4
Public Health and Medical Care Systems
One explanation for the health disadvantage of the United States relative to other high-income countries might be deficiencies in health services. Although the United States is renowned for its leadership in biomedical research, its cutting-edge medical technology, and its hospitals and specialists, problems with ensuring Americans’ access to the system and providing quality care have been a long-standing concern of policy makers and the public (Berwick et al., 2008; Brook, 2011b; Fineberg, 2012). Higher mortality rates from diseases, and even from transportation-related injuries and homicides, may be traceable in part to failings in the health care system.
The United States stands out from many other countries in not offering universal health insurance coverage. In 2010, 50 million people (16 percent of the U.S. population) were uninsured (DeNavas-Walt et al., 2011). Access to health care services, particularly in rural and frontier communities or disadvantaged urban centers, is often limited. The United States has a relatively weak foundation for primary care and a shortage of family physicians (American Academy of Family Physicians, 2009; Grumbach et al., 2009; Macinko et al., 2007; Sandy et al., 2009). Many Americans rely on emergency departments for acute, chronic, and even preventive care (Institute of Medicine, 2007a; Schoen et al., 2009b, 2011). Cost sharing is common in the United States, and high out-of-pocket expenses make health care services, pharmaceuticals, and medical supplies increasingly unaffordable (Commonwealth Fund Commission on a High Performance System, 2011; Karaca-Mandic et al., 2012). In 2011, one-third of American households reported problems paying medical bills (Cohen et al., 2012), a
problem that seems to have worsened in recent years (Himmelstein et al., 2009). Health insurance premiums are consuming an increasing proportion of U.S. household income (Commonwealth Fund Commission on a High Performance System, 2011).
Apart from challenges with access, many Americans do not experience optimal quality when they do receive medical care (Agency for Healthcare Research and Quality, 2012), a problem that health policy leaders, service providers, and researchers have been trying to solve for many years (Brook, 2011a; Fineberg, 2012; Institute of Medicine, 2001). In the United States, health care delivery (and financing) is deeply fragmented across thousands of health systems and payers and across government (e.g., Medicare and Medicaid) and the private sector, creating inefficiencies and coordination problems that may be less prevalent in countries with more centralized national health systems. As a result, U.S. patients do not always receive the care they need (and sometimes receive care they do not need): one study estimated that Americans receive only 50 percent of recommended health care services (McGlynn et al., 2003).
Could some or all of these problems explain the U.S. health disadvantage relative to other high-income countries? This chapter reviews this question: it explores whether systems of care are associated with adverse health outcomes, whether there is evidence of inferior system characteristics in the United States relative to other countries, and whether such deficiencies could explain the findings delineated in Part I of the report.
The panel defines “health systems” broadly, to encompass the full continuum between public health (population-based services) and medical care (delivered to individual patients). As outlined in previous Institute of Medicine reports (e.g., 2011e), health systems involve far more than hospitals and physicians, whose work often focuses on tertiary prevention (averting complications among patients with known disease). Both public health and clinical medicine are also concerned with primary and secondary prevention.1 The health of a population also depends on other public health services and policies aimed at safeguarding the public from health and injury risks (Institute of Medicine, 2011d, 2011e, 2012) and attending to the needs of people with mental illness (Aron et al., 2009). There
_________________
1Examples of primary prevention include smoking cessation, increased physical activity, administering immunizations to eliminate susceptibility to infectious diseases, and helping people avoid harmful environmental exposures (e.g., lead poisoning). Secondary prevention includes early detection of diseases and risk factors in asymptomatic persons (e.g., cancer and serum lipid screening).
is mounting evidence that chronic illness care requires better integration of professions and institutions to help patients manage their conditions, and that health care systems built on an acute, episodic model of care are ill equipped to meet the longer-term and fluctuating needs of people with chronic illnesses. Wagner and colleagues (1996) were among the first to document the importance of coordination in managing chronic illnesses. Many countries differ from the United States because public health and medical care services are embedded in a centralized health system and social and health care policies are more integrated than they are in the United States (Phillips, 2012).
The panel believes that the totality of this system, not just the health care component, must be examined to explore the reasons for differences in health status across populations. For example, a country may excel at offering colonoscopy screening, but ancillary support systems may be lacking to inform patients of abnormal results or ensure that they understand and know what to do next. Hospital care for a specific disease may be exemplary, but discharged patients may experience delayed complications because they lack coverage, access to facilities, transportation, or money for out-of-pocket expenses, and those with language or cultural barriers may not understand the instructions. The health of a population is influenced not only by health care providers and public health agencies but also by the larger public health system, broadly defined.2
Data are lacking to make cross-national comparisons of the performance of health systems, narrowly or broadly defined, in adequate detail. Only isolated measures are available, such as the 30-day case-fatality rate for a specific disease or the percentage of women who obtain mammograms. Nor is it clear what the ideal rate for a given health system measure (e.g., optimal wait times or density of physicians) should be for any given country. Out of necessity, this chapter focuses on the “keys under the lamppost”—the health system features for which there are comparable cross-national data—but the panel acknowledges that better data and measures are needed before one can properly compare the performance of national health care systems.
Based on the data that do exist, how well does the U.S. health care system prevent and treat injury and disease when compared with other high-income countries? As noted earlier, this chapter and the four that follow address three core questions. For this chapter, the three core questions are:
_________________
2The larger public health system includes not only public health agencies, but also public and private entities involved with food and nutrition, physical activity, housing and transportation, and other social and economic conditions that affect health (Institute of Medicine, 2011e). As discussed further in Chapter 8, public- and private-sector leaders are increasingly recognizing the health implications of “nonhealth” policies that relate to agriculture, transportation, land use, energy, housing, and other environmental conditions.
• Do public health and medical care systems affect health outcomes?
• Are U.S. health systems worse than those in other high-income countries?
• Do U.S. health systems explain the U.S. health disadvantage?
QUESTION 1:
DO PUBLIC HEALTH AND MEDICAL CARE SYSTEMS
AFFECT HEALTH OUTCOMES?
As other chapters in this report emphasize, population health is shaped by factors other than health care, but it is clear that health systems—both those responsible for public health services and medical care—are instrumental in both the prevention of disease and in optimizing outcomes when illness occurs. The importance of population-based services is marked by the signature accomplishments of public health, such as the control of -vaccine-preventable diseases, lead abatement, tobacco control, motor vehicle occupant restraints, and water fluoridation to prevent dental caries (Centers for Disease Control and Prevention, 1999, 2011b). Public health efforts are credited with much of the gains in life expectancy that high-income countries experienced in the 20th century (Cutler and Miller, 2005; Foege, 2004). The effectiveness of a core set of clinical preventive services (e.g., cancer screening tests) is well documented in randomized controlled trials (U.S. Preventive Services Task Force, 2012), as are a host of effective medical treatments for acute and chronic illness care (Cochrane Library, 2012). For example, gains in cardiovascular health have occurred with the adoption of evidence-based interventions including antiplatelet therapy, beta-blockers, and reperfusion therapy (Khush et al., 2005; Kociol et al., 2012).
Although some authors have questioned the impact of medical care on health (McKeown, 1976; McKinlay and McKinlay, 1977), others estimate that between 10-15 percent (McGinnis et al., 2002) to 50 percent (Bunker, 2001; Cutler et al., 2006b) of U.S. deaths that would otherwise have occurred are averted by medical care. Across various countries, medical care is credited with 23-47 percent3 of the decline in coronary artery disease mortality that occurred between 1970 and 2000 (Bots and Grobbee, 1996; Capewell et al., 1999, 2000; Ford and Capewell, 2011; Ford et al., 2007; Goldman and Cook, 1984; Hunink et al., 1997; Laatikainen et al., 2005; Unal et al., 2005; Young et al., 2010).
