8
Achieving and Rewarding High-Value Care
After starting to feel chest pains, a 52-year-old female nurse went to her primary care physician to be evaluated. Even though her initial physical exam and diagnostic tests indicated there was little probability she had a serious cardiac disease, she received a cardiac computed tomography (CT) scan and coronary angiography for reassurance. During the cardiac catheterization for angiography, her left main coronary artery was torn after the second contrast injection, which required immediate coronary bypass surgery. Following a long hospital stay, the patient’s heart was not pumping normally, and she was discharged home to undergo intensive cardiac rehabilitation. After a difficult clinical experience over 6 months, her condition deteriorated, and she underwent coronary angioplasty and therapies to prevent blood clots. Eight weeks later, she was having severe heart problems related to her previous surgeries and required an emergency heart transplant. This case highlights the fact that all tests and interventions have the potential to lead to harm, and illustrates the need for measurement, transparency, and alignment of incentives focused on value (Becker et al., 2011; Redberg, 2011).
Health care payment policies strongly influence how care is delivered, whether new scientific insights and knowledge about best care are diffused broadly, and whether improvement initiatives succeed. As with most aspects of the health care enterprise, a variety of financial incentives and payment
models currently are in use. However, most of these models tend to pay clinicians and health care organizations without a specific focus on patient health and value, which has contributed to waste and inefficiency.
Opportunities exist to eliminate wasteful spending while maintaining or enhancing health care quality and improving overall health outcomes. Several health care organizations and health insurers have been leveraging these opportunities to test new models of paying for care and organizing care delivery. Many individual initiatives have demonstrated success, but systematic reviews and studies continue to find conflicting evidence as to which payment models might work best and under what circumstances. While there will likely continue to be a diversity of payment systems, then, the opportunity exists for additional learning on the relative effectiveness of different payment systems with respect to learning. It is clear, however, that high-value care—the best care for the patient, with the optimal result for the circumstances, delivered at the right price—requires that incentives be structured to reward the best outcomes for the patient.
This chapter begins by describing the obstacles that constrain the delivery of high-value care. Next it addresses in turn the measurement of results and value and strategies for achieving transparency. Methods for transitioning to a system that rewards continuous improvement are then discussed. The final section presents recommendations for realizing the vision of a health care system that achieves and rewards high-value care.
Expenditures on health care are imposing an increasing burden on the budgets of the federal government, state governments, and families without producing commensurate improvements in health or the quality of care. Rather, much of the money spent on health care is wasted, in some cases causing harm. As detailed in Chapter 3, the total amount of waste falls into six broad categories, illustrated in Figure 8-1. Many factors are responsible for this lack of value, from misaligned incentives to a lack of transparency on cost and quality. Overcoming these obstacles will require a determined effort to understand the results achieved from health care; improvements in the structure of and incentives for care; engagement strategies, such as shared decision making, that focus care on patient needs and goals (see Chapter 7); and changes in health care culture needed to support these initiatives (the subject of Chapter 9).
Financial incentives play an important role in the way the health care system learns (see Chapter 6 for a discussion of the factors affecting the spread of knowledge in health care). They create the economic reality for providers and strongly influence how care is delivered (Flodgren et al., 2011; Halvorson, 2009; Hillman, 1991; IOM, 2001). For example,
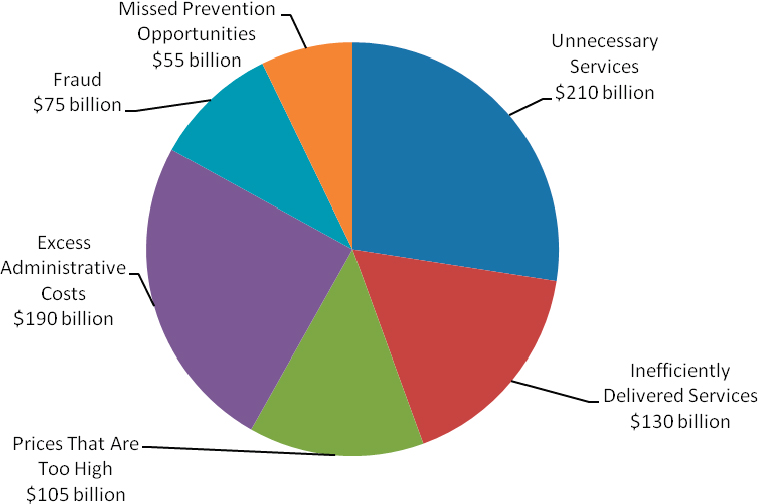
FIGURE 8-1 Sources of waste and excess costs in health care.
SOURCE: Data derived from IOM, 2010b.
clinicians who are paid for each service tend to recommend more visits and services than clinicians who are paid under other methods (Gosden et al., 2000; Helmchen and Lo Sasso, 2010; Hickson et al., 1987). In one study, when primary care physicians began to be paid for each procedure and encounter, the number of procedures increased, and the number of encounters increased from 11 to 61 percent depending on the specialty (Helmchen and Lo Sasso, 2010).
As with many other aspects of the health care enterprise, a variety of financial incentives and payment models are currently in use. Some are modeled on a fee-for-service structure and some on a capitated or global payment system; other models exist as well. The most common models for both public and private plans tend to pay clinicians based on the volume of individual procedures and tests. Higher-quality care rarely is rewarded by payment and contracting policies, so there is little relationship between the cost or price of care and the quality and outcomes of the care provided (Fisher et al., 2003; Office of Attorney General of Massachusetts, 2011; Yasaitis et al., 2009). One study found, on average, only a 4.3 percent correlation (as measured by a coefficient of determination) between the quality of care delivered and the price of the medical service; indeed, higher prices often were associated with lower quality (Office of Attorney General of Massachusetts, 2011).
Several common payment systems can promote greater use of care. When each service generates additional revenue, there is a strong economic incentive for clinicians and health care organizations to provide more interventions and diagnostic procedures, treat with greater intensity, and care for more patients. At the same time, focusing payment on services discourages providers from undertaking other important activities that could improve a patient’s health, such as spending more time talking with the patient, counseling about prevention, communicating by e-mail or telephone, coordinating care across providers, and spending time with family members.
Financial incentives can either aid or inhibit the success of organizational initiatives to improve quality and value (Mandel, 2010; Robinson et al., 2009). Many current payment models can serve as a disincentive for provider organizations seeking to implement high-quality care protocols, given that they may see lower revenues as a result of performing fewer services. This trade-off is exemplified by the experience of one nonprofit health care organization that implemented a program to improve care for back pain. Under its improvement program, the organization changed the care it delivered at its spine clinic to begin with physical therapy, reserving magnetic resonance imaging (MRI) and intensive evaluation for patients with complex cases. The protocol accorded with several evidence-based guidelines; imaging for lower back pain often is overused as an early diagnostic tool when it is unlikely to improve outcomes (Good Stewardship Working Group, 2011). After implementing the protocol, the organization found that patient waiting times were reduced, outcomes improved, and overall costs were low. Under the current payment system, however, the institution was paid for high-cost imaging studies, which it was conducting less frequently, but it was not paid for inexpensive follow-up care such as telephone consultations, which it was conducting more often. As a result, the organization began to lose money. To sustain the improvement initiative, it had to negotiate with local insurers and employers to establish a new payment system for back pain (Blackmore et al., 2011; Fuhrmans, 2007). Box 8-1 provides another example of the disjunction between evidence-based practice and current payment models.
Finally, most current incentive structures fail to distinguish among those treatments that are highly effective for patients with a particular condition, such as aspirin for heart attack patients or antibiotics for treating bacterial infections; those that are effective for some patients but are administered to patients for whom they are ineffective; and those of questionable effectiveness for most patients. Whereas treatments that are generally effective and applied appropriately account for a small fraction of the health care system’s total cost growth, the latter two categories of treatments incur substantial costs (Baicker and Chandra, 2011; Chandra and Skinner, 2011).
