KEY SPEAKER THEMES
Bisognano
- Realizing the Triple Aim—better care, better health, lower costs—requires involving organizations and individuals outside the health care system.
- To move forward on the Triple Aim, an integrator plays a key role in bringing together the various improvement efforts along each dimension of quality, health, and cost.
- There is a critical need for measurements that enable learning as a means of improving health and health care.
Isham
- Health care is a complex adaptive system, and the way to optimize such a system is to create a general vision that provides enough space for natural creativity to emerge.
- Setting specific targets could stimulate innovation and trigger efforts to identify what is and what is not working to optimize health and health care.
- Families of measures are useful for assessing the same concept at multiple levels of aggregation in the health system.
Before turning to the substantial task of developing a set of core metrics for assessing health outcomes, care quality, and costs, it is necessary to have a clear understanding of why the three-part aim is critical to transforming the nation’s health care system. Maureen Bisognano, president and chief executive officer of the Institute for Healthcare Improvement (IHI), focused her presentation on some of the lessons that have been learned from several initial efforts at creating health care systems based around the three-part aim. George Isham, senior advisor at HealthPartners and senior fellow at the HealthPartners Research Foundation, discussed the need to consider the overall structure of the health system, and not just its subsystems, when designing metrics for measuring improvements in the system.
VISION AND THE IMPORTANCE OF MEASURING PROGRESS ON CARE, POPULATION HEALTH, AND COSTS
To start her presentation, Maureen Bisognano reviewed the history of the Triple Aim, which was first formulated in 2006 when a group of people at IHI first began to think about whether the goal of the health care system should be health care or health. She explained that its genesis lay in a series of discussions her colleagues were having with leaders of a variety of health care systems around the country. These conversations highlighted the incredible diversity of thought about the importance of different goals and aims for health care improvement. Moreover, very few people within the health care system were, in fact, talking about health. After reviewing data from the Commonwealth Fund Scorecard, the Dartmouth Atlas, and other research studies, the IHI devised the Triple Aim to focus efforts to improve the health care system (see Figure 2-1). The Triple Aim takes a comprehensive view of improvement—improve the health of populations, improve the individual experience of care, and reduce the per capita costs of care for populations—in order to identify all of the factors that influence health and health care (Berwick et al., 2008). Soon after the Triple Aim’s creation, 15 organizations joined with IHI to develop a learning community that would test the impact of these aims and whether their implementation could lead to a more efficient and effective health care system.
Bisognano outlined three important lessons from this early effort. The first was how critical it is to have someone or some organization serve as an integrator that will keep activities focused on addressing all components of the Triple Aim. Second, it is important to identify a population on which to focus concrete efforts. The third lesson, the most complicated, is that no single intervention will provide sustainable progress toward all three aims. Because of this, initiatives must implement a portfolio of projects that consider the multiple drivers that can affect different aspects of the Triple Aim.
As an early example of the type of success that can come from focusing
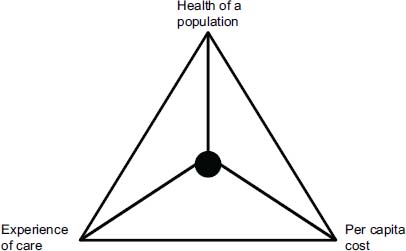
FIGURE 2-1 The IHI Triple Aim.
SOURCE: Institute for Healthcare Improvement.
on the Triple Aim, Bisognano described QuadMed, a health care system developed by Wisconsin-based Quad/Graphics. Quad/Graphics, a large industrial printing company, was considering strategies for improving health care for its employees while reducing company costs. Quad/Graphics joined the Triple Aim effort and created a model based on the patient-centered medical home. The model the company created, QuadMed, employs its own internists, pediatricians, family practitioners, and some specialists; manages its own laboratories, pharmacies, and rehabilitation centers; and contracts with specialists and hospitals for other services. To focus attention on quality instead of volume, physician pay is based on satisfaction and clinical outcomes, and relevant metrics are enabled by a data system that tracks the system’s entire patient population. From its inception, QuadMed achieved improved clinical outcomes and rapid cost reductions—today, costs are 32 percent less than the Midwest average—and its focus on evidence-based medicine has led to gains in overall outcomes that outpace national benchmarks for conditions such as acute lower back pain, diabetes, hypertension, and hyperlipidemia. QuadMed has been so successful that other companies outside the printing industry and beyond the borders of Wisconsin are now hiring it to provide health care for their employees. This example, Bisognano said, shows that building a model around the Triple Aim, one that uses measurement for comparison and learning and that has strong governance, can produce a system that both improves health and reduces per capita costs.
