Few dispute obesity is a significant and growing public health issue, but no one has identified a single or simple solution. The overweight and obesity1 epidemic cannot await the completion of all the rigorous research studies that would lend greater certainty to the efficacy of interventions and their applicability to varied populations. Instead, some carefully selected interventions can and must proceed on a trial-and-error basis to build a responsible response to the epidemic in an evidence-informed and theory-inspired manner. Evaluation builds on the body of science aimed at better understanding the complex biology of obesity, and on efficacy-tested interventions to combat the epidemic. Evaluation also recognizes that even the best scientific evidence of efficacy does not guarantee that an intervention will be effective when applied in specific populations and within community contexts.
Evaluation offers evidence on the need for, and the quality and effectiveness of, a range of interventions aimed at preventing obesity (interventions include policies, programs, services, and environmental changes). It can offer (1) assessment of the distribution of the problem and need for intervention; (2) monitoring of interventions, a source of quality assurance on how well those responsible for implementing programs or enforcing policies are performing their functions; (3) through surveillance, a long-term assurance that the implementation of interventions is achieving intended outcomes or impact; and (4) summative evaluation providing judgment of a program’s or policy’s merit and worth. Evaluation is central and essential to a “learning organization,” to responsible legislators in amending or changing policies, to advocates in making their case, and to administrators in their stewardship of resources and programs.
PURPOSE OF THE REPORT
The purpose of this report, developed by the Institute of Medicine’s (IOM’s) Committee on Evaluating Progress of Obesity Prevention efforts, is to develop a concise and actionable plan for measuring progress in obesity prevention efforts for the nation and adaptable guidelines for community assessments and evaluation. The Committee was tasked to
_____________
1Overweight and obesity are defined in Appendix B.
1. draw on the recommendations and recommended indicators of progress from the preceding IOM Committee and report Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation (APOP); consider currently used and new tools and metrics (e.g., trend analysis, community/local measures) to measure progress; and develop a plan for a national-level evaluation of obesity prevention efforts by sector and, if appropriate, across sectors;
2. develop a community-level evaluation plan that adds detail and support to the national-level evaluation plan; and
3. identify measurement ideas that can determine the specific impact of the Home Box Office (HBO)/IOM campaign The Weight of the Nation (TWOTN).
The audience for the report includes decision makers, community members, researchers, and evaluators at all levels and across all sectors. The report’s recommendations are not expected to be implemented or even relevant to every level of evaluation from community and organizational to national, but report users can build on available monitoring and surveillance data and evaluations to aggregate up to community and even state and national evaluations of specific components of obesity control efforts, and they draw on the Committee’s recommended resources to strengthen their capacity for evaluation.
This chapter sets the stage by articulating the Committee’s vision for evaluating progress of obesity prevention efforts at national, state, and community levels, and introducing a framework for evaluation. The chapter then describes how the Committee approached its task by (1) providing an overview of the needs of important users of evaluation, (2) describing the scope and use of existing objectives and strategies (as defined by its task), and (3) reviewing the current context of surveillance and summative evaluation. This chapter offers a brief introduction and background to the Committee’s task and how it will be particularly relevant and useful to evaluation users, helping to establish an infrastructure for monitoring progress of obesity prevention efforts at national, state, and community levels.
Much of this report’s guidance for evaluation plans may seem like generic methodological convention to the research-minded reader, so it is helpful to describe some ways in which the evaluation of progress in obesity prevention is similar to, and different from, evaluation of other prevention efforts. The fields of evaluation, policy analysis, surveillance, and community health assessment are hardly new, and this background knowledge contributed greatly to the Committee’s ability to anticipate issues, relate them to other prevention experience, and where necessary, differentiate the evaluation of obesity prevention from that experience.
EVALUATING OBESITY PREVENTION COMPARED TO OTHER PREVENTION EFFORTS
The prevention field generally, and obesity prevention in particular, need to engage in surveillance of diseases and related conditions and assess the relative importance and trends in prevalence of factors associated with diseases and related conditions (see Chapters 3 through 8). In evaluating interventions, prevention efforts need to focus not only on implementation and outcomes but also on the reach of interventions—their ability to influence large numbers of people to achieve population-level benefits (Gaglio and Glasgow, 2012; Glasgow et al., 1999; Green and Glasgow, 2006). The ecological model of prevention identifies many potential influences on health, and evaluation permits prevention practitioners to select the most powerful levers for change among the multiple ecological levels. National monitoring of preven-
tion efforts needs to include some key indicators of these powerful levers at various levels of the ecological model, including the whole-systems level. Prevention of obesity offers a case in point, as noted in the very first IOM report on the subject (IOM, 2004). There is a growing realization for obesity prevention, as in the case of controlling tobacco and other drugs (Eriksen, 2004; Mercer et al., 2010), that policy and environmental approaches offer powerful levers for change. As discovered in these other areas, however, it is difficult to use the most rigorous experimental designs in evaluating policy and environmental approaches. Evaluation of obesity prevention is on track to develop and adapt quasi-experimental methods with enough rigor to reduce uncertainty about what works.
However, given the stage of development of obesity prevention and the wide range of potential levers for change, evaluation faces some challenges that distinguish it from other prevention efforts. At the time of this Committee’s deliberations, it was still uncertain which factors can provide the most powerful levers, and the range of potential levers related to nutrition and physical activity is much greater than one would find even in complex situations such as HIV prevention or tobacco control. The range of factors is problematic at the national level, but it is especially challenging at the community level. Complex situations require a much better understanding of the community context of obesity prevention. Although community context is essential to understand in other prevention efforts, it is even more important for obesity prevention efforts because the risk factors related to eating and activity affect everyone. This fact induces considerably more variation in community evaluations than in these other areas. It is imperative that obesity prevention narrow the range of possibilities. Two strategies to do so are outlined in Chapter 8: a strategy that screens and assesses the “evaluability” of many possible approaches before evaluating them and a strategy that investigates the “dose” of the intervention: intensity, duration, and reach into the target population.
CURRENT CONTEXT FOR EVALUATING OBESITY EFFORTS
As described in the prior section, much remains to be known about the determinants of obesity and the efficacy of interventions to reduce its incidence, prevalence, and consequences. The epidemic of overweight and obesity, however, demands action in the relative absence of (1) completed and compiled basic science on causal mechanisms and (2) controlled trials of interventions in representative populations. Many of the program and policy interventions needed to confront the epidemic successfully on a population scale will not lend themselves to the full battery of experimental controls. Randomized controlled trials are ideal, but the ideal is not always possible nor may it answer questions being asked by decision makers interested in obesity prevention (Casazza and Allison, 2012; IOM, 2010a; Majumdar and Soumerai, 2009; Mercer et al., 2007; Rosen et al., 2006). The alternative is to take advantage of the innovative “natural experiments” that are being conducted nationally and locally. For example, New York City’s requirement of menu labeling in restaurants was a natural experiment, insofar as there was limited evidence that menu labeling would reduce calorie consumption. Yet this intervention offered an opportunity to test whether the requirement would have that effect. The evidence has since been mixed (Morrison et al., 2011), but the example illustrates the opportunity to test innovative interventions through summative evaluation of field trials. State and district policies on competitive foods and beverages in schools (foods that “compete” with the school breakfast and lunch) have contributed to changing the school food environment in which the policies are implemented and will soon lead to uniform federal standards. Evaluations of the natural experiments of mass media campaigns, state and community policy initiatives,
and programs in communities and organizations become sources of evidence for national and state initiatives and models to be emulated in other communities and organizations if and when these natural experiments are evaluated with sufficient attention to a common framework and the comparable indicators suggested in this report.
The APOP report (IOM, 2012a) makes using “natural experiments” as the main source of evaluation all the more compelling. The APOP report, to which this report is sequenced, framed obesity prevention by targeting policies, systems, and environments, rather than emphasizing changes in individual behavior, as many previous recommendations and published evaluations had done. Actions through such policies, systems, and environments are under way across the country in multiple forms, and surveillance systems exist to compare their effects over time and between jurisdictions. Much of what this report recommends, then, is a more systematic application of these natural experiments to bring their results to scale and to the aid of states, communities, and organizations.
This report is about how all societal sectors and levels can increase the likelihood that adopted obesity prevention interventions will be (1) matched to the assessed needs of populations, (2) monitored for their progress in adopting, implementing, and maintaining tested interventions, (3) evaluated in light of program/policy objectives, and (4) widely disseminated. The use of existing surveillance systems to maximize comparability of results across interventions, populations, and jurisdictions has provided much of the inspiration and role modeling of promising practices from one setting to another, and it can continue to expand the reach of such interventions with the addition of recommended indicators of need and effectiveness.
