Health care in America presents a fundamental paradox. The past 50 years have seen an explosion in biomedical knowledge, dramatic innovation in therapies and surgical procedures, and management of conditions that previously were fatal, with ever more exciting clinical capabilities on the horizon. Yet, American health care is falling short on basic dimensions of quality, outcomes, costs, and equity. Available knowledge is too rarely applied to improve the care experience, and information generated by the care experience is too rarely gathered to improve the knowledge available. The traditional systems for transmitting new knowledge—the ways clinicians are educated, deployed, rewarded, and updated—can no longer keep pace with scientific advances. If unaddressed, the current shortfalls in the performance of the nation’s health care system will deepen on both quality and cost dimensions, challenging the well-being of Americans now and potentially far into the future.
Consider the impact on American services if other industries routinely operated in the same manner as many aspects of health care:
- If banking were like health care, automated teller machine (ATM) transactions would take not seconds but perhaps days or longer as a result of unavailable or misplaced records.
- If home building were like health care, carpenters, electricians, and plumbers each would work with different blueprints, with very little coordination.
- If shopping were like health care, product prices would not be posted, and the price charged would vary widely within the same store, depending on the source of payment.
- If automobile manufacturing were like health care, warranties for cars that require manufacturers to pay for defects would not exist. As a result, few factories would seek to monitor and improve production line performance and product quality.
- If airline travel were like health care, each pilot would be free to design his or her own preflight safety check, or not to perform one at all.
The point is not that health care can or should function in precisely the same way as all other sectors—each is very different from the others, and every industry has room for improvement. Yet, if some of the transferable best practices from banking, construction, retailing, automobile manufacturing, flight safety, public utilities, and personal services were adopted as standard best practices in health care, the nation could see patient care in which:
- records were immediately updated and available for use by patients;
- care delivered were proven reliable at the core and tailored at the margins;
- patient and family needs and preferences were a central part of the decision process;
- all team members were fully informed in real time about each other’s activities;
- prices and total costs were fully transparent to all participants;
- payment incentives were structured to reward outcomes and value, not volume;
- errors were promptly identified and corrected; and
- results were routinely captured and used for continuous improvement.
Unfortunately, these are not features that would describe much of health care in America today. Health care can lag behind many other sectors with respect to its ability to meet patients’ specific needs, to offer choice, to adapt, to become more affordable, to improve—in short, to learn. Americans should be served by a health care system that consistently delivers reliable performance and constantly improves, systematically and seamlessly, with each care experience and transition.
THE NEED FOR A CONTINUOUSLY LEARNING HEALTH CARE SYSTEM
Decades of rapid innovation and technological improvement have created a health care system that is extraordinarily complex. The discovery of penicillin, which could treat many previously incurable bacterial diseases quickly and completely, heralded the advent of widespread antibiotic treatments for many communicable diseases. The development of insulin therapy has allowed diabetics to control their blood sugar and manage their condition effectively. Imaging systems, from computed tomography (CT) scans to magnetic resonance imaging (MRI), have allowed clinicians to view the inside of the body in extraordinary detail. These and other innovations have benefited millions of patients, but they also have introduced new challenges for both clinicians and patients in treating and managing health conditions.
Today in health care, there is more to know, more to manage, and more to do than ever before. The rate at which new scientific knowledge is being produced outstrips the cognitive capacity of even the most adroit clinician to monitor and evaluate effectively. Physicians specialize and subspecialize to manage the growing stores of health care knowledge, and patients now visit multiple providers for most conditions. New developments promise to accelerate this trend and further challenge the ability of clinicians to remain current on the state of the field. New research in genetics, epigenetics, proteomics, and related molecular biology topics, for example, is adding myriad factors to what clinicians may have to consider when helping patients choose the most appropriate treatment for their circumstances.
Most physicians, nurses, and other health care professionals work diligently to care for their patients, but they often are contending with the challenges of a system that is poorly configured for the current complexity of treatments, technologies, and clinical science. These difficulties are exacerbated by administrative and organizational complexity that requires time that could be spent with patients.