Barriers to health care also influence health outcomes. Inadequate
_________________
3The same studies estimate that between 44 and 72 percent of the fall in mortality resulted from a reduction in cardiovascular risk factors (smoking, lipids, and blood pressure); see Chapter 5.
health insurance coverage is associated with inferior health care and health status and with premature death (Freeman et al., 2008; Hadley, 2003; Institute of Medicine, 2003b, 2009a; Wilper et al., 2009). Conversely, universal coverage has been associated with improved health, both in U.S. states (Courtemanche and Zapata, 2012) and in other countries (Hanratty, 1996). Two other barriers, inadequate numbers of physicians and a weak primary care system, are associated with higher all-cause mortality, all-cause premature mortality, and cause-specific premature mortality (Chang et al., 2011; Macinko et al., 2003, 2007; Or et al., 2005; Phillips and Bazemore, 2010; Starfield, 1996; Starfield et al., 2005).
Health is also affected by the quality of care. The Institute of Medicine (2000) estimated that medical errors claim 98,000 lives each year in the United States. Coordination of care also affects health outcomes because miscommunication, flawed handoffs, and confusion can result in lapses in patient safety and gaps and delays in the delivery of care (Institute of Medicine, 2007b).
Many of the specific causes of death discussed in Part I—such as -transportation-related injuries, homicide, communicable diseases, and chronic diseases—have some connection to health professionals and medical care. For example, the survival of injury victims and their rehabilitation are dependent on emergency medical services and speedy, effective trauma care (Cudnick et al., 2009; Institute of Medicine, 2007a; MacKenzie et al., 2006). Medical care has obvious connections to other areas of the U.S. health disadvantage, such as infant mortality and other adverse birth outcomes, HIV infection, heart disease, and diabetes.
QUESTION 2:
ARE U.S. HEALTH SYSTEMS WORSE THAN THOSE IN
OTHER HIGH-INCOME COUNTRIES?
The United States spends significantly more on health care than any other country (Anderson and Squires, 2010; Reinhardt et al., 2004; Squires, 2011). Median per capita spending among all OECD countries in 2009 was $3,223, which is less than half of the $7,960 per capita spent in the United States (OECD, 2011b). Such statistics have rallied interest in addressing the inefficiency of the health system and the causes of medical cost inflation (Berwick and Hackbarth, 2012; Fisher et al., 2011; Institute of Medicine, 2010; OECD, 2010b) and have sparked a campaign by medical organizations to discourage overutilization (Cassel and Guest, 2012).
Whether the high level of spending on health care contributes to the U.S. health disadvantage is not entirely clear. This spending, some of which
reflects inefficiencies in health care delivery,4 accounted for 17.9 percent of the nation’s gross domestic product in 2010 (Martin et al., 2012). That spending carries a large opportunity cost: it could be diverting resources that might otherwise be applied to public health, education, social services, and the growth of businesses and the economy. The ramifications could include a deleterious effect on the health of Americans relative to their peers in other countries, but the panel found little empirical evidence to support this.
The panel did find some evidence comparing other characteristics of the health system—access and quality—that might explain the inferior health outcomes in the United States. This evidence is reviewed below.
Access to Public Health and Medical Care in the United States
Access to Public Health Services
Public health services in the United States are highly fragmented and are financed by a complex mixture of federal, state, local, and private sources that vary across communities, are earmarked for specific categorical disease priorities,5 and fluctuate over time depending on budgets and separate appropriation decisions at the federal, state, and local level (Fielding and Teutsch, 2011; Institute of Medicine, 2012). The 2,565 local health departments in the United States operate under highly disparate resources and authorities (National Association of County and City Health Officials, 2011). In contrast, public health services in other countries are often coordinated by a central governmental body. It is estimated that the United States spends from 3 to 9 percent of its health budget on public health (Mays and Smith, 2011; Miller et al., 2008, 2012), and its model of specialized categorical program funding to subsidize public health activities does not always match well with the needs of catchment areas (Institute of Medicine, 2012).6 However, there is no evidence that public health spending is higher per capita in other countries or that other countries are more effective in using public health investments to drive improvements in population health.
_________________
4Although a body of evidence suggests that a large proportion of health care spending in the United States is related to waste and inefficiency (Berwick and Hackbarth, 2012), the high consumption of health care resources may also be the product of the U.S. health disadvantage (reverse causality). Conversely, other evidence hints at an iatrogenic effect in which higher intensity of health care is associated with more unfavorable health outcomes (Fisher et al., 2003).
5Examples include maintaining programs in emergency preparedness, tuberculosis, HIV, maternal/child health activities, environmental sanitation, and hygiene.
6For example, on average, only 1.9 percent of the budget of the Centers for Disease Control and Prevention (CDC) and the budget of large metropolitan health departments is devoted to cardiovascular disease, the leading cause of death. State governments spend $1.22 per person on tobacco control, less than a quarter of the minimum level recommended by the CDC (Institute of Medicine, 2012).
Access to Medical Care
Access to medical care is limited for many people in the United States, a potentially important factor in understanding the U.S. health disadvantage relative to other countries. Americans seem less confident than people in other countries that the system will deliver the care they need. In a 2010 Commonwealth Fund survey, only 70 percent of U.S. adults reported being confident or very confident that they would receive the most effective treatments (e.g., drugs, tests) if they were seriously ill (Schoen et al., 2010). Patients in all countries but Norway and Sweden expressed greater confidence.
Health Insurance Coverage The large uninsured (and underinsured) population is a well-recognized problem in the United States. All other peer countries offer their populations universal or near-universal health insurance coverage. Only three OECD countries—Chile, Mexico, and Turkey—provide less coverage than the United States (OECD, 2011b).
Affordability Americans face greater financial barriers in accessing care—insurance deductibles, copayments, and out-of-pocket expenses—than do those in other high-income countries (Schoen et al., 2009b, 2010, 2011) (see Box 4-1). One out of three U.S. patients with a chronic illness or a recent need for acute care reports spending more than $1,000 per year in out-of-pocket costs (Schoen et al., 2011) (see Table 4-1). Higher medical costs could contribute to the U.S. health disadvantage if they cause patients to forgo needed care (Wendt et al., 2011). Even insured and higher-income Americans are more likely than their counterparts in other countries to report problems getting care (Huynh et al., 2006). Among insured adults in the United States under age 65, 25 percent reported serious difficulties paying medical bills, and approximately 40 percent reported access problems due to cost, out-of-pocket expenses exceeding $1,000, and gaps in care coordination (Schoen et al., 2011). In a comparison that looked specifically at adults with above-average incomes in 11 countries, only 74 percent of high-income respondents in the United States were confident that they would be able to afford needed care if they were to become seriously ill; in all comparison countries, the corresponding percentages were higher (Schoen et al., 2010).
Access to Clinicians For various reasons, U.S. patients are less likely to visit physicians than patients in other OECD countries. In 2009, annual consultations in the United States were 3.9 per capita, a lower rate than in all peer countries but Sweden and lower than the OECD average of 6.5 per capita (OECD, 2011b). However, physician consultation rates are an
BOX 4-1
Health Care Decommodification
“Health care decommodification” refers to the extent to which individuals’ access to health care is independent of their financial resources or the market. To compare access based on resources across nations, the British social scientist Clare Bambra (2005) developed a health care decommodification index based on the following three variables: private health expenditure as a percentage of gross domestic product, private hospital beds as a percentage of total bed stock, and the percentage of the population covered by the health care system. She found that the United States had a lower decommodification score (9.0) than all the countries, including 14 peer countries (see Figure 4-1a). Bambra concluded that access to health care is much more market dependent in the United States than in other countries and therefore makes access to care more susceptible to the socioeconomic status of the patient.
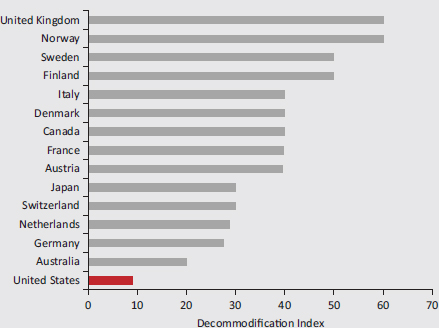
FIGURE 4-1a Access to health care independent of personal resources.
