12
Depression
Of all the possibilities for improving the lot of the elderly in this country, none may yield greater returns in human happiness and economic well-being than recognition and appropriate control of depression. Recent advances have made depression an eminently treatable disorder; yet only a minority of elderly depressed persons are receiving adequate treatment, in large part because of inadequate recognition of the disorder. Depression is seriously underdiagnosed and often misdiagnosed. Vast resources are expended in fruitless diagnostic searches, in medical treatment of somatic symptoms without a detectable basis, and in neglect of the underlying, treatable psychiatric disorder. This chapter addresses a broad range of medical and social factors that contribute to these difficulties and reviews the prevalence, definition, risk factors, and remediability of depression. It concludes with recommendations to improve the treatment of depression in the elderly.
DEFINITION AND PREVALENCE
Until quite recently, the prevalence and incidence of depression among the elderly have been sorely neglected topics of interest and research. Present assessments remain clouded by the difficulties of reaching a consensus on a definition of depression. "Depression" can mean many things—a mood, a symptom, or a psychiatric disorder. Although moods and symptoms may unfavorably influence the
quality of life, it is depression as a psychiatric disorder that provides the greatest opportunity for the reduction of suffering and the containment of costs. Accordingly, this chapter focuses on depression as a psychiatric disorder. Table 12-1 summarizes the results of recent studies comparing the percentage of depressive symptoms with the percentage of depressive disorders. As the table shows, there is a far lower rate of disorders than of symptoms.
The most striking feature of recent studies is the very low prevalence of depression among elderly persons who do not have associated medical problems. The highest figures are lower than those for younger persons, and studies explicitly comparing the prevalence of depression across age groups have led to a growing consensus that major depressive disorders (in contrast to symptoms) are less prevalent among the elderly.7 As noted above, in the elderly, symptoms of depression are more frequent than the psychiatric disorder, but whether they are more prevalent than among younger persons is not clear.
TABLE 12-1 Results of Recent Studies Among the Elderly Comparing Rates (percentage) of Depressive Disorders with Rates of Depressive Symptoms
|
Author |
Year Reported |
Rate of Depressive Disorders (%) |
Rate of Depressive Symptoms (%) |
|
Community surveys |
|
|
|
|
Blazer et al.5 |
1987 |
4.0 |
27 |
|
Blazer and Williams9 |
1980 |
3.7 |
4-13 |
|
Weissman et al.67 |
1985 |
1.9 |
|
|
Nielsson and Persson50 |
1984 |
1.0 |
|
|
Berkman et al.4 |
1986 |
|
15 |
|
Medical facilities (outpatients) |
|
|
|
|
Borson et al.10 |
1986 |
1.0 |
24 |
|
Koenig et al.40 |
1988 |
11.5 |
23 |
|
Nursing home |
|
|
|
|
Parmelee et al.51 |
1989 |
12.4 |
30.5 |
|
Goldman et al.26 |
1986 |
|
31-57 |
|
Demented |
|
|
|
|
Reifler et al.53 (community) |
1982 |
23.0 |
|
|
Wragg and Jeste70 (review of 30 studies of Alzheimer's disease) |
1989 |
10.0–20.0 |
40–50 |
|
Ernst et al.16 (nursing home) |
1977 |
25.0 |
56 |
The evidence regarding the mental health of the elderly comes as something of a surprise, and the reasons for it are unclear. Perhaps it is a survival effect: those persons more prone to depression may have died. Among elderly persons with associated physical illness the prevalence of depression is much higher, perhaps by a factor of four or five. The presumption that physical illness is a causal factor in this increased prevalence is supported by research of Harwood and Turner;33 they found that older persons were less apt to be depressed than younger persons when the influence of physical illness was controlled. The fact that physical illness and disability not only influence depression but are often inextricably intertwined with it further complicates an understanding of these problems.
High rates of depression and of depressive symptoms have been found in select populations—for example, among the elderly in nursing homes, where illness and disability are complicated by dependency and the loss of personal control. The highest rates of depression are found among the demented. Nearly a quarter of the demented suffer from major depression, and a majority are at least mildly depressed, adding to the already staggering burden of care.
Clearly, depression is common and inflicts a disproportionate burden of illness on older people. Just how great a burden is unclear because of problems in the diagnosis of depression. Depression among the elderly can appear almost as a different disorder from depression among younger persons, a difference that has found expression in such terms as ''masked depression" or "somatic equivalents." A striking difference is in the significance of depressed mood. Among the elderly, just as fever may be absent in infection, so too may depressed mood be present in the absence of detectable disease.11,19 At the same time, somatic symptoms play a far larger role in depression among the elderly than among younger persons. Somatic symptoms in the absence of physical disease present serious diagnostic difficulties to physicians and to survey researchers attempting to assess the extent of an individual's problem.
These difficulties in defining depression render critical aspects of health policy analysis more difficult. Once specific criteria for the diagnosis of depression in older persons are better defined and instruments developed for their application, far more effective studies of prevalence, incidence, and symptom severity can be carried out, both in the community and in high-risk groups. In addition, more precise estimates of the monetary as well as the psychological and emotional costs of depression will be possible, and improved cost-effectiveness estimates of treatment can be made.
RISK FACTORS
A discussion of risk factors in relation to depression encompasses two different directions of influence. The first is risk factors for depression; the second is depression as a risk factor for distress, disability, and suicide. The first of these directions has been investigated more thoroughly than the second, and a rather high degree of consensus has been reached about some of the major factors. These factors are listed in Table 12-2.
Blazer and Maddox8 have focused on the risk factor of social stress and its interaction with social support in the onset of late life depression. Blazer describes nine potential mechanisms (for further discussion of social isolation as a risk factor, see Chapter 14):
-
Social stressors, such as stressful life events, cause major depressive illness.
-
Social stressors decrease physical health status. The individual may react to the decline in physical health with a major depressive illness.
