3
Implementing Interprofessional Education for Improving Collaboration
Summary: Educating formal and informal leaders about the value of interprofessional education (IPE) may be a mechanism for getting leadership support for IPE at the leaders’ institutions. This was one message presented by the speaker representing the breakout group on “leadership,” and it is a primary focus of this chapter. The chapter begins with the case for why interprofessional education is important, and then it addresses some of the obstacles that implementers may face when promoting or initiating IPE. The discussion includes details on how innovators have overcome or addressed challenges to implementing or sustaining IPE at their universities. In the final section of the chapter, George Thibault reviews some lessons he has learned that could guide future discussions on mainstreaming IPE, which could expand opportunities for students to experience high-quality IPE and collaboration.
MAKING THE CASE FOR IPE
In the words of Forum and planning committee member George Thibault of the Josiah Macy Jr. Foundation, whose introductory talk addressed why IPE is a key innovation in health professions education, “Interprofessional education is a tool. It’s a tool to accomplish linkages between the education system and the health care delivery system. It is a tool to achieve better patient care. It is a tool to achieve better health for the public. It is a tool to achieve a more efficient and affordable health care system.” In essence, Thibault said, IPE is a tool for achieving the “triple
aim” constructed by the Institute for Healthcare Improvement (IHI)1 and adapted in this report for use with IPE as follows:
• IPE to achieve better patient care
• IPE to achieve better health (outcomes)
• IPE to achieve more efficient and affordable educational and health care systems
IPE to Achieve Better Patient Care
There is evidence, Thibault said, that care delivered by well functioning teams is better than care provided by health professionals practicing without coordination (Shortell, 1994; Goni, 1999; Campbell et al., 2001; Stevenson et al., 2001; Mukamel, 2006). There are many examples, he said, of teams that functioned poorly because their members lacked the appropriate knowledge, attitudes, and skills. And now more than ever the adverse consequences of poorly functioning teams are causing adverse consequences for many aspects of care outcomes; these consequences include medical errors, inefficient patient care (driving up costs), and a diminished quality of care for patients. Therefore, Thibault said, team-based competencies should be a core goal of health professions education and that some part of all health professions education must be interprofessional. This is the line of reasoning that Thibault stressed in making the case for why education should be taught interprofessionally. As one of the patient representatives at the workshop indicated, patients are the ones who stand to benefit most from improvements in provider communication and collaboration.
Workshop speaker Valentina Brashers, who is part of the University of Virginia’s Interprofessional Education Initiative Team, offered an example of achieving improved patient care through IPE, and she addressed the challenge of bridging the gap between IPE and patient care outcomes. Although it is still a work in progress, she said, the university has taken concrete steps to move IPE from the classroom to the simulation center to the bedside using its Health System Collaborative Care Project (see Table 3-1). This award-winning program offers incentives to health care teams in the hospital setting to develop new models of interprofessional care that involve students at various learning levels. Part of the criteria for receiving these incentives is the inclusion of metrics that ideally include provider outcomes as well as measurements of patient outcomes.
_______________
1 The Institute for Healthcare Improvement (IHI) “triple aim” is a framework developed by IHI that describes an approach to optimizing health system performance. It is IHI’s belief that new designs must be developed to simultaneously pursue three dimensions—population health, patient experience, and per capita cost—which they call the “triple aim.”
TABLE 3-1 University of Virginia Five-Step Model to Advance Team-Based Education and Collaborative Practice
|
|
|
| 1. | Clinically relevant IPE based on collaborative care best-practice models |
| 2. | IPE required and integrated throughout the learning continuum |
| 3. | Longitudinal assessment of IPE competencies |
| 4. | Commitment to continued rigorous IPE research and dissemination of results |
| 5. | Bridging the gap between IPE and patient care and outcomes |
|
|
|
IPE to Achieve Better Health (Outcomes)
The number of persons with chronic conditions continues to rise rapidly in the United States and around the world, said Forum and planning committee member Harrison Spencer of the Association of Schools and Programs of Public Health, referring to reports from the World Health Organization (WHO) (2011, 2013). If these current world trends in noncommunicable diseases (NCDs) continue, low-income countries are projected to have eight times more deaths due to NCDs than high-income countries by 2030 (Wu and Green, 2000). But “despite the presence of concepts, competencies, rationale, and well-defined need,” Spencer said, “public health and its framework of population health have not been integrated into interprofessional education.” In Spencer’s view, IPE is not about achieving better health, but rather about achieving better health outcomes. These outcomes are the end result of a health-related intervention or health care process affecting the health and well-being of patients and populations (AHRQ, 2000). Gaining better health outcomes will require a population perspective, and the only way to achieve positive results, he added, is through more robust funding streams that focus on health outcomes, with IPE as a tool.
