Interim Report of the Committee on Geographic Variation in Health Care Spending and Promotion of High-Value Care: Preliminary Committee Observations
In 2009, following negotiations related to passage of the Patient Protection and Affordable Care Act (ACA),1 a group of U.S. House of Representatives members, known as the Quality Care Coalition, asked the Secretary of the U.S. Department of Health and Human Services (HHS), Kathleen Sebelius, to sponsor two Institute of Medicine (IOM) studies focused on geographic payments under Medicare, independent of final health reform legislation (Sebelius, 2010). The first study evaluated the accuracy of Medicare’s geographic adjustment factors, which alter physician and hospital payment rates based on specific, geographically based input prices (IOM, 2011, 2012). For the second study, the subject of this interim report, the IOM Committee on Geographic Variation in Health Care Spending and Promotion of High-Value Care (“the committee”) was asked to investigate geographic variation in health care spending and quality and to analyze Medicare payment polices that could encourage high-value care, including adoption of a geographically based value index. This index would account for both the health benefit obtained from health care services delivered and the cost of those services, as discussed later in this report. The committee’s final report is due for release in summer 2013.
This interim report is designed to provide the committee’s preliminary observations for the 113th Congress as it considers further Medicare reform. This report contains only key preliminary observations related primarily to the committee’s commissioned analyses of Medicare Parts A (Hospital Insurance program), B (Supplementary Medical Insurance program) and D (outpatient prescription drug benefit), complemented by other empirical investigations. It does not contain any observations related to the committee’s commissioned analyses of the commercial insurer population, Medicare Advantage, or Medicaid, which will be presented in the committee’s final report after completion of quality-control activities.
This interim report excludes conclusions or recommendations related to the committee’s consideration of the geographic value index or other payment reforms designed to promote highvalue care. Additional analyses are forthcoming, which will influence the committee’s deliberations. These analyses include an exploration of how Medicare Part C (Medicare Advantage) and commercial spending, utilization, and quality vary compared with, and possibly are influenced by, Medicare Parts A and B spending, utilization, and quality. The committee also is assessing potential biases that may be inherent to Medicare and commercial claims-based measures of
___________________________
1 Patient Protection and Affordable Care Act, Public Law 111–148, 111th Cong., 2nd sess., (March 23, 2010).
health status. Based on this new evidence and continued review of the literature, the committee will confirm the accuracy of the observations presented in this interim report and develop final conclusions and recommendations, which will be published in the committee’s final report.
Geographic Variation and the Pursuit of Value in U.S. Health Care
For more than three decades, experts at the Dartmouth Institute for Health Policy and Clinical Practice (“Dartmouth”) have documented significant variation in Medicare spending and quality across geographic regions, producing a series of maps that have become known as the Dartmouth Atlas (Dartmouth Institute for Health Policy and Clinical Practice, 2013b; Wennberg and Cooper, 1998). From this seminal body of work, a finding emerged that dramatically changed the health care policy debate in the United States; health care spending (including utilization) rates varied widely, but did not appear to be consistently related to health outcomes or patient satisfaction among Medicare beneficiaries (Baicker and Chandra, 2004; Fisher et al., 2003a,b; MedPAC, 2009, 2011; Zhang et al., 2010b).
The debate about geographic variation and value essentially involves the role that geographic variation should play in Medicare health care policy reform. Seeking strategies to reduce Medicare costs, policy makers naturally wondered whether cutting payment rates to high-cost areas would save money without adversely affecting health care quality for Medicare beneficiaries. According to one study, Medicare spending would drop by as much as 29 percent if practices of low-cost, high-quality regions were adopted nationwide, significantly improving health care for Medicare beneficiaries (Wennberg et al., 2002). Moreover, some argue that Medicare’s traditional fee-for-service reimbursement system, which rewards volume rather than value of services provided, can generate unfair payments. For instance, congressional representatives in areas generally associated with high-quality, low-cost health care argue that highly efficient hospitals and providers are penalized under the current payment system.2
Based on these observations, some policy makers believe that Medicare should adjust hospital and physician reimbursement rates based on regional performance to encourage more uniform health care system performance for Medicare beneficiaries across hospital markets (Hahn, 2009).3,4,5 Proponents of a geographic value index theorize that regional payment adjustments would encourage all hospitals and providers within an area to coordinate care, leading to better system efficiencies across the entire region.2,6,7
Other health care experts counter that recommendations stemming from Dartmouth’s research conflate the issue of improving value with that of reducing geographic variation. Geographic variation in health care resource use and quality reflects both “acceptable” and “unacceptable” sources of variation. “Acceptable” sources of variation tend to be health and demographic characteristics that lead to a greater need for care. Aspects of health status or population demographics account for significant variation among geographic areas (Skinner et al., 2010; Wennberg et al., 2002; Zuckerman et al., 2010). Spending calculations for any unit of analysis, such as geographic units, should adjust for such characteristics to shield providers from any negative effects associated with treating higher-risk populations. “Unacceptable” sources of variation
___________________________
2 Personal communication, Michael Kitchell, Iowa Medical Society, January 7, 2011.
3 Medicare Payment Improvement Act of 2009, S. 1249, 111th Cong., 1st sess. (June 12, 2009).
4 Medicare Payment Improvement Act of 2009, H.R. 2284, 111th Cong., 1st sess. (June 15, 2009).
5 It should be noted that Dartmouth researchers do not recommend regional payments (Skinner et al., 2010).
6 Personal communication, Michael Richards, Gundersen Lutheran Health Services, January 17, 2011.
7 U.S. Congress, Senate. 2009. Health Care Reform. 111th Cong. (July 30, 2009).
include aspects of system inefficiencies, such as overuse of low-value services and unnecessary duplication of services. Reducing geographic variation is desirable only to the degree that measured variation represents health care inefficiencies. And it is not clear that any existing methodology can adequately disentangle acceptable and unacceptable variation (Bach, 2010; Bernstein et al., 2011; Bertko, 2003; Sheiner, 2012; Zuckerman et al., 2010).
Still other health care experts argue that regionally based payments are inherently unfair and would fail to create market incentives necessary to promote high-value, patient-centered care. Region-level measures of variation mask variation within regions. Such variation means provider payments based on regional area performance would reward inefficient providers in low-cost regions and punish more efficient providers in high-cost regions (MedPAC, 2007).
To better understand the relevance of geographic variation to payment policies designed to promote value across the U.S. health care system, the Centers for Medicare & Medicaid Services (CMS) contracted with the IOM to conduct a 3-year consensus study under the guidance of a 20-member committee. The committee included experts in health economics, statistics, health care financing, value-based health care purchasing, health services research, health law, and health disparities. The committee’s Statement of Task (see Appendix B) draws on language in earlier federal health care reform legislation8 and includes the following three tasks:9
(1) to independently evaluate geographic variation in health care spending levels and growth among Medicare, Medicaid, privately insured, and uninsured populations in the United States;
(2) to make recommendations for changes in Medicare Parts A, B, and C payments, considering findings from task (1) of the study and changes to Medicare payment systems under the ACA; and
(3) to address whether Medicare payments for physicians and hospitals should incorporate a value index that would modify provider payments based on geographic-area performance. This interim report largely focuses on this third question.
RESEARCH FRAMEWORK AND STATISTICAL MODELING APPROACH
To respond to its statement of task, the committee identified two basic questions:
(1) What is known about geographic variation in health care spending, utilization, and quality?
(2) Should geographically based measures of value be used to adjust Medicare fee-for-service hospital and provider reimbursement rates in a geographic region?
To help answer these questions, the committee commissioned an extensive body of new statistical analyses and four papers from subject-matter experts and held two public workshops to complement its review of existing literature. The committee’s statistical analyses were focused
___________________________
8 The Affordable Health Care for America Act, H.R. 3962, 111th Cong., 1st sess. (October 29, 2009).
9 Preservation of Access to Care for Medicare Beneficiaries and Pension Relief Act of 2010, Public Law 111-192, 111th Cong., 2nd sess. (June 25, 2010).
on describing and accounting for geographic variation in health care spending, utilization, and quality; performing quantitative and qualitative syntheses of those analyses; and conducting a micro-simulation analysis of impacts of certain potential committee recommendations. As discussed above, only results related to Medicare Parts A, B, and D are included in this interim report. All other results will be presented in the committee’s final report.
