5
Interprofessional Education Within the Health System
Summary: Interprofessional education (IPE) is part of a broader system of health and education. This chapter attempts to describe how IPE fits into the continuum of these systems. Examples of IPE that span education and practice are provided from the Department of Veterans Affairs (VA), the University of Virginia (UVA), and Kaiser Permanente. These examples led participants to question whether there are high-functioning collaborative practices that do not currently engage students but that could be opportunities for learners to better understand the values around high-functioning teams and collaborations. Vermont’s Blueprint for Health was one example of such an opportunity that is described in this chapter. Following this description, there is a discussion of important health care issues involving workforce development and the expansion of the ethnic and cultural diversity of health providers and workers through IPE. The chapter closes with a discussion on the effective use of funds in IPE and in health care to lower costs while improving the value and the quality of care for patients and their caretakers, who are at the center of the health care system.
In her role as co-chair of the workshop, Forum member Lucinda Maine of the American Association of Colleges and Pharmacy described the model for continuous improvement in clinical education and practice that was developed by the Forum and planning committee member Malcolm Cox, from the VA (see Figure 5-1). In this model, in which educational reform and interprofessional practice (IPP) are inextricably linked, the patient is at
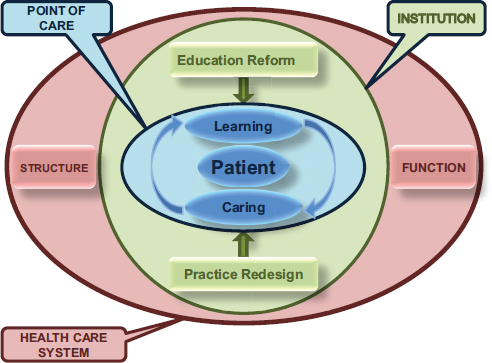
FIGURE 5-1 Patient-centered model for continuous improvement in clinical education and practice.
SOURCE: VA, 2012 (courtesy of Malcolm Cox).
the center of a clinical microsystem (“point of care”) surrounded by a positively reinforcing learning and caring feedback loop. The model illustrates the fact that, collectively, many such microsystems of clinical care and education are embedded in health care systems (“institutions”). According to Cox, education reform and practice redesign are continuously interacting, so that changes in one—by way of the learning and caring feedback loop— will inevitably influence the other. Cox explained that each institutional mesosystem is, in turn, embedded in the overall health care macrosystem (“health care system”). And at each level of this complex adaptive system, myriad processes are subject to analysis and improvement.
This networked system of education and practice was the focus of many presenters at the workshop. One such presenter was Kathryn Rugen from the VA, who reported that the goal of the VA’s centers of excellence in primary care education is to develop and test innovative structural and curriculum models that foster the transformation of health care training from the professional silos to interprofessional team-based education and clinical care delivery.
She said that the VA has been providing interprofessional team-based
care for decades in areas such as geriatrics and palliative care but have not officially declared it as such. Because the VA has the largest medical education and health professionals training program in the United States, academic leaders there recognized the opportunity this creates for IPE. They decided to name their previously undefined model of interprofessional team-based geriatric and palliative care, and expand it to primary care training. According to Rugen, this led to what are now known as the VA centers of excellence in primary care education. The core requirements for these centers include co-direction by a physician and a nurse practitioner; joint sponsorship and engagement with academic affiliates; integrated, interprofessional teams in the workplace; and a commitment from trainees that 30 percent of their academic clinical training will be at the centers of excellence. Rugen provided the following list of primary learners:
• Physician resident trainees: internal medicine PGY 1, 2, 3, chief resident; family medicine PGY1; psychiatry
• Nurse practitioner trainees: pre-master’s, pre-doctorate of nursing practice, post-master’s fellows
• Postdoctorate pharmacy residents
• Postdoctorate psychology fellows and psychology interns
Besides these primary learners, there is also some engagement from the social work and nutrition areas, bachelor’s degree nursing students, medical students, podiatry, and physician assistants.
Rugen said that each center balances formal IPE instruction with workplace learning and reflection that is both inter- and intraprofessional. Table 5-1 provides details about these educational strategies which use formal instruction within developmentally appropriate learning activities to support workplace learning and purposeful reflective practices. The table also lists, for each educational domain, examples of evaluation methods employed by the VA that measure what works, for whom, under what circumstances, and why.
Another program, described by workshop speaker Valentina Brashers from UVA, is similarly focused on the education-to-practice continuum. The program strives to provide clinically relevant IPE. According to Brashers, this education is required and fully integrated across the learning continuum and assessed longitudinally, it is associated with a commitment to rigorous research and dissemination of results, and it is intended to bridge the gaps between education, patient care, and patient outcomes.