Spencer also said that in shifting the focus to health outcomes and population health, one needs to think beyond the acute care setting and to consider less traditional partners from other sectors. He pointed to the model of inter- and transprofessional education (see Figure 3-1) on page 40 of the Lancet Commission report (Frenk et al., 2010) that leads to this sort of broader thinking by including a wider circle of partners, such as community health workers and non-health professions. As Forum member and workshop speaker Gillian Barclay from the Aetna Foundation noted, with such creative modeling comes innovation that resonates throughout the continuum of education and practice.
Spencer said that in population health there are two main sets of partners for IPE that can be drawn from either the clinical professions or from the nonclinical professions. These are not traditional partnerships. As such,
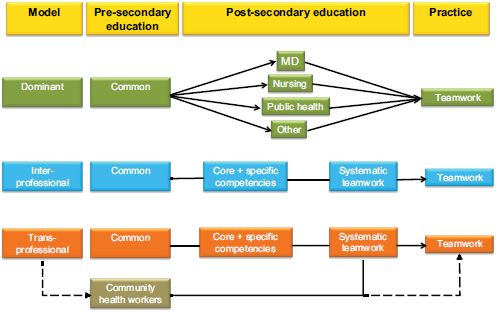
FIGURE 3-1 Models of inter- and transprofessional education.
SOURCE: Frenk et al., 2010.
there is need for new definitions of competencies as well as other relevant details concerning the appropriateness and effectiveness of IPE among the new partners. The issues are summarized in the following two sets of questions posed by Spencer:
Population Health IPE Collaborations with Clinical Professions
• What are the population-level competencies that clinical professions should develop?
• What specific examples of teamwork between clinical and population health professionals can be referred to in developing competencies?
• Are there competencies common to all health professionals in problem solving, communication, and teamwork?
• How do different institutional designs affect the effectiveness of IPE?
Population Health IPE Collaborations with Nonhealth Professions
• Public health is inherently multidisciplinary. Should it be made intentionally interprofessional?
• What are the specific competencies that should be developed vis-à-vis collaboration with lawyers, engineers, economists, policy analysts, urban planners, journalists, and other relevant professions?
In her summary remarks, Forum member and workshop speaker Marilyn Chow from Kaiser Permanente expressed her enthusiasm for the population health perspective, saying that the discussions may have gotten her to rethink whether the core competencies should include competencies related to population health, which would bring to the forefront thinking about the population and the patients as they incorporate public health principles.
IPE to Achieve More Efficient and Affordable Educational and Health Care Systems
Although “start up” funds often are needed to get IPE initiated, once IPE becomes standard practice, educational and health care systems stand to benefit financially through two mechanisms, according to Forum and planning committee member Madeline Schmitt of the University of Rochester. “It seems to me a good part of the costs on the interprofessional side is the cost of going around the silos that we’ve built,” she said. Recognizing the enormous amount of duplication in the content taught in silos is a first step toward cost containment. This recognition does not itself provide interprofessional learning, but it does establish a base from which students and faculty can work together to build interprofessional learning. The second aspect of costs that Schmitt addressed related to the practice side and the need to invest in the retraining of new graduates. “There are real costs associated with that retraining, which we could and should rethink on the education side,” she said. This message was aggressively promoted by workshop speaker Paul Grundy, who is the global director of the IBM Healthcare Transformation.