The growing complexity of health care challenges not only providers but also patients. Increasing specialization has made it difficult for patients to navigate the system and find the right care for their conditions. Furthermore, as patients move among providers and settings, they often encounter communication and coordination problems that can result in treatment errors, duplicative services, and fragmented care. Improving the quality of care, patient health outcomes, and the value of care is possible, but will require broad changes in the culture, incentives, administration, and information supports that govern the current health care environment.
Absent such change, the very solvency of the system is threatened, because the cost of health care continues to rise relentlessly. In 2012, the United States will spend an estimated $2.8 trillion on the health care
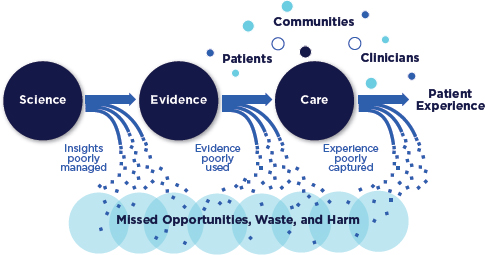
FIGURE 1-1 Schematic of the health care system today.
system, or about 18 percent of gross domestic product (CMS, 2012; Keehan et al., 2011). For 31 of the past 40 years, health care costs have increased at a greater rate than the rest of the economy, and the cumulative increase over that time has been 2.5 times the economy’s growth (BEA, 2011; CMS, 2011). If this level of expenditure produced extraordinary results, it could be justified. On the contrary, however, assessments show that much of this investment is wasted on care activities that do little to improve patients’ health or quality of life.
In sum, as illustrated in Figure 1-1, each stage in the processes that shape the health care received—knowledge development, translation into medical evidence, application of evidence-based care—has prominent shortcomings and inefficiencies that contribute to a large reservoir of missed opportunities, waste, and harm. The threats to the health and economic security of Americans are clear, present, and compelling. What is needed—and possible—to transform care is a system that leverages the growing scientific evidence base, knowledge from other sectors on how to design reliable processes, and advances in information systems to enable continuous improvement in care, consistent implementation of best practices, and the ability to draw on knowledge generated every day through clinical care.
In the face of these realities, the Institute of Medicine (IOM) convened the Committee on the Learning Health Care System in America to explore
the most fundamental challenges to health care today and to propose actions that can be taken to achieve a health care system characterized by continuous learning and improvement. This study builds on earlier IOM studies on various aspects of the health care system, from To Err Is Human: Building a Safer Health System (1999), on patient safety; to Crossing the Quality Chasm: A New Health System for the 21st Century (2001), on health care quality; to Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care (2003b), on health care disparities. The study process also was facilitated and informed by published summaries of workshops conducted under the auspices of the IOM Roundtable on Value & Science-Driven Health Care. Over the past 6 years, 11 workshop summaries have been produced, exploring various aspects of the challenges and opportunities in health care today, with a particular focus on the foundational elements of a learning health system.
While examples of progress exist, many of the problems documented by these reports persist. Medical errors are far too common, different patient populations receive different intensities of services for the same conditions, and health care quality remains uneven. The lack of widespread progress on these now well-documented dimensions of care highlights the need for a substantially new approach. In some cases, successful pilot projects have been undertaken, yet their results have not been disseminated. In other cases, the problem may lie in the need to help clinicians manage the flow of knowledge and apply relevant information to their practice. In still other cases, the difficulty may occur because clinicians and front-line staff do not have at their disposal the tools needed to answer the questions they encounter. These problems point to the need for a transformation in how the health care enterprise generates, processes, and applies information to further patient care.
Meeting the challenges outlined in the above IOM reports has taken on great urgency as a result of two overarching imperatives:
- to manage the health care system’s ever-increasing complexity, and
- to curb ever-escalating costs.
The convergence of these imperatives makes the status quo untenable. At the same time, however, opportunities exist to address these problems—opportunities that did not exist even a decade ago:
- vast computational power that is affordable and widely available;
- connectivity that allows information to be accessed in real time virtually anywhere;
- human and organizational capabilities that improve the reliability and efficiency of care processes; and
- the recognition that effective care must be delivered by collaborations between teams of clinicians and patients, each playing a vital role in the care process.
This report presents a vision for a continuously learning health care system that can leverage these opportunities and recommends priority actions that can be taken to accelerate progress toward that vision.
