A panel of experts discussed the use of telehealth technologies by a variety of health care providers and in a variety of settings of care across the health care continuum. This included consideration for the use of telehealth for health promotion and disease prevention, for acute care, and for chronic disease management. The following sections reflect the individual speaker’s comments and reflections.
PROMOTING HEALTH, PREVENTING DISEASE,
AND PROMPTING POPULATION PROGRESS
William K. Appelgate, Ph.D.
Iowa Chronic Care Consortium
Population health management has three parts. First is disease and care management for individuals in the population at risk who are actively receiving health care services. This is usually the group that gets most of the attention. Second is lifestyle and health behavior management for individuals in the population who are at risk, but not currently sick. Finally, there is health maintenance and promotion for the population with no known risk factors.
Salutogenesis (the optimization of health) is the opposite of pathogenesis in that it focuses on the building and establishment of health, rather than the costly approach of addressing disease. What prevents the transformation from pathogenesis to salutogenesis? First, the current health care system is primarily oriented to acute disease and diagnosing chronic condi-
tions, and does very little to mitigate the progression of disease. Second is the misappropriation of education—that is, patients need to be activated to change their behaviors rather than to merely be given information. Lastly, there is an overreliance on coming to the health care provider for chronic disease management. Instead of waiting for patients to present with exacerbated symptoms, health care providers need to approach chronic disease proactively.
The Cost of Chronic Disease
Chronic disease accounts for the vast majority of health care spending. However, chronically ill patients only receive a little more than half of all clinically recommended health care, and there is a lag between the establishment of evidence and the adoption of a new care pattern. Half of the people on Medicare right now only cost $550 per year or less, which means that the other half is very expensive. For example, in 2007 the annual average expenditure for Medicare beneficiaries with heart failure was about $25,000; it was about $20,000 for beneficiaries with chronic obstructive pulmonary disease, and about $13,000 for beneficiaries with diabetes. ED visits and hospitalizations account for 83 percent of the cost of chronic care in the Medicare population. Chronic care management interventions can dramatically reduce costs and improve health by keeping individuals out of EDs and hospitals.
Experiences of the Iowa Chronic Care Consortium
Telehome Care Models
A large health system asked the Iowa Chronic Care Consortium (ICCC) to design a heart failure program for their Medicaid population. At the start of the project, the 266 Medicaid heart failure patients had an annual cost of $24,000 each. The ICCC used daily contact and care management, all by phone. The program led to a net savings in excess of $3 million in the study cohort, primarily due to avoided hospitalizations (see Figure 6-1). This was demonstrated through a matched cohort study design, wherein the matched cohort had an increase in costs of $2 million during the same time period.
Similarly, the ICCC’s Medicaid Diabetes Telehomecare Project led to a 54 percent reduction in inpatient visits, a 13 percent reduction in outpatient visits, and a 6 percent reduction in office visits among the study cohort as compared to the match cohort (see Figure 6-2). This resulted in an overall reduction in costs of about 20 percent. Sometimes these interventions led to an increase in the number of office visits, but they are so much less costly than a hospitalization that costs are still greatly reduced.
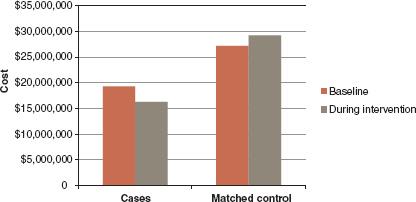
FIGURE 6-1 Total cost of health care service use (Medicaid Heart Failure Program).
SOURCE: Reprinted with permission from William K. Appelgate (2012).
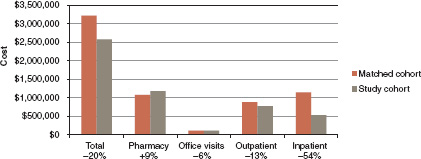
FIGURE 6-2 Medicaid diabetes telehomecare project, preliminary cost data 2010-2012.
