://www.bls.gov/oes/current/oes193031.htm (accessed April 6, 2012).
———. 2012b. Occupational employment and wages, May 2011. 21-1011 Substance abuse and behavioral disorder counselors. http://www.bls.gov/oes/current/oes211011.htm (accessed April 13, 2012).
———. 2012c. Occupational employment and wages, May 2011. 21-1013 Marriage and family therapists. http://www.bls.gov/oes/current/oes211013.htm (accessed April 13, 2012).
———. 2012d. Occupational employment and wages, May 2011. 21-1014 Mental health counselors. http://www.bls.gov/oes/current/oes211014.htm (accessed April 13, 2012).
———. 2012e. Occupational employment and wages, May 2011. 21-1023 Mental health and substance abuse social workers. http://www.bls.gov/oes/current/oes211023.htm (accessed April 13, 2012).
———. 2012f. Occupational employment and wages, May 2011. 29-1066 Psychiatrists. http://data.bls.gov/cgi-bin/print.pl/oes/current/oes291066.htm (accessed April 13, 2012).
———. 2012g. Occupational employment and wages, May 2011. 29-1122 Occupational therapists.
http://www.bls.gov/oes/current/oes291122.htm (accessed March 29, 2012).
———. 2012h. Occupational outlook handbook, occupational therapy assistants and aides. http://www.bls.gov/ooh/Healthcare/Occupational-therapy-assistants-and-aides.htm (accessed March 29, 2012).
Bluebird, G. 2008. Paving new ground: Peers working in inpatient settings. Alexandria, VA: National Association of State Mental Health Program Directors.
Bobby, C. L., and R. I. Urofsky. 2008. CACREP adopts new standards. Counseling Today 51(2):59-60.
Bookman, A., and M. Harrington. 2007. Family caregivers: A shadow workforce in the geriatric health care system? Journal of Health Politics, Policy and Law 32(6):1005-1041.
Boston University Institute for Geriatric Social Work. 2011. Online training programs. http://www.bu.edu/igsw/online-training-programs/ (accessed June 11, 2012).
BPS (Board of Pharmacy Specialties). 2005. Content outline for the Psychiatric Pharmacy Specialty Certification Examination. http://www.bpsweb.org/pdfs/content_outline_psychiatric.pdf (accessed December 5, 2011) ———. 2011. Pharmacists certified by the Board of Pharmacy Specialties. http://www.bpsweb.org/resources/BPSInformationalSlides.pdf (accessed December 5, 2011).
Brown, C., H. C. Schulberg, and M. J. Madonia. 1996. Clinical presentations of major depression by African Americans and whites in primary medical care practice. Journal of Affective Disorders 41(3):181-191.
Bruce, M. L., E. L. Brown, P. J. Raue, A. E. Mlodzianowski, B. S. Meyers, A. C. Leon, M. Heo, A. L. Byers, R. L. Greenberg, and S. Rinder. 2007. A randomized trial of depression assessment intervention in home health care. Journal of the American Geriatrics Society 55(11):1793-1800.
Brugna, R., J. Cawley, and M. Baker. 2007. Physician assistants in geriatric medicine. Clinical Geriatrics 15(10):22.
CAADAC (California Association of Alcoholism and Drug Abuse Counselors). 2011. California Certification Board of Alcohol and Drug Counselors (CCBADC) requirements for certification. https://www.caadac.org/ladder/ (accessed October 20, 2011).
CACREP (Council for Accreditation of Counseling and Related Educational Programs). 2010. Council for Accreditation of Counseling and Related Educational Programs 2009.
http://www.cacrep.org/doc/2009%20Standards%20with%20cover.pdf (accessed March 28, 2012).
———. 2011. Scope of accreditation. http://67.199.126.156/template/page.cfm?id=52 (accessed October 20, 2011).
CalSWEC (California Social Work Education Center). 2011a. Evaluation and research. http://calswec.berkeley.edu/CalSWEC/MH_EvalRes.html (accessed December 22, 2011).
———. 2011b. Mental health curriculum resources. http://calswec.berkeley.edu/CalSWEC/MHInitiative_CurricRes.html (accessed December 22, 2011).
Cates, M. E., M. R. Monk-Tutor, and S. O. Drummond. 2007. Mental health and psychiatric pharmacy instruction in U.S. colleges and schools of pharmacy. American Journal of Pharmaceutical Education 71(1):1-5.
CCGP (Commission for Certification in Geriatric Pharmacy). 2011. Exam content. http://www.ccgp.org/pharmacist/certification/disease.htm (accessed September 27, 2011).
Center to Champion Nursing in America. 2010. Preparation and roles of nursing care providers in America. http://championnursing.org/resources/preparation-and-roles-nursing-care-providers-america (accessed December 5, 2011).
