White House. 1961. Executive Order 10914—Providing for an expanded program of food distribution to needy families. Federal Register 26:639.
Wilde, P. E. 2007. Measuring the effect of food stamps on food insecurity and hunger: Research and policy considerations. Journal of Nutrition 137(2):307-310.
Wolkwitz, K. 2007. Characteristics of food stamp households: Fiscal year 2006. Submitted by Mathematica Policy Research, Inc. to U.S. Department of Agriculture, Food and Nutrition Service, Alexandria, VA. http://www.fns.usda.gov/ora/menu/Published/snap/FILES/Participation/2006Characteristics.pdf (accessed May 24, 2012).
Yen, S. T., M. Andrews, Z. Chen, and D. B. Eastwood. 2008. Food Stamp Program participation and food insecurity: An instrumental variables approach. American Journal of Agricultural Economics 90(1):117-132.
Ziliak, J. P. 2008. Effective tax rates and guarantees in the Food Stamp Program. University of Kentucky. http://gatton.uky.edu/Faculty/ziliak/ERS_FSP_Rates&Guarantees_042308.pdf (accessed June 5, 2012).
Ziliak, J. P. 2011. Recent developments in antipoverty policies in the United States. University of Kentucky Center for Poverty Research Discussion Paper Series, DP2011-05. http://www.ukcpr.org/Publications/DP2011-05.pdf (accessed May 24, 2012).
Ziliak, J. P., C. Gundersen, and D. N. Figilio. 2003. Food Stamp caseloads over the business cycle. Southern Economic Journal 69(4):903-919.
3
Food Security and Access to a
Healthy Diet in Low-Income Populations
To set the stage for its examination of evidence to support the feasibility of defining the adequacy of Supplemental Nutrition Assistance Program (SNAP) allotments, the committee first reviewed evidence on relationships between participation in SNAP and the potential for participants to reach the goals of improved food security and access to a healthy diet. This evidence on program outcomes underpins the committee’s examination of individual, household, environmental, and program-related factors that serve as components of a science-driven definition of the adequacy of SNAP allotments. The chapter first examines trends in food production, availability, and consumption at the population level. Although food availability data do not account for spoilage and other losses and do not provide a direct measure of consumption, they do serve as an indicator of food consumption trends over time. Next, the chapter examines food purchasing patterns and dietary intake among low-income households and SNAP participants. The chapter then describes evidence on access to a healthy diet and food insecurity among low-income SNAP-eligible as well as SNAP-participating households, including evidence on the impact of SNAP benefits. Next is a discussion of the data and analytical challenges faced in assessing the adequacy of SNAP allotments. The final section presents a summary of findings and conclusions.
FOOD PRODUCTION, AVAILABILITY, AND
CONSUMPTION AT THE POPULATION LEVEL
Changes in food production over the course of the last century have led to an increase in total calories available per capita, as well as a change in
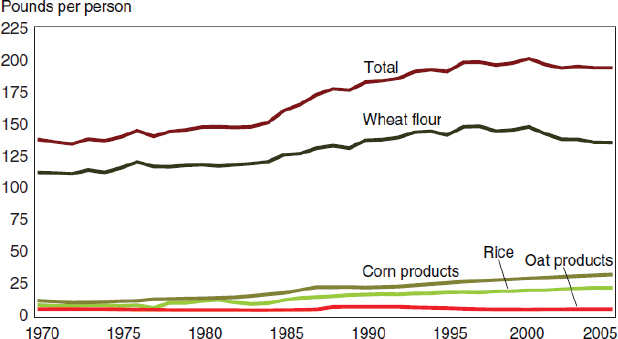
FIGURE 3-1 Per capita total grain availability, 1970-2005.
NOTE: Data for 2005 based on a 2,000-calorie diet.
SOURCE: Wells and Buzby, 2008. USDA, ERS Food Availability (per capita) Data System.
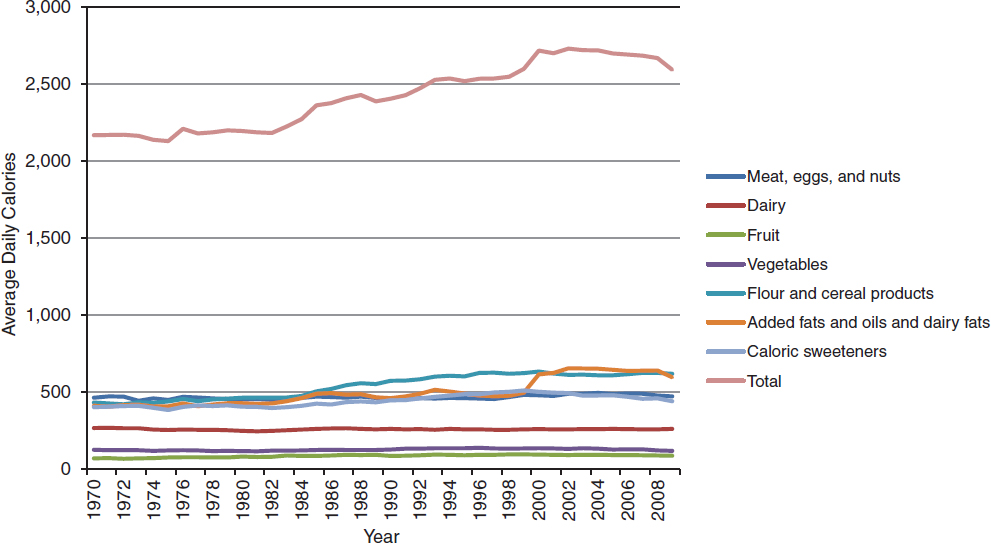
FIGURE 3-2 Increase in average daily per capita energy (calorie) availability in the United States between 1970 and 2009.
SOURCE: Data from ERS, 2012. ERS Food Availability (per capita) Data System, adjusted for spoilage and other waste.
the composition of foods available. In particular, over the past four decades, production and availability have increased for grains more than for other types of foods. Grains of all types—including wheat, corn, rice, and oats—have become more readily available in the food supply. Total grain availability per person increased from 137 pounds in 1970 to 192 pounds in 2005 (Wells and Buzby, 2008; see Figure 3-1).
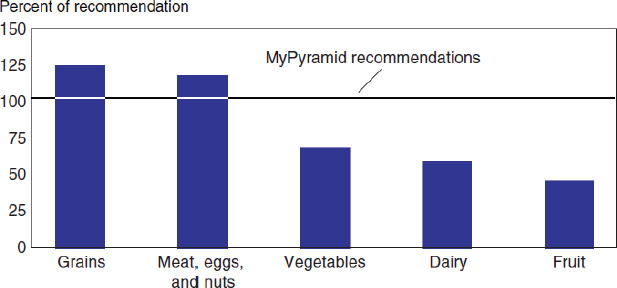
According to a 2008 U.S. Department of Agriculture (USDA) report on the major trends in food availability,1 not only did the availability of grains increase by 41 percent from 1970 to 2005, but the availability of all major food groups increased as well—fruits and vegetables (by 19 percent); meat, eggs, and nuts (8 percent); and milk/dairy products (6 percent). In addition, availability increased for fats and oils (62 percent) and added sugars and sweeteners (19 percent) (Wells and Buzby, 2008). As a result of increased production of grains and other foods, per capita total energy availability has risen substantially during the last 30 years—from 2,169 to 2,594 calories between 1970 and 2009 (Figure 3-2), with the largest proportion of the increase coming from fats and processed grain products (ERS, 2012). On the other hand, per capita availability of vegetables, fruits, and dairy products currently is less than 70 percent of the recommended amounts (Figure 3-3).
These aggregate production numbers may simply reflect Americans’ consumption preferences and choices. If so, then if the U.S. population were to make healthier choices, that change might be reflected in the aggregate production numbers. Alternatively, people may eat what is available. In this case, if the overall availability of different types of foods is inconsistent with current dietary recommendations—as the evidence suggests—individuals are unlikely to be able to meet the recommendations.
FOOD PURCHASING PATTERNS AND DIETARY INTAKE AMONG
LOW-INCOME HOUSEHOLDS AND SNAP PARTICIPANTS
Food Purchasing Patterns
As discussed in Chapter 1, dietary intake is complex and multi-dimensional and includes food preferences, cultural appropriateness, preparation methods, meal patterns, and individual health needs, among other components. The following section reviews evidence on overall expenditures on food, the marginal propensity to consume food, where SNAP
____________________
1Food availability is defined as the total amount of food available for consumption and is calculated as the sum of annual production, beginning stocks, and imports minus exports, ending stocks, and nonfood uses.
FIGURE 3-3 Loss-adjusted per capita food availability compared with dietary recommendations.
NOTE: Data for 2005 based on a 2,000-calorie diet.
SOURCE: Wells and Buzby, 2008. USDA, ERS Food Availability (Per Capita) Data System.
participants purchase food, and the types of food purchased by low-income and SNAP populations.
Overall Expenditures
The origin of the federal poverty measure is Statistical Policy Directive No. 14, developed in 1968 and revised in 1969 and 1981 (OMB, 2012). As discussed in Chapter 2, the basis of the poverty measure is USDA’s economy food plan, which was derived from a 1955 Survey of Food Consumption. This survey found that the average American household spent about one-third (30 percent) of its income on food (U.S. Census Bureau, 1982). The 30 percent figure, however, has been criticized as no longer being relevant to expenditure patterns among U.S. households; the implication for SNAP participants is that they cannot supplement their benefit with the income amount assumed by this figure.
Castner and Mabli (2010) used data from the 2005 Consumer Expenditure Survey to examine the allocation of resources (including SNAP benefits) for household expenditures (including food) across various consumption categories for SNAP, SNAP-eligible but not participating, and SNAP-ineligible groups. They found that SNAP households allocate about 22 percent of their total household expenditures for food consumed at home, compared with 18 percent for SNAP-eligible but not participating households. SNAP households use a greater proportion of their total
expenditures as well as a greater total amount, $4,013 annually, for food, compared with SNAP-eligible nonparticipants, who spend about $3,443 annually for food. Although SNAP-ineligible households spend the most on food, $4,709, that amount represents a smaller percentage of their income than is the case for either SNAP or SNAP-eligible but not participating households. These findings, along with other recent evidence (Frazao et al., 2007; Schnepf and Richardson, 2009), are generally consistent with Engel’s Law, which states that as a household’s income rises, the amount of that income spent on food also rises, but the proportion of income spent on food declines.
As with general food spending, SNAP participants spend more than eligible nonparticipants on food consumed at home. Specifically, SNAP participants spend 24 percent more than eligible nonparticipants but 5 percent less than ineligible nonparticipants on food consumed at home. By contrast, SNAP participants spend significantly less than eligible and noneligible nonparticipants on food consumed away from home. In terms of actual dollars spent, the 2005 Consumer Expenditure Survey showed that an individual SNAP participant spent about $445 per year on food consumed away from home, compared with $560 for eligible nonparticipants and $945 for noneligible nonparticipants (Castner and Mabli, 2010).
Marginal Propensity to Consume
The marginal propensity to consume is defined as the amount by which expenditures on goods and services in a budget category will increase in response to an increase in income of $1.00. A different but related measure is the marginal propensity to consume food with SNAP benefits, which reflects the change in food expenditures that results from a $1.00 increase in these benefits (Castner and Mabli, 2010). The increase in food spending that accompanies an increase in income is not necessarily the same as the increase that accompanies an increase in SNAP benefits since, unlike regular income, these benefits must be spent on food. If participants’ desired spending on food exceeds their benefits, however, economic theory predicts that an increase in SNAP benefits and an increase in income will have the same influence on food expenditures. Still, the marginal propensity to consume as applied to SNAP benefits has been estimated to be $0.17 to $0.47, compared with an average of $0.10 as applied to regular income (Breunig and Dasgupta, 2003; Burnstein et al., 2005; Fox et al., 2004; Fraker, 1990).
The difference between the effects of cash income and SNAP benefits on food expenditures was illustrated in the “food stamp cashout” studies of the 1980s. In these studies, participants were randomly assigned to receive their benefits either in the form of cash or, as was standard at the time, in the form of food stamps. Researchers examined participants’ food expenditures,
and found that food spending was about 7 percent higher when the benefits came in the form of food stamps rather than an equivalent amount of cash (Breunig et al., 2001; Fraker et al., 1995). These findings implied a marginal propensity to consume food with SNAP benefits of $0.18-$0.28, which falls within the $0.17 to $0.47 range noted above.
Hoynes and Schanzenbach (2009) studied the influence of the receipt of nutrition assistance benefits, such as SNAP, through in-kind transfer, such as vouchers or Electronic Benefit Transfer (EBT) cards, on the purchasing power of low-income households. They examined data from the Panel of Income Dynamics from 1968 to 1978 to determine the impact of SNAP on food consumption and the effect of SNAP participation on labor supply. Collectively, their findings support the theory that SNAP benefits decrease overall out-of-pocket food spending but increase total spending on food. The analysis also found a decrease in the tendency of SNAP participants to consume food away from home, although the overall food environment during their study period of 1968-1978 was very different from the food environment of today. In addition, the program at that time had a “purchase requirement” that participants purchase food stamps, which could then be redeemed in stores to obtain foods having a value greater than the original price of the stamps; this requirement was eliminated in 1977. In contrast to the findings reported above, however, the marginal propensity to consume with SNAP income appears to be similar to that for cash income.
