6
Osteoporosis
Osteoporosis involves bone loss from the skeleton that leads to reduced bone strength and an increased likelihood of fractures. A variety of processes cause bone loss, which may progress silently for decades until fractures occur late in life. Strictly speaking, osteoporosis ("porous bone") is a histological diagnosis wherein the bone tissue is relatively normal but there is too little of it. Clinically, osteoporosis is heralded by the occurrence of characteristic fractures or, prior to the onset of fractures, by reduced bone mineral density as assessed by noninvasive techniques. Although some confusion results from the use of these different definitions, the condition is indisputably a common one. An estimated 20 to 25 million Americans are at increased risk for fracture by virtue of low bone density, and more than a million fractures in the United States each year are attributable to osteoporosis. Many of these fractures result in disability or death; together, they cost the nation an estimated $7 to $10 billion annually, costs that will rise in the future as the population ages. Some of these fractures can be prevented by reducing bone loss, but methods for accomplishing such reductions have not been systematically applied. This chapter summarizes present knowledge concerning the pathophysiology of osteoporosis and reviews evidence regarding the efficacy of potential interventions. On the basis of this information, recommendations are made that should lead to a reduction in the disability produced by this important disorder of older Americans.
BURDEN OF OSTEOPOROSIS AND FRACTURES
Osteoporosis may affect the entire skeleton but, with the exception of tooth loss and ill-fitting dentures related to bone loss in the oral cavity,20 fractures constitute the only important adverse health consequence of this disorder. However, the medical and social consequences of these age-related fractures make osteoporosis a significant public health problem. Table 6-1 indicates some of the dimensions of this problem.
Morbidity
The fractures linked to osteoporosis occur at many skeletal sites because bone loss is widespread, but proximal femur (hip) fractures, distal forearm (wrist or Colles') fractures, and vertebral (spine) fractures are the most important types. Each year in the United States there may be up to a quarter of a million each of hip fractures and wrist fractures and perhaps twice that number of vertebral fractures.27 More precise figures are difficult to obtain—hip fracture victims are generally hospitalized, but hospital discharge data also count readmissions for additional care. Most other fractures, including the majority of wrist and spine fractures, are treated on an outpatient basis, but outpatient data are not routinely collected. This lack of accurate data on fracture occurrence nationally is an impediment to the design and implementation of an effective control program. Some steps to improve this situation were outlined in a 1985 National Research Council/Institute of Medicine report entitled Injury in America;
TABLE 6-1 Impact of Fractures in the United States
|
Consequence |
Hip Fracture |
Wrist Fracture |
Spine Fracture |
|
Excess mortality |
12% |
None |
None |
|
Morbidity |
|
|
|
|
Lifetime risk |
|
|
|
|
Males |
5% |
2% |
? |
|
Females |
15% |
15% |
35% |
|
Cases per year (approximate) |
250,000 |
240,000 |
500,000 |
|
Disability |
+++a |
+ |
++ |
|
Cost (1984) All fracture sites combined = $18 billion |
|||
|
a Indicates relative impact. |
|||
they include the establishment of an injury surveillance system with more accurate identification of specific injuries and their causes.
Nevertheless, it is clear that fractures are quite common and that osteoporosis is responsible for a substantial portion of them, a figure currently estimated at more than 1.3 million fractures annually.35 The significance of these numbers is better grasped by noting that the lifetime risk of a hip fracture, 15 percent in white women and 5 percent in men,5 is equivalent to the combined lifetime risk of developing breast, uterine, or ovarian cancer in women and about the same as the lifetime risk of prostate cancer in men. These fractures increase dramatically in incidence with aging, and, at any age, rates are greater for women than for men (Figure 6-1). Based on the few data available, the same general pattern applies to nonwhite populations, but rates for these groups are lower.27
Mortality
The fractures associated with osteoporosis may, in turn, lead to substantial disability and, in the case of hip fractures, even death. Hip fractures lead to an overall 5 to 20 percent reduction in expected survival.5 The excess mortality may be seen for up to six months following the fracture and varies with age and sex (there appear to be no detailed data concerning the influence of race). For example, about 90 percent of hip fracture victims under 75 years of age are still alive one year later (92 percent of those expected to be alive), compared with only 73 percent (83 percent of expected) of those aged 75 years and older at the time of their fracture.27 Despite their greater average age when fractures occur, survival is better among women, 83 percent of whom are still alive one year after the fracture, compared with only 63 percent of men. Survival is mediated primarily by coexisting serious illnesses24 but, after the first six months, is about as expected for persons of comparable age and sex in the general population. Still, hip fractures are associated with many deaths and are partly responsible for the fact that falls are the leading cause of accidental death among men and women aged 75 years or older in the United States and the second leading cause among those aged 45 to 74 years. In contrast, wrist fractures and osteoporotic spine fractures cause no increase in mortality.27
Disability
A substantial minority of hip fracture patients are nonambulatory or dependent even before the fracture. However, the devastating
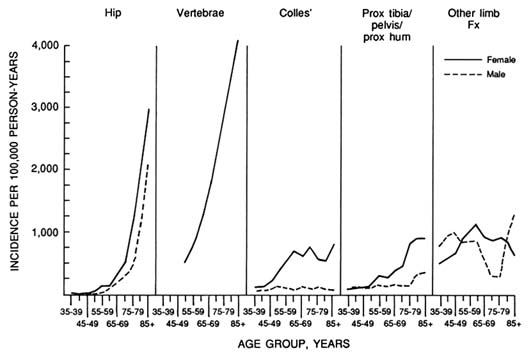
FIGURE 6-1 Age- and sex-specific incidence rates for various fractures among Rochester, Minnesota, residents. Source: L. J. Melton III and S. R. Cummings, ''Heterogeneity of Age-related Fractures: Implication for Epidemiology," Bone and Mineral, Vol. 2, pp. 321-331, 1987. Elsevier Science Publishers, used with permission.