-
Social stressors in an individual's past lead to a physical and
TABLE 12-2 Categories of Risk Factors for Depression and Depressive Symptoms
|
Category |
Factor |
|
Biological |
Family history of depression; Depression earlier in life |
|
Changes in physical function |
Illness and medically imposed limitation; Limitations in strength or ambulation, or both; Changes in cognitive function; Sensory losses |
|
Grief and bereavement |
Loss of a child; Loss or disability of spouse; Death of siblings; Death(s) of friends or extended family |
|
Changes in network of support |
Geographic isolation; Loss of loved ones from death or illness; Unplanned retirement; Lack of confiding relationships |
|
SOURCE: Adapted from G. L. Gottlieb, "Optimizing Mental Function of the Elderly" in Practicing Prevention for the Elderly, by R. Lavizzo-Mourey, S. C. Day, D. Diserens, and J. A. Grisso, Hanley and Bellfus, Inc., Philadelphia, 1988, pp. 153-166. |
|
-
psychological condition that predisposes the individual to develop a major depressive illness at a later time.
-
Decreased social interaction causes major depressive illness.
-
Although social stressors lead to major depressive illness, this relationship is buffered by perceived social support. When perceived social support decreases, the effects of stressors are enhanced.
-
The lack of significant roles and attachments, such as the presence of a spouse, leads to major depressive illness.
-
The absence of important attachments in the social network leads to a decreased frequency of social interaction, which in turn leads to an increase in major depressive illness.
-
A decline in perceived social support directly contributes to an increase in major depressive illness.
-
The causal relationship of social stressors and major depressive illness is buffered by the frequency of social interaction. When frequency of social interaction decreases, the causal relationship between social stressors and depressive illness becomes clearer.
Constraints on sexuality have been identified by Butler and Lewis12 as a significant risk factor for depression. Some of these constraints are social, deriving from prejudice against sexual activity on the part of older persons that limits their opportunities and impairs their confidence in themselves. Other constraints may be pharmacological, especially the wide use of antihypertensive medications, and, paradoxically, medication for the treatment of depression itself.
Although not a risk factor, sleep disorders occur with some frequency concurrently with depression in the elderly.21,54 Physicians should be sensitive to sleep difficulties in older patients, especially early morning waking or frequent interruptions in sleep, as indications of depression.
REMEDIABILITY: OUTCOME OF TREATMENT
Treatment of depression in the elderly is one of the most rewarding activities that a health care worker can undertake. Many older people respond well to treatment. Such response is gratifying to both patients and their families who all too often may see the older person's deteriorating condition as an irreversible aspect of normal aging. Because relapse and recurrence of depression are all too frequent, continuing ready access to treatment is important.
Given the effectiveness of treatment for depression, the first and perhaps most serious problem in managing depression is the failure
to recognize its presence. It appears likely that a majority of elderly depressed patients escape medical attention for their disorder. Both patients and physicians, each for their own reasons, contribute to this problem. Many older persons find it painful to acknowledge the presence of emotional difficulties, and they find it even harder to seek medical attention for them. It may seem easier to ascribe their problems to the normal aging process and to believe there is nothing to be done about them.
Physicians often share their patients' disinclination to recognize depression, in part because their medical education has left them poorly equipped to cope with the complicated psychiatric problems of the elderly. Most are far more comfortable making a physical rather than a psychiatric diagnosis. Furthermore, even physicians who are prepared to make a psychiatric diagnosis may find themselves daunted by the special features of depression in the elderly, which may appear to be quite different from depression in the young. The absence of depressed mood may be particularly confusing; in addition, depression in the elderly is not infrequently intertwined with physical illness that complicates and obscures it.
Fortunately, this problem is remediable by improvement in the teaching of psychiatry and geriatrics. Even modest educational efforts can be useful. Thus, feedback of the results of a screening test to primary care physicians significantly improved their recognition of depression.23,25
Primary care physicians are strategically placed to recognize the presence of depression and may be the only source of care acceptable to the patient and his or her family. Patients and their families usually seek help from primary care physicians, and these care givers supply a greater proportion of the care of depressed elderly individuals than any other group of health workers. In addition, depression is one of the most common problems seen in their practices, occurring in as many as 30 percent of their patients. Many primary care physicians are skilled at recognizing depression; many, however, do not recognize, let alone diagnose and treat, this condition.64,65 The immediate result of this lack of recognition may be neglect of the problem or inappropriate and expensive medical workups, as well as a longer duration of illness, a risk factor for chronicity. The final result may be a significant increase in direct and indirect medical costs and in psychosocial costs.29
The first step in treatment, before any prescription, is a careful history and physical examination. There are several medical disorders that can lead to a depressed mood, and despite the strictures against excessive diagnostic workups, these disorders should be ruled out
first. Correction of electrolyte disturbance or hypothyroidism can be a most effective and economical way of controlling depressive symptoms that arise from these sources.
The value of a review of medications should not be underestimated. A significant percentage of the disorders that afflict the elderly, including depression, are drug induced. Some of these disorders are ones in which medication toxicity is more readily recognized, such as the confusional states and dementias. Attention to medications thus can pay large dividends. There are two major approaches to the treatment of depression in the elderly: somatic and psychosocial. Both forms of treatment are often indicated.
Antidepressant medication is the mainstay of treatment for major depression, and the most widely used agents are tricyclic antidepressants. In the hands of well-trained physicians, they are quite effective. Most younger depressed patients respond to such medication—about 60 to 70 percent of patients to the first tricyclic and another 20 percent to a second.27,41 These agents are the most widely used antidepressants among the elderly as well as among younger persons. Unfortunately, however, there is little information about their effects in the elderly. As Jarvik and Gerson37 point out in their review, it is paradoxical that older persons, for whom such information is sorely needed, have been largely excluded from treatment outcome research. Although understandable in terms of the difficulty of conducting such trials, this omission has left serious gaps in knowledge regarding how to treat depression in the elderly. This gap is particularly serious in the area of side effects, which constitute a formidable problem in the elderly, one that may well contribute to the inadequate treatment of depression in this age group. Many physicians are sufficiently daunted by this problem to refrain from the kind of vigorous pharmacotherapy of depression that would produce results.