Where SNAP Participants Purchase Food
As described above, Frazao and colleagues (2007) and Castner and Mabli (2010) found that expenditures of SNAP participants and low-income households on food consumed at home represent the largest share of total food expenditures. A Canadian study derived similar results from a secondary analysis of nationally representative food expenditure data (Kirkpatrick and Tarasuk, 2003). Among the population groups studied, low-income households spent less overall on food but also spent 83.5 percent of their total food budget on food consumed at home, compared with 73.3 percent among higher-income households.
Evidence from USDA’s Food and Nutrition Service (FNS) on where food for consumption at home is purchased suggests that the majority of SNAP participants use larger food outlets as their primary source for food and that they shop outside their immediate neighborhood. Mantovani and Welsh (1996) and Ohls and colleagues (1999) both report that about 90 percent of SNAP participants used a supermarket as their main food shopping outlet. However, many also shopped at other types of food outlets, including convenience stores, bakeries, produce stands, and farmers’
markets as secondary food sources. More recent data from USDA-FNS (Castner and Henke, 2011) about where EBT cards were used by participants show that about 64 percent of EBT purchases were made at super-markets, accounting for 84 percent of the dollar value of foods purchased with SNAP benefits.
Types of Food Purchased by Low-Income and SNAP Populations
Leibtag and Kaufman (2003) analyzed food store scanner data to examine how low-income households economize on food purchases. They found that low-income households purchase more discounted items and private-label store brand products; take greater advantage of volume discounts; and purchase less expensive versions of a given product compared with higher-income households. Among the food types purchased, they found that low-income households purchase fewer fruits and vegetables and pay less for them than high-income households.
Frazao and colleagues (2007) found that among the lowest-income households, the largest food expenditure at grocery stores is for “other foods”—frozen prepared meals, canned and packaged prepared foods, snack foods, condiments and seasonings, sugar and other sweets, fats and oils, and nonalcoholic beverages. Meat purchases account for about 30 percent of the money spent on food in grocery stores, followed by fruits and vegetables (fresh, frozen, canned, dried, or juice), and lastly cereals and bakery products or dairy products.
Stewart and Blisard (2008) found that, compared with middle- and upper-income households, those with an income at or below 130 percent of the poverty threshold spent significantly less on six of the seven food categories studied—bread and baked goods, milk and dairy, beef, fruits, vegetables, and frozen prepared foods; only the amount spent on eggs did not vary by household income. However, a small increase in income corresponded to households allocating more money to only two of the seven categories—beef and frozen prepared foods. The authors note that these two categories of foods may be priorities for reasons of taste and convenience. For additional money to be allocated to fruits and vegetables, a household’s income must be slightly greater than 130 percent of the federal poverty threshold.
Mabli and colleagues (2010b) did not directly examine what foods were purchased by SNAP participants but instead examined changes in the proportion of food expenditures going to foods identified in the 2010 DGA as “foods recommended for frequent consumption” and “foods not recommended for frequent consumption” when households spend more on food overall. In general, the study found that households spending more on food overall allocated a higher proportion of their total food expenditures
to foods such as fruits, vegetables, and dried beans and peas (i.e., foods recommended for frequent consumption), but also spent a higher proportion on “foods not recommended for frequent consumption” (e.g., baked desserts, salty snacks, other sweets) compared with households with lower total food expenditures. Because SNAP benefits raise households’ purchasing power, the implication is that the benefits at least have the potential to raise the share of a household’s food expenditures going toward these recommended foods.
Finally, to investigate whether additional SNAP benefits result in increased purchases of fruits and vegetables, Frazao and colleagues (2007) analyzed 2004-2005 data on household spending from the Consumer Expenditure Survey (BLS, 2012). They found that additional income influenced food purchasing patterns for fruits and vegetables only at incomes above $70,000 per year. Further, their analysis suggested that the cost of fruits and vegetables affects low-income households’ purchases in the expected direction, but the magnitude of this effect is modest. A 10 percent discount in the price of fruits and vegetables leads to a 5 to 6 percent increase in purchases by low-income households, while coupons for 10 percent off lead to a 2 to 11 percent increase in purchases. These magnitudes are small enough to suggest that reductions in the cost of these foods would not have a large influence on the proportion of low-income households achieving recommended intakes of fruits and vegetables (Dong and Leibtag, 2010).
Dietary Intake
The committee considered evidence about the quality of dietary in-take. In particular, the committee reviewed evidence on whether the steep increase in the quantity of grains available in the U.S. food supply as described earlier suggests an overall increase in carbohydrate intake among the U.S. population.
Kant and Graubard (2007) examined secular trends in the association between diet and indicators of socioeconomic position. Data from the National Health and Nutrition Examination Survey (NHANES) were analyzed for total carbohydrate intake over time, by poverty/income ratio and level of education, as indicators of socioeconomic position. The authors found persistent positive associations of poverty/income ratio and education level with consumption of nutrient-dense foods, particularly fruits and vegetables, and higher intakes of vitamins A and C and calcium. Across time, the percentage of obese adults increased in all socioeconomic groups, although the poverty/income ratio differential in obesity prevalence persisted (Kant and Graubard, 2007). The study further identified a positive association between socioeconomic position and amount of food and energy intake, as well as potassium intake, an association that has persisted over three decades.
Kirkpatrick and colleagues (2012) extended this research and assessed the extent to which Americans met dietary standards between 2000 and 2004. They found that few Americans met dietary recommendations for total fruits (17.5 percent), whole fruits (25.1 percent), total vegetables (12.9 percent), dark green vegetables (5.9 percent), orange vegetables (1.9 percent), dry beans and peas (3.5 percent), starchy vegetables (38.3 percent), whole grains (0.8 percent), and milk (7.7 percent). In addition, individuals from middle- and low-income households had significantly lower intakes for all of these food groups except dry beans and peas and starchy vegetables. Among racial/ethnic groups, the lowest percentage of those meeting the recommendations were African Americans. Most children also failed to meet current recommendations, although fewer differences were found by income in this age group. Most adults and children had high consumption of solid fats and added sugars.
Using data from the What We Eat in America component of NHANES (2007-2008), the committee reviewed intakes of selected micronutrients and macronutrients for Americans 2 years of age and older. In the bivariate analysis presented below, the committee made no attempt to adjust the estimated intake levels for the demographic characteristics of individuals in each of the groups examined. For example, lower-income and higher-income Americans may have different age distributions, which, in turn, could explain differences in their intake levels, as opposed to different consumption patterns. While NHANES has excellent measures of dietary intake and clinical markers of nutritional status, income and participation in nutrition assistance are not well measured. The survey does include the full 18-item Core Food Security Module, as well as information on SNAP participation. Nevertheless, it is but one dataset that includes only about 5,000 persons located in 15 counties across the country each year. The bivariate analysis may suggest whether there are substantial differences in dietary patterns between Americans at different intake levels that are worthy of further investigation.
On the other hand, data from the Institute of Medicine report Strategies to Reduce Sodium Intake (IOM, 2010) show that the median sodium intake from foods for individuals aged 2 years and over from households at greater than 185 percent of the poverty threshold was 3,362 mg/day, compared with 3,098 and 3,079 mg/day for those from households at 131-185 percent and at or below 131 percent of the poverty threshold, respectively (NHANES 2003-2006), suggesting, as noted above, that individuals from low-income households limited their sodium intake more than did those from higher-income households.
Findings of a report by Cole and Fox (2008), based on NHANES data, suggest that for all vitamins, minerals, and macronutrients assessed, the dietary intake among SNAP participants was comparable to that of
SNAP-eligible nonparticipants. Compared with higher-income adults, however, SNAP participants had lower intakes of several vitamins and minerals.
SNAP participants also had significantly lower scores for several of the components of the Healthy Eating Index (HEI)-2005, including total fruits, whole fruits, total vegetables, whole grains, milk, and healthy oils and solid fats and added sugars (Cole and Fox, 2008). (The HEI is discussed further below.) On the other hand, scores on the HEI-2005 components of dark green and orange vegetables, total grains, meat and beans, saturated fats, and sodium were no different for SNAP participants and higher-income individuals. Finally, Fernandes (2012) found that SNAP participation was not associated with frequency of consumption of soft drinks, 100 percent fruit juice, or milk among youth. Overall, the HEI-2005 score was statistically lower among SNAP participants compared with higher-income nonparticipants (Figure 3-4).
The available evidence does lead to one clear conclusion. Given changes in the availability of certain nutrients in the food supply and lower availability of fruits, vegetables, and low-fat or nonfat milk products, relative to current recommendations, along with evidence for a positive association between socioeconomic status and amount of food and energy intake, many U.S. population groups fall short of meeting current dietary recommendations.
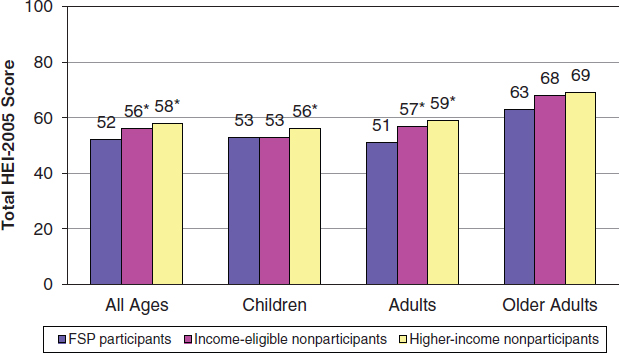
FIGURE 3-4 Healthy Eating Index-2005: Total scores.
NOTES: FSP = Food Stamp Program; HEI = Healthy Eating Index.
*Denotes statistically significant difference from Food Stamp Program participants at the 0.05 level or better. Estimates are age adjusted.
SOURCE: Cole and Fox, 2008.
Role of the DGA (Dietary Guidelines for Americans)
As noted in Appendix G, the DGA (USDA and HHS, 2010) serve as the scientific basis for all federal nutrition policy and nutrition programs, including SNAP. Since 1980 when the first DGA were published (USDA and USDHEW, 1980), the goals of the guidelines have evolved with changes in understanding of nutritional health needs. Today, however, a large proportion of the population, while meeting or exceeding the goals for intake of fat, saturated fat, grains, and protein, is failing to meet the goals for intake of fruits and vegetables, dietary fiber, and milk (Wells and Buzby, 2008).
This finding may be driven by a number of personal (individual), social, and environmental factors. As captured in the committee’s framework (see Chapter 1), personal choice, food preferences, and taste are primary influences on food selection (see also Chapter 4). At the same time, environmental factors in some locales, such as limited availability of healthy foods, greater availability of highly processed foods, and limited access to outlets that offer a variety of food choices, may be key modifiable variables with an impact on food purchasing power—a particularly important concern for participants in nutrition assistance programs such as SNAP.
To assess the extent to which SNAP allotments are adequate to purchase a healthy diet, it is useful to have a tool for measuring the quality of participants’ diets. While there is no single standard tool for this purpose, the HEI (Box 3-1) is one of several measures considered for assessing diet quality among SNAP households, maintenance of an adequate level of nutrition, and access to a healthy diet (see Chapter 1). The HEI was designed to measure and monitor the quality of diets consumed by the U.S. population and the low-income subpopulation (CNPP, 2012). Figure 3-5 shows that scores on the components of the original HEI remained relatively stable over the first decade of its use.
The HEI serves not only as a monitor for dietary intake over time but also as a predictor of health outcomes. To examine the effectiveness of the HEI in predicting health outcomes, McCullough and colleagues (2000a) used a food frequency questionnaire to measure the index (HEI-f) among healthy adults and estimated their risk for certain chronic diseases. They found that, compared with adults with good HEI-f scores (>80), a poor HEI-f score was only modestly associated with an increased risk of cardio-vascular disease among women and with an increased risk of chronic disease and cardiovascular disease among men, and no associations were found between HEI-f score and cancer risk. The authors conclude that the weak association found between HEI-f score and markers of chronic disease may be due either to methodological limitations or to failure of the HEI
BOX 3-1
The Healthy Eating Index
The Healthy Eating Index (HEI) is a measure of the quality of diets consumed by Americans and assesses conformance to federal dietary guidance. It was developed using three 24-hour recalls as the data collection method. At present, there is no dietary questionnaire or screening tool that can be used to calculate the HEI.
The U.S. Department of Agriculture originally created a general classification for the HEI with a score >80 designated as good dietary intake, 51-80 as “needs improvement,” and <51 as poor dietary intake. The original HEI was based on 10 foods or food components—grains, vegetables, fruits, milk, and meats; total fat and saturated fat as a percentage of total energy; total cholesterol; total sodium; and variety in the diet—each scored at a maximum of 10 points for a maximum total score of 100.
