SCREENING, ASSESSMENT, AND TREATMENT
![]()
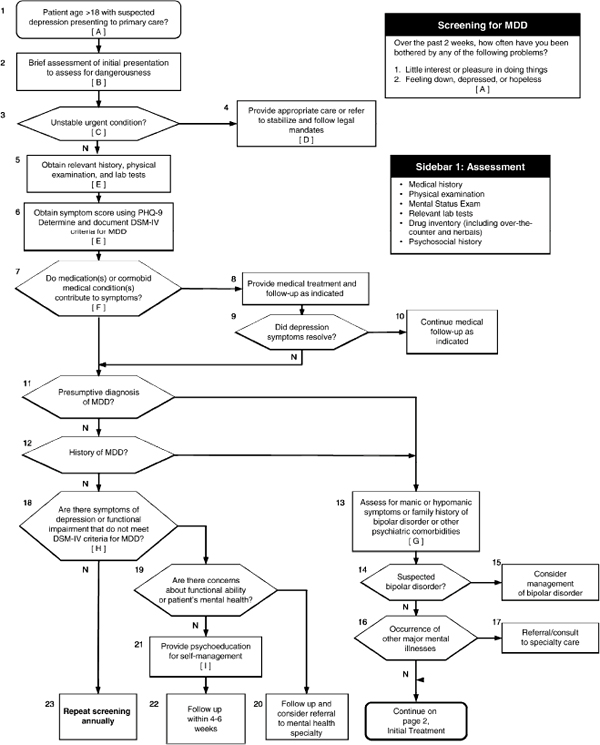
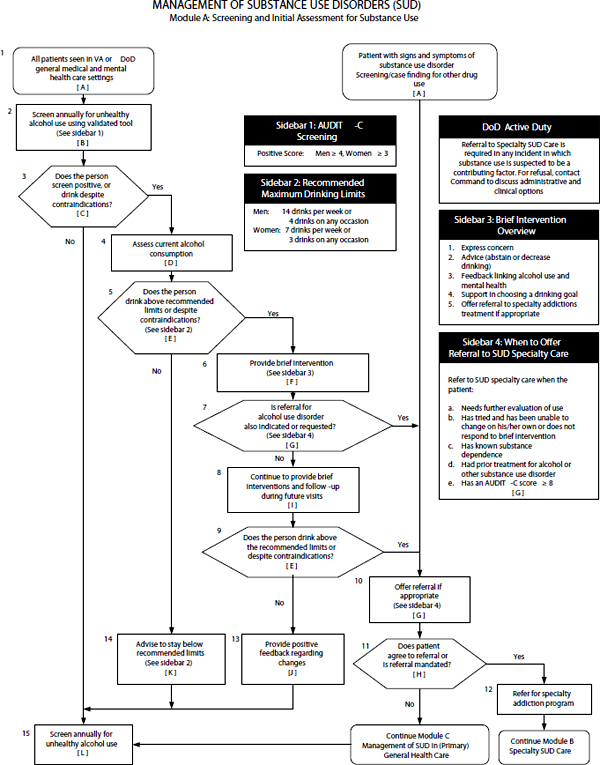
In this chapter, the committee assesses the approaches used in the Department of Defense (DOD) and Department of Veterans Affairs (VA) to identify service members and veterans with neurologic or psychologic health conditions and treat them. The committee reviews health screening and assessment practices and treatment interventions for six conditions that can affect readjustment after military deployment: traumatic brain injury (TBI), posttraumatic stress disorder (PTSD), major depressive disorder (MDD), substance-use disorders (SUDs), suicidal ideation, and comorbid conditions. Their assessment relies on clinical and scientific evidence to examine the efficacy of approaches that DOD and VA use in the management of those conditions.
The committee reviewed the clinical practice guidelines (CPGs) developed jointly by VA and DOD1 and compared them with clinical guidelines developed by leading scientific and professional organizations. CPGs are statements and recommendations for clinical care that are informed by a systematic review of evidence and an assessment of the benefits and harms of alternative care options (IOM, 2011a). The committee also reviewed the research and policy literature as a basis for discussing standard-of-care recommendations that are presented throughout this chapter.2
The committee acknowledges that the presence of clinical guidelines does not ensure that people receive optimal evidence-based care. Poor dissemination practices and other barriers affect the extent to which clinicians use CPGs (Stein et al., 2009). The committee examined the sparse data available to address the question of whether military members and veterans actually receive evidence-based interventions offered in the VA and DOD health systems. Our inquiries to VA and DOD did not yield much about results of using clinical performance measures, metrics that are designed for assessing and monitoring clinical processes or patient outcomes.
The committee became aware of a few sources of clinical performance measures relevant to VA’s monitoring of mental-health care delivery and discusses this information in each section. For example, the VA Office of Quality and Performance contracts with an external agency to
__________________
1Under the auspices of the VA/DOD Evidence Based Practice-Guidelines Work Group, representatives of VA and DOD serve on committees for developing, updating, and implementing joint CPGs for a number of physical- and mental-health conditions. VA/DOD joint guidelines exist for TBI, PTSD, MDD, and SUD but not for suicidal ideation and comorbid conditions.
2The literature review concentrated on new studies since publication of the CPGs and on synthesized analyses of randomized controlled trials.
conduct monthly standardized medical-record reviews of outpatient care as part of the External Peer Review Program and uses the data to monitor according to national performance measures. In addition, much of the data on implementation and monitoring of evidenced-based practices included in this chapter comes from an independent evaluation of the quality of VA mental-health and substance-use care. VA commissioned the RAND Corporation and Altarum Institute to perform the evaluation, which they conducted between 2006 and 2010 (Watkins and Pincus, 2011). The study was authorized by the Government Performance and Results Act of 1993 and Title 38 of the US Code, which require independent evaluations of large government programs. In general, studies have shown that the health care that VA provides for a number of conditions, such as diabetes and heart disease, is on par with or better than care provided in non-VA settings (Jha et al., 2003; Trivedi et al., 2011). However, as discussed in this chapter, VA’s performance in mental health is not as strong, given the variation found among service networks and the low rate of delivery of some evidence-based practices (Watkins et al., 2011).
DOD has an extensive centralized Military Health System–wide database for population health management called the Military Health System Population Health Portal.3 However, clinical performance measures in the dataset do not address mental-health care. In 2010, the Defense Health Board recommended to the assistant secretary of defense for health affairs that “evidence-based metrics for processes of mental health care” should be developed and monitored to address questions of mental health care quality and adequacy of clinical capacity/resources (Defense Health Board, 2010). The Defense Health Board added that DOD should evaluate clinician competence in providing evidence-based treatment and patience adherence to treatment.
As VA and DOD continue to advance their efforts to evaluate mental-health care services, they face a number of challenges, such as the lack of validated clinical performance measures that assess the full array of psychologic health services and the lack of appropriate benchmarks that VA and DOD can use to compare their performance. Measurement of clinical performance is not as advanced in mental health as it is in other types of care (Pincus et al., 2011; Watkins et al., 2010). That potentially presents opportunities for VA and DOD to collaborate with each other and with others in the field to advance clinical performance measurement aimed at improving the quality of mental health care and care for brain injury.
ORGANIZATION OF THE CHAPTER
The chapter is organized in six main sections: TBI, PTSD, MDD, SUDs, suicidal ideation, and comorbid conditions. By structuring the chapter according to each condition, the committee does not mean to suggest that it is always the case that a single diagnosis can account for all symptoms or that a single set of clinical guidelines and evidenced-based treatments will address all symptoms. Many patients, particularly in military settings, present with complex problems that do not fall neatly into single diagnostic categories. Comorbid, co-occurring, and dual diagnosis are terms used to indicate that more than one disorder is occurring in the same person, simultaneously or sequentially, and that associated interactions between the illnesses affect the course and prognosis of each. This chapter uses the terms comorbid and co-occurring.
__________________
3The Military Health System Population Health Portal contains administrative health care data on TRICARE Prime/Plus enrollees who receive care through military treatment facilities and contracted providers.
Each section presents screening, assessment, and treatment interventions. In this chapter, screening refers to a process for identifying people who may be at risk for a specific disease that uses tests (or screening instruments), examinations, or other procedures. Screening instruments are helpful for identifying people who might have a disease but are not very useful for assessing progression, prognosis, or treatment efficacy (IOM, 2006). A person who has positive screening results should be referred for assessment by a medical professional for diagnosis and treatment. Assessment refers to a process for defining the nature of a problem, determining a diagnosis, and developing recommendations for addressing the problem or diagnosis (SAMHSA, 2009).
Within the discussion of screening, assessment, and treatment, the chapter describes the VA and DOD clinical guidance and practices used in the management of the selected conditions. The chapter often refers to screening processes achieved in the US military during the deployment cycle—the predeployment health assessment, the Post-Deployment Health Assessment (PDHA), and the Post-Deployment Health Re-Assessment (PDHRA) (Terrio et al., 2011). Predeployment health assessments are administered at home stations or at mobilization processing stations before deployment. The PDHA is conducted 3–10 days after deployment, and the PDHRA 90–180 days after deployment. On return from deployment, service members are required to complete assessment forms that ask about their deployment history and that screen for a number of physical and psychologic conditions, including TBI, PTSD, MDD, SUDs, and suicidal ideation. Health care providers followup with all service members on completion of the forms to make referrals to appropriate health care or community-based services if further evaluation or treatment is needed.
For each health condition, there is a discussion of the evidence underlying the validity of the screening and assessment instruments used by VA and DOD health practitioners. A review of treatment interventions includes a comparison of the VA and DOD recommended practices with recommendations in other relevant CPGs. Finally, we present information available on the extent to which VA and DOD are implementing evidenced-based interventions for screening, assessment, and treatment.
TRAUMATIC BRAIN INJURY
A TBI is the result of a blow or jolt to the head or a penetrating head injury that disrupts the function of the brain. In 2007, DOD formally defined TBI as a “traumatically induced structural injury or physiological disruption of brain function as a result of an external force” (DCoE, 2012e). Such an injury may range from “mild”—a brief change in mental status or consciousness—to “severe,” an extended period of unconsciousness or amnesia after the injury. The terms concussion and mild TBI are used interchangeably. See Chapter 4 for a full definition of TBI and for details about its prevalence in the military and veteran populations.
Numerous symptoms are associated with mild TBI, including headaches, dizziness, fatigue, inability to concentrate, memory problems, irritability, balance problems, vision change, and sleep disturbance. Most people who sustain a mild TBI usually recover completely with minimal intervention. A TBI classified as moderate or severe can result in short-term or longterm problems with independent function (IOM, 2009). As discussed in Chapter 4, TBIs of all severities, including a small fraction of mild cases, are known to be associated with adverse long-term neurologic outcomes, such as seizures, cognitive dysfunction, and neurodegeneration. The military emphasizes early assessment for TBI on the battlefield in recognition that delayed
diagnosis might be detrimental to a service member’s health and combat readiness (DOD, 2010b; Helmick, 2011).
To assess the efficacy of current screening and treatment approaches for mild TBI, the committee examined a number of clinical guidelines and DOD and VA policy directives for TBI. This section’s emphasis is on mild TBI, inasmuch as such cases are the most common and the most frequently underrecognized and undertreated.
Department of Defense and Department of Veterans Affairs Guidance for Screening for Mild Traumatic Brain Injury
Detecting mild TBI close to the time of injury is best for preventing symptoms, optimizing care, and improving outcomes; however, mild TBI can be difficult to identify. The rigor of combat operations and lack of observable head trauma may delay assessment. In addition, identifying a head injury often relies on self-reported symptoms, but service members may be reluctant to report symptoms because they do not want to be separated from their unit and wish to avoid any stigma associated with psychologic or psychiatric services. Moreover, the frequent presence of comorbid conditions, such as PTSD, complicates recognition of mild TBI based on symptoms alone.
DOD and VA have system wide screening and assessment procedures in place at multiple points of care to identify mild TBI in service members. A positive screen indicates the need for further evaluation to diagnose a TBI. Diagnosis cannot be made on the basis of a positive screening test alone.
Department of Defense
In DOD, service members may be screened for TBI in a theater of combat operations, in MTFs, and on return from theater (postdeployment). In addition to screening, DOD requires all service members to undergo a baseline neurocognitive assessment before deployment.
Neurocognitive Testing
Neurocognitive testing helps to determine the degree of cognitive impairment after head injury. In 2006, a DOD expert panel concluded that neurocognitive assessment is an important part of a TBI evaluation (DVBIC, 2006). In May 2008, DOD issued guidance requiring each service to implement baseline predeployment neurocognitive assessment for service members with the Automated Neuropsychological Assessment Metrics (ANAM) tool (Casscells, 2008a). Developed, tested, and implemented by DOD, the ANAM is a computer-based assessment of cognitive functions likely to be affected by a concussion, including attention, concentration, reaction time, memory, processing speed, and decision making (DVBIC, 2006). The ANAM is not used as a TBI screening tool itself but serves as a baseline with which a post-TBI evaluation can be compared. Service members take the predeployment neurocognitive assessment within 12 months of deployment. Injured service members can be given a second ANAM test in theater, which should be administered 24–72 hours after injury if possible, and the results are compared with the original test scores to look for changes in cognitive function (DCoE, 2011b).
DOD policy does not require that all service members receive a postdeployment neurocognitive assessment, such as one with the ANAM, but recommends that care providers in
theater consider postinjury neurocognitive testing as a component of the comprehensive TBI evaluation and return-to-duty assessment (DCoE, 2011b; GAO, 2011).
Screening in Theater and in Medical Facilities
During deployment, service members are screened for possible TBI, whether on the basis of self-reported symptoms or an event that occurred. In 2006, the Defense and Veterans Brain Injury Center (DVBIC) recommended screening service members in military operational settings (DVBIC, 2006); in the following year, the Army required screening of service members who were exposed to a blast or other injury event and had associated loss of consciousness, amnesia, or alteration in mental status, however brief (DVBIC, 2007). In June 2010, DOD broadened the screening criteria: all service members exposed to a “mandatory event”—regardless of initial symptoms—are screened for TBI and required to rest for 24 hours (DOD, 2010b). Mandatory events are defined as being in a vehicle associated with a blast, collision, or rollover; being within 50 m of a blast; a direct blow to the head or witnessed loss of consciousness; or command-directed, especially in a case with multiple blast events. The 24-hour rest period is mandatory regardless of the results of TBI screening (DOD, 2010b).
DOD’s TBI screening tool, the Military Acute Concussion Evaluation (MACE), is suitable for use in theater and in medical facilities. The DVBIC developed the MACE in conjunction with national experts in sports concussion. The MACE has history and evaluation components. The history component can confirm the diagnosis of mild TBI after it is established that trauma has occurred and that the service member experienced an alteration in consciousness. The evaluation component, designed to be used easily by medics and corpsmen in combat theater, consists of a symptom inventory and a brief assessment of neurocognitive deficits in four domains: orientation, immediate memory, concentration, and delayed recall (DVBIC, 2006, 2008a; French et al., 2008).
The MACE is also used to screen wounded service members who are evaluated in tactical medical units that provide Level III care (resuscitative care, stabilization, and hospitalization), such as the Air Force Theater Hospital in Balad, Iraq, or in definitive care (Level IV) regional medical facilities outside the area of operations, such as the Landstuhl Regional Medical Center in Germany (these two types of facilities have somewhat different procedures for following up a positive screen). Of stateside inpatient MTFs that provide comprehensive care (Level V), only Walter Reed National Military Medical Center was conducting TBI screening since 2007 (DOD, 2010b).
Postdeployment Screening
In 2008, DOD started routine screening of Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) service members for TBI immediately on their return from the combat theater and again 3–6 months after return as part of the required PDHA and PDHRA process (briefly described at the beginning of this chapter). Routine screening was not implemented until 2008, so many service members have never been screened for mild TBI (Iverson et al., 2009).
The TBI screen used in the DOD health assessments is a modified version of the Brief Traumatic Brain Injury Screen (BTBIS) (Schwab et al., 2007), which was validated by further research and adapted for use in the PDHA and PDHRA (Terrio et al., 2011). Returning service members report responses to four screening questions about exposure to an injury event, the later
loss of or alterations in consciousness, the presence of symptoms at the time of injury, and the presence of current symptoms (see questions in Box 5.1). A positive response regarding at least one problem in each of the four questions means that the screen is positive. A service member who has a positive screen is referred for a full TBI evaluation (Helmick, 2011).
BOX 5.1
TBI Screening Questions in DOD’s PDHA and PDHRA
9.a. During this deployment, did you experience any of the following events? (Mark all that apply.)
1. Blast or explosion (IED, RPG, land mine, grenade, etc.)
2. Vehicular accident/crash (any vehicle, including aircraft)
3. Fragment wound or bullet wound above your shoulders
4. Fall
5. Other event (for example, a sports injury to your head). Describe:
9.b. Did any of the following happen to you, or were you told happened to you, IMMEDIATELY after any of the event(s) you just noted in question 9.a.? (Mark all that apply.)
1. Lost consciousness or got “knocked out”
2. Felt dazed, confused, or “saw stars”
3. Didn’t remember the event
4. Had a concussion
5. Had a head injury
9.c. Did any of the following problems begin or get worse after the event(s) you noted in Question 9.a.? (Mark all that apply.)
1. Memory problems or lapses
2. Balance problems or dizziness
3. Ringing in the ears
4. Sensitivity to bright light
5. Irritability
6. Headaches
7. Sleep problems
9.d. In the past week, have you had any of the symptoms you indicated in 9.c.? (Mark all that apply.)
1. Memory problems or lapses
2. Balance problems or dizziness
3. Ringing in the ears
4. Sensitivity to bright light
5. Irritability
6. Headaches
7. Sleep problems
SOURCE: DOD, 2008.
Department of Veterans Affairs
In April 2007, VA started screening all OEF and OIF veterans who were receiving medical care in the Veterans Health Administration (VHA) for TBI; those who screen positive are offered further evaluation and treatment by clinicians who have expertise in TBI (VA, 2010c; VA and VHA, 2007). VHA’s screening tool, the Traumatic Brain Injury Screening Instrument (TBISI), has four questions based on the BTBIS, the tool designed for active-duty military personnel (Carlson et al., 2010); see questions in Box 5.2.
Box 5.2
TBI Screening Questions in VA’s TBISI
Section 1: During any of your OEF and OIF deployment(s), did you experience any of the following events? (Check all that apply.)
1. Blast or explosion
2. Vehicular accident/crash (including aircraft)
3. Fragment wound or bullet wound above shoulders
4. Fall
Section 2: Did you have any of these symptoms IMMEDIATELY afterwards? (Check all that apply.)
1. Losing consciousness/ “knocked out”
2. Being dazed, confused or “seeing stars”
3. Not remembering the event
4. Concussion
5. Head injury
Section 3: Did any of the following problems begin or get worse afterwards? (Check all that apply.)
1. Memory problems or lapses
2. Balance problems or dizziness
3. Sensitivity to bright light
4. Irritability
5. Headaches
6. Sleep problems
Section 4: In the past week, have you had any of the symptoms from section 3? (Check all that apply.)
1. Memory problems or lapses
2. Balance problems or dizziness
3. Sensitivity to bright light
4. Irritability
5. Headaches
6. Sleep problems
SOURCE: GAO, 2008.
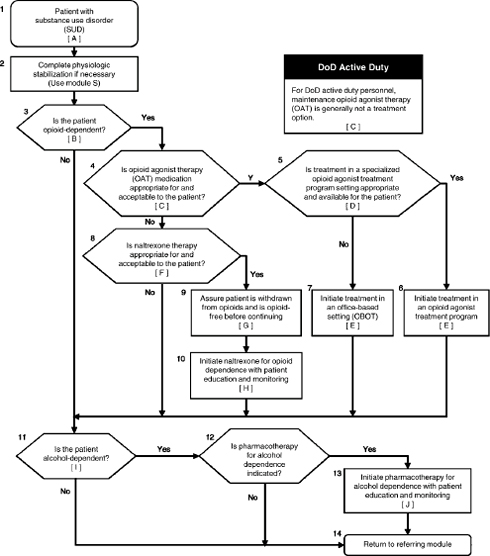
The screening process for TBI (see Figure 5.1) is executed as part of the VHA automated clinical reminder system used by clinicians at its medical facilities (Carlson et al., 2010). An
OEF or OIF veteran who reports having received a TBI diagnosis at some point is offered a referral; a veteran who reports no prior TBI diagnosis during deployment is asked to answer the four screening questions. The screen is positive if the veteran says yes to any response item in each of the four questions (GAO, 2008). A veteran who had a positive screen is offered a followup evaluation with a specialty provider at a specified medical center. VA clinicians have to document any refusal of specialty care in the veteran’s electronic medical record (VA, 2010c).
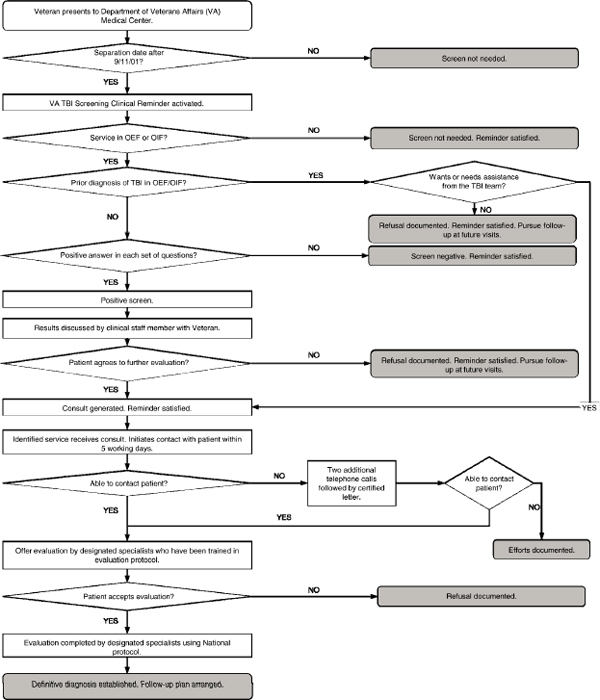
FIGURE 5.1 Flow chart for VHA screening and evaluation of possible traumatic brain injury in OEF and OIF veterans.
SOURCE: VA, 2010c.
Validity of Tools for Neurocognitive Assessment and Screening for Mild Traumatic Brain Injury
Automated Neuropsychological Assessment Metrics
A 2010 comprehensive review of the DOD ANAM program, prepared by the Army’s Office of the Surgeon General, states that the lack of clear scientific evidence supporting ANAM’s effectiveness raises important questions about whether DOD is using the best available technology to assess cognitive function after head injury (Department of the Army, 2010a). Research data raise questions about the accuracy of the ANAM for detecting cognitive dysfunction—and recovery from this dysfunction—after mild TBI.
In one study, among 956 soldiers returning from Iraq or Afghanistan, a history of selfreported mild TBI or current postconcussive symptoms was not associated with poor ANAM performance (Ivins et al., 2009). In another study, 502 service members recently deployed to Iraq or Afghanistan who had self-reported TBI and predeployment and postdeployment ANAM testing were compared with 400 service members who had no history of TBI. The two groups performed similarly on predeployment testing. Of the entire group that reported TBI during deployment, 70% had no significant change in cognitive performance compared with their baseline ANAM test (Roebuck-Spencer et al., 2012). Research is under way to address questions about the ANAM (see Appendix D). This is an important subject of study because ANAM scores are being used to inform return-to-duty decisions.
Military Acute Concussion Evaluation
Used both in theater and in medical facilities, the MACE is the most widely used TBI screen in DOD; however, there is some concern that it might fail to detect a large proportion of service members’ concussions. Embedded in the MACE is the Standardized Assessment of Concussion (SAC), a brief cognitive screening tool developed to assess the acute effects of sports-related mild TBI. The SAC has demonstrated reliability, validity, sensitivity, and specificity in athletic cohorts (McCrea et al., 2003). The MACE, however, when administered more than 12 hours after injury in a military setting and compared with a clinical diagnosis of concussion, had a sensitivity of only 51% (specificity 64%) when a cutoff score of 27 was used. At the suggested cutoff score of 25, the sensitivity was even less at 20% (specificity 88%) (Coldren et al., 2010). Research is under way to determine the validity of this tool at earlier times and to attempt to improve its accuracy through comparison with predeployment scores (see Appendix D).
Brief Traumatic Brain Injury Screen
Initial research with the BTBIS postdeployment TBI screen suggested that it was a reasonably accurate screening tool for TBI. In 2007, the BTBIS was administered to 596 soldiers returning from Iraq or Afghanistan and compared with two longer surveys—the Quarterly Survey and the Computerized TBI Questionnaire—that were used to elicit a history of TBI. The BTBIS had a sensitivity of 90% when compared with the Quarterly Survey and 88% when compared with the Computerized TBI Questionnaire. It had a specificity of 88% when compared with the Quarterly Survey and 97% when compared with the Computerized TBI Questionnaire (Schwab et al., 2007).
However, a 2011 study suggested that the false-negative rate of the DOD postdeployment TBI screen—which was adapted from the BTBIS—was high. Its four questions were compared with a brief structured clinical interview for mild TBI in 3,072 soldiers who were returning from a 15-month tour of duty in Iraq. The sensitivity and specificity of the DOD screening tool (positive response to all four items) were 60% and 96%, respectively. The sensitivity increased to 80%, with a slight decrease in specificity to 93%, when affirmative responses only to questions 1 and 2 were included. Thus, omission of the last two questions significantly reduced the false-negative rate from 40% to 20% (Terrio et al., 2011).
Traumatic Brain Injury Screening Instrument
Research on the accuracy of the TBISI, the screening tool used by VA, is emerging (VA, 2012). The Government Accountability Office (GAO) emphasized the need for empirical evidence on the sensitivity and specificity of the VA TBI screening instrument in a 2008 report (GAO, 2008). A 2010 study revealed that the test–retest reliability of the VHA postdeployment TBI screen was low. In 44 OEF and OIF veterans referred for neuropsychologic evaluation after a positive TBI screen, agreement was low between answers to the original TBI screen and rescreening 6 months later for mechanism of injury and symptoms immediately after injury but high for current symptoms (Van Dyke et al., 2010). A recent psychometric study of the TBISI involving 500 OEF and OIF veterans concluded that the instrument appears to be reliable and valid. The results showed high internal consistency (0.77) and test–retest reliability (0.80), high sensitivity (0.94), and moderate specificity (0.59) (Donnelly et al., 2011).
Implementation of Department of Defense and Department of Veterans Affairs Guidance for Screening for Mild Traumatic Brain Injury
This section presents information available to the committee on the extent to which DOD and VA are implementing and tracking screening procedures to identify possible TBI. The committee identified various sources of information but notes the lack of readily available centralized sources of data, particularly within DOD, on the numbers of people who are screened and have a positive screen.
Department of Defense
Neurocognitive Testing
More than 1 million service members had received neurocognitive tests as of September 30, 2011 (DCoE, 2012a). The ANAM is not Web-enabled, and data are not stored in a centralized database; therefore, summary statistics comparing ANAM scores before and after injury are not available.
Screening in Theater and in Medical Facilities
Over 9,000 soldiers have been screened for mild TBI in theater since August 2010 (Department of the Army, 2012). An article in the popular press reported that from January to September 2011, nearly 1,400 service members had screened positive in Afghanistan and Iraq as part of the new mandatory evaluation requirements that broadened the screening criteria (Zoroya, 2011). DOD policy requires the documentation of all service members who were exposed to potential concussive events and the development of a medical quality-assurance program and
metrics to track implementation of TBI screening procedures (DOD, 2010b). In response, US Central Command developed an automated reporting module called the Blast Exposure and Concussion Incident Report, but data have yet to be publicly released (USMedicine.com, 2012).
An article in Military Medicine raised concern about the quality of screening implementation, stating that “there is no standardized training or evaluation of administration competence on the MACE for medical providers in Iraq” (Coldren et al., 2010).
Postdeployment Screening
During FY 2009 and 2010, 2% of service members who were returning from tours of duty screened positive for TBI on the PDHA, and 4% on the PDHRA (DOD, 2012). In a study of 7,909 marines of the First Marine Expeditionary Force who were returning home during 2004– 2006, 9% screened positive on the BTBIS. It appears that the investigators considered only responses on the first two questions of the screen. Of those who screened positive for TBI, 70.5% (500) were first identified with the screen (Drake et al., 2010).
Department of Veterans Affairs
VA measures the rates of TBI screening of all veterans returning from Iraq and Afghanistan who present for medical care; the VA’s Office of Quality and Performance (OQP) has set a target of screening 95% of all veterans (Sayer, 2009). From April 2007 to November 2012, over 644,000 veterans have been screened for TBI. This represents approximately 95% of those eligible for screening. Through July 2012, 127,901 (20%) of OEF/OIF/OND veterans have screened positive for TBI (Sayer, 2012).
Department of Defense and Department of Veterans Affairs Guidance for Assessment and Diagnosis of Mild Traumatic Brain Injury
There is no biologic “gold standard” for diagnosing mild TBI. On the basis of a positive TBI screen test, further clinical evaluation is needed to make a diagnosis.
Department of Defense
In DOD, the level of the medical care facility determines the nature of the assessment. In Level I and II facilities in theater, MACE screening results are used to determine the disposition of service members. Those who screen negative can return to active duty after 24 hours of rest. Those who screen positive receive concussion education or management of symptoms and can return to duty when they are asymptomatic at rest and then asymptomatic after exertion but no sooner than 24 hours after injury. Service members who receive a diagnosis of a second concussion in a 12-month period must rest for 7 days. Service members who suffer three or more concussions in a 12-month period cannot return to duty until a Recurrent Concussion Evaluation is completed by a neurologist or other qualified licensed provider who is knowledgeable about concussion. The evaluation includes the Neurobehavioral Symptom Inventory, the Acute Stress Disorder Questionnaire, a vestibular assessment, and neurobehavioral testing (no specific instrument is recommended). Neuroimaging (with computed tomography [CT] or magnetic resonance imaging) and a functional assessment are initiated at the discretion of the health care provider (DOD, 2010b).
In Level III and IV facilities, those who screen positive are referred to a TBI specialty center if they are still symptomatic; they are then evaluated by a trained nurse or physician (Dempsey et al., 2009). In Level V facilities, those who screen positive get education, PTSD or acute stress disorder (ASD) screening, neuroimaging, and basic cognitive testing (DOD, 2010b).
Department of Veterans Affairs
VA policy dictates that service members who screen positive be referred for a comprehensive TBI evaluation by a specialized team in VA’s Polytrauma–TBI system of care (VA, 2010c). The Comprehensive TBI Evaluation includes the origin or etiology of the patient’s injury, assessment for neurobehavioral symptoms (with the 22-question Neurobehavioral Symptom Inventory), a targeted physical examination, and a followup treatment plan. All TBI evaluations and diagnostic conclusions are documented with an electronic Comprehensive TBI Evaluation template (VA, 2010c).
Comparison of Guidelines for Assessment and Diagnosis of Traumatic Brain Injury
The strategy of using a brief TBI screen followed by a confirmatory evaluation in those who screen positive is particular to DOD and VA guidelines. Current civilian guidelines use selfreporting of injury mechanisms and symptoms as the sole means to trigger a diagnostic evaluation (CDC, 2003). The use of a separate screening process for those at risk is not addressed in civilian guidelines. Because neuroimaging studies are often used in the evaluation of civilian mild TBI—to exclude other diagnoses—guidelines for their use have been recommended (Holm et al., 2005; Jagoda et al., 2009; NICE, 2007).
The DOD in-theater TBI guidelines use the American College of Emergency Physicians (ACEP) recommendations for head CT scanning. Head CT scanning is recommended in headtrauma patients who suffer loss of consciousness or posttraumatic amnesia and have one or more of the following: headache, vomiting, age over 60 years, drug or alcohol intoxication, deficits in short-term memory, physical evidence of trauma above the clavicle, posttraumatic seizure, focal neurologic deficit, and coagulopathy. However, because most in-theater mild TBI involves blast and the ACEP guidelines were based on cohorts that were not injured by blasts, it is unclear how fully the ACEP guidelines identify clinically significant brain injury in military settings.
Civilian studies have suggested that comparison of preinjury baseline and postconcussion performance on neuropsychologic tests is the most sensitive and objective method for detecting the presence and resolution of cognitive postconcussion symptoms (Erlanger et al., 1999).
Implementation of Department of Defense and Department of Veterans Affairs Guidance for Assessment and Diagnosis of Mild Traumatic Brain Injury
This section presents information available to the committee on the extent to which DOD and VA conduct followup and evaluation of service members and veterans who have positive TBI screens. The committee notes the lack of readily available, centralized sources of data within the DOD about the implementation of TBI assessment processes and the need for improved followup and evaluation of veterans who might have TBI.
The committee was unable to identify data on the number of service members that received comprehensive TBI evaluation because of a positive TBI screen or other clinical indication in either in-theater or postdeployment settings. In a recent report to Congress, DOD reported that systems for documenting and tracking potentially concussive events would allow DOD to obtain data to facilitate proper identification of and care for service members who are at risk for mild TBI (DOD, 2012).
Department of Veterans Affairs
As of July 2012, 50,869 of the 127,901 OEF/OIF/OND veterans who screened positive received a confirmed diagnosis of TBI on the basis of a comprehensive TBI evaluation (7.9% of the total number who were screened) (Sayer, 2012).
VA implemented two performance measures to evaluate the degree to which veterans who have positive TBI screens are followed up and evaluated. One measure assesses whether veterans who have positive TBI screens are contacted within 14 working days to schedule a comprehensive evaluation for TBI; 84% of all cases is set as the target rate. The other measure assesses whether veterans have the comprehensive evaluation for TBI completed within 30 days of a positive screen; 75% of all cases is set as the target rate (Sayer, 2012).
Data suggest that VA needs to improve the rate of followup evaluations of those who screen positive for TBI. The rate of completion for comprehensive TBI evaluations varies considerably at the facility level. The rate of followup evaluation ranges from 48% to 99%, and the TBI diagnosis rate in those who screened positive ranges from 21% to 91% (Sayer, 2012). In an evaluation of a TBI screening program in one VA medical center, 52% of OEF and OIF veterans who had positive TBI screens had later appointments in a TBI polytrauma specialty clinic within 18 months of TBI screening (Sayer et al., 2011). Moreover, a 2008 GAO report found that some providers reported difficulties in implementing electronic requests for followup evaluations and did not always use a symptom checklist—to assess the presence and severity of symptoms associated with mild TBI—during followup evaluations (GAO, 2008).
Department of Defense and Department of Veterans Affairs Guidance for Treatment for Mild Traumatic Brain Injury
The DVBIC published its recommendations for the Acute Management of Mild TBI in Military Operational Settings in 2006 (DVBIC, 2006) and updated them in 2008 (DVBIC, 2008b). The guidelines make recommendations in four aspects of care for mild TBI: symptom management, rest or return to duty, educational initiatives, and supportive therapies. The guidelines recognize that strong evidence supporting the use of pharmacologic treatment of patients for mild TBI is lacking; however, it provides some guidance on which medications to use for common mild-TBI complaints (such as headache). The overall treatment strategy relies on obtaining an initial symptom inventory first. Physical examination, later testing, and treatment options are then dictated by the particular symptoms endorsed by the service member. The guidelines recommend that treatment for mild TBI be managed with the guidance of an interdisciplinary team and that referrals for physical therapy, occupational therapy, speech and language therapy, pharmacy, audiology and vestibular care, and optometry be made when appropriate. They also recommend that coping strategies, stress management, and avoidance of
excessive alcohol and drugs be communicated via patient education. Finally, they note that duty restrictions for service members who have TBI should be considered to protect them from risk of secondary injury or reexposure. For example, in the subacute phase (over 7 days), symptomatic patients should be considered for limited duty hours.
VA/DOD Clinical Practice Guideline: Management of Concussion/Mild Traumatic Brain Injury (VA and DOD, 2009b) was designed to provide guidance for treatment more than 7 days after mild TBI. The guidelines contain evidence-based recommendations for management at initial presentation, treatment for specific symptoms, and management of persistent symptoms. They also recommend patient education, screening for the presence of comorbid psychiatric problems (such as depression, PTSD, and SUD), and medications to treat for symptoms, such as headaches, depression and anxiety, and sleep disturbances.
The Defense Centers of Excellence for Psychological Health & Traumatic Brain Injury (DCoE) Case Management of Concussion/Mild TBI provides guidelines for managing postconcussive symptoms that last longer than about 4–6 weeks (DCoE, 2010). Case management for this subset of concussed service members entails identifying barriers to a service member’s successful return to duty and assisting in developing a recovery care plan. That may involve education, facilitating medical appointments, and acting as liaison between the service member and VA.