SOURCE: Reprinted with permission from William K. Appelgate (2012).
ICCC is in the process of evaluating a current project on health and wellness behavior change in the pre-Medicare population (farmers between the ages of 58 and 63). This intervention included health risk assessments; patient education; diet and exercise incentives; and coaching. The intervention resulted in reduced risk, improved health status, and zero trending.
Many lessons can be learned from experiences with these telehome care models. First, most health care takes place within the home; therefore, to dramatically change health care, the home is the ideal point of delivery. Second, engaging individuals in the self-management of their health is a pri-
ority. Finally, simple approaches can show the value of care management. For example, most of the ICCC’s intervention models are designed just for the use of a telephone.
Evidence-Based Health Coaching
Behavioral patterns and lifestyle choices have some of the largest impacts on health and premature death. In addition, most health care is self-care, and the individual patient is the biggest untapped resource in health care. However, the current system does not activate individuals to change their behaviors. ICCC developed evidence-based health coaching, which involves two elements: transforming the conversation (e.g., between provider and individual) and transforming the care process.
Potential Next Steps
Appelgate stated that telehealth projects and demonstrations with high-quality evaluations should be supported. Matched control groups and other powerful designs can show clinical improvement, reduced costs, patient satisfaction, and improvement in patient functionality. To do this, he said, technical assistance should be provided for the design and evaluation of new projects. Collaboration is needed with CMS to test the best demonstrations in Medicare and Medicaid. More projects that leverage work on costly chronic conditions are especially needed. Finally, remembering that most care is a function of self-management, the value of health coaching should be evaluated.
TELEHEALTH IN AN ACUTE CARE SETTING
Joseph A. Tracy, M.S.
Lehigh Valley Health Network
Challenges in health care today include an aging population, an increased demand for providers, and increased costs. In turn, there is an increased demand for ICU care, which costs about $107 billion annually. Approximately 540,000 people die in ICUs each year, with mortality rates of 10 to 20 percent in most hospitals. Although the number of ICU beds has increased, the number of hospitals with ICU beds has decreased. Only 10 to 20 percent of hospitals have dedicated ICU staffing, and only 1 percent
have it at night. By 2020, there will be a 35 percent shortage of intensivists.1 Therefore, we need to spread this expertise beyond the large centers.
Tele-ICU
The Lehigh Valley Health Network (LVHN) includes the largest academic community hospital in Pennsylvania and the largest Level One trauma center in the region, with more than 11,000 employees and three hospital campuses. Ten years ago the LVHN developed a model for a tele-ICU unit, the Advanced ICU (AICU). The basis for its development included patient safety issues, the need to maintain a high level of ICU care at smaller hospitals, the desire to go beyond Leapfrog requirements for the intensivist staffing model, and finally, its development became simply the right thing to do. The development of the AICU took a lot of time and resources, as well as the involvement of all key stakeholders.
In the AICU model, between 7 a.m. and 7 p.m., the health care team visits patients at six critical care units at two different campuses. Starting at 7 p.m., this team hands off patients to the tele-ICU team, which works remotely (separate from the other facilities), and consists of one board-certified intensivist, three critical care nurses, and one clerical team member. The intensivist works at one of four identical pods with a health information technology bundle that includes every information tool that would be at the bedside (see Figure 6-3). Among the tools, the bundle includes a picture archiving and communication system (PACS), real-time audio and video into each room, which can be used to zoom in and look at pupillary reaction; the ICU electronic medical record, which is connected to the master medical record; an electronic algorithmic event system, which sends an immediate notification for any negative changes in a patient’s vital signs; and direct access to all laboratory results.