Bisognano noted the tension between using measurement to enable learning and improvement versus using measurement to drive incentives and payment. She noted that when measurement is heavily linked to incentives, organizations and individuals may limit their focus to local actions that affect specific measures as opposed to building coalitions and collaborations that address the broader Triple Aim. As a result, care systems are being designed that are quite different than that of Quad/Graphics, which has redesigned its care processes, benefits, and care availability to focus on comprehensive primary care, prevention and wellness, the patient experience, and the value of the entire care experience.
In the early models of the Triple Aim, the focus was on working within the confines of the current health care system. However, IHI and its partners soon concluded that the Triple Aim could not be realized if they confined their work to traditional health care organizations such as hospitals, primary care centers, and safety net centers. “We needed to go outside the walls of the hospital if we’re going to actually move the Triple Aim,” Bisognano said. She noted the need for a broader coalition to make progress across the Triple Aim, and the need for collaboration to influence the wide range of factors that influence the aims. As an example, she described how IHI’s partners started working in Memphis and neighboring Shelby County, Tennessee, where they engaged health care leaders, the chief executive officers of the local hospitals, the commissioner of public health, school nurses, and the like, but the metrics were not improving. After expanding their vision of who should be included in the effort, the team began involving the extensive network of churches and local community leaders in the area. Bisognano recounted the comment that one minister made at one of the project’s meetings in the context of addressing diabetes. He remarked that while a physician might see a patient twice per year for 15 minutes, he saw the same person twice a week for two hours. Making the connection with the local churches and community leaders, Bisognano said, changed the entire dynamic of the reform efforts.
Thinking about these success stories opens the door to an entirely new way of defining health care. This new view highlights the importance of governance and its role in engaging different groups of people in a different set of activities and with a specific population and intervention in mind. In the case of Memphis and Shelby County, IHI and its partners started small by activating a virtual faith-based network and focused on two goals: reducing untreated and unmanaged hypertension among low-income African American men and reducing the risk and incidence of uncontrolled chronic disease for vulnerable women. The Memphis Congregational Health Network, formed by integrating three existing church networks, influenced
entire congregations to adopt health and healing as part of their mission and provided reliable sources of information as well as training to trusted lay members on how to convey that information and advocate for health. For the initiative focused on female health, the effort began with 30 existing members of the Congregational Health Network in the first year, with plans to scale to 2,000 designated health volunteers from 300 churches over 3 years, with the goal of reaching more than 8,000 women across the community. For the male health initiative, onsite screening for hypertension and other health risks will be carried out at approximately 400 congregations over the first 2 years; this is expected to reach almost 2,700 individuals with previously undiagnosed or untreated hypertension who can be brought into community-based treatment.
Bisognano explained that value is achieved by optimizing all three aspects of the Triple Aim. There are two issues facing such an optimization: Different stakeholders may weigh the three dimensions differently, and it is necessary to understand the population of individuals being considered in this value measurement. She also noted that two important measures—efficiency and effectiveness—can be calculated by combining individual components of the Triple Aim. Efficiency, she said, is measured by combining the per capita costs and care experience aspects, as this would describe the level of resources required to achieve a given quality of care. Effectiveness can be derived from the combination of the population health and care experience dimensions, as this shows how health care delivery affected health outcomes for a local population. Combining all of these metrics together enables the measurement of cost-effectiveness and overall value (Stiefel and Nolan, 2012).
Bisognano ended her comments by stressing how important it is to not overemphasize the population at the expense of the individual. Doing so risks missing opportunities to understand the consequences of various health issues and policies for individuals. She also emphasized that designing metrics for a population using a variety of different perspectives is a complicated task. She noted that simplicity and comparability will be key for national learning about metrics and that it will be critical to develop actionable metrics as a means of driving the momentum of transformation.
In response to a question about the role of the integrator, Bisognano explained that the integrator is often a group of individuals from various organizations who work together. To be effective, such a group requires strong governance and an individual to lead its efforts. It also needs to be independent so that it can address broad-based needs and coordinate work on all three aims.