Comparison of Guidelines for Treatment for Mild Traumatic Brain Injury
In addition to the guidelines promulgated by VA and DOD, guidelines for treatment for civilian mild TBI have been published by the Ontario Neurotrauma Foundation (ONF) (Ontario Neurotrauma Foundation, 2011), the East Practice Management Work Group (Cushman et al., 2001), the Scandinavian Neurotrauma Committee (Ingebrigtsen et al., 2000), and the National Institute for Health and Clinical Excellence (NICE, 2007). Guidelines for the management of concussions in athletes have been published by the International Conference on Concussion in Sports (Aubry et al., 2002; McCrory et al., 2005, 2009), the American Academy of Neurology (AAN) (American Academy of Neurology, 1997), the Canadian Academy of Sports Medicine (Canadian Academy of Sport Medicine Concussion Committee, 2000), and McGill (Johnston et al., 2001). There is substantial overlap between those guidelines and the VA/DOD guidelines for treatment for mild TBI (see Table 5.1). All indicate that the vast majority of mild TBI cases will resolve within 7 days to 3 months (McCrea et al., 2003).
The greatest distinction among the guidelines is related to the timeframe after the injury (see Table 5.1). Some deal only with the acute phase (up to 1 week after injury), whereas others deal with the subacute phase (day 7 to 4–6 weeks after injury) or the chronic phase (more than 4– 6 weeks after injury). There are some minor distinctions among the guidelines regarding treatment for headache. Headache is the most prominent symptom after mild TBI, occurring in 30%–90% of patients (Bazarian et al., 1999). All guidelines that address posttraumatic headache recommend pharmacotherapy, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or amitriptyline, but some guidelines, such as those promulgated by the DCoE and the ONF, distinguish between tension headaches and migraine headaches; NSAIDs are recommended for tension headaches, whereas triptans, such as sumatriptan and rizatriptan, are recommended for migraine headaches. The ONF is the only one that recommends, in appropriate circumstances, prophylactic treatment for headaches with tricyclic antidepressants, venlafaxine, tizanidine, or
other adjunctive therapies. In addition to or in lieu of pharmacologic treatments, nonpharmacologic treatment for headaches—such as sleep education, physical therapy, and relaxation—is also recommended by the DCoE and VA/DOD. The ONF cautions against overuse of headache medications because a patient may experience rebound symptoms that perpetuate headaches. All the guidelines caution against the use of narcotics to control headaches.
Memory loss, difficulty in concentrating, and difficulty in making decisions are cognitive deficits that are highly prevalent after mild TBI. Recommendations for cognition assessment and treatment are highly variable. The need for cognition assessment is articulated in all the guidelines, but there is no uniformity in which questionnaires or other measurement instruments should be used to assess the nature and degree of abnormalities. Treatment is also variable. The VA/DOD and DCOE guidelines are the only ones that provide for specific pharmacologic and nonpharmacologic interventions. The former are selective serotonin reuptake inhibitors and stimulants; the latter include reassurance, aerobic exercise, and sleep hygiene education. Finally, there is some variability regarding the specific psychiatric disorders and SUDs to assess for comorbidities (see Table 5.1).
Subspecialty Recommendations
In the period after acute evaluation of and treatment for TBI, patients who remain symptomatic are referred for subspecialty care. Recommendations for treatment of military personnel for mild TBI have been published for various aspects of management, such as the role of neuropsychology (McCrea et al., 2009), rehabilitation psychology (McCrea et al., 2009), speech and language pathology (Cherney et al., 2010), audiology (Cherney et al., 2010), treatment for persistent cognitive dysfunction (Cozzarelli, 2010), cognitive rehabilitation (Helmick, 2010), physical therapy (Weightman et al., 2010), and occupational therapy (Radomski et al., 2009). Among civilians after mild TBI, the effectiveness of psychologic treatments (Snell et al., 2009), cognitive rehabilitation (Cappa et al., 2003; NIH, 1999; Rohling et al., 2009), and drug treatment for neurobehavioral disorders (Neurobehavioral Guidelines Working Group, 2006) have all been systematically reviewed. The effectiveness of cognitive rehabilitation for TBI was examined by a DVBIC-sponsored randomized controlled trial (RCT) (Vanderploeg et al., 2008). In 2011, the Institute of Medicine (IOM) recommended continuing use of cognitive rehabilitation therapy for people who had TBI despite the need for additional research to address shortcomings in the supporting evidence (IOM, 2011b). Many of those recommendations were published after the VA/DOD guidelines were released and are not reflected in documentation reviewed by the present committee. Therefore, the committee is unable to ascertain whether VA and DOD implement the recommendations in their practice standards.
TABLE 5.1 Comparison of Department of Veterans Affairs and Department of Defense Guidelines with Other Guidelines for Mild Traumatic Brain Injury
| Aspect of Care | VA/DOD | DVBICa | DCOEb | ONFc | 3rd ICC Sportsd | NICEe |
| Target population | Military, postdeployment | Military in theater | Military | Civilians, athletes | Athletes | Civilians with mild to severe TBI |
| Postinjury period covered | Over 7 days | Acute | Over 4–V6 weeks | Acute, subacute, chronic | Acute | Acute |
| Overall treatment strategy | Comprehensive assessment, management | Testing, referral, treatment based on symptoms | Case management | Comprehensive assessment, management | Assessment, management | Assessment, management en route to and in emergency room |
| Rates level of evidence supporting the recommendations | √ | √ | ||||
| Treatment of headache | √ | √ | √ | √ | ||
| Pharmacologic, nonpharmacologic | Pharmacologic, nonpharmacologic | Including prophylactic pharmacotherapy | ||||
| Treatment of memory impairment, other cognitive symptoms | √ | √ | √ | √ | ||
| SSRI,f stimulants, nonpharmacologic methods | SSRI, stimulants, nonpharmacologic methods | Cognitive rest | ||||
| Treatment of balance problems | √ | √ | √ | |||
| Treatment of irritability | √ | √ | √ | |||
| Treatment of sleep disturbance | √ | √ | √ | |||
| Treatment of mood changes | √ | √ | √ | |||
| Aspect of Care | VA/DOD | DVBICa | DCOEb | ONFc | 3rd ICC Sportsd | NICEe |
| Indications for neuroimaging | √ | √ | √ | √ | √ | |
| Highly detailed | ||||||
| Cognitive testing? | √ | √ | √ | √ | √ | |
| Reliable, standardized | Military Acute Concussion Evaluation | Rivermead Post-Concussion Symptom Questionnaire | Maddock's questions or Standard Assessment of Concussion | |||
| Indications for referral to specialist | √ | √ | √ | √ | √ | |
| Education recommended | √ | √ | √ | √ | √ | |
| Screening recommended for other disorders? | √ | √ | √ | √ | √ | |
| Psychiatric, SUDsg | Depression, acute stress reaction | Depression, PTSD, SUDs | Depression, anxiety, PTSD, SUDs, somatoform disorder | Depression | ||
aDefense and Veterans Brain Injury Center.
bDefense Centers of Excellence for Psychological Health & Traumatic Brain Injury.
cOntario Neurotrauma Foundation.
dInternational Conference on Concussion in Sports.
eNational Institute for Health and Clinical Experience.
fSelective serotonin reuptake inhibitors.
Guidelines for Management of Severe Traumatic Brain Injury
A number of civilian guidelines exist for the management of civilians who have more severe TBI. They include guidelines by the New Zealand Guidelines Group (2006), the Scottish Intercollegiate Guidelines Network (2009), and the Brain Trauma Foundation (BTF) (Brain Trauma Foundation et al., 2007; Bullock et al., 2006; Knuth et al., 2005). The committee is uncertain about the extent to which DOD and VA are evaluating the guidelines for the evidence base to support their best-practices recommendations. For example, the BTF published a series of guidelines for several aspects of field management of combat-related moderate to severe TBI, including pain management, assessment of oxygenation and blood pressure, airway management, brain-directed pharmacologic interventions, use of the Glasgow Coma Scale, triage and transport, and fluid resuscitation (Knuth et al., 2005). The BTF also published guidelines for several aspects of the management of civilian moderate to severe TBI, including steroids, nutrition, deep-vein thrombosis prophylaxis, hyperventilation, sedation, antiseizure prophylaxis, blood pressure and oxygenation, brain-oxygen monitoring, hyperosmolar therapy, intracranialpressure monitoring, infection prophylaxis, cerebral perfusion, and hypothermia (Brain Trauma Foundation et al., 2007). The BTF published guidelines related to the surgical management of epidural hematoma, subdural hematoma, traumatic parenchymal lesions, posterior fossa mass lesions, and depressed cranial fractures (Bullock et al., 2006). The AAN published guidelines on the use of antiepileptic drugs after severe TBI (Chang et al., 2003).
Implementation of Department of Defense and Department of Veterans Affairs Guidance for Treatment for Traumatic Brain Injury
This section presents information available to the committee on the extent to which DOD and VA monitor and implement their treatment guidelines. The committee notes a lack of data in that regard.
Department of Defense
The committee is not aware of any metrics used by DOD to assess the extent to which the TBI guidelines are being implemented and treatments provided. DOD outlines a number of subjects in need of quality and performance metrics in its 2008 report to Congress, Comprehensive Approach to Psychological Health and Traumatic Brain Injury. Regarding surveillance, the report states that “there is a need to further develop a robust system that allows tracking and monitoring of both TBI and mental health conditions and treatment outcomes” (Casscells, 2008b). In a later report to Congress, DOD reported its work with the VA on standardizing TBI-related diagnosis codes to facilitate proper diagnosis and tracking of clinical outcomes (DOD, 2011a). In that report, DOD described plans for a clinical-outcomes project in which standardized outcome assessments (functional status and quality of life) are administered to mild-TBI patients at intake, on discharge, and at predetermined followup times. The objective is to relate patient outcome with specific clinical practices and programs to determine clinical best practices (DOD, 2011a).
Department of Veterans Affairs
To support the implementation of the 2009 VA/DOD CPG for managing concussion and mild TBI, various educational interventions—including noninteractive Web-based education—have been implemented (DCoE, 2011e). However, the committee in not aware of the existence of performance measures related to the guidelines (Sayer, 2009).
Summary
There are aspects of VA’s and DOD’s screening, assessment, and treatment interventions for mild TBI for which questions of efficacy and effectiveness have not been conclusively answered. Scientific evidence supporting ANAM’s effectiveness in the assessment of cognitive function after head injury is insufficient. Additional psychometric studies are needed on VHA’s TBI screening tool that are based on military cohorts. Studies are also needed to address the extent to which DOD’s use of civilian guideline recommendations for head CT scanning identify clinically significant brain injury in military settings. Of the guidelines reviewed, the VA/DOD and DCOE guidelines are the only ones that provide for specific pharmacologic and nonpharmacologic interventions. RCTs are needed determine the efficacy of those interventions, for which there is not yet a strong evidence base. There is a lack of readily available, centralized sources of data on the implementation of TBI assessment processes and treatment outcomes. The limited data available suggest that there is a need for improved followup and evaluation of service members and veterans who might have TBI.
POSTTRAUMATIC STRESS DISORDER
Posttraumatic stress disorder (PTSD) can result from the direct, personal experience or witnessing of an event that poses a perceived threat of death or serious injury (APA, 2000). Symptoms that are characteristic of PTSD include reexperiencing of the traumatic event, often through intrusive thoughts, flashbacks, or nightmares; avoidance of stimuli associated with the trauma; numbing of emotions; and hyperarousal, often manifested by difficulty in sleeping and lack of concentration. For a diagnosis of PTSD, symptoms of acute stress must persist for at least a month and cause substantial impairment in important aspects of daily life (IOM, 2006). (Chapter 4 presents the diagnostic criteria for defining PTSD and data on its prevalence in the military and veteran populations.)
PTSD can be difficult to diagnose and treat. No objective measure can confirm a diagnosis of PTSD; diagnosis ultimately rests on a careful and comprehensive clinical evaluation performed by a qualified professional (a psychologist, social worker, psychiatrist, or psychiatric nurse practitioner) under conditions of privacy and confidentiality (IOM, 2012). Determining appropriate treatment can be complicated because PTSD presents with varied psychosocial morbidity and functional impairment and is often comorbid with other psychiatric disorders, particularly SUD, major depression, and mild TBI. In addition, fear of negative consequences for a military career and the perceived stigma associated with mental-health problems may discourage service members and veterans from seeking treatment (Hoge et al., 2004; Nash et al., 2009).
To assess the efficacy of current screening, assessment, and treatment approaches for PTSD in DOD and VA, the committee reviewed the 2010 VA/DoD Clinical Practice Guideline
for the Management of Post-Traumatic Stress (VA and DOD, 2010). The guideline documents evidence-based procedures for assessment and diagnosis of and treatment for posttraumatic stress in adults who are treated in any DOD or VA clinical setting. The committee compared key aspects of the recommended practices in the VA–DOD guideline with state-of-the-art clinical guidelines (reviewed later in this chapter) and evidence in the literature on the management of PTSD.
A substantial contribution to the body of literature on PTSD that is reflected in the present report is the recently published IOM report Treatment for Posttraumatic Stress Disorder in Military and Veteran Populations: Initial Assessment (IOM, 2012). In response to a congressional mandate to assess PTSD programs and services in DOD and VA, the Committee on the Assessment of Ongoing Efforts in the Treatment of Posttraumatic Stress Disorder conducted a thorough synthesis of evidence related to many aspects of PTSD. Its report covers the history, diagnostic criteria, epidemiology, and neurobiology of PTSD. It summarizes the DOD and VA health care systems and examples of PTSD programs and services offered and their prevention of and screening approaches for PTSD, including the tools and instruments most commonly used by DOD and VA. The report evaluates the evidence supporting the many options for PTSD treatment, including treatment for PTSD comorbid conditions and novel interventions. Findings from that report are discussed in this chapter.
Prevention of Posttraumatic Stress Disorder
DOD supports a number of programs that are aimed at preventing the development of PTSD by building resilience and helping service members to anticipate some of the traumatic events that they may experience in a combat zone. For example, Army prevention programs include Battlemind and, most recently, the Comprehensive Soldier Fitness program that will be used for all Army personnel before deployment (Brusher, 2011; Casey, 2011). All four services have a variety of programs to help service members who have symptoms of PTSD to avoid chronic PTSD. VA attempts to prevent chronic PTSD by working with veterans who have symptoms and has programs that help veterans with PTSD to regain functioning in civilian life and to prevent further PTSD-related disability (IOM, 2012).
After examining prevention of and prophylaxis for PTSD in active-duty and veteran populations, the IOM Committee on the Assessment of Ongoing Efforts in the Treatment of Posttraumatic Stress Disorder concluded that “while there are a variety of DoD and VA programs that target PTSD prevention, it is important to note that, at present, none of them has evidence for their effectiveness in preventing or reducing PTSD or stress in service members or their families” (IOM, 2012). This committee agrees with that conclusion and with the need that the report highlights for systematic evaluation of such programs, ideally before widespread implementation.
Provision of Services for Posttraumatic Stress Disorder
DOD provides PTSD services to service members in numerous programs, and settings, including counseling centers, general inpatient and outpatient mental-health services, and specialized treatment programs. PTSD care for service members includes programs that are DOD-wide and programs that are specific to the Army, Air Force, Navy, Marine Corps, reserves, or National Guard. Treatment for PTSD in DOD is provided by a variety of health professionals
in the theater of war and in other settings on and off base. Many service members who have a diagnosis of PTSD receive counseling, medication, or both in an outpatient setting through a mental-health department (IOM, 2012).
VA provides PTSD services in VHA hospitals, outpatient clinics, community-based outpatient clinics (CBOCs), and Vet Centers. In addition, VA pays for some care delivered through outside providers. PTSD treatment delivered in outpatient clinics and CBOCs is through either general mental-health clinics or, less commonly, specialized programs provided by PTSD clinical teams, substance-use PTSD teams, and women’s stress-disorder treatment teams. Hospitalizations for PTSD include both traditional inpatient stays and specialized programs involving short residential stays; the latter involve counseling and treatment with social, vocational, and recreational therapies (CBO, 2012).
Department of Defense and Department of Veterans Affairs Guidance for Screening for Posttraumatic Stress Disorder
Evidence suggests that identifying PTSD early and referring people to treatment can decrease symptoms and lessen the severity of functional impairment (VA and DOD, 2010). PTSD screening instruments help to identify people who have PTSD symptoms and inform decisions about who should receive a full diagnostic assessment by a health professional. A diagnosis of PTSD cannot be made on the basis of a positive screening test alone.
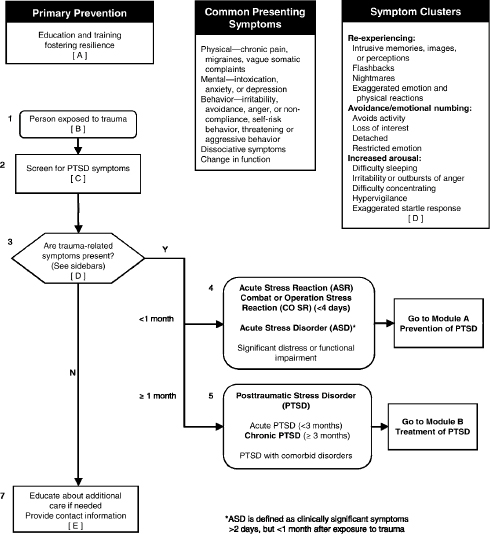
The VA/DOD guideline specifies that all new patients be screened for symptoms of PTSD and then rescreened annually or more frequently if it is clinically indicated by clinical suspicion, recent trauma exposure, or history of PTSD. Figure 5.2 shows the process for initial evaluation and triage of patients who might have PTSD in a primary care setting as presented in the VA/ DOD guideline.
The guideline endorses the use of validated instruments for screening for PTSD. It suggests the use of a number of possible screening instruments but does not offer specific guidance on which one to use, citing insufficient evidence to support a recommendation of one PTSD screening tool vs another. The Primary Care PTSD Screen (PC-PTSD) is the instrument most commonly used by DOD and VA. The PC-PTSD (Prins et al., 2004) is a validated fourquestion screening measure designed for use in primary care settings (see Box 5.3).
Department of Veterans Affairs
In the VA system, all veterans coming to VA for the first time are screened for PTSD. The PC-PTSD screening tool is incorporated into the VHA Clinical Reminder tracking system used in its medical facilities. A clinician accessing a veteran’s electronic VA medical record is prompted to complete the screening. The reminder furnishes the four PC-PTSD questions to screen for risk factors associated with PTSD. A veteran who screens positive—defined by VA as a positive response to three or more questions, which is different from the scoring used by DOD—is evaluated further by a primary care provider or is referred to a mental-health clinician.
FIGURE 5.2 Algorithm for initial evaluation of and triage for PTSD.
SOURCE: VA and DOD, 2010.
BOX 5.3
The Primary Care PTSD Screen
In your life, have you ever had any experience that was so frightening, horrible, or upsetting that, in the past month, you:
1. Have had nightmares about it or thought about it when you did not want to?
YES / NO
2. Tried hard not to think about it or went out of your way to avoid situations that reminded you of it?
YES / NO
3. Were constantly on guard, watchful, or easily startled?
YES / NO
4. Felt numb or detached from others, activities, or your surroundings?
YES / NO
SOURCE: Prins et al., 2004.
The veteran is also assessed for suicide risk (VA, 2007). Followup screening for PTSD is repeated every year for the first 5 years that the veteran is in VA care and every 5 years thereafter unless there is a clinical need more frequently (VA, 2010b). In addition, veterans seen in any of the roughly 300 VA Vet Centers are screened for PTSD.
The difference between PC-PTSD scoring thresholds used by DOD and VA hampers the ability to make valuable clinical and research comparisons between the two systems of care. The next section discusses research findings about PC-PTSD scoring methods.
Validity of Tools for Screening for Posttraumatic Stress Disorder
A wide array of PTSD screening tools are available for identifying undiagnosed cases of PTSD (National Center for PTSD, 2004), but there is little evidence to support recommending one PTSD screening tool over another (VA and DOD, 2010). A systematic review of validated screening instruments for civilian PTSD found that instruments that have fewer items, simpler response scales, and simpler scoring methods perform as well as if not better than longer and more complex measures (Brewin, 2005). As mentioned previously, the VA and DOD use the four-item PC-PTSD screening tool.
Research with VA primary care patients has shown that the PC-PTSD is optimally efficient (yielding a sensitivity of 0.78 and a specificity of 0.87) when a cutoff score of 3 is used, meaning that patients answering yes to at least three questions should be considered for further evaluation for PTSD (Prins et al., 2004). Recent studies of the performance of the PC-PTSD in military populations also found that a cutoff of 3 has an acceptable level of sensitivity to identify people who have PTSD (the range is 0.76–0.83) and a high degree of specificity to identify people who do not have PTSD (the range is 0.82–0.92) (Bliese et al., 2008; Calhoun et al., 2010). However, given the measure's relative susceptibility to false positives (positive results in people who do not have PTSD), Calhoun et al. (2010) suggest that, within primary care, the PC-PTSD may be most advantageously used in the context of staged screening—using the PC-PTSD followed by another assessment tool. As mentioned above, DOD uses a staged approach in which a cutoff score of 2 on the PC-PTSD is followed by use of the PCL to assess symptom severity.
Research suggests that DOD postdeployment mental-health screening may fail to identify a sizable fraction of service members who need mental-health services because of service members’ concerns about anonymity. In one study by (Warner et al., 2011b), a brigade of Army soldiers first completed the PDHA on returning from Iraq, and a subsample completed an anonymous survey that consisted of the same mental-health questions as were on the PDHA. Service members reported much higher rates regarding all mental-health concerns on the anonymous survey; of those who screened positive for PTSD or depression, 20.3% reported that they were uncomfortable about reporting their answers honestly on the PDHA (Warner et al., 2011a). Concerns related to stigma are a problem in the accurate assessment of PTSD and other psychopathologic conditions.
Implementation of Department of Defense and Department of Veterans Affairs Guidance for Screening for Posttraumatic Stress Disorder
The section presents sparse information on the extent to which DOD and VA are implementing and tracking screening procedures to identify possible PTSD. The lack of VA data raises questions about how well it is implementing and assessing their screening practices to ensure the best possible result.
Department of Defense
The Armed Forces Health Surveillance Center (AFHSC) reports PTSD screening rates on the basis of data from postdeployment health screenings (with the PDHA and the PDHRA). In the first quarter of 2010, about 10% of active and reserve service members who returned from OEF and OIF deployments screened positive on the PC-PTSD, which is included in the health assessments (DeFraites and Vythilingam, 2011). As mentioned above, research suggests that postdeployment health screenings may underestimate the number of service members who might have PTSD (Warner et al., 2011a).
Data from the RESPECT-Mil program show that from February 2007, when the program began, through the end of FY 2011, 76 clinics at 31 active RESPECT-Mil sites provided more than 1.6 million primary care visits by active-duty service members, of which 1.3 million visits—almost 80%—included screening for PTSD and depression. Although there is opportunity to improve screening, that rate shows that attention is being given to screening at the RESPECT-Mil sites. Of visits that included screening, nearly 13% (168,519) resulted in positive screens; 49% of positive screens resulted in primary care diagnoses of depression, possible PTSD, or both (DCoE, 2012b).
Department of Veterans Affairs
In VA’s Performance Management Program, VA uses several measures to see whether veterans are being screened for PTSD (AHRQ, 2012). The committee was unable to identify results of using those measures. Inquiries to VA about performance measures did not yield information about them.
One measure is the percentage of eligible patients who are screened for PTSD at required intervals. Another is the percentage of veterans who have positive PC-PTSD screens whose disposition is documented in the record. A disposition is defined as either a timeline for care; an arrangement for treatment, such as a mental-health appointment; or giving of instructions to a patient. A related measure looks at whether disposition is timely. Timely is defined as completion of the disposition by the next calendar day after a positive screen.
Department of Defense and Department of Veterans Affairs Guidance for Assessment and Diagnosis of Posttraumatic Stress Disorder
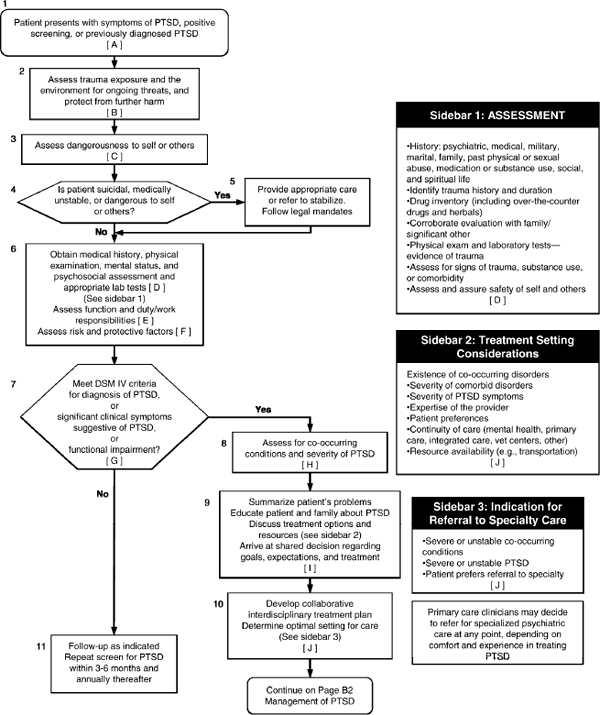
Figure 5.3 shows the process presented in the VA/DOD guideline for managing the assessment and diagnosis of PTSD in patients who have a positive PTSD screen.
For patients who screen positive for PTSD, the VA/DOD guideline states that clinicians should perform a comprehensive clinical assessment to obtain relevant information to guide accurate diagnosis and appropriate clinical decision making. In a comprehensive clinical
interview, a provider should focus on the traumatic event, danger to self or others, relevant history, physical and mental status examinations, relevant laboratory tests, psychosocial functioning, and possible comorbid conditions (such as SUDs and depression). The provider should assess the patient’s symptoms against each of the 17 PTSD criteria in the Diagnostic and Statistical Manual, Fourth Edition (DSM-IV) and gather details about time of onset, frequency, course, severity, level of distress, and functional impairment. A functional assessment should evaluate the patient’s current level of family, relationship, work or school, and social functioning and fitness for duty.
As part of the comprehensive assessment, there are several instruments to assist the clinician in making a PTSD diagnosis, documenting a traumatic event, and assessing symptom severity. Two main types of instruments are used in PTSD evaluations: structured (or semistructured) interview questions that a clinician asks and self-reporting questionnaires that a patient completes. Typically, both structured interviews and self-reporting questionnaires are used in clinical settings to measure PTSD symptoms (National Center for PTSD, 2012a).
The VA/DOD guideline recommends the use of structured interviews and specifically mentions the Clinician-Administered PTSD Scale (CAPS) to support a diagnosis of PTSD on the basis of symptoms related to each of the DSM-IV diagnostic criteria for PTSD. The CAPS (Blake et al., 1995) is a semistructured interview that should be administered by a trained health professional to determine whether a patient meets the DSM-IV diagnostic criteria for PTSD. It has the advantage of assessing the array of PTSD symptoms and their severity (frequency and intensity), but it cannot be used to determine the presence of comorbid psychiatric disorders. The CAPS contains 34 questions, 17 of which measure symptom frequency and 17 measure symptom intensity. A total symptom severity score (which ranges from 17 to 85) can be obtained by summing the scores on each of the 17 items. The CAPS generally takes about 40–60 minutes to administer (IOM, 2006).
The VA/DOD guideline also recommends the use of a validated self-administered checklist of symptoms and history of trauma exposure and specifically mentions the PTSD Checklist (PCL). The PCL (Blanchard et al., 1996; Weathers et al., 1991) assesses DSM-IV symptoms of PTSD and symptom severity. With the PCL, patients use a 1–5 scale to rate the frequency and intensity of their symptoms (IOM, 2006).
Acknowledging the high prevalence of psychiatric comorbidities in the PTSD population, the VA/DOD guideline states that screening for depression and other psychiatric disorders is warranted. The section “Comorbid Conditions” discusses the management of comorbid conditions.
Department of Defense
In DOD, as previously mentioned, a service member who has a positive result on the PCPTSD should complete the PCL-C as part of the deployment health-assessment process and the RESPECT-Mil program before evaluation in a diagnostic interview. However, the deployment health assessments and the RESPECT-Mil program use different scoring thresholds for purposes of diagnosis and treatment. According to clinician training materials for the DOD deployment health assessment, a PCL score of less than 30 means no PTSD symptoms, scores of 30–39 correspond to mild PTSD symptoms, scores of 40–49 correspond to moderate PTSD symptoms, and a score of 50 or more means severe PTSD symptoms (Vythilingam et al., 2010).
FIGURE 5.3 Algorithm for the assessment and diagnosis of posttraumatic stress disorder.
SOURCE: VA and DOD, 2010.
According to the RESPECT-Mil clinician manual, a score of less than 13 means no PTSD, scores of 13–32 correspond to mild PTSD, and scores of 33 or greater correspond to moderate to severe PTSD. As a result of the different definitions for symptom severity, the treatment recommendations are inconsistent between the deployment health assessment and the RESPECT-Mil programs.
Department of Veterans Affairs
In the VA health system, a veteran who has a positive result on the PC-PTSD is evaluated further by the primary care provider or is referred to a mental-health clinician—such as a psychiatrist, psychologist, or trained clinician—for further evaluation. Patients referred for mental-health services must have an initial assessment within 24 hours and a first full evaluation appointment within 14 days. Established patients require followup appointments within 30 days (VA, 2010b). The PCL-C is the most widely used severity scale for veterans who have positive PC-PTSD screens, but its use is optional (VA, 2007). The VA National Center for PTSD indicates that a cut score should be based on prevalence and setting characteristics. For VA primary care settings, the suggested cut scores are 36–44; for VA specialty mental-health clinics, the suggested point range is 45–50 (National Center for PTSD, 2012b).
Validity of Tools for Assessment of Posttraumatic Stress Disorder
The CAPS, the structured interview recommended in the VA/DOD guideline, is considered the gold standard in PTSD assessment (National Center for PTSD, 2012a). All the major CPGs for the management of PTSD recommend its use (Forbes et al., 2007; International Society for Traumatic Stress Studies, 2009; National Collaborating Centre for Mental Health, 2005; Ursano et al., 2004). Less frequently cited validated diagnostic instruments referred to in the guidelines include the Structured Clinical Interview for DSM-IV (Spitzer et al., 1992), the PTSD Symptom Scale–Interview Version (Foa et al., 1993), and the Structured Interview for PTSD (Davidson et al., 1997). See IOM’s Treatment for Posttraumatic Stress Disorder in Military and Veteran Populations: Initial Assessment for a discussion of those and other instruments used in screening for and assessment of PTSD (IOM, 2012).
Among self-reported measures recommended by the VA/DOD guideline, the PCL is well validated and is most frequently cited in the major CPGs for the management of PTSD (Forbes et al., 2007; International Society for Traumatic Stress Studies, 2009; National Collaborating Centre for Mental Health, 2005; Ursano et al., 2004). There are three versions of the PCL: in the “specific” version (PCL-S), symptoms are rated in relation to a particular event; in the “military” version (PCL-M), symptoms are rated in relation to an event experienced during military service; and in the “civilian” version (PCL-C), ratings are based on any stressful life experiences. The PCL-C and PCL-S are appropriate for a wide array of patients, including military personnel and veterans. The PCL can be scored in several ways, including combining methods to ensure that a patient meets both the symptom pattern and the severity threshold (National Center for PTSD, 2012b).
A review that synthesized 72 research studies that evaluated the psychometric properties of one or more versions of the PCL found the PCL to be a well-validated measure. In general, it is psychometrically sound and shows good temporal stability, internal consistency, test–retest reliability, and convergent validity (Wilkins et al., 2011). However, the VA National Center for PTSD states that “there is no absolute method for determining the correct cut score on the PCL” (National Center for PTSD, 2012b). On the basis of the PCL’s total symptom severity score (which ranges from 17 to 85), studies have shown considerable variability in the PCL’s sensitivity and specificity depending on the cutoff score used. For example, studies’ recommended cutoff scores to indicate a positive screen in veteran populations were 28, 31, 38, and 48 (McDonald and Calhoun, 2010). In their review of the diagnostic accuracy of the PCL,
McDonald and Calhoun (2010) concluded that the variability in the PCL’s sensitivity and specificity suggests that interpretation of a score depends on the characteristics of a respondent's setting and the goal of assessment. Specifically, more studies of the PCL’s diagnostic accuracy in Iraq and Afghanistan war veterans are needed. Wilkins et al. (2011) expounded on the PCL’s strengths and limitations and emphasized that caution should be used if the PCL is expected to differentiate PTSD from similar disorders or to be used to assess treatment-related change in symptoms.
Although the PCL threshold recommended by VA is consistent with the thresholds reported in the literature, the committee is not aware of the evidence underlying the specific thresholds used in DOD’s deployment health assessment and RESPECT-Mil programs.
Implementation of Department of Defense and Department of Veterans Affairs Guidance for Assessment and Diagnosis of Posttraumatic Stress Disorder
This section presents the information on the extent to which DOD and VA conduct followup and evaluation of service members and veterans who have positive PTSD screens. The data suggest that DOD and VA need to improve their assessment practices to ensure the best possible patient care.
Department of Defense
The AFHSC reports depression referral rates according to data from the PDHA and the PDHRA. In the first quarter of 2010, the percentage of active-duty and reserves who had positive PTSD screens and who received referrals to mental-health primary or specialty care increased from about 20% to 40% over a 4-year period and achieved the 2010 target referral rate of 40% (DeFraites and Vythilingam, 2011). The committee is not aware how the targets are determined.
The committee did not find data from the RESPECT-Mil program on rates of followup and assessment of service members who were seen in primary care settings and who had positive PTSD screens.
Department of Veterans Affairs
VA reports that the numbers of referrals to diagnosis and to treatment cannot be determined, because such referrals are not coded consistently in the administrative medical record (IOM, 2012). Some data on the assessment process are available from a recent evaluation and from the Office of Inspector General (OIG).
In 2006, VA contracted with the Altarum Institute and RAND to conduct an independent evaluation of the quality of VA mental-health and substance-use care (Watkins and Pincus, 2011). The evaluation included PTSD-related measures calculated for a cohort of veterans who had PTSD that were identified for each fiscal year from FY 2004 through FY 2008. The PTSD cohort selection was based on International Classification of Diseases, Ninth Revision codes in the administrative records and reflected at least one inpatient episode or two outpatient visits (for any mental-health or non-mental-health diagnosis) in a fiscal year.
In FY 2007, of patients in the PTSD cohort who were defined as experiencing a new treatment episode (NTE),4 fewer than 5.6% had documentation of assessment for PTSD symptoms with a standard instrument within 30 days. Standard instruments included the PCL and the CAPS. That low rate is noteworthy given that the VA/DOD guideline recommends that clinicians use a standard assessment tool to inform clinical assessment. In addition, the extent of improvement needed in VA’s implementation of assessment practices is underscored in light of more recent VA policy that calls for providing patients referred for mental-health services with an initial assessment within 24 hours and a full evaluation within 14 days (VA, 2010b).
In response to concerns about belated mental-health assessments for veterans returning from Iraq and Afghanistan, Congress called for an investigation by the OIG. The OIG concluded that “VHA does not have a reliable and accurate method of determining whether they are providing patients timely access to mental health care services. VHA did not provide first-time patients with timely mental health evaluations and existing patients often waited more than 14 days past their desired date of care for their treatment appointment.” The OIG made a series of recommendations for revision of existing measures and for evaluation of possible alternative measures, staffing analysis, and improvements in data collection (VA Office of Inspector General, 2012). The committee is concerned about the OIG’s findings and underscores the importance of those recommendations for providing timely health care to our veterans.
Department of Defense and Department of Veterans Affairs Guidance for Treatment for Posttraumatic Stress Disorder
In general, treatment for PTSD symptoms includes three broad intervention categories: psychotherapy (based on psychology techniques), pharmacotherapy (using prescription medication), and education (including coping mechanisms for the patient and family members).