This study entailed identifying the principal structural, economic, and cultural obstacles to improving health care; reviewing strategies that have been successful to date in transforming care; and assessing the potential consequences of inaction. The actions required will be notable, substantial, and highly disruptive. If these changes do not occur, however, the health care system will continue on its current path. Some patients will receive excellent, world-class care, while too many others will experience unnecessary harm and poor quality. The stress placed on physicians will grow as modern health care becomes ever more complex. At the system level, costs and waste will continue to increase, further taxing national, state, and family budgets. The choice, then, is not whether or when the necessary transformation should be initiated—it is how.
Related Assessments of Others
The scale of actions needed to transform the health care system will require concerted effort on the part of numerous individuals and organizations. Indeed, a variety of organizations have devoted substantial effort to initiatives aimed at improving the safety, effectiveness, patient-centeredness, quality, and value of the health care enterprise. This report is intended to build on this important contextual work. This section highlights several notable examples of these prior initiatives; further examples are noted throughout the report.
One notable initiative aimed at revitalizing the health care system is the Commission on a High Performance Health System, sponsored by the Commonwealth Fund. The goal of this effort is “to promote a high-performing health system that provides Americans with affordable access to high-quality, safe care while maximizing efficiency in its delivery and administration” (The Commonwealth Fund, 2012). Major accomplishments of the Commission include measuring health system performance, highlighting areas for improvement, and recommending strategies for addressing those gaps. A number of the policy options advanced by the Commission are being implemented, in part under provisions of the Affordable Care Act (ACA) of 2010 (The Commonwealth Fund, 2012).
The Robert Wood Johnson Foundation’s Aligning Forces for Quality initiative is an effort to “improve health care quality in targeted communities,
reduce racial and ethnic disparities in care, and provide models for national reform” (Robert Wood Johnson Foundation, 2012). A goal is to build multistakeholder alliances to focus on common areas for progress at the local level. These alliances include physicians, nurses, patients, consumers and consumer groups, purchasers, hospitals, health plans, safety-net providers, and others. The Aligning Forces initiative has spread to 16 communities in different geographic areas with various demographic and economic profiles. Communities involved in the initiative have assisted providers seeking to improve the care they offer, increased the measurement and reporting of care performance, and expanded the ability of patients and consumers to recognize and demand high-quality care (Robert Wood Johnson Foundation, 2012).
The Brookings Institution’s Engelberg Center for Health Care Reform seeks to develop data-driven, practical policy solutions that promote broad access to high-quality, affordable, and innovative care. The Center pursues this goal by conducting research, making policy recommendations, facilitating consensus around key issues, and providing technical support to stakeholders implementing new solutions. Specific projects in which the Center has been involved include the Accountable Care Organization (ACO) Learning Network, a member-driven network that provides participating organizations the tools necessary to implement accountable care successfully; the Quality Alliance Steering Committee, a collaborative effort aimed at implementing measures to improve the quality and efficiency of health care; and the Medicare Payment Reform Project, which is developing policy proposals to reward providers for improving the efficiency, quality, and coordination of care by moving toward greater accountability and support for overall quality and value (The Brookings Institution, 2012; Quality Alliance Steering Committee, 2012).
These examples highlight the diversity of initiatives that are under way, as well as the energy available for transformative action. They are part of a large body of work on which this report draws in exploring what is needed to move toward a health care system that continuously learns and improves.
Related Work of the Institute of Medicine
With a dedicated commitment to improving the quality of care delivered in the United States, the IOM has produced a number of highly influential reports—such as To Err Is Human: Building a Safer Health System (1999), Crossing the Quality Chasm: A New Health System for the 21st Century (2001), Building a Better Delivery System: A New Engineering/Health Care Partnership (2005), Knowing What Works in Health Care: A Roadmap for the Nation (2008b), and Initial National Priorities for Comparative Effectiveness Research (2009a). These reports have drawn
attention to key shortfalls in the performance of the health care system, have led to demonstrable changes in policy, and have helped identify priorities for improving the care delivery system.
