5
Observations on the Larger Policy Context
This report assessed the potential impact of changes in provider payment on access to health care and quality of care that would result from implementing the committee’s proposed revisions of Medicare geographic adjustment factors. The relevant existing literature is based on research conducted primarily in a fee-for-service Medicare payment environment where provider revenue depends on price per unit of service combined with volume of services delivered. In this environment, the concern is that any change in price per unit, such as could be experienced by a change in Medicare’s geographic adjustment factor, could change provider behavior.
In particular, in areas where implementation of the proposed changes in geographic adjustments would result in lower per-unit prices, there have been concerns that providers would accept fewer Medicare patients or move to geographic areas where payment adjustments are more favorable, creating access problems for Medicare beneficiaries, or that they could reduce quality to maintain incomes in the face of lower payments.
The committee did not find any evidence, either from its review of the literature, its payment simulations, or its analysis of beneficiary survey data, that changes in geographic adjustment could have an impact on quality of care. The committee also did not find that any specific type of hospital would be disproportionately advantaged or disadvantaged by using the technically more accurate index it recommended, with the exception of the hospitals operating under policy adjustments such as market reclassifications and floors.
However, the payment simulations did show that implementation of the recommended changes to payment areas for physicians would result in payment redistribution from nonmetropolitan to metropolitan areas, although there was wide variation in the estimated payment changes. While the committee noted that many of the rural practitioners in Health Professional Shortage Areas (HPSAs) would be eligible for primary care bonuses through Medicare, which might partially offset the proposed reductions, the committee was concerned about the impact of its recommendations on practitioners and beneficiaries in HPSAs. This impact will need to
be further evaluated in the future and addressed through another policy mechanism, but not through geographic adjustment.
This chapter briefly addresses two overarching policy issues that arose many times during the committee’s deliberations—the overall effect that certain Medicare payment policies may have on the geographic distribution of the health care workforce, and the clear evidence of disparities in the care provided in different geographic areas, which in turn may be reflected in the health of the population in different areas.
Because of its sheer size and influence on providers and other payers, Medicare tends to be seen as a policy driver in discussions of health care delivery reform. The committee discussed two features of Medicare’s fee-for-service payment systems—the manner in which fees for services are established and the subsidization of graduate medical education (GME).
Disparities are especially important to consider in the context of analysis that uses averages to compare and contrast different areas. This is so because averages have a tendency to obscure potentially important differences in the well-being of racially and ethnically distinct populations in local communities.
While the committee does not offer recommendations on disparities and these features of Medicare payment policies, it believes that serious debate over geographic access to care, including workforce policy, needs to take them into account.
UNINTENDED EFFECTS OF MEDICARE PAYMENT POLICIES
During its Phase I deliberations, when the committee was focused on Medicare geographic adjustments to fee-for-service provider payments, several committee members observed that there were other important features of Medicare payment that affect the distribution of Medicare dollars among Medicare providers and geographic areas. The committee eventually decided that the fee-for-service geographic adjustments should be used only to adjust payments for underlying geographic differences in the costs of providing services, and several recommendations were offered that would improve the current system in achieving that objective (IOM, 2011).
However, during Phase II, the committee discussed other aspects of Medicare payment that could be appropriate targets for payment reform to improve geographic access to high-quality health care. These discussions centered on the Medicare fee schedule for physicians and other individual practitioners and on the supplemental payments to hospitals to subsidize the costs of GME.
Fee-for-Service Payment
In Chapter 2 of this report, the committee examined statistical simulations of its recommended changes to geographic adjustments to Medicare payments to clinical practitioners and considered how the changes might affect Medicare beneficiary access to health care. Known individually as the geographic practice cost indexes (GPCIs) and collectively as the geographic adjustment factor, the physician fee schedule adjustments are applied to the fees that Medicare pays physicians and other practitioners who are authorized to bill for services under Medicare (IOM, 2011). Over the course of its deliberations, the committee came to realize that the ways that Medicare sets its national fees, before geographic adjustments are applied, may have consequences for beneficiary access to health services through their influence on professional income and medical specialty choice.