First-line psychotherapy treatments recommended by the VA/DOD guideline are traumafocused psychotherapy that includes components of exposure or cognitive restructuring or stress inoculation training (SIT). Specifically, the approach may include an exposure-based therapy, such as prolonged exposure (PE); a cognitive-based therapy, such as cognitive processing therapy (CPT); stress management therapy (such as SIT); or eye-movement desensitization and reprocessing (EMDR). In addition, the guideline identifies other approaches as having possible benefit in treating for PTSD, including relaxation techniques, imagery-reversal therapy, brief psychodymamic therapy, hypnosis, and group therapy. Dialectical behavioral therapy or family and couples therapy are not recommended as first-line treatment for PTSD. The guideline states that the treatment approach selected should reflect symptom severity, clinician expertise, and patient preference. In VA, CPT and PE must be available to all who need and want it (VA, 2008a). Data presented later in this section suggest that there are shortcomings in the implementation of that policy.
With respect to the use of technology for the delivery of treatment, the VA/DOD guideline does not recommend Internet-based interventions for treatment for PTSD; however, it supports the use of telephone delivery and videoconferencing, particularly to overcome geographic distance or other barriers to care. Although controlled trials of technology-based
__________________
4Defined by either the exacerbation of a condition that requires psychiatric inpatient care or the initiation of outpatient treatment after a break of 5 or more months without care.
delivery of PTSD treatments are under way, there are no definitive conclusions about its effectiveness (IOM, 2012).
Among the pharmacotherapy interventions, first-line agents recommended by the VA/DOD guideline are mainly the antidepressants SSRIs and serotonin norepinephrine reuptake inhibitors (SNRIs). If needed, the guideline suggests that the use of second-line agents, such as mirtazapine, nefazodone, tricyclic antidepressants (TCAs), and monoamine oxidase inhibitors (MAOIs) be considered. In addition, the guideline recommends the atypical antipsychotics risperidone or olanzapine as adjunctive treatment with antidepressants.
Comparison of Guidelines for Treatment for Posttraumatic Stress Disorder
In addition to the recommendations by the VA/DOD guideline, major CPGs for treatment for PTSD have been published by the American Psychiatric Association (APA) (Ursano et al., 2004), the United Kingdom National Institute of Health and Clinical Excellence (NICE) (National Collaborating Centre for Mental Health, 2005), the Australian National Health and Medical Research Council (Forbes et al., 2007), and the International Society for Traumatic Stress Studies (ISTSS) (International Society for Traumatic Stress Studies, 2009). Table 5.2 compares treatment recommendations and their various systems for indicating their strength (IOM, 2012).
TABLE 5.2 Guideline Recommendations for Treatment for Posttraumatic Stress Disorder
| Treatment Modality | VA/DOD | APA | NICE | NHMRC | ISTSS |
| Psychotherapy | |||||
| Exposure therapy | A | I | A | ||
| Prolonged exposure | A | I | A | A | |
| Virtual reality exposure | |||||
| Other exposure therapies | |||||
| Cognitive-based therapies | A | I | A | A | A |
| Trauma-focused cognitive | A | A | A | ||
| Behavioral therapy | I | ||||
| Cognitive processing therapy | |||||
| Internet-based | I | ||||
| Eye movement desensitization and reprocessing | A | II | A | A (with in vivo exposure) | A |
| Stress inoculation training | A | II | A | ||
| Group therapy | C | III | |||
| Hypnosis | C | ||||
| Imagery rehearsal therapies | C | II | |||
| Psychodynamic psychotherapy | C | II | C (stress management) | D | |
| Patient education | C | ||||
NOTE: VA/DOD: A = good evidence that the intervention improved outcomes; B = a fair amount of evidence supported the use of the intervention; C = the working group did not make a recommendation for or against the routine use of the intervention as the risk-benefit ratio was too close to make a general recommendation; D = presence of evidence that either the intervention was harmful or the risks outweighed the benefits offered by it; I = evidence was lacking, of insufficient quality, or conflicting; therefore a recommendation could not be made for or against providing the treatment routinely. APA: I = intervention recommended with substantial clinical confidence; II = intervention recommended with moderate clinical confidence; III = intervention recommended on the basis of individual circumstances. NICE: A = intervention was supported by a consistent body of evidence, including at least one RCT; B = treatment was supported by well-conducted clinical trials but no RCTs had tested the intervention; C = treatment was supported by expert committee reports or opinion but good clinical studies were absent; GPP (good practice point) = treatment was considered good practice by the guideline development group. NHMRC: 5-point scale (A, B, C, D, GPP) with A indicating that a treatment had the strongest evidence supporting its use and D indicating that a particular treatment had very weak evidence supporting its use. GPP = treatments deemed to be effective based on expert consensus opinion despite lacking empirical evidence. ISTSS: A = evidence for a particular treatment was based on RCTs; B = evidence was based on well-designed studies without randomization or placebo comparison; C = evidence was based on naturalistic clinical studies and clinical observations; D = evidence was based on long-standing and widespread clinical practice that had yet to be tested empirically; E = evidence was based on long-standing practice by a selected group of clinicians that had not been tested empirically; F = a new treatment that had not been tested empirically.
SOURCE: IOM, 2012.
Psychosocial Treatments
In its review of the guideline recommendations for psychosocial treatments for PTSD (see Table 5.2), the earlier IOM committee drew the following conclusions:
There are many similarities among the recommendations of the reviewed guidelines…. All the guidelines strongly support the use of trauma-focused psychotherapy treatment for PTSD in adults and children with an emphasis on trauma-focused CBT, such as PE and CT. All but one of the guidelines recommended against the use of psychologic debriefing soon after exposure to trauma (IOM, 2012).
That committee noted that eye-movement desensitization and reprocessing (EMDR) is one example of the variation in the guidelines assessment of a specific therapy. EMDR was given the highest rating in all but one of the guidelines. The APA guideline gave it a second-tier rating. What contributed to that difference among the guidelines was how the absence of support for the use of eye movements in EMDR was addressed.
After reviewing the psychosocial treatments whose efficacy had been examined in RCTs or open trials, IOM (2012) found that the vast majority of treatments that have been examined via RCTs are in the general group of psychosocial therapies called cognitive behavioral therapy (CBT). They include exposure therapies such as prolonged exposure (PE), stress inoculation training or anxiety-management programs, cognitive therapies such as cognitive processing therapy (CPT), and EMDR. RCTs have shown that cognitive therapy alone results in PTSD symptom reduction and improved mood and functioning (IOM, 2012).
In addition, the earlier committee considered the evidence base for numerous other psychosocial therapies, including psychodynamic psychotherapy, brief eclectic psychotherapy, hypnosis, relaxation, stress inoculation training, interpersonal therapy, skills training in affect and interpersonal regulation, and group therapy. That committee found that, with the exception of CBT-based group therapy, the efficacy of the other psychosocial therapies is supported by
only a few RCTs. Small RCTs and open trials of acceptance and commitment therapy have been conducted and warrants further review. Until the results from the four ongoing RCTs are available, there is insufficient evidence for the efficacy of virtual reality exposure programs that integrate computer graphics and head-mounted visual displays as a tool to deliver PE to reduce PTSD symptoms (IOM, 2012). See IOM (2012) for a full discussion of the evidence supporting the use of various psychosocial therapies for PTSD.
Pharmacologic Treatments
As shown in Table 5.2, PTSD treatment guidelines, including the 2010 VA/DOD guideline, all recommend the use of antidepressants, specifically, an SSRI or an SNRI, in treatment for chronic PTSD. The US guidelines—VA/DOD, ISTSS, and APA—all recommend the use of SSRIs or the SNRI antidepressant venlafaxine as a first-line therapy with status equal to that of psychotherapy. The UK and Australian guidelines recommend pharmacotherapy only as a second choice unless a patient declines psychotherapy or manifests particular clinical features (IOM, 2012).
The recently published IOM report (IOM, 2012) also cited reviews and meta-analyses that found good evidence that pharmacotherapy reduces symptoms in chronic PTSD, including combat-related PTSD (see Ipser and Stein, 2012; Stein et al., 2006; Stewart and Wrobel, 2009). See IOM 2012 for a full discussion of the evidence supporting the use of various pharmacologic treatments for PTSD.
Emerging Therapies
Guideline recommendations do not show strong evidence supporting the use of various innovative or alternative treatments for PTSD, such as couple and family therapy and complementary and alternative medicine (CAM), which includes yoga, contemplative treatments, and acupuncture. IOM (2012) concluded that these treatments do not have a substantial evidence base; evidence of the effectiveness of these therapies for PTSD is based on small RCTs, case studies, or anecdotal reports.
Implementation of Department of Defense and Department of Veterans Affairs Guidance for Treatment for Posttraumatic Stress Disorder
This section presents information available to the present committee on the extent to which DOD and VA provide treatment for service members and veterans who have PTSD. There is a striking lack of data to inform conclusions about the extent to which PTSD treatments are offered, delivered, and completed and about whether they are leading to improved patient outcomes.
Department of Defense
The AFHSC reports PTSD referral rates on the basis of data from the postdeployment health screenings (PDHA and PDHRA). In the first quarter of 2010, 65% of active-duty and reserve personnel who had a positive PTSD screen and who received a referral to mental-health primary or specialty care were engaged in treatment, that is, had a mental-health–related clinic encounter during the 180 days after their return. That reached the 2010 target referral rate of 65%
(DeFraites and Vythilingam, 2011). The committee does not know how the targets are determined.
Department of Veterans Affairs
VA reports that there is no mechanism for tracking the delivery of evidence-based therapies in the VA centralized databases. The VHA is developing progress-note templates for CPT, PE, and other evidence-based treatments that will allow documentation of care in the computerized record in a manner that will facilitate the collection of centralized aggregate data (IOM, 2012). The committee obtained the data discussed below, which suggest that many veterans are not getting necessary treatment and that most of those who are do not complete the full course.
VA reported to the Congressional Budget Office (CBO) that 40% of OEF and OIF veterans initiating CPT or PE therapy complete a full course of therapy, which is typically at least nine treatment sessions ideally administered weekly (Seal et al., 2010). The CBO report states that veterans who completed PE therapy attended an average of 11 sessions, whereas those who did not complete therapy attended an average of five sessions; results were similar for patients undergoing CPT. A recently published study found that of 49,425 veterans with newly diagnosed PTSD in VA, fewer than 10% completed the recommended treatment in the first year of diagnosis (Seal et al., 2010).
As mentioned previously, VA contracted with Altarum Institute and RAND to conduct an independent evaluation of the quality of VA mental-health and substance-use care (Watkins and Pincus, 2011). The evaluation included PTSD-related measures calculated for a cohort of veterans who had PTSD. In FY 2007, 27.9% of veterans in the PTSD cohort in a new treatment episode had documentation of an adequate trial (at least 60 days) of SSRIs or a documented reason for discontinuing. Only 19.9% in the PTSD cohort who received psychotherapy had documentation of receiving at least one visit for CBT (including behavioral therapy and cognitive therapy) in the study period. Some 16.3% of veterans in the PTD cohort received VA's Specialized Intensive PTSD Programs (SIPP) within 60 days of a new treatment episode, and 25.3% received SIPP during the study period. Veterans over 65 years old and veterans who resided in rural areas had the lowest use of SIPP, and there was considerable variation among the Veterans Integrated Service Networks.
To improve implementation of treatment regimens, VA is undertaking a national effort to disseminate evidence-based psychotherapies for PTSD and other mental-health conditions throughout the VA health care system. Since 2007, VA has been working to disseminate CPT and PE therapy for PTSD. Competence-based training of VA mental-health care providers in the delivery of those therapies is a component of the initiative. It involves experientially based workshop training followed by weekly consultation for 6 months with an expert in the treatment (Karlin et al., 2010). As of May 31, 2010, VA had provided training to over 2,700 VA mental-health staff in the delivery of CPT or PE, and some staff have been trained in the delivery of both (Karlin, 2010). Additional efforts to promote communication and sharing of best practices throughout VA include the PTSD national mentoring program and the appointment of evidenced-based coordinators at each medical center. The committee is impressed by the training of clinicians in evidence-based therapies (PE and CPT) and commends VA on its psychotherapy dissemination efforts. What remains a question to the committee is how much the treatments are
actually offered, delivered, and completed and whether they are leading to improved patient outcomes.
Summary
The VA/DOD clinical guidelines for PTSD are in line with the available evidence base and state-of-the-art clinical guidelines put forth by other professional organizations (such as APA and NICE). The VA/DOD guidelines suggest standards for the screening for and assessment of PTSD that are generally reasonable and evidence based. They also make treatment recommendations that are in line with the evidence base and other state-of-the-art guidelines. VA has undertaken a large, impressive effort to disseminate the evidence-based therapies PE and CPT for PTSD. It is to be commended for that effort and for its success in training large numbers of clinicians. The committee has concerns, however, about the timeliness of assessments and treatment delivery for veterans who need them. On the basis of the relatively modest data that we could access, wait times are too long, and appropriate assessment and treatment delivery are delayed beyond what is acceptable. The committee also has concerns about how well the dissemination effort has “penetrated” into practice. To judge by the data that we reviewed, most veterans who have PTSD do not receive evidence-based psychotherapy (many receive SSRIs but not necessarily in adequate dosage or for an adequate duration), and most of those who receive it do not complete an adequate course of treatment.
MAJOR DEPRESSIVE DISORDER
Diagnosis of major depressive disorder (MDD) is based on the presence of depressed mood or a marked reduction in or loss of interest or pleasure in all or nearly all activities for most of the day and the presence of at least four additional symptoms, such as substantial change in weight, change in sleeping patterns, fatigue, feelings of worthlessness, and suicidal ideation (APA, 2000). To warrant the diagnosis, symptoms must persist for at least 2 weeks and involve substantial impairment in functioning. Chapter 4 presents the diagnostic criteria of MDD and gives details about the prevalence of MDD in the military and veteran populations.
To assess the efficacy of current screening, assessment, and treatment approaches to MDD in DOD and VA, the committee reviewed the VA/DOD Clinical Practice Guideline for Management of Major Depressive Disorder (MDD), May 2009 (VA and DOD, 2009a). The guideline is intended to assess, diagnose, and treat for MDD in the military and veteran populations and is intended to be used in the primary care setting. Here, the committee assesses key aspects of the recommended practices in the VA/DOD guideline in light of evidence in the literature and other clinical guidelines for the management of MDD.
Department of Defense and Department of Veterans Affairs Guidance for Screening for Major Depressive Disorder
Among service members and veterans, systematic screening for depression is especially vital considering its prevalence, its associated risk of suicide, and the perceived stigma that deters the receipt of mental-health care. The VA/DOD guideline for MDD recommends annual screening in the primary-care setting. Figure 5.4 shows the process presented in the VA/DOD guideline for the initial assessment (including screening) and diagnosis of MDD in primary care.
FIGURE 5.4 Algorithm for initial assessment and diagnosis of MDD in primary care.
SOURCE: VA and DOD, 2009a.
To screen for MDD, the guideline recommends the use of a standardized screening tool, the Patient Health Questionnaire (PHQ-2), which is a validated two-item screen (see Box 5.4). A PHQ-2 score ranges from 0 to 6. Patients who screen positive on the PHQ-2 should be given a more detailed quantitative questionnaire and a full clinical interview that includes evaluation for suicide risk.
BOX 5.4
Patient Health Questionnaire-2 (PHQ-2)
Over the past 2 weeks, how often have you been bothered by any of the following problems?
Little interest or pleasure in doing things.
0 = Not at all
1 = Several days
2 = More than half the days
3 = Nearly every day
Feeling down, depressed, or hopeless.
0 = Not at all
1 = Several days
2 = More than half the days
3 = Nearly every day
SOURCE: Kroenke et al., 2003.
Department of Defense
In DOD, depression screening occurs routinely as a component of periodic health assessments, the PDHA and PDHRA, which are briefly described in the introduction to this chapter. It also occurs routinely in primary care settings. The US Army Medical Command implemented the RESPECT-Mil, which provides primary care–based screening, assessment, treatment, and referral of active-duty personnel who have PTSD or depression. DOD is implementing a triservice expansion of the program (DCoE, 2012b). Service members who present in RESPECT-Mil clinics are screened for depression and for PTSD at every primary care provider visit. To screen for depression, both the deployment health assessment and RESPECTMil use the PHQ-2 questions. The screen is considered positive if a service member indicates that either one or both symptoms are present either “more than half the days” or “nearly every day.” Service members who screen positive are evaluated further with the nine-item PHQ-9 (Department of the Army, 2010b; Vythilingam et al., 2010).
Department of Veterans Affairs
In the VA health system, all veterans who come to VA for the first time are screened for depression. The PHQ-2 screening tool is incorporated into the VHA clinical-reminder tracking system. A clinician who accesses a veteran’s electronic VA medical record is prompted to complete the screening. The reminder presents the two PHQ-2 questions; a cutoff score of 3 is used to define a positive screen. Veterans who screen positive are assessed for suicide risk and then, if it is warranted, evaluated by either a primary care provider or a mental-health specialist. The PHQ-2 should be completed annually by all patients who are seen in a primary care setting (VA, 2010b). VA has several care-management models that integrate mental-health and primary
care and in which depression screening and treatment take place. Such programs include Translating Initiatives for Depression into Effective Solutions (TIDES), the Behavioral Health Laboratory, the Post-Deployment Integrated Care Initiative, and Patient-Care Alignment Teams. In addition, veterans seen in any of the roughly 300 Vet Centers are screened for depression.
Validity of Tools for Screening for Major Depressive Disorder
Evidence supports the practice of screening for depression in primary care (US PSTF, 2009; Yano et al., 2012), as recommended by the VA/DOD MDD guideline. In reviewing evidence on the accuracy of screening instruments to identify depressed adults, the US Preventive Services Task Force (USPSTF) found little evidence to support recommending one screening tool over another. It concluded that asking the two questions on the PHQ-2 may be as effective as using more complex instruments (USPSTF, 2009). A recent systematic review found that the PHQ-2 has good sensitivity (83%) and specificity (92%) for detecting depressive disorders with a cutoff score of 3 (Kroenke et al., 2010). A separate study, an RCT of screening for depression in primary care, suggests that using a threshold score of 2 is superior to detecting cases on the basis of a score of 3 or more (Arroll et al., 2010). Using a score of 2 or more, the PHQ-2 screen had a sensitivity of 86% and a specificity of 78%. Using a score of 3 or more, the study reported a sensitivity of 61% and a specificity of 92%. VA currently uses a cutoff score of 3 on the PHQ-2 as the basis of a positive MDD screen.
Implementation of Department of Defense and Department of Veterans Affairs Guidance for Screening for Major Depressive Disorder
This section presents information available to the committee on the extent to which DOD and VA are implementing and tracking screening procedures to identify MDD. The sparse data suggest that there is room for improvement in DOD and VA screening practices for MDD.
Department of Defense
The AFHSC reports depression-screening rates by using data from the PDHA and the PDHRA. In the first quarter 2010, about 10% of active and reserve service members who had returned from OEF and OIF deployments screened positive on the PHQ-2 (DeFraites and Vythilingam, 2011).
Data from the RESPECT-Mil program show that from February 2007 through the end of FY 2011, 76 clinics at 31 active RESPECT-Mil sites provided more than 1.6 million primary care visits to active-duty service members, of which 1.3 million visits included screening for PTSD and depression. That represents an overall 80% screening rate for active-duty primary care visits to participating clinics since the program began. Of visits with screening, nearly 13% (168,519) resulted in positive screens; and 49% of positive screens resulted in a primary care diagnosis of depression, possible PTSD, or both (DCoE, 2012b).
Department of Veterans Affairs
Under VA’s Performance Management Program, VA uses several measures to see whether veterans are being screened for depression (AHRQ, 2012). The committee was unable to identify results of using those measures, and inquiries to VA about performance measures did not yield information about them.
One measure is the percentage of eligible patients who are screened annually for depression with the PHQ-2 or PHQ-9. Another is the percentage of veterans who have a positive screen during their annual depression screening and have a disposition documented in the record. A disposition is defined as a timeline for care; an arrangement for treatment, such as a mental-health appointment; or the giving of instructions to the patient. A separate measure looks at whether documentation of the disposition is timely, which is defined as completion of the disposition by the next calendar day after a positive screen.
A study that used 2002 data on a national sample of VA medical outpatients found that overall about 85% of eligible veterans (18,245) were screened for depression in the study year. However, patients who were more likely to screen positive (veterans who were younger, were unmarried, or had more medical comorbidity) were less likely to be screened (Desai et al., 2006).
Department of Defense and Department of Veterans Affairs Guidance for Assessment and Diagnosis of Major Depressive Disorder
For patients who screen positive for depression, the VA/DOD guideline states that the primary care provider should perform a clinical interview that focuses on relevant history, physical and mental-status examinations, relevant laboratory tests, drug inventory, and comorbid conditions. Providers should also evaluate the patient with a standardized assessment tool, the PHQ-9, and should assess for symptoms, symptom severity, and effects on daily functioning. See Figure 5.4 above for the process presented in the VA/DOD guideline for managing the assessment and diagnosis of MDD in primary care.
The PHQ-9 is a validated self-administered or interviewer-administered instrument that assesses the nine DSM, Fourth Edition, Text Revision (DSM-IV-TR) criterion symptoms and effects on functioning. It also assesses severity and treatment response. See questions in Box 5.5.
BOX 5.5
PHQ-9 Questions*
Over the last 2 weeks, how often have you been bothered by
1. Little interest or pleasure in doing things
2. Feeling down, depressed, or hopeless
3. Trouble falling or staying asleep, or sleeping too much
4. Feeling tired or having little energy
5. Poor appetite or overeating
6. Feeling bad about yourself—or that you are a failure or have let yourself or your family down
7. Trouble concentrating on things, such as reading the newspaper or watching television
8. Moving or speaking so slowly that other people could have noticed. Or the opposite—being so fidgety or restless that you have been moving around a lot more than usual
9. Thoughts that you would be better off dead, or hurting yourself in some way
The first nine questions have a possible answer of:
• Not at all
• Several days
• More than half the days
_______________________
10. How difficult have these problems made it for you to do your work, take care of things at home, or get along with other people?
Question 10 has a possible answer of:
• Not difficult at all
• Somewhat difficult
• Very difficult
• Extremely difficult
*PHQ-9 is adapted from PRIME MD TODAY, developed by Drs. Robert L. Spitzer, Janet B.W. Williams, Kurt Kroenke, and colleagues, with an educational grant from Pfizer Inc. Copyright ©1999 Pfizer Inc. All rights reserved. PRIME MD TODAY is a trademark of Pfizer Inc.
Each of the first nine items on the PHQ is scored 0–3, providing a 0–27 severity score. A total score of 10–14 is classified as meaning mild MDD, a score of 15–19 means moderate MDD, and a score of 20 or higher means severe MDD. A diagnosis is further modified as having complications if it co-occurs with PTSD, SUD, psychosis, suicide risk, mania, significant social stressors, or war-related conditions; and it is considered chronic if symptoms persist for more than 2 years despite treatment (VA and DOD, 2009a).
Department of Defense
In deployment health assessments, DOD uses a variation of the PHQ-9, the PHQ-8, which omits the suicide-screening item because suicide screening and assessment do not occur until the diagnostic interview. Clinicians are to administer the PHQ-8 to service members who have positive PHQ-2 screens. They are to provide depression education or support counseling and consider referral to mental-health care for service members who have mild or moderate symptoms (a PHQ-8 score of 10–18) and make a referral for service members who have severe symptoms (a PHQ-8 score of 19 or higher) (Vythilingam et al., 2010). In the RESPECT-Mil program, service members who have positive PHQ-2 screens will complete the PHQ-9 (Department of the Army, 2010b). Treatment recommendations are to provide an antidepressant or psychotherapy for scores of 10–19 and an antidepressant and psychotherapy for scores of 20 or higher (Oxman et al., 2008).
Department of Veterans Affairs
VA uses the PHQ-9—it is integrated into the clinical reminder—but not exclusively, inasmuch as the choice of instrument is determined by the care provider. However, the clinical reminder will prompt clinicians to perform the PHQ-9 test if a PHQ-2 test is positive (a score of 3 or higher). Any patient who has a PHQ-9 score over 10 or a response to question 9 of the PHQ-9 other than “not at all” must have an assessment for suicide risk and disposition by a provider within a day of the positive screen (VA, 2007).
Validity of Tools for Assessment and Diagnosis of Major Depressive Disorder
The PHQ-9 has been found to be a reliable and valid measure of depressive disorders and depression severity (Kroenke et al., 2001). One systematic review of the psychometric literature
on the PHQ-9 reported a sensitivity of 88% and a specificity of 88% when a cutoff score of 10 was used (Wittkampf et al., 2007). Because of the risk of overdiagnosis with that level of specificity, researchers concluded using a cutoff score of 10 is acceptable in patient populations that have a relatively high prevalence of MDD (Wittkampf et al., 2007).
Implementation of Department of Defense and Department of Veterans Affairs Guidance for Assessment and Diagnosis of Major Depressive Disorder
This section presents information available to the committee on the extent to which DOD and VA conduct followup and evaluation of service members and veterans who have positive MDD screens. The information raises questions about how well DOD and VA are implementing and tracking their assessment practices to ensure the best possible patient care.
Department of Defense
The AFHSC reports depression referral rates by using data from the PDHA and PDHRA. In the first quarter of 2010, the proportion of active-duty and reserve personnel referred to mental-health primary or specialty care, substance-abuse care, chaplains, or Military OneSource for further evaluation or treatment had increased from about 25% to 60% over a 4-year period, surpassing the 2010 target referral rate of 40% (DeFraites and Vythilingam, 2011).
The committee did not find data from the RESPECT-Mil program on rates of followup and assessment of service members who were seen in primary care settings and who had positive MDD screens.
Department of Veterans Affairs
Under VA’s Performance Management Program, VA collects two performance measures related to depression and suicide risk assessment (AHRQ, 2012). The committee was unable to identify results of using those measures, and inquiries to VA about performance measures did not yield information about them.
One measure is the percentage of patients who screen positive on a depression screen (PHQ-2 or PHQ-9) and have a suicide-risk evaluation completed within 24 hours. The other measure is the percentage of patients who screen positive on the depression screen (PHQ-2 or PHQ-9) and on the PTSD screen (PC-PTSD) and have a suicide-risk evaluation completed within 24 hours.
A study that used 2002 data from a national sample of VA medical outpatients found that veterans who had depressive symptoms were not being assessed as recommended. The results showed that overall 84.9% of eligible patients (18,245) were screened for depression in the study year. Although 8.8% screened positive, only about half (54.0%) the patients who screened positive received recommended followup evaluation for diagnostic confirmation and only 1.1% of those who screened positive received a new depression diagnosis (Desai et al., 2006).
Department of Defense and Department of Veterans Affairs Guidance for Treatment for Major Depressive Disorder
For initial treatment for mild or moderate MDD, the VA/ DOD guideline advocates the use of monotherapy—either psychotherapy or pharmacotherapy with a single antidepressant.
Combination treatment with pharmacotherapy and psychotherapy should be used for moderate to severe MDD or for patients who have a poor response to monotherapy. The guideline advises that patients who receive a diagnosis of mild or moderate MDD may be treated in primary care. Patients who have severe MDD or any complicated MDD and comorbidities should be referred to specialty care for treatment. Figure 5.5 is the algorithm from the VA/DOD guideline for treatment for MDD in primary care.
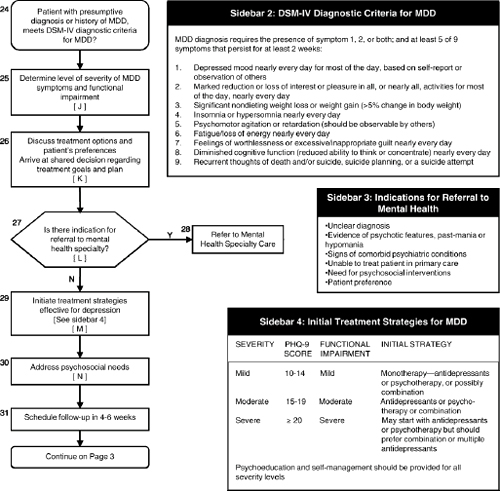
FIGURE 5.5 Algorithm for treatment of MDD in primary care.
SOURCE: VA and DOD, 2009a.
The recommended first-line medications include SSRIs, such as sertraline and paroxetine, and SNRIs, such as bupropion and mirtazapine. The guideline notes that all the SSRIs, excluding fluvoxamine, may be used as first-line agents in the treatment of adults for MDD. Patients who do not remit or are intolerant to one SSRI may be switched to another SSRI or to another class of antidepressant, such as TCAs or MAOIs. Augmentation may be considered for those who show only partial response to an SSRI.
The recommended first-line psychotherapies include CBT, interpersonal psychotherapy (IPT), problem-solving therapy (PST), and behavior therapy, including behavioral activation (BA). Second-line interventions include short-term psychodynamic psychotherapy, couplefocused and marital-focused therapies, client-centered counseling, and acceptance and mindfulness therapies, such as acceptance and commitment therapy (ACT). The guideline also
cites computer-based CBT as an alternative to traditional individual or group psychotherapy. Guided self-help is listed as an option for mild to moderate depression.
The guideline recommends individual CBT, 16–20 sessions long, as a monotherapy for patients who have moderate depression. CBT in combination with pharmacotherapy is a recommended option for patients who do not respond to monotherapy and for patients who have severe, recurrent MDD (defined as three or more episodes).
Individual IPT is recommended for adults who have uncomplicated mild to moderate MDD. The recommended treatment is 16–20 sessions delivered by mental-health professionals who are trained in this modality. PST can be used for uncomplicated mild to moderate MDD, particularly in the primary care setting, and can be delivered by primary care physicians or nurses. Six sessions, delivered over the course of 3 months, is a recommended option for patients who have uncomplicated mild to moderate MDD.
Electroconvulsive therapy (ECT) should be considered for patients who have severe MDD and cannot tolerate or have not responded to several trials of antidepressant treatment unless a patient has substantial comorbid medical conditions that would increase the risks associated with ECT.
The guideline recommends against the use of vagus nerve stimulation (VNS) as an intervention for treatment-resistant depression because when it was published, in 2009, VNS had not been demonstrated to be safe and effective. The controversy over the use of VNS is discussed later.
Among the possible complementary and alternative treatments, the guideline recommends the use of exercise as an adjunct to other empirically supported treatments for depression, particularly antidepressant medication. It recommends the consideration of light therapy for some patients who have MDD, particularly if they have seasonal affective disorder. The guideline suggests that St. John’s wort may be used by patients who have mild MDD and who have a strong preference for herbal treatments. The guideline does not recommend acupuncture as a treatment for MDD on the basis of insufficient evidence to determine its efficacy.
After initiation of treatment, the patient should be periodically assessed to determine treatment effects. The PHQ-9 should be used to monitor treatment response 4–6 weeks after initiation of treatment, after each change in treatment, and periodically until full remission is achieved. In patients who reach full remission, assessment of symptoms should be continued periodically to monitor for relapse or recurrence.
A VHA 2008 directive states that all veterans who have depression (or anxiety disorders) must have access to CBT, ACT, or IPT. Medical centers and large community-based outpatient clinics (CBOCs) must provide adequate staff capacity to deliver evidence-based psychotherapy when it is clinically indicated. Large and middle-sized CBOCs may provide the services through telemental health when necessary (VA, 2008a). In addition to the required evidence-based treatments, VA offers a variety of treatments that fit into the CAM category and have almost no evidence base, such as spirituality group, relaxation group, relaxation yoga group, group ear acupuncture, socialization group, Tai-Chi group, and yoga nidra group. Many of those approaches have been used for relaxation in other settings.
Comparison of Guidelines for Treatment for Major Depressive Disorder
In this section, the VA/DOD guideline is compared with evidence-based CPGs for the management of MDD developed by APA (2010) and NICE (2009). Table 5.3 compares treatment recommendations in the guidelines and uses their rating systems to indicate the strength of the evidence supporting them.
TABLE 5.3 Summary of Guideline Recommendations for Treatment for Depression
| Treatment Modality | VA/DOD | APA | NICE | |||
| Psychotherapy | ||||||
| Cognitive behavioral therapy (CBT) | A | I | √ | |||
| Interpersonal psychotherapy (IPT) | A | I | √ | |||
| Problem-solving therapy (PST) | A | I | √ | |||
| Behavioral therapy/behavioral activation | A | √ | ||||
| Computer-based cognitive behavioral therapy | B | √First-line | ||||
| Couple/marital-focused therapies | C | II | √ | |||
| Guided self-help (GSH) | B | √ First-line | ||||
| Client-centered counseling | C | √ when other treatments are declined | ||||
| Acceptance and Mindfulness | ||||||
| Dialectical behavioral therapy | C | |||||
| Mindfulness-based cognitive therapy | A | √ | ||||
| Acceptance and commitment therapy | No rating | |||||
| Psychodynamic psychotherapy | C | II | √ when other treatments are declined | |||
| Group therapy | B (CBT) | III | √ CBT First-line | |||
| Pharmacotherapy | ||||||
| Antidepressants | ||||||
| SSRI | First-line (excluding Fluvoxamine) | I | √ | |||
| SNRI | First-line | I | ||||
| Bupropion | First-line | I | ||||
| Mirtazapine | First-line | I | ||||
| Tricyclic (TCA) | I | |||||
| MAOIs | B | I | ||||
| If poor response w/other; no strength rating | ||||||
| Somatic Treatment | ||||||
| Electroconvulsive therapy | A | A | √ | |||
NOTE: VA/DOD: A = good evidence that the intervention improved outcomes; B = a fair amount of evidence supported the use of the intervention; C = the working group did not make a recommendation for or against the routine use of the intervention as the risk-benefit ratio was too close to make a general recommendation; D = presence of evidence that either the intervention was harmful or the risks outweighed the benefits offered by it; I = evidence was lacking, of insufficient quality, or conflicting; therefore a recommendation could not be made for or against providing the treatment routinely. APA: I = intervention recommended with substantial clinical confidence; II = intervention recommended with moderate clinical confidence; III = intervention recommended on the basis of individual circumstances. NICE: No rating system was used. For purposes of this report, v denotes that use of the treatment was recommended; X indicates that the recommendation advises against the use of the treatment.
Treatment Strategy
Overall, the VA/DOD, APA, and NICE guidelines are consistent in recommending monotherapy as the initial treatment of choice for mild or moderate MDD. The VA/DOD guideline advocates the use of either pharmacotherapy alone or psychotherapy alone for mild or moderate MDD, whereas the APA and NICE guidelines suggest that psychotherapy alone may be the preferred initial treatment for mild and moderate MDD to be followed by the use of medication if symptoms persist. Research shows that the efficacy of psychotherapy for mild to moderate MDD is about the same as that of pharmacotherapy (Cuijpers et al., 2011; Thase, 2011).
Controversy surrounds the utility of antidepressants for treatment for mild depression. Because of small effect sizes, several reviews and meta-analyses have raised questions about the interpretation of results of RCTs. Examples of published reviews and meta-analyses relevant to the debate include (Hegerl et al., 2012; Pigott et al., 2010; Stewart et al., 2012; Thase, 2011; Vohringer and Ghaemi, 2011).
For moderate and severe MDD, all the guidelines recommend the use of pharmacotherapy alone or in combination with psychotherapy. RCTs in the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) Study, funded by the National Institute of Mental Health, have shown that people whose depression is resistant to initial antidepressant treatment can achieve remission when treated with a secondary strategy. Patients benefited from either augmenting or switching medications or from augmenting with or switching to cognitive therapy; however, remission may take longer to achieve with the use of cognitive therapy (Warden et al., 2007). The meta-analysis by Cuijpers et al. (2011) concluded that combined treatment is more effective than psychotherapy alone and pharmacotherapy alone even for chronic depression. However, a more recent systematic review of the evidence could not provide clear evidence supporting the augmentation of pharmacotherapy with psychotherapy in treatment for chronic depression (von Wolff et al., 2012).
On the basis of extensive research support, all the guidelines recommend CBT and IPT as first-line psychotherapy treatments. They also recommend PST and BA. Cuijpers et al. (2011) found only small differences between types of efficacious psychotherapies, including CBT, IPT, PST, nondirective supportive therapy, and BA. Compared with the other guidelines, the NICE guideline places a higher priority on a group-based format vs an individual format for delivering psychotherapy. The APA guideline does not strongly support the use of a group format for CBT or IPT, because a meta-analyses of their relative effectiveness did not include patients who had rigorously defined MDD. The NICE guideline also makes a stronger recommendation for the use of guided self-help materials and computer-based applications. A recent systematic literature review of computer-based psychologic treatments for depression and a meta-analysis of 19 RCTs support the efficacy and effectiveness of computer-based psychologic treatments for depression in diverse settings and in different populations (Richards and Richardson, 2012).