The IPE innovators of the program, of which Brashers is one, developed what they call the Collaborative Care Best Practice Model to support the creation of their interprofessional education experiences. This model is based in clinical guidelines that address areas of need in the health system
TABLE 5-1 VA Centers of Excellence Educational Strategies and Evaluation Methods
| Educational Domain | Definition | Activity Examples | Evaluation Examples |
| Shared decision making | Care is aligned with the values, references, and cultural perspective of the patient; curricula focus on the communication skills necessary to promote patients’ self-efficacy. |
• Ottawa Shared Decision • Three-Part Longitudinal • Motivational Interviewing |
• Mini-Clinical Evaluation Exercise • Decision Support Analysis Tool • Dyadic OPTION Scale • Learner Perception Survey– |
| Sustained relationships | Care is designed to promote continuity of care; curricula focus on longitudinal learning relationships. |
• Home visits • “Lost Opportunities” |
• Modified Continuity of Care Index • Qualitative interviews • Learner Perception Survey– • PACT continuity encounter |
| Interprofessional collaboration | Care is team-based, efficient, and coordinated; curricula focus on developing trustful, collaborative relationships. |
• University of Toronto Centre • Huddle-Coaching Program |
• Longitudinal semi-structured • Team Development Measure • Readiness for Interprofessional |
| Performance improvement | Care is designed to optimize the health of populations; curricula focus on using the methodology of continuous improvement in redesigning care to achieve quality outcomes. |
• Curriculum of Inquiry • Panel Management • All sites looking at emergency |
• Clinical outcomes • Quality Improvement Knowledge |
SOURCE: Department of Veterans Affairs.
for improved teamwork, she said, adding that expert interprofessional panels choose the guidelines and develop cases and checklists of behaviors that are essential for adequate implementation of those guidelines. The checklists fully integrate both the profession-specific and the interprofessional skills for optimal guideline implementation. From these collaborative care best practices models, Brashers said, she and her colleagues can create not only clinically relevant interprofessional experiences, but also assessment opportunities. They call their collaborative-behavior observational assessment tools—which are used to assess students during interprofessional teamwork—OSCEs, or objectively structured clinical examinations. By creating tools and experiences with this method, Brashers said, it is possible to use the same process to adapt tools appropriately for the target learner. In this way the model used to assess undergraduate students is simpler than that used for residents and graduate nursing students, she said, whereas fellows, clinicians, and faculty receive what she called the “gold standard model” of assessment.
Brashers said that this process embeds IPE in a clinical base because the skills needed for interprofessional collaboration around a crashing sepsis patient are somewhat different from the skills necessary for appropriate interprofessional collaboration around an end-of-life discussion with a family member. Tailoring IPE in this way provides opportunities to develop interprofessional experiences and assessment tools that address specific patient populations, illness experiences, and care settings. The advantages to using this method, she said, are that it provides very specific and measurable learning objectives to work with, it integrates profession-specific skills with interprofessional learning so that students do not see a divide between what they need to know and how they need to deliver that care, and it establishes IPE as a core element of the clinical and clerkship experiences of students.
Although both UVA and the VA provide good examples of the continuum between education and practice, workshop speaker Dennis Helling from Kaiser Permanente Colorado Region drew the audience’s attention to the second workshop objective: “identify and examine academic/practice partnerships that demonstrate purposeful modeling to advance team-based education and collaborative practice.” After reading this objective, Helling said, “I think that statement and objective makes a huge assumption that there are critical numbers and access by universities to high-performing, interprofessional teams delivering interprofessional health care.” But, he said, that is not always the case. He added that while there must be academic-based training on interprofessional education, the course work should be reinforced with real-life experiential practices. Helling spent some time explaining how he came to this opinion, a discussion that is captured in Box 5-1 along with a description of some of Helling’s work exposing pharmacy students to high-functioning teams at Kaiser Permanente.
BOX 5-1
Dennis Helling, Pharm.D., D.Sc., FCCP, FASHP
Kaiser Permanente Colorado Region, Department of Pharmacy

During the first 19 years of his career, Dennis Helling was an academic chair for clinical pharmacy and an associate dean for clinical affairs at the University of Iowa and then at the Texas Medical Center. He was very active in building academic programs to locate in what he hoped would be collaborative IPP sites. Often Helling felt stressed when attempting to find strong IPP sites that mirrored the principles and values he taught in the classroom about IPP. When he put the students in sites that provided sub-optimal interprofessional experiences, sometimes what he told the students in class did match up with what they found in the practice environment. It was then that Helling made a personal career decision to, as he said, “walk the talk.”