BOX 8-1
Waste in Health Care:
The Underuse and Overuse of Screening Colonoscopy
The case of colonoscopy screening illustrates the disjunction between evidence and current payment models. Summarizing the current evidence on colorectal cancer screening, the U.S. Preventive Services Task Force (USPSTF) recommends regular screening for colorectal cancer for adults aged 50 to 75, using a fecal occult blood test (FOBT), sigmoidoscopy, or colonoscopy. The USPSTF notes that routine colonoscopies should be repeated only every 10 years, advises against routine screening of adults aged 76 to 85, and discourages any screening for patients older than 85 (USPSTF, 2008). These recommendations reflect the balance between clinical benefits of screening and the potential for the procedure to result in serious harm, such as colon perforation and adverse cardiovascular events, especially among older patients (Warren et al., 2009).
However, current use of colonoscopy frequently strays from these evidence-based recommendations. Only 65 percent of adults aged 50 to 75 receive the recommended colorectal cancer screenings (CDC, 2011). Yet, overuse occurs as well. Among Medicare patients, almost one-quarter repeat the test within 7 years instead of the recommended 10, with no demonstrated clinical rationale for doing so. The portion of patients repeating the test early remains high for those older than 75, 17 percent of whom repeat the test within 7 years without a clinical indication. These trends occur despite the USPSTF recommendations, as well as Medicare regulations that limit payment for screening colonoscopy to once every 10 years (Goodwin et al., 2011).
Conclusion 8-1: The prevailing approach to paying for health care, based predominantly on individual services and products, encourages wasteful and ineffective care.
Related findings:
- Clinicians who are paid for each service tend to recommend more visits and services than those who are paid under other payment methods. In one study, the initiation of encounter- and procedure-based payment for primary care led to an increased number of encounters and procedures, with visits increasing from 11 to 61 percent depending on the specialty.
- The current payment model does not reward quality. One study found, on average, only a 4.3 percent correlation between the quality of care delivered and the price of the medical service; indeed, higher prices often were associated with lower quality.
MEASUREMENT OF RESULTS AND VALUE
One important tool for improving the value of health care is having a reliable method for defining the value of different interventions, innovations, and care practices. In simple terms, value is the level of benefit achieved for a given cost. However, this concept is complicated by the fact that the perceived benefits of a particular intervention, diagnostic technology, or process will vary for each stakeholder in the health care system (Hussey et al., 2009; IOM, 2010b). Given the system’s clear imperative to focus on the patient (see Chapter 7), value measurement for a particular intervention needs to consider improvements in patient health (length of life, health status), patient quality of life, the patient’s sense of well-being, quality of care (technical and with respect to compassion), and population health (overall and among different groups). In considering the cost component, a comprehensive measure of value would include all financial resources devoted to the particular treatment for the patient’s medical condition, as well as potential adverse outcomes. The definition of cost is further complicated by the fact that different stakeholders have different perspectives on costs—patients may consider out-of-pocket costs, hospitals may look at production costs, and payers may review the medical loss ratio—and each perspective raises additional methodological issues (Fishman and Hornbrook, 2009; Hussey et al., 2009; IOM, 2010b).
One major difficulty in measuring value is finding metrics that can accurately quantify performance with available data. These performance measurement challenges range from providing adequate statistical accuracy to adjusting the measures to account for differences in patient populations (see Table 8-1). Another issue is ensuring the availability of adequate high-quality data with which to calculate the performance metric. Current measures often rely on administrative and claims data; unfortunately, administrative data sources frequently lack information identifying the patient’s underlying clinical condition and indicating whether patient care was delivered according to best practices (Devoe et al., 2011; Tang et al., 2007). The increasing use of interoperable electronic health records, which contain detailed information on care processes, may address these shortcomings and yield further improvements in clinical performance measurement.
Another challenge to performance measurement is the fact that individual clinicians often see few patients for any given performance measure, which can cause two similar clinicians to have very different performance scores. The statistical accuracy of these measurements can be further reduced if they are calculated from claims data, because each health plan collects and maintains its claims data separately (Landon and Normand, 2008; Landon et al., 2003; Scholle et al., 2008, 2009). One strategy for improving the reliability of performance metrics is to combine data from multiple
TABLE 8-1 Challenges Faced in Developing Metrics for Assessing Value
| Measurement Challenge | Questions to Consider |
| Attribution | How can patient health outcomes be attributed to a specific provider or health care organization, especially for chronic care management? |
|
Data sources |
Can this metric be calculated from existing electronic health records or related clinical data sources? |
|
Statistical accuracy |
For the average provider or health care organization, will there be a sufficient number of patients with which to estimate this performance metric with adequate confidence for use in a payment mechanism? |
|
Tailoring of care |
Does the metric exclude patients who, based on clinical practice guidelines, should not receive the care? |
|
Risk adjustment |
Can the performance metrics be properly adjusted for different patient populations with different risk factors, demographics, and health conditions? |
|
Setting benchmarks |
Do sufficient data exist with which to establish a performance benchmark for this metric? |
SOURCE: Adapted with permission from Schneider et al., 2011.
health plans, which has shown success in pilot experiments conducted in Colorado, Florida, and Wisconsin (Higgins et al., 2011b; Toussaint et al., 2011). Further efforts to ensure accuracy are necessary to build buy-in from providers and organizations for the goals of these measures.
Another outstanding issue is the need to ensure that performance metrics are linked to patient health outcomes. In some cases, process measures have been found to correlate poorly with clinical outcomes, such as in the case of heart failure (Fonarow et al., 2007). Moreover, there is concern that if performance metrics were applied, providers would focus on the specific processes that were defined as high-quality to the exclusion of other important, but difficult to measure, aspects of care (IOM, 2007; Werner and Asch, 2007). Effective metrics that drive improvement are defined by four characteristics: solid evidence that the measured process leads to improved health outcomes, certainty that the metric records whether the desired care has been delivered, close linkage between the process and the desired health outcome, and limited adverse consequences (Chassin et al., 2010). Metrics also must be updated frequently to accord with changes in knowledge over time; the goal is to ensure that metrics reward clinical care that agrees with the currently available evidence. Standards-setting organizations, such as
the National Quality Forum (NQF), and measurement organizations, such as the National Committee for Quality Assurance (NCQA), are currently working to improve the accuracy, utility, and application of performance metrics.
Instead of focusing on processes, some metrics are drawn directly from patient health outcomes. A motivation for this strategy is the fact that what matters to patients is the outcome of their care—the effect of their care on the length of their life, their quality of life, and their overall functioning and well-being. One of the difficulties of this model is accurately measuring outcomes that are relevant for patients rather than limiting assessments to what can be easily measured and ensuring that care decisions flow from patient needs, goals, and circumstances (see Chapter 7 for a discussion of patients’ perceptions and needs in maintaining their health and shared decision-making frameworks). For instance, while mortality can be quantified simply, it provides only a limited picture of the total value a patient receives from a given intervention.
After identifying the metrics that best quantify health outcomes, the next challenge is attributing the effect of a given treatment or the actions of a given provider to these metrics. Some treatments, such as surgical procedures, often allow for closer linkages between a procedure and its outcomes, while others, notably chronic care management, have longer time lags between the provision of care and its ultimate outcomes. For chronic care, the patient’s health depends on years, or even decades, of medical treatments, with many providers being involved in the care process. In addition, worse health outcomes often are associated with factors outside the traditional health care system, such as diet and smoking (McGinnis and Foege, 1993). Assessing the value of care based on outcomes for patients with chronic conditions will therefore require a hybrid strategy that involves evaluating both care processes and health outcomes so value metrics can accurately assess the care provided.
STRATEGIES FOR ACHIEVING TRANSPARENCY
Measurement itself is only part of the improvement process. Transparency on results supplies data that clinicians can use for improvement initiatives, provides information that patients and consumers can use to select care and providers, and draws attention to high-value health care providers and organizations (IOM, 2006, 2010a). Some of the earliest such efforts include New York State’s initiative to report the mortality and complications associated with coronary artery bypass graft surgery and the Health Care Financing Administration’s (HCFA’s) reporting of hospital mortality (Berwick and Wald, 1990; Hannan et al., 1994). Since these initial efforts, multiple reporting systems have been introduced, from the Healthcare
Effectiveness Data and Information Set (HEDIS) for health plans to the Centers for Medicare & Medicaid Services’ (CMS’) initiatives on comparing the quality of hospitals and health care providers (Friedberg and Damberg, 2012; NCQA, 2011; O’Neil et al., 2010).