Another way that IPE could decrease costs would be through a decrease in medical errors produced by improved communication. Communication is a cornerstone of interprofessional education, as was emphasized by each of the breakout group leaders’ presentations on IPE for “improving health,” “providing better care,” “enhancing access to education,” and “lowering costs.” One topic of discussion at the workshop was the high rate of medical errors in the United States, with one participant citing the landmark IOM (1999) report To Err Is Human. In that report, published estimates from two major studies indicated that up to 98,000 people “die in hospitals each year as a result of medical errors that could have been prevented”; and, as one speaker pointed out, such medical errors continue today (Levinson, 2010, 2012). Given that the Joint Commission (2012)
estimated that 80 percent of all serious medical errors in the United States involve miscommunication, it can be expected that patient safety will improve when students enter the work environment with the superior communication skills that are provided by interprofessional education. As the leader of the IPE and lower costs small group at the workshop, Thomas Feeley of the MD Anderson Cancer Center said that improving outcomes and quality of care lowers the costs of care.
This notion of using IPE to “lower health care costs” did not resonate with all the workshop participants. Forum and planning committee member Jan De Maseaneer of Ghent University in Belgium noted that in many developing countries, spending on health care is minimal and inadequate. Given this situation, he said, the discussion should be about the improved value that IPE could bring to health care in developing countries rather than about lowering costs.
OVERCOMING OBSTACLES TO IMPLEMENTING IPE
George Thibault said that he is a fervent advocate of IPE, although he understands the challenges faced by those implementing IPE programs. The challenges to initiating or sustaining IPE can be logistical, curricular, and cultural and can be more or less difficult depending on the interest of the leadership and the faculty. In his presentation, Thibault laid out a number of potential obstacles to implementing IPE, each of which has been overcome by at least one of the programs in the examples that follow.
Logistical Challenges
According to Thibault, finding the right timing for IPE and the right match of learners among the professions is a concern for planners, as is student engagement in clinical service experiences. Learners want meaningful assignments with real patient care responsibilities, but providing such enriching experiences is difficult when learners are not available consistently throughout the year. To overcome this particular challenge, workshop speaker Dennis Helling, executive director of pharmacy operations and therapeutics at Kaiser Permanente Colorado Region, devised detailed plans for the continuation of the pharmacy service with or without students. In this way, patient care was enhanced by students and was not negatively affected by their absence.
Another logistical challenge that received significant attention at the workshop was the issue of physical space. Workshop speaker Rose Nabirye from the Department of Nursing at Makerere University in Uganda cited this in her workshop presentation. Because she and her colleagues conduct multiple simultaneous small-group discussions of 10 to 12 students, one
large lecture hall is not adequate. Her discussion groups now fill any and all available spaces, including professorial offices. Nor was this challenge of physical space unique to Uganda. Workshop speaker Steven Chen from the University of Southern California described space as a “huge issue” for him in his work with students in California at the Safety Net Clinics. As Chen explained, “You do not have a lot of room for all these students. We have had to pair up different disciplines and have different focuses at different visits in order to accommodate that problem.”
At the five Department of Veterans Affairs (VA) centers of excellence in primary care education, space has become an institutional issue, according to VA nurse consultant Kathryn Rugen, who spoke at the workshop. She agreed with Nabirye about needing particular spaces for students and not just having them sit in a large room together and listen to a lecture. Specifically, she said, “it has to be an environment where students can have some dialogue and socialize.” This was echoed by Forum member Darla Coffey from the Council on Social Work Education, who reminded workshop participants about the importance of having a “social space” outside of the classroom where learning from other professions takes place through thoughtful reflections. “Without this protected space,” she said, “the most important element of interprofessional education is lost.”
Maria Tassone of the University of Toronto, who spoke at the workshop as the co-leader of the Canadian Collaborative, said that moving from uniprofessional spaces to interprofessional spaces in order to have space to interact is also important for teams working within the practice setting. That idea resonated with workshop speaker David Collier, who directs the Pediatric Healthy Weight Research and Treatment Center at East Carolina University. Collier has found space for clinicians to see patients to be a major issue in his clinic because an initial comprehensive visit could take up to 4 hours. In such situations, working with the manager or others to identify unused office space or to improve the flow of patients, professionals, and students through busy environments like health clinics may help to alleviate space issues—in much the same way as Chen described overcoming the “space” challenge at the Safety Net Clinics.