Chadiha, L. A., E. Brown, and M. P. Aranda. 2006. Social work practice with older African Americans and other black populations. In Handbook of social work in aging, edited by B. Berkman. New York: Oxford University Press.
Champagne, T., and K. Gray. 2011. Occupational therapy’s role in mental health recovery. http://www.aota.org/Practitioners/PracticeAreas/Aging/Tools/MH-Recovery.aspx?FT=.pdf (accessed April 12, 2012).
Christian, S., C. Dower, and E. O’Neil. 2007. Chart overview of nurse practitioner scopes of practice in the United States. San Francisco, CA: UCSF Center for the Health Professions.
Clay, R. 2006. Geropsychology grants in peril. Monitor on Psychology 37(4):46.
CMS (Centers for Medicare & Medicaid Services). 2007. State Medicaid Director Letter #07-011. http://downloads.cms.gov/cmsgov/archived-downloads/SMDL/downloads/SMD081507A.pdf (accessed December 13, 2011).
CNC (Commission on Nurse Certification). 2011. Frequently asked questions about CNL ® certification. http://www.aacn.nche.edu/leading-initiatives/cnl/cnl-certification/pdf/faq.pdf (accessed October 13, 2011).
Colenda, C. C., J. E. Wilk, and J. C. West. 2005. The geriatric psychiatry workforce in 2002: Analysis from the 2002 National Survey of Psychiatric Practice. American Journal of Geriatric Psychology 13(9):756.
Commission for Accreditation of Marriage and Family Therapy Education. 2005. MFT educational guidelines. http://www.aamft.org/imis15/Documents/COAMFTE_MFT_Educational_Guidelines.pdf (accessed October 24, 2011).
CORE (Council on Rehabilitation Education). 2010. CORE accreditation standards. http://www.core-rehab.org/Files/Doc/PDF/COREStandards20120204.pdf (accessed March 29, 2012).
Corwin, S. J., K. Frahm, L. A. Ochs, C. E. Rheaume, and E. Roberts. 2006. Medical student and senior participants’ perceptions of a mentoring program designed to enhance geriatric medical education. Gerontology & Geriatrics Education 26(3):47-65.
Council on Credentialing in Pharmacy. 2009. Scope of contemporary pharmacy practice: Roles, responsibilities, and functions of pharmacists and pharmacy technicians. Washington, DC. http://www.accp.com/docs/positions/misc/ccpwpscope_pharmacy_practice_2-2009.pdf (accessed December 5, 2011).
Couture, S., and D. Penn. 2003. Interpersonal contact and the stigma of mental illness: A review of the literature. Journal of Mental Health 12(3):291-305.
Covinsky, K. E., R. Newcomer, P. Fox, J. Wood, L. Sands, K. Dane, and K. Yaffe. 2003. Patient and caregiver characteristics associated with depression in caregivers of patients with dementia. Journal of General Internal Medicine 18(12):1006-1014.
CRCC (Commission on Rehabilitation Counselor Certification). 2011. Rehabilitation counseling. http://www.crccertification.com/pages/rehabilitation_counseling/30.php (accessed March 29, 2012).
Crystal, S., U. Sambamoorthi, J. T. Walkup, and A. Akincigil. 2003. Diagnosis and treatment of depression in the elderly Medicare population: Predictors, disparities, and trends. Journal of the American Geriatrics Society 51(12):1718-1728.
CSAT (Center for Substance Abuse Treatment). 2005. A national review of state alcohol and drug treatment programs and certification standards for substance abuse counselors and prevention professionals. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Cummings, S. M., G. Adler, and V. A. DeCoster. 2005. Factors influencing graduate-social-work students’ interest in working with elders. Educational Gerontology 31(8):643-655.
Daniels, A. S., E. Grant, B. Filson, I. Powell, L. Fricks, and L. Goodale. 2010. Pillars of peer support: Transforming mental health systems of care through peer support services. http://www.power2u.org/downloads/PillarsOfPeerSupportServiceReport.pdf (accessed December 15, 2011).
Daniels, A. S., L. Fricks, and T. P. Tunner. 2011. Pillars of peer support-2: Expanding the role of peer support services in mental health systems of care and recovery. www.pillarsofpeersupport.org (accessed April 12, 2011).
Direct Care Alliance. 2011a. Direct Care Alliance personal care and support credential. http://www.directcarealliance.org/document/docWindow.cfm?fuseaction=document.viewocument&documentid=19&documentFormatId=21 (accessed April 12, 2012).
———. 2011b. Direct Care Alliance personal care and support credential 2011 candidate handbook. http://directcarealliance.org/document/docWindow.cfm?fuseaction=document.viewDocument&documentid=2&documentFormatId=2 (accessed October 10, 2011).