IPE for Workforce Development
Sarita Verma and Maria Tassone are co-leads of the Canadian Interprofessional Health Leadership Collaborative, which is described in Appendix C. They explained the origins of IPE in Canada, which was engineered specifically to meet the health care needs of Canada. Verma began by saying that, starting in 2002, the famous Romanow commission recommended that educational programs be changed to focus on more integrated, team-
Helling left full-time academia and joined Kaiser Permanente in Denver, Colorado, 20 years ago to focus on building an advanced collaborative practice for pharmacists. In testing this collaborative practice model—on how pharmacists, physicians, nurses, and others could deliver superior care together while Pharmacy Doctorate students, residents, and fellows actively participate—Helling demonstrated the positive return on investment of pharmacy services through a rigorous evaluation of the model.
Helling said that the department where he works includes roughly 500 pharmacists and is the largest employer of pharmacists in the state of Colorado. Furthermore, he said, his institution is the largest provider of advanced practice experiences in the state of Colorado, working both with the University of Colorado and Regis University. Helling spoke with representatives from both of these universities to consider what an ideal rotation or advanced practice experience would look like. Based on these discussions, Helling determined that, ideally, the IPE experiences would increase the students’ self-directed learning, their independence, and their self-confidence. They would also provide benefits to the preceptor site that would exceed the cost of the precepting. In essence, Helling said, “we would add value to the organization and to our patients.” And, he added, he and his colleagues would prepare students so they were “team ready” after they finished their advanced practice experience at Kaiser.
Helling next described having students placed in each of 27 areas, including applied pharmacogenomics, travel clinics, neurology, oncology, behavioral health, geriatrics, and endocrinology. According to Helling, his department can offer opportunities to students in each of the practice sites that have clinical pharmacy specialists because the medical group and pharmacy came to an agreement that the medical group needed clinical pharmacy services to advance access, quality, and affordability.
In summarizing his talk, Helling said that he and his colleagues feel that (1) students can be trusted to work independently with supervision, (2) having an opportunity to make an impact is important, (3) students help preceptors expand their capacity and ability, and (4) an organized service program that is built on a strong, IPP prepares students to be team ready.
based approaches to meet the health care and service delivery needs of the Canadian population. The Accord on Health Care Renewal, which focuses on accessibility, quality, and affordability of care, is one agreement between the provinces and the federal government that deals with IPE.
In the mid-2000s, Verma said, an advisory committee of high-level political leaders and deputy ministers was formed that drove innovations in health care in the Canada’s 13 provinces and territories. But the seminal moment for IPE was in 2004 when Health Canada provided funding for
projects that launched the activities that led to health professions education reform in Canada.
Continuing the presentation, Tassone reported that IPE for collaborative patient-centered care projects originally received more than 20 million Canadian dollars over the 4 years from 2004 to 2008 to catalyze this work and to strengthen these linkages. What happened, according to Tassone, is that the early projects, about 20 of them, created the country’s national exemplars in the three following areas:
1. Educational and instructional curricular activities and IPE courses,
2. Continuing professional development focusing on enhancing collaborative competencies, and
3. IPP-based learning experiences.
The first area, Tassone said, centers on curriculum activities that provide students opportunities to engage in a longitudinal curriculum. The second area incorporates a professional development perspective. A number of programs across the country started by training educators in how they can teach and model collaboration. Tassone said that those programs are increasingly being extended in order to partner with collaborations in the practice environment. There are now roughly equal numbers of educators, practitioners, and practice leaders learning these competencies, which not only relate to how they are teaching students but also to how they are behaving in practice settings. Tassone said she believes that the third area of focus resonates most with the students. This area involves IPP-based learning and includes structured experiences in which students come together to work on quality-improvement projects within a hospital or in a community setting. As an example of this experiential learning, Tassone pointed to the health mentor programs offered across the country that allow students to shadow patients with chronic diseases.
Tassone also commented on another important piece of work involving an organization that was funded and promoted by Health Canada, the Canadian Interprofessional Health Collaborative. This is a voluntary organization with a very small secretariat that provides Canadians with an opportunity to collect and distill some of the local examples and IPE innovations across Canada while also looking at work that is happening beyond the Canadian borders.
In her closing remarks, Tassone said that she thinks IPE is “a common theme across all of the professions and it’s an enabler of all the things that are really important to us in health education and health care quality, safety, and sustainability of the health care system.”