impact of this injury on the remainder cannot be denied. Of those able to walk before sustaining a hip fracture, for example, half cannot walk independently afterward.30 The ability of such patients to get about and care for themselves is obviously compromised and their quality of life considerably reduced. Indeed, poor ambulation is one of the strongest predictors of nursing home admission,4,10 along with the absence of caretakers in the home.4 In addition to their preexisting medical problems, hip fracture survivors often develop other complications such as pressure sores, pneumonia, urinary tract infections, and arrhythmias, which add to the problems of rehabilitation posed by the fracture itself. Also, depression, common in these individuals, may be exacerbated by the fracture and subsequent hospitalization.31 Ultimately, up to one-third of hip fracture victims may be totally dependent.16 As a result of these factors, the risk of institutionalization is great. More than 60,000 nursing home admissions have been attributed to hip fractures annually,36 along with more than 7 million restricted activity days (62.5 days per episode) among noninstitutionalized individuals in the United States each year.14 As many as 8 percent of all nursing home residents have had a hip fracture.14
Functional recovery after a hip fracture is predicted by prefracture independence (in terms of mobility and performing the activities of daily living), mental impairment (dementia and psychosis as well as confusion during hospitalization), depression, and surgical result, among others.4,31,33 There is indirect evidence, however, that these factors can be manipulated to alter recovery outcomes. When, as a result of introducing the prospective payment system, the average duration of hospitalization for hip fracture in one large community hospital fell from 21.9 to 12.6 days, the proportion of patients who remained in nursing homes one year later rose from 9 percent to 33 percent.10 This change was accompanied by a decline in the number of physical therapy sessions and a reduction in the distance patients could walk prior to discharge. Health maintenance organization (HMO) enrollees in the same system, however, performed even less well by these measures yet were only half as likely to be in a nursing home at the end of the year. Moreover, early discharge has been associated with a high level of return to pre-injury independence in selected patients when a program of home rehabilitation is employed.38 There are several uncontrolled studies such as this that provide tantalizing evidence that an organized program of rehabilitation might yield impressive gains in functioning following a hip fracture. Delineation of an optimal program and its test by clinical trial is an urgent priority.
Despite the fact that only one-fifth of patients with wrist fractures are hospitalized, they account for 48,000 hospital admissions and a further 422,000 physician office visits by persons 45 years of age or older in the United States each year.14 Distal forearm fractures also lead to more than 6 million restricted activity days annually but have generally been considered free of long-term disability. Yet more recent reviews show that persistent pain, loss of function (diminished range of motion or strength), neuropathies, and posttraumatic arthritis are quite common.8,9 One-fifth to one-third of wrist fracture patients have a fair to poor functional result,8 but it is not known whether this leads to any particular handicap. The main risk factors for poor outcome are the severity of the original injury and the adequacy of fracture reduction.
Patients with collapse fractures of the vertebrae often present in considerable pain, but the more common types of spine fractures (anterior wedging and vertebral endplate fractures) may occur gradually and be diagnosed only incidentally on a chest x-ray taken for another purpose.27 Because atraumatic vertebral fractures do not require reduction and almost never lead to spinal cord injury, only a minority of patients are medically attended. Still, vertebral fractures in patients aged 45 years or older account for 52,000 hospital admissions and 161,000 physician office visits each year, as well as more than 5 million restricted activity days.14 Although it is generally understood that these fractures may lead to progressive loss of height, kyphosis, posture changes, and persistent pain that interferes with activities of daily living,46 neither acute nor chronic disabilities associated with vertebral fractures have ever been assessed in a systematic way. This unsatisfactory situation should be corrected as soon as possible.
Costs
The total cost of fractures may be as much as $18 billion per year, and osteoporosis accounts for at least a third of this total,14 estimated most recently at $7 to $10 billion annually.35 Because most of these fractures occur in elderly individuals, wages foregone or years of life lost are not the primary determinants of cost. Rather, the important expenses are for inpatient and outpatient medical services and for nursing home care. In 1986 these direct costs included an estimated 322,000 hospitalizations and almost 4 million hospital days for women aged 45 and older for whom osteoporosis-related conditions were the primary cause of admission; more than half of the total was for hip fractures.36 Osteoporosis was a contributing cause of admission in an additional 170,000 hospitalizations
for an extra 290,000 hospital days. In women of this age, there were 2.3 million physician visits for osteoporosis in 1986. At each visit, one-third of the women needed an x-ray, one-fourth required physiotherapy, and most received a prescribed medication for the condition. There were also an estimated 83,000 nursing home stays for osteoporosis-related causes in 1986, with an average duration of stay of one year. Altogether, these direct costs of osteoporosis totaled $5.2 billion for women alone, of which $2.8 billion were for inpatient services and $2.1 billion were for nursing home care.36
Such costs can only rise in the future because the elderly population is growing rapidly. Between 1988 and 2050, the actual number of individuals aged 65 and older will increase from 30 to 67 million in the United States.5 Because the incidence of osteoporosis-related fractures rises with age, this growth in the elderly population will eventually result in a doubling or tripling of the number of hip fractures seen each year, with increases for the other fracture sites as well. It is projected that in only 30 years' time, there could be almost 350,000 hip fractures each year in the United States at an annual cost estimated to be between $31 and $62 billion.7 This alarming situation can be at least partially avoided if methods to preserve bone mass can be refined and exploited for the entire population, young and old.
DETERMINANTS OF FRACTURES
The risk of fracture in any given situation depends on the degree of trauma experienced and the ability of the skeleton to resist such forces. Bone density in the skeleton can decline to such a point that fractures occur spontaneously, and violent accidents can impose loads capable of breaking any bone. Usually, however, both skeletal integrity and trauma are important. For example, the risk of falling (and particularly of falling heavily) generally increases with age, whereas bone strength diminishes. As a consequence, fracture incidence rises dramatically (especially for hip fractures for which the age-related increase is exponential), and the amount of trauma required to produce a fracture declines.27 Although the occurrence of a fracture is a complex event (Figure 6-2), interventions are usually directed either at bone mass or trauma, and risk factors should be considered in that light.
Bone Mass
The skeleton is constantly being renewed through a linked process of bone resorption and bone formation.34 In young adults,
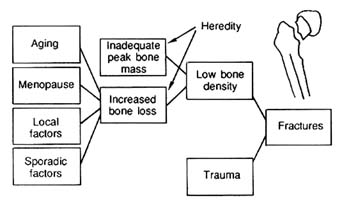
FIGURE 6-2 Conceptual model of the pathogenesis of fractures related to osteoporosis. Source: Modified from B. L. Riggs, "Osteoporosis" in Cecil Textbook of Medicine, J. B. Wyngaarden and L. H. Smith, eds., 18th ed., W. B. Saunders, Philadelphia, Pa., 1988, pp. 1510-1515. Reprinted with permission.