The revised HEI-2005 consists of 12 components (see text for description). The authors also removed the classification of “poor,” “needs improvement,” and “good” from the scoring system. Dietary intake is assessed on an energy-adjusted density basis (per 1,000 calories), providing an estimate of the relative proportions rather than the quantity of foods consumed. Higher scores are given for greater consumption of food-based components and lower scores for greater consumption of sodium and of solid fats and added sugars. The maximum scores per component range from 5 to 20, with a possible total of 100 points.
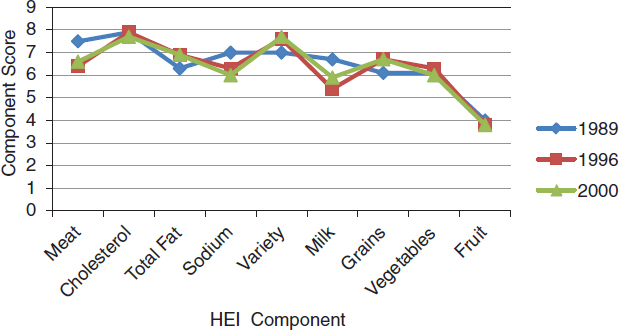
FIGURE 3-5 Comparison of Healthy Eating Index component scores, 1989-2000.
SOURCES: Basiotis et al., 2002; Bowman et al., 1998; CNPP, 1995.
to reflect an optimal diet, so that it is inconclusive as to diet quality as a predictor of risk for chronic disease.
Another study, using NHANES data, found that HEI categories were significantly associated with higher odds of overweight and obesity after controlling for age, gender, income, education, race/ethnicity, physical activity, smoking, and alcohol use. These outcomes were similar and significant in gender-stratified models (Guo et al., 2004). Other studies found that lower HEI scores were associated with greater abdominal fat stores (Tande et al., 2010) and increased all-cause and cardiovascular mortality among older Americans (Rathod et al., 2012), lending support to the HEI as a predictor of diet-related health outcomes. These studies are important for understanding the methodological approach and effectiveness of the HEI as a monitoring tool for assessing diet quality and ultimately for establishing an approach to defining the adequacy of SNAP allotments.
The 2005 HEI update added new components, including oils, calories from alcohol, solid fats and added sugars, whole fruit, dark green and orange vegetables, legumes, and whole grains, consistent with the 2005 DGA (Guenther et al., 2007; HHS and USDA, 2005). Figure 3-6 shows the HEI scores for low-income compared with all income groups in the
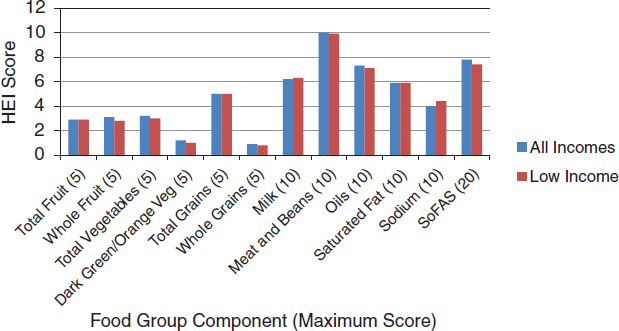
FIGURE 3-6 Comparison of Healthy Eating Index component scores (2005) for low-income and all income groups. Higher scores are given for greater consumption of food-based components and lower scores for greater consumption of sodium, saturated fat, and solid fats and added sugars.
NOTES: HEI = Healthy Eating Index; SoFAS = calories from solid fats and added sugars.
SOURCE: CNPP, 2008.
United States based on data gathered in NHANES 2003-2004 and reported in 2005 (CNPP, 2008). For this time frame, the overall average HEI scores were similar for both low-income and all income groups—56.5 and 57.8, respectively. When individual component scores were compared, however, low-income groups scored significantly lower on total vegetables, dark green and orange vegetables, legumes, and whole grains compared with all income groups, indicating lower compliance with the DGA in the former group.
Because of limitations of the HEI and changes in the DGA since 1990, researchers have sought to improve upon the original HEI and create a number of more specific indices in addition to the updated HEI-2005. Kant and colleagues (2000) created the Recommended Food Score (RFS), a tally of 23 recommended foods (such as oranges, broccoli, and baked or broiled fish) consumed at least once a week for a maximum total score of 23. McCullough and colleagues (2002) created the Alternate Healthy Eating Index (AHEI), comprising servings of vegetables, fruits, nuts, and protein; ratio of white to red meat; grams of cereal fiber; percentage of energy from trans fat; ratio of polyunsaturated to saturated fatty acids; multivitamin use; and servings of alcohol. Comparing the RFS with the AHEI, McCullough and colleagues found both to be strongly and significantly associated with chronic disease in men, particularly cardiovascular disease, while high AHEI scores were also associated with reductions in risk for chronic disease in women (McCullough et al., 2002). Chiuve and colleagues (2012) compared an updated AHEI-2010 with the HEI-2005 and found low scores on both to be strongly associated with coronary heart disease and diabetes.
Finally, in addition to the HEI, RFS, and AHEI, researchers developed the 2005 Dietary Guidelines Adherence Index, used to assesses adherence to the DGA recommendations specific to dietary intake and comprising 11 energy-specific food intake items and nine nutrient intake items (Fogli-Cawley et al., 2006). Higher scores on this index were associated with lower markers of insulin resistance and fasting insulin (Fogli-Cawley et al., 2007).
In assessing the strength and quality of the evidence, the committee determined that, because all the studies assessing the association between diet quality and chronic disease outcomes are cross-sectional and involve adult cohorts, a causal relationship between diet quality and risk for chronic disease cannot be demonstrated. However, there is no standard approach to measuring diet quality comprehensively. As the nutrition field continues to develop more refined and nuanced measures of diet quality that are specific to various chronic diseases, work is likely to continue on developing a comprehensive diet quality index that can be used to measure an optimal diet that is linked to the DGA and can serve as an indicator of risk of chronic disease.
At present, the most effective tool for measuring diet quality is the HEI-2005, which can be applied to subgroups such as low-income, including SNAP, populations within the general U.S. population. There are limitations, however, to the effectiveness of the HEI-2005 as a tool for evaluating the adequacy of SNAP allotments, because there is no consensus on how well the index actually tracks dietary intake and therefore how useful it is as a measure for optimal diet. Thus, one cannot conclude that the SNAP program does not contribute to improved diet quality because it may be that (1) the measure used for nutritional status is not reliable and/or (2) a number of other factors beyond income and participation in nutrition assistance programs influence dietary intake. In sum, the available evidence is insufficient to draw conclusions about associations between dietary intakes consistent with recommendations of the DGA and the adequacy of SNAP benefits to ensure access to a healthy diet.
Impact of SNAP Benefits
The committee considered the analytical challenge of self-selection of SNAP participants into the program, as well as the issue of underreporting of participation in the studies reviewed. The committee also considered the challenge of measuring indicators of diet quality because, in addition to the limitations discussed above, such studies typically are based on information collected through dietary surveys, which are expensive and rely on self-reported information. Moreover, a number of studies designed to estimate the impact of SNAP on indicators of diet quality were conducted more than 10 years ago.
Fox and colleagues (2004) summarize this older research, concluding that “the literature strongly suggests that the Food Stamp Program (SNAP) has little to no impact on individuals’ dietary intake” (p. 62). Gleason and colleagues (2000) estimated the effects of program benefits on individuals’ dietary intake using a regression model to control for observable characteristics, including demographic and socioeconomic characteristics, as well as less common controls, such as dietary knowledge and attitudes, health status, and exercise frequency. Overall, this study found no statistically significant relationships between receipt of SNAP benefits and mean intake of nearly all the vitamins, minerals, and food groups they examined. In a similar study, Wilde and colleagues (2000) found no association between SNAP participation and consumption of fruits, vegetables, grains, and dairy products, nor did they find that SNAP participation was associated with increased consumption of meats, added sugars, or total fat.
The body of research examining the impact of SNAP on participants’ body mass index (BMI) and obesity risk is also ambiguous. Some studies found evidence for a positive association between SNAP participation and
increased BMI and risk of obesity among adult women, but not among children, the elderly, or adult men. Others found no significant relationship between SNAP and obesity even among adult women (Chen et al., 2005; Gundersen et al., 2009; Jilcott et al., 2011a,b).
A recent literature review on the relationship between SNAP participation and obesity found no evidence to support a significant relationship among children, adult men, or elderly participants of either sex (Ver Ploeg and Ralston, 2008). However, the same review did find evidence of a positive correlation between SNAP participation and mean BMI and obesity risk among adult women. A number of observational studies found a positive relationship between SNAP participation and risk for increased BMI or obesity, particularly among women (Baum, 2011; Chen et al., 2005; Gibson, 2003, 2006; Leung et al., 2012; Meyerhoefer and Pylypchuk, 2008); however, estimates of the magnitude of the effect varied widely across studies, ranging from 3 percent to about 60 percent.
Other research failed to find a significant relationship between SNAP participation and obesity among adult women. Kaushal (2007) examined effects of SNAP participation on BMI among adults in immigrant families using participation data collected after eligibility revisions that followed enactment of the Personal Responsibility and Work Opportunity Reconciliation Act of 1996.2 The study found no significant association between SNAP participation and increased BMIs among low-educated unmarried mothers. Burgstahler and colleagues (2012) examined whether SNAP participation with or without household financial stress was associated with childhood overweight and obesity. Data derived from the Survey of Household Finances and Childhood Obesity were used to compare childhood obesity outcomes among 360 SNAP-eligible children, aged 2 to 18 (70.3 percent of whom were SNAP participants). After controlling for household financial stress, the study found a negative association between SNAP participation and obesity among SNAP-eligible children.
Kreider and colleagues (2012) analyzed data from the 2001-2006 NHANES using a method to derive informative bounds on the average treatment effect of SNAP on a range of health outcomes, including obesity. This method was used to account for both program self-selection bias and underreporting of participation status. The analysis could not rule out the possibility that SNAP participation either increases or decreases poor health, but the authors concluded that it may be inversely related to risk for child obesity.
Collectively, this evidence is insufficient to conclude a causal relationship between SNAP benefits and diet-related health outcomes in the
____________________
2Personal Responsibility and Work Opportunity Reconciliation Act of 1996, Public Law 104-193 (August 22, 1966).
low-income population. There is some evidence, although inconsistent, to support an association between SNAP participation and risk for high BMI in women.
As discussed in Chapter 2, food insecurity, defined as “inadequate or unsure access to enough food for active, healthy living” (Andrews and Nord, 2009, p. 33), is due most often to a lack of money or other resources. (A description of how food security is measured is also given in Chapter 2.) As noted by Coleman-Jensen and colleagues (2012a), food insecurity is determined by the resources a household has available with which to purchase food. For example, high housing costs can result in less money available to purchase food, particularly among low-income populations (Fletcher et al., 2009; Kirkpatrick and Tarasuk, 2007, 2011). Seasonally increased household expenses for heating and other utilities can also compromise the amount of money available for food purchases (Bhattacharya et al., 2003; Nord and Kantor, 2006).
While food insecurity affects only a portion of the U.S. population, it is an increasing concern, particularly among SNAP participants, because of its effects on health, productivity, and well-being. The following discussion summarizes the evidence on measures of food insecurity and its prevalence among low-income and SNAP populations, along with use of the emergency food system. It then examines the relationship between food security and measures of the quantity and type of food available for consumption, as well as the health effects associated with food insecurity. The discussion includes a summary of the evidence on the impact of SNAP benefits on food insecurity among participants.