Similar to Tassone and Verma, Sanjay Zodpey is a Forum member heading the Forum’s Innovation Collaborative. His Collaborative is out
of the Public Health Foundation of India in New Delhi that is designed to build the capacity of health professionals in India by establishing a cluster for health workforce planners with a focus on the education of health professionals. One objective of their work is to identify the interdisciplinary health care leadership competencies relevant to medical, nursing, and public health professional education in India. Once these competencies are identified, Zodpey said, his collaborative plans to develop and pilot an interprofessional training model for physicians, nurses, and public health professionals to develop the leadership skills relevant to the 21st-century health systems in India.
In Uganda, workshop speaker and Innovation Collaborative lead Nelson Sewankambo worked with colleagues to introduce IPE in 2001 because there was a shortage of teachers and health workers in the country. In designing the IPE curriculum for Makerere University, Sewankambo worked closely with the Ministry of Health to ensure that its graduates entered the workforce with the right set of skills to affect the entire population and community they are trying to serve. A description of the Indian and the Ugandan innovation collaborations and how their collaborative work relates to the Global Forum can be found in Appendix C.
IPE and the Industrialization of Health Care
Workshop speaker Rosemary Gibson from the Archives of Internal Medicine suggested that the challenges facing IPE are related to the broader health care system in which it is operating. Considering the impact of the system on IPE, she addressed what she refers to as the “industrialization of health care,” which has led to a system that values health as a commodity. She noted that within this culture patients stand a high risk of diminished safety and care.
Before providing comments on system issues related to IPE, she shared her experience of mainstreaming palliative care into the health care system as an example of a promising interprofessional enterprise. In 1995, a major study showed how poorly the U.S. health care system takes care of people at the end of life (SUPPORT Investigators, 1995). In response, the Robert Wood Johnson Foundation, where Gibson was working, made $250 million in investments to address end-of-life issues. Palliative care teams were assembled in a number of hospitals with these funds that consisted of physicians, nurses, pharmacists, clergy, and volunteers working together to care for seriously ill patients at the end of their lives. The palliative care model developed in this effort has been considered a success by those working in palliative care, with 1,500 hospitals employing palliative care teams in 2012. Furthermore, the American Academy of Hospice and Palliative
Medicine now holds its meetings jointly with hospice and palliative nurses, which Gibson called a giant leap forward.
Fifteen years after development of the palliative care teams model, Gibson said that while improvements in care have been made, what has been accomplished is putting “palliative care teams out there in rowboats to rescue people from the rising waters of the medical–industrial complex, but they are not able to stop those rising waters.” As other speakers had mentioned, culture affects IPE, and the culture of the industrialization of health care definitely impacts care of patients.
Gibson made a few observations about that industrialized health care system and what it means for IPE and team-based care. She suggested that although more drugs and devices are being pushed into the system, conversation is being driven out, particularly in the inpatient setting. The system is minimizing time to talk to patients. However, the palliative care teams are an exception, and some lessons can be learned from models that have been able to work within the industrialized health care system. Gibson also suggested that such a system operates with high volume and overtreatment and is continuously being pushed to operate faster. “I’m sure you all saw the study of burnout among 46 percent of physicians, particularly emergency room physicians and internal medicine doctors,” she said, referring to a 2012 study by Schattner. “The ones that did not report as much burnout were those taking care of people at the end of life.” Gibson suggested that such burnout is a result of the industrialization of the health care system.
Considering the characteristics of the industrialized health care system, Gibson asked how IPE and teams can be designed to survive and thrive in this system. How will a team’s function be communicated to patients in terms of accountability and individual identity within the team? Gibson suggested that the development of highly functioning teams will depend on the quality of the system in which these teams perform. As teams are being set up, efforts need to be made to create a system in which teams can function and thrive. She thinks this can be and is being done; however, an understanding of the parameters is needed within which the teams can work productively. Her suggestions were to “create those teams, make them work, but protect them and create these boundaries around them so they are preserved, so they can function, and do as they’re supposed to do, while at the same time we figure out about this bigger picture, big industrial health care issues that I think we’re all facing.”
Collaborative Practices for IPE Experiences
The presentation by Dennis Helling led Forum and planning committee member George Thibault to ask whether some health professions other than pharmacy might take advantage of the strong collaborative environment set
up by Kaiser Permanente. Although the question was posed to Helling, it was also relevant to other speakers, such as Craig Jones, who presented an excellent example of a collaborative practice during the workshop. This example, described in Box 5-2, is the Vermont Blueprint for Health, where Jones is the executive director. Another example of a practice environment that could be used for interprofessional education came from David Collier, who directs the East Carolina University Pediatric Healthy Weight Research and Treatment Center. Given that obesity is a complex bio-psycho-social disease, Collier said, the best treatment and prevention modalities are those that are interprofessional. According to Collier, obesity research and treatment offers an excellent environment for IPE. Collier said that his clinic seeks to bring many services together so that patients can see all the services at the same time; then the different health professionals work together to develop a plan that best fits the needs of a patient and his or her family. The professional expertise represented in the clinic includes pharmacy, physical therapy, nutrition, public health, periodontics, psychological and behavioral counseling, medicine, and nursing.