the two processes are closely coupled so that bone mass remains stable until the early to middle thirties. With aging, however, bone formation does not keep pace with resorption, and bone mass gradually diminishes. Over the course of their life, women may lose a third of their original cortical (or compact) bone, which forms the shafts of limb bones and constitutes up to 80 percent of the skeleton.43 They may lose half of their trabecular (or cancellous) bone, which accounts for the remaining 20 percent and makes up the ends of the limb bones and most of the spine, pelvis, and other flat bones of the skeleton. Men lose about two-thirds of these amounts. This bone loss is the result of (1) age-related endogenous factors that occur universally in the population and account for the slow bone loss that occurs over life in both sexes; (2) an accelerated phase of bone loss associated with menopause in women and hypogonadism in a small number of men; and (3) factors that occur sporadically in the population and, when present, increase the rate of bone loss (e.g., certain medical and surgical diseases that produce "secondary" osteoporosis).43
This decline in bone mineral density (a pathogenic trait) leads to a disproportionately greater decrease in bone strength (asymptomatic disease) and to an increase in symptomatic disease (i.e., fractures). Because there are no symptoms until fractures occur, relatively few people are diagnosed in time for effective therapy to be administered, even though bone mineral density can be accurately assessed in vivo as a measure of fracture risk (see the appendix to this chapter). Population-based studies demonstrate a gradient of continuously increasing hip fracture incidence associated with declining bone
mineral density in the proximal femur, rising wrist fracture incidence with decreasing bone mass in the radius, and increasing vertebral fracture incidence and prevalence with falling bone density in the spine.17 Several prospective studies show, in addition, that bone mass measurements predict the risk of fractures generally.15,49 Altogether, roughly 20 to 25 million individuals in the United States have sufficiently low bone density that they are at increased risk of fracture.35
Although bone mineral density accounts for most of the ultimate strength of bone tissue,26 other skeletal factors may be important as well. Biomechanically, the body compensates for age-related bone loss by an increase in the diameter of limb bones, which raises their resistance to bending and twisting. However, this compensatory process is less marked at the ends of limb bones or in the vertebrae, sites at which the fractures associated with osteoporosis typically occur. Strength may also be compromised by age-related increases in the fragility of bone tissue.26 Although bone architecture and bone quality are important determinants of bone strength, neither can be accurately assessed by noninvasive means for use in risk prediction, and neither can be intentionally altered by a specific therapy. Consequently, they are not considered further.
Trauma
Some fractures are spontaneous, whereas others (especially vertebral fractures) result from everyday activities. Most of the fractures related to osteoporosis, however, occur in conjunction with falls. Falling increases the chance of fracture at any given level of bone mass, as does the inability to dissipate the kinetic energy produced by a fall.26 The annual risk of falling rises with age, from about one of five women aged 60 to 64 to one in three aged 80 to 84,6 but only about 5 to 6 percent of falls lead to a fracture of any kind, and only 1 percent lead to a hip fracture.11
The pathophysiology of falling is not well understood, and many of the risk factors that have been recognized, such as gait and balance disorders, diminished reflexes and strength, or reduced vision,48 are difficult to correct. Once bone mass has fallen to such a point that fractures begin to occur, however, there are few other therapeutic options than to try to prevent falls. Among elderly women, for example, who have lost most of the bone they will lose over life and who may have bone density so low that they are at high risk of fracture, the emphasis in prevention has to be on falling. Therefore, programs to reduce the fractures associated with osteoporosis must
also include attempts to lower the frequency and severity of falls (see Chapter 15).
PREVENTABILITY OF OSTEOPOROSIS
The bone mass a person has in later life is determined by the peak bone mass achieved in young adulthood and by the subsequent rate of bone loss. Peak bone mass has a strong genetic component because skeletal size is heritable; it would not be surprising if bone loss had a similar genetic element, but this has not been described. Neither peak bone mass nor subsequent bone loss are obviously affected by traditional environmental factors like sanitation or pollution, although fractures are influenced by environmental hazards that induce falls. Instead, host factors are predominant. Endogenous factors such as age, sex, and the effects of specific diseases are considered to be important, and attention has also focused on certain behaviors, including diet, exercise, and smoking. Present knowledge relates these factors mostly to bone mass or fracture risk. How they might influence rehabilitation and health outcomes has been little studied.
Peak Bone Mass
The factors that influence peak adult bone mass are not well described. In general, however, white women have lighter skeletons than white men or black women, whereas black men have the heaviest skeletons.43 The skeletons of Asians appear to be intermediate between those of blacks and whites. In all three races, women have lower peak bone mass than men. Because initial bone mass is an important determinant of bone mass later in life, these differences may partially explain observed racial and sexual differences in the incidence of osteoporosis and fractures. However, such generalizations should not obscure the fact that some whites have high bone mass, whereas individual nonwhites may have low bone mass and fractures. Moreover, there seem to be exceptions to the general pattern: Hispanics appear to have hip fracture rates that are even lower than American blacks,45 whereas the Bantu people of South Africa have extremely low fracture rates but also low bone mass.27 These observations highlight the need to delineate the factors that determine peak bone mass and to better quantify the effect of peak bone mass on fracture risk at older ages. Because no intervention regarding peak bone mass is possible at age 50, however, emphasis in this report must be placed on the risk factors for bone loss.
Hypogonadal Bone Loss
Estrogen deficiency at menopause is an important cause of bone loss and subsequent fractures. Perimenopausal women experience an accelerated phase of bone loss lasting five years or more that accounts for a substantial proportion of their lifetime bone loss.43 This accelerated phase is associated with a high rate of bone turnover (there is an increase in bone formation but an even greater increase in bone resorption) that can be prevented by estrogen replacement therapy (ERT). Men do not undergo the equivalent of menopause, but gonadal function does decrease in some elderly men, and overt male hypogonadism often is associated with vertebral fractures.28
A large number of trials have compared estrogens with placebos and other treatments to determine their effect on bone mass, and nearly all indicate that estrogens are more effective in maintaining bone mass.17 For example, in one randomized controlled trial of three groups of women followed from six weeks, three years, or six years after oophorectomy, estrogen significantly retarded bone loss for as long as prescribed but at least ten years.22 Recent data suggest that ERT may be effective in slowing bone loss up to the age of 70.39 Because the effect of treatment is to reduce bone resorption, however, postmenopausal ERT can slow bone loss, but it cannot restore the biomechanical competence of the skeleton to normal once a substantial amount of bone has been lost.34 Because lost bone is essentially irreplaceable, emphasis in women 50 to 69 years of age must be on preserving existing bone mass. Greater benefits are achieved with earlier treatment because bone mass is maintained at a higher level.