Direct Service Workforce Resource Center. 2011. Building capacity and coordinating support for family caregivers and the direct service workforce: Common goals and policy recommendations emerging from the CMS leadership summit on the direct service workforce and family caregivers. http://dswresourcecenter.org/tiki-index.php?page=Reports (accessed October 11, 2011).
DOLETA (U.S. Department of Labor Employment and Training Administration) Office of Apprenticeship. 2012. Registered apprenticeship training in long-term care. Washington, DC: U.S. Department of Labor.
Donald W. Reynolds Foundation. 2011. Description of geriatrics training grants approved in June 2006. http://www.dwreynolds.org/Programs/National/Aging/Cohort3.htm (accessed December 20, 2011).
Eaton, J. S. 2011. An overview of U.S. accreditation. Washington, DC: Council for Higher Education Accreditation. http://www.chea.org/pdf/Overview%20of%20US%20Accreditation%2003.2011.pdf (accessed April 9, 2012).
Eaton, S. C., C. Green, R. Wilson, and T. Osypuk. 2001. Extended Care Career Ladder Initiative (ECCLI): Baseline report of a Massachusetts nursing initiative. Cambridge, MA: Kennedy School of Government.
Ehrlich, A. R., and L. G. Jacobs. 2004. Albert Einstein College of Medicine of Yeshiva University. Academic Medicine 79(7):S3-S6.
Eleazer, G. P., D. Wieland, E. Roberts, N. Richeson, and J. T. Thornhill. 2006. Preparing medical students to care for older adults: The impact of a senior mentor program. Academic Medicine 81(4):393.
Evercare. 2007. Evercare Survey of graduating high school seniors finds prospective nurses lack interest in geriatrics despite growing senior population. http://www.businesswire.com/news/home/20070801005845/en/Evercare-Survey-Graduating-High-School-Seniors-Finds (accessed December 19, 2011).
Faulkner, L. R., D. Juul, N. N. Andrade, B. A. Brooks, C. C. Colenda, R. W. Guynn, D. A. Mrazek, V. I. Reus, B. S. Schneidman, and K. R. Shaw. 2011. Recent trends in American Board of Psychiatry and Neurology psychiatric subspecialties. Academic Psychiatry 35(1):35-39.
Federation of State Medical Boards of the United States, and National Board of Medical Examiners. 2011. 2011 Step 2 Clinical Knowledge (CK) content description and general information. http://www.usmle.org/examinations/step2/ck/2011Step2CK.pdf (accessed December 5, 2011).
Feinberg, L., S. C. Reinhard, A. Houser, and R. Choula. 2011. Valuing the invaluable: 2011 update: The growing contributions and costs of family caregiving. http://assets.aarp.org/rgcenter/ppi/ltc/i51-caregiving.pdf (accessed April 12, 2012).
Geriatric Mental Health Foundation. 2012. The role of the geriatric psychiatrist. http://www.gmhfonline.org/gmhf/consumer/factsheets/geriatric_psychiatrist.html (accessed January 19, 2012).
Geriatric Social Work Initiative. 2012. Hartford Pre-Dissertation Award Program in Geriatric Social Work. http://www.gswi.org/programs/predissertation.html (accessed April 6, 2012).
Goodwin, K., and L. Tobler. 2008. Community health workers: Expanding the scope of the health care delivery system. http://www.ncsl.org/print/health/CHWBrief.pdf (accessed April 12, 2012).
GWPSC (Geriatrics Workforce Policy Studies Center). 2009a. Figure 4.1, Required time (half days in 2002 and 2008/weeks in 2005) devoted to clinical instruction in geriatric medicine during 3-year general internal medicine residency in 2002, 2005, and 2008. http://www.adgapstudy.uc.edu/figs_graduate.cfm (accessed December 5, 2011).
———. 2009b. Figure 4.5, Required time (half days) devoted to clinical instruction in geriatric medicine during 3-year family medicine residency in 2001, 2004, and 2008. http://www.adgapstudy.uc.edu/figs_graduate.cfm (accessed December 5, 2011).
———. 2009c. Table 4.11, Required geriatric experiences in family medicine residency programs, 2004 and 2008. http://www.adgapstudy.uc.edu/figs_graduate.cfm (accessed December 5, 2011).
———. 2010a. Table 3.2, Geriatric medicine fellowship programs, family medicine and internal medicine 1991/92-2010/11. http://www.adgapstudy.uc.edu/figs_graduate.cfm (accessed December 5, 2011).