Prominent side effects are those involving the cardiovascular system, including increased conduction time and increased heart rate. Earlier concerns that tricyclic antidepressants might induce arrhythmias, however, were probably unwarranted; in fact, they may even reduce arrhythmias. Other side effects are anticholinergic ones such as dry mouth, blurred vision, and urinary retention, a problem of particular concern in the elderly. Constipation and delirium are other troublesome side effects because of their negative influence on elderly patients' trust in their physician. Postural hypotension is another common problem and a reason for intensive education, particularly to prevent falls.
Overdosage is a concern that affects all pharmacotherapy of the
elderly. The decreased rate of drug clearance is a particular problem with the tricyclic antidepressants. Current practice is to start these medications at one-third to one-half the standard dosage and to increase it carefully thereafter.61
These problems warrant caution in the use of tricyclic antidepressants, but the experienced clinician can still use them to good effect.24 Electrocardiographic monitoring during the course of treatment greatly reduces cardiovascular risks, and recognition of the various side effects permits rapid response to problems that may develop. Still, the many side effects of tricyclic antidepressants raise the question of whether there may not be other, safer medications. These concerns have led to increased attention to another family of antidepressants, the monoamine oxidase (MAO) inhibitors. Among younger patients in recent years the effectiveness of tricyclic antidepressants and various problems with the MAO inhibitors had led to a decline in their use, except for some forms of treatment-resistant depression. The minimal cardiac and anticholinergic effects of the MAO inhibitors, however, have brought about a revival of interest in their use for the treatment of depression in the elderly.24
Problems with traditional antidepressant medication have led to great interest in new generations of these agents. Although tests in the elderly of the new generation of antidepressants have been limited, three new agents, Trazadone, Prozac, and Wellbutrin, have few side effects and are believed to have efficacy at least as great as that of older agents. Rapid development of new and more potent antidepressants means that medication will assume increasing importance in the years ahead.
It is to be hoped that past reluctance to assess the effects of medication in older persons will be overcome in the near future and that there will be no further delay in determining the value of these agents and indications for their use in the elderly. Indeed, excellent opportunities exist for industry to target this age group for clinical trials of antidepressant medications. Such trials would be expensive, but the expense could well be repaid, even in the short-term, by the recognition that would be accorded an agent that had undergone testing in the elderly.
Electroconvulsive therapy, or ECT, deserves special attention in a discussion of treatment of depression among the elderly. Its use in this population has been limited by the same kind of prejudice that affects its use in general, an unfortunate outcome because ECT appears to be significantly more effective than medication in various forms of severe depression. In one instructive series, 86 percent of patients with delusional depression responded to ECT, compared
with 32 percent who responded to medication.44 Thus, ECT may be both more effective and safer than the tricyclic antidepressants. It also has fewer side effects, but its major side effect, memory loss, although usually transient, creates special problems in a population in which memory loss is already a problem. Yet the efficacy of ECT is so marked that it might be considered the first form of treatment for some severely depressed patients, without waiting for the failure of drug therapy, as is now the case. Further research could yield rich dividends in establishing more precise indications for its use among the elderly.17,66
Primary care physicians are capable of treating most older depressed patients who come to them, but there are some circumstances in which physicians should seek consultation from a psychiatrist until they gain sufficient experience in managing antidepressant medications. Gottlieb28 recommends such consultation, preferably with a geriatric psychiatrist, and in some instances referral of patients with certain specific problems: major depression with delusional or other psychotic features; suicidal or homicidal ideation or a previous history of destructive behavior; treatment-resistant depression; symptoms (medical and neurological) that are difficult to distinguish from depression; and medical conditions that are made worse by depressive symptoms or antidepressant interventions.
The discussion above has considered the treatment of depression largely in terms of pharmacotherapy delivered by primary care physicians. Psychosocial therapies for depression in the elderly are also reasonably effective—and safer. Cognitive-behavioral treatment of depression has proved to be as effective as pharmacotherapy in less severe depressions, and it avoids the troublesome side effects of medication. A major limitation of such labor-intensive treatment is its cost. Even when delivered by nonphysicians, the fact that it is not reimbursable puts it beyond the reach of most elderly persons.
The issue of costs highlights the attractiveness of community-based programs that rely on volunteer or low-cost personnel more than on professional help. The experience of recent years has suggested that these approaches have merit, although few have achieved any degree of permanence and fewer yet have been evaluated. A common feature of these programs is their anticipation of stressful events, particularly bereavement, and their provision of supportive services.36,52,57 Controlled trials showed that one program of bereavement counseling achieved a significant decrease in morbidity,52 whereas a television-assisted approach produced some improvement in mood in the study participants.46 One innovative approach that deserves further exploration attempted to change negative attitudes
toward aging and the aged by emphasizing Eastern philosophical traditions that associate aging with increased spiritual development.1 The results of these various efforts are promising, and further research into this area seems warranted.
Finally, the committee notes that there is a serious discrepancy between the need for professional mental health assistance for elderly depressed people and the availability of such assistance. A survey in North Carolina revealed that no more than 8 percent of mentally impaired persons were receiving any professional mental health services, even though 20 percent of them were receiving psychotropic medication from their primary care physicians.8 The inadequacy of professional mental health care is even more striking among minority groups. A survey of an elderly Hispanic population with a high prevalence of depressive disorders showed that not a single person had ever received any professional mental health care, or even any antidepressant medication, even though at least 75 of them were judged to be suffering from a major depression.38
COSTS
An understanding of the costs of mental illness in general and of depression in particular lags far behind knowledge of the treatment of these disorders. This statement is true of all age groups and is particularly true of the elderly. The importance of obtaining more accurate estimates of these costs is underscored by the disproportionate use of medical resources by the elderly: although they constitute 12 percent of the population, they utilize 30 percent of medical resources.22 This problem of health care costs will increase with the growth of the elderly population, and particularly of the very old population with its even higher utilization of medical resources.