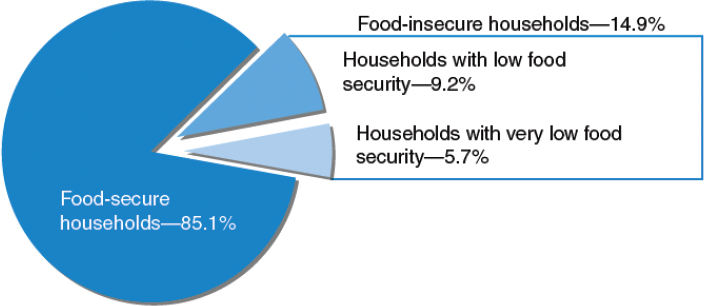
Prevalence of Food Insecurity
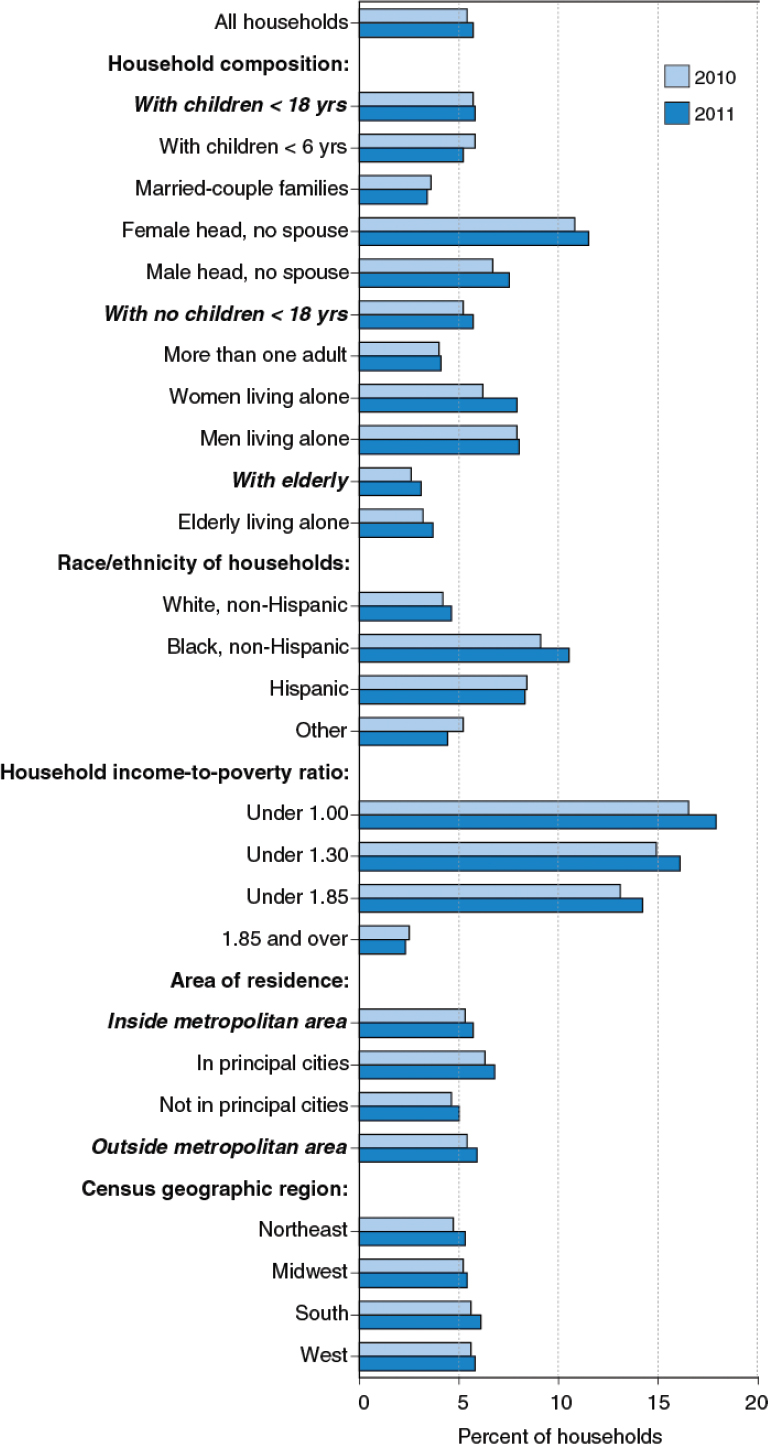
Population data from the 2011 Current Population Survey Food Security Module (CPSFSM) show that 85.1 percent of all households in the United States were food secure and 14.9 percent were food insecure, including 5.7 percent (6.8 million households) that had very low food security at some point during the past year (Coleman-Jensen et al., 2012a). This means that for one or more individuals in the household, eating patterns were disrupted or food intake was reduced at some point during the previous 12 months (Figure 3-7).
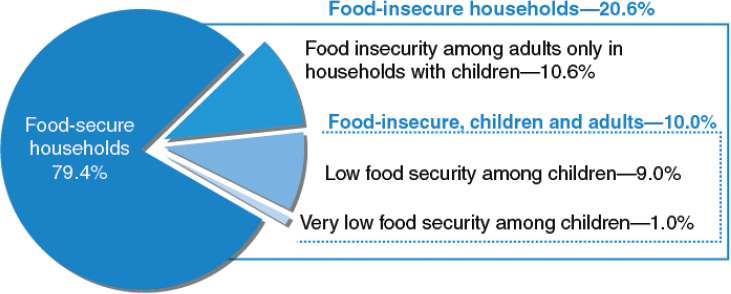
In the same report, the prevalence of food insecurity was found to be higher among households with children (birth through 18 years). Within that group of households, 20.6 percent were food insecure, including 10.6 percent in which only adults experienced food insecurity and 10.0 percent in
FIGURE 3-7 U.S. households by food security status, 2011.
SOURCE: Coleman-Jensen et al., 2012a. Calculated using data from the December 2011 Current Population Survey Food Security Supplement.
which both adults and children did so. These national figures suggest that very low food insecurity among children is relatively rare. While children experienced low food security in 9.0 percent of such households, they had very low food security in only 1.0 percent of such households (Figure 3-8).
Trends between 2010 and 2011, shown in Figure 3-9, suggest that the prevalence of food insecurity has remained relatively stable, after rising sharply in 2008 (see also Chapter 2, Figure 2-5, for trends between 1995 and 2011). There was a slight but statistically significant decrease in very low food security in 2010, although 6.4 million households still were thus categorized (Coleman-Jensen et al., 2011). In 2011, very low food security in households with children was most common in households headed by single women (1.8 percent) and in African American and Hispanic households (1.9 percent each) (Coleman-Jensen et al., 2012a).
As discussed in Chapter 2, the current classification of household food security status also recognizes the category of “marginal food security,” defined as answering in the affirmative one or two of the CPSFSM questions. Although marginal food security is not directly reported in the annual Household Food Security report, the report’s Statistical Supplement does report responses to individual questions (Table S-6): 19.7 percent reported they were “worried food would run out before I/we got money to buy more,” and 16.2 percent reported “the food bought didn’t last and I/we didn’t have money to buy more” (Coleman-Jensen et al., 2012b). Previously, these households were classified as food secure; however, a number of studies have demonstrated that individuals from marginally food secure households have demographic and socioeconomic characteristics similar to those from households with low food security (Coleman-Jensen, 2010;
FIGURE 3-8 U.S. households with children by food security status of adults and children, 2011.
SOURCE: Coleman-Jensen et al., 2012a. Calculated using data from the December 2011 Current Population Survey Food Security Supplement.
Laraia et al., 2006) and have increased risk of poor cognitive and health outcomes (Jyoti et al., 2005; Parker et al., 2010; Whitaker et al., 2006; Winicki and Jemison, 2003).
As with other social and economic indicators, food insecurity is unevenly distributed across the population. There are clear differences in prevalence depending on household composition, race/ethnicity, household income/poverty ratio, area of residence, and geographic region of the country (Figure 3-9). Food insecurity is more prevalent in households with incomes below the federal poverty threshold—41.1 percent, compared with 7.0 percent among those with incomes greater than 185 percent of the poverty threshold (Coleman-Jensen et al., 2012a). Compared with the national average, higher rates of food insecurity are found in households with children (11.3 percent of children live in households in which one or more children are food insecure), those headed by a single woman or man (36.8 and 24.9 percent, respectively), and African American (25.1 percent) and Hispanic (26.2 percent) households. The 2011 CPSFSM also identified differences in the prevalence of food insecurity for large cities (17.7 percent), nonmetropolitan areas (15.4 percent), and suburbs and non-principal-city metropolitan areas (13.2 percent). Geographically, food insecurity is greater in the South and West, while the prevalence pattern for very low food insecurity is similar in all areas (5.3-6.1 percent) (Coleman-Jensen et al., 2012a).
In addition to being more prevalent among low-income households, food insecurity is much more prevalent among SNAP participants than among nonparticipants. Among households that received SNAP benefits in 2010, Table 3-1 indicates that more than half (51.7 percent) were food insecure,
TABLE 3-1 Food Security Status Among SNAP-Eligible Households with Incomes Below 130 Percent of the Federal Poverty Threshold, 2011
| Food Insecure (%) | ||||
| Food Secure (%) | All | Low Food Security | Very Low Food Security | |
| Received SNAP benefits in previous 12 months | 48.3 | 51.7 | 28.7 | 23.0 |
| Received SNAP benefits in all 12 months | 50.9 | 49.1 | 26.8 | 22.3 |
| Received SNAP benefits in 1 to 11 months | 44.0 | 56.0 | 31.8 | 24.2 |
| Did not receive SNAP benefits | 72.3 | 27.7 | 16.4 | 11.3 |
NOTE: SNAP = Supplemental Nutrition Assistance Program (formerly the Food Stamp Program).
SOURCE: Coleman-Jensen et al., 2012a. Calculated by the Economic Research Service using data from the December 2011 Current Population Survey Food Security Supplement.
including 23.0 percent that had very low food security (Coleman-Jensen et al., 2012a). These rates of food insecurity among SNAP participants were much higher than the rates among the U.S. population overall, but also were much higher than the rates among other low-income households. Among income-eligible households that did not participate in SNAP in 2011, 27.7 percent were food insecure, including 11.3 percent with very low food security (Coleman-Jensen et al., 2012a; see Table 3-1). In other words, the rates of food insecurity among SNAP households were nearly twice those of other low-income households. As discussed below, this does not mean that SNAP contributed to higher food security among participating households; rather, it suggests that households experiencing low and very low food security turn to SNAP for relief.
Use of the Emergency Food System
A private emergency food system operates alongside the federal nutrition assistance programs, primarily through food pantries and soup kitchens, to help alleviate food insecurity. In the 2011 CPSFSM, 5.6 percent of respondents reported using a pantry and 0.5 percent eating at a soup kitchen. Nearly 53 percent of pantry users had also been SNAP participants during the previous 30 days (Coleman-Jensen et al., 2012b). Feeding America (formerly America’s Second Harvest)—the largest network of food banks in the United States, serving about 37 million people annually—regularly surveys its participating agencies and clients, most recently in 2009 (Mabli et al., 2010a). The 2009 survey showed that 71 percent of clients had incomes below the federal poverty threshold, and three-quarters were food insecure. More than 40 percent of clients were from households receiving
SNAP benefits, compared with 35 percent in the 2005 survey. In 2009, about 14.5 million low-income households received emergency food services, “an increase of 46 percent in unduplicated annual clients since the Hunger in America 2006 report” (Feeding America, 2010, p. 4). The 2008 Farm Bill3 authorized the appropriation of $15 million for each of fiscal years 2008 to 2012 to bolster this informal system. Additionally, funding for the Emergency Food Assistance Program (TEFAP), which supports food purchases by food banks and other emergency feeding organizations, was set at $140 million per year.
Between the federal data sources on emergency food use and the Feeding America survey data, it is clear that while federal nutrition assistance programs, including SNAP, provide substantial support to improve the food security of many households, a considerable number of people remain food insecure and must seek additional food from other sources, such as the emergency food system. The far-reaching and pervasive use of food pantries and soup kitchens provides anecdotal support for the proposition that SNAP may not be meeting the food/food security needs of the low-income population.
Food Security and the Quantity and Availability of Food
There is evidence to suggest a relationship between food security and measures of the quantity and types of food available for consumption (Brinkman et al., 2010). While some evidence shows a negative although nonlinear association between income level and availability of food (Leete and Bania, 2010), other evidence shows that low-income households may compromise on the type of food consumed while the quantity may be the same. To illustrate, Kendall and colleagues (1996), using the Radimer/Cornell measure of household food security, found that among a small sample (N = 193) of women in rural upstate New York, those living in food insecure households had less food available in the household than those in more food secure households. Two cross-sectional surveys examining relationships between income level and diet quality found that low-income families view food costs as “flexible” when faced with financial constraints and find ways to stretch food dollars that include purchasing less expensive versions of the same foods they would purchase if more money were available (Dachner et al., 2010; Hoisington et al., 2002).
A report on interviews regarding food management practices among people with limited resources identified both acceptable and unacceptable practices used to manage the household food supply. The acceptable practices included preparing low-cost foods and preserving home-grown
____________________
3Food, Conservation, and Energy Act of 2008, Public Law 110-234, Sec. 4202, p. 612.
foods. Unacceptable practices included amending spoiled foods, restricting personal food intake to feed other family members, and obtaining food opportunistically (Kempson et al., 2002). Taken together, these studies indicate that food insecurity aligns with decreased food intake.
Bauer and colleagues (2012) analyzed responses to a survey of parents of 432 kindergarten-age children living on the Pine Ridge Indian reservation. The survey included measures of food security, children’s BMI and dietary intake (by frequency of consumption), home food availability, food practices, and barriers to having healthful foods in the home. About 40 and 30 percent of parents, respectively, reported experiencing food insecurity or very low food security in the previous 12 months. Children of parents who reported very low food security were significantly more likely to have consumed hot or ready-made food from a convenience store or gas station, although there were no differences by food security status in food availability, frequency of fast-food consumption, number of family meals, or food shopping trips among the families surveyed. Parents who were food insecure were more likely to report little variety in fruit and vegetable choices, poor condition of fruits and vegetables in their food stores, low acceptance of fruits and vegetables by family members, and lack of time for food preparation.