The tele-ICU team does not replace the health care professionals already present in the ICU. Instead, the tele-ICU team is an added layer of care for patients during the night. In addition, none of the members of tele-ICU team works full time; they all have part-time floor duties to ensure they maintain their skills. The team also has access to anesthesiologists and trauma surgeons at night, in case invasive procedures (e.g., central line placement, intubation) are needed. It should be noted that the LVHN is a closed system, so the intensivist can intervene and consult on every case in every ICU. Additionally, separate ICUs for trauma and burn patients have
______________
1 Intensivists are physicians who are board certified in a medical specialty, and then receive special education, training, and subspecialty board certification specifically in critical care (SCCM, 2012).
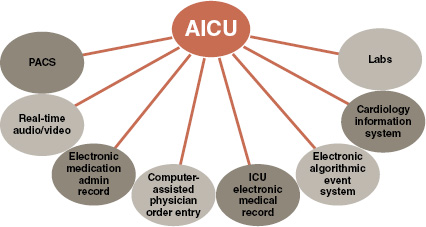
FIGURE 6-3 AICU health information technology bundle.
SOURCE: Reprinted with permission from Joseph Tracy (2012).
physicians in-house all night, so those cases are not covered by the tele-ICU team.
Evidence for Tele-ICU
Some studies show that the implementation of tele-ICU is associated with decreases in mortality, length of stay, and costs, which may in turn lead to an increase in the overall number of ICU admissions. For example, in a 2010 study of tele-ICU at LVHN, the authors showed a 31 percent relative mortality risk reduction in the study group, as well as significant reduction in the use of mechanical ventilation (McCambridge et al., 2010). LVHN estimates that the AICU has resulted in 500 more patients leaving alive each year. LVHN also estimates that each ICU nurse gains about 95 minutes more of direct patient time (during a 12-hour shift), in part due to reduced charting responsibilities. However, other studies have not shown benefit. This may be because of the design of the tele-ICU model rather than the quality of the study methodology. For example, some of the other studies did not use the technology to its fullest capacity (e.g., only for selected cases or specific conditions), thereby creating two levels of care.
Tele-Infectious Disease
LVHN also has a program for inpatient infectious disease consultations with remote physicians. Again, the model uses a standard set of technologies (e.g., interactive video, stethoscope exam cameras, access to labs). This is a true consultation wherein the remote physician provides documentation back to the hospital group, which retains responsibility for patient care. As a result, 85 percent of patients are staying in the smaller hospital instead of being transferred. This has big implications for payers because many of these consultations are to small rural hospitals without infectious disease specialists. Laboratory testing and X-rays are performed at the smaller hospital, which is a much lower cost environment, and all the transport costs associated with an interfacility transfer are saved. Additionally, beds in the bigger tertiary care center are left open for people who really need them.
Concluding Remarks
Tracy concluded that the use of telehealth technologies for acute care can keep patients close to home in a safe and lower cost environment, which may in turn increase a rural hospital’s case mix index. However, reimbursement and licensure remain a persistent barrier in all of telehealth. Some of these barriers can be overcome by defining the site of care to be where the provider is located.
As new models emerge, such as for tele-ICU, questions will arise as to what the minimum standards are for such care. Other questions arise related to anti-kickback statutes. For example, in 2011, the Office of Inspector General (OIG) issued an opinion2 regarding a telestroke program designed to keep patients in their local hospitals and communities (OIG, 2011). The distant telestroke provider wanted to provide the equipment, protocols, and education, all without any charge for the service. In return, the hospital would only use the telestroke services of this provider for 2 years. The OIG said that under normal circumstances this would be a clear violation of the anti-kickback statutes, but that based on the premise that telestroke patients would be kept in their local communities, they would not prosecute. Perhaps, Tracy said, more of these waivers are needed to measure the true capacity and value of telehealth programs.
______________
2 The OIG said that this opinion only applies to the requestor, and the OIG relies strictly on the materials supplied by the requestor of the opinion.
Sanjeev Arora, M.D., FACP, FACG
University of New Mexico
The mission of Extension for Community Healthcare Outcomes (ECHO) project is to expand the capacity to provide care based on best practices for common and complex diseases in underserved areas, and to monitor outcomes.