More than a decade ago, the IOM released its groundbreaking report To Err Is Human. According to that report, at least 44,000 and perhaps as many as 98,000 people die in hospitals each year as a result of preventable medical errors (IOM, 1999). The report notes that individual error is not the main cause of adverse events; rather, most medical errors are caused by poorly designed systems and processes that fail to prevent adverse events. This report was followed soon after by Crossing the Quality Chasm (IOM, 2001), which highlights the gap between the care that is possible given advances in science and medical knowledge and the care that is routinely received by patients. The report identifies six aims for the health care system: care should be safe, effective, patient-centered, timely, efficient, and equitable (Box 1-1).
Following up on the Quality Chasm report, the IOM conducted a summit on health professions education, releasing the results of this summit in the 2003 report Health Professions Education: A Bridge to Quality. This report cites the need for major changes in health professions education to keep pace with shifts in the nation’s patient population and health care delivery environment and a rapidly expanding evidence base (IOM, 2003a).
In 2004, the IOM launched the Redesigning Health Insurance Performance Measures, Payment, and Performance Improvement Project, which
BOX 1-1
Six Aims of Health Care Improvement
- Safe—avoiding injuries to patients from the care that is intended to help them.
- Effective—providing services based on scientific knowledge to all who could benefit and refraining from providing services to those not likely to benefit.
- Patient-centered—providing care that is respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions.
- Timely—reducing waits and sometimes harmful delays for both those who receive and those who give care.
- Efficient—avoiding waste, in particular waste of equipment, supplies, ideas, and energy.
- Equitable—providing care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status.
SOURCE: IOM, 2001, pp. 39-40.
produced the Pathways to Quality Health Care series of reports. Each report in this series addresses a different aspect of health care quality, including measuring and reporting performance data, designing payment incentives, and structuring quality improvement initiatives. Performance Measurement: Accelerating Improvement reviews the performance measures then available and highlights the need to develop improved measures that are longitudinal, comprehensive, population based, and patient-centered (IOM, 2006b). Medicare’s Quality Improvement Organization Program: Maximizing Potential considers the Quality Improvement Organization program and the need for technical assistance to aid providers undertaking improvement initiatives (IOM, 2006a). The final publication in the series, Rewarding Provider Performance: Aligning Incentives in Medicare, explores the potential of pay-for-performance systems and payment incentives to improve value in health care, especially in the context of the Medicare program (IOM, 2007b).
Most recently, the IOM Roundtable on Value & Science-Driven Health Care has marshaled the insights of the nation’s leading experts to explore in detail the prospects, and the imperative, for transformational change in the fundamental elements of health and health care. The result has been the Learning Health System series of publications, which summarize 15 public workshops held to identify and consider the foundational elements of a learning health system. Brief synopses of the 11 volumes of the series are presented below:
- Vision—The Learning Healthcare System, the first in the series, explores the various dimensions—evidence development and standards, care culture, system design and operation, health data, clinical research, information technology, value—on which emerging insights and scientific advances can be applied to achieve health care in which both the development and application of evidence flow seamlessly and continuously in the course of care (IOM, 2007a).
- Care Complexity—Evidence-Based Medicine and the Changing Nature of Health Care considers the forces, such as genetic insights and increasing care complexity, driving the need for better medical evidence; the challenges with which patients and providers must contend; the need to transform the speed and reliability of new medical evidence; and the legislative and policy changes that could enable the evolution of an evidence-based, learning system (IOM, 2008a).
- Effectiveness Research—Redesigning the Clinical Effectiveness Research Paradigm: Innovation and Evidence-Based Approaches reviews the growing scope and scale of the need for clinical
- effectiveness research alternatives, the limits of current approaches, the potential for emerging research and data networks, innovative study designs, and new methods of analysis and modeling (IOM, 2010b).
- The Data Utility—Clinical Data as the Basic Staple of Health Learning: Creating and Protecting a Public Good identifies the transformational prospects for large interoperable clinical and administrative data sets to allow real-time discovery on issues ranging from disease etiology to personalized diagnosis and treatment. It also explores the key priorities for data stewardship if clinical data are to be a carefully nurtured resource for continuous learning and better care (IOM, 2011a).
- Evidence—Learning What Works: Infrastructure Required for Comparative Effectiveness Research assesses the nature and magnitude of needed capacity for new knowledge and evidence about what care works best under different circumstances, including the necessary skills and workforce, data linkage and improvement, study coordination and dissemination of results, and innovation in research methods (IOM, 2011c).
