The Department of Veterans Affairs/Department of Defense (VA/DoD) Health Executive Council (HEC) executive decision memorandum (EDM) of October 2002 was only the beginning of a long and complicated process of consolidating federal health care delivery activities in North Chicago into a single federal health care facility (FHCC).1 Some of the key decisions were made in the 2002 EDM, namely, that the Navy would close its hospital (Building 200H) and move inpatient services to the nearby North Chicago VA Medical Center (NCVAMC) building and outpatient services to a new, Navy-constructed ambulatory care center (ACC) connected to the NCVAMC hospital building. Other key decisions were made later, such as adopting a single chain of command, transferring civilians employed by the Navy to the VA, creating a unified financial system and jointly funded Department of the Treasury (Treasury) account for the combined facility, and creating a single interface with both the VA and the DoD electronic health record (EHR) systems. There were statements that VA and Navy providers would be working side by side, there would be a single standard of care regardless of beneficiary status, and the needs of both VA and Navy beneficiaries would be met seamlessly, but the steps it would take to achieve these goals were not clear at first.
__________________
1 Initially, the proposed joint health care delivery initiative was called the federal health care facility, or FHCF. It began to be called a federal health care center in late 2007, in conjunction with plans to name the joint medical center after Captain James A. Lovell. “Federal health care center,” or “FHCC,” will be used in the rest of this report regardless of the time period. It should also be noted that while the Lovell FHCC name is singular, it comprises a number of buildings on the east and west campuses and three outlying outpatient centers.
By 2006, the concept of a three-phase implementation process was adopted. Phase 1 was the shifting of inpatient mental health services from the Naval Hospital Great Lakes (NHGL) to the NCVAMC that had taken place in 2003. Phase 2 was the shifting of emergency services and inpatient medical, surgical, and pediatric services from the Navy hospital to the NCVAMC in 2006, after the NCVAMC’s emergency department (ED) and surgical facilities were upgraded by the VA. Phase 3 was the shift of all Navy outpatient services to the new ACC building and other renovated spaces on the west campus of the Lovell FHCC, as well as the implementation of the FHCC as a single organization under a single chain of command in 2010.
Phase 1
In accordance with the October 2002 EDM, the Navy and the VA entered into a resource sharing agreement in which the Navy would discontinue acute inpatient psychiatric services at 200H and the NCVAMC would assume responsibility for the treatment of Navy patients in its acute mental health inpatient unit and lodge discharged mental patients in its psychiatric medical holding unit. According to the agreement, the Navy would compensate the NCVAMC for the services as a TRICARE network provider (i.e., at 90 percent of the CHAMPUS2 maximum allowable charge for the specific diagnosis related group) and provide several psychiatric support staff (Harnly, 2005). The agreement was implemented in October 2003, when six patients were transferred to the NCVAMC (Kuczka, 2003).
In August 2004, the Navy and the VA signed another resource sharing agreement in which the Navy operates a blood donor processing center in the NCVAMC in return for providing the NCVAMC with blood products. The NCVAMC agreed to provide 3,242 square feet of unused laboratory space and utilities, in addition to staff to monitor the cooling equipment after hours. The Navy agreed to pay $40,000 for renovations and $46,600 in rent. In exchange, the NCVAMC agreed to buy 415 units of blood products annually at a cost that was approximately equal to the rent (Harnly, 2005). The arrangement has benefited the Navy because the space in which it was located at Building 81H on the Navy base was no longer adequate and would have cost more than $3 million to renovate; in return, the NCVAMC has benefited by paying less for blood products (Hassan et al., 2008).
Neither of the sharing agreements was free of problems at first. The Navy and the NCVAMC disagreed on the amount of air-conditioning that would be needed for the blood processing laboratory, and experience
__________________
2 CHAMPUS stands for the Civilian Health and Medical Program of the Uniformed Services.
soon showed that more air-conditioning capacity was needed (Harnly, 2005). Although the Navy offered to operate the acute psychiatric unit, the NCVAMC preferred to provide the service and be reimbursed. The volume and acuity of patients and therefore the amounts of reimbursement were less than forecast, and, finding itself overstaffed and losing money, the NCVAMC sought more reimbursement, which the Navy was unwilling to pay (Harnly, 2005).
The NCVAMC held a press conference in November 2003 to announce that the transfer of mental health patients from the NHGL to the NCVAMC had begun. Representative Mark Kirk announced that construction on a $170 million joint VA/Navy health care facility next to the NCVAMC would begin in about 5 years. He told veterans at a Veterans Day ceremony the same day that “if the Navy moves into this facility, it can never close.” NCVAMC director Patrick Sullivan said that the expanded volume of Navy patients would lead to the addition of inpatient surgical services in 2005 (Susnjara, 2003).
Phase 2
The second phase of the VA/DoD partnership was the moving of inpatient surgical and medical services and emergency services from the NHGL to the NCVAMC. The Navy could have sent its inpatient and emergency cases to community hospitals, but using the NCVAMC promised to be less expensive and would allow Navy clinicians to maintain their surgical skills. The move would enable the NCVAMC to have a large enough workload to offer inpatient surgery for the first time since 1992 and to upgrade and enlarge its ED, which would benefit its veteran enrollees (VA, 2002). Before 2006, veterans needing surgery had to be sent 45 miles or more to another VAMC (located either west of Chicago at Hines, in Chicago at the Jesse Brown VAMC, or in Milwaukee, Wisconsin) or referred to a community hospital.
The Navy providers were understandably concerned about moving surgical services to a VAMC where inpatient surgeries had not been performed for 20 years. When they toured the VAMC, they were concerned about the poor condition of the operating suites (Interviews3). The Navy was unwilling to expand the partnership unless appropriate renovations were done at the NCVAMC.
The VA worked with Congress to allocate $13 million in fiscal year (FY) 2004 construction funds to renovate the ED and construct a new surgical center because VA renovation projects were limited to $4 million (Chu, 2003). The number of ED examination rooms was increased from 6
__________________
3 This indicates information provided by anonymous interviews with Lovell FHCC staff.
to 14; 4 new operating rooms and related facilities (e.g., recovery rooms) were built; and 4 existing operating rooms were renovated. The construction award was made in September 2004 and the project was completed in 2006 (U.S. Senate, 2005).
Meanwhile, the physician leaders of the NHGL and the NCVAMC began to work closely together to plan and implement the move of surgical services in 2006. Both leaders were able to remain throughout the implementation process, providing stable leadership to plan and launch the Lovell FHCC in 2010. In 2010, the NCVAMC chief of staff became the associate director for patient care/chief medical executive and the NHGL director became the assistant director for patient care/assistant chief medical executive. This continuity of clinical leadership is considered by the FHCC leadership to have been an important factor in achieving the degree of clinical integration that has been attained (the degree of clinical integration is discussed in Chapter 4).
In June 2006, after the ED, operating rooms, and intensive/critical care unit were upgraded, inpatient medical and surgical services for DoD beneficiaries were moved to the NCVAMC. Navy physicians provided inpatient surgery and pediatric services (the first time pediatrics had been offered at any VA health care facility). With the removal of all inpatient services in 2006, the NHGL was redesignated as the Naval Health Clinic Great Lakes (NHCGL).
Even before the inpatient services at the NHGL were transferred in 2006, there was a fair amount of clinical sharing. In July 2004, the Government Accountability Office (GAO) reported that
VA provides inpatient psychiatry and intensive care, and outpatient clinic visits, for example, pulmonary care, neurology, gastrointestinal care, diabetic care, occupational and physical therapy, speech therapy, rehabilitation, and diagnostic tests to Navy beneficiaries. VA also provides medical training to Naval corpsmen, nursing staff, and dental residents. The Navy provides selected surgical services for VA beneficiaries such as joint replacement surgeries and cataract surgeries. In addition, as available, the Navy provides selected outpatient services, mammograms, magnetic resonance imaging (MRI) examinations, and laboratory tests. (GAO, 2004, pp. 16–17)
After the inpatient medical-surgical transfer, the reimbursement methodology for inpatient services was facility charges at the TRICARE network negotiated rate (Lovell FHCC, 2006). The VA paid the Navy about $295,000 and the Navy paid the VA $502,000 during FYs 2002 and 2003, which was estimated to be approximately $88,000 less than the VA and the Navy would have paid for the same services in the private sector, and having the VA provide acute mental health services in the 10-bed ward
and the 10-bed medical hold unit saved the Navy about $323,000 per year (GAO, 2004, p. 17).
Governance of these collaborative activities was through an executive steering committee co-chaired by the NCVAMC director and the NHGL commanding officer. The executive steering committee worked through administrative, clinical, and mental health subcommittees (Lovell FHCC, 2006).
The VA/Navy merger process also benefited from a series of early Joint Incentive Fund (JIF) awards. In FY 2004, for example, the NHGL and the NCVAMC received JIF funds for two joint projects—mammography and a women’s health clinic—to enhance access and quality of care for women veterans. The new women’s health clinic, which offers mammography, ultrasound, gynecology, and case managers in one location, would not have been possible to sustain without the volume added by Navy beneficiaries. In FY 2005, the FHCC received JIF awards to purchase a magnetic resonance imaging (MRI) machine, start an oncology/hematology clinic, and build a high-capacity fiber optic cable to connect the facilities on the VA campus with the Navy clinics that would remain on the base. In FY 2006, there were awards to add a hospitalist and the capacity to perform digital radiography (picture archiving and communication system, or PACS), capitalizing on the new fiber optic connection between the campuses. (Additional JIF awards during Phase 3 are reviewed in Box 3-1.)
Phase 3
On May 26, 2005, William Winkenwerder, the assistant secretary of defense for health affairs, and Jonathan Perlin, the under secretary of veterans affairs for health, the co-chairs of the HEC, signed an EDM that approved construction of a Navy-funded ACC adjoining the North Chicago VA medical center hospital building (Building 133) and creation of a single-chain-of-command governance structure for a joint federal health care facility.
The approved costs included construction of the ACC, renovation of space in the VA hospital building for some of the outpatient clinics, and construction of a 562-car, 4-story parking garage and a 540-car surface parking lot. The total amount of $139.1 million was less than the $160.6 million originally proposed. It was achieved by reducing the size of the ACC through renovating additional space in Building 133 and by cutting additional administrative positions. The original cost also presumed that the ACC would be built on the south side of Building 133, which would have required demolition of a nursing home care unit (NHCU) and construction of a new $25 million NHCU elsewhere on the VA campus. The south site was preferred by the Navy because it was the largest, but scaling back the
BOX 3-1
Joint Incentive Fund Awards to North Chicago, Fiscal Years 2004–2007
Women’s Health Clinic (FY 2004)
$852,000
Mammography Services (FY 2004)
$470,000
These JIF [Joint Incentive Fund] awards established a comprehensive women’s health center to serve both female veterans and DoD [Department of Defense] beneficiaries. VA [Department of Veterans Affairs] hired gynecology staff (replacing a lost Navy physician billet), purchased digital mammography equipment and a stereotactic unit, and hired two wellness/case management nurses. A partial cost savings of $70,000 resulted during the fiscal year, for example, by paying less for stereotactic mammograms in the private sector (VA/DoD, 2008a, p. 29). The center was a significant expansion of services for veteran and DoD women.
Hematology-Oncology Program (FY 2005)
$685,000
A hematology-oncology program was added to include consultations, inpatient support, outpatient care, and a chemotherapy infusion center for VA and DoD beneficiaries. Neither the VA nor [the] DoD previously provided these services, and all patients had been referred to the local community for care. By combining services, access was improved and patients no longer needed to travel long distances to receive their care (VA/DoD, 2006a, p. 18).
Joint Magnetic Resonance Imaging (FY 2005)
$3,426,000
The award was to purchase a 3-Tesla state-of-the-art open-field MRI [magnetic resonance imaging unit] that was permanently housed in a modern MRI suite. The full-time fixed-site MRI, which became functional in March 2007, has reduced patient wait time and expensive referrals for contract care. It reduced delays in treatment and thus reduced the length of stay for acutely ill inpatients. This project included funding for a radiologist to perform interpretation of MRIs and [to] consult with providers (VA/DoD, 2006a, p. 18).
Clinical Fiber Optics (FY 2005)
$248,000
The project provided high-speed clinical connectivity between both facilities to transmit clinical images for the VA’s PACS [picture archiving and communication system], VistA [Veterans Health Information Systems and Technology Architecture] imaging, and computerized patient record system (CPRS) (VA/DoD, 2006a, p. 18).
Hospitalist (FY 2006)
$403,000
The presence of the two hospitalists has enabled VA and Navy internal medicine, primary care, and specialty providers to increase capacity in the outpatient
setting and to recapture and empanel more patients to the clinics. The program has shown a decrease in the average length of stay of patients while maintaining good clinical outcomes. It provides for the continuity of inpatient care, post-discharge planning and follow-up, and eliminates the uncertainty of who will be caring for patients on a day-to-day basis (VA/DoD, 2008a, pp. 28–29).
Digital Radiography (FY 2006)
$638,000
This project involves installing a PACS at NHGL [Naval Hospital Great Lakes] that will provide unlimited web-based access from NCVAMC [North Chicago Veterans Affairs Medical Center] as well as from within NHGL and its branch health clinics, and allow providers at both facilities greater access to patients’ imaging studies. Additionally, this project will improve the NCVAMC PACS to include an upgraded memory for image archive, an updated software platform for PACS, and upgraded viewing stations. This will provide comparable imaging services at each facility with the availability for easy exchange of radiology information and images (VA/DoD, 2006b, p. 6).
Project Management Support (FY 2007)
$1,770,000
This award provided a dedicated contract staff for project management support of the steering group, the six national work groups, and a number of local joint committees engaged in planning the FHCC [federal health care center] (VA/DoD, 2006b, p. 6).
Enterprise Information Management/Information Technology Requirements at the Lovell Federal Health Care Center (FY 2008)
$11,000,000
This enterprise-level JIF project supported the development of the technical requirements for the basic interoperability capabilities that the Lovell FHCC staff would need to enter, edit, and retrieve patient information in both the VA and [the] DoD EHRs [electronic health record systems] simultaneously (VA/DoD, 2008b, pp. 17–18).
Enterprise Information Management/Information Technology Development at the Lovell Federal Health Care Center (FYs 2009/2010) $100,020,000
This enterprise-level JIF project supported the work of VA and DoD IT staff and private contractors to develop new interoperability software to enable the Lovell FHCC staff to enter, edit, and retrieve patient information in both the VA and DoD EHRs simultaneously (VA, 2010a, pp. 1G–4G).
Interim Pharmacy Solution at the Lovell Federal Health Care Center (FY 2010) $1,000,000
This enterprise-level JIF award supported the interim solution to the lack of interoperability between VA and DoD EHRs that would have created unacceptable patient safety risks. The interim solution was to hire five licensed pharmacists to manually check for potential drug-drug and drug-allergy interactions in both EHRs for every prescription (VA/DoD, 2011, p. 57).
footprint of the ACC meant it could be built on the east site, obviating the need to replace the NHCU.