“Promising practices” have taken on new meaning in obesity control as the relative paucity and dubious representativeness, time intensiveness, or applicability of rigorously tested practices have forced national organizations and communities to innovate and apply ideas from public health successes and community projects (Brennan et al., 2011). The evaluation results of those public health successes (e.g., the National High Blood Pressure Education Program, the National Cholesterol Education Program, and tobacco control) and community projects, however, might not be applicable to the varied obesogenic circumstances of communities of varied ethnicity, resources, and socioeconomic conditions (Green and Glasgow, 2006). Evaluation of promising interventions, then, becomes more important for each community to test the intervention’s applicability there, and then cumulatively important for its broader applicability or adaptability across a wider variety of communities.
A NOTE ON TERMINOLOGY
In the literature, terms such as assessment, surveillance, monitoring, and evaluation are often used interchangeably or with meanings that vary among professions, disciplines, and settings. In this report the Committee uses these terms as described in Box 1-1, which may mean that the Committee’s usage in this report will sometimes not match the usage elsewhere. In this report, the Committee uses the term evaluation to refer to combinations or culmination of all four of these functions from needs to processes to outcomes. The Committee uses the term summative evaluation, as in the evaluation literature where a distinction is needed, to refer to the addition of experimental or quasi-experimental design features that provide greater certainty that the outcomes or impact can be attributed to the interventions. All of these forms of evaluation can apply to any combination of programs or components of programs, systems,
BOX 1-1
A Note on Terminology
• Assessment is an effort to use data on the community or other jurisdiction to characterize the problem, its distribution, and efforts to address it.
• Monitoring is the tracking of the implementation of interventions* compared to standards of performance.
• Surveillance is the ongoing systematic collection, analysis, and interpretation of data tracked over time to detect patterns, disparities, and changes that may be associated with interventions or other causes.
• Summative Evaluation is the effort to detect changes in output, outcomes, and impacts associated with interventions and to attribute those changes to the interventions.
• Evaluation refers to all four or various combinations of these functions (assessment, monitoring, surveillance, and summative evaluation).
______________
* In this report, interventions refer to programs, systems, policies, environmental changes, services, products, or any combination of these multifaceted initiatives.
policies, environmental changes, services, and products. The Committee will refer to these objects of evaluation collectively and in their various combinations as interventions.
VISION
Several IOM committees have given prominence in their reports to the importance and challenges of evaluating and measuring the progress of obesity prevention in terms of (1) assessment and monitoring of progress in implementing efforts and actions (interventions) to prevent obesity and (2) surveillance of changes and summative evaluation of progress in obesity control as a result of those interventions. For example, the 2004 IOM report Preventing Childhood Obesity: Health in the Balance grappled with the use of body mass index as the most common measure of overweight and obesity and evaluation of outcomes in obesity prevention efforts (IOM, 2004). It also addressed the growing expectation for community engagement in participatory studies, funding issues, and various design issues. In 2007, IOM released Progress in Preventing Childhood Obesity: How Do We Measure Up? That report concluded “evaluation serves to foster collective learning, accountability, responsibility, and cost-effectiveness to guide improvements in … obesity prevention policies and programs,” and it identified surveillance, monitoring, and research as fundamental components of these evaluation efforts (IOM, 2007, p. 8). The Committee refers the reader to previous reports, especially those on the linkage of research and summative evalua-
tion (IOM, 1997), issues of cost, cost-effectiveness, and cost-benefit in community evaluation, and the weighing of trade-offs between benefits and harms of interventions (IOM, 2012b). The 2010 IOM report Bridging the Evidence Gap in Obesity Prevention: A Framework to Inform Decision Making addressed the need for development and integration of various sources of evidence and offered a framework for locating, assessing, and applying evidence to guide decision making (IOM, 2010a). This report builds on these other reports to offer an evaluation framework depicting resources, inputs, strategies, actions, and a range of outcomes important to prevention, all amenable to documentation, measurement, and evaluation (see Figure 1-1). As did previous committees, this Committee stresses the necessity of engaging multiple sectors and stakeholders in evaluations to assess and stimulate progress in obesity prevention over the short, intermediate, and long terms.
To provide a vision of how and where this report should begin and where it should lead, the Committee developed a graphic representation, or framework, of the scope of inputs or people, resources, activities, outputs, outcomes, and, ultimately, impacts, that would need to be encompassed by the cumulative evaluation efforts, if not the individual strategies and methods of each project applying the recom-
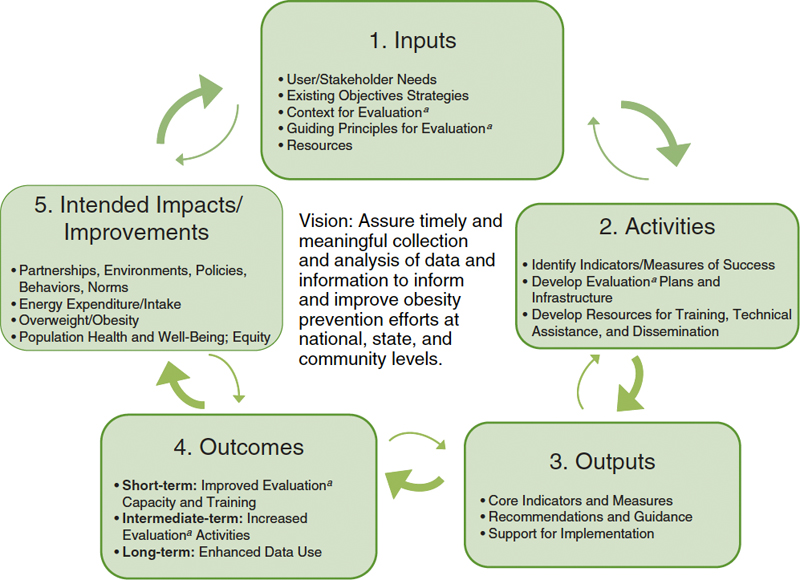
FIGURE 1-1 Framework for evaluating progress of obesity prevention efforts.
aEvaluation refers to assessment, monitoring, surveillance, and summative evaluation activities.
mendations (see Figure 1-1). The Committee aims to assure timely and meaningful collection and analysis of data to inform and improve obesity prevention efforts at national, state, and community levels. This framework addresses the full spectrum of resources or inputs to consider, activities to undertake, and the expected outputs, outcomes, and impacts that would result in fully realizing this vision. As such, the framework seeks to inform a systems perspective on the full range of influences on obesity and their relationships to each other. The Committee used this framework to inform its approach to developing the national, state, and community obesity evaluation planning and measurement ideas and recommendations. This framework and its components are fully described in Chapter 3. The Committee approached its tasks by searching for methods and indicators that would contribute to a model of evaluation that emphasizes its value as a professional or community learning tool to not only improve efforts, but also to prove their generalizable effectiveness (e.g., Green et al., 2009; Kottke et al., 2008). The Committee framed the evaluation not as an event, but as a continuous process of assessing community needs, planning services, programs or policies, and environmental changes, and monitoring their implementation and summatively evaluating their effectiveness.
USERS OF EVALUATION
Detailed in Chapter 2, key audiences for the report’s recommended plans and indicators are decision makers, community members, researchers, and evaluators at all levels and across all sectors, and the organizations that mandate or fund them. The Committee consisted of representatives from many of these stakeholders, and it reached out to representatives of other “end users” of this report’s recommendations to understand their needs and expected applications of evaluation ideas and measures. These consultations included representatives from the Centers for Disease Control and Prevention (CDC) and National Institutes of Health (NIH), the main federal funders of evaluation of obesity prevention and the research that informs it, and agencies that need evaluation to accomplish their missions and objectives related to obesity prevention.
EXISTING OBJECTIVES AND STRATEGIES OF OBESITY PREVENTION EFFORTS
The most recent among the several IOM obesity committee reports, referred to in this report as the APOP report (IOM, 2012a), supported the growing consensus of public health science and practice experts that environmental and policy strategies hold the most promise to accelerate progress in preventing obesity over the next decade. Unlike the more central role of clinical and pharmaceutical strategies central to the National High Blood Pressure and National Cholesterol Control programs, the 20 APOP strategies were organized around five environments:
1. the physical activity environment, which includes the aspects of the physical and built environment2 as well as norms and processes that increase access to, opportunities for, and social reinforcement of activity and decrease barriers to engaging in physical activity;
_____________
2 Aspects related to the physical and built environment include transportation infrastructure, land use patterns, and urban design.