Estrogens also appear to be effective in preventing fractures. One randomized controlled trial showed that only 4 percent of oophorectomized women on ERT lost height compared with 38 percent of women who were not being treated; almost 90 percent of the latter group with height loss had evidence of vertebral fractures.23 Although randomized trials of ERT for prevention of hip fracture are less feasible owing to the long delay between menopause and the typical age at which these fractures occur, case-control studies consistently show about a 50 percent reduction in hip and Colles' fractures with long-term ERT.17
To intervene by preserving bone density before irreversible bone loss has occurred, patients must be stratified on the basis of fracture risk so that high-risk individuals can be identified. The bone density of any specific individual cannot be determined without direct measurement.17 A variety of noninvasive bone mass measurement techniques can be used (Table 6-2), including single-photon absorptiometry
TABLE 6-2 Comparison of Bone Densitometry Techniques
|
Techniquea |
Site |
Relative Sensitivity (%) |
Precision (%) |
Duration of Accuracy (minutes) |
Absorbed Examination (milligrams) |
Dose |
Cost ($) |
|
Standard technique |
|||||||
|
SPA |
Proximal radius |
1X |
2–3 |
5 |
15 |
10 |
75 |
|
DPA |
Spine, hip |
2X |
2–4 |
4–10 |
20–40 |
5 |
100–150 |
|
QCT |
Spine |
3–4X |
2–5 |
5–20 |
10–20 |
100–1,000 |
100–200 |
|
Newer developments |
|||||||
|
SPA-R |
Distal radius, calcaneus |
2X |
1–2 |
5 |
10–20 |
5–10 |
50b |
|
DEXA |
Spine, hip |
2X |
1–2 |
3–5 |
5 |
1–3 |
75b |
|
QCT-A |
Spine, hip |
3–4X |
1–2 |
5–10 |
10 |
100–300 |
100b |
|
a SPA = single-photon absorptiometry; SPA-R = rectilinear SPA; DPA = dual-photon absorptiometry, DEXA = DPA with a dual-energy x-ray source; QCT = quantitative computed tomography; QCT-A = QCT with advanced software and hardware capabilities. b Projected cost. Source: H. K. Genant, J. E. Block, P. Steiger, C. C. Glueer, B. Ettinger, and S. T. Harris, "Appropriate Use of Bone Densitometry," Radiology , Vol. 170, pp. 817-822, 1989. |
|||||||
(SPA), dual-photon absorptiometry (DPA), dual-energy x-ray absorptiometry (DEXA), and quantitative computed tomography (QCT), which are outlined in the appendix to this chapter. Because the range of bone mass at each age is great relative to the small accuracy error of measurement by any of these techniques, women with low, average, or high bone mass can be easily identified. These noninvasive tests are safe and well accepted by patients. Moreover, the accuracy of bone mass measurement compares favorably with that of many accepted clinical tests, including such screening tests as those for serum cholesterol.17 However, the efficacy of osteoporosis screening for preventing fractures has not been demonstrated directly, and no program has been endorsed.40
The level of bone mineral density at which treatment should be initiated for fracture prevention is another criterion that has not yet been determined.17 At present, this decision is made by individual physicians and patients; the absence of generally accepted guidelines for patient management further hinders the implementation of a population-wide mass screening program for osteoporosis. Nonetheless, Ross and colleagues44 modeled the savings that might result from treating 50-year-old white women with a regimen that slowed bone loss by 50 percent. They estimated that osteoporotic fractures could be reduced by one-third if the women in the lowest half of the bone mass distribution were all treated. Similarly, Cummings and colleagues7 calculated a 25 percent reduction in hip fractures in white women by the year 2020 if half of them accepted long-term estrogen use beginning at age 50; they estimated that the overall reduction in hip fractures would be less (18 percent) because men and nonwhite women would be unaffected by this strategy. Indeed, there is no current strategy for preventing osteoporosis in men and nonwhite women, even though they constitute a substantial proportion of all fracture victims.
Previous cost-effectiveness analyses showed little change in life expectancy but some improvement in quality-adjusted life with ERT in women aged 55 to 70 years with osteoporosis.50 The cost for each quality-adjusted year of life gained was $5,460 to $15,100 for women with a uterus (depending on whether endometrial biopsies were done periodically) and $3,250 for women without a uterus. These figures were said to be comparable to the benefits of treating moderate to severe high blood pressure. However, osteoporosis was defined in that study on the basis of vertebral fractures alone; consequently, the benefits were understated. By considering the risks of hip, wrist, pelvis, humerus, and spine fractures, along with the possible adverse effects of ERT on cancer risk and its potential beneficial effects on cardiovascular disease, Hillner and colleagues12 found that 15 years
of ERT in 50-year-old women were associated with an additional 0.67 quality-adjusted years of life. This benefit increased by 0.17 quality-years for each 10 percent decrease in fracture rates.
Despite data that consistently show a beneficial effect of estrogen on bone mass and fracture risk, only about 5 percent of post-menopausal women are on long-term ERT.17 The reluctance of physicians to prescribe and of women to comply with such therapy may be related to uncertainty regarding benefits and risks. Endometrial cancer is a concern18 unless progesterone is used concomitantly, but progesterone may negate the cardioprotective effects of unopposed estrogen.3 There is also the possibility of an increased incidence of breast cancer. Although such an increase appears to be small and has not been found in all studies, recent suggestions of a heightened risk of breast cancer following combined estrogen and progestin administration1 indicate a need for additional research to resolve this important question. On the other hand, almost all studies have found a decreased risk for cardiovascular disease in unopposed estrogen users,2,47 although no controlled clinical trials have been completed. Although the potential cardiovascular benefits of estrogen are likely to be greater than the benefits of fracture reduction, prevention of heart disease is not an approved indication for ERT. In short, many unanswered questions remain.
The other approved therapy for osteoporosis, calcitonin, has not been used extensively for preventing bone loss because of its expense and the need for parenteral administration of present formulations.35 Calcitonin, and investigational drugs like the bisphosphonates, also act by reducing bone loss. Sodium fluoride, an investigational drug known to increase bone mass in the spine and believed to reduce vertebral fracture rates, has little effect on bone mass in the limbs. Because hip fracture risk is not reduced and may actually be increased somewhat, fluoride has no role in osteoporosis prophylaxis.29 As is obvious from these observations, improved therapeutic approaches are needed, especially approaches that preserve bone without introducing unpleasant side effects or worrisome complications.
Age-related Bone Loss
This slow form of bone loss continues throughout life and is the major source of bone loss in both sexes. The determinants of age-related bone loss are not precisely known but may include impaired regulation of osteoblasts (the cells that make bone), deficiencies of calcium or vitamin D, and decreased muscle mass associated with inactivity. Bone cell function and regulation is the subject of
intensive research at present,35 but it is not yet possible to intervene to improve osteoblast function. Consequently, attention is directed to the role that calcium, vitamin D, and exercise play in bone loss.