The decision to downsize the ACC by half, to 201,000 square feet, had another impact. It affected decisions on which and how many clinics to combine instead of to maintain as separate Navy and VA clinics (discussed below). It drove a decision to adopt the VA’s Consolidated Mail Order Pharmacy (CMOP) program so that the pharmacy dispensing space in the ACC could be downsized, which became a problem when the DoD decided against letting the FHCC use the CMOP. The reduced size of the pharmacy space also made it more difficult to implement a manual workaround when the IT solution to enable orders portability between the DoD and the VA EHR systems was not ready in time (discussed below).
In addition to a lower-cost construction project, the proposal contained a substantially revised governance structure. At the March 2005 meeting of the HEC, the VA and Navy planning group had proposed a dual command and reporting structure in which the NCVAMC director and the NHGL commanding officer would be coequals, each reporting to his or her respective department. Under them would be consolidated directorates for clinical services, patient services, and administration, each headed by coequal associate directors. There would be a single medical staff working within a matrix system under a single set of bylaws. This partnership was considered to be a step toward the ultimate goal of full integration. The HEC, at the urging of Vice Admiral Donald Arthur, the Navy surgeon general, directed the planning group to plan a fully integrated organization under a single-line-of-authority governance structure.
The revised governance EDM listed the pros and cons for what it called the federal health care model, in which all services currently provided by the Navy and the VA in North Chicago would be located within a single organizational structure under a single chain of command. The single chain of command would be a VA senior executive service director and chief executive officer and a Navy captain deputy director and chief of operations, who would report to a board of directors under the HEC. The EDM identified the pros of establishing a single organization, as it would
- increase the range of specialty care services available to VA and DoD beneficiaries,
- meld the medical staff into one body for clinical oversight,
- create a single standard of care for all beneficiaries and thus provide a seamless patient care environment, and
- reduce redundancies and thus reduce operating costs.
The cons were a prescient listing of the challenges that were subsequently encountered during the implementation. The creation of a combined health care center would require
- significant communication efforts among all senior members of the DoD, the Navy, and the VA to support the development and implementation of the combined federal health care organization;
- each parent organization to accept a significant reorganization resulting in a loss of autonomy over its respective personnel and assets;
- the crossing of cultural borders when personnel from one organization were supervised by the other organization’s personnel for daily functions;
- the establishment of an interdepartmental process for resolution of disputes; and
- the development of support systems (e.g., acquisition, information, budgeting, human resources) that would meet the standards and reporting requirements of the VA, the Navy, and the DoD.
The working group identified areas in which issues would have to be addressed, some of which might require legislative relief or changes in one or both departments’ policies, regulations, or business rules. These included personnel management, information management/information technology (IM/IT), budgeting, eligibility, and pharmacy. To identify these and explore the options for resolving any differences, the HEC chartered six national task groups:
- Leadership
- Finance and budgeting
- Human resources
- IM/IT
- Clinical
- Administration
In 2007, another task group, for communications, was established to inform stakeholders about and involve them in the integration process.
The task group members were national and local subject matter experts and were co-chaired by a VA official and a Navy or a DoD official. In all, more than 100 individuals served as members of task groups.
Each task group was charged with
- identifying all policies, directives, regulations, and laws (e.g., Titles 5, 10, and 38 of the U.S. Code) specific to each department’s operations in the task group’s subject area that would have to be changed or dropped to allow integration of NCVAMC and NHGL health care operations in the FHCC;
- developing a timeline for the full implementation of the operational plan, including milestones and activities; and
- developing recommendations of ways to overcome any barriers to full implementation of the FHCC.
On October 17, 2005, Winkenwerder and Gordon Mansfield, the VA deputy secretary, announced the joint agreement during a press conference in North Chicago. A local newspaper headline was “Navy, VA do hospital deal; Sailors, vets to get care under 1 roof” (Gibbard, 2005). In a press release, Winkenwerder said that the process of combining the two health centers would be “difficult,” but the benefit would be “the continued provision of accessible, high quality health care for active duty and veteran patients that benefits taxpayers through the reduction of costs by reducing duplication between these two health care delivery systems.” He also said that the collaboration would “improve the seamless delivery of care to patients, from entry into the armed forces through veteran status” (Ellis, 2005).
The national task groups began to meet periodically, usually quarterly, either in North Chicago or in the Washington, DC, area. They were mirrored by local task groups that met more often, usually biweekly but sometimes weekly. The national leadership task group (LTG) met biweekly by telephone to address governance and other organizational and management issues and to oversee the progress of the other task groups. The LTG and some of the other task groups held periodic 2-day retreats and, once or twice per year, all the national task groups met in retreat for several days. There was also a series of cross–task group meetings to address issues that affected two or more task groups.
The procedure was for each task group to develop an EDM for HEC approval for each of the issues in its jurisdiction that could not be decided under local authority. The EDMs were to present options, usually three but sometimes two or four, with pros and cons for each option, and to recommend one option for HEC consideration and decision. The plan was to use the approved EDMs to develop a concept of operations as the basis for a business plan and then for detailed standard operating procedures.
Developing the EDMs was generally a lengthy process involving numerous revisions as they were circulated locally, then at the regional level (Veterans Integrated Service Network [VISN] 12 and Navy Medicine East [NME]), then at the national level (typically involving multiple offices within the VA, the Navy, and the DoD, and on matters involving legislation, the Office of Management and Budget [OMB]), and the Executive Office of the President. Most of the EDMs were not signed until July 2008, more than 3 years after the start of the process.
The EDM process was intended to identify operational differences in
the departments’ policies and procedures and resolve them at the lowest level possible. As it turned out, many aspects of the FHCC required higher-level approval, usually changes in the standard procedures or program policies of one department or the other, or of both. The task groups spent a great deal of time trying to identify who needed to be consulted at the regional or national level, or both, and getting them to the table to make decisions. In some cases, the LTG had to appeal to the HEC to intervene to obtain needed decisions when there was agreement to disagree between the departments. When funding was involved, the department comptrollers and the OMB had to approve. Ultimately, legislative authority was required to resolve some matters, which had to be worked out with the Armed Services committees or the Veterans’ Affairs committees of the House and Senate, or all four of them, and sometimes also with the House and Senate Appropriations Subcommittees for Defense and Veterans Affairs. Despite strong support for VA/DoD health care collaborations by Congress, full legislative authority required to create, staff, and fund the FHCC was not received until the National Defense Authorization Act for FY 2010 (NDAA 20104) was signed on October 28, 2009, less than a year before the FHCC was officially established on October 1, 2010. This created a great deal of uncertainty during most of the planning process, which began in earnest in 2005, about whether the FHCC would be considered to be a military treatment facility (MTF) so that cost sharing would not have to be required from DoD beneficiaries; whether the ownership of the ACC and equipment in the Navy hospital could be transferred to the VA to operate and maintain; what the status of Navy civilian employees would be; and what the funding mechanism would be.
ISSUES AFFECTING THE INTEGRATION PROCESS5
The task groups were oriented by a video teleconference in September 2005 and began work. All the task groups met in Washington, DC, for several days in December 2005 to report on issues, recommend solutions and plans of action, and set milestones for Phase 3 leading to the launching of the FHCC in 2010. Early on, the task groups classified issues they identified as “big rock” EDMs, “critical” EDMs, or issues that could be settled without an EDM. Big rocks were issues that were deemed to be key
__________________
4 National Defense Authorization Act (NDAA), Public Law 111-84. http://www.intelligence.senate.gov/pdfs/military_act_2009.pdf (accessed August 6, 2012).
5 This section of Chapter 3 provides a detailed account of implementation issues encountered at the Lovell FHCC. Table 3-2 summarizes the implementation issues likely to be encountered in creating other integrated VA/DoD health care centers, based on the Lovell FHCC experience.
to success but difficult to resolve and potentially requiring higher-level sign-off, if not legislation.6
Governance was a big rock, because the proposed line of authority from the FHCC director to a board of directors appointed by an interdepartmental group (the HEC) was something that would clearly have to be approved at the national level. Another big rock was the ability to treat DoD beneficiaries the same as they would be treated at the NHGL or at any other MTF; that is, they would not have to pay deductibles and copayments.
Other big rocks included the transfer of Navy civilians to the VA, ACC ownership, funding and reconciliation arrangements between the VA and the DoD, joint pharmacy, treatment of other health insurance, joint asset management, joint acquisition and contracting, joint credentialing, interagency IT network trust, and the safe exchange of patient care data between the VA and the DoD IT systems able to support an integrated VA/DoD health care facility with multiple care locations (Hassan et al., 2008).
Many of the issues were resolved by EDMs approved by the HEC co-chairs, or by other means, such as memoranda for the record, after being thoroughly vetted by many individuals at multiple levels in the VA, the Navy, the DoD, and the OMB—local, regional, and national. Four big rocks, however, required legislative relief, which was not achieved until the passage of NDAA 2010 in October 2009, nearly 2 years after the package of legislative proposals was sent to Capitol Hill. These were the transfer of civilian personnel from the DoD to the VA, ownership of the ACC facility, the scope of benefits for DoD beneficiaries, and a mechanism for joint funding of the FHCC.
The Vision of a Federal Health Care Center
The local leaders of the leadership task group—the director of the NCVAMC7 and the current commander of the NHGL/NHCGL8 as well as key members of their staffs—had a consistent vision of the way the Lovell FHCC should function to achieve its mission of providing seamless health care to all patients, regardless of their status as VA or DoD beneficiaries or providers. The vision was to have, to the fullest extent possible, one
__________________
6 The “big rocks” are enumerated in Hassan et al. (2008).
7 Patrick Sullivan has been the director of the North Chicago Veterans Affairs Medical Center since 2003 and was the associate director for the previous 6 years.
8 There have been three commanders since 2003: Captains Michael H. Anderson (2003–2006), Thomas McGue (2006–2010), and David Beardsley (2010–present). A new commander will be appointed in 2012. Both McGue and Beardsley were posted to North Chicago to work with their predecessors several months before taking command in an effort to preserve continuity of leadership.
set of standards and a single set of processes for meeting those standards. For example, the local leadership wanted a single set of medical bylaws and quality of care standards. They pushed for single systems for finance (e.g., purchasing, logistics and inventory, payroll, assets), personnel and human resources management, facilities management, appointment scheduling, medical records and other IM systems, credentialing, workload measurement, performance measures, and inspector general inspections. They wanted a single operating fund and budget so that the FHCC staff did not have to determine which department’s funds were being used and for what purpose in daily operational decision making. They envisioned a combined medical staff organized in single departments and clinics under one chief medical officer, operating under a single set of bylaws and with one standard of care for all patients.
Governance
The governance goal was to create a unified management and accountability structure for an organization that was to be neither VA nor Navy but a blending of the best of both. The intent was to achieve efficiencies by reducing redundancies and to deliver seamless care to servicemembers and their family members whether they are active duty or veterans or transitioning from active duty to veteran status.
As noted above, in 2005, the VA/DoD North Chicago–Great Lakes Task Force had proposed coequal directors, each reporting to his or her respective department, with coequal associate directors but a unified medical staff. The HEC directed the group to establish a single line of authority, a task made easier when the Navy surgeon general offered to have the Navy take the deputy director position. The EDM also created a board of directors appointed by the HEC to which the VA director and the Navy deputy director would report. The Navy surgeon general called it a “hybrid organization with new paradigms and practices” that would have a changed relationship with the parent organizations, VISN 12 and the Bureau of Medicine and Surgery (BUMED) (Arthur, 2006, p. 5).
This approach was not feasible because it violated the principle of unified executive authority. The department secretaries could not delegate their authority to an entity outside their departments. Congress would have had to create a new executive branch agency, which was not a solution desired either by it or by the administration. Accordingly, the governance EDM was revised in 2007 to comply with existing authority under 38 U.S.C. § 8111 and 10 U.S.C. § 1104.
The revised governance EDM established what it called an integrated governance model. It might have been called the lead agency model, because it made the Lovell FHCC director directly responsible to the VA rather than
to a joint board of directors. The Navy deputy director was dually designated as the commanding officer of military personnel for military matters, including the exercise of the Uniform Code of Military Justice authority. An extensive executive sharing agreement between the department secretaries would be used to spell out how the FHCC would operate in an integrated fashion to provide seamless care to both VA and DoD beneficiaries. The intent was to have an organization that would seamlessly serve both DoD and VA beneficiaries yet be fiscally and operationally accountable for each agency’s assets and costs.
Instead of a board of directors, there would be an advisory board with a similar membership, for example, senior representatives from the Veterans Affairs Central Office, the Department of the Navy BUMED, the Naval Education Training Command, VISN 12, and the NME. There would also be a stakeholders’ advisory council and a local management council of senior VA and DoD staff. Dispute resolution would be handled first by the departments’ respective chains of command, then—if necessary—by the Joint Health Care Facility Operations Steering Group, then by the HEC, and then by the Joint Executive Council (JEC).
Initially, the plan was to organize all operations of the Lovell FHCC through three directorates—Clinical Care, Patient Services, and Facility Support (administration)—which was the standard VA model. Over time, three more directorates were established: first a Dental Directorate (medical and dental are separate commands in the Navy and the dental program for the 50,000 recruits and students each year was a very large program to manage in its own right); then a Resources Directorate (carved out of Facility Support); and finally a Branch Clinics Directorate (the medical program for 50,000 recruits and students each year was also a very large program to manage). Three directorates were headed by a VA associate director and a DoD assistant director, and three were headed by a DoD associate director and a VA assistant director. The expanded number of directorates recognized certain realities—the size and organization of the Navy dental program for recruits and students and the special, time-critical mission of the Navy branch health clinics in ensuring medically fit recruits—and it provided more high-level slots for two organizations that were retaining all those they had employed before the merger. The resulting organization chart is complicated and somewhat unorthodox (see Figure 3-1). It has a bold line for “management authority from executive agreement (EA)” from the command suite to the VA (the command suite box includes the VA director and Navy deputy director). Another line—denoting an “operational line of authority”—connects the VA director to the VA via the VISN and the Veterans Health Administration. A similar line—denoting “military reporting relationship & accountability”—connects the Navy deputy director to the DoD via NME and BUMED. The command suite is connected to the Navy
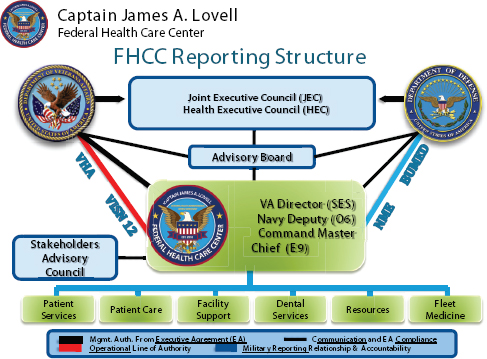
by a dotted line—denoting “communication and EA compliance.” The Advisory Board and Stakeholders Advisory Council also have bold line relationships with the command suite and, in the case of the Advisory Board, to the DoD and the VA for communication and compliance with the EA.
Scope of Beneficiary Services
Another critical issue was the status of DoD beneficiaries. A primary goal of creating the Lovell FHCC was to have a single organization delivering health care to the beneficiaries of both the DoD and the VA to achieve efficiencies and seamless service delivery. The benefits of the 25,000 VA beneficiaries using the NCVAMC were not to be affected by the creation of the FHCC. The problem was that TRICARE Prime enrollees and other TRICARE beneficiaries (when they use an MTF on a space-available basis) are not charged deductibles or copayments, but they are subject to copayments and, in some cases, deductibles if they use a non-MTF facility, such as a VAMC. In fact, from 2006, when all inpatient and emergency services for Navy beneficiaries moved to the NCVAMC, until 2010, when the FHCC
opened, Navy patients used the NCVAMC through the TRICARE network, which required copayments for all patients except active duty servicemembers and their family members.9 This joint venture arrangement involved a third party in a vendor relationship between the VA and the DoD in what was supposed to become a single, merged organization.