Practitioners are currently paid under the Resource-based Relative Value Scale (RBRVS) system. Medicare established the RBRVS in 1992 to replace the Customary-Prevailing-Reasonable method of setting fees. The RBRVS comprises approximately 7,000 services, each of which is assigned a number of relative value units (RVUs) that determine the amount any given service is paid compared to any other service. For example, a service that is assigned 20 RVUs is paid twice as much as a service that is assigned 10 RVUs. Once a dollar conversion factor is determined, a national fee schedule in dollar terms is established. Both the conversion factor and the RVUs, including adding RVUs for newly covered services, typically are updated once per year.
The committee observed that an unintended consequence of the way Medicare sets its national fees may be leading to shortages of both primary care and specialists in rural and other underserved areas. The 10 percent primary care bonus that is in effect from January 1, 2011, to December 31, 2015, may not be sufficient to address the inherent limitations of the RBRVS system for primary care. Although it is beyond the scope of this study to analyze the RBRVS and how the RVUs are determined and updated, several researchers and studies have concluded that the RBRVS tends to undervalue primary care services and overvalue specialty services in relative terms (e.g., Berenson et al., 2010; MedPAC, 2010, 2011). That is, evaluation and management services tend to yield far less Medicare income than procedures and tests, which in turn has contributed to a substantial income gap between primary care practitioners and specialists (Bodenheimer et al., 2007).
As discussed in Chapter 4, differences in earnings for primary and specialty care may have consequences for access to care because of their influence on specialty and practice location choices, in that specialists tend to locate their practices in areas with larger populations. Figure 5-1 illustrates the differences in primary care billings for metropolitan and nonmetropolitan areas. More than 60 percent of all RVUs billed in nonmetropolitan areas are from primary care services. In contrast, primary care services account for about 20 percent of all RVUs billed in metropolitan areas.
In 2006, the American Medical Association RVU Update Committee established a workgroup to identify potentially misvalued services using objective mechanisms for reevaluation (AMA, 2012), and many services, such as low-value/high-volume procedure codes, have been reviewed. Approximately $1 billion was redistributed in 2011 related to the physician work and practice expense RVUs (AMA, 2012), although some observers regarded that amount as far short of what might have been done. More recently, the Affordable Care Act requires the secretary of HHS to periodically review and identify potentially misvalued codes and make appropriate adjustments to the relative value of services, as well as to establish a formal process to validate RVUs under the physician fee schedule.
The committee therefore agreed that a reevaluation of the accuracy of the RVUs, as has been proposed by the Medicare Payment Advisory Commission (MedPAC), seems desirable in view of geographic variations in practice locations and their implications for access to care.
Financing GME
Medicare is the single largest source of funding for GME, spending $9.5 billion in 2009 (MedPAC, 2010). By contrast, in FY 2010, the Health Resources and Services Administration (HRSA) spent a combined amount of $532 million to fund the National Health Service Corps and more than 40 health professions education programs authorized under Title VII and Title VIII of the Public Health Service Act (GAO, 2006; Salinsky, 2010).
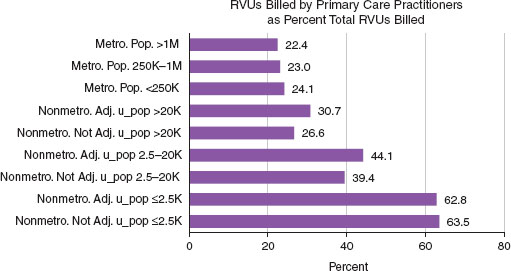
FIGURE 5-1 Primary care billings reflect a higher proportion of total RVUs in nonmetropolitan areas.
NOTE: The figure is based on the share of national total Part B RVUs billed in 2010 by physicians identified as internists, geriatricians, family practitioners, and pediatricians, plus RVUs billed by nurse practitioners and physician assistants. RVU = relative value unit.
SOURCE: County totals of RVUs billed by primary care and non—primary care practitioners in 2010 were provided to RTI by the CMS contractor, Acumen, LLC.
The current structure of GME has been essentially intact since an explicit subsidy was designed in 1983 with the introduction of the Medicare Prospective Payment System (Rich et al., 2002). Less than half the amount spent by Medicare on GME reflects direct costs of GME. The larger share is spent to cover indirect clinical cost of such education. Recipients of these funds, which in the vast majority of cases are individual teaching hospitals and the organizations that sponsor residency programs, are able to determine the mix of residency programs with minimal direction from Medicare and other public programs that subsidize GME (MedPAC, 2010).