———. 2010b. Table 3.5, Geriatric psychiatry fellowship programs 1995/96-2010/11: American Geriatrics Society. http://www.adgapstudy.uc.edu/figs_graduate.cfm (accessed December 5, 2011).
Hanrahan, N. P., and D. Hartley. 2008. Employment of advanced-practice psychiatric nurses to stem rural mental health workforce shortages. Psychiatric Services 59(1):109-111.
Happell, B. 2008. The importance of clinical experience for mental health nursing—Part 2: Relationships between undergraduate nursing students’ attitudes, preparedness, and satisfaction. International Journal of Mental Health Nursing 17(5):333-340.
Happell, B., and C. Roper. 2003. The role of a mental health consumer in the education of postgraduate psychiatric nursing students: The students’ evaluation. Journal of Psychiatric and Mental Health Nursing 10(3):343-350.
Harmuth, S., and T. R. Konrad. 2010. Strengthening the direct care workforce in North Carolina. North Carolina Medical Journal 71(2):158-160.
Hartigan, C. 2011. APRN regulation: The licensure-certification interface. AACN Advanced Critical Care 22(1):15.
Hewitt, A., S. Larson, S. Edelstein, D. Seavey, M. A. Hoge, and J. Morris. 2008. A synthesis of direct service workforce demographics and challenges across intellectual/developmental disabilities, aging, physical disabilities, and behavioral health. Falls Church, VA: The Lewin Group.
HHS (U.S. Department of Health and Human Services). 1999. Mental health: A report of the Surgeon General. Rockville, MD: HHS.
Hinrichsen, G. A. 2010. Public policy and the provision of psychological services to older adults. Professional Psychology: Research and Practice 41(2):97-103.
Hinrichsen, G. A., A. M. Zeiss, M. J. Karel, and V. A. Molinari. 2010. Competency-based geropsychology training in doctoral internships and postdoctoral fellowships. Training and Education in Professional Psychology 4(2):91.
Hoffman, K. G., P. Gray, M. C. Hosokawa, and S. C. Zweig. 2006. Evaluating the effectiveness of a senior mentor program: The University of Missouri-Columbia School of Medicine. Gerontology & Geriatrics Education 27(2):11.
Hogan, M. F. 2003. The President’s New Freedom Commission: Recommendations to transform mental health care in America. Psychiatric Services 54(11):1467-1474.
Hoge, M. A., J. A. Morris, A. S. Daniels, G. W. Stuart, L. Y. Huey, N. Adams, and Annapolis Coalition on the Behavioral Health Workforce. 2007. An action plan for behavioral health workforce development: Executive summary. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Hooker, R. S. 2006. Physician assistants and nurse practitioners: The United States experience. Medical Journal of Australia 185(1):4.
HRSA (Health Resources and Services Administration). 2007. Community Health Worker National Workforce Study. Rockville, MD. http://bhpr.hrsa.gov/healthworkforce/reports/chwstudy2007.pdf (accessed April 12, 2012).
———. 2010. The registered nurse population: Findings from the 2008 National Sample Survey of Registered Nurses. U.S. Department of Health and Human Services. http://bhpr.hrsa.gov/healthworkforce/reports/chwstudy2007.pdf (accessed April 12, 2012).
———. 2012. Guidelines for mental health HPSA designation. http://bhpr.hrsa.gov/shortage/hpsas/designationcriteria/mentalhealthhpsaguidelines.html (accessed March 28, 2012).
Hunter, S. 2005. Midlife and older LGBT adults: Knowledge and affirmative practice for the social sciences. New York: Haworth Press, Inc.
Interprofessional Education Collaborative Expert Panel. 2011. Core competencies for Interprofessional Collaborative Practice: Report of an expert panel. Washington, DC: Interprofessional Education Collaborative. http://www.aacn.nche.edu/education-resources/ipecreport.pdf (accessed December 5, 2011).
IOM (Institute of Medicine). 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
———. 2006. Improving the quality of health care for mental and substance-use conditions. Washington, DC: The National Academies Press.
———. 2008a. Cancer Care for the Whole Patient: Meeting Psychosocial Needs. Washington, DC: The National Academies Press.
———. 2008b. Retooling for an aging America: Building the health care workforce. Washington, DC: The National Academies Press.
———. 2011. The future of nursing: Leading change, advancing health. Washington, DC: The National Academies Press.
Janevic, M. R., and C. M. Connell. 2001. Racial, ethnic, and cultural differences in the dementia caregiving experience: Recent findings. Gerontologist 41(2):334-347.
Johnson, E. 2008. Minnesota peer support implementation consultant’s report. http://www.californiaclients.org/pdf/Sue%20Watson%20Presentation%20Attachment.pdf (accessed April 12, 2012).
