2
Implications of Health Care Reform for People with HIV in the United States
Health spending in the United States reached $2.79 trillion (seasonally adjusted annual rate) in April 2012, approximately 18 percent of the gross domestic product (GDP) (Center for Sustainable Health Spending, 2012), up from $2.59 trillion, 17.9 percent of the GDP, in 2010 (CMS, 2012, Table 1). U.S. health expenditures are the highest among 13 industrialized nations, whose health expenditures accounted for 12 percent or less of their GDPs in 2009 (Squires, 2012). Despite much higher spending, health care quality in the United States is not significantly better than that provided in less expensive systems (Squires, 2012). Higher health spending in the United States is likely a result of higher prices and, perhaps, more accessible technologies and greater levels of obesity (Squires, 2012).
At the same time as U.S. health expenditures continue to soar, 48.6 million people nationally (15.7 percent) lacked health insurance in 2011 (DeNavas-Walt et al., 2012),1 and 29 million adults under 65 years of age
_________________
1“For reporting purposes, the U.S. Census Bureau broadly classifies health insurance coverage as private coverage or government coverage. Private health insurance is a plan provided through an employer or a union or purchased by an individual from a private company. Government health insurance includes such federal programs as Medicare, Medicaid, and military health care; the Children’s Health Insurance Program (CHIP); and individual state health plans. [Types of insurance are not mutually exclusive; people may be covered by more than one during the year.] People were considered ‘insured’ if they were covered by any type of health insurance for part or all of the previous calendar year. They were considered ‘uninsured’ if, for the entire year, they were not covered by any type of health insurance” (DeNavas-Walt, 2012, p. 21).
were underinsured in 2010 (Schoen et al., 2011).2 Although the number and percent of uninsured decreased between 2010 and 2011, millions of people in the United States, including approximately one-third of those with HIV, still lack health insurance (HHS, 2012a). It is against this background that the Patient Protection and Affordable Care Act (ACA) (P.L. 111-148), as amended by the Health Care and Education Reconciliation Act of 2010 (P.L. 111-152), was signed into law on March 23, 2010. This chapter is not designed to provide a comprehensive and detailed review of all aspects of the ACA that have implications for people living with HIV but rather to highlight the aspects of the ACA that the committee anticipated would be most pertinent to its task, such as those that are likely to effect changes in sources of health coverage for that population and to establish the basis for the selection of data systems that would be most relevant to tracking the impact of the ACA on health coverage and care for people with HIV (e.g., Medicaid, Medicare, Ryan White HIV/AIDS Program, private insurers).
The ACA has the potential to significantly improve access to and quality of health care for the majority of people living with HIV in the United States. The law sets out numerous provisions that will be implemented over time, with major changes occurring in 2014. Most notably, the law includes both a provision that most citizens and legal residents of the United States must have qualifying health insurance coverage by 2014 or pay a tax penalty and a provision for the expansion of Medicaid coverage to most non–Medicare eligible individuals under age 65 with incomes less that 133 percent of the federal poverty level (FPL) (KFF, 2011a).3 The ACA includes additional provisions of particular importance to people with HIV, such as increased access to private health insurance and consumer protections, establishment of state or regional health insurance exchanges (the legislation uses the term “health benefit exchange”), gradual elimination of the Medicare Part D prescription drug coverage gap, and development of an “essential health benefits package” and improved coverage for preventive care services.4
_________________
2Individuals were identified as underinsured if they had health insurance for the full year but also had very high medical expenses relative to their income (Schoen et al., 2011). In this study, “health insurance” referred to private health insurance, Medicaid or some other type of state medical assistance for low-income people, Medicare, and “health insurance through any other source, including military or veteran’s coverage” (Commonwealth Fund, 2010, Questionnaire).
3A “mandatory income disregard” equal to 5 percent of the FPL will make the “effective income limit 138 percent of the FPL” (Natoli et al., 2011).
4Other major provisions of the ACA are not discussed here, including the development of accountable care organizations, increased payments for primary care providers, and expanded
In response to enactment of the ACA, Florida and 25 other states, the National Federation of Independent Business, and other interested parties filed suit challenging the constitutionality of the health insurance coverage requirement (“individual mandate”) and the Medicaid expansion, questions that were ultimately appealed to the U.S. Supreme Court. The Court heard oral arguments pertaining to the case in late March 2012 and issued its ruling upholding the insurance coverage requirement on June 28, 2012, finding that Congress has the authority to levy a tax on individuals who choose to forgo such coverage. With respect to the Medicaid expansion provision, the Court ruled that “Congress is not free … to penalize States that choose not to participate in that new program by taking away their existing Medicaid funding” but that “[n]othing in our opinion precludes Congress from offering funds under the Affordable Care Act to expand the availability of health care, and requiring that States accepting such funds comply with the conditions on their use.”5
In practice, the Court ruling makes it optional for the states to adopt the Medicaid expansion provision. Although some states already have taken steps to expand Medicaid before 2014 (as permitted by the ACA), other states, in the wake of the Supreme Court ruling, may choose not to do so at all. A compilation of statements by lawmakers, press releases, and media coverage indicates that as of September 12, 2012, 12 states and the District of Columbia had opted to expand Medicaid and 6 states had elected not to do so (Daily Briefing, 2012).
The six states identified as not participating in Medicaid expansion under the ACA had uninsurance rates above the national average of 44 percent for adults 19 to 64 years of age with incomes less than 139 percent of the FPL in 2010 (KFF, 2012e). One of the concerns raised by the variation in state adoption of Medicaid expansion is the potential lack of health coverage options for individuals who remain ineligible for Medicaid in states that opt out of Medicaid expansion but who have incomes below the level of eligibility for federal subsidies to purchase insurance coverage through the state exchanges (KFF, 2012a).