2. the food and beverage environment, which seeks to increase the availability, attractiveness, and affordability of healthful foods and make unhealthful foods less available, attractive, and affordable;
3. the message environment that encompasses media and marketing that often promotes unhealthful foods and sedentary lifestyles but can be harnessed to counter those messages and promote healthful food and active lifestyles;
4. the health care and worksite environments in which promotion of healthful foods and physical activity can be arranged and promotion of unhealthful foods and sedentary lifestyles discouraged, with referrals of patients or employees to existing community resources for support and guidance; and
5. the school environment as a hub of health promotion, given the daily hours spent there by children and youth, with potential for incorporating opportunities for healthful food and physical activity as well as health education and promotion, as well as for reducing access to unhealthful foods and sedentary lifestyles.3
Table 1-1 itemizes the specific APOP strategies by major level or sector for action, for which this report’s recommended obesity plans and supporting recommended actions are intended to apply. The APOP report supported the inclusion of these strategies using the best available evidence and implementation research.
The APOP report stressed that the recommended strategies identified in the five key environments are interrelated and their collective implementation would have the most promise to accelerate obesity prevention over the next decade. Importantly, the report declared that successful implementation of the strategies will require engagement across all levels and sectors of society and leadership. This systems approach to obesity prevention, featured in Chapter 9 of this report, would coordinate the messages and environmental changes across multiple sectors and levels to provide maximum impact with minimal resources.
The APOP report also identified extant and promising “indicators of progress” that could be measured and analyzed to assess the impact of the APOP strategies. The APOP committee stressed that “it will be essential to monitor and track progress in the implementation” of the most promising strategies, “as well as to conduct sustained research on the magnitude and nature of their impact” (IOM, 2012a, p. 9). This Committee emphasized conclusions from prior reports that, although each strategy has the potential to accelerate progress, the system of large-scale transformative approaches that they recommended will be successful only if all stakeholders commit to a sustained effort in implementation and evaluation of these strategies.
THE WEIGHT OF THE NATION CAMPAIGN
Concurrent with the publication of the APOP report, HBO’s documentary film division and the IOM launched a coordinated, multi-media, multi-organizational campaign called TWOTN in May 2012. Presented in association with CDC and NIH, and in partnership with the Michael & Susan Dell Foundation and Kaiser Permanente, the campaign was designed to help create awareness, inform, and motivate action to slow, arrest, and reverse the trend of obesity across the country. The campaign includes
_____________
3 Strategies related to child care fall under physical activity, food and beverage, worksite, and health care environments.
TABLE 1-1 Accelerating Progress in Obesity Prevention Report Recommended Policy and Environmental Strategies by Level or Sector of Action
| Major Levels | Accelerating Progress in Obesity Prevention Report Recommended Strategies |
| (Sectors) of Action | (abbreviated topic version)* |
| Systems level |
• Development, implementation, and coordination of common messages, processes, and strategies |
| National (public sector) |
• Physical education and physical activity in schools • Physical activity in child care centers • Science and practice of physical activity • Sugar-sweetened beverages • Nutritional standards for all food and beverages • U.S. agriculture policy and research • Social marketing program • Food and beverage marketing standards for children • Nutrition labeling system • Nutrition education policies • Food literacy in schools • Weight gain and breastfeeding • School food and beverage standards |
| State (public sector) |
• Physical education and physical activity in schools • Physical activity in child care centers • Science and practice of physical activity • Sugar-sweetened beverages • Nutritional standards for all food and beverages • Food and beverage retailing and distribution policies • Food literacy in schools |
| Community (citizens and civic organization) |
• Enhancing the physical and built environments • Physical activity-related community programs • Sugar-sweetened beverages • Nutritional standards for all food and beverages • Food and beverage retailing and distribution policies • Social marketing program • Weight gain and breastfeeding |
| Schools (public sector) |
• Physical education and physical activity in schools • Physical activity in child care centers • Sugar-sweetened beverages • Nutritional standards for all food and beverages • Food literacy in schools • School food and beverage standards |
| Worksite |
• Sugar-sweetened beverages • Coverage of access to and incentives for obesity prevention, screening, diagnosis, and treatment • Healthy living and active living at work • Weight gain and breastfeeding |
| Major Levels | Accelerating Progress in Obesity Prevention Report Recommended Strategies |
| (Sectors) of Action | (abbreviated topic version)* |
| Health care |
• Sugar-sweetened beverages • Nutritional standards for all food and beverages • Health care and advocacy • Coverage of access to and incentives for obesity prevention, screening, diagnosis, and treatment • Healthy living and active living at work • Weight gain and breastfeeding |
| Business community/private sector |
• Sugar-sweetened beverages • Food and beverage options for children in restaurants • Nutritional standards for all food and beverages • Food and beverage retailing and distribution policies • Food and beverage marketing standards for children • Nutrition labeling system |
* There are a total of 20 recommended strategies. Strategies are duplicated in the table if more than one level or sector of action can support the implementation of the strategy.
SOURCE: IOM, 2012a.
a four-part television documentary series for a national audience (aired May 2012, but available for download or on CD without charge to communities for community screenings) and a set of activities for use by individual communities, including a series of bonus video shorts on specific topics related to obesity, a companion trade publication for a broad adult audience, three other documentaries for children and families (to be released May 2013), and a book and action guide geared to elementary school students and their teachers. The campaign is supported by a national-level information- and video-rich website4 and an extensive presence on social networks. Thus, TWOTN has both national (primarily the HBO series and associated website) and community components (e.g., community screenings, school initiatives). Chapters 6 (national) and 8 (community) will address the potential evaluation of TWOTN in response to the Committee’s charge to identify “measurement ideas” to determine the reach, implementation, outcomes, and impact of the overall campaign. Given the range of social media and advocacy efforts involved in TWOTN, it can serve as an illustrative example of some of the challenges and opportunities that are inherent in evaluation of similar obesity prevention initiatives. Box 1-2 provides background on the importance of the evaluation of TWOTN and other large-scale programs or campaigns.
OBESITY-RELATED RESEARCH PRIORITIES
Once established, obesity is difficult to reverse, and obese children are much more likely to become obese adults (American Dietetic Association, 2006; Bao et al., 1995; Bouchard, 1997; Freedman et al., 1999; Serdula et al., 1993; Thompson et al., 2007). Childhood obesity and weight gain may be associated with higher mortality and morbidity in adulthood, including cardiovascular disease, cancer, diabetes, sleep apnea, gout, and orthopedic problems (IOM, 2012a). Obese children also face social problems, such as
_____________
4 See http://theweightofthenation.hbo.com (accessed November 11, 2013).
BOX 1-2
Importance of Evaluating The Weight of the Nation and Other Large-Scale Social Media and Advocacy Efforts
The Weight of the Nation (TWOTN) is an example of one of many initiatives that have been undertaken to raise awareness and promote the rationale behind and recommendations of the Accelerating Progress in Obesity Prevention report (IOM, 2012a). Evaluation is one way to determine the effects TWOTN has on awareness of obesity and other outcomes, whether these effects were related to how the information was presented (e.g., through the television broadcast, website, or community events), and what potential actions were taken as a result. Evaluation results can then be used to guide future dissemination efforts for TWOTN, as well as for similar programs/campaigns.
Careful formative evaluation increases the chances of success of programs/campaigns (Worden et al., 1988). Unfortunately too few studies have investigated uses of mass media for changing social networks, communities, and places to fully understand how effective they can be (Abroms and Maibach, 2008).
How effective are small-scale community programs/campaigns? Unfortunately most small-scale, community, mass media programs alone have not been effective (Noar, 2006; Snyder and Hamilton, 2002). One exception is long-term campaigns designed to increase advocacy for community policy changes that are framed on the themes of children’s health and social justice (Freudenberg et al., 2009). Most community-level campaign effects are small in size; Snyder and Hamilton’s (2002) meta-analysis of 48 mass media health campaigns found an average effect size (mean of correlations, Mr) of only 0.09. Moreover, the average effect size for purely persuasive campaigns were about half (Mr=0.05), whereas the average effect size for campaigns that promoted behaviors that were enforceable by law (e.g., seat-belt use) were almost double (Mr=0.17).