Karel, M. J., E. E. Emery, and V. Molinari. 2010a. Development of a tool to evaluate geropsychology knowledge and skill competencies. International Psychogeriatrics 22(6):886-896.
Karel, M. J., B. G. Knight, M. Duffy, G. A. Hinrichsen, and A. M. Zeiss. 2010b. Attitude, knowledge, and skill competencies for practice in professional geropsychology: Implications for training and building a geropsychology workforce. Training and Education in Professional Psychology 4(2):75-84.
Kennedy Malone, L., J. Penny, and M. E. Fleming. 2008. Clinical practice characteristics of gerontological nurse practitioners: A national study. Journal of the American Academy of Nurse Practitioners 20(1):17-27.
Knight, B. G., and P. Sayegh. 2010. Cultural values and caregiving: The updated sociocultural stress and coping model. Journals of Gerontology Series B Psychological Sciences 65B(1):5-13.
Knight, B. G., M. J. Karel, G. A. Hinrichsen, S. H. Qualls, and M. Duffy. 2009. Pikes Peak model for training in professional geropsychology. American Psychologist 64(3):205-214.
Koder, D., and E. Helmes. 2008. Predictors of interest in working with older adults: A survey of postgraduate trainee psychologists. Gerontology & Geriatrics Education 29(2):158.
Lafer, G., and H. Moss. 2007. The LPN: A practical way to alleviate the nursing shortage. University of Oregon. http://www.afscme.org/news/publications/health-care/the-lpn-a-practical-way-to-alleviate-the-nursing-shortage (accessed December 5, 2011).
Liaison Committee on Medical Education. 2011. Functions and structure of a medical school: Standards for accreditation of medical education programs leading to the M.D. degree. http://www.lcme.org/functions2011may.pdf (accessed December 22, 2011).
Magaña, S. M., J. I. R. García, M. G. Hernández, and R. Cortez. 2007. Psychological distress among Latino family caregivers of adults with schizophrenia: The roles of burden and stigma. Psychiatric Services 58(3):378-384.
Maryland Board of Nursing. 2010. Nursing assistant certification. http://www.mbon.org/main.php?v=norm&p=0&c=cna/cna_info.html (accessed January 25, 2012).
McFarlane, W. R., L. Dixon, E. Lukens, and A. Lucksted. 2003. Family psychoeducation and schizophrenia: A review of the literature. Journal of Marital and Family Therapy 29(2):223-245.
Meyers, J. E. 1995. From “forgotten and ignored” to standards and certification: Gerontological counseling comes of age. Journal of Counseling and Development 74(2):143-149.
Michalski, D., T. Mulvey, and J. Kohout. 2010. 2008 APA Survey of Psychology Health Service Providers. Washington, DC: American Psychological Association.
Midwest Pharmacy Workforce Research Consortium. 2010. 2009 National Pharmacist Workforce Survey. http://www.aacp.org/resources/research/pharmacymanpower/Documents/2009%20National%20Pharmacist%20Workforce%20Survey%20-%20FINAL%20REPORT.pdf (accessed December 5, 2011).
Migrant Health Promotion. 2012. Who are promotores(as)? http://www.migranthealth.org/index.php?option=com_content&view=article&id=41&Itemid=38 (accessed April 4, 2012).
Money, N., M. Moore, D. Brown, K. Kasper, J. Roeder, P. Bartone, and M. Bates. 2011. Best practices identified for peer support programs. Defense Centers for Excellence for Psychological Health and Traumatic Brain Injury. http://www.dcoe.health.mil/Content/Navigation/Documents/Best_Practices_Identified_for_Peer_Support_Programs_Jan_2011.pdf (accessed December 16, 2011).
Montrose Counseling Center. 2012a. 4Ever Family Project. http://www.montrosecounselingcenter.org/?page_id=5634 (accessed April 11, 2012).
———. 2012b. SPRY: Seniors Preparing for Rainbow Years. http://www.spryhouston.org/ (accessed April 11, 2012).
Morgan, P. A., and R. S. Hooker. 2010. Choice of specialties among physician assistants in the United States. Health Affairs 29(5):887.
NADSP (National Alliance for Direct Support Professionals). 2011a. 15 NADSP competency areas. https://www.nadsp.org/images/NADSP_Competency_Areas.pdf (accessed April 15, 2012).
———. 2011b. About DSP credentialing. https://nadsp.org/dsp-credentialing/about-dsp-credentialing.html (accessed April 15, 2012).
NAMI (National Alliance on Mental Illness) New Hampshire. 2010. Side by side for independent living evaluation summary. Concord, NH: NAMI NH.
———. 2012. Side by Side. http://www.naminh.org/side-by-side (accessed April 9, 2012).