Despite the uncertainty surrounding what states ultimately might do, a number of the ACA’s provisions are expected to improve access to health care coverage not only for people living with HIV, but also for individuals living with other chronic medical conditions, such as diabetes, hypertension, rheumatoid arthritis, and the like. Several of these provisions have
_________________
service capacity at community health centers, including federally qualified health centers, which are an important source of care for people living with HIV who are less able to access traditional sources of medical care.
5National Federation of Independent Business v. Sebelius, 567 U.S. ___ (2012), 55, slip opinion.
been implemented already, and others are slated for implementation in 2014.6
HEALTH REFORM AND PEOPLE WITH HIV
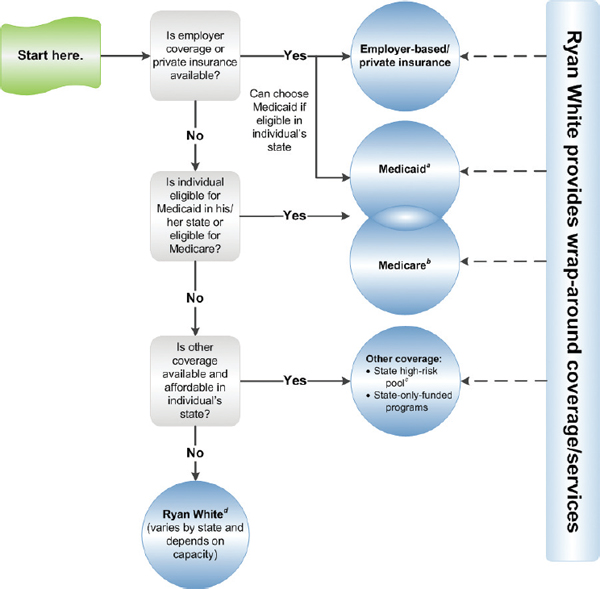
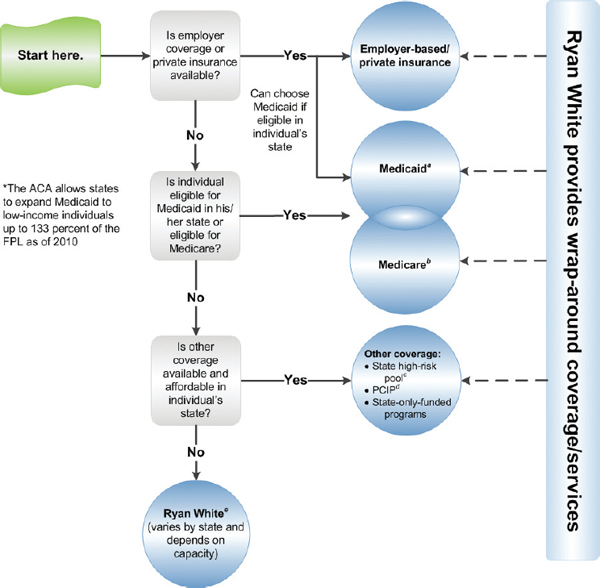
Among people with HIV in the United States, almost 30 percent have no health care coverage and only 17 percent have private insurance: the remaining 53 percent are covered by government programs such as Medicaid, Medicare, and the Ryan White HIV/AIDS Program (HHS, 2012a). As the ACA is implemented, most people with HIV in the United States will move into or shift between sources of care coverage. Figures 2-1, 2-2, and 2-3 depict the pathways to care coverage for people with HIV before, during, and following implementation of the ACA. As shown in Figure 2-2, as of 2010, the ACA gave states the option to expand Medicaid coverage to low-income adults up to 133 percent of the FPL regardless of disability or other status, which some states have done. In addition, individuals without access to employer-based coverage or who cannot purchase insurance in the individual market and are not eligible for Medicaid or Medicare can now purchase insurance through Preexisting Condition Insurance Plans (PCIPs) created under the ACA. PCIPs are high-risk pools operated by states or the federal government to provide insurance for individuals who are U.S. citizens or reside legally in the United States, have a preexisting condition, and have been without health coverage for at least 6 months.7 As depicted in Figure 2-3, beginning in 2014, low-income adults up to133 percent of the FPL become a new Medicaid-eligible group, although the Supreme Court has limited the authority of the federal government to enforce this provision, and therefore, eligibility for Medicaid coverage is likely to vary across states. Individuals without access to employer-based coverage who are not eligible for Medicaid or Medicare but are eligible for tax credits to purchase insurance and/or can afford to pay for health insurance may do so through state health insurance exchanges established to facilitate the purchasing of health insurance by qualified individuals and employers. As it did prior to the enactment of the ACA, the Ryan White HIV/AIDS Program continues to serve as a payer of last resort for people with HIV who are under- or uninsured. Federal funding is provided to states, cities, and providers but does not always match the number of people who need services or the cost of their care.
_________________
6Some provisions of the ACA apply to all health care plans, others (e.g., coverage for preventive care without cost sharing) do not apply or apply differently for grandfathered plans (i.e., those in which an individual was enrolled on March 23, 2010, the date the ACA was enacted).