The special problem of underdiagnosis of depression among the elderly makes cost estimates especially difficult. Such cost estimates are important because of the very large hidden costs arising from three problems noted earlier: expensive and often fruitless diagnostic searches for physical illness; the often risky medical treatment of somatic symptoms without a physical basis; and inadequate or delayed treatment of depression leading to chronicity and disability. This triad of problems has not been addressed in any estimates of the costs of medical care of the elderly, and there is every reason to believe that it contributes significantly to such costs.
In addition to the monetary costs associated with depression, profound social and psychological costs have become apparent. These costs are described in the report of the RAND Corporation's recent
Medical Outcomes Study.58,67 This large "treated prevalence" outpatient study utilized a 20-item general health survey to measure the functioning and well-being of patients suffering from depression and eight chronic medical conditions—angina, arthritis, back problems, coronary artery disease, diabetes, gastrointestinal problems, high blood pressure, and lung problems. The survey of 11,000 patients revealed serious underestimation of the impact of depression on such routine activities as bathing, climbing stairs, dressing, socializing with friends, walking, and working. Its disabling effects were comparable to those of a serious heart condition and greater than those of most of the seven other medical conditions.68 Only arthritis was judged to be more painful, and only serious heart conditions resulted in more days in bed.
An important and surprising finding of the study was the extent of the disability experienced by persons with depressive symptoms who did not meet the full criteria for a depressive disorder: these patients suffered from disability as severe as that of patients who did meet the full criteria.68 The reasons for this unexpected finding are unclear; it may have been a result of the additive effect of chronic medical conditions. Nevertheless, because so little is known about the treatment of depressive symptoms independent of major depressive disorder, this finding is a major challenge to the health care system.
There have been few reports of studies of the economic costs of depression. The study of Stoudemire and colleagues59 placed a lower bound on the costs of depression at $16.3 billion in 1986, and these authors suggest that a full economic burden calculation might produce high estimates. Harwood and coworkers32 estimated the total costs of mental illness in 1980 to be $54.2 billion. It now appears that these values underestimated the actual costs. More precise estimates wait on additional assessments, such as that of the Medical Outcomes Study.
The potential for cost savings from more accurate psychiatric diagnosis and more appropriate treatment is suggested by growing understanding of the so-called "offset effect." An offset effect occurs when the provision of one type of service leads to a reduction in other types of services. A review by Mumford and colleagues47 described 58 reports of reductions of medical services in conjunction with the provision of mental health services. This review established that outpatient psychiatric treatment reduced the overall costs of medical care, primarily through reduced utilization of inpatient medical services. Of particular importance was the finding that the effect was larger for persons over the age of 55 than for younger individuals.
Subsequent research has begun to define the parameters of importance. For example, the offset effect is particularly marked in the case of alcoholism34,43 and is considerably weaker among persons of lower socioeconomic status.43 One striking, well-controlled study (that of Levitan and Kornfeld42) showed that the introduction of a part-time psychiatrist into an orthopedic ward decreased the median duration of stay from 42 to 30 days among elderly patients who underwent surgical repair of the femur. In New York City at this time (1980), hospital costs averaged $200 per day, and the authors estimated that a reduction of this magnitude in length of stay resulted in savings of $55,200 over the six-month period while the cost of the psychiatrist was only $5,000. Given the costs of underdiagnosis of psychiatric disorders and the inadequacy of psychiatric treatment, introducing psychiatric programs into medical care of the elderly should realize major cost savings.
Four studies provide convincing evidence of the value of outpatient psychiatric treatment. McCaffree44 demonstrated that cost reductions for custodial care more than compensated for increased costs of active intervention in the Washington State mental hospital system. In addition, Cassel and colleagues13 and Endicott and coworkers15 found that community-based psychiatric treatment was as effective, and less expensive, than hospital-based treatment. Finally, the Hu research group35 showed that the costs of caring for an elderly demented person at home were no more than half the costs incurred in a nursing home.
SUICIDE
One type of cost specific to depression is suicide. Stoudemire59 has estimated a total mortality cost of suicide resulting from depression at $4.2 billion, but the costs in human suffering are more difficult to estimate. Although official statistics show that suicide claims 30,000 lives in the United States each year,60 this figure is almost certainly larger owing to underreporting. Underreporting of suicide probably affects older persons more strongly than younger ones (R. Butler, Mount Sinai Medical Center, personal communication, June 1989) because physicians and the families of the elderly may be likely to ascribe death to causes other than suicide out of sentiment and compassion.
More than half of all suicides occur in persons suffering from depression.2 The increased risk of suicide among depressed persons of all ages is 30 times that of the non-affectively ill population; the lifetime risk of suicide of persons suffering from depression is 15
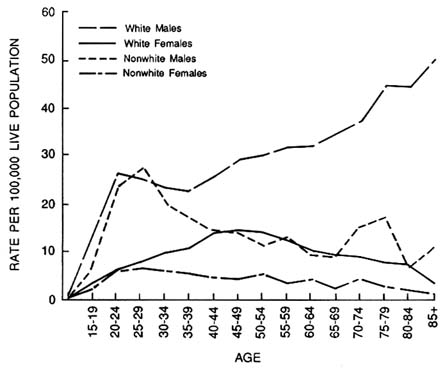
FIGURE 12-1 Suicide rates in the United States by age for white and nonwhite males and females. Source: National Center for Health Statistics, Mortality Statistics Branch, ''Suicide Rates in the United States by Age, Sex, and Color, 1975."