How effective are national programs/campaigns? It is clear that national programs that have clear objectives, are intensive and focused, and are long term can achieve greater effects than those that do not (e.g., the Legacy truth® campaign) (Farrelly et al., 2005, 2009). Furthermore, adding community activities can help to increase reach and effectiveness (e.g., the VERBTM campaign, see Bauman et al., 2008; Berkowitz et al., 2008; Huhman and Patnode, 2013; Huhman et al., 2010); but sustained resources and funding are necessary.
How can TWOTN or similar programs be evaluated? First, the objectives of a program/campaign need to be very clear—concise, well understood, and widely communicated. An important component is the socio-ecological levels at which the effects are expected to occur, that is, on individuals (awareness, attitudes, or behavior), social networks (peer pressure or social support), or communities/institutions (community action/advocacy or policy) (Maibach et al., 2007). Equally important, what kinds of changes are expected? Some or all of the following may be in play: increased awareness of health issues or their social determinants (Clarke et al., 2012), individual-level antecedents to behavior (e.g., knowledge, attitudes, perceptions, self-efficacy, or intentions) (Fishbein and Ajzen, 2009), improved behavior of individuals, changed peer pressures, or social support within social networks (Rogers, 2003; Valente and Saba, 2001), community action/advocacy toward policy development/change (Freudenberg et al., 2009), or changes in characteristics of places (Maibach et al., 2007). To design an appropriate evaluation, evaluators need to understand the socio-ecological levels and the nature of the expected effects of the program or campaign they will be evaluating. Evaluations also need to be planned well ahead of the campaign so that appropriate control or comparison sites/data can be identified and pretest data can be collected. See Chapter 6 for detailed suggestions and considerations for evaluating the national-level objectives, Chapter 8 for evaluating the community-level objectives of TWOTN, and Chapter 10 for a summary of the challenges and opportunities inherent in evaluation of similar obesity prevention initiatives.
exclusion and victimization, and are more likely to have psychological problems, such as depression and low self-esteem (Eisenberg et al., 2003).
The impact of obesity has been estimated in direct costs as well as nondollar metrics such as days lost at work, years of life lost, excess fuel use, and level of education completed—the costs related to remedial spending, productivity, transportation, military readiness, and human capital (Hammond and Levine, 2010). Economic growth across the past few decades has shifted concern from issues of underweight to issues of overweight. Community factors have created environments that have changed the physical activity patterns and food consumption in people’s daily lives in directions that produce obesity. Although recent prevalence data may suggest that interventions aimed at obesity for the past several years are beginning to have a cumulative effect, obesity levels remain high and, in some populations, significant increases continue (Howard, 2012; IOM, 2012a).
Obesity poses one of the biggest public health challenges of the 21st century, and yet several questions about the epidemic and its basic biology and pathophysiology and the effectiveness of behavioral, clinical, and public health interventions remain perplexing. Therefore, while taking action to contain the epidemic and to test and evaluate interventions is inescapably necessary, focused effort to address the research gaps also remains imperative. Indicators of progress toward obesity prevention need to embrace measures that can chart the application and progress of research to tackle the epidemic from a strong science and evidence base. This attention would seek to bridge the gap between what is known or presumed from research to be widely effective and what is being adopted and applied, with what degree of fidelity or type of adaptation, and with what relative success in varied populations and circumstances (Green, 2001; IOM, 2010a). Part of the problem of bridging the gaps lies in the scientific pipeline of vetting and publishing the research in ways that anticipate end-user needs for implementation. These include reporting of null or negative results, selectivity of and attrition from study samples, and sufficient detail about the interventions to enable researchers to understand and compare them, and practitioners to replicate or adapt them (Briss et al., 2004; Colditz et al., 2012; Green et al., 2009; IOM, 1997). The gaps discovered in this part of the evaluation efforts would help the scientific enterprise to circle back and reconsider the more basic and applied research on which assumptions of wide applicability had their origins (Garfield et al., 2003).
Although recommendations on basic research are beyond the scope of this report, the Committee deemed it important to acknowledge the limitations of basic research foundations in areas identified in the next few paragraphs. Also needed in linking evaluation with gaps in the research base is a better analysis of the age-period-cohort effect of the obesity epidemic over long periods of time. The gaps in the research base for obesity reqiure attention along several fronts concomitant with the evaluation of the progress of efforts to control the epidemic. For example, although national survey data indicate a high prevalence of obesity, recent data indicate that the rise in prevalence may be plateauing in adults and children (Flegal et al., 2012; Ogden et al., 2012a,b). In addition to national prevalence data based on measured overweight and obesity, a better grasp of what is going on with the obesity epidemic will also require national data on incidence (i.e., new cases) and its trends over time and in specific age-sex-ethnic groups, in particular among adults. Incidence could be a more sensitive indicator of success in primary prevention than prevalence in adults insofar as it measures with greater sensitivity new cases of overweight or obesity rather than the combination of new and continuing cases. Continuing cases measure success or failure of weight-reduction treatment rather than prevention, or duration rather commencement of the problem.
Although obesity has varied impacts on each of several aspects of health (mortality; incidence and prevalence of diabetes, cardiovascular disease, and cancers; and disability), epidemiological data suggest that the association between body weight and mortality is U-shaped, while those between body weight and other outcomes are linear. These seemingly contradictory relationships warrant careful future investigation and raise questions about the trade-off between avoiding mortality and preventing morbidity when it comes to obesity prevention interventions (Flegal et al., 2013). For example, maintaining “normal” weight ranges in the early and middle adult years is generally protective in the older years. Yet, a degree of overweight may be protective when some illnesses arise, although the issue of reverse causality in the U-shaped association between obesity and the diseases causing mortality cannot be ruled out. In fact, robust evidence from randomized controlled trials on clinical interventions have so far been limited to the effectiveness of weight loss on diabetes incidence among people with prediabetes (Garfield et al., 2003; Knowler et al., 2002) and on disability among people with prediabetes or diabetes (Look AHEAD5), while some trials of cardiovascular prevention have produced null findings (e.g., MRFIT6). Trials of bariatric surgery to induce weight loss have demonstrated positive benefits on health outcomes, however, these data apply to special clinical situations and are less applicable to public health approaches (Shea et al., 2010). On the other hand, recent evidence from a randomized controlled trial indicates the positive benefits of a high-quality diet (i.e., rich in fruits and vegetables, whole grain, and monosaturated fat; low in red meat and saturated fat) on health outcomes, including cardiovascular disease incidence, even when weight loss is not achieved (Estruch et al., 2013). A recent analysis by CDC (Flegel et al., 2013) indicates that the widespread assumption of a linear relationship between overweight or obesity and mortality does not hold in analyses of large national samples, which is particularly significant to the conduct and evaluation of efforts to prevent obesity.
Even more challenging is that affecting and maintaining weight loss are often difficult. Weight gain is accompanied by impressive changes in neuroendocrine hormones (e.g., leptin, ghrelin), and these hormonal changes seem to persist and fight to restore the body’s pre-weight-loss homeostasis for several months following significant weight loss (Sumithran et al., 2011). Thus, weight loss is affected by not only the socio-behavioral-cultural-environmental determinants on which interventions are acting, complex as these are, but also biological processes and interventions. Better understanding of the biological basis of weight gain and weight loss, including determinants of eating preferences and cultural norms for feeding in early childhood, is needed, so that effective interventions can be developed and tested within the context of the environments and lifespan in which they would be applied. Considerable investment in rigorous, high-quality research therefore is needed to (a) understand more fully the biology of overweight and obesity and (b) test interventions to prevent overweight and obesity in individuals and populations in various settings (e.g., home, work, school) and at various developmental levels (e.g., toddler, child, adolescent, adult). The IOM report Bridging the Evidence Gap in Obesity Prevention identified ways to “locate, evaluate, and assemble evidence to inform decisions” for evidence-based practice while generating more practice-based evidence that would contribute to building a strong evidence base to identify,
_____________
5 Look AHEAD (Action for Health in Diabetes) is a multicenter randomized clinical trial to examine the effects of a lifestyle intervention on weight loss over the long term. Look AHEAD is focusing on type 2 diabetes and cardiovascular disease (http://www2.niddk.nih.gov/Research/ScientificAreas/Obesity/ClinicalStudies/AHEAD.htm, accessed November 11, 2013).