Public reporting has been correlated with improved performance on those measures reported and has encouraged organizations to undertake improvement activities (Hafner et al., 2011; Hibbard et al., 2003, 2005a). For instance, the Joint Commission found that compliance with best practices, such as the administration and discontinuation of prophylactic antibiotics for selected surgical patients, increased dramatically after the metric was publicly reported (Chassin et al., 2010); the rates of compliance with the Joint Commission’s pneumonia care composite metric rose from 72 percent to 95 percent in 8 years (Joint Commission, 2011). Similarly, after CMS released measurements of the quality of heart attack care, improvements such as lower mortality, reduced lengths of stay, and reduced readmissions soon followed (Werner and Bradlow, 2006, 2010). Based on these and related successes, many health care opinion leaders believe increased transparency is an important factor in improving the overall performance of the health care system (Stremikis et al., 2010).
One channel through which transparency can improve health care quality and value is by affecting the selection of providers and health care organizations. In every community, hospitals and physician practices are delivering both high- and low-value care. Patients, however, are not equipped with the tools needed to identify organizations that provide high-quality, high-value care. The public often has more information when making decisions about purchasing consumer goods, such as refrigerators or televisions, than when making decisions about health care.
An aim of public reporting and improved transparency is to remedy this lack of information. By drawing attention to high-value providers and organizations, public reporting can affect the number of patients who choose to visit a given clinician or health care organization, thereby providing a business case for improving value (IOM, 2006, 2010a; Werner et al., 2010). One tool for drawing additional attention to high-value providers and organizations is the use of tiered benefit plans, which have lower patient cost sharing for those providers deemed to be of higher quality (an example is described in Box 8-2). By coupling reporting with financial incentives, these types of plans may drive greater patient volume to providers and organizations that offer higher-value care. Such benefit structures highlight the need for accurate measurement of care value.
Today, however, few consumers use publicly reported information to make decisions about clinicians or health care organizations; a 2008 survey found that only 14 percent of respondents had seen and used comparative quality information about health plans, clinicians, or health care
BOX 8-2
Making Information on Quality Accessible to Consumers
Although accessible information exists to support consumer purchasing for most goods and services, few comprehensive resources are available for comparing the quality of health care providers and hospitals. One effort aimed at expanding the amount of such information is the getbettermaine.org initiative, sponsored by the Maine Health Management Coalition in partnership with the Maine Quality Forum, Maine Quality Counts, the Maine Health Access Foundation, and the Robert Wood Johnson Foundation. The goal of this initiative is to provide patients and consumers with easily accessible information on care quality for various providers and hospitals in the state. Provider and hospital participation, which is voluntary, has been high, with all Maine hospitals and about 70 percent of the state’s physicians participating. This information is being leveraged in the design of health insurance benefits through value-based insurance design. Insurance benefits for state employees provide lower deductibles and copays for the use of providers and care settings deemed of high quality by the initiative, which can encourage providers and hospitals to consider their care quality measures (Richardson, 2011).
organizations in the past year (Kaiser Family Foundation, 2008). Many Americans choose health care providers based on the advice of friends, relatives, and coworkers or on recommendations from a current provider or their health plan (Blendon et al., 2011; Kaiser Family Foundation, 2011; Tu and Lauer, 2008). One reason for the low usage of publicly reported information is that many consumers believe care quality does not vary significantly among different health care organizations and different clinicians, which limits their motivation to make use of independent quality assessments. Moreover, many current reporting efforts use language and presentation formats that impede consumers’ ability to use them for making decisions (Hibbard and Peters, 2003; Hibbard and Sofaer, 2010; Hibbard et al., 2002; Vaiana and McGlynn, 2002). Finally, consumers are heterogeneous in their use of publicly reported information, with usage varying based on demographic and socioeconomic factors. Thus the presentation and content of public reports need to be tailored to individual characteristics (Kolstad and Chernew, 2009).
Reporting also offers opportunities for clinicians to improve the quality of the care they provide by giving them more information on their current performance (Berwick et al., 2003). This type of information fills a critical need, because most physicians lack data on the care provided in their own practice, from their own rates of hospital readmissions to when their patients return to work. Without a baseline, clinicians cannot know
whether their practices are improving. Reporting this type of information focuses attention on a specific quality issue and may support physicians and organizations in efforts to improve their practices (Porter, 2010). Other efforts, using voluntary reporting initiatives, sponsored by medical specialty societies or an integrated delivery system, have shown promise in providing information that clinicians can use for quality improvement activities (Ferguson et al., 2003; Grover et al., 2001).
A final means by which transparency may lead to improvement is by impacting a provider’s or health care organization’s reputation (Hibbard et al., 2005b). In a hospital reporting initiative in Wisconsin, hospitals indicated their belief that the report would affect their public reputation, although not patient volume (Hibbard et al., 2003). This concern appeared to motivate hospitals to undertake quality improvement initiatives.
Although reporting and transparency have had demonstrated impacts on clinical behavior, limited evidence exists about their overall impact on value. Studies and systematic reviews of the public reporting literature suggest that reporting of performance data stimulates quality improvement activities, especially at hospitals, but the impact on effectiveness, safety, and patient-centeredness remains unknown (Fung et al., 2008; Smith et al., 2012). Moreover, recent studies have shown limited effects of public reporting on the quality of care processes or health outcomes, such as mortality, suggesting that there are opportunities for improvement in designing and implementing transparency initiatives to produce optimal results (Ryan et al., 2012; Tu et al., 2009).
Improving transparency initiatives will require action on multiple fronts. First, there is a need to increase alignment among different transparency initiatives. Many reporting efforts are currently under way, each measuring different aspects of care delivery; this multiplicity can confuse consumers and limit impact (Rothberg et al., 2008). Second, there is concern that transparency initiatives may exacerbate health care disparities, as organizations and providers in geographic areas with limited resources may have less ability to undertake improvement efforts (Casalino et al., 2007). Finally, reporting requires that health care practices incur costs for establishing metrics in their data systems, for maintaining the data, and for entering data during each patient visit (Halladay et al., 2009). Although further work is needed to improve the practical implementation of transparency and minimize negative consequences, greater transparency is necessary to provide the information needed to promote continuous learning and improvement.
There also are specific issues to consider when transparency initiatives focus on cost, seeking to increase public knowledge and allow consumers to engage in cost-conscious shopping and thereby stimulate competition on cost and quality (Sinaiko and Rosenthal, 2011). The health care market
is unusual in that the prices for services are largely confidential. Several aspects of the health care market make cost information difficult to obtain. These include health care factors such as the fragmented billing of different providers for an episode of care, the difficulty of predicting the services that will be provided during an episode of care, and varying insurance benefit structures, as well as legal factors such as antitrust law, contractual obligations between insurers and providers, and hesitancy to disclose negotiated rates (Government Accountability Office, 2011a).
Additional challenges facing this type of reporting include the common perception that higher-cost care is higher-quality, limited provider competition in some geographic areas, and differences between prices for procedures and overall health care costs (Ginsburg, 2007; Hibbard et al., 2012; Tu and Lauer, 2009). While there is significant interest in overcoming these barriers to improve the transparency of cost information, such transparency initiatives have been implemented in few places, and their effectiveness remains unclear (Government Accountability Office, 2011a). Nonetheless, evidence demonstrates that transparency can focus employer and policy attention on price differences (Tu and Lauer, 2009). Increased penetration of high-deductible health plans also may encourage greater use of reported information, although this will require that the information be available in an understandable format and customizable for a particular patient’s situation.
Conclusion 8-2: Transparency of process, outcome, price, and cost information, both within health care and with patients and the public, has untapped potential to support continuous learning and improvement in patient experience, outcomes, and cost and the delivery of high-value care.
Related findings:
- Reporting and transparency improve performance in certain circumstances. Following public reporting of pneumonia care measures, for example, rates of compliance rose from 72 percent to 95 percent in 8 years.
- Reporting and transparency provide clinicians with information they want and need. Results of one initiative indicated that coupling financial incentives with assistance to clinicians in monitoring their practice patterns against those of others decreased spending growth by 2 percent per quarter while improving overall care quality.