For patients who have moderate depression, the VA/DOD guideline recommends 16–20 sessions of individual CBT for MDD as a monotherapy, whereas the NICE guideline recommends six to eight sessions (face to face or via telephone), taking place over 9–12 weeks. A synthesis of findings of systematic reviews and trials encompassing 1,716 patients who had MDD or depressive symptoms found that brief CBT and PST (up to eight sessions) are efficacious for acute-phase treatment for depression in primary care (Nieuwsma et al., 2011). That does not appear to be the case for patients who have depressive relapse. A recent systematic review concluded that there is inadequate evidence to determine the effectiveness of brief (lowintensity) interventions (such as mindfulness-based cognitive therapy) for the prevention of relapse or recurrence of depression (Rodgers et al., 2012).
Regarding couple-focused therapy, the VA/DOD guideline notes that there is a smaller body of evidence than for other interventions and therefore recommends its use only for mild to moderate depression in patients who are experiencing marital distress. The findings from a Cochrane Collaboration support that recommendation. The authors concluded that the available evidence suggests that there is no reason to consider marital therapy as more or less effective than individual therapy even when it is associated with marital distress (Barbato and D’Avanzo, 2006).
Although there is a promising empirical base for ACT, a recent review of 18 RCTs found that ACT was not superior to control conditions for distress problems (anxiety and depression) (Powers et al., 2009). Additional research with larger samples and more rigorous designs is needed before more definitive claims can be made about the effectiveness of ACT (Montgomery et al., 2011). Given the lack of evidence supporting ACT as a first-line treatment for MDD, it is worth noting that a VA directive stipulates that veterans who have depression must have access to ACT as one of the treatments (VA, 2008a). ACT is on a priority list of psychotherapies for depression that is part of VA’s initiative to disseminate evidence-based psychotherapies. VA has already provided training in ACT to hundreds of its clinicians.
Pharmacologic Therapies
Each of the three guidelines recommends SSRIs as first-line pharmacotherapy. The APA and VA/DOD guidelines also recommend the SNRIs, bupropion, and mirtazapine as first-line medications. Second-generation antidepressants, such as SSRIs and SNRIs, are more commonly
prescribed over first-generation antidepressants, such as TCAs and MAOIs, because they have lower toxicity (Qaseem et al., 2008). Research shows no clinically meaningful differences in efficacy between the various classes of antidepressant medications. Therefore, prescribing decisions should depend largely on side-effect profile, patient preference and previous experience with treatments, propensity to cause discontinuation symptoms, and safety in overdose (APA, 2010; NICE, 2009). The NICE guideline advocates the use of SSRIs “because SSRIs are equally effective as other antidepressants and have a favourable risk–benefit ratio.”
Somatic Treatments
Each of the guidelines advises the use of ECT for severe MDD. In contrast with the VA/DOD guideline, the APA guideline considers VNS an option for treatment-resistant cases. In 2005, the Federal Drug Administration (FDA) approved the use of VNS in patients who had not responded to at least four trials of antidepressant medication or ECT. However, the role of VNS is the subject of debate (APA, 2010). In 2007, the Centers for Medicare and Medicaid Services decided not to provide coverage for VNS therapy and stated that the only well-designed trial had not demonstrated benefit and the observational studies had biases that made conclusions difficult (Phurrough et al., 2007). A recent systematic review and meta-analysis concluded that insufficient data are available to determine the efficacy of VNS (Martin and Martin-Sanchez, 2012).
Transcranial magnetic stimulation (TMS) is considered a recommended treatment only by APA, which noted that results of RCT had been variable. The treatment had received FDA approval in 2008 for people who had MDD and had not responded to antidepressants. A recent meta-analysis of TMS found that it appeared to be effective although at 4 weeks of followup there had been no further improvement beyond that at the end of treatment (Allan et al., 2011).
Complementary and Alternative Treatments
There are few data on complementary and alternative treatments for MDD. NICE is the only guideline that recommends exercise as a stand-alone first-line treatment; the VA/DOD and APA guidelines consider exercise a helpful adjunct to the treatment plan for MDD. A recent Cochrane Collaboration review combined data from 30 trials and found that exercise seemed to improve the symptoms of depression; however, a much smaller effect on depression was found when the analysis included only methodologically robust trials (Rimer et al., 2012).
The three guidelines differ in their recommendations for light therapy, but each acknowledges that although a number of studies have addressed efficacy they have notable methodologic limitations. On the basis of eight trials, the VA/DOD guideline recommends light therapy only for seasonal MDD. NICE does not recommend light therapy, arguing that studies are difficult to interpret because of equivocal results and methodologic differences. APA gives light therapy its lowest rating for strength of evidence, stating that it appeared effective for seasonal affective disorder and nonseasonal MDD generally in short-term, placebo-controlled trials. A Cochrane Collaboration review of the evidence on light therapy concluded that its benefit is modest, although promising, for nonseasonal depression, but that the results need to be interpreted with caution because of the limited data (for example, many studies were short term or lacked systematic reporting of adverse effects) and the heterogeneity of studies (Tuunainen et al., 2004).
The NICE guideline advises against any use of St John’s wort for depression because of the stated uncertainty about appropriate doses, variation in potencies of preparations, and potential interactions with other drugs; however, the VA/DOD and APA guidelines suggest that use of St. John’s wort may be considered for those who prefer alternative therapies. There is greater consensus about its use in mild to moderate MDD and less for use in more severe MDD (Freeman et al., 2010).
The APA Task Force on Complementary and Alternative Medicine reviewed the available data from RCTs on commonly used CAM treatments for MDD (acupuncture, omega-3 fatty acids, S-adenosyl methione (SAM-e), light therapy, exercise, mindfulness psychotherapies, folate, and St. John’s wort). The task force’s consensus was that although the treatments appear promising, more rigorous and larger studies are needed to determine whether any of them should be formally indicated for MDD (Freeman et al., 2010).
Overall, in light of the results of the guideline comparison and recent research studies, the committee concluded that the VA/DOD guideline recommends state-of-the-art treatment approaches. The one exception, as discussed above, is VA’s emphasis on the use of ACT despite its lack of efficacy in treating for MDD.
Implementation of Department of Defense and Department of Veterans Affairs Guidance for Treatment for Major Depressive Disorder
This section presents information available to the committee on the extent to which DOD and VA provide treatment for service members and veterans who have received a diagnosis of MDD. There is a striking lack of data to inform questions about the extent to which depression treatments are offered, delivered, and completed and whether they are leading to improved patient outcomes.
Department of Defense
The AFHSC reports rates of depression treatment by using data from the PDHA and the PDHRA. In the first quarter of 2010, 67% of active-duty and reserve personnel who received a referral had a health-related clinical encounter within 180 days of return; this slightly exceeded the 2010 target referral rate of 65% (DeFraites and Vythilingam, 2011).
The DOD’s Military Health System Population Health Portal, a centralized database for population health management, includes measures for assessing antidepressant medication and followup care for mental-health hospitalizations, but the committee was unable to identify results of the use of the measures. The specifications for depression-related measures are based on the Antidepressant Medication Management (AMM) measure in the Healthcare Effectiveness Data and Information Set (HEDIS) that the National Committee for Quality Assurance (NCQA) reports annually regarding the commercial, Medicare, and Medicaid markets. One measure focuses on compliance with medication regimens for treating MDD. Two rates are reported for the measure: the percentage of patients who have diagnoses of a new episode of major depression and who were treated with antidepressant medication and remained on the treatment for at least 12 weeks (“effective acute phase treatment”) and the percentage who remained on medication for at least 6 months (“effective continuation phase treatment”). The other measure assesses followup therapy to patients after they have been hospitalized for mental illness. Two rates are reported for the measure: the percentage of patients who were hospitalized for selected
mental-health disorders and who received followup within 7 days of discharge and the percentage who received followup within 30 days of discharge (MHSPHP, 2012).
Department of Veterans Affairs
VA reports that there is no mechanism for tracking the delivery of evidence-based therapies in the VA centralized databases. VHA is developing progress-note templates for evidence-based treatments that will allow documentation of care in the computerized record in a manner that will facilitate the collection of centralized aggregate data (IOM, 2012). The committee obtained the data discussed below, which suggest that many veterans are not getting necessary treatment and that most of those who are getting it are not completing the full course.
In 2006, VA contracted with Altarum Institute and RAND to conduct an independent evaluation of the quality of VA mental-health and substance-use care (Watkins and Pincus, 2011). The evaluation included several depression-related measures calculated for a cohort of veterans who had MDD and were identified for each fiscal year from FY 2004 through FY 2008. The MDD cohort selection was based on International Classification of Diseases, Ninth Revision codes in the administrative records and reflected at least one inpatient episode or two outpatient visits (for any mental-health or non-mental-health diagnosis) of a given patient in a given fiscal year.
In FY 2007, of patients in the MDD cohort and defined as experiencing a new treatment episode, 49% received a 12-week supply of antidepressants within 12 weeks, and 31% received a 180-day supply within 180 days. In addition, 60% of veterans in the MDD cohort who had at least one filled prescription for an antidepressant received a 12-week supply within 12 weeks. (That measure is one of the rates in the NCQA HEDIS AMM measure, which is also reported by DOD, as mentioned above.) Those results suggest that adequate followup care is needed to improve patients’ adherence to treatment.
Indicators used to measure followup assessment examined whether there was documentation that a patient responded to treatment, including side effects and adherence. About one-fourth of veterans in the MDD cohort who were receiving psychotherapy had documentation of an assessment of response to psychotherapy, and 55% of those who received at least one prescription for psychiatric medications had documentation of assessment of response. Those findings reflect a need for improvement in continuing patient care and assessment once treatment is provided.
Treatment rates also appeared to be low. For the indicator used to assess use of evidenced-based treatments for MDD as documented in administrative and medical-record data, 31% of those in the MDD cohort who received psychotherapy had documentation of at least one visit for CBT (including behavioral therapy and cognitive therapy). The researchers noted that it is possible that some veterans were receiving evidence-based treatments other than those measured. For example, they were unable to assess whether veterans received IPT, an evidencebased psychotherapy often used instead of CBT.
To improve implementation of treatment regimens, VA is undertaking a national effort to disseminate throughout its health care system evidence-based psychotherapies for depression and other mental-health conditions. Since 2007, VA has been working to disseminate CBT and ACT. It began working to disseminate IPT in 2011. Competence-based training of VA mental-health care providers in the delivery of those therapies is a component of the strategic plan. Such
training involves experientially based workshop training followed by weekly consultation for 6 months with an expert in the treatment (Karlin et al., 2010). As of March 31, 2010, VA has provided training for 330 VA mental-health staff in the delivery of CBT or ACT, and some staff have been trained in the delivery of both (Karlin, 2010).
Overall, the committee commends VA on its effort to improve the implementation of CBT for depression, but it questions the inclusion of ACT in the psychotherapy dissemination effort. As discussed above, there is a lack of evidence supporting ACT as a first-line treatment for MDD. The committee is confounded by VA’s directive stipulating access to ACT as one of the treatments for depression (VA, 2008a) and its decision to include ACT in the national training and rollout of evidence-based psychotherapies.
Summary
Overall, our review suggests that the screening for, diagnostic assessment of, and treatment for depression through DOD and VA is consistent with current standards and guidelines for care. The measures that are used have adequate psychometric properties and are among those advocated by experts in the field. With the exception of ACT, the VA/DOD guidelines for the assessment and treatment of depression are by and large consistent with other practice guidelines—those developed by APA and NICE—in the field. What remains questionable to the committee is how much the treatments are actually offered, delivered, and completed and whether they are leading to improved patient outcomes.
SUBSTANCE-USE DISORDERS
The term substance-use disorders encompasses different substances—such as alcohol, opioids, cocaine, cannabis, prescription medications, and nicotine—and various disorders that are associated with their use, including abuse, dependence, intoxication, withdrawal, and resulting psychiatric problems. Substance abuse and dependence constitute formal diagnostic categories that are described in Chapter 4. Substance misuse is often used to characterize use that is thought to be clinically significant insofar as it is associated with specific adverse consequences, it but does not meet the diagnostic criteria (Kleber et al., 2006).
As prevalence data in Chapter 4 show, a substantial number of service members and veterans of OEF and OIF have had diagnoses of SUDs, and the numbers have been increasing since the conflicts began. Because SUDs have harmful effects on physical, psychologic, and social well-being, it is important to identify and evaluate people who are at risk for SUDs and to treat those who have a diagnosis of substance abuse or dependence. The goals of treatment include abstinence or reduction in substance use, relapse prevention, and improvement in psychologic and social functioning. The specific type of intervention or treatment will depend on the type of substances used, the intensity of use, and the patient’s individual needs. SUDs commonly occur with other mental-health conditions (such as PTSD and depression) and with chronic medical illnesses (such as diabetes) that also require treatment. For many, a SUD is a chronic disorder that requires multiple interventions and continuing monitoring.
To assess the efficacy of current screening, assessment, and treatment approaches to SUDs in DOD and VA, the committee reviewed the VA/DOD Clinical Practice Guideline for the Management of Substance Use Disorders (SUD), August 2009 (VA and DOD, 2009c). The
VA/DOD guideline applies to adult patients who have substance-use conditions that are treated in a VA/DOD clinical setting, including patients who have both substance-use and other health conditions and patients who have any level of severity ranging from hazardous and problematic use to SUDs. The guideline is relevant to all health care professionals who provide or direct treatment services to patients who have substance-use conditions in any VA/DOD health care setting, including specialty SUD care. The committee focused on the management of patients who have dependence on alcohol or opioids and to a smaller extent patients who have dependence on cocaine and cannabis. The committee did not address nicotine dependence in its assessment, because nicotine, although strongly linked with important medical consequences, rarely causes the behavioral or social harm seen with alcohol or illicit-drug dependence (Kleber et al., 2006).
Recently, the IOM Committee on Prevention, Diagnosis, Treatment, and Management of Substance Use Disorders in the U.S. Armed Forces completed a comprehensive assessment of the current policies and programs in place in the different branches of the military that pertain to the prevention of, screening for, diagnosis of, and treatment for SUDs in active-duty service members, members of the National Guard and reserves, and military dependents. The 2010 National Defense Authorization Act in Sec. 596 authorized the Comprehensive Plan on Prevention, Diagnosis, and Treatment of Substance Use Disorders and Disposition of Substance Abuse Offenders in the Armed Forces, which mandated an internal program review by DOD (DOD, 2011b) and an external review by an independent organization, such as IOM. See IOM’s Substance Use Disorders in the U.S. Armed Forces (IOM, 2013) for all the committee’s major findings and recommendations for improvements in SUD prevention, diagnosis, and treatment for active-duty service members, military dependents, and members of the reserves.
Provision of Substance-Use Disorder Services
Department of Defense
DOD substance-use screening, assessment, and treatment services for all beneficiaries are provided through the direct military health care system and TRICARE-authorized providers in the private sector. Current policy permits substance-use treatment in TRICARE-authorized hospitals, clinics, and certified freestanding treatment facilities. TRICARE does not cover substance-abuse care delivered in an individual provider’s office and has in place yearly and lifetime limits on some forms of care that may affect the delivery of appropriate care. DOD reported to Congress that TRICARE is actively pursuing modification of the policies to expand coverage of substance-abuse treatment in primary care (DOD, 2011b).
DOD policy does not address the standardized collection of clinical and administrative data and outcome measures that would be useful for monitoring the provision of SUD prevention, diagnosis, and treatment services. Nor does it address the degree to which clinical practice recommendations related to SUD assessment and treatment are implemented (DOD, 2011b).
Department of Veterans Affairs
VA provides SUD services in SUD-specific settings that include inpatient programs, residential rehabilitation treatment programs, outpatient programs that provide intensive treatment (at least 3 hours per day 3 days per week) or low-intensity or medication-assisted
treatment services. VA also provides SUD-related care in non-SUD settings, such as primary care clinics, mental-health clinics, and specialized programs for treating PTSD (GAO, 2010).
Prevention of Substance-Use Disorders
In IOM’s Substance Use Disorders in the U.S. Armed Forces, the committee stated that “effective prevention has the potential to minimize the need for diagnosis, treatment, and management of SUDs and reduce the enormous social and economic costs of alcohol and drug dependence.” That report cites the 2011 National Drug Control Strategy, which identifies the military personnel, veterans, and their families as important populations for receiving substanceabuse prevention services (IOM, 2013).
DOD SUD-prevention services range from individual screening and counseling services to large multimedia campaigns. Strategies include implementing policies and programs that regulate alcohol availability and pricing, deglamorize alcohol use, and promote personal responsibility and good health. Despite the military’s efforts to address problems with substance use, there has been little formal evaluation of the effectiveness of programs, and program implementation is not widespread or sufficiently targeted to high-risk populations, such as service members who have PTSD (Ames and Cunradi, 2004; DOD, 2011b; Seal et al., 2011).
Department of Defense and Department of Veterans Affairs Guidance for Screening for Substance-Use Disorders
The VA/DOD SUD guideline recommends universal screening for alcohol use; however, it does not recommend universal screening for other drug use, because there is a lack of evidence of the efficacy of screening for substances other than alcohol and tobacco (Polen et al., 2008). Neither the military nor VA conducts universal screening for the misuse of nonalcoholic substances. However, DOD policy requires drug testing (urine analysis) for a variety of illegal and legal drugs under various circumstances—in new military entrants, for probable cause, for medical reasons, and so on (DOD, 1994). In February 2012, DOD announced an expansion of its drug-testing program to include widely abused prescription medications that contain hydrocodone and benzodiazepines. Service members who have approved prescriptions for those medications will not be subject to disciplinary action for using them within the dosage and time prescribed. VA policy guidance states that health care providers should use targeted case-finding methods to identify substance use in patients and evaluate signs and symptoms of substance use in patients who have other relevant conditions, such as other mental-health disorders, hepatitis C, and HIV (VA, 2008a).
The VA/DOD SUD guideline calls for annual screening of patients in general care and mental-health care settings to identify unhealthy alcohol use. The guideline’s reference to unhealthy alcohol use encompasses drinking behavior that includes severe alcohol dependence as defined by DSM-IV (see Chapter 4) and drinking above limits established by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) (NIAAA, 2008). NIAAA recommends maximum alcohol limits of no more than 14 drinks in a week and no more than four drinks in a day for men and no more than seven drinks in a week and no more than three drinks in a day for
women.5 Drinking above the recommended limits is called risky or hazardous drinking. Figure 5.6 shows the process for screening for and initial assessment of substance use as presented in the VA/DOD guideline.
The VA/DOD guideline recommends annual screening for unhealthy alcohol use with one of two brief, standardized screening instruments: the AUDIT Consumption Questions (AUDIT-C) (Babor et al., 2001) and the version of the Single-Item Alcohol Screening Questionnaire (SASQ) recommended by NIAAA (2008).6 The AUDIT-C comprises the first three questions on the 10-item Alcohol Use Disorders Identification Test (AUDIT), which was developed by the World Health Organization (WHO) for use in primary care settings to identify persons whose alcohol consumption has become hazardous or harmful. The three-item AUDIT-C asks about quantity and frequency of drinking and is scored on a scale of 0 to 12. The screen is considered positive for unhealthy alcohol use if the total score for a patient’s responses is 4 or higher for men or 3 or higher for women. However, when the points are all from Question 1 (that is, the scores for Questions 2 and 3 are zero), a patient is considered to be drinking below recommended limits (see Box 5.6).
The version of the SASQ recommended by NIAAA comprises a single item that asks about heavy drinking in the preceding year. A positive screen is any report of having five or more drinks for men or four or more for women on an occasion in the preceding year (see Box 5.7).
For patients who screen positive or who have clinical conditions that contraindicate alcohol use, the VA/DOD guideline recommends assessing current alcohol consumption relative to NIAAA’s recommended limits. If they are exceeded, brief alcohol counseling by a clinician or counselor (often termed brief intervention) is recommended. Brief interventions can be a single session or multiple sessions involving motivational interviewing techniques focused on drinkingrelated consequences and benefits of reducing alcohol use.
The guideline recommends referral to specialty SUD care for addiction treatment for a patient who has an AUDIT-C score of 8 or higher or who meets one of the following criteria: needs additional evaluation, does not respond to brief intervention, has a DSM diagnosis of alcohol or other substance dependence, or has received previous treatment for SUDs. In addition, any DOD active-duty member involved in an incident in which substance use is suspected to be a contributing factor is required to be referred to specialty SUD care for evaluation.
__________________
5NIAAA recommendations are based on definitions of a standard drink as 12 oz of beer, 5 oz of wine, and 1.5 oz of hard liquor (80-proof spirits).
6The AUDIT-C and SASQ are first-line screening instruments recommended by the VA/DOD guideline, but the guideline also identifies other commonly used screening tests (for example, the CAGE questionnaire augmented with the 10-item AUDIT instrument).
BOX 5.6
AUDIT Consumption Questions (AUDIT-C)
How often did you have a drink containing alcohol in the past year?
0 = Never
1 = Monthly or less
2 = Two to four times per month
3 = Two to three times per week
4 = Four or more times per week
On days in the past year when you drank alcohol how many drinks did you typically drink?
0 = 0-2 drinks
1 = 3 or 4 drinks
2 = 5 to 6 drinks
3 = 7 to 9 drinks
4 = 10 or more drinks
How often did you have six or more drinks on one occasion in the past year?
0 = Never
1 = Less than monthly
2 = Monthly
3 = Weekly
4 = Daily or almost daily
SOURCE: Babor et al., 2001.
BOX 5.7
Single-Item Alcohol Screening Questionnaire (SASQ)
Do you sometimes drink beer, wine or other alcoholic beverages?
Yes or No
If Yes,
How many times in the past year have you had…
5 or more drinks in a day (men)
4 or more drinks in a day (women)
SOURCE: HHS, 2005.
Department of Defense
In DOD, routine alcohol screening with the AUDIT-C occurs during DOD’s periodic health assessments, the PDHA and the PDHRA, which are briefly described in the introduction to this chapter. In addition, urinalysis testing is random and applied to all personnel.
Commanders may order a drug test if there is suspicion of drug use. In May 2012, DOD also implemented new practices for its urinalysis drug testing programs to screen for some of the most commonly abused prescription medications (for example, hydrocodone and benzodiazepines). It is too early to tell whether these new measures will affect the prevalence of prescription drug abuse in the military (IOM, 2013). Screening may occur at medical appointments, but DOD does not mandate a common set of screening tools and processes in primary care settings.
Department of Veterans Affairs
VA implemented routine screening for alcohol misuse in 2004 and since 2006 has required that the AUDIT-C be used for screening in either an outpatient or an inpatient setting. VA policy stipulates that all veterans coming to VA for the first time must be screened for alcohol misuse and again annually for patients in primary care, appropriate medical specialty care settings, and mental-health care services (VA, 2008a). In 2008, the VHA clinical-reminder tracking system used at its medical facilities incorporated the AUDIT-C questions; the system prompts clinicians to conduct appropriate followup (for example, brief intervention or referral to specialty care) on the basis of patient responses.
Validity of Tools for Screening for Substance-Use Disorders
In 2004, the USPSTF found good evidence that screening in primary care settings can accurately identify patients whose levels or patterns of alcohol consumption place them at risk for increased morbidity and mortality. The USPSTF also found good evidence that brief behavioral-counseling interventions produce small to moderate reductions in alcohol consumption (HHS, 2004). Similarly, results of a 2007 Cochrane Collaboration meta-analysis of 22 RCTs (which enrolled 7,619 participants) showed that male but not female participants who received brief intervention had lower alcohol consumption than the control group after followup of a year or longer (Kaner et al., 2007).
Screening, Brief Intervention, and Referral to Treatment Model
Clinical guidance for the management of SUDs developed by VA/DOD, APA (Connery and Kleber, 2007; Kleber et al., 2006), NIAAA (2008), and NICE (2011) are consistent in recommending the SBIRT model, a comprehensive mental-health approach for the prevention of and intervention in risky alcohol use. The model includes screening for at-risk drinking, providing a brief intervention, and providing referral to specialty substance-use treatment for those who have alcohol dependence (IOM, 2012a; SAMHSA, 2011).
Evidence supporting the efficacy of the SBIRT model is not yet as plentiful or compelling for drug misuse as it is for alcohol misuse. It is also important to note that the effectiveness of SBIRT programs can depend on their fidelity, application, and comprehensiveness (SAMHSA, 2011), and significant staff training and continuing monitoring are needed to sustain their effective implementation.
Alcohol Use Disorders Identification Test-Consumption Questions
Extensive research shows that the AUDIT-C is an effective screening instrument for alcohol misuse in men and women and that the optimal screening threshold (maximizing
sensitivity and specificity) for alcohol misuse is a cut score of 4 in men and a cut score of 3 in women (Bradley et al., 2003, 2007; Dawson et al., 2005).
Single-Item Alcohol Screening Questionnaire
Findings from a cross-sectional study showed that the single screening question recommended NIAAA accurately identifies unhealthy alcohol use in a sample of primary care patients. The sensitivity and specificity (81.8% and 79.3%, respectively) of the single-question screen was comparable to that reported for longer instruments in other studies, including the AUDIT, which is among the best validated options for alcohol screening in primary care settings (Smith et al., 2009).
Implementation of Department of Defense and Department of Veterans Affairs Guidance for Screening for Substance-Use Disorders
Below is information available to the committee on the extent to which DOD and VA are implementing and tracking screening procedures to identify possible SUD. The sparse information shows lapses in the DOD and VA’s identification of and followup with patients with substance use problems. It raises concerns about how well the DOD and VA are implementing and monitoring their SUD screening practices.
Department of Defense
DOD’s internal review of SUD programs and policies (DOD, 2011b) found that with the exception of the deployment cycle, evidence-based screening tools are not consistently used among the military services. Non-active-duty service-member beneficiaries who screen positive for SUDs in primary care are probably referred to the TRICARE network, and this decreases the likelihood of patient followup for care. Furthermore, DOD stated that staff shortages may prevent adequate screening and identification of at-risk substance-use behavior, particularly during high-demand periods, such as when many service members are returning from deployment (DOD, 2011b). In IOM’s Substance Use Disorders in the U.S. Armed Forces, the committee found that current DOD policy and screening practices to detect the use of drugs and alcohol are relatively inefficient and identify only a portion of drug users at risk for developing SUDs (IOM, 2013). That committee strongly emphasized the need for systematic and routine substance use screenings in DOD health care settings and improvements in the monitoring of prescriptions.
Department of Veteran Affairs
Under VA’s Performance Management Program, VA uses several performance measures to see whether veterans are being screened for SUD (AHRQ, 2012). The committee was unable to identify results of using those measures, and inquiries to VA about performance measures did not yield information about them.
One measure assesses the percentage of eligible patients who are seen in outpatient or inpatient settings and screened annually for alcohol misuse with the three-item AUDIT-C. Another measure assesses the percentage of veterans who are screened for alcohol misuse with AUDIT-C and meet or exceed a threshold score of 5 and who have timely brief alcohol counseling. The VA/DOD guideline indicates that although AUDIT-C scores greater than 4
points in men and greater than 3 points in women mean a positive screen, an AUDIT-C score of 5 or more is appropriate for performance measurement in a setting where brief alcohol counseling is required for everyone who screens positive for alcohol misuse.
In response to a recent GAO review of VA’s provision of SUD services, VA reported that in FY 2009 about 96% of a sample of veterans seen in VA medical centers throughout the nation received the recommended screening for alcohol misuse (GAO, 2010). Although SUD screening rates in VA are high, research suggests that relatively few of those who screen positive receive guideline-recommended brief intervention, referral to treatment, or followup. In a national sample of 1,508 OEF and OIF veterans who were screened in an outpatient setting, 40% screened positive for potentially hazardous drinking. Of the veterans who had potentially hazardous drinking behavior, 31% reported being counseled to cut back on or abstain from drinking. The likelihood of risk-reduction counseling increased with the severity of alcohol misuse (higher AUDIT-C scores). Those findings are based on data collected in 2005 from the Survey of Healthcare Experiences (SHEP); the response rate was 21%, and nonresponders were more likely to be male and to have served in active-duty units vs those in the reserves or National Guard (Calhoun et al., 2008).
In another study that compared a national sample of OEF and OIF veterans with a sample of non-OEF and non-OIF veterans, researchers examined rates of documented brief interventions and rates of referrals to treatment. The study sample included outpatients who were screened for alcohol misuse in 2006–2007. About half of all the veterans who screened positive for alcohol misuse had brief interventions or referrals for treatment documented in the medical record. The difference in rates between OEF and OIF veterans (50.9%) and the other veterans (52.3%) was not statistically significant. Researchers noted one possible study limitation: the study sample reflects a period that preceded VA’s implementation of a performance measure that requires documentation of brief intervention for patients who screen positive for alcohol misuse and the implementation of the electronic clinical reminder that facilitates appropriate screening and followup (Hawkins et al., 2010). In fact, a recent study found that implementation of the clinical reminder for brief interventions is associated with increases in the prevalence of documented brief alcohol interventions in VA. The percentage of patients with alcohol misuse who had documentation of brief intervention increased from 5.5% prior to the implementation of the clinical reminder to 29% after implementation (Lapham et al., 2012).
Findings from Bradley et al. (2011) suggest that many veterans, particularly black veterans, are being missed by clinical screening. Using a national sample of 6,861 patients in VA outpatient care in 2007–2008, the study compared AUDIT-C results that were documented during routine outpatient care (referred to as the “clinical screen”) with AUDIT-C results collected by a mailed survey. Alcohol-screening results were considered discordant if patients screened positive on the clinical screen or on the mailed survey screen but not both. About twice as many patients screened positive for alcohol misuse on the mailed survey screen as on the clinical screen: 11.1% (765) and 5.7% (6,096), respectively. About 60% (468) screened positive on the mail survey and negative on the clinical screen. Only 1.5% (93) of patients screened negative on the mail survey and positive on the clinical screen. The researchers found that discordance was significantly higher in black patients than in white patients; however, they noted the difference might be due to a greater tendency among black patients to attempt to answer questions in a manner viewed favorably by the researchers or to variation in the administration of the AUDIT-C.
Department of Defense and Department of Veterans Affairs Guidance for Assessment and Diagnosis of Substance-Use Disorders
After screening for SUD, a clinical interview may be needed for further assessment of a substance-use problem against diagnostic criteria and for determination of the type and intensity of treatment needed. Figure 5.7 shows the process presented in the VA/DOD guideline for assessing, diagnosing, and treating for SUDs in a primary care setting.
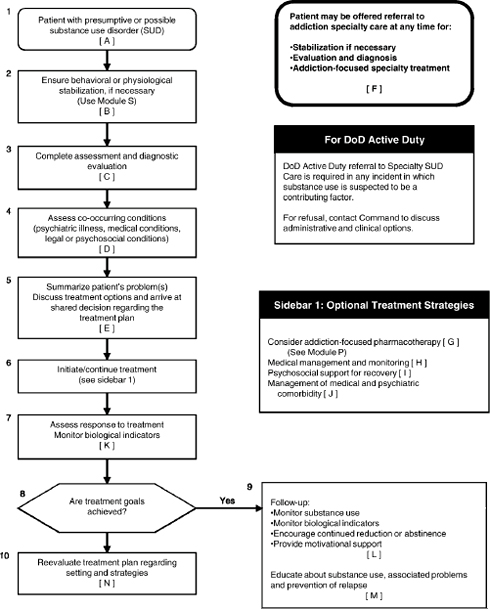
FIGURE 5.7 Algorithm for SUD care in primary care.
SOURCE: VA and DOD, 2009c.
The VA/DOD guideline instructs providers to conduct a comprehensive biopsychosocial assessment that covers physical, emotional, cognitive, behavioral, emotional, and environmental domains. The assessment should gather information about the patient’s personal and family medical, psychologic, social, and alcohol-use and drug-use history. Providers should conduct appropriate laboratory tests (for example, for sexually transmitted diseases and liver function) and a mental-status examination. The guideline emphasizes that co-occurring disorders are
common with SUDs and should be identified as part of the comprehensive assessment. A provider’s documented summary of the assessment serves as the basis of the treatment plan.
The guideline does not exclusively endorse the use of any particular instrument as the basis of a comprehensive assessment; however, the Addiction Severity Index (ASI) (McLellan et al., 1980) is identified as an accepted tool. The ASI is a standardized, rater-administered interview that assesses seven functional domains considered important in an overall addiction evaluation: medical status, employment status, legal problems, family and social relations, drug use, alcohol use, and psychiatric status.
The guideline indicates that patients may be referred to specialty care on the basis of the following indications for treatment: an AUDIT-C score of 8 or more for men and women, hazardous use of a substance, substance abuse, substance dependence, risk of relapse, suspected or possible SUD, and mandated referral within DOD.
The guideline identifies care-placement criteria that were developed by the American Society of Addiction Medicine (ASAM) and are used to steer providers in the determination of the appropriate treatment setting. The criteria consider problem severity in making recommendations for specific levels of care. Although ASAM criteria constitute the most widely accepted placement system, the guideline indicates that there is little evidence to support its validity on the basis of controlled trials.
After initial treatment, the VA/DOD guideline recommends periodically reassessing a patient’s response to treatment (for example, continuing substance use, medication side effects, and emerging symptoms) by using a standardized and valid instrument and laboratory tests. The Brief Addiction Monitor (BAM), a newly introduced 17-item questionnaire developed by VA that measures symptom-level outcomes and functional outcomes, is offered as an example of a monitoring instrument.
Validity of Tools for Assessment and Diagnosis of Substance-Use Disorders
The outcomes of an effective assessment are a valid, reliable diagnosis and referral to the most appropriate level of care of treatment services. According to the Substance Abuse and Mental Health Services Administration, many public-sector substance-abuse treatment systems define assessment procedures that require use of a level-of-care assessment tool (often the ASAM criteria) and a comprehensive addiction severity and outcome measure, such as the ASI (Center for Substance Abuse Treatment, 2005).
Addiction Severity Index
The ASI, developed in VA, is considered the most widely used clinical and research assessment instrument for people who have SUDs. It is a semistructured interview used to assess SUD severity and quantifies change over time in problems commonly associated with substance abuse. In clinical settings, it is useful for treatment planning and outcome evaluation in that it identifies problems in need of targeted intervention. The ASI should be administered, scored, and interpreted by a trained technician or clinician. Good reliability and validity have been demonstrated in a variety of settings (Alcohol and Drug Abuse Institute Library, 2012). Extensive use of the ASI and changes in the SUD field over the years has revealed its limitations. Research is going on to remedy gaps in content and psychometric deficiencies (Cacciola et al., 2011).
Addiction Medicine Patient Placement Criteria, Second Edition-Revised
As mentioned, ASAM has uniform criteria for treatment planning and placement for clients who have addiction and co-occurring disorders. The current edition, ASAM PPC-2R (Mee-Lee et al., 2001), includes criteria for comorbid mental-health and substance-related disorders. The criteria are used to match intensity of service to severity of illness in a continuum of care and to prescribe a treatment level that can accomplish treatment objectives (American Society of Addiction Medicine, 2012).
The ASAM PPC-2R has not undergone much validity testing, but it is widely accepted by public and private treatment programs and has been used to guide addiction treatment placement in more than half the states. Other placement instruments are considered simpler to use than ASAM PPC-2R but are less sensitive to the needs of people who have SUDs and do not differentiate between mental and substance-related symptoms (Center for Substance Abuse Treatment, 2005).
Brief Addiction Monitor
As a treatment monitoring instrument, the BAM, if fully implemented, could be used to evaluate outcomes and effectiveness of SUD treatments throughout the VA system (GAO, 2010). The first study to evaluate the BAM’s psychometric properties revealed good validity (Cacciola et al., 2012), but further research is warranted.
Implementation of Department of Defense and Department of Veterans Affairs Guidance for Assessment and Diagnosis of Substance-Use Disorders
This section presents information available to the committee on the extent to which DOD and VA conduct followup and evaluation of service members and veterans who have positive SUD screens. The information shows significant gaps in DOD and VA SUD assessment and referral to treatment. The significant number of service members and veterans who are at risk of SUD but are not receiving needed interventions is a serious concern.