Curriculum Content
Among the other obstacles to implementing IPE cited by Thibault were knowing the appropriate curricular content and the suitable topics to teach interprofessionally. Another obstacle is knowing how to weave that content into meaningful clinical and community experiences like those set up by Steven Chen at the University of Southern California, which are described in Box 3-1.
As was mentioned previously in the summary of Thibault’s comments,
experiential learning is a critical component of IPE because it is where the imprinting of health professions education takes place. However, imprinting can also take place through a “hidden curriculum” which was identified by a number of workshop speakers. Students may be formally taught to work collaboratively, but within the hidden curriculum, experience educational and health care systems remain mostly siloed. The existence of this hidden curriculum risks sending conflicting messages to students regarding the value of collaboration, said workshop speaker Barbara Brandt from the University of Minnesota. One way to avoid these conflicting signals is to expose students only to well-functioning teams. For example, Brandt described sending students to the Broadway Family Medicine Clinic in North Minneapolis, where they experience a unique culture in terms of both language and behavior. The front desk receptionist leads the staff meeting, and physicians interact fully with nurse practitioners. Although student education is not the primary focus of the clinic, Brandt said, learners internalize the values and behaviors expressed in this nonhierarchical, collaborative environment.
Another technique for dealing with the hidden curriculum was described by workshop speaker Mark Earnest from the University of Colorado. He uses the hub-and-spoke model (described in Appendix D) in which students learn how to work interprofessionally in clinical settings and then return to the university preceptor to discuss their experience. The preceptors tell their students they will learn by negative as well as positive examples of collaboration. A goal of this program, as Earnest described it, is to help keep students focused on the positive examples and to be agents of change to create such environments wherever they go.
Culture
Cultural entrenchment within education and practice remains a significant barrier to collaboration in and across these environments. This was one message from Forum member Warren Newton of the American Board of Family Medicine, who led the small group discussing the initiation of collaborative partnerships. From Thibault, the message was, “We’ve built up cultures that actually reinforce separation, actually sometimes rejoice in separation and in citing differences rather than the commonality that we have across the health professions with a common goal of improving patient care.” Those silos are manifested by poorly aligned calendars, inadequate collaborative space, the perceived lack of time necessary to do interprofessional work, and the need for new models of education, he said. Overcoming these challenges means understanding the different incentives, drivers, and reward systems that exist within the two worlds of education and practice. Once these are recognized, Thibault said, strategies can
be developed to break down the traditional professional silos that value independence over collaboration both within education and practice and between them.
External forces sometimes drive cultural changes from traditional, fragmented, discipline-based curriculums to integrated patient- and problem-based curriculums that emphasize interprofessional education. For example, Jan De Maeseener reported how he and medical faculty colleagues were confronted with a very negative assessment by the accreditation board, which pushed them to adapt IPE approaches. Similarly, Nelson Sewankambo reported being forced into IPE because of external circumstances. Despite a 90-year history of providing siloed education to students at Makerere University in Uganda, he and his colleagues introduced IPE in 2001 because of workforce shortages. “We had no choice,” he said, because “there was a shortage of teachers and health workers in the country. That is why we went into interprofessional education.” In designing the curriculum, Sewankambo worked closely with the Ministry of Health to ensure that graduates entered the workforce with the right set of skills to affect the entire population in addition to the individual communities they served.
IPE innovators around the world may take inspiration from these examples out of Belgium and Uganda and might also consider the idea proposed by Marilyn Chow. She suggested the creation of an entity that is unencumbered by the tradition and bureaucracy of education and health care that could spur a rapid development of new ideas and pilot them through the education and care innovators.
Leadership
Throughout the workshops, an overarching theme was the importance of leadership in bringing about culture change. This point was brought out by Elizabeth Speakman from Thomas Jefferson University (see Box 3-2) and then reiterated by Dawn Forman of Curtin University when Forum co-chair Afaf Meleis from University of Pennsylvania School of Nursing questioned her about the development of interprofessional education at her University. Forman said, “I certainly believe that had it not been for the leadership within the university and also within the Department of Health … that interprofessional education would not have been started.” Forman went on to cite experiences of universities with IPE programs that were discontinued following a change in leadership. “Leadership is absolutely critical,” she concluded.