SOURCE: Adapted from Bambra and Beckfield (2012, Table 2).
| Percentage of Respondents Reporting Access Problems in Selected Countries | |||||||||||
| Problem | Austria | Canada | France | Germany | Netherlands | New Zealand | Norway | Sweden | Switzerland | United Kingdom | United States |
| Difficulty paying or unable to pay medical bills | 8 | 8 | 5 | 6 | 14 | 11 | 7 | 4 | 8 | 1 | 27 |
| Cost-related access problems | 30 | 20 | 19 | 22 | IS | 26 | 14 | 11 | 18 | 11 | 42 |
| Did not visit a doctor when had a medical problem | 17 | 7 | 10 | 12 | 7 | 18 | 8 | 6 | 11 | 7 | 29 |
| Did not get recommended test, treatment, or follow-up | 19 | 7 | 9 | 13 | 8 | 15 | 7 | 4 | 11 | 4 | 31 |
| Did not fill a prescription or skipped doses | 16 | 15 | 11 | 14 | 8 | 12 | 7 | 7 | 9 | 4 | 30 |
SOURCE: Data from Schoen et al. (2011, Exhibit 1).
imperfect measure of access because they are confounded by many factors, such as policies that require an in-person physician visit for a referral or to refill a prescription.
Physician Density One reason for fewer physician visits in the United States may be a lower concentration of providers. According to the OECD, physician density (the number of practicing physicians per 1,000 population) in 2009 was 2.4 in the United States, lower than all peer countries but Japan (OECD, 2011b).7 Physician density grew in the United States by only 0.5 per 1,000 people between 2000 and 2009, a lower growth rate in physician density than that reported by any peer country but France.8 Access to physicians varies by geography, a particular problem in the United States with its large rural expanses.9
Primary Care Although the United States does well in providing access to many specialists, access to primary care physicians and a regular health care provider is more limited than in many other countries (OECD, 2011b; Schoen et al., 2009b, 2011; Starfield et al., 2005; World Health Organization, 2008b). According to the OECD, only 12.3 percent of U.S. physicians engage in primary care, the lowest proportion among 15 peer countries providing data (see Figure 4-1).10 Macinko et al. (2003) applied 10 criteria to rank the primary care systems of 18 high-income countries (including Canada, Australia, Japan, and 14 European countries). The United States had the weakest primary care score of all the countries in 1975 and 1985 and the third weakest in 1995 (Macinko et al., 2003).
Continuity of care from a regular provider, which is important to effective management of chronic conditions (Liss et al., 2011), may be more tenuous in the United States than in comparable countries. Only slightly more than half (57 percent) of U.S. respondents to the 2011 Commonwealth
_________________
7U.S. physician density was lower than that of 28 other countries, including all of Western and Eastern Europe (except Poland), Canada, Australia, New Zealand, and Russia (OECD, 2011b).
8In contrast, the density of nurses in the United States was 10.8 per 1,000 population in 2009, higher than the OECD average and the sixth highest nurse-to-physician ratio in OECD countries (OECD, 2011b).
9As of mid-2012, the Health Resources and Services Administration (HRSA) in the United States had formally designated 5,703 areas as having a primary care health professional shortage (U.S. Department of Health and Human Services, 2012c). The 54.5 million people living in these areas need another 15,168 health practitioners to meet their primary health care needs, assuming a population to practitioner ratio of 2,000:1. Almost 50 percent of U.S. counties had no obstetrician-gynecologists (National Center for Health Statistics, 2007).
10This percentage is less than half the OECD average (25.9 percent) and below the rates reported by such countries as Mexico, Turkey, and some Eastern European countries (e.g., the Czech Republic, Estonia, the Slovak Republic, Slovenia) (OECD, 2011b).
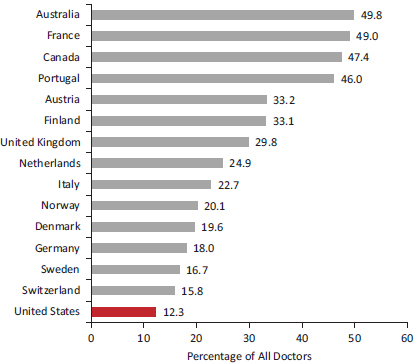
FIGURE 4-1 General practitioners as a proportion of total doctors in 15 peer countries, 2009.
SOURCE: Data from OECD (2011b, Figure 3.2.2).
Fund survey reported being with the same physician for at least 5 years, a lower rate than all comparison countries except Sweden (Schoen et al., 2011). In another Commonwealth Fund survey, U.S. patients were more likely than patients in other countries except Canada to report visiting an emergency department for a condition that could have been treated by their regular physician had one been available (Schoen et al., 2009b).
Access to Health Care Facilities The United States has fewer hospital beds per capita than most other countries, but this measure may be confounded by increasing efforts to deliver care in less expensive outpatient settings. The density of hospital beds decreased in most OECD countries between 2000 and 2009 (OECD, 2011b). In a comparison of eight countries, Wunsch and colleagues (2008) reported that the United States had the third highest concentration of critical care beds (beds in intensive care units per 100,000 population). However, the availability of long-term care beds for U.S. adults ages 65 and older is lower than for those in 10 of the 16 peer countries. Where such care is delivered also differs in the United
States: in most high-income countries, long-term care is usually provided in the patient’s home, but in the United States, less than half of adults report receiving long-term care at home (OECD, 2011b).
Timeliness of Care Inadequate insurance, limited access to clinicians and facilities, and other delivery system deficiencies can affect how quickly patients receive the care they need. Responses to the Commonwealth Fund surveys suggest that U.S. patients with complex care needs are more likely than those in many other countries to face delays in seeing a physician or nurse within 1-2 days, especially after normal office hours, making it necessary to rely on an emergency department (Schoen et al., 2011). However, waiting times for nonemergency elective care appear to be shorter in the United States than in most other countries (Davis et al., 2010; Schoen et al., 2010).
Quality of Public Health and Medical Care Systems
Although there is evidence of variance in health protection and other public health services across communities and population groups in the United States (Culyer and Lomas, 2006),11 there is little direct evidence to determine whether and how this differs across high-income countries. Comparing the quality of public health services in the United States to that of other countries is difficult due to the lack of comparable international data on the delivery of core public health functions.12
There are also important differences between countries in what types of programs and services are counted within the broad categories of public health, preventive medicine, and medical care. Thus, the only way to compare the public health services of countries is to examine proxy measures, but proxies often miss other important differences in population-based public health protections. This section discusses several measures of the quality of public health and medical care systems: immunizations, health
_________________
11Examples include variations in motor vehicle safety regulations, illegal blood alcohol concentrations, and requirements to wear safety helmets: they vary greatly across the 50 states and the District of Columbia but are often uniform in many high-income countries (Transportation Research Board, 2011).
12In the United States, the 10 essential public health services include monitoring health status, diagnosing and investigating health problems, informing the public, mobilizing community partnerships, developing policies and plans, enforcing laws and regulations, linking people to needed health services, assuring a competent workforce, evaluating quality of health services, and research (Institute of Medicine, 2011e). Similar core public health functions are identified globally by WHO (World Health Organization, 2008b). See Chapter 7 for data on differences in the quality of environment health protections in the United States and other countries.
promotion, screening tests, acute care, chronic illness care, medical errors, and optimizing health care delivery.
Immunizations
Childhood immunization coverage in the United States, although much improved in recent decades, is generally worse than in other high-income countries. For example, according to the OECD, 83.9 percent of U.S. children have been vaccinated against pertussis, the lowest rate of all peer countries but Austria; the U.S. rate is the third lowest among 39 OECD countries and well below the OECD average of 95.3 percent (OECD, 2011b). Conversely, immunization rates for older adults appear to be higher in the United States than in most OECD countries. According to the OECD, 66.7 percent of U.S. adults age 65 and older received influenza vaccination in 2009, a rate below that of France, the United Kingdom, Australia, and the Netherlands but higher than those of the other peer countries.