Department of Defense
DOD is missing opportunities to intervene with service members who have high levels of drug or alcohol consumption. Data shows that treatment providers may fail to identify at-risk substance users who need referral to specialty care. Additionally, many patients may be offered a referral, but choose not to accept it, or encounter barriers, such as concerns about confidentiality, that prevent visits to specialty care (Glass et al., 2010; Milliken et al., 2007). In FY 2010, there were over 24,000 referrals of soldiers to the Army Substance Abuse Program; of those referred, about 50% enrolled. Although 12% of soldiers reported alcohol problems on the PDHRA, only 2% have been referred for further evaluation or treatment (Department of the Army, 2012). Among soldiers returning from Iraq, Milliken et al. (2007) found that soldiers frequently reported alcohol problems but were rarely referred for alcohol treatment and were infrequently followed up. Of 56,350 active-duty soldiers, 6,669 (11.8%) endorsed alcohol misuse, 134 (0.2%) were referred, and only 29 were seen within 90 days (Milliken et al., 2007). Some of the possible reasons cited include the stigma associated with receiving any form of mental-health care and concerns related to present military policies; SUD treatment triggers involvement of a soldier’s
commander, and failure to comply with the treatment program can have adverse career ramifications (Burnett-Zeigler et al., 2011; Milliken et al., 2007).
In response to the concerns over confidentiality and possible stigma, the Army implemented a pilot program, Confidential Alcohol Treatment and Education Pilot (CATEP), which allows service members to refer themselves for alcohol-abuse treatment without notifying their chains of command. In its Comprehensive Plan, DOD reported that it will evaluate the findings from CATEP to determine the effect of waiving the policy requirement for command notification (unless a soldier’s condition poses a threat to safety, security, or mission) (DOD, 2011b). Under current DOD policy for active-duty members, clinical providers convene with command to review the treatment plan and goals. Service members who fail to engage in recommended treatment are informed that such a decision could result in involuntary separation from military service.
Department of Veteran Affairs
In VA, rates of referral to SUD treatment indicate a large number of veterans with alcohol misuse appear not to be receiving referrals. Hawkins et al. (2010) reported that half the veterans who screened positive for alcohol misuse had a documented brief intervention or referral to alcohol treatment. In GAO’s assessment of VA’s SUD services, providers reported that limitation in resources was a factor in decisions about referrals for treatment (GAO, 2010).
Department of Defense and Department of Veterans Affairs Guidance for Treatment for Substance-Use Disorders
Withdrawal Management
Detoxification and withdrawal management is often a necessary first step toward treatment of those who have SUDs. The VA/DOD guideline defines withdrawal management from a substance as “non-pharmacologic and/or pharmacologic medical care with a goal of safely transitioning a patient from active use to sustained treatment for the patient’s substance use disorder.”
Pharmacologically supervised withdrawal is warranted only for alcohol, sedative hypnotics, and opioids; it is not warranted for stimulant and cannabis disorders.
For inpatient treatment for alcohol withdrawal, the VA/DOD guideline recommends the use of benzodiazepines as first-line treatment with other agents (such as beta-blockers and clonidine) as adjuncts in some patients. For opioid withdrawal, the guideline recommends initial stabilization and then short or extended tapering with buprenorphine and naloxone or methadone in 4–7 days in an inpatient setting. Withdrawal management should be followed by appropriate pharmacologic maintenance or behavioral therapies.
Addiction-Focused Treatment
In general, the VA/DOD guideline recommends the use of addiction-focused pharmacotherapy and psychosocial treatments after patients who were dependent on alcohol or opioids have undergone successful withdrawal.
Figure 5.8 shows the process presented in the VA/DOD guideline for treating patients who have a diagnosis of SUD with medications.
FIGURE 5.8 Algorithm for addiction-focused pharmacotherapy.
SOURCE: VA and DOD, 2009c.
For patients with alcohol-use disorders (AUDs), the first-line pharmacotherapies recommended by the VA/DOD guideline are oral naltrexone and/or acamprosate7; both are FDA approved for this indication. The guideline discusses psychosocial interventions that research has shown to be effective: behavioral couples counseling, cognitive behavioral coping skills training, community reinforcement, motivational enhancement, and 12-step facilitation.
For patients who are dependent on opioids, the VA/DOD guideline recommends as firstline treatment methadone or the sublingual combination product of buprenorphine and naloxone. Those drugs are used in opioid-agonist treatment (OAT), which consists of administering one of the opioid-agonist medications in combination with a variety of medical, counseling, and rehabilitative services. OAT can be delivered through a VHA-licensed OAT clinic or through office-based treatment; however, buprenorphine is the only medication approved for office-based OAT. As adjunct interventions in pharmacotherapy, the guideline identifies cognitive behavioral therapy (CBT) and contingency management as effective psychosocial therapies for opioid dependence.
__________________
7The guideline recommends injectable naltrexone when medication adherence is an important concern.
For DOD active-duty members, OAT is generally not a treatment option. DOD has reported to Congress that TRICARE is pursuing changes in the Code of Federal Regulations that would permit the use of opioid agonists and partial agonists (such as methadone and buprenorphine) for opioid-dependence maintenance treatment of non-active-duty beneficiaries (DOD, 2011b). The recent IOM Committee on Prevention, Diagnosis, Treatment, and Management of Substance Use Disorders in the U.S. Armed Forces supports that change in policy. That committee concluded that “the TRICARE benefit for SUD care should provide coverage for all evidence-based forms of care, including maintenance medications” (IOM, 2013).
The VA/DOD guidance regarding the management of cocaine and marijuana use is limited to recommendations for psychosocial interventions. CBT, behavioral couples therapy, and contingency management are identified as interventions supported by the most evidence of effectiveness in treating for cocaine dependence. For cannabis, the guideline indicates that there is some evidence that CBT is effective.
Comparison of Guidelines for Treatment for Substance-Use Disorders
This section compares the VA/DOD SUD guidelines with evidence-based CPGs for the management of SUD developed by APA (Connery and Kleber, 2007; Kleber et al., 2006), NIAAA (2008), NICE (National Collaborating Centre for Mental Health, 2011), and WHO (2009). As discussed below, all the guidelines are mainly consistent in their recommendations for specific treatments for managing SUD. IOM’s Substance Use Disorders in the U.S. Armed Forces (IOM, 2013) provides additional details about the types of SUD pharmacotherapies and psychotherapies discussed below.
Alcohol
The VA/DOD, APA, NIAAA, and NICE guidelines are largely consistent in their recommendations for specific treatments for managing alcohol dependence. Standard clinical practice for treatment for alcohol dependence supports the use of complementary approaches—medications, professional counseling, and mutual help groups—to address the neurobiologic, psychologic, and social aspects of alcohol dependence. Table 5.4 compares treatment recommendations of these guidelines and their various systems for indicating their strength.
TABLE 5.4 Summary of Guideline Recommendations for Treating for Alcohol-Use Disorders
| Treatment Modality | VA/DOD | APA | NIAAA | NICE |
| Management of withdrawal Thiamine | I | √ | √ | |
| Benzodiazepines | A | I | √ | √ |
| Anticonvulsants, beta adrenergic blockers or antipsychotics agents | C (adjunct therapy) | II (adjunct therapy) | √ (adjunct therapy) | |
| Psychotherapy | ||||
| Motivational Interventions | First line | I | √ | √ |
| Twelve Step Facilitation (TSF)/Mutualhelp groups (e.g., Alcoholics Anonymous) | First line | I | √ | √ |
| Cognitive behavioral therapy (CBT) | First line | I | √ | √ |
| Couple/marital-focused therapies | First line | I | √ | √ |
NOTE: VA/DOD: A = good evidence that the intervention improved outcomes; B = a fair amount of evidence supported the use of the intervention; C = the working group did not make a recommendation for or against the routine use of the intervention as the risk-benefit ratio was too close to make a general recommendation; D = presence of evidence that either the intervention was harmful or the risks outweighed the benefits offered by it; I = evidence was lacking, of insufficient quality, or conflicting; therefore, a recommendation could not be made for or against providing the treatment routinely. APA: I = intervention recommended with substantial clinical confidence; II = intervention recommended with moderate clinical confidence; III = intervention recommended on the basis of individual circumstances. NIAAA and NICE: No rating system was used. For purposes of this report, v denotes that use of the treatment was recommended.
Pharmacotherapy
The VA/DOD, APA, NIAAA, and NICE guidelines are consistent in recommending the use of benzodiazepines for the management of alcohol withdrawal before the initiation of treatment for alcohol dependence. The VA/DOD guideline is the only one that does not mention the administration of thiamine. All guidelines except NICE also suggest the use of anticonvulsants, beta adrenergic blockers, or antipsychotics as adjuncts to benzodiazepines in treatment for alcohol-withdrawal syndrome.
All the guidelines state that after successful withdrawal by people who have moderate or severe alcohol dependence, medications for alcohol dependence used in conjunction with brief support or more extensive psychosocial therapy can be effective in primary care and specialty care medical settings.
FDA has approved three medications for the treatment of alcohol dependence: disulfiram, acamprosate, and naltrexone (in daily oral and monthly injectable formulations). Those medications for alcohol-dependent patients have well-established efficacy. They have been shown to help patients to reduce drinking, avoid relapse to heavy drinking, and achieve and maintain abstinence (NIAAA, 2008).
Each guideline recommends naltrexone and acamprosate as first-line pharmacologic treatments for alcohol dependence. Disulfiram is considered to be an effective adjunct to a comprehensive treatment program for patients who are motivated to abstain. NIAAA is the only guideline that suggests the use of topiramate, an anticonvulsant, to treat for alcohol dependence; it notes that FDA has not approved the drug for this purpose. The NICE guideline indicates that the evidence does not show an advantage of topiramate over other pharmacologic interventions for alcohol dependence. Several reviews of the evidence have concluded that topiramate is more efficacious than placebo in reducing drinking and improving other self-reported drinking outcomes. However, results of controlled trials reveal topiramate-induced adverse side effects, and this suggests that more research is needed to determine optimal dosing strategies to minimize
side effects while maximizing therapeutic benefit (Arbaizar et al., 2010; Johnson and Ait-Daoud, 2010; Shinn and Greenfield, 2010).
The guidelines are in agreement that there is no evidence that combining any of the medications to treat alcohol dependence improves outcomes over the use of any one medication alone, according to the Combining Medications and Behavioral Interventions (COMBINE) clinical trial sponsored by NIAAA (Anton et al., 2006).
Psychotherapy
All the guidelines are in agreement that pharmacotherapy for alcohol dependence is most effective when combined with behavioral counseling that is focused on encouraging abstinence, adherence to the medication, and participation in community support groups. The guidelines indicate that there is evidence of the effectiveness of a number of psychosocial interventions for treatment for AUD, including CBT, couples therapy, community reinforcement, and couple or marital-focused therapies. There is no clear evidence that any one of those approaches is the treatment of choice or can be accurately matched to specific patient characteristics (VA and DOD, 2009c).
All the guidelines recommend that clinicians use motivational techniques during therapeutic encounters with patients and encourage patient participation in 12-step programs, such as Alcoholics Anonymous, which research has found to be associated with improved addiction outcomes compared with baseline (VA and DOD, 2009c). Twelve-step facilitation (TSF) refers to formal psychotherapy administered by a professional that is intended to foster a patient’s active participation in Alcoholics Anonymous or other 12-step mutual-help programs. The NICE guideline states that the evidence is not strong enough to support motivational techniques or TSF as stand-alone alcohol-treatment interventions.
Only the NICE guideline offers specific guidance for the delivery of psychologic interventions, for example, that CBT and behavioral couples therapy should usually consist of one 60-minute session per week for 12 weeks and community reinforcement of eight 50-minute sessions over 12 weeks.
Opioids
The VA/DOD, APA, and WHO guidelines are mainly consistent in their recommendations for specific treatments for opioid dependence. Standard treatment is the use of OAT combined with psychosocial interventions. Table 5.5 compares treatment recommendations of these guidelines and their various systems for indicating their strength.
Pharmacotherapy
For medically supervised opioid withdrawal, the VA/DOD, APA, and WHO guidelines recommend the substitution of the opioid with methadone, buprenorphine, or buprenorphine combined with naloxone and then gradual tapering. The APA and WHO guidelines also support the use of clonidine to reduce the severity of opioid-withdrawal symptoms. The APA guideline states that the use of clonidine combined with naltrexone has been demonstrated to be a safe and effective approach for rapid detoxification.
TABLE 5.5 Summary of Guideline Recommendations for Treating for Opioid Dependence
| Treatment Modality | VA/DOD | APA | WHO | |
| Management of withdrawal | ||||
| Buprenorphine or Buprenorphine/naloxone | B | I | √ | |
| Methadone | B | I | √ | |
| Clonidine or clonidine/naltrexone | II | √ | ||
| Psychotherapy | ||||
| Cognitive behavioral therapy (CBT) | adjunct | II (adjunct) | √ (adjunct) | |
| Contingency management | adjunct | II (adjunct) | √ (adjunct) | |
| Psychodynamic therapy | III (adjunct) | |||
| Self-help groups | III (adjunct) | |||
| Family therapy | III (adjunct) | |||
| Pharmacotherapy | ||||
| Methadone | A (first-line) | I | First line | |
| Buprenorphine | A (first-line buprenorphine/naloxone combo) | I | Second line | |
| Naltrexone | C | I | √ | |
NOTE: VA/DOD: A = good evidence that the intervention improved outcomes; B = a fair amount of evidence supported the use of the intervention; C = the working group did not make a recommendation for or against the routine use of the intervention as the risk-benefit ratio was too close to make a general recommendation; D = presence of evidence that either the intervention was harmful or the risks outweighed the benefits offered by it; I = evidence was lacking, of insufficient quality, or conflicting; therefore, a recommendation could not be made for or against providing the treatment routinely. APA: I = intervention recommended with substantial clinical confidence; II = intervention recommended with moderate clinical confidence; III = intervention recommended on the basis of individual circumstances. WHO: No rating system was used. For purposes of this report, v denotes that use of the treatment was recommended.
The VA/DOD, APA, and WHO guidelines recommend maintenance treatment with methadone or buprenorphine as the primary treatment for opioid dependence. Maintenance treatment with naltrexone is considered an alternative strategy for preventing relapse although all the guidelines indicate that naltrexone’s value is often limited by the lack of patient adherence and low treatment retention.
Psychotherapy
All three guidelines consider psychosocial treatment—primarily CBT and contingency management—effective as a component of a comprehensive treatment plan for patients who have opioid dependence. A recent review by the Cochrane Collaboration found that there was not enough evidence to conclude that psychosocial treatments alone are adequate to treat people for opioid abuse and dependence (Mayet et al., 2005).
Cannabis
There is no evidence that supports the use of any specific pharmacotherapy for marijuana withdrawal or dependence. Although further study of psychosocial therapies for treatment for
marijuana dependence is necessary, studies suggest that adding contingency management to behavioral interventions is efficacious in reducing marijuana use (Budney et al., 2000).
Stimulants
No pharmacologic treatment for people who are dependent on stimulants, such as cocaine and amphetamines, is approved by FDA. Research to determine the most efficacious psychosocial interventions for reducing use of stimulants is still evolving. The Cochrane Collaboration reviewed 27 RCTs of the efficacy of psychosocial treatments for dependence on cocaine, amphetamine, and other stimulants. Comparisons of interventions favored treatment with some form of contingency management to reduce the use of stimulants (Knapp et al., 2007).
Implementation of Department of Defense and Department of Veterans Affairs Guidance for Treatment for Substance-Use Disorders
This section presents information available to the committee on the extent to which DOD and VA provide treatment for service members and veterans who have diagnoses of SUD. There is a striking lack of data to inform questions about the extent to which SUD treatments are offered, delivered, and completed and about whether they are leading to improved patient outcomes. The available data show that many service members and veterans in need of SUD treatment are not receiving it.
Department of Defense
As discussed previously, referral rates for treatment of service member are very low (Department of the Army, 2012; Milliken et al., 2007); consequently, few service members are receiving treatment. A 2009 survey of 585 Michigan Army National Guard service members returning from Iraq and Afghanistan found that 36% met the criteria for alcohol misuse according to the AUDIT (10-item screen). Of the 36%, 31% reported receiving any mental-health services in the preceding year, but only 2.5% reported receiving specific substance-abuse treatment. The researchers pointed to other research that suggested the stigma attached to receiving mental-health treatment is a reason for the low rates of treatment (Burnett-Zeigler et al., 2011).
On the basis of TRICARE data on pharmacological SUD treatments for active-duty service members diagnosed with SUD, the earlier IOM committee declared, “It is apparent that the use of these medications is not an integral part of SUD treatment for most individuals despite the evidence for their effectiveness” (IOM, 2012). That committee found
when one compares the number of ADSMs diagnosed with alcohol use disorders (6,175) with the number who received either naltrexone (1,034, some of which would have been prescribed for alcohol dependence, but some for opioid dependence), antabuse (605), and camparal (619), it is clear that many individuals with alcohol use disorders did not receive medication therapy. Among those diagnosed with drug use disorders (2,900), only 400 were prescribed buprenorphine.
VA reports that there is no mechanism for tracking the delivery of evidence-based therapies in the VA centralized databases. VHA is developing progress-note templates for evidence-based treatments that will allow documentation of care in the computerized record in a manner that will facilitate the collection of centralized aggregate data (IOM, 2012). The committee obtained the data discussed below, which suggest that many veterans are not getting necessary treatment and that most of those who are getting it are not completing the full course.
In 2006, VA contracted with Altarum Institute and the RAND Corporation to conduct an independent evaluation of the quality of VA mental-health and substance-use care (Watkins and Pincus, 2011). One aspect of the study assessed the availability of evidenced-based practices related to SUDs by using VA facility survey data collected in May 2007 and October 2009. The Altarum–RAND team administered surveys to 139 parent-facility service areas (PFSAs).8 Although there was substantial growth in the availability of OAT (with either buprenorphine or methadone) among PFSAs, from 45% to 81%, the researchers concluded that OAT may warrant more widespread implementation inasmuch as it is available in fewer than 90% of the PFSAs. The availability of intensive outpatient treatment for SUD dropped slightly from 95% of the PFSAs in 2007 to 91% in 2009. Psychosocial interventions for SUD had a high rate of availability and remained stable from 2007 to 2009, in 98% and 99% of PFSAs, respectively.
The Altarum–RAND team collected data on three performance measures that address use of evidence-based practices for treatment for SUD as documented in VA medical records and administrative data. The SUD-related measures were calculated for a cohort of veterans who had SUD and were identified for each fiscal year from FY 2004 through FY 2008.9 For FY 2007, the study team observed low rates of relapse-prevention therapy, maintenance pharmacotherapy, and contingency management in veterans in the SUD cohort. Specifically, about one-fifth of patients in the SUD cohort (21.5%) received psychotherapy with documentation of relapse-prevention therapy, one-fourth (24.8%) in the SUD cohort that had opiate dependence had documentation that maintenance pharmacotherapy was offered or contraindicated within 30 days of a new treatment episode, and only 1.0% had documentation that they had received contingency management.
Regarding rates of pharmacotherapy for opioid dependence, another recent study by Oliva et al. found similar rates for FY 2008 (27.3% of those with an opioid-use disorder) and substantial facility-level variability in the proportion of patients who were treated with OAT, ranging from 0% to 66%. Slightly over 40% of facilities treated under 5% of their patients with OAT (Oliva et al., 2012). It should be noted that both this study and the Altarum–RAND evaluation were conducted before the VHA national mandate of access to buprenorphine OAT established by the VHA handbook Uniform Mental Health Services in VA Medical Centers and Clinics (VA, 2008a).
__________________
8The study team defined a PFSA as VA service area that is anchored, in most cases, by a VA medical center and supporting community-based outpatient clinics. PFSAs have nonoverlapping geographic areas of responsibility.
9The SUD-cohort selection was based on International Classification of Diseases, Ninth Revision codes in the administrative records and reflected at least one inpatient episode or two outpatient visits (for any mental-health or non-mental-health diagnosis) in a given fiscal year.
The Altarum–RAND evaluation found that in FY 2007 about 15% of veterans in the SUD cohort who were in a new treatment episode10 initiated treatment within the first 2 weeks of the episode, and about 14% became engaged with treatment (defined as two or more outpatient visits) within a month of the new treatment episode. One-fourth received followup care within 90 days of the new treatment episode. On those measures, the data showed statistically significant variation by sex: women had higher rates of treatment initiation, treatment engagement, and treatment followup. There was also statistically significant variation in all three indicators by OEF or OIF status.
Another measure related to treatment engagement, collected in VA’s Performance Management Program, is the percentage of patients who maintain treatment involvement for at least 90 days after beginning a new treatment episode. In FY 2009 about 52% of veterans who entered VA specialty SUD treatment programs stayed in them for at least 90 days (GAO, 2010). However, a recent study raised a question about the utility of this measure: an analysis of patientlevel data found that it was not associated with improvements in clinical outcomes (Harris et al., 2009).
Regarding types of treatment interventions provided to veterans who are alcoholdependent, the Altarum–RAND evaluation found that 71.3% had documentation of a brief intervention, current specialty care, or a completed referral to specialty mental-health care during FY 2007 and that 16.4% had documentation in the medical record that pharmacotherapy (naltrexone, disulfiram, or acamprosate) was offered or contraindicated within 30 days of a new treatment episode.
Other studies corroborate the underuse of medications for AUD in VA. Harris et al. (2010) examined pharmacy-record data to determine the rate at which patients fill prescriptions for naltrexone, disulfiram, or acamprosate. Of the roughly one-fourth of a million VHA patients who have AUDs, 3% filled at least one prescription for those medications in FY 2007. The rate was 3.4% in FY 2009 (Harris et al., 2012).
Possible reasons for the underuse of pharmacotherapies for alcohol and opioid dependence in the VA may include providers’ lack of awareness of or training in pharmacotherapy and reluctance to use them (GAO, 2010).
The present committee notes that to improve implementation of treatment regimens, VA has made extensive efforts to train clinicians in specialty substance-use care to deliver evidencebased therapies, such as CBT and contingency management (Karlin et al., 2010); however, there have been relatively few efforts to evaluate outcomes or to document the quality of implementation of treatment.
Summary
Overall, the VA/DOD guidelines for the management of SUD reflect evidence-based approaches to screening and assessment of and treatment for SUD. Taken together, the research studies and policy assessments of the effectiveness of practices in the military and VA show that more needs to done to improve dissemination of the practices, to understand the barriers to improvements in care for SUDs, and to determine which practices produce the best clinical
__________________
10Defined by either the exacerbation of a condition that requires psychiatric inpatient care or the initiation of outpatient treatment after a break of 5 or more months without care.
outcomes. VA has recently undertaken a number of national efforts to improve its SUD services that, according to VA officials, may address multiple challenges that VA faces in providing SUD services. VA’s efforts include increasing access to SUD services, promoting evidence-based treatments for SUDs, and assessing SUD services and monitoring treatment effectiveness.
SUICIDAL IDEATION
Suicide is a leading cause of deaths of US service members (Trofimovich et al., 2012). Research has shown that unrecognized or untreated mental-health disorders are a major risk factor for suicide in the general population. At least 90% of people who die by suicide have a mental illness at the time of their death. The most common is MDD, followed by SUD, but almost all the psychiatric disorders are associated with increased suicide rates (Moscicki, 2001). Data from the DOD Suicide Event Report, the standardized suicide-surveillance effort throughout the services, illustrate the relationship between psychiatric problems and suicide attempts and suicide in military members. Of the 863 service members who attempted suicide in 2010, 63.7% had a history of at least one documented psychiatric disorder, and 37.3% had at least two co-occurring diagnoses. Nearly 40% of service members who attempted suicide had a diagnosis of a mood disorder, most frequently MDD (17.7%), and 26.07% had a diagnosis of anxiety disorder, most frequently PTSD (8.1%); 23.4% had a known history of substance abuse; fewer than 10% had documentation of personality disorders; and fewer than 5% had sustained a TBI (2.43%) or had a diagnosis of psychotic disorder (1.27%). The rates of psychiatric disorders are slightly lower in the 281 military members who died by suicide in 2010. Slightly over 40% had a history of at least one documented behavioral-health disorder, and one-fourth had at least two co-occurring diagnoses (DCoE, 2011d). Although those rates are informative, the rates of undetected psychiatric disorders in service members who either attempted suicide or died by suicide are unclear. Chapter 4 further defines the scope of the problem of suicide in military and veteran populations by presenting rates of suicide and suicide attempts; it also provides details about risk factors for suicide and suicidal ideation.
In this section, to assess the efficacy of current screening, assessment, and treatment approaches for suicidal ideation, the committee examines a number of major clinical guidelines, policy directives, and research studies related to the management of suicidal ideation in DOD and VA populations. As noted previously, VA and DOD have collaborated in the development of CPGs for several health conditions, including TBI, PTSD, MDD, and SUDs. Those CPGs address the assessment of suicidality as only one component of the management of the diagnostic condition without a focus on the management of suicidality as the core issue. There is no joint VA/DOD evidence-based CPG specifically for assessing and treating patients who have suicidal thoughts and behaviors, but such a guideline is under development. VA and DOD have chartered a working group to draft a joint VA/DOD CPG that will provide clinicians with evidence-based guidance on the assessment and management of a person who has suicidal ideation (Woodson, 2011).
In DOD, the Air Force Guide for Managing Suicidal Behavior (MSB) is a recognized example of DOD clinical guidance (Air Force Medical Operations Agency, undated; DOD, 2010a). Noting the variability in clinical practices for the management of suicidal behaviors among the services, the DOD Task Force on the Prevention of Suicide by Members of the
Armed Forces recommended the development of clinical practice standards to promote systemwide use of evidence-based practices (DOD, 2010a).
Suicide-Related Terminology
The use of standardized suicide-related terminology for the purposes of clinical care, surveillance, and research is a fundamental issue in the literature on suicide and suicidal ideation. A 2002 IOM report on reducing suicide in the nation emphasized the need for universally accepted definitions for suicide and suicidal behaviors to facilitate efforts in the field (IOM, 2002). Echoing the need for standardization, a 2008 VA-chartered Blue Ribbon Work Group on Suicide Prevention in the Veteran Population recommended that VHA collaborate with other federal agencies to create uniform definitions (Blue Ribbon Work Group on Suicide Prevention in the Veteran Population, 2008). In response, VA collaborated with the Centers for Disease Control and Prevention (CDC) to develop the Self-Directed Violence Classification System (SDVCS). Both VA and DOD have adopted the classification system as the basis of data collection and reporting and eventually for the purpose of risk assessment and case management (Brenner et al., 2011; DCoE, 2011a).
The SDVCS defines two types of self-directed violence—thoughts and behaviors—and defines various characteristics associated with each, including whether the thoughts and behaviors are suicide related. The nomenclature uses the term suicidal ideation to describe thoughts of engaging in suicide-related behavior. The thoughts may or may not involve suicidal intent, which is defined as the presence of “past or present evidence (implicit or explicit) that an individual wishes to die, means to kill him/herself, and understands the probable consequences of his/her actions or potential actions.” Suicidal behavior encompasses the “acts or preparation toward self-directed violence,” “behavior that is self-directed and deliberately results in injury or the potential for injury to oneself,” and “evidence, whether implicit or explicit, of suicidal intent.” Suicide is death caused by self-directed injurious behavior with any intent to die as a result of the behavior (Brenner et al., 2011).
Suicide Prevention
The DOD and VA have many programs, policies, and interventions in place to prevent and manage suicidal ideation in service members and veterans. Bagley et al. (2010) systematically reviewed the state of evidence on suicide prevention for military and veteran populations. The researchers identified seven studies of military personnel containing interventions that may reduce the risk of suicide. Their review found that multifaceted interventions for active duty military personnel are supported by consistent evidence, although of very mixed quality. There were insufficient studies of US veterans to reach conclusions. The Blue Ribbon Work Group produced an overview of key components of VA’s suicide-prevention strategy (Blue Ribbon Work Group on Suicide Prevention in the Veteran Population, 2008).
RAND conducted an assessment of DOD suicide-prevention programs offered by each military service (Ramchand et al., 2011). Its report covers an array of suicide interventions that address primary prevention (targeting the entire population), secondary prevention (targeting selected groups on the basis of common risk factors), indicated prevention (targeting people who have detectable symptoms), and dimensions of self-care and environmental safety (limiting lethal means) and postvention (interventions for survivors and bereaved after a suicide loss).
Ramchand et al. (2011) indicate there is evidence that restricting access to lethal means is an effective way to prevent suicide and conclude that suicide-prevention programs should limit gun availability to persons deemed to be at high risk of suicide.
Restricting Access to Lethal Means
As discussed in Freeman et al. (2003), research shows unequivocal evidence of an association between firearm possession and increased risk of suicide. Guns are the primary method of suicide by service members and veterans; these groups are known to have high rates of gun ownership (Claassen and Knox, 2011). A recent population-based study of veterans found that they were twice as likely as nonveterans to die by suicide and 58% more likely than nonveterans to use firearms rather than other suicide methods to end their lives (Kaplan et al., 2007). According to the DOD Suicide Event Report program for calendar year 2010, of the 281 military members in all services who died by suicide, 175 (62%) used firearms to kill themselves. Of those who used firearms, 136 (78%) used non-military-issue firearms, and a much smaller number, 39, used military-issue firearms. That underscores the importance of assessing and addressing access to non-military-issue firearms, as well as military-issue firearms, by people who are at risk for suicide (DCoE, 2011d).
International experts who reviewed the literature on suicide-prevention interventions have concluded that restriction of access to lethal means is one of the few suicide-prevention policies that has proven effectiveness. A systematic review on suicide prevention by Mann et al. (2005) concluded that among methods used to reduce suicide (physician education, restricting lethal means, public education, screening programs, and mass-media education), restricting access to lethal methods and education of physicians in MDD recognition and treatment were found to prevent suicide.
As discussed later, DOD gun-safety protocols for military-issued weapons exist, but the guidance on lethal-means counseling and restricting gun access is vague. Current DOD policy does not have provisions for restricting access to privately owned firearms for those believed to be at risk for suicide. In fact, the FY 2011 National Defense Authorization Act (PL 111-383, Section 1062) prohibits the secretary of defense from issuing any regulation or policy on legally owned personal firearms or ammunition kept by troops or civilian employees off base and from collecting any information on their guns or ammunition.11 More recently, however, DOD military leaders have been quoted in the popular press as stating that they are considering policy that “will allow separation of privately owned firearms from those believed to be at risk of suicide” (Jordan, 2012).
Department of Defense and Department of Veterans Affairs Guidance for Screening for Suicidal Ideation
In the absence of a joint VA/DOD CPG for the management of suicidal behavior, screening and assessment of suicidal ideation in VA and DOD is guided by a variety of policies and programs.
__________________
11PL 111-383: 111th Congress, Jan 7, 2011.
DOD uses a set of questions that specifically ask about suicidal thoughts and risk factors to screen for suicide risk (shown in Table 5.6). The questions are administered as part of DOD’s periodic health assessments, the PDHA and the PDHRA, which are briefly described in the introduction to this chapter. All service members meet in person with a provider, who conducts a full clinical interview that includes specific questions pertaining to suicide assessment.
TABLE 5.6 Periodic Health-Assessment Suicide-Screening Questions
| Periodic Health Assessment Questions Asked by Mental-Health Professionals or Certified Health Care Providers During Person-to-Person Interviews | Responses |
| Over the past month, have you been bothered by thoughts that you would be better off dead or of hurting yourself in some way? | Yes, no |
| If “yes,” ask “How often have you been bothered by these thoughts?” | Very few days More than half the time Nearly every day |
| Have you ever had thoughts of actually hurting yourself? If “yes,” ask the following four questions: |
Yes, no |
| Have you thought about how you might actually hurt yourself? | No, yes If yes, how? |
| How likely do you think it is that you will act on these thoughts about hurting yourself or ending your life over the next month? | Not at all likely Somewhat likely Very likely |
| Is there anything that would prevent or keep you from harming yourself? | No, yes If yes, what? |
| Have you ever attempted to harm yourself in the past? | No, yes If yes, when? |
| Assess other risk factors for suicide, including interpersonal conflicts, social isolation, current alcohol or substance abuse, hopelessness, severe agitation or anxiety, diagnosis of depression or other psychiatric disorder, recent loss, financial stress, legal disciplinary problems, serious physical illness | Yes, no |
SOURCE: Adapted from Vythilingam et al., 2010.
According to DOD training materials for administering the periodic health assessments (Vythilingam et al., 2010), respondents to these questions are designated as being at high risk for suicide if they have an active desire to commit suicide in addition to having no self-control, having no external supports, or having comorbid alcohol abuse, PTSD, or MDD; high-risk patients are given an emergency mental-health referral and provided with safe transportation to a mental-health clinic or emergency room. Respondents are designated as being at intermediate risk of suicide if they have current suicidal thoughts but no active plan for committing suicide (the suicidal thoughts may or may not be accompanied by other risk factors); intermediate-risk patients are referred to a mental-health specialist for an assessment within 48 hours or monitored by primary care clinicians at each visit, depending on the clinicians’ judgment. Health records of service members who are determined to be a danger to themselves or to others are flagged with a “behavioral health alert” (Woodson, 2011).
The Air Force MSB guide recommends that clinical staff use a one-item screening question for patients seen in a mental-health setting. The question is adapted from the National Depression Screening Project (Greenfield et al., 2000). “Over the past two weeks, how often have you had thoughts about wanting to commit suicide”? People who respond “sometimes,” “frequently,” or “always” undergo further assessment. A negative screen is the endorsement of "never" or "rarely" (Air Force Medical Operations Agency).
Department of Veterans Affairs
VA screens for suicide risk in primary care if patients screen positive for PTSD or MDD, in which case screening for suicide risk is mandatory. The suicide risk assessment includes having a patient respond to the questions in Box 5.8, which are included in two clinical tools for providers—Suicide Risk Assessment Guide: Reference Manual (VA, undated-a) and Suicide Risk Assessment Pocket Card (VA, undated-b)—and are incorporated into the VA clinical-reminder system in the electronic patient record.
BOX 5.8
VA Suicide-Assessment Questions
Are you feeling hopeless about the present/future? If yes, ask:
Have you had thoughts about taking your life? If yes, ask:
When did you have these thoughts, and do you have a plan to take your life?
Have you ever had a suicide attempt?
SOURCE: VA, undated-a.
Any reference to suicidal ideation, intent, or plans mandates a referral to specialty mental-health care for a mental-health assessment. When there is a referral or request for mental-health services, veterans must receive an initial evaluation within 24 hours (Kemp, 2011).
Evidence Related to Screening for Suicide Risk
There is no widely accepted and scientifically validated tool for screening for suicide risk, partly because of the complex set of biologic, psychologic, and social factors associated with suicide. On the basis of insufficient evidence on the accuracy of screening tools in identifying suicide risk in the primary care setting, the USPSTF found no evidence that screening for suicide risk reduces suicide attempts or mortality. The USPSTF found that commonly used screening instruments—the Scale for Suicidal Ideation, the Scale for Suicidal Ideation–Worst, and the Suicidal Ideation Questionnaire—have not been validated for assessing suicide risk in primary care settings and that there has been little testing of the Symptom-Driven Diagnostic System for Primary Care (USPSTF, 2004).
In its assessment of DOD screening practices, the 2010 Task Force on the Prevention of Suicide by Members of the Armed Forces concluded that “current screening efforts are not effective in identifying Service Members at risk for suicide and tend to perpetuate negative feelings about mental health care, which leads to further stigma.” In addition, the task force found that “current screening efforts are not effective in identifying Service Members who have significant moral and ethical problems resulting from their combat experience, resulting in a
sense of guilt and loss of self-worth that places them at risk for suicide.” The task force recommendations included ensuring service member receive routine mental-fitness assessment and wellness education and encouraging service members to obtain referrals to appropriate caregivers for concerns beyond a chaplain’s scope of expertise and experience (DOD, 2010a).
In examining VA’s suicide-prevention programs, the Blue Ribbon Work Group found that suicide-screening processes being implemented in VA primary care clinics go beyond the current evidence and may have unintended effects. The Work Group cited a lack of sufficient evidence to support mandatory suicide screening in non-mental-health settings. The Work Group recommended that VA revise and reevaluate the current policies regarding mandatory suicide screening assessments, stating that “this screening process, as designed, affects a large number of veterans, is time consuming, potentially stigmatizing, likely to be variable in implementation, and not evidence-based, and may result in unnecessary referrals to specialty mental health services” (Blue Ribbon Work Group on Suicide Prevention in the Veteran Population, 2008). In 2010, VA reported to Congress that a work group had reviewed VA practices and the evidence base on screening for and evaluation of suicide risk and recommended continuation of VA’s existing policy (VA, 2010b).
Implementation of Department of Defense and Department of Veterans Affairs Guidance for Screening for Suicidal Ideation
This section presents information available to the committee on the extent to which DOD and VA are implementing and tracking screening procedures to identify people who are at risk for suicide. The information raises questions about how well DOD and VA are implementing, tracking, and assessing their screening practices to ensure the best possible result.