Associations Between Food Security and Diet Quality
Food insecurity, as noted above, can be associated with the quantity and types of food available to households. Evidence is more limited, however, on the relationship between food insecurity and diet quality. A recent study of 67 residents of Boston used concept mapping to discern which factors drive food purchasing behaviors across income levels and how the consequent purchases influence diet quality (Walker and Kawachi, 2012). The study found that both food secure and food insecure participants considered the same factors to be important for healthy eating; both groups also assigned the same importance to factors that hinder healthy eating. The groups differed in food choices, however, with the food insecure choosing more energy-dense foods than the food secure. Food insecure participants described their food availability as being dependent largely on emergency food assistance programs. The prevalence of obesity among study participants was greater in the food insecure than in the food secure group. The energy density of the foods that were received or selected by participants was unknown. The authors interpret the study results as suggesting that food insecure participants may be consuming larger quantities of food from all available sources because of the uncertainty of having food available, which may have an impact on caloric intake.
Additional evidence for an impact of food security on diet quality supports a positive relationship between increased spending on food and diet
quality, although the improvement, as measured by HEI score, is small and varies by food category (Bernstein et al., 2010; Mabli et al., 2010a). As indicated by the Walker and Kawachi (2012) study, households may respond to the dilemma of limited resources for food by substituting energy-dense, nutrient-poor, less expensive foods for more expensive nutrient-dense ones, with a resulting decrease in micronutrient intake (Basiotis and Lino, 2002; Darmon et al., 2002; Drewnowski et al. 2004). Such a diet can contribute to overweight or obesity, which in turn increases the risk for chronic diseases and may also contribute to the risk for nutrient inadequacy.
Few specific nutrient deficiencies have been linked to food insecurity in developed countries such as the United States. Using the child food security scale developed by Nord and Bickel (2002) and measures of iron status, Skalicky and colleagues (2006) examined associations between food insecurity and iron nutriture in young children (aged 6 months to 3 years) seen in hospital emergency departments. Although the numbers are small, the adjusted logistic regression analysis controlling for confounders showed that food insecure children were nearly more than twice as likely to have iron deficiency anemia compared with food secure children. Brotanek and colleagues (2007) conducted a retrospective analysis of iron deficiency prevalence in children using data from the 1999-2002 National Health and Nutrition Examination Survey (NHANES). Although the results were not statistically significant, the prevalence of anemia in children from food insecure households was 12 percent, compared with 7 percent in those from food secure households. Similarly, in their analysis of NHANES data (1988-1994), Alaimo and colleagues (2001) found that the prevalence of iron deficiency was higher in food insufficient preschool children than in food sufficient children (11.6 percent vs. 8.6 percent), although this differential was not significant in a regression analysis.
Many of the studies reviewed by the committee that evaluate associations between household food security and nutritional status in population subgroups are inconsistent in both design and quality. Taken together, however, they suggest that associations between low household food security and some measure of decreased nutritional status, particularly among women (Kendall et al., 1996; Tarasuk, 2001; Tarasuk and Beaton, 1999) and the elderly (Bhattacharya et al., 2004; Dixon et al., 2001; Lee and Frongillo, 2001a,b; Wolfe et al., 1998), should be taken into consideration. While not finding specific nutrient deficiencies, Dixon and colleagues (2001) report both lower dietary intakes (<50 percent of the Recommended Dietary Allowances [RDAs]) and lower serum levels for selected nutrients in adults classified as being from food insufficient families compared with those from food sufficient families in NHANES III. Younger adults (aged 20-59) had 1-day intakes below 50 percent of the RDAs for vitamin E and Adequate Intake (AI) for calcium for 1 day, while older adults (>60)
had lower 1-day intakes (<50 percent of the RDAs) for zinc and iron. The authors report that about one-third of the younger and older adults from food insecure families had lower serum concentrations of total carotene and vitamin C. It is important to note that factors such as smoking or infection could also affect serum levels of these indicators. Additionally, while the serum nutrients and dietary intakes were individual, food insufficiency was measured at the household level.
In their analysis of NHANES III, Bhattacharya and colleagues (2004) found that food insecurity in adults (aged 18-64) had “large effects on the probability of being low in serum nutrients among both whites and blacks,” as well as Hispanics with low incomes. They concluded that for adults, food insecurity was associated with poorer-quality diets and higher probabilities of low serum nutrients. However, the committee concluded that evidence for an association between food insecurity and prevalence of nutrient inadequacy is less compelling than that for an association between food insecurity and risk for chronic disease.
Health Effects Associated with Food Insecurity
There are various health conditions for which an association with food insecurity has been reported. Only selected examples are discussed below.
Pregnancy and Breastfeeding Outcomes
Evidence reviewed in the Institute of Medicine report Weight Gain During Pregnancy (IOM, 2009) strongly suggests that the most influential factors in fetal growth are prepregnancy BMI and weight gain during the first and second trimesters. Olson and Strawderman (2008) examined food insecurity in early pregnancy but did not find an association with increased risk for obesity in food insecure women up to 2 years postpartum. The study findings were strong, however, for an association between both obesity and food insecurity during early pregnancy and risk for excess gestational and post-partum weight gain. In a study of women in the Pregnancy, Infection, and Nutrition prospective cohort, Laraia and colleagues (2010) found that in a model adjusted for demographic and socioeconomic characteristics, food insecurity at any level was positively associated with gestational diabetes. They also found that food insecurity was strongly related to prepregnancy obesity and excessive weight gain during pregnancy, both of which are associated with poorer birth outcomes. Early evidence from studies of pregnancy outcomes suggests that gestational weight gain may be a determinant of risk for obesity and obesity-related health outcomes in the offspring; however, this evidence is still emerging (Li et al., 2007; Oken et al., 2007; Ong et al., 2000; Sowan and Stember, 2000; Wrotniak et al., 2008).
Carmichael and colleagues (2007) examined data from a large, population-based case control study of primarily Hispanic women in California to determine associations between three levels of food security (food secure, food insecure without hunger, and food insecure with hunger) and risk for neural tube defects, orofacial cleft, and conotruncal heart defect. Their survey of 1,189 cases and 695 controls identified positive associations between food insecurity and anencephaly, cleft palate (modified by BMI), and tetralogy of Fallot (indicator of neural tube defect), suggesting that food insecurity is associated with increased risk for poor developmental outcomes.
Few studies have been conducted on the effects of food insecurity on breastfeeding. Zubieta and colleagues (2006) examined breastfeeding duration in infants from food secure and food insecure households using data from NHANES (1999-2000 and 2001-2002). They found that fewer infants were breastfed in the food insecure households, and among all infants that were breastfed, the duration was 38 days longer in the food secure than in the food insecure households.
Risk for Chronic Disease
Diabetes is a serious chronic disease that is particularly prevalent in low-income and minority populations (Beckles et al., 2011). African American and Latino adults are 1.7 to 1.8 times more likely to have diabetes than white adults (Schiller et al., 2012). In a two-city study of a community safety net clinic serving low-income, multiethnic individuals with type II diabetes, Seligman and colleagues (2011) found that nearly half were food insecure. Compared with food secure participants, those who were food insecure had higher levels of glycosylated hemoglobin (HbA1c), an important marker of glucose control. Further, about 30 percent of participants reported having a severe hypoglycemic event in the past year, and 9 percent reported four or more such events. The significance of these differences remained after adjusting for demographic and other risk factors. The relationship between food insecurity and lack of glycemic control was partially explained by difficulty following a prescribed diet and increased emotional distress related to diabetes. Consistent with these studies, Marjerrison and colleagues (2011), using a combination of telephone interviews and chart reviews for 183 Nova Scotian families with a child with type I diabetes, found that HbA1c levels were higher in children from food insecure households than in those from food secure households (9.5 ± 2.13 percent versus 8.96 ± 1.50 percent).
Seligman and colleagues (2010a) used NHANES (1999-2004) data to examine diet-related chronic diseases and prevalence of food insecurity in adult low-income (<200 percent of the poverty threshold) participants. They found that in adjusted models, food insecurity was associated with
self-reported hyperlipidemia and hypertension. Further, adults living with the most severe levels of food insecurity had a twofold increased risk of diabetes compared with adults with immediate access to healthful foods. Additional work by Seligman and colleagues (2010a,b, 2011) showed that food insecure individuals with diabetes were twice as likely as food secure individuals with diabetes to experience severe hypoglycemic episodes and poor diabetes self-management.
Self-Reported Health or Health Status
Various studies examining food insecurity have found that individuals who are food insecure often report poorer health. To illustrate, self-reported health status in food secure and food insecure women was reported in a study using data from the 1999 Panel Study of Income Dynamics (Jones and Frongillo, 2006). Although only 8 percent of all women surveyed were food insecure, younger food insecure women reported fewer sick days but were far more likely to report their health as fair or poor compared with older food secure women. Another study of food insecurity and self-reported health of adults in the lower Mississippi Delta found that about 20 percent of this population-based sample was food insecure and that the food insecure were more than twice as likely as food secure participants to report their health as fair/poor (Stuff et al., 2004). In a multisite study of young children that was part of the Children’s Sentinel Nutrition Assessment Project, parents in food insecure households were nearly twice as likely as parents in food secure households to report their child’s health as fair or poor (Cook et al., 2004).
Collectively, the strongest evidence for an association between food insecurity and adverse health outcomes is in adults. Evidence for an association between food insecurity and increased risk for obesity is also stronger for adults than for children, and the association with increased risk for type 2 diabetes or adverse diabetes outcomes is stronger than that for other chronic diseases. The evidence is unclear, however, on whether poor health status and risk for chronic disease are due to food insecurity or whether they lead to greater risk for food insecurity.
Impact of SNAP Participation on Food Insecurity
Evidence reviewed by the committee suggests that SNAP participation can reduce the prevalence of food insecurity (Borjas, 2004; Mykerezi and Mills, 2010; Nord and Prell, 2011; Van Hook and Balistreri, 2006; Yen et al., 2008). In interpreting this evidence, the committee considered that self-selection of SNAP participants into the program could create a bias. For example, Nord and Golla (2009) examined monthly data on both house-
hold SNAP participation and food insecurity and found that in the months immediately prior to entering the program, households experienced a steady increase in food insecurity. In particular, the prevalence of very low food security rose from 8 percent to 20 percent in the months before a household entered SNAP. This pattern suggests that these households were experiencing events that both led to food insecurity and prompted their decision to enter the program. In the months following their entry into SNAP, the households’ levels of food insecurity declined (with very low food security declining back to about 12 percent), evidence suggestive of beneficial effects of the program on this outcome (Nord and Golla, 2009).
In contrast to the findings of Nord and Golla (2009), several other studies examining whether SNAP participation improves food security while accounting for self-selection bias found that the benefits either had no effect or were associated with higher levels of food insecurity (Gibson-Davis and Foster, 2006; Gundersen and Oliveira, 2001; Jensen, 2002; Wilde and Nord, 2005). More recently, however, Bartfeld and Dunifon (2006) found lower food insecurity among near-poor and low-income populations in states with high SNAP participation rates compared with states with low participation rates, suggesting the possibility of beneficial program effects. Borjas (2004) and Van Hook and Balistreri (2006) examined food insecurity among immigrants whose program eligibility was affected by the Personal Responsibility and Work Opportunity Reconciliation Act4 and found lower levels of food insecurity among immigrant households that remained eligible for SNAP compared with similar groups that lost their eligibility as a result of the legislated changes. Similarly, Nord and Prell (2011) found that food insecurity among the SNAP-eligible population fell after passage of the American Recovery and Reinvestment Act of 2009 (ARRA),5 which increased SNAP benefit levels. The study found further that the amount spent on food by SNAP-eligible low-income households increased by 5.4 percent, and about 2.2 percent of that increase may be attributable to changes resulting from passage of the ARRA. SNAP-ineligible households with incomes just above the poverty threshold increased their food expenditures by a smaller percentage than low-income SNAP-eligible households, and the prevalence of food insecurity among the former households did not decline. There was no similar trend of increased food expenditures among those eligible for SNAP. Finally, two other studies using a statistical approach to account for both measured and unmeasured characteristics potentially related to entry into SNAP found that SNAP participation led
____________________
4Personal Responsibility and Work Opportunity Reconciliation Act of 1996, Public Law 104-193, 104th Congress (August 22, 1966).
5American Recovery and Reinvestment Act of 2009, Public Law 111-5, 111th Congress (February 17, 2009).
to a statistically significant reduction in rates of food insecurity (Mykerezi and Mills, 2010; Yen et al., 2008).
An additional study estimated the impact of SNAP on food security using an approach for dealing with self-selection into the program that relied on a few strong assumptions and produced upper and lower bounds on the possible effect of the program (Kreider et al., 2012). The study focused on the impact of SNAP on child nutritional health based on data derived from the 2001-2006 NHANES. The analysis included households with children eligible to participate in SNAP; a final weighted sample of 4,418 children was obtained. Socioeconomic and demographic characteristics of the sample were compared with national estimates obtained from the 2003 CPS, December Supplement. The study also accounted for the possibility of error in the measurement of SNAP participation in survey data. Each of the studies of the impact of SNAP on food insecurity noted above relied on survey-based measures of SNAP participation that have been found to be subject to measurement error when compared with more accurate administrative sources of this information (Meyer et al., 2009). Kreider and colleagues (2011) found that both the lower and upper bounds of the estimated impact of SNAP on food insecurity fell below zero, suggesting that the program reduces food insecurity among participants. In one model, the results implied that SNAP reduces the prevalence of food insecurity by at least 8 percentage points, and perhaps by a larger amount. Taken together, the evidence suggests that SNAP benefits can help alleviate food insecurity; however, the evidence is less conclusive among certain subgroups of SNAP participants.