David Krol of the Robert Wood Johnson Foundation, who represented the foundation at the workshop, saw Collier’s work as an opportunity not just to expose students to team-based care of pediatric obesity, but also to give students the chance to engage in advocacy on issues of community policy, such as the issue of vending machines in schools. Collier agreed with Krol on the importance of student engagement in community efforts against obesity. He said that his team does mentor students and facilitate student-run activities in nutrition education and physical activity promotion in communities. However, he added, sustaining the student-initiated programs is one challenge he has not yet overcome.
Forum member Gillian Barclay from the Aetna Foundation, a member of the reflection panel addressing principles and gaps in IPE, reminded the workshop participants of the Community-Oriented Primary Care movement which dated back to the 1970s and 1980s. This movement, she said, was intended to improve community health by employing principles from public health, epidemiology, and primary care (IOM, 1983; Longlett et al., 2001). A number of attempts were made during this movement to have the community intersect with academia. Barclay suggested that the lessons learned from those strategies and experiences would be extremely relevant to IPE. She then challenged the audience to think beyond the walls of the clinical environment. How, she asked, might IPE be part of population and community health in a way that could integrate health and wellness with community-based social support services? Barclay talked about the difference it would make to students’ educational experiences if they were exposed to interprofessional care coordination in community settings that intersect with primary care.
BOX 5-2
Craig Jones, M.D.
Vermont Blueprint for Health

Craig Jones is the executive director of Vermont’s Blueprint for Health, which is one of the state-led initiatives seeking to transform health care delivery throughout Vermont. By acting as an agent of change, Jones said, Blueprint for Health is creating a comprehensive community system of health from the current system, which contains multiple providers, practices, and insurers (Department of Vermont Health Access, 2012).
One method that Blueprint for Health is using to achieve this goal is encouraging practices to become patient-centered medical homes (PCMHs), also known as advanced primary care practices. Jones described the National Committee for Quality Assurance’s established standards and criteria for practices seeking to become patient-centered medical homes and the Blueprint for Health’s role in developing a formal method of helping practices in Vermont prepare to be scored
Having funded some of this work when she was at the W.K. Kellogg Foundation, Barclay was able to speak to the workshop participants about the difficulties faculty members faced in engaging communities, especially members of the medical faculty who wanted to work with faculty members from other disciplines to focus on community needs. “It really affected their tenure or their ability to achieve tenure,” she said, because such collaborative work may not lead to the sorts of papers and publications that could advance academic careers.
against these standards. After a practice has prepared, it is scored by an independent team from the University of Vermont; the scoring is done by a different team in order to maintain objectivity because the payment that the practice will eventually receive from insurers is based on this score. With the multi-insurer payment reforms, Jones said, all insurers share the costs and make a per-person, per-month payment that is directly proportional to the score received; thus, this additional payment represents a quality payment on top of the fee for services.
Blueprint for Health has gone to even greater measures to provide coordinated support to the citizens of Vermont, Jones said. A PCMH could be improving access, communication, and guideline-based care, he explained, but still lack the true multidisciplinary support that people need. To supplement the PCMH, Blueprint for Health asked insurers to support community health teams. These locally designed, locally organized, and integrated multidisciplinary teams work to bridge the gap of support for the general population. Although case management traditionally has been available for those with specific conditions and those who are very sick, Jones said, there was a lack of interprofessional and multidisciplinary support for the general population that the community health teams seek to fill.
Jones said that some insurers have added more professionals specialized in case management among high-risk populations to their community health teams. For example, Medicare now pays for support and service at home (SASH) teams, which are coordinators that work at the household level in publicly subsidized housing in especially high-risk Medicare populations. These SASH teams, Jones said, provide in-home supports, helping with daily activities, safety, and assessment, and then link back with the community health teams to streamline care.
Jones said that the work of the Vermont Blueprint for Health is founded on trust. Although it took time for Blueprint for Health to build the trust of those they serve, part of that trust was developed through the community teams which hired health educators who live and work within the communities they serve. Jones said that this is critically important for gaining the trust of the patients being served.