NASW (National Association of Social Workers). 2005. NASW standards for clinical social work in social work practice. http://www.socialworkers.org/practice/standards/NASWClinicalSWStandards.pdf (accessed December 5, 2011).
———. 2011a. The advanced social worker in gerontology (ASW-G). http://www.socialworkers.org/credentials/specialty/asw-g.asp (accessed December 5, 2011).
———. 2011b. The certified clinical alcohol, tobacco, and other drugs social worker (C-CATODSW). http://www.socialworkers.org/credentials/specialty/c-catodsw.asp (accessed December 5, 2011).
———. 2011c. The clinical social worker in gerontology (CSW-G). http://www.socialworkers.org/credentials/specialty/csw-g.asp (accessed December 5, 2011).
———. 2011d. Social work profession. http://www.socialworkers.org/pressroom/features/general/profession.asp (accessed October 19, 2011).
———. 2011e. The social worker in gerontology (SW-G). http://www.socialworkers.org/credentials/specialty/sw-g.asp (accessed December 5, 2011).
———. 2012. Continuing education for social workers. http://www.socialworkers.org/ce/ (accessed April 10, 2012).
National Alliance for Caregiving and AARP. 2009. Caregiving in the U.S. 2009. http://www.caregiving.org/data/Caregiving_in_the_US_2009_full_report.pdf (accessed April 12, 2012).
National Clearinghouse on the Direct Care Workforce. 2004. Job duties and training requirements: Nursing assistants. http://www.directcareclearinghouse.org/dev/i_jobs_na.jsp (accessed December 12, 2011).
National Matching Services. 2011. Summary of programs and positions offered & filled by program type for the 2011 match. http://www.natmatch.com/ashprmp/ (accessed September 26, 2011).
NBOME (National Board of Osteopathic Medical Examiners). 2011. COMLEX-USA bulletin of information. http://www.nbome.org/docs/comlexBOI.pdf (accessed December 5, 2011).
NCCPA (National Commission on Certification of Physician Assistants). 2009a. Psychiatry—content blueprint. http://www.nccpa.net/Psychiatrycb.aspx (accessed September 27, 2011).
———. 2009b. Psychiatry CAQ. http://www.nccpa.net/Psychiatry.aspx (accessed September 27, 2011).
NCSBN (National Council of State Boards of Nursing). 2004. White paper on the state of the art of approval/accreditation processes in boards of nursing. https://www.ncsbn.org/Final_11_05_Approval_White_Paper.pdf (accessed December 5, 2011).
———. 2010a. 2010 NCLEX-RN detailed test plan. https://www.ncsbn.org/APRN_Consensus_Model_FAQs_August_19_2010.pdf (accessed October 12, 2011) ———. 2010b. APRN consensus model frequently-asked questions. https://www.ncsbn.org/APRN_Consensus_Model_FAQs_August_19_2010.pdf (accessed October 12, 2011).
———. 2011a. 2011 NCLEX-PN detailed test plan. https://www.ncsbn.org/2011_PN_DetailedTestPlan_Educator.pdf (accessed December 5, 2011).
———. 2011b. Fact sheet: Licensure of nursing and state boards of nursing. https://www.ncsbn.org/Fact_Sheet_Licensure_of_Nurses_and_State_Boards_of_Nursing.pdf (accessed April 9, 2012).
———. 2011c. The consensus model for APRN regulation: Licensure, accreditation, certification, and education. https://www.ncsbn.org/aprn.htm (accessed October 13, 2011).
North Dakota Board of Addiction Counseling Examiners. 2000. Licensure. http://www.ndbace.org/licensure.htm (accessed October 20, 2011).
O’Brien-Mazza, D., and M. Chinman. 2011. Peer support implementation in DVA mental health programs; maximizing the effectiveness of mental health services in the prevention of suicide. Paper presented at DoD/VA Suicide Prevention Conference, All the Way Home: Preventing Suicide in Service Members and Veterans, Boston, March 23.
Office of Inspector General. 2002. State nurse aide training: Program information and data. Report OEI-05-01-00031. HHS Region V, General Office of Evaluation and Inspections. http://www.directcareclearinghouse.org/download/OIGrpt_state_CNA_training_prgms.pdf (accessed April 15, 2012).
Ozga, M. 2012. Iowa direct-care workers may require license. http://phinational.org/archives/iowa-direct-care-workers-may-require-license/ (accessed April 6, 2012).
Partnership for Health in Aging. 2010. Multidisciplinary competencies in the care of older adults at the completion of the entry-level health professional degree. http://www.americangeriatrics.org/files/documents/pha/PHAMultidiscComps.pdf (accessed December 5, 2011).