THE PATH TO A SYSTEM THAT PAYS FOR CONTINUOUS IMPROVEMENT
To address the current flawed payment system, it is necessary to ensure that financial incentives promote quality care and patient health. Health care organizations and private health plans have been testing new models of care delivery; many of these innovations have shown initial success in improving quality and value (Higgins et al., 2011a; Milstein and Gilbertson, 2009; Song et al., 2011). Similarly, the Patient Protection and Affordable Care Act of 2010 has created opportunities to explore pilot delivery models, such as through the Center for Medicare & Medicaid Innovation, and established several new models for Medicare and Medicaid payment, such as the formation of accountable care organizations (Thorpe and Ogden, 2010). Both private and public innovations in health care payment offer opportunities to transition the health care system toward one characterized by continuous improvement. One example is described in Box 8-3.
There are multiple methods for transitioning health care incentives from the current system toward one that rewards value (Table 8-2). These methods may build on existing models, such as by adding incentives for care coordination or shared decision making to procedure-based payment. Another approach entails policies on coverage with evidence development, which are focused on incorporating new treatments and technologies into payment policies while building an evidence base on their effectiveness. More fundamental shifts include global payment systems that provide clinicians with a single payment for all the care needed by a given patient (with some versions adjusting for patient health status and other factors, as well as including incentives for improved patient outcomes). These incentive models also differ in whether they target changing provider or consumer behavior. Table 8-2 does not include all strategies for improving value; for instance, conditions of participation in an insurance plan could be a strong motivation for changing provider behavior. However, the table does highlight the breadth of payment and delivery system organization models currently under consideration.
Properly designed financial incentives can improve the quality of care and its outcomes (Conrad and Perry, 2009). As noted in the Institute of Medicine (IOM) report Rewarding Provider Performance: Aligning Incentives in Medicare, however, an evidence base does not yet exist for determining which type of payment strategy would best improve care quality (IOM, 2007). Since the publication of that report, systematic reviews and studies have continued to find conflicting evidence on which payment models best improve the quality and value of care delivered by individual clinicians and through health care organizations (Government Accountability Office, 2011b; Petersen et al., 2006; Rosenthal, 2008; Scott et al., 2011;
BOX 8-3
Innovations in Health Care Payment:
The Alternative Quality Contract
Blue Cross Blue Shield of Massachusetts established the Alternative Quality Contract (AQC) in January 2009, combining two forms of payment to providers. The program provides a global payment to cover all care services for a given patient—primary care, specialty care, hospital care, prescription drugs, and other services. The global payment, adjusted for age, sex, and health status, is negotiated in a 5-year contract. This time frame, which is longer than that of most payment contracts, allows providers to make investments that permit them to change their care practices over time. Additionally, the program includes payment incentives of up to 10 percent of the global budget tied to performance measures.
The provider groups in the program receive technical support, such as reports on spending, utilization, and quality. As noted earlier in this chapter, providers often lack such information about their panel of patients, which hinders many improvement efforts and limits the ability to manage a patient’s care. The program also shares data on variations in practice patterns for many common conditions, such as back pain and gastroesophageal reflux disease, and use of procedures, such as advanced imaging, allowing individual providers to learn how other clinicians are treating similar conditions.
Currently, the AQC includes only patients in health maintenance organization (HMO) or point of service (POS) plans. Initial results suggest that the program was associated with modest reductions in the growth of medical costs (2 percent per quarter) and improved quality in its first year. Further, all of the groups participating in the AQC earned quality bonuses in the first year. In interviews, the participating medical groups said they have focused on building their infrastructure for primary care providers, managing referrals, and improving their data management capabilities. While initial results are promising, further research will be needed to understand whether this type of plan can reduce long-term growth in health spending while improving overall care quality.
SOURCES: Chernew et al., 2011; Mechanic et al., 2011; Song et al., 2011.
Werner et al., 2011). Because the ideal payment model is unknown, there is an opportunity for additional learning and for building an evidence base on what works best.
As part of the learning process for discovering the ideal payment model, it is important to consider the differing impacts of a particular value initiative on different organizations and clinicians. Because organizations vary, a given intervention will work better in some environments than in others (Government Accountability Office, 2011b). For instance, some providers can bear greater levels of financial risk than others, which impacts their ability to accept payment methods such as bundled and global payments
TABLE 8-2 Selected List of Payment Policies and Delivery System Reforms That Change the Method for Recognizing High-Value Care
| Payment Strategy | Program | Summary |
| Incentives for Process | Payment for shared decision making | Incentive payments are provided for clinicians that use validated patient decision aids and other shared decision-making tools, with the aim of encouraging the consideration of patient needs, values, goals, and preferences in clinical decisions. |
| Incentives for disease management/incentives for coordination | A payer makes additional payments to a provider for care coordination activities. | |
| Penalties for Unwanted Outcomes | Penalties for health care–acquired conditions | A payer applies financial disincentives to clinicians or hospitals for conditions that are acquired in the course of care, such as infections or “never” events (e.g., preventable falls, medical errors). |
| Penalties for potential preventable hospital readmissions | A payer financially penalizes a hospital for potentially avoidable readmissions within a set time frame (such as 30 days). | |
| Payment Methods That Share Accountability | Value-based purchasing/pay for performance | Providers or hospitals are rewarded based on performance, which can be defined in multiple ways, including adhering to a specified process, avoiding overuse, or improving a given health outcome. |
| Gain sharing/performance-based risk sharing | Savings (and potentially excess costs) are shared between stakeholder groups, such as hospitals and physicians, hospitals and payers, physicians and payers, or other combinations. | |
| Bundled payment | For a given condition or clinical episode, the payment is bundled into a single, comprehensive payment that covers all services involved in the patient’s care. | |
| Global payment | A single payment covers all services provided to a patient population during a defined time period. This model shares features of capitation, although it often includes adjustments for performance and patient risk. | |
| Payment Strategy | Program | Summary |
| Accountable care organizations | Groups of providers voluntarily assume responsibility for the care of a population of patients and share savings if they meet specified quality and cost performance benchmarks. | |
| Medical homes | A medical home provides comprehensive primary care services to a population of patients, with responsibilities to coordinate care, provide whole-person care, and ensure timely access to care. | |
| Consumer-Directed Payment Methods | Value-based insurance design | The premise of this type of insurance design is to align benefits (coverage levels, co-payments, deductibles) with the demonstrated value of treatments and diagnostics. Most current plans of this type have been limited to prescription drugs. |
| Tiered networks | A variant of value-based insurance design, a tiered network plan varies the cost sharing for providers and hospitals based on their tier. Tiers are determined according to providers’ quality or value as measured or determined by the health plan. | |
| Consumer-directed health plans | Consumer-directed plans generally couple high deductibles with a health savings account, with the goal of increasing consumer price sensitivity. | |
(Office of Attorney General of Massachusetts, 2011). Similarly, it is important to understand potential adverse effects of a given incentive structure on clinicians (Kurtzman et al., 2011).
A second challenge is the need to understand how different incentive structures affect patients. Many payers have developed financial incentives specifically focused on patients and consumers, including consumer-directed health plans, employer wellness programs, and value-based insurance design. As an example, value-based insurance design models configure benefit design (such as co-payments, clinician networks, and deductibles) to encourage patient and consumer use of high-value services. Such models have shown potential in several cases, although obstacles still exist to their widespread adoption (Chernew et al., 2010; Fendrick et al., 2009, 2010). For these types of models to be successful, it is necessary to understand how
patients actually respond to financial incentives. Current evidence shows that increasing overall cost sharing for patients often lowers the consumption of both effective and ineffective care (Baicker and Goldman, 2011; Beeuwkes Buntin et al., 2011; Chandra et al., 2010; Chernew et al., 2008; Choudhry et al., 2010b; Hsu et al., 2006; Manning et al., 1987).
One field of study that has substantial relevance to understanding the effect of different incentive structures is behavioral economics (Volpp et al., 2008a). This field has shown that people’s responses to different incentive structures may depart, sometimes dramatically so, from the predictions of traditional economics and its conception of the ideal decision maker (Loewenstein et al., 2012). While people respond differently from traditional theories, however, they do react according to several common pathways, including loss aversion, optimism bias, and a bias toward the present (Volpp et al., 2009b). To translate the impact of one of these factors, the fact that most people focus on the present means that incentives with the same frequency as the desired actions are more likely to be effective; a monthly or yearly incentive, for example, will not effectively motivate daily action (Volpp et al., 2008b, 2011). In applying these principles to practice, special consideration should be given to customizing incentives to different populations to ensure their effectiveness (Choudhry et al., 2010a, 2011; Volpp et al., 2009a).
