Making strong global, national, and programmatic commitments to HIV prevention is critical to any balanced attempt to change the course of the HIV epidemic, and PEPFAR has made major investments in activities aimed at reducing HIV transmission. The congressional charge for this evaluation, as laid out in the Lantos-Hyde Act of 2008, requested both “an assessment of progress toward prevention, treatment, and care targets” and “an evaluation of the impact of prevention programs on HIV incidence in relevant population groups.”1 This chapter presents the committee’s assessment of PEPFAR’s prevention activities.
In this chapter a brief overview of the evolution of HIV prevention science is followed by an overview of PEPFAR’s programmatic targets and funding for prevention and then discussions about the prevention of sexual transmission, including prevention for people who engage in sex work and prevention for men who have sex with men; prevention of mother-to-child transmission (PMTCT); prevention for people who inject drugs; and a limited assessment of PEPFAR’s efforts in the areas of blood and medical injection safety. The sections for each prevention area contain relevant historical and contextual framing and an assessment using the program impact pathway framework of inputs, activities, and, to the extent possible, the outcomes and impact of PEPFAR’s prevention efforts. This is followed by a
__________________
1 Tom Lantos and Henry J. Hyde United States Global Leadership Against HIV/AIDS, Tuberculosis, and Malaria Reauthorization Act of 2008, P.L. 110-293, 110th Cong., 2nd sess. (July 30, 2008) at ![]() 101(c), 22 U.S.C. 7611(c)(2)(B)(i) and (v).
101(c), 22 U.S.C. 7611(c)(2)(B)(i) and (v).
discussion of the role of counseling and testing within a prevention context, with more in-depth discussion and analysis of this topic in Chapter 6, “Care and Treatment.” Finally, there is a discussion of emerging prevention interventions and the committee’s recommendation for strategically strengthening PEPFAR’s prevention efforts. Further discussion of PEPFAR’s activities related to reducing HIV risk for women and girls and for men who have sex with men can be found in Chapter 8, “Gender.”
The IOM committee is mindful that, over the course of its existence, PEPFAR has had dual roles as both a catalyst and a respondent to various developments in global HIV prevention. The committee recognizes both the opportunities and the challenges inherent in these roles, and the results of this evaluation are described in this context.
EVOLUTION OF HIV PREVENTION SCIENCE
Throughout the history of the HIV epidemic, including the years of PEPFAR implementation, HIV prevention has been evolving, influenced by developments in science, policy, and advocacy in the context of an ever-changing epidemiological, political, and economic landscape. There are multiple, overlapping constructs through which HIV prevention efforts have been envisioned and organized. These include
• modes of transmission (sexual, parenteral, perinatal);
• populations and HIV-risk exposure behaviors (heterosexual men and women, men who have sex with men, transgender persons, people who inject drugs, HIV serodiscordant couples, pregnant women, young people, sex workers, etc.);
• unit- or level-targeted (individual, couple, network, community); and
• disciplinary, science-based approaches (biomedical, epidemiological, behavioral, social/structural).
Over time and in different geographic locations, some of these constructs have been emphasized over others, based on current science, epidemiological trends, or political shifts.
Evolution of Interventions to Prevent or Reduce HIV Infection
The search for an AIDS vaccine—considered an ultimate goal to prevent infection—began as soon as HIV was discovered to be the causative agent of AIDS. Finding an effective vaccine quickly proved to be elusive, and it remains a challenge given the rapidly adaptive nature of the virus (NIAID, 2012). Meanwhile, in the early years of the HIV response most
prevention efforts were focused on behavioral change strategies that had the potential to be effective in slowing the epidemic. These efforts were supported by observational data from developing countries suggesting that behavioral change made a significant difference in reducing HIV transmission (Gregson et al., 2006; Stoneburner and Low-Beer, 2004).
In addition to behavior change efforts, biomedical approaches became a focus of HIV prevention. One of the most exciting developments in biomedical prevention approaches was the discovery that the administration of antiretroviral (ARV) drugs (initially zidovudine and then nevirapine) to pregnant women and their newborns could significantly reduce HIV transmission from mother to child before, during, and after delivery (Connor et al., 1994; Guay et al., 1999; Shaffer et al., 1999; Sperling et al., 1996). This initial finding was followed by research on reducing the risk of transmission through breast feeding (Nduati et al., 2000).
The focus on PMTCT added urgency to addressing HIV infection in women; epidemiological data have shown high and often unequal rates of HIV infections among women as compared to men in many regions (WHO, 2011). In addition, the recognition that women do not control male condom use, the most widely available method to prevent sexual transmission of HIV (UNAIDS, 2009), highlighted the need for women-focused and women-initiated HIV prevention strategies. Female condoms have become more widely available since 2009, but have several disadvantages, including cost and difficulty of use based on current designs, which have limited their utilization. The global availability and distribution of female condoms remains less than for male condoms, and the World Health Organization (WHO) and the Joint United Nations Programme on HIV/AIDS (UNAIDS) are encouraging more widespread access and use to prevent pregnancy and sexually transmitted infections (Avert.org, 2012). Research to develop effective vaginal microbicides began to gain support in the early 1990s, but clinical trials of various compounds proved unsuccessful until 2010, when the Centre for the AIDS Program of Research in South Africa (CAPRISA) trial results were released showing reduced risk of HIV infection with use of an ARV-based gel (Abdool Karim et al., 2010).
In the 1990s evidence emerged supporting the effectiveness of harm reduction strategies as a way to prevent HIV transmission among people who inject drugs. Harm reduction efforts seek to minimize negative health outcomes associated with drug use, including reducing the risk of HIV transmission, for people who are unwilling or unable to quit their addiction (IHRA, 2009). These strategies may include sterile needle and syringe exchange programs, the relaxation of drug paraphernalia and possession laws, and the provision of medication for substitution therapy (Harm Reduction International, 2012). The adoption of harm reduction approaches varied considerably, but in cities with sterile needle and syringe exchange programs
in place, significant reductions have been seen in HIV epidemics where transmission was concentrated among people who inject drugs (Hurley et al., 1997). Despite the mounting evidence of its effectiveness, harm reduction has continued to be very politically and culturally controversial and was not widely implemented, even in some countries with ongoing or emergent concentrated HIV epidemics (Auerbach, 2009).
Other HIV prevention strategies explored and implemented in the first two decades of the global epidemic included the treatment of other sexually transmitted infections (STIs) to reduce the increased risk of HIV infection that accompanies STIs, and expanded blood donor HIV testing and other efforts to ensure the safety of blood and blood products and infection control practices in hospitals and other health care settings to reduce iatrogenic transmission (Auerbach et al., 2006).
By the time PEPFAR was initiated in 2003–2004, global experts had identified several effective, evidence-based prevention strategies and interventions that were recommended for implementation and scale-up to address HIV epidemics in developing and developed countries alike (Global HIV Prevention Working Group, 2003). These included
• behavioral change programs to reduce sexual risk behaviors and behavioral prevention programs specifically targeted to HIV-positive individuals;
• harm reduction services for people who inject drugs;
• antiretroviral prophylaxis for PMTCT;
• universal safety precautions, blood safety practices, and infection control in health care settings;
• identification and treatment of STIs in addition to HIV;
• HIV counseling and testing; and
• policy reforms (such as those to reduce the vulnerability of women and girls or to expand access to effective prevention strategies).
The HIV prevention field has continued to evolve, influenced by ongoing research on approaches to address social, economic, political, and environmental factors linked to HIV risk, also referred to as structural interventions for HIV prevention (Gupta et al., 2008). Such interventions aim to create an enabling environment that will allow individuals to act in their own and their partners’ best interests by supporting policy or legal and environmental changes, shifting harmful social norms, catalyzing social and political change, and empowering communities and groups (Auerbach, 2009; Gupta et al., 2008). Multiple structural interventions have been effective at achieving HIV prevention outcomes such as reductions in HIV transmission and social and structural risks that contribute to HIV vulnerability (Baird et al., 2012; Gupta et al., 2008; Pronyk et al.,
2006). Studies in this area are important because they provide evidence that structural interventions can influence the social determinants of HIV risk, reduce sexual and other HIV risk behaviors, and lower the rate of HIV infection.
Clinical interventions have also been a part of the evolution of the field of HIV prevention. In 2005 evidence of the efficacy of medical male circumcision for preventing HIV acquisition among men emerged (Auvert et al., 2005; Bailey et al., 2007; Gray et al., 2007). More recently, findings have been reported from clinical trials investigating the effectiveness of interventions such as oral pre-exposure prophylaxis (PrEP), topical microbicides, and antiretroviral therapy (ART) for prevention of HIV transmission (Abdool Karim et al., 2010; Cohen et al., 2011; Microbicide Trials Network, 2012a,b). These advances tremendously altered the prevention landscape—shifting from the historic emphasis on behavioral change strategies to one focused on biomedical prevention technologies.
As HIV prevention has evolved over time to encompass a broad array of strategies and interventions that have been informed by an evolving evidence base, appreciation has grown for a “combination approach” that integrates effective biomedical, behavioral, and structural components of HIV prevention—as appropriate for a given setting or population—for maximum effect (Auerbach and Coates, 2000; Global HIV Prevention Working Group, 2003; Hankins and de Zalduondo, 2010; Kurth et al., 2011; Padian et al., 2011; WHO, 2011).
In addition, the adoption and implementation of interventions to prevent HIV infection also occur in the context of historical and contemporary stigmatization. Both the ways in which HIV is transmitted—predominantly through sexual intercourse and illicit drug injection—and the social attitudes about people identified as most vulnerable—including men who have sex with men, sex workers, people who inject drugs, individuals with multiple or concurrent sex partners, young women, and HIV serodiscordant couples—have contributed to stigmatization (Avert.org, n.d.). These political and cultural aspects of HIV prevention must be acknowledged when assessing how donors, governments, civil society, communities, and individuals have addressed the epidemic.
OVERVIEW OF PEPFAR-SUPPORTED PREVENTION PROGRAMS
Programmatic Targets and Goals for HIV Prevention Over Time
The key programmatic target for prevention activities during the first phase of PEPFAR was to prevent 7 million new infections worldwide (OGAC, 2004b). In the 2008 reauthorization legislation, this target was increased to preventing 12 million new infections by 2013, and the goal
was added of providing “at least 80 percent of the target population with access to counseling, testing, and treatment” for PMTCT.2
History of PEPFAR Funding for Prevention
Figure 5-1 depicts the amount of planned/approved funding for PEPFAR’s prevention activities, not including counseling and testing, from fiscal year (FY) 2005 to FY 2011, disaggregated by PMTCT and all other prevention activities combined. Publicly available funding data do not provide any disaggregation of spending within prevention modalities—for example, how much is spent on activities, the procurement of supplies, workforce training, infrastructure, etc. The aggregate dollar amount of funding for these prevention activities has increased each year. The proportion of funds spent on prevention relative to total PEPFAR funding was highest in FY 2005 at 30 percent, and then declined for 2 years, followed by a steady increase from 18 percent in FY 2007 to 24 percent in FY 2011.
The 2003 authorizing legislation included a prevention funding allocation requirement that required that not less than 33 percent of PEPFAR prevention funds be spent on programs promoting abstinence until marriage,3 which PEPFAR interpreted as including programs addressing both abstinence and being faithful within a monogamous relationship (later commonly referred to as “AB”) (Ryan et al., 2012). Early in the implementation of PEPFAR, frustration was expressed by PEPFAR headquarters (HQ), mission teams, and other stakeholders about the rigidity of budget allocations that explicitly required a certain proportion of expenditures on abstinence and be faithful activities, which limited PEPFAR’s ability to tailor activities to respond to country epidemiological information and to align with national AIDS plans (GAO, 2006; IOM, 2007a). In 2007 an IOM committee recommended that these not be legislative requirements (IOM, 2007a), and the earmark was removed in the 2008 reauthorization legislation. The requirement was amended to state that prevention program portfolios should include a balanced funding approach within their prevention of sexual transmission activities.4 Additionally, in countries with generalized epidemics, a justification was required if programs promoting abstinence, delay of sexual debut, monogamy, fidelity, and partner reduction constituted less than 50 percent of funds spent on prevention of sexual transmission.5
__________________
2Supra, note 1 at ![]() 301(a)(2), 22 U.S.C. 2151b-2(b)(1)(A)(i) and (iv).
301(a)(2), 22 U.S.C. 2151b-2(b)(1)(A)(i) and (iv).
3 United States Leadership Against HIV/AIDS, Tuberculosis, and Malaria Act of 2003, P.L. 108-25, 108th Cong., 1st sess. (May 27, 2003) ![]() 402(b)(3).
402(b)(3).
4Supra, note 1 at ![]() 403, 22 U.S.C. 7673(a)(1)(A).
403, 22 U.S.C. 7673(a)(1)(A).
5Supra, note 1 at ![]() 403, 22 U.S.C. 7673(a)(2)(B).
403, 22 U.S.C. 7673(a)(2)(B).
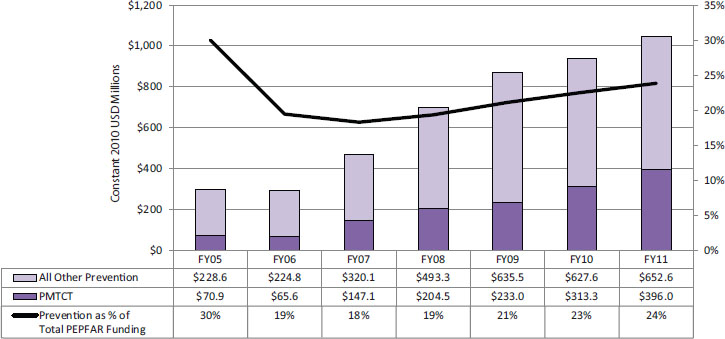
FIGURE 5-1 PEPFAR’s planned/approved funding over time for prevention (FY 2005–FY 2011).
NOTES: This figure represents funding for all PEPFAR countries as planned/approved through PEPFAR’s budget codes. The budget codes are the only available source of funding information disaggregated by type of activity, and are therefore used in this report as the most reasonable and reliable approximation of PEPFAR investment by programmatic area. (See Chapter 4 for a more detailed discussion of PEPFAR’s budget codes and the available data for tracking PEPFAR funding.) Data are presented in constant 2010 USD for comparison over time. These data represent planned/approved funding for the PMTCT budget code and all other prevention budget codes combined. In this graph, “All Other Prevention” includes funding for abstinence and be faithful, other sexual prevention, blood safety, injection safety, male circumcision, and injecting and non-injecting drug use budget codes. (Male circumcision and injecting and non-injecting drug use were not reported as unique budget codes until FY 2009; prior to FY 2009 they were included in a budget code labeled “Other Prevention.”) Funding for counseling and testing is not included in prevention here (which differs from the presentations in Chapter 4). The funding data for the counseling and testing budget code, which was included first in the care technical area and since 2009 in the prevention technical area, are presented independently in Chapter 6.
SOURCES: OGAC, 2005b, 2006c, 2007c, 2008b, 2010d, 2011e,f.
Evolution of PEPFAR Prevention Programming
As HIV prevention science has evolved, PEPFAR’s programming has shifted from an initial focus on a limited number of behavioral and biomedical interventions to an expanded prevention portfolio that includes new, evidence-based biomedical, behavioral, and structural approaches. When PEPFAR began in 2004, its prevention programs built on existing U.S. government (USG) activities focused on the prevention of PMTCT and expanded to include blood and medical injection safety, as well as behavior change strategies in line with the “Abstinence, Be faithful, and correct and consistent Condom use” approach (also known as “ABC”) (OGAC, 2004b). Although PMTCT remains a central pillar of prevention programming, the PEPFAR portfolio has since broadened to include a more diverse array of strategies for people vulnerable to sexual and drug-use-related HIV transmission. This includes the incorporation of strategies for which evidence emerged or for which evidence existed but had not yet
been adopted or scaled up by PEPFAR, such as voluntary medical male circumcision, promoting the use of female condoms, and harm reduction programs (OGAC, 2008b, 2009b, 2010b, 2011c). In line with the global HIV prevention movement, PEPFAR now supports a combination prevention strategy, which it defines as
HIV prevention using a suite of mutually reinforcing interventions to address the risks of transmission and acquisition as thoroughly and strategically as possible. It is predicated on the idea that no single intervention is efficacious enough to bring an HIV epidemic under control on its own, but that the optimal set of interventions implemented with quality and to scale can significantly reduce HIV incidence. (OGAC, 2011a, p. 7)
This process of evolution in PEPFAR’s support for prevention programs, which has been occurring much more slowly than many in the public health community would like, reflects the difficulties of implementing these programs which, more than care and treatment, intersect with a particularly sensitive context globally, domestically in the United States, and in partner countries. This affects both general programming for the prevention of sexual transmission and even more so, programming to meet the prevention needs of marginalized populations at elevated risk for HIV infection. As one stakeholder interviewed for this evaluation noted:
“I think one of the great challenges for PEPFAR has been on the one hand, professing to be evidence driven and interested in best practice and standards for HIV prevention, treatment, and care and at the same time, being constrained by the very real political realities of the U.S. where both sex work and injection drug use have been identified as things that the U.S. should not be funding.”6(NCV-24-USNGO)7
__________________
6 Single quotations denote an interviewee’s perspective with wording extracted from transcribed notes written during the interview. Double quotations denote an exact quote from an interviewee either confirmed by listening to the audio-recording of the interview or extracted from a full transcript of the audio-recording.
7 Country Visit Exit Synthesis Key: Country # + ES Country Visit Interview Citation Key: Country # + Interview # + Organization Type Non-Country Visit Interview Citation Key: “NCV” + Interview # + Organization Type Organization Types: United States: USG = U.S. Government; USNGO = U.S. Nongovernmental Organization; USPS = U.S. Private Sector; USACA = U.S. Academia; Partner Country: PCGOV = Partner Country Government; PCNGO = Partner Country NGO; PCPS = Partner Country Private Sector; PCACA = Partner Country Academia; Other: CCM = Country Coordinating Mechanism; ML = Multilateral Organization; OBL = Other (non-U.S. and non-Partner Country) Bilateral; OGOV = Other Government; ONGO = Other Country NGO.
A more in-depth discussion of the evolution of PEPFAR’s activities within specific areas of HIV prevention programming is provided in subsequent sections of this chapter. The committee chose to focus on three components of PEPFAR’s prevention programming for its primary analysis: prevention of sexual transmission, including prevention with people who engage in sex work and prevention with men who have sex with men; PMTCT; and prevention of HIV transmission among people who inject drugs. These were selected because they correspond to the greater share of HIV transmission; comprise the majority of PEPFAR’s prevention efforts, accounting for 58 to 70 percent of the program’s prevention spending from FY 2005 to FY 2011 (OGAC, 2005b, 2006c, 2007c, 2008b, 2010d, 2011e,f); and were a reasonable and feasible focus given the time and resource limitations for this evaluation. Additionally, these three components allowed the committee to evaluate PEPFAR’s prevention activities over time across the broadest possible range of countries, populations, and epidemic types. The remaining PEPFAR prevention program components are also addressed briefly, but because the committee did not conduct an extensive analysis of these activities, no conclusions were drawn in these areas.
PREVENTION OF SEXUAL TRANSMISSION
Background
More than 85 percent of new HIV infections are estimated to be sexually acquired (Abdool Karim et al., 2007; Gouws et al., 2006). As such, the prevention of sexual transmission of HIV infection among both heterosexuals and men who have sex with men (MSM) (including sexually active people who inject drugs) is critical to bringing the epidemic under control and has been a primary focus of global prevention efforts.
Early in the HIV/AIDS response in the United States, rigorously tested behavioral change intervention models in areas of health that pre-dated HIV/AIDS were adapted to develop HIV interventions (FHI 360, 2004; National Cancer Institute, 2005). These models focused on how an individual conceptualizes and the acts upon health-related beliefs and behaviors that are relevant to transmissible diseases, such as HIV. Behavior change strategies have continued to be expanded and refined, particularly with respect to focusing on specific populations. Predominant strategies that have been used over time to increase male condom use, reduce the number of sex partners, and, for young people, delay onset of sexual activity, include individual and group behavioral change interventions, social marketing techniques, and mass media-based communications campaigns (Global HIV Prevention Working Group, 2008).
Today, the modalities available for the prevention of sexual transmission are varied and expanding, and most contain a mixture of biomedical and behavioral elements. The quantity and type of evidence available for each prevention modality varies substantially, ranging from interventions having multiple scientific studies demonstrating efficacy and population-level impact, to interventions based on established theory or observational data only. This was illustrated by a recent review of prevention interventions in generalized epidemics conducted as part of a consultation for the World Bank, the United Nations Population Fund (UNFPA), and UNAIDS (Hearst et al., 2012). Hearst et al. found that voluntary medical male circumcision and interventions designed for identifiable sex worker populations have the most robustly documented evidence base within generalized epidemics (Hearst et al., 2012). In the case of behavior change activities designed to reduce multiple concurrent partnerships, observed changes in sexual behavior have been followed by declines in HIV transmission in several countries (Hearst et al., 2012); however, several randomized clinical trials of behavior change interventions to reduce sexual risk behaviors have been unable to replicate this effect (Corbett et al., 2007; Cowan et al., 2010; Gregson et al., 2007; Jewkes et al., 2008; Kamali et al., 2003; Pronyk et al., 2006; Ross et al., 2007). The efficacy of correct and consistent male and female condom use is well-proven, but the effectiveness of condom promotion and distribution campaigns has yet to be established in a real-world context (Hearst et al., 2012). Finally, for other interventions, especially structural efforts and new biomedical tools such as microbicides and prevention benefits of antiretroviral therapy, evidence for potential effectiveness is emerging, and ongoing data collection is under way. The committee’s analysis of the implication of these gaps in knowledge regarding the prevention of sexual transmission and the pressing need to address them is presented in the section on the analysis of prevention impact later in this chapter.
In addition to the varying levels of evidence for intervention approaches, there has also been large variation across countries and populations in the extent to which prevention of sexual transmission strategies have been adopted. For example, UNFPA estimated that in 2011 there were nine male condoms purchased with donor support for each male aged 15 to 49 in sub-Saharan Africa, and 2 billion condoms were procured by low- and middle-income countries in 2010; however, this is far short of the 13 billion condoms estimated to be needed by 2015 (UNAIDS, 2012b). There is very little known about the coverage of individual and mass media behavior change education programming, but in 26 countries with generalized epidemics reporting to UNAIDS, less than half of young women reported comprehensive knowledge of HIV transmission and prevention (UNAIDS, 2012b). Only 13 countries have established national targets for voluntary
medical male circumcision; of these, 10 had achieved 20 percent or less of their goal by 2011 (UNAIDS, 2012b).
PEPFAR’s Prevention of Sexual Transmission Efforts
Initially PEPFAR efforts and activities to prevent sexual transmission focused on the promotion of behavior change interventions. The 2003 PEPFAR authorizing legislation highlighted the “ABC model”—Abstinence, Be faithful, and correct and consistent Condom use—as a successful approach to the prevention of sexual transmission of HIV.8 It instructed PEPFAR to support “programs and efforts that are designed or intended to impart knowledge with the exclusive purpose of helping individuals avoid behaviors that place them at risk of HIV infection,” which included delay of sexual debut, fidelity and monogamy, abstinence, reduction of casual sexual partnering, and condoms.9 The 2008 reauthorization legislation expanded the scope of program activities, incorporating additional approaches, such as health education for serodiscordant couples, and structural interventions to address sexual transmission risk from vulnerabilities related to gender and age.10
In addition to the legislative directives, PEPFAR’s portfolio of HIV prevention activities is also driven by guidance documents—directives specifying what can and should be supported with PEPFAR resources—that are fundamental to operationalizing programmatic targets and goals. A general discussion on the role of Office of the U.S. Global AIDS Coordinator (OGAC) in issuing PEPFAR guidance can be found in Chapter 3. For the purposes of this chapter, the following sections provide a brief review of the guidance for the prevention of sexual transmission issued by OGAC over time and describe how PEPFAR-supported activities have evolved.