Department of Defense
The US Army Medical Command’s RESPECT-Mil program provides primary care– based screening, assessment, treatment, and referral of active-duty personnel who have PTSD or MDD. Since 2007, 1.3 million visits have involved screening for PTSD and MDD. Of those, more than 13,600 (1%) involved suicidality and received mental-health intervention (DCoE, 2012c). Identification of suicide risk appears to be improving: over half the 13,600 visits involving suicidality were reported in 2011.
Department of Veteran Affairs
Under its Performance Management Program, VA uses three performance measures related to screening and suicide-risk assessment (AHRQ, 2012). The committee was unable to identify results of using those measures, and inquiries to VA about performance measures did not yield information about them.
One measure is the percentage of patients who screen positive on a screen for MDD (PHQ-2 or PHQ-9 or endorsement of question 9 on the PHQ-9) and have a suicide-risk evaluation completed within 24 hours. Another is the percentage of eligible patients who screen positive on the PTSD screen (PC-PTSD) and who have a suicide-risk evaluation completed within 24 hours. A third measure combines the populations of the first two to assess the percentage of patients who screen positive for MDD (on the PHQ-2 or PHQ-9) or positive for PTSD (on the PC-PTSD) and who have a suicide-risk evaluation completed within 24 hours.
Department of Defense and Department of Veterans Affairs Guidance for Assessment and Diagnosis of Suicidal Ideation
Available guidance in VA and DOD (such as the VA/DOD CPGs for PTSD, MDD, and SUDs and the Air Force MSB guide) emphasizes the importance of a formal assessment to determine suicide risk. Generally, the guidelines recommend the identification of risk factors and the use of a direct line of questioning to elicit details about suicidal thoughts and intent (for example, the VA/DOD MDD guideline recommends a group of questions modified from Hirschfeld and Russell, 1997). The Air Force MSB guide, refers to 31 suicide-assessment instruments on the basis of a comprehensive review by Brown (2000). Of those, the MSB guide recommends the Suicide Status Form-II, Suicide Tracking Form-I, and the Beck Scale for Suicide Ideation (Air Force Medical Operations Agency). Recently, the DOD/VA Suicide Prevention Tools Working Group compiled a descriptive summary of suicide assessment and prevention tools. The working group identified 26 clinical and 14 nonclinical suicide-prevention tools; of these, 25 were classified as aiming to assess suicidal ideation. The group’s report did not make any recommendations about the tools reviewed (DCoE, 2011f).
In the VA, the VA Suicide Risk Assessment Guide: Reference Manual (VA, undated-a) provides guidance to clinicians to support determinations of high-risk people. Suicide-prevention coordinators in each VA medical facility play a key role in, among other things, assessing and monitoring high-risk people, providing direct clinical care for veterans who are at increased risk for suicide, and tracking and reporting suicidal behavior. In 2008, a VHA directive established the use of “flags” in the electronic medical records of patients who are assessed as having a high risk of suicidal behavior (VA, 2008b).
Validity of Tools for Assessment of Suicide Risk
The purpose of a comprehensive suicide-risk assessment is, in addition to estimating the risk of suicidal behavior, to guide clinical action. In general, the greater the number of risk factors and the fewer the protective factors, the higher the risk of suicide and suicidal behavior. Many approaches to suicide-risk assessment emphasize the importance of systematically eliciting patient information in a number of key domains. For example, the APA Practice Guideline for the Assessment and Treatment of Patients with Suicidal Behaviors identifies five domains of a suicide assessment: the patient’s current presentation (such as suicidal thoughts, plans, behaviors, and intent), previous psychiatric illness and treatment, history of self-harming behavior and family history of suicide or mental illness, psychosocial situation (for example, relationships, employment, finances, and domestic or sexual abuse), and individual strengths and vulnerabilities, such as coping skills and personality traits. Once risk factors are identified, the clinician should focus interventions on factors that can be modified, for example, treating psychiatric symptoms, increasing social support, and removing access to lethal means (APA, 2003).
Suicide-specific assessment instruments can assist providers in clinical assessment of suicidal ideation and behavior. However, assessment instruments are not a substitute for clinical judgment; no single test or panel of tests accurately identifies the emergence of a suicide crisis (Fowler, 2012). An array of suicide-assessment instruments are available (IOM, 2002). Recently, the VA’s Evidence-based Synthesis Program completed a systematic review to determine what assessment tools are effective in assessing risk of suicidal self-directed violence in veteran and
military populations. The researchers found that evaluation of the effectiveness of riskassessment tools is lacking. They noted there is a dearth of evidence from prospective studies that examined associations between suicide-prevention assessment tools and suicidal selfdirected violence outcomes (Haney et al., 2012).
As described by Brown (2000), numerous suicide-assessment instruments have demonstrated adequate internal reliability and concurrent validity, but the predictive validity of most suicide measures has not been established. The Scale for Suicide Ideation and the Beck Hopelessness Scale are among the few instruments that have been found to yield scores that represent important risk factors for suicide (Brown, 2000). Factors that contribute to the difficulty of determining the predictive validity of suicide-assessment measures include the low base rate of suicidal behavior and the high false-positive rates associated with the use of such relatively distal variables as psychiatric diagnosis, demographics, and self-reported psychologic states (Fowler, 2012). Brown (2000) concluded that further research that uses large samples and a prospective design is needed to investigate the predictive validity of standardized measures of suicide attempts and suicide.
To address the need for measures that are predictive of suicide, researchers at Columbia University compared the psychometric properties of the Columbia-Suicide Severity Rating Scale (C-SSRS) with those of other measures. Posner et al. (2011) found that the C-SSRS, which assesses both behavior and ideation, could reliably predict a suicide attempt in those who had previously attempted suicide. The researchers concluded that the tool can help to determine who is most at risk for suicide by pinpointing the threshold at which a person’s suicidal thinking is severe enough to warrant professional intervention.
As an example of research on the predictive validity of a suicide-assessment tool that addresses specific populations, Breshears et al. (2010) sought to validate objective personality measures for use with those who have a history of TBI; the goal was to understand suicide risk better. The researchers investigated the Personality Assessment Inventory (PAI) Suicide Potential Index and Suicide Ideation scale as predictors of suicidal behavior in military personnel. They analyzed medical records of 154 veterans who had TBI and documented instances of suicidal behavior in the 2 years after PAI administration. The results suggest that the PAI may assist in assessing suicide risk in those who have TBI, particularly when populationbased cutoffs are considered (on a score range of 0 to 20, a score of 15 or higher yields a sensitivity of 90.9% and a specificity of 95.1%). However, the relatively small number of suicides (11) raises questions as to the generalizability of the findings and some statistical issues (Breshears et al., 2010).
In addition to the need for diagnostic tests that can predict suicide risk accurately, there is an issue regarding the capabilities of those who conduct the risk assessments. On the basis of RAND’s research on the DOD suicide-prevention program (Ramchand et al., 2011), the DOD Task Force on the Prevention of Suicide by Members of the Armed Forces reported that military health care providers (including mental-health care providers) and chaplains are insufficiently trained to deliver evidence-based assessment, management, and treatment to service members who exhibit suicide-related behaviors. The task force recommended that all military health care providers and chaplains receive training and continuing education in evidence-informed suiciderisk assessment, management, and treatment planning (DOD, 2010a).
Implementation of Department of Defense and Department of Veterans Affairs Guidance for Assessment and Diagnosis of Suicidal Ideation
There appear to be very few data on the extent to which DOD and VA conduct suiciderisk assessments of service members and veterans who might be at risk for suicide.
Department of Defense
The committee is unaware of any metrics in DOD for tracking the number of service members that have received suicide-risk assessment in the Military Health System.
Department of Veteran Affairs
VA contracted with Altarum Institute and RAND to conduct an independent evaluation of the quality of VA mental-health care and substance-use care (Watkins and Pincus, 2011). The evaluation included one performance indicator related to suicide assessment in VA. On the basis of medical-record data from FY 2007, the Altarum–RAND team found 81% of study veterans had documentation of an assessment for suicidal ideation. Women were 9 percentage points more likely than men to have a documented assessment for suicidal ideation; OEF and OIF veterans were significantly more likely than non-OEF and non-OIF veterans to have a documented assessment for suicidal ideation or to have their symptoms reassessed. The research team surveyed all VA facilities nationwide in 2007 and again in 2009 to assess the availability of basic and specialized services. The unit of analysis was a parent-facility service area (PFSAs).12 In 2009, all PFSAs reported having policies for flagging and 99% policies for tracking veterans who express suicidal thoughts. Results of the May 2007 survey indicated that 44% of the PFSAs reported having policies for flagging and 29% policies for tracking veterans who express suicidal thoughts (Watkins and Pincus, 2011).
Department of Defense and Department of Veterans Affairs Guidance for Treatment for Suicidal Ideation
The Air Force MSB guide recommends that treatment plans specifically target suicidal symptoms and risk factors (Air Force Medical Operations Agency, undated). The guideline notes that treatment plans that target only a psychiatric diagnosis are insufficiently specific and may fail to address the multidimensional nature of suicide risk fully. Yet, with the exception of the Air Force MSB guide, the primary focus of the current DOD and VA treatment guidelines is on the therapeutic approaches that target the individual specific disorders that are the subjects of the guideline (MDD, PTSD, SUD, and TBI). Less emphasis is placed on the treatment of patients who may also have suicidal symptoms, although the VA/DOD guideline for MDD includes an appendix that has specific guidance for managing suicidality. The forthcoming VA/DOD guideline on assessing and managing suicidal behaviors may provide more detailed guidance. In this section, we highlight the few recommendations for treating suicidal thoughts and behaviors in the various existing VA/DOD guidelines for MDD (VA and DOD, 2009a), PTSD (VA and DoD, 2010), and SUD (VA and DoD, 2009c).
__________________
12The study team defined a PFSA as VA service area that is anchored, in most cases, by a VA medical center and supporting community-based outpatient clinics. PFSAs have nonoverlapping geographic areas of responsibility.
The VA/DOD MDD guideline discusses the use of behavioral therapy and pharmacotherapy under specific circumstances in the treatment of patients who have a diagnosis of MDD and are exhibiting suicidal behaviors. In patients who have a history of suicide attempts, CBT is recommended for reducing the risk of further suicide attempts. The guideline notes that one RCT found that a 10-session CBT led to 50% fewer suicide attempts than enhanced usual care (tracking and referral) without reducing rates of suicidal ideation (Brown et al., 2005). When antidepressant pharmacotherapy is used to treat MDD, clinicians are encouraged to inform patients that a slight increase in suicidal ideation may occur in the early phase of treatment. Clinicians are warned to use tricyclic antidepressants cautiously in patients who are at high risk for suicide and only when consultation with an appropriate specialist guides the therapy. Electroconvulsive therapy (ECT) should be considered in patients who have severe MDD and severe suicidality.
The VA/DOD guideline for PTSD provides some guidance in the use of two psychotherapies in patients who are at risk for suicide. The guideline alerts clinicians to use caution when considering exposure-based therapies (ETs) for patients who are at substantial risk for suicide. ET has not been studied in patients who have health problems that preclude exposure to intense physiologic arousal and some patients may experience an increased level of distress when confronting trauma memories. Although there is insufficient evidence to recommend for or against dialectical behavior therapy (DBT) as first-line treatment for PTSD, the guideline indicates that DBT can be considered for patients who have borderline personality disorder typified by parasuicidal behaviors (attempted self-injury in which the aim is not death). The guideline cites studies that identify DBT as a promising treatment for suicide but acknowledges the need for further research.
The VA/DOD guidelines for MDD, PTSD, and SUD address the sequencing of treatment for suicidal ideation in the context of comorbidity with these conditions. The guidelines indicate that if severe suicidality is identified during the clinical assessment, the clinician should first concentrate on management of suicide risk before initiating treatment for any other condition. In addition, The VA/DOD MDD guideline and the Air Force MBS guide recommend that clinicians adopt a systematic approach for making clinical decisions about potentially suicidal patients that involves identifying risk factors, classifying the level of suicide risk, and using that information to determine the course of action.
Although it is not specifically endorsed in DOD or VA clinical guidelines, the Collaborative Assessment and Management of Suicidality (CAMS) is an approach that some Air Force clinics and other military settings are using to monitor and manage suicidal behavior. CAMS is a therapeutic framework that targets suicide as the primary focus of assessment and problem-focused intervention. The Suicide Status Form (SSF) is used to guide assessment, treatment, and continuing suicide risk until suicidality resolves (Jobes, 2012). Six published correlational studies and one RCT support the use of CAMS and the SSF; additional RCTs and CAMS-related projects are under way (Jobes, 2012). In a US Air Force Study (n = 55), use of CAMS was related to more rapid resolution of suicidal thinking and decreases in emergencydepartment and primary care visits (Jobes et al., 2005).
In 2008, VA implemented a safety planning protocol for use with patients who are at high risk for suicide. A safety plan is a predetermined priority list of coping strategies, sources of support, and help-seeking behaviors that patients can refer to during vulnerable periods. As a therapeutic technique, a safety plan plays a role in the continuing mental-health treatment in
outpatient settings (Stanley and Brown, 2008). As used in VHA, the safety plan involves the following steps: recognition of signs of increasing risk, use of coping strategies to manage episodes of suicidal ideation, use of social contacts that can distract from suicidal ideation and provide support, contact with family members or friends who can assist in resolving an episode of high-risk suicidal ideation, contact with professionals and agencies, and reduction in access to lethal means (Claassen and Knox, 2011). Protocol requires that the plan be included in the patient’s medical record and that a copy be given to the patient.
Evidence Related to Treatment for Suicidal Ideation
Research shows that 90% of people who committed suicide had psychiatric and mood disorders and that more than 80% had not received treatment at the time of death (Mann et al., 2005). Thus, a primary component of suicide prevention is prompt evidence-based treatment for psychiatric illness. Therapeutic approaches for addressing suicidality should target specific psychiatric disorders (such as MDD and PTSD), associated symptoms (such as anxiety), and the predominant psychodynamic or psychosocial stressors (APA, 2003).
Prescribed medications should be those necessary to treat for underlying disorders (IOM, 2002). There is evidence that lithium treatment for bipolar disorder significantly reduces suicide rates (APA, 2003; IOM, 2002). In a meta-analysis of 33 studies of the efficacy of lithium, Baldessarini et al. (2001) found that lithium reduces the incidence of completed suicide by 13-fold. Other studies of antipsychotic medications have found that clozapine is associated with significant decreases in suicide attempts by people who have schizophrenia or schizoaffective disorder (APA, 2003; IOM, 2002).
Meta-analyses of RCTs have not found independent benefit regarding suicide or suicide attempts in studies of the use of antidepressants for mood and other psychiatric disorders. Few studies prospectively used suicidal behavior as an outcome measure (Mann et al., 2005).
Although numerous studies have documented the efficacy of psychotherapy, especially CBT, in treating for mental disorders that increase suicide risk, such as MDD and PTSD, far fewer studies have documented the direct effects of therapy on suicidal behavior (IOM, 2002). Some studies have shown promising results for CBT as an intervention to reduce suicide (see a systematic review by Tarrier et al., 2008), but the use of small samples limits the ability to reach conclusions about efficacy from these studies (Hawton et al., 2000; Tarrier et al., 2008).
Implementation of Department of Defense and Department of Veterans Affairs Gun-Safety Protocols
Gun-safety protocols for military-issued weapons are part of the standard of care for suicidal patients in VA and DOD clinical settings, but there is evidence that implementation may be inconsistent.
Department of Defense
In the military, the standard practice for service members who are at risk for suicide consists of “lethal-means counseling,” removing service members from weapon-carrying duties, and putting the service members’ weapons in the base armory for safekeeping. But there are no clear guidelines, decision tree, or risk stratification to guide a clinician. A key recommendation
by the 2010 DOD Task Force on the Prevention of Suicide by Members of the Armed Forces (DOD, 2010a) is to
establish clear DoD, Joint and Service guidance for removal and subsequent reissue of military weapon and ammunition for Service Members recognized to be at risk for suicide. The guidance should emphasize a collaborative, team approach to the decision-making process and specify documentation requirements.
Department of Veterans Affairs
In the VA system, the Office of Inspector General evaluated the extent to which VA mental-health care providers consistently developed suicide-prevention safety plans (SPSPs) for patients assessed as being at high risk for suicide. Inspectors evaluated SPSP practices in 45 facilities during January 1–September 30, 2010. Of the 469 medical records reviewed, 412 (88%) had documented SPSPs; of the 469,389 (83%) fully addressed the six essential components of the safety plan. Reducing the potential for use of lethal means is one of the components (VA Office of Inspector General, 2011).
Summary
Suicide remains a paramount problem in the military despite substantial efforts. Although there are no VA/DOD joint evidence-based CPGs for screening for, assessing, or treating for suicidal thoughts and behaviors, a work group has been formed to draft such joint guidelines. The Air Force MSB guide is a recognized example in DOD, and the 2003 APA “Practice Guidelines for the Assessment and Treatment of Patients with Suicidal Behaviors” represents the prevailing national standard.
A substantial array of programs and resources has been developed by VA/DOD in an effort to enhance suicide prevention. However, there remains a lack of standardization or coordination. In fairness, the overall evidence base on screening and assessment approaches is sparse, in part because of challenges related to predicting and reducing the number of events that occur in a small proportion of the population. Consequently, there has been widespread controversy about the optimal approach. DOD screens as part of the PDHA, whereas VA assesses suicide risk in people who screen positive for PTSD or MDD.
Both DOD and VA recognize the importance of formal assessment of suicide risk. There are evidence-based approaches, such as those outlined by APA. Although DOD and VA have compiled resources, a standardized approach remains to be established and implemented. Likewise, there is a recognized need to improve the training of VA and DOD health care providers and chaplains in assessing suicide risk.
Interventions for suicidal ideation have focused principally on treatment for underlying psychiatric conditions. However, in accord with the prevailing evidence base, approaches should also focus on monitoring and managing suicidal behavior, as exemplified by CAMS (used by the US Air Force) and a safety plan (used by VA). The most compelling evidence-based approach to suicide prevention emphasizes the importance and potential favorable effects of restricting access to lethal means. In the case of service members and veterans, firearms constitute the leading lethal means of suicide. Standard practices have been developed that entail “lethal-means counseling” by DOD and “suicide-prevention safety plans” in VA, but a more robust and
effective standardized complement of policies, procedures, and practices needs to be established and reliably implemented throughout DOD and VA.
COMORBID CONDITIONS
The terminology used to describe the presence of more than one distinct health condition in a person is variable. Some common terms are comorbidity, dual diagnosis, co-occurring disorders, and multimorbidity; however, there is no consensus regarding the definitions of these terms (Center for Substance Abuse Treatment, 2006; de Groot et al., 2003; Valderas et al., 2009). That is important because the lack of consensus about how to define and measure the concept of multiple health conditions complicates attempts to study their effects on an array of outcomes—for example, death, functional status, and health care quality—and to develop clinical guidance on their management. Moreover, comorbidity is associated with worse health outcomes, more complex clinical management, and increased health care costs (Valderas et al., 2009).
According to Valderas et al. (2009), there are several characteristics associated with definitions of comorbidity. Some definitions are based on health conditions linked to classification systems, such as ICD and DSM; others are not. Definitions either identify one central disease, referred to as the index condition, which is relative to secondary conditions, or take an approach in which no particular condition is privileged over any other, as implied by the term multimorbidity. One dimension of comorbidity is the chronology of multiple health conditions. Conditions may be present simultaneously or during a period but not simultaneously; and they can appear in a particular sequence regardless of the period. Morbidity burden and patient complexity are other concepts associated with comorbidity (Valderas et al., 2009).
Among military and veteran personnel, rates of comorbid diagnosis are high; the most common overlapping disorders are PTSD, SUD, MDD, and postconcussive symptoms attributed to mild TBI. (See Chapter 4 for a full discussion of each condition and its associated comorbidities, including prevalence.)
DOD data show many service members are receiving diagnoses of more than one mental-health condition, and the trend is increasing slightly. In 2007, throughout the armed forces (excluding reserves and National Guard), 35,226 persons received 46,482 mental-health diagnoses,13 for an average of 1.32 diagnoses per person. The average number of diagnoses increased to 1.38 in 2008, 1.42 in 2009, and 1.43 in 2010 (AFHSC, 2010).
In the veteran population, the rates of comorbidity are substantial. Carlson et al. (2010) examined rates of clinician-diagnosed psychiatric disorders in a sample of 13,201 OIF and OEF veterans who had been screened for TBI and found that over 80% of veterans who screened positive had psychiatric diagnoses. In an evaluation of VA mental-health programs, the Altarum– RAND evaluation team examined data for a FY 2008 cohort of 906,394 veterans who had at least one mental-health diagnosis.14 Among those veterans, 53% had a mental-health diagnosis
__________________
13Mental health diagnosis is defined as a diagnostic code for PTSD, MDD, bipolar disorder, alcohol dependence, or substance dependence and at least one inpatient encounter or two outpatient encounters on separate days for the recorded diagnostic code; cases were counted by using the earliest medical encounter for a given person.
14The cohort consisted of veterans whose VHA use records contained at least one of 38 study-relevant ICD-9-CM diagnosis codes for the five study conditions (MDD, PTSD, SUD, schizophrenia, and bipolar disorder) and at least one inpatient episode or two outpatient visits annually for any diagnosis.
other than their cohort-qualifying diagnosis, 50% had at least one physical-health comorbidity, and 23% had co-occurring SUD. From an economic standpoint, RAND found that treating mental-health problems that co-occur with SUD substantially increases the cost of treatment per veteran. On the average in the FY 2008 study cohort, the per-veteran cost of treating a mental-health condition with co-occurring SUD was $20,903, compared with $11,342 for PTSD only, $14,202 for depression only, and $12,600 for SUD only (Watkins and Pincus, 2011).
Clinical management of the complex array of symptoms that is typical of patients who have comorbid conditions is challenging (Lew et al., 2008). Comorbidities require clinical attention at the point of diagnosis and throughout the process of treatment. Comorbid medical and psychiatric conditions are important to recognize because they can modify clinical determinations of prognosis, patient or provider treatment priorities, selection of interventions, and the setting where care will be provided. Current evidence-based practices to identify and treat people for conditions also may be less accurate or effective when conditions co-occur (Carlson et al., 2009).
As described in other sections of this chapter, substantial evidence-based clinical guidance exists for the management of individual health conditions that are prevalent among service members and veterans. However, there are no empirically validated therapies for comorbid PTSD, MDD, and postconcussive disorders, which may be confounded by substance use (Lew et al., 2008). No evidence was found to support particular sequencing of treatments in implementing practice recommendations of individual guidelines.
In the absence of a strong evidence base related to comorbid conditions, clinical judgment based on systematic symptom monitoring and the patient relationship is needed in deciding which specific treatments to implement, for which patients, and under which treatment conditions (National Center for PTSD, 2010a; Otis et al., 2011). As discussed below, experts agree that, given the lack of evidence on efficacious treatments for comorbid conditions, best practices involve treating for symptoms regardless of etiology by using current CPGs (Brenner et al., 2009; National Center for PTSD, 2010a, 2010b; Otis et al., 2011).
Department of Defense and Department of Veterans Affairs Guidance for Comorbid Conditions
The various VA/DOD clinical guidelines reviewed by the committee acknowledge that few published trials can provide clinicians with guidance in treating for conditions that are complicated by comorbid illness. The guidance given is generally in the form of background information about commonly occurring comorbid conditions with some recommendations for patient management. Among the VA/DOD guidelines, the PTSD guideline provides the most extensive and detailed guidance for the management of comorbid conditions. In general, the recommendations in the guidelines are consistent and can be categorized into a few central themes, as summarized below.
Assessment of the Presence of Comorbid Conditions
Each VA/DOD guideline states that in performing patient clinical assessments clinicians should determine whether comorbid medical or psychiatric conditions are present and are possible causes of the patient’s symptoms. The VA/DOD MDD guideline identifies bipolar disorder, PTSD, SUD, suicidality and homicidality, and psychosis as conditions that commonly
occur with MDD. The VA/DOD PTSD guideline recommends that providers assess PTSD patients for MDD and other psychiatric disorders, patterns of current and past use of substances, pain and sleep disturbances, physical and cognitive health symptoms, and high-risk behaviors. The TBI guideline indicates that patients with concussion or mild TBI should be screened for psychiatric symptoms and comorbid psychiatric disorders, including MDD, PTSD, and SUD. The SUD guideline emphasizes that SUD correlates highly with PTSD and other psychologic disorders, infectious diseases, and nicotine dependence.
In addition to medical and psychiatric comorbid conditions, the guidelines recommend that people be assessed for any important unmet psychosocial needs or situational stressors, such as financial difficulties, problematic family relationships, poor social support, or occupational problems.
Priority Setting in Treatment for Symptoms
Overall, the guidelines recommend that management of patients who have comorbidities focus on identifying and treating for the symptoms that are causing the most impairment regardless of cause or diagnosis. Of all the guidelines, the TBI guideline expresses this most directly:
The expected outcome of intervention should be to improve the identified problem areas, rather than discover a disease etiology or “cure.” The presence of comorbid psychiatric problems such as a major depressive episode, anxiety disorders (including post-traumatic stress disorder), or substance abuse—whether or not these are regarded as etiologically related to the mild TBI—should be treated aggressively using appropriate psychotherapeutic and pharmacologic interventions (VA, 2009).
Treatment for Comorbid Disorders
The VA/DOD guidelines indicate that presence of comorbid conditions should be considered in choosing treatments. Each guideline refers clinicians to specific VA/DOD guidelines for information about best practices in treatment for individual disorders (such as MDD, PTSD, SUD, and mild TBI).
The individual guidelines provide some minimal guidance about treating for comorbidities. For example, the VA/DOD guideline for MDD states that a patient who has a depressive disorder and a coexisting mental-health disorder that complicates treatment (such as a history of hypomania or a manic episode, PTSD, psychosis, or SUD) may require the use of multiple psychotropic medications and ancillary services, which may include the use of moodstabilizing medications, antipsychotics, multiple antidepressants, benzodiazepines, case management, family support, peer support, group therapy, or mobile treatment units. The guideline also identifies the potential contraindications for ECT in patients who recently had an intracerebral hemorrhage, which may have occurred in TBI.
For the management of concurrent PTSD and SUD, the VA/DOD PTSD guideline indicates that there is insufficient evidence to recommend using or not using any specific psychosocial approach to addressing PTSD that is comorbid with SUD. The guideline (VA and DOD, 2010) states further that “no systematic findings indicate harm to patients provided integrated treatment for co-occurring SUD and PTSD and there is recognition that both
conditions ought to be addressed.” The guideline recommends addiction-focused pharmacotherapy in addition to any indicated pharmacotherapy for coexisting PTSD and the provision of specialty psychosocial treatment and adjunctive services.
The VA/DOD TBI guideline states that treatment for psychiatric or behavioral symptoms after concussion or mild TBI should be based on individual factors and on the nature and severity of symptoms and may include both psychotherapeutic and pharmacologic treatment. People who sustain a concussion or mild TBI and present with anxiety symptoms or irritability should be offered a several-week trial of pharmacologic agents. For the management of sleep dysfunction, the guideline recommends evaluating for potential comorbid psychiatric conditions, including MDD and anxiety, and, if they are present, considering the use of standard medications to improve sleep.
In connection with sequencing of various treatments, the PTSD guideline recommends treating for comorbid mental-health conditions concurrently with PTSD treatment, although a stated exception is severe substance dependence that requires medical detoxification before other forms of treatment. With respect to co-occurring TBI, the PTSD guideline (VA and DOD, 2010) states that “there is no evidence to support withholding PTSD treatments while addressing postconcussive symptoms” and that “physical or cognitive symptoms, such as headaches or memory problems, or other persistent post-concussive symptoms should be treated symptomatically whether or not concussion/mTBI is thought to be one of the causal factors.”
Referrals and Coordination of Care
Each VA/DOD guideline encourages providers to consider the existence of comorbid conditions when deciding whether to treat patients in the primary care setting or to refer them for specialty mental-health care. For example, the PTSD guideline states that referral to specialty mental-health care is indicated if a patient who has PTSD has comorbid mental disorders that are severe or unstable. The examples given include patients whose MDD is accompanied by suicidality, patients who have substance dependence, and patients who have concurrent psychotic or bipolar disorder.
All the guidelines emphasize the importance of communication and coordination of care between primary care and mental-health care providers if a patient is referred to specialty care for treatment for comorbid conditions. The VA/DOD MDD guideline mentions that care management—“a clinical approach to coordinate the management of several chronic health conditions that may be integrated into primary care settings”—may be appropriate for those who have a variety of medical and psychiatric comorbid conditions that require integrated care.
The PTSD guideline states that integrated care, in which the physical-health and mental-health needs of patients are addressed in a single setting by a multidisciplinary provider team, has the potential to reduce the perceived stigma associated with help-seeking. As discussed later, the SUD guideline indicates that a growing body of research is demonstrating that integrated services produce better outcomes for people who have co-occurring disorders, particularly serious or complex conditions.
Clinician Toolkits
The Defense Centers of Excellence for Psychological Health & Traumatic Brain Injury developed a clinical tool, Co-Occurring Conditions Toolkit: Mild Traumatic Brain Injury and
Psychological Health, to guide primary care providers in assessing and managing patients when multiple diagnoses may be present. The toolkit synthesizes evidenced-based approaches from VA/DOD CPGs that address concussion, PTSD, MDD, chronic opioid therapy, and SUD. It is organized by symptom (such as sleep, mood, attention, and chronic pain) and identifies the probable etiology of symptoms (such as concussion, PTSD, MDD, chronic pain, headache, and SUD). Screening, assessment, and treatment steps are recommended. Information regarding potential side effects of particular drugs on co-occurring disorders is provided with specific drug information (doses, side effects, and safety warnings) (DCoE, 2011c).
Implementation of Department of Defense and Department of Veterans Affairs Guidance for Comorbid Conditions
VA contracted with the Altarum Institute and RAND to conduct an independent evaluation of the quality of VA mental-health and substance-use care (Watkins and Pincus 2011). One of the research questions examined was whether veterans who have dual diagnoses (including co-occurring SUD and the mental-health diagnoses included in the evaluation) are receiving integrated care that manages both conditions. In this context, integrated care refers to mental-health and substance-abuse treatment delivered by a single clinical team or a clinician who is cross-trained in mental health and SUD. The performance indicator developed for the evaluation is the proportion of veterans who have co-occurring SUD with documentation of any visits that treated them for both SUD and the mental-health disorder on the same day within 3 months of a new treatment episode. For FY 2007, the study found that 47% of veterans in the cooccurring SUD cohort had a visit that treated them for the mental-health condition and a visit that treated them for SUD on the same day. The authors noted that VHA care for co-occurring SUD may be fairly well coordinated, if not integrated, inasmuch as it is likely that visits occurring on the same day reflect care that is more integrated than visits that are separated by months (Watkins and Pincus, 2011).
Evidence Related to Treatment for Comorbid Conditions
There is little evidence on the best approaches for the assessment and treatment of patients who have comorbidities. The literature is insufficient to determine whether diagnostic or even screening instruments commonly used for assessing the symptoms of a particular condition perform accurately when a person has more than one condition. Nor does the literature support any one instrument over others. Examples of studies with those findings were related to instruments for detecting MDD in patients who also have mild TBI (Guillamondegui et al., 2011) and for screening for and diagnosing mild TBI in patients who have PTSD (Carlson et al., 2011).
As described below, findings from several studies demonstrate the lack of knowledge about whether evidence-based treatments for a single condition are effective when conditions cooccur or unique therapies are necessary for people who have multiple conditions.
Traumatic Brain Injury and Posttraumatic Stress Disorder
In 2009, the VA Office of Mental Health Services (OMHS) and Office of Rehabilitation Services sponsored a consensus panel to make practice recommendations related to the diagnosis and management of PTSD, pain, and a history of mild TBI in veterans. The panel reviewed results of a systematic review of evidence on the epidemiology, assessment, and treatment of
adults who had mild TBI and PTSD. The reported prevalence of comorbid TBI and PTSD varied widely among the studies reviewed. No published studies addressed the relative accuracy of diagnostic tests used for assessing mild TBI or PTSD when one condition co-occurs with the other. And no published studies evaluated treatments for the symptoms of mild TBI and PTSD together (Carlson et al., 2009). The consensus panel recommended the use of current VA/DOD CPGs for treating for PTSD, mild TBI, and pain in patients who meet diagnostic criteria for at least two of these disorders concurrently. The panel noted that there was no evidence to support modifying the current CPGs for treatment for comorbid PTSD, mild TBI, and pain (National Center for PTSD, 2010b).
Posttraumatic Stress Disorder and Substance-Use Disorder
In 2009, VA’s OMHS convened a consensus panel to develop recommendations related to the clinical management of veterans who had comorbid SUD and PTSD. The panel’s recommendations were informed by results in 52 articles on the assessment and treatment of veterans who had co-occurring SUD and PTSD (the report notes that an exhaustive review of the literature was not conducted). The panel found there are findings to support the provision of integrated treatment for SUD and PTSD, and no findings indicated harm to clients who received integrated treatment for co-occurring SUD and PTSD. The review of the research does not suggest the necessity of stabilizing SUD in patients fully before they receive any services for PTSD. And the data do not clearly identify one specific treatment as the “gold standard” (National Center for PTSD, 2010a). In the absence of guidelines that specifically address treatment for comorbid PTSD and SUD, the panel concluded that the use of current VA/DOD CPGs for PTSD and SUD is appropriate for treating patients who simultaneously meet the diagnostic criteria for these disorders. The panel’s recommendations state that in general treatments of patients for both PTSD and SUD can be effectively delivered concurrently (National Center for PTSD, 2010a).
With respect to specific treatments, the panel urged VA SUD and PTSD specialists to use effective first-stage treatment strategies, such as use of motivational interviewing principles and Seeking Safety, a treatment model specifically for co-occurring SUD and PTSD (National Center for PTSD, 2010a). Seeking Safety is a strongly recommended treatment in the 2008 VHA Handbook for Uniform Mental Health Services in VA Medical Centers and Clinics (VA, 2008a).
There is little evidence that supports any particular treatments for co-occurring PTSD and SUD, but some treatments are available (see Foa et al., 2009; Gulliver and Steffen, 2010). Of the existing treatments, Seeking Safety is the most researched (Foa et al., 2009). Seeking Safety is a manualized treatment (having a set protocol of actions) for people who have comorbid PTSD and substance abuse or dependence. Its primary goal is to reduce both PTSD and SUD by focusing on safe coping skills that are addressed through cognitive, behavioral, interpersonal, and casemanagement approaches (Boden et al., 2012). The International Society for Traumatic Stress Studies guidelines classify the level of evidence for Seeking Safety as Level A, which is evidence that is based on randomized, well-controlled clinical trials for people who have PTSD. As reported by Desai et al. (2008) and Boden et al. (2012), various studies have shown that clients appeared to respond positively to the Seeking Safety intervention, and it outperformed treatment as usual. To test how Seeking Safety fares when incorporated into the VA SUD programs, Boden et al. (2012) conducted a randomized controlled effectiveness trial with 117 veterans who had diagnoses of SUD and co-occurring PTSD symptoms. They concluded that
findings provided support for the feasibility and benefit of addressing PTSD and SUD simultaneously and early in SUD treatment as opposed to requiring separate or sequential treatments or a period of abstinence before PTSD-focused care. A review of the evidence by the National Center for PTSD was more tempered: the authors noted that RCT results, although promising, were equivocal and thus concluded that Seeking Safety should probably be combined with other treatments to ensure that all problematic behaviors decrease (Gulliver and Steffen, 2010).
Depression and Substance-Use Disorder
Over the last 20 years, results of well-controlled trials have shown that antidepressants reduced depressive symptoms in patients who have MDD and alcohol dependence. In most of the trials, however, antidepressant medications had virtually no effect in reducing excessive drinking (Pettinati and Dundon, 2011). Findings of a recent controlled trial (Pettinati et al., 2010) indicate that integrating or combining medications showed promising results in treating for cooccurring MDD and alcohol dependence. More depressed alcohol-dependent patients who received the combination of sertraline (an antidepressant) and naltrexone (to treat alcohol dependence) achieved abstinence from alcohol, had delayed relapse to heavy drinking, reported fewer serious adverse events, and tended not to be depressed by the end of treatment (Pettinati and Dundon, 2011). The researchers noted that those findings require replication before changes in clinical practice can be recommended.