The NHCGL was serving approximately 50,000 Navy recruits and students annually. In addition, the NHCGL catchment area contained approximately 59,000 DoD beneficiaries, of whom approximately 19,000 were enrolled at the NHCG. Most of the 19,000 enrolled beneficiaries were TRICARE Prime beneficiaries but some (approximately 500) were TFL and other direct care patients. Most of the 40,000 non-enrolled beneficiaries were non-Prime beneficiaries who could receive care on a space-available basis.
The vision of the Lovell FHCC planners was to serve all these TRICARE patient categories as if they were still using an MTF, that is, without imposing any cost-sharing requirements. It was feared that copayments would interrupt the continuity of care when DoD beneficiaries seen in the ACC (which could be designated as an MTF as long as the Navy retained ownership) were referred to inpatient care or to those specialty clinics located in the VA building. Copayments would also have to be administered by the TRICARE managed care support contractor, which does not become involved when a DoD beneficiary uses an MTF. There was another practical consideration. A DoD analysis of the impact of copayments predicted a 50 percent or greater reduction in DoD beneficiaries seeking treatment at the FHCC because it would no longer benefit them to travel there when they could get private care closer to home for the same or lesser copayments (DoD, 2010). The joint venture was already experiencing a fall-off in demand from TFL beneficiaries for this reason in the period leading up the launching of the FHCC in 2010 (Interviews). The initial strategy was to obtain dual designation as an MTF and a VAMC. However, department lawyers ruled that, because the law (Title 10 U.S.C.) refers to MTFs as “facilities of the uniformed services,” they must be under the direct control of the secretary of defense, which would not be the case with the FHCC.10
In response, the scope of beneficiary benefits in the EDM (originally the dual designation EDM) laid out three options. Option 1 was to change
__________________
9 Military retirees may also qualify for free care as veterans, for example, for a service-connected disability or for all care if they are rated 50 percent disabled or higher.
10 There are uniformed services in three departments: the Department of Defense (DoD) (the Air Force, the Army, the Navy, and the Marines); the Department of Homeland Security (the Coast Guard and the commissioned corps of the National Oceanic and Atmospheric Administration); and the Department of Health and Human Services (the commissioned corps of the Public Health Service), although only the DoD currently has health facilities, that is, military treatment facilities (MTFs) (the Public Health Service stopped running hospitals in 1981).
TRICARE regulations to allow TRICARE Prime enrollees and their family members to receive care at the FHCC without deductibles or copayments as before. Non-enrolled beneficiaries could also receive free inpatient medical, surgical, and pediatric services provided in the VA building if they were referred there by their DoD primary care providers. Option 2 was to seek legislative relief to allow the FHCC to be “MTF-like”—able to serve all DoD beneficiary groups without cost sharing. Option 3 was to have the VA part of the FHCC continue to be a TRICARE network provider, the arrangement in force since 2006 when all inpatient and emergency services for DoD beneficiaries were shifted to the NCVAMC.
The problems with Option 1 were that (1) the number of non-enrolled beneficiaries would be limited by the number of DoD primary care providers required to refer them to non-MTF care, and (2) TFL beneficiaries would have to be charged because the VA is not permitted to bill Medicare, the first payer for these beneficiaries enrollees. The problem with Option 2 was the uncertainty that the departments, the OMB, and Congress would agree to authorize the FHCC to operate as though it were an MTF. Also, the departments would have to pay for the expenses of TFL beneficiaries that otherwise would have been paid by Medicare. The problem with Option 3 was not only that it required cost sharing from non-enrolled beneficiaries but also that it would have involved the TRICARE managed-care support contractor, which created a vendor rather than a direct relationship between the DoD and the VA.
The LTG recommended and the HEC co-chairs agreed to pursue Option 2, with Option 1 as a fallback if authorizing legislation was not passed. The draft bill introduced by Senator Dick Durbin in September 2008 would have “deemed” the Lovell FHCC to be an MTF “for the purposes of eligibility for health care.” When Durbin resubmitted the bill in June 2009, the language was changed to say the FHCC “may be treated” as an MTF “for the purposes of eligibility for health care,” and this language was retained in the version of the bill that became law (NDAA 2010). Although sponsors of the bill thought the language would eliminate the requirement for cost sharing by DoD beneficiaries (Bean, 2009; Durbin, 2009), the language of the law did not explicitly exclude it. The solution was to have the secretary of defense publish a notice in the Federal Register waiving TRICARE deductibles, cost shares, and copayments for eligible beneficiaries seeking care at the FHCC as part of the 5-year DoD/VA Medical Demonstration Project. The notice specifically noted that the waiver was “consistent with current policies and procedures followed at all MTFs” (DoD, 2010, p. 59238). The notice was put on a fast track for publication and appeared three days before the October 1, 2010, advent of the FHCC.
The main downside of the inclusive benefit policy was the loss of Medicare reimbursement for TFL patients because the VA is prohibited from bill-
ing Medicare. The loss was estimated to be between $85,000 and $100,000 per year (the higher amount if use by TFL patients increased because of the lack of copayments). The DoD and the VA agreed to split the lost revenue from dual-eligible TFL beneficiaries through the financial reconciliation process (TFL beneficiaries must elect to be a VA or DoD beneficiary during each episode of care, which could be tracked for cost allocation purposes).
Transfer of Ownership of the Ambulatory Care Center Facility
Another big rock issue was the planned transfer of the Navy-built ACC to the VA. The intent was to have a single organization maintain and repair the buildings on the VA campus, rather than to have two organizations maintain and repair buildings that are interconnected physically and operationally. It made the most sense to have the VA own the ACC because it was already maintaining all other facilities and equipment on the VA campus. The VA would also be providing the utility infrastructure for the new facility. The main argument against the transfer of the ACC was its status if the FHCC did not meet expectations and was dissolved. Another argument emerged when it became questionable whether the FHCC would be designated as an MTF.
The facility ownership EDM, developed by a working group of VA, Navy, and DoD personnel, presented two options. Option 1 was to have the Navy transfer custody and accountability for the new ACC and parking facilities to the VA to achieve unified oversight over and responsibility for the FHCC facilities on the VA campus, which would require legislation. Option 2 was for the Navy to retain ownership of and responsibility for the new facilities, which would not require legislation. It would also make it much less complicated if the FHCC did not work out as planned.
Under Option 1, the responsibility for funding maintenance and repairs and purchasing equipment would be more equitably distributed between the two departments through the financial reconciliation process that was being developed by the financial task group. Each department would pay for the facilities in proportion to its usage of the Lovell FHCC (the financial reconciliation model developed for the FHCC is discussed below).
There was consensus that the new facilities should be transferred to the VA, but current law did not make it easy. The Navy did not have authority to transfer property to any agency other than the other military services. The General Services Administration had authority to transfer a facility that was declared to be surplus, but even assuming a new facility could be declared surplus, the VA would have had to reimburse the Navy for the full value of the facility unless the OMB granted an exemption. The EDM working group drafted proposed legislation granting the Navy the authority to transfer the ACC and related facilities to the VA.
The EDM recommended and the HEC co-chairs approved Option 1 and the seeking of legislation authorizing the transfer of ownership from the Navy to the VA. Draft legislation was vetted up both the DoD and the VA chains of command and worked out with Durbin, who introduced it as an amendment to the NDAA 2009 in September 2008, but it was introduced too late in the congressional process to be adopted. The legislation was reintroduced several more times as the Captain James A. Lovell Federal Health Care Center Act before it was passed as part of the NDAA 2009. Although the legislation was revised in conference, the substance of the section on transfer of property stayed the same. The DoD secretary was authorized, but not required, to transfer the Navy-built facilities and related medical personal property and equipment to the VA without reimbursement, and the VA secretary was authorized to transfer the facilities back to the DoD without reimbursement “in [the] event of lack of facilities integration.”
By this time, the Navy had decided to retain ownership for the time being (the Navy still owned the facilities at the time this report was drafted). One impetus for this was the uncertainty about whether some DoD beneficiaries would be charged copayments and deductibles if the Lovell FHCC was not deemed to be an MTF. If the ACC was an MTF, it could serve DoD beneficiaries without copayments, and no beneficiaries, except TFL, would have to pay copayments to use the VA facilities if they were referred by their primary care providers (this was Option 1 in the scopes of beneficiary benefits EDM, which was the fallback option if legislative authority for the transfer of property was not granted).
Personnel
Another big rock was achieving a single personnel system for all civilian employees. Having a single personnel system would help unify the new organization. It would also avoid a situation that had been encountered in the VA/DoD joint ventures, that is, employees of the DoD and the VA working side by side performing the same jobs but receiving different pay, benefits, incentive bonuses, and other perquisites, which was bad for morale and productivity.
The NHCGL employed 533 civilians under the authority of Title 5. The original plan was to use a mechanism called “transfer of function” to move the Navy civilians into the VA’s Title 38 personnel system without loss of pay and benefits; however, transfer of function can only be used within, not between, executive departments. Ultimately, the transfer of civilians from the Department of the Navy to the VA had to be authorized by legislation. The alternative to legislative relief was to let go the former NHCGL civil-
ians through reduction-in-force actions and rehire them through regular competitive procedures, which would have caused a number of difficulties.
The legislation (NDAA 2010) authorized the DoD and the Navy secretaries to transfer functions required for successful operation of the Lovell FHCC and the VA secretary to accept them. Transferred employees would maintain their rate of total compensation (including physician comparability allowances); not have to undergo the 1-year probationary period normally required of VA employees if they had served the probationary period under Title 5; and, for 2 years, keep collective bargaining rights under Title 5.11 The FHCC had also previously stipulated that no civilian would lose his or her job in the integration.
There were complications:
- Only 40 percent of Title 5 DoD civilians had occupational titles that also existed in Title 38, which meant that 60 percent of them had to be placed in new occupations that were comparable in duties and pay.
- Some NHCGL employees in hard-to-recruit professions were receiving special additional pay, which the VA had to match.
- Some NHCGL workers were employed through personal services contracts (PSCs), which the VA does not have authority to use. The contracts totaled more than $16 million a year, nearly $11 million of which was dedicated to pay more than 100 staff in the dental clinics on the Great Lakes Navy base. The use of the PSCs gave the Navy more flexibility in meeting the ups and downs in the number of recruits and students over time. The solution was to allow the Navy to maintain the PSCs using the Navy Medical Logistics Command (NMLC) rather than to try to convert the contractors to civil service positions.
- Several IM/IT staff members remained Title 5 employees because access to certain computer systems is restricted to DoD employees. Ultimately, the Navy retained 14 NHCGL civilian positions for this reason.
The personnel transfer issue affected two other issues: security clearances and IM/IT access cards.
__________________
11 For example, DoD civilians have the right to appeal adverse personnel actions to the Merit Systems Protection Board, but Department of Veterans Affairs (VA) employees do not.
Security Clearance Policy
To achieve the Lovell FHCC vision, the hope was to have one security clearance policy for all FHCC staff to allow seamless access to IM/IT systems. The Navy’s policy for access to patient records was stricter than the VA’s and used different security clearance procedures and ways of paying for it. As a practical matter, the time and expense needed to achieve secret-level security clearances for all FHCC personnel, as required by the Navy for access to patient records, would have crippled the effort to launch the FHCC on schedule.
The VA’s security clearance system is based on the public trust model and does not require secret clearances. Most VA employees receive either a special agreement check or the National Agency Check with Inquiries (NACI) using the SF85P form—VA executives and managers and IT personnel are subject to two higher levels of security clearance (minimum background investigation or background investigation), using the more extensive SF86 form. The VAMC pays for the costs of the checks.
The Navy’s security clearances are based on the national security model, ranging from confidential, to secret, to top secret, and Navy policy on access to information protected by the Privacy Act requires a secret clearance and the SF86 form. The Navy, not the individual facility, pays the costs of the Access National Agency Check with Inquiries (ANACI),12 about $350 for military servicemembers and $427 for DoD civilians in FY 2011 (GAO, 2012a).
Also, non–U.S. citizens were barred from access to patient information by the Navy except on an individual waiver basis. Approximately a dozen active duty sailors and 10 Navy contractors at the NHCGL were noncitizens requiring an individual waiver. The NCVAMC, in contrast, employed many more noncitizens—about 100—as medical students, interns, residents, and physicians, which would have overwhelmed the individual waiver process. However, the FHCC’s joint teaching mission depends on students, interns, and residents—many of them noncitizens—having access to patient records.
The matter was slow to be resolved because the Navy was reluctant to lower its standards.13 On the other hand, it did not seem to make sense
__________________
12 An “Access National Agency Check with Inquiries” is used for the initial investigation for federal employees at the confidential and secret access levels. It consists of employment, education, residence, reference, and law enforcement agency checks, as well as a national agency check, which includes data from military records and from the Federal Bureau of Investigation’s investigative index (GAO, 2012b).
13 This is one of a number of instances in which the department involved—the VA, the Navy, or the DoD—was reluctant to set a precedent by granting the FHCC an exception. This in turn limited the extent to which the FHCC could achieve internal consistency in its policies and procedures.
to require everyone at the FHCC to obtain a secret clearance just to access the DoD’s EHR system, which does not contain classified information. The situation became more amenable to solution when the Navy’s medical records were moved from the Navy computer system enclave to the Military Health System (MHS) computer system enclave under DoD jurisdiction, because the MHS uses the public trust model used by the VA. At that point, the departments agreed to resolve the minimum level of clearance needed to access the medical IT systems of the DoD through a memorandum of agreement (MOA) rather than an EDM.
The impasse was eased further when legal counsel advised that a secret clearance is not legally required to access information protected by the Privacy Act. However, the Navy insisted on requiring all FHCC employees to undergo an ANACI investigation. The MOA, not signed until October 20, 2010, required an SF86 form and an ANACI investigation of all VA personnel but allowed interim access for a year while the investigations were conducted. U.S. citizens and permanent residents who had completed a NACI investigation by October 1, 2010, were allowed access to the DoD system until they successfully completed the ANACI process. U.S. citizens and permanent residents who arrived after October 1 had to undergo the SF86/ANACI process but would be given interim access after a favorable fingerprint check and confirmation that the Office of Personnel Management (OPM) had scheduled an investigation. The solution to the need for foreign students, interns, and residents to have access to patient records was to continue the VA’s policy of requiring NACI investigations and to allow local authorities to grant access to the clinical applications in DoD’s Armed Forces Health Longitudinal Technology Application (AHLTA) EHR system to the extent required by each individual’s duties.
Implementing the ANACI clearance process was a substantial undertaking. The VA was not set up to process more than 900 ANACI clearances, even on a phased basis. Lovell FHCC staff assisted the VA in reducing the submission time of ANACI requests to OPM from several months to a few weeks.