6 MRFIT (Multiple Risk Factor Intervention Trial for the Prevention of Coronary Heart Disease) was a special intervention program consisting of stepped-care treatment for hypertension, counseling for cigarette smoking, and dietary advice for lowering blood cholesterol levels (http://www.trialresultscenter.org/study7914-MRFIT.htm, accessed November 11, 2013).
improve, and refine promising obesity prevention practices for different sectors, populations, and settings (IOM, 2010a).
CONTEXT FOR ASSESSMENT, MONITORING, SURVEILLANCE, AND SUMMATIVE EVALUATION NEEDS
In its deliberations and recommendation development, the Committee held paramount the over-arching principles of an ecological and systems understanding of the obesity problem in society overall and in specific populations. The Committee’s remit was to recommend evaluation plans to address the APOP-recommended interventions, which were concentrated on environmental and population, rather than clinical, domains. This focus meant a search for and a commitment to indicators that would measure social and policy determinants of obesity and health, as well as an understanding of the interaction of these with organizational, family, and individual determinants and outcomes. The latter would include clinical interventions that are not the focus of this report, although the Committee recognizes the importance and the promise of clinical interventions within the ecology of obesity. The Committee viewed policies and policy changes relating to the environment as key leverage points at the broad population, organization, community environment, and individual levels. These changes include specific environmental, economic, and behavioral restraints on or incentives for the manufacturers, vendors, and marketers of obesity-related products and services; and influencing organizations, families, and social groups that influence individual behavior. The chapters that follow lay out the considerations and the recommendations on each of the foregoing aspects of evaluating progress in obesity prevention. Some aspects of evaluation remain necessarily incomplete or underdeveloped given the gaps in scientific knowledge of the determinants of overweight and obesity and of the relative effectiveness of interventions for various population groups and settings. Some of the strategies for evaluating obesity prevention efforts considered, therefore, draw on the notable public health successes in the past (CDC, 2007; Isaacs and Schroeder, 2001; Ward and Warren, 2006), for example in reducing mortality from and prevalence of cardiovascular diseases (e.g., coronary heart disease and stroke) and some of the risk factors associated with them, such as smoking, total cholesterol, and hypertension.
Societies have gradually associated overweight, obesity, inadequate physical activity, and unhealthful dietary habits (e.g., low fruit and vegetable consumption, high intake of refined grains and foods high in fats and/or sugars and low in nutrients, and excessive calorie intake), individually and collectively, with the characteristics of an epidemic (or set of converging epidemics). The United States, among other countries, faced the rude awakening that few tools were at hand to deal with the behaviors: no immunization, limited pharmaceutical or surgical options, and no simple or single environmental or behavioral change to prevent obesity’s relentless rise and spread across the nation, indeed the world. Furthermore, the scientific understanding of the biological basis of obesity, and how genes and changes in the environment affect it, remain rudimentary and often unclear or mixed. If a multitude of strategies to understand the causes (biological, behavioral, and societal, and their interactions) of obesity and strategies to prevent or control it need to be pursued and coordinated, then they need to be evaluated, as well. Such strategies cannot be pursued with confidence that the prior evidence for their presumed effectiveness is generalizable to different settings and populations (Garfield et al., 2003; Green, 2001; Green and Glasgow, 2006; Green et
al., 2009; Kottke et al., 2008). Evidence on which strategies will work in which combinations, for which populations, through which channels, and in which amounts or intensity or duration remains scant.
Monitoring
Monitoring involves a phase of evaluation focused on the implementation of planned interventions, from the tracking of legislative proposals and policies to the adoption and the quality and extent of implementation of practices by government agencies and other organizations, or by their practitioners. Public health law and policy monitoring involves the “ongoing, systematic collection, analysis, interpretation, and dissemination of information about a given body of public health law and policy” such as state laws related to competitive food sales in schools, community zoning ordinances governing the availability of food outlets, state and school district policies governing physical education requirements, and state licensing requirements for health care providers (Chriqui et al., 2011, p. 21). Policy monitoring systems examine changes in on-the-books, formal, codified laws (regulations or other policies that implement the law or proposed bills) over time (based on a given reference date such as January 1 of each year) and typically compare change on quantitative measures that assess the nature and extent of a given law or policy (e.g., not only whether a policy exists but also whether it is required or encouraged) (Chriqui et al., 2011).
Policy monitoring data make it possible to examine the appearance and distribution of laws and policies and, when combined with surveillance or other monitoring and evaluation systems, the influence or impact of a given law or policy across jurisdictions on changes in the environment or behaviors over time. For example, policy monitoring systems compiled by the National Cancer Institute and through the Robert Wood Johnson Foundation–supported Bridging the Gap Program have enabled examination of the association between a variety of state school-based food and physical activity–related laws and changes in school practices, student attitudes, and student behaviors over time (Chriqui et al., 2012; Perna et al., 2012; Taber et al., 2012; Turner et al., 2012). Other applications have included assessing the influence of sponsored research programs on policy advocacy or decision making (Ottoson et al., 2009, 2013). When designed and implemented properly (see Chriqui et al., 2011), policy monitoring systems, combined with surveillance or with monitoring of organizational, environmental, and practitioner behavioral changes, can be an enormous asset for policy development, advocacy, and evaluation, and can be particularly useful for examining the impact that an individual policy or a group of policies can have over time and across jurisdictions.
Policy monitoring systems often build on and complement policy “tracking” systems, which provide important information about the policy-making process and content, particularly to advocates and decision makers interested in the “traction” on a given issue. For example, more than 1,700 obesity-related bills and resolutions were introduced and adopted from 2006 to 2009 across the 50 states and the District of Columbia (Eyler et al., 2012). Data from policy monitoring systems allow for comparisons of progress among states and for determination of the types of bills that are being introduced and passed (e.g., school nutrition standards, safe routes to school programs). Table 1-2 compares policy monitoring and policy surveillance systems. Both types of systems and their resultant data may be useful for examining progress in obesity-related policy making.
Monitoring of implementation quality and effort with other interventions besides policies involves consolidated record-keeping, reporting, and observational or survey systems that track the adoption
TABLE 1-2 Comparison of the Concepts of Surveillance and Summative Evaluation
| Characteristic | Surveillance | Summative Evaluation |
| Goals |
• Set public health priorities • Detect outbreaks and epidemics • Track behavioral changes over time • Evaluate programs • Track environmental changes • Provide data for research and evaluation |
• Measure effectiveness • Improve programs by making course corrections • Adjust funding, effort, and sustainability • Disseminate knowledge |
| Design | More comparability to other jurisdictions and national | Flexible |
| Focus | Consistency of data for comparisons over time and between jurisdictions | Internal validity of associating interventions with outcomes |
| Type of data | Mainly quantitative | Both qualitative and quantitative |
| Controlling entity | Stakeholders/practitioners | Stakeholders/practitioners |
| Time frame | Ongoing | Usually episodic* |
* Sometimes follows a specific time frame based on funding or the objective of the summative evaluation.
and implementation of evidence-based or mandated practices in or across jurisdictions or organizations or sub-organizational units. It is helpful to know which kinds of organizations are adopting and implementing policies and new practices and at what rate. This can inform the plans for intensification and allocation of dissemination efforts and technical assistance to increase adoption, implementation, and maintenance of practices (Brownson et al., 2012). Within organizations, practitioners sometimes take up a self-study or continuous quality improvement process to monitor their implementation of new practices recommended by new evidence of effectiveness (Mittman, 2012). Across public health organizations, performance monitoring has developed around “rapid-cycle improvement techniques” associated with a core set of services (IOM, 2010b; Jacobson and Lotstein, 2013).
Summative Surveillance
Surveillance7 is a cornerstone of public health (McQueen and Puska, 2003; Teutsch and Churchill, 2000), and its importance is illustrated in the adage “what gets measured, gets done” (Thacker, 2007; Thacker and Berkelman, 1988). Public health surveillance, including the ongoing, systematic collection, analysis, and interpretation of outcome-specific data is essential to the planning, implementation, and evaluation of public health interventions. These functions are closely integrated with timely dissemination and utilization of these data by those responsible for prevention and control (Goodman et al., 2000; Ottoson and Wilson, 2003; Thacker and Berkelman, 1988).