IPE for Diversity Opportunities
Gillian Barclay suggested to audience members that, when educating students in interprofessional environments, they consider those opportunities that go beyond health care and that could contribute to reducing racial and ethnic inequities in health. For example, when Jack Geiger was working in rural Mississippi in the 1960s, he saw the built environment as a contributor to poor patient outcomes, so he created an IPP that involved those sectors in the built environment that could help improve nutrition. Aetna Foundation is funding some of the evaluation measures within this unique IPP to see how the farmers and farmers markets, physicians, managers, and chief executive officers of these community health centers develop an inter-
professional process to improve the health outcomes of patients and their communities. According to Barclay, this is the sort of culture shift to which students should be exposed. However, it is not enough to get students from different professions together; it is also important to pay close attention to race and ethnicity, looking closely at community needs and building the interprofessional training on those needs.
Melissa Simon from Northwestern University, who participated in the workshop, emphasized the opportunity that IPE brings for increasing diversity not just in professions, but also in race, religious background, sexual orientation, and other factors. This discussion resonated with the Forum member Beverly Malone, who pointed out that the main diversity issue being discussed at the workshop was differences among professional groups. Adding a consideration of color, race, and underrepresented groups, she said, makes the conversation much more complex. Although Malone said she was not sure how to weave the complex issues of diversity into the discussions and the fabric of interprofessional education, she said she felt strongly that members of the Forum need to address such issues before it is too late.
Health Disparities
The United States spends more per capita on health care than any other developed nation, yet, in comparison, Americans have shorter lives and poorer health, according to a recent report by the Institute of Medicine (2013). In looking at the U.S. health care spending curve (see Figure 5-2), small-group leader Thomas Feeley of the MD Anderson Cancer Center pointed out that U.S. spending on health care rose rapidly from the 1960s to today, when it is a total of $2.8 trillion, and that U.S. spending is projected to increase even further, to $4.6 trillion, by 2020. The United States now spends more than $8,000 per person on health, which is double the spending of the United Kingdom and Canada and more than 60 times that of any African nation (OECD, 2012). However, as was pointed out by workshop speaker Paul Worley from the School of Medicine at Flinders University, Australia, what is lost in these statistics is that spending on health is not uniform in developed countries. In his presentation, Worley cited the work of Michael Marmot (2005), which notes that there are socioeconomic disparities in health outcomes even within the richest cities of the world. A disparity in spending and in health outcomes has also been reported in the United States (Bustamante and Chen, 2011), although poor health outcomes may not result only from disparities in health care spending (Lê Cook and Manning, 2009).
Forum and planning committee member Jan De Maeseneer from
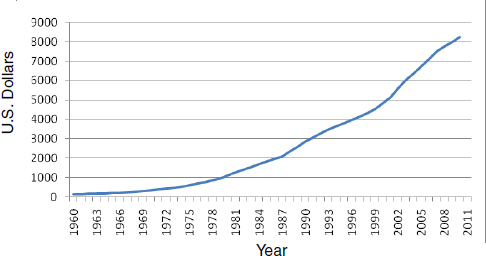
FIGURE 5-2 Mean per capita expenditure on health in the United States: 1960–2011.
SOURCE: OECD, 2012.
Ghent University in Belgium made an important point concerning the situation in sub-Saharan Africa, which is quite different from that of the United States. The Abuja Declaration of 2001 committed governments to spending at least 15 percent of their annual budgets on improvements to the health sector, De Maeseneer noted. However, on average, southern African nations today spend less than 3 percent of gross domestic product on health (World Bank, 2011). Given this stark contrast, Feeley—who led the breakout group on cost—and De Maeseneer agreed that it is appropriate to reframe the focus to reducing health care costs in areas where spending is excessive and that increased spending on health should be the focus of underserved populations. De Maeseneer and Feeley suggested reframing the discussion in terms of improving the “value” of health care. In this way, there is a balance between costs and outcomes, so an ideal health care system improves value when it improves outcomes without increasing cost. When costs are reduced, Feeley said, the reduction does not impair outcomes; such outcomes focus on the patient or the person and take into account what patients think are important outcomes in their care.