PEPFAR Guidance for the Prevention of Sexual Transmission
In 2005 PEPFAR released ABC Guidance #1 (OGAC, 2005a). With respect to the relative role and incorporation of the different elements of the ABC approach in its prevention program, the guidance stated, “Emergency Plan funds may be used for abstinence and/or be faithful programs that are implemented on a stand-alone basis. For programs that include a “C” component, information about the correct and consistent use of condoms must be coupled with information about abstinence as the only 100 percent effective method of eliminating risk of HIV infection; and the importance of
__________________
8Supra, note 3 at ![]() 2(20)(c).
2(20)(c).
9Supra, note 3 at ![]() 301(a)(2), 22 U.S.C. 2151b(d)(1)(A).
301(a)(2), 22 U.S.C. 2151b(d)(1)(A).
10Supra, note 1 at ![]() 101(a), 22 U.S.C. 7611(a)(12)(A-J).
101(a), 22 U.S.C. 7611(a)(12)(A-J).
HIV counseling and testing, partner reduction, and mutual faithfulness as methods of risk reduction” (OGAC, 2005a, p. 5). A distinction was made between youth (aged 10 to 14 years), for whom only AB programs were appropriate, and older youth (14 years and older), for whom a combination of ABC could be permitted. PEPFAR funds were not allowed for the distribution or marketing of condoms in schools. The ABC Guidance #1 called special attention to specific populations that include “sex workers and their clients, sexually active discordant couples or couples with unknown HIV status, substance abusers, mobile male populations, men who have sex with men, people living with HIV/AIDS, and those who have sex with an HIV-positive partner or one whose status is unknown,” and encouraged a range of interventions related to counseling, testing, and behavior change approaches be used for these populations (OGAC, 2005a, p. 8).
Six years later, in 2011, OGAC released its Guidance for the Prevention of Sexually Transmitted HIV Infections (OGAC, 2011a). This was the first comprehensive prevention guidance related to sexual transmission released since ABC Guidance #1. In the document, PEPFAR endorsed combination prevention for all country programs and reorganized the categorical divisions within prevention of sexual transmission from the original ABC organization to biomedical interventions, behavioral interventions, structural supports, and prevention for specific populations. Biomedical interventions include the provision and promotion of male and female condoms; voluntary medical male circumcision (VMMC); HIV counseling and testing; diagnosis and treatment of sexually transmitted infections; antiretroviral drug-based prevention for post-exposure prophylaxis; and, in keeping with country guidelines, offering antiretroviral therapy to HIV-positive partners who are in known serodiscordant relationships and have CD4 counts of 350/mm3 or lower. Behavioral interventions include standalone behavioral interventions to minimize risk or increase protection and supportive behavioral interventions to optimize biomedical prevention. Structural supports include legal and policy reform. Prevention packages for specific populations include comprehensive prevention for populations at elevated risk of HIV infection; positive health, dignity and prevention for persons living with HIV (PLHIV); and prevention interventions for young people (OGAC, 2011a).
One challenge in implementing prevention programs for specific populations is that occasionally there is a lack of agreement among the range of stakeholders involved in the response about which populations are at elevated risk in a country or how they should be prioritized for intervention (240-9-USG; 331-5-ML; 587-3-USG; 166-5-USG; 240-ES; 587-ES; 461-ES; 331-ES; 166-ES; 196-ES; 935-ES)—even with the newly released guidance and considerations for a given country or setting. Although PEPFAR indicators specifically mention people who inject drugs, MSM, and sex workers (OGAC, 2009c), in some countries
these categories are not sufficient to capture all the populations understood or demonstrated to be at risk and in need of targeted prevention services; examples of other populations include HIV serodiscordant couples (including those desiring family planning), clients of sex workers, truckers, young women, transgender persons (especially those who engage in sex work), and non-injecting substance abusers (including those who abuse alcohol) (196-ES; 116-ES; 166-ES; 935-ES; 461-ES; 934-ES; 240-35-PCNGO; 272-25-USG).
Overall, the updated guidance on prevention of sexual transmission represents notable progress since ABC Guidance #1 and provides a more transparent and detailed technical articulation of the strength of the scientific evidence supporting each HIV prevention method and the rationale for suggesting program implementation measures. In addition, it takes a more operational approach and is less proscriptive and more amenable to contextualization for different country programs.
PEPFAR-Supported Activities for the Prevention of Sexual Transmission
Since its inception in 2003, PEPFAR has supported the scale-up of a broad range of interventions designed to prevent sexual transmission of HIV. The types of activities that PEPFAR has supported over time for the prevention of sexual transmission are described here and summarized in Table 5-1. Across PEPFAR programs, supported interventions have always included behavior change communication activities, mass media campaigns, and condom distribution (OGAC, 2005a). As described above, an initial focus of behavior change activities on messaging that promotes abstinence and partner faithfulness has been substantially broadened to include more tailored and comprehensive risk-reduction counseling and outreach approaches, as well as biomedical and structural interventions (OGAC, 2005a, 2009b, 2011a). The promotion and distribution of condoms and condom-compatible lubricants continue to be core elements of PEPFAR’s prevention portfolio across countries and epidemic types, especially for populations at elevated risk of HIV acquisition (OGAC, 2005a, 2011c). More recently, greater emphasis has been placed on addressing structural barriers to prevention of sexual transmission and on creating a supportive and enabling environment for individuals to access prevention services (OGAC, 2008a, 2009b). PEPFAR also supports prevention activities for specific populations at elevated risk, including men who have sex with men, sex workers, and people who inject drugs and their sexual partners (OGAC, 2009b). (More information on these activities can be found in the relevant sections that follow within this chapter and in Chapter 8, “Gender.”)
The interventions included as a part of PEPFAR’s prevention programming have changed over time, in part because the field of prevention science continues to evolve. The need to adapt to and incorporate emerging preven-
| Biomedical | Behavioral | Structural |
| Provision of male and female condoms | Mass media communication Community interventions |
Reducing stigma and discrimination against PLHIV and marginalized populations |
| Treatment of sexually transmitted infections | Interpersonal communication | Gender inequality and gender-based violence |
| Antiretroviral-based prevention: post exposure prophylaxis for occupational exposure and survivors of sexual assault |
Focal topics: • Correct and consistent condom use • Multiple concurrent partnerships |
Economic empowerment and other multisectoral approaches |
| Voluntary medical male circumcision (VMMC) (since 2009) |
• Intergenerational and transactional sex • Abstinence and age of sexual debut |
Linkages to HIV and non-HIV health care and treatment services, as well as to non-health services (e.g., legal services) |
| Antiretroviral-based prevention: Treatment for HIV-positive partners who are in known discordant relationships and have CD4 counts of 350/mm3 or lower (included in Prevention since 2011) |
• Creating demand for prevention services • VMMC client education • Antiretroviral therapy adherence and education |
Education |
| HIV testing and counseling (included in Prevention since 2009) | ||
NOTE: Interventions are categorized as described in PEPFAR guidance documents.
SOURCES: OGAC, 2005a, 2007a, 2009b, 2011a.
tion evidence into program planning, guidance, and implementation is an important challenge and an ongoing process. One example of this process has been PEPFAR’s response to the discovery of the prevention benefit of VMMC, described in Box 5-1.
At the level of country programs, the specific portfolio or combination of interventions supported and implemented has varied. A review of annual PEPFAR Country Operational Plans from the countries selected for visits for this evaluation revealed that in most countries, there has been at least one activity supported within each of the modalities listed above. Interviewees in nearly all countries visited described the implementation of a broad array of interventions intended to prevent sexual transmission of HIV. A few examples of the activities described include media campaigns (166-5-USG; 272-18-PCNGO; 461-10-PCNGO; 461-14-USG), the use of peer educators (331-7-PCNGO; 166-5-USG), increasing the availability of condoms (116-4-USG), community organizing for public health messaging (166-23-USG), school- and sports-based youth programs (272-15-PCNGO), building government capacity to address prevention (272-12-USNGO), and male circumcision (934-10-PCGOV). Indeed, the approach to prevention portfolios in PEPFAR country programs was sometimes diffuse;
BOX 5-1
PEPFAR’s Adoption and Scale Up of
Voluntary Medical Male Circumcision
In 2007 the outcomes of three randomized controlled trials indicated that voluntary medical male circumcision (VMMC) reduced men’s risk of HIV acquisition by 50 to 60 percent (Auvert et al., 2005; Bailey et al., 2007; Gray et al., 2007). Follow-up of all participants eventually circumcised at approximately 2.5 years post-trial indicated that the protective effect increased to 67 percent (Kong et al., 2011). This emerging evidence on the effectiveness of VMMC led, in PEPFAR II, to the adoption of this intervention as part of the prevention portfolio and to the scale-up of delivery of VMMC.
Following the publication of these study results, PEPFAR initiated an effort to actively incorporate VMMC into its prevention guidance and into the portfolios of partner countries where this intervention would be appropriate, primarily those with high-prevalence generalized HIV epidemics. The U.S. government’s commitment to the scale-up of VMMC began with the 2008 Reauthorization Legislation, where it was endorsed as a crucial emerging prevention approach.a In 2009 PEPFAR introduced a separate budget code within its prevention funding categories designated specifically for programming on VMMC (OGAC, 2008a). In 2011, in PEPFAR’s newly released guidance on the prevention of sexual transmission of HIV, voluntary medical male circumcision was included as one of the many methodologies that should be used as part of a combination prevention approach (OGAC, 2011a).
PEPFAR-supported activities for VMMC are under way, and implementation scale-up has already begun in some locations. In FY 2009, 14 countries reported budgets for VMMC, totaling $34.9 million (current USD). In FY 2011, the number of countries with a VMMC budget was still 14, but the total amount of funding planned was $86.9 million (current USD), an increase of almost 150 percent in just 2 years (OGAC, 2010d, 2011e,f).
Interviewees described efforts across partner countries to incorporate VMMC into their prevention portfolios and to scale up services (196-12-PCGOV; 116-4-USG; 116-12-PCNGO; 166-4-USG; 272-12-USNGO; 272-17-USG; 272-25-USG; 461-3-USG; 461-8-PCGOV; 934-10-PCGOV). However, these efforts were not without challenges, with a significant one being the process of working to secure the support of partner governments, which was seen as an important step, but could sometimes result in delays (636-16-USG; 116-2-USG; 461-7-PCNGO; 461-13-USACA). Multiple interviewees also highlighted the need to incorporate communication and behavior change activities into VMMC interventions (636-6-USG; 272-12-USNGO; 934-12-CCM).
In addition to these challenges, one important additional limitation to note with respect to the role of VMMC in prevention portfolios is that any HIV prevention benefit for women is at best indirect, resulting from the number of HIV-positive men in the population decreasing over time.
There is not yet evidence that among serodiscordant couples circumcision reduces the transmission rate from men to their uninfected female partners (Turner et al., 2007; Wawer et al., 2009).
Although challenges and limitations remain, the roll-out and scale-up of VMMC represents an example of PEPFAR’s adaptation to the evolving scientific evidence-base and contains lessons for the program as it incorporates new technologies in the future.
__________________
a Supra, note 1 at ![]() 101(a), 22 U.S.C. 7611(a)(14)(A).
101(a), 22 U.S.C. 7611(a)(14)(A).
SOURCES: Auvert et al., 2005; Bailey et al., 2007; Gray et al., 2007; Kong et al., 2011; OGAC, 2008a, 2010d, 2011a,e,f; Turner et al., 2007; Wawer et al., 2009.
as one interviewee described, ‘The prevention program initially was a “go everywhere, do a lot of activities” kind of approach’ (272-17-USG).
Effects of PEPFAR’s Prevention of Sexual Transmission Efforts
The committee attempted an assessment of PEPFAR’s activities for prevention of sexual transmission using program monitoring data reported annually to OGAC by PEPFAR mission teams. (For more information on programmatic reporting, see Chapter 11, “PEPFAR’s Knowledge Management.”) Of the relevant data requested and received from OGAC, only two prevention indicators had data to document time trends (FY 2004–FY 2009) (OGAC, 2007b):
| Indicator 2.1 | Number of individuals reached through community outreach that promotes HIV/AIDS prevention through abstinence and/or being faithful |
| Indicator 5.2 | Number of individuals reached through community outreach that promotes HIV/AIDS prevention through other behavior change beyond abstinence and/or being faithful |
In FY 2004 and FY 2005 the number of individuals reached annually with messages that promote HIV/AIDS prevention through abstinence or being faithful was 24 and 25 million respectively. Between FY 2006 and FY 2009 the number of individuals reached annually ranged between 38
million and 46 million per fiscal year, an increase that is in part due to the increased number of countries receiving PEPFAR funding and reporting data related to this indicator. This data is summarized in Table 5-2.
Table 5-3 shows a large number of individuals have also been reached with messages regarding HIV/AIDS prevention through behavior change beyond abstinence and/or being faithful. With each successive year of PEPFAR implementation, the number of individuals reached with these messages increased, beginning with 12 million in FY 2004 and ending with 36 million in FY 2009. Again, there was a large increase in the number of countries funded by PEPFAR and reporting program monitoring data between FY 2004 and FY 2006.
In 2009, PEPFAR introduced the Next Generation Indicators (NGIs). Many previous indicators were discontinued and some new program monitoring indicators were introduced (the evolution of PEPFAR indicators is discussed in more depth in Chapter 11 on PEPFAR’s knowledge management); the two process measures for behavior change activities described above were essentially maintained. There are currently six NGIs, listed in Box 5-2, that attempt to monitor PEPFAR efforts related to prevention of sexual transmission of HIV (OGAC, 2009c). Mission teams began reporting data on these indicators in FY 2010; therefore, longitudinal data to assess PEPFAR’s impact using these indicators were not available to the committee.
In addition to the available indicator data, interviewees in countries described some observed successes in the area of prevention of sexual
| FY 04 | FY 05 | FY 06 | FY 07 | FY 08 | FY 09 | |
| Total | 24.0 | 24.9 | 44.9 | 45.8 | 38.4 | 41.4 |
NOTES: For FY 2004 and FY 2005, the number of countries reporting data was 15. In FY 2006, 27 countries reported data. For FY 2007–FY 2009 all 31 countries included as the focus of this evaluation reported data (see Chapter 2).
SOURCE: Program monitoring indicators provided by OGAC.
| FY 04 | FY 05 | FY 06 | FY 07 | FY 08 | FY 09 | |
| Total | 11.9 | 17.9 | 26.0 | 21.7 | 32.5 | 36.2 |
NOTES: For FY 2004 and FY 2005, the number of countries reporting data was 15. In FY 2006, 27 countries reported data. For FY 2007–FY 2009 all 31 countries included as the focus of this evaluation reported data (see Chapter 2).
SOURCE: Program monitoring indicators provided by OGAC.
BOX 5-2
Centrally Reported Next Generation Indicators
for Prevention of Sexual Transmission
P8.1.D Number of targeted population reached with individual and/or small group level preventive interventions that are based on evidence and/or meet the minimum standards required
P8.2.D Number of the targeted population reached with individual and/or small group level preventive interventions that are primarily focused on abstinence and/or being faithful, and are based on evidence and/or meet the minimum standards required
P8.3.D Number of Most-At-Risk Persons reached with individual and/or small group level interventions that are based on evidence and/or meet the minimum standards required
• Disaggregated by population: commercial sex workers, people who inject drugs, men who have sex with men
P5.1.D Number of males circumcised as part of the minimum package of male circumcision for HIV prevention services
• Disaggregated by age: <1, 1–14, 15+
P6.1.D Number of persons provided with post-exposure prophylaxis (PEP)
• Disaggregated by exposure type: Occupational, Rape/Sexual Assault Victims, or Other Non-Occupational
P7.1.D Number of persons living with HIV/AIDS (PLHIV) reached with a minimum package of Prevention with PLHIV (PWP) interventions
SOURCE: OGAC, 2009c.
transmission efforts, which they attributed at least in part to the work of PEPFAR. These included a perceived reduction in prevalence (240-3-USG; 331-6-CCM; 272-5-PCGOV; 461-8-PCGOV), a delay in the age of sexual debut for youth (461-8-PCGOV), and increased rates of condom use among youth (272-1-USG) and in the general population (272-5-PCGOV). Output successes were also reported, such as the distribution of large numbers of free condoms (240-9-USG; 240-29-USNGO) and increased awareness of HIV risk prevention (240-35-PCNGO; 240-29-USNGO; 196-18-PCNGO; 196-23-PCNGO).
Data Limitations for the Assessment of Prevention of Sexual Transmission
While the annual increases in the number of individuals reached by each type of outreach activity are notable, the two process measures pre-
sented in Tables 5-2 and 5-3 are not sufficient to provide PEPFAR with an understanding of its programming in this area. These process indicators do not serve to contribute to an overall understanding of the impact of PEPFAR’s prevention activities on incidence or infections averted. (This is also discussed in greater detail later in the chapter, in the section on analysis of prevention impact.) For example, for behavior change interventions, it is not possible through these indicators to assess whether the activities were associated with individual behavior change and risk reduction outcomes. To better understand the effectiveness of its programs for behavior change to prevent sexual transmission, PEPFAR will require more information on the populations in need and a clearer approach to assessing the link between having been reached by a prevention message and a resultant change in sexual risk behavior.
Stakeholders interviewed by the evaluation committee echoed this assessment. Although interviewees recognized PEPFAR’s support for a range of activities for the prevention of sexual transmission and noted some achievements in this area, many interviewees emphasized that the current PEPFAR prevention indicators do not capture the efforts and outcomes of prevention well, including changes in behavior (587-12-USG; 166-12-USG; 166-23-USG; 461-14-USG; 396-15-USNGO; 935-17-USG). Interviewees pointed to a lack of data available for prevention programming, both in terms of understanding the current epidemic in their countries and tracking the outcomes of prevention programs (240-9-USG; 587-12-USG; 166-5-USG; 272-6-ML). One interviewee commented, for example, that ‘what little data the country does have on condoms is not being used’ (272-6-ML). However, some interviewees highlighted achievements in the use of data. For example, one participant cited as progress ‘transitioning from an emergency, scaled-up approach using general knowledge/awareness focus with little data, to targeting prevention strategies that are informed by data’ (587-12-USG). Interviewees identified several data-collection activities that were under way to support these decision-making efforts, and a number of these were supported by PEPFAR (240-8-USG; 587-5-PCGOV; 196-12-PCGOV; 166-5-USG):
“PEPFAR-funded programs play a critical role in [this country] being able to report on UNGASS11 and other groups. Especially when it comes to prevention.” (587-25-ML)
Conclusion: Because of a lack of systematically collected information on activities, outputs, and outcomes, PEPFAR is unable to adequately track the implementation of prevention of sexual transmission, one of the most important components of its prevention
__________________
11 The UNGASS indicators are a set of national measures (currently 25) used since the 2001 United Nations General Assembly Special Session (UNGASS) on HIV/AIDS to track global progress toward addressing the HIV epidemic. The indicators are typically reported biannually to UNAIDS (UNAIDS, 2010).
programming. The committee was unable to assess the effectiveness or to determine the outcomes or impact of PEPFAR’s efforts across partner countries to reduce sexually transmitted HIV infections.
Despite the widespread adoption of interventions to prevent sexual transmission, outcomes for HIV prevention are inherently difficult to measure. Indeed, there is not clarity in the global community on how to routinely track their implementation and effects, especially for structural interventions, behavior change, and combination prevention. The lack of measurable effects has led to skepticism about the effectiveness of these approaches. For example, several large-scale trials in sub-Saharan Africa addressing the management of STIs, voluntary counseling and testing, individual and community education, intimate partner violence, condom distribution, income-generating activities, and combination approaches have had mixed results. While several of these studies found significant effects on knowledge and behavior, all failed to detect significant changes in HIV incidence (Corbett et al., 2007; Cowan et al., 2010; Gregson et al., 2007; Jewkes et al., 2008; Kamali et al., 2003; Pronyk et al., 2006; Ross et al., 2007). However, the methodological designs of these trials may have limited their ability to demonstrate outcomes because randomized controlled designs may be both unrealistic and inappropriate for evaluating the effectiveness of structural, behavioral, and combination prevention approaches (Laga et al., 2012; Stephenson and Cowan, 2003). Alternative evaluation designs exist, including large-scale cohort studies, non-randomized and quasi-experimental plausibility approaches, and evaluations triangulating across multiple methodologies (Gupta et al., 2008; Laga et al., 2012). PEPFAR’s use of these approaches for monitoring, evaluating, and reporting on its non-biomedical prevention efforts is limited. PEPFAR is currently supporting several trials on the effectiveness of combination prevention approaches that address multiple modes of HIV transmission; with respect to sexual transmission, these include biomedical and some limited behavioral interventions (NCV-31-USG) (Essex and DeGruttola, 2012; Kerrigan and Sweat, 2012). While these trials can be expected to make important contributions to the knowledge base and to future program planning, they will not be sufficient to address this fundamental knowledge gap.
Although there is strong foundational knowledge that supports the principles and the design of behavioral and structural interventions, persistent gaps in the field include a lack of knowledge about what the appropriate measures are for meaningfully tracking scale-up and coverage of these interventions; a lack of established and agreed-upon behavior change outcome measures and proxy outcome measures; an insufficient understanding of the effectiveness of these interventions when implemented at scale in producing changes in outcomes; and a lack of knowledge of how the rates of change in behavioral and proxy outcomes are associated with
rates of change in HIV transmission. However, the challenges of measuring the effects of these interventions and the limited availability of research using appropriately matched methodologies do not mean that these interventions are inherently ineffective. Rather, it is an indication that there is a substantial knowledge gap in this area relative to biomedical prevention modalities, both within PEPFAR and in the greater global health community. This important need was illustrated by the perspective of one interviewee: ‘Behavioral interventions cannot be proven as easily. This is also a challenge for scientists to determine how to prove behavioral interventions work’ (272-12-USNGO).
This is an area in which PEPFAR, given the scale of its programs and its commitment to implementation research, has a unique opportunity to contribute to much-needed ongoing research in developing and assessing behavioral and structural interventions, building on the methodological approaches that are currently available and in use, and supporting innovation where needed. The principle of “Know your epidemic, know your response” emphasizes the importance of understanding and responding to the factors that contribute to the epidemic within each country (UNAIDS, 2007). Given that sexual transmission is the primary global driver of HIV infection, effective interventions to address sexual transmission will need to be a central component of any comprehensive national response. Behavioral and structural drivers of the epidemic will not be addressed through biomedical approaches alone, and PEPFAR, along with the international HIV community, has emphasized that the most effective approach is likely to be a combination of interventions designed to reduce high-risk sexual behavior, efforts to modify the structural factors that lead to increased vulnerability, and the use of established and emerging biomedical tools (OGAC, 2011a; WHO, 2011). However, the evidence available on how to best identify, combine, implement, and scale up each of these intervention components is inadequate to guide the response at the global, national, and community levels. An evidence-based response requires responsiveness both to the currently available intervention effectiveness evidence and to the evidence on the epidemiological drivers and other contextual factors that affect the epidemic. Therefore, where intervention effectiveness is lacking for key drivers, efforts to fill that gap will by necessity be a part of the response. If PEPFAR is to be able to support programs that are tailored appropriately and effectively to the varied contexts in which it operates, more effort will be needed to advance the field of HIV prevention science, especially for behavioral and structural interventions.