The following six subcontractors supported the committee’s statistical analytic work: Acumen, LLC; Dartmouth; Harvard University; The Lewin Group; Precision Health Economics (PHE); and the University of Pittsburgh (“Pittsburgh”). Using large public and commercial claims databases (listed in Box 1), these subcontractors examined variation in aggregate health care spending, utilization, and quality across different units of analysis, including various geographic areas, as well as hospitals and providers.
The subcontractors performed regression analyses to quantify how demographic and health plan characteristics of beneficiaries, as well as price and market factors, affect spending across geographic areas. In addition to the overall Medicare population (aggregate analyses), 15 subpopulations with specific acute and chronic clinical conditions were studied (cohort analyses). The extent of geographic variation was examined within and across geographic units; across clinical condition cohorts, and over time. Per CMS’s direction, Medicare expenditures related to graduate medical education (GME), disproportionate share hospitals (DSH), and health information technology (HIT) were not included in any spending calculations.
|
Subcontractor |
Data Source |
|
Acumen, LLC |
Medicare Parts A, B, and D, as well as Medicare Advantage (Part C) dataa |
|
Harvard University |
Thomson Reuters MarketScan Commercial Claims and Encounters database |
|
The Lewin Group |
Optum De-identified Normative Health Information Database (dNHI) database and CMS Chronic Conditions Warehouse database |
|
University of Pittsburgh |
Medicare Part D (Prescription Drug Plans) |
|
Dartmouth Institute for Health Policy and Clinical Practice |
Medicare Parts A and B |
|
Precision Health Economics |
Synthesized data from the aforementioned analyses, as well as the uninsured |
SOURCE: http://www.iom.edu/geovariationinterim.
_____________________
a Analyses include all spending for dual-eligibles (by both Medicare and Medicaid) that is used for Medicare-covered services.
The committee defined geographic units consistent with prior literature, such as hospital referral regions (HRRs), hospital service areas (HSAs), and metropolitan statistical areas (MSAs). Box 2 defines these units, and Figure 1 provides a map of the United States by HRRs. The committee focused largely on variation between and within HRRs. The subcontractor analyses also examined spending, utilization, and quality for populations with specific diseases or conditions across HRRs.
Because of concerns involving proprietary information and patient privacy, the committee was unable to access individual claims data used by the subcontractors. Consequently, the committee’s results are based predominantly on aggregated output supplied by the subcontractors. However, the committee also contracted with two independent firms, IMPAQ International and RTI International, to perform a quality-control audit of the research methods and statistical analyses applied to this IOM study. The results of these audits will be available upon release of the committee’s final report.
BOX 2
Definitions of Geographic Units Frequently Used in Health Services Research
• Hospital referral regions (HRRs): Created by Dartmouth to represent regional health care markets for tertiary (complex) medical care. Dartmouth defined 306 HRRs by assigning hospital service areas (HSAs) to regions where the greatest proportion of major cardiovascular procedures were performed, “with minor modifications to achieve geographic contiguity, a minimum total population size of 120,000, and a high localization index” (Dartmouth Institute for Health Policy and Clinical Practice, 2013a).
• Hospital service areas (HSAs): Created by Dartmouth and defined by assigning to an HSA the ZIP codes from which a hospital or several hospitals draw the greatest proportion of their Medicare patients. There are 3,426 HSAs (Dartmouth Institute for Health Policy and Clinical Practice, 2013a). The Centers for Medicare & Medicaid Services (CMS) adjusts hospital payments according to input prices calculated for HSAs.
• Metropolitan statistical areas (MSAs): Created by the Office of Management and Budget using counties. Each of 441 MSAs includes one or more counties with one core urban area of 50,000 individuals or more, as well as adjacent counties exhibiting a high degree of social and economic integration (as measured by such factors as commuting patterns) with an urban core (OMB, 2010). Areas that do not qualify as MSAs are often classified as “outside” MSAs (OMB, 2010) or non-MSAs. CMS adjusts physician payments according to input prices calculated for MSAs.
FIGURE 1 Map of the United States with hospital referral region boundaries.
SOURCE: Generated by The Lewin Group on behalf of the committee.
An important part of the committee’s Statement of Task and research framework focuses on “whether Medicare payment systems should be modified to provide incentives for high-value, high-quality, evidence-based, patient-centered care through adoption of a value index (based on measures of quality and cost) that would adjust payments on a geographic area basis.” To create a research framework that would generate useful information for policy makers, the committee needed to understand the dimensions of the geographically based value index, described in its Statement of Task, and related terms (see the glossary in Appendix A).
In general, a value index is a relative measure of value—for example, a measure of improvement in patient-centered, clinical health outcomes per unit of resources used in one area relative to the national average. The committee defined health care value as the excess (or short-fall) of overall health benefit and/or well-being produced net of health care cost. To operationalize this definition, health benefit and cost must be valued in the same units. The only unit conventionally used for this purpose is dollars.10 Conceptually, then, health benefit and well-being are assessed as health outcomes, valued in dollars. In principle, the measure of health care costs should reflect the opportunity costs of the resources used to produce medical services, but these
___________________________
10 The committee’s final report will address challenges associated with value measurement.
costs are not typically observed. Consequently, the committee defines “costs” as Medicare spending for services for the purpose of this report.
Value indexes can take specific forms and serve many purposes. In health care, indexes can be used to adjust hospital or provider reimbursement rates based on measures of relative performance. For example, CMS’s hospital value-based purchasing program and physician payment modifier (authorized under Sections 3001 and 3007 of the ACA, respectively) adjust hospital and provider payments according to observed hospital and individual provider performance compared with national averages. Health benefit and well-being are, of course, affected by many factors other than the provision of health services, such as individual behavior, biology, and genetics (McGinnis et al., 2002). If a value index influences health care payments, it is important that related measures of health outcomes be attributable to specific health care interventions. Therefore, clinical health outcomes (i.e., the health state of a patient resulting from health care) may be preferred measures of health benefit or well-being (AHRQ, 2013).
As described above, this interim report will focus primarily on a geographically based value index. Section 1159 of the Affordable Health Care for America Act (H.R. 3962), on which the committee’s charge is based, asked the IOM to consider a “value index based on a composite of appropriate measures of quality and cost that would adjust provider payments on a regional or provider-level basis.”11 Thus, the committee limited its evaluation of a “geographically based value index” to a relative ratio that uses area-level composite measures of clinical health outcomes and cost to adjust individual hospital and provider payments under Medicare Parts A and B (“a geographic value index”).12
EVALUATION OF A GEOGRAPHIC VALUE INDEX
Whether a geographic value index is an appropriate policy depends on whether payment modifications pursuant to the payment model effectively shift provider behavior toward greater efficiency (i.e., using fewer resources) without substantially diminishing health care outcomes. Additionally, a geographic value index for Medicare must generate hospital and provider payments that are perceived as fair. Both conceptual and empirical limitations exist.
Conceptual Assessment of a Geographic Value Index
Health care decision making generally occurs at the individual practitioner or organizational level, such as hospitals or physician groups (IOM, 2001, 2010), not at the geographic region level.13 Payments that target these actors are more likely to trigger behavioral change, because providers will be held directly accountable for the value of health care services delivered (Baicker and Chandra, 2004; McKethan et al., 2009).
___________________________
11 Supra., note 8 at §1159(c).
12 Note that such an index differs from CMS’s hospital value-based purchasing program and physician payment modifier, as described above.
13 Public health measures, such as educational programs, may be directed at the geographic region. However, such interventions are not typically covered under Medicare, and they are typically the domain of public health agencies, such as the Centers for Disease Control and Prevention and state and county health departments (Salinsky, 2010).
Observation 1
Health care decision making occurs at the individual practitioner or organizational level, such as hospitals or physician groups, not at the geographic region level.