The Cochrane Collaboration recently published findings of a systematic review of RCTs of the efficacy of antidepressant medication in treat depressed people who were dependent on opioids (such as morphine and heroin, codeine, oxycodone, and hydrocodone). The authors concluded that it was not possible to draw confident conclusions about the efficacy and safety of antidepressants for treatment for MDD in people who are dependent on opioids, because of clinical and methodologic differences between studies (Pani Pier et al., 2010).
With respect to psychotherapy for co-occurring MDD and SUD, Hides et al. (2010) systematically reviewed the few clinical trials that have examined the efficacy of CBT. They concluded there is minimal evidence of the effectiveness of CBT either alone or in combination with antidepressant medication for treatment for co-occurring MDD and SUD.
Integrated Treatments and Care Models
There are several approaches to treatment for comorbid conditions: integrated (simultaneous treatment for the comorbid disorders by the same provider or clinical team), parallel (simultaneous treatment for each disorder but in different settings), sequential (treatment for one disorder followed by treatment for another), and single (treatment for only one disorder) (Foa et al., 2009; Pettinati and Dundon, 2011). An emerging body of literature reports promising results associated with integrated treatments according to principles inspired by integrated dual diagnosis treatment for co-occurring SUD and severe mental illness (Drake et al., 1998). Seeking Safety, mentioned above, is one example. Although there has been little research on and experience with integrated treatment for comorbid MDD and SUD, Pettinati and Dundon (2011) cite research demonstrating that integrated approaches (such as CBT with standard pharmacotherapy) are superior to other approaches. Otis et al. (2011) identified studies of the effectiveness of various integrated treatment approaches for veterans for combinations of pain, mild TBI, and PTSD, including cognitive processing therapy (CPT) for PTSD and CBT for
chronic pain management in veterans who have comorbid chronic pain and PTSD, a sleep intervention program for veterans who have blast-induced mild TBI and headache, and a CPTbased treatment program for veterans who have comorbid PTSD and mild TBI. The authors concluded that “the results of these studies support an integrated approach to treatment and tailoring of existing evidence-based treatments to meet the specific needs of veterans.”
Integrated-care models are evolving in VA. For example, the Patient Aligned Care Teams deliver comprehensive care coordinated by primary-care providers and specialists, and SUD and PTSD specialists coordinate treatment planning and delivery of SUD services that best meet the needs of patients who have co-occurring PTSD and SUD. Nonetheless, VA faces challenges in delivering comprehensive and fully integrated care for patients who have a complex cluster of medical, psychiatric, and psychosocial conditions. Reports from VA’s consensus panels mentioned above (one addressing comorbid TBI, pain, and PTSD and the other addressing comorbid SUD and PTSD) emphasized that a major challenge for clinicians was the development of an interdisciplinary treatment plan that coordinates and incorporates input from all necessary specialty services. Obstacles cited include the long time needed to consult with clinicians in other disciplines and the lack of motivation of consulting practitioners who often do not receive clinical workload “credit” for such activities (National Center for PTSD, 2010a, 2010b). Similarly, Lew et al. (2008) highlighted aspects of VA’s polytrauma rehabilitation centers and PTSD programs that undermine integrated care delivery.
Summary
The co-occurrence of mental-health problems or the combination of mental-health problems with neurologic disorders places additional demands on treatments designed for one of these conditions in isolation. The current literature emphasizes the need for research to develop an evidence base and identify best practices for patients who have comorbid conditions. In addition to determining which interventions are efficacious in treating for comorbid conditions, research studies should examine facets of clinical effectiveness, such as treatment adherence, engagement, and tolerability (Brenner et al., 2009; Carlson et al., 2011; Dobscha et al., 2009; Lew et al., 2008; National Center for PTSD, 2010b). The great burden associated with comorbid conditions underscores the need for coordinated care among providers for the delivery of patientcentered care for all conditions experienced by service members and veterans.
It is not known whether simple adaptations of evidence-based treatments will be sufficient to preserve their efficacy or whether a fundamentally different treatment approach will be required. An example of the latter evolved for people who had dual diagnoses of SUD and severe mental illness with the development of integrated dual diagnosis treatment (Drake et al., 2001). That approach introduced such ideas as holistic case conceptualization and individualized staging of treatment components to address the complexity of the clinical manifestation of cooccurring disorders. The complexity of co-occurring PTSD, TBI, MDD, and SUD may necessitate the development of new treatment concepts to treat veterans of OEF and OIF.
CONCLUSIONS
Overall, the VA and DOD clinical guidelines for screening, assessment, and treatment are in line with the available evidence base and the state-of-the-art CPGs put forth by various
professional organizations. Screening for, assessment of, and treatment for brain injuries and psychologic problems are not always implemented in a consistent manner or in line with the evidence base between and within DOD and VA. The available data suggest that patients who need evidence-based care may not be receiving it.
VA’s performance-measurement initiatives are at the forefront of mental-health care evaluation. The VA performance measures that the committee reviewed, which mostly examine processes of care, appear to be based on sound evidence. Measures related to patient health outcomes are lacking. VA could do more to make information about the mental-health measures being collected and their results systematically available. DOD has an established mechanism for collecting performance data—the Military Health System Population Health Portal—but lacks an emphasis on mental health. There is an opportunity for VA and DOD to synchronize their efforts in this field.
FUTURE RESEARCH DIRECTIONS
As the committee reviewed the literature and examined the array of federally funded research on screening, assessment, and treatment of OEF and OIF service members and veterans (Appendix D), it identified several subjects for future research. The committee notes that a number of studies that are under way will shed light on the potential effectiveness of a variety of interventions. However, there are gaps in the empirical base that warrant additional systematic research:
• Studies of the psychometric properties of screening and assessment instruments to determine appropriate screening and diagnostic thresholds specifically for VA and DOD populations, determine the validity and reliability of VHA’s TBI screening tool, and determine the accuracy of the DOD head computed-tomography guidelines (adapted from American College of Emergency Physicians guidelines) for detecting clinically significant brain injury in theater.
• RCTs to determine the efficacy of interventions that do not yet have a strong evidence base, including telehealth mental-health care delivery, Internet-based clinician training and treatment interventions, complementary medicine approaches (such as yoga), staged and stepped care, and TBI treatments recommended by VHA guidelines.
• Comparative-effectiveness trials to determine the effectiveness of group vs individual treatments, duration of psychotherapies, dose and duration in the use of SSRIs, and combination treatments.
• Studies of the effectiveness and efficacy of treatment interventions in producing improved desired outcomes in veterans and service personnel.
• Studies to identify what modifications, if any, need to be made in the current evidence-based treatment recommendations for each condition for the management of comorbid conditions.
• Research to assess consumer (patient and family) preferences for educational materials that explain the different evidence-based treatments that are available; such studies should determine the most effective formats for facilitating informed decision making.
Screening, assessment, and treatment approaches for brain injuries and psychologic health problems are not always implemented between and within DOD and VA in a consistent manner or aligned with the evidence base. DOD and VA use different thresholds for some of the same mental-health screening and assessment instruments, such as the Primary Care PTSD screen and the PTSD Checklist for PTSD and the Patient Health Questionnaire for depression. Parts of VA and DOD clinical guidance lack recommendations for a specific assessment instrument and leave the selection of instrument to the clinician, for example, for suicide-risk assessments and TBI neurocognitive assessments.
The committee identified topics on which VA and DOD policies are out of step with the evidence base. There is a lack of clear scientific evidence supporting the effectiveness of the neurocognitive assessment tool (Automated Neuropsychological Assessment Metrics) used by DOD to assess cognitive function after a head injury. With respect to suicide prevention, DOD policy prohibits restricting access to privately owned weapons for those who might be at risk for of suicide, but research shows that restricting access to lethal means prevents suicides. VA has included Acceptance and Commitment Therapy for depression in its national rollout of evidenced-based treatments, however, there is not sufficient evidence to support its use as a firstline intervention. Moreover, the limited data that are available suggest that patients in need of evidence-based care might not be receiving it. The committee has serious concerns about inadequate and untimely clinical followup and low rates of delivery of evidence-based treatments, particularly psychotherapies to treat PTSD and depression and approved pharmacotherapies for substance use disorder.
The committee recommends that the Department of Defense and the Department of Veterans Affairs select instruments and their thresholds for mental-health screening and assessment in a standardized way on the basis of the best available evidence. The committee also recommends that the two departments ensure that treatment offerings are aligned with the evidence base, particularly before national rollouts, and that all patients consistently receive first-line treatments as indicated.
Unwarranted variability in clinical practices and deviations from the evidence base presents threats to high-quality patient care. Such variability also hampers opportunities to make research comparisons that can inform and improve the effectiveness of screening, assessment, and treatment practices. The committee notes that the emphasis on promoting evidence-based practices should not discourage the use of new or experimental interventions where there is reason to believe that they might lead to better outcomes than standard interventions.
In many ways, DOD and VA clinicians are at the forefront of providing evidence-based care for service members and veterans who have brain injuries and psychologic-health problems. But there are opportunities to improve processes of training and evaluating clinicians. DOD does not have a standardized process for assessing clinicians’ competence to administer the Military Acute Concussion Evaluation for TBI. VA is implementing a robust clinician-training program to disseminate evidence-based psychotherapies, but the program appears to lack periodic clinician assessments beyond the 6-month training period to ensure that continued treatment fidelity is maintained. Current approaches for training clinicians on the management of comorbid conditions (by disseminating clinician resources, for example) are not adequate.
The committee recommends that the Department of Defense and the Department of Veterans Affairs incorporate continuing supervision and education into programs that train clinicians in the use of selected assessment instruments and evidence-based treatments. Once clinicians are trained, the two departments should systematically and periodically evaluate them to assess the degree to which therapeutic interventions are accurately implemented according to a manual, protocol, or model as supported by evidence. The committee also recommends that the two departments place greater focus on coordinated, interdisciplinary care to ensure optimal treatment for service members and veterans.
The committee determined that there are few data on whether screening, assessment, and treatment interventions in DOD and VA are being implemented according to clinical guidelines and VA and DOD policy. Minimal data is readily available on the numbers of people who have been screened and the extent to which followup is appropriate and timely for those who screen positive. There is a dearth of data on which treatments patients receive and whether the treatments were appropriate, timely, and delivered at the recommended intensity level (for example, individual vs group format and frequency and duration of sessions).
The committee recommends that the Department of Defense and the Department of Veterans Affairs conduct systematic assessments to determine whether screening and treatment interventions are being implemented according to clinical guidelines and department policy. Data systems should be developed to assess treatment outcomes, variations among treatment facilities, and barriers to the use of evidence-based treatment.
REFERENCES
AFHSC (Armed Forces Health Surveillance Center). 2010. Supplemental report: Selected mental health disorders among active component members, US Armed Forces, 2001-2010. Medical Surveillance Monthly Report 17(11):2-5.
AHRQ (Agency for Healthcare Research and Quality). 2012. National Quality Measures Clearinghouse. www.qualitymeasures.ahrq.gov/browse/by-organization.aspx?alpha=V (accessed June 18, 2012).
Air Force Medical Operations Agency. undated. Air Force Guide for Managing Suicidal Behavior: Strategies, Resources and Tools. Brooks, TX: Air Force Medical Operations Agency.
Alcohol and Drug Abuse Institute Library. 2012. Screening and Assessment Instruments: Addiction Severity Index—Baseline and Follow-Up. 5th Ed. bit.ly/ASI_inst (accessed July 2, 2012).
Allan, C. L., L. L. Herrmann, and K. P. Ebmeier. 2011. Transcranial magnetic stimulation in the management of mood disorders. Neuropsychobiology 64(3):163-169.
American Academy of Neurology. 1997. Practice Parameter: The Management of Concussion in Sports. St. Paul, MN: Quality Standards Subcommittee, American Academy of Neurology.
American Society of Addiction Medicine. 2012. The ASAM Patient Placement Criteria. http://www.asam.org/publications/patient-placement-criteria (accessed July 3, 2012).
Ames, G., and C. Cunradi. 2004. Alcohol use and preventing alcohol-related problems among young adults in the military. Alcohol Research and Health 28(4):252-257.
Anton, R. F., S. S. O’Malley, D. A. Ciraulo, R. A. Cisler, D. Couper, D. M. Donovan, D. R. Gastfriend, J. D. Hosking, B. A. Hosking, B. A. Johnson, J. S. LoCastro, R. Longabaugh, B. J. Mason, M. E. Mattson, W. R. Miller, H. M. Pettinati, C. L. Randall, R. Swift, R. D. Weiss, L. D. Williams, and A. Zweban. 2006. Combined pharmacotherapies and behavioral interventions for alcohol dependence: The combine study: A randomized controlled trial. Journal of the American Medical Association 295(17):2003-2017.
APA (American Psychiatric Association). 2000. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR), 4th Ed. Washington, DC: American Psychiatric Association.
———. 2003. Practice Guideline for the Assessment and Treatment of Patients with Suicidal Behaviors. Washington, DC: American Psychological Association.
———. 2010. Practice Guideline for the Treatment for Patients with Major Depressive Disorder, 3rd Ed. Arlington, VA: Workgroup on Major Depressive Disorder, American Psychiatric Association.
Arbaizar, B., T. Diersen-Sotos, I. Gomez-Acebo, and J. Llorca. 2010. Topiramate in the treatment of alcohol dependence: A meta-analysis. Actas Españolas de Psiquiatría 38(1):8-12.
Arroll, B., F. Goodyear-Smith, S. Crengle, J. Gunn, N. Kerse, T. Fishman, K. Falloon, and S. Hatcher. 2010. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Annals of Family Medicine 8(4):348-353.
Aubry, M., R. Cantu, J. Dvorak, T. Graf-Baumann, K. Johnston, J. Kelly, M. Lovell, P. McCrory, W. Meeuwisse, and P. Schamasch. 2002. Summary and agreement statement of the First International Conference on Concussion in Sport, Vienna 2001: Recommendations for the improvement of safety and health of athletes who may suffer concussive injuries. British Journal of Sports Medicine 36(1):6-10.
Babor, T. F., J. C. Higgins-Biddle, J. B. Saunders, and M. G. Monteiro. 2001. AUDIT: Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care, 2nd Ed. Geneva: The World Health Organization.
Bagley, S. C., B. Munjas, and P. Shekelle. 2010. A systematic review of suicide prevention programs for military or veterans. Suicide and Life-Threatening Behavior 40(3):257-265.
Baldessarini, R. J., L. Tondo, and J. Hennen. 2001. Treating the suicidal patient with bipolar disorder. Reducing suicide risk with lithium. Annals of the New York Academy of Sciences 932:24-38; discussion 39-43.
Barbato, A., and B. D’Avanzo. 2006. Marital therapy for depression. Cochrane Database of Systematic Reviews(2):CD004188.
Bazarian, J. J., T. Wong, M. Harris, N. Leahey, S. Mookerjee, and M. Dombovy. 1999. Epidemiology and predictors of post-concussive syndrome after minor head injury in an emergency population. Brain Injury 13(3):173-189.
Blake, D. D., F. W. Weathers, L. M. Nagy, D. G. Kaloupek, F. D. Gusman, D. S. Charney, and T. M. Keane. 1995. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress 8(1):75-90.
Blanchard, E. B., J. Jones-Alexander, T. C. Buckley, and C. A. Forneris. 1996. Psychometric properties of the PTSD checklist (PCL). Behaviour Research and Therapy 34(8):669-673.
Bliese, P. D., K. M. Wright, A. B. Adler, O. Cabrera, C. A. Castro, and C. W. Hoge. 2008. Validating the primary care posttraumatic stress disorder screen and the posttraumatic stress disorder checklist with soldiers returning from combat. Journal of Consulting and Clinical Psychology 76(2):272-281.
Blue Ribbon Work Group on Suicide Prevention in the Veteran Population. 2008. Report to James B. Peake, MD, Secretary of Veterans Affairs, June 30, 2008. http://www.mentalhealth.va.gov/suicide_prevention/Blue_Ribbon_Report-FINAL_June-30-08.pdf (accessed October 13, 2012).
Boden, M. T., R. Kimerling, J. Jacobs-Lentz, D. Bowman, C. Weaver, D. Carney, R. Walser, and J. A. Trafton. 2012. Seeking safety treatment for male veterans with a substance use disorder and posttraumatic stress disorder symptomatology. Addiction 107(3):578-586.
Bradley, K. A., K. R. Bush, A. J. Epler, D. J. Dobie, T. M. Davis, J. L. Sporleder, C. Maynard, M. L. Burman, and D. R. Kivlahan. 2003. Two brief alcohol-screening tests from the alcohol use disorders identification test (audit): Validation in a female veterans affairs patient population. Archives of Internal Medicine 163(7):821-829.
Bradley, K. A., A. F. DeBenedetti, R. J. Volk, E. C. Williams, D. Frank, and D. R. Kivlahan. 2007. Audit-C as a brief screen for alcohol misuse in primary care. Alcoholism, Clinical and Experimental Research 31(7):1208-1217.
Bradley, K. A., G. T. Lapham, E. J. Hawkins, C. E. Achtmeyer, E. C. Williams, R. M. Thomas, and D. R. Kivlahan. 2011. Quality concerns with routine alcohol screening in VA clinical settings. Journal of General Internal Medicine 26(3):299-306.
Brain Trauma Foundation, American Association of Neurological Surgeons, and Congress of Neurological Surgeons. 2007. Guidelines for the management of severe traumatic brain injury. Journal of Neurotrauma 24(1 Suppl):S1-106.
Brenner, L., R. Breshears, L. Betthauser, K. Bellon, E. Holman, J. Harwood, M. Silverman, J. Huggins, and H. Nagamoto. 2011. Implementation of a suicide nomenclature within two VA healthcare settings. Journal of Clinical Psychology in Medical Settings (2):116-128.
Brenner, L. A., R. D. Vanderploeg, and H. Terrio. 2009. Assessment and diagnosis of mild traumatic brain injury, posttraumatic stress disorder, and other polytrauma conditions: Burden of adversity hypothesis. Rehabilitation Psychology 54(3):239-246.
Breshears, R. E., L. A. Brenner, J. E. Harwood, and P. M. Gutierrez. 2010. Predicting suicidal behavior in veterans with traumatic brain injury: The utility of the personality assessment inventory. Journal of Personality Assessment 92(4):349-355.
Brewin, C. R. 2005. Systematic review of screening instruments for adults at risk of PTSD. Journal of Traumatic Stress 18(1):53-62.
Brown, G. K. 2000. A Review of Suicide Assessment Measures for Intervention Research with Adults and Older Adults. Philadelphia, PA: University of Pennsylvania.
Brown, G. K., T. Ten Have, G. R. Henriques, S. X. Xie, J. E. Hollander, and A. T. Beck. 2005. Cognitive therapy for the prevention of suicide attempts: A randomized controlled trial. Journal of the American Medical Association 294(5):563-570.
Brusher, E. A. 2011. Chapter 4: Combat and operational stress control. In Textbooks of Military Medicine: Combat and Operational Behavioral Health, edited by E. C. Ritchie. Fort Detrick, MD: Office of the Surgeon General, Borden Institute.
Budney, A. J., S. T. Higgins, K. J. Radonovich, and P. L. Novy. 2000. Adding voucher-based incentives to coping skills and motivational enhancement improves outcomes during treatment for marijuana dependence. Journal of Consulting and Clinical Psychology 68(6):1051-1061.
Bullock, M. R., R. Chesnut, J. Ghajar, D. Gordon, R. Hartl, D. W. Newell, F. Servadei, B. C. Walters, and J. E. Wilberger. 2006. Guidelines for the surgical management of traumatic brain injury. Neurosurgery 58(3):S2-vi.
Burnett-Zeigler, I., M. Ilgen, M. Valenstein, K. Zivin, L. Gorman, A. Blow, S. Duffy, and S. Chermack. 2011. Prevalence and correlates of alcohol misuse among returning Afghanistan and Iraq veterans. Addictive Behaviors 36(8):801-806.
Cacciola, J. S., A. I. Alterman, B. Habing, and A. T. McLellan. 2011. Recent status scores for version 6 of the addiction severity index (ASI-6). Addiction 106(9):1588-1602.
Cacciola, J. S., A. I. Alterman, D. Dephilippis, M. L. Drapkin, C. Valadez, Jr., N. C. Fala, D. Oslin, and J. R. McKay. 2012. Development and initial evaluation of the Brief Addiction Monitor (BAM). Journal of Substance Abuse Treatment (Epub).
Calhoun, P. S., J. R. Elter, E. R. Jones, H. Kudler, and K. Straits-Troster. 2008. Hazardous alcohol use and receipt of risk-reduction counseling among US veterans of the wars in Iraq and Afghanistan. Journal of Clinical Psychiatry 69(11):1686-1693.
Calhoun, P. S., S. D. McDonald, V. S. Guerra, A. M. Eggleston, J. C. Beckham, K. Straits-Troster, and VA Mid-Atlantic MIRECC OEF/OIF Registry Workgroup. 2010. Clinical utility of the primary care—PTSD screen among US veterans who served since September 11, 2001. Psychiatry Research 178(2):330-335.
Canadian Academy of Sport Medicine Concussion Committee. 2000. Guidelines for assessment and management of sport-related concussion. Clinical Journal of Sport Medicine 10(3):209-211.
Cappa, S. F., T. Benke, S. Clarke, B. Rossi, B. Stemmer, C. M. van Heugten, and European Federation of Neurological Societies. 2003. EFNS guidelines on cognitive rehabilitation: Report of an EFNS task force. European Journal of Neurology 10(1):11-23.
Carlson, K., N. Greer, S. Kehle, R. MacDonald, L. Meis, I. Rutks, and T. J. Wilt. 2009. The Assessment and Treatment of Individuals with History of Traumatic Brain Injury and Post-Traumatic Stress Disorder: A Systematic Review of the Evidence. Minneapolis, MN: Evidence-based Synthesis Program (ESP) Center.
Carlson, K. F., D. Nelson, R. J. Orazem, S. Nugent, D. X. Cifu, and N. A. Sayer. 2010. Psychiatric diagnoses among Iraq and Afghanistan war veterans screened for deployment-related traumatic brain injury. Journal of Traumatic Stress 23(1):17-24.
Carlson, K. F., S. M. Kehle, L. A. Meis, N. Greer, R. MacDonald, I. Rutks, N. A. Sayer, S. K. Dobscha, and T. J. Wilt. 2011. Prevalence, assessment and treatment of mild traumatic brain injury and posttraumatic stress disorder: A systematic review of the evidence. Journal of Head Trauma Rehabilitation 26(2):103-115.
Casey, G. W., Jr. 2011. Comprehensive soldier fitness: A vision for psychological resilience in the US Army. American Psychologist 66(1):1-3.
Casscells, S. W. 2008a. Baseline Pre-deployment Neurocognitive Functional Assessment—Interim Guidance. Washington, DC: Department of Defense.
———. 2008b. Report to Congress in Response to National Defesnse Authorization Act, Fiscal Year 2007: House Report 109-452. Comprehensive Approach to Psychological Health and TBI. Washington, DC: Department of Defense.
CBO (Congressional Budget Office). 2012. The Veterans Health Administration’s Treatment of PTSD and Traumatic Brain Injury Among Recent Combat Veterans. Washington, DC: Congressional Budget Office.
CDC (Centers for Disease Control and Prevention). 2003. Report to Congress on Mild Traumatic Brain Injury in the United States: Steps to Prevent a Serious Public Health Problem. Atlanta, GA: National Center for Injury Prevention and Control, CDC.
Center for Substance Abuse Treatment. 2005. Substance Abuse Treatment for Persons with Co-Occurring Disorders: Treatment Improvement Protocol (TIP) Series 42. Rockville, MD: Substance Abuse and Mental Health Services Administration.
———. 2006. Definitions and Terms Relating to Co-Occurring Disorders. Rockville, MD: Substance Abuse and Mental Health Services Administration, and Center for Mental Health Services.
Chang, B. S., D. H. Lowenstein, and Quality Standards Subcommittee of the American Academy of Neurology. 2003. Practice parameter: Antiepileptic drug prophylaxis in severe traumatic brain injury: Report of the quality standards subcommittee of the American Academy of Neurology. Neurology 60(1):10-16.
Cherney, L. R., P. Gardner, J. A. Logemann, L. A. Newman, T. O'Neil-Pirozzi, C. R. Roth, and N. P. Solomon. 2010. The role of speech-language pathology and audiology in the optimal management of the service member returning from Iraq or Afghanistan with a blast-related head injury: Position of the communication sciences and disorders clinical trials research group. Journal of Head Trauma Rehabilitation 25(3):219-224.
Claassen, C. A., and K. L. Knox. 2011. Chapter 5: Assessment and management of high-risk suicidal states in postdeployment Operation Enduring Freedom and Operation Iraqi Freedom military personnel. In Caring for Veterans with Deployment-Related Stress Disorders: Iraq, Afghanistan and Beyond, edited by J. I. Ruzek, P. P. Schnurr, J. J. Vasterling, and M. J. Friedman. Washington, DC: American Psychological Association. Pp. 109-127.
Coldren, R. L., M. P. Kelly, R. V. Parish, M. Dretsch, and M. L. Russell. 2010. Evaluation of the military acute concussion evaluation for use in combat operations more than 12 hours after injury. Military Medicine 175(7):477-481.
Connery, H. S., and H. D. Kleber. 2007. Guideline watch (April 2007): Practice guideline for the treatment of patients with substance use disorders, 2nd edition. Focus 5(2).
Cozzarelli, T. A. 2010. Evaluation and treatment of persistent cognitive dysfunction following mild traumatic brain injury. Journal of Special Operations Medicine 10(1):39-42.
Cuijpers, P., F. Clignet, B. van Meijel, A. van Straten, J. Li, and G. Andersson. 2011. Psychological treatment of depression in inpatients: A systematic review and meta-analysis. Clinical Psychology Review 31(3):353-360.
Cushman, J. G., N. Agarwal, T. C. Fabian, V. Garcia, K. K. Nagy, M. D. Pasquale, A. G. Salotto, and East Practice Management Guidelines Work Group. 2001. Practice management guidelines for the management of mild traumatic brain injury: The East Practice Management Guidelines Work Group. Journal of Trauma—Injury, Infection, and Critical Care 51(5):1016-1026.
Davidson, J. R., S. W. Book, J. T. Colket, L. A. Tupler, S. Roth, D. David, M. Hertzberg, T. Mellman, J. C. Beckham, R. D. Smith, R. M. Davison, R. Katz, and M. E. Feldman. 1997. Assessment of a new self-rating scale for post-traumatic stress disorder. Psychological Medicine 27(1):153-160.
Dawson, D. A., B. F. Grant, F. S. Stinson, and Y. Zhou. 2005. Effectiveness of the derived Alcohol Use Disorders Identification Test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population. Alcoholism: Clinical and Experimental Research 29(5):844-854.
DCoE (Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury). 2010. Case Management of Concussion/Mild TBI. Silver Spring, MD: Department of Defense.
———. 2011a. All the Way Home: Preventing Suicide Among Service Members and Veterans. Boston, MA: DoD/VA Annual Suicide Prevention Conference, March 13-17, 2011.
———. 2011b. Clinical Recommendation: Indications and Conditions for In Theater Post-Injury Neurocognitive Assessment Tool (NCAT) Testing. Silver Spring, MD: Department of Defense.
———. 2011c. Co-Occurring Conditions Toolkit: Mild Traumatic Brain Injury and Psychological Health, Revised September 2011. Silver Spring, MD: Department of Defense.
———. 2011d. Department of Defense Suicide Event Report: Calendar Year 2010 Annual Report. Washington, DC: National Center for Telehealth and Technology, Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury.
———. 2011e. Guidance for Training, Education on Clinical Practice Guidelines. Arlington, VA: Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury.
———. 2011f. Screening and Assessment Tools for Suicide Prevention: Compilation by the DOD/VA Suicide Prevention Tools Working Group. Arlington, VA and Silver Spring, MD: Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury.
———. 2012a. Defense and Veterans Brain Injury Center. Silver Spring, MD: Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury.
———. 2012b. Fact Sheet Summer 2012. Silver Spring, MD: Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury.
———. 2012c. Overview of DCOE and DOD Suicide Prevention Efforts. Silver Spring, MD: Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury.
———. 2012d. RESPECT-Mil: Re-Engineering Systems of Primary Care Treatment in the Military. Washington, DC: Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury.
———. 2012e. Traumatic Brain Injury. Silver Spring, MD: Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury.
de Groot, V., H. Beckerman, G. J. Lankhorst, and L. M. Bouter. 2003. How to measure comorbidity: A critical review of available methods. Journal of Clinical Epidemiology 56(3):221-229.
Defense Health Board. 2010. Memorandum: Findings Pertaining to Evidence-Based Metrics for Department of Defense Mental Health Pre-Clinical Program Effectiveness and Clinical Program Outcomes. Falls Church, VA: Defense Health Board.
DeFraites, R., and M. Vythilingam. 2011. DOD Deployment Mental Health Assessments: A Review and Update. Falls Church, VA: Force Health Protection and Readiness.
Dempsey, K. E., W. C. Dorlac, K. Martin, R. Fang, C. Fox, B. Bennett, K. Williams, and S. Flaherty. 2009. Landstuhl Regional Medical Center: Traumatic brain injury screening program. Journal of Trauma Nursing 16(1):6-7, 10-12.
Department of the Army. 2010a. The DOD Automated Neuropsychological Assessment Metric Program: A Critical Review of Supporting Documentation. Falls Church, VA: Department of the Army Office of the Surgeon General.
———. 2010b. Re-Engineering Systems of the Primary Care Treatment (of Depression and Post-Traumatic Stress Disorder) in the Military Documentation Form. Fort Sam Houston, TX: United States Army Medical Command.
———. 2012. Army 2020: Generating Health and Discipline in the Force. Washington, DC: Department of Defense.
Desai, M., R. Rosenheck, and T. J. Craig. 2006. Case-finding for depression among medical outpatients in the veterans health administration. Medical Care 44(2):175-181.
Desai, R. A., I. Harpaz-Rotem, L. M. Najavits, and R. A. Rosenheck. 2008. Impact of the seeking safety program on clinical outcomes among homeless female veterans with psychiatric disorders. Psychiatric Services 59(9):996-1003.
Dobscha, S. K., M. E. Clark, B. J. Morasco, M. Freeman, R. Campbell, and M. Helfand. 2009. Systematic review of the literature on pain in patients with polytrauma including traumatic brain injury. Pain Medicine 10(7):1200-1217.
DOD (Department of Defense). 1994. Directive 1010.1: Military Personnel Drug Abuse Testing Program. Washington, DC: Department of Defense.
———. 2008. DD Form 2796. Washington, DC: Department of Defense.
———. 2010a. The Challenge and the Promise: Strengthening the Force, Preventing Suicide and Saving Lives. Washington, DC: Department of Defense Task Force on the Prevention of Suicide By Members of the Armed Forces.
———. 2010b. Directive-Type Memorandum DTM 09-033: Policy Guidance for Management of Concussion/Mild Traumatic Brain Injury in the Deployed Setting. Washington, DC: Department of Defense.
———. 2011a. Report to Congress on Expenditures for Activities on Traumatic Brain Injury and Psychological Health, Including Posttraumatic Stress Disorder, for 2010. Washington, DC: Department of Defense ———. 2011b. Section 596 of the FY 2010 National Defense Authorization Act (NDAA) Comprehensive Plan on Prevention, Diagnosis, and Treatment of Substance Use Disorders (SUDS) and Disposition of Substance Use Offenders in the Armed Forces. Washington, DC: Department of Defense.
———. 2012. Report to Congress: Cognitive Rehabilitation Therapy for Traumatic Brain Injury for Fiscal Year 2011. Washington, DC: Department of Defense.
Donnelly, K. T., J. P. Donnelly, M. Dunnam, G. C. Warner, C. J. Kittleson, J. E. Constance, C. B. Bradshaw, and M. Alt. 2011. Reliability, sensitivity, and specificity of the VA traumatic brain injury screening tool. Journal of Head Trauma Rehabilitation 26(6):439-453.
Drake, A. I., K. S. Meyer, L. M. Cessante, C. R. Cheung, M. A. Cullen, E. C. McDonald, and M. C. Holland. 2010. Routine TBI screening following combat deployments. NeuroRehabilitation 26(3):183-189.
Drake, R. E., C. Mercer-McFadden, K. T. Mueser, G. J. McHugo, and G. R. Bond. 1998. Review of integrated mental health and substance abuse treatment for patients with dual disorders. Schizophrenia Bulletin 24(4):589-608.
Drake, R. E., S. M. Essock, A. Shaner, K. B. Carey, K. Minkoff, L. Kola, D. Lynde, F. C. Osher, R. E. Clark, and L. Rickards. 2001. Implementing dual diagnosis services for clients with severe mental illness. Psychiatric Services 52(4):469-476.
DVBIC (Defense and Veterans Brain Injury Center). 2006. Acute Management of Mild Traumatic Brain Injury in Military Operational Settings: Clinical Practice Guideline and Recommendations. Washington, DC: Defense and Veterans Brain Injury Center.
———. 2007. Joint Theater Trauma System Clinical Practice Guideline: Theater Screening and Management of Mild Traumatic Brain Injury (Concussion). Silver Spring, MD: Department of Defense.
———. 2008a. Consensus Conference on the Acute Management of Concussion/Mild Traumatic Brain Injury (mTBI) in the Deployed Setting. Washington, DC: Defense and Veterans Brain Injury Center.
———. 2008b. Updated Mild Traumatic Brain Injury (mTBI) Clinical Guidance. Washington, DC: Defense and Veterans Brain Injury Center.
Erlanger, D. M., K. C. Kutner, J. T. Barth, and R. Barnes. 1999. Neuropsychology of sports-related head injury: Dementia pugilistica to post concussion syndrome. Clinical Neuropsychologist 13(2):193-209.
Foa, E., T. Keane, and M. Friedman. 2009. Effective Treatments for PTSD, Practice Guidelines from the International Society for Traumatic Stress Studies, 2nd Ed. New York: The Guilford Press.
Foa, E. B., D. S. Riggs, C. V. Dancu, and B. O. Rothbaum. 1993. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress 6(4):459-473.
Forbes, D., M. Creamer, A. Phelps, R. Bryant, A. McFarlane, G. J. Devilly, L. Matthews, B. Raphael, C. Doran, T. Merlin, and S. Newton. 2007. Australian guidelines for the treatment of adults with acute stress disorder and post-traumatic stress disorder. Australian and New Zealand Journal of Psychiatry 41(8):637-648.
Fowler, J. C. 2012. Suicide risk assessment in clinical practice: Pragmatic guidelines for imperfect assessments. Psychotherapy 49(1):81-90.
Freeman, M. P., M. Fava, J. Lake, M. H. Trivedi, K. L. Wisner, and D. Mischoulon. 2010. Complementary and alternative medicine in major depressive disorder: The American Psychiatric Association Task Force report. Journal of Clinical Psychiatry 71(6):669-681.
Freeman, T. W., V. Roca, and T. Kimbrell. 2003. A survey of gun collection and use among three groups of veteran patients admitted to veterans affairs hospital treatment programs. Southern Medical Journal 96(3):240-243.
French, L., M. McCrea, and M. Baggett. 2008. The Military Acute Concussion Evaluation (MACE). Journal of Special Operations Medicine 8(1):68-77.
GAO (Government Accountability Office). 2008. VA Health Care: Mild Traumatic Brain Injury Screening and Evaluation Implemented for OEF/OIF Veterans, but Challenges Remain. Washington, DC: GAO.
———. 2010. VA Faces Challenges in Providing Substance Use Disorder Services and is Taking Steps to Improve These Services for Veterans. Washington, DC: GAO.
———. 2011. Department of Defense: Use of Neurocognitive Assessment Tools in Post-deployment Identification of Mild Traumatic Brain Injury. Washington, DC: GAO.
Glass, J. E., B. E. Perron, M. A. Ilgen, S. T. Chermack, S. Ratliff, and K. Zivin. 2010. Prevalence and correlates of specialty substance use disorder treatment for Department of Veterans Affairs healthcare system patients with high alcohol consumption. Drug and Alcohol Dependence 112(1-2):150-155.
Greenfield, S. F., J. M. Reizes, L. R. Muenz, B. Kopans, R. C. Kozloff, and D. G. Jacobs. 2000. Treatment for depression following the 1996 National Depression Screening Day. American Journal of Psychiatry 157(11):1867-1869.
Guillamondegui, O. D., S. A. Montgomery, F. T. Phibbs, M. L. McPheeters, P. T. Alexander, R. N. Jerome, J. N. McKoy, J. J. Seroogy, J. J. Eicken, S. Krishnaswami, R. M. Salomon, and K. E. Hartmann. 2011. Traumatic Brain Injury and Depression. Rockville, MD: Agency for Healthcare Research and Quality.