Conclusion: Behavioral and structural interventions, especially those targeted at prevention of sexual transmission, are critical components of a balanced and comprehensive prevention portfolio. Yet, within PEPFAR there is disproportionately less program
monitoring data and rigorous research evidence available on these interventions than on PMTCT and other biomedical prevention programs. Improved monitoring, evaluation, and research methods appropriate to assessing behavioral and structural activities are needed by PEPFAR to enable both OGAC and country implementers to select the most effective interventions and programs and to assess their outcomes once implemented. There is a critical need for improved application of advances in social and behavioral science-based research and evaluation science for prevention to determine the most effective combinations of prevention interventions in diverse country contexts. Given the scale of its programs and its commitment to implementation research, PEPFAR can contribute to a more effective HIV response by serving as a platform for innovation to fill the gap in knowledge and availability of effective interventions.
Sex Workers
Background
Among the populations at elevated risk included within PEPFAR’s prevention of sexual transmission efforts are people who engage in sex work. Sex work, which is sometimes referred to as “transactional sex,” describes a wide variety of activities depending on local context. It may be formal or informal, occasional, or a full-time occupation. Sex workers may be female, male, or transgendered persons (UNFPA, 2001). While robust data on the number of persons engaging in sex work and the health status and other outcomes for these individuals are limited, disproportionately high HIV prevalence rates have been documented in persons engaging in sex work as compared to the general adult population in many countries (WHO, 2011).
PEPFAR-Supported Activities for Sex Workers
Legislation The legislation initially authorizing PEPFAR recognized that “[t]he sex industry, the trafficking of individuals into such industry, and sexual violence are additional causes of and factors in the spread of the HIV/AIDS epidemic.”12 The authorizing legislation imposed a restriction on PEPFAR’s programmatic activities in a sub-clause stating that “no funds made available to carry out this Act, or any amendment made by this Act, may be used to promote or advocate the legalization or practice of
__________________
12Supra, note 3 at ![]() 2(23).
2(23).
prostitution or sex trafficking”13 nor “to provide assistance to any group or organization that does not have a policy explicitly opposing prostitution and sex trafficking.”14 However, the authorizing legislation also noted that the legislation should not “be construed to preclude the provision to individuals of palliative care, treatment, or post-exposure pharmaceutical prophylaxis, and necessary pharmaceuticals and commodities, including test kits, condoms, and, when proven effective, microbicides.”15 The legislation also emphasized that in the required Five-Year Strategy a priority within prevention efforts should be the reduction of behavioral risks for HIV, in part by “eradicating prostitution, the sex trade, rape, sexual assault and sexual exploitation of women and children.”16
When PEPFAR was reauthorized in the Lantos-Hyde Act of 2008, the limitation on funds was preserved as previously written in the authorizing legislation. The requirement for a new Five-Year Strategy in the reauthorization specified that the strategy should “make the reduction of HIV/AIDS behavioral risks a priority of all prevention efforts”17 in part by “educating men and boys about the risks of procuring sex commercially”18 and by “supporting comprehensive programs to promote alternative livelihoods, safety, and social reintegration strategies for commercial sex workers and their families.”19 The reauthorization legislation also charged the U.S. Global AIDS Coordinator to work “with partner countries in which the HIV/AIDS epidemic is prevalent among individuals involved in commercial sex acts to establish, as a national priority, national prevention programs, including education, voluntary testing, and counseling, and referral systems that link HIV/AIDS programs with programs to eradicate trafficking in persons and support alternatives to prostitution.”20
The application of the law to U.S.-based organizations has been challenged in court, and, under the most recent ruling, the U.S. Court of Appeals for the Second Circuit held that the pledge requirement infringes on the First Amendment rights of the plaintiff-appellee nongovernmental organizations (NGOs).21 As a result, the government is currently prohibited from enforcing the pledge requirement against most U.S.-based recipients of PEPFAR funds.
__________________
13Supra, note 3 at ![]() 301(e).
301(e).
14Supra, note 3 at ![]() 301(f).
301(f).
15Supra, note 3 at ![]() 301(e).
301(e).
16Supra, note 3 at ![]() 101(a)(4).
101(a)(4).
17Supra, note 1 at ![]() 101(a), 22 U.S.C. 7611(a)(12).
101(a), 22 U.S.C. 7611(a)(12).
18Supra, note 1 at ![]() 101(a), 22 U.S.C. 7611(a)(12)(F).
101(a), 22 U.S.C. 7611(a)(12)(F).
19Supra, note 1 at ![]() 101(a), 22 U.S.C. 7611(a)(12)(H).
101(a), 22 U.S.C. 7611(a)(12)(H).
20Supra, note 1 at ![]() 102(2)(F), 22 U.S.C. 2651(f)(2)(B)(ii)(XI).
102(2)(F), 22 U.S.C. 2651(f)(2)(B)(ii)(XI).
21 Alliance for Open Soc’y Int’l, Inc. v. U.S. Agency for Int’l Dev., 651 F.3d 218, 235 (2d Cir. 2011) cert. granted, 133 S. Ct. 928, 184 L. Ed. 2d 719 (U.S. 2013).
A subsequent section will further discuss the consequences of the legislation’s limitation on funding to organizations, which is often called the “anti-prostitution pledge” and has received strong criticism from global health advocates and some program implementers over concern that it restricts the funding for and provision of evidence-based HIV services and activities for men, women, and transgendered persons engaged in sex work.
Guidance PEPFAR does not issue specific programmatic guidance on activities for sex workers. PEPFAR supports activities for this population primarily within its prevention of sexual transmission portfolio, and sex workers are covered within the guidance documents previously described as one of the populations to consider when implementing prevention interventions. In addition, although this population is not named explicitly in PEPFAR’s documentation of its gender strategy (OGAC, 2012d), there is an increasingly articulated intersection with PEPFAR’s gender-focused efforts and activities, as evidenced by the inclusion of sex workers in the U.S. Agency for International Development’s (USAID’s) recent technical documents focused on integration of gender strategies into HIV programs for populations at elevated risk (USAID, 2011b) and on integrating multiple PEPFAR gender strategies to improve HIV interventions (USAID, 2011a).
It is also worth noting that in some partner country settings there are high rates of injection drug use among sex workers, and there are efforts to provide them PEPFAR-supported services for people who inject drugs. (Injection drug use is discussed later in this chapter.) In addition, individuals who engage in sex work who are HIV-positive are also in need of HIV care and treatment services, which in many partner countries are supported by PEPFAR. The USAID technical document on integrating gender strategies recommends providing comprehensive services to this population, emphasizing that
Addressing the particular challenges sex workers face is essential to slowing the epidemic in many communities. Sex workers, regardless of the illegality of their work or status in a country, require comprehensive, stigma-free, and safe services. Moreover, comprehensive services should support, where possible, sex workers’ access to alternative livelihoods. (USAID, 2011a, p. 11)
It notes that “few services such as HIV care and treatment, HIV testing and counseling, and legal protection are available” to sex workers and that “as a result, in many communities, both the supply of and demand for sex work play a significant and unchecked role in spreading the epidemic for all members of the community, including sex workers themselves, their
male clients, the wives of these men, and the other partners of both men and women” (USAID, 2011a, p. 11).
Effects of PEPFAR-Supported Activities for Sex Workers
In nearly all PEPFAR partner countries visited, interviewees identified sex workers—most frequently women, but, in some cases also men and transgendered persons—as important focus populations for the HIV response (240-9-USG; 331-7-PCNGO; 587-7-PCGOV; 196-8-ML; 116-1-USG; 166-5-USG). In many cases it was also emphasized that individuals may belong to multiple populations at elevated risk; in particular, sex workers who also inject drugs and MSM who are engaged in sex work were identified as populations with distinct needs (240-9-USG; 331-7-PCNGO; 396-27-PCGOV; 396-37-USNGO; 196-25-PCNGO). Some interviewees noted that it was a challenge to get all stakeholders, and in particular partner country governments, to recognize the vulnerability of sex workers as part of the HIV response and to garner the political will to include appropriate efforts for them. In some cases stakeholders preferred instead to focus on the general population or on children and youth (542-9-PCGOV; 587-ES; 166-5-USG).
Educational activities and peer outreach targeted at sex workers were important components of PEPFAR’s efforts; engaging with and educating pimps, brothel owners, clients, and other non-paying sexual partners was also emphasized as important (331-14-USG; 396-36-PCGOV; 196-10-PCGOV; 196-19-PCNGO; 196-24-PCNGO; 196-25-PCNGO; 542-9-PCGOV; 166-27-PCNGO). As one interviewee noted, ‘most female sex workers know that condoms can prevent transmission’ but ‘often the clients do not want to use condoms. It’s difficult from the bargaining position to convince the clients to use condoms’ (196-10-PCGOV). Multiple interviewees described efforts to improve sex workers’ negotiation skills and to empower them to request the use of condoms with their clients as well as to provide more general skills training and empowerment (196-23-PCNGO; 396-36-PCNGO; 587-21-PCNGO; 240-22-PCNGO). One challenge identified was that low-cost or free condoms are not sufficiently available or accessible (396-36-PCGOV; 196-6-USG). Program implementers were working to address this limitation in access to prevention services, such as one example, where condom distribution was brought closer to the brothels in which sex workers operated (196-6-USG). Another frequently noted challenge was that sex workers are highly mobile and often don’t have stable housing, making consistent access to services difficult (196-24-PCNGO; 196-25-PCNGO).
Across countries, interviewees described seeing some successes as a result of the efforts of civil society organizations and other partners that work with sex workers, including sex workers who are now successfully negotiating condom use and have started buying condoms when free condoms are not available; interviewees also described seeing declining HIV prevalence and fewer deaths from HIV in sex worker communities (396-36-PCGOV; 396-37-USNGO; 196-19-PCNGO; 542-9-PCGOV). Several local civil society organizations,
many of which were established and run by sex workers, noted the positive role of PEPFAR in supporting and empowering them to provide assistance and services to sex workers as well as to engage with local governments and influence policy (396-8-PCNGO; 196-19-PCNGO; 196-24-PCNGO; 196-25-PCNGO). Operational challenges for civil society organizations, including limits in the opportunities available for civil society organizations to be funded through partner country government mechanisms was described as a difficulty; as a result, these organizations were entirely dependent on external donors or other sources of revenue (542-9-PCGOV; 196-10-PCGOV; 196-ES; 396-ES; 240-ES).
While activities for sex workers are organized under PEPFAR’s prevention portfolio, individuals who engage in sex work also need other services, and PEPFAR-supported program implementers in several countries have been responsive to this through referrals, mobile testing clinics, the building of networks and relationships with facilities, and the direct provision of health services to this population, including STI services, ART services, and PMTCT services (196-10-PCGOV; 196-19-PCNGO; 196-21-PCGOV; 196-24-PCGOV; 166-27-PCNGO), although unmet needs for reproductive health and STI services were also noted (396-36-PCGOV). Programs to offer vocational and other training activities to persons engaged in sex work to help them find alternate sources of income are also supported by PEPFAR; though, one challenge identified was supporting activities that were successful enough to allow beneficiaries to match even the very low income levels they were able to derive from sex work (196-9-USNGO; 166-27-PCNGO; 935-16-USNGO; 240-29-USNGO).
Interviewees across countries described stigma or discrimination faced by sex workers, which led to such experiences as harassment and violence and rejection by their families (587-21-PCNGO; 166-5-USG; 196-24-PCNGO; 542-9-PCGOV). Accessing health services was highlighted by interviewees in several countries as a key challenge for sex workers (196-9-USNGO; 587-21-PCNGO; 396-37-USNGO), and one reason given for this was stigmatization, which made them less likely to go to a facility (587-21-PCNGO; 196-9-USNGO).
One major challenge, not specific to PEPFAR, is that there is very little data on this population. As a result, it is difficult to determine whether their HIV prevention, treatment, and care needs are being adequately covered, and the lack of information was sometimes used as a rationale for not supporting additional activities (396-24-USNGO; 636-6-USG). Interviewees lamented the lack of reliable population size estimates, and the high mobility of this population, in addition to discrimination and stigma, were noted as contributing to the limited availability of epidemiological data on sex workers in general and, in particular, on sex workers with overlapping risk, especially people who inject drugs and MSM (166-5-USG; 396-24-USNGO; 240-9-USG; 331-7-PCNGO; 396-37-USNGO). In some countries PEPFAR has supported or is supporting special studies or surveys to try to address this gap and to help target interventions and influence policy and planning for activities targeted
to sex work as part of the response (196-24-USNGO; 935-16-USNGO; 542-9-PCGOV; 116-8-USG; 396-24-USNGO). Within PEPFAR there are also limited data. PEPFAR’s program-monitoring system includes few indicators that are relevant for supported activities for this population; none that are centrally reported to OGAC. There is also little available data on outcomes to assess the effectiveness of the activities supported by PEPFAR.
Interviewees described the previous requirement to allocate a specified proportion of prevention funding to “abstinence” and “be faithful” programs as a former limitation, and they highlighted the inherent mismatch between an abstinence/be faithful approach and programs for individuals engaged in sex work (396-39-USG; NCV-24-USNGO). Interviewees acknowledged that the lifting of the required budgetary allocation earmark in the reauthorization legislation afforded country programs and implementing partners greater flexibility in planning prevention portfolios and providing programs for this population, whether as part of the effort to address the major drivers in a concentrated epidemic or as an important population to target for interventions and services within generalized epidemics (396-39-USG).
Conclusion: There is recognition in PEPFAR of the important role of efforts for sex workers as a part of the national response in both concentrated and generalized epidemics. There are some examples of success as a result of PEPFAR-supported activities for this population, and increased flexibility for prevention programming with the elimination of the budget earmark for abstinence and be faithful programs in PEPFAR II has enabled country programs to more readily plan activities for sex workers.
Consequences of the Legislative Limitation on PEPFAR Funds
A major issue that is often raised in relation to PEPFAR’s efforts for sex workers is the legislative limitation on providing funding to any group or organization that does not have a policy explicitly opposing prostitution and sex trafficking.22 Although PEPFAR has supported programs and partner organizations in efforts for sex workers, nonetheless there is concern that the legislative limitation on funding has been an impediment to PEPFAR’s work on prevention of HIV transmission for this population (NCV-22-USNGO; NCV-24-USNGO). This committee’s assessment was limited to the activities and efforts for sex workers that PEPFAR has funded, consistent with the congressional mandate to evaluate the “efforts that are supported by United States funding.”23 Therefore, although the committee
__________________
22Supra, note 3 at ![]() 301(f).
301(f).
23Supra, note 1 at ![]() 101(c), 22 U.S.C. 7611(c)(2)(A)(ii).
101(c), 22 U.S.C. 7611(c)(2)(A)(ii).
recognized the important issues and concerns raised by the legislative limitation, given the entirety of the scope to be covered in this evaluation, it was not feasible to conduct the data gathering and analysis for the kind of complex, comprehensive assessment in the policy, legal, stakeholder perspective, and health-outcomes domains that would be needed to draw conclusions about the effects on the HIV response and HIV epidemic in partner countries of the legislative restriction and of what PEPFAR has not funded as a result.
Nonetheless, the committee reflects here the concerns that have been expressed in the global health community, where there has been strong criticism of the legislation and the resulting implementation and enforcement of it through USAID and Department of Health and Human Services policies (Brennan Center for Justice, 2012; CHANGE, 2008; Evertz, 2010; Law Students for Reproductive Justice, 2012; UNDP, 2012). Regarding the public health effects of the legislative limitation, there is concern that the restriction has meant that organizations created by sex workers themselves, that could be providing services and are uniquely positioned to access this population, have been excluded from PEPFAR’s efforts, as have activities to limit the severity of criminal penalties for sex workers, penalties that can interfere with HIV-related services and outcomes. These efforts have been restricted even though their inclusion would not necessitate a direct link to promoting the legalization of prostitution. This exclusion is seen by a range of stakeholders in the global health community as impeding access to HIV services for sex workers and as a missed opportunity for PEPFAR to more effectively contribute to the HIV response in partner countries and to the reduction of HIV transmission (Brennan Center for Justice, 2012; CHANGE, 2008; Evertz, 2010; Law Students for Reproductive Justice, 2012; UNDP, 2012).
Men Who Have Sex with Men
Included within PEPFAR’s prevention of sexual transmission efforts is another population that is at elevated risk and bears a disproportionate burden of HIV disease, men who have sex with men. HIV prevalence for MSM is significantly higher than it is among the general population in all regions of the world (Beyrer et al., 2012). There are several factors that contribute to the increased rate of HIV infection in MSM, including the increased biological risk of HIV transmission via unprotected anal sex as well as behavioral risk factors and lack of access to services, both of which are compounded by stigma and discrimination, socio-cultural norms, and national laws and policies (AMFAR, 2010; Beyrer et al., 2012; Grulich and Zablotska, 2010).
PEPFAR has supported some activities for this population since its inception. From 2004 to 2010, information on activities for HIV prevention with MSM was incorporated into overarching guidance documents and the annual Country Operational Plan guidance, where MSM were identified as one of many populations that may be at elevated risk of HIV acquisition through sexual transmission (OGAC, 2004a, 2005a,c, 2006b, 2007a, 2008a). In 2011, as a supplement to the updated prevention of sexual transmission guidance discussed previously, OGAC also released its Technical Guidance on Combination HIV Prevention for Men Who Have Sex with Men (OGAC, 2011d). This document articulated a new six-part comprehensive prevention approach to be applied going forward: “community-based outreach; distribution of condoms and condom-compatible lubricants; HIV counseling and testing; active linkage to health care and antiretroviral therapy; targeted information, education and communication; and sexually transmitted infection prevention, screening and treatment” (OGAC, 2011d, p. 5).
As noted above, there were no PEPFAR programmatic indicators for monitoring prevention of sexual transmission efforts specifically for MSM until 2010 when, as a part of the NGIs process, a new required measure was introduced for the number of persons reached with individual and/or small group–level interventions with disaggregation by population at elevated risk. As a result, longitudinal program-monitoring data on activities and outputs for MSM are not available.
Data from semi-structured interviewees provided insight into the types of prevention activities supported by PEPFAR for MSM and into some of the effects of these activities. Multiple interviewees described general prevention efforts for MSM as components of their programs (240-9-USG; 331-14-USG; 331-18-USNGO; 166-5-USG; 396-5-USNGO), including activities to increase access for MSM to condoms (331-14-USG; 196-25-PCNGO), behavior change campaigns (331-14-USG; 166-5-USG), support for prevention programs for male sex workers (196-25-PCNGO), and programs to encourage HIV testing and address stigma in local communities (331-7-PCNGO; 196-25-PCNGO). Across different types of services, the use of peer educators was highlighted as a key positive element of many MSM outreach activities (331-7-PCNGO; 331-14-USG; 166-5-USG; 196-25-PCNGO) as was PEPFAR support for local civil society and nongovernmental organizations working with this population (331-22-PCNGO; 196-25-PCNGO).
One major challenge noted by interviewees is that there is also limited data on this population. Similar to its efforts for sex workers, PEPFAR has responded to this challenge in several countries where it has supported or is planning to support special studies, surveillance activities, and pilot studies to obtain better population size estimates and other country-specific information on MSM, as well as to increase attention to MSM in the planning
and implementation of the national HIV response (331-ES; 240-ES; 396-ES; 196-ES; 240-9-USG; 166-5-USG; 396-9-PCGOV). For example, in Ghana PEPFAR partnered with the University of California, San Francisco, to support the Ghana Men’s Study, and similar efforts are under consideration in Ethiopia (PEPFAR/Ethiopia, 2010; UCSF, 2012).
As with all populations at elevated risk, the needs of MSM cut across not only prevention programming but also other categories of services supported by PEPFAR, including access to HIV care and treatment. A more comprehensive discussion of PEPFAR’s support for policy, programs, and data collection for MSM can be found in Chapter 8, “Gender.” PEPFAR has recently included MSM in its comprehensive framing for addressing the role of gender in the HIV epidemic and response, emphasizing that “gender norms around masculinity and sexuality also put men who have sex with men (MSM) at increased risk for HIV by creating additional stigma and discrimination that can prevent them from seeking and accessing services” (OGAC, 2012d).
Conclusion: Over time, PEPFAR has increasingly supported data collection efforts and prevention programming for men who have sex with men, which PEPFAR has recently codified in programmatic guidance. Men who have sex with men are recognized as an important population for prevention and other PEPFAR-supported programming.
PREVENTION OF MOTHER-TO-CHILD TRANSMISSION
Background
The United Nations Children’s Fund (UNICEF) has estimated that of the 115 million annual births in low- and middle-income countries, approximately 1.5 million are to HIV-infected women (UNICEF, 2008b). It was estimated that in 2009, 370,000 infections in children were attributable to mother-to-child transmission (MTCT), down from 500,000 in 2001 (UNAIDS, 2010).
In 1994 the results of the first clinical trial demonstrating that antiretrovirals, specifically zidovudine (AZT), could reduce MTCT of HIV-1 became available (Connor et al., 1994). In 1998 UNICEF created 11 pilot programs using AZT for PMTCT (UNICEF, 2008a), and by 1999 it was demonstrated that a single dose of nevirapine administered to a woman in labor in combination with a single dose of nevirapine administered to the newborn could successfully diminish transmission of HIV-1 from women to their infants by approximately 47 percent compared to zidovudine (Guay et al., 1999). Around the same time, work supported by the U.S. Centers
for Disease Control and Prevention (CDC) in Thailand also demonstrated the efficacy of a short course of zidovudine for reducing HIV-1 MTCT (Shaffer et al., 1999). Implementation of the results of these trials marked the beginning of the successful interruption of MTCT of HIV in developing countries, and in the 1990s, support from the private sector and nonprofit organizations led to some of the first PMTCT efforts in the developing world (Spensley et al., 2009).
In the United States it was feasible to rapidly implement testing of pregnant women for HIV and to use recommended ARVs beginning with AZT in l994 (IOM, 1999). Data from the CDC (see Figure 5-2) show the rapid decline in reported pediatric AIDS diagnoses attributable largely to the successful prevention of mother-to-child HIV-1 transmission, with fewer than 200 cases per year of pediatric AIDS reported in the United States since 1999 (CDC, 2012; IOM, 1999). This striking decline demonstrates that even with the earliest ARV regimens it was possible to prevent most MTCT. Over time, PMTCT has been done more efficiently and safely, employing more complex antiretroviral regimens.
Randomized, controlled clinical trials have shown that, in the absence of any antiretroviral treatment, 20–45 percent of infants born to HIV-positive mothers are infected with HIV (WHO, 2010a). When prolonged breast feeding occurs for 18 to 24 months, an estimated 12 percent of HIV infection occurs prior to 36 weeks gestation, 29 percent from 36 weeks
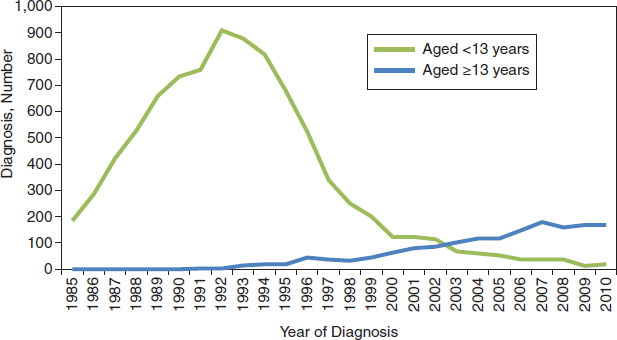
FIGURE 5-2 AIDS diagnoses among perinatally infected persons, 1985–2010, in the United States and six U.S.-dependent areas.