A geographic value index does not target an appropriate level of clinical decision making to trigger behavioral change at the patient-provider level. In fact, a geographic value index is not designed to target any level of actual decision making. Rather, it treats all providers in a geographic area alike, assuming that area-level payment modifications will incentivize the various decision makers within an area to coordinate care and improve efficiencies across the area. However, two practical considerations suggest otherwise. First, collaboration among competing providers, absent clinical and financial integration, may raise antitrust issues (Kass and Linehan, 2012).
Second, payment modifications that target large areas do not link individual physician behaviors to spending increases or decreases. Consequently, a physician (or physician group practice) who reduces volume does not see a proportional increase in payment, but rather sees reduced income (MedPAC, 2007). For example, the sustainable growth rate (SGR) system, which is designed to automatically decrease physician payments each year if their total expenditures exceed Medicare spending targets in the previous year (and vice versa), has not incentivized providers to constrain spending growth. Rather, overall spending has increased annually since 2003 (Hahn and Mulvey, 2011).
While setting provider payments by region, as under the geographic value index, is more targeted than the current SGR, similar concerns about altering provider behavior exist. Regions large enough to have year-to-year stability in spending (e.g., HRR, MSA), are still too large for any individual provider to have enough influence over total expenditures to alter provider behavior patterns (MedPAC, 2007). One exception is when a single delivery system dominates care in an area. However, this scenario does not pertain to the majority of the country because currently only 9 percent of physicians practice in groups of 10 or more (Audet, 2012).
In recent years, multiple stakeholders (e.g., payers, providers, employers, local governments) have formed region- or community-based “collaboratives,” focused on improving the value of health care for their populations.14 In some cases, payments may also appropriately target these regional or community-based collaboratives. Like accountable care organizations and other integrated organizations, collaboratives vary in size and structure and may or may not align with traditional geographic units and, thus, are distinct from geographic areas targeted by a geographically based value index.
Empirical Assessment of a Geographic Value Index
Proponents of a geographic value index argue that paying more (per unit of service or in total) to providers in areas that are better stewards of health care resources is fair. But area-level payments are only fair under certain conditions. First, all hospitals and providers within an area must be equally deserving of the reward (or penalty), implying that they behave similarly.
___________________________
14 These collaboratives may implement a range of initiatives, including but not limited to improvement in data collection and dissemination, efficient promotion of health service delivery, and provision of financial incentives for high-value care (Alliance for Health Reform, 2013).
Second, assuming that all providers are behaving similarly, performance levels in high-value areas must be achievable in low-value areas through the elimination of inefficiencies. In other words, the differences in measured value between low- and high-spending areas cannot include differences stemming from underlying health status and other acceptable sources of variation.
The committee commissioned original analyses to test the accuracy of these premises empirically. Appendix A defines technical terms related to these analyses. The committee’s preliminary observations are discussed below. In its final report, the committee will compare the results of its own empirical work with evidence from the published literature.
Observation 2
Substantial variation in spending and utilization exists within progressively smaller units of analysis.
To determine whether provider organizations within an identified area behave similarly, the committee examined patterns of health care resource use across sub-regions, service types, and clinical condition categories, as well as condition-specific quality measures across HRRs. As noted above, if providers do not behave similarly, a fairness problem arises whereby low-value providers are rewarded simply by practicing in areas that are on average high-value (the reverse is also true). Starting with HRRs, the committee examined the amount of variation within progressively smaller units of analysis (HSA, hospital, practice, and individual provider level).
Variation at the Hospital Service Area Level Within Hospital Referral Regions
The committee investigated the extent and range of variation in spending in sub-regions within HRRs to test whether the HRR is an appropriate geographic unit upon which to base provider payment. HSAs have been defined within HRRs, with an average of 11 per HRR, although there is considerable variability (a range of 1 to 76 HSAs per HRR).15 As one measure of variability within an HRR, the committee examined the ratio of the highest-spending to the lowest-spending HSA within each HRR. For example, at the median (50th percentile) of these ratios, the highest-spending HSA spends 24 percent more than the lowest-spending HSA (Acumen LLC, 2013a, p. 41). In the 76 highest-spending HRRs (above the 75th percentile), the highest-spending HSA within each HRR spends at least 36 percent more than the lowest-spending HSA within that HRR.
An analogous assessment analyzed how much variation exists between HSAs within an HRR as opposed to across HRRs. In analyses for the committee, Pittsburgh investigators found that approximately 57 percent of the variation in adjusted HSA medical spending is within HRRs, compared with 43 percent between HRRs (University of Pittsburgh, 2013, p. 13). Similarly, about 59 percent of the variation in adjusted HSA Medicare drug spending is within HRRs, compared to 41 percent between HRRs. For example, Manhattan (New York) is one of the HRRs with the highest adjusted drug spending, while Albuquerque (New Mexico) is one of the lowest, yet the lowest-spending HSA in Manhattan spends less than 25 percent of HSAs within Albu-querque. In addition to heterogeneity in spending, there is substantial heterogeneity in utilization patterns.
___________________________
15 Personal communication, Jonathan S. Skinner, Ph.D., Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine, February 12, 2013.
To illustrate the substantial local variation in drug and non-drug spending and utilization, the Pittsburgh investigators calculated that about half of the HSAs located within the borders of the highest-drug-spending HRR quintile are not in the highest-drug-spending quintile of HSAs, and approximately half of the HSAs in the lowest-drug-spending quintile of HRRs are not in the lowest-drug-spending quintile of HSAs. Figures 2 and 3 illustrate this quintile analysis for adjusted pharmacy spending for HRRs and HSAs. The light blue and light pink shaded areas that lie outside the heavy lines are, respectively, high- and low-drug-spending HSAs that are not in high- or low-drug-spending HRRs. Non-shaded areas within the heavy lines are, respectively, not high- and not low-drug-spending HSAs within high- and low-drug-spending HRRs. In sum, these maps show substantial misalignment of high-drug-spending HSAs and HRRs.
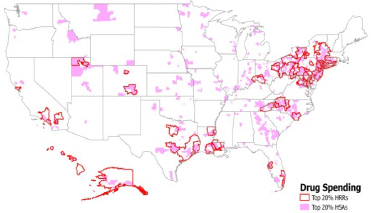
FIGURE 2 Top 20 percent of hospital referral regions and hospital service areas in drug spending.
SOURCE: University of Pittsburgh, 2013, p. 21.
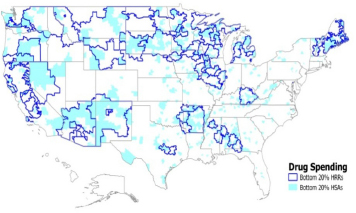
FIGURE 3 Bottom 20 percent of hospital referral regions and hospital service areas in drug spending.
SOURCE: University of Pittsburgh, 2013, p. 21.
Variation at the Hospital Level Within Hospital Referral Regions
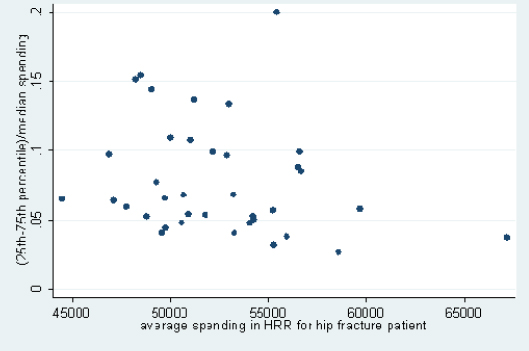
Hospitals in the same HRR also vary substantially in their resource use, as can be seen from the committee’s analysis of data from Dartmouth that examined cohorts of patients treated for three major conditions. This variation exists in both lower- and higher-spending HRRs, meaning that there are high-spending hospitals in low-spending regions and low-spending hospitals in high-spending regions (this analysis was limited to HRRs with four or more hospitals with data on spending for a given condition). Figures 4, 5, and 6, respectively, display results of analyses of variation in Medicare spending at the hospital level within each HRR for the three clinical conditions examined—stroke, hip fracture, and heart attack—with adjustments for input price and health status. For example, referencing the right-most point in Figure 4, in HRRs that spend approximately $45,000 per stroke patient, the difference between spending for hospitals in the 75th and 25th percentiles is around 17 percent of the median value. Differences between hospitals at more extreme points, such as the 90th and 10th percentiles, would, of course, be even larger. Figures 4 through 6 demonstrate that hospitals within HRRs do not tend to be uniformly high- or low-cost.