To determine who can provide leadership and support for IPE, members of the leadership breakout group decided that the first step is to identify the leaders and other stakeholders as well as their relationships to each other and their institutions. The group acknowledged both formal and
BOX 3-1
Steven Chen, Pharm.D.
University of Southern California

Workshop speaker Steven Chen commented in his talk that three settings where he and his colleagues have IPE students are areas that desperately need help and are prime areas for interprofessional education. These include the safety net system, geriatrics, and psychiatry. In the safety net area, he said, resources like space and supplies are extremely limited and there are very few specialists willing to see the underserved. The primary care providers are heavily burdened to provide great care for those patients, adding that he and his colleagues have seen dramatic shifts in the demographics of patients they serve as the economy continues to struggle. Although Chen said they started with minority patients in most clinics, they now see a wider variety of ethnicities in the clinics with whom they partner.
Literacy, culture, and poverty are major barriers to adherence with medications as well as following lifestyle and self-management recommendations. These barriers frustrate even the most competent physicians, who find it impossible to address all of them adequately for the highest-risk patients. As a result, Chen said it is difficult to retain providers because of the high stress level of the safety net environment. Team-based care, where every member of the team provides services at their maximum scope of practice, provides great value in this setting by addressing patient needs and reducing physician workload and stress.
The first of three student programs Chen and/or his colleagues initiated that involve safety net settings is called SHARE or Students Helping and Receiving Education. It is an 8-year program that offers critical services, such as medication reconciliation and smoking cessation classes, through pharmacy student volunteers, but now engages other disciplines. Chen says this work was aided significantly by the Center for Medicare and Medicaid Innovation (CMMI) grant that is allowing them to integrate clinical pharmacy services into a network of safety net clinics during the next 3 years. Services provided through the SHARE program to other safety net clinics are now being developed for the safety net clinic organization supported by the CMMI grant.
The second program Chen described was the University of Southern California (USC) student-run clinic (see Figure 3-2). The difference between SHARE and
the USC student-run clinic, he said, is that SHARE was a student IPE program that was integrated into an existing practice whereas the student-run clinic was created specifically for IPE by students. “This is one of those examples,” said Chen, “of ‘get out of the way and let the students run it’ because they do such a great job.”
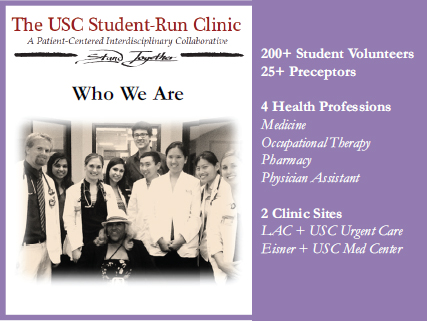
FIGURE 3-2 The USC student-run clinic.
SOURCE: Courtesy of Steven Chen.
Another program that Chen discussed exposes students to team-based care for chronic condition, like asthma. In this example, Chen helps students develop or update asthma education materials that are used to teach a monthly student-run patient education program on asthma management at a safety net clinic. The class is mandated for all patients with newly diagnosed asthma at the clinic and is an integral part of a clinic-wide asthma management program. Students teach about the basic pathophysiology of asthma in simple terms, how to recognize and manage symptoms, what the medications do and how they should be taken, how to use asthma-related devices, and how to measure peak flow. Most patients with very poorly controlled asthma are also enrolled into the pharmacist-run asthma management program. In testing their effectiveness, Chen reported a greater than two-fold likelihood of patients reaching their asthma control goals, as defined by current guidelines, when they are enrolled in the clinical pharmacy program and participate in the asthma education class versus not being involved. Chen attributed the positive results to a combination of hard work by the clinic providers, including the clinical pharmacist, as well as students’ involvement.