The ECHO Model
Project ECHO is based on four principles. First is the use of technology (e.g., videoconferencing, the Internet) to leverage scarce resources (e.g., specialists). Second is the use of a disease management model focused on improving outcomes by reducing variation and sharing best practices. Third is the use of case-based learning whereby primary care clinicians comanage patients with experts in order to “learn by doing.” Lastly is the use of the Internet to track outcomes.
Within these parameters, health care providers are first trained in the disease and in the use of Web-based software to track patients. These providers then participate in telemedicine clinics, called knowledge networks, wherein experts come together simultaneously on an interactive video network to give advice to the primary care provider for the comanagement of the patient. During the 2 hours of a clinic, the team comanages 15 patients, and then gives a didactic presentation on some aspect of the disease. No patient ever comes onto this network. Providers learn and become experts through a learning loop—they learn from experts through advice, from didactic presentations, from each other, and mostly by doing.
Through the telemedicine clinics, Project ECHO provides continuing education credits to physicians and nurses at no cost. It seeks to reduce professional isolation by improving interaction for rural providers, and to bring a mix of work and learning, which is often not available for rural providers. It also uses simple technologies.
Project ECHO and Hepatitis C
Project ECHO initially developed through the collaboration of many partners to address the lack of providers to care for patients with hepatitis C in New Mexico. Hepatitis C is a global health problem. While it is curable, if untreated, hepatitis C can lead to death due to end-stage liver disease or liver cancer. In New Mexico, about 28,000 people have hepatitis C, yet less than 5 percent have been evaluated, just 3 or 4 percent have been
treated, and none of the 2,300 prisoners who have been diagnosed have been treated. New Mexico has the highest rate of chronic liver disease, cirrhosis, and deaths in the nation (twice the national average). In 2003, not a single primary care doctor in New Mexico was treating hepatitis C, and people would have to have to get on long waiting lists and drive hundreds of miles to receive care. The care is complex, with regimens that have a high level of side effects.
A large trial of the ECHO model in New Mexico demonstrated that rural primary care clinicians provided hepatitis C care that was as safe and effective as care provided at a specialty clinic at the University of New Mexico. Additionally, cure rates were better than in other large trials. Other studies have shown that clinicians’ self-efficacy in the assessment and care of patients with hepatitis C improved after participation in the clinics. Rural clinicians also report diminished professional isolation, enhanced professional satisfaction, and expansion of patient access. To date, Project ECHO has held 500 telehealth clinics for hepatitis C, with more than 5,000 case presentations. Project ECHO has expanded to include multiple diseases, and overall provided 27,000 hours of continuing medical education credit to rural clinicians in New Mexico for 19 different conditions.
Expansion of Project ECHO
Project ECHO identified six criteria for extending the model to other diseases:
- The disease is common.
- Management is complex.
- New treatments are evolving.
- The disease has high societal impacts (e.g., health, economics).
- Untreated disease leads to serious outcomes.
- Treatments are effective.
The key to Project ECHO is the force multiplier, a logarithmic improvement in the capacity to provide care for very complex problems. Force multiplication occurs through the use of existing community clinicians to provide the same level of care as a specialist. ECHO projects now exist for cardiac risk reduction, asthma, substance abuse, chronic pain, rheumatology, HIV, and many other diseases. The ultimate vision is to transform primary care so that every primary care provider has an area of special interest, creating supporting networks of trained primary care providers (for different diseases) in every region. This is needed because medical knowledge is increasing exponentially, and there is an increasing gap between what a doctor needs to know and what he or she can possibly
learn in order to provide the best care for every disease. Project ECHO also trains community health workers, medical assistants, and others because of the need for team-based care in chronic disease management.