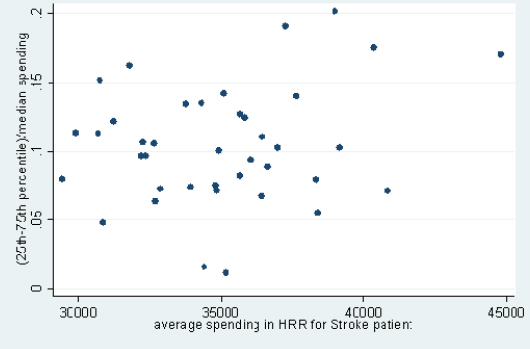
FIGURE 4 Variation in price- and risk-adjusted Medicare spending for stroke in a hospital referral region.
SOURCE: Committee analysis of unpublished Dartmouth data.16
___________________________
16 Personal communication, Jonathan S. Skinner, Ph.D., Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine, February 6, 2013.
FIGURE 5 Variation in price- and risk-adjusted Medicare spending for hip fracture in a hospital referral region.
SOURCE: Committee analysis of unpublished Dartmouth data.16
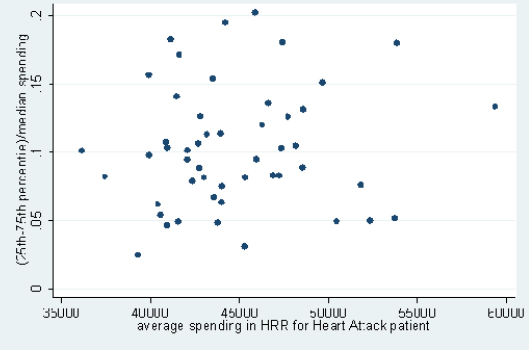
FIGURE 6 Variation in price- and risk-adjusted Medicare spending for heart attack in a hospital referral region.
SOURCE: Committee analysis of unpublished Dartmouth data.16
Variation Within Provider Practices
A large body of work finds variation among physicians within specialties (e.g., cardiology) (Cherkin et al., 1994; Lucas et al., 2010; MedPAC, 2009). Yet, the committee could not examine variation below the hospital level in its original analyses because of privacy concerns. A review of the relevant literature revealed that this issue has received little attention. For example, a 2000 grant project found that individual provider practice patterns vary “within the same specialty in the same practice treating panels of patients exhibiting the same conditions” (Center for Research in Ambulatory Health Care Administration, Inc, 2000).
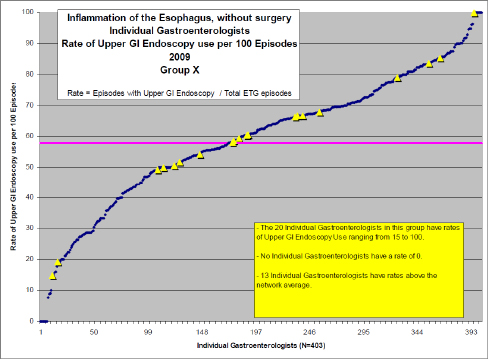
However, health plans and hospital administrators provided the committee with supplementary data that showed variation in health care resource use and quality within the physician group practice and individual physician levels. For more than two dozen clinical conditions, Blue Cross Blue Shield of Massachusetts (BCBSMA) regularly examines variations in practice patterns among physicians within a particular specialty, comparing physicians with their immediate practice peers as well as all comparable specialists across the state. BCBSMA uses episode treatment groups to establish a patient population with a defined clinical condition and then to identify the one or two most salient differences among physicians in treating such patients—for example, among patients with a new episode of knee pain, the tendency of primary care physicians to refer patients to an orthopedic surgeon or not, or among patients with simple hypertension, the tendency of cardiologists to prescribe an angiotensin-converting enzyme inhibitor versus a more expensive, branded angiotensin receptor blocker. For each condition, these data show that variation among specialists who work in the same group practice is as great as variation among specialists across the entire state.17 For example, there is almost as much variation in the use of upper gastrointestinal (GI) endoscopy for patients with gastroesophageal reflux disorder seen by a gastroenterologist (a major driver of spending in that specialty) among 20 physicians within a single practice (denoted by the yellow triangles) as exists for all gastroenterologists in the state (denoted by the blue dots)18 (see Figure 7).
___________________________
17 Personal communication, Dana Gelb Safran, Blue Cross Blue Shield of Massachusetts, July 17, 2011.
18 It should be noted that the committee was not provided with measures of variability at the patient level, and some of this variation is attributable to random differences in the nature of patients seen rather than the physician’s style of practice. Nonetheless, the variation is, in all likelihood, substantially larger than what could have been explained by chance.
FIGURE 7 Use of upper GI endoscopy among gastroenterologists treating gastroesophageal reflux disease.19
Variation at the Individual Provider Level Across Clinical Conditions
Even individual physician performance varies across different measures of efficiency. A study by Partners HealthCare, of six primary care physicians (PCPs) within the same practice group found that individual levels of utilization and quality varied across nine distinct measures associated with diabetes, cholesterol, and hypertension control; ordering of radiology tests and generic prescriptions; and rate of admissions and emergency department visits (Partners HealthCare, 2012). No single physician was high or low across all measures; instead, each physician was above average for some and below average for others. Similar analyses have been generated for more than 1,100 PCPs and many specialty groups within the Partners health system. These data demonstrate that it is difficult to classify even individual physicians as high- or low-value providers. The committee was not provided with standard errors for these analyses, and some of the variation observed is random. Nonetheless, this variation at the physician level suggests that variation among providers within HSAs could be substantial, so estimates of variation within HRRs attributable to variation among HSAs are a lower bound on variation among all providers within an HRR. Put another way, it is highly unlikely that all physicians within an HSA practice similarly. As a result, area-level performance calculations would likely mischaracterize the actual value of services delivered by many providers and hospitals, resulting in unfair payments.
___________________________
19 Personal communication, Dana Gelb Safran, Blue Cross Blue Shield of Massachusetts, July 17, 2011.
Observation 3
Quality across conditions and treatments varies widely within HRRs; utilization across conditions is moderately correlated within HRRs.
Additional Empirical Analyses
The delivery of health care has become increasingly specialized. Although claims-based quality measures are sparse in some specialized clinical areas, these measures are plentiful and robust in other areas (CMS, 2011). Because a geographic value index calculates a composite quality score for a region, many providers in an area will be assessed on measures not applicable to their practice. Therefore, for a geographic value index to generate fair reimbursement rates, data should indicate that performance across a wide range of quality measures is relatively consistent within an area.
To test this notion, the committee performed pairwise correlations between 18 condition-specific quality measures (Acumen, LLC, 2013a, p. 129). Correlations ranged from –0.38 (between diabetes retinal screening and cholecystectomy measures) to 0.67 (between chronic obstructive pulmonary disease [COPD] and congestive heart failure [CHF] admissions). Approximately 38 percent of quality measures are negatively correlated with each other, 40 percent have correlation coefficients between 0 and 0.19, and only one-fifth are above 0.20. In short, areas with high scores on some quality measures do not necessarily have high scores on other quality measures, particularly if the measures relate to conditions treated by different types of specialists. As a result, an area in which providers deliver high-value treatment for one condition may well have providers who deliver low-value treatment for other conditions, thus again demonstrating that provider performance within an area is not homogeneous.
Utilization measures across conditions are more highly correlated than quality measures within an HRR (see Table 1); nonetheless, an HRR that uses many services to treat a given condition (e.g., prostate cancer) does not necessarily use many services to treat another (e.g., lower back pain).
|
|
||||||
| LBP | Cataracts | CHF | Breast Cancer | Prostate Cancer | Cholecystectomy | |
|
|
||||||
| LBP | 1.00 | |||||
| Cataracts | 0.477 | 1.00 | ||||
| CHF | 0.907 | 0.483 | 1.00 | |||
| Breast Cancer | 0.574 | 0.311 | 0.583 | 1.00 | ||
| Prostate Cancer | 0.485 | 0.230 | 0.502 | 0.524 | 1.00 | |
| Cholecystectomy | 0.593 | 0.353 | 0.624 | 0.406 | 0.406 | 1.00 |
|
|
||||||
NOTE: CHF = congestive heart failure; LBP = lower back pain.