A surveillance system includes a functional capacity for data collection, analysis, and dissemination linked to public health programs. Three features of a public health surveillance system are critical. First, its activities must be ongoing with systematic periodicity; one-time surveys and sporadic epidemiologic studies are not sufficient. Second, the system must be integrated with public health activities (e.g., pro-
_____________
7 In a community context, collecting baseline data of status is commonly referred to as an “assessment.” Surveillance provides repeated or continuous assessments of progress or change over time.
vides early warning of health problems to guide control measures) (Thacker et al., 1989). Third, the use of the disseminated data must be regularly evaluated (German et al., 2001). The key characteristics of surveillance and how they differ for summative evaluation are shown in Table 1-2.
The origins of public health surveillance are rooted in infectious disease control, dating back to tracking the bubonic plague in the 14th century (Thacker and Stroup, 2006). The early systems for surveillance followed the discovery of the agents responsible for infectious diseases such as smallpox, typhus, and yellow fever. Langmuir and colleagues extended the definition of surveillance from tracking afflicted persons to tracking populations in the 1940s (Langmuir, 1963). The expansion of surveillance to include chronic diseases and risk factors (including obesity) began in the 1970s and continued with the push in the early 1980s to gather surveillance data relevant to evaluating progress in relation to the first round of the Healthy People objectives for the nation (Green et al., 1983). More recently, global behavioral risk factor surveillance has gathered momentum (McQueen and Puska, 2003; Warren et al., 2000) and, particularly relevant for this report, the definition of obesity-related surveillance has been expanded to include environments and policies (Ottoson et al., 2009).
Measuring Prevalence and Incidence of Obesity
Today, numerous useful surveillance systems exist in the health sector for tracking obesity and obesity risk factors (e.g., diet, physical activity) and in other sectors for tracking changes in risk conditions such as the built environment and transportation systems and their utilization; sports participation; park and recreational area availability and use; school lunch and playground policies; and agricultural food supply, manufacture, and distribution (e.g., Hallal et al., 2012). National datasets (e.g., BRFSS, NHANES, NHIS8) permit the surveillance of overweight/obesity prevalence by age, gender, and race/ethnicity over time (described in more detail in Chapter 4). International datasets are emerging for physical activity surveillance (e.g., Bauman et al., 2011; Rutten et al., 2003). As described in Chapters 5, 6, and 8, however, precise estimates for some particular U.S. populations (e.g., Asians and Pacific Islanders) are often challenging and require preferential sampling in national surveys. Only the BRFSS, which collects self-reported data on weight and height, can provide subnational estimates (state level or county level for some localities, or by synthetic estimates from state data) of obesity prevalence. The United States has no national system to measure incidence of obesity directly to enable analysis of trends in rates of appearance of new cases of obesity. A national system could be helpful, at least for data on adults. A few regional and community cohort studies, such as the Bogalusa Heart Study, the Framingham Heart Study, the Pima Indian Study, and the Hispanic Community Health Study/Study of Latinos may permit measurement of incidence of obesity for selected populations (see Chapter 7 for community surveillance and “community health assessment” examples).
Newer Types of Surveillance
Sufficient epidemiologic data now exist for estimating which population groups and which regions of the country are affected by obesity and how prevalence patterns are changing over time with respect to the epidemic. To supplement these data, however, we need better information on a broad array of environmental (e.g., commercial, recreational, and built environments) and policy factors (e.g., state laws) that
_____________
8 BRFSS = Behavioral Risk Factor Surveillance System; NHANES = National Health and Nutrition Examination Survey; NHIS = National Health Interview Survey.
determine these patterns (Chriqui et al., 2011; Ottoson et al., 2009), as well as better understanding of how and how well surveillance data are being used (Ottoson and Wilson, 2003).
Environmental surveillance relevant to obesity includes national, state, and small area (e.g., county, municipality, school district, zip code) measures of the physical environment that influence individuals’ and families’ decision making relative to their energy intake and energy expenditure. Environmental data may be obtained from geographic information systems (GIS) that depict land uses (e.g., parks, streets, bike paths, buildings), commercial or other data sources that contain information on the existence of specific types of facilities and outlets (e.g., recreational facilities, fast food, farmers’ markets, and other food retail), or through audit-type evaluations that document characteristics of the physical, food, school, child care, worksite, and other related environments (Brownson et al., 2009; McKinnon et al., 2009). For these data to be useful for surveillance purposes, however, they need to be publicly available and consistently compiled over time (Lee et al., 2010). Environmental surveillance efforts exist to some extent nationally (e.g., at the census block group or zip code levels) but only for limited measures of land use. Many individual research and evaluation studies and individual communities have compiled data on the physical environment, but few exist nationwide, statewide, or consistently across small geographic areas (e.g., counties, municipalities, school districts, zip codes, etc.). National and community obesity prevention–related evaluation studies would benefit from consistent compilation and tracking of environmental data across geographic areas and over time. Environmental sensors in new wireless communication technologies hold promise for more data of this kind becoming publicly available (e.g., Bravo et al., 2012), which could be combined with GIS data to measure physical activity or obesogenic environments (Frank et al., 2012; Kerr et al., 2011).
Evaluation
The culmination of the series of assessment, surveillance, and monitoring strategies and systems just described leads to summative evaluation. Evaluation lies in using interventions selectively or collectively, together with summative evaluation designs for comparison (over time or between groups of organizations, communities, or people exposed or not exposed to an intervention) and measures based on common indicators to associate the intervention(s) with the outputs, outcomes, or impacts. This report will use the term evaluation to encompass the collectivity of the assessment, monitoring, and surveillance methods or systems and the summative evaluation designs to relate interventions to their outputs, outcomes, and impacts.
The overriding purpose of summative evaluation is to be able to attribute, with a known degree of certainty, whatever outputs, outcomes, or impacts (effects) are found to the interventions presumed to have caused them. Such attribution depends on controlling with experimental and statistical methods the competing explanations for the effects. The degree of certainty is the statistical notion of “significance,” that is, the probability that a given observed and measured effect could have been caused by chance. Summative evaluations require at a minimum some pairing of pretest and post-test measures of the desired effects, or another method to compare a population exposed to one not exposed to the intervention. The variations in experimental and quasi-experimental designs to control for threats to the validity of the cause-and-effect attribution are widely established in the literature and textbooks of experimental research and program evaluation (e.g., Campbell and Stanley, 1966; Shadish et al., 2002).
Indicators of Progress
As detailed in Chapter 3, an overriding factor in the Committee’s selection of indicators for evaluation (assessment, monitoring, surveillance, and summative evaluation) relates to balancing the tension between comprehensiveness and selectivity. The Committee favored the latter. The nine guiding principles for indicator selection include accuracy, comparability, feasibility, health disparities/equity, parsimony, priority setting, relevance, scalability, and sustainability (see Appendix C). The portfolio of indicators presented in Chapter 4 balances measures of structure (e.g., inputs, resources), process (e.g., actions), and outcomes (e.g., incidence and prevalence of obesity, changes in diet and activity behaviors). For all indicators, the Committee paid careful attention to end-user relevance, so that the measurement is not simply an academic exercise but rather a process to stimulate conversations among various stakeholders and to facilitate evidence-based action. In accordance with its task, the Committee selected of indicators that align with the APOP strategies and that focus on policy, behavioral, and environmental changes related to food and physical activity. As discussed in Chapter 4, sleep, endocrine disruptors, and other physiological functions may be important areas to measure to address broader population health and obesity prevention–related issues that do not directly link to APOP report topics (Keith et al., 2006). Finally, differences between evaluation of interventions with children and evaluation of interventions with adults have been considered in the selection of indicators.
Promoting Health Equity and Reducing Disparities
Of particular concern to the Committee from the outset of its discussions was the growing recognition that evaluating progress for the nation as a whole, or even for regions of the United States, will need to pay special attention to the disparities that have accompanied the obesity epidemic. This central concern is driven in part by the commitment of the Healthy People 2020 disease prevention and health promotion objectives for the nation, which focus on the social determinants of health and the elimination of disparities in health a centerpiece (Koh et al., 2011b). The concern for reducing disparities/promoting health equity is also driven by the growing recognition that the nation’s progress on several other health promotion objectives has been impressive in the aggregate, but often at the expense of widening rather than narrowing the disparities between segments of the population that are grouped by income, education, and sometimes ethnicity or race. Chapter 5 more fully addresses these issues, together with issues of representativeness of the survey samples and the periodicity and oversampling of key population segments in the NHANES.