percent.31 Elderly depressed persons are at even higher risk than younger ones: 20 percent of all suicides occur in persons over the age of 65, and the rates are strikingly higher for elderly white men than for other groups (see Figure 12-1).62
These grim figures also have an optimistic side. Suicide is second only to lung cancer as a potentially preventable disorder, and there is usually considerable warning before a suicide attempt. Two-thirds of persons who take their lives have communicated their intent to at least one person, and most of them have consulted a physician hours to weeks before their suicide.55 Consultation with suicidal patients often presents physicians with a golden intervention opportunity, as most patients will tell their physicians of their plans if they are asked. Preventing suicide, however, requires recognition of the problem, and the same factors that limit recognition of depression in the elderly (inadequate teaching and training of physicians
in both psychiatry and geriatrics) also affect recognition of suicidal intent. An inexperienced physician may dismiss as perfectly understandable the depressive ruminations of elderly patients who have recently undergone losses. But, as Fawcett17 maintains, "the presence of a reason for depression is not a good reason to ignore the presence of a reason for depression is not a good reason to ignore the presence of depression." Thus, the clinician would be well advised to follow the injunction of Robins55 who asserts that the risk of suicide in elderly, depressed white men who express suicidal intent is so great that they should be hospitalized without delay.
The prevention of suicide requires not only better recognition of persons at risk but also improved mental health services, especially for the elderly. The benefits of improved mental health services in suicide prevention are indicated by the record of specialized centers for the treatment of affective disorders at which, even among the very high-risk populations in these centers, the suicide rate is negligible.39
REIMBURSEMENT
Reimbursement is a critical aspect of the management of depression, and control of depression could be greatly improved by changes in reimbursement schedules.30 Seventy-five percent of hospital care for the elderly is provided by Medicare, with private insurance covering 8 percent of costs and 5 percent each being contributed by Medicaid, the Veterans Administration, and other governmental agencies. Nursing home care, on the other hand, is financed to a great extent (50 percent) by patients and their families. Outpatient care is financed by Medicare Part B, a voluntary individual insurance program. (The monthly premium in 1989 was $31.90, and the plan had an annual deductible of $75.)
In contrast to federal support of most medical care, federal support of psychiatric care is severely limited. Although there is no limit to the total number of days provided for surgical or medical diagnoses, coverage in psychiatric hospitals is limited to a lifetime total of 190 days. Medicare reimbursement for outpatient psychiatric treatment has been even more limited—with even more deleterious consequences. Only "acute care" can be reimbursed, and a copayment of 50 percent is required for mental health care, compared with 20 percent for other medical treatment. Medicaid provides some support for psychiatric services, but reimbursement remains far below prevailing fees in most states. Private insurance coverage of psychiatric disorders is also severely limited: only 53 percent of private policies cover inpatient mental illness expenses in the same
way that they cover physical illness, and no more than 7 percent cover outpatient expenses in a manner similar to coverage of outpatient medical costs.30 In November 1989, Congress took a large step toward removing discrimination in the treatment of psychiatric disorders by eliminating a long-standing limitation on the total annual payment for mental health services. The other limitations, however, persist.
Even attempts to improve coverage for psychiatric disorders may misfire. The Omnibus Budget Reconciliation Act (OBRA) of 1987 required that all patients applying for admission to nursing homes be screened for mental disorders. The goal of this regulation was to provide appropriate care for these patients, but the result has too often been the opposite—preventing access to nursing home care for patients found to be in need of "active psychiatric treatment."
These discriminatory reimbursement practices severely limit the use of psychiatric services in hospitals, nursing homes, and ambulatory settings. The inadequacy of psychiatric services in nursing homes is particularly egregious. Furthermore, current practices lead to a serious imbalance in the type of site at which services are rendered, with expensive inpatient treatment being favored over more economical outpatient services. The limitation of support for outpatient care of psychiatric disorders, with its potential for the cost savings conferred by avoidance of hospitalization, is particularly short-sighted. Such discrimination also reinforces the disinclination of primary care physicians to make psychiatric diagnoses and encourages their often fruitless treatment of depressive symptoms while ignoring the root disorder. Finally, inadequate reimbursement seriously limits the availability of psychiatrists skilled in geriatrics.
RESEARCH AND THE FUTURE
Research advances promise major improvements in treatment of depression in the elderly. Attempts to predict the future direction of such treatment, however, are fraught with difficulty because the most important developments in treatment are likely to occur not in targeted areas but from unanticipated consequences of basic research. The prospects of unanticipated consequences of research on depression are good, and they are getting better.
Studies of Alzheimer's disease have already established a genetic basis for some instances of that disorder and have begun to elucidate patterns of transmission. The rapid development of molecular genetics gives hope that one day the genetic basis of Alzheimer's disease will be understood and an effective therapy will be available. Another
important research area is that of the newer imaging techniques, which provide extraordinary views of brain structure and function. These techniques range from computerized tomography that provides increasingly detailed pictures of brain structure to electrical assessment of brain physiology and fine-grained analyses of brain metabolism provided by positron emission tomography and magnetic resonance imaging. Finally, continuing progress in understanding the biochemistry of neurotransmitters and neuromodulators will inevitably pay dividends in improved diagnosis and treatment.
RECOMMENDATIONS
Services
Insurance Providers (Governmental and Private)
Despite the recent removal of the Medicare limitation on outpatient care, inadequate reimbursement for psychiatric care in both the public and private sectors contributes to the (mis)diagnosis of depression as physical illness and, as a consequence, inadequate treatment. The committee's major service recommendation is the removal of discriminatory limitations of reimbursement for psychiatric care. Removal of the Medicare cap should be accompanied by reduction of the 50 percent copayment required for "psychiatric" treatment to the 20 percent copayment now required for "medical" treatment.