SOURCE: Acumen, LLC, 2013a, p. 127.
Observation 4
Although a non-trivial amount of geographic variation can be explained by specific demographic and, potentially, health status variables, a substantial amount of variation remains unexplained.
As discussed earlier, variation in health care resources use and quality across geographic areas reflects “acceptable” and “unacceptable” sources of variation, where unacceptable sources of variation (e.g., provider style unrelated to patient health status) represent inefficiencies in the health care system. Some proponents of the geographic value index contend that, even if providers behave differently within an area, area-level payments may still be appropriate, reasoning that all remaining variation, after controlling for acceptable sources of variation, represents inefficiencies correctable through area-level payment incentives. To evaluate this assertion, the committee commissioned analyses to determine whether all sources of variation can be identified.20
Table 2 shows how the spending ratio in high- (90th percentile) and low- (10th percentile) spending regions changes as one adjusts for generally acceptable sources of variation (i.e., age, sex, and health status) and various market-level factors,21 which may include both acceptable and unacceptable sources of variation. Adjusting for age and sex at the HRR level has a negligible effect on geographic variation in spending, indicating that the age and sex distribution is similar across HRRs. Health status, by contrast, does considerably decrease spending variation between high- and low-spending regions.22 Cluster 5 in Table 2 indicates that adjusting for race and income also has a negligible effect on variation, after health status is accounted for.
___________________________
20 In its final report, the committee will also consider whether all sources of acceptable health care spending and quality variations can be controlled for in geographic variations research. Note that unacceptable variation can arise from both overuse ad underuse.
21 The list of market-level predictors can be found in Table 2, note b.
22 This observation should be interpreted with caution. In this analysis, health status risk scores are computed based on diagnoses codes recorded on Medicare claims. Risk adjustment based on Hierarchical Condition Category codes (or other claims-based measures) may be subject to some bias, as regions that have higher spending and greater intensity of practice, are also likely to code more intensively, thus overstating beneficiaries’ severity of illness (Song et al., 2010). As a result, at least some of the reduction in variation attributable to health status using claims-based measures could be an artifact of more aggressive surveillance and diagnosis in higher spending regions. The committee is currently investigating the degree to which this reduction may be overstated.
TABLE 2 90th:10th Percentile Ratios of Input-Price-Adjusted Spending Across Payers, When Adjusted for Selected Predictors
|
|
||
|
Input-Price-Adjusted Spending, |
Medicare |
|
|
Control: |
||
|
|
||
|
Cluster 1: |
1.44 |
|
|
1.23 |
||
|
Cluster 5: |
1.25 |
|
|
1.25 |
||
|
|
||
a In addition to the specified predictors, Cluster 2 also includes an Age-Sex interaction term.
b The analysis utilizes CMS’s (2008) definition of Hierarchical Condition Categories as an indicator of health status (Acumen, LLC., 2013a).
c In addition to the specified predictors, Cluster 8 also includes dummy indicators for Institutional Status, Dual Enrollment Status and Supplemental Medicare Insurance.
d Market-level predictors include the following variables: Hospital Competition, % Uninsured Population, Supply of Medical Services, Malpractice Environmental Risk, Physician Composition, Access to Care, Payer Mix, Medicaid Penetration, Health Professional Mix, Supplemental Medicare Insurance.
NOTE: Underlying data will be released with the final report in Summer 2013.
SOURCE: Committee analysis of Acumen Medicare data.
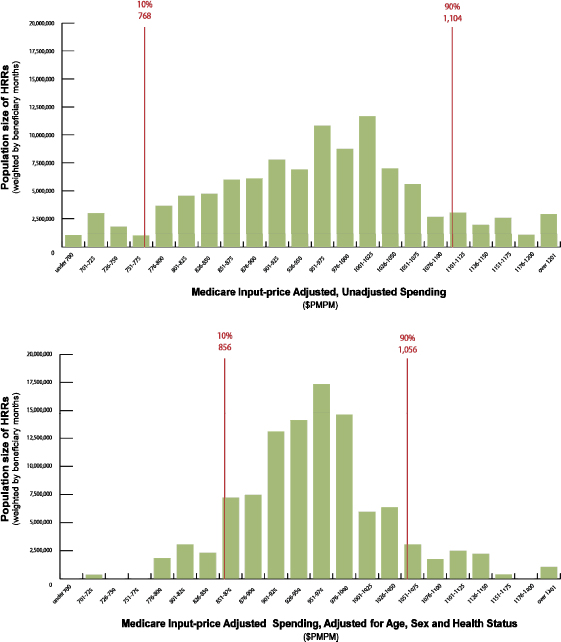
Figure 8 illustrates that, when the effects of age, sex, and health status are controlled for, the spread of 90th:10th percentile of spending narrows. In other words, a greater number of HRRs (weighted by beneficiary-months) falls in the middle range of Medicare spending.
FIGURE 8 Number of beneficiaries in HRRs within 22 categories of monthly per-capita spending, with input-price adjustment alone (top) and with input price adjustment, plus age, sex, and health-status adjustment (bottom).
NOTE: Underlying data will be released with the final report in Summer 2013.
SOURCE: Developed by the Committee and IOM staff based on the data from Acumen Medicare Analysis.
Cluster 8 in Table 2 indicates that market factors add little explanatory power, and a substantial amount of variation remains unexplained after controlling for all predictors measureable within our data and supported by the literature. This analysis cannot confirm whether unexplained
variation is attributable to unacceptable sources of variation (e.g., physician discretion and unmeasured market factors) or acceptable sources of variation (e.g., unmeasured health status).
Observation 5
HRR-level quality is not consistently related to spending or utilization.
A geographic value index could use composite measures of health care quality and service use within a payment region to calculate the numerator and denominator of a single payment adjustment as proxy measures of value (Hahn, 2009).23,24,25 Composite measures aggregate multiple measures of health care service use and quality at an area level. The case for an areawide payment adjuster is stronger if a payment change has consistent, comparable effects on each of the quality measures that together comprise the composite.
The committee’s research did not reveal a consistent positive or negative correlation between condition-specific utilization and condition-specific quality measures in the Medicare population. Table 3 shows correlations between HRR-level quality indexes and an area-wide measure of utilization for each quality measure. Positive correlations (highlighted) indicate those measures for which higher utilization is associated with higher quality of care.26 The strongest positive correlation with utilization exists for disease-modifying antirheumatic drugs (DMARD) for arthritis (0.085); the strongest negative correlation with utilization exists for COPD bronchodilators (–0.48).
___________________________
23Supra., note 3.
24Supra., note 4.
25 The Congressional Research Service interpreted legislative language to refer to MSAs and HRRs.
26 For some quality measures, a lower score indicates better quality. The correlations in Table 3 have been renormalized for interpretability so that a positive correlation always means that higher costs are associated with a higher quality of care. In addition, while Table 3 presents Pearson correlations, the Spearman rank correlations show similar results.
TABLE 3 Pearson Correlations of Condition-Specific Medicare Quality and Condition-Specific Utilization
|
|
|
|
Quality Measure |
Correlation with Utilization |
|
|
|
|
AMI–Beta Blockers |
–0.186 |
|
Arthritis–DMARD |
0.085 |
|
Breast Cancer–Radiation |
0.005 |
|
Breast Cancer–Screening |
0.036 |
|
Cataract–Complications |
–0.061 |
|
CHD–Antiplatelets |
–0.012 |
|
CHF–Admissions |
–0.349 |
|
Cholecystectomy–Laparoscopy Rate |
–0.078 |
|
COPD–Admissions |
–0.324 |
|
COPD–Bronchodilators |
–0.483 |
|
Depression–12 Weeks |
–0.287 |
|
Depression–6 Months |
–0.340 |
|
Diabetes–Amputation |
–0.081 |
|
Diabetes–Hemoglobin |
–0.203 |
|
Diabetes–Retinal Screening |
–0.363 |
|
LBP–Imaging |
–0.401 |
|
Pneumonia–Admissions |
–0.005 |
|
Stroke–Antiplatelets |
–0.061 |
|
|
|
NOTE: AMI = acute myocardial infarction; CHF = congestive heart failure; CHD = coronary heart disease; COPD = chronic obstructive pulmonary disease; DMARD = disease-modifying antirheumatic drug; LBP = lower back pain.