Gulliver, S. B., and L. E. Steffen. 2010. Towards Integrated Treatments for PTSD and Substance Use Disorders. Washington, DC: National Center for PTSD.
Haney, E. M., M. E. O’Neil, S. Carson, A. Low, K. Peterson, L. M. Denneson, C. Oleksiewicz, and D. Kansagara. 2012. Suicide Risk Factors and Risk Assessment Tools: A Systematic Review. Portland, OR: Evidence-based Synthesis Program (ESP) Center.
Harris, A. H., K. Humphreys, T. Bowe, D. R. Kivlahan, and J. W. Finney. 2009. Measuring the quality of substance use disorder treatment: Evaluating the validity of the Department of Veterans Affairs continuity of care performance measure. Journal of Substance Abuse and Treatment 36(3):294-305.
Harris, A. H., D. R. Kivlahan, T. Bowe, and K. N. Humphreys. 2010. Pharmacotherapy of alcohol use disorders in the Veterans Health Administration. Psychiatric Services 61(4):392-398.
Harris, A. H., E. Oliva, T. Bowe, K. N. Humphreys, D. R. Kivlahan, and J. A. Trafton. 2012. Pharmacotherapy of alcohol use disorders by the Veterans Health Administration: Patterns of receipt and persistence. Psychiatric Services 63:679-685.
Hawkins, E. J., G. T. Lapham, D. R. Kivlahan, and K. A. Bradley. 2010. Recognition and management of alcohol misuse in OEF/OIF and other veterans in the VA: A cross-sectional study. Drug and Alcohol Dependence 109(1-3):147-153.
Hawton, K., E. Townsend, E. Arensman, D. Gunnell, P. Hazell, A. House, and K. van Heeringen. 2000. Psychosocial versus pharmacological treatments for deliberate self harm. Cochrane Database of Systematic Reviews (2):CD001764.
Hegerl, U., P. Schonknecht, and R. Mergl. 2012. Are antidepressants useful in the treatment of minor depression: A critical update of the current literature. Current Opinion in Psychiatry 25(1):1-6.
Helmick, K. 2010. Cognitive rehabilitation for military personnel with mild traumatic brain injury and chronic post-concussional disorder: Results of April 2009 consensus conference. NeuroRehabilitation 26(3):239-255.
Helmick, K. M. 2011. Continuum of care for traumatic brain injury in the Department of Defense. Paper read at 2011 Military Health System Conference, February 7, 2011, Washington, DC.
HHS (US Department of Health and Human Services). 2004. United States Preventative Services Task Force: Screening and Behavioral Counseling Interventions in Primary Care to Reduce Alcohol Misuse: Recommendation Statement. Rockville, MD: Agency for Healthcare Research and Quality, US Department of Health and Human Services.
———. 2005. Helping Patients Who Drink Too Much. A Clinicians Guide. Washington, DC: Department of Health and Human Services.
Hides, L., S. Samet, and D. I. Lubman. 2010. Cognitive Behaviour Therapy (CBT) for the treatment of co-occurring depression and substance use: Current evidence and directions for future research. Drug and Alcohol Review 29(5):508-517.
Hirschfeld, R. M., and J. M. Russell. 1997. Assessment and treatment of suicidal patients. New England Journal of Medicine 337(13):910-915.
Hoge, C. W., C. A. Castro, S. C. Messer, D. McGurk, D. I. Cotting, and R. L. Koffman. 2004. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine 351(1):13-22.
Holm, L., J. D. Cassidy, L. J. Carroll, J. Borg, and WHO Collaborating Centre for Neurotrauma Task Force on Mild Traumatic Brain Injury. 2005. Summary of the WHO Collaborating Centre for Neurotrauma Task Force on Mild Traumatic Brain Injury. Journal of Rehabilitation Medicine 37(3):137-141.
Ingebrigtsen, T., B. Romner, and C. Kock-Jensen. 2000. Scandinavian guidelines for initial management of minimal, mild, and moderate head injuries. The Scandinavian Neurotrauma Committee. Journal of Trauma-Injury Infection and Critical Care 48(4):760-766.
International Society for Traumatic Stress Studies. 2009. Effective Treatments for PTSD: Practice Guidelines from the International Society for Traumatic Stress Studies, 2nd Ed. Edited by E. B. Foa, T. M. Keane, M. J. Friedman and J. A. Cohen. New York: Guilford Press.
IOM (Institute of Medicine). 2002. Reducing Suicide: A National Imperative. Washington, DC: The National Academies Press.
———. 2006. Posttraumatic Stress Disorder: Diagnosis and Assessment. Washington, DC: The National Academies Press.
———. 2009. Gulf War and Health, Volume 7: Long-Term Consequences of Traumatic Brain Injury. Washington, DC: The National Academies Press.
———. 2011a. Clinical Guideline Practices We Can Trust. Washington, DC: The National Academies Press.
———. 2011b. Cognitive Rehabilitation Therapy for Traumatic Brain Injury: Evaluating the Evidence. Washington, DC: The National Academies Press.
———. 2012. Treatment for Posttraumatic Stress Disorder in Military and Veteran Populations: Initial Assessment. Washington, DC: The National Academies Press.
———. 2013. Substance Use Disorders in the US Armed Forces. Washington, DC: The National Academies Press.
Ipser, J. C., and D. J. Stein. 2012. Evidence-based pharmacotherapy of post-traumatic stress disorder (PTSD). International Journal of Neuropsychopharmacology 15(6):825-840.
Iverson, G. L., J. A. Langlois, M. A. McCrea, and J. P. Kelly. 2009. Challenges associated with postdeployment screening for mild traumatic brain injury in military personnel. Clinical Neuropsychologist 23(8):1299-1314.
Ivins, B. J., R. Kane, and K. A. Schwab. 2009. Performance on the automated neuropsychological assessment metrics in a nonclinical sample of soldiers screened for mild TBI after returning from Iraq and Afghanistan: A descriptive analysis. Journal of Head Trauma Rehabilitation 24(1):24-31.
Jagoda, A. S., J. J. Bazarian, J. J. Bruns, Jr., S. V. Cantrill, A. D. Gean, P. K. Howard, J. Ghajar, S. Riggio, D. W. Wright, R. L. Wears, A. Bakshy, P. Burgess, M. M. Wald, and R. R. Whitson. 2009. Clinical policy: Neuroimaging and decisionmaking in adult mild traumatic brain injury in the acute setting. Journal of Emergency Nursing 35(2):e5-e40.
Jha, A. K., J. B. Perlin, K. W. Kizer, and R. A. Dudley. 2003. Effect of the transformation of the Veterans Affairs health care system on the quality of care. New England Journal of Medicine 348(22):2218-2227.
Jobes, D. A. 2012. The Collaborative Assessment and Management of Suicidality (CAMS): An evolving evidence-based clinical approach to suicidal risk. Suicide and Life-Threatening Behavior 42(6): 640-653.
Jobes, D. A., S. A. Wong, A. K. Conrad, J. F. Drozd, and T. Neal-Walden. 2005. The collaborative assessment and management of suicidality versus treatment as usual: A retrospective study with suicidal outpatients. Suicide and Life-Threatening Behavior 35(5):483-497.
Johnson, B. A., and N. Ait-Daoud. 2010. Topiramate in the new generation of drugs: Efficacy in the treatment of alcoholic patients. Current Pharmaceutical Design 16(19):2103-2112.
Johnston, K. M., M. Lassonde, and A. Ptito. 2001. A contemporary neurosurgical approach to sportrelated head injury: The McGill Concussion Protocol. Journal of the American College of Surgeons 192(4):515-524.
Jordan, B. 2012. DOD Could Renew Push to Restrict Personal Weapons. http://www.military.com/dailynews/2012/06/21/DoD-could-renew-push-to-restrict-personal-weapons.html (accessed October 1, 2012).
Kaner, E. F., F. Beyer, H. O. Dickinson, E. Pienaar, F. Campbell, C. Schlesinger, N. Heather, J. Saunders, B. Burnand. 2007. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database of Systematic Reviews 2.
Kaplan, M. S., N. Huguet, B. H. McFarland, and J. T. Newsom. 2007. Suicide among male veterans: A prospective population-based study. Journal of Epidemiology and Community Health 61(7):619-624.
Karlin, B. E. 2010. Evidence based psychotherapy and psychogeriatrics update. Paper read at Presentation to the 13th Annual VA Psychology Leadership Conference of the Association of VA Psychologist Leaders, May 14, 2010.
Karlin, B. E., J. I. Ruzek, K. M. Chard, A. Eftekhari, C. M. Monson, E. A. Hembree, P. A. Resick, and E. B. Foa. 2010. Dissemination of evidence-based psychological treatments for posttraumatic stress disorder in the veterans health administration. Journal of Traumatic Stress 23(6):663-673.
Kemp, J. E. 2011. Witness Testimony: Understanding and Preventing Veteran Suicide, December 12, 2011. Washington, DC: House Committee on Veterans Affairs.
Kleber, H. D., R. D. Weiss, R. F. Anton Jr., T. P. George, S. F. Greenfield, T. R. Kosten, C. P. O’Brien, B. J. Rounsaville, E. C. Strain, D. M. Ziedonis, G. Hennessy, and H. Smith Connery. 2006. Practice Guideline for the Treatment of Patients with Substance Use Disorder. Washington, DC: American Psychiatric Association.
Knapp, W. P., B. G. Soares, M. Farrel, and M. S. Lima. 2007. Psychosocial interventions for cocaine and psychostimulant amphetamines related disorders. Cochrane Database of Systematic Reviews 3:CD003023.
Knuth, T., P. B. Letarte, G. Ling, L. E. Moores, P. Rhee, D. Tauber, and A. Trask. 2005. Guidelines for the Field Management of Combat Related Head Trauma. New York: Brain Trauma Foundation.
Kroenke, K., R. L. Spitzer, and J. B. Williams. 2001. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine 16(9):606-613.
Kroenke K., R. L. Spitzer, and J. B. Williams. 2003. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Medical Care 41(11):1284-1292.
Kroenke, K., R. L. Spitzer, J. B. Williams, and B. Lowe. 2010. The patient health questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. General Hospital Psychiatry 32(4):345-359.
Lapham, G. T., C. E. Achtmeyer, E. C. Williams, E. J. Hawkins, D. R. Kivlahan, and K. A. Bradley. 2012. Increased documented brief alcohol interventions with a performance measure and electronic decision support. Medical Care 50(2):179-187.
Lew, H. L., R. D. Vanderploeg, D. F. Moore, K. Schwab, L. Friedman, J. A. Yesavage, T. M. Keane, D. L. Warden, and B. J. Sigford. 2008. Overlap of mild TBI and mental health conditions in returning OIF/OEF service members and veterans. Journal of Rehabilitation Research and Development 45(3):xi-xvi.
Mann, J. J., A. Apter, J. Bertolote, A. Beautrais, D. Currier, A. Haas, U. Hegerl, J. Lonnqvist, K. Malone, A. Marusic, L. Mehlum, G. Patton, M. Phillips, W. Rutz, Z. Rihmer, A. Schmidtke, D. Shaffer, M. Silverman, Y. Takahashi, A. Varnik, D. Wasserman, P. Yip, and H. Hendin. 2005. Suicide prevention strategies: A systematic review. Journal of the American Medical Association 294(16):2064-2074.
Martin, J. L., and E. Martin-Sanchez. 2012. Systematic review and meta-analysis of vagus nerve stimulation in the treatment of depression: Variable results based on study designs. European Psychiatry 27(3):147-155.
Mayet, S., M. Farrell, M. Ferri, L. Amato, and M. Davoli. 2005. Psychosocial treatment for opiate abuse and dependence. Cochrane Database Systematic Reviews (1):CD004330.
McCrea, M., K. M. Guskiewicz, S. W. Marshall, W. Barr, C. Randolph, R. C. Cantu, J. A. Onate, J. Yang, and J. P. Kelly. 2003. Acute effects and recovery time following concussion in collegiate football players: The NCAA Concussion Study. Journal of the American Medical Association 290(19):2556-2563.
McCrea, M., G. L. Iverson, T. W. McAllister, T. A. Hammeke, M. R. Powell, W. B. Barr, and J. P. Kelly. 2009. An integrated review of recovery after mild traumatic brain injury (mTBI): Implications for clinical management. Clinical Neuropsychologist 23(8):1368-1390.
McCrory, P., K. Johnston, W. Meeuwisse, M. Aubry, R. Cantu, J. Dvorak, T. Graf-Baumann, J. Kelly, M. Lovell, and P. Schamasch. 2005. Summary and agreement statement of the 2nd International Conference on Concussion in Sport, Prague 2004. British Journal of Sports Medicine 39(4):196-204.
McCrory, P., W. Meeuwisse, K. Johnston, J. Dvorak, M. Aubry, M. Molloy, and R. Cantu. 2009. Consensus statement on concussion in sport: The 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Journal of Athletic Training 44(4):434-448.
McDonald, S. D., and P. S. Calhoun. 2010. The diagnostic accuracy of the PTSD checklist: A critical review. Clinical Psychology Review 30(8):976-987.
McLellan, A. T., L. Luborsky, G. E. Woody, and C. P. O’Brien. 1980. An improved diagnostic evaluation instrument for substance abuse patients. The addiction severity index. Journal of Nervous and Mental Disease 168(1):26-33.
Mee-Lee, D., G. D. Schulman, M. Fishman, D. R. Gastfriend, and J. H. Griffith. 2001. ASAM Patient Placement Criteria for the Treatment of Substance-Related Disorders, Second Edition-Revised (ASAM-PPC-2R). Chevy Chase, MD: American Society of Addiction Medicine Inc.
MHSPHP (Military Healthcare System Population Health Portal). 2012. Methodology Document —Draft. San Antonio, TX: Health Informatics Division.
Milliken, C. S., J. L. Auchterlonie, and C. W. Hoge. 2007. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. Journal of the American Medical Association 298(18):2141-2148.
Montgomery, K. L., J. S. Kim, and C. Franklin. 2011. Acceptance and commitment therapy for psychological and physiological illnesses: A systematic review for social workers. Health and Social Work 36(3):169-181.
Moscicki, E. K. 2001. Epidemiology of completed and attempted suicide: Toward a framework for prevention. Clinical Neuroscience Research 1:310-323.
Nash, W. P., C. Silva, and B. Litz. 2009. The historic origins of military and veteran mental health stigma and the stress injury model as a means to reduce it. Psychiatric Annals 39(8):789-794.
National Center for PTSD. 2004. Iraq War Clinician Guide, 2nd ed. White River Junction, VT: Department of Veterans Affairs.
———. 2010a. Report of (VA) Consensus Conference: Practice Recommendations for Treatment of Veterans with Comorbid Substance Abuse and PTSD. Washington, DC: Department of Veterans Affairs.
———. 2010b. Report of (VA) Consensus Conference: Practice Recommendations for Treatment of Veterans with Comorbid TBI, Pain, and PTSD. Washington, DC: Department of Veterans Affairs.
———. 2012a. Assessment. http://www.ptsd.va.gov/professional/pages/assessments/assessment.asp (accessed August 1, 2012).
———. 2012b. Using the PTSD Checklist (PCL). Washington, DC: US Department of Veterans Affairs.
National Collaborating Centre for Mental Health. 2005. Post-traumatic Stress Disorder (PTSD): The Management of PTSD in Adults and Children in Primary and Secondary Care, Clinical Guideline 26. London, UK: National Institute for Clinical Excellence.
———. 2011. Alcohol-use Disorders: Diagnosis, Assessment and Management of Harmful Drinking and Alcohol Dependence. Leicester, UK: The British Psychological Society.
Neurobehavioral Guidelines Working Group. 2006. Guidelines for the pharmacologic treatment of neurobehavioral sequelae of traumatic brain injury. Journal of Neurotrauma 23(10):1468-1501.
New Zealand Guidelines Group. 2006. Evidence-Based Best Practice Guideline: Traumatic Brain Injury: Diagnosis, Acute Management and Rehabilitation. Wellington, New Zealand: New Zealand Guidelines Group.
NIAAA (National Institute on Alcohol Abuse and Alcoholism). 2008. Helping Patients Who Drink Too Much: A Clinician’s Guide. Washington, DC: National Institutes of Health.
NICE (National Institute for Health and Clinical Excellence). 2007. Head Injury: Triage, Assessment, Investigation and Early Management of Head Injury in Infants, Children and Adults. London, UK: National Institute for Health and Clinical Excellence.
———. 2009. Depression: Treatment and Management of Depression in Adults Including Adults with Chronic Physical Health Problems. London: National Institute for Health and Clinical Excellence.
Nieuwsma, J. A., R. B. Trivedi, J. McDuffie, I. Kronish, D. Benjamin, and J. W. J. Williams. 2011. Brief Psychotherapy for Depression in Primary Care: A Systematic Review of the Evidence. Washington, DC: Department of Veterans Affairs.
NIH (National Institutes of Health). 1999. Consensus development panel: Rehabilitation of persons with traumatic brain injury. Journal of the American Medical Association 282(10):974-983.
Oliva, E. M., A. H. Harris, J. A. Trafton, and A. J. Gordon. 2012. Receipt of opioid agonist treatment in the Veterans Health Administration: Facility and patient factors. Drug and Alcohol Dependence 122(3):241-246.
Ontario Neurotrauma Foundation. 2011. Guidelines for Mild Traumatic Brain Injury and Persistent Symptoms. Toronto, Canada: Ontario Neurotrauma Foundation.
Otis, J., R. McGlinchey, J. Vasterling, and R. Kerns. 2011. Complicating factors associated with mild traumatic brain injury: Impact on pain and posttraumatic stress disorder treatment. Journal of Clinical Psychology.
Oxman, T., A. J. Dietrich, J. John W. Williams, C. C. Engel, M. Friedman, P. Schnurr, S. Rosenberg, and S. L. Barry. 2008. Three Component Model for Primary Care Management of Depression and PTSD (Military Version). Bethesda, MD: Deployment Health Clinical Center.
Pani Pier, P., R. Vacca, E. Trogu, L. Amato, and M. Davoli. 2010. Pharmacological treatment for depression during opioid agonist treatment for opioid dependence. Cochrane Database of Systematic Reviews (9).
Pettinati, H. M., and W. D. Dundon. 2011. Comorbid depression and alcohol dependence: New approaches to dual therapy challenges and progress. Psychiatric Times 28(6).
Pettinati, H. M., D. W. Oslin, K. M. Kampman, W. D. Dundon, H. Xie, T. L. Gallis, C. A. Dackis, and C. P. O'Brien. 2010. A double-blind, placebo-controlled trial combining sertraline and naltrexone for treating co-occurring depression and alcohol dependence. American Journal of Psychiatry 167(6):668-675.
Phurrough, S., M. E. Salive, B. Lofton, and J. Schafer. 2007. Decision Memo for Vagus Nerve Stimulation for Treatment of Resistant Depression (TRD) (CAG-00313R). Washington, DC: Centers for Medicaid and Medicare Services.
Pigott, H. E., A. M. Leventhal, G. S. Alter, and J. J. Boren. 2010. Efficacy and effectiveness of antidepressants: Current status of research. Psychotherapy and Psychosomatics 79(5):267-279.
Pincus, H. A., B. Spaeth-Rublee, and K. E. Watkins. 2011. The case for measuring quality in mental health and substance abuse care. Health Affairs 30(4):730-736.
Polen, M. R., E. P. Whitlock, J. P. Wisdom, P. Nygren, and C. Bougatsos. 2008. Screening in Primary Care Settings for Illicit Drug Use: Staged Systematic Review for the United States Preventive Services Task Force. Rockville, MD: Agency for Healthcare Research and Quality.
Posner, K., G. K. Brown, B. Stanley, D. A. Brent, K. V. Yershova, M. A. Oquendo, G. W. Currier, G. A. Melvin, L. Greenhill, S. Shen, and J. J. Mann. 2011. The Columbia-Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. American Journal of Psychiatry 168(12):1266-1277.
Powers, M. B., M. B. Zum Vorde Sive Vording, and P. M. Emmelkamp. 2009. Acceptance and commitment therapy: A meta-analytic review. Psychotherapy and Psychosomatics 78(2):73-80.
Prins, A., P. Ouimette, R. Kimerling, R. P. Camerond, D. S. Hugelshofer, J. Shaw-Hegwer, A. Thrailkill, F. D. Gusman, and J. I. Sheikh. 2004. The Primary Care PTSD Screen (PC-PTSD): Development and operating characteristics. Primary Care Psychiatry 9(1):9-14.
Qaseem, A., V. Snow, T. D. Denberg, M. A. Forciea, and D. K. Owens. 2008. Using second-generation antidepressants to treat depressive disorders: A clinical practice guideline from the American College of Physicians. Annals of Internal Medicine 149(10):725-733.
Radomski, M. V., L. Davidson, D. Voydetich, and M. W. Erickson. 2009. Occupational therapy for service members with mild traumatic brain injury. American Journal of Occupational Therapy 63(5):646-655.
Ramchand, R., J. Acosta, R. M. Burns, L. H. Jaycox, and C. G. Pernin. 2011. The War Within: Preventing Suicide in the US Military. Santa Monica, CA: RAND Corporation.
Richards, D., and T. Richardson. 2012. Computer-based psychological treatments for depression: A systematic review and meta-analysis. Clinical Psychology Review 32(4):329-342.
Rimer, J., K. Dwan, D. A. Lawlor, C. A. Greig, M. McMurdo, W. Morley, and G. E. Mead. 2012. Exercise for depression. Cochrane Database Systematic Reviews 7.
Rodgers, M., M. Asaria, S. Walker, D. McMillan, M. Lucock, M. Harden, S. Palmer, and A. Eastwood. 2012. The clinical effectiveness and cost-effectiveness of low-intensity psychological interventions for the secondary prevention of relapse after depression: A systematic review. Health Technology Assessment 16(28):1-130.
Roebuck-Spencer, T. M., A. S. Vincent, D. A. Twillie, B. W. Logan, C. M. Lopez, C. K. Friedl, S. J. Grate, R. E. Schlegel, and K. Gilliland. 2012. Cognitive change associated with self-reported mild traumatic brain injury sustained during the OEF/OIF conflicts. Clinical Neuropsychologist 26(3):473-489.
Rohling, M. L., M. E. Faust, B. Beverly, and G. Demakis. 2009. Effectiveness of cognitive rehabilitation following acquired brain injury: A meta-analytic re-examination of Cicerone et al.’s (2000, 2005) systematic reviews. Neuropsychology 23(1):20-39.
SAMHSA (Substance Abuse and Mental Health Services Administration). 2009. Chapter 4: Screening and assessment. In Substance Abuse Treatment: Addressing the Specific Needs of Women. Treatment Improvement Protocol (TIP) Series, NO. 51. Rockville, MD: Substance Abuse and Mental Health Services Administration.
———. 2011. Screening, Brief Intervention and Referral to Treatment (SBIRT) in Behavioral Healthcare. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Sayer, N. 2009. Polytrauma/Blast-Related Injuries QUERI Center: Strategic Plan. Washington, DC: Quality Enhancement Research Initiative (QUERI), Department of Veterans Affairs.
———. 2012. Department of Veterans Affairs Quality Enhancement Research Initiative (QUERI) Polytrauma/Blast-Related Injuries QUERI Center Strategic Plan FY 2013 through FY 2015. Washington, DC: Department of Veterans Affairs.
Sayer, N. A., D. Nelson, and S. Nugent. 2011. Evaluation of the Veterans Health Administration traumatic brain injury screening program in the upper Midwest. Journal of Head Trauma Rehabilitation 26(6):454-467.
Schwab, K. A., B. Ivins, G. Cramer, W. Johnson, M. Sluss-Tiller, K. Kiley, W. Lux, and D. Warden. 2007. Screening for traumatic brain injury in troops returning from deployment in Afghanistan and Iraq: Initial investigation of the usefulness of a short screening tool for traumatic brain injury. Journal of Head Trauma Rehabilitation 22(6):377-389.
Scottish Intercollegiate Guidelines Network. 2009. Early management of patients with a head injury: A national clinical guideline. Edinburgh, Scotland: NHS Quality Improvement Scotland.
Seal, K. H., S. Maguen, B. Cohen, K. S. Gima, T. J. Metzler, L. Ren, D. Bertenthal, and C. R. Marmar. 2010. VA mental health services utilization in Iraq and Afghanistan veterans in the first year of receiving new mental health diagnoses. Journal of Traumatic Stress 23(1):5-16.
Seal, K. H., G. Cohen, A. Waldrop, B. E. Cohen, S. Maguen, and L. Ren. 2011. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001-2010: Implications for screening, diagnosis and treatment. Drug and Alcohol Dependence 116(1-3):93-101.
Shinn, A. K., and S. F. Greenfield. 2010. Topiramate in the treatment of substance-related disorders: A critical review of the literature. Journal of Clinical Psychiatry 71(5):634-648.
Smith, P. C., S. M. Schmidt, D. Allensworth-Davies, and R. Saitz. 2009. Primary care validation of a single-question alcohol screening test. Journal of General Internal Medicine 24(7):783-788.
Snell, D. L., L. J. Surgenor, E. J. Hay-Smith, and R. J. Siegert. 2009. A systematic review of psychological treatments for mild traumatic brain injury: An update on the evidence. Journal of Clinical and Experimental Neuropsychology: Official Journal of the International Neuropsychological Society 31(1):20-38.
Spitzer, R. L., J. B. Williams, M. Gibbon, and M. B. First. 1992. The structured clinical interview for DSM-III-R (SCID): History, rationale, and description. Archives of General Psychiatry 49(8):624-629.
Stanley, B., and G. K. Brown. 2008. Safety Plan Treatment Manual to Reduce Suicide Risk: Veteran Version. Washington, DC: Department of Veterans Affairs.
Stein, D. J., J. C. Ipser, and S. Seedat. 2006. Pharmacotherapy for post traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews 1.
Stein, D. J., J. C. Ipser, and N. McAnda. 2009. Pharmacotherapy of posttraumatic stress disorder: A review of meta-analyses and treatment guidelines. CNS Spectrums 14(1 Suppl 1):25-31.
Stewart, C. L., and T. A. Wrobel. 2009. Evaluation of the efficacy of pharmacotherapy and psychotherapy in treatment of combat-related post-traumatic stress disorder: A meta-analytic review of outcome studies. Military Medicine 174(5):460-469.
Stewart, J. A., D. A. Deliyannides, D. J. Hellerstein, P. J. McGrath, and J. W. Stewart. 2012. Can people with nonsevere major depression benefit from antidepressant medication? Journal of Clinical Psychiatry 73(4):518-525.
Tarrier, N., K. Taylor, and P. Gooding. 2008. Cognitive-behavioral interventions to reduce suicide behavior: A systematic review and meta-analysis. Behavior Modification 32(1):77-108.
Terrio, H. P., L. A. Nelson, L. M. Betthauser, J. E. Harwood, and L. A. Brenner. 2011. Postdeployment traumatic brain injury screening questions: Sensitivity, specificity, and predictive values in returning soldiers. Rehabilitation Psychology 56(1):26-31.
Thase, M. E. 2011. The small specific effects of antidepressants in clinical trials: What do they mean to psychiatrists? Current Psychiatry Reports 13(6):476-482.
Trivedi, A. N., S. Matula, I. Miake-Lye, P. A. Glassman, P. Shekelle, and S. Asch. 2011. Systematic review: Comparison of the quality of medical care in Veterans Affairs and non-Veterans Affairs settings. Medical Care 49(1):76-88.
Trofimovich, L., N. A. Skopp, D. D. Luxton, and M. A. Reger. 2012. Health care experiences prior to suicide and self-inflicted injury, active component, US Armed Forces, 2001-2010. Medical Surveillance Monthly Report 19(2):2-6.
Tuunainen, A., D. F. Kripke, and T. Endo. 2004. Light therapy for non-seasonal depression. Cochrane Database Systematic Reviews 2.
Ursano, R. J., C. Bell, S. Eth, M. Friedman, A. Norwood, B. Pfefferbaum, R. Pynoos, D. F. Zatzick, and D. M. Benedek. 2004. Practice Guideline for the Treatment of Patients with Acute Stress Disorder and Posttraumatic Stress Disorder. Arlington, VA: American Psychiatric Association.
USMedicine.com. 2012. Technology Makes for Efficient Application of New mTBI Policy. Lambertville, NJ: Marathon Medical Communications, Inc.
USPSTF (US Preventive Services Task Force). 2004. Screening for Suicide Risk, Topic Page. http://www.uspreventiveservicestaskforce.org/uspstf/uspssuic.htm (accessed October 22, 2012).
———. 2009. Screening for depression in adults: US Preventive Services Task Force recommendation statement. Annals of Internal Medicine 151(11):784-792.
VA (Department of Veterans Affairs). 2007. Vista Clinical Reminders: User Manual Washington, DC: Health Provider Systems Office of Information and Technology, Department of Veterans Affairs.
———. 2008a. Uniform Mental Health Services in VA Medical Centers and Clinics. Washington, DC: Department of Veterans Affairs.
———. 2008b. VHA Directive 2008-036: Use of Patient Record Flags to Identify Patients at High Risk for Suicide. Washington, DC: Department of Veterans Affairs.
———. 2010a. Examining the Process of Suicide Prevention Outreach Efforts at the US Department of Veterans Affairs, Committee on Veterans' Affairs, Subcommittee on Oversight and Investigations. Washington, DC: US Government Printing Office.
———. 2010b. Programs for Veterans with Post-Traumatic Stress Disorder (PTSD). Washington, DC: Department of Veterans Affairs, Veterans Health Administration.
———. 2010c. VHA Directive 2010-012 Screening and Evaluation of Possible Traumatic Brain Injury in Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) Veterans. Department of Veterans Affairs.
———. 2012. Quality Enhancement Research Initiative (QUERI): PT/BRI Queri TBI Screening and Evaluation Research Fact Sheet. Washington, DC: Department of Veterans Affairs.
———. undated-a. Suicide Risk Assessment Guide: Reference Manual. www.mentalhealth.va.gov/docs/Suicide_Risk_Assessment_Guide.doc (accessed October 22, 2012).
———. undated-b. Suicide Risk Assessment Pocket Card. http://www.mentalhealth.va.gov/docs/Suicide-Risk-Assessment-Guide.pdf (accessed October 22, 2012).
VA and DOD. 2009a. VA/DOD Clinical Practice Guideline for Management of Major Depressive Disorder (MDD). Washington, DC: Department of Veterans Affairs and Department of Defense.
———. 2009b. VA/DOD Clinical Practice Guidelines for Management of Concussion/Mild Traumatic Brain Injury (mTBI) Washington, DC: Department of Veterans Affairs and Department of Defense.
———. 2009c. VA/DOD Clinical Practice Guidelines for Management of Substance Use Disorders (SUD). Washington, DC: Department of Veterans Affairs and Department of Defense.
———. 2010. VA/DOD Clinical Practice Guideline for Management of Post-Traumatic Stress. Washington, DC: Department of Veterans Affairs and Department of Defense.
VA and VHA (Veterans Health Administration). 2007. VHA Directive 2007-013: Screening and Evaluation of Possible Traumatic Brain Injury in Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) Veterans. Washington, DC: Department of Veterans Affairs, Veterans Health Administration.
VA Office of Inspector General. 2011. Combined Assessment Program Summary Report Re-evaluation of Suicide Prevention Safety Plan Practices in Veterans Health Administration Facilities. Washington, DC: Department of Veterans Affairs.
———. 2012. Veterans Health Administration: Review of Veterans’ Access to Mental Health Care. Washington, DC VA Office of Inspector General.
Valderas, J. M., B. Starfield, B. Sibbald, C. Salisbury, and M. Roland. 2009. Defining comorbidity: Implications for understanding health and health services. Annals of Family Medicine 7(4):357-363.
Van Dyke, S. A., B. N. Axelrod, and C. Schutte. 2010. Test-retest reliability of the traumatic brain injury screening instrument. Military Medicine 175:947-949.
Vanderploeg, R. D., K. Schwab, W. C. Walker, J. A. Fraser, B. J. Sigford, E. S. Date, S. G. Scott, G. Curtiss, A. M. Salazar, and D. L. Warden. 2008. Rehabilitation of traumatic brain injury in active duty military personnel and veterans: Defense and Veterans Brain Injury Center randomized controlled trial of two rehabilitation approaches. Archives of Physical Medicine and Rehabilitation 89(12):2227-2238.
Vohringer, P. A., and S. N. Ghaemi. 2011. Solving the antidepressant efficacy question: Effect sizes in major depressive disorder. Clinical Therapeutics 33(12):B49-B61.
von Wolff, A., L. P. Holzel, A. Westphal, M. Harter, and L. Kriston. 2012. Combination of pharmacotherapy and psychotherapy in the treatment of chronic depression: A systematic review and meta-analysis. BMC Psychiatry 12(1):61.
Vythilingam, M., J. Davison, C. Engel, and H. V. Ritschard. 2010. Training to Administer DOD Deployment Mental Health Assessments. Washington, DC: Department of Defense.
Warden, D., A. J. Rush, M. H. Trivedi, M. Fava, and S. R. Wisniewski. 2007. The STAR*D project results: A comprehensive review of findings. Current Psychiatry Reports 9(6):449-459.
Warner, C. H., G. N. Appenzeller, T. Grieger, S. Belenkiy, J. Breitbach, J. Parker, C. M. Warner, and C. Hoge. 2011a. Importance of anonymity to encourage honest reporting in mental health screening after combat deployment. Archives of General Psychiatry 68(10):1065-1071.
Warner, C. H., G. N. Appenzeller, J. R. Parker, C. M. Warner, and C. W. Hoge. 2011b. Effectiveness of mental health screening and coordination of in-theater care prior to deployment to Iraq: A cohort study. American Journal of Psychiatry 168(4):378-385.
Watkins, K. E., and H. A. Pincus. 2011. Veterans Health Administration Mental Health Program Evaluation Capstone Report. Santa Monica, CA: RAND Corporation.
Watkins, K. E., D. J. Keyser, B. Smith, T. E. Mannle, D. R. Kivlahan, S. M. Paddock, T. Mattox, M. Horvitz-Lennon, and H. A. Pincus. 2010. Transforming mental healthcare in the Veterans Health Administration: A model for measuring performance to improve access, quality, and outcomes. Journal for Healthcare Quality 32(6):33-42.
Watkins, K. E., H. A. Pincus, S. Paddock, B. Smith, A. Woodroffe, C. Farmer, M. E. Sorbero, M. Horvitz-Lennon, T. Mannle, Jr., K. A. Hepner, J. Solomon, and C. Call. 2011. Care for veterans with mental and substance use disorders: Good performance, but room to improve on many measures. Health Affairs 30(11):2194-2203.
Weathers, F., J. Huska, and T. M. Keane. 1991. PTSD Checklist—Military Version (PCL-M). http://www.metrowestneurofeedback.com/files/62410952_ptsd_checklist.pdf (accessed March 15, 2011).
Weightman, M. M., R. Bolgla, K. L. McCulloch, and M. D. Peterson. 2010. Physical therapy recommendations for service members with mild traumatic brain injury. Journal of Head Trauma Rehabilitation 25(3):206-218.
WHO (World Health Organization). 2009. Guidelines for the Psychosocially Assisted Pharmacological Treatment of Opioid Dependence. Geneva, Switzerland: WHO.
Wilkins, K. C., A. J. Lang, and S. B. Norman. 2011. Synthesis of the psychometric properties of the PTSD Checklist (PCL) military, civilian, and specific versions. Depression and Anxiety 28(7):596-606.
Wittkampf, K. A., L. Naeije, A. H. Schene, J. Huyser, and H. C. van Weert. 2007. Diagnostic accuracy of the mood module of the patient health questionnaire: A systematic review. General Hospital Psychiatry 29(5):388-395.
Woodson, J. 2011. Military Suicide: An Update. Washington, DC: House Armed Services Committee, Military Personnel Subcommittee.
Yano, E. M., E. F. Chaney, D. G. Campbell, R. Klap, B. F. Simon, L. M. Bonner, A. B. Lanto, and L. V. Rubenstein. 2012. Yield of practice-based depression screening in VA primary care settings. Journal of General Internal Medicine 27(3):331-338.
Zoroya, G. 2011. More Troops’ Mild Brain Trauma Diagnosed. http://usatoday30.usatoday.com/news/military/story/2011-09-27/military-diagnoses-more-brain-injuries-trauma-battle-combat-policy/50575536/1 (accessed March 22, 2012).