Another challenge faced in developing patient incentives is ensuring that patients have the tools necessary to take advantage of the incentives. Many consumer-focused payment models require that consumers estimate their out-of-pocket costs for their specific situation and under different benefit plans. New tools, such as calculators supplied by large employers and health plans, have been developed to make this task easier. Ensuring that information on health care costs is understandable to a broad audience is key to several new initiatives, such as the proposed standardized summary of insurance benefits (Quincy, 2011).
Payment policies and incentives may need to take into account the heterogeneity of patient health care usage. In 2008, the half of the population with the lowest expenditures accounted for 3.1 percent of total health care costs, while (as noted in Chapter 2) the 5 percent of patients with the highest expenditures accounted for 50 percent of the total (Cohen and Yu, 2011). This concentration of care among a small number of patients has encouraged new initiatives designed to focus efforts on patients with the greatest health care needs, given the potential to improve outcomes and value for that population. Box 8-4 highlights one example. Other initiatives likewise have shown statistically significant cost reductions, with one site realizing a 12 to 16 percent reduction in monthly expenditure growth by focusing on its medically complex patients (McCall et al., 2010).
BOX 8-4
Tailoring Care for Medically Complex Patients:
The AtlantiCare Special Care Center
Tailoring of care for medically complex patients can lead to improved care quality and patient health. One clinic using this model is the AtlantiCare Special Care Center—a clinic established to serve the small percentage of patients with multiple chronic diseases that accounted for the majority of the health care spending of the Local 54 Health and Welfare Fund, a union providing benefits to Atlantic City hospitality industry workers. The benefits of focusing on patients with multiple conditions can be seen in the case of Vibha Gandhi. Vibha, struggling with diabetes, obesity, and heart disease, was confined to her wheelchair and had just suffered her third heart attack. Her physicians had described her advanced coronary artery disease as inoperable just before she visited the Special Care Center for the first time.
Upon checking in, Vibha met with a health coach, Jayshree, who provided support and could connect with Gujarati-speaking patients like Vibhali while care was specially coordinated among the clinic’s doctors, nurses, other clinicians, and health coaches. With Jayshree’s encouragement, Vibha’s health began to improve. She changed her dietary habits, committed to exercise, closely monitored her diabetes, and even took up yoga every Tuesday. Now capable of walking for a quarter mile without losing her breath, Vibha is able to live a sustainable life as a result of intensive monitoring, coaching, and personalized care.
In addition to cases of patients like Vibha, the broad results of the Special Care Center approach have been encouraging. Fully 93 percent of patients offered positive remarks on care coordination, compared with 51 percent under the previous care model. Moreover, 93 percent of patients reported that their clinic doctor seemed to know all the important information about their medical history, compared with 56 percent previously. At the same time, the clinic has increased its patients’ rate of prescription drug compliance, lowered patients’ smoking rates below the national average through its smoking cessation program, and helped patients lower their LDL (low-density lipoprotein) cholesterol levels by 10 percentage points in just 1 year.
SOURCES: Blash et al., 2010; Gawande, 2011.
For all payment models, it is necessary to ensure that they support patient-centered care. One concern is ensuring that incentive structures do not penalize clinicians who customize their care to patient needs, goals, and circumstances even when that care departs from guidelines (Keirns and Goold, 2009). Furthermore, some types of payment models can exacerbate disparities in health care (Blustein et al., 2011). These considerations are important to minimizing unintended consequences.
Another challenge in implementing new models is aligning incentives in the current multipayer environment. Different payers, including private health insurance plans, Medicaid, and Medicare, often use different measures to assess and reward provider performance (Lee et al., 2010). As a result, practices and hospitals must have multiple incentive models for their patients. Yet most clinicians tend to provide similar care for all of their patients, regardless of the type of insurance they hold (Baker, 1999; Glied and Zivin, 2002). The lack of alignment limits opportunities for learning by reducing the potential for a given incentive model to change medical practice in a fundamental way.
Finally, it is important to note that financial incentives do not operate in a vacuum. They are one factor, although an important one, in moving the system toward high-value care. In addition to financial incentives, other factors, such as the use of electronic health records and the organizational structure of health care (Chapter 9), play significant and important roles (Conrad and Perry, 2009; IOM, 2007). Nonetheless, payment is a crucial element for accomplishing widespread change.
FRAMEWORK FOR ACHIEVING THE VISION1
Rising health care costs in the United States are straining the budgets of federal and state payers, employers, and patients. Yet many of these expenditures are wasted and do not improve patient health. Continuously improving the value achieved by health care, thereby continually reducing waste, requires greater availability of information on health care performance in terms of patient experience, outcomes, and cost.
Health care payment practices also play an important role in determining the value achieved by the health care system. While current payment practices often reward service volume over value, a continuously learning health care system aligns its incentives to reward evidence-based, high-quality care. Recommendation 8 describes actions necessary to encourage incentives for continuous learning and improvement, as well as to develop the metrics needed to measure value.
Recommendation 8: Financial Incentives
Structure payment to reward continuous learning and improvement in the provision of best care at lower cost. Payers should structure payment models, contracting policies, and benefit designs to reward care that is effective and efficient and continuously learns and improves.
___________________________________________________
1Note that in Chapters 6-9, the committee’s recommendations are numbered according to their sequence in the taxonomy in Chapter 10.
Strategies for progress toward this goal:
- Public and private payers should reward continuous learning and improvement through outcome- and value-oriented payment models, contracting policies, and benefit designs. Payment models should adequately incentivize and support high-quality team-based care focused on the needs and goals of patients and families.
- Health care delivery organizations should reward continuous learning and improvement through the use of internal practice incentives.
- Health economists, health service researchers, professional specialty societies, and measure development organizations should partner with public and private payers to develop and evaluate metrics, payment models, contracting policies, and benefit designs that reward high-value care that improves health outcomes.
Also necessary for continuous learning and improvement is transparency. Recommendation 9 outlines broad measures needed to increase the transparency of information in health care along multiple dimensions of performance. Further, the recommendation encompasses actions by public and private payers to supply such data and an increase in these transparency initiatives.
Recommendation 9: Performance Transparency
Increase transparency on health care system performance. Health care delivery organizations, clinicians, and payers should increase the availability of information on the quality, prices and cost, and outcomes of care to help inform care decisions and guide improvement efforts.
Strategies for progress toward this goal:
- Health care delivery organizations should collect and expand the availability of information on the safety, quality, prices and cost, and health outcomes of care.
- Professional specialty societies should encourage transparency on the quality, value, and outcomes of the care provided by their members.
- Public and private payers should promote transparency in quality, value, and outcomes to aid plan members in their care decision making.
- Consumer and patient organizations should disseminate this information to facilitate discussion, informed decision making, and care improvement.
Recommendations 8 and 9 are intended to promote continuous learning with respect to the value achieved by the health care system. They build on the successes realized by health care organizations and insurers in developing new models of paying for care and organizing care delivery. While a diversity of payment systems is likely to persist, these successes highlight the opportunity for incentives designed to encourage learning and improvement. By aligning incentives to focus on the patient, new payment and incentive methods can promote high-value care that reduces waste and fosters a sustainable health care system for the future.
Baicker, K., and A. Chandra. 2011, August 8. Aspirin, angioplasty, and proton beam therapy: The economics of smarter health care spending. Paper presented at Jackson Hole Economic Policy Symposium, Jackson Hole, Wyoming.
Baicker, K., and D. Goldman. 2011. Patient cost-sharing and healthcare spending growth. Journal of Economic Perspectives 25(2):47-68.
Baker, L. C. 1999. Association of managed care market share and health expenditures for fee-for-service Medicare patients. Journal of the American Medical Association 281(5):432-437.
Becker, M. C., J. M. Galla, and S. E. Nissen. 2011. Left main trunk coronary artery dissection as a consequence of inaccurate coronary computed tomographic angiography. Archives of Internal Medicine 171(7):698-701.