Clinicians (Particularly Primary Care Physicians)
The following recommendations are directed toward clinicians whose practice includes the elderly.
-
New patients and, periodically, old patients should be screened for the presence of emotional disturbance (particularly depression), using, for example, either the Beck Depression Inventory3 or the Geriatric Depression Scale,71 and for the presence of related cognitive dysfunction using the Mini-Mental State Examination.20
-
Psychosocial and environmental stressors in the patient's life should be identified. Grief and bereavement are probably the most powerful external threats to emotional well-being but the clinician should assess all of the risk factors for depression noted earlier in this chapter.
-
The bereaved or grieving patient should be encouraged to establish at least one intimate, confiding relationship. The primary
-
care physician is ideally placed to assist in this effort, which may include mobilization of friends and relatives, referral to senior adult programs, and, if necessary, referral for supportive psychotherapy during the period of acute loss.
-
The person about to retire should be encouraged to plan carefully. Social workers, occupational therapists, and career counselors may be quite helpful in locating skilled volunteer work, part-time employment, and structured recreational activities.
-
The extent of loss in the functionally impaired patient should be assessed. Auditory and visual function should be evaluated and corrected to the extent possible with hearing aids and glasses; cataracts and glaucoma should be treated. Physical and occupational therapies can be helpful in compensating at least partially for disability resulting from medical, orthopedic, and neurologic disorders.
Persons Over the Age of 50
Elderly individuals should recognize that depression and cognitive dysfunction are pathological and not a normal result of the aging process. They should be encouraged to seek out and participate in activities designed to prevent withdrawal and social isolation. The essential ingredient of these activities is that they be meaningful.
Research
-
The committee's major recommendation in this area is to increase financial support for research on depression in the elderly. This support should be directed to two agencies: the Program on Mental Health of the Aging in the National Institute of Mental Health (its $47 million research budget on the aging currently funds only 25 percent of the grants that are approved on the basis of scientific merit) and the National Institute on Aging, which should pursue research on depression secondary to physical illness and medication.
-
Diagnostic criteria for depression in the elderly and instruments (including structured interviews) for their application should be developed and assessed. These instruments should then be used to determine the prevalence, incidence, costs, and symptom severity of depression in elderly populations, including the institutionalized, the medically ill, and community samples stratified according to socioeconomic status.
-
A practicable case-finding package (that includes depression and dysphoria) should be developed for high-risk groups. It should be used to extend prevalence and cost studies to such high-risk groups
-
as persons over the age of 85, elderly persons living alone, persons who have recently changed their dwelling, widows and widowers, and persons who have recently been discharged from the hospital.65
-
Studies should be conducted to compare treatment costs for depressed elderly persons in nursing homes with costs for matched, depressed elderly persons in the community.
-
Criteria should be developed for evaluation and treatment of older adults with psychiatric disorders to improve the quality of care and encourage third parties to assume broader coverage of these disorders.
-
Treatment strategies directed toward nonresponse, recurrence, and relapse should be pursued. Studies should include an examination of innovative, nontraditional treatments and the development of protocols for continuation of treatment and maintenance following treatment.
-
Small-scale pilot studies of intervention efficiency should be carried out, using cost-effectiveness analyses to evaluate resource utilization, economic costs, and utility (perceived value).
-
The efficacy and safety of electroconvulsive therapy should be assessed and the indications for its use in the elderly determined.
-
Studies should be conducted on innovative psychosocial measures (particularly in the community) designed to restore and preserve morale during stressful periods such as bereavement.
-
The pharmaceutical industry should conduct controlled trials of antidepressants in the elderly to determine their efficacy, safety, and indications.
Education
The committee's major recommendation regarding education is to develop programs to train physicians to detect and treat mental disorders, including depression, in the elderly. In addition, older persons should be informed that depression is an illness that can be successfully treated and that it may occur in the absence of a depressive mood. Information is best conveyed in settings such as senior centers and before the onset of symptoms.
REFERENCES
1. American Institute for Research. Senior actualization and growth explorations: A geriatric human potential program. Innovations 1977; 4:11-18.
2. Barraclough, B., Bunch, J., Nelson, B., and Sainsbury, P. A hundred cases of suicide: Clinical observations. British Journal of Psychiatry 1974; 125:355-373.
3. Beck, A. T., Ward, C. H., Mendelson, M., et al. An inventory for measuring depression. Archives of General Psychiatry 1961; C:561-571.
4. Berkman, L. F., Berkman, C. S., Casl, S., Freeman, D. H., Leo, L., et al. Depressive symptoms in relation to physical health and functioning in the elderly. American Journal of Epidemiology 1986; 124:372-388.
5. Blazer, D. G., Hughes, D., and George, L. K. The epidemiology of depression in an elderly community population. The Gerontologist 1987; 27:281-287.
6. Blazer, D. G. Depression in Late Life. St. Louis: C. V. Mosby, 1982.
7. Blazer, D. G. The epidemiology of late life depression and dementia: A comparative study. In: A. Tasman (ed.), The Annual Review of Psychiatry, vol. 9 . Washington, D.C.: American Psychiatric Press, 1990, pp. 210-219.
8. Blazer, D. G., and Maddox, G. Using epidemiology survey data to plan geriatric mental health services. Hospital and Community Psychiatry 1982; 33:42-45.
9. Blazer, D. G., and Williams, C. D. Epidemiology of dysphoria and depression in an elderly population. American Journal of Psychiatry 1980; 137:439-444.
10. Borson, S., Barnes, R. A., Kukull, W. A., Okimoto, J. T., Veith, R. C., et al. Symptomatic depression in elderly medical outpatients. I . Prevalence, demography and health service utilization. Journal of the American Geriatrics Society 1986; 34:341-347.
11. Busse, E. W., and Simpson, D. Depression and antidepressants and the elderly. Journal of Clinical Psychiatry 1983; 44(5):35-39.