7These criteria apply to people living in states served by the federally run PCIP (HHS, 2012b). State-run PCIPs have their own eligibility criteria.
aMedicaid eligibility (state-based): low-income and categorically eligible (disabled, pregnant women, children, medically needy); states may seek waivers to cover other groups (such as nondisabled, childless adults); must be a U.S. citizen or legal resident for at least 5 years. For current state eligibility requirements, see Kaiser Family Foundation (KFF), State Health Facts, Medicaid Income Eligibility Limits for Adults as a Percent of Federal Poverty Level, http://statehealthfacts.org/comparereport.jsp?rep=130&cat=4. For more information on Medicaid, see KFF, Medicaid: A Primer, http://www.kff.org/medicaid/7334.cfm.
bMedicare eligibility (national): ≥65, disabled (Social Security Disability Insurance [SSDI]) or end-stage renal disease; must be a U.S. citizen or legal resident for at least 5 years. For more information on Medicare, see KFF, Medicare: A Primer, http://www.kff.org/medicare/7615.cfm.
cState high-risk insurance pools: Prior to the ACA, health plans were permitted to deny coverage to individuals with pre-existing conditions or to charge them higher
premiums. Because of this, several states operate high-risk insurance pools, which provide health insurance to residents who are considered medically uninsurable and are unable to buy coverage in the individual market. See KFF, State Health Facts, State High Risk Pool Programs and Enrollment, http://www.statehealthfacts.org/comparetable.jsp?ind=602&cat=7.
dRyan White: The Ryan White HIV/AIDS Program, the single largest federal program designed specifically for people with HIV in the United States, provides care and services for people with HIV who are uninsured or underinsured, serving as payer of last resort. It includes the AIDS Drug Assistance Program (ADAP). Federal funding is provided to states, cities, and providers but may not match the number of people who need services or the cost of their care. For more information, see KFF, The Ryan White Program, http://www.kff.org/hivaids/7582.cfm.
SOURCE: Adapted from KFF, 2012b.
NOTE: The ACA provides new dependent coverage for children up to age 26 for all individual group policies. In addition, insurers are prohibited from denying coverage to children with preexisting conditions.
aMedicaid Eligibility (state-based): low-income and categorically eligible (disabled, pregnant women, children, medically needy); states may seek waivers to cover other groups (such as non-disabled, childless adults); must be a U.S. citizen or a legal resident for at least 5 years. As of 2010, the ACA gave states the option to expand coverage to low-income individuals up to 133 percent of the federal poverty level (FPL), regardless of disability or other status (which some states have done). For current state eligibility requirements and information on which states have moved to expand Medicaid as permitted by the ACA, see, Kaiser Family Foundation, State Health Facts, Medicaid Income Eligibility Limits for Adults as a Percent of Federal Poverty Level, http://statehealthfacts.org/comparereport.jsp?rep=130&cat=4. For more information on Medicaid, see, Kaiser Family Foundation, Medicaid: A Primer, http://www.kff.org/medicaid/7334.cfm.
bMedicare Eligibility (national): ≥65, disabled (SSDI), or end stage renal disease; must be a U.S. citizen or a legal resident for at least 5 years. Medicare beneficiaries are getting discounts on drugs while in the Medicare coverage gap and preventive services are covered without cost sharing. For more information on Medicare, see, Kaiser Family Foundation, Medicare: A Primer, http://www.kff.org/medicare/7615.cfm.
cState High-Risk Insurance Pools: Prior to the ACA, health plans were permitted to deny coverage to individuals with pre-existing conditions or to charge them higher premiums. Because of this, several states operate state high risk pools which provide health insurance to residents who are considered medically uninsurable and are unable to buy coverage in the individual market. See Kaiser Family Foundation, State Health Facts, State High Risk Pool Programs and Enrollment, http://www.statehealthfacts.org/comparetable.jsp?ind=602&cat=7. In addition, the ACA created the temporary PCIP program in 2010 (see below).
dPre-Existing Condition Insurance Plan (PCIP): Created by the ACA, PCIP is a temporary program that runs from 2010-2014 to provide health coverage to individuals with pre-existing medical conditions who have been uninsured for at least six months. The plan will be operated by the states or the federal government. For more information on the current status of PCIPs, see, Kaiser Family Foundation, State Health Facts, Pre-Existing Condition Insurance Plan: Operation Decisions and Preliminary Funding Allocations, http://www.statehealthfacts.org/comparemapreport.jsp?rep=67&cat=17.
eRyan White: The Ryan White HIV/AIDS Program, the single largest federal program designed specifically for people with HIV in the United States, provides care and services for people with HIV who are uninsured or underinsured, serving as payer of last resort. It includes the AIDS Drug Assistance Program (ADAP). Federal funding is provided to states, cities and providers but may not match the number of people who need services or the cost of their care. For more information, see, Kaiser Family Foundation, The Ryan White Program, http://www.kff.org/hivaids/7582.cfm.
SOURCE: Adapted from KFF, 2012b.
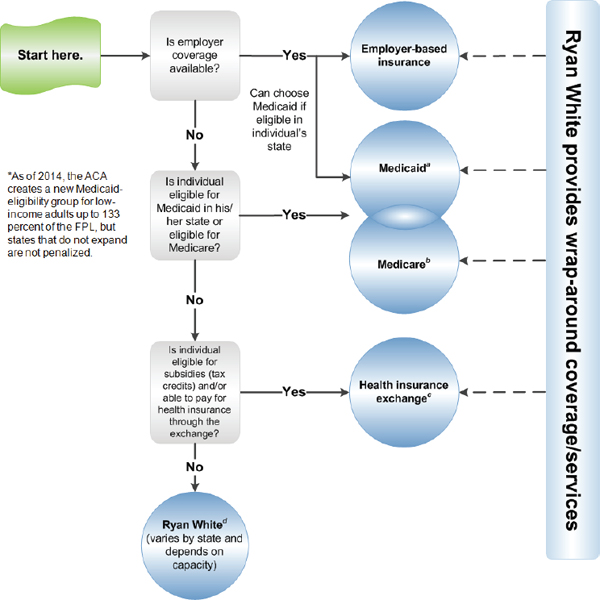
FIGURE 2-3 Pathways to coverage for people with HIV: Full implementation of the ACA, 2014 and beyond.