Health Promotion
Although the prevalence of unhealthy behaviors (e.g., smoking) and other modifiable risk factors (e.g., obesity, environmental exposures) can be compared across countries, data are lacking to accurately compare the quality of public health agencies or programs to address these risk factors, including the extent of health promotion programs aimed at controlling behavioral and environmental risks. This information would have relevance to tobacco and obesity-related diseases that claim excess years of life in the United States or to higher death rates from alcohol, other drugs, and transportation-related injuries (see Chapters 1 and 2). Patient surveys show no evidence that U.S. physicians are less likely to offer behavioral counseling than their counterparts in other countries (Davis et al., 2010), and they appear more likely to prescribe pharmacotherapy (e.g., varenicline) to help with smoking cessation (Fix et al., 2011). (See Chapter 7 for further discussion of how the environmental influences on health behaviors might differ between the United States and other countries.)
Screening Tests
The United States appears to administer more screening tests than do other countries (Gohmann, 2010; Howard et al., 2009). According to the OECD, the United States has the third highest rate of mammography screening among peer countries, surpassed only by the Netherlands and Finland, and it has the highest cervical cancer screening rate among peer countries (and all OECD countries) (OECD, 2011b). In an analysis of
survey data from the United States and 10 European countries, Howard and colleagues (2009) reported that the European/U.S. ratio for frequency of screening for adults age 50 and older was 0.22-0.60 for mammography, 0.43-0.49 for colon cancer screening, 0.55-0.88 for cervical cancer screening, and 0.58-0.64 for prostate cancer screening—all indicating that the comparison countries screened less often.
Acute Care
Evidence is limited to compare the quality of acute care services in high-income countries. Some data are available regarding the quality of trauma care in the United States, a form of acute care that is especially relevant to the U.S. health disadvantage because of the country’s high death toll from transportation-related injuries and homicide (see Chapters 1 and 2). Although there is evidence that outcomes vary across U.S. trauma centers, even after risk adjustment (Haider et al., 2012), there is little empirical evidence to compare the quality of trauma care in the United States to that in other countries. Such comparisons require a close examination of interrelated determinants of trauma care (e.g., health insurance coverage), socioeconomic and policy contexts (discussed in later chapters), and differences in geography (see Box 4-2).
Chronic Illness Care
As detailed in Part I of this report, deaths and morbidity from noncommunicable chronic diseases are higher in the United States than in peer countries, which invites speculation about deficiencies in the quality of medical care for these conditions. Evaluating the quality of chronic illness care is complex because of the multifactorial influences on care management and coordination. The Commonwealth Fund Commission on a High Performance Health System (2008) evaluates the quality of health care on four measures: effectiveness, safety, coordinated care, and patient-centered, timely care. We focus here on the following measures of the quality of chronic illness care: achieving treatment targets, case fatality rates, other clinical outcomes, and proxies for health care quality.
Achieving Treatment Targets The United States is making progress in meeting specified treatment targets, especially those established in practice guidelines, quality performance indicators, and criteria used for pay-for-performance incentives. Establishing higher reimbursements and other incentives has spurred many U.S. providers and hospitals to improve their performance outcomes (Epstein, 2007; Institute of Medicine, 2007c). Treatment goals for controlling hypertension, elevated serum lipids, and diabetes
BOX 4-2
Case Study:
Trauma Care in the United States
Circumstances in the United States could affect the ability of the health care system to render aid to victims of transportation-related injuries and violence, two leading contributors to the U.S. health disadvantage relative to other high-income countries. These circumstances illustrate not only the role of the health care system, as discussed in this chapter, but the important interconnections with socioeconomic factors and public policy as discussed in subsequent chapters. This interdependence is illustrated by two barriers to trauma care services in the United States—lack of health insurance and the geography of the United States—both of which may affect survival and rehabilitation (Greene et al., 2010).
Lack of Health Insurance: Case-fatality rates from the National Trauma Data Bank indicate that injury victims are more likely to die at hospitals with a large percentage of minority patients, and this risk is compounded if they are uninsured (Haider et al., 2012). A separate study reported that risk of death on the first hospital day after injury differs by insurance status, and this disparity becomes more pronounced throughout the hospital stay (Downing et al., 2011). After excluding on-scene deaths, Harris and colleagues (2012) found that U.S. assault victims brought to high-level trauma centers were more likely to die if they were black, even after adjusting for other variables.
These associations raise as many questions as they answer and point to “upstream” factors examined in subsequent chapters of the report. For example, disparities in the outcomes of trauma care do not always appear to relate to the quality of care provided at the institutions themselves (Vettukattil et al., 2011). The trauma literature points to the socioeconomic status of patients and the infrastructure and resources available to trauma centers operating in underserved areas. For example, as Haider and colleagues (2012, p. 68) explain:
[t]he underinsured population with likely much less resources, which is seen at predominantly minority hospitals, may bring significant residual confounding that could not be controlled for. Issues such as treatment delay, health illiteracy, and differential rates of follow-up and access to rehabilitation services have been implicated as potential reasons for the worse quality of care and worse outcomes among uninsured patients. Additional issues at public hospitals include nurse staffing shortages, constrained budgets, and lack of capital and technical support.
This analysis points directly to the relevance of the socioeconomic conditions of trauma victims (see Chapter 6) and to the role of public policies in shaping conditions that affect health (see Chapter 8).
Geography: The large rural expanses in the United States have relevance to the death toll from transportation-related injuries, because 61 percent of traffic fatalities occur in rural locations (Zwerling et al.,
2005). Trauma outcomes appear to be worse for U.S. patients in nonurban areas (Sihler and Hemmila, 2009; Zwerling et al., 2005). Although factors unrelated to health care could contribute greatly to crash survival (e.g., rural road design and vehicles, speed limits, and the age, alcohol levels, and health status of rural drivers) (Transportation Research Board, 2011; Zwerling et al., 2005), an important factor is how quickly victims can be stabilized and transported to trauma centers by emergency medical personnel. Both time and distance have been shown to inversely affect survival from major trauma in rural areas (Durkin et al., 2005; Grossman et al., 1997; Howell et al., 2010). An analysis in the 1990s reported that emergency response time, scene time, and transportation time to the hospital were longer for rural victims of major trauma than for urban victims. Trauma victims transported by helicopter have lower mortality rates than those conveyed by ground transportation (Sullivent et al., 2011).
Rural physicians and hospitals that are close to crash sites may lack capacity to stabilize patients. One study demonstrated that mortality from motor vehicles crashes was lower in counties with 24-hour availability of a general surgeon, orthopedic surgeon, neurosurgeon, computed tomographic scanner, and operating room and in those with trauma centers (Melton et al., 2003). The absence of onsite specialists can be consequential. For example, survival from traumatic brain injury is improved if there is less than a 4-hour delay between arrival in the emergency department and the performance of a craniotomy or the drainage of a hematoma (Kim, 2011).
Helicopter transportation can therefore be important in saving time and reaching qualified trauma centers, but resources for such services are uneven across rural U.S. counties and are determined by diverse stakeholders. This, too, illustrates the interconnections between health care and public policy. The same applies to the staffing of medical helicopters, which differs in the United States. In a survey of emergency medical services for mountain areas of 14 countries in Europe and North America, Brugger and colleagues (2005) found that 63 percent of European helicopters have a physician on board and 18 percent are staffed with a paramedic, as compared with 32 percent and 60 percent, respectively, of North American helicopters. Policy challenges, among them limited budgets (see Chapter 8), may make it difficult to place more physicians on medical helicopters, especially in rural areas.
Finally, survival from transportation-related injuries or violence cannot be evaluated in isolation from other conditions responsible for the U.S. health disadvantage, such as obesity or diabetes, because comorbidity from chronic illnesses increases the risk of death from injuries (Morris et al., 1990).
rely heavily on the use of prescription drugs, and the United States has higher per capita consumption of pharmaceuticals than peer countries (Morgan and Kennedy, 2010; Squires, 2011). In 2009, per capita spending on pharmaceuticals in the United States was $947, nearly twice the OECD average of $487 (OECD, 2011b). Evidence is available on how the United States compares with other countries in achieving specific cardiovascular and diabetes treatment targets.