Beeuwkes Buntin, M., A. M. Haviland, R. McDevitt, and N. Sood. 2011. Healthcare spending and preventive care in high-deductible and consumer-directed health plans. American Journal of Managed Care 17(3):222-230.
Berwick, D. M., and D. L. Wald. 1990. Hospital leaders’ opinions of the HCFA mortality data. Journal of the American Medical Association 263(2):247-249.
Berwick, D. M., B. James, and M. J. Coye. 2003. Connections between quality measurement and improvement. Medical Care 41(Suppl. 1):I30-I38.
Blackmore, C. C., R. S. Mecklenburg, and G. S. Kaplan. 2011. At Virginia Mason, collaboration among providers, employers, and health plans to transform care cut costs and improved quality. Health Affairs 30(9):1680-1687.
Blash, L., S. Chapman, and C. Dower. 2010. The special care center: A joint venture to address chronic disease. San Francisco, CA: Center for the Health Professions.
Blendon, R. J., J. M. Benson, G. K. SteelFisher, and K. J. Weldon. 2011. Report on Americans’ views on the quality of health care. Cambridge, MA: Robert Wood Johnson Foundation and the Harvard School of Public Health.
Blustein, J., J. S. Weissman, A. M. Ryan, T. Doran, and R. Hasnain-Wynia. 2011. Analysis raises questions on whether pay-for-performance in Medicaid can efficiently reduce racial and ethnic disparities. Health Affairs (Millwood) 30(6):1165-1175.
Casalino, L. P., A. Elster, A. Eisenberg, E. Lewis, J. Montgomery, and D. Ramos. 2007. Will pay-for-performance and quality reporting affect health care disparities? Health Affairs (Millwood) 26(3):w405-w414.
CDC (Centers for Disease Control and Prevention). 2011. Vital signs: Colorectal cancer screening, incidence, and mortality—United States, 2002-2010. Morbidity and Mortality Weekly Report 60(26):884-889.
Chandra, A., and J. S. Skinner. 2011. Technology growth and expenditure growth in health care. Cambridge, MA: National Bureau of Economic Research.
Chandra, A., J. Gruber, and R. McKnight. 2010. Patient cost-sharing and hospitalization offsets in the elderly. American Economic Review 100(1):193-213.
Chassin, M. R., J. M. Loeb, S. P. Schmaltz, and R. M. Wachter. 2010. Accountability measures—using measurement to promote quality improvement. New England Journal of Medicine 363(7):683-688.
Chernew, M. E., M. R. Shah, A. Wegh, S. N. Rosenberg, I. A. Juster, A. B. Rosen, M. C. Sokol, K. Yu-Isenberg, and A. M. Fendrick. 2008. Impact of decreasing copayments on medication adherence within a disease management environment. Health Affairs (Millwood) 27(1):103-112.
Chernew, M. E., I. A. Juster, M. Shah, A. Wegh, S. Rosenberg, A. B. Rosen, M. C. Sokol, K. Yu-Isenberg, and A. M. Fendrick. 2010. Evidence that value-based insurance can be effective. Health Affairs (Millwood) 29(3):530-536.
Chernew, M. E., R. E. Mechanic, B. E. Landon, and D. G. Safran. 2011. Private-payer innovation in Massachusetts: The “alternative quality contract.” Health Affairs (Millwood) 30(1):51-61.
Choudhry, N. K., M. A. Fischer, J. Avorn, S. Schneeweiss, D. H. Solomon, C. Berman, S. Jan, J. Liu, J. Lii, M. A. Brookhart, J. J. Mahoney, and W. H. Shrank. 2010a. At Pitney Bowes, value-based insurance design cut copayments and increased drug adherence. Health Affairs (Millwood) 29(11):1995-2001.
Choudhry, N. K., M. B. Rosenthal, and A. Milstein. 2010b. Assessing the evidence for value-based insurance design. Health Affairs (Millwood) 29(11):1988-1994.
Choudhry, N. K., J. Avorn, R. J. Glynn, E. M. Antman, S. Schneeweiss, M. Toscano, L. Reisman, J. Fernandes, C. Spettell, J. L. Lee, R. Levin, T. Brennan, and W. H. Shrank. 2011. Full coverage for preventive medications after myocardial infarction. New England Journal of Medicine 365(22):2088-2097.
Cohen, S. B., and W. Yu. 2011. The concentration and persistence in the level of health expenditures over time: Estimates for the U.S. population, 2008-2009. Rockville, MD: Agency for Healthcare Research and Quality.
Conrad, D. A., and L. Perry. 2009. Quality-based financial incentives in health care: Can we improve quality by paying for it? Annual Review of Public Health 30:357-371.
Devoe, J. E., R. Gold, P. McIntire, J. Puro, S. Chauvie, and C. A. Gallia. 2011. Electronic health records vs. Medicaid claims: Completeness of diabetes preventive care data in community health centers. Annals of Family Medicine 9(4):351-358.
Fendrick, A. M., M. E. Chernew, and G. W. Levi. 2009. Value-based insurance design: Embracing value over cost alone. American Journal of Managed Care 15(Suppl. 10):S277-S283.
Fendrick, A. M., D. G. Smith, and M. E. Chernew. 2010. Applying value-based insurance design to low-value health services. Health Affairs (Millwood) 29(11):2017-2021.
Ferguson, T. B., E. D. Peterson, L. P. Coombs, M. C. Eiken, M. L. Carey, F. L. Grover, E. R. DeLong, and Society of Thoracic Surgeons and the National Cardiac Database. 2003. Use of continuous quality improvement to increase use of process measures in patients undergoing coronary artery bypass graft surgery: A randomized controlled trial. Journal of the American Medical Association 290(1):49-56.
Fisher, E. S., D. E. Wennberg, T. A. Stukel, D. J. Gottlieb, F. L. Lucas, and E. L. Pinder. 2003. The implications of regional variations in Medicare spending. Part 1: The content, quality, and accessibility of care. Annals of Internal Medicine 138(4):273-287.
Fishman, P. A., and M. C. Hornbrook. 2009. Assigning resources to health care use for health services research: Options and consequences. Medical Care 47(7 Suppl. 1):S70-S75.
Flodgren, G., M. P. Eccles, S. Shepperd, A. Scott, E. Parmelli, and F. R. Beyer. 2011. An overview of reviews evaluating the effectiveness of financial incentives in changing healthcare professional behaviours and patient outcomes. Cochrane Database of Systematic Reviews (7):CD009255.
Fonarow, G. C., W. T. Abraham, N. M. Albert, W. G. Stough, M. Gheorghiade, B. H. Greenberg, C. M. O’Connor, K. Pieper, J. L. Sun, C. Yancy, J. B. Young, and OPTIMIZE-HF Investigators and Hospitals. 2007. Association between performance measures and clinical outcomes for patients hospitalized with heart failure. Journal of the American Medical Association 297(1):61-70.
Friedberg, M. W., and C. L. Damberg. 2012. A five-point checklist to help performance reports incentivize improvement and effectively guide patients. Health Affairs 31(3):612-618.
Fuhrmans, V. 2007. A novel plan helps hospital wean itself off pricey tests. Wall Street Journal, January 12.
Fung, C. H., Y. W. Lim, S. Mattke, C. Damberg, and P. G. Shekelle. 2008. Systematic review: The evidence that publishing patient care performance data improves quality of care. Annals of Internal Medicine 148(2):111-123.
Gawande, A. 2011. The hot spotters: Can we lower medical costs by giving the neediest patients better care. New Yorker 40-51.
Ginsburg, P. B. 2007. Shopping for price in medical care. Health Affairs (Millwood) 26(2):w208-w216.
Glied, S., and J. G. Zivin. 2002. How do doctors behave when some (but not all) of their patients are in managed care? Journal of Health Economics 21(2):337-353.
Good Stewardship Working Group. 2011. The “top 5” lists in primary care: Meeting the responsibility of professionalism. Archives of Internal Medicine 171(15):1385-1390.
Goodwin, J. S., A. Singh, N. Reddy, T. S. Riall, and Y. F. Kuo. 2011. Overuse of screening colonoscopy in the Medicare population. Archives of Internal Medicine 171(15):1335-1343.