NOTE: All displayed data have been statistically adjusted to account for reporting delays, but not for incomplete reporting.
SOURCE: Adapted from CDC, 2012.
to delivery, 20 percent during delivery, and 39 percent postpartum during breast feeding (Kourtis et al., 2006). Various antepartum, intrapartum, and postpartum regimens with AZT have all been shown to reduce transmission of HIV from mother to infant (Connor et al., 1994; Guay et al., 1999; Lallemant et al., 2000; Petra Study Team, 2002; Shaffer et al., 1999). The administration of an abbreviated antepartum course of zidovudine to the mother (for 4 to 6 weeks) is effective, but is less so than longer courses (Lallemant et al., 2000). When a shorter antepartum course is used, the addition of lamivudine to the mother’s regimen has been shown to increase its effectiveness (Chaisilwattana et al., 2002; Dabis et al., 2005; Mandelbrot et al., 2001). Adding single-dose nevirapine to short-course AZT for the mother may also improve efficacy in breast-fed and formula-fed infants (Dabis et al., 2005; Shapiro et al., 2006), and when the mother does not receive treatment, single dose nevirapine plus AZT for the infant has better efficacy than nevirapine alone (Taha et al., 2003, 2004). Either administering antiretrovirals to a breast-feeding infant or treating the infant’s HIV-infected mother can also greatly reduce transmission during breast feeding (Chasela et al., 2010; Kumwenda et al., 2008).
WHO Recommendations to Prevent MTCT of HIV
In 2010 WHO revised its 2006 guidelines for PMTCT and the care of mothers and recommended initiation of ART for all HIV-infected pregnant women with CD4 counts below 350/mm3 (from below 200/mm3 in 2006) or in WHO clinical stage 3 or 4 (WHO, 2006, 2010a). The 2010 WHO PMTCT guidelines recommended that all infants born to women receiving ART should receive either AZT or nevirapine for 4 to 6 weeks and that those mothers who do not need ART for their own health should start ARV prophylaxis as early as 14 weeks of pregnancy, replacing the initiation at 28 weeks in the 2006 recommendations. The 2010 guidelines also recommended two options for PMTCT, Option A and Option B.24 The guidelines placed the responsibility on national authorities to decide whether mothers
__________________
24 Option A includes zidovudine (AZT) antepartum, with nevirapine/AZT/lamivudine (3TC) during labor and delivery. AZT/3TC should then be continued for 7 days postpartum. The infant, if breast fed, should receive nevirapine for a minimum of 4 to 6 weeks from birth until 1 week after exposure to breast milk has stopped. Non-breast feeding infants should all receive either daily infant nevirapine or single dose nevirapine with AZT for 4 to 6 weeks.
Option B includes AZT/3TC/lopinavir/ritonavir or the substitution of abacavir or efavirenz for lopinavir/ritonavir starting from 14 weeks gestation until delivery or until 1 week after exposure to breast milk has stopped if breast feeding. Alternatively tenofovir disoproxil fumarate/3TC or emtricitabine/efavirenz could be used. In Option B, all infants should receive nevirapine or AZT for 4 to 6 weeks.
In both Option A and B, women should be treated according to existing WHO guidelines for treatment initiation (WHO, 2010a).
should breast feed and receive ARVs or avoid all breast feeding with the goal of achieving maximum HIV-free survival for the child. When breast feeding is the best option, it should be exclusive for the first 6 months and then continued with the introduction of appropriate complementary foods; breast feeding should continue until the infant is 12 months of age (WHO, 2010a). In 2012 WHO released a programmatic update to its 2010 guidelines, which included a new third option called Option B+. Option B+ includes the same recommendations for prophylaxis but suggests that ARV treatment for women be continued beyond pregnancy regardless of CD4 count (WHO, 2012a).
PMTCT Coverage
UNAIDS has set a goal of increasing coverage to 90 percent of HIV-positive women with WHO-recommended regimens with the target of decreasing the number of children infected annually to fewer than 43,000 (WHO, 2011). PMTCT programs have expanded over time and are present in most low- and middle-income countries. WHO estimated that only 10 percent of the world’s HIV-positive women had access to PMTCT services in 2004 (WHO, 2008a). The subsequent scale-up in global resources contributed to an increase in PMTCT coverage, and in 2010 an estimated 35 percent of pregnant women in low- and middle-income countries received HIV testing and counseling, with coverage of counseling and testing for pregnant women increasing from an estimated 35 percent to 42 percent between 2009 and 2010 in sub-Saharan Africa (WHO, 2011). In 2009 an estimated 53 percent of pregnant women living with HIV in low- and middle-income countries received antiretroviral medication to prevent MTCT of HIV, up from an estimated 45 percent in 2008 (WHO, 2010b).
There are few countries that provide access to services for at least 80 percent of pregnant women, the target given in the commitment document released following the 2001 UNGASS session (United Nations, 2001; WHO, 2011). Challenges to reaching this goal include establishing services in health systems that are not optimally staffed; ensuring a reliable supply chain for diagnostics and ARVs; and having the essential funds to support the necessary costs of implementation (UNAIDS, 2011). The knowledge of how to virtually eliminate pediatric HIV transmitted from mother-to-child currently exists; the greatest gap is in providing access to services. Figure 5-3 illustrates the cascade of services that, if available and accessible to pregnant women, can maximize children’s HIV-free survival and improve maternal health (Stringer et al., 2008).
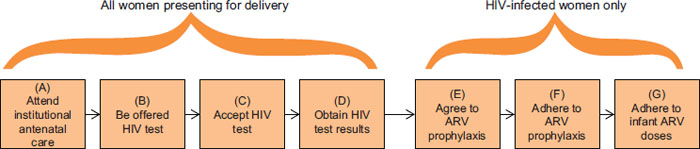
FIGURE 5-3 PMTCT cascade.
NOTE: ARV = antiretroviral.
SOURCE: Stringer et al., 2008. Used with permission.
PEPFAR’s PMTCT Efforts
Building on the success of the MTCT initiative started by President Bush in 2002, the 2003 authorizing legislation emphasized that MTCT of HIV was largely preventable and directed PEPFAR to support activities for this purpose,25 with the aim of “meeting or exceeding the goal to reduce the rate of mother-to-child transmission of HIV by 20 percent by 2005 and by 50 percent by 2010.”26 In 2008 the reauthorizing legislation added the goal of helping “partner countries in the effort to achieve goals of 80 percent access to counseling, testing, and treatment”27 for PMTCT. PEPFAR was directed to support countries to reach “80 percent of pregnant women for prevention and treatment of mother-to-child transmission of HIV in countries in which the United States is implementing HIV/AIDS programs by 2013” and to promote “infant feeding options and treatment protocols that meet the most recent criteria established by the World Health Organization.”28
PEPFAR’s PMTCT activities have evolved with the changing evidence base, and PEPFAR has endorsed the adaptation of the updated 2010 WHO PMTCT guidelines described above into their programming (OGAC, 2011c). PEPFAR defers to the WHO normative guidelines and itself issues only PMTCT-specific operational guidance. PEPFAR implementers may offer Option A or Option B, and some sites, including several in Malawi, have begun to roll out Option B+, with initial data confirming the feasibility of implementation, though challenges exist (Chinkonde-Nkhoma et al., 2012; Holmes, 2012).
To support the scale-up of PMTCT and pediatric HIV services, PEPFAR currently organizes its activities around addressing three distinct aims mandated by the reauthorization legislation: “a) support HIV testing and counseling for 80% of pregnant women in countries most affected by HIV/
__________________
25Supra, note 3 at ![]() 301(a)(2), 22 U.S.C. 2151(d)(1)(E).
301(a)(2), 22 U.S.C. 2151(d)(1)(E).
26Supra, note 3 at ![]() 312(b)(1).
312(b)(1).
27Supra, note 1 at ![]() 101(a), 22 U.S.C. 7611(a)(4)(D).
101(a), 22 U.S.C. 7611(a)(4)(D).
28Supra, note 1 at ![]() 301(c)(1)(E), 22 U.S.C. 2151b-2(d)(1)(F).
301(c)(1)(E), 22 U.S.C. 2151b-2(d)(1)(F).
AIDS; b) support antiretrovirals (ARVs) for PMTCT and/or their own health as medically indicated for 85% of HIV-positive pregnant women in those countries; and c) ensure that the proportion of children receiving care and treatment meets their proportion of the HIV-infected individuals in each country” (OGAC, 2011b, p. 1). In order to accomplish these goals, PEPFAR not only supports efforts in partner countries but also works in concert with international partners, such as through its support of the UNICEF Inter-Agency Task Team and through PEPFAR’s contribution to the 2011 Global Plan Towards the Elimination of New HIV Infections Among Children by 2015 and Keeping Their Mothers Alive (OGAC, 2011c; UNAIDS, 2011). The centrality of PMTCT activities to PEPFAR’s overall prevention programming was reinforced as part of the recent “AIDS-Free Generation” goals articulated by the U.S. government (OGAC, 2012c).
PEPFAR’s Contribution to the Scale-Up and Coverage of PMTCT Services
Two centrally reported programmatic indicators requested and provided to the committee by OGAC serve to assess PEPFAR’s contribution to the scale-up and delivery of PMTCT services. These indicator data show that, in the 31 countries that are the focus of this evaluation, the number of pregnant women who received PEPFAR-supported HIV counseling and testing for PMTCT and who received their test results increased from approximately 600,000 in FY 2004 to more than 7.3 million in FY 2009. The number of pregnant women who received PEPFAR-supported antiretroviral prophylaxis for PMTCT increased from nearly 48,000 in FY 2004 to more than 600,000 in FY 2010.
The indicator for the number of pregnant women tested was no longer reported after 2009 as a result of the Next Generation Indicator revision process in 2009; instead, a revised indicator reports the number of pregnant women with known HIV status, including women who were tested for HIV and received their results, as well as pregnant women with already known HIV status who attended antenatal care (ANC) services (OGAC indicator P1.1D) (OGAC, 2009c). Rather than a count of HIV tests provided to pregnant women, this provides a measure of the pregnant women whose eligibility for PMTCT is known. Although not centrally reported, disaggregation by those who are HIV-positive is recommended at the program implementation level. Going forward, this could serve as a denominator to assess the coverage in PEPFAR-supported programs of pregnant women who receive ARC prophylaxis for PMTCT. However, this indicator was added too recently to provide an assessment of coverage over time for this evaluation.
As a broad assessment of PEPFAR’s contribution to the national coverage of PMTCT services in partner countries, Figure 5-4 shows PMTCT coverage in the 31 countries included as the focus for this evaluation from 2006 to 2009 (the years for which the best data were available at the time of the committee’s assessment). The annual figures for national coverage, inclusive of PEPFAR, and PEPFAR’s contribution to overall coverage were obtained by combining two publicly available indicators from the UNAIDS UNGASS reporting system: the national number of HIV-positive pregnant women receiving antiretroviral prophylaxis for PMTCT divided by the national estimated number of HIV-positive pregnant women. The annual figures for PEPFAR coverage alone were obtained by dividing PEPFAR’s programmatic indicator for pregnant women who received ARV prophylaxis for PMTCT (OGAC indicator 1.3) by the same UNGASS indicator
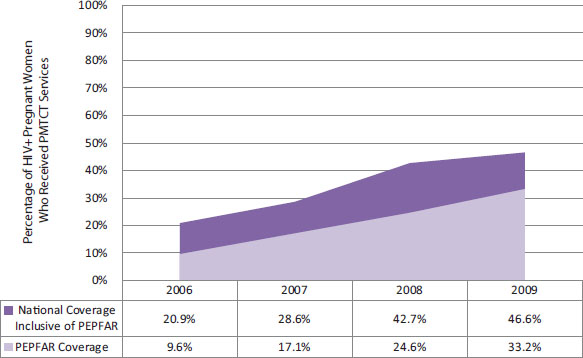
FIGURE 5-4 PEPFAR’s contribution to PMTCT coverage, 2006 to 2009 (aggregate data from 31 countries).
NOTES: This figure represents data from the 31 countries identified as the focus of this evaluation (see Chapter 2). Several adjustments were made in order to compare the data from OGAC and UNAIDS.
(1) When countries did not report PEPFAR programmatic data for a given year, this was interpreted as “0.”
(2) If the reported number of women reached with PMTCT by PEPFAR exceeded the reported national number of women reached with PMTCT, the committee set the reported national value equal to the reported PEPFAR PMTCT value. This occurred for four countries in 2006, three countries in 2007, and three countries in each 2008 and 2009.
(3) If the estimated national number of HIV-positive pregnant women or the national number of women reached with PMTCT services were missing or implausible, the committee created an estimate on the basis of available UNGASS indicator values from the surrounding years. Two countries were missing values in 2006, eight in 2007, two in 2008, and three in 2009.
SOURCE: Program monitoring indicators provided by OGAC; also UNAIDS, 2012a.
| Year | Estimated # of HIV+ Pregnant Women (National) | # HIV+ Pregnant Women Receiving ARV Prophylaxis for PMTCT (National) | # HIV+ Pregnant Women Receiving ARV Prophylaxis for PMTCT (PEPFAR) | PEPFAR Contribution to Overall PMTCT Services | |
| 2006 | 1,541.7 | 321.5 | 147.3 | 46% | |
| 2007 | 1,436.6 | 410.9 | 245.5 | 60% | |
| 2008 | 1,563.0 | 667.3 | 384.4 | 58% | |
| 2009 | 1,534.2 | 714.3 | 509.8 | 71% | |
NOTES: This figure represents data from the 31 countries identified as the focus of this evaluation (see Chapter 2). Several adjustments were made in order to compare the data from OGAC and UNAIDS.
SOURCE: Program monitoring indicators provided by OGAC; also UNAIDS, 2012a.
used as the denominator above, the national estimated number of HIV-positive pregnant women.
On average, more than half of all PMTCT services provided each year are supported by PEPFAR, and in 2009 PEPFAR contributed to supporting about 71 percent of all women receiving ARV for PMTCT in these partner countries (see Table 5-4).
Estimated and observed results from several studies conducted in PEPFAR partner countries have demonstrated not only successful efforts to scale up PMTCT services, but also a positive impact of PMTCT on the reduction of HIV transmission to infants, including in operational settings. Studies in Kenya, Swaziland, and Zambia have highlighted the feasibility and effectiveness of implementing PMTCT programs in underresourced settings (Azcoaga-Lorenzo et al., 2011; Bancheno et al., 2010; Stringer et al., 2003). In Nigeria, a retrospective review of records of 702 mother–infant pairs enrolled in PMTCT programs across six health facilities found that mothers who received ARVs were eight times less likely to transmit HIV to their children than those who did not receive treatment (Anoje et al., 2012). Another study in Haiti used mother–infant pair records from the primary HIV testing and treatment center in Port-au-Prince and found that in the group of those who completed the PMTCT program, MTCT was 9.2 percent, significantly lower than Haiti’s historical transmission rate of 27 percent (Deschamps et al., 2009). Additional studies of PMTCT program effectiveness in South Africa, Angola, and Zambia have found that these programs led to reduced vertical transmission rates in real settings that were consistent with the results of clinical trials using similar drug regimens (Coetzee et al., 2005; Colvin et al., 2007; Lussiana et al., 2012; Torpey et al., 2010). A recent population-based study evaluated PMTCT coverage and HIV-free infant survival in 26 communities throughout Côte d’Ivoire, South Africa, Cameroon, and Zambia using community surveys and testing to collect data on 7,985 infants. It found that community PMTCT coverage
was moderately correlated with HIV-free survival of 24-month-old children, and that a potent ARV regimen was the co-factor most strongly associated with the prevention of vertical transmission and child survival at 24 months (Stringer et al., 2013).
Interviewees from country visits consistently noted the increase in PMTCT services over time and the impact of this on reducing HIV transmission to infants, and they emphasized PEPFAR’s contribution to this achievement (240-13-PCGOV; 331-38-USPS; 587-2-USG; 587-5-PCGOV; 636-2-USG; 636-9-USACA; 636-16-USG; 272-22-USG; 272-24-USG; 461-4-USG; 461-17-PCNGO; 934-17-PCGOV).
Conclusion: PEPFAR support for the scale-up of services for prevention of MTCT has made a major contribution to meeting the need in partner countries.
Even with the major increase over time in the number of pregnant women receiving services, the data in Figure 5-4 and Table 5-4 also show that overall coverage for PMTCT is still well below what is needed in PEPFAR partner countries. Overall coverage of PMTCT services from all actors in the response was less than 50 percent in 2009 in the 31 countries under review, which is well below PEPFAR’s stated goal of supporting the provision of ARV prophylaxis for PMTCT for 85 percent of eligible women by 2013. This is consistent with the reality that, given the current rate of global scale-up, the world is not on track to meet the global target of 80 percent coverage in the near future.
Indeed, despite the large scale-up and increase in access to PMTCT, challenges remain with PMTCT service delivery and access. Studies on PMTCT services in PEPFAR partner countries have identified sub-optimal coverage and follow-up rates and have noted contributing factors such as socioeconomic factors, staff shortages, adherence, and other service delivery factors (Azcoaga-Lorenzo et al., 2011; Bancheno et al., 2010; Colvin et al., 2007; Doherty et al., 2005; Lussiana et al., 2012). Challenges with access and service delivery were also highlighted by interviewees across countries. In many locations, part of this challenge was due to women being more likely to seek prenatal care in places other than at an antenatal clinic or hospital, which then limits access to PMTCT if it is provided only in those facilities. The cultural practice of having children at home was identified as one driver of this decision (240-12-USG). In several countries, interviewees highlighted difficulties in reaching pregnant women in geographically remote regions (587-5-PCGOV) and pointed to distance and transportation as challenges for women in accessing PMTCT services (240-2-USG; 240-13-PCGOV; 240-19-USACA; 240-24-USG; 636-2-USG; 461-7-PCNGO; 396-42-PCGOV). Lack of road infrastructure (461-7-PCNGO) and topographical barriers such as mountains prevented patients from reaching facilities. Additionally, participants
noted that the cost of obtaining transportation and staying overnight near services made it prohibitively expensive for women to deliver in settings other than their homes (240-24-USG; 461-7-PCNGO). Other challenges identified included staffing (587-5-PCGOV; 116-18-PCNGO) and the quality of PMTCT services, service providers, and facilities (240-5-PCGOV; 240-13-PCGOV; 240-19-USACA; 240-24-USG; 461-7-PCNGO)—for example, unclean facilities that were not perceived as patient friendly (240-5-PCGOV).
Gender-related issues, including gender-based violence, emerged as a theme among participants because of their effects on the access of women and infants to services. Gender dynamics, including their intersection with access and service delivery, are discussed in greater detail in Chapter 8, but the following quote is revealing:
“The culture is very machismo here. [. . .] And you’ll see a lot of women who are victims of domestic violence. They get HIV through that. They are very scared to disclose. And wouldn’t protect their baby because of that, or wouldn’t use replacement feeding because of those reasons. But you hear a lot of this anecdotally and through the health care workers. And so those are very complex issues to address. And we’ve only, like, touched on them.” (587-5-PCGOV)
Interviewees offered a variety of potential solutions for addressing the limitations in PMTCT access. Interviewees in multiple countries noted the approach of creating demand for PMTCT services through communication and behavior change messaging, which has been supported by PEPFAR (240-19-USACA; 331-43-USG; 636-16-USG). Others stated that it was seeing the success of PMTCT itself and the impact within communities of seeing a baby born HIV-negative that influenced women’s decisions to seek access to services (396-21-USG; 934-17-PCGOV). Other approaches included allowing maternal and child health (MCH) nurses to provide ARVs to pregnant women (166-29-PCGOV) and using mobile clinics to reach pregnant women in remote regions (587-5-PCGOV). Another approach supported by UNICEF has been to offer pre-packaged PMTCT drugs and materials for women to take home at their first visit; this accommodates the fact that women typically attend only a single ANC visit during their pregnancy (Kelland, 2010; UNICEF, 2012).
Challenges and Successes of Integration of PMTCT with Other Services
As a part of the campaign for scaling up universal access to PMTCT services, WHO recommends that “[n]ational programmes should establish the necessary links to ensure large-scale access to a comprehensive package of services defined according to local context, including epidemiology and available resources” (WHO, 2007, p. 15). WHO places special emphasis
on integrating family planning services into HIV prevention and care programs in order to maximize the potential health benefits of these activities (WHO, 2007). Evidence supporting improved health outcomes as a result of PMTCT integration is limited, but several studies comparing service uptake in integrated versus standalone care have shown positive results (Tudor Car et al., 2012).
PEPFAR has endorsed the WHO recommendations, and in 2011 it articulated a goal of increasing activities related to integration, with its release of Guidance on Integrating Prevention of Mother-to-Child Transmission of HIV, Maternal, Neonatal, and Child Health and Pediatric HIV Services (OGAC, 2011b). The guidance recognizes that the evidence base for integration methods and outcomes is still emerging, but it recommends an integrated package of services for women, including voluntary family planning; provider-initiated HIV testing and counseling; routine ANC, malaria, and tuberculosis services; nutrition counseling; prophylaxis for women who test HIV positive through completion of breast feeding for PMTCT; and ARV treatment for women who are eligible (OGAC, 2011b). For children up to age 5, the package includes essential newborn care, counseling and testing, ARV therapy for those eligible, and social services for OVC (OGAC, 2011b).
Interviewees in several different partner countries described the integration of PMTCT activities into other health service delivery platforms. The most common of these were antenatal care (240-2-USG; 636-16-USG; 116-4-USG; 272-24-USG) and maternal and child health (587-5-PCGOV; 166-10-USNGO; 396-21-USG); other examples included family and children’s health care (240-3-USG; 331-44-USNGO), tuberculosis services (636-17-PCGOV), and the overall health system (587-10-USG; 587-12-USG; 396-21-USG). Participants noted that integration was associated with health systems strengthening and sustainability (331-2-USG; 587-6-CCM; 636-9-USACA; 396-21-USG), including improvements in infrastructure to integrate PMTCT into antenatal care and MCH (240-19-USACA; 166-10-USNGO).
Specific examples of successes related to the integration of PMTCT in other health services included ‘strong commitment from the government to integrate HIV services for children’ (240-24-PCGOV) and increasing ‘the capacity of maternal and child health’ (396-21-USG). Capacity building occurred through the training of health workers in skills in maternal and child health, as well as in the referral of children to care and treatment services (587-5-PCGOV; 166-10-USNGO; 396-21-USG; 396-42-PCGOV; 934-17-PCGOV; 587-5-PCGOV; 166-10-USNGO). The incorporation of PMTCT training into training for health care workers was also important, including the development of manuals and curricula (240-24-USG; 587-5-PCGOV):
“And then integrated in the sense that there are a lot of people trained in MCH. There are general nurses that are also trained in
PMTCT. And then we’re administratively integrated into MCH.” (587-5-PCGOV)
Additionally, improving the patient experience (934-15-PCGOV) and meeting obstetric needs (934-44-PCACA) were offered as successes:
“I think it’s been positive because what has often happened is with the integration of HIV services within health centers, within district hospitals, it becomes very difficult to isolate someone who comes for obstetric needs or services from someone who comes for purely HIV needs. Obstetrics is a good one because everybody then goes through evaluation of the PMTCT program.” (934-44-PCACA)
Several interviewees cited the challenges of integration of PMTCT services (240-24-USG; 587-2-USG; 587-5-PCGOV; 196-8-ML; 636-9-USACA; 461-18-USG). ‘PEPFAR is being implemented in a system that is far from perfect,’ noted one (587-2-USG), and another noted that standalone PMTCT sites still exist, necessitating referrals to other health facilities (587-5-PCGOV), and that integration with family planning was difficult (240-24-USG). Another concern expressed was the potential decline in quality of services for both MCH and PMTCT after integration:
“Yeah, there have been concerns, obviously. That sometimes when you integrate the quality of care, yeah, may actually diminish. When you have a specialized person who is focusing on PMTCT, the person does a better job [. . .]. So people are a bit worried in terms of how well will be the quality.” (934-10-PCGOV)
Finally, the integration of PMTCT data collection into existing, often administratively divided, systems was identified as a challenge that had to be addressed, with some success attributed to PEPFAR’s efforts (196-8-ML; 461-14-USG; 587-5-PCGOV), for example, through support for revised and standardized registers that integrate tracking of information for both general ANC and PMTCT (587-5-PCGOV).