Overall, the evidence on the impact of SNAP participation on food insecurity is moderately strong. While there have been no randomized controlled trials that can shed light on how SNAP affects household food insecurity, the nonexperimental studies examining this question have made serious efforts to account for the possibility of selection bias in the impact estimates. In particular, these studies have used various methods to account for observed and unobserved factors that lead some households to receive SNAP benefits and others to not participate. Although their methods have varied, the studies generally have found consistently that SNAP benefits lead to a reduction in rates of food insecurity among participating households. The available evidence is not clear, however, on whether poor health status and risk for chronic disease are due to or lead to greater risk for food insecurity.
DATA AND ANALYTICAL CHALLENGES TO ASSESSING
THE ADEQUACY OF SNAP ALLOTMENTS
A number of challenges arise in assessing access to a healthy diet. First, nutrition has many dimensions, and no single measure or standard
approach can capture these multiple dimensions. The most commonly used summary measure of diet quality is the HEI-2005, and improvement in HEI scores among both the general population and low-income groups is a performance measure for the goal of “improving the nation’s nutrition and health” in USDA’s Strategic Plan for 2005-2010.
HEI-2005 scores show that most Americans, including SNAP participants and other low-income groups, are falling short of meeting the current DGA. This failure among Americans at all income levels highlights that the HEI-2005 (or other measures of diet quality) should not be used as a sole measure of the adequacy of SNAP allotments. SNAP participants—and other Americans—may have reasons for choosing foods with low nutrient density, and limited household resources for obtaining food is just one of these reasons. A related challenge to assessing access to a healthy diet is entailed in measuring diet quality. A number of methodologies are used to collect data on dietary intake. Interviewer-administered 24-hour dietary recalls are appropriate for a less educated population for monitoring and surveillance purposes. This method decreases respondent burden and greatly improves data quality compared with other methods; however, it is expensive, and a protocol using multiple 24-hour recalls is challenging to complete.
A limited number of datasets include dietary intake at the individual level. Most national-level datasets cannot be used to assess individual-level diet quality because this type of data cannot be aggregated by income level or program participation. Given these limitations, NHANES is currently the best dataset available for examining diet quality in low-income, including SNAP, populations because it is based on state-of-the-art data collection on dietary intake, includes the full 18-item Core Food Security Module, and includes information on SNAP participation. Nevertheless, NHANES is only one dataset, and although it examines a nationally representative sample, only about 5,000 persons located in 15 counties across the country are sampled each year. Furthermore, inherent challenges arise in identifying whether respondents within the same household are related and with linking individuals to external data sources. In addition, NHANES measures SNAP participation through self-report and includes substantial measurement error. Linking the NHANES data to another administrative data source with more accurate reporting of SNAP participation might improve understanding of the association between SNAP participation and dietary intake. Another limitation of NHANES is that, because it is cross-sectional, it does not permit tracking changes in food security or access to a healthy diet over time.
More research is needed to test the validity of the HEI as a comprehensive measure that captures overall diet quality, whether it is internally reliable and therefore highly correlated with other important components of
the diet, and whether it is a reliable measure across time and across studies. It will be difficult to evaluate the adequacy of SNAP allotments until agreement is reached on the type of diet quality index needed for this purpose.
Thus, longitudinal data on SNAP participation, food security, and dietary intake are needed. With such data, researchers could track changes in the outcomes of food security and diet quality over time and relate changes in SNAP participation to changes in these outcomes. While assessment of the adequacy of SNAP allotments may be based on examining whether program participants appear to be meeting the goals of improving food security and access to a healthy diet, it is not clear what standards should be used to determine whether food security has been sufficiently improved or whether participants truly have access to a healthy diet. For example, what level of food security among participants would be required to determine that SNAP benefits are adequate? Should SNAP benefits be expected to eliminate low and/or very low food security entirely (if both, this would imply that the resulting rate of food insecurity should be zero percent among participants for benefits to be judged adequate)? Or would a more appropriate standard be to expect the rate of low and/or very low food security to be approximately the same among participants as among low-income nonparticipants? And what standards of nutrient adequacy should be expected—perhaps an HEI-2005 score equal to that of nonparticipants?
Key to defining the adequacy of SNAP allotments is having estimates of the impact of these benefits on such outcomes as diet quality, obesity, or food security. However, self-selection into SNAP greatly complicates such estimates. Because individuals and households choose whether to participate in the program if they are eligible, the unmeasured characteristics of participants may differ in important ways from those of nonparticipants. Further, these differences in unmeasured characteristics may be related to key outcomes of interest. Thus, a difference in outcomes between participants and nonparticipants could be due either to differences in their unmeasured characteristics or to the effect of program participation. Although a number of sophisticated methods have been developed to address this challenge, none of these methods is perfect, and critics have challenged their validity.
In assessing the feasibility of defining the adequacy of SNAP allotments, the committee considered a range of evidence on the impact of SNAP program participation on achieving the program goals of improving food security and access to a healthy diet. In general, the committee found that it would be useful to conduct further research examining food security and
access to a healthy diet among program participants and estimating the impact of SNAP benefits on these outcomes.
Food Security
Overall, the evidence on the impact of SNAP participation on food insecurity is moderately strong. While there have been no randomized controlled trials that can shed light on how SNAP affects household food insecurity, the nonexperimental studies reviewed have made serious efforts to account for the possibility of selection bias in their impact estimates. In particular, these studies have used various methods to account for observed and unobserved factors that lead some households to receive SNAP benefits and others not to participate.
The evidence suggests that food insecurity is common among SNAP participants. As discussed above, data from 2011 show that just under half of SNAP households (48 percent) were food secure, with 29 percent having low food security and 23 percent having very low food security. These rates of low and very low food security were nearly twice the rates for income-eligible households that did not participate in the program, 16 percent of which had low food security and 11 percent very low food security. Among higher-income households (those with incomes above 185 percent of the federal poverty threshold), more than 90 percent were food secure.6 Subgroups for which food insecurity is particularly prevalent include female-headed households with children and African American– and Hispanic-headed households (Coleman-Jensen et al., 2012a).
Although the prevalence of food insecurity is relatively high among SNAP participants, the most recent research suggests that it would be even higher absent SNAP benefits—in other words, that SNAP benefits have positive impacts on participants’ food security (i.e., reducing households’ likelihood of food insecurity). This finding raises the question of whether the high prevalence of food insecurity among SNAP households could be further reduced with higher benefit levels.
Taken together, the evidence suggests that SNAP benefits help alleviate food insecurity, but not enough to reduce the level of insecurity to that of either higher-income households or lower-income households that do not participate in the program. Evidence is less complete on the levels of food insecurity and impacts of benefits among subgroups of participants.
____________________
6These statistics are based on the 12-month measure of food insecurity and thus may be influenced by the households’ experiences prior to entering SNAP. The patterns of food insecurity based on the 30-day measure were similar to those reported here, although the food insecurity rates were somewhat lower (Coleman-Jensen et al., 2012a).
As discussed above, many SNAP households have diets that are not nutritious in all respects. The committee found that evidence on the question of whether SNAP benefits contribute to improving dietary quality is limited and insufficient to permit drawing conclusions on this question. In addition, significant methodological challenges arise in assessing diet quality in the SNAP population. Along with these challenges, the lack of evidence on this issue may be due to the time lag between receipt of the SNAP benefits and subsequent dietary intake and the failure of many studies to account for selection bias.
Alaimo, K., C. M. Olson, E. A. Frongillo Jr., and R. R. Briefel. 2001. Food insufficiency, family income, and health in U.S. preschool and school-aged children. American Journal of Public Health 91(5):781-786.
Andrews, M., and M. Nord. 2009. Food insecurity up in recessionary times. Amber Waves, http://webarchives.cdlib.org/sw1vh5dg3r/http://ers.usda.gov/AmberWaves/December09/Features/FoodInsecurity.htm (accessed April 8, 2013).
Bartfeld, J., and R. Dunifon. 2006. State-level predictors of food insecurity among households with children. Journal of Policy Analysis and Management 25(4):921-942.
Basiotis, P. P., and M. Lino. 2002. Food insufficiency and prevalence of overweight among adult women, Nutrition Insight 26. Washington, DC: USDA, CNPP. http://www.cnpp.usda.gov/Publications/NutritionInsights/Insight26.pdf (accessed August 23, 2012).
Basiotis, P. P., A. Carlson, S. A. Gerrior, W. Y. Juan, and M. Lino. 2002. The Healthy Eating Index: 1999-2000, CNPP-12. Washington, DC: USDA, CNPP. http://www.cnpp.usda.govpublications/hei/hei99-00report.pdf (accessed June 13, 2012).
Bauer, K. W., M. O. Hearst, K. Escoto, J. M. Berge, and D. Neumark Sztainer. 2012. Parental employment and work-family stress: Associations with family food environments. Social Science and Medicine 75(3):496-504.
Baum, C. L. 2011. The effects of food stamps on obesity. Southern Economic Journal 77(3):623-651.
Beckles, G. L., J. Zhu, and R. Moonesinghe. 2011. Diabetes—United States, 2004 and 2008. Morbidity and Mortality Weekly Report 60(Suppl. 1):90-93. http://www.cdc.gov/mmwr/preview/mmwrhtml/su6001a20.htm (accessed September 10, 2012).
Bhattacharya, J., T. DeLeire, S. Haider, and J. Currie. 2003. Heat or eat? Cold-weather shocks and nutrition in poor American families. American Journal of Public Health 93(7):1149-1154.
Bhattacharya, J., J. Currie, and S. Haider. 2004. Poverty, food insecurity, and nutritional outcomes in children and adults. Journal of Health Economics 23(4):839-862.
BLS (Bureau of Labor Statistics). 2012. Consumer Expenditure Survey. http://www.bls.gov/cex (June 7, 2012).
Borjas, G. J. 2004. Food insecurity and public assistance. Journal of Public Economics 88(7-8):1421-1443.
Bowman, S. A., M. Lino, S. A. Gerrior, and P. P. Basiotis. 1998. The Healthy Eating Index: 1994-96, CNPP-5. Washington, DC: USDA, CNPP. http://www.cnpp.usda.gov/publications/hei/hei94-96report.PDF (accessed June 13, 2012).
Breunig, R., and I. Dasgupta. 2003. Are people ashamed of paying with food stamps? Journal of Agricultural Economics 54(2):203-225.
Breunig, R., I. Dasgupta, C. Gundersen, and P. Pattanaik. 2001. Explaining the food stamp cash-out puzzle. Washington, DC: USDA, ERS. http://www.ers.usda.gov/publications/fanrr12 (accessed June 7, 2012).
Brinkman, J. J., S. De Pee, I. Sanogo, L. Subran, and M. W. Bloem. 2010. High food prices and the global financial crisis have reduced access to nutritious foods and worsened nutritional status and health. Journal of Nutrition 140(1):153S-161S.
Brotanek, J. M., J. Gosz, M. Weitzman, and G. Flores. 2007. Iron deficiency in early childhood in the United States: Risk factors and racial/ethnic disparities. Pediatrics 120(3):568-575.
Burgstahler, R., C. Gundersen, and S. Garasky. 2012. The Supplemental Nutrition Assistance Program, financial stress, and childhood obesity. Agricultural and Resource Economics Review 41(1):29-42.
Burnstein, N. R., W. L. Hamilton, M. K. Fox, C. Price, and M. P. Battaglia. 2005. Assessing the food security and diet quality impact of FNS program participation: Final report. Submitted by Abt Associates, Inc. to U.S. Department of Agriculture, Food and Nutrition Service, Alexandria, VA. http://www.fns.usda.gov/ora/menu/Published/snap/FILES/Other/DietQuality.pdf (accessed February 9, 2012).
Carmichael, S. L., W. Yang, A. Herring, B. Abrams, and G. M. Shaw. 2007. Maternal food insecurity is associated with increased risk of certain birth defects. Journal of Nutrition 137:2087-2092.
Castner, L., and J. Henke. 2011. Benefit redemption patterns in the Supplemental Nutrition Assistance Program. Submitted by Mathematica Policy Research, Inc. to U.S. Department of Agriculture, Food and Nutrition Service, Alexandria, VA. http://www.fns.usda.gov/ora/menu/Published/SNAP/FILES/ProgramOperations/ARRASpendingPatterns.pdf (accessed January 14, 2013).