Gosden, T., F. Forland, I. S. Kristiansen, M. Sutton, B. Leese, A. Giuffrida, M. Sergison, and L. Pedersen. 2000. Capitation, salary, fee-for-service and mixed systems of payment: Effects on the behaviour of primary care physicians. Cochrane Database of Systematic Reviews (3):CD002215.
Government Accountability Office. 2011a. Health care price transparency: Meaningful price information is difficult for consumers to obtain prior to receiving care. Washington, DC: Government Accountability Office.
Government Accountability Office. 2011b. Value in health care: Key information for policymakers to assess efforts to improve quality while reducing costs. Washington, DC: Government Accountability Office.
Grover, F. L., A. L. Shroyer, K. Hammermeister, F. H. Edwards, T. B. Ferguson, S. W. Dziuban, J. C. Cleveland, R. E. Clark, and G. McDonald. 2001. A decade’s experience with quality improvement in cardiac surgery using the Veterans Affairs and Society of Thoracic Surgeons national databases. Annals of Surgery 234(4):464-472.
Hafner, J. M., S. C. Williams, R. G. Koss, B. A. Tschurtz, S. P. Schmaltz, and J. M. Loeb. 2011. The perceived impact of public reporting hospital performance data: Interviews with hospital staff. International Journal for Quality in Health Care 23(6):697-704.
Halladay, J. R., S. C. Stearns, T. Wroth, L. Spragens, S. Hofstetter, S. Zimmerman, and P. D. Sloane. 2009. Cost to primary care practices of responding to payer requests for quality and performance data. Annals of Family Medicine 7(6):495-503.
Halvorson, G. C. 2009. Health care will not reform itself: A user’s guide to refocusing and reforming American health care. New York: CRC Press.
Hannan, E. L., H. Kilburn, M. Racz, E. Shields, and M. R. Chassin. 1994. Improving the outcomes of coronary artery bypass surgery in New York state. Journal of the American Medical Association 271(10):761-766.
Helmchen, L. A., and A. T. Lo Sasso. 2010. How sensitive is physician performance to alternative compensation schedules? Evidence from a large network of primary care clinics. Health Economics 19(11):1300-1317.
Hibbard, J. H., and E. Peters. 2003. Supporting informed consumer health care decisions: Data presentation approaches that facilitate the use of information in choice. Annual Review of Public Health 24:413-433.
Hibbard, J. H., and S. Sofaer. 2010. Best practices in public reporting no. 1: How to effectively present health care performance data to consumers. Rockville, MD: Agency for Healthcare Research and Quality.
Hibbard, J. H., P. Slovic, E. Peters, and M. L. Finucane. 2002. Strategies for reporting health plan performance information to consumers: Evidence from controlled studies. Health Services Research 37(2):291-313.
Hibbard, J. H., J. Stockard, and M. Tusler. 2003. Does publicizing hospital performance stimulate quality improvement efforts? Health Affairs (Millwood) 22(2):84-94.
Hibbard, J. H., J. Stockard, and M. Tusler. 2005a. Hospital performance reports: Impact on quality, market share, and reputation. Health Affairs (Millwood) 24(4):1150-1160.
Hibbard, J. H., J. Stockard, and M. Tusler. 2005b. It isn’t just about choice: The potential of a public performance report to affect the public image of hospitals. Medical Care Research and Review 62(3):358-371.
Hibbard, J. H., J. Greene, S. Sofaer, K. Firminger, and J. Hirsh. 2012. An experiment shows that a well-designed report on costs and quality can help consumers choose high-value health care. Health Affairs (Millwood) 31(3):560-568.
Hickson, G. B., W. A. Altemeier, and J. M. Perrin. 1987. Physician reimbursement by salary or fee-for-service: Effect on physician practice behavior in a randomized prospective study. Pediatrics 80(3):344-350.
Higgins, A., K. Stewart, K. Dawson, and C. Bocchino. 2011a. Early lessons from accountable care models in the private sector: Partnerships between health plans and providers. Health Affairs (Millwood) 30(9):1718-1727.
Higgins, A., T. Zeddies, and S. D. Pearson. 2011b. Measuring the performance of individual physicians by collecting data from multiple health plans: The results of a two-state test. Health Affairs (Millwood) 30(4):673-681.
Hillman, A. L. 1991. Managing the physician: Rules versus incentives. Health Affairs 10(4):138-146.
Hsu, J., M. Price, J. Huang, R. Brand, V. Fung, R. Hui, B. Fireman, J. P. Newhouse, and J. V. Selby. 2006. Unintended consequences of caps on Medicare drug benefits. New England Journal of Medicine 354(22):2349-2359.
Hussey, P. S., H. de Vries, J. Romley, M. C. Wang, S. S. Chen, P. G. Shekelle, and E. A. McGlynn. 2009. A systematic review of health care efficiency measures. Health Services Research 44(3):784-805.
IOM (Institute of Medicine). 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
IOM. 2006. Performance measurement: Accelerating improvement. Washington, DC: The National Academies Press.
IOM. 2007. Rewarding provider performance: Aligning incentives in Medicare. Washington, DC: The National Academies Press.
IOM. 2010a. The healthcare imperative: Lowering costs and improving outcomes: Workshop series summary. Washington, DC: The National Academies Press.
IOM. 2010b. Value in health care: Accounting for cost, quality, safety, outcomes, and innovation: Workshop summary. Washington, DC: The National Academies Press.
Joint Commission. 2011. Improving America’s hospitals: The Joint Commission’s annual report on quality and safety. http://www.jointcommission.org/assets/1/6/TJC_Annual_Report_2011_9_13_11_.pdf (accessed September 25, 2011).
Kaiser Family Foundation. 2008. 2008 update on consumers’ views of patient safety and quality information. Menlo Park, CA: Kaiser Family Fundation.
Kaiser Family Foundation. 2011. Trends in the use of hospital and provider quality ratings. Menlo Park, CA: Kaiser Family Foundation.
Keirns, C. C., and S. D. Goold. 2009. Patient-centered care and preference-sensitive decision making. Journal of the American Medical Association 302(16):1805-1806.
Kolstad, J. T., and M. E. Chernew. 2009. Quality and consumer decision making in the market for health insurance and health care services. Medical Care Research and Review 66(Suppl. 1):S28-S52.
Kurtzman, E. T., D. O’Leary, B. H. Sheingold, K. J. Devers, E. M. Dawson, and J. E. Johnson. 2011. Performance-based payment incentives increase burden and blame for hospital nurses. Health Affairs 30(2):211-218.
Landon, B. E., and S. L. Normand. 2008. Performance measurement in the small office practice: Challenges and potential solutions. Annals of Internal Medicine 148(5):353-357.
Landon, B. E., S. L. Normand, D. Blumenthal, and J. Daley. 2003. Physician clinical performance assessment: Prospects and barriers. Journal of the American Medical Association 290(9):1183-1189.
Lee, P. V., R. A. Berenson, and J. Tooker. 2010. Payment reform—the need to harmonize approaches in Medicare and the private sector. New England Journal of Medicine 362(1):3-5.
Loewenstein, G., K. G. Volpp, and D. A. Asch. 2012. Incentives in health: Different prescriptions for physicians and patients. Journal of the American Medical Association 307(13):1375-1376.
Mandel, K. E. 2010. Aligning rewards with large-scale improvement. Journal of the American Medical Association 303(7):663-664.
Manning, W. G., J. P. Newhouse, N. Duan, E. B. Keeler, A. Leibowitz, and M. S. Marquis. 1987. Health insurance and the demand for medical care: Evidence from a randomized experiment. American Economic Review 77(3):251-277.
McCall, N., J. Cromwell, and C. Urato. 2010. Evaluation of Medicare Care Management for High Cost Beneficiaries (CMHCB) demonstration: Massachusetts General Hospital and Massachusetts General Physicians Organization (MGH). Research Triangle Park, NC: RTI International.
McGinnis, J. M., and W. H. Foege. 1993. Actual causes of death in the United States. Journal of the American Medical Association 270(18):2207-2212.
Mechanic, R. E., P. Santos, B. E. Landon, and M. E. Chernew. 2011. Medical group responses to global payment: Early lessons from the “alternative quality contract” in Massachusetts. Health Affairs (Millwood) 30(9):1734-1742.
Milstein, A., and E. Gilbertson. 2009. American medical home runs. Health Affairs (Millwood) 28(5):1317-1326.