Conclusion: Integration of PMTCT into maternal and child health is occurring and is a sign of the evolution of the program. However, integration at the facility level with other services is variable, and the link between PMTCT and ART for both women and children is still a challenge.
The linkages from PMTCT to ART services are also discussed in Chapter 6, “Care and Treatment.” Service integration, including that of PMTCT, is further discussed in Chapter 9 on health systems strengthening.
Background
The United Nations Office on Drugs and Crime (UNODC) estimates that approximately 205 million people use drugs illegally, with more than 10 percent of users meeting the criteria for drug dependence (UNODC, 2008). Use of injection as the primary mode of drug consumption introduces specific health risks, such as venous collapse and ulcers, hemorrhage due to inadvertent injection into the artery, increased risk of blood-borne infections including HIV and viral hepatitis, and bacteremia and septicemia (WHO Regional Office for South-East Asia, 2009). The link between injection drug use and HIV infection is particularly significant and has motivated a robust response from the international health community.
HIV transmission among people who inject drugs occurs primarily through the sharing of used needles and other injection equipment contaminated with HIV, although sexual transmission between drug users and their partners—who may or may not themselves be injectors—is also common and of concern. Because injection drug use is illegal nearly everywhere, it is difficult to measure the prevalence of this behavior, which limits the ability to determine the prevalence (and incidence) of HIV among people who inject drugs. However, in 2008 it was estimated that of the estimated 16 million people who inject drugs worldwide, one-fifth were likely to be HIV positive (Mathers et al., 2008). In countries where injection drug use is the primary driver of the epidemic, HIV prevalence in people who inject drugs may exceed 40 percent (Mathers et al., 2011). Outside of sub-Saharan Africa, transmission via injection drug use is responsible for an estimated 30 percent of all new HIV infections (WHO, 2009a). Given the substantial health and economic burden caused by HIV, addressing the risks of drug dependency is a key focus for global health programs operating in countries with concentrated HIV epidemics and an increasing focus in countries where illicit drug use is emerging as a driver of HIV transmission within generalized epidemics.
Harm Reduction
In the 1990s polymerase chain reaction (PCR) testing detected HIV on used needles and syringes (Heimer et al., 1992), and mathematical modeling of the circulation of HIV-contaminated syringes used by people who inject drugs (Kaplan and Heimer, 1994) added evidence for advocates and public health practitioners to press governments to permit legal implementation of harm reduction strategies as a way to prevent HIV transmission among people who inject drugs. However, UNAIDS estimated that only 19 percent
of individuals at risk of injection drug use–related HIV acquisition had access to harm reduction interventions in 2001 (Global HIV Prevention Working Group, 2003), and the adoption of harm reduction approaches has remained politically and culturally controversial and has varied among countries (Auerbach, 2009).
Harm reduction strategies may include sterile needle and syringe exchange programs, the relaxation of drug paraphernalia and possession laws, and the provision of medication for substitution therapy (Harm Reduction International, 2012). This harm reduction approach emphasizes the public good in limiting the transmission and acquisition of infectious blood-borne pathogens (i.e., HIV and hepatitis C virus) even while individuals might not be able to successfully stop using drugs altogether, with or without referrals for addiction and substance abuse treatment, although both UNODC and WHO identify drug dependence as a disease that should be addressed with evidence-based treatment options (UNODC, 2008; WHO, 2009a).
Medication-assisted treatment (MAT) is the provision of a daily dose of methadone or buprenorphine to people who are addicted to opiates. Methadone and buprenorphine are synthetic agents that affect the brain receptors that are responsive to heroin and other opiates and block the sedative effect of these drugs, reducing cravings and alleviating the symptoms of opiate withdrawal (CDC, 2002; Kumar, 2012). MAT has been shown to be effective in reducing the extent and frequency of injection and in reducing HIV risk behaviors among people who inject drugs (IOM, 2007b). WHO guidelines state that the provision of methadone as a part of maintenance therapy for people who inject drugs is the minimal acceptable standard for national opioid treatment programs, although ideally both buprenorphine and opioid antagonists should also be made available (WHO, 2009a). MAT also increases patient adherence to antiretroviral treatment (WHO, 2009a).
In addition to voluntary treatment for drug dependence or addiction and detoxification programs that assist or medically monitor patients who stop using drugs and experience withdrawal symptoms, WHO has also recognized the effectiveness of sterile needle and syringe exchange programs in reducing transmission of HIV (WHO, 2004). Despite this recognition, WHO has yet to release comprehensive international guidelines on incorporating these strategies into national policies. In cities with programs to expand sterile syringe access, HIV prevalence among people who inject drugs has been significantly reduced (Hurley et al., 1997).
PEPFAR’s Activities for Prevention with People Who Inject Drugs
The 2003 PEPFAR authorizing legislation was the original document that instructed the program to include activities in its prevention portfolio aimed at addressing “substance abuse and intravenous drug use that can
lead to HIV infection.”29 In response to this legislative authorization, activities focused on people who inject drugs were first incorporated into the annual budget request narrative for “Other Prevention” activities (OGAC, 2004a). Early prevention activities for this population included peer- and community-based outreach and education, especially focused on encouraging people who inject drugs to access voluntary counseling and testing; support to reduce needle sharing; evidence gathering and research; and technical assistance to support policy change and development (PEPFAR/Vietnam, 2004, 2005).
Guidance for the Prevention of HIV for People Who Inject Drugs
The first formal guidance on PEPFAR activities specifically targeting HIV prevention among people who use drugs was released in 2006 (OGAC, 2006d). The guidance document acknowledged the important role that the use of injection drugs played in the HIV epidemic and outlined a three-part strategy of activities that could be supported by PEPFAR. The strategy consisted of tailoring existing prevention of sexual transmission activities and counseling and testing activities to people who inject drugs; supporting substance abuse programs, including medication-assisted treatment; and providing individuals with comprehensive HIV treatment services (OGAC, 2006d). Notably, this guidance prohibited the use of PEPFAR funds for sterile needle and syringe exchange programs (OGAC, 2006d).
The guidance was updated in 2010 in the document Comprehensive HIV Prevention for People Who Inject Drugs, Revised Guidance, which endorsed a modified three-component strategy that included community-based outreach programs; sterile needle and syringe exchange programs; and treatment for drug dependence, such as opioid substitution therapy (OGAC, 2010a). The shift in policy about supporting needle and syringe exchange programs followed a change in U.S. law, when Congress removed the prohibition in 2009. In 2011 the ban on the use of foreign assistance for needle and syringe exchange was included by Congress in the omnibus spending bill for FY 2012, halting the scale-up of these programs for a second time (Harm Reduction International, 2012). Of note, these changes to PEPFAR guidance and U.S. law occurred during the course of the study’s data collection period, and the committee interpreted the available data in light of this evolution.
Communicating the content and intent of changes in this guidance and policy to the field remains a persistent challenge for OGAC and may potentially limit the effectiveness of program implementation. Interviewees in several countries visited, as well as advocates and OGAC headquarters
__________________
29Supra, note 3 at ![]() 301(a)(2), 22 U.S.C. 2151b-2(d)(1)(G).
301(a)(2), 22 U.S.C. 2151b-2(d)(1)(G).
staff, described instances in which a lack of clarity about changes in the guidance led to confusion (396-56-USNGO; 396-59-USG; NCV-19-USG; NCV-24-USNGO). There was awareness of the change in PEPFAR policy related to needle and syringe exchange programs (196-11-USNGO; 396-7-PCGOV; 935-17-USG), but there were also concerns about difficulties due to the lack of clarity on whether scale-up would be able to proceed (196-11-USNGO; 396-2-USG):
“the guidance on needle syringe programming for [this country] is not 100 percent clear. Are we allowed to do it? We were informed [. . .] that perhaps procurement is still not cleared in the latest congressional budget. You know it’s a very different epidemic [. . .] so we really need to understand what the guidance is on that. And of course when there’s a change in administration things change.” (396-15-USG)
PEPFAR-Supported Services for People Who Inject Drugs
In part because of how recently relevant indicators and a dedicated budget code were introduced, it is difficult to determine the scope of PEPFAR’s activities for people who inject drugs over time. Of the 15 original focus countries, 6 described activities that included efforts, beyond improved measurement, for people who inject drugs in their Country Operational Plan narratives in at least 1 year during the first phase of PEPFAR (PEPFAR/Kenya, 2006; PEPFAR/Mozambique, 2006; PEPFAR/Nigeria, 2006; PEPFAR/South Africa, 2006; PEPFAR/Tanzania, 2006; PEPFAR/Vietnam, 2006). In 2009 planned funding for activities for this population was disentangled from other prevention efforts, and a new budget code titled Injecting and Non-injecting Drug Use was created (OGAC, 2010d, 2011e). Select country data extracted by the IOM from Country Operational Plans of the 31 countries that were the focus of this evaluation indicate that 10 countries planned activities under this budget code in FY 2009 and FY 2010. In FY 2011, 12 countries (Cambodia, China, Guyana, India, Indonesia, Kenya, Mozambique, Russia, Tanzania, Thailand, Ukraine, Vietnam) and the Central Asian Region included specific budgets for activities for people who inject drugs in their HIV prevention programming portfolio (OGAC, 2011f). This reflects an expansion of PEPFAR’s efforts in this area, from an initial focus on implementing programs primarily in concentrated epidemics to the development of pilot programs in some countries with generalized epidemics where injection drug use is emerging as an important HIV transmission risk (Nieburg and Carty, 2011). Because these efforts are still in their pilot stages, there were no data available for the committee to include in its assessment of the impact of PEPFAR’s activities. To expand access to HIV services, current PEPFAR prevention efforts for people who inject drugs
include support for activities in an increasing variety of facility and community settings. Services supported include ART and treatment for co-morbidities, including hepatitis B and C; education on safer sexual practices and condom provision; and medication-assisted treatment, which is a focus for PEPFAR (OGAC, 2011c).
Injection drug users were identified as a vulnerable or at-risk group in most countries visited by the evaluation team, regardless of national epidemic type (331-14-USG; 587-7-PCGOV; 196-7-PCNGO; 166-5-USG; 272-6-ML; 935-14-USG; 461-1-USG; 542-8-ML; 396-1-USG). Interviewees described numerous ongoing activities supported by PEPFAR for both HIV prevention and treatment for people who inject drugs. Prevention efforts include the use of peer educators (166-5-USG; 935-17-USG), the provision of condoms (196-6-USG; 196-21-PCGOV), counseling and testing services (196-6-USG; 196-11-USNGO; 196-17-PCGOV), and activities for people who inject drugs in prisons (331-14-USG; 542-6-ML; 196-11-USNGO). As described above, interviewees noted limitations and challenges regarding the use of PEPFAR funds for needle and syringe exchange (935-17-USG; 196-12-PCGOV; 396-56-USNGO; 396-59-USG; 196-11-USNGO; 396-7-PCGOV; 396-2-USG; 396-57-USG). PEPFAR is also supporting substance abuse treatment services in several countries, including efforts to increase access to methadone (196-11-USNGO; 196-14-PCGOV; 542-6-ML; 935-17-USG; 542-8-USNGO) and the provision of a safe space for services (166-5-USG), as well as providing ART for people who inject drugs who are HIV-positive (542-8-USNGO).
Importance of the National Policy Context for Efforts for Prevention for People Who Inject Drugs
The policy environment, which includes the USG policies described above, as well as a partner country’s own laws and policies related to drug users, has been a crucial driver of the response to HIV in PEPFAR-supported countries where transmission among people who inject drugs is a major driver of the epidemic. Criminalization of injection drug use and types of enforcement mechanisms vary greatly in PEPFAR partner countries with concentrated epidemics (Chiu and Burris, 2011). Given the sensitive nature of providing services for people who inject drugs, the policy context within which PEPFAR provides these services can affect program impact. For FY 2012 mission teams were expressly tasked with supporting national governments and NGOs to “address policies that serve as barriers (criminalization for seeking health-care, policy to not initiate ART until patient has stopped using drugs, etc.) or facilitators (use of case managers for service coordination, promotion of drug treatment over criminalization, etc.) to drug-using populations accessing HIV-related services” (OGAC, 2011c, p. 56).
Interview data reflect the effects that the national policy context has had over time on PEPFAR’s efforts to provide HIV prevention services for
people who inject drugs. Although there were variations in the specific effects due to differences in national and local legislation, legal and policy issues were highlighted across countries as a challenge to implementing services for people who inject drugs (196-12-PCGOV; 542-6-ML; 396-2-USG; 396-57-USG). Some interviewees noted that laws within a country were often in conflict with each other and that this conflict sometimes affected service delivery in these locations (396-2-USG; 542-6-ML; 196-ES). As a result, some interviewees identified the need for PEPFAR to work with governmental sectors beyond the Ministry of Health, noting that many other agencies are involved in or have the ability to affect the provision of harm reduction services (396-2-USG; 396-23-USG).
Effects of PEPFAR’s Activities for Prevention Among People Who Inject Drugs
PEPFAR indicators for monitoring activities for people who inject drugs were not defined or part of required reporting until FY 2010, when a Next Generation Indicator was introduced: the number of people who inject drugs on opioid substitution therapy (OGAC, 2009c). OGAC programmatic indicator data provided to the committee showed that in FY 2010 four countries (China, Tanzania, Ukraine, and Vietnam) and one region (Central Asia) in which injection drug use was a key driver of the HIV epidemic reported targets for this indicator and only two, Ukraine and Vietnam, reported results toward achieving this goal. The committee’s ability to interpret effect sizes or health impacts from these data was extremely limited, but in the future, should this indicator continue to be collected consistently, PEPFAR should be able to assess trends in the scale-up of its opioid-substitution therapy services and to evaluate the impact of this important component of the HIV response.
Declining HIV prevalence among people who inject drugs was described by interviewees in PEPFAR partner countries (196-12-PCGOV; 542-6-ML; 396-12-USG), and was directly attributed to the use of opioid substitution therapy and sterile needle and syringe exchange programs (542-6-ML; 396-12-USG). Interviewees also identified a range of other achievements, both specific to PEPFAR and for people who inject drugs in general. These included acknowledgment that PEPFAR’s work on harm reduction programs had been innovative; successful awareness and advocacy work with key stakeholders; provision of technical assistance to national counterparts; and recognition that PEPFAR had established a reputation of being ‘well-respected’ in its work with populations at elevated risk in the country (196-11-USNGO; 542-6-ML; 396-23-USG; 196-8-ML). Interviewees in multiple countries mentioned the work of external partners, including PEPFAR, in contributing to positive shifts in the approach of the national government response (396-12-USG; 396-39-USG; 542-6-ML). One implementing partner noted, “It is because of PEPFAR, frankly, that even
some of these issues get discussed,” including the government’s willingness to discuss a “really good spectrum of services for injecting drug users that goes from like this intervention of reducing initiation but then also addiction counseling, job placement for them, methadone. This is all PEPFAR” (396-15-USNGO). Another interviewee described the importance of successful pilot studies supported by PEPFAR in influencing national governments:
“[T]he truth is that in multiple ways whether it’s for delivery of ARV or substitution treatment, which PEPFAR has funded [. . .] showing that something is possible and that nothing bad will happen has been enormously influential in getting national governments to relax and to allow things to proceed and in some cases to fund it themselves. So again, taking the example of substitution treatment, even though it was a very long and labored process and even though the absolute numbers of people on substitution treatment in [one country] remain small, I think it is very clear that without PEPFAR there would be (a) no one on substitution treatment, and (b) no national targets for the government to scale up substitution treatments.” (NCV-24-USNGO)
Despite these successes, services for people who inject drugs remain inadequate in many countries in which PEPFAR works. Interviewees noted remaining unmet need for harm reduction services (196-13-OGOV; NCV-24-USNGO), skills training (196-17-PCGOV), HIV services, including for female drug users (542-3-USG; 396-13-PCGOV; 396-21-USG), and, in some cases, for other health services, such as support for treatment for hepatitis C (542-11-PCNGO; 396-36-PCGOV). Interviewees also identified a need for continued work on restrictive national policies that limit access to services for people who inject drugs (NCV-24-USNGO). Globally, while the number of countries reporting data is limited, a 2012 UNAIDS report noted that most country programs provide fewer than 100 needles per year per person who injects drugs (UNAIDS, 2012b); one study estimates that sterile injecting equipment is used for only 5 percent of injections globally among people who inject drugs (Degenhardt et al., 2010). Additionally, access to HIV counseling and testing services is low, with, on average, fewer than 40 percent of individuals in urban areas reporting having received an HIV test in the past year (UNAIDS, 2012b). Inadequate information on people who inject drugs was also identified by interviewees as a global challenge that has affected the implementation of PEPFAR’s programs (331-15-USG; 196-8-ML; NCV-24-USNGO; NCV-7-USG). Efforts, some PEPFAR-supported, were under way in several countries to address this (331-14-USG; 196-11-USNGO; 935-14-USG; 461-1-USG), ranging from integrated biological and behavioral surveys (331-24-PCGOV; 196-12-PCGOV), to support for surveillance systems (935-14-USG; 461-1-USG), to the production of peer-reviewed literature (196-11-USNGO).
Conclusion: PEPFAR has been instrumental in facilitating and supporting some harm reduction approaches in countries with epidemics for which injection drug use is a major or emerging driver. Notwithstanding restrictive U.S. and partner country policy and legal environments, a positive effect of these activities and programs is being seen in countries in which PEPFAR works, but substantial unmet need remains for harm reduction and other services for this population.
BLOOD AND MEDICAL INJECTION SAFETY
Blood safety is a critical element of a comprehensive approach to HIV prevention. In 2003 WHO estimated that 5 to 10 percent of HIV infections were acquired though transfusion-related transmission (OGAC, 2004b). Voluntary, non-remunerated blood donors have the lowest rates of infectious disease, including HIV, and thus WHO recommends that by 2020, 100 percent of blood and blood products used for transfusion come from this type of donor (WHO, 2009b). In order to meet national need, it is estimated that 1–3 percent of a country’s population must regularly donate blood products (WHO, 2008b). While this target has been met in most developed countries, as of 2010 there were still 70 developing countries falling short of this goal (World Health Assembly, 2010).
Blood and medical injection safety have been components of PEPFAR’s prevention efforts since the program’s inception in 2003. The authorizing legislation included “assistance to ensure a safe blood supply and sterile medical equipment”30 among the prevention activities supported by the program, and the 2008 reauthorization legislation reiterated support for these prevention areas.31 PEPFAR has never released guidance specific to either topic, but the first Five-Year Global HIV/AIDS strategy identified blood and injection safety as two critical components of the prevention portfolio that should be rapidly scaled up (OGAC, 2004b). PEPFAR’s primary type of activity related to blood safety is the provision of technical assistance and capacity building (OGAC, 2011c). USG staff and partners have worked with national governments over time to implement activities related to both blood and injection safety (OGAC, 2011c).
Several challenges related to the implementation of blood safety activities were mentioned in partner countries visited by the evaluation committee. These included measuring and tracking the need for blood and blood products (331-15-USG), issues with the infrastructure of blood banks (166-11-USG), and the out-of-pocket cost of blood critically needed for obstet-
__________________
30Supra, note 3 at ![]() 301(a)(2), 22 U.S.C. 2151b-2(d)(1)(F).
301(a)(2), 22 U.S.C. 2151b-2(d)(1)(F).
31Supra, note 1 at ![]() 101(a), 22 U.S.C. 7611(a)(14)(B & D).
101(a), 22 U.S.C. 7611(a)(14)(B & D).
ric care (934-17-PCGOV). Despite these challenges, participants identified blood safety work as a PEPFAR success in several countries (935-3-USG; 166-11-USG; 934-18-PCGOV; 935-7-USG; 935-17-USG; 240-9-USG; 240-7-PCGOV). One participant noted that before PEPFAR’s efforts in that country, blood testing processes had been less rigorous, but more recently, improvements had been seen (166-11-USG). Interviewees also described how capacity in national blood safety systems had been built with PEPFAR support (240-9-USG; 240-7-PCGOV; 935-3-USG).
In the first 5 years of implementation, PEPFAR’s program monitoring indicators tracked the number of activities related to improving blood safety, but did not measure outcomes on blood safety at the programmatic level. Currently, there are four PEPFAR blood safety indicators; central reporting to OGAC is not required for any of them (OGAC, 2009c). Although available PEPFAR programmatic data are limited, globally reported data indicate that some improvements were made during the time of PEPFAR’s implementation. In all but 1 of the 15 original PEPFAR focus countries, the number of blood units screened for HIV in centers or laboratories that followed basic quality-assurance processes increased between 2007 and 2009 (UNAIDS, 2012a). Additionally, as of 2009, 12 PEPFAR-funded countries reported that they were screening 100 percent of donated blood (UNAIDS, 2012a).
Achieving the goal of universal access to safe blood and blood products for transfusion in PEPFAR countries is inseparable from health systems strengthening and policy development efforts. Many of the challenges are similar to those identified for other components of the health system (see Chapter 9 for further discussion on health systems strengthening). The Melbourne Declaration highlights the importance of leadership from national governments as they work to build blood safety systems focused on quality, sustainability, and effective monitoring (WHO, 2009b).
While smaller than the blood safety program, support for safe medical injection practices and prophylaxis in the event of exposure has also been a component of PEPFAR’s prevention portfolio since 2004 (OGAC, 2003). From FY 2004 to FY 2011, across all countries in which it operated, PEPFAR planned/approved nearly $187 million for medical injection safety (OGAC, 2005b, 2006c, 2007c, 2008b, 2010d, 2011e,f), which PEPFAR defined as “policies, training, waste-management systems, advocacy and other activities to promote (medical) injection safety, including distribution/supply chain, cost and appropriate disposal of injection equipment and other related equipment and supplies” (OGAC, 2006b, p. 55). From 2004 to 2009, one indicator tracking the number of individuals trained in medical injection safety was required to be reported to OGAC (2007b). In 2009, as a part of the NGIs, use of this indicator was discontinued and a new measure was added requiring countries to report on the number of individuals provided with post-exposure prophylaxis, disaggregated by
exposure type (occupational, rape/sexual assault, and non-occupational) (OGAC, 2009c).
Counseling and testing serves many functions within an effective response to HIV. Initially, voluntary HIV testing programs were primarily intended to increase the number of people aware of their HIV status and to serve as an entry point for counseling and prevention services, both for those who were HIV-positive and for those who were HIV-negative, with the aim of reducing HIV transmission and infection. With the introduction of more widespread care and treatment services, HIV testing now serves as a crucial gateway for enrolling those who are HIV-positive into services for HIV treatment, care and support, and for the prevention of vertical HIV transmission, while still functioning to provide counseling and an entry point to prevention services (Marum et al., 2012). The use of HIV counseling and testing as a direct prevention tool was supported by early evidence suggesting that testing and post-test counseling were followed by positive reductions in sexual risk behavior (OGAC, 2006a; Weinhardt et al., 1999). Today, the potential impact of counseling and testing on directly reducing HIV incidence is unclear, with studies showing both decreases and increases in sexual risk behavior following counseling and testing and the knowledge of one’s serostatus (Corbett et al., 2007; OGAC, 2011c; Sherr et al., 2007; Voluntary HIV-1 Counseling and Testing Efficacy Study Group, 2000; Weinhardt et al., 1999).