The dietary requirement for calcium is relatively high because of the obligatory fecal and urinary losses of 150 to 250 milligrams per day (mg/day).41 When the amount of calcium absorbed from the diet is insufficient to offset these losses, calcium must be withdrawn from bone, which contains 99 percent of the total body stores. Moreover, active intestinal absorption of calcium decreases with aging, particularly after age 70, in response to a decrease in biologically active vitamin D.41 This phenomenon, in turn, may be due to age-related loss of kidney tissue with its enzyme that converts vitamin D to the active form or to a decrease in vitamin D receptors in intestinal cells.
The level of calcium intake required to overcome these problems is controversial, and population studies generally have not demonstrated a strong relationship between calcium intake and bone loss.19 The recommended daily allowance (RDA) for calcium has not been rigorously established but is currently set at 800 mg/day for adults.35 The efficacy of this recommendation is uncertain, however. Recent trials have generally found that calcium supplementation shortly after the menopause has little effect on spinal bone loss and only a modest effect on bone loss from the limbs.41 It is conceivable that calcium would be more effective after the estrogen-dependent phase of accelerated bone loss has ended, but data regarding this hypothesis are conflicting as well. A prospective study that measured rates of bone loss from the vertebrae and radius by serial bone density measurements found no relationship between calcium intake and bone loss.42 In contrast, a cohort study of elderly men and women living in a retirement community in California showed that those who had hip fractures within 14 years after initial evaluation had had a lower calcium intake at the baseline examination.13 There are no randomized controlled clinical trials that show directly that calcium supplementation prevents fractures. Nonetheless, the mean dietary calcium intake reported for the general population barely approximates the RDA for calcium in American men and is only 550 mg/day in middle-aged and elderly women.35 Consequently, it seems prudent to ensure at least the minimum recommended levels of calcium intake at all ages. Detailed guidelines are available.32
Similarly, it is reasonable to ensure an adequate vitamin D intake. Such assurance is important because there is an age-related decrease in the ability of the skin to synthesize vitamin D and in the ability of the intestine to absorb it.41 Thus, although most people get
enough vitamin D through sunlight exposure and their normal diet, housebound elderly persons are prone to vitamin D deficiency,32 particularly when they do not take supplementary vitamins and are consuming a diet marginal in vitamin D. The full extent of this problem is unknown; however, it is correctable with appropriate vitamin D supplementation.
Finally, it has been suggested that age-related bone loss could result, in part, from a decline in activity and fitness.37 Certainly it is true that bone responds to changes in loading: activity may cause an increase in bone mass, whereas disuse can result in dramatic bone loss.46 One study21 of hospitalized adults who required therapeutic bed rest showed that the bone mineral content in the lumbar spine decreased about 0.9 percent per week (equivalent to one year's worth at normal rates), although the rate of loss usually declines over time until a new steady state is reached. The exact pathophysiology of disuse osteoporosis is not known, nor are there specific approaches to remedy the situation except through restored activity. Nonetheless, this type of osteoporosis is a particular concern with regard to the rehabilitation of elderly people after an injury or other serious insult.
On a more positive note, it is thought that increased activity might help to retard bone loss and prevent osteoporosis.35 A number of short-term trials, mostly uncontrolled, indicate that exercise programs may augment bone mass,25 but it is not known whether these gains are maintained or whether they lead to a reduction in fractures. Increased activity throughout life appears to be generally beneficial, however, and should be encouraged.32 Specific recommendations regarding increased activity for older individuals are provided in Chapter 13.
Secondary Osteoporosis
Bone loss may be exacerbated by certain medical diseases, surgical procedures, and medications (Figure 6-3). Although such conditions may be a major cause of osteoporosis in some individuals, in general the bone loss from these factors is additive to the age-related slow bone loss that occurs universally and to the accelerated bone loss that occurs postmenopausally in women.43 Relatively common causes of this additional bone loss are corticosteroid and anticonvulsant use, gastrectomy, hyperthyroidism, and chronic obstructive lung disease. Less common are such conditions as Cushing's disease, acromegaly, hypopituitarism, and multiple myeloma. Altogether, one or more of these factors may be present in as many as 20 percent
|
Uncommon Conditions that Contribute Little to Osteoporosis |
||
|
Acromegaly |
Hyperparathyroidism |
Osteogenesis imperfecta |
|
Cushing's disease |
Hypopituitarism |
Multiple myeloma |
|
Important Risk Factors |
||
|
Cigarette smoking |
Gonadal hypofunction |
Leanness |
|
Dilantin therapy |
Hemiplegia |
Obstructive lung disease |
|
Ethanol consumption |
Hyperthyroidism |
Phenobarbital therapy |
|
Gastrectomy |
Inactivity |
Thyroidectomy |
|
Common Conditions with No Increased Risk for Osteoporosis |
||
|
Diabetes mellitus |
Parkinsonism |
Peripheral vascular disease |
|
Diverticulitis |
Peptic ulcer disease |
Stroke (without paralysis) |
|
Inguinal hernia |
(without gastrectomy) |
Thyroid adenoma |
|
Osteoarthritis |
Rheumatoid arthritis (without disability) |
Urolithiasis |
FIGURE 6-3 Relative impact in the community of various purported causes of ''secondary" osteoporosis. Source: L. J. Melton III and B. L. Riggs, "Clinical Spectrum," Chapter 6 in B. L. Riggs and L. J. Melton III, eds., Osteoporosis: Etiology, Diagnosis, and Management , Raven Press, New York, 1988, pp. 155-179.
of women and 40 percent of men with vertebral or hip fractures.28 The greater proportion of men affected by secondary osteoporosis is due to their lower background level of the condition—men start with greater bone mass, lose bone less rapidly over life, and do not live as long as women. Consequently, men with fractures are more likely to have a specific cause of excessive bone loss; thus, identification and management of secondary osteoporosis should be a primary consideration for them.
The actual importance, however, of many of the putative causes of "secondary" osteoporosis (along with a host of other conditions not listed here) is uncertain. For example, population-based studies have shown that non-insulin-dependent diabetes mellitus was not associated with any increased risk of fracture or bone loss (in contrast to results of less rigorous clinical studies); recent work raises similar questions about the impact of asymptomatic hyperparathyroidism,28 which is the form increasingly being diagnosed. Other conditions, like rheumatoid arthritis and stroke, are only indirectly linked to bone loss and fractures as a result of disease-induced disability and consequent disuse osteoporosis.28 An important research priority, therefore, is to assess the practical impact of the myriad conditions associated with secondary osteoporosis to identify those with a significant influence on fracture risk in the population.