In a 2003 study of future roles of academic health centers, an Institute of Medicine (IOM) committee observed that the financing of GME in the United States through the Medicare program is focused on inpatient hospital care and specialty services most often delivered in urban settings. That committee recommended reprogramming many of these expenditures to support more interdisciplinary, team-based, nonhospital training focused on improving the health of patients and populations (IOM, 2003a).
In 2010, the MedPAC concluded that “the specialty mix of physicians coming through the GME pipeline is not well matched to the needs of an efficient, high-quality, high-value delivery system.” MedPAC further concluded that “there is insufficient socioeconomic diversity among physicians entering the pipeline, and too few are drawn from rural areas and inner cities, which may mean a reduced propensity to practice in these often underserved areas” (MedPAC, 2010). MedPAC did not propose specific criteria for determining the mix of residency positions by specialty, geographic area, and characteristics of the residents enrolled in such programs. However, it did call for studies to be conducted on these issues followed by a report on strategies that are likely to be most effective in achieving health care system priorities.
The IOM recently initiated a study that will provide a comprehensive review of policy options concerning Medicare’s approach to governance and financing of GME. The study will be completed in 2013.
Within the context of the U.S. health care marketplace, one of the specific tasks of the committee was to evaluate and consider the effects of the geographic adjustment factors on population health and quality of care. Arguably, one of the most pervasive affronts to population health is the persistence of racial and ethnic health disparities. Racial and ethnic minorities and low-income individuals face more barriers when trying to access care and also receive a lower quality of care (IOM, 2003b).
The committee’s primary focus was on investigating geographic differences in Medicare beneficiaries’ ability to access health care and the quality of that care. While the differences between metropolitan and nonmetropolitan regions were generally found to be small in aggregate, geographic differences in access to care were noted in Chapter 3, with some communities and areas of the country experiencing greater access problems than others. Moreover, the committee’s impact analyses showed that payment to practitioners in HPSAs, which are disproportionately populated by racial and ethnic minorities, would be adversely affected by the Phase I recommendations.
As described throughout the report, the committee found substantial literature documenting problems both of access and of quality of care for racial and ethnic minority and low-income populations. Racial and ethnic minorities consistently face more barriers when trying to access care (AHRQ, 2010), but individual-level factors such as health status, personal preferences, and insurance status are not the only determinants of access to health care (Gaskin et al., 2011). Systematic differences in the characteristics of the health care system and availability of services, including the distribution of services within neighborhoods, also contribute to lower levels of access by racial and ethnic minorities (IOM, 2003b).
For example, a recent study explored geographic barriers to care by examining the association between residential segregation and geographic access to primary care physicians in metropolitan statistical areas (Gaskin et al., 2011). Researchers combined ZIP code data on primary care physicians from the 2006 American Medical Association Masterfile and used logistic regression to predict the odds of a ZIP code being a primary care physician shortage area. They found the odds were 67 percent higher for ZIP codes with a majority African American population.
Residents of predominantly African American, Hispanic, and integrated ZIP codes have also been found to be less likely to use services provided by nurse practitioners and physician assistants (Gaskin et al., 2011). This finding contrasts with previous studies indicating greater trust and higher levels of satisfaction with care provided by nurses and nurse practitioners among low-income African Americans (Benkert et al., 2008). The lower utilization could be caused by lack of familiarity with these clinicians, or lack of supply within minority neighborhoods, and suggests that there are many opportunities to increase access to primary care services by increasing the number of qualified practitioners who are able to practice to the full extent of their educational preparation, as the committee recommends in Chapter 6.