BOX 3-2
Elizabeth Speakman, Ed.D., R.N., CDE, ANEF
Jefferson InterProfessional Education Center, Thomas Jefferson University

Although many interprofessional activities were occurring at Thomas Jefferson University prior to the establishment of the Jefferson InterProfessional Education Center (JCIPE), presenter Elizabeth Speakman said, the activities were mainly occurring sporadically among different programs. Speakman acknowledged realizing that many faculty champions would be necessary to make it possible to implement interprofessional education the way the early innovators envisioned. Additionally, a way was needed for this vision to be solidified and coordinated through a particular organization. This was the vision of the university president, she said. In 2007, the JCIPE was developed, based on the president’s vision, to establish such a coordinating center, which was supported by the deans. It was this unified effort that led to the establishment of a standalone center at Jefferson with its own budget. This independent budget, Speakman said, helps the faculty produce some of the IPE activities offered at the university.
Speakman also said that JCIPE is supported by a very robust steering committee which came together to draft the center’s mission and vision. The center has an interprofessional curriculum committee that is headed by the JCIPE but that also includes service providers as well as representatives from library services. All stakeholders from Thomas Jefferson University were invited to come together to review the curriculum being proposed by the committee.
From these reviews it became evident that a framework was needed for the curriculum. In response, the curriculum committee worked on adapting the International Education Collaboration curriculum and came up with four competencies that every Jefferson student would have upon graduation. The next step, which Speakman said she and her colleagues are working on now, is moving toward requiring students to meet these competencies in order to graduate from Jefferson. None of this would have been possible, Speakman said, without the support of the university leadership.
informal levels of leadership and the importance of engaging all leaders as change agents.
Leaders with little IPE experience will require education on what IPE is and the value that it can provide for students, faculty, and, more broadly, the entire health care system. Providing clear and consistent messages, definitions, and evidence is the most effective way to arm the leader with what is needed to advocate for IPE. However, a leader needs to understand that there are different types of evidence. There is initiating evidence used to define the problem, and there is sustaining evidence which is generated continuously to show the ongoing impact being made through IPE.
Those providing the evidence must be cognizant of the different meanings that their data could hold for different stakeholders and be clear about the purpose of the information provided. As Melissa Simon from Northwestern University, the presenter for the leadership breakout group, explained, “There is a flash point. There is a critical mass of the amount of evidence that we build, how visible we become, and what is the economy of scale.” Her remarks were sensitive to the challenges leaders face in having to sort through facts for relevant information. When providing evidence, Simon said, it is best to include specifically how, when, and why—and the context within which—the evidence was obtained. The purpose is not merely to convince, but also to build relationships and connections with leaders that involve patients who can demand change and students who are the leaders of tomorrow.
Simon shared other views expressed by many members of the leadership breakout group, which included several expectations for leaders. Leaders must be permissive, encouraging, directive, and explicit while also delivering resources. Additionally, they must model and enforce accountability among others by promoting and sustaining a culture of teamwork and respect. Members of the group also spoke of leaders’ responsibility for building champions of IPE through scholarships, publications, and dissemination of current IPE activity outcomes and urged that leaders support capacity-building activities, such as leadership training and interprofessional collaboration. This type of leadership capacity building is exemplified in the Canadian Collaborative described in Appendix C of this report. Finally, members of the group spoke of the need for positive assessment and evaluation outcomes in order to more effectively and fluently convince leadership of the importance of IPE.
Faculty Development
In the closing remarks of his presentation, George Thibault focused on the importance of committing time and energy to faculty development in an effort to decrease reluctance about interprofessional education. This
resonated with Nelson Sewankambo, who described how he experienced faculty reluctance to IPE firsthand in 2001 at Makerere University. Initially, he said, faculty were apprehensive about educating students interprofessionally because they themselves were not trained in IPE and understandably felt great discomfort in teaching this way. However, Sewankambo said, many of the faculty members at Makerere who embraced a more holistic approach to health professions education pushed to receive master’s degree–level training so they could better understand health professions education. In turn, he said, those faculty members became the advocates of IPE at the university. J. Lloyd Michener, workshop speaker from Duke University, described experiencing a similar faculty excitement over IPE; once the faculty accepted and understood the elements of interprofessional education, he said, they realized the work was “really fun.”