Cardiovascular Care U.S. patients appear more likely than those in peer countries to have their blood pressure and serum cholesterol levels checked (Davis et al., 2010; Schoen et al., 2004; Thorpe et al., 2007). The use of preventive drugs for people at risk of cardiovascular disease is more common in the United States than in Europe (Crimmins et al., 2010). In a comparison of medication use in the United States with 10 European countries, Thorpe and colleagues (2007) found that use of antihypertensive agents did not differ significantly but that use of cholesterol-lowering drugs and medication for heart disease was greater in the United States than in Europe. A National Research Council (2011) study also documented that patients with high blood cholesterol and hypertension were more likely to receive medications in the United States than in comparable countries. A 2004 analysis of survey data collected in the 1990s demonstrated that blood pressure was more effectively controlled in the United States than in Canada or Europe (Wolf-Maier et al., 2003), but a more recent patient survey did not reach the same conclusion (Schoen et al., 2011). There is also some evidence that the speed of cardiovascular care for acute coronary syndrome in the United States may match or exceed that of Europe (Goldberg et al., 2009).
Diabetes Care The United States may be less exemplary than other countries in meeting testing and treatment targets for diabetes care. In one survey, patients with diabetes in half the countries were more likely to report a recent hemoglobin A1c test, foot examination, eye examination, and serum cholesterol measurement than patients in the United States (Schoen et al., 2009b). An OECD report found that the United States ranked fourth among 12 countries in the frequency of eye examinations of patients with diabetes (OECD, 2007).
Case-Fatality Rates A measure of the quality of care of life-threatening illnesses is the probability of death following treatment, also known as the case-fatality rate. According to the OECD, U.S. patients admitted for acute myocardial infarction have a relatively low age-adjusted case-fatality rate within 30 days of admission (4.3 per 100 patients) compared with the OECD average (5.4 per 100 patients); however, as shown in Figure 4-2, they have a higher rate than patients in six peer countries. An earlier OECD
analysis, based on mortality data from the 1990s, reported that the United States had low case-fatality rates at 30 days, 90 days, and 1 year after acute myocardial infarction (Moise et al., 2003). In a comparison of 5-year mortality rates following acute myocardial infarction among U.S. and Canadian patients, Kaul and colleagues (2004) found that U.S. patients had significantly lower rates, 19.6 percent versus 21.4 percent for Canadians.
The U.S. age-adjusted 30-day case-fatality rate for ischemic stroke is 3.0 per 100 patients, which is below the OECD average of 5.2 per 100 patients, but it is higher than those of four peer countries (Denmark, Finland, Japan, and Norway) (OECD, 2011b). An earlier OECD analysis reported that the U.S. 1-year case-fatality rate from stroke was higher than the OECD average (Moon et al., 2003).
One study calculated the ratio between diabetes mortality for 1994-1998 and incidence at ages 0-39 in 29 industrialized countries. The United States had the 10th highest ratio—higher than all Western European countries,
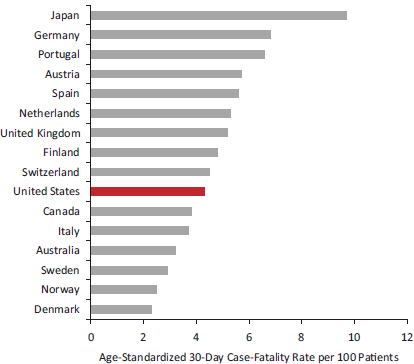
FIGURE 4-2 In-hospital case-fatality rates for acute myocardial infarction in 16 peer countries.
NOTES: Data are for 2009 or nearest year; data apply to deaths within 30 days of admission for acute myocardial infarction.
SOURCE: Data from OECD (2011b, Figure 5.3.1).
Canada, Australia, and New Zealand—but the comparison was subject to a variety of limitations (Nolte et al., 2006).
Other Clinical Outcomes Apart from time-limited case-fatality rates, the panel found no comparable data for comparing the effectiveness of medical care across countries. Data are available for comparing cancer survival rates, which are generally higher in the United States, but cancer survival is confounded by lead-time and length biases introduced by screening (Ciccolallo et al., 2005), a more common practice in the United States than elsewhere. U.S. patients may live longer after their cancer diagnosis simply because the disease is detected at an earlier stage, not because death is delayed. This screening artifact could explain both the higher incidence (Thorpe et al., 2007) and survival rates (Gatta et al., 2000; Verdecchia et al., 2007) for cancer reported by the United States.
Proxies of Health Care Quality There is some evidence that U.S. patients may be more likely to experience postdischarge complications and require readmission to the hospital than do patients in other countries. In one survey, U.S. patients were more likely than those in other surveyed countries to report visiting the emergency department or being readmitted after discharge from the hospital (Schoen et al., 2009). Another study reported that 30-day readmission rates for a common form of myocardial infarction were higher in the United States than in Canada, Australia, New Zealand, and 13 European countries (Kociol et al., 2012).13
Little evidence exists to compare the frequency of hospitalization for ambulatory care-sensitive conditions (Institute of Medicine, 2009d)—a proxy for the quality of outpatient care—except for two conditions (asthma and diabetes), and they portray different patterns. Although OECD (2011b) data for peer countries indicate that the United States has the highest asthma hospitalization rate among persons age 15 and older, the U.S. admission rate for uncontrolled diabetes in the same age group is below the OECD average (see Figures 4-3 and 4-4).14 These proxies are imperfect because countries may differ in their capacity to manage uncontrolled disease complications outside the hospital.
Outcomes after organ transplantation offer an interesting comparative picture of the quality of perioperative care and subsequent chronic care in the United States. Dawwas and colleagues (2007) compared outcomes for
_________________
13In a pattern observed by other health services researchers, Kociol and colleagues (2012) observed that differences in readmission diminished after adjusting for length of stay. Lengths of stay in the United States are shorter than those in other countries and may contribute to higher readmission rates (see Baker et al., 2004).
14Earlier OECD data (from 2007) reported that the United States had the highest rate of lower extremity amputations for diabetes among the peer countries (OECD, 2009c).
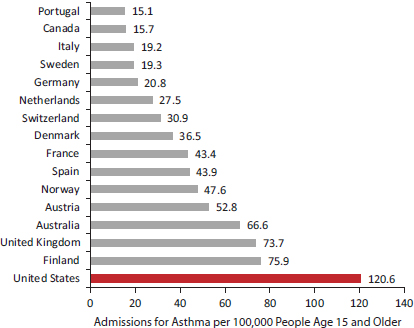
FIGURE 4-3 Hospital admissions for asthma in 16 peer countries.
NOTE: Rates are age-standardized and based on data for 2009 or nearest year.
SOURCE: Data from OECD (2011b, Figure 5.1.1, p. 107).
adults who underwent a first single organ liver transplant between 1994 and 1995 in the United Kingdom or Ireland with those in the United States. Risk-adjusted mortality in both countries was generally higher than in the United States during the first 90 days, equivalent between 90 days and 1 year post-transplantation, and lower than the United States after the first post-transplant year. “Our results are consistent with the notion that the United States has superior acute perioperative care whereas the UK appears to provide better quality chronic care following liver transplantation surgery” (Dawwas et al., 2007, p. 1,606).
Another imperfect measure of the performance of health care systems is to estimate the mortality that is considered amenable to health care (Nolte and McKee, 2003; Rutstein et al., 1976). Relying on the assumption that all deaths from a list of more than 30 causes (and 50 percent of deaths from ischemic heart disease) could be averted by better health care,15 Nolte and McKee concluded that the United States had the highest amenable mortality
_________________
15This measure, which has been used in a number of studies (Bunker et al., 1994; Commonwealth Fund Commission on a High Performance System, 2011), relies on certain assumptions about attributable mortality and does not adjust for disease prevalence (Gay et al., 2011).