Concluding Remarks
Arora asserted that ECHO models benefit the current health care system through improvements in quality and safety, rapid learning, reduction in the variation of care, improvements in access for rural and underserved patients, reduction in disparities, and workforce training. Additionally, Arora said, there are force multiplier effects by de-monopolizing knowledge, improving professional satisfaction, supporting the medical home model, avoiding excessive testing and travel, and integrating public health into the treatment paradigm. Project ECHO is being replicated across the country and around the world. In conclusion, Arora said, using multipoint video conferencing, following best practice protocols, and comanaging patients with case-based learning together form a robust way to safely and effectively treat chronic common complex diseases in underserved areas and to monitor outcomes.
Moderator: Sherilyn Z. Pruitt, M.P.H.
Health Resources and Services Administration
An open discussion followed the panelists’ presentations. Pruitt began the session by noting that all three presentations demonstrated how telehealth leverages partnerships—in each case, the technology itself was not emphasized, but rather, what people could do together with a technology. Audience members were then able to give comments and ask questions of the panelists. The following sections summarize the discussion session.
Payment
One participant asked why we have not been able to transform payment policy in relation to population health management data, and whether the answer is shared savings. Appelgate said the current reimbursement system is not very amenable to innovations in paying for the care of populations. Appelgate and Arora agreed that there has not necessarily been enough compelling evidence of the value of telehealth to completely transform payment systems.
The participant also asked about moving ECHO to a model where the consultants who help the primary care providers are paid under a consul-
tation model. Arora responded that when a health plan is responsible for the total costs of the patient, they see the value of ECHO because they immediately accrue the benefits of cost savings, and pay for the model as a whole. He added that Project ECHO is more focused on developing partnerships with the health plans and having the plans covering the costs of the infrastructure rather than focusing on individual payments.
Translation of Knowledge into Practice
One participant asked the speakers to comment on challenges with the translation of knowledge into practice and sustainability. Appelgate responded that the ICCC often does not continue the operation of a project after a certain period of time, so they build a sustainability clause into their contracts that requires the people they train to continue running the project for a set period of time after the external funding is used up if performance measures are achieved. Tracy added that LVHN has little grant funding, so telehealth is actually part of the strategic plan of the network. Arora agreed, saying this is exactly the problem Project ECHO is trying to solve. Because health care providers cannot possibly know everything about all of health care (and put it into their practices), Arora noted that Project ECHO seeks to give the providers the mentorship they need to provide the best practice in a particular area of their choice.
The Design of Telehealth Programs
One participant noted that the speakers gave examples of telehealth programs that did not achieve positive results, but suggested this may have been due to the protocols and designs. The participant then asked about the role of best practices and practice guidelines in growing the field of telehealth. Arora said that best practices and practice guidelines are key to the future of telehealth. He noted that part of the reason that payers do not see clear value is because of all the contradicting studies, and so more attention is needed to methodologies of designing telehealth models. Tracy noted that various programs around the country have had mixed results, and agreed that guidelines are needed. He suggested that the Office for the Advancement of Telehealth within HRSA might use their telehealth resource centers to assemble information on what works (or does not work) in the programs in each of their regions. Appelgate reiterated the need for technical assistance to individuals starting telehealth programs.
Transformation of the Health Care System
One participant recalled writings by Atul Gawande on health care reform and the compelling arguments he has given about the changes that have to occur in the system, such as focusing on the highest consumers of health care, the unnecessary variations in care patterns, and the need to follow evidence-based best practices. Arora responded that he (and his colleagues) have a CMMI grant to develop a new specialty in medicine—the outpatient intensive care team—to target the 5 percent of Medicaid patients who consume 57 percent of the resources with the support of ECHO-like knowledge networks. Arora added that reducing variation was not an explicit goal of Project ECHO, but noted that when best practices are used and decisions are discussed in a forum of peers, variation automatically reduces. Tracy pointed out that variation can also be due to institutional politics, noting that unless ICUs are closed (with an intensivist in the lead), the multiple providers may not be willing to consult with each other in decision making. Appelgate responded that population health care managers need strategies to adapt projects to any location.