SYSTEMS FOR BETTER HEALTH, BETTER CARE, AND LOWER COSTS
George Isham began his presentation by providing a conceptual framework for the nation’s health system and proposing that the health system be considered as a complex adaptive system (IOM, 2001; Plsek and Greenhalgh, 2001). In a complex adaptive system, the system, along with the individuals and organizations within it, evolves over time, often in unpredictable ways. Furthermore, the system consists of interconnected organizations and individuals, and their actions affect the context for others. Because of the complexity and fragmentation of the system, it cannot be controlled with a single overarching approach. Rather, a better approach for managing a complex adaptive system such as the health system is to specify a small number of simple rules with minimum specifications, which will allow organizations and individuals to develop and adapt solutions suited for their specific circumstances and needs. In this spirit, Isham presented five simple rules that could provide a starting point for the discussion of core metrics (Kottke et al., 2012):
- Stakeholders should agree on a set of mutually measurable goals for the system. In the case of health care, the three-part aim sets suitable goals and the National Quality Strategy provides sub-goals, but further work is needed (AHRQ, 2011).
- The extent to which the goals are being achieved will be reported to the public. Concerning data reporting, Isham said that there is a wealth of data available, but better systems are needed to convey these data in an understandable and impactful manner to the public.
- Resources will be available to achieve the goals.
- Stakeholder incentives, imperatives, and penalties will be aligned with these goals.
- Leaders of all stakeholders will endorse, promote, and honor the goals.
Turning to the opportunities to improve health, health care, and cost, Isham cited the case of France, where life expectancy is three years longer than in the United States, and yet the cost per capita is about $4,000 less, according to the latest data from the Organisation for Economic Co-operation and Development (OECD) (see Figure 2-2). After reviewing some specific data on imaging tests and chronic disease, he said that these data lead to two conclusions. First, the incentives for clinicians and health care organizations may not align with the goals of the overall health care system. For example, the primary incentive structure is the fee-for-service
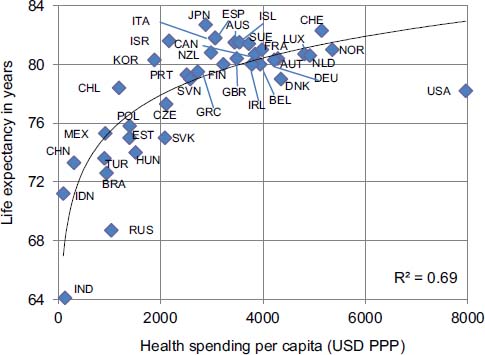
FIGURE 2-2 Life expectancy at birth and health spending per capita, 2009.
SOURCE: OECD, 2011.
payment system, which encourages greater use of health care services and therefore higher costs, yet this is in conflict with the national interest in a sustainable spending level for health care. Second, the nation needs to set specific targets to meet in terms of improving health, health care, and costs. Isham cited the recommendation made in 2012 by an IOM committee that the Secretary of the Department of Health and Human Services (HHS) should set national goals on life expectancy and per capita health expenditures for 2030 that would bring the United States to average levels comparable to other wealthy nations (IOM, 2012). Setting specific targets for cost, Isham said, would stimulate innovation, particularly in the policy arena, that could improve the nation’s competitiveness, something that he believes will not happen with incremental thinking. Creating a national challenge for improving life expectancy would trigger efforts to identify on a state-by-state and locality-by-locality basis what is not working in terms of optimizing health and health care.
Isham then discussed an idea that David Kindig, emeritus vice chancellor for health sciences at the University of Wisconsin School of Medicine and Public Health, has put forward about how the components of the three-part aim measure the broader determinants of health. Kindig pointed out that population health is a function not only of health care, but also of health behaviors, social and economic factors, the physical environment, and other influences (Kindig, 2011). These factors outside the health care
system are often not specifically assessed in most assessment frameworks. Isham said that today, with the current emphasis on accountable care organizations (ACOs), most care delivery systems are starting to think about ways of working with populations of patients, but that concept does not go far enough to improve total population health. It is time, then, to begin thinking about how to integrate the health of all of the subpopulations in a way that improves the health of the total population. It is also timely to consider the appropriate metrics to use at different levels of the system and how they can be integrated into a national perspective. Isham described the conceptual framework that he and his collaborators at HealthPartners developed to identify those drivers that were within the realm of their capabilities and those that would benefit from partnerships with public health and community-based organizations (see Figure 2-3). The drivers could serve as focal points for developing metrics.