NOTE: The ACA provides new dependent coverage for children up to age 26 for all individual and group policies. Also, as of 2014, the ACA prohibits health plans from being able to deny coverage to people with pre-existing health conditions. Individuals with pre-existing conditions will be able to obtain insurance in the exchange or non-group market (the temporary PCIP program will no longer be needed).
aMedicaid eligibility (state-based): low-income and categorically eligible (disabled, pregnant women, children, medically needy); states may seek waivers to cover other groups (such as nondisabled, childless adults); must be a U.S. citizen or legal resident for at least 5 years. Under the ACA, as of 2014, low-income adults up to 133 percent of the FPL become a new Medicaid-eligibility group. The Supreme Court has limited the authority of the federal government to enforce this provision, making it uncertain whether all states will comply. For current state eligibility requirements and information on which states have moved to expand Medicaid as permitted by the ACA, see KFF, State Health Facts, Medicaid Income Eligibility
Limits for Adults as a Percent of Federal Poverty Level, http://statehealthfacts.org/comparereport.jsp?rep=130&cat=4. For more information on Medicaid, see KFF, Medicaid: A Primer, http://www.kff.org/medicaid/7334.cfm.
bMedicare eligibility (national): ≥65, disabled (SSDI) or end-stage renal disease; must be a U.S. citizen or legal resident for at least 5 years. For more information on Medicare, see KFF, Medicare: A Primer, http://www.kff.org/medicare/7615.cfm.
cHealth insurance exchange: A key component of the ACA, exchanges are entities that will be set up in states to facilitate the purchasing of health insurance by qualified individuals and employers. All legal, non-incarcerated residents are eligible to purchase insurance through the exchanges. Additionally, all legal, non-incarcerated residents are eligible for subsidies, in the form of tax credits, if they do not have access to employer-sponsored insurance, Medicaid, or Medicare, and their incomes are between 100 and 400 percent of the FPL. In addition, if an employer plan does not cover at least 60 percent of average health expenses or the employee must pay more than 9.5 percent of his/her income for the premium, individuals, depending on income, may be eligible for a tax credit to offset premiums for coverage purchased through an exchange. Exchanges are required to be fully operational in every state by 2014. See KFF, State Health Facts, State Action Toward Creating Health Insurance Exchanges, http://www.statehealthfacts.org/comparemaptable.jsp?ind=962&cat=17.
dRyan White: The Ryan White HIV/AIDS Program, the single largest federal program designed specifically for people with HIV in the United States, provides care and services for people with HIV who are uninsured or underinsured, serving as payer of last resort. It includes ADAP. Federal funding is provided to states, cities, and providers but may not match the number of people who need services or the cost of their care. For more information, see KFF, The Ryan White Program, http://www.kff.org/hivaids/7582.cfm.
SOURCE: Adapted from KFF, 2012b.
The provisions of the ACA discussed in the following sections are likely to have the greatest impact on care and care coverage for people with HIV.
Pre-Existing Conditions, Rescission, and Limits on Coverage
Currently, children with pre-existing medical conditions (e.g., HIV/AIDS, diabetes) no longer can be denied health care insurance coverage (Keith et al., 2012; KFF, 2011a).8 Beginning in 2014, insurers also will no longer be able to deny coverage to or charge higher premiums for adults
_________________
8In addition, coverage must now be extended for dependent children on parental policies up to age 26 (Keith et al., 2012; KFF, 2011a). Since young adults, ages 20 to 29, have the highest rates of new HIV diagnoses among all age groups in the United States (CDC, 2012, Table 1a), extension of coverage for older dependent children is a potentially important source of coverage for HIV care for this population.
with pre-existing conditions. In the interim, adults with pre-existing conditions who have been without health coverage for at least 6 months are eligible to purchase coverage through federal or state-run, high-risk PCIPs (Figure 2-2; KFF, 2011a). In addition, insurance providers no longer can rescind coverage due to health status, except in cases of fraud or intentional misrepresentation (Keith et al., 2012; KFF, 2011a). The ACA also prohibits the imposition of lifetime dollar limits on coverage for essential health benefits and restricts and phases out annual dollar limits on coverage for essential health benefits, unless waived by the Department of Health and Human Services (HHS).9 Waivers for annual dollar limits on coverage will be discontinued in 2014, eliminating annual dollar limits on coverage for all plans in small- and large-group markets (Keith et al., 2012).
Medicaid Expansion
Medicaid currently is the largest single source of health care coverage for people living with HIV, providing coverage for 47 percent of HIV-infected individuals estimated to be receiving regular medical care (Kates, 2011, p. 1). In fiscal year 2007, 212,892 Medicaid beneficiaries were HIV-positive (Kates, 2011, p. 1). In states that choose to expand their Medicaid program as allowed under the ACA, Medicaid eligibility will be extended to most “non-Medicare eligible individuals under age 65 (children, pregnant women, parents, and adults without dependent children)” with incomes up to 133 percent of the FPL (Figure 2-3; KFF, 2011a).10 Currently, most Medicaid beneficiaries with HIV (74 percent) qualify through the disability pathway, meaning their disease is sufficiently advanced to preclude them from working (Kates, 2011, p. 4). With Medicaid expansion, as passed by law under the ACA, low-income individuals who have HIV, including those without dependent children (“childless adults”), will be eligible for Medicaid before their disease becomes disabling. For those who become newly eligible for Medicaid, the federal government will assume 100 percent of Medicaid costs during 2014-2016, phased down to a minimum of 90 percent thereafter.