Smoking is also associated with reduced bone mass, as well as with hip and vertebral fractures, and is correlated with another risk
factor, ethanol use.5 Ethanol may depress bone formation by a direct toxic effect on osteoblasts, and tobacco consumption may exert a similar effect on bone.28 However, smoking is also associated with earlier menopause and with less obesity (which is protective for osteoporosis), whereas excess alcohol use has been linked with nutritional deficiencies and abnormal vitamin D metabolism.28 Because smoking has other adverse effects (see Chapter 11), the habit should be discouraged. What impact a reduction in smoking would have on reducing osteoporotic fractures, however, is not known.
RECOMMENDATIONS
Services
-
A surveillance system should be developed to monitor osteoporosis prevention efforts. One element of such an effort should be the organization of national fracture data bases that capture outpatient fractures and fracture-related disability and institutionalization. In addition, "small area" analysis should be performed to identify populations at high risk for fracture.
-
As recommended in the report Injury in America, a national capacity should be developed for the quick identification and control of outbreaks of specific injuries, as well as a consistent, accurate system for coding the causes of injuries to be used by hospitals. In addition, more refined data on the specific types and causes of injuries are needed to develop effective interventions, and research is needed to determine the short- and long-term costs of injuries.
-
Osteoporosis prevention efforts should be integrated into national and local injury control programs. Adequate reimbursement (both public and private) should be sought for osteoporosis prevention efforts, including bone mass screening tests, drug prophylaxis for bone loss, and rehabilitation after fracture, once these strategies have demonstrated efficacy in reducing adverse health outcomes.
-
To increase the likelihood of rehabilitation after any disabling illness or injury, better methods should be developed to integrate the activities of medical care providers of various disciplines along with community and family resources.
Research
-
Specific bone mass screening and treatment recommendations should be developed, in particular the delineation of guidelines for standardized bone mass measurements and consensus on an overall treatment approach to osteoporosis prophylaxis. In addition,
-
the U.S. Preventive Services Task Force guidelines on osteoporosis screening should be reassessed. Related efforts should include quantification of the costs and benefits of estrogen replacement therapy (ERT), especially those relating to its controversial effects on the risk of coronary heart disease and breast cancer, and an investigation of the potential role of screening for men and nonwhite women.
-
Better therapies are needed to prevent postmenopausal bone loss. New drugs for osteoporosis prophylaxis should be developed and tested that do not have ERT side effects or complications (bisphosphonates, etc.).
-
The pathophysiology of age-related bone loss should be characterized to help identify new leads for therapy. In particular, the use of ERT for bone loss in the elderly should be evaluated. Controlled clinical trials should also be conducted to investigate the effects of calcium supplements and more realistic exercise programs for preventing bone loss in the elderly.
-
The prevalence and importance of risk factors for osteoporosis should be determined, including estimations of the national population at risk of fracture by virtue of low bone mass (men as well as women and nonwhites as well as whites) and the prevalence of risk factors (for attributable risk). Any difference in risk factor prevalence among races, genders, regions, or other demographic variables should be identified. Such research should also seek an explanation for the lower fracture risk (as compared to whites) found among Hispanic, black, and Asian populations. In addition, the important causes of secondary osteoporosis should be determined.
-
An optimal, postfracture rehabilitation program should be developed. Related research should include efforts to generate better data about fracture-related disabilities (especially those resulting from spinal fractures), quantify the determinants of functional impairment after hip or other such fractures, and determine barriers to aggressive rehabilitation. Controlled clinical trials should be conducted to demonstrate the merits of promising rehabilitation activities.
-
Research should continue on identifying modifiable determinants of serious falls (see Chapter 15).
Education
Policymakers
Recent research findings that bear on governmental policy matters should be interpreted to encourage more informed decisions by
policymakers. In addition, the effects of mid-life actions on subsequent medical costs to corporations for osteoporosis and fractures among their retirees should be documented and disseminated.
Providers
Treatment guidelines for osteoporosis screening and prophylaxis should be widely disseminated, and physicians, nurses, therapists, and other care providers should be educated regarding the need for and techniques of rehabilitation. Particular attention should be given to preventing vitamin D deficiency in the housebound elderly.
The Public
Women should be informed about the circumstances (risk factors, etc.) under which they should seek assessment for osteoporosis. Healthy lifestyles should be promoted (although there is no certainty that this will significantly reduce fracture occurrence), with an emphasis on good nutrition (including adequate intake of calcium and vitamin D), increased exercise, and decreased smoking and alcohol use. Practical information regarding calcium supplementation (preparation, dosages, etc.) should also be disseminated.
APPENDIX
SCREENING TESTS FOR OSTEOPOROSIS
Many different techniques have been used to assess bone mass. The most widely available, as well as the most accurate and precise, methods include single-photon absorptiometry, dual-photon absorptiometry, and quantitative computed tomography. These have been reviewed extensively (see P. L. Kimmel, "Radiologic Methods to Evaluate Bone Mineral Content, "Annals of Internal Medicine, Vol. 100, pp. 908-911, 1984); thus, only those aspects especially pertinent to screening are summarized here, along with features of the newest modality, dual-energy x-ray absorptiometry. Much of the information in the appendix is taken from two reports from the National Center for Health Services Research and Health Care Technology (M. Erlichman, Dual Photon Absorptiometry for Measuring Bone Mineral Density and Single Photon Absorptiometry for Measuring Bone Mineral Density, Health Technology Assessment Reports No. 6 and 7, respectively, U. S. Department of Health and Human Services, Rockville, Md., 1986).
SINGLE-PHOTON ABSORPTIOMETRY
Single-photon absorptiometry (SPA) is a widely used technique that involves passing a highly collimated monoenergetic beam of photons (using 125I as the source) across a limb and monitoring the transmitted radiation with a sodium iodide scintillation detector. Differential photon absorption between bone and soft tissue allows calculation of the total bone mineral content in the path of the beam, measured as grams per centimeter. This technique is limited to peripheral sites such as the radius or os calcis; as a result, it cannot measure bone density in the hip or spine, nor can it discriminate between cortical and trabecular bone.
The accuracy error for SPA is generally said to be around 4 to 5 percent. The precision (reproducibility) of the latest SPA technology (rectilinear SPA) is good, in the range of 1 to 2 percent in clinical settings. Patient acceptability is also quite good, and scan times are relatively short—an examination requires that a person sit in a chair for approximately 10 to 20 minutes. The radiation dose is low (2 to 5 millirems [mR]), with a negligible whole-body dose. Charges per scan range from $35 to $120.