12. Butler, R. N., and Lewis, M. I. Love and Sex After Sixty. New York: Harper & Row, 1988.
13. Cassel, W. A., Smith, C. M., Grunberg, F., Boan, J. A., and Thomas, R. F. Comparing costs of hospital and community care. Hospital and Community Psychiatry 1972; 23:197-200.
14. Diehr, P., Williams, S. J., Martin, D. P., and Price, K. Ambulatory health services utilization in three provider plans. Medical Care 1984; 22:1-13.
15. Endicott, J., Herz, M. I., and Gibbon, M. Brief vs. standard hospitalization: The differential costs. American Journal of Psychiatry 1978; 135:707-712.
16. Ernst, P., Badash, D., Beran, B., et al. Incidence of mental illness in the aged: Unmasking the effects of diagnosis of chronic brain syndrome. Journal of the American Geriatrics Society 1977; 8:371-375.
17. Fawcett, J. Suicidal depression and physical illness. Journal of the American Medical Association 1972; 219:1303-1306.
18. Fogel, B. S. Electroconvulsive therapy in the elderly: A clinical research agenda. International Journal of Geriatric Psychiatry 1988; 3:181-190.
19. Fogel, B. S., and Fretwell, M. Reclassificiation of depression among the medically ill elderly. Journal of the American Geriatrics Society 1985; 33:446-448.
20. Folstein, M. F., Folstein, S. E., and McHugh, P. R. "Mini-mental state": A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research 1975; 12:189-198.
21. Ford, D. E., and Kamerow, D. B. Epidemiologic study of sleep disturbances and psychiatric disorders. Journal of the American Medical Society 1989; 262:1479-1484.
22. Fowles, D. G. A Profile of Older Americans, 1987. Washington, D.C.: American Association of Retired Persons, 1988.
23. Gask, L., Goldberg, D., Lesser, A. L., and Millar, T. Improving the psychiatric skills of the general practice trainee: An evaluation of a group training course. Medical Education 1988; 22(2):732-738.
24. Georgotas, A., McCue, R. E., Hapworth, W., Friedman, E., Kim, O.M., Welkowitz, J., Chang, I., and Cooper, T. B. Comparative efficacy and safety of MAOIs versus TCAs in treating depression in the elderly. Biological Psychiatry 1986; 21:1155-1166.
25. German, P. S., Shapiro, S., Skinner, E. A., Von Korff, M., Klein, L. E., Turner, R. W., Teitelbaum, M. L., Burke, J., and Burns, B. J. Detection and management of mental health problems of older patients by primary care providers. Journal of the American Medical Association 1987; 257:489-493.
26. Goldman, H., Feder, J., and Scanlon, W. Chronic mental patients in nursing homes: Reexamining data from the National Nursing Home Study. Hospital and Community Psychiatry 1986; 37:269-272.
27. Goodwin, F. K. Drug treatment of affective disorders: General principles. In: M. E. Jarvik, (ed.), Psychopharmacology in the Practice of Medicine. New York: Appleton-Century-Crofts, 1976, pp. 241-253.
28. Gottlieb, G. L. Optimizing mental function of the elderly. In: R. Lavizzo-Mourey, S. C. Day, D. Diserens, and J. A. Grisso, Practicing Prevention for the Elderly. Philadelphia: Hanley and Bellfus, Inc., 1988, pp. 153-166.
29. Gottlieb, G. L. Cost implications of depression in older adults. International Journal of Geriatric Psychiatry 1988; 3:191-200.
30. Gottlieb, G. L. Financial issues affecting geriatric psychiatric care. In: L. Lazarus, L. Jarvik, et al. (eds.), Essentials of Geriatric Psychiatry. New York: Springer, 1988, pp. 230-248.
31. Guze, S., and Robins, E. Suicide and primary affective disorders. British Journal of Psychiatry 1970; 117:437-438.
32. Harwood, H. J., Napolitano, D. M., Kristiansen, P. L., and Collins, J. J. Economic costs to society of alcohol and drug abuse and mental illness: 1980. Research Triangle Park, N.C.: Research Triangle Institute, 1984.
33. Harwood, H. J., and Turner, H. B. Social dimensions of mental illness among rural elderly populations. International Journal of Aging and Human Development 1988; 26(3):169-190.
34. Holder, H. D. Alcoholism treatment and potential cost saving. Medical Care 1987; 25:52-71.
35. Hu, T., Huang, L., and Cartwright, W. S. Evaluation of the costs of caring for senile demented elderly: A pilot study. Gerontologist 1986; 26:158-163.
36. Jacobson, A. Melancholy in the 20th century: Causes and prevention. Journal of Psychiatric Nursing and Mental Health Services 1980; 18:11-21.
37. Jarvik, L. F., and Gerson, S. Outcome of drug treatment in depressed patients over the age of 50. In: C. A. Shamoian (ed.), Treatment of Affective Disorders in the Elderly. Washington, D.C.: American Psychiatric Press, Inc., 1985, pp. 29-36.
38. Kemp, B. J., Staples, F., and Lopez-Acqueres, W. Epidemiology of depression and dysphoria in an elderly Hispanic population. Journal of the American Geriatrics Society 1987; 35:920-926.
39. Khuri, K., and Akiskal, H. S. Suicide prevention: The necessity of treating contributing psychiatric disorders. Psychiatric Clinics of North America 1983; 6:193-207.
40. Koenig, H. G., Meador, K. G., Cohen, H. J., and Blazer, D. G. Depression in elderly hospitalized patients with medical illness. Archives of Gerontological Medicine 1988; 148:1929-1936.
41. Lehman, H. E. Affective disorders in the aged. Psychiatric Clinics of North America 1982; 5:27-44.
42. Levitan, S. J., and Kornfeld, D. S. Clinical and cost benefits of liaison psychiatry. American Journal of Psychiatry 1981; 138(6):790-793.