Recently, the World Health Organization Commission on Social Determinants of Health (Solar and Irwin, 2010) postulated three mechanisms by which health inequities are produced: (1) differential exposure to intermediary factors (e.g., poor material circumstances such as inadequate housing, hazards, and harsh living conditions); (2) differential vulnerability to health-compromising conditions (e.g., through limited education, income, and associated lower socioeconomic position); and (3) differential consequences (e.g., poor-quality services or no access to services). In Chapter 8, the Committee seeks to provide framing and support for summative evaluation of interventions and tracking of progress across populations at greater risk of obesity.
In accordance with Section 4302 of the Affordable Care Act (ACA),9 passed in 2010, the Department of Health and Human Services (HHS) has developed and adopted new data collection standards for race, ethnicity, sex, primary language, and disability status. The data standards represent a new opportunity for HHS to collect and use demographic data uniformly to shape its programs and policies. In April 2011, HHS unveiled its 2011 Action Plan to Reduce Racial and Ethnic Health Disparities (Disparities Action Plan) (Koh et al., 2011a). The Disparities Action Plan leveraged multiple provisions embedded within the ACA, which not only offer a wide array of opportunities to improve access to care and to eliminate disparities, but also strengthen the federal government infrastructure for data collection. Specifically, Section 4302 focuses on the standardization, collection, analysis, and reporting of health disparities data. In October 2011, the newly adopted HHS data standards for race, ethnicity, sex, primary language, and disability status began to be implemented in all new HHS-sponsored population health surveys (at the time of the next major revision to current surveys) (Dorsey and Graham, 2011). This provides an example of efforts to standardize data collection to improve comparability across evaluation efforts, across jurisdictions and organizations, and over time.
Taking a Systems Science Approach to Evaluation
The biology of obesity is complex, and so are the behavioral and environmental triggers that contribute to obesity. Numerous seemingly disparate factors interact in ways, known or unknown, to create a powerful set of dynamics that promote obesity. Any solution to obesity will need to account for this complex web of biological, behavioral, and environmental factors. Building on current evaluation methods, this systems science approach requires that evaluation planners consider the properties of a complex system while evaluating obesity prevention efforts. Several of the principles of systems science identified in this report are linked with diffusion theory (Rogers, 2003) that posits the importance of opinion leaders within systems and the impact of complexity on adoption of a new innovation.
The Committee’s recommendation of indicators to assess the APOP report strategies and the national and community obesity evaluation plans are guided by the properties of complex systems, and the consideration of community and population values for evaluation of health promotion interventions outlined in previous IOM reports (IOM, 2010a, 2012a,b). To establish a robust evaluation framework (see Figure 1-1), the Committee considers the application of a complex systems science approach to be a promising and much-needed means of ensuring ongoing insight and lessons that will continue to inform the field (see Chapter 9).
Why is a focus on complex systems different from what previous models used to frame obesity prevention evaluation? The socio-ecological model has been well accepted and continues to provide important insights as a descriptive model. The Committee recognized, however, the need to emphasize, not only the structural layers of systems, but also the interactions and reciprocal causal relationships among the many elements of the system, properties that the socio-ecological model does not capture as well. Hence, the recommendation to enhance the use of systems science approaches in evaluating progress in obesity prevention extends the evaluation methods from “complicated” systems (e.g., socio-ecological model) to “complex” systems.
_____________
9 See http://www.gpo.gov/fdsys/pkg/CREC-2009-11-19/pdf/CREC-2009-11-19-pt1-PgS11607-3.pdf#page=127 (accessed November 11, 2013).
SUMMARY
The solution to the obesity crisis depends on finding what is working to affect the causes of obesity. This will require evaluation, which will depend on developing agreement on the use of (a) common indicators in assessing the status of communities; (b) surveillance to track changes in the status of communities, regions, and the nation; (c) monitoring of the policies, programs, and other interventions associated with changes; and (d) summative evaluation of the extent to which interventions and combinations of interventions result in changes in outcomes. These essential ingredients to tracking progress in the nation’s efforts to prevent and control obesity are detailed in the chapters that follow. This iterative process begins with an assessment of the needs of the users of evaluation products and development of a framework that places the ingredients and products in relation to each other in a cycle of cause-effect assessments. This process ends with examinations of the implications of evaluation, from the perspective of populations experiencing disparities in overweight and obesity and from the perspective of whole systems. Although it would be ideal to approach evaluation from a complex multilevel framework and to adopt the evaluation plans found in this report, the Committee acknowledges that in several situations funding or logistical constraints may preclude such a full approach. Nevertheless, acquiring scaling evaluation data through more feasible means, such as “practice-based evidence” methods or grassroots-driven evaluation, may provide valuable insights and inform programs on how innovations might diffuse through systems (Brownson et al., 2012; Rogers, 2003).
OVERVIEW OF THE REPORT
Adapting the framing presented in the 2010 IOM report Bridging the Evidence Gap in Obesity Prevention, this report suggests ways to answer three questions in evaluation: Why, What, and How (see Figure 1-2). The answers seek to make the assessment, monitoring, surveillance, or summative evaluation procedures undertaken in given settings productive of evidence that will be relevant and useful to the evaluation users (reviewed in Chapter 2) and help to establish an infrastructure for monitoring progress of obesity prevention efforts at national, state, and community levels.
This report answers the following questions:
• Why? Describing why the proposed methods, procedures, or indicators for assessment, monitoring, surveillance, and summative evaluation need to be considered sequentially;
• What? Describing what has been or can be accomplished through assessment, monitoring, surveillance, and summative evaluation, including
— describing the prevalence/incidence and trends of obesity and its determinants;
— describing the prevalence/incidence and trends of obesity prevention activities;
— understanding the effectiveness of the delivery and implementation of obesity prevention interventions; and
— identifying what plans to implement and improvements to make given a particular user’s context; and
• How? Describing how to implement the “what” in a concrete and actionable way.
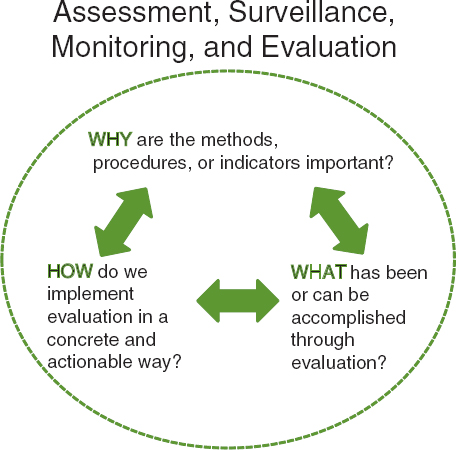
FIGURE 1-2 Questions that guide evaluation research efforts.
The Committee recognizes that a myriad of responses can be offered to the why, what, and how. In developing this report, the Committee sought to build on the APOP report and to apply state-of-the-art principles in evaluation, stakeholder engagement, and systems science.
The next two chapters provide background on and fundamental concepts of evaluation. Chapter 2 focuses on the main stakeholders’ preferences and needs for evaluation information, including those of policy makers, advocates for interventions, community coalitions, and program managers. Chapter 3 presents the framework for realizing the Committee’s vision—the inputs, activities, outputs, outcomes, and impacts necessary to improve assessment, monitoring, surveillance, summative evaluation, and enhanced data use to reduce obesity and improve population health and health equity. Chapters 2 and 3 are particularly geared toward a better understanding of how the Committee’s recommendations contribute toward closing evidence-to-practice gaps to improve and inform obesity prevention efforts.
In Chapter 4 the Committee identifies readily available indicators that can be used at the national, and sometimes at the state and community levels, to measure progress in obesity prevention. Chapter 5 focuses on tools and research methods for measuring progress that are appropriate for populations with health disparities that are closely linked with social, economic, and environmental disadvantage. Chapter 6 details a National Obesity Evaluation Plan with suggested adaptations for state and regional plans. Chapter 7 presents a plan for community health assessments and surveillance and Chapter 8 presents a plan for monitoring of implementation and summative evaluations of the effects of community-level interventions. Chapter 9 offers a systems perspective for evaluating progress in obesity prevention. Measurement ideas for the HBO/IOM TWOTN campaign can be found in Chapters 6 (its national
components) and 8 (its community components) and are offered as examples of opportunities and challenges inherent in evaluation, considering the respective national and community obesity evaluation plans. Chapter 10 concludes the report by presenting recommended plans, action-oriented recommendations to support the implementation of the recommended plans, and measurement ideas for the HBO/IOM TWOTN campaign.