Castner, L., and J. Mabli. 2010. Low-income household spending patterns and measures of poverty. Submitted by Mathematica Policy Research, Inc. to U.S. Department of Agriculture, Food and Nutrition Service, Alexandria, VA. http://www.fns.usda.gov/ora/menu/Published/snap/FILES/Participation/SpendingPatterns.pdf (accessed February 9, 2012).
Chen, Z., S. T. Yen, and D. B. Eastwood. 2005. Effects of food stamp participation on body weight and obesity. American Journal of Agricultural Economics 87(5):1167-1173.
Chiuve, S. E., T. T. Fung, E. B. Rimm, F. B. Hu, M. L. McCullough, M. Wang, M. J. Stampfer, and W. C. Willett. 2012. Alternative dietary indices both strongly predict risk of chronic disease. Journal of Nutrition 142(6):1009-1018.
CNPP (Center for Nutrition Policy and Promotion). 1995. The Healthy Eating Index. Washington, DC: USDA, CNPP. http://www.cnpp.usda.gov/publications/hei/HEI89-90report.pdf (accessed June 12, 2012).
CNPP. 2008. Diet quality of low-income and higher income Americans in 2003-04 as measured by the Healthy Eating Index-2005, Nutrition Insight 42. Washington, DC: USDA, CNPP. http://www.cnpp.usda.gov/Publications/NutritionInsights/Insight42.pdf (accessed June 5, 2012).
CNPP. 2012. Healthy Eating Index. http://www.cnpp.usda.gov/HealthyEatingIndex.htm (June 11, 2012).
Cole, N., and M. K. Fox. 2008. Diet quality of Americans by food stamp participation status: Data from the National Health and Nutrition Examination Survey, 1999-2004. Submitted by Abt Associates, Inc. to U.S. Department of Agriculture, Food and Nutrition Service, Alexandria, VA. http://www.fns.usda.gov/ora/menu/Published/snap/FILES/Participation/NHANES-FSP.pdf (accessed February 9, 2012).
Coleman-Jensen, A. J. 2010. U.S. food insecurity status: Toward a refined definition. Social Indicators Research 95:215-230.
Coleman-Jensen, A., M. Nord, M. Andrews, and S. Carlson. 2011. Household food security in the United States in 2010. Washington, DC: USDA, ERS. http://www.ers.usda.gov/publications/err-economic-research-report/err125.aspx (accessed June 11, 2012).
Coleman-Jensen, A., M. Nord, M. Andrews, and S. Carlson. 2012a. Household food security in the United States in 2011. Washington, DC: USDA, ERS. http://www.ers.usda.gov/publications/err-economic-research-report/err141.aspx (accessed September 6, 2012).
Coleman-Jensen, A., M. Nord, M. Andrews, and S. Carlson. 2012b. Household food security in the United States in 2011: Statistical supplement. Washington, DC: USDA, ERS. http://www.ers.usda.gov/publications/ap-administrative-publication/ap-058.aspx (accessed September 6, 2012).
Cook, J. T., D. A. Frank, C. Berkowitz, M. M. Black, P. H. Casey, D. B. Cutts, A. F. Meyers, N. Zaldivar, A. Skalicky, S. Levenson, T. Heeren, and M. Nord. 2004. Food insecurity is associated with adverse health outcomes among human infants and toddlers. Journal of Nutrition 134(6):1432-1438.
Dachner, N., L. Ricciuto, S. I. Kirkpatrick, and V. Tarasuk. 2010. Food purchasing and food insecurity among low-income families in Toronto. Canadian Journal of Dietetic Practice and Research 71(3):e50-e56.
Darmon, N., E. L. Ferguson, and A. Briend. 2002. A cost constraint alone has adverse effects on food selection and nutrient density: An analysis of human diets by linear programming. Journal of Nutrition 132(12):3764-3771.
Dixon, L. B., M. A. Winkleby, and K. L. Radimer. 2001. Dietary intakes and serum nutrients differ between adults from food-insufficient and food-sufficient families: Third National Health and Nutrition Examination Survey, 1988-1994. Journal of Nutrition 131(4):1232-1246.
Dong, D., and E Leibtag. 2010. Promoting fruit and vegetable consumption: Are coupons more effective than pure price discounts? ERR-96. Washington, DC: USDA, ERS. http://www.ers.usda.gov/publications/err-economic-research-report/err96.aspx (accessed July 3, 2012).
Drewnowski, A. 2004. Obesity and the food environment: Dietary energy density and diet costs. American Journal of Preventive Medicine 27(3 Suppl.):154-162.
ERS (Economic Research Service). 2012. Loss-adjusted food availability. http://www.ers.usda.gov/data-products/food-availability-(per-capita)-data-system.aspx#26705 (accessed July 5, 2012).
Feeding America. 2010. Hunger in America 2010: Executive summary. Chicago, IL: Feeding America. http://www.cafoodbanks.org/docs/Hunger%20Study%20Executive%20 Summary.pdf (accessed August 23, 2012).
Fernandes, M. M. 2012. Effect of the Supplemental Nutrition Assistance Program (SNAP) on frequency of beverage consumption among youth in the United States. Journal of the Academy of Nutrition and Dietetics 112(8):1241-1246.
Fletcher, J. M., T. Andreyeva, and S. H. Busch. 2009. Assessing the effect of changes in housing costs on food insecurity. Journal of Children and Poverty 15(2):79-93.
Fogli-Cawley, J. J., J. T. Dwyer, E. Saltzman, M. L. McCullough, L. M. Troy, and P. F. Jacques. 2006. The 2005 Dietary Guidelines for Americans adherence index: Development and application. Journal of Nutrition 136(11):2908-2915.
Fogli-Cawley, J. J., J. T. Dwyer, E. Saltzman, M. L. McCullough, L. M. Troy, J. B. Meigs, and P. F. Jacques. 2007. The 2005 Dietary Guidelines for Americans and insulin resistance in the Framingham offspring cohort. Diabetes Care 30(4):817-822.
Fox, M. K., W. Hamilton, and B. H. Lin. 2004. Effects of food assistance and nutrition programs on nutrition and health: Volume 3, literature review, FANRR 19-3. Submitted by Abt Associates, Inc. to U.S. Department of Agriculture, Economic Research Service, Washington, DC. http://webarchives.cdlib.org/sw1s17tt5t/http://ers.usda.gov/Publications/FANRR19-3 (accessed July 3, 2012).
Fraker, T. 1990. The effects of food stamps on food consumption: A review of the literature. Alexandria, VA: USDA, FNS.
Fraker, T. M., A. P. Martini, and J. C. Ohls. 1995. The effect of food stamp cashout on food expenditures. Journal of Human Resources 30(4):633-649.
Frazao, E., M. Andrews, D. Smallwood, and M. Prell. 2007. Can food stamps do more to improve food choices? An economic perspective—Food spending patterns of low-income households: Will increasing purchasing power result in healthier food choices?, EIB-29-4. Washington, DC: USDA, ERS. http://www.ers.usda.gov/publications/eib-economic-information-bulletin/eib29.aspx (accessed July 3, 2012).
Gibson, D. 2003. Food Stamp Program participation is positively related to obesity in low income women. Journal of Nutrition 133(7):2225-2231.
Gibson, D. 2006. Long-term food stamp program participation is positively related to simultaneous overweight in young daughters and obesity in mothers. Journal of Nutrition 136(4):1081-1085.
Gibson-Davis, C. M., and E. M. Foster. 2006. A cautionary tale: Using propensity scores to estimate the effect of food stamps on food insecurity. Social Service Review 80(1):93-126.
Gleason, P., A. Rangarajan, and C. Olson. 2000. Dietary intake and dietary attitudes among food stamp participants and other low-income individuals. Submitted by Mathematica Policy Research, Inc. to U.S. Department of Agriculture, Food and Nutrition Service, Alexandria, VA. http://www.fns.usda.gov/ora/menu/published/NutritionEducation/Files/FSPDiet.pdf (accessed February 9, 2012).
Guenther, P. M., J. Reedy, S. M. Krebs-Smith, B. B. Reeve, and P. P. Basiotis. 2007. Development and evaluation of the Healthy Eating Index-2005: Technical report. Washington, DC: USDA, CNPP. http://www.cnpp.usda.gov/Publications/HEI/HEI-2005/HEI-2005TechnicalReport.pdf (accessed July 12, 2012).
Gundersen, C., and V. Oliveira. 2001. The Food Stamp Program and food insufficiency. American Journal of Agricultural Economics 83(4):875-887.
Gundersen, C., S. Garasky, and B. J. Lohman. 2009. Food insecurity is not associated with childhood obesity as assessed using multiple measures of obesity. Journal of Nutrition 139(6):1173-1178.
Guo, X., B. A. Warden, S. Paeratakul, and G. A. Bray. 2004. Healthy eating index and obesity. European Journal of Clinical Nutrition 58(12):1580-1586.
Hernandez, D. C., and A. Jacknowitz. 2009. Transient, but not persistent, adult food insecurity influences toddler development. Journal of Nutrition 139(8):1517-1524.
HHS and USDA (U.S. Department of Health and Human Services and U.S. Department of Agriculture). 2005. Dietary Guidelines for Americans. Washington, DC: U.S. Government Printing Office. http://www.health.gov/dietaryguidelines/dga2005/document (accessed June 4, 2012).
Hoisington, A., J. A. Shultz, and S. Butkus. 2002. Coping strategies and nutrition education needs among food pantry users. Journal of Nutrition Education and Behavior 34(6):326-333.
Hoynes, H. W., and D. W. Schanzenbach. 2009. Consumption responses to in-kind transfers: Evidence from the introduction of the Food Stamp Program. American Economic Journal: Applied Economics 1(4):109-139.
IOM (Institute of Medicine). 2009. Weight gain during pregnancy: Reexamining the guidelines. Washington, DC: The National Academies Press.
IOM. 2010. Strategies to reduce sodium intake in the United States. Washington, DC: The National Academies Press.
Jensen, H. H. 2002. Food insecurity and the Food Stamp Program. American Journal of Agricultural Economics 84(5):1215-1228.
Jilcott, S. B., E. D. Wall-Bassett, S. C. Burke, and J. B. Moore. 2011a. Associations between food insecurity, Supplemental Nutrition Assistance Program (SNAP) benefits, and body mass index among adult females. Journal of the American Dietetic Association 111(11):1741-1745.
Jilcott, S. B., H. Liu, K. D. Dubose, S. Chen, and S. Kranz. 2011b. Food stamp participation is associated with fewer meals away from home, yet higher body mass index and waist circumference in a nationally representative sample. Journal of Nutrition Education and Behavior 43(2):110-115.
Jones, S. J., and E. A. Frongillo. 2006. The modifying effects of Food Stamp Program participation on the relation between food insecurity and weight change in women. Journal of Nutrition 136(4):1091-1094.
Jyoti, D. F., E. A. Frongillo, and S. J. Jones. 2005. Food insecurity affects school children’s academic performance, weight gain, and social skills. Journal of Nutrition 135(12):2831-2839.
Kant, A. K., and B. I. Graubard. 2007. Secular trends in the association of socio-economic position with self-reported dietary attributes and biomarkers in the U.S. population: National Health and Nutrition Examination Survey (NHANES) 1971-1975 to NHANES 1999-2002. Public Health Nutrition 10(2):158-167.
Kant, A. K., A. Schatzkin, B. I. Graubard, and C. Schairer. 2000. A prospective study of diet quality and mortality in women. Journal of the American Medical Association 283(16):2109-2115.
Kaushal, N. 2007. Do food stamps cause obesity? Evidence from immigrant experience. Journal of Health Economics 26(5):968-991.
Kempson, K. M., D. P. Keenan, P. S. Sadani, S. Ridlen, and N. S. Rosato. 2002. Food management practices used by people with limited resources to maintain food sufficiency as reported by nutrition educators. Journal of the American Dietetic Association 102(12):1795-1799.
Kendall, A., C. M. Olson, and E. A. Frongillo Jr. 1996. Relationship of hunger and food insecurity to food availability and consumption. Journal of the American Dietetic Association 96(10):1019-1024.
Kirkpatrick, S. I., and V. Tarasuk. 2003. The relationship between low income and household food expenditure patterns in Canada. Public Health Nutrition 6(6):589-597.
Kirkpatrick, S. I., and V. Tarasuk. 2007. Adequacy of food spending is related to housing expenditures among lower-income Canadian households. Public Health Nutrition 10(12):1464-1473.
Kirkpatrick, S. I., and V. Tarasuk. 2011. Housing circumstances are associated with household food access among low-income urban families. Journal of Urban Health 88(2):284-296.
Kirkpatrick, S. I., K. W. Dodd, J. Reedy, and S. M. Krebs-Smith. 2012. Income and race/ethnicity are associated with adherence to food-based dietary guidance among U.S. adults and children. Journal of the Academy of Nutrition and Dietetics 112(5):624-635.
Kreider, B., J. V. Pepper, C. Gundersen, and D. Joliffe. 2012. Identifying the effects of SNAP (Food Stamps) on child health outcomes when participation is endogenous and misreported. Journal of American Statistical Association 107(499):958-975.