Effective Use of Funds in IPE and Health Care
Paul Grundy, who is the director of healthcare transformation at IBM, offered the perspective of an employer of health professional graduates. IBM is the largest corporate employer in Vermont, he said, and having worked closely with both a Republican and a Democratic governor, Grundy
said he and his colleagues at IBM understand that a healthy workforce exists only within a healthy community. As a result of IBM’s holistic care, he said, the company’s trend line is down 11 percent, while trend lines are up 36 percent across the country. He attributed this success to IBM’s effective, team-based, person-centered care. For example, when an IBM employee is diagnosed with diabetes, a care-coordinator from the employee’s medical home exercises with the employee and educates him or her on proper food selection at local supermarket. Although the example Grundy pointed to was in Vermont, he was quick to add that similar care teams have been established in other states, such as Minnesota and North Carolina. These PCMHs were started by IBM and other organizations in 2006, and, as Grundy emphasized, this model is premised on greater access to primary care leading to healthier populations and decreased spending on costly treatments. The approach is team-based and patient-centered, and, according to the Agency for Healthcare Research and Quality, the team of providers cares for all of a patient’s physical and mental health care needs from prevention and wellness through chronic care (AHRQ, 2012). At the close of his presentation, Grundy strongly encouraged educators to expose health professions students to cost-effective, collaborative care models like the PCMHs so that job applicants will be ready to begin work as a team and will not require 3 to 4 years of retraining to get them to become effective collaborators and team members. Also, he said, learning from cost-effective collaborative care models will help break the cycle of overspending that wastes billions of dollars every year in the United States (IOM, 2013).
Forum co-chair Afaf Meleis of the University of Pennsylvania School of Nursing questioned speakers who use IPE as an educational innovation to see whether they found IPE in education or team work in health care to be a financial burden or a cost savings. She also asked if there are ways by which educators and health professionals could deliver quality of care and IPE education economically.
Workshop speaker Elizabeth Speakman from Thomas Jefferson University began her response to Meleis’s question with an example. She said that at some point the deans at her institution complained that faculty were spending large amounts of time with IPE. As a result, Speakman said, her institution now takes full advantage of existing IPE experiences such as the Disposition Dilemma in Rehabilitation Medicine and team-based rounds in surgery. By bringing the student to what is already taking place, Speakman said, the work is more cost-effective than bringing a new team together and having the faculty spend time developing the experience.
Workshop speaker Carla Dyer from the University of Missouri agreed with Speakman and added that when she and her colleagues work on their Achieving Competence Today program with their integrated residents, they ask department chairs which faculty members might be available for IPE
training. They often stress a preference for faculty members who are new to the institution or who are early faculty who are in need of some quality improvement education. According to Dyer, a chair is asked to give protected time for the roughly 8 hours required for training over the course of 3 months. In return for this investment, the faculty members develop relationships with new types of health professional students and obtain an additional skill set that can be applied to their own clinical setting. Thus, Dyer said, everybody benefits.
The third speaker in the session, Dennis Helling, also emphasized the need for the work to be a “win-win” in terms of finances. He commented on the tension that exists between very active practice sites and academic institutions wanting to put students there. Creating and maintaining a learning environment in a practice setting takes time that can slow the pace of a busy team. It also takes a lot of time to coordinate all the students, and this draws preceptors away from other work. In making the student experience cost effective and thus justify the time spent preparing the experience, Helling explained that sometimes students pay for the advanced practice experience; other times funding is used that supports residents, research fellows, or a joint faculty position in their unit. Financial support and time are very real issues when delivering large numbers of advanced practice experiences said Helling.
In his report back to the participants about the breakout group discussions he had led on lower cost, Thomas Feeley talked about the “value proposition” in health care. This refers to a balance between health outcomes and dollars expended, and those outcomes need to be patient-centered outcomes. He advised educators and health providers to better understand what the patients think are important outcomes in their care, and then he described the framework change that he proposed to focus on for improving outcomes and quality while decreasing cost.
Feeley continued his report by describing his group’s discussions based on the five areas of innovation noted in first objective of the breakout group session: curricular innovations, pedagogic innovations, cultural elements, human resources for health, and metrics. In the case of curricular design, Feeley said, health economics and quality improvement could be taught more broadly. The curriculum might also provide better critical and systems thinking, better communication skills, and better information and knowledge about information technology.
For pedagogic innovations, Feeley felt that simulation has tremendous appeal. There are some barriers, such as finding experienced staff, creating realistic scenarios, and general acceptance by educators, but regardless of the barriers, he said, simulation is generally thought to be an extremely important tool for interprofessional education. Another pedagogic innovation Feeley noted was the greater engagement of nonacademic health care
schools, a step that could be cost-effective. The partners might include community colleges and various nontraditional partners that could influence IPE with their unique perspectives, leading to breakthrough innovations. Feeley said that such innovative ideas are appearing already with social media, gaming, and engineering. One other possible pedagogic innovation would be for interprofessional grand rounds to receive a greater focus than the traditional siloed grand rounds.