SOURCE: Acumen, LLC, 2013a, p. 131.
These results do not support the hypothesis that increased utilization is associated with higher- or lower-quality outcomes, for three reasons. First, few of the correlations differ substantially from zero. Second, the methodology for risk adjustment of quality measures may not adequately capture differences in health status. Third, mechanical relationships between quality measures and utilization cause correlations to be artificially strong. For example, the outcome for the COPD admissions quality measure is an inpatient admission. As the rate of COPD admissions increases in a region, indicating a lower quality of COPD care, utilization necessarily increases. Thus, this relationship mechanically generates a negative correlation between utilization and the quality of care provided.
In sum, the committee found no evidence of a consistent relationship between disease- or condition-specific measures of utilization and disease- or condition-specific measures of quality. As a result, a geographic value index that used these measures would negatively affect some health outcomes and positively affect others.
These results from the committee’s empirical analysis are consistent with those from a recent systematic review that found an inconsistent relationship between health care quality and cost (Hussey et al., 2013). Of the 61 studies selected for review, 21 (34 percent) found a positive or mostly positive association, 18 (30 percent) found a negative or mostly negative association, and 22 (36 percent) found an inconsistent or no association. Further, the authors concluded that the magnitude of the cost–quality association was generally low or moderate in terms of clinical significance.
It is important to note that this particular observation is limited to area-level, composite measures of value and should not be interpreted as condemning initiatives to improve health care value. Nor does it imply that particular providers in low- or high-cost areas are currently being compensated appropriately. Indeed, value improvement activities are essential to ensure the sustainability of high-quality health care services for Medicare beneficiaries. Such activities require accurate, reliable, and valid measures of provider performance and are integral to ensuring that payment policies create the necessary incentives to improve value (IOM, 2006). However, significant challenges are associated with such value measurement. Given the fragmented structure of the U.S. health care system and limitations of health outcome measurement, condition-specific and process measures are logical choices to guide value-related activities in these early stages.
The committee commends the efforts of public- and private-sector organizations such as the National Quality Forum, the Agency for Healthcare Research and Quality, the National Committee for Quality Assurance, the Joint Commission, the American Medical Association, and CMS to advance the field of health care performance measurement and encourage public dissemination of results. The committee also recognizes efforts to use increasingly sophisticated, multidimensional measures of health care resource use and quality as a basis for payment reforms to promote high-value care. By identifying attainable performance standards and generating mechanisms by which to hold providers accountable for performance levels, these organizations, in partnership with other health care system stakeholders, are paving a path toward better value throughout the Medicare program and the U.S. health care system.
CONTRIBUTORS TO GEOGRAPHIC VARIATION IN MEDICARE SPENDING
Previous studies have documented large differences in health care spending and utilization by geographic area (CBO, 2008a,b; Fisher et al., 2003a,b; GAO, 2009; MedPAC, 2003, 2009, 2011; Wennberg et al., 2002, 2008; Zuckerman et al., 2010). Consistent with this literature, the committee’s commissioned analyses indicate that substantial variation in health care spending, utilization, and quality exists at various geographic levels.27
Starting at the HRR level, with no adjustments for any differences among HRRs, the HRR at the 90th percentile spent 42 percent more per Medicare beneficiary than the HRR in the 10th percentile. Variation was similar at the MSA unit; the MSA at the 90th percentile of unadjusted spending spent 38 percent more per Medicare beneficiary than the MSA at the 10th percentile.28 Removing Medicare per-person spending attributable to input prices—meaning differences in the price of capital, labor, and other overhead costs (such as rent and insurance)—isolates the variation in spending attributable to differences in service use or utilization. When compared with unadjusted spending, input price adjustments slightly increased variation; input-price-adjusted spending in the 90th percentile was 44 percent and 41 percent more per Medicare beneficiary than input-price-adjusted spending in the 10th percentile for HRRs and MSAs, respectively.29
___________________________
27 To keep the presentation manageable, many of the committee’s analyses present the 90th percentile of Medicare spending in Parts A and B compared to the 10th percentile for the aggregated years 2007-2009. This is approximately the ratio of average spending in the highest spending quintile compared to the average spending in the lowest spending quintile of geographic units.
28 Committee analysis of Acumen Medicare data.
29 Note that this result differs from the finding in the Medicare Payment Advisory Commission’s (MedPAC’s) 2011 Report to Congress: Regional Variation in Medicare Service Use, which reported that input price adjustment decreased variation of MSAs in the 90th to 10th percentile from 55 percent to 30 percent. Differences in the time period (MedPAC data are from 2006-2008), the data file used (MedPAC uses the beneficiary level annual summary file [BASF] and inpatient claims), and especially in standardization methods could explain this discrepancy. Acumen used claim-level standardization for all Medicare Part A and B services, while MedPAC used claim-level standardization only for inpatient claims and the BASF for all other claims. In the BASF files, payment adjustments are based on the location of the beneficiary rather than the location of the provider. Acumen adjusted all Parts A and B spending for the input price of the provider’s location. Acumen then aggregated each individual’s total price-adjusted spending and assigned this amount to the location (i.e., HRR) in which the individual resides.
Using measures of variation for the aggregated years 2007-2009, relative Medicare utilization levels by HRR are highly stable over time. This means that high- and low-spending HRRs tend to remain high- or low-spending relative to other HRRs. Furthermore, a sufficient sample size exists in each HRR to conclude that random variation in average HRR-level spending each year is small relative to the mean (ranging from 2 percent for the largest HRR to 4 percent for the smallest HRR30). Because HSAs are smaller than HRRs, they naturally have more variation from year to year as a result of random variation.
Additionally, the committee’s commissioned analyses found that low- and high-cost regions experience similar spending growth rates. Between 1992 and 2010, geographic areas grouped by spending in 1992 experienced similar growth patterns; regions that were high (or low) in cost in 1992 generally remained high (or low) subsequently. Figure 9 classifies HRRs into quintiles based on expenditure levels in 1992, such that the same HRRs are included in each cost quintile throughout the period of analysis. The lines closely follow the same trajectory over time (with the exception of some regression toward the mean for quintile 5, the highest spending quintile in 1992). Utilization growth rates mirror spending patterns presented in Figure 9.
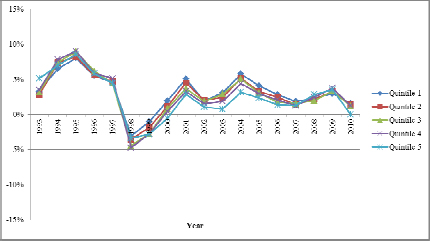
FIGURE 9 Growth rates of spending among quintiles of HRRs based on expenditure levels in 1992.
SOURCE: Acumen, LLC, 2013b, p. 14.
___________________________
30 Committee analysis of Acumen Medicare data.
Observation 6
Geographic variation in total Medicare spending is strongly influenced by the utilization of post-acute care. Most remaining variation is attributable to inpatient care.