Where Medicaid is expanded, particularly if coupled with more effective enrollment of currently eligible individuals, it is expected that there could be as many as 11.6 million new people entered into the Medicaid system in 2014 and 20 million by 2019, representing 21 and 34 percent increases, respectively, over pre-ACA projections (CMS, 2010). It is anticipated that the majority of individuals with HIV who currently receive clinical or related
_________________
9A discussion of “essential health benefits” is included later in the chapter.
10Recent (less than 5 years in the United States) and undocumented immigrants will remain ineligible for Medicaid.
supportive service care and prescription drug assistance through the Ryan White HIV/AIDS Program (>500,000) will become eligible for Medicaid in 2014 (KFF, 2011b; NASTAD, 2012b; Project Inform, 2012). The implications of this coverage shift are discussed later in this chapter.
Health Insurance Exchanges
The ACA also mandates the establishment of state or regional health insurance exchanges by January 2014 (Figure 2-3). The exchanges are meant to provide a marketplace in which eligible individuals and small businesses (less than 100 employees) can easily obtain and compare information on different health insurance options and purchase insurance coverage (KFF, 2011a). Individuals and families with incomes between 100 and 400 percent of the FPL will be eligible for federal subsidies to help cover insurance premiums and out-of-pocket health care costs (KFF, 2011a).
Medicare Part D Drug Coverage Gap
Medicare Part D prescription drug plans currently contain a coverage gap (“donut hole”) that can impose significant financial burdens on enrollees. Prior to the enactment of the ACA, Medicare Part D beneficiaries were required to pay the full cost of their prescription drugs while in the coverage gap between the time they and their drug plans spent a specified dollar amount on covered drugs and the time beneficiaries’ “true out-of-pocket” (TrOOP) costs reached the threshold catastrophic coverage. Of importance specifically for people with HIV, AIDS Drug Assistance Program (ADAP) benefits now count toward Medicare Part D recipients’ TrOOP costs for medications, allowing them to move through the coverage gap more quickly. Additional ACA provisions will ease the burden of out-of-pocket drug costs for all individuals in the donut hole. Currently, pharmaceutical manufacturers are required to provide a 50 percent discount on prescriptions of brand name medications filled in the gap, and the beneficiary coinsurance rate will be reduced from 100 percent to 25 percent by 2020 (KFF, 2011a).
Essential Health Benefits Package and Preventive Care
The ACA charges HHS with establishing an “essential health benefits package” within specified parameters whose scope “is equal to the scope of benefits provided under a typical employer plan, as determined by the [HHS] Secretary” (P.L. 111-148, Sec. 1302 [42 U.S.C. 18022]). At a minimum, the essential health benefits package must include items and services in 10 areas of care: ambulatory patient services; emergency services; hospitalization; maternity and newborn care; mental health and substance use
disorder services, including behavioral health treatment; prescription drugs; rehabilitative and habilitative services and devices; laboratory services; preventive and wellness services and chronic disease management; and pediatric services, including oral and vision care (P.L. 111-148, Sec. 1302 [42 U.S.C. 18022]). HHS decided to allow each state the flexibility to select a plan from several options to serve as the benchmark for the essential health benefits package in that state.11 Services covered by the benchmark plan in each of the 10 mandated areas become the essential benefits for plans in that state (Cassidy, 2012).
Health plans within and outside of the health insurance exchanges, except grandfathered plans, must provide, at a minimum, coverage for the essential benefits package of at least 60 percent of the actuarial value of the covered benefits, with limits on annual cost sharing (KFF, 2011a). Medicaid programs within states that implement the expansion provision of the ACA also must provide benefits comparable to those in the essential health benefits package to newly eligible adults (KFF, 2011a).
As of 2010, the ACA improves preventive care coverage by eliminating cost sharing within Medicare for preventive services recommended by the U.S. Preventive Services Task Force (USPSTF) (i.e., services rated A or B) and requiring health plans to provide the same services without cost sharing, as well as recommended immunizations, pediatric and adolescent preventive care, and preventive care and screenings for women (KFF, 2011a). The ACA also offers incentives to states in which Medicaid covers USPTF A- and B-rated services and recommended immunizations without cost sharing (KFF, 2011a).
Although the ACA establishes federal mandates and standards regarding health insurance, states are among those entities responsible for implementing some of the most significant changes, such as establishment of state health insurance exchanges and whether to accept the Medicaid expansion provision.12Box 2-1 lists some of areas in which state variation in implementation of the ACA is anticipated.
_________________
11States may choose as their benchmark “one of the three largest small group plans in the state by enrollment, one of the three largest state employee health plans by enrollment, one of the three largest federal employee health plan options by enrollment, or the largest health maintenance organization (HMO) plan offered in the state’s commercial market by enrollment” (Cassidy, 2012).