The Department of Health and Human Services (HHS) has developed a long-term strategic framework to address disparities at three levels (see Box 5-1): the level of the individual, including factors such as health knowledge, beliefs, and behaviors; at the environmental and com-
I. Transform Health Care
1. Percentage of the U.S. nonelderly population with health coverage
2. Percentage of people who have a specific source of ongoing medical care
3. Percentage of people who did not receive or delayed getting medical care due to cost in the past 12 months
4. Percentage of people who report difficulty seeing a specialist
5. Percentage of people who reported that they experienced good communication with their health care provider
6. Rate of hospitalization for ambulatory-sensitive conditions
7. Percentage of adults who receive colorectal cancer screening as appropriate
II. Strengthen the Nation’s Health and Human Services Infrastructure and Workforce
1. Percentage of clinicians receiving National Health Service Corps scholarships and loan repayment services
2. Percentage of degrees awarded in the health professionals, allied, and associated health professionals fields
3. Percentage of practicing physicians, nurses, and dentists
III. Advance the Health, Safety, and Well-Being of the American People
1. Percentage of infants born at low birth weight
2. Percentage of people receiving seasonal influenza vaccination in the last 12 months
3. Percentage of adults and adolescents who smoke cigarettes
4. Percentage of adults and children with healthy weight
SOURCE: HHS, 2011.
munity level, including the physical, social, and economic environment, as well as assets and values in the community; and at the systems level, including health planning, resource targeting and infrastructure development, and information sharing to apply research and evaluation results that are adopted for continuous improvement (HHS, 2011). At the National Institutes of Health (NIH), the National Institute for Minority Health and Health Disparities will seek to reduce disparities by strengthening the basic, clinical, social, and behavioral research base and developing an integrated trans-NIH research agenda. Taken together, these national initiatives may provide the attention needed to address these long-standing, systemic problems.
GEOGRAPHIC ADJUSTMENT AND PAYMENT REFORM
Geographic adjustment to Medicare payment makes up an important but small part of the overall multipayer fee-for-service payment system. It has a limited ability to influence many of the factors the committee was asked to evaluate and consider, including access, health care qual-
ity, efficiency, workforce supply and distribution, and population health. However, geographic adjustment also is embedded in the larger payment system and subject to larger policy issues that affect the health care delivery system and the health care workforce.
Currently, Medicare is experimenting with alternative provider reimbursement methods with the potential to replace or modify payment per unit of service. Collectively, these different approaches (pay for performance, bundled payments, accountable care organizations, or ACOs) have been referred to as “value-based” reimbursement. In each case, payment is based to varying degrees on achieving quality benchmarks. Under pay-for-performance models, providers receive a portion of their fees based on their performance on a prespecified set of quality of care measures. In contrast, under ACO models, providers must meet quality performance standards in order to be eligible for participation in “shared savings” resulting from delivering care that is less costly than predicted by Medicare for a defined group of patients. Under value-based payment arrangements, instead of asking how changes in payment will affect quality of care, one might ask how changes in quality will affect payment levels.
Under value-based payment will there continue to be a role for geographic adjustment of prices assigned to units of service? Clearly, under a pay-for-performance program the basis for payment continues to be the per-unit price, and the logic of adjusting this price for geographic differences in the cost of providing care remains unchanged. However, geographic adjustment also will be an important factor in determining provider payments under shared gain payment models. In these models, actual provider costs are compared to benchmark cost estimates to determine if there are “gains” to be shared by providers who meet quality goals. The benchmark for a given provider will be determined by estimating costs under fee-for-service in the past for patients assigned to a provider (or, possibly, for Medicare beneficiaries in the region where the provider is located) and trending these costs forward. The geographic adjustment factor will affect this estimate because geographic adjustment was incorporated in previous payments to providers. It appears that the actual costs incurred by providers will be determined by weighting services provided to Medicare beneficiaries by ACOs using the Medicare fee schedule, which incorporates in it a geographic adjustment factor. Thus, geographic adjustment is likely to have an impact on both the benchmark used to determine savings as well as the estimate of the costs of services delivered to ACO patients.
For this reason, one would expect to see providers and other stakeholders raise issues regarding what constitutes accurate and appropriate geographic adjustment under a value- based reimbursement model, similar to issues they have raised in the past regarding geographic adjustment under traditional fee-for-service payment. In fact, there is early evidence of this. Some providers under ACO contracts who have traditionally delivered care to Medicare beneficiaries at a relatively low cost are now arguing that basing their estimate of savings on historical performance penalizes them for past efficiencies, such as early adoption of electronic health records, e-prescribing, and other information technologies that streamline and improve the flow of clinical information.