Variation in Utilization of Specific Health Care Services
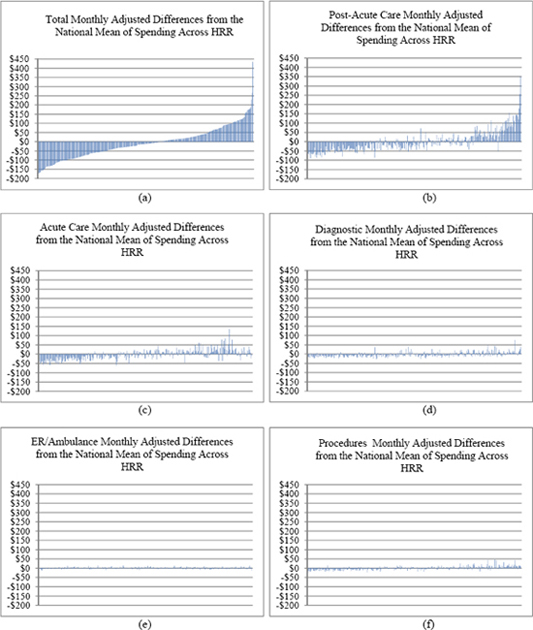
To determine the extent to which variation in particular health care services contributes to total variation in Medicare spending, the committee disaggregated Medicare spending into seven types of services: (1) acute (inpatient) care, (2) post-acute care, (3) prescription drugs, (4) diagnostics, (5) procedures, (6) emergency department visits, and (7) other.31 Based on the subcontractors’ analyses, it appears that utilization of post-acute care services is a key driver of HRR-level variation in Medicare spending, with most of the remaining variation stemming from use of inpatient services. Acute and post-acute service utilization are linked, since post-acute services are covered only after a 3-day inpatient stay, with the exception of some home health services.
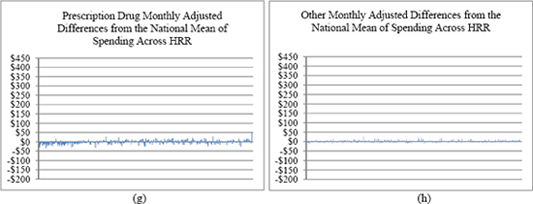
The key role played by post-acute care services can be clearly seen in Figures 10a through 10h, a series of charts in which the horizontal axis represents HRRs ordered from left to right by total, per-member-per-month, input-price-standardized spending (a measure of utilization) between 2007 and 2009 for Medicare Parts A and B. Thus, in each graph, the lowest total use area (Rochester, New York) is the left-most bar, and the highest total use area (Miami, Florida) is the right-most. The vertical axis represents the deviation of input-price-adjusted spending (utilization) in a particular HRR from the national mean utilization for the type of service shown after adjusting for patient demographics and health status (see the note to the figures). In other words, the residuals represent unexplained variation. Figure 10a shows the total Medicare utilization across HRRs that remains unexplained after adjusting for input prices, demographics, and health status, while Figures 10b through 10h display the unexplained variation in utilization in specific service categories only. These residual charts suggest that variation in post-acute care utilization accounts for a large portion of the unexplained variation in total utilization. Areas to the far left in Figure 10a have utilization roughly $50 to $150 below the adjusted national mean, whereas those on the far right have utilization roughly $100 to $200 above the adjusted national mean. Miami is an outlier, which the committee addresses in greater detail below.
Almost all of the remaining variation is accounted for by variation in acute (inpatient) care use (Figure 10c). The remaining services shown (e.g., diagnostic, which includes outpatient physician services, emergency room/ambulance service, and prescription drugs) have much less unexplained variation.
___________________________
31 “Acute care” includes inpatient claims at acute hospitals and Part B claims where the place of service is an inpatient hospital; it excludes claims from psychiatric and rehabilitation facilities. “Post-acute care” includes home health, skilled nursing, hospice care, rehabilitation and long term care hospitals. “Prescription drugs” includes Medicare Parts B and D. “Diagnostics” includes outpatient physician visits and imaging. “Other” includes all claims not included in the first six categories.
FIGURES 10a-10h Medicare service category utilization (monthly cost residual) by HRR.
NOTE: In this analysis, utilization is measured as the input-price-adjusted cost. The predictor variables include beneficiary age, sex, age-sex interaction, health status coded by Hierarchical Condition Category, eligibility for low-income subsidy under Part D, partial-year enrollment, new enrollee indicator (prior-year diagnoses are not available for them), and indicators for year (2007, 2008, 2009).
SOURCE: Acumen, LLC, 2013a, pp. 48-49.
Sources of Variation Within Post-Acute Care
Because of the importance of the topic, the committee commissioned a separate analysis of Medicare post-acute care spending (for years 2007-2009) using CMS’s Chronic Conditions Warehouse database.32 The Lewin Group examined the following subcategories of post-acute care spending: skilled nursing facilities, home health, hospice, long-term care hospital, and inpatient rehabilitation facility. To identify how much each of these post-acute care services contributes to variation in total post-acute care, the investigators compared the unadjusted mean of post-acute care spending with the four subcomponent spending variables if each were set at its national mean for all HRRs. That is, the investigators computed how much the total variation would decrease if there were no variation in each of these post-acute care services, first taken one at a time and then if there were no variation in any of them. Additionally, they assessed how much each of the post-acute care subcomponents would contribute to variation in total, all-cause Medicare spending.
___________________________
32 CMS data are available for public access on the IOM site at http://www.iom.edu/Activities/HealthServices/GeographicVariation/Data-Resources.aspx.
The results, shown in Table 4,33 demonstrate that the variation in total Medicare spending across HRRs is heavily influenced by variation in the utilization of post-acute care services. More precisely, 40 percent (0.40 = 2702.77/6739.66) of all variation in Medicare spending is explained by variation in post-acute care services. Within post-acute care, the home health and skilled nursing facility categories have the strongest influence on the variation in spending. Note that the rows in Table 4 are not cumulative, and represent only the reduction attributable to each subcomponent within post-acute care services taken one at a time. The last row substitutes the national means for each service, and thus represents the reduction in variance due to all post-acute care services. Figure 11 illustrates the values in Table 4, and displays the amount of variation in total Medicare spending that is explained by each subcomponent of post-acute care, where “other” represents all non-post-acute services. The subcontractor’s findings are consistent with the Medicare Payment Advisory Commission’s (MedPAC’s) 2012 report to Congress, which found that home health utilization varies substantially by region and state and that rural and urban counties within a region behave similarly (MedPAC, 2012). For example, rural areas in Minnesota compared with the urban areas of LaCrosse, Wisconsin, averaged 5 and 2 home health episodes per 100 Medicare beneficiaries, respectively, in 2009 (MedPAC, 2012).34 That same year, rural areas in Texas and urban areas of Dallas-Fort Worth, Texas, averaged 41 and 38 home health episodes per 100 beneficiaries, respectively.
___________________________
33 The committee requested new data from CMS (http://www.iom.edu/Activities/HealthServices/GeographicVariation/Data-Resources.aspx) to further explore sources of geographic variation. Table 4 displays the results of the committee’s subsequent analyses. CMS did not apply risk adjustments for post-acute care and hospice spending. The data reflected above are standardized to remove geographic differences in payments due to factors such as local wages, input prices, medical education, and critical access hospitals (CMS, 2012b).
34 Home health services are paid on the basis of a 60-day episode; that is, if a beneficiary receives 5 or more visits in a 60-day period, the home health agency receives a fixed payment for all visits in that 60-day period. If the beneficiary receives 4 or fewer visits, the agency is paid per visit. Eight rural Texas counties averaged more than 100 episodes per beneficiary in 2009.
TABLE 4 Reduction in Variation in Post-Acute Care Spending and Total, All-Service Medicare Spending from Holding Each Component of Post-Acute Care at Its National Mean
|
|
||||
| Post-Acute Care Spending | Total Medicare Spending | |||
| Variance | Reduction in Variance | Variance | Reduction in Variance | |
|
|
||||
| Unadjusted | 388.18 | 6,739.66 | ||
| Substitute HH Means | 167.15 | 221.03 | 5,780.93 | 958.72 |
| Substitute SNF Means | 182.45 | 205.43 | 5,645.24 | 1,094.42 |
| Substitute HOS Means | 307.90 | 80.28 | 6,380.85 | 358.81 |
| Substitute IRF Means | 330.82 | 57.36 | 6,494.76 | 244.89 |
| Substitute LTCH Means | 310.42 | 77.76 | 6,439.75 | 299.91 |
| Substitute All Means | 4,036.89 | 2,702.77 | ||
|
|
||||
NOTE: HH = home health; HOS = hospice; IRF = inpatient rehabilitation facility; LTCH = long-term care hospital; SNF = skilled nursing facility. Each row showing the reduction in variance shows the reduction from eliminating only the variation in that post-acute care service; that is, the rows are not cumulative. The “All Means” row shows the reduction in total variance from eliminating the variance in all post-acute care spending. The sum of the amount of variation explained by individual post-acute care covariance terms (HH + SNF + HOS + IRF + LTCH=2,956.75) would add less than 10 percent to the total variance reduced (2,956.75/2,702.77 = 1.094), or explain 44 percent of the variation in total Medicare spending (2,956.75/6,739.66). For ease of interpretation, this table ignores the variation attributable to the covariance terms.