12Most of the consumer protection and insurance reform provisions of the ACA apply to the U.S. territories as well as states and the District of Columbia, although there are some differences (NASTAD, 2012a). People residing in the territories are exempt from the individual mandate, and the territories are not required to establish health insurance exchanges, although
- Expansion of Medicaid to childless adults up to 133 percent FPLa
- Specific services included in “essential benefits” packages
- Restrictions on Medicaid-covered servicesb
- Federal versus state oversight of pre-existing conditions insurance plans
- Federal versus state oversight of health benefits exchanges
- Mechanisms (e.g., websites) to facilitate client enrollment into public and private insurance
- Inclusion of pilot programsc
- Regionalized Systems for Emergency Care Pilots: Sec. 3504
- Healthy Aging, Living Well Pilot Program: Sec. 4202
- Environmental Health Hazards Primary Pilot Program: Sec. 10323
- National Pilot Program on Payment Bundling: Sec. 3023
_________________
aEligibility requirements currently vary widely from state to state and likely will continue to do so. Some states have programs with FPL cutoffs higher than 133 percent, and others will continue to have less generous eligible criteria.
bThis already occurs, such as limits on the number of prescriptions per month, or preauthorization for specific medications.
cThe implementation of pilot programs is not subject to state choice.
Some states are in a better starting position than others to implement the ACA. Massachusetts, for example, enacted health reform legislation in 2006 that is similar to the ACA, including an individual mandate, Medicaid expansions, subsidized private insurance coverage, and a purchasing pool (Long and Masi, 2009). Vermont enacted single-payer health care legislation in 2011. Although the Vermont system, when implemented, may provide benefits equivalent to or better than those provided under the ACA, the state has also established a health insurance exchange to fulfill the ACA mandate until it can apply for a waiver once the single-payer system is implemented (Hsiao et al., 2011; KFF, 2012d, Vermont). New York State already has in place a number of the protections for health insurance
_________________
tablish an insurance exchange will receive additional funding for their Medicaid programs. Medicaid programs in the territories operate under broad federal guidelines but with different funding and coverage requirements. The ACA does increase the amount of federal Medicaid cap in these areas, resulting in more federal money for their Medicaid programs. Among the U.S. territories and dependent areas, health reform in Puerto Rico and the U.S. Virgin Islands will have the greatest effect on people living with HIV due to the high prevalence of HIV in those areas.
consumers included in the ACA (NYS, 2012), such as guaranteed issue. In 1974, Hawaii became the first state to create a near universal health care system, requiring most employers to provide health care coverage to eligible employees and setting minimum standards for the coverage benefits (State of Hawaii, 2012).
States have used waivers to extend Medicaid benefits to at least some portion of their “childless adult” population (MACPAC, 2012, pp. 108-110, Table 10). In addition, states have different income thresholds for eligibility, ranging from well below 100 percent of the FPL to well above 133 percent of the FPL, although in some cases the benefits covered may be more limited than those provided under the regular state plan (KFF, 2012f). Among the states that choose to implement the Medicaid expansion provision of the ACA, those that already have more generous Medicaid eligibility requirements may experience fewer changes in their programs than those that have not. State Medicaid programs also vary in the scope of their benefits. For example, some states limit the number of prescriptions covered per month or require preauthorization for certain medications.
States also are at different stages regarding implementation of their health insurance exchanges. Table 2-1 summarizes state action on establishing exchanges as of November 19, 2012. At that time, seventeen states and the District of Columbia had established exchanges; six states had decided to pursue the establishment of a federal–state partnership exchange; and sixteen states had defaulted to a federal exchange (KFF, 2012c). Eleven states were still undecided (KFF, 2012c).13
OPPORTUNITIES, CHALLENGES, AND LIMITATIONS
The ACA offers great opportunities for significant expansion of access to health care, improved health outcomes, and emphasis on preventive care for millions of Americans including most of the almost 30 percent of people living with HIV who currently lack any form of health care coverage (CMS, 2010; HHS, 2012a). States such as Massachusetts and Vermont have enacted sweeping health reform initiatives independent of the ACA, and many other states have taken various actions to increase access to health care. Despite their promise to increase access to health care and improve the health of people living with HIV, health reform efforts under the ACA also raise numerous challenges.
Economic sustainability is one challenge of health reform efforts that include expanded access, guaranteed coverage, and the removal of dollar limits on benefits. The requirement that most individuals be insured or pay
_________________
13Detailed health exchange profiles for each state are available at http://healthreform.kff.org/State-Exchange-Profiles-Page.aspx (accessed June 26, 2012).
TABLE 2-1 State Action Toward Creating Health Insurance Exchanges, November 19, 2012
| Declared State-Based Exchange (17 + DC) | Planning for Partnership Exchange (6) | Default to Federal Exchange (16) | Undecided (11) |
| California, Colorado, Connecticut, Hawaii, Iowa, Kentucky, Maryland, Massachusetts,a Minnesota, Mississippi, Nevada, New Mexico, New York, Oregon, Rhode Island, Vermont, Washington | Arkansas, Delaware, Illinois, Michigan, North Carolina, Ohio | Alabama, Alaska, Georgia, Kansas, Louisiana, Maine, Missouri, Nebraska, New Hampshire, North Dakota, Oklahoma, South Carolina, South Dakota, Texas, Wisconsin, Wyoming | Arizona, Florida,b Idaho, Indiana, Montana, New Jersey, Pennsylvania, Tennessee, Utah,a Virginia, West Virginia |
| District of Columbia | |||
aPassed laws prior to the enactment of the ACA in March 2010, but not yet decided on implementing an ACA-compliant exchange.
bAlthough not compliant with the ACA, Florida is proceeding with plans that predate passage of the ACA to establish an insurance marketplace for small businesses (KFF, 2012d, Florida).