From the start of PEPFAR through FY 2008, the budget for counseling and testing activities was captured as a part of the larger technical area of HIV Care (OGAC, 2005b, 2006c, 2007c, 2008b). In FY 2009 the budget code was relocated to the technical area of Prevention, and, as a result, funding for counseling and testing has since been included by PEPFAR in the overall spending on HIV prevention efforts (OGAC, 2010d, 2011e,f). PEPFAR’s 2006 Guidance for a Preventative Care Package for Adults included “services and counseling to prevent the transmission of HIV to others” and “HIV counseling and testing of family members and other contacts” as key components of its care approach (OGAC, 2006a, pp. 2, 9). The goal of these elements was to connect HIV-infected persons with prevention messages and with needed medical care and treatment and to aid in early identification of other HIV-positive family members and sexual partners (OGAC, 2006a). Thus, the aim of linking to prevention interventions, especially for those identified as HIV-positive, was from the beginning a component of PEPFAR’s counseling and testing activities, with a special emphasis on the promotion of condom use for PLHIV (OGAC, 2008a). PEPFAR has also more recently stated that it is intensifying its efforts to
implement modified case management approaches with individuals who test HIV negative (OGAC, 2010c). When PEPFAR updated its guidance on the prevention of sexually transmitted infections in 2011, it incorporated counseling and testing as one of its recommended biomedical approaches to prevention (OGAC, 2011a).
Evidence regarding effective and appropriate counseling and testing modes and settings has expanded over time, and the activities that PEPFAR supports have subsequently evolved as well. Currently, in line with WHO recommendations, PEPFAR funds both client- and provider-initiated voluntary counseling and testing, primarily in clinic settings, but is increasingly investing in home- and community-based approaches, to varying degrees across countries (OGAC, 2011a; WHO, 2012b).
Counseling and testing continues to play an important gateway role for entry into prevention activities, most notably for identifying individuals eligible for VMMC and PMTCT (OGAC, 2011c), while many behavior change–based prevention methods, such as condom use, are effective regardless of whether individuals are aware of their HIV serostatus. Moving forward, the increasing focus on interventions aimed at serodiscordant couples and the prevention benefits of antiretroviral therapy, discussed in greater detail below, will also rely on the linkages between testing and prevention services.
The committee recognized the important role that counseling and testing plays as a part of both the effective implementation of HIV prevention services and the effective implementation of care and treatment services. However, the data collection for the committee’s evaluation revealed that there is little information on the coverage or quality of the implementation of the counseling activities for risk reduction supported by PEPFAR as part of counseling and testing or on the effects of these efforts on HIV risk behavior. Similarly, there is little information regarding how well individuals who test HIV negative are linked to appropriate prevention services. Program monitoring indicators for counseling and testing are focused on documenting the number of people who access the service and receive their results (OGAC, 2007b, 2009c), and interview data were most robust on the role of testing within PEPFAR for linking individuals who test HIV-positive to ART and other care and treatment services. Therefore, the primary discussion of PEPFAR’s achievements and ongoing challenges in counseling and testing can be found in Chapter 6, “Care and Treatment.”
PEPFAR’s support for the scale-up of HIV prevention activities across prevention modalities has been an achievement and a contribution to the response to the epidemic in partner countries. However, given the various
data challenges described in this chapter, the committee was limited in the extent to which it could draw conclusions about the overall impact of PEPFAR’s HIV prevention programs on HIV transmission and on population incidence of HIV infection in the countries in which it operates. The committee recognized the difficulty of assessing prevention impact, both in general and specifically for PEPFAR, given the complexity of interventions, the shifting landscape in which PEPFAR has been operating over time, and limitations in the field of prevention science to systematically monitor and evaluate prevention outcomes and impact.
When considered in the context of the program impact pathway that guided this evaluation, the inputs (such as funding and guidance) for prevention interventions are documented within PEPFAR across the various prevention modalities. However, information about other steps in the impact pathway varied considerably, depending on the modality. For PMTCT, it was possible to document and understand the scope of PEPFAR’s contribution to inputs and activities in terms of the specific funding for PMTCT and the services that PEPFAR supports, as well as the output of these activities in terms of the number of pregnant women who have received PMTCT services. It was also feasible to reasonably assess coverage as one outcome of this contribution. In addition, there is well-established evidence for the effectiveness of PMTCT that makes it possible to credibly conclude that PEPFAR’s successful contribution to outputs and outcomes has contributed directly to reducing vertical transmission of HIV. For other modalities, such as VMMC and certain elements of harm reduction approaches for people who inject drugs, the committee was able to document PEPFAR’s support for the scale-up of specific activities related to these interventions. The committee also anticipates that in the future PEPFAR’s program-monitoring system will provide some estimates of intervention outputs and coverage, which will allow for reasonable conclusions to be drawn about the expected prevention impact of such interventions, although the committee was limited in doing so at this time because the relevant indicators were only recently added.
Behavioral and structural interventions for prevention of sexual transmission were the modalities with the least information available with which to draw conclusions along the steps of the program impact pathway. Through a review of guidance, the committee was able to document over time which activities PEPFAR has recommended be funded. Semi-structured interviews and a review of Country Operational Plans from the partner countries visited for this evaluation indicated that there has been implementation of activities across the range identified in the guidance. However, these data sources revealed a wide and diffuse range of activities, and it was difficult to gain a comprehensive understanding of how PEPFAR’s support has been distributed among different activities and what the outputs of
those activities have been. This is because there is a lack of useful, centrally reported process indicators, as well as other systematically collected and synthesized information, as an alternative to indicators. In addition, there is very limited information on the outcomes of these activities that could be used to support conclusions about their likely contribution to impact on HIV transmission or population incidence.
The challenges in monitoring and evaluating prevention interventions are not unique to PEPFAR. Indeed, there is not clarity in the global community about how to routinely track their implementation and effects. Behavioral and structural interventions in particular are difficult to measure and evaluate because they are affected by many individual, interpersonal, and contextual factors and because their practical implementation as part of programs does not lend itself readily to controlled, random assignment evaluation designs. However, the challenges of measuring the effects of these interventions do not mean that they are inherently ineffective. Rather it is an indication that there is a substantial knowledge gap in this area relative to biomedical prevention modalities, both within PEPFAR and in the greater global health community. Although there is strong foundational knowledge to support the principles and the design of these interventions, the persistent gaps in the field include a lack of knowledge on what the appropriate measures are for meaningfully tracking scale-up and coverage of behavioral and structural interventions; a lack of established and agreed-upon behavior change outcome measures and proxy outcome measures; an insufficient understanding of the effectiveness of these interventions when implemented at scale in producing changes in outcomes; and a lack of knowledge about how the rates of change in behavioral and proxy outcomes are associated with rates of change in HIV transmission.
This is an area in which PEPFAR, given the scale of its programs and its commitment to implementation research, has an opportunity to contribute to much-needed ongoing research and development for assessing behavioral and structural interventions, building on the methodological approaches that are currently available and in use. These include, for example, large-scale cohort studies, non-randomized and quasi-experimental plausibility designs, and evaluations triangulating across multiple methodologies. PEPFAR’s use of these approaches for monitoring, evaluating, and reporting on its non-biomedical prevention efforts is currently quite limited. The benefits of investing in closing this knowledge gap would not be limited to prevention programs, but also would apply to programmatic approaches in areas such as gender, orphans and vulnerable children, and nonclinical care for people living with HIV. In addition, there is an ongoing need to assess the effectiveness of biomedical preventions when implemented at scale, and advances of this kind would contribute to assessing and addressing behavioral aspects that are critical elements of uptake, access, adherence,
and quality for biomedical prevention interventions as well as for care and treatment programs and services.
In addition to understanding the effects of prevention programs on intermediate outcomes and on HIV transmission, the ultimate goal of any prevention intervention is to affect incidence rates in the target population. Incidence rates cannot yet be easily measured directly. Therefore, it is necessary to estimate incidence rates indirectly, and an accepted method for attempting to capture the impact of prevention programming across prevention modalities is incidence modeling. Several approaches, each with its own limitations, have been developed to model the impact of prevention activities and to estimate HIV infections averted, including coverage-based modeling, behavior-based modeling, and disease modeling (Heaton et al., 2008). The coverage-based approach relies on an estimate of the efficacy of the intervention on incident HIV infection but two critical inputs (the coverage and the relative risk) are important sources of uncertainty with this approach (Heaton et al., 2008). The behavior-based approach relies on a model that describes how HIV infection is mediated by behavior, incorporating evidence of the effects of behavior change on incident HIV infection and the change in prevalence of the high-risk behaviors resulting from the intervention. A key limitation of this method is the lack of reliable behavioral data in many developing countries. The third approach of disease modeling is based on a comparison of observed HIV incidence trends with the expected or baseline HIV incidence trends. However, few countries have been able to collect true population-level incidence data, and there have been difficulties with measuring incidence using measures such as BED immunoassays32 (Hallett et al., 2008; Murphy and Parry, 2008). Indirect strategies for estimating HIV incidence, which include models, such as the Estimation and Projection Package and the Spectrum software, developed at UNAIDS, have been used by some researchers to predict HIV prevalence. Comparisons of the observed trends with the modeled or expected trends have been used to estimate infections averted.
PEPFAR uses a model produced by the U.S. Census Bureau to estimate the overall number of infections averted in partner countries and to measure progress toward its congressionally mandated targets (IOM, 2007a); however, the results of these modeling estimates are not publicly available (OGAC, 2012b). The Census Bureau model (known as RUPHIVAIDS) follows a disease-modeling approach in which expected or baseline HIV
__________________
32 The BED-CEIA (HIV-1 subtype B, CRF_01AE, and subtype D-Capture Enzyme Immunoassay) is a commercially available product designed specifically for the purpose of identifying HIV-1 infections that were recently acquired—using the three specific peptides to cover much of the extent of antigenic diversity to overcome some of the subtype differences associated with the “detuned” assays (Murphy and Parry, 2008).
incidence estimates are developed with data prior to 2005 and compared to re-estimated trends in HIV incidence from new surveillance data available after 2004. The difference in the number of new infections, based on this comparison approach, is used as the number of infections averted. The model incorporates estimates of HIV prevalence from the Estimation and Projection Package to project HIV incidence, and applies various assumptions in relation to the sex distribution of HIV infection, the sex ratios of new infections, the rate of MTCT, and disease progression as recommended by the UNAIDS Reference Group on Estimates, Modelling and Projections (U.S. Census Bureau, 2010).
PEPFAR does release publicly the number of estimated infant infections averted through its PMTCT programs; these estimates use a different methodology. PEPFAR calculates infant infections averted by “multiplying the total number of HIV+ pregnant women who received ARV prophylaxis [supported by PEPFAR] by 19 percent, reflecting a consensus estimate that current interventions (which vary by country and site) are reducing transmission, on average, from a background of 35 percent to 16 percent. Countries with more effective interventions (e.g., Botswana) are likely averting more infant infections than [the estimate reports]” (OGAC, 2009a, p. 44). At the completion of the first phase of PEPFAR in 2008, the program estimated that its support for PMTCT activities had averted nearly 240,000 infant HIV infections (PEPFAR, 2008). The committee did not conduct any additional modeling of its own for this study.
Conclusion: There are limitations to measuring the effects of prevention programs across modalities and, in particular, for behavioral and structural interventions. These limitations are not unique to PEPFAR, and a substantial increase in attention and effort will be required to address them, yet more comprehensively identifying and understanding the outputs, coverage, and outcomes of prevention interventions would be of immense value in accurately assessing and documenting the impact of prevention efforts. Across modalities, measuring and achieving key intermediate outcomes for prevention efforts is as important a goal for PEPFAR as achieving estimated impact on the number of infections averted.
INTERVENTIONS ON THE HORIZON FOR PREVENTION STRATEGIES
As noted throughout this report, PEPFAR has evolved over time, adapting itself to changes in science, politics and policy, and the nature of the HIV epidemic itself. Going forward, programmatic agility will be required as PEPFAR attempts to incorporate a number of important scientific develop-
ments that have occurred in the past few years. Many of these developments relate to HIV prevention technologies, including oral pre-exposure prophylaxis, topical microbicides, and ART for the prevention of transmission.
A key development in HIV prevention methods for women occurred in the summer of 2010, when the CAPRISA 004 study found that a vaginal microbicide of 1 percent tenofovir gel reduced the risk of HIV infection among women in South Africa by 39 percent (Abdool Karim et al., 2010). Although it achieved a less-than-optimal level of efficacy, the trial did establish proof of concept of an ART-based vaginal microbicide that women could control. Confirmatory trials were quickly designed to see if the efficacy results could be replicated and improved, as required by regulatory bodies. The VOICE (Vaginal and Oral Interventions to Control the Epidemic) trial was initiated to determine whether a woman’s daily application vaginal gel or taking a daily tablet containing either 1 percent tenofovir or Truvada®33 would be effective methods of preventing sexual transmission of HIV. Following a midterm review, the tenofovir arms of the intervention were discontinued due to a lack of evidence of effectiveness; however, the evaluation of Truvada was maintained, and results are expected to be released in 2013 (Microbicide Trials Network, 2012b). The FACTS 001 (Follow-on African Consortium for Tenofovir Studies) trial began in 2011 and is studying the same tenofovir gel regimen as the CAPRISA 004 study in 2,200 women across South Africa; results from this trial are not expected to be available until 2014 (Microbicide Trials Network, 2012a). Clinical trials of other microbicidal products and routes of administration (e.g., time-release medication in vaginal rings) are also under way, with results expected in the next few years (AVAC, 2010). One study has also demonstrated the efficacy of vaginal tenofovir gel for use as a rectal microbicide, and several trials are currently under way to evaluate the safety, acceptability, and adherence for this product (Microbicide Trials Network, 2012a).
In the autumn of 2010 another HIV prevention milestone was achieved when the iPrEX study found that daily PrEP with Truvada reduced risk of HIV acquisition among gay and other MSM in the Americas, Asia, and Africa by 44 percent (Grant et al., 2010). In 2011 two additional trials of heterosexual HIV-serodiscordant couples and individuals in a number of African countries (TDF2 and Partners PrEP) also showed that daily, oral PrEP with Truvada reduced the risk of HIV infection by 62 percent and 73 percent (Baeten et al., 2012; Thigpen et al., 2012). However, a third study in Africa (FEM-PrEP) found no efficacy of oral, daily PrEP on HIV infection in women (Van Damme et al., 2012). In all of these studies, the key factor affecting the level of the product’s efficacy was adherence: the more individuals adhered to the prescribed drug regimen, the higher the level of
__________________
33 Truvada is a fixed-dose combination of tenofovir disoproxil fumarate and emtricitabine.
efficacy was. In iPrEX, for example, drug level tests showed that those who took their pill on at least 90 percent of days as prescribed reduced their risk of HIV acquisition by more than 70 percent (HHS, 2010).
HIV treatment with ART leads to significant increases in CD4 count (Coetzee et al., 2004) and thus reduced viral load, and several studies analyzing the relationship between viral load and heterosexual transmission have found that reduced viral load was associated with reduced HIV transmission among serodiscordant couples (Attia et al., 2009; Donnell et al., 2010; Quinn et al., 2000). In the recent multisite HPTN 052 study published in 2011, 1,763 HIV-serodiscordant couples at 13 sites in 9 countries were enrolled either in an early-therapy group (individuals with a CD4 count of 350 to 550) for which treatment was started immediately, or in a delayed-therapy group, where ARV was initiated at a CD4 count of 250 or after the development of an AIDS-related illness. The couples who were enrolled in the study were predominantly heterosexual (97 percent) and married (94 percent). They were required to have had a stable relationship for at least 3 months and to be willing to disclose their HIV status to their partners. During the trial, 12 additional HIV-uninfected partners were enrolled as the result of a new relationship, with the original partner being released from the study. As part of the study protocol, both groups were provided with ongoing couples counseling on risk reduction, condoms, and adherence counseling at three monthly visits after enrollment, followed by quarterly visits. Adherence to the study treatment regimen was measured by pill count; in 79 percent of participants in the early-therapy group and in 74 percent of those in the delayed-therapy group adherence was at least 95 percent.
In the initial trial design, the authors anticipated a total of 188 incidences of transmission. In the actual trial results, a total of 39 HIV transmission events were observed during the study period (a median follow-up of 1.7 years), of which 35 were in the delayed-therapy group and 4 in the early-therapy group. Of 39 total transmissions, 28 were confirmed to be linked virologically to the HIV-infected partner in the study, of which 27 occurred in the delayed-therapy group and one in the early-therapy group. The investigators concluded that early initiation of antiretroviral therapy significantly reduced HIV transmission from HIV-infected individuals to their HIV-uninfected partners (Cohen et al., 2011). The study authors noted that the population of stable serodiscordant couples in the study may not be representative of the general population and that the provision of ongoing counseling and condoms likely contributed to the low incidence of HIV infection. They also reported more adverse events related to antiretroviral therapy in the early therapy group than in the delayed-therapy group.
In combination with the PrEP trials, this study added to the existing evidence that antiretrovirals can play a role in HIV prevention, and the
HPTN 052 results have influenced the direction of current HIV prevention efforts both globally and in PEPFAR. Ongoing efforts continue to contribute to the knowledge base on the likely effectiveness and contribution of antiretrovirals as a part of the prevention component of the HIV response. For example, a recent retrospective cohort analysis in China included more than 38,000 serodiscordant heterosexual couples and analyzed the annual rate of HIV infection in the HIV-negative partners, stratified by whether the HIV-positive partner had received ART or was treatment-naïve. The authors found a 26 percent relative reduction in HIV transmission for the cohort receiving treatment (Jia et al., 2012).
Despite emerging evidence and enthusiasm for the potential role of treatment of HIV-infected persons in secondary prevention of transmission to their sexual partners, the cost, complexity, and clinical and public health implications of implementing this as a long-term approach at scale outside of trial conditions are not fully understood. Incorporating this as a prevention approach will not eliminate the need for effective primary prevention interventions delivered to uninfected persons at elevated risk of sexual HIV exposure (Hallett et al., 2011).
Given the potential of these and future prevention technologies to markedly reduce HIV transmission and acquisition globally, it will be important for PEPFAR to quickly determine how best to incorporate them into the programs it supports; the committee understands that PEPFAR is already taking these scientific advancements into consideration. This will involve engaging and supporting social science research and implementation science (or operations research) to answer questions about the desirability, feasibility, cost-effectiveness, and impact of scaling-up new prevention methods in various countries, settings, and health care delivery and community-based service systems.
Making strong global and national commitments to HIV prevention, with commensurate resources, expertise, and research, is critical to any balanced attempt to change the course of the HIV epidemic. The UN’s Declaration on Commitment on HIV/AIDS, written in 2001, recognizes that “Prevention must be the mainstay of our response” (United Nations, 2001, p. 19). Not only does this continue to be a central tenet of the global HIV/AIDS response, but also PEPFAR was directed by its reauthorization legislation to prioritize HIV prevention going forward, and this expectation is being passed on to partner countries as part of the emphasis for sustainable management of HIV responses. As a common theme during country visit interviews, the committee also heard that prevention must be a mainstay of
an HIV response and that many stakeholders felt that their countries’ HIV prevention efforts need to be strengthened.
With the evolution of PEPFAR’s prevention programming and changing priorities, prevention has developed into a “catchall” term for many disparate concepts and activities that have not been clearly oriented around a strategic objective. Over time, OGAC has provided more guidance and technical support documentation, including population-specific guidance. In addition, PEPFAR has recently articulated a commitment to overarching goals for prevention (Clinton, 2011, 2012; OGAC, 2012a). However, despite these developments, there continues to be ambiguity about the operational objectives and targeted outcomes for prevention as well as the best ways to develop, implement, and monitor all the modalities within a comprehensive prevention portfolio that reflects country context and incorporates the ongoing evolution of the evidence base.
For prevention activities to be maximally effective, program planners must have access to appropriate data that will inform which combinations of prevention activities and interventions are most effective and best suited for implementation for specific populations, epidemiological contexts, and a variety of settings, including different geographic areas, governmental and nongovernmental sectors, facilities, and communities. Despite the knowledge gaps that remain for monitoring and evaluating prevention interventions, PEPFAR has supported a variety of data collection for prevention planning, especially at the country level.
Overall Conclusion: PEPFAR’s support for the scale-up of HIV prevention activities across prevention modalities has been an achievement and a contribution to the response to the epidemic in partner countries. Within PEPFAR, there has been an evolution in prevention programming, from an initial focus on a limited number of behavioral and biomedical interventions to an expansion of prevention portfolios that reflect both existing and emergent evidence-based approaches. Although PEPFAR has articulated a commitment to overarching goals for prevention, it lacks clear target outcomes and objectives across all prevention modalities; this is especially the case for behavioral and structural interventions for prevention of sexual transmission, the primary global driver of HIV infection. To achieve its overall goal of reducing new infections and stopping the spread of the epidemic, PEPFAR will need a more comprehensive and balanced approach, with greater clarity in its operational guidance and mechanisms to support the development, implementation, monitoring, and evaluation of prevention portfolios in country programs that are aligned with the drivers of epidemics and the needs for prevention services. Greater attention
to developing appropriate approaches to assess the effectiveness of prevention interventions across all modalities and modes of transmission would contribute to this more balanced and comprehensive operational approach.
Recommendation 5-1: To contribute to the sustainable management of the HIV epidemic in partner countries, PEPFAR should support a stronger emphasis on prevention. The prevention response should prioritize the reduction of sexual transmission, which is the primary driver of most HIV infections, while maintaining support for interventions targeted at other modes of transmission. The response should incorporate an approach balanced among biomedical, behavioral, and structural interventions that is informed by epidemiological data and intervention effectiveness evidence. PEPFAR should support advances in prevention science to expand the availability of effective interventions where knowledge is lacking.
Further considerations for implementation of this recommendation:
• PEPFAR has made a commitment to overarching goals for prevention and for achieving an AIDS-Free Generation, but this does not constitute a long-term prevention strategy that clearly states prevention objectives and the pathways to achieving them. The following elements will be critical for a more comprehensive strategy to achieve successful execution of prevention programs:
o PEPFAR should continue to enhance its efforts to involve partner country stakeholders and incorporate country-specific epidemiology, context, and priorities in planning appropriately matched prevention programs that achieve a balanced approach to HIV prevention across the available modalities. To provide greater technical and operational clarity, OGAC should provide mechanisms to support the development, implementation, and monitoring of comprehensive prevention portfolios, including how to determine which populations need which directed prevention activities in which settings. Areas of prevention where current interventions are successful and effective, such as PMTCT, should be continued and scaled up to ensure access, coverage, and quality. As new PEPFAR-supported prevention activities are adopted, OGAC should communicate its ob-
jectives and the methods for introducing or scaling up with specified populations.
o OGAC should improve mechanisms to collect and incorporate evidence on the effectiveness of prevention activities implemented in partner countries. The key components for the future assessment and evaluation of HIV prevention should include need, coverage of need, quality of services provided, and behavioral and epidemiological outcomes. OGAC should provide clearly defined process and outcome measures as well as impact assessment methods to evaluate progress.
o PEPFAR’s prevention strategy should include balanced support for innovation, research, and evaluation to contribute to the evolving evidence base and to advance understanding of the effectiveness of interventions within all prevention modalities. To define and ensure this balance, OGAC should, through its existing mechanisms, convene and use expertise spanning behavioral, structural, and biomedical prevention intervention approaches. PEPFAR-supported research and evaluation activities should employ appropriate methodologies and study designs, without unduly emphasizing random assignment designs. PEPFAR should support innovations in prevention science methodologies where needed to achieve its programmatic research aims (see also Recommendation 11-1).