Access Cards
To provide seamless, coordinated, and safe care, VA employees need a way to access AHLTA and other DoD electronic information systems. Similarly, active duty personnel need a way to access the VA’s Veterans Health Information Systems and Technology Architecture (VistA) EHR and other information systems, for example, the financial management, decision support, and acquisition and contracting systems. Each agency uses access cards to control access to their computer systems. Again, the DoD has stricter policies. The DoD does not allow anyone outside the DoD to
have a common access card (CAC). The solution was to enable employees with CACs to access VA systems and to allow VA employees to use their personal identity verification (PIV) cards to access AHLTA (but not other DoD systems), which took some time to negotiate and required expensive software and hardware changes and updates.
The changeover was briefly interrupted when the VA decided to upgrade the security code of its PIV cards nationally, without realizing the impact this would have on the logistics of having everyone at the Lovell FHCC obtain AHLTA-enabled PIV cards by October 2010. The upgrading was delayed.
Interagency Information Technology Network Trust
The plan was to connect the two department computer systems with a wide bandwidth fiber optic cable so that everyone could access both systems through his or her computer. As noted above, a JIF-funded fiber optic cable was installed between the campuses to allow this to happen. Each department had protocols, however, for allowing access to their computer systems, called “interagency IT network trust.” The alternative was to have two computer rooms and networks and two computers on each desktop. The problems were the stricter standards for “dot.mil” than for “dot.va” systems, programs, and applications, and the high level of review and approval that would be needed in each department to upgrade the VA systems to dot.mil standards and establish a gateway between the systems. On the DoD side, for example, the Defense Information Systems Agency had to agree that adequate interagency trust was achieved, and final sign-off authority at the DoD was at the deputy secretary level.
Interagency Funding Mechanism
Another goal of the Lovell FHCC integration was to have a unified financial system. Part of this goal was to fund the FHCC in a way that was not categorical, for example, “these are VA dollars that must be used for this but not for that,” and “these are DoD dollars that can be used only for these purposes.” Other aspects of what the FHCC planners called the “unified financial vision” are presented below.
The Lovell FHCC could not receive funds directly from the DoD or the VA for the same reason it could not be run by a board of directors. This would make it an independent federal agency, which was not the intent. The first alternative was to explore whether the JIF could serve as the funding vehicle. Congress had established the JIF as a Treasury fund to which the departments could contribute funding for joint venture projects. Although the NHGL/NHCGL and the NCVAMC had received a number of JIF proj-
ects to fund joint services and infrastructure, they were expected by the DoD and the VA to be self-sustaining within 2 years. There was resistance from both the executive and the legislative side to expanding the purpose of the JIF so substantially from its original purpose and scope.14
Ultimately, Congress established a separate Treasury fund for the Lovell FHCC, called the Joint Medical Facility Demonstration Fund (JMFDF). The demonstration fund was established on the financial accounting ledgers of the VA, and the VA and the DoD were authorized to transfer funds that are authorized and appropriated specifically for the FHCC in amounts determined by a formula agreed to by the two department secretaries. This is tighter control than Congress exercises over the JIF, to which the departments are directed to contribute “at least” $15 million per year each and to use the funds until expended (i.e., “no-year” money). The Armed Services committees are requiring annual authorization of 1-year funding of DoD contributions; the VA committees are authorizing funding that can be used over a period of 2 years. This difference in congressional policies had an upside; it allowed the FHCC to be funded by the VA during the first few months when the DoD appropriation was held up by a continuing resolution (CR) in Congress.
Ambulatory Care Center Building and Equipment Ownership
The original plan was to transfer the Navy-built ACC to the VA immediately, which, it was determined, would require legislation to permit. Subsequently, the Navy decided to hold off on transferring the building because of concern about losing MTF status for the ACC when it became apparent that the entire Lovell FHCC would not be designated as an MTF. The legislation (NDAA 2010) states that the Navy may transfer the building to the VA at any time during the 5-year demonstration period. The legislation also included procedures for transferring the building back to the Navy if it was decided not to continue the FHCC during or after the demonstration period. Keeping the ACC under Navy ownership also avoided a VA requirement that the pharmacy be equipped with ballistic glass.15 At
__________________
14 “The purpose [of the DoD-VA Health Care Sharing Incentive Fund] is to provide seed money for creative sharing initiatives at facility, regional and national levels to facilitate the mutually beneficial coordination, use, or exchange of health care resources, with the goal of improving the access to, and quality and cost effectiveness of, the health care provided to beneficiaries of both departments” (DoD/VA, 2009).
15 According to the VA’s security handbook, at the time the ambulatory care center was constructed, “Windows and walls of pharmacy dispensing must meet the U.L. Standard 752 for Class III Ballistic Level” (VA, 2004). This requirement was continued in the 2010 update of the handbook (VA, 2010b).
the time this report was drafted, there were no active plans to transfer the ACC to the VA.
Financial System and Reconciliation
The accounting system may seem to be a trivial part of such a substantial organizational effort, but the vision of the Lovell FHCC was for each partner to pay for its share of the health care provided by the FHCC. This required the development of an accounting system meeting both departments’ needs. Such an accounting system did not exist. After much discussion at different levels and a summit meeting of the VA chief financial officer, the BUMED deputy chief of resource management, and the director of health budgets and financial policy in the Office of the Assistant Secretary of Defense for Health Affairs, the decision was made to adopt the VA’s Financial Management System (FMS) as the basis for a unified financial system.
Once the FMS was chosen, it became logical to adopt other VA administrative systems compatible with it, such as the VA decision support, payroll, and logistics systems. The key question was whether the VA’s Decision Support System (DSS), a managerial cost accounting system, could accurately allocate costs to the services provided to VA beneficiaries and DoD beneficiaries so that each department could be charged appropriately.
The DSS was developed by adapting commercial software to interface with and be populated by VistA and other VA databases to provide data on costs of goods and services for patients down to the encounter and laboratory test level. According to the VA,
DSS provides a mechanism for integrating expenses, workload, and patient utilization. DSS information supports process and performance improvement by measuring quality of care, clinical outcomes, and financial impact.16
The problem was that the DSS did not accept financial and workload data from DoD systems in a manner that could be used for both the workload and costing portions of the financial reconciliation process. First, the departments had to agree on how to measure workload. Accordingly, workload data documented in VistA (for example, VA primary care, inpatient care, and the combined VA/DoD specialty care) are obtained from the VA’s Allocation Resource Center (ARC) on a quarterly basis and provided to the DoD’s Office of Health Affairs (OHA). This workload is then imported into Centers for Medicare & Medicaid Services (CMS) tables to determine
__________________
16 See http://www.virec.research.va.gov/DataSourcesName/DSS/DSSintro.htm (accessed October 14, 2012).
the relative value unit (RVU), relative weighted product (RWP), and dental weighted value (DWV) workload values. The workload statistics documented in DoD systems (such as the branch health clinics and the DoD primary care clinic) are obtained by the OHA from DoD’s M2 system, which determines enhanced CMS values for all MTFs (Lovell FHCC, 2010b).
For the cost allocation portion of the financial reconciliation process, the Defense Medical Human Resources Systems-internet (DMHRSi) is used to document and capture labor costs for active duty personnel, DoD contractors, and the few remaining DoD civilian positions. DMHRSi labor costs are then mapped into the DSS, which allows all FHCC costs to be contained within it. The FHCC’s health care business office processes DSS costs for the quarterly financial reconciliation and provides that output to the OHA for final processing. The FHCC, the OHA, and other stakeholders are presently developing an automated reconciliation process, as outlined in the financial reconciliation EDM.
In order to meet the requirements of the Economy Act, there was a need for budget reconciliation such that each department would pay only for the amount of care provided to its beneficiaries while functions unique to one department should be funded only by that department (Opsut, 2011). The latter are called mission specific pass-throughs (MSPTs), for example, recruit medical and dental care for the Navy and veterans nursing home and long-term care for the VA. The approach adopted was to divide all care into 10 “buckets” (categories); determine the total cost of each of the categories using the DSS; use the industry standard workload measures to determine the proportion of workload accounted for by each department’s beneficiaries in each category; multiply the proportion times the total cost in each category to get each department’s costs; and sum the costs across the 10 categories to determine each department’s total costs (see Table 3-1 for the 10 categories and workload measures). The MSPT costs are then added to determine the final bill.
Applying this model to FY 2009 data from the DSS and DoD’s cost accounting system found that services to VA beneficiaries cost $119.6 million (including $36,000 from DoD providers) and services to DoD beneficiaries cost $60.3 million (including $8.3 million from VA providers). Once the Navy’s higher MSPT costs for the branch medical clinics were added in, the total costs were nearly split, $196.9 million for the VA versus $187.1 million for the DoD.
Historical trends are being used to fund the Lovell FHCC for the first 3 years (FY 2011–FY 2013), after which the reconciliation methodology will be used to determine each department’s costs. It is too early to tell if utilization patterns will shift enough to substantially change total costs or their allocation between the departments, or both. If utilization declines
TABLE 3-1 Workload Categories and Measures
| Categories | Workload Measures |
| Non–mental health inpatient | MS-RWPs adjusted for length of stay |
| Mental health inpatient | Bed days |
| Outpatient | Work + practice RVUs |
| Same-day surgery | Work + practice RVUs + APCs |
| Emergency department | Work + practice RVUs + APCs |
| Outpatient laboratory | Work + practice RVUs |
| Outpatient radiology | Work + practice RVUs |
| Outpatient pharmacy | Actual costs |
| Prosthetics | Actual costs |
| Dental | Actual costs |
NOTE: APC = ambulatory payment classification; MS-RWP = Medicare severity relative weighted product; RVU = relative value unit.
while fixed costs stay the same, it will be difficult for the Lovell FHCC to be more economical than its predecessor organizations.
Purchasing of Supplies
The choices were to use the Navy supply system, the VA supply system, or both. The preference was to use one system for the Lovell FHCC to best support the unified administration of the FHCC rather than two systems side by side. The decision was to use the VA system because it was compatible with the FMS that was going to be used (the VA’s).
The VA’s Great Lakes Acquisition Center (GLAC) also had an advantage because of its higher contracting limit than that of the National Naval Medical Center Portsmouth ($100 million versus $10 million), although supplies might be more expensive through the VA because the DoD purchases in larger quantities. There was also a concern whether the GLAC had the capacity to keep the Navy recruit clinics supplied on a timely basis. Another issue was how to supply non-NHCGL medical activities (e.g., Naval Hospital Corpsman School, Naval Drug Screening Laboratory, Naval Institute for Dental and Biomedical Research).
After a year’s experience using the GLAC, the FHCC is drafting a revised acquisition and contracting EDM recommending that the NMLC and the Naval Facilities Engineering Command (NFEC) be added to the GLAC as sources of supplies and services. The NMLC was already being used for the PSCs for personnel working in the branch clinics on the east campus, because the VA does not have authority for PSCs and converting the contractors to federal civil service employees would have been much more costly. The recommendation to allow the use of the NFEC results
from the need to have a mechanism for repairing the branch health clinics, which are Navy facilities on Navy land (the EA specifies that each department is responsible for maintaining its own buildings).
Asset Management
Like other administrative functions, the Lovell FHCC planners hoped to use one asset management system rather than two programs to enhance accountability and efficiency. The DoD and the VA each had an automated program for asset management. DoD’s asset management program was and still is the Defense Medical Logistics Standard Support (DMLSS) automated information system, a Web-based program that was deployed in 2001. The VA’s system is the disk operating system (DOS)-based Generic Inventory Package (GIP).17 The administrative task group recommended using the VA asset management system for the same reason they had recommended using the VA’s systems for personnel, acquisition and contracting, payroll, and decision support, namely, because it interfaced with the VA’s FMS, the financial system chosen for the FHCC.
At the time the asset management EDM was being developed, the VA was developing a new automated asset management program as a component of its Financial and Logistics Integrated Technology Enterprise (FLITE) program (VA OIG, 2010).18 The new asset management program will be a customized version of MAXIMO, a commercial, Web-based asset management software program, and will replace the GIP. However, the MAXIMO program was not ready for use in October 2010, and the FHCC has had to continue to use the GIP. The former Navy personnel were unhappy because the DOS commands used in the GIP are much clumsier to use than DMLSS’s point-and-click system and some of the prices are higher (Interviews). The FHCC has submitted a revised asset management EDM recommending that the use of the DMLSS be explored, and a VA/DoD work group was chartered in September 2012 to explore the feasibility of using the DMLSS at the FHCC and, potentially, at other joint venture sites.
Pharmacy
The Lovell FHCC vision was to have a single pharmacy, with a single drug formulary, rather than to have VA and DoD pharmacies with different formularies operating side by side in the ACC, to simplify administration, reduce personnel costs, and avoid a perception of unequal benefits between
__________________
17 The VA also has a separate specialized prosthetics inventory program.
18 The Financial and Logistics Integrated Technology Enterprise program, except for the MAXIMO module, was canceled in 2010 for lack of progress.
VA and DoD beneficiaries. The decision to have one pharmacy was also driven in part by space considerations. The pharmacy area and number of outpatient windows had been reduced when the size of the ACC was halved, on the assumption that refills would be provided by mail using the VA’s CMOP.
Other issues that had to be addressed were the following:
- Pharmacy security. VA regulations require that pharmacy windows and walls be bullet proof. The DoD requires that every patient be counseled when filling a prescription, and opposed having a window at the dispensing counter. Redesigning the pharmacy area to include a room for counseling that met the VA’s ballistic standards—typical of VA pharmacies—would have reduced the pharmacy’s already minimal storage area by a third, cut the number of automation units from three to two, and increased construction costs. An impasse was avoided when the Navy decided to retain ownership of the ACC.
- Choice of formulary. Because of differences in populations served, the VA and the Navy had different formularies. Lovell FHCC planners would have preferred to create a new FHCC formulary—including pediatric and women’s medications—which combined and reduced overlaps between the VA and the DoD core formularies, but after much discussion, the outcome was to continue to use the VA formulary for VA patients and a combination of the VA formulary and the current Navy formulary for DoD beneficiaries.
- Choice of prime vendor. The Lovell FHCC hoped to use the DoD or the VA pharmaceutical prime vendor that offered the best terms to maximize purchasing power and economies of scale. This would have required the FHCC to stop using the current VA or DoD prime vendor, which might have violated the contract. The decision was made to have a single prime pharmacy vendor in 2012, after existing VA and DoD contracts expired and a new combined contract could be competed.
- CMOP access for all DoD beneficiaries for prescription refills. The Lovell FHCC wanted to use the VA’s CMOP service for DoD beneficiaries to save money and also to reduce waiting time at the space-limited pharmacy. The DoD does not participate in the CMOP and did not wish to set a precedent by making an exception for the FHCC.19 There was hope that the tri-service integration
__________________
19 The DoD experimented with the use of the Consolidated Mail Order Pharmacy (CMOP) at three MTFs in FY 2003. The Government Accountability Office reported that drug costs using the CMOP were 3.9 percent less than the DoD’s, but this saving was offset by the ad-
-
of health care services in the National Capital Area would set a precedent, but that did not work out when it was determined that the CMOP would not be cost effective there. It was also possible that permitting DoD beneficiaries to use the CMOP would require legislative action. The CMOP option for DoD beneficiaries was dropped, although the FHCC continues to seek permission to use it (Interviews).