SOURCE: KFF, 2012c.
a tax is designed to bring young and healthy individuals into the insurance pools, which will help to offset the increased costs associated with expanded access and increased benefits. To be economically sustainable, sufficient numbers of such “low-risk” individuals will have to enter the insurance pools or the tax levied on those who fail to do so will have to be sufficient to offset the additional cost burden.
Another challenge raised by health care reform is that increased access to health care coverage under the ACA will facilitate but not ensure linkage to, retention in, and provision of quality clinical HIV care for people living with HIV. Although the number of uninsured HIV-infected individuals will decrease, people near the eligibility borders may be expected to “churn” (i.e., move back and forth) between different sources of coverage, which may affect the continuity of their care and the package of benefits for which they are eligible at any given time. Such movement may be especially pronounced between Medicaid and state insurance exchanges, affecting individuals at 125 to 135 percent of the FPL. Ensuring continuity of clinical HIV care and supportive services throughout movement across sources of coverage is important for improving individual health outcomes and reducing the risk of transmitting the virus to others. Maintaining formerly incarcerated individuals in clinical HIV care as they transition from the prison health care system to mainstream sources of health coverage is similarly important.
Movement of individuals from the Ryan White HIV/AIDS Program (as their primary source of coverage for HIV care) into Medicaid or other sources of coverage may affect the scope of services they receive. Given the significant interstate variation in Medicaid benefits, for example, some Ryan White HIV/AIDS Program clients might experience a reduction in services under Medicaid. In addition, the Ryan White HIV/AIDS Program covers many nonclinical services, such as food and nutrition, transportation, child care, and case management services, that are important to the success of clinical HIV care. To the extent that individuals no longer receive such supportive services when they move to other sources of coverage, their clinical service utilization and health outcomes may be negatively affected.
In addition to concerns about individuals maintaining access to continuous, high-quality clinical HIV care and supportive services, some people living with HIV in the United States, such as recent and undocumented immigrants, will remain ineligible for health coverage under the ACA and will continue to face challenges in accessing needed health care services.
Another challenge pertains to the availability of sufficient health care services to meet the anticipated increase in demand. The influx of new patients into the health care system, especially individuals with chronic diseases such as HIV who were previously unable to obtain coverage, can be expected to place additional burdens on an already strained system. A
2011 Institute of Medicine report assessing the capacity of the U.S. health care system to accommodate increased HIV testing and provision of care found that the HIV health care “workforce is decreasing relative to the number of individuals expected to require care” (IOM, 2011, p. 39). The number of HIV-infected individuals needing care will continue to grow with ongoing new infections; increases in HIV testing, diagnosis, and linkage to care; increased survival; and increased access to care as a result of health reform efforts. At the same time, many professionals engaged in HIV care are nearing retirement, and insufficient numbers of new practitioners proficient in HIV care are entering the workforce to accommodate the growing need (HRSA, 2010; IOM, 2011). Fiscal constraints are further decreasing the system’s capacity to provide care for more people with HIV (IOM, 2011).
The possibility of “churning” between coverage sources, the movement of individuals from the Ryan White HIV/AIDS Program into other subsidized programs, and concerns about the availability of competent health care services sufficient to meet the needs of people living with HIV underscore the importance not only of tracking changes in health care coverage for people with HIV but also of monitoring service utilization and care quality using indicators such as those recommended in the committee’s first report (IOM, 2012).
Cassidy, A. Health Policy Brief: Essential health benefits. Health Affairs, April 25. http://healthaffairs.org/healthpolicybriefs/brief_pdfs/healthpolicybrief_68.pdf (accessed July 17, 2012).
CDC (Centers for Disease Control and Prevention). 2012. Diagnoses of HIV infection and AIDS in the United States and dependent areas, 2010. HIV Surveillance Report. Volume 22. March. http://www.cdc.gov/hiv/surveillance/resources/reports/2010report/index.htm (accessed July 3, 2012).
Center for Sustainable Health Spending, Altarum Institute. 2012. Health Sector Economic Indicators.SMInsights from Monthly National Health Expenditure Estimates through April 2012. Spending Brief #12-06: April 2012 Data (June 7). http://www.altarum.org/files/imce/CSHS-Spending-Brief_June%202012_060612.pdf (accessed June 20, 2012).
CMS (Centers for Medicare & Medicaid Services). 2010. 2010 Actuarial Report on the Financial Outlook for Medicaid. https://www.cms.gov/ActuarialStudies/downloads/MedicaidReport2010.pdf (accessed March 29, 2012).
CMS. Office of the Actuary, National Health Statistics Group. 2012. National Health Care Expenditures Data. https://www.cms.gov/Research-Statistics-Data-and-Systems/StatisticsTrends-and-Reports/NationalHealthExpendData/downloads/tables.pdf (accessed June 20, 2012).
Commonwealth Fund. The Commonwealth Fund 2010 Biennial Health Insurance Survey. http://www.commonwealthfund.org/Surveys/2011/Mar/2010-Biennial-Health-InsuranceSurvey.aspx (accessed August 16, 2012)
Daily Briefing. 2012. Where Each State Stands on ACA’s Medicaid Expansion: A Roundup of What Each State’s Leadership Has Said About Their Medicaid Plans. http://www.advisory.com/Daily-Briefing/2012/07/05/Where-each-state-stands-of-the-Medicaidexpansion (accessed September 17, 2012).