DUAL-PHOTON ABSORPTIOMETRY
This technique emits photons at two different energies (using 153Gd as the source), which permits direct measurement of bone mineral density (area density in grams per square centimeter) in the proximal femur and lumbar spine. However, dual-photon absorptiometry (DPA) cannot distinguish between cortical and trabecular bone at those sites.
The accuracy error of DPA is about 3 to 6 percent for spine and 3 to 4 percent for the femoral neck; the estimated precision for measurements of the lumbar spine is about 2 to 4 percent and for the femoral neck, about 4 percent. Patient acceptability is good, but rectilinear scanning times are long, varying from 20 to 40 minutes for regional measurements and up to 40 to 60 minutes for total body measurement. A regional scan entails only 5- to 15-mR exposures, although the use of spine films to rule out fractured vertebrae increases the radiation dose substantially. Charges for DPA vary widely but usually exceed $125.
DUAL-ENERGY X-RAY ABSORPTIOMETRY
In this new absorptiometry technique, the dual-energy peaks are obtained by filtering x-rays or switching kilovoltage. The high count
rate obtained from the x-ray source permits considerably faster scan times with improved precision, which should increase the utility of this modality for osteoporosis screening. Source size and columnation are also smaller, and spatial resolution is better as a result. The precision of this technique is on the order of 1 percent or less. Dual-energy x-ray absorptiometry, or DEXA, can assess the spine or proximal femur with radiation exposure of less than 5 mR.
QUANTITATIVE COMPUTED TOMOGRAPHY
Quantitative computer tomography (QCT) also depends on the differential absorption of ionizing radiation by calcified tissue. Measurements, usually from a single energy source, are compared with a standard mineral reference (such as K2HPO4 solution) to calculate the bone mineral equivalent, which is expressed in milligrams of K2HPO4 per cubic centimeter. Areas of interest can be selected, including cortical bone, trabecular bone, or an integral assessment of the entire bone. Usually, the lumbar spine is chosen for assessment, but the technique can be adapted to other skeletal sites.
The accuracy error for QCT in the clinical setting is about 5 to 10 percent, with reproducibility of 1 to 4 percent. Patient acceptance is good, and a scan of the spine can be performed in about 15 minutes. Charges range from $100 to $400. In the most modern scanners, the radiation dose for single-energy QCT of the vertebrae is as low as 100 to 300 mR, but the dose varies widely and, depending on the equipment, can range up to 1,250 or 1,500 mR with scout films of the spine.
REFERENCES
1. Bergkvist, L., Adami, H. O., Persson, I., Hoover, R., and Schairer, C. The risk of breast cancer after estrogen and estrogen-progestin replacement. New England Journal of Medicine 1989; 321:293-297.
2. Bush, T. L., Barrett-Connor, E., Cowan, L. D., Criqui, M. H., Wallace, R. B., Suchindran, C. M., Tyroler, H. A., and Rifkind, B. M. Cardiovascular mortality and noncontraceptive use of estrogen in women: Results from the Lipid Research Clinics Program follow-up study. Circulation 1987; 75:1102-1109.
3. Bush, T. L., and Barrett-Connor, E. Noncontraceptive estrogen use and cardiovascular disease. Epidemiology Reviews 1985; 7:80-104.
4. Ceder, L., Thorngren, K. G., and Walldén, B. Prognostic indicators and early home rehabilitation in elderly patients with hip fractures. Clinical Orthopedics and Related Research 1980; 152:173-184.
5. Cummings, S. R., Kelsey, J. L., Nevitt, M. C., and O'Dowd, K. J. Epidemiology of osteoporosis and osteoporotic fractures. Epidemiology Reviews 1985; 7:178-208.
6. Cummings, S. R., and Nevitt, M. C. Epidemiology of hip fractures and falls.
In: M. Kleerekoper, and S. M. Krane (eds.), Clinical Disorders of Bone and Mineral Metabolism. New York: Mary Ann Liebert, Inc., Publishers, 1989,pp. 231-236.
7. Cummings, S. R., Rubin, S. M., and Black, D. The coming epidemic of hip fractures in the United States. Clinical Orthopedics and Related Research, in press.
8. de Bruijn, H. P. The Colles fracture, review of literature (Chap. 3). Acta Orthopaedica Scandinavica 1987; 58(Suppl. 223):7-25.
9. Dobyns, J. H., and Linscheid, R. L. Fractures and dislocations of the wrist. In: C. A. Rockwood, Jr., and D. P. Green (eds.), Fractures, vol. 1. Philadelphia: J. B. Lippincott Company, 1975, pp. 345-440.
10. Fitzgerald, J. F., Moore, P. S., and Dittus, R. S. The care of elderly patients with hip fracture: Changes since implementation of the prospective payment system. New England Journal of Medicine 1988; 319:1392-1397.
11. Gibson, M. J. The prevention of falls in later life. Danish Medical Bulletin 1987; 34(Suppl. 4):1-24.
12. Hillner, B. E., Hollenberg, J. P., and Pauker, S. G. Postmenopausal estrogens in prevention of osteoporosis: Benefit virtually without risk if cardiovascular effects are considered. American Journal of Medicine 1986; 80:1115-1127.
13. Holbrook, T. L., Barrett-Connor, E., and Wingard, D. L. Dietary calcium and risk of hip fracture: 14-year prospective population study. Lancet 1988; 2:1046-1049.
14. Holbrook, T. L., Grazier, K., Kelsey, J. L., and Stauffer, R. N. The Frequency of Occurrence, Impact and Cost of Selected Musculoskeletal Conditions in the United States. Chicago: American Academy of Orthopedic Surgeons, 1984.
15. Hui, S. L., Slemenda, C. S., and Johnston, C. C., Jr. Age and bone mass as predictors of fracture in a prospective study. Journal of Clinical Investigation 1988; 81:1804-1809.
16. Jensen, J. S., and Bagger, J. Long-term social prognosis after hip fractures. Acta Orthopaedica Scandinavica 1982; 53:97-101.
17. Johnston, C. C., Melton, L. J. III, and Lindsay, R. Clinical indications for bone mass measurements. Report of the Scientific Advisory Committee of the National Osteoporosis Foundation. Journal of Bone and Mineral Research 1989; 4(Suppl. 2):1-28.
18. Judd, H. L., Meldrum, D. R., Defton, L. J., and Henderson, B. E. Estrogen replacement therapy: Indications and complications. Annals of Internal Medicine 1983; 98:195-205.
19. Kanis, J. A., and Passmore, R. Calcium supplementation of the diet. II. Not justified by present evidence. British Medical Journal 1989; 298:205-208.