- Pharmacy inspection. The Lovell FHCC hoped to have a single inspection process for the pharmacy rather than separate inspections by the VA and the Navy. The departments did not agree, and both are inspecting the pharmacy.
- Use of Navy pharmacy technicians as technician checkers at the FHCC or just at Navy branch clinics. The clinical task group (CTG) hoped to rotate Navy and civilian pharmacy technicians who completed military pharmacy training through the Lovell FHCC, satellite, and three Navy branch clinic pharmacies. This would reduce the number of licensed registered pharmacists needed to staff the three Navy branch clinics by up to five and also would maintain the operational readiness of Navy pharmacy technicians for deployment to combat operations.20 However, VA pharmacy regulations do not allow the use of technician checkers, and the Joint Commission would have to expand its current waiver allowing MTFs to use technician checkers to the FHCC. The recommendation was to use pharmacy technicians only at the Navy branch clinics, which did not require any rule changes and still contributed to the operational readiness of the Navy pharmacy technicians.
- Ensuring patient safety. Using two EHR systems for the same patient population raised the specter of patient injury because of negative drug interactions or allergic reactions occurring when the provider and pharmacist using one EHR system is unaware of prescriptions or allergies entered into the other EHR system. For this reason, the CTG had prefaced its pharmacy options with a caveat that everything depended on orders portability for
____________________
ministrative costs of maintaining the pharmacies at the MTFs. The DoD did not want to close the MTF pharmacies, which are necessary for filling initial prescriptions and are convenient for the MTF’s TRICARE Prime users. It was concerned that if it closed the MTF pharmacies, at least some beneficiaries would join the growing percentage of beneficiaries using retail pharmacies—the most expensive option for the DoD—instead of using the CMOP (already, from 2001–2004, the percentage of pharmacy benefit customers using retail pharmacies rather than the MTF pharmacies or TRICARE’s mail order pharmacy program had increased from approximately 26 to 42 percent) (GAO, 2005).
20 Navy pharmacy technicians (Navy Enlisted Classification HM-8482) are qualified to prepare and dispense prescribed pharmaceuticals (U.S. Navy, 2011, p. 168).
pharmacy because of its critical role in ensuring patient safety. Orders portability for pharmacy—the ability to enter a prescription into either the DoD EHR system or the VA EHR system and have it appear in the other system simultaneously so that potential drug interactions and allergies could be recognized—was one of the basic IM/IT requirements that was supposed to be operational by October 1, 2010. As it became clear that this would not be achieved and would pose an unacceptable threat to patient safety, an interim workaround solution had to be developed.21 Funded as a $1 million JIF project for 1 year, the plan involved hiring seven to nine additional pharmacists to perform manual checks and finding room for them to work. Ultimately, only five pharmacists were needed, but the pharmacy space is still very crowded. Since then, the project has been extended past 1 year.
When the DoD and the VA secretaries agreed in March 2011 to develop jointly a single EHR system to replace their legacy systems (AHLTA and VistA, respectively), they decided to complete the undelivered IM/IT solutions for the Lovell FHCC as part of the new joint EHR system development process. This included orders portability for pharmacy (also orders portability for consults and referrals). The new EHR system is being developed in stages, but the pharmacy is in the initial development group, with the FHCC designated as the primary development site. The current schedule is for it to be ready for use in 2014.
Patient Records
The vision of the Lovell FHCC was for VA or Navy beneficiaries to be treated by either VA or DoD providers (depending on availability) so that care was seamless from the patient’s perspective. This meant that Navy providers would have to be able to access and update the patient records of VA beneficiaries they treated in VistA (the VA’s EHR system) and VA clinicians would have to be able to access and update the patient records of DoD beneficiaries in AHLTA (the DoD’s EHR system) as well as in VistA. There was also a need for information recorded in VistA for Navy patients (e.g., inpatients, those using the ED, and those seeing VA specialists) to be replicated in AHLTA, so that their medical operational readiness could be determined and their medical records would be complete when they left for new assignments beyond North Chicago. Orders for laboratory and radiol-
__________________
21 The events leading to the delay of orders portability for pharmacy and other computer software interoperability solutions are described in more detail in the next section, on information management systems.
ogy tests, for prescriptions, and for consultations and referrals and their results needed to be viewable in both systems regardless of the system in which they were entered, a capability called orders portability. As discussed above, orders portability for pharmacy was especially important to prevent drug interactions and allergic reactions.
As of 2006, when the Lovell FHCC’s IM/IT systems were being planned, VA and DoD providers had limited access to each other’s patient information. The two departments had developed two interim solutions for sharing clinical information: (1) the Bi-directional Health Information Exchange (BHIE), a program that enables VA and DoD providers to view clinical data from each other’s EHR system, and (2) the Clinical Data Repository/Health Data Repository (CHDR), a program that enables VA and DoD clinical data repositories to share computable pharmacy and drug allergy data. The BHIE was initially implemented in 2005, and the CHDR was at the field-testing stage in 2006.
NHCGL and NCVAMC providers had dual icons on their computer screens for accessing the two EHR systems; however, there were significant limitations to the functionality of the two programs (DoD, 2011). Providers had to log on to each EHR system separately. VA provider access was on a read-only basis, which meant that information on inpatient, emergency, and specialty provider encounters on the west campus had to be entered into AHLTA separately. The information only pertained to “active dual consumers,” that is, military retirees also eligible for VA health care, not active duty servicemembers who had not yet retired, such as the recruits, students, and staff at Great Lakes (although arrangements could be made—and were—to flag recruits and other active duty servicemembers at Great Lakes as active dual consumers). The ability to look back, that is, see information from earlier encounters, was limited. In addition, CHDR/BHIE functionality was not expected to be reliable enough in 2010 to meet the tempo of health care delivery at the Lovell FHCC, especially for the recruits for whom medical status had to be current on a daily basis (Maldonado and Poulin, 2012). As the pharmacy discussion (above) indicates, the CHDR was not considered reliable enough for patient safety and an interim manual workaround was instituted and is still in place. The BHIE is still considered to be too awkward and too slow to use in patient encounters (Interviews).
From the beginning, the CTG recommended having one patient record system or a single-user interface to both systems (VistA and AHLTA) for entering and retrieving patient clinical information. The CTG concluded that it would not be realistic to expect a single EHR system to be ready by the time the FHCC opened in 2010. Given the continuing existence of VistA and AHLTA, the focus was on achieving interoperability, that is, finding a user-friendly front-end or back-end software bridge between the two systems so that clinicians could log onto either system and see, enter, and
update patient information in both systems simultaneously (Brewin, 2007). Single entry into and simultaneous access to both systems would not only be more efficient, it would promote continuity and coordination of care and help reduce errors that might affect patient safety.
The departments agreed with the need for interoperable EHR systems when the Lovell FHCC was launched in 2010. Development of interoperability solutions—beginning with the identification of system requirements to meet the needs of the clinicians and the identification of sources of funding for development—began in earnest in late 2007. A proposal for JIF funds was developed for $11 million for support for 2–2.5 years of a joint local program management office and a joint enterprise-level (i.e., national-level) office for systems development (Hassan et al., 2008). The proposal, which was funded, was justified in part on the basis that the interoperability solutions—although expensive to develop—could be used by all VA/DoD joint health care ventures (VA/DoD, 2009, p. 46) and could potentially be exported to all other VA and DoD facilities to provide a seamless medical record from active duty to veteran status. The $11 million was for developing the requirements, not the solutions. Funding for the latter was estimated to be $100 million over 3 years.
A tiger team was dispatched several times to North Chicago to identify the technical requirements for critical interoperability solutions—including a single sign-on solution that would allow providers to log in once to see clinical data from both AHLTA and VistA (including the medical readiness status of active duty servicemembers).
When the JIF funds became available, contracts were awarded to complete the specifications for solutions that would meet the Lovell FHCC’s baseline functional requirements when it started up in 2010. The CTG had come up with various lists of critical functional requirements. Certain items were common to those lists:
- Single patient registration in AHLTA and VistA
- Single medical sign-on to access AHLTA and VistA
- Single entry into either AHLTA or VistA that allows the user to
- enter and view the results of laboratory, radiology, and pharmacy orders, and order and view consults and referrals, and have them appear in the other system while preventing duplication (i.e., orders portability)
- read test results and progress notes originating from either system and enter or revise them once and have them appear in both systems
- be assured that the records are for the same patient, regardless of the application, a function called “context management”
- Medical operational readiness status, for example, the ability to enter readiness data into VistA that is viewable in AHLTA throughout the world
In addition to single patient registration, single sign-on, and orders portability processes and support for the DoD operational readiness system, the contractors also worked on requirements for outpatient appointment scheduling and for producing data on clinical costs and workload needed for financial reconciliation. The requirements for these six capabilities were completed in July 2009 in the form of business requirements documents for each.
The next step was to obtain the $100 million needed to develop the interoperability capabilities, which were supposed to be ready by June 2010, leaving 90 days to ensure that they were stable before the FHCC opening. A proposal to use the JIF mechanism to provide the $100 million was submitted in mid-2009 and it had to be reviewed by the OMB and the congressional appropriations committees before it was approved in August 2009. By this time, the likelihood of completing the set of initial EHR system capabilities by October 2010 was fading, and the departments began to prioritize among them. In July 2009, the DoD notified Congress that the departments were seeking to have three of the key capabilities ready by October 2010: (1) single patient registration, (2) single sign-on with context management for clinical users, and (3) the “first phase” of orders portability for laboratory, radiology, pharmacy, and consultations and referrals. In October 2010, they expected to be just beginning the development of applications to support the Navy’s operational readiness requirements, in the process of developing the requirements for producing financial reconciliation data, and exploring a joint appointment scheduling system (U.S. House of Representatives, 2009). In its annual report, the JEC also reported that single patient registration, single sign-on, and orders portability were the three necessary initial capabilities for implementing the Lovell FHCC, noting that the $100 million in JIF funding was not approved until August 2009, “leaving little time for IT design, development, testing, information assurance, and deployment” (VA/DoD, 2011, p. 41). However, the EA between the departments signed in April 2010 specified that single patient registration, single sign-on, and orders portability would be ready on opening day, as well as documentation of medical and dental operational readiness of recruits and other active duty servicemembers (DoD/VA, 2010, Attachment A).
The funding plan was for the departments to deposit $25 million each in the JIF funds in FY 2009 and another $25 million each in FY 2010, for a total of $100 million. The VA and the DoD began the contracting process using the FY 2009 funding in August 2009. The VA was able to deposit and
use the FY 2010 funding, but the DoD could not because its appropriations bill had not been passed and the DoD was operating under a CR. This delayed DoD funding of work on orders portability until January 2010. DoD funding was further held up by a congressional committee pending submission of a report on joint medical IT.
By early 2010, it was evident that orders portability for laboratory, radiology, pharmacy, and consultations and referrals were probably not going to be ready by October, and that a “Plan B”—a workaround solution—was going to be necessary for the pharmacy to assure patient safety. In February, the VA’s chief information officer told Congress that single patient registration, single sign-on, and orders portability for laboratory, pharmacy, and radiology would not be ready until the end of November 2010 (and orders portability for consults not until later in 2011), which would delay the move of the Navy’s outpatient clinics to the ACC (U.S. House of Representatives, 2010, p. 39). At that time, “significant concerns regarding the ability to deliver IT capabilities in such a compressed time frame were elevated to the Deputy Secretaries of Defense and Veterans Affairs” (VA/DoD, 2011, p. 41). They assigned the Interagency Program Office (IPO) to oversee and coordinate the Lovell FHCC IM/IT development effort. The IPO developed a joint interagency master schedule and established an executive committee of top national and local VA and DoD IT officials that met biweekly. The VA and the DoD controlled the funding, however, and proceeded to develop the interoperability capabilities on parallel tracks, which made it difficult for the IPO to coordinate the development process (Filippi, 2011). The IPO reported later that it encountered long lead times because of the separate review processes within each department and the need to adjudicate differences (IPO, 2012, p. 6).22
The main stumbling block in developing orders portability for pharmacy was the need to have sequential prescription numbers that are the same in both EHR systems, which could not be achieved without making changes in AHLTA and VistA. The departments, however, had agreed that no changes would be made in those legacy systems. This left a gap in IT capability, because the orders in VistA would not be consistent in AHLTA, and vice versa. “This gap created several unacceptable patient safety risks that could only be overcome by having licensed pharmacists manually input the necessary functions that will be performed automatically when the IT solution is deployed” (VA/DoD, 2011, p. 57). The departments agreed to provide $1 million through the JIF to fund up to seven pharmacists for a year as a workaround until orders portability for pharmacy could be de-
__________________
22 The DoD and the VA revised the Interagency Program Office charter in October 2011 to make it “the single point of accountability for [i.e., have the authority to manage] the development and implementation of the integrated electronic health record” (DoD/VA, 2011).
veloped, which was estimated to be ready by the last quarter of FY 2011. This arrangement has been extended beyond 1 year until the pharmacy capability of the joint VA/DoD integrated EHR (iEHR) system is developed, currently scheduled to occur in 2014 (the iEHR, the next generation EHR system being developed jointly by the VA and the DoD to replace VistA and AHLTA, is described at the end of this section).
Meanwhile, the schedules for the other capabilities proved to be too ambitious and were not met. Each department was developing solutions for its own system and testing them in laboratory conditions rather than in a live environment (GAO, 2011, p. 21). In some cases, the two department solutions did not work well together when field-tested in North Chicago. For example, each department selected a different commercial program for single sign-on with context management, and it proved to be difficult for the two programs to work together through DoD’s firewall and server. Mostly, it just took longer than expected to develop the various capabilities and then longer than expected to implement them because of unexpected glitches. As Lovell FHCC IT leaders put it, “integration was dependent on the computer systems functioning as planned” (Poulin et al., 2012). Unfortunately, things did not always go as planned.
The single patient registration and single sign-on with context management capabilities were delivered to the Lovell FHCC on December 13, 2010, and were operational by the end of the month, except for delays in access to single sign-on for some users and limitations on context management because of inconsistent family member codes between the DoD and the VA and other problems. Because of continuing problems with using two single sign-on with context management programs at Lovell, the IPO recently decided to use just one of the two programs for use in the iEHR system (Brewin, 2012).
Orders portability for laboratory and radiology were also delivered in December 2010, but user testing found that additional testing and development were required (IPO, 2011). Limited use of orders portability for radiology and laboratory was deployed in March 2011, but the Lovell FHCC decided to delay implementation of orders portability for laboratory until radiology was running smoothly—that is, achieving a rate of 90 percent matching of patients with images—which was achieved by the end of 2011 (GAO, 2011). Orders portability for laboratory was deployed initially in a few clinics in January 2012, after remaining software defects, complete user account and laboratory test mapping, and patient registration issues were resolved.
Current Status of Information Management/Information Technology for Patient Care
As of June 2012, when this report was written, the status of IM/IT for patient care was as follows:
- Single patient registration. Deployed on December 13, 2010. Operational after fixes to accommodate batch processing of recruit classes.
- Single sign-on with context management. Deployed on December 13, 2010. Operational after fixes to deal with inconsistent family member codes used by the DoD and the VA. Continuing problems aligning DoD and VA versions of the program. Due to be replaced by a single program as part of the iEHR system.