43. Luckey, J. W. Cost savings of alcohol treatment. Alcohol, Health and Research World 1987; 12(1):8-15.
44. McCaffree, K. M. The cost of mental health care under changing treatment methods. American Journal of Public Health 1966; 556:1013-1025.
45. Meyers, B. S., Greenberg, R., and Mei-Tal, V. Delusional depression in the elderly. In: C. A. Shamoian (ed.), Treatment of Affective Disorders in the Elderly. Washington, D.C.: American Psychiatric Press, 1985, pp. 17-28.
46. Munoz, R. F., Glish, M., Soo-Hoo, T., and Robertson, J. The San Francisco mood survey project: Preliminary work toward the prevention of depression. American Journal of Community Psychology 1982; 10:317-329.
47. Mumford, E., Schlesinger, H. J., Glass, G. V., et al. A new look at evidence about reduced cost of medical utilization following mental health treatment. American Journal of Psychiatry 1984; 141:1145-1158.
48. Murrell, S. A., Himmelfarb, S., and Wright, K. Prevalence of depression and its correlates in older adults. American Journal of Epidemiology 1983; 2(117):173.
49. Myers, J. K., Weissman, M. M., Tischler, G. L., et al. Six month prevalence of psychiatric disorders in three communities. Archives of General Psychiatry 1984; 41:959-967.
50. Nielsson, L. V., and Persson, G. Prevalence of mental disorders in an urban sample examined at 70, 75 and 79 years of age. Acta Psychiatrica Scandinavica 1984; 69:519-527.
51. Parmelee, P. A., Katz, I. R., and Lawton, M. P. Depression among institutionalized aged. Assessment and prevalence estimation. Journal of Gerontology: Medical Sciences 1989; 44:1722-1729.
52. Raphael, B. Preventive intervention with the recently bereaved. Archives of General Psychiatry 1977; 34:1450-1454.
53. Reifler, B. V., Larson, E., and Hanley, R. Coexistence of cognitive impairment and depression in geriatric outpatients. American Journal of Psychiatry 1982; 139:623-626.
54. Reynolds, C. F., Kupfer, D. J., Taska, L. S., Hoch, C. C., et al. EEG sleep in elderly depressed, demented, and healthy subjects. Society of Biological Psychiatry 1985: 20:431-442.
55. Robins, E. Suicide. In: H. Kaplan and B. J. Sadock (eds.), Comprehensive Textbook of Psychiatry, 4th ed., vol. 2. Baltimore, Md.: Williams & Wilkins, 1985, p. 1313.
56. Robins, E., Gasner, S., Kayes, J., et al. The communication of suicidal intent: A study of 134 consecutive cases of successful (completed) suicide. American Journal of Psychiatry 1959; 115:724-733.
57. Smyer, M. A., Davies, B. W., and Cohn, M. A prevention approach to critical life events of the elderly. Journal of Primary Prevention 1982; 2:195-204.
58. Stewart, A. L., Greenfield, S., Hays, R. D., Wells, K., Rogers, W. H., Berry, S. D., McGlynn, E. A., and Ware, J. E., Jr. Functional status and well-being of patients with chronic conditions: Results from the Medical Outcomes Study. Journal of the American Medical Association 1989; 262:907-913.
59. Stoudemire, A., Frank, R., Hedemark, N., Kamlet, M., and Blazer, D. The economic burden of depression. General Hospital Psychiatry 1986; 8:387-394.
60. U.S. Bureau of the Census. Statistical Abstract of the United States, 1989 (109th ed.). Deaths and Death Rates, by Selected Causes: 1970-1986 (Table No. 117). Washington, D.C., 1989.
61. Veith, R. C. Cardiovascular effects of the antidepressants: Treating the elderly patient. In: C. A. Shamoian (ed.), Treatment of Affective Disorders
in the Elderly. Washington, D.C.: American Psychiatric Press, 1985, pp. 37-50.
62. Vital Statistics of the United States. Suicide rates in the United States by age, sex and color, 1975. Washington, D.C.: Mortality Statistics Branch, National Center for Health Statistics.
63. Wasylenki, D. Depression in the elderly. Canadian Medical Association Journal 1980; 122:525-532.
64. Waxman, H. M., and Carner, E. A. Physicians' recognition, diagnosis and treatment of mental disorder in elderly medical patients. Gerontologist 1984; 24:593-597.
65. Waxman, H. M., Carner, E. A., and Klein, M. Underutilization of mental health professionals by community elderly . Gerontologist 1984; 24:23-30.
66. Weiner, R. D. Does electroconvulsive therapy cause brain damage? Behavioral and Brain Sciences 1984; 7:1-53.
67. Weissman, M. M., Meyers, J. K., Tischler, G. L., Holzer, C. E., Leaf, P. J., et al. Psychiatric disorders (DSM-III) and cognitive impairment among the elderly in a U.S. urban community. Acta Psychiatrica Scandinavica 1985; 71:366-379.
68. Wells, K. S., Stewart, A. L., Hays, R. D., Burman, M. A., Rogers, W. H., Daniels, M., Berry, A. D., Greenfield, S., and Ware, J. E., Jr. The functioning and well-being of depressed patients: Results from the Medical Outcomes Study. Journal of the American Medical Association 1989; 262:914-919.
69. Williamson, J. Screening, surveillance and case-finding. In: T. Arie (ed.), Health Care of the Elderly. London: Croom Helm, 1981.
70. Wragg, R. E., and Jeste, D. V. Overview of depression and psychosis in Alzheimer's disease. American Journal of Psychiatry 1989; 146:577-587.
71. Yesavage, J. A., Brink, T. L., Rose, T. L., et al. Development and validation of a geriatric depression screening scale: A preliminary report. Journal of Psychiatric Research 1983; 17:37-49.






