DeNavas-Walt, C., B. D. Proctor, and J. C. Smith. 2012. Income, Poverty, and Health Insurance Coverage in the United States: 2011. U.S. Census Bureau, Current Population Reports, P60-243. Washington, DC: U.S. Government Printing Office.
HHS (U.S. Department of Health and Human Services). 2012a. How Does the Affordable Care Act Impact People Living with HIV/AIDS. http://aids.gov/federal-resources/policies/health-care-reform/ (accessed July 16, 2012).
HHS. 2012b. Who’s Eligible for PCIP Coverage? https://pcip.gov/Who’s_Eligible.html (accessed September 17, 2012).
HRSA (Health Resources and Services Administration). 2010. Workforce capacity in HIV. HRSA Care Action (April):1-12.
Hsiao, W. C., A. G. Knight, S. Kappel, and N. Done. 2011. What other states can learn from Vermont’s bold experiment: Embracing a single-payer health care financing system. Health Affairs 30(7):1232-1241.
IOM (Institute of Medicince). 2011. HIV Screening and Access to Care: Health Care System Capacity for Increased HIV Testing and Provision of Care. Washington, DC: The National Academies Press.
IOM. 2012. Monitoring HIV Care in the United States: Indicators and Data Systems. Washington, DC: The National Academies Press.
Kates, J. 2011. Medicaid and HIV: A National Analysis. Washington, DC: Henry J. Kaiser Family Foundation. http://www.kff.org/hivaids/upload/8218.pdf (accessed January 11, 2012).
Keith, K., K. W. Lucia, and S. Corlette. 2012. Implementing the Affordable Care Act: State action on early market reforms. Issue Brief 6 (March). Publication 1586. Commonwealth Fund.
KFF (Kaiser Family Foundation). 2011a. Focus on Health Reform: Summary of the New Health Reform Law. Publication 8061. http://www.kff.org/healthreform/upload/8061.pdf (accessed March 30, 2012).
KFF. 2011b. The Ryan White Program. HIV/AIDS Policy Fact Sheet. Publication 7582-06. http://www.kff.org/hivaids/upload/7582-06.pdf (accessed June 26, 2012).
KFF. 2012a. Focus on Health Reform: A Guide to the Supreme Court’s Affordable Care Act Decision. Publication 8332. http://www.kff.org/healthreform/upload/8332.pdf (accessed July 18, 2012).
KFF. 2012b. How the ACA Changes Pathways to Insurance Coverage for People with HIV. http://healthreform.kff.org/notes-on-health-insurance-and-reform/2012/september/how-the-aca-changes-pathways-to-insurance-coverage-for-people-with-hiv.aspx (accessed September 18, 2012).
KFF. 2012c. State Action Toward Creating Health Insurance Exchanges, as of November 19, 2012. http://statehealthfacts.kff.org/comparemaptable.jsp?ind=962&cat=17 (accessed November 20, 2012).
KFF. 2012d. State Health Exchange Profiles. http://healthreform.kff.org/State-ExchangeProfiles-Page.aspx (accessed June 27, 2012).
KFF. 2012e. State Health Facts: Health Insurance Coverage of Adults (19-64) with Incomes Under 139% of the Federal Poverty Level (FPL), States (2009-2010), U.S. (2010). http://www.statehealthfacts.org/comparetable.jsp?ind=779&cat=3 (accessed July 18, 2012).
KFF. 2012f. State Health Facts: Income Eligibility Limits for Working Adults at Application as a Percent of the Federal Poverty Level (FPL) by Scope of Benefit Package, January 2012. http://www.statehealthfacts.org/comparereport.jsp?rep=54&cat=4#notes-1 (accessed March 29, 2012).
Long, S. K., and P. B. Masi. 2009. Access and affordability: An update on health reform in Massachusetts, Fall 2008. Health Affairs 28(4):w578-w587.
MACPAC (Medicaid and CHIP Payment and Access Commission). 2012. Report to the Congress on Medicaid and CHIP. March. http://www.macpac.gov/reports (accessed September 5, 2012).
NASTAD (National Alliance of State and Territorial AIDS Directors). 2012a. Frequently Asked Questions on Health Reform, August 2012. http://www.nastad.org/Docs/014950_NASTAD,%20Health%20Reform%20FAQs%20August%202012.pdf (accessed September 17, 2012).
NASTAD. 2012b. National ADAP Monitoring Project Annual Report. http://www.nastad.org (accessed June 26, 2012).
Natoli, C., V. Cheh, and S. Verghese. 2011. Who will enroll in Medicaid in 2014? Lessons from Section 1115 Medicaid waivers. Medicaid Policy Brief (1). Mathematica Policy Research.
NYS (New York State). 2012. Federal Health Care Reform in New York State: Summary of Health Care Reform. http://www.healthcarereform.ny.gov/summary (accessed March 29, 2012).
Project Inform. 2012. Frequently Asked Questions: Health Care Reform and People Living with HIV. http://www.projectinform.org/pdf/hcr_faq.pdf (accessed March 30, 2012).
Schoen, C., M. M. Doty, R. H. Robertson, and S. R. Collins. 2011. Affordable Care Act reforms could reduce the number of underinsured U.S. adults by 70 percent. Health Affairs 30(9):1762-1771.
Squires, D. A. 2012. Explaining high health care spending in the United States: An international comparison of supply, utilization, prices, and quality. Issues in International Health Policy 10 (May). Publication 1595. Commonwealth Fund.
State of Hawaii. Department of Labor and Industrial Relations. 2012. About PrePaid Health Care. http://hawaii.gov/labor/dcd/aboutphc.shtml (accessed September 17, 2012).