20. Kribbs, P. J., Smith, D. E., and Chesnut, C. H. III. Oral findings in osteoporosis. Part II. Relationship between residual ridge and alveolar bone resorption and generalized skeletal osteopenia. Journal of Prosthetic Dentistry 1983; 50:719-724.
21. Krølner, B., and Toft, B. Vertebral bone loss: An unheeded side effect of therapeutic bed rest. Clinical Science 1983; 64:537-540.
22. Lindsay, R., Aitken, J. M., Anderson, J. B., Hart, D. M., McDonald, E.B., and Clark, A. C. Long-term prevention of postmenopausal osteoporosis by estrogen. Lancet 1976; 1:1038-1041.
23. Lindsay, R., Hart, D. M., Forrest, C., and Baird, C. Prevention of spinal osteoporosis in oophorectomized women. Lancet 1980; 2:1151-1154.
24. Magaziner, J., Simonsick, E. M., Kashner, T. M., Hebel, J. R., and Kenzora, J. E. Survival experience of aged hip fracture patients. American Journal of Public Health 1989; 79:274-278.
25. Marcus, R., and Carter, D. R. The role of physical activity in bone mass regulation. Advances in Sports Medicine and Fitness 1988; 1:63-82.
26. Melton, L. J. III, Chao, E. Y. S., and Lane, J. Biomechanical aspects of fractures. In: B. L. Riggs and L. J. Melton III (eds.), Osteoporosis: Etiology, Diagnosis, and Management. New York: Raven Press, 1988, pp. 111-131.
27. Melton, L. J. III. Epidemiology of fractures. In: B. L. Riggs and L. J. Melton III (eds.), Osteoporosis: Etiology, Diagnosis, and Management. New York, Raven Press, 1988; pp. 133-154.
28. Melton, L. J. III, and Riggs, B. L. Clinical spectrum. In: B. L. Riggs and L. J. Melton III (eds.), Osteoporosis: Etiology, Diagnosis, and Management. New York: Raven Press, 1988, pp. 155-179.
29. Melton, L. J. III. Fluoride in the prevention of osteoporosis and fractures. Journal of Bone and Mineral Research 1990; 5:S163-S167.
30. Miller, C. W. Survival and ambulation following hip fracture. Journal of Bone and Joint Surgery 1978; 60-A:930-934.
31. Mossey, J. M., Mutran, E., Knott, K., and Craik, R. Determinants of recovery 12 months after hip fracture: The importance of psychosocial factors. American Journal of Public Health 1989; 79:279-286.
32. National Institute of Arthritis and Musculoskeletal and Skin Diseases. Osteoporosis: Cause, Treatment, Prevention. NIH Publ. No. 86-2226. Bethesda, Md.: National Institutes of Health, 1984.
33. Nickens, H. W. A review of factors affecting the occurrence and outcome of hip fracture, with special reference to psychosocial issues. Journal of the American Geriatrics Society 1983; 31:166-170.
34. Parfitt, A. M. Bone remodeling: Relationship to the amount and structure of bone, and the pathogenesis and prevention of fractures. In: B. L. Riggs and L. J. Melton III (eds.), Osteoporosis: Etiology, Diagnosis, and Management . New York: Raven Press, 1988, pp. 45-93.
35. Peck, W. A., Riggs, B. L., Bell, N. H., Wallace, R. B., Johnston, C. C., Jr., Gordon, S. L., and Shulman, L. E. Research directions in osteoporosis. American Journal of Medicine 1988; 84:275-282.
36. Phillips, S., Fox, N., Jacobs, J., and Wright, W. E. The direct medical costs of osteoporosis for American women aged 45 and older, 1986. Bone 1988; 9:271-279.
37. Pocock, N., Eisman, J., Gwinn, T., Sambrook, P., Kelly, P., Freund, J., and Yeates, M. Muscle strength, physical fitness, and weight but not age predict femoral neck bone mass. Journal of Bone and Mineral Research 1989; 4:441-448.
38. Pryor, G. A., and Williams, D. R. R. Rehabilitation after hip fractures: Home and hospital management compared. Journal of Bone and Joint Surgery 1989; 71-B:471-474.
39. Quigley, M. E. T., Martin, P. L., Burnier, A. M., and Brooks, P. Estrogen therapy arrests bone loss in elderly women. American Journal of Obstetrics and Gynecology 1987; 156:1516-1523.
40. Report of the U.S. Preventive Services Task Force. Chapter 40. Screening for postmenopausal osteoporosis. In: Guide to Clinical Preventive Services. Washington, D.C., 1989.
41. Riggs, B. L., and Melton, L. J. III. Involutional osteoporosis. In: Oxford Textbook of Geriatric Medicine, in press.
42. Riggs, B. L., Wahner, H. W., Melton, L. J. III, Richelson, L. S., Judd, H. L., and O'Fallon, W. M. Dietary calcium intake and rates of bone loss in women. Journal of Clinical Investigation 1987; 80:979-982.
43. Riggs, B. L., and Melton, L. J. III. Medical Progress: Involutional osteoporosis. New England Journal of Medicine 1986; 314:1676-1684.
44. Ross, P. D., Wasnich, R. D., MacLean, C. J., Hagino, R., and Vogel, J. M. A model for estimating the potential costs and savings of osteoporosis prevention strategies. Bone 1988; 9:337-347.
45. Silverman, S. L., and Madison, R. E. Decreased incidence of hip fracture in Hispanics, Asians, and blacks: California hospital discharge data. American Journal of Public Health 1988; 78:1482-1483.
46. Sinaki, M. Exercise and physical therapy. In: Riggs, B. L., and Melton, L. J. III (eds.), Osteoporosis: Etiology, Diagnosis, and Management. New York: Raven Press, 1988, pp. 457-479.
47. Stampfer, M. J., Willett, W. C., Colditz, G. A., Rosner, B., Speizer, F. E., and Hennekens, C. H. A prospective study of postmenopausal estrogen therapy and coronary heart disease. New England Journal of Medicine 1985; 313:1044-1049.
48. Tinetti, M. E., Speechley, M., and Ginter, S. F. Risk factors for falls among elderly persons living in the community. New England Journal of Medicine 1988; 319:1701-1707.
49. Wasnich, R. D. Fracture prediction with bone mass measurements. In: H. K. Genant (ed.), Osteoporosis Update 1987. San Francisco: Radiology Research and Education Foundation, 1987, pp. 95-101.
50. Weinstein, M. C. Estrogen use in postmenopausal women—costs, risks, and benefits. New England Journal of Medicine 1980; 303:308-316.

