SOURCE: The Lewin Group, 2013, p. 2.
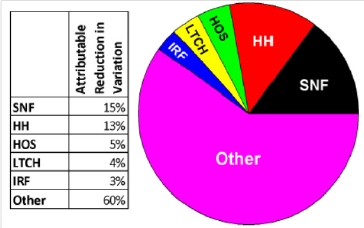
FIGURE 11 Variation in total all-services per capita Medicare spending explained by categories of post-acute care spending and all other spending (2007-2009).
NOTE: HH = home health; HOS = hospice; IRF = inpatient rehabilitation facility; LTCH = long-term care hospital; SNF = skilled nursing facility. For ease of interpretation, the values have been computed setting covariance terms to zero; they account for another approximate 9 percent of total variation. The “Other” category represents variation due to non-post-acute care services.
SOURCE: Developed by the committee based on the Lewin post-acute care analysis in Table 4.
The committee noted certain geographic areas spent considerably more for specific high-margin goods and services (e.g., home health and durable medical equipment [DME]) than other areas. The geographic variation in home health spending may be partially accounted for by the variation in beneficiary and provider adherence to program standards (MedPAC, 2012). The comprehensive coverage criteria allow beneficiaries to receive an unlimited number of home
health episodes once they qualify, and provide no incentives for either beneficiaries or physicians to consider alternative treatments. Some evidence also suggests that providers do not consistently follow Medicare’s standards in designing treatment. Although these differences in practice patterns explain some variation in home health, the literature suggests that large deviations from the national average in spending and utilization among nearby areas may be an indication of fraud (Bernstein et al., 2011; MedPAC, 2009). In fact, the U.S. Office of the Inspector General (OIG) identified certain geographic areas in Florida, Texas, Louisiana, Illinois, New York, and Michigan as high-risk for Medicare fraud (OIG, 2012). For example, Table 5 shows data from MedPAC on home health and DME spending in the four southernmost Florida counties in 2006 and 2008 (MedPAC, 2011). Miami-Dade County is a clear outlier, with per capita spending substantially greater than that of other nearby areas. Additionally, “in 2009, OIG found that Miami-Dade County, Florida, accounted for more home health outlier payments35 in 2008 than the rest of the Nation combined and that 67 percent of HHAs that received outlier payments greater than $1 million were located in Miami-Dade County” (OIG, 2012, p. 9).
As described earlier, not all sources of variation can be measured, and variation in spending attributable to geographic variation in fraud is one such source. Although the amount of annual Medicare spending due to fraud is, by definition, unknown (Goldman, 2012), recent estimates indicate that Medicare and Medicaid paid as much as $98 billion in fraudulent and abusive charges in 2011 (Berwick and Hackbarth, 2012). Because fraud inherently indicates inefficiency (because the care is never delivered to a patient), a geographic payment adjustment based on area-level performance would penalize every geographic area with above-average fraud. Yet, if such counties were penalized for being low-value, all legitimate providers in those counties would bear the consequences.
|
|
||||
| DME Spending per Capita | Home Health Spending per Capita | |||
| Area | 2006 | 2008 | 2006 | 2008 |
|
|
||||
| South Florida County | ||||
| Broward | $394 | $321 | $1,002 | $1,390 |
| Collier | $207 | $202 | $305 | $395 |
| Miami-Dade | $2,043 | $828 | $2,591 | $5,318 |
| Monroe | $237 | $210 | $237 | $334 |
| National | $263 | $282 | $392 | $488 |
|
|
||||
NOTE: DME = durable medical equipment. Spending data are annualized for beneficiaries with either Part A or Part B coverage for at least 1 month during 2006. The results are not adjusted for differences in beneficiaries’ health status or prices.
SOURCE: MedPAC, 2011, p. 11.36
___________________________
35 CMS provides additional payments, known as outlier payments, for home health episodes “with unusually large costs due to patient Home Health care needs” (CMS, 2012a, p. 10).
36 In March 2007, the U.S. Department of Justice, the U.S. Attorney’s Office for the Southern District of Florida, HHS, OIG, and state and local law enforcement launched the Medicare Fraud Strike Force in South Florida. In its early stages, the Task Force targeted fraud in HIV infusion therapy and DME (DOJ, 2013; Katz, 2012), which may explain the significant drop in DME spending observed between 2006 and 2008 in Miami-Dade County.
A geographic value index would adjust payment to all providers within a defined area based on aggregate measures of spending and quality. The committee sought to determine empirically whether providers within a defined area behave similarly (e.g., exhibit similar patterns of service use across sub-regions, clinical conditions, and quality measures). Consistent with a body of literature, analyses commissioned by the committee observed variation in health care spending at every geographic level (HRR, HSA, MSA) studied, and additional research found variation among hospitals within HRRs, among physicians in the same group practice, and even within individual providers when treating different conditions. Further, HRRs do not consistently rank high or low across quality measures, nor is there a consistent relationship between utilization and various quality measures. These preliminary observations suggest that a geographic value index would reward low-value providers in high-value regions and punish high-value providers in low-value regions.
Health policy leaders suggest that, to improve value, payment reforms need to create incentives to encourage behavioral change at the locus of care (provider and patient), and thus payment should target decision-making units, whether they be at the level of individual providers, hospitals, health care systems, or stakeholder collaboratives. Payment reforms contained in the ACA (e.g., value-based purchasing, accountable care organizations, bundled payments) and being tested in the commercial market and Medicaid, do target decision makers rather than geographic areas. Because these reforms are relatively new, there is little evidence to date about their effects on the value of care. Nevertheless, the results of the subcontractors’ work for this study suggest that tying a decision-making unit’s payment to its actions, as these reforms do, is preferable to induce desired changes in care. Further, because post-acute care, particularly home health and skilled nursing, is a major source of unexplained variation in Medicare spending, reforms that address incentives to overuse post-acute care, including fraud in that use, could have a large impact on health care efficiency.
The literature devoted to geographic variation in health care utilization, spending, and quality suffers from a number of methodological and statistical limitations. The committee’s work shares certain of these limitations and challenges. The Medicare data the committee examined for this study exclude the Medicare Advantage population, which in 2012 made up 27 percent of all Medicare beneficiaries (Gold et al., 2011). The existing literature suggests that service utilization and baseline health status differ between Medicare Advantage and fee-for-service populations, although these differences appear to have narrowed considerably in the past 10 years (Newhouse, 2012). Further, most analyses exclude Part D spending, which is correlated only weakly with spending in Parts A and B (r = 0.10) (Zhang, et al., 2010a). As well, analyses of claims data inevitably are not current, although the persistence of spending across HRRs suggests more that current results would likely be similar.
Furthermore, many independent or predictor variables of potential importance to understanding geographic variation in health care utilization, spending, and quality may not be measured with accuracy in claims data. The challenges of measuring health status have been detailed earlier. Additionally, reliance on administrative billing data for quality measurement may be misleading. In comparing the clinical accuracy of claims data and those derived from clinicians for
measurement of quality, significant differences have been identified (Tang et al., 2007). And although the literature suggests that different sources of data vary with respect to their estimation of quality, it is demonstrated that absent true clinical data, delineating patients falling within clinical conditions with claims data is difficult (Keating et al., 2003). As well, claims-based quality measures tend to inflate performance (Tang et al., 2007). With respect to the committee’s commissioned work, specifically, valid and reliable indictors of health care quality for many conditions are not available within Medicare data; hence, those conditions could not be investigated in the analyses for this study.
Finally, several variables demonstrated to affect variation, including patient care preferences, provider discretion, and patient–provider interactions, are not specified in the models estimated here (Eisenberg, 2002; Nicholas et al., 2011). Interpretation of the committee’s results is limited by its inability to control for such factors in understanding interrelationships between variables in its models and the phenomenon of geographic variation.