- Orders portability for pharmacy. This capability turned out to be too complex to develop by the end of 2010. In March 2011, when the DoD and VA secretaries decided to jointly develop a single EHR system (the iEHR), they elected to use the iEHR’s orders portability solutions for pharmacy and for consultations and referrals at the Lovell FHCC rather than continue to attempt to develop an interoperable solution using the legacy systems, VistA and AHLTA. In the interim, five registered pharmacists are conducting manual checks of prescriptions for potential drug interactions and allergies at a cost of approximately $700,000 per year.
- Orders portability for radiology. User testing in December 2010 found that further development was needed. It was initially deployed in June 2011 and fully operational by the end of 2011.
- Orders portability for laboratory. User testing in December 2010 found that further development was needed. Deployment was delayed until January 2012, after orders portability for radiology was implemented and made fully operational.
- Orders portability for consultations and referrals. This capability is complex to develop and, early in 2010, it was postponed until later in 2011, in favor of making single patient registration, single sign-on, and orders portability for laboratory, radiology, and pharmacy ready for the opening of the Lovell FHCC. Along with orders portability for pharmacy (see above), the DoD and VA secretaries decided in March 2011 to cancel the effort to make consultations and referrals interoperable between the two legacy EHR systems and instead to develop a single joint solution as part of the iEHR system. This would have delayed the capability for several years. Subsequently, given the urgent need for this capability at the Lovell FHCC, an effort to develop an interoperable solution for the
FHCC has been reestablished. As of September 2012, consult and referral interoperability was being phased in.
Plans for a Joint Department of Veterans Affairs/Department of Defense Electronic Health Record System
In 2010, the VA and DoD secretaries began to meet every two months to discuss progress on developing a joint disability evaluation system to replace their separate systems and interoperability between their EHR systems, and the situation at the Lovell FHCC was an explicit agenda item. In early 2011, aware of major problems in the effort to develop interoperability software for use at the FHCC, they decided to halt the upgrade programs for their respective EHR systems, AHLTA and VistA, and instead develop a new EHR system for joint use, dubbed the iEHR.
Aware of the ongoing needs at the Lovell FHCC, they decided to follow through on the software programs that were in advanced development for the FHCC, namely, the programs for radiology and laboratory orders portability. The two programs in early development, which were orders portability for pharmacy and consults and referrals, were stopped in favor of developing a single joint solution for them as part of the iEHR. Recognizing the need at the Lovell FHCC, the pharmacy solution was chosen to be one of the first several products of the iEHR development process, with the FHCC as the alpha test site. The goal is to have an operational pharmacy program for the FHCC in 2014. Meanwhile, the FHCC will continue its workaround arrangement for ensuring patient safety from harmful drug interactions and allergies. At the time this report was drafted, there were discussions about restarting the development of an interoperable capability for consults and referrals because of the lack of a workable temporary workaround such as that for pharmacy.
Among the early decisions on the structure of the iEHR was one to adapt Janus, a user interface developed for the joint venture in Hawaii, which allows clinicians at the Honolulu VAMC and the Tripler Army Hospital, which provides inpatient care for veterans, to read a patient’s records in both systems. In December 2011, the Lovell FHCC began testing Janus in its clinics. In its current form, it is read-only, but it does pull the information into a single view rather than requiring a provider to look at information in the VA and the DoD EHR systems separately. The plan is to further develop Janus so that patient information can be entered and updated, as well as viewed, in real time.
Credentialing and Privileging Clinical Providers
The VA and the DoD database software packages that are currently used to credential independent licensed and licensed non-independent health care providers—VetPro and the Centralized Credentials and Quality Assurance System (CCQAS), respectively—are not interoperable, although each is designed to meet the same Joint Commission standards. FHCC planners preferred to have a single system wherever possible for efficient operation of the FHCC. In this case, however, there was early agreement that both credentialing systems had to be maintained because information about active duty providers had to be in CCQAS when they transferred to their next duty station, and information about VA providers had to be in VetPro for the same reason. In addition, CCQAS includes information about adverse actions, training, and other types of information not tracked in VetPro. In 2003, the VA and the DoD piloted a common interface to the two systems at several VA/DoD joint ventures. An evaluation determined that the interface, while technically feasible, was not cost effective unless nearly 1,000 providers per year were processed (the Lovell FHCC was expected to have approximately 565 providers) (DoD/VA, 2008, p. 56).
Because it was determined that use of a single credentialing system did not meet VA and DoD organizational requirements, and that using an interface to create interoperability was not cost effective, Lovell FHCC planners proposed and the HEC co-chairs approved using CCQAS for active duty providers and VetPro for civilian providers and establishing a combined credentialing office in which staff would be cross-trained to use both systems. This solution was functional but less efficient than staffing a single system.
The Navy proposed having the active duty providers be privileged by the senior Navy captain acting as the commanding officer (CO) of the NHCGL as well as the deputy director of the Lovell FHCC. The VA director of the FHCC would in turn accept or deny the privileges granted by the deputy director, based on the Inter-facility Credentialing Transfer Brief (ICTB) provided by the Navy. This would have required a change in VA policies, which at the time did not accept ICTBs from other agencies and instead verified all information directly with the primary sources. This approach was seen as inconsistent with the single-chain-of-command concept and the staff integration concept of the medical bylaws. The credentialing EDM recommended and the HEC co-chairs approved the option where the FHCC director is the credentialing and privileging approval authority for DoD and VA providers at the FHCC with input from the deputy director. The deputy director privileges the active duty providers for Navy, not for FHCC, purposes. Granting of Navy privileges by the deputy director acting as the CO of the NHCGL is required to maintain readiness for deployment and to meet the Navy mission requirements.
Scope of Practice for Advanced Practice Nurses and Navy Hospital Corpsmen
One of the Navy’s main concerns about participating in the creation of the Lovell FHCC was ensuring that the consolidated health care system would not degrade military operational readiness. One area of concern was maintenance of the clinical proficiency of active duty nurse practitioners and other advanced practice nurses (APNs), hospital corpsmen, and other allied health professionals. The problem was the difference between VA and DoD policies on privileging health professionals other than physicians, psychologists, podiatrists, optometrists, dentists, and chiropractors.
The VA will privilege APNs, audiologists, pharmacists, and social workers only if their state licenses allow for independent practice. Other VA health professionals—for example, physician’s assistants (PAs), dietitians, marriage and family therapists, occupational therapists, and physical therapists—function under a scope of practice and protocols approved by the medical staff, but they are not a part of the medical staff. In contrast, the Navy privileges APNs, audiologists, pharmacists, and social workers, as well as dietitians, marriage and family therapists, occupational therapists, physical therapists, and speech-language pathologists—and PAs supervised by a physician—and recognizes them as part of the medical staff. The Navy will also grant privileges on a waiver basis even if the provider’s state license does not allow independent practice.
When asked by Congress about obstacles to integration at the Lovell FHCC, the Navy surgeon general identified one of them as VA policies on credentialing of ancillary health workers:
The VA and how they credential is different than what we do in DoD because very few VA providers, perhaps none, but very few VA providers are operationally oriented or deploy. But I have to make sure my providers maintain their operational medical skills so that when I tap them to deploy to an operational area they are full up. So I have to make sure that we have the credentialing issues that are taken care of and that we are going to solve problems that I may have in the Navy. (Robinson, 2009, p. 31)
On this issue, the CTG could not reach consensus and the VA and the Navy agreed to disagree. The VA wanted to use VA privileging policies for all providers at the Lovell FHCC, arguing that a scope of practice arrangement would maintain the clinical skills required for military operational readiness; the Navy wanted to privilege APNs, hospital corpsmen, and other health professionals as permitted by Navy policies. The Navy’s position was that independent practice was needed to develop the critical thinking skills that such health professionals would need when deployed where there are no physicians to consult. The VA’s position was consistent with
the vision of an integrated organization under a single chain of command. Ultimately, agreement was reached on an alternative, approved by the HEC co-chairs, in which active duty health professionals who could not be privileged according to VA policies would be able to practice at the Lovell FHCC with the clinical proficiencies required to maintain Navy privileges included in their scope of practice.23
Another obstacle to maintaining operational readiness was posed by the lack of active duty nurses in the inpatient wards and the ED. These positions had been lost in 2006 when inpatient and emergency care was moved to the NCVAMC. The Navy wants hospital corpsmen to gain experience in inpatient and emergency settings but that requires supervision by an active duty nurse. The workaround was an agreement that hospital corpsmen can be supervised on a daily basis by VA nurses and meet Navy requirements as long as they have an active duty nurse mentor who meets with them regularly.
Corpsmen, especially those with advanced training that qualifies them as independent duty corpsmen (IDCs), carry out certain functions that are reserved to registered nurses and to PAs in the civilian sector. To forestall resistance from VA physicians and nurses to allowing IDCs to perform medical and nursing procedures, the Lovell FHCC provided training to familiarize VA staff with the skill sets of corpsmen and to underscore the need to allow them to practice those skills to develop and maintain the clinical proficiencies they will need when deployed to posts where they are the only medical professionals.
Collection of Other Health Insurance
The VA and the DoD have different processes for billing other insurance companies. Although governed by different laws, in both cases any monies collected must be deposited in the department’s appropriation system. The Lovell FHCC planners hoped to adopt one billing process and deposit the collected funds in the FHCC’s account for budgeting and spending without regard to the source of the funds.
The NCVAMC was using VISN 12’s central billing office, located in Madison, Wisconsin, for billing and collecting from insurance programs. The NHCGL performed its own collections. The options were to (1) have the VISN 12’s central billing office in Madison perform billing and collections for the Lovell FHCC using the VA’s reimbursement rates; (2) have the Lovell FHCC perform the billing and collections using the VA’s reim-
__________________
23 The proficiencies are included in clinical privilege sheets appended to Navy BUMED (Bureau of Medicine and Surgery) Instruction 6320.66E (Appendix H for APNs and Appendix G for other allied health specialists).
bursement rates; or (3) have the FHCC perform the billing and collections using the DoD’s and the VA’s reimbursement rates and processes. Option 1 was preferred because Option 2 would have required the FHCC to hire and train additional staff and Option 3 would have required running two systems, which would be less efficient and more prone to error. Option 1 also bypassed the question about whether legislation would be needed for the DoD to deposit collections in a non-DoD account.
The decision was to adopt Option 1, that is, to have the VA perform all the billing and collections through VISN 12’s billing center in Madison, using VA reimbursement rates but providing a discount for services provided to certain DoD beneficiaries, such as foreign military servicemembers training in the United States. The EA, invoking NDAA 2010, specifies that all monies collected from other insurers by the Lovell FHCC will be deposited in the JMFDF.
Cultural Integration
The Lovell FHCC planners recognized the existence of—and the importance of overcoming—differences in the organizational cultures of the Navy and the VA to achieve success in creating an integrated health care delivery system. There was also recognition that the beneficiary groups and other stakeholders would have concerns about potential negative impacts affecting them with the creation of the FHCC. Some Navy personnel worried that the FHCC would encumber their mission of medically processing recruits and ensuring they were medically fit for deployment, while some veterans worried that they would receive lower priority than active duty servicemembers in obtaining services (Interviews).
The 2005 governance and sitting EDM talked about the need for a communications plan to address the concerns of those affected by the integration effort. The Lovell FHCC leadership’s presentation at the February 2006 VA/DoD joint venture conference began by quoting the eight steps to achieve organizational change from Leading Change, the 1996 book by Harvard Business School professor John P. Kotter (Lovell FHCC, 2006):
- Establishing a sense of urgency,
- Creating the guiding coalition,
- Developing a vision and strategy,
- Communicating the change vision,
- Empowering employees,
- Generating short-term wins,
- Consolidating gains and producing more change, and
- Anchoring new approaches in the culture.
The presentation then reported on how each of the steps was being addressed. For example, a sense of urgency and the creation of a guiding coalition of the Navy and the VA were traced to the impact of the 2001 reports that identified the need for a new Navy facility and the underutilization of the NCVAMC inpatient facility. The vision was total integration, and the strategy for promoting the adaptation of the two organizational cultures to each other by 2010 was the three-phase approach. Communicating the vision included the establishment of a marketing task group. The membership of NHGL and NCVAMC personnel on the national task groups was the example of empowering employees. Short-term wins included cost avoidance from shifting inpatient mental health (Phase 1) and inpatient medicine, surgery, and pediatrics (Phase 2) to the NCVAMC rather than building and maintaining a new Navy hospital. Other short-term wins were the Navy’s use of NCVAMC space for its new blood donor processing center (instead of renovating the building it had been using on the Navy base) and the winning of six JIF awards to expand services. The example of consolidating gains and producing more change was the effort to address cultural differences.
As mentioned earlier, a communications task group was added to the six original task groups in 2007 and renamed the communications and organization culture task group in 2008. The group’s assignment was to conduct an assessment of the local, regional, and national stakeholders, including the staff and beneficiaries of the NHGL and the NCVAMC, and then to develop a communications plan and marketing strategy to inform each audience about the benefits of an integrated FHCC. The initial steps included a quarterly newsletter, an FHCC website, and all-employee meetings. The FHCC’s logo and motto—“Proud to Partner: Excellence in Federal Health Care!”—were developed early in the process (Lovell FHCC, 2006).
The VA’s National Center for Organizational Development (NCOD) and the Naval Postgraduate School were engaged to assess Phase 2, survey employee attitudes, conduct focus groups with patients and employees, identify barriers to collaboration, and hold offsite retreats of VA and DoD personnel (Lovell FHCC, 2009). The NCOD surveyed VA and Navy staff in May 2006, September 2007, and February 2008. The goal of these assessments was “to identify what is currently working well and what opportunities currently exist to enhance integration efforts for all staff” (Lovell FHCC, 2010a).
There was a considerable effort by the human resources task group to keep employees, especially the Navy civilians who were going to be transferred to the VA, informed about their status. Fourteen hundred civilian employees of the NHCGL and the NCVAMC received letters at the end of August 2009 stating their job titles and locations; the remaining 600 civil-
ians received letters confirming that they had jobs at the Lovell FHCC, although its location had not been determined. VA and DoD human resources specialists were available at the NHCGL the week following the notification letters to answer questions, and several frequently asked questions documents were issued that provided answers to anticipated concerns. There were at least three sets of town hall meetings in 2009 and 2010.
The joint strategic planning conferences held periodically to plan the Lovell FHCC explicitly considered the cultural aspects of merging programs and departments. There were conscious efforts to invite key stakeholders in the VA, the Navy, and Congress to tour the nascent FHCC resulting from the first two phases of the integration process. The HEC received periodic briefings on cultural blending initiatives. The Navy surgeon general and the VA secretary testified before Congress on the challenges of merging the two organizations (Robinson, 2009; Shinseki, 2009).
The first Stakeholder Advisory Committee (SAC) meeting was held in July 2010. The SAC members included community representatives and representatives of veterans service organizations, the Navy line commands and the Navy ombudsman at the NSGL, the TRICARE regional office and managed care support contractors, VISN 12 representatives, the Rosalind Franklin University of Medicine and Science, and a congressional liaison. In August 2010, a final round of leadership meetings and mini-retreats of VA and DoD staff was held to keep employees informed and discuss cultural issues.