At the University of Southern California, Steven Chen reported that one of the biggest challenges to developing IPE is getting faculty to understand what other professions do. This has been addressed by hosting a series of seminars and workshops that run throughout the year. All faculty members who participate in their IPE programs are invited to these events as a way of learning about the other professions in their IPE program. Chen added that when he hosts these seminars, he models them after the Health Resources and Services Administration Patient Safety and Clinical Pharmacy Services and the Institute for Healthcare Improvement’s “all teach, all learn” approach.
Gillian Barclay reported that at the Aetna Foundation, the WHO definition of IPE—noted in Chapter 2 in this report—is modified to read “faculty from two or more professions learn about and with each other to enable effective collaboration and improve health outcomes.” In her opinion, if the students can do it, it is important for faculty to also work and learn in the same way.
Because of the critical importance of a trained staff to providing interprofessional education, most if not all of the IPE programs described at the workshop were reported as offering some component related to faculty development. Across Canada, faculty development is an important feature of IPE, and it is designed for clinical as well as educational faculty. The University of Toronto alone has trained more than 700 faculty members in IPE. Although this seems an impressive accomplishment, Maria Tassone put that effort into perspective by noting that the University of Toronto has 5,000 clinicians, and thus a lot of work remains. Appendix D lists some faculty development programs at various universities.
LESSONS LEARNED
George Thibault commented that the Forum members, speakers, and participants attending the workshop represented an incredible wealth of experience. Everybody had his or her own stories to tell and his or her own biases, he said, and a number of important lessons emerged, dating as far back as the earliest experiences with IPE. These lessons can guide future discussions on mainstreaming IPE and can expand opportunities for high-quality interprofessional education and collaboration. Thibault offered six lessons from his own experience, elaborating on each in turn. The lessons were
1. Leadership from the top is essential.
2. Extensive planning is necessary for rigorous experiences.
3. Experiences need to be repeated throughout the educational continuum.
4. IPE must accomplish real work; it is not an end in itself.
5. New technologies can assist in accomplishing goals.
6. A major commitment to faculty development is required.
Leadership from the Top Is Essential
Although the importance of leadership from the top may be a truism that applies to multiple situations, Thibault said, it has been absolutely imperative for success within IPE. Without leadership from the top, the logistical barriers become obstacles that cannot be overcome. Thibault made the point by noting that deans can change schedules, they can change the reward structure for faculty, they can assign time differently, and they can make resources available. He also stressed that the institutions that have gone farthest with IPE have gotten support at the highest level of leadership, including deans, provosts, chancellors, and presidents.
Extensive Planning Is Necessary for Rigorous Experiences
According to Thibault, some of the early encounters in interprofessional education may have been looked at negatively because they were seen as extracurricular and not truly educational. Socialization is an important part of education, he added, but it is not education in and of itself. The classic high school mixer is not an educational experience, for example. Interprofessional educational experiences need to be planned rigorously with clear educational goals in mind, clear metrics, and measured outcomes, he said. They are not casual encounters.
Experiences Need to Be Repeated Throughout the Educational Continuum
Thibault commented that even the most thoroughly well-planned single encounter will not have a lasting impact. Experiences need to be repeated in order to overcome cultural barriers, and they need to be reinforced, given the huge volume of information that all health professions students must learn and experience to become fully developed professionals. If IPE is offered only as an annual event, then the message is clearly given that it is not core. To be core, he said, it must be seen as something that is repeated regularly throughout education.
IPE Must Accomplish Real Work; It Is Not an End in Itself
When the interprofessional educational activity is aligned with real-life situations and challenges, Thibault said, the IPE experience becomes more tangible and applicable to real work. Such an experience has a more lasting and enduring impact and is more valued by learners. Designers of IPE need to look for those opportunities that can only be done or are best accomplished interprofessionally, he said. If the activity does not require collaboration and it does not provide real-life experiences, Thibault said, it should not be called “interprofessional education.”
New Technologies Can Assist in Accomplishing Goals
Thibault said that technology for IPE is just beginning to unlock the possibilities of how learners are learning and will learn differently. It opens up huge possibilities for interprofessional work, he said, as educators become freed from the confines of the fixed classroom and can think in terms of virtual space for education.