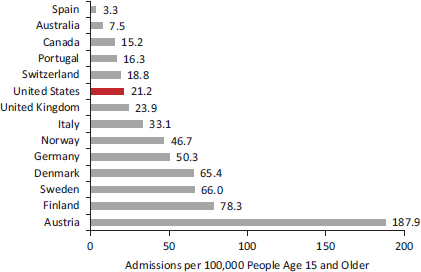
FIGURE 4-4 Hospital admissions for uncontrolled diabetes in 14 peer countries.
NOTE: Rates are age-sex standardized, and they are based on data for 2009 or nearest year.
SOURCE: Data from OECD (2011b, Figure 5.1.1, p. 107).
rate among 16 countries (Nolte and McKee, 2011). Building on this analysis for a larger set of countries, the Commonwealth Fund Commission on a High Performance System concluded (2011, p. 9):
The U.S. now ranks last out of 19 countries on a measure of mortality amenable to medical care, falling from 15th as other countries raised the bar on performance. Up to 101,000 fewer people would die prematurely if the U.S. could achieve leading, benchmark country rates.
Medical Errors
U.S. patients surveyed by the Commonwealth Fund were more likely to report certain medical errors and delays in receiving abnormal test results than were patients in most other countries (Schoen et al., 2011). U.S. patients with chronic illnesses were more likely than those in all comparable countries included in the survey to recall a medical error (Schoen et al., 2009b).16 Survey data about perceived errors must be interpreted cautiously, however, because contextual variables may influence perceptions
_________________
16Conversely, another survey found that U.S. patients with chronic illnesses or recent needs for acute care were least likely to report a hospital-related infection (Schoen et al., 2011).
and interpretations of events (Davis et al., 2010). Clinically recorded errors are also imperfect and are only available across countries for a few indicators. According to OECD data, the incidence of postoperative pulmonary embolism or deep vein thrombosis in the United States is 1,019 per 100,000 discharges (the second highest rate among peer countries), three peer countries have higher rates than the United States for postoperative sepsis, and five have higher rates for accidental puncture/laceration and leaving a foreign body in during a procedure (OECD, 2011b).17
Optimizing Care Delivery
A factor that could diminish the effectiveness of health care in the United States is disruptions in the care delivery process. For many years, quality improvement programs and health services research have recognized that the fragmented nature of the U.S. health care system, miscommunication, and incompatible information systems foment lapses in care; oversights and errors; and unnecessary repetition of testing, treatment, and associated risks because records of prior services are unavailable (Fineberg, 2012; Institute of Medicine, 2000, 2010).18 Problems are more pronounced during “handoffs,” when patients transition from one care setting to another. Differences in medical error rates between countries have an independent association with breakdowns in care coordination (Lu and Roughead, 2011).
The only detailed data to compare care delivery practices across countries come from surveys conducted each year by the Commonwealth Fund. These data have a variety of limitations. For example, they rely on perceptions (of patients and physicians) rather than independently documented outcomes. Although the surveys have been administered annually since 1998 to thousands of patients and physicians in up to 11 countries, they include dozens of questions about care delivery practices that have varied in wording and administration methods over the years. However, a consistent pattern emerges in the U.S. responses (see Box 4-3). U.S. patients generally give their physicians high marks in the attention they pay to clinical details, to engaging
_________________
17The United States (12.5 percent) and Canada (13.7 percent) have the highest rate of obstetrical trauma among 20 OECD countries (OECD, 2011b).
18The question of whether physicians in the U.S. system are less effective in producing health than are physicians in other OECD countries has also been studied. Although specific results varied with the health indicator chosen, Or et al. (2005) found that the productivity of U.S. physicians was typically near the middle of the range. Unusually low physician productivity would not, therefore, appear to contribute to the U.S. health disadvantage.
BOX 4-3
Quality of Care:
Survey Findings from Commonwealth Fund Surveys
Strengths: United States at or Better Than Average
• Attention to clinical detail
Practice knows important information about medical history
Pharmacist/physician reviews and discusses medications
Tracking adverse events
Regular self-assessment of outcomes and patient satisfaction
• Patient-centered communication
Encourages questions
Discusses goals and priorities
Explains treatment options
Involves patient in decision as much as wanted
Helps make daily treatment plan
Gives clear instructions about warning symptoms
• Hospital discharge planning
Instructions about symptoms to watch for and when to seek further carea
Who to contact for questions about condition or treatmenta
Written care plan for care after dischargea
Arrangements made for follow-up visits
Clear instructions about medications to takea
Weaknesses: United States Worse Than Average
• Coordination of care
Wasted time
Wasted time a “major problem” for primary care physician
Unnecessary treatment
Duplicate testingb
No tracking system to ensure results reach clinician
No system for physician to send reminders
Not using nonphysician staff to coordinate care
Not using written guidelines
• Medical errors
Medical mistake made in treatment
Given wrong medication or wrong dose
Given incorrect test results on diagnostic test
Delays in being notified of abnormal results
• Dissatisfaction with health care system
Patient dissatisfaction with the health systemb
Primary care provider dissatisfaction with the health system
• Miscommunication
Communication between providers:
Not sharing medical information
Not informed about specialist consultation
Regular doctor not informed about hospitalization or surgery
Communication between provider and patient:
Getting answer on day called
Obtaining advice from help line
Spends enough time with them
Explanations easy to understand
• Inadequate information systems
No electronic medical record
No capacity for electronic ordering of laboratory tests
No capacity for electronic entry of clinical notes
No electronic access to test results
No capacity to electronically prescribe medications
No electronic alerts/prompts about drug dose/interactions
No computerized reminders for guideline-based interventions or screening tests
Medical record system cannot generate list of:
![]() patients due for tests or preventive care
patients due for tests or preventive care
![]() all medications taken by patient
all medications taken by patient
![]() patients due for tests or preventive care
patients due for tests or preventive care
![]() patients by diagnosis or test result
patients by diagnosis or test result
_____________
NOTES: Survey findings are based on self-report of survey participants (patients and providers). Data based on surveys conducted in 2004, 2008, 2009, 2010, and 2011. The countries included in the 2011 survey were Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, the United Kingdom, and the United States. Earlier surveys included fewer countries.
aMore than half of surveyed countries reported a higher prevalence of problems than in the United States.
bHalf or fewer surveyed countries reported a higher prevalence of problems.
SOURCES: Schoen et al. (2004, 2009a, 2009b, 2010, 2011).
patients in decision-making conversations, and to discharge planning19 after hospitalization or surgery. However, U.S. respondents are more likely than those in the other surveyed countries to have problems in four key areas that could affect the quality of care outside the hospital, particularly management of chronic illnesses: confusion and poorly coordinated care, inadequate information systems to access needed clinical data, miscommunication between providers and between patients and providers, and medical errors.
• Poor coordination: reported problems included unnecessary treatment, duplicate testing, wasted time, not ensuring laboratory results reach the clinician, not sending reminders to patients, not using nonphysician staff to coordinate care, and not spending enough time with the patient;20
• Inadequate information technology: reported problems include lack of electronic medical records; inability to electronically order laboratory tests, access test results, prescribe medications, enter clinical notes, or receive drug alerts; and inability to generate lists of patients with specific conditions (e.g., diabetes), laboratory abnormalities, overdue tests or vaccines, or medications;21
• Miscommunication: reported problems include physicians not sharing important medical information with each other; “regular” physicians not being informed about specialist care or hospitalizations; test results, medical records, or reasons for referral not being available in time for appointments; and patients not getting a quick telephone response from their regular provider on the day they call with a medical question or from help lines; and
_________________
19U.S. patients who had been hospitalized were more likely than their counterparts in all other countries to report receiving written care plans, arrangements for follow-up visits, instructions about medications warning symptoms, and information about whom to contact with questions (Davis et al., 2010).