Laraia, B. A., A. M. Siega-Riz, C. Gundersen, and N. Dole. 2006. Psychosocial factors and socioeconomic indicators are associated with household food insecurity among pregnant women. Journal of Nutrition 136(1):177-182.
Laraia, B. A., A. M. Siega-Riz, and C. Gundersen. 2010. Household food insecurity is associated with self-reported pregravid weight status, gestational weight gain, and pregnancy complications. Journal of the American Dietetic Association 110(5):692-701.
Lee, J. S., and E. A. Frongillo Jr. 2001a. Factors associated with food insecurity among U.S. elderly persons: Importance of functional impairments. Journals of Gerontology—Series B, Psychological Sciences and Social Sciences 56(2):S94-S99.
Lee, J. S., and E. A. Frongillo Jr. 2001b. Nutritional and health consequences are associated with food insecurity among U.S. elderly persons. Journal of Nutrition 131(5):1503-1509.
Leete, L., and N. Bania. 2010. The effect of income shocks on food insufficiency. Review of Economics of the Household 8(4):505-526.
Leibtag, E, and P. R. Kaufman. 2003. Exploring food purchase behavior of low-income households: How do they economize?, AIB 747-07. Current Issues in Economics of Food Markets. http://www.ers.usda.gov/publications/aib747/aib74707.pdf (accessed April 8, 2013).
Leung, C. W., W. C. Willett, and E. L. Ding. 2012. Low-income Supplemental Nutrition Assistance Program participation is related to adiposity and metabolic risk factors. American Journal of Clinical Nutrition 95(1):17-24.
Li, C., M. I. Goran, H. Kaur, N. Nollen, and J. S. Ahluwalia. 2007. Developmental trajectories of overweight during childhood: Role of early life factors. Obesity 15(3):760-771.
Mabli, J., R. Cohen, F. Potter, and Z. Zhao. 2010a. Hunger in America 2010. Submitted by Mathematica Policy Research, Inc. to Feeding America, Chicago, IL. http://www.mathematica-mpr.com/publications/PDFs/Nutrition/Hunger_in_America_2010.pdf (accessed July 12, 2012).
Mabli, J., L. Castner, J. Ohls, M. K. Fox, M. K. Crepinsek, and E. Condon. 2010b. Food expenditures and diet quality among low-income households and individuals: Final report. Submitted by Mathematica Policy Research, Inc. to U.S. Department of Agriculture, Food and Nutrition Service, Alexandria, VA. http://www.mathematica-mpr.com/publications/PDFs/nutrition/FoodExpendDietQuality.pdf (accessed February 9, 2012).
Mantovani, R. E., and J. Welsh. 1996. Authorized Food Retailer Characteristics Study (technical report III): Geographic analysis of retailer access. Submitted by Macro International, Inc. to U.S. Department of Agriculture, Food and Consumer Service, Alexandria, VA. http://naldc.nal.usda.gov/download/46420/PDF (accessed June 7, 2012).
Marjerrison, S., E. A. Cummings, N. T. Glanville, S. F. L. Kirk, and M. Ledwell. 2011. Prevalence and associations of food insecurity in children with diabetes mellitus. Journal of Pediatrics 158(4):607-611.
McCullough, M. L., D. Feskanich, E. B. Rimm, E. L. Giovannucci, A. Ascherio, J. N. Variyam, D. Spiegelman, M. J. Stampfer, and W. C. Willett. 2002. Adherence to the Dietary Guidelines for Americans and risk of major chronic disease in men. American Journal of Clinical Nutrition 72(5):1223-1231.
Meyer, B. D., W. K. C. Mok, and J. X. Sullivan. 2009. The under-reporting of transfers in household surveys: Its nature and consequences. NBER Working Paper 15181. http://www.nber.org/papers/w15181.pdf (accessed December 14, 2012).
Meyerhoefer, C. D., and Y. Pylypchuk. 2008. Does participation in the food stamp program increase the prevalence of obesity and health care spending? American Journal of Agricultural Economics 90(2):287-305.
Mykerezi, E., and B. Mills. 2010. The impact of Food Stamp Program participation on household food insecurity. American Journal of Agricultural Economics 92(5):1379-1391.
Nord, M., and G. Bickel. 2002. Measuring children’s food security in U.S. households, 1995-99, FANRR No. 25. Washington, DC: USDA, ERS. http://webarchives.cdlib.org/sw1tx36512/http://www.ers.usda.gov/Publications/fanrr25 (accessed July 3, 2012).
Nord, M., and M. Golla. 2009. Does SNAP decrease food insecurity? Untangling the self-selection effect, ERR-85. Washington, DC: USDA, ERS. http://www.ers.usda.gov/publications/err-economic-research-report/err85.aspx (accessed August 13, 2012).
Nord, M., and L. S. Kantor. 2006. Seasonal variation in food insecurity is associated with heating and cooling costs among low-income elderly Americans. Journal of Nutrition 136(11):2939-2944.
Nord, M., and M. Prell. 2011. Food security improved following the 2009 ARRA increase in SNAP benefits, ERR-116. Washington, DC: USDA, ERS. http://www.ers.usda.gov/publications/err116 (accessed June 7, 2012).
Ohls, J. C., M. Ponza, L. Moreno, A. Zambrowski, and R. Cohen. 1999. Food stamp participants’ access to food retailers: Final report. Submitted by Mathematica Policy Research, Inc. to U.S. Department of Agriculture, Food and Nutrition Service, Alexandria, VA. http://www.fns.usda.gov/ora/menu/published/snap/FILES/ProgramOperations/retailer.pdf (accessed June 7, 2012).
Oken, E., E. M. Taveras, K. P. Kleinman, J. W. Rich-Edwards, and M. W. Gillman. 2007. Gestational weight gain and child adiposity at age 3 years. American Journal of Obstetrics and Gynecology 196(4):322.e1-322.e8.
Olson, C. M., and M. S. Strawderman. 2008. The relationship between food insecurity and obesity in rural childbearing women. Journal of Rural Health 24(1):60-66.
OMB (Office of Management and Budget). 2012. OMB Statistical Policy Directive No. 14. http://www.census.gov/hhes/povmeas/methodology/ombdir14.html (accessed June 7, 2012).
Ong, K. K. L., M. L. Ahmed, D. B. Dunger, P. M. Emmett, and M. A. Preece. 2000. Association between postnatal catch-up growth and obesity in childhood: Prospective cohort study. British Medical Journal 320(7240):967-971.
Parker, E. D., R. Widome, J. A. Nettleton, and M. A. Pereira. 2010. Food security and metabolic syndrome in U.S. adults and adolescents: Findings from the National Health and Nutrition Examination Survey, 1999-2006. Annals of Epidemiology 20(5):364-370.
Rathod, A. D., A. S. Bharadwaj, A. O. Badheka, M. Kizilbash, and L. Afonso. 2012. Healthy Eating Index and mortality in a nationally representative elderly cohort. Archives of Internal Medicine 172(3):275-277.
Rose, D., and R. Richards. 2004. Food store access and household fruit and vegetable use among participants in the U.S. Food Stamp Program. Public Health Nutrition 7(8):1081-1088.
Schiller, J. S., J. W. Luas, B. W. Ward, and J. A. Peregoy. 2012. Summary health statistics for U.S. adults: National Health Interview Survey, 2010. National Center for Health Statistics. Vital Statistics (252), http://www.cdc.gov/nchs/data/series/sr_10/sr10_252.pdf (accessed April 8, 2013).
Schnepf, R., and J. Richardson. 2009. Consumers and food price inflation. Washington, DC: CRS. http://www.nationalaglawcenter.org/assets/crs/R40545.pdf (accessed June 7, 2012).
Seligman, H. K., B. A. Laraia, and M. B. Kushel. 2010a. Food insecurity is associated with chronic disease among low-income NHANES participants. Journal of Nutrition 140(2):304-310.
Seligman, H. K., T. C. Davis, D. Schillinger, and M. S. Wolf. 2010b. Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes. Journal of Health Care for the Poor and Underserved 21(4):1227-1233.
Seligman, H. K., E. A. Jacobs, A. Lopez, U. Sarkar, J. Tschann, and A. Fernandez. 2011. Food insecurity and hypoglycemia among safety net patients with diabetes. Archives of Internal Medicine 171(13):1204-1206.
Skalicky, A., A. F. Meyers, W. G. Adams, Z. Yang, J. T. Cook, and D. A. Frank. 2006. Child food insecurity and iron-deficiency anemia in low-income infants and toddlers in the United States. Maternal and Child Health Journal 10(2):177-185.
Sowan, N. A., and M. L. Stember. 2000. Parental risk factors for infant obesity. American Journal of Maternal Child Nursing 25(5):234-240.
Stewart, H., and N. Blisard. 2008. Are lower income households willing and able to budget for fruits and vegetables?, ERR-54. Washington, DC: USDA, ERS. http://www.ers.usda.gov/publications/err-economic-research-report/err54.aspx (accessed July 3, 2012).
Stuff, J. E., J. A. Horton, M. L. Bogle, C. Connell, D. Ryan, S. Zaghloul, A. Thornton, P. Simpson, J. Gossett, and K. Szeto. 2004. High prevalence of food insecurity and hunger in households in the rural Lower Mississippi Delta. Journal of Rural Health 20(2):173-180.
Tande, D. L., R. Magel, and B. N. Strand. 2010. Healthy Eating Index and abdominal obesity. Public Health Nutrition 13(2):208-214.
Tarasuk, V. S. 2001. Household food insecurity with hunger is associated with women’s food intakes, health and household circumstances. Journal of Nutrition 131(10):2670-2676.
Tarasuk, V. S., and G. H. Beaton. 1999. Women’s dietary intakes in the context of household food insecurity. Journal of Nutrition 129(3):672-679.
U.S. Census Bureau. 1982. Characteristics of the population below the poverty level: 1980. Washington, DC: Government Printing Office.
USDA and HHS (U.S. Department of Agriculture and U.S. Department of Health and Human Services). 2010. Dietary Guidelines for Americans, 2010. Washington, DC: Government Printing Office. http://www.health.gov/dietaryguidelines/2010.asp (accessed June 11, 2012).
USDA and USDHEW (U.S. Department of Agriculture and U.S. Department of Health, Education, and Welfare). 1980. Nutrition and your health: Dietary Guidelines for Americans. Washington, DC: Government Printing Office. http://www.cnpp.usda.gov/DGAs1980Guidelines.htm (accessed July 16, 2012).
Van Hook, J., and K. S. Balistreri. 2006. Ineligible parents, eligible children: Food stamps receipt, allotments, and food insecurity among children of immigrants. Social Science Research 35(1):228-251.
Ver Ploeg, M., and K. Ralston. 2008. Food stamps and obesity: What do we know?, EIB-34. Washington, DC: USDA, ERS. http://www.ers.usda.gov/publications/eib-economic-information-bulletin/eib34.aspx (accessed July 3, 2012).
Walker, R. E. and I. Kawachi. 2012. Use of concept mapping to explore the influence of food security on food buying practices. Journal of the Academy of Nutrition and Dietetics 112:711-717.
Wells, H. F., and J. C. Buzby. 2008. Dietary assessment of major trends in U.S. food consumption, 1970-2005, EIB-33. Washington, DC: USDA, ERS. http://www.ers.usda.gov/publications/eib-economic-information-bulletin/eib33.aspx (accessed July 3, 2012).
Whitaker, R. C., S. M. Phillips, and S. M. Orzol. 2006. Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics 118(3):e859-e868.
Wilde, P. E., and M. Nord. 2005. The effect of food stamps on food security: A panel data approach. Review of Agricultural Economics 27(3):425-432.
Wilde, P. E., P. E. McNamara, and C. K. Ranney. 2000. The effect on dietary quality of participation in the Food Stamp and WIC Programs, FANRR. Washington, DC: USDA, ERS. http://webarchives.cdlib.org/sw1bc3ts3z/http://ers.usda.gov/publications/fanrr9 (accessed July 12, 2012).
Winicki, J., and K. Jemison. 2003. Food insecurity and hunger in the kindergarten classroom: Its effect on learning and growth. Contemporary Economic Policy 21(2):145-157.
Wolfe, W. S., C. M. Olson, A. Kendall, and E. A. Frongillo Jr. 1998. Hunger and food insecurity in the elderly: Its nature and measurement. Journal of Aging and Health 10(3):327-350.
Wrotniak, B. H., J. Shults, S. Butts, and N. Stettler. 2008. Gestational weight gain and risk of overweight in the offspring at age 7 y in a multicenter, multiethnic cohort study. American Journal of Clinical Nutrition 87(6):1818-1824.
Yen, S. T., M. Andrews, Z. Chen, and D. B. Eastwood. 2008. Food Stamp Program participation and food insecurity: An instrumental variables approach. American Journal of Agricultural Economics 90(1):117-132.
Zubieta, A. C., H. Melgar-Quinonez, and C. Taylor. 2006. Breastfeeding practices in U.S. households by food security status. Faseb Journal 20(5):A1004-A1005.