Abdool Karim, Q., S. S. Abdool Karim, J. A. Frohlich, A. C. Grobler, C. Baxter, L. E. Mansoor, A. B. Kharsany, S. Sibeko, K. P. Mlisana, Z. Omar, T. N. Gengiah, S. Maarschalk, N. Arulappan, M. Mlotshwa, L. Morris, D. Taylor, and Caprisa Trial Group. 2010. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science 329(5996):1168-1174.
Abdool Karim, S. S., Q. Abdool Karim, E. Gouws, and C. Baxter. 2007. Global epidemiology of HIV-AIDS. Infectious Disease Clinics of North America 21(1):1-17.
amfAR (The Foundation for AIDS Research). 2010. MSM and the global HIV/AIDS epidemic: Assessing PEPFAR and looking forward. Washington, DC: amfAR.
Anoje, C., B. Aiyenigba, C. Suzuki, T. Badru, K. Akpoigbe, M. Odo, S. Odafe, O. Adedokun, K. Torpey, and O. N. Chabikuli. 2012. Reducing mother-to-child transmission of HIV: Findings from an early infant diagnosis program in south-south region of Nigeria. BMC Public Health 12:184-191.
Attia, S., M. Egger, M. Muller, M. Zwahlen, and N. Low. 2009. Sexual transmission of HIV according to viral load and antiretroviral therapy: Systematic review and meta-analysis. AIDS 23(11):1397-1404.
Auerbach, J. 2009. Transforming social structures and environments to help in HIV prevention. Health Affairs 28(6):1655-1665.
Auerbach, J. D., and T. J. Coates. 2000. HIV prevention research: Accomplishments and challenges for the third decade of AIDS. American Journal of Public Health 90(7):1029-1032.
Auerbach, J. D., R. J. Hayes, and S. M. Kandathil. 2006. Overview of effective and promising interventions to prevent HIV infection. World Health Organization Technical Reporting Service 938:43-78; discussion 317-341.
Auvert, B., D. Taljaard, E. Lagarde, J. Sobngwi-Tambekou, R. Sitta, and A. Puren. 2005. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: The ANRS 1265 Trial. PLOS Medicine 2(11):e298.
AVAC. 2010. HIV prevention research: Timeline of expected efficacy trial results. http://data.avac.org/Timeline.aspx (accessed February 8, 2013).
Avert.org. 2012. The female condom. http://www.avert.org/female-condom.htm (accessed November 7, 2012).
Avert.org. n.d. HIV & AIDS stigma and discrimination. http://www.avert.org/hiv-aids-stigma.htm (accessed March 25, 2013).
Azcoaga-Lorenzo, A., C. Ferreyra, A. Alvarez, P. P. Palma, E. Velilla, and J. del Amo. 2011. Effectiveness of a PMTCT programme in rural Western Kenya. AIDS Care—Psychological and Socio-Medical Aspects of AIDS/HIV 23(3):274-280.
Baeten, J. M., D. Donnell, P. Ndase, N. R. Mugo, J. D. Campbell, J. Wangisi, J. W. Tappero, E. A. Bukusi, C. R. Cohen, E. Katabira, A. Ronald, E. Tumwesigye, E. Were, K. H. Fife, J. Kiarie, C. Farquhar, G. John-Stewart, A. Kakia, J. Odoyo, A. Mucunguzi, E. Nakku-Joloba, R. Twesigye, K. Ngure, C. Apaka, H. Tamooh, F. Gabona, A. Mujugira, D. Panteleeff, K. K. Thomas, L. Kidoguchi, M. Krows, J. Revall, S. Morrison, H. Haugen, M. Emmanuel-Ogier, L. Ondrejcek, R. W. Coombs, L. Frenkel, C. Hendrix, N. N. Bumpus, D. Bangsberg, J. E. Haberer, W. S. Stevens, J. R. Lingappa, C. Celum, and Partners PreP Study Team. 2012. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. New England Journal of Medicine 367(5):399-410.
Bailey, R. C., S. Moses, C. B. Parker, K. Agot, I. Maclean, J. N. Krieger, C. F. Williams, R. T. Campbell, and J. O. Ndinya-Achola. 2007. Male circumcision for HIV prevention in young men in Kisumu, Kenya: A randomised controlled trial. Lancet 369(9562):643-656.
Baird, S. J., R. S. Garfein, C. T. McIntosh, and B. Ozler. 2012. Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: A cluster randomised trial. Lancet 379(9823):1320-1329.
Bancheno, W. M., F. Mwanyumba, and J. Mareverwa. 2010. Outcomes and challenges of scaling up comprehensive PMTCT services in rural Swaziland, Southern Africa. AIDS Care 22(9):1130-1135.
Beyrer, C., S. D. Baral, F. van Griensven, S. M. Goodreau, S. Chariyalertsak, A. L. Wirtz, and R. Brookmeyer. 2012. Global epidemiology of HIV infection in men who have sex with men. Lancet 380(9839):367-377.
Brennan Center for Justice. 2012. AOSI v. USAID. http://www.brennancenter.org/content/resource/aosi_v_usaid (accessed November 10, 2012).
CDC (U.S. Centers for Disease Control and Prevention). 2002. Methadone maintenance treatment. Atlanta, GA: CDC.
CDC. 2012. Pediatric HIV surveillance slide sets. http://www.cdc.gov/hiv/topics/surveillance/resources/slides/pediatric/index.htm (accessed November 11, 2012).
Chaisilwattana, P., K. Chokephaibulkit, A. Chalermchockcharoenkit, N. Vanprapar, K. Sirimai, S. Chearskul, R. Sutthent, and N. Opartkiattikul. 2002. Short-course therapy with zidovudine plus lamivudine for prevention of mother-to-child transmission of human immunodeficiency virus type 1 in Thailand. Clinical Infectious Diseases 35(11):1405-1413.
CHANGE (Center for Health and Gender Equity). 2008. Implications of U.S. policy restrictions for HIV programs aimed at commercial sex workers. Washington, DC: CHANGE.
Chasela, C. S., M. G. Hudgens, D. J. Jamieson, D. Kayira, M. C. Hosseinipour, A. P. Kourtis, F. Martinson, G. Tegha, R. J. Knight, Y. I. Ahmed, D. D. Kamwendo, I. F. Hoffman, S. R. Ellington, Z. Kacheche, A. Soko, J. B. Wiener, S. A. Fiscus, P. Kazembe, I. A. Mofolo, M. Chigwenembe, D. S. Sichali, C. M. van der Horst, and B. A. N. Study Group. 2010. Maternal or infant antiretroviral drugs to reduce HIV-1 transmission. New England Journal of Medicine 362(24):2271-2281.
Chinkonde-Nkhoma, J. R., M. Hosseinipour, A. M. I. Mofolo, E. K. T. Mtande, M. Mwale, P. Champiti, A. Msekandiana, R. Chihana, B. Phiri, F. Chibwandira, M. Eliya, K. Matumba, L. Mwangomba, A. Mphweya, G. Mwale, J. Sundby, F. Martinson, I. Hoffman, C. van der Horst, and the Safeguard the Family Project. 2012. A review of the “Option B Plus” roll-out in the five districts of Malawi. Abstract presented at the XIX International AIDS Conference, July 22-27, Washington, DC.
Chiu, J., and S. Burris. 2011. Punitive drug law and the risk environment for injecting drug users: Understanding the connections. New York: Technical Advisory Group of the Global Commission on HIV and the Law.
Clinton, H. 2011. Remarks on “Creating an AIDS-Free Generation.” http://www.state.gov/secretary/rm/2011/11/176810.htm (accessed December 10, 2012).
Clinton, H. 2012. Remarks at the 2012 International AIDS Conference. Presentation at the XIX International AIDS Conference, Washington, DC.
Coetzee, D., K. Hildebrand, A. Boulle, G. Maartens, F. Louis, V. Labatala, H. Reuter, N. Ntwana, and E. Goemaere. 2004. Outcomes after two years of providing antiretroviral treatment in Khayelitsha, South Africa. AIDS 18(6):887-895.
Coetzee, D., K. Hilderbrand, A. Boulle, B. Draper, F. Abdullah, and E. Goemaere. 2005. Effectiveness of the first district-wide programme for the prevention of mother-to-child transmission of HIV in South Africa. Bulletin of the World Health Organization 83(7):489-494.
Cohen, M. S., Y. Q. Chen, M. McCauley, T. Gamble, M. C. Hosseinipour, N. Kumarasamy, J. G. Hakim, J. Kumwenda, B. Grinsztejn, J. H. Pilotto, S. V. Godbole, S. Mehendale, S. Chariyalertsak, B. R. Santos, K. H. Mayer, I. F. Hoffman, S. H. Eshleman, E. Piwowar-Manning, L. Wang, J. Makhema, L. A. Mills, G. de Bruyn, I. Sanne, J. Eron, J. Gallant, D. Havlir, S. Swindells, H. Ribaudo, V. Elharrar, D. Burns, T. E. Taha, K. Nielsen-Saines, D. Celentano, M. Essex, T. R. Fleming, and HPTN Study Team. 2011. Prevention of HIV-1 infection with early antiretroviral therapy. New England Journal of Medicine 365(6):493-505.
Colvin, M., M. Chopra, T. Doherty, D. Jackson, J. Levin, J. Willumsen, A. Goga, P. Moodley, and Good Start Study Group. 2007. Operational effectiveness of single-dose nevirapine in preventing mother-to-child transmission of HIV. Bulletin of the World Health Organization 85(6):466-473.
Connor, E. M., R. S. Sperling, R. Gelber, P. Kiselev, G. Scott, M. J. O’Sullivan, R. VanDyke, M. Bey, W. Shearer, R. L. Jacobson, et al. 1994. Reduction of maternal-infant transmission of human immunodeficiency virus type 1 with zidovudine treatment. New England Journal of Medicine 331(18):1173-1180.
Corbett, E. L., B. Makamure, Y. B. Cheung, E. Dauya, R. Matambo, T. Bandason, S. S. Munyati, P. R. Mason, A. E. Butterworth, and R. J. Hayes. 2007. HIV incidence during a cluster-randomized trial of two strategies providing voluntary counselling and testing at the workplace, Zimbabwe. AIDS 21(4):483-489.
Cowan, F. M., S. J. Pascoe, L. F. Langhaug, W. Mavhu, S. Chidiya, S. Jaffar, M. T. Mbizvo, J. M. Stephenson, A. M. Johnson, R. M. Power, G. Woelk, R. J. Hayes, and Regai Dzive Shiri trial team. 2010. The Regai Dzive Shiri project: results of a randomized trial of an HIV prevention intervention for youth. AIDS 24(16):2541-2552.
Dabis, F., L. Bequet, D. K. Ekouevi, I. Viho, F. Rouet, A. Horo, C. Sakarovitch, R. Becquet, P. Fassinou, L. Dequae-Merchadou, C. Welffens-Ekra, C. Rouzioux, V. Leroy, and ANRS Ditrame Plus Study Group. 2005. Field efficacy of zidovudine, lamivudine and single-dose nevirapine to prevent peripartum HIV transmission. AIDS 19(3):309-318.
Degenhardt, L., B. Mathers, P. Vickerman, T. Rhodes, C. Latkin, and M. Hickman. 2010. Prevention of HIV infection for people who inject drugs: Why individual, structural, and combination approaches are needed. Lancet 376(9737):285-301.
Deschamps, M. M., F. Noel, J. Bonhomme, J. G. Devieux, G. Saint-Jean, Y. W. Zhu, P. Wright, J. W. Pape, and R. M. Malow. 2009. Prevention of mother-to-child transmission of HIV in Haiti. Pan American Journal of Public Health 25(1):24-30.
Doherty, T. M., D. McCoy, and S. Donohue. 2005. Health system constraints to optimal coverage of the prevention of mother-to-child HIV transmission programme in South Africa: lessons from the implementation of the national pilot programme. African Health Sciences 5(3):213-218.
Donnell, D., J. M. Baeten, J. Kiarie, K. K. Thomas, W. Stevens, C. R. Cohen, J. McIntyre, J. R. Lingappa, C. Celum, and the Partners in Prevention H. S. V. H. I. V. Transmission Study Team. 2010. Heterosexual HIV-1 transmission after initiation of antiretroviral therapy: A prospective cohort analysis. Lancet 375(9731):2092-2098.
Essex, M., and V. DeGruttola. 2012. Presentation to the PEPFAR SAB: Botswana Combination Prevention Project (BCPP). Washington, DC: Harvard University and CDC.
Evertz, S. 2010. How ideology trumped science: Why PEPFAR has failed to meet its potential. Washington, DC: Council for Global Equality.
FHI (Family Health International) 360. 2004. Behavior change—a summary of four major theories. http://www.fhi360.org/nr/rdonlyres/ei26vbslpsidmahhxc332vwo3g233xsqw22er3vofqvrfjvubwyzclvqjcbdgexyzl3msu4mn6xv5j/bccsummaryfourmajortheories.pdf (accessed January 29, 2013).
GAO (U.S. Government Accountability Office). 2006. Global health: Spending requirement presents challenges for allocating prevention funding under the President’s Emergency Plan for AIDS Relief. Washington, DC: GAO.
Global HIV Prevention Working Group. 2003. Access to HIV prevention closing the gap. Washington, DC: The Kaiser Family Foundation and the Bill & Melinda Gates Foundation.
Global HIV Prevention Working Group. 2008. Behavior change and HIV prevention: (Re)considerations for the 21st century. Washington, DC: The Kaiser Family Foundation and the Bill & Melinda Gates Foundation.
Gouws, E., P. J. White, J. Stover, and T. Brown. 2006. Short term estimates of adult HIV incidence by mode of transmission: Kenya and Thailand as examples. Sexually Transmitted Infections 82(Suppl 3):iii51-iii55.
Grant, R. M., J. R. Lama, P. L. Anderson, V. McMahan, A. Y. Liu, L. Vargas, P. Goicochea, M. Casapia, J. V. Guanira-Carranza, M. E. Ramirez-Cardich, O. Montoya-Herrera, T. Fernandez, V. G. Veloso, S. P. Buchbinder, S. Chariyalertsak, M. Schechter, L. G. Bekker, K. H. Mayer, E. G. Kallas, K. R. Amico, K. Mulligan, L. R. Bushman, R. J. Hance, C. Ganoza, P. Defechereux, B. Postle, F. Wang, J. J. McConnell, J. H. Zheng, J. Lee, J. F. Rooney, H. S. Jaffe, A. I. Martinez, D. N. Burns, D. V. Glidden, and the iPrEx Study Team. 2010. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. New England Journal of Medicine 363(27):2587-2599.
Gray, R. H., G. Kigozi, D. Serwadda, F. Makumbi, S. Watya, F. Nalugoda, N. Kiwanuka, L. H. Moulton, M. A. Chaudhary, M. Z. Chen, N. K. Sewankambo, F. Wabwire-Mangen, M. C. Bacon, C. F. Williams, P. Opendi, S. J. Reynolds, O. Laeyendecker, T. C. Quinn, and M. J. Wawer. 2007. Male circumcision for HIV prevention in men in Rakai, Uganda: A randomised trial. Lancet 369(9562):657-666.
Gregson, S., G. P. Garnett, C. A. Nyamukapa, T. B. Hallett, J. J. Lewis, P. R. Mason, S. K. Chandiwana, and R. M. Anderson. 2006. HIV decline associated with behavior change in eastern Zimbabwe. Science 311(5761):664-666.
Gregson, S., S. Adamson, S. Papaya, J. Mundondo, C. A. Nyamukapa, P. R. Mason, G. P. Garnett, S. K. Chandiwana, G. Foster, and R. M. Anderson. 2007. Impact and process evaluation of integrated community and clinic-based HIV-1 control: A cluster-randomised trial in eastern Zimbabwe. PLOS Medicine 4(3):e102.
Grulich, A. E., and I. Zablotska. 2010. Commentary: Probability of HIV transmission through anal intercourse. International Journal of Epidemiology 39(4):1064-1065.
Guay, L. A., P. Musoke, T. Fleming, D. Bagenda, M. Allen, C. Nakabiito, J. Sherman, P. Bakaki, C. Ducar, M. Deseyve, L. Emel, M. Mirochnick, M. G. Fowler, L. Mofenson, P. Miotti, K. Dransfield, D. Bray, F. Mmiro, and J. B. Jackson. 1999. Intrapartum and neonatal single-dose nevirapine compared with zidovudine for prevention of mother-to-child transmission of HIV-1 in Kampala, Uganda: HIVNET 012 randomised trial. Lancet 354(9181):795-802.
Gupta, G. R., J. O. Parkhurst, J. A. Ogden, P. Aggleton, and A. Mahal. 2008. Structural approaches to HIV prevention. Lancet 372(9640):764-775.
Hallett, T. B., B. Zaba, J. Todd, B. Lopman, W. Mwita, S. Biraro, S. Gregson, J. T. Boerma, on behalf of the Alpha Network. 2008. Estimating incidence from prevalence in generalised HIV epidemics: Methods and validation. PLOS Medine 5(4):e80.
Hallett, T. B., J. M. Baeten, R. Heffron, R. Barnabas, G. de Bruyn, I. Cremin, S. Delany, G. P. Garnett, G. Gray, L. Johnson, J. McIntyre, H. Rees, and C. Celum. 2011. Optimal uses of antiretrovirals for prevention in HIV-1 serodiscordant heterosexual couples in South Africa: A modelling study. PLOS Medicine 8(11).
Hankins, C. A., and B. O. de Zalduondo. 2010. Combination prevention: A deeper understanding of effective HIV prevention. AIDS 24(Suppl 4):S70-S80.
Harm Reduction International. 2012. The global state of harm reduction 2012: Towards an integrated response. London: Harm Reduction International.
Hearst, N., A. Ruark, and N. Fraser. 2012. AIDS prevention in Africa’s generalized epidemics: What should we be doing? What are we doing? A review of HIV/AIDS prevention in the national strategic planning process in sub-Saharan Africa. Presentation at the XIX International AIDS Conference, July 24, Washington, DC.
Heaton, L. M., R. Komatsu, D. Low-Beer, T. B. Fowler, and P. O. Way. 2008. Estimating the number of HIV infections averted: An approach and issues. Sexually Transmitted Infections 84(Suppl 1):i92-i96.
Heimer, R., S. S. Myers, E. C. Cadman, and E. H. Kaplan. 1992. Detection by polymerase chain reaction of human immunodeficiency virus type 1 proviral DNA sequences in needles of injecting drug users. Journal of Infectious Diseases 165(4):781-782.
HHS (U.S. Department of Health and Human Services). 2010. The iPrEx study: Pre-exposure prophylaxis as HIV prevention among men who have sex with men. http://www.niaid.nih.gov/news/QA/Pages/iPrExQA.aspx (accessed February 8, 2013).
Holmes, C. B. 2012. PEPFAR document to the field on Option B+. Washington, DC: OGAC.
Hurley, S. F., D. J. Jolley, and J. M. Kaldor. 1997. Effectiveness of needle-exchange programmes for prevention of HIV infection. Lancet 349(9068):1797-1800.
IHRA (International Harm Reduction Association). 2009. What is harm reduction? London: IHRA.
IOM (Institute of Medicine). 1999. Reducing the odds: Preventing perinatal transmission of HIV in the United States. Washington, DC: National Academy Press.
IOM. 2007a. PEPFAR implementation: Progress and promise. Washington, DC: The National Academies Press.
IOM. 2007b. Preventing HIV infection among injecting drug users in high risk countries: An assessment of the evidence. Washington, DC: The National Academies Press.
Jewkes, R., M. Nduna, J. Levin, N. Jama, K. Dunkle, A. Puren, and N. Duvvury. 2008. Impact of stepping stones on incidence of HIV and HSV-2 and sexual behaviour in rural South Africa: Cluster randomised controlled trial. BMJ 337:a506.
Jia, Z., Y. Ruan, Q. Li, P. Xie, P. Li, X. Wang, R. Y. Chen, and Y. Shao. 2012. Antiretroviral therapy to prevent HIV transmission in serodiscordant couples in China (2003-11): A national observational cohort study. Lancet. Available online December 2012, http://dx.doi.org/10.1016/S0140-6736(12)61898-4.
Kamali, A., M. Quigley, J. Nakiyingi, J. Kinsman, J. Kengeya-Kayondo, R. Gopal, A. Ojwiya, P. Hughes, L. M. Carpenter, and J. Whitworth. 2003. Syndromic management of sexually-transmitted infections and behaviour change interventions on transmission of HIV-1 in rural Uganda: A community randomised trial. Lancet 361(9358):645-652.
Kaplan, E. H., and R. Heimer. 1994. A circulation theory of needle exchange. AIDS 8(5): 567-574.
Kelland, K. 2010. Mother-baby HIV box targets transmission. http://www.reuters.com/article/2010/11/09/us-hiv-mother-baby-idUSTRE6A82AX20101109 (accessed November 12, 2012).
Kerrigan, D., and M. Sweat. 2012. Presentation to the PEPFAR SAB: Evaluating a combination prevention intervention to reduce HIV transmission in Iringa, Tanzania. Washington, DC: Johns Hopkins University and Medical University of South Carolina.
Kong, X., G. Kigozi, V. Ssempija, D. Serwadda, F. Nalugoda, F. Makumbi, T. Lutalo, S. Watya, M. Wawer, and R. Gray. 2011. Longer-term effects of male circumcision on HIV incidence and risk behaviors during post-trial surveillance in Rakai, Uganda. Abstract presented at the 18th Conference on Retroviruses and Opportunistic Infections, Boston, MA.
Kourtis, A. P., F. K. Lee, E. J. Abrams, D. J. Jamieson, and M. Bulterys. 2006. Mother-to-child transmission of HIV-1: Timing and implications for prevention. Lancet Infectious Diseases 6(11):726-732.
Kumar, M. S. 2012. Opioid substitution treatment (buprenorphine): Prevention of transmission of HIV among drug users in SAARC countries (RAS/H13). New Delhi, India: United Nations Office on Drugs and Crime, Regional Office for South Asia.
Kumwenda, N. I., D. R. Hoover, L. M. Mofenson, M. C. Thigpen, G. Kafulafula, Q. Li, L. Mipando, K. Nkanaunena, T. Mebrahtu, M. Bulterys, M. G. Fowler, and T. E. Taha. 2008. Extended antiretroviral prophylaxis to reduce breast-milk HIV-1 transmission. New England Journal of Medicine 359(2):119-129.
Kurth, A. E., C. Celum, J. M. Baeten, S. H. Vermund, and J. N. Wasserheit. 2011. Combination HIV prevention: Significance, challenges, and opportunities. Current HIV/AIDS Reports 8(1):62-72.
Laga, M., D. Rugg, G. Peersman, and M. Ainsworth. 2012. Evaluating HIV prevention effectiveness: The perfect as the enemy of the good. AIDS 26(7):779-783.
Lallemant, M., G. Jourdain, S. Le Coeur, S. Kim, S. Koetsawang, A. M. Comeau, W. Phoolcharoen, M. Essex, K. McIntosh, and V. Vithayasai for the Perinatal HIV Prevention Trial (Thailand) Investigators. 2000. A trial of shortened zidovudine regimens to prevent mother-to-child transmission of human immunodeficiency virus type 1. New England Journal of Medicine 343(14):982-991.