Perry, K. M., and M. T. Boccaccini. 2009. Specialized training in APA accredited clinical psychology doctoral programs: Findings from a review of program websites. Clinical Psychology: Science and Practice 16(3):348-359.
PHI (Paraprofessional Health Care Institute). 2011. Facts 3. Who are direct-care workers? http://www.directcareclearinghouse.org/download/NCDCW%20Fact%20Sheet-1.pdf (accessed April 15, 2012).
Physician Assistant Education Association. 2009. Twenty-fifth annual report on physician assistant educational programs in the United States. Alexandria, VA: Physician Assistant Education Association. http://www.paeaonline.org/index.php?ht=a/GetDocumentAction/i/107753 (accessed December 5, 2011).
Pinquart, M., and S. Sorensen. 2005. Ethnic differences in stressors, resources, and psychological outcomes of family caregiving: A meta-analysis. Gerontologist 45(1):90-106.
POGOe (Portal of Geriatric Online Education). 2010. Geriatric nursing key concepts. http://www.pogoe.org/sites/default/files/Key%20concepts_GPNC.pdf (accessed December 5, 2011).
Professional Examination Service. 2011. Information for candidates examination in marital and family therapy. http://www.amftrb.org/PDF/info4candidate.pdf (accessed October 21, 2011).
Qualls, S. H., F. Scogin, R. Zweig, and S. K. Whitbourne. 2005a. Predoctoral training models in professional geropsychology. Training and Education in Professional Psychology 4(2):85.
Qualls, S. H., D. L. Segal, C. C. Benight, and M. P. Kenny. 2005b. Geropsychology training in a specialist geropsychology doctoral program. Gerontology & Geriatrics Education 25(4):21-40.
Resnick, S. G. 2010. Who attends Vet-to-Vet? Predictors of attendance in mental health mutual support. Psychiatric Rehabilitation Journal 33(4):262-268.
Resnick, S. G., M. Armstrong, M. Sperrazza, L. Harkness, and R. A. Rosenheck. 2004. A model of consumer-provider partnership: Vet-to-Vet. Psychiatric Rehabilitation Journal 28(2):185-187.
Rhett-Mariscal, W. 2008. Promotores in mental health in California and the prevention and early intervention component of the MHSA. http://www.cimh.org/LinkClick.aspx?fileticket=Qw5mqcEahTI%3d&tabid=568 (accessed April 12, 2012).
Robiner, W. N. 2006. The mental health professions: Workforce supply and demand, issues, and challenges. Clinical Psychology Review 26(5):600-625.
Ross, C. A., and E. M. Goldner. 2009. Stigma, negative attitudes and discrimination towards mental illness within the nursing profession: A review of the literature. Journal of Psychiatric and Mental Health Nursing 16(6):558-567.
SAMHSA (Substance Abuse and Mental Health Services Administration). 1999. Mental health: A report of the Surgeon General. http://profiles.nlm.nih.gov/ps/access/NNBBHS.pdf (accessed December 21, 2011).
———. 2011a. FY 2011 grant request for applications (RFA): Minority Fellowship Program (short title: MFP). http://www.samhsa.gov/Grants/2011/SM_11_005.aspx (accessed March 15, 2012).
———. 2011b. FY 2011 SAMHSA grant awards: CMHS/SM-11-005 Minority Fellowship Program. http://www.samhsa.gov/grants/2011/awards/sm_11_005.aspx (accessed April 6, 2012).
Sartorius, N., W. Gaebel, H. R. Cleveland, H. Stuart, T. Akiyama, J. Arboleda-Flórez, A. E. Baumann, O. Gureje, M. R. Jorge, and M. Kastrup. 2010. WPA guidance on how to combat stigmatization of psychiatry and psychiatrists. World Psychiatry 9(3):131.
Sengupta, M., L. D. Harris-Kojetin, and F. K. Ejaz. 2010. A national overview of the training received by certified nursing assistants working in U.S. nursing homes. Gerontology & Geriatrics Education 31(3):201-219.
Sirojudin, S., and A. Jacob. 2009. Mental health social work stipend program: Three-year outcome report, 2005-2008. University of California, Berkeley. http://calswec.berkeley.edu/CalSWEC/MH_StipendProgramReport_2009.pdf (accessed December 22, 2012).
SIS (Seniors in Sobriety). 2012. Seniors in Sobriety (SIS): A history. http://www.seniorsinsobriety.org/history.htm (accessed April 7, 2012).
Social Work Policy Institute. 2010. Social work services in nursing homes: Toward quality psychosocial care. http://www.socialworkpolicy.org/research/social-work-services-in-nursing-homes-toward-quality-psychosocial-care.html (accessed January 13, 2012).