- Digital Platform—Digital Infrastructure for the Learning Health System: The Foundation for Continuous Improvement in Health and Health Care explores current efforts and opportunities to accelerate progress in improving health and health care through information technology systems. The publication presents summary overviews and priority follow-up action targets in four important cross-cutting dimensions: technical innovation, data and research insights, patient and public engagement, and stewardship and governance (IOM, 2011b).
- Systems Engineering—Engineering a Learning Healthcare System: A Look at the Future reviews lessons from the systems and operations engineering sciences applicable to improving the organization, structure, and function of the delivery, monitoring, and change processes in health care—in effect, engineering approaches to continuous feedback and improvement on quality, safety, knowledge, and value in health care (IOM and NAE, 2011).
- Patients and the Public—Patients Charting the Course: Citizen Engagement and the Learning Health System assesses the prospects for improving health and lowering costs by advancing patient involvement in the elements of a learning health system. It underscores the centrality of communication strategies that account for and engage individual perspectives, needs, preferences, and understanding and the support necessary to mobilize change (IOM, 2011d).
- Cost and Outcomes—The Healthcare Imperative: Lowering Costs and Improving Outcomes presents a six-domain framework for understanding and estimating excessive health care costs: unnecessary services, inefficiently delivered services, excessive administrative costs, prices that are too high, missed prevention opportunities, and medical fraud. Additionally, it summarizes estimates of the excessive costs, reviews approaches to their control, and considers ways to reduce health expenditures by 10 percent within 10 years without compromising health status or valued innovation (IOM, 2010a).
- Value—Value in Health Care: Accounting for Cost, Quality, Safety, Outcomes, and Innovation explores alternative perspectives and approaches for defining, estimating, and attaining value in health care. It includes case studies on value-enhancing strategies in development, such as value-based insurance design and ACOs, and emphasizes the basic need for broad transparency on cost, quality, and outcomes in care (IOM, 2010c).
- Leadership—Leadership Commitments to Improve Value in Health Care: Finding Common Ground presents discussions of opportunity statements from those in key health stakeholder sectors—patients, clinicians, health organizations, insurers, product manufacturers, employers, government, information technology, and researchers—on priority actions they can and will undertake cooperatively to transform quality and value in health care (IOM, 2009b).
STATEMENT OF TASK, SCOPE, AND METHODS
As the above discussion makes clear, the work of the IOM Committee on the Learning Health Care System in America was undertaken as the health care system confronts these very real challenges in order to consider ways of leveraging undeniable opportunities for best care at lower cost. The committee, whose work was supported by the Blue Shield of California Foundation, the Charina Endowment Fund, and the Robert Wood Johnson Foundation, was charged with (1) identifying how the effectiveness and efficiency of the current health care system can be transformed through tools and incentives for continuous assessment and improvement and (2) developing recommendations for actions that can be taken to that end (see Box 1-2). This transformation has the potential to improve the entire health care system, leading to progress in patient safety, health care quality, and value for patients.
The enormity of the challenges currently facing the health care system can be overwhelming to the professionals seeking to improve the health of patients and the public. The learning health care system provides an
BOX 1-2
Charge to the IOM Committee on the
Learning Health Care System in America
An ad hoc Committee will consider the urgent and longer-term actions necessary to foster the development of a continuously learning health care system. Building on recent related work of the Institute of Medicine, particularly that undertaken to inform the dialogue and discussions of the Roundtable on Value & Science-Driven Health Care, the Committee will conduct a study and make recommendations that can help transform the current health care delivery system into one of continuous assessment and improvement for both the effectiveness and efficiency of health care.
Effectiveness. The Committee will define the foundational elements of a learning system for health care that is effective and continuously improving—that marshals the best and most appropriate evidence for application at the point of decision; accounts for patient circumstances and preferences; employs information systems that can accurately record and exchange information on care processes and results; is designed to capture information from the care experience in order to improve care through real-time insights, learning, and evidence development; accelerates the dissemination of innovation through processes, such as regulations, business models, and economic approaches, that also assure safety and value; and ensures continuous feedback for all decision levels.