A Major Commitment to Faculty Development Is Required
Finally, Thibault commented that most faculties have not experienced IPE or worked across faculty boundaries. As a result, many educators are uncomfortable with teaching interprofessionally because they do not know what to expect with learners of other professions. The enabling technologies for teaching interprofessionally may be unfamiliar to some educators, he stressed, thus causing the educators greater apprehension about engaging in IPE activities. To overcome these challenges, a major investment in faculty development is necessary, Thibault said. For those institutions that have made the investment, IPE has been an incredible source of renewal in terms of energizing the faculty by teaching them new tools, having them be
with students from different professions, and engaging kindred spirits from other faculties. It has proven to be a way of reinforcing the importance of the educational mission and why educators chose to become faculty members in the first place.
Key Messages Raised by Individual Speakers
• IPE is a tool for achieving the triple aim. (Thibault) IPE is about achieving better health outcomes. (Spencer)
• Recognizing the enormous amount of duplication in the content taught in silos is a first step toward cost containment. (Schmitt)
• There are real costs associated with retraining, which could be rethought by educators. (Grundy and Schmitt)
• The hidden curriculum risks sending conflicting messages to students regarding the value of collaboration. (Brandt)
REFERENCES
AHRQ (Agency for Healthcare Research and Quality). 2000. Outcomes Research: Fact Sheet. March 2000. Agency for Healthcare Research and Quality, Rockville, MD. http://www.ahrq.gov/research/findings/factsheets/outcomes/outfact/index.html (accessed June 26, 2013).
Campbell, S. M., M. Hann, J. Hacker, C. Burns, D. Oliver, A. Thapar, N. Mead, D. G. Safran, and M. O. Roland. 2001. Identifying predictors of high quality care in English general practice: Observational study. British Medical Journal 323(7316):784–787.
Frenk, J., L. Chen, Z. A. Bhutta, J. Cohen, N. Crisp, T. Evans, H. Fineberg, P. Garcia, Y. Ke, P. Kelley, B. Kistnasamy, A. Meleis, D. Naylor, A. Pablos-Mendez, S. Reddy, S. Scrimshaw, J. Sepulveda, D. Serwadda, and H. Zurayk. 2010. Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. Lancet 376(9756):1923–1958.
Goni, S. 1999. An analysis of the effectiveness of Spanish primary health care teams. Health Policy 48:107–117.
IOM (Institute of Medicine). 1999. To err is human: Building a safer health system. Washington, DC: National Academy Press.
Joint Commission. 2012. Joint Commission online. June 27. http://www.jointcommission.org/assets/1/23/jconline_June_27_12.pdf (accessed on April 9, 2013).
Levinson, D. R. 2010. Adverse events in hospitals: National incidence among Medicare beneficiaries. Washington, DC: Department of Health and Human Services, Office of the Inspector General.
Levinson, D. R. 2012. Hospital incident reporting systems do not capture most patient harm. Washington, DC: Department of Health and Human Services, Officer of the Inspector General.
Mukamel, D. B., H. Temkin-Greener, R. Delavan, D. R. Peterson, D. Gross, S. Kunitz, and T. F. Williams. 2006. Team performance and risk-adjusted health outcomes in the program of all-inclusive care for the elderly (PACE). Gerontologist 46(2):227–237.
Shortell, S. M., J. E. Zimmerman, D. M. Rousseau, R. R. Gillies, D. P. Wagner, E. A. Draper, W. A. Knaus, and J. Duffy. 1994. The performance of intensive care units: Does good management make a difference? Medical Care 32(5):508–525.
Stevenson, K., R. Baker, A. Farooqi, R. Sorrie, and K. Khunti. 2001. Features of primary health care teams associated with successful quality improvement of diabetes care: A qualitative study. Family Practice 18(1):21–26.
WHO (World Health Organization). 2011. Global status report on noncommunicable diseases 2010. http://www.who.int/nmh/publications/ncd_report2010/en (accessed March 22, 2013).
WHO. 2013. Deaths from noncommunicable diseases. http://www.who.int/gho/ncd/mortality_morbidity/ncd_total/en/index.html (accessed March 4, 2013).
Wu, S., and A. Green. 2000. Projection of chronic illness prevalance and cost inflation. Santa Monica, CA: RAND Corporation.


