South Carolina Lieutenant Governor’s Office on Aging. 2010. South Carolina geriatric loan forgiveness program. Columbia, SC. http://aging.sc.gov/providers/Pages/GeriatricLoanForgivenessProgram.aspx (accessed December 22, 2011).
———. 2011a. Geriatric loan forgiveness program. http://aging.sc.gov/providers/Pages/GeriatricLoanForgivenessProgram.aspx (accessed December 22, 2011).
———. 2011b. Geriatric loan forgiveness program application. http://aging.sc.gov/SiteCollectionDocuments/G/GLFApplication.pdf (accessed December 22, 2011).
Squillace, M. R., R. E. Remsburg, L. D. Harris-Kojetin, A. Bercovitz, E. Rosenoff, and B. Han. 2009. The National Nursing Assistant Survey: Improving the evidence base for policy initiatives to strengthen the certified nursing assistant workforce. Gerontologist 49(2):185-197.
Stanford Geriatric Education Center. 2004. Diversity, healing, and health care. http://www.bonshome.org/diversity/cohort/cohort1.htm (accessed November 1, 2011).
Stone, R., and Urban Institute Staff. 2011. Long-term care for the elderly. Washington, DC: Urban Institute Press.
Union of Pan Asian Communities. 2011. Elder multicultural access and support services: Prevention and early intervention report. EMASS Newsletter 2(4):1.
University of Washington Professional and Continuing Education. 2012. Certificate in geriatric mental health. http://www.pce.uw.edu/certificates/geriatric-mental-health/downtown-seattle-autumn-2012/?tab=Overview (accessed June 11, 2012).
Veterans Health Administration. 2011. Psychosocial rehabilitation and recovery services peer support. http://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=2430 (accessed April 12, 2012).
Voogt, S. J., M. Mickus, O. Santiago, and S. E. Herman. 2008. Attitudes, experiences, and interest in geriatrics of first]year allopathic and osteopathic medical students. Journal of the American Geriatrics Society 56(2):339-344.
Wallendal, M., R. Gramann, J. Kowalsky, K. Staehler, P. S. Davis, N. Amoroso, and R. Schroeder. 2009. Exposure to older adults influences social work student’s attitudes related to working in the field of aging. http://socialwork.nyam.org/nsw/students/journals/Exposure_to_Older_Adults_Influences_Social_Work_Students_Attitudes.pdf (accessed December 19, 2011).
Warshaw, G. A., E. J. Bragg, R. W. Shaull, and C. J. Lindsell. 2002. Academic geriatric programs in U.S. allopathic and osteopathic medical schools. JAMA 288(18):2313-2319.
Washkowiak, J., M. Wronski, L. K. Jones, E. Velasco, K. Schrubba, and S. J. Elliot. 2010. Occupational therapy’s role in skilled nursing facilities. Bethesda, MD. http://www.aota.org/Consumers/Professionals/WhatIsOT/RDP/Facts/SNFs.aspx (accessed April 12, 2012).
Weill Cornell Homecare Research Partnership. 2004. Depression screening tool kit. Weill Medical College of Cornell University. http://www.geriu.org/uploads/applications/DepressionInHomecare/ToolKit.pdf (accessed December 5, 2011).
Weill Medical College of Cornell University. 2004. Depression recognition and assessment in older homecare patients. http://www.geriu.org/uploads/applications/DepressionInHomecare/DinHomecare.html (accessed November 10, 2011).
Whitaker, T., T. Weismiller, and E. Clark. 2006. Assuring the sufficiency of a frontline workforce: A national study of licensed social workers. Special report: Social work services for older adults. Washington, DC: National Association of Social Workers.
Williams, D. R., H. M. Gonzalez, H. Neighbors, R. Nesse, J. M. Abelson, J. Sweetman, and J. S. Jackson. 2007. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: Results from the National Survey of American Life. Archives of General Psychiatry 64(3):305-315.
Wilson, R., S. C. Eaton, and A. Kamanu. 2003. Extended Care Career Ladder Initiative (ECCLI) round 2: Evaluation report. Cambridge, MA: Kennedy School of Government.
Wood, A. L., and O. F. Wahl. 2006. Evaluating the effectiveness of a consumer-provided mental health recovery education presentation. Psychiatric Rehabilitation Journal 30(1):46-53.
World Psychiatric Association and World Health Organization. 2002. Reducing stigma and discrimination against older adults with mental disorders: A technical consensus statement. Geneva. http://www.who.int/mental_health/media/en/499.pdf (accessed December 21, 2011).
This page intentionally left blank.


















































