NCQA (National Committee for Quality Assurance). 2011. HEDIS & quality measurement. http://www.ncqa.org/tabid/59/Default.aspx (accessed September 24, 2011).
Office of Attorney General of Massachusetts. 2011. Examination of health care cost trends and cost drivers. Boston, MA: Massachusetts Attorney General.
O’Neil, S., J. Schurrer, and S. Simon. 2010. Environmental scan of public reporting programs and analysis. Cambridge, MA: Mathematica Policy Research.
Petersen, L. A., L. D. Woodard, T. Urech, C. Daw, and S. Sookanan. 2006. Does pay-for-performance improve the quality of health care? Annals of Internal Medicine 145(4): 265-272.
Porter, M. E. 2010. What is value in health care? New England Journal of Medicine 363(26):2477-2481.
Quincy, L. 2011. Making health insurance cost-sharing clear to consumers: Challenges in implementing health reform’s insurance disclosure requirements. New York: The Commonwealth Fund.
Redberg, R. F. 2011. PCI for late reperfusion after myocardial infarction continues despite negative OAT trial: Less is more. Archives of Internal Medicine 171(18):1645.
Richardson, J. 2011. New website helps patients find quality care. Morning Centinal, August 27.
Robinson, J. C., L. P. Casilino, R. R. Gillies, D. R. Rittenhouse, S. S. Shortell, and S. Fernandes-Taylor. 2009. Financial incentives, quality improvement programs, and the adoption of clinical information technology. Medical Care 47(4):411-417.
Rosenthal, M. B. 2008. Beyond pay for performance—emerging models of provider-payment reform. New England Journal of Medicine 359(12):1197-1200.
Rothberg, M. B., E. Morsi, E. M. Benjamin, P. S. Pekow, and P. K. Lindenauer. 2008. Choosing the best hospital: The limitations of public quality reporting. Health Affairs (Millwood) 27(6):1680-1687.
Ryan, A. M., B. K. Nallamothu, and J. B. Dimick. 2012. Medicare’s public reporting initiative on hospital quality had modest or no impact on mortality from three key conditions. Health Affairs (Millwood) 31(3):585-592.
Schneider, E. C., P. S. Hussey, and C. Schnyer. 2011. Payment reform: Analysis of models and performance measurement implications. Santa Monica, CA: RAND Corporation.
Scholle, S. H., J. Roski, J. L. Adams, D. L. Dunn, E. A. Kerr, D. P. Dugan, and R. E. Jensen. 2008. Benchmarking physician performance: Reliability of individual and composite measures. American Journal of Managed Care 14(12):833-838.
Scholle, S. H., J. Roski, D. L. Dunn, J. L. Adams, D. P. Dugan, L. G. Pawlson, and E. A. Kerr. 2009. Availability of data for measuring physician quality performance. American Journal of Managed Care 15(1):67-72.
Scott, A., P. Sivey, D. Ait Ouakrim, L. Willenberg, L. Naccarella, J. Furler, and D. Young. 2011. The effect of financial incentives on the quality of health care provided by primary care physicians. Cochrane Database of Systematic Reviews 9:CD008451.
Sinaiko, A. D., and M. B. Rosenthal. 2011. Increased price transparency in health care—challenges and potential effects. New England Journal of Medicine 364(10):891-894.
Smith, M. A., A. Wright, C. Queram, and G. C. Lamb. 2012. Public reporting helped drive quality improvement in outpatient diabetes care among Wisconsin physician groups. Health Affairs (Millwood) 31(3):570-577.
Song, Z., D. G. Safran, B. E. Landon, Y. He, R. P. Ellis, R. E. Mechanic, M. P. Day, and M. E. Chernew. 2011. Health care spending and quality in year 1 of the alternative quality contract. New England Journal of Medicine 365(10):909-918.
Stremikis, K., K. Davis, and S. Guterman. 2010. Health care opinion leaders’ views on transparency and pricing. New York: The Commonwealth Fund.
Tang, P. C., M. Ralston, M. F. Arrigotti, L. Qureshi, and J. Graham. 2007. Comparison of methodologies for calculating quality measures based on administrative data versus clinical data from an electronic health record system: Implications for performance measures. Journal of the American Medical Informatics Association 14(1):10-15.
Thorpe, K. E., and L. L. Ogden. 2010. Analysis & commentary. The foundation that health reform lays for improved payment, care coordination, and prevention. Health Affairs (Millwood) 29(6):1183-1187.
Toussaint, J. S., C. Queram, and J. W. Musser. 2011. Connecting statewide health information technology strategy to payment reform. American Journal of Managed Care 17(3):e80-88.
Tu, H. T., and J. Lauer. 2008. Word of mouth and physician referrals still drive health care provider choice. Washington, DC: Center for Studying Health System Change.
Tu, H. T., and J. Lauer. 2009. Impact of health care price transparency on price variation: The New Hampshire experience. Washington, DC: Center for Studying Health System Change.
Tu, J. V., L. R. Donovan, D. S. Lee, J. T. Wang, P. C. Austin, D. A. Alter, and D. T. Ko. 2009. Effectiveness of public report cards for improving the quality of cardiac care: The effect study: A randomized trial. Journal of the American Medical Association 302(21):2330-2337.
USPSTF (U.S. Preventive Services Task Force). 2008. Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Annals of Internal Medicine 149(9):627-637.
Vaiana, M. E., and E. A. McGlynn. 2002. What cognitive science tells us about the design of reports for consumers. Medical Care Research and Review 59(1):3-35.
Volpp, K. G., L. K. John, A. B. Troxel, L. Norton, J. Fassbender, and G. Loewenstein. 2008a. Financial incentive-based approaches for weight loss: A randomized trial. Journal of the American Medical Association 300(22):2631-2637.
Volpp, K. G., G. Loewenstein, A. B. Troxel, J. Doshi, M. Price, M. Laskin, and S. E. Kimmel. 2008b. A test of financial incentives to improve warfarin adherence. BMC Health Services Research 8:272.
Volpp, K., A. Troxel, J. Long, D. Frosch, S. Kumanyika, R. Townsend, A. Reed, J. Smith, M. Helweg-Larsen, K. Enge, and S. Kimmel. 2009a. Impact of financial incentives on blood pressure: Results from the collaboration to reduce disparities in hypertension study. Paper presented at Society of General Internal Medicine Annual Meeting, Miami Beach, FL.
Volpp, K. G., M. V. Pauly, G. Loewenstein, and D. Bangsberg. 2009b. P4P4P: An agenda for research on pay-for-performance for patients. Health Affairs (Millwood) 28(1):206-214.
Volpp, K. G., D. A. Asch, R. Galvin, and G. Loewenstein. 2011. Redesigning employee health incentives—lessons from behavioral economics. New England Journal of Medicine 365(5):388-390.
Warren, J. L., C. N. Klabunde, A. B. Mariotto, A. Meekins, M. Topor, M. L. Brown, and D. F. Ransohoff. 2009. Adverse events after outpatient colonoscopy in the Medicare population. Annals of Internal Medicine 150(12):849-857, w152.
Werner, R. M., and D. A. Asch. 2007. Clinical concerns about clinical performance measurement. Annals of Family Medicine 5(2):159-163.
Werner, R. M., and E. T. Bradlow. 2006. Relationship between Medicare’s hospital compare performance measures and mortality rates. Journal of the American Medical Association 296(22):2694-2702.
Werner, R. M., and E. T. Bradlow. 2010. Public reporting on hospital process improvements is linked to better patient outcomes. Health Affairs (Millwood) 29(7):1319-1324.
Werner, R., E. Stuart, and D. Polsky. 2010. Public reporting drove quality gains at nursing homes. Health Affairs (Millwood) 29(9):1706-1713.
Werner, R. M., J. T. Kolstad, E. A. Stuart, and D. Polsky. 2011. The effect of pay-for-performance in hospitals: Lessons for quality improvement. Health Affairs (Millwood) 30(4):690-698.
Yasaitis, L., E. S. Fisher, J. S. Skinner, and A. Chandra. 2009. Hospital quality and intensity of spending: Is there an association? Health Affairs (Millwood) 28(4):w566-w572.




