Turning this conceptual approach into action requires identifying all of the stakeholders that need to be involved and providing leadership and communication among efforts to improve each sub-domain (Jacobson and Teutsch, 2012). Then resources can be identified and allocated to address the primary drivers of each health determinant in a coordinated manner that meets the three-part aim. To identify and allocate new resources, Isham said that it will be necessary to get a better return on investment from
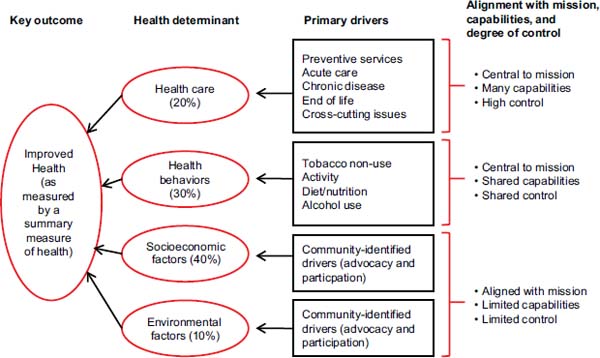
FIGURE 2-3 Conceptual framework depicting measurement domains of a “system within a system” approach and the drivers of health determinants.
SOURCE: Isham, 2012.
policies and programs both inside and outside health care and to capture funding by reducing ineffective health care spending. It will be necessary, too, to strengthen government funding for population health improvement at all levels with an increased focus on philanthropy that also engages corporate business leaders.
In his final remarks, Isham addressed the issue of metrics. It will be essential, he said, to identify the right kinds of measures that work in a multilevel approach that goes from the individual to the organizational level and then up to the regional, state, and federal levels. In this regard, a concept developed by the National Quality Forum could prove useful when it comes to developing families of measures and core measures. This concept defines families of measures as “related available measures and measure gaps that span programs, care settings, levels of analysis, and populations” (MAP, 2012, p. 28). Families of measures have been identified for concepts such as safety, care coordination, and prevention and treatment of cardiovascular conditions and diabetes (MAP, 2012). A core measure set could then identify families of measures for particular concepts, with measures tailored to specific programs, care settings, levels of analysis, and populations.
Isham also noted that his colleagues at HealthPartners have been developing a standard open-architecture measure of total cost of care that could provide a standard metric for the affordability component of the three-part aim. While plans and government programs have a general ability to assess costs, a standardized approach would help increase transparency for the public. This total-cost-of-care metric could be analyzed to understand the impact of different drivers of total resource use, such as price, at every level. HealthPartners has used this metric with its clinics to measure progress toward the three-part aim. In one example of assessing progress along each dimension, the organization found it was able to reduce the total cost of care relative to its market while improving the overall experience of care and boosting overall health, as measured by the percentage of patients with optimal control of diabetes. Isham said that the diabetes measure is simply an initial surrogate measure for overall health and that HealthPartners is attempting to replace it with more advanced measures.
In summary, Isham said that the health system, as well as the clinical care and public health subsystems, are complex adaptive systems. Understanding and redesigning simple rules for this system and its subsystems may offer the opportunity for enhancing population and individual three-part aim outcomes. Creating clear and commonly understood definitions of the three-part aim, and its related concepts, is important to facilitating progress. Further, explicit numerical goals should be set for each aspect of the three-part aim and at each level of the health system in order to both gauge progress and encourage innovation.
Engaging each state and community across the country, as well as key
stakeholders at each level, needs to be part of a national strategy to meet the three-part aim, Isham said. He emphasized that this effort cannot be just about numbers and regulations. For the system and subsystems, it is essential to describe the current status and explain why improving the current system is important to many different stakeholders and the nation as a whole. He said that families of measures for priorities and conditions and core measure sets for actors could help reduce the complexity of measurement and improve its applicability at multiple levels. Finally, he emphasized how critical transparency is for making progress and for raising awareness about current gaps throughout the system.
During the discussion period that followed the two presentations, Cathy Schoen, senior vice president for research and evaluation at the Commonwealth Fund, suggested that a suitable cost metric might be cost relative to growth of the economy, whether that be at the local, state, or federal level. Then, one goal could be to get the same or better health outcomes out of the health care system for the same or lesser share of the local, state, or national economy. Improvements in this relative cost metric would free up resources to deal with larger population issues that are outside the control of the health care system. Isham agreed that this would be an appropriate metric to help set national targets and enable the scale of re-engineering that is needed to improve the nation’s competitiveness.