Efficiency. The Committee will define the foundational characteristics of a health care system that is efficient, delivers increased value, and is continuously innovating and improving in its ability to deliver high value to patients—that has agreed-upon key elements and analytic methods for assessing the value proposition in health care; is fully transparent as to costs and outcomes in care; continuously assesses the effectiveness of health care delivered; accelerates exploration of alternatives; accounts appropriately for differences in patient circumstances and preferences; and appropriately assesses opportunity costs.
Based on this work, the Committee will prepare its Report with findings on major opportunities, deficiencies, and their consequences; identify the key pressure points; and propose policy initiatives and priorities for government and other stakeholders to accelerate progress for continuous improvement in the value of health care delivered to Americans.
organizing conceptual framework for addressing these challenges. The goal is not to create an ideal system that overcomes all of today’s challenges. Because of the ever-changing nature of health care and the complexity of the enterprise, the goal is to transition to a system that can adapt—that is, continuously learn how to improve, manage new challenges, and take advantage of opportunities. Changes recommended by the committee should not be viewed as individual actions, but as means of achieving this overarching aim of continuous learning and improvement.
The committee’s charge was broad, because the dramatic improvements needed in health care will require coordinated and systemwide change. Accordingly, the IOM assembled a committee comprising a diverse group of 18 individuals that included experts in health economics, health care delivery, information technology, systems, education, operations management, and patient safety, as well as individuals who understand the perspectives of employers, insurers, clinicians, researchers, and patients. Brief biographies of the committee members are presented in Appendix D.
Recognizing that achieving a continuously learning health care system will require concerted actions on the part of all stakeholders in the system, the committee designed an ambitious outreach strategy to gather feedback. Staff contacted 248 health care leaders from 215 organizations to solicit their thoughts on the current state of learning and improvement in the health care system and strategies for increasing learning among health care organizations and professionals. The committee received comments and suggestions from 137 individuals, who outlined the issues and challenges and highlighted successful strategies for moving forward. This feedback informed the committee’s deliberations by providing a wide range of perspectives on the current functioning of the health care system and its potential for improvement.
The committee deliberated during four in-person meetings and several conference calls between January 2010 and March 2012. Its initial deliberations focused on clarifying the scope of the study, while later meetings focused on developing recommendations for moving the system forward. To accelerate its efforts, the committee drew on related IOM work, particularly that undertaken to inform the dialogue and discussions of the Roundtable on Value & Science-Driven Health Care. Staff and committee members reviewed the relevant literature in the field and investigated case studies of organizations in different stages of their journey toward adopting learning practices.
This report explores in detail the imperatives of managing complexity, achieving greater value, and capturing opportunities from emerging tools and technologies and from a changing health policy landscape; the vision and foundation of a continuously learning health care system; the path to its accomplishment through transformations in clinical research, patient engagement, cost and outcomes, transparency, and care teamwork and continuity; and the critical need for stakeholder leadership. Detailed findings are highlighted throughout the report, with attendant conclusions and recommendations. Each recommendation describes the core improvement aim for the area, followed by specific strategies representing initial steps that stakeholders should take in acting on the recommendation. Additional
activities will have to be undertaken by numerous stakeholders to sustain and advance the continuous improvement required.
The title of the report underscores that care that is based on the best available evidence, takes appropriate account of individual preferences, and is delivered reliably and efficiently—best care—is possible today. When such care is routinely implemented, moreover, it is generally less expensive than the less effective, less efficient care that is now too commonly provided. Moreover, the transition to best care envisioned in this report is urgently needed given the budgetary, economic, and health pressures facing the nation’s health care system.
This report is divided into three parts. Part I builds the case for a continuously learning health care system, considering the challenges of managing complexity (Chapter 2), achieving greater value in health care (Chapter 3), and capturing opportunities that now make achievement of such a system possible (Chapter 4). Part II outlines a vision for the system, highlighting the key aims for improvement and the foundational elements of performance (Chapter 5). Part III outlines a path for achieving this vision, including new methods for generating and disseminating health care knowledge (Chapter 6); patient, family, and community engagement (Chapter 7); approaches for increasing the value achieved by the system (Chapter 8); and creation of a new culture of care (Chapter 9). Each of these chapters provides a framework for progress on its specific focus, outlining goals and recommendations for improvement, along with specific strategies that stakeholders can undertake to achieve these goals. Finally, Chapter 10 summarizes the actions recommended for each stakeholder to achieve the committee’s vision of a learning health care system based on the conclusions and recommendations presented in prior chapters.