However, another reason their overall costs may have been low is that their cost of inputs was relatively low, as reflected in their geographic adjustment factor, in addition to their being efficient providers of services. Some are lobbying for a benchmark constructed using national data, a parallel argument used by providers in lower input cost regions who want geographic adjustment factors to be calculated based on relatively large geographic areas that include areas with higher input costs. The committee’s observations about geographic adjustment in
this report thus might prove useful in future deliberations about payment and delivery system reform.
A commitment to improving the accuracy of geographic adjustments to fee-for-service Medicare payments shaped the committee’s deliberations and development of its recommendations. However, the committee also noted that payment policies of the larger delivery system and certain demographic factors potentially had more influence on access, efficiency, and quality of care than did geographic adjustment.
In conducting the statistical simulations of the impact of its Phase I recommendations on clinical practitioners, the committee found a disproportionate impact on certain geographic areas, such as rural and frontier areas, and on racial and ethnic minorities in underserved communities. In keeping with its principles from Phase I, the committee found that other adjustments such as bonus payments were more appropriate to address payment differences than geographic adjustment.
Given its charge to evaluate and consider the impact of geographic adjustment on the workforce, the committee also reviewed and discussed some of the current policy, payment, and program changes that are aimed at strengthening the nation’s primary care infrastructure and promoting beneficiaries’ access to care that is appropriate and well-coordinated across different clinical settings. Attainment of both of those goals will affect the workforce by providing incentives to deliver care in teams with physicians, nurse practitioners, physician assistants, and other clinical and support personnel who work together across clinical settings to improve patient outcomes and experiences. These workforce shifts will not only affect Medicare, but all payers.
AHRQ (Agency for Healthcare Research and Quality). 2010. National healthcare disparities report. Rockville, MD: AHRQ. http://www.ahrq.gov/qual/nhdr10/nhdr10.pdf (accessed August 10, 2012).
AMA (American Medical Association). 2012. http://www.ama-assn.org/resources/doc/cpt/02-2011-ruc-process-traugottnew.pdf (accessed August 15, 2012).
Benkert, R., R. M. Peters, N. Tate, and E. Dinardo. 2008. Low-income African Americans’ trust of nurse practitioners and physicians. Journal of the American Academy of Nurse Practitioners 20:273-280. Berenson, R., S. Zuckerman, K. Stockley, R. Nath, D. Gans, and T. Hammons. 2010. What if all physicians’ services were paid under the Medicare fee schedule? An analysis using medical group management association data. Washington, DC: The Urban Institute.
Bodenheimer, T. R., R. Berenson, and P. Rudolph. 2007. The primary care-specialty income gap: Why it matters. Annals of Internal Medicine 146(4):301-306.
GAO (U.S. Government Accountability Office). 2006. Health Professional Shortage Areas: Problem remain with primary care shortage designation system. GAO-07-84. Washington, DC: GAO.
Gaskin, D., G. Y. Dinwiddie, K. S. Chan, and R. McCleary. 2011 (published online October 4). Residential segregation and disparities in health care services utilization. Medical Care Research and Review, http://mcr.sagepub.com/content/early/2011/09/21/1077558711420263.
HHS (Department of Health and Human Services). 2011. Action plan to reduce racial and ethnic health disparities. http://minorityhealth.hhs.gov/npa/files/Plans/HHS/HHS_Plan_complete.pdf (accessed August 10, 2012).
IOM (Institute of Medicine). 2003a. Governance and financing of graduate medical education. Washington, DC: The National Academies Press.
IOM. 2003b. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: The National Academies Press.
IOM. 2011. Geographic adjustment in Medicare payment: Phase I: Improving accuracy. Washington, DC: The National Academies Press.
MedPAC (Medicare Payment Advisory Commission). 2010. Report to the Congress: Aligning incentives in Medicare. Washington, DC: MedPAC.
MedPAC. 2011. Report to the Congress: Moving forward from the sustainable growth rate (SGR) system. Washington, DC: MedPAC.
Rich, E. C., M. Liebow, M. Srinivasan, D. Parish, J. O. Wolliscroft, O. Fein, and R. Blaser. 2002. Medicare financing of graduate medical education: Intractable problems, elusive solutions. Journal of General Internal Medicine 17:283-292.
Salinsky, E. 2010. Health care shortage designations: HPSA, MUA, and TBD. National Health Policy Forum Background Paper No. 75. Washington, DC: The George Washington University.
This page intentionally left blank.