20Such problems are compounded when multiple providers are involved. When four or more physicians were involved, 45 percent of U.S. patients reported a medical test or record coordination problem, compared with 21-35 percent in the seven comparison countries (Schoen et al., 2009b).
21Some national health systems have centralized databases that are used to identify people in need of public health and preventive services or for outreach for chronic illness management. Long-standing population-based cancer registry systems with national coverage (often regionally organized) and with virtually complete case follow-up exist in all Nordic countries, the United Kingdom, and many Baltic and central European countries (Quinn, 2003). In most European countries, organized breast and cervical cancer screening programs can use these databases to mail periodic screening invitations to all women in the target age group (Howard et al., 2009). Use of such registries in Sweden and other countries has been shown to improve health outcomes, often at lower cost (Larsson et al., 2012).
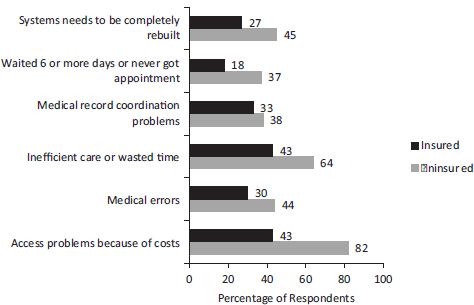
FIGURE 4-5 Frequency of complaints among insured and uninsured U.S. patients with chronic conditions.
NOTE: Based on surveys of patients with chronic illnesses conducted by the Commonwealth Fund.
SOURCE: Adapted from Schoen et al. (2009b, Exhibit 6, p. w12).
• Medical errors: reported problems included medical mistakes, incorrect medication or dosage, incorrect results on diagnostic tests, and delays in being notified of abnormal results.
Among surveyed countries, U.S. patients and physicians are most likely to express dissatisfaction with the health system and to recommend rebuilding it (Davis et al., 2010; Schoen et al., 2009a, 2009b, 2011).22
Could these coordination problems reflect the large proportion of U.S. patients who lack health insurance coverage? In 2008, the Commonwealth Fund stratified the survey responses of chronically ill patients based on their insurance status. As shown in Figure 4-5, coordination problems were more common among the uninsured, as would be expected, but large proportions of insured patients (up to 43 percent) also reported difficulties getting appointments, inefficient care or wasted time, and medical test or record coordination problems. One in four insured patients was sufficiently dissatisfied to recommend rebuilding the health system (Schoen et al., 2009b).
_________________
22In the 2009 survey, German physicians were more likely than U.S. physicians to recommend completely rebuilding the health care system (Schoen et al., 2009a).
QUESTION 3:
DO U.S. HEALTH SYSTEMS EXPLAIN THE
U.S. HEALTH DISADVANTAGE?
The evidence reviewed above supports the following conclusions: The U.S. public health system is more fragmented than those in other countries, but there are insufficient data to compare core public health functions cross-nationally. More data are available for comparing health care systems across countries. American patients and primary care physicians are more dissatisfied with their health care system and are more likely to want major reforms than are patients and physicians in other countries. A conspicuous problem in the United States is the lack of universal health insurance, something recent reforms have sought to address, but deficiencies in access and quality are pervasive and plague even insured and high-income patients. Notably, U.S. patients with complex care needs—insured and uninsured alike—are more likely than those in other countries to complain of medical costs or defer recommended care as a result.
The United States has fewer practicing physicians per capita than comparable countries. Specialty care is relatively strong and waiting times for elective procedures are relatively short, but Americans have less access to primary care. Continuity of care is weaker in the United States than in other countries: U.S. patients with complex illnesses are less likely to keep the same physician for more than 5 years. Compared to people living in comparable countries, Americans do better than average in being able to see a physician within 1-2 days of a request, but they find it more difficult to obtain medical advice after business hours or to get calls returned promptly by their regular physicians.
There appear to be differences in the quality of hospital and ambulatory care across countries. Compared with most peer countries, U.S. patients who are hospitalized with acute myocardial infarction or ischemic stroke are less likely to die within the first 30 days. And U.S. hospitals also appear to excel in discharge planning. However, quality appears to drop off in the transition to long-term outpatient care. U.S. patients appear more likely than those in other countries to require emergency department visits or readmissions after hospital discharge, perhaps because of premature discharge or problems with ambulatory care.
The U.S. health system shows certain strengths: cancer screening is more common in the United States, enough to create a potential lead-time increase in 5-year survival. Pharmacotherapy and control of blood pressure and serum lipids are above the average for comparable countries. However, systems to manage illnesses with ongoing, complex care needs appear to be weaker. Long-term care for older adults is less common. U.S. primary care physicians are more likely to lack electronic medical records, registry
capacities, tracking systems for test results, and nonphysician staff to help with care management. Confusion, poor coordination, and miscommunication are reported more often in the United States than in comparable countries. Moreover, these problems are reported in large numbers by insured and above-average income patients.
Whether poor coordination of complex care needs for chronic -conditions—such as asthma, congestive heart failure, depression, and diabetes—is contributing to the U.S. health disadvantage is still unclear. The current evidence is mixed. For example, U.S. hospitalizations for asthma are among the highest of peer countries, but asthma is influenced by factors outside of health care (e.g., air pollution, housing quality) (Etzel, 2003; Lanphear et al., 2001; Sly and Flack, 2008). Testing of patients with diabetes may be less common in the United States than in some other countries, but only five peer countries have a lower rate of hospitalizations for uncontrolled diabetes.
The quality problems with U.S. ambulatory care, though recognized, should not be overstated. The same surveys that describe coordination problems also suggest that U.S. primary care physicians perform as well as those in other countries in some aspects of care coordination, such as being attentive to clinical details, using reminders to monitor test results, and giving patients medication lists and written instructions. U.S. physicians reportedly perform better than their counterparts in providing patient-centered communication.
WHAT U.S. HEALTH SYSTEMS CANNOT EXPLAIN
Problems with health care in the United States are important, but at best, they can explain only part of the U.S. health disadvantage for three reasons. First, some causes of death and morbidity discussed in Part I are only marginally influenced by health care. For example, homicide and suicide together account for 23 percent of the extra years of life lost among U.S. males relative to other countries (see Chapter 1), but victims often die on the scene before the health care system is involved, especially when firearms are involved. Deficiencies in ambulatory care in the United States bear little on the large number of deaths from transportation-related injuries. Access to emergency medical services and skilled surgical facilities could play a role, but there is no evidence that rescue services or trauma care in the United States are inferior to the care available in other countries (see Box 4-2). Other factors, ranging from road safety to drunk driving and socioeconomic conditions, may matter more (Transportation Research Board, 2011).
Second, although poor medical care could be plausibly linked to communicable and noncommunicable diseases, which claim 20-30 percent of the extra years of life lost in the United States (see Chapter 1), the available evidence for two common noncommunicable diseases—myocardial
infarction and ischemic stroke—suggests that U.S. outcomes are better than the OECD average. The United States excels in performing screening tests that are known to reduce mortality. However, it is possible that the health disadvantage arises from shortcomings in care outcomes that are not currently measured and from gaps in insurance, access, and coordination. Even the measures that are available for myocardial infarction and stroke are limited to short follow-up periods after the acute event, and outcomes may deteriorate thereafter.
Part I lists nine domains in which the U.S. health disadvantage is documented: (1) adverse birth outcomes (e.g., low birth weight and infant mortality); (2) injuries, accidents, and homicides; (3) adolescent pregnancy and sexually transmitted infections; (4) HIV and AIDS; (5) drug-related mortality; (6) obesity and diabetes; (7) heart disease; (8) chronic lung disease; and (9) disability. Deficiencies in public health systems or in access to quality health care could conceivably play a role in each of these domains. For example, the United States has a high rate of preterm births (see Chapter 2), a large proportion of which appear to be initiated by health care providers (Blencowe et al., 2012). Higher death rates from HIV infection could relate to deficiencies in care. Other U.S. health disadvantages may reflect some degree of inferior medical care, but empirical evidence for any such hypotheses is lacking.