BEA (Bureau of Economic Analysis). 2011. National economic accounts data. http://www.bea.gov/national/index.htm#gdp (accessed April 18, 2012).
The Brookings Institution. 2012. Engelberg Center for Health Care Reform: About us. http://www.brookings.edu/health/About-Us.aspx (accessed April 12, 2012).
CMS (Centers for Medicare & Medicaid Services). 2011. National health expenditure data. https://www.cms.gov/NationalHealthExpendData/01_Overview.asp (accessed April 18, 2012).
CMS. 2012. National health expenditures summary and GDP: Calendar years 1960-2010. http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/downloads/tables.pdf (accessed August 31, 2012).
The Commonwealth Fund. 2012. Commission on a high performance health system. http://www.commonwealthfund.org/Program-Areas/Health-Reform-Policy/Commission-on-a-High-Performance-Health-System.aspx (accessed April 12, 2012).
IOM (Institute of Medicine). 1999. To err is human: Building a safer health system. Washington, DC: National Academy Press.
IOM. 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
IOM. 2003a. Health professions education: A bridge to quality. Washington, DC: The National Academies Press.
IOM. 2003b. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: The National Academies Press.
IOM. 2005. Building a better delivery system: A new engineering/health care partnership. Washington, DC: The National Academies Press.
IOM. 2006a. Medicare’s quality improvement organization program: Maximizing potential. Washington, DC: The National Academies Press.
IOM. 2006b. Performance measurement: Accelerating improvement. Washington, DC: The National Academies Press.
IOM. 2007a. The learning healthcare system: Workshop summary. Washington, DC: The National Academies Press.
IOM. 2007b. Rewarding provider performance: Aligning incentives in Medicare. Washington, DC: The National Academies Press.
IOM. 2008a. Evidence-based medicine and the changing nature of health care: 2007 IOM annual meeting summary. Washington, DC: The National Academies Press.
IOM. 2008b. Knowing what works in health care: A roadmap for the nation. Washington, DC: The National Academies Press.
IOM. 2009a. Initial national priorities for comparative effectiveness research. Washington, DC: The National Academies Press.
IOM. 2009b. Leadership commitments to improve value in health care: Finding common ground: Workshop summary. Washington, DC: The National Academies Press.
IOM. 2010a. The healthcare imperative: Lowering costs and improving outcomes: Workshop series summary. Washington, DC: The National Academies Press.
IOM. 2010b. Redesigning the clinical effectiveness research paradigm: Innovation and practice-based approaches: Workshop summary. Washington, DC: The National Academies Press.
IOM. 2010c. Value in health care: Accounting for cost, quality, safety, outcomes, and innovation: Workshop summary. Washington, DC: The National Academies Press.
IOM. 2011a. Clinical data as the basic staple of health learning: Workshop summary. Washington, DC: The National Academies Press.
IOM. 2011b. Digital infrastructure for the learning health system: The foundation for continuous improvement in health and health care: A workshop summary. Washington, DC: The National Academies Press.
IOM. 2011c. Learning what works: Infrastructure required for comparative effectiveness research: Workshop summary. Washington, DC: The National Academies Press.
IOM. 2011d. Patients charting the course: Citizen engagement in the learning health system: Workshop summary. Washington, DC: The National Academies Press.
IOM and NAE (National Academy of Engineering). 2011. Engineering a learning healthcare system a look at the future: Workshop summary. Washington, DC: The National Academies Press.
Keehan, S. P., A. M. Sisko, C. J. Truffer, J. A. Poisal, G. A. Cuckler, A. J. Madison, J. M. Lizonitz, and S. D. Smith. 2011. National health spending projections through 2020: Economic recovery and reform drive faster spending growth. Health Affairs (Millwood) 30(8):1594-1605.
Quality Alliance Steering Committee. 2012. About QASC. http://www.healthqualityalliance.org/ (accessed May 11, 2012).
Robert Wood Johnson Foundation. 2012. Aligning forces for quality. http://forces4quality.org/ (accessed April 12, 2012).
