Despite the efforts to forge identification of the employees at the NHCGL and the NCVAMC with the Lovell FHCC rather than with the Navy or the VA, not everyone was happy with the change. Not all Navy personnel, including those transferred to the VA personnel system, thought that the FHCC was a good idea. From their point of view, the fast-paced mission of preparing recruits for deployment has not changed, but achieving it has become more complicated and time-consuming. The main problem for the branch clinics on the Navy base is the need to manually obtain and enter patient information into AHLTA (the DoD EHR system) from VistA (the VA EHR system) when recruits, students, and Navy staff receive emergency, inpatient, or specialty medical services on the west campus. In addition, IT support, laboratory services, and supply, which have been centralized, are seen as less responsive than when they were part of the NHCGL.
Legislative Process
The six task groups formed in 2005 were instructed to identify any laws, regulations, policies, and procedures that would have to be revised or dropped to enable the VA and the Navy to integrate their health care centers
in North Chicago. The approach was to minimize legislative changes and rely as much as possible on existing law, specifically, 38 U.S.C. § 8111, “Sharing of Department of Veterans Affairs and Department of Defense Health Care Resources.”
Certainly there was room for optimism that Congress would revise the statutes where needed. Congress had repeatedly encouraged greater cooperation in delivering health care between the DoD and the VA in laws, conference committee reports on VA and DoD bills, and by requesting annual and ad hoc reports on the state of VA/DoD sharing. The NDAA 200224 had mandated a series of demonstrations of mechanisms to facilitate VA/DoD sharing and created the JIF award program. The appropriations committees had approved $13 million in 2004 to renovate the NCVAMC surgical suite and ED, and $135 million in 2007 to construct the ACC and related facilities. In 2008, they had allowed the VA and the DoD to funnel an additional $100 million through the JIF program to develop software to enable the two EHR systems to work together at the Lovell FHCC.
The Lovell FHCC planners gradually identified the minimum set of legislative changes that would be required to implement the FHCC. The lack of authority to transfer Navy civilians to the VA was evident early on. It also became evident that the governance model in which the FHCC reported to a DoD/VA committee under the HEC would require legislation to implement. In that case, the departments changed the model in 2007 so that the FHCC director reported to the VA, because legislation to create what in effect would be a new federal agency did not seem likely to pass. There was no acceptable way for the Navy to transfer the ACC to the VA under existing legislation (discussed above). The planners hoped to avoid the need for legislation to create a joint fund for the FHCC by using the JIF mechanism, which was resisted by VA and DoD comptrollers and by the congressional appropriations committees, so legislation establishing a new Treasury account was required. Finally, legislation would be needed to designate the FHCC as an MTF to enable it to provide health care to DoD beneficiaries without charging deductibles and copayments required if they used non-MTF facilities.
In 2008, the congressional affairs offices of the VA and the DoD worked with members of the Illinois delegation to draft language permitting the transfer of personnel from the Navy to the VA, allowing the transfer of ownership of the ACC from the Navy to the VA, designating the Lovell FHCC as an MTF, and establishing a JIF-like mechanism to allow the department to fund the FHCC jointly. In September 2008, Senator Dick Durbin introduced an amendment to the NDAA for FY 2009 (NDAA
__________________
24 NDAA for Fiscal Year 2002, Public Law 107-107 (December 28, 2001). http://www.dod.gov/dodgc/olc/docs/2002NDAA.pdf (accessed August 6, 2012).
200925), but the process of passing the bill was too far along to include the FHCC provisions. Instead, when the NDAA 2009 was passed by Congress, it included a section on “Guidelines for Combined Medical Facilities of the Department of Defense and the Department of Veterans Affairs” that required the DoD and VA secretaries to execute a binding operational agreement on nine areas:
- Governance
- Patient priority categories
- Budgeting
- Staffing and training
- Construction
- Physical plant management
- Contingency planning
- Quality assurance
- Information technology
Although the NDAA 2009 allowed the DoD and the VA to negotiate an operational agreement for a combined facility, it did not explicitly confer additional legal authority regarding beneficiary benefits, ACC ownership, employee transfers, or a joint funding mechanism. In June 2009, Senators Durbin and Daniel Akaka reintroduced legislation in the new Congress with the four specific authorities needed for the Lovell FHCC to function with hopes that it would pass as part of a DoD supplemental appropriations bill. The fast-track initiative failed and the bill became part of the regular NDAA process. One area that required considerable negotiation was the transfer of personnel. The draft language was designed to “protect” the Navy civilians moving into the VA personnel system by specifying that they would not lose pay or seniority or be subject to a probationary period if they had already completed this as a DoD employee. Although the departments agreed on the language, the union representing Navy civilians at Great Lakes—the American Federation of Government Employees—opposed the language because the Navy personnel would lose the right under the VA’s Title 38 personnel system to appeal to the Merit Systems Appeal Board (Robinson, 2009, p. 98). The Durbin-Akaka bill extended collective bargaining rights under Title 5 to transferred employees for 2 years, at which time the VA secretary, in consultation with the DoD and Navy secretaries, would determine whether the appeal rights should be terminated, revised, or retained.
__________________
25 NDAA, S. 3001, January 3, 2008. http://www.gpo.gov/fdsys/pkg/BILLS-110s3001enr/pdf/BILLS-110s3001enr.pdf (accessed August 6, 2012).
The DoD was also concerned about using the JIF program as the funding mechanism, because it wanted to control how much and when the funding would be spent (the JIF legislation says each department has to contribute “at least $15 million a year” which becomes “no year” money—that is, there is no limit on what a department can contribute and it does not have to be spent the same year) (Robinson, 2009). The departments had already stretched the intent of the JIF program in using it to provide the $100 million for interoperable IT solutions for the Lovell FHCC. The Durbin-Akaka bill provided for a Treasury fund under the VA to which the DoD and the VA could transfer funds for the FHCC, and it stipulated that the funds would be available for 1 FY, except for 2 percent, which could be carried over into a second year.
After a fair amount of behind-the-scenes negotiating in the executive branch, and then between the House and the Senate, which had passed different versions of the NDAA 2010, the Department of Defense-Department of Veterans Affairs Medical Facility Demonstration Project was passed as part of the NDAA 2010 and signed into law on October 28, 2009. The House had not included a Lovell FHCC section in its bill but acceded to the Senate language with certain modifications and additions. The final bill did not refer to the Captain James A. Lovell FHCC because the name had not been approved through customary procedures. The final version directed the DoD and VA secretaries to submit a copy of the EA required by the NDAA 2009 to Congress at least 7 days before finalizing it. It also directed the GAO to review and assess progress annually. The legislation renamed the Treasury fund the “Joint Department of Defense-Department of Veterans Affairs Medical Facility Demonstration Fund,” and said that DoD and VA funds for the joint fund had to be specifically authorized and appropriated for that purpose. It specified that the first priority for care would be given to active duty servicemembers. The department secretaries were required to submit a final report to Congress after 5 years, describing and assessing the demonstration and recommending whether or not to continue it.
In the meantime, the Lovell FHCC planners began to draft an EA covering the nine areas specified in the NDAA 2009. The EA draft went through nearly 70 iterations while it was reviewed up the two department chains before being signed by the three secretaries (VA, DoD, and Navy) on April 23, 2010. At the same time, the Lovell FHCC began drafting an executive sharing agreement (ESA) to prepare for the possibility that the joint Treasury fund might not be ready, or the appropriations for it passed, by October 1, 2010. In fact, the FHCC was operated under the ESA for the first 9 months because the defense appropriations bill for FY 2011 was not passed and the DoD had to operate under a CR. This meant that the
requirement in the NDAA 2010 that funds be specifically appropriated for the FHCC could not be fulfilled.
SUMMARY OF IMPLEMENTATION CHALLENGES
The experience of the planning and implementation of the Lovell FHCC provides many examples of the issues that arise—and how they can resolved—when the VA and the DoD decide to serve their respective beneficiary populations by combining their medical centers. Some of the significant issues that had to be addressed to implement the Lovell FHCC are listed in Table 3-2. This history is ripe for the evaluation of lessons learned that should be considered in designing any future FHCCs. Some of the solutions developed by the Lovell FHCC might be adopted by future FHCCs. Many of them are compromises or time-consuming workarounds necessitated by differing policies and procedures of the VA, the DoD, and
| Implementation | |
| Issue | Discussion |
| Joint governance | The desire to have a joint governance structure must be reconciled with the requirement that a federal health care center (FHCC) be assigned to, and the director/chief executive officer to come from, one department or the other. The requirement that the ranking active duty military officer, if he or she is not the director, exercise the Uniform Code of Military Justice and other command responsibilities is another irreducible complication in achieving a single chain of command. |
| Beneficiary benefits and copayments | Although the intent at the Lovell FHCC was to treat everyone equally, this was not totally achieved. Because the Navy’s boot camp for enlisted recruits is at Naval Station Great Lakes, there was an agreement, which was specified in the 2010 National Defense Authorization Act (NDAA), that active duty servicemembers are to receive first priority in scheduling appointments and receiving services. This is most evident at the west campus pharmacy, where active duty beneficiaries go to the head of the line, making some veterans unhappy (see Chapter 4). The FHCC planners also wanted Department of Defense (DoD) beneficiaries to be exempt from cost sharing, as they are at military treatment facilities (MTFs). Congress allowed the FHCC to be an MTF for eligibility purposes, but only during the 5-year demonstration, and the DoD secretary had to issue a ruling that cost sharing would not be required as part of the 5-year demonstration. A more permanent arrangement will have to be worked out if FHCCs become standard programs rather than demonstration projects. |
| Implementation | |
| Issue | Discussion |
| Joint funding mechanism and reconciliation model | The solution in North Chicago was to create a Department of the Treasury (Treasury) fund under the Department of Veterans Affairs (VA) where the departments could pool their funds and to develop a reconciliation process based on workload measures to apportion responsibility between the Navy and the VA for funding after the fact. The reconciliation methodology could be a model for future FHCCs, but the VA decision support system does not routinely track industry standard workload measures (e.g., relative value units and relative weighted products) that, therefore, have to be determined manually as a workaround. Also, the Treasury fund is only authorized for the 5-year demonstration in North Chicago and would have to be extended by Congress to additional FHCC sites. In addition, the reconciliation methodology has not yet been put to the test; the FHCC funding is based on historical levels during the first 3 years. |
| Employee status | It is desirable for several reasons to have all employees in the same personnel system. In a VA/DoD FHCC, active duty personnel will always be in a separate personnel system. However, civilians can be put under one department or the other, if Congress approves. Nonetheless, differences regarding job descriptions, compensation, and collective bargaining rights must be resolved. At this time, the authority to transfer Navy civilians to the VA is only granted for the 5-year demonstration in North Chicago and would have to be extended to any additional sites by Congress. |
| Joint workforce | The VA and the military department (the Navy in the case of the Lovell FHCC) must agree on staffing levels and a mechanism for revising them during the year in response to shifts in workload. The situation is complicated at the Lovell FHCC because the Navy personnel rotate out after 2 or 3 years and are often deployed once or twice during their rotation at Great Lakes. |
| Joint electronic health record (EHR) system | Although joint use of the DoD and the VA EHR systems was considered to be a prerequisite for seamless health care delivery at the Lovell FHCC, attempts to develop a minimum set of software capabilities (e.g., single patient registration, single sign-on, and single order entry and results retrieval) by the opening of the Lovell FHCC were not successful. In fact, the lack of integration of the DoD and the VA EHR systems has caused time-consuming workarounds to ensure that patient information is the same and current in both of them and integrated health care delivery has been inhibited. The Lovell FHCC experience was a major factor in the decision of the DoD and the VA secretaries to cancel updates of their legacy EHR systems and jointly develop a single EHR system for use by both departments. Having a single EHR system designed to meet the needs of both departments would greatly facilitate integrated health care delivery. |
| Implementation | |
| Issue | Discussion |
| Information technology (IT) network trust, security, and computer system access | Ideally, there would be network trust so that users of one computer system would be automatically allowed access to the other. The VA “dot.gov” system does not meet the DoD’s “dot.mil” security standards and it would be very costly to bring it up to DoD standards. The Navy relented on requiring a secret-level security clearance to access the DoD EHR system when the VA agreed to have all VA personnel undergo a more intensive security investigation. The departments also could not reach agreement on using a single access card and more than 1,000 VA employees had to be issued special access cards, a process that could not be completed by October 1, 2010. |
| Credentialing and privileging | It was not cost effective to operate a common interface for the VA and DoD credentialing verification systems at the Lovell FHCC, even though both are based on the same Joint Commission standards. As at the Lovell FHCC, future FHCCs would have to staff and operate both systems unless the departments agreed to develop a single, joint system similar to what the Lovell FHCC decided to do in the case of the incompatible EHR systems. Although there was agreement that the FHCC director, a career VA employee, would be the final privileging authority, the deputy director, as the ranking active duty officer, must also privilege active duty clinicians for certain military purposes. |
| Privileging and supervision of active duty advanced practice nurses (APNs), hospital corpsmen, and independent duty hospital corpsmen (IDCs) | The DoD has more permissive privileging rules than the VA because it deploys registered nurses and hospital corpsmen with advanced training to assignments in locations where they must perform independently of physicians. The solution at the Lovell FHCC was for the VA to agree to a scope of practice that included the specific functions that APNs and IDCs are expected by the DoD to perform, which are broader than the VA’s usual scope of practice for these positions. Supervision of corpsmen is also an issue. The Navy requires them to be supervised by an active duty nurse, which inhibits staff integration. The workaround at the FHCC was to allow corpsmen working on the west campus to be supervised by civilian nurses in their daily work as long as there is an active duty nurse mentor. |
| Procurement | There was agreement that the Lovell FHCC would use the VA procurement system, but experience has shown that it would be more cost effective if the Navy facilities command could be used for certain base operations. It is also more cost effective to use personal services contracts (PSCs) for staffing the east campus branch clinics, given that the workload there varies, but the VA does not have authority to use them. The FHCC would like the VA to obtain authority from Congress to use the PSCs. Meanwhile, despite the agreement to use the VA logistics system, the Navy logistics command is administering the PSCs on the east campus. |
| Implementation | |
| Issue | Discussion |
| Pharmacy formulary | It might be more efficient to have one formulary, but the decision for the Lovell FHCC was to maintain two of them. If the two departments could agree on a common formulary, it also might lead to lower prices because of their combined demand. |
| Mail order pharmacy | The Lovell FHCC saved space in the ambulatory care center by deciding to rely on the VA’s Consolidated Mail Order Pharmacy (CMOP) for prescription refills, but the DoD does not want to allow DoD beneficiaries to use this program. The resulting backup at the FHCC pharmacy has been a major consumer dissatisfaction issue. This question—whether or not to use the CMOP for DoD beneficiaries—should be settled before designing the pharmacy space in future FHCCs. |
| Military operational readiness | The issue is finding a way to document the current individual medical readiness of active duty servicemembers who obtain emergency, inpatient, or specialty services on the east campus. Because of the lack of interoperability between the VA and the DoD EHR systems, entries in the VA EHR system used at these west campus locations are not simultaneously recorded automatically in the DoD EHR system. This problem is being addressed by the development of the integrated EHR system, the iEHR. |
| Law enforcement and security | The Lovell FHCC expected to integrate the Navy and the VA police forces, but efforts have been stymied by the Posse Comitatus Act, which generally prohibits active duty servicemembers from arresting civilians. In August 2012, permission was granted for the Navy masters-at-arms to attend the 8-week VA Police Academy in Little Rock, Arkansas, after which they will be able to carry lethal and nonlethal weapons as they participate in patrolling the west campus of the FHCC. |
the affected military service (in this case, the Navy) that could be addressed more effectively at the enterprise level. Others may be unique to North Chicago, for example, the priority given to active duty servicemembers because of the demands of the recruit training mission.