Third, even conditions that are treatable by health care have many origins, and causal factors outside the clinic may matter as much as the benefits or limitations of medical care. For example, smoking and obesity are heavily influenced by the environment and policy decisions (see Chapters 5 and 7). Physicians play an important, but marginal, role in screening for unhealthy behaviors, measuring body weight, prescribing adjunctive pharmacotherapy to support smoking cessation or weight management, performing bariatric surgery for morbid obesity, and referring patients to telephone quit lines and other intensive behavioral counseling programs (Fielding and Teutsch, 2009; Ogden et al., 2012b; Woolf et al., 2005). Physicians can write prescriptions for antihypertensive drugs, statins, oral contraceptives, and antibiotics and antiretroviral agents for sexually transmitted infections and HIV infection. They can encourage healthy behaviors, but other factors exert greater influences on diet, physical activity, sexual habits, alcohol and other drug use, and needle exchange practices (Woolf et al., 2011). Pediatricians can remind parents to secure their children in car seats, but they cannot control motor vehicle crashes. Physicians can screen for and treat depression and be alert for suicidal ideation and signs of family violence but they have limited influence on the prevalence of firearms or the societal conditions that precipitate crime and violence.
One difficulty in attributing the U.S. health disadvantage to deficiencies in the public health or medical care system is that countries with better health outcomes lack consistent evidence that their systems perform better. In some countries, patients are more likely to report problems. For example, Sweden consistently ranks among the healthiest countries in the OECD, but, in the Commonwealth Fund surveys, its patients were more likely than U.S. patients to report problems with chronic illness care. Sweden has high hospitalization rates for uncontrolled diabetes (Figure 4-4). In 2007, Switzerland had the highest male life expectancy among the 17 peer countries (see Table 1-3, in Chapter 1), but the availability of general practitioners is the second lowest (see Figure 4-1). Australia has the second highest male life expectancy of the peer countries (see Table 1-3, in Chapter 1), but it has the fifth highest case-fatality rate for ischemic stroke (OECD, 2011b). The Netherlands, which ranks highly on many surveys by the Commonwealth Fund, has historically had shorter life expectancy than some other comparable countries.
Various potential explanations could account for these inconsistencies. The simplest is that medical care matters little to health, a thesis that some have advanced as part of a more general argument that health is shaped primarily by the social and physical environment. Indeed, some studies have already questioned whether there is specific evidence to implicate the health care system as the cause of the U.S. mortality disadvantage after age 50 (Ho and Preston, 2010; National Research Council, 2011).23
A second possibility is that health care does matter but that only certain aspects affect outcomes. For example, deficiencies in mammography screening or printing medication lists may not matter, and countries with consistently superior health outcomes may excel in the facets of health care that are consequential. Health care may also matter more in certain places or for certain patient populations.
A third explanation—which the panel deems most likely—is that health care exerts a partial influence on health outcomes in concert with other important determinants of health such as lifestyle, socioeconomic status, and public policy. Longer life expectancy and improved health is probably traceable to some combination of health system characteristics and these
_________________
23That study focused on the population age 50 and older, for whom deficiencies in medical care in the United States may be less of an issue because of Medicare, which serves adults age 65 and older and the disabled. The study also examined a smaller set of indicators than are reviewed in this chapter, and based on those indicators, found little evidence to suspect that the quality of health care was responsible for the growing mortality disadvantage among older Americans compared with seniors in other countries.
other individual and community conditions, but the exact contribution of each factor is unknown and may vary over place and time.
A life-course perspective adds additional complexity to the analysis because differences in health outcomes may relate not only to contemporaneous characteristics of health systems, but also to those that existed years earlier when current conditions or diseases were developing. This scenario is especially true for chronic diseases like diabetes and heart failure, which claim lives decades after problems with cardiovascular risk factors and glycemic control first appear. For such conditions, deficiencies in primary care in the 1970s and 1980s may explain current death rates better than the features of today’s health systems. The current health system matters more for care conditions that lead directly to health outcomes, such as birth outcomes and survival after a car crash or gunshot wound.
The research comparing health care systems cross-nationally is still evolving and cannot yet support any definitive conclusions about how the U.S. health system might contribute to or ameliorate the U.S. health disadvantage. Comparable international data for meaningful inferences require better data on both dependent (health outcomes) and independent variables (health systems). Although data from the OECD and WHO provide some comparative information on a handful of health system measures, these are much like the keys under the lamppost. A richer and more comprehensive set of data on a variety of carefully selected dimensions of morbidity and mortality and outcomes of care would be needed across countries to make valid comparisons.24
Few indicators for assessing the various dimensions of health care have been developed or undergone proper scientific validation. In particular, questions used on surveys such as those conducted by the Commonwealth Fund, which are widely cited in this chapter, have unknown correlations with health outcomes and may have variable meanings across countries. Limitations in statistical power and wide confidence intervals may limit the significance of rankings between one country and another or changes in ranking from year to year. Some questions used by the Commonwealth Fund change from year to year; these changes offer new insights on health systems, but they make it difficult to compare outcomes across time. The Commonwealth Fund gives equal weight to each measure; some weighting is probably warranted, but an empirical basis is lacking to know which characteristics patients value more highly or are more predictive of health outcomes.
Even the proper domains for assessing the performance of health systems
_________________
24Such data are lacking even within the United States. A recent Institute of Medicine (2011e) report indicated the lack of adequate data to evaluate the health of the American public or the performance of governmental public health agencies and recommended bold transformation of the nation’s health statistics enterprise.
have yet to be identified. In the first major attempt to rank health care systems, the WHO World Health Report 2000 introduced a ranking based on health attainment, equity of health outcomes, “patient responsiveness,” and “fairness of financial contributions” (World Health Organization, 2000b). The U.S. health system ranked 37th based on this methodology, but the measures, methods, and data were criticized (Jamison and Sandbu, 2001; Navarro, 2002). Another such effort is that of the Commonwealth Fund, which established a Commission on a High Performance Health System in 2005 that regularly issues a “national scorecard” based on five dimensions: quality, access, efficiency, equity, and long, healthy, and productive lives (Commonwealth Fund Commission on a High Performance Health System, 2011). In 2008, WHO identified five shortcomings in health care delivery that are found in systems around the world: inverse care, impoverishing care, fragmented and fragmenting care, unsafe care, and misdirected care (World Health Organization, 2008b). International health experts have not reached consensus on the optimal parameters for measuring and tracking the performance of national health systems.
Statistics for all these dimensions are difficult to capture. The capacity of different countries to collect appropriate data and to do so -systematically—using consistent sampling procedures, data collection techniques, coding practices, and measurement intervals (e.g., annually)—is challenging for practical reasons and limited budgets. To cite just one example, patient safety indicators for hospital care are not standardized across countries (Drösler et al., 2012). Access to medical records or administrative data is uneven across countries. International surveys face methodological challenges that introduce sampling biases. One example is survey methodology: some surveys have used a combination of landlines and mobile telephones to conduct interviews, and some countries have low response rates or mobile telephone usage. Adults with complex conditions, low income, or language barriers may be undersampled. Surveys of patients or physicians’ perceptions of the quality of care are ultimately perceptions and may not correspond with objective measures. The research challenges and priorities to address these gaps in the science are discussed further in Chapter 9, along with recommendations to remedy the problem.
Despite these limitations, the existing evidence is certainly sufficient for the panel to conclude that public health and medical systems in the United States have important shortcomings, some of which appear to be more pronounced in the United States than in other high-income countries. Subsequent chapters address the factors outside the clinic that may lead to greater illness and injury among Americans, but health problems ultimately lead most people to the health care system, or at least to attempt to obtain clinical assistance. The difficulties Americans experience in accessing these services and receiving high-quality care, as documented in this chapter, cannot be ignored as a potential contributor to the U.S. health disadvantage.
