Law Students for Reproductive Justice. 2012. U.S. foreign policy. Oakland, CA: Law Students for Reproductive Justice.
Lussiana, C., S. V. Clemente, A. Ghelardi, M. Lonardi, I. A. Pulido Tarquino, and M. Floridia. 2012. Effectiveness of a prevention of mother-to-child HIV transmission programme in an urban hospital in Angola. PLOS ONE 7(4):e36381.
Mandelbrot, L., A. Landreau-Mascaro, C. Rekacewicz, A. Berrebi, J. L. Benifla, M. Burgard, E. Lachassine, B. Barret, M. L. Chaix, A. Bongain, N. Ciraru-Vigneron, C. Crenn-Hebert, J. F. Delfraissy, C. Rouzioux, M. J. Mayaux, S. Blanche, and Agence Nationale de Recherches sur le SIDA Study Group. 2001. Lamivudine-zidovudine combination for prevention of maternal-infant transmission of HIV-1. Journal of the American Medical Association 285(16):2083-2093.
Marum, E., M. Taegtmeyer, B. Parekh, N. Mugo, S. Lembariti, M. Phiri, J. Moore, and A. Cheng. 2012. “What took you so long?” The impact of PEPFAR on the expansion of HIV testing and counseling services in Africa. Journal of Acquired Immune Deficiency Syndrome 60(Suppl 3):S63-S69.
Mathers, B. M., L. Degenhardt, B. Phillips, L. Wiessing, M. Hickman, S. A. Strathdee, A. Wodak, S. Panda, M. Tyndall, A. Toufik, R. P. Mattick, and Reference Group to the UN on HIV and Injecting Drug Use. 2008. Global epidemiology of injecting drug use and HIV among people who inject drugs: A systematic review. Lancet 372(9651):1733-1745.
Mathers, B., L. Degenhardt, and M. Sabin. 2011. Context and progress of the global response to HIV among people who inject drugs. Australia: University of New South Wales and the Burnet Institute.
Microbicide Trials Network. 2012a. About microbicides. http://www.mtnstopshiv.org/node/706 (accessed November 12, 2012).
Microbicide Trials Network. 2012b. VOICE (MTN-003). http://www.mtnstopshiv.org/news/studies/mtn003 (accessed November 12, 2012).
Murphy, G., and J. V. Parry. 2008. Assays for the detection of recent infections with human immunodeficiency virus type 1. Eurosurveillance 13(36):18966.
National Cancer Institute. 2005. Theory at a glance: A guide for health promotion practice (second edition). Washington, DC: HHS and National Institutes of Health.
Nduati, R., G. John, D. Mbori-Ngacha, B. Richardson, J. Overbaugh, A. Mwatha, J. Ndinya-Achola, J. Bwayo, F. E. Onyango, J. Hughes, and J. Kreiss. 2000. Effect of breastfeeding and formula feeding on transmission of HIV-1: A randomized clinical trial. Journal of the American Medical Association 283(9):1167-1174.
NIAID (National Institute of Allergies and Infectious Diseases). 2012. HIV/AIDS vaccine research. http://www.niaid.nih.gov/topics/hivaids/research/vaccines/Pages/default.aspx (accessed March 20, 2013).
Nieburg, P., and L. Carty. 2011. HIV prevention among injection drug users in Kenya and Tanzania. Washington, DC: Center for Strategic and International Studies.
OGAC (Office of the U.S. Global AIDS Coordinator). 2003. PEPFAR country operational plan guidelines for FY04. Washington, DC: OGAC.
OGAC. 2004a. The President’s Emergency Plan for AIDS Relief: FY05 country operational plan guidance. Washington, DC: OGAC.
OGAC. 2004b. The President’s Emergency Plan for AIDS Relief: U.S. five-year global HIV/AIDS strategy. Washington, DC: OGAC.
OGAC. 2005a. ABC guidance #1 for United States government in-country staff and implementing partners applying the ABC approach to preventing sexually-transmitted HIV infections within the President’s Emergency Plan for AIDS Relief. Washington, DC: OGAC.
OGAC. 2005b. The President’s Emergency Plan for AIDS Relief Fiscal Year 2005 operational plan: June 2005 update. Washington, DC: OGAC.
OGAC. 2005c. President’s Emergency Plan for AIDS Relief: FY06 country operational plan final guidance. Washington, DC: OGAC.
OGAC. 2006a. Guidance for United States government in-country staff and implementing partners for a preventive care package for adults—#1. Washington, DC: OGAC.
OGAC. 2006b. The President’s Emergency Plan for AIDS Relief: FY2007 country operational plan guidance. Washington, DC: OGAC.
OGAC. 2006c. The U.S. President’s Emergency Plan for AIDS Relief Fiscal Year 2006: Operational plan. 2006 August update. Washington, DC: OGAC.
OGAC. 2006d. The U.S. President’s Emergency Plan for AIDS Relief HIV prevention among drug users guidance #1: Injection heroin use. Washington, DC: OGAC.
OGAC. 2007a. The President’s Emergency Plan for AIDS Relief: FY2008 country operational plan guidance. Washington, DC: OGAC.
OGAC. 2007b. The President’s Emergency Plan for AIDS Relief: Indicators, reporting requirements, and guidelines. Indicators reference guide: FY2007 reporting/FY2008 planning. Washington, DC: OGAC.
OGAC. 2007c. The U.S. President’s Emergency Plan for AIDS Relief Fiscal Year 2007: Operational plan. 2007 June update. Washington, DC: OGAC.
OGAC. 2008a. The President’s Emergency Plan for AIDS Relief: FY2009 country operational plan guidance. Washington, DC: OGAC.
OGAC. 2008b. The U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) fiscal year 2008: PEPFAR operational plan. June 2008. Washington, DC: OGAC.
OGAC. 2009a. Celebrating life: The U.S. President’s Emergency Plan for AIDS Relief 2009 annual report to Congress. Washington, DC: OGAC.
OGAC. 2009b. The President’s Emergency Plan for AIDS Relief: FY2010 country operational plan guidance: Programmatic considerations. Washington, DC: OGAC.
OGAC. 2009c. The President’s Emergency Plan for AIDS Relief: Next generation indicators reference guide. Version 1.1. Washington, DC: OGAC.
OGAC. 2010a. Comprehensive HIV prevention for people who inject drugs, revised guidance. Washington, DC: OGAC.
OGAC. 2010b. The President’s Emergency Plan for AIDS Relief: FY2011 country operational plan guidance and appendices. Washington, DC: OGAC.
OGAC. 2010c. Report to Congress on prevention. Washington, DC: OGAC.
OGAC. 2010d. The U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) fiscal year 2009: PEPFAR operational plan. November 2010. Washington, DC: OGAC.
OGAC. 2011a. Guidance for the prevention of sexually transmitted HIV infections. Washington, DC: OGAC.
OGAC. 2011b. PEPFAR guidance on integrating prevention of mother to child transmission of HIV, maternal, neonanatal, and child health and pediatric HIV services. Washington, DC: OGAC.
OGAC. 2011c. The President’s Emergency Plan for AIDS Relief: FY 2012 country operational plan guidance technical considerations. Washington, DC: OGAC.
OGAC. 2011d. Technical guidance on combination HIV prevention for men who have sex with men. Washington, DC: OGAC.
OGAC. 2011e. The U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) Fiscal Year 2010: PEPFAR operational plan. Washington, DC: OGAC.
OGAC. 2011f. The U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) Fiscal Year 2011: PEPFAR operational plan. Washington, DC: OGAC.
OGAC. 2012a. Combination prevention in PEPFAR. Washington, DC: OGAC.
OGAC. 2012b. Email communication between OGAC staff and IOM: “Follow-up queries for IOM PEPFAR evaluation.” Washington, DC: OGAC.
OGAC. 2012c. PEPFAR blueprint: Creating an AIDS-free generation. Washington, DC: OGAC.
OGAC. 2012d. PEPFAR: Addressing gender and HIV/AIDS. Washington, DC: OGAC.
Padian, N. S., S. I. McCoy, S. S. Karim, N. Hasen, J. Kim, M. Bartos, E. Katabira, S. M. Bertozzi, B. Schwartlander, and M. S. Cohen. 2011. HIV prevention transformed: The new prevention research agenda. Lancet 378(9787):269-278.
PEPFAR (U.S. President’s Emergency Plan for AIDS Relief). 2008. World AIDS day 2008: Celebrate life! http://2006-2009.pepfar.gov/112351.htm (accessed November 12, 2012).
PEPFAR/Ethiopia. 2010. PEPFAR country operational plan FY2011. Washington, DC: OGAC.
PEPFAR/Kenya. 2006. PEPFAR country operational plan FY2007. Washington, DC: OGAC.
PEPFAR/Mozambique. 2006. PEPFAR country operational plan FY2007. Washington, DC: OGAC.
PEPFAR/Nigeria. 2006. PEPFAR country operational plan FY2007. Washington, DC: OGAC.
PEPFAR/South Africa. 2006. PEPFAR country operational plan FY2007. Washington, DC: OGAC.
PEPFAR/Tanzania. 2006. PEPFAR country operational plan FY2007. Washington, DC: OGAC.
PEPFAR/Vietnam. 2004. PEPFAR country operational plan FY2005. Washington, DC: OGAC.
PEPFAR/Vietnam. 2005. PEPFAR country operational plan FY2006. Washington, DC: OGAC.
PEPFAR/Vietnam. 2006. PEPFAR country operational plan FY2007. Washington, DC: OGAC.
Petra Study Team. 2002. Efficacy of three short-course regimens of zidovudine and lamivudine in preventing early and late transmission of HIV-1 from mother to child in Tanzania, South Africa, and Uganda (Petra study): A randomised, double-blind, placebo-controlled trial. Lancet 359(9313):1178-1186.
Pronyk, P. M., J. R. Hargreaves, J. C. Kim, L. A. Morison, G. Phetla, C. Watts, J. Busza, and J. D. Porter. 2006. Effect of a structural intervention for the prevention of intimate-partner violence and HIV in rural South Africa: A cluster randomised trial. Lancet 368(9551):1973-1983.
Quinn, T. C., M. J. Wawer, N. Sewankambo, D. Serwadda, C. Li, F. Wabwire-Mangen, M. O. Meehan, T. Lutalo, and R. H. Gray for the Rakai Project Study Group. 2000. Viral load and heterosexual transmission of human immunodeficiency virus type 1. New England Journal of Medicine 342(13):921-929.
Ross, D. A., J. Changalucha, A. I. Obasi, J. Todd, M. L. Plummer, B. Cleophas-Mazige, A. Anemona, D. Everett, H. A. Weiss, D. C. Mabey, H. Grosskurth, and R. J. Hayes. 2007. Biological and behavioural impact of an adolescent sexual health intervention in Tanzania: A community-randomized trial. AIDS 21(14):1943-1955.
Ryan, C. A., S. R. Conly, D. L. Stanton, and N. S. Hasen. 2012. Prevention of sexually transmitted HIV infections through the President’s Emergency Plan for AIDS Relief: A history of achievements and lessons learned. Journal of Acquired Immune Deficiency Syndrome 60(Suppl 3):S70-S77.
Shaffer, N., R. Chuachoowong, P. A. Mock, C. Bhadrakom, W. Siriwasin, N. L. Young, T. Chotpitayasunondh, S. Chearskul, A. Roongpisuthipong, P. Chinayon, J. Karon, T. D. Mastro, and R. J. Simonds for the Bangkok Collaborative Perinatal HIV Transmission Study Group. 1999. Short-course zidovudine for perinatal HIV-1 transmission in Bangkok, Thailand: A randomised controlled trial. Lancet 353(9155):773-780.
Shapiro, R. L., I. Thior, P. B. Gilbert, S. Lockman, C. Wester, L. M. Smeaton, L. Stevens, S. J. Heymann, T. Ndung’u, S. Gaseitsiwe, V. Novitsky, J. Makhema, S. Lagakos, M. Essex, K. McIntosh, T. Peter, S. Kim, E. van Widenfelt, C. Moffat, P. Ndase, P. Arimi, P. Kebaabetswe, P. Mazonde, T. H. Lee, and R. Marlink. 2006. Maternal single-dose nevirapine versus placebo as part of an antiretroviral strategy to prevent mother-to-child HIV transmission in Botswana. AIDS 20(9):1281-1288.
Sherr, L., B. Lopman, M. Kakowa, S. Dube, G. Chawira, C. Nyamukapa, N. Oberzaucher, I. Cremin, and S. Gregson. 2007. Voluntary counselling and testing: Uptake, impact on sexual behaviour, and HIV incidence in a rural Zimbabwean cohort. AIDS 21(7):851-860.
Spensley, A., T. Sripipatana, A. N. Turner, C. Hoblitzelle, J. Robinson, and C. Wilfert. 2009. Preventing mother-to-child transmission of HIV in resource-limited settings: The Elizabeth Glaser Pediatric AIDS Foundation experience. American Journal of Public Health 99(4):631-637.
Sperling, R. S., D. E. Shapiro, R. W. Coombs, J. A. Todd, S. A. Herman, G. D. McSherry, M. J. O’Sullivan, R. B. Van Dyke, E. Jimenez, C. Rouzioux, P. M. Flynn, and J. L. Sullivan for the Pediatric AIDS Clinical Trials Group Protocol 076 Study Group. 1996. Maternal viral load, zidovudine treatment, and the risk of transmission of human immunodeficiency virus type 1 from mother to infant. New England Journal of Medicine 335(22):1621-1629.
Stephenson, J. M., and F. M. Cowan. 2003. Evaluating interventions for HIV prevention in Africa. Lancet 361(9358):633-634.
Stoneburner, R. L., and D. Low-Beer. 2004. Population-level HIV declines and behavioral risk avoidance in Uganda. Science 304(5671):714-718.
Stringer, E. M., M. Sinkala, J. S. A. Stringer, E. Mzyece, I. Makuka, R. L. Goldenberg, P. Kwape, M. Chilufya, and S. H. Vermund. 2003. Prevention of mother-to-child transmission of HIV in Africa: Successes and challenges in scaling-up a nevirapine-based program in Lusaka, Zambia. AIDS 17(9):1377-1382.
Stringer, E. M., B. H. Chi, N. Chintu, T. L. Creek, D. K. Ekouevi, D. Coetzee, P. Tih, A. Boulle, F. Dabis, N. Shaffer, C. M. Wilfert, and J. S. Stringer. 2008. Monitoring effectiveness of programmes to prevent mother-to-child HIV transmission in lower-income countries. Bulletin of the World Health Organization 86(1):57-62.
Stringer, J. S. A., K. Stinson, P. M. Tih, M. J. Giganti, D. K. Ekouevi, T. L. Creek, T. K. Welty, B. H. Chi, C. M. Wilfert, N. Shaffer, E. M. Stringer, F. Dabis, and D. Coetzee. 2013. Population HIV-free survival among children under 2 years of age in 4 African countries: The PEARL Community Survey. PLOS Medicine.
Taha, T. E., N. I. Kumwenda, A. Gibbons, R. L. Broadhead, S. Fiscus, V. Lema, G. Liomba, C. Nkhoma, P. G. Miotti, and D. R. Hoover. 2003. Short postexposure prophylaxis in newborn babies to reduce mother-to-child transmission of HIV-1: NVAZ randomised clinical trial. Lancet 362(9391):1171-1177.
Taha, T. E., N. I. Kumwenda, D. R. Hoover, S. A. Fiscus, G. Kafulafula, C. Nkhoma, S. Nour, S. Chen, G. Liomba, P. G. Miotti, and R. L. Broadhead. 2004. Nevirapine and zidovudine at birth to reduce perinatal transmission of HIV in an African setting: A randomized controlled trial. Journal of the American Medical Association 292(2):202-209.
Thigpen, M. C., P. M. Kebaabetswe, L. A. Paxton, D. K. Smith, C. E. Rose, T. M. Segolodi, F. L. Henderson, S. R. Pathak, F. A. Soud, K. L. Chillag, R. Mutanhaurwa, L. I. Chirwa, M. Kasonde, D. Abebe, E. Buliva, R. J. Gvetadze, S. Johnson, T. Sukalac, V. T. Thomas, C. Hart, J. A. Johnson, C. K. Malotte, C. W. Hendrix, J. T. Brooks, and the T. D. F. Study Group. 2012. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. New England Journal of Medicine 367(5):423-434.
Torpey, K., P. Kasonde, M. Kabaso, M. A. Weaver, G. Bryan, V. Mukonka, M. Bweupe, C. Zimba, F. Mwale, and R. Colebunders. 2010. Reducing pediatric HIV infection: Estimating mother-to-child transmission rates in a program setting in Zambia. Journal of Acquired Immune Deficiency Syndrome 54(4):415-422.
Tudor Car, L., M. H. Van Velthoven, S. Brusamento, H. Elmoniry, J. Car, A. Majeed, P. Tugwell, V. Welch, A. Marusic, and R. Atun. 2012. Integrating prevention of mother-to-child HIV transmission programs to improve uptake: A systematic review. PLOS ONE 7(4):e35268.
Turner, A. N., C. S. Morrison, N. S. Padian, J. S. Kaufman, R. A. Salata, T. Chipato, F. A. Mmiro, R. D. Mugerwa, F. M. Behets, and W. C. Miller. 2007. Men’s circumcision status and women’s risk of HIV acquisition in Zimbabwe and Uganda. AIDS 21(13):1779-1789.
UCSF (University of California, San Francisco). 2012. Ghana—global reserach at UCSF. http://globalresearch.ucsf.edu/ghana.html (accessed December 4, 2012).
UNAIDS (Joint United Nations Programme on HIV/AIDS). 2007. Practical guidelines for intensifying HIV prevention: Towards a universal approach. Geneva: UNAIDS.
UNAIDS. 2009. Condoms and HIV prevention: Position statement by UNAIDS, UNFPA, and WHO. http://www.unaids.org/en/resources/presscentre/featurestories/2009/march/20090319preventionposition (accessed February 7, 2012).
UNAIDS. 2010. UNAIDS report on the global AIDS epidemic—2010. Geneva: UNAIDS.
UNAIDS. 2011. Global plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive. Geneva: UNAIDS.
UNAIDS. 2012a. AIDSInfo, maintained by UNAIDS. Geneva: UNAIDS.
UNAIDS. 2012b. UNAIDS report on the global AIDS epidemic: 2012. Geneva: UNAIDS.
UNDP (United Nations Development Programme). 2012. Global commission on HIV and the law: Risks, rights, and health. New York: UNDP.
UNFPA (United Nations Population Fund). 2001. HIV/AIDS, Gender and Sex Work. New York: UNFPA.
UNICEF (United Nations Children’s Fund). 2008a. Guidance on ensuring effective supply chain planning for commodities needed for implementation and scale up of services for the prevention of mother to child transmission (PMTCT) of HIV infection. New York: UNICEF.
UNICEF. 2008b. Towards universal access, scaling up HIV services for women and children in the health sector. Progress report 2008. New York: UNICEF.
UNICEF. 2012. Mother-baby pack update: More efforts needed to prevent mother-to-child transmission of HIV. http://www.unicef.org/aids/index_58357.html (accessed November 12, 2012).
United Nations. 2001. Declaration of commitment on HIV/AIDS. New York: United Nations.
UNODC (United Nations Office of Drugs and Crime). 2008. Principles of drug dependence treatment. Vienna, Austria: UNODC.
U.S. Census Bureau. 2010. International data base population estimates and projections methodology. Washington, DC: U.S. Census Bureau.
USAID (U.S. Agency for International Development). 2011a. Integrating multiple PEPFAR gender strategies to improve HIV interventions: Recommendations from five case studies of programs in Africa. Washington, DC: USAID.
USAID. 2011b. Integrating PEPFAR gender strategies into HIV programs for most-at-risk populations. Washington, DC: USAID.
Van Damme, L., A. Corneli, K. Ahmed, K. Agot, J. Lombaard, S. Kapiga, M. Malahleha, F. Owino, R. Manongi, J. Onyango, L. Temu, M. C. Monedi, P. Mak’Oketch, M. Makanda, I. Reblin, S. E. Makatu, L. Saylor, H. Kiernan, S. Kirkendale, C. Wong, R. Grant, A. Kashuba, K. Nanda, J. Mandala, K. Fransen, J. Deese, T. Crucitti, T. D. Mastro, D. Taylor, and F. EM-PrEP Study Group. 2012. Preexposure prophylaxis for HIV infection among African women. New England Journal of Medicine 367(5):411-422.
Voluntary HIV-1 Counseling and Testing Efficacy Study Group. 2000. Efficacy of voluntary HIV-1 counselling and testing in individuals and couples in Kenya, Tanzania, and Trinidad: A randomised trial. Lancet 356(9224):103-112.
Wawer, M. J., F. Makumbi, G. Kigozi, D. Serwadda, S. Watya, F. Nalugoda, D. Buwembo, V. Ssempijja, N. Kiwanuka, L. H. Moulton, N. K. Sewankambo, S. J. Reynolds, T. C. Quinn, P. Opendi, B. Iga, R. Ridzon, O. Laeyendecker, and R. H. Gray. 2009. Circumcision in HIV-infected men and its effect on HIV transmission to female partners in Rakai, Uganda: A randomised controlled trial. Lancet 374(9685):229-237.
Weinhardt, L. S., M. P. Carey, B. T. Johnson, and N. L. Bickham. 1999. Effects of HIV counseling and testing on sexual risk behavior: A meta-analytic review of published research, 1985-1997. American Journal of Public Health 89(9):1397-1405.
WHO (World Health Organization). 2004. Effectiveness of sterile needle and syringe programming in reducing HIV/AIDS among injecting drug users. Geneva: WHO.
WHO. 2006. Antiretroviral drugs for treating pregnant women and preventing HIV infection in infants: towards universal access. Geneva: WHO.
WHO. 2007. Guidance on global scale-up of the prevention of mother-to-child transmission of HIV. Geneva: WHO.
WHO. 2008a. Towards universal access: Scaling up priority HIV/AIDS interventions in the health sector: Progress report 2008. Geneva: WHO.
WHO. 2008b. Universal access to safe blood transfusion. Geneva: WHO.
WHO. 2009a. Guidelines for the psychosocially assisted pharmacological treatment of opioid dependence. Geneva: WHO.
WHO. 2009b. The Melbourne declaration on 100% voluntary non-remunerated donation of blood and blood components. Geneva: WHO.
WHO. 2010a. Antiretroviral drugs for treating pregnant women and preventing HIV infection in infants: Recommendations for a public health approach (2010 version). Geneva: WHO.
WHO. 2010b. Towards universal access: Scaling up priority HIV/AIDS interventions in the health sector: Progress report 2010. Geneva: WHO.
WHO. 2011. Global HIV/AIDS response: Epidemic update and health sector progress towards universal access. Progress report 2011. Geneva: UNAIDS.
WHO. 2012a. Programmatic update: Use of antiretroviral drugs for treating pregnant women and preventing HIV infection in infants. Geneva: WHO.
WHO. 2012b. Service delivery approaches to HIV testing and counselling (HTC): A strategic HTC policy framework. Geneva: WHO.
WHO Regional Office for South-East Asia. 2009. Management of common health problems of drug users. Indraprastha Estate, Mahatma Gandhi Marg, New Delhi, India: WHO.
World Health Assembly. 2010. A63/20. Availability, safety and quality of blood products: Report by the Secretariat. Geneva: World Health Assembly.










































