Arthur, D. 2006. Written statement of Vice Admiral Donald C. Arthur, Surgeon General of the Navy, before the Subcommittee on Military Quality of Life and Veterans Affairs of the House Appropriations Committee (also before Senate Appropriations Subcommittee on Defense on May 3, 2006). http://www.med.navy.mil/bumed/comms/Pages/CongressionalTestimony.aspx (accessed August 7, 2012).
Bean, M. L. 2009. Speech of Hon. Melissa L. Bean of Illinois in the House of Representatives, June 24. Congressional Record. Pp. E1620–E1621.
Brewin, B. 2007. Navy eyes front-end system for joint health facility. GovernmentHealthIT, February 26. http://www.govhealthit.com/news/navy-eyes-front-end-system-joint-healthfacility-0 (accessed October 14, 2012).
Brewin, B. 2012. Defense and VA tap vendor to save clinicians from multiple log-ons. Next Gov.com, May 21. http://www.nextgov.com/health/2012/05/defense-and-va-tap-vendorsave-clinicians-multiple-log-ons/55832/?oref=ng-dropdown (accessed August 7, 2012).
Chu, D. 2003. Testimony of the under secretary of defense for personnel and readiness at the House Committee on Veterans’ Affairs hearing to discuss the report of the President’s Task Force to Improve Health Care Delivery for Our Nation’s Veterans. June 17. Washington, DC: U.S. Government Printing Office. http://democrats.veterans.house.gov/hearings/schedule108/jun03/6-3-03/6-3_6-17-03.pdf (accessed September 17, 2012).
DoD (Department of Defense). 2010. TRICARE copayment waiver at Captain James A. Lovell Federal Health Care Center Demonstration Project. Federal Register, September 27, pp. 59237-59238. http://edocket.access.gpo.gov/2010/pdf/2010-24092.pdf (accessed August 7, 2012).
DoD. 2011. DoD-VA integrated electronic health record pharmacy solution: Request for information. Solicitation Number: TMA-0007-iEHR. https://www.fbo.gov/utils/view?id=3af028f1d3bd70860228f8256bca9ef0 (accessed August 7, 2012).
DoD/VA (Department of Veterans Affairs). 2008. Fiscal Year 2003 National Defense Authorization Act Department of Defense and Department of Veterans Affairs Demonstration Projects: Final report. July. http://www.tricare.mil/DVPCO/downloads/DSS%20Consolidated%20Final%20Report%20v%202.31%20formatted.doc (accessed August 7, 2012).
DoD/VA. 2009. DOD/VA Joint Incentive Fund guide. November. vadodrs.amedd.army.mil/jif/JIFGuideFinal.doc (accessed August 21, 2012).
DoD/VA. 2010. Executive agreement for the Department of Defense-Department of Veterans Affairs Medical Facility Demonstration Project Federal Health Care Center. April 23. http://tricare.mil/tma/congressionalinformation/downloads/2010310/111-288%20Section%201701(d)(1)%20FHCC%20EA.pdf (accessed September 6, 2012).
DoD/VA. 2011. Department of Defense and Department of Veterans Affairs Interagency Program Office (IPO) charter. http://www.tricare.mil/tma/ipo/documents/IPO.pdf (accessed August 15, 2012).
Durbin, R. 2009. Lovell Health Center one step closer to completion. Press Release, June 23. http://durbin.senate.gov/public/index.cfm/pressreleases?ID=f993baba-956b-4ba1-9d1b-e3e4382a70d7 (accessed August 7, 2012).
Ellis, K. 2005. Navy partners with North Chicago Veterans Affairs Medical Center. America’s Navy, Story Number NNS 051024-09. http://www.navy.mil/submit/display.asp?story_id=20692 (accessed August 7, 2012).
Filippi, D. 2011. Testimony of Debra M. Filippi, former Director, DoD/VA Interagency Program Office, before the House Veterans Affairs Committee Hearing on H.R. 2383, H.R. 2243, H.R. 2388 and H.R. 2470. http://veterans.house.gov/prepared-statement/prepared-statement-debra-m-filippi-former-director-us-department-defenseus (accessed August 15, 2012).
GAO (U.S. Government Accountability Office). 2004. VA and DoD health care: Resource sharing at selected sites. GAO-04-792. Washington, DC: GAO. http://www.gao.gov/new.items/d04792.pdf (accessed August 7, 2012).
GAO. 2005. Mail order pharmacies: DOD’s use of VA’s mail pharmacy could produce savings and other benefits. GAO-05-555. Washington, DC: GAO. http://www.gao.gov/assets/250/246841.pdf (accessed August 7, 2012).
GAO. 2011. VA and DoD health care: First federal health care center established, but implementation concerns need to be addressed. GAO-11-570. Washington, DC: GAO. http://www.gao.gov/new.items/d11570.pdf (accessed August 7, 2012).
GAO. 2012a. Background investigation: Office of Personnel Management needs to improve transparency of its pricing and seek cost savings. GAO-12-197. Washington, DC: GAO. http://www.gao.gov/assets/590/588947.pdf (accessed August 7, 2012).
GAO. 2012b. Security clearances: Agencies need clearly defined policy for determining civilian position requirements. GAO-12-800. Washington, DC: GAO. http://gao.gov/assets/600/592371.pdf (accessed August 7, 2012).
Gibbard, M. D. 2005. Navy, VA do hospital deal: Sailors, vets to get care under 1 roof. Chicago Tribune, October 18. http://articles.chicagotribune.com/2005-10-18/news/0510180212_1_va-hospital-va-deputy-secretary-va-facility (accessed August 7, 2012).
Harnly, M. J. 2005. A qualitative analysis of resource sharing agreements between Naval Hospital Great Lakes and North Chicago Veterans Affairs Medical Center: The iron triangle theory of healthcare integration. Master’s Thesis, Army-Baylor Program in Healthcare Administration, Fort Sam Houston, TX. http://www.dtic.mil/dtic/tr/fulltext/u2/a443921.pdf (accessed August 7, 2012).
Hassan, T., R. Kline, and M. A. Cardinali. 2008. Federal Health Care Center Great Lakes. Presentation at the 2008 VA/DoD Joint Venture Conference, Honolulu, Hawaii, March 5. http://www.tricare.mil/DVPCO/Hawaii/2008%20JV%20Conf%20-%20FHCC%20Great%20Lakes.ppt (accessed August 7, 2012).
IPO (Interagency Program Office). 2011. DoD/VA Interagency Program Office annual report to Congress 2010. http://www.govexec.com/pdfs/033111bb1.pdf (accessed August 7, 2012).
IPO. 2012. DoD/VA Interagency Program Office annual report to Congress 2011. http://tricare.mil/tma/congressionalinformation/downloads/FullyInteroperableElectronicPersonalHealthInformationDoDDVA.pdf (accessed July 31, 2012).
Kuczka, S. 2003. VA hospital gets Navy patients; Great Lakes sends 6 to North Chicago. Chicago Tribune, November 8, 2003. http://articles.chicagotribune.com/2003-11-08/news/0311080208_1_va-facility-va-campus-navy-patients (accessed October 5, 2012).
Lovell FHCC (Captain James A. Lovell Federal Health Care Center). 2006. The joint initiative between the North Chicago VAMC and Naval Hospital Great Lakes. Presentation at the 2006 Military Health System Conference, January 31. www.tricare.mil/dvpco/bummed/NHGL%20NCVAMC%20BRIEF.ppt (accessed August 24, 2012).
Lovell FHCC. 2009. Captain James A. Lovell Federal Health Care Center. Presentation by Patrick Sullivan and Captain Thomas E. McGue at the 2009 VA/DoD Joint Venture Conference, June 3. http://www.tricare.mil/DVPCO/downloads/20090625/Breakout4cJVUpdateGreatLakesNorthChicago.ppt (accessed October 5, 2012).
Lovell FHCC. 2010a. Captain James A. Lovell Federal Health Care Center concept of operations. October 1. Provided to the Committee on Evaluation of the Lovell Federal Health Care Center Merger by the Lovell FHCC.
Lovell FHCC. 2010b. FY 2011 business plan, April 5. Provided to the IOM Committee on Evaluation of the Lovell Federal Health Care Center Merger by the Lovell FHCC.
Maldonado, F. A., and D. M. Poulin. 2012. IT news from James A. Lovell Federal Health Care Center. Presentation at the 2012 annual meeting of the Healthcare Information and Management Systems Society, New Orleans, Louisiana, February 23. http://69.59.162.218/HIMSS2012/Venetian%20Sands%20Expo%20Center/2.23.12_Thu/Marco%20Polo%20803/Thu_1300/157-11_Donna_Poulin_Marco%20Polo%20803/157MaldonadoPoulin.pdf (accessed August 7, 2012).
Opsut, R. 2011. Reconciling financial liability for the North Chicago Federal Health Care Center. Presentation by Dr. Robert Opsut, TRICARE Management Agency, DoD, to the IOM Committee on Evaluation of the Lovell Federal Health Care Center Merger, Washington, DC, February 25.
Poulin, D., C. Foster, and J. Nelson. 2012. Lovell Federal Health Care Center lessons learned. Presentation by LCDR Donna Poulin, LCDR Chuck Foster, and Mr. Joseph Nelson at the Tri-Service Medical Information Management Symposium 2012. http://cdn.govexec.com/media/gbc/docs/pdfs_edit/052112bb1.pdf (accessed August 7, 2012).
Robinson, A. M, Jr. 2009. Statement of Vice Admiral Adam M. Robinson, Jr., Surgeon General of the Navy, United States Navy. Transcript of Hearing on the Defense Health Program appropriations for FY 2010 held by the Senate Appropriations Defense Subcommittee, March 18. Washington, DC: U.S. Government Printing Office. http://www.gpo.gov/fdsys/pkg/CHRG-111shrg48290/pdf/CHRG-111shrg48290.pdf (accessed August 7, 2012).
Shinseki, E. 2009. Statement of Secretary of Veterans Affairs Eric K. Shinseki at Update on the State of the U.S. Department of Veterans Affairs. Hearing before the Committee on Veterans’ Affairs, U.S. House of Representatives, October 14. http://www.gpo.gov/fdsys/pkg/CHRG-111hhrg53434/html/CHRG-111hhrg53434.htm (accessed September 7, 2012).
Susnjara, B. 2003. VA hospital’s future gets a boost. Daily Herald, November 11. http://www.jsosolutions.com/archive/kirkforcongress/inthenews_DailyHerald111103.htm (accessed September 7, 2012).
U.S. House of Representatives. 2009. Examining the progress of electronic health record interoperability between the U.S. Department of Veterans Affairs and U.S. Department of Defense. Hearing before the Subcommittee on Oversight and Investigations of the Committee on Veterans’ Affairs, July 14. Washington, DC: U.S. Government Printing Office. http://www.gpo.gov/fdsys/pkg/CHRG-111hhrg51872/pdf/CHRG-111hhrg51872.pdf (accessed August 7, 2012).
U.S. House of Representatives. 2010. U.S. Department of Veterans Affairs Office of Inspector General and Office of Information Technology budget requests for fiscal year 2011. Hearing before the Subcommittee on Oversight and Investigations, Committee on Veterans’ Affairs, February 23. Washington, DC: U.S. Government Printing Office. http://frwebgate.access.gpo.gov/cgi-bin/getdoc.cgi?dbname=111_house_hearings&docid=f:55228.pdf (accessed August 7, 2012).
U.S. Navy. 2011. Manual of Navy enlisted manpower and personnel classifications and occupational standards, Volume II, Navy enlisted classifications (NECs). January. http://www.public.navy.mil/bupers-npc/enlisted/detailing/personnelreadiness/Documents/NECVol2.pdf (accessed August 7, 2012).
U.S. Senate. 2005. Military construction and Veterans Affairs, and related agencies appropriations for fiscal year 2006. Hearing before the Subcommittee on Military Construction and Veterans Affairs, and Related Agencies, Committee on Appropriations, March 8. Washington, DC: U.S. Government Printing Office. http://frwebgate.access.gpo.gov/cgibin/getdoc.cgi?dbname=109_senate_hearings&docid=f:99875.wais (accessed August 7, 2012).
VA (Department of Veterans Affairs). 2002. VA and DoD agree on health care in North Chicago. VA press release, October 18. http://www.va.gov/opa/pressrel/pressrelease.cfm?id=523 (accessed September 4, 2012).
VA. 2004. Security and law enforcement. VA handbook 0730/1. http://www1.va.gov/vapubs/viewPublication.asp?Pub_ID=96 (accessed August 7, 2012).
VA. 2010a. FY 2011 congressional budget submission, Vol. II, medical programs & information technology programs. http://www.va.gov/budget/docs/summary/archive/FY-2011_VA-BudgetSubmission.zip (accessed August 7, 2012).
VA. 2010b. Security and law enforcement. VA handbook 0730/2. http://www.va.gov/vapubs/viewPublication.asp?Pub_ID=488&FType=2 (accessed August 7, 2012).
VA/DoD. 2006a. VA/DoD Joint Executive Council FY 2005 annual report. http://www.tricare.mil/DVPCO/downloads/VADoD2005.pdf (accessed August 7, 2012).
VA/DoD. 2006b. VA/DoD Health Executive Council executive decision memorandum, Second call for Joint Incentive Fund (JIF) projects. http://www.tricare.mil/DVPCO/downloads/JIF-Projects-2006-2.pdf (accessed August 7, 2012).
VA/DoD. 2008a. VA/DoD Joint Executive Council FY 2007 annual report. http://www.tricare.mil/DVPCO/downloads/VA%20DoD%202007%20Annual%20Report%20FINAL%203-14-08.pdf (accessed August 7, 2012).
VA/DoD. 2008b. VA/DoD Joint Executive Council FY 2008 annual report. http://www.tricare.mil/DVPCO/downloads/VA%20DoD%20Joint%20Executive%20Council%20Annual%20Report.pdf (accessed August 7, 2012).
VA/DoD. 2009. VA/DoD Joint Executive Council FY 2009 annual report. http://prhome.defense.gov/docs/2009%20VA%20DoD%20Joint%20Executive%20Council%20Annual%20Report%20and%20Joint%20Strategic%20Plan.pdf (accessed August 7, 2012).
VA/DoD. 2011. VA/DoD Joint Executive Council FY 2010 annual report. http://www.tricare.mil/DVPCO/downloads/2010%20JEC%20Annual%20Report%20to%20Congress%20(signed).pdf (accessed August 7, 2012).
VA OIG (VA Office of the Inspector General). 2010. Audit of the FLITE Strategic Asset Management Pilot Project. #09-03861-238, September 14. http://www.va.gov/oig/52/reports/2010/VAOIG-09-03861-238.pdf (accessed August 15, 2012).
























