In the area of culture, Feeley said there appears to be a disconnect between what educators view as needed in the health care workforce and what providers feel they need. Feeley identified learning opportunities to build the workforce from such things as task sharing and by applying experiences from the military, which has always focused on cost-effective, high-quality care. Feeley was quick to point out that task sharing is distinct from task shifting, which is very important in the cost discussion. Almost every time there is a cost discussion in the United States, it involves who can do the best job at the lowest cost, he said, but the responsibility for high quality is not shifted from one to another. Quality is a responsibility that needs to be “shared” among all health workers, regardless of the remuneration provided for accomplishing the task. Adding to the human resources comments, Feeley asked how people other than health professionals, such as patients, caregivers, volunteers, aides, and clerks, can be included in the conversations about what is needed to provide high-quality, lower-cost health and health care.
Parenthetically, Feeley said, patients in the United States are not engaged in the cost of their care, and that is a huge problem. It is equally important to find better definitions of cost and of whose cost is being described—the provider, the payer, government, or the patient. This leads to the notion of metrics. According to Feeley, measurements are often described in terms of money or dollars, but metrics could also include human values that are important to patients. Also, he said that data systems, which are critical for measurement, are incredibly deficient.
There is much energy and optimism, Feeley said, but not much proof that IPE improves values or that it is the right starting point in health care. Obtaining such proof may require rethinking who is on the team (i.e., patients, caretakers, etc.) and how health care is structured. Given that prevention and early detection will lower costs, Feeley said, how might a system transition from health care to one that ensures better health?
In closing, Feeley acknowledged that many provider organizations and many governments are looking at controlling costs. He also encouraged providers and educators to better educate the public about health costs. “It is safe to talk about costs,” said Feeley, “and we need to all address how we do more with less.”
Key Messages Raised by Individual Speakers
• Education reform and practice redesign are continuously interacting. (Brashers, Cox, Helling, and Rugen)
• Course work in IPE must be reinforced with real-life experiential practices. (Brashers, Helling, Rugen, Sewankambo, Tassone, and Verma)
• IPE could be part of a population and community health system that could integrate health and wellness with community-based social support services. (Barclay and Feeley)
• IPE brings opportunities for expanding diversity not just in professions but also in race, religious background, and sexual orientation. (Malone and Simon)
• An ideal health care system improves value when it improves outcomes without increasing cost. (De Maeseneer and Feeley)
REFERENCES
AHRQ (Agency for Healthcare Research and Quality). 2012. Patient centered medical home resource center. http://www.pcmh.ahrq.gov/portal/server.pt/community/pcmh__home/1483/pcmh_defining_the_pcmh_v2 (accessed March 4, 2013).
Bustamante, A. V., and J. Chen. 2011. Physicians cite hurdles ranging from lack of coverage to poor communication in providing high-quality care to Latinos. Health Affairs 30(10): 1921–1929.
Department of Vermont Health Access. 2012. Vermont Blueprint for Health 2011 annual report. Williston, VT: Department of Vermont Health Access.
IOM (Institute of Medicine). 1983. Community oriented primary care: New directions for health services delivery. Washington, DC: National Academy Press.
IOM. 2013. Best care at lower cost: The path to continuously learning health care in America. Washington, DC: The National Academies Press.
Lê Cook, B., and W. Manning. 2009. Measuring racial/ethnic disparities across the distribution of health care expenditures. Health Services Research 44(5, Pt. 1):1603–1621.
Longlett, S. K., J. E. Kruse, and R. M. Wesley. 2001. Community-oriented primary care: Critical assessment and implications for resident education. Journal of the American Board of Family Practice 14(2):141–147.
Marmot, M. 2005. Social determinants of health inequalities. Lancet 365:1099–1104.
OECD (Organisation for Economic Co-operation and Development). OECD health data 2012—frequently requested data. http://www.oecd.org/els/health-systems/oecdhealthdata2012-frequentlyrequesteddata.htm (accessed March 4, 2013).
Schattner, E. 2012. The physician burnout epidemic: What it means for patients and reform. The Atlantic. http://www.theatlantic.com/health/archive/2012/08/the-physician-burnout-epidemic-what-it-means-for-patients-and-reform/261418 (accessed March 4, 2013).
SUPPORT Investigators. 1995. A controlled trial to improve care for seriously ill hospitalized patients. JAMA 274(20):8.
World Bank. 2011. Global economic perspectives regional annex: Sub-Saharan Africa. http://siteresources.worldbank.org/INTGEP/Resources/335315-1307471336123/7983902-1307479336019/AFR-Annex.pdf (accessed March 4, 2013).




