As an example of how this could work, Leslie Mikkelsen, managing director of the Prevention Institute, cited the Accountable Care Community of Akron, Ohio, which brings together seven health care partners and 70 community organizations with the Austen BioInnovation Institute playing the role of integrator. She said that this group’s efforts have focused on reducing the cost of diabetes care and that the group uses some of the savings to fund activities that go beyond those that typically fall under the purview of the health care system. She said that she was looking forward to the development of metrics that encourage this kind of bridging and that can change community environments to support better health outcomes.
Eugene Nelson, professor at the Dartmouth Institute for Health Policy and Clinical Practice, remarked that one important unanswered question is how to have a governance structure and payment system align for health and health care so that they work in a given community. In other words, he said, there is a need to develop approaches to link payment systems to governance for health and health care in a given region. Bisognano commented that this requires a visionary and selfless leader to step in and coordinate the three-part aim, particularly since the incentives in use today
place such a heavy emphasis on optimizing everything in terms of cost for a given organization, rather than for the nation as a whole. Randall Cebul, director of the Center for Health Care Research and Policy at Case Western Reserve University, said that community leaders can often serve as selfless, proactive three-part aim-oriented leaders.
Addressing the issue of population heterogeneity, Bruce Ferguson, Jr., inaugural chairman of the Department of Cardiovascular Sciences at East Carolina University, asked if there was some theoretical level of heterogeneity in a population beyond which it becomes difficult to integrate data into one metric. In particular, he cited his own personal experience as a cardiac surgeon in which he observed that patients who are referred to his clinic from the southeastern United States have double the mortality of local patients whom he treats using the same level of care. Bisognano replied that she is increasingly optimistic that it is possible to design models to accommodate diverse populations such as this.
AHRQ (Agency for Healthcare Research and Quality). 2011. Report to Congress: National Strategy for Quality Improvement in Public Health. Washington, DC: Department of Health and Human Services.
Berwick, D. M., T. W. Nolan, and J. Whittington. 2008. The triple aim: Care, health, and cost. Health Affairs 27(3):759–769.
IOM (Institute of Medicine). 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press.
———. 2012. For the Public’s Health: Investing in a Healthier Future. Washington, DC: The National Academies Press.
Isham, G. J. 2012. HealthPartners’ Approach to Assessing Opportunities to Improve Community Health: A Perspective of a Consumer Governed, Not-for-Profit Healthcare Financing and Delivery System. http://uwphi.pophealth.wisc.edu/about/staff/kindig-david/Isham-HealthPartners%20model.pdf#search=” health partners is ham consumer governed” (accessed April 10, 2013).
Jacobson, D. M., and S. Teutsch. 2012. An Environmental Scan of Integrated Approaches for Defining and Measuring Total Population Health by the Clinical Care System, the Government Public Health System and Stakeholder Organizations. Commissioned Working Paper, National Quality Forum.
Kindig, D. A. 2011. Unpacking the Triple Aim Model. http://www.improvingpopulationhealth.org/blog/2011/01/unpacking_triple_aim.html (accessed February 26, 2013).
Kottke, T. E., N. P. Pronk, and G. J. Isham. 2012. The simple health system rules that create value. Preventing Chronic Disease 9:110179.
MAP (Measure Applications Partnership). 2012. MAP Families of Measures: Safety, Care Coordination, Cardiovascular Conditions, Diabetes. Washington, DC: National Quality Forum.
OECD (Organisation for Economic Co-operation and Development). 2011. Health at a Glance 2011: OECD Indicators. Paris, France: OECD Publishing. http://dx.doi.org/10.1787/health_glance-2011-en (accessed February 26, 2013).
Plsek, P. E., and T. Greenhalgh. 2001. Complexity science: The challenge of complexity in health care. BMJ 323:625–628.
Stiefel, M., and K. Nolan. 2012. A Guide to Measuring the Triple Aim: Population Health, Experience of Care, and Per Capita Cost. IHI Innovation Series White Paper. Cambridge, Massachusetts: Institute for Healthcare Improvement.