REFERENCES
Abroms, L. C., and E. W. Maibach. 2008. The effectiveness of mass communication to change public behavior. Annual Review of Public Health 29:219-234.
American Dietetic Association. 2006. Position of the American Dietetic Association: Individual-, family-, school-, and community-based interventions for pediatric overweight. Journal of the American Dietetic Association 106(6):925-945.
Bao, W., S. R. Srinivasan, W. A. Wattigney, and G. S. Berenson. 1995. The relation of parental cardiovascular disease to risk factors in children and young adults. The Bogalusa Heart Study. Circulation 91(2):365-371.
Bauman, A., H. R. Bowles, M. Huhman, C. D. Heitzler, N. Owen, B. J. Smith, and B. Reger-Nash. 2008. Testing a hierarchy-of-effects model: Pathways from awareness to outcomes in the VERB campaign 2002-2003. American Journal of Preventive Medicine 34(6 Suppl):S249-S256.
Bauman, A., B. E. Ainsworth, J. F. Sallis, M. Hagstromer, C. L. Craig, F. C. Bull, M. Pratt, K. Venugopal, J. Chau, M. Sjostrom, and International Prevalence Study Group. 2011. The descriptive epidemiology of sitting. A 20-country comparison using the International Physical Activity Questionnaire (IPAQ). American Journal of Preventive Medicine 41(2):228-235.
Berkowitz, J. M., M. Huhman, C. D. Heitzler, L. D. Potter, M. J. Nolin, and S. W. Banspach. 2008. Overview of formative, process, and outcome evaluation methods used in the VERB campaign. American Journal of Preventive Medicine 34(6 Suppl):S222-S229.
Bouchard, C. 1997. Obesity in adulthood—the importance of childhood and parental obesity. New England Journal of Medicine 337(13):926-927.
Bravo, J., V. Villarreal, R. Hervas, and G. Urzaiz. 2012. Using a communication model to collect measurement data through mobile devices. Sensors 12:9253-9272.
Brennan, L., S. Castro, R. C. Brownson, J. Claus, and C. T. Orleans. 2011. Accelerating evidence reviews and broadening evidence standards to identify effective, promising, and emerging policy and environmental strategies for prevention of childhood obesity. Annual Review of Public Health 32:199-223.
Briss, P. A., R. C. Brownson, J. E. Fielding, and S. Zaza. 2004. Developing and using the guide to community preventive services: Lessons learned about evidence-based public health. Annual Review of Public Health 25:281-302.
Brownson, R. C., C. M. Hoehner, K. Day, A. Forsyth, and J. F. Sallis. 2009. Measuring the built environment for physical activity: State of the science. American Journal of Preventive Medicine 36(4 Suppl):S99-S123, e112.
Brownson, R. C., G. A. Colditz, and E. K. Proctor, eds. 2012. Dissemination and implementation research in health: Translating science to practice. New York: Oxford University Press.
Campbell, D. T., and J. C. Stanley. 1966. Experimental and quasi-experimental designs for research. Chicago, IL: Rand McNally.
Casazza, K., and D. B. Allison. 2012. Stagnation in the clinical, community, and public health domain of obesity: The need for probative research. Clinical Obesity 2(3/4):83-85.
CDC (Centers for Disease Control and Prevention). 2007. Best practices for comprehensive tobacco control programs—October 2007. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health.
Chriqui, J. F., J. C. O’Connor, and F. J. Chaloupka. 2011. What gets measured, gets changed: Evaluating law and policy for maximum impact. Journal of Law, Medicine and Ethics 39(Suppl 1):21-26.
Chriqui, J. F., D. R. Taber, S. J. Slater, L. Turner, K. M. Lowrey, and F. J. Chaloupka. 2012. The impact of state safe routes to school-related laws on active travel to school policies and practices in U.S. elementary schools. Health Place 18(1):8-15.
Clarke, C. E., J. Niederdeppe, and H. C. Lundell. 2012. Narratives and images used by public communication campaigns addressing social determinants of health and health disparities. International Journal of Environmental Research and Public Health 9(12):4254-4277.
Colditz, G. A., K. Y. Wolin, and S. Gehlert. 2012. Applying what we know to accelerate cancer prevention. Science Translational Medicine 4(127):127rv.
Dorsey, R., and G. Graham. 2011. New HHS data standards for race, ethnicity, sex, primary language, and disability status. Journal of the American Medical Association 306(21):2378-2379.
Eisenberg, M. E., D. Neumark-Sztainer, and M. Story. 2003. Associations of weight-based teasing and emotional well-being among adolescents. Archives of Pediatrics and Adolescent Medicine 157(8):733-738.
Eriksen, M. 2004. Lessons learned from public health efforts and their relevance to preventing childhood obesity. Appendix D. In Preventing childhood obesity: Health in the balance, edited by IOM (Institute of Medicine). Washington, DC: The National Academies Press. Pp. 343-375.
Estruch, R., E. Ros, J. Salas-Salvado, M. I. Covas, D. Corella, F. Aros, E. Gomez-Gracia, V. Ruiz-Gutierrez, M. Fiol, J. Lapetra, R. M. Lamuela-Raventos, L. Serra-Majem, X. Pinto, J. Basora, M. A. Munoz, J. V. Sorli, J. A. Martinez, M. A. Martinez-Gonzalez, and PREDIMED Study Investigators. 2013. Primary prevention of cardiovascular disease with a Mediterranean diet. New England Journal of Medicine 368(14):1279-1290.
Eyler, A. A., L. Nguyen, J. Kong, Y. Yan, and R. Brownson. 2012. Patterns and predictors of enactment of state childhood obesity legislation in the United States: 2006-2009. American Journal of Public Health 102(12):2294-2302.
Farrelly, M. C., K. C. Davis, M. L. Haviland, P. Messeri, and C. G. Healton. 2005. Evidence of a dose-response relationship between “Truth” antismoking ads and youth smoking prevalence. American Journal of Public Health 95(3):425-431.
Farrelly, M. C., K. C. Davis, J. Duke, and P. Messeri. 2009. Sustaining “truth”: Changes in youth tobacco attitudes and smoking intentions after 3 years of a national antismoking campaign. Health Education Research 24(1):42-48.
Fishbein, M., and I. Ajzen. 2009. Predicting and changing behavior. New York: Psychology Press, Taylore & Francis Group.
Flegal, K. M., M. D. Carroll, B. K. Kit, and C. L. Ogden. 2012. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. Journal of the American Medical Association 307(5):491-497.
Flegal, K. M., B. K. Kit, H. Orpana, and B. I. Graubard. 2013. Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. Journal of the American Medical Association 309(1):71-82.
Frank, L. D., B. E. Saelens, J. Chapman, J. F. Sallis, J. Kerr, K. Glanz, S. C. Couch, V. Learnihan, C. Zhou, T. Colburn, and K. L. Cain. 2012. Objective assessment of obesogenic environments in youth: Geographic information system methods and spatial findings from the Neighborhood Impact on Kids Study. American Journal of Preventive Medicine 42(5):e47-e55.
Freedman, D. S., W. H. Dietz, S. R. Srinivasan, and G. S. Berenson. 1999. The relation of overweight to cardiovascular risk factors among children and adolescents: The Bogalusa Heart Study. Pediatrics 103(6 Pt 1):1175-1182.
Freudenberg, N., S. P. Bradley, and M. Serrano. 2009. Public health campaigns to change industry practices that damage health: An analysis of 12 case studies. Health Education and Behavior 36(2):230-249.
Gaglio, B., and R. Glasgow. 2012. Evaluation approaches for dissemination and implementation research. In Dissemination and implementation research in health: Translating science to practice, edited by R. C. Brownson, G. A. Colditz, and E. K. Proctor. New York: Oxford University Press. Pp. 327-356.
Garfield, S. A., S. Malozowski, M. H. Chin, K. M. Narayan, R. E. Glasgow, L. W. Green, R. G. Hiss, and H. M. Krumholz. 2003. Considerations for diabetes translational research in real-world settings. Diabetes Care 26(9):2670-2674.
German, R. R., L. M. Lee, J. M. Horan, R. L. Milstein, C. A. Pertowski, and M. N. Waller. 2001. Updated guidelines for evaluating public health surveillance systems: Recommendations from the guidelines working group. MMWR Recommendations and Reports 50(RR-13):1-35; quiz CE31-CE37.
Glasgow, R. E., T. M. Vogt, and S. M. Boles. 1999. Evaluating the public health impact of health promotion interventions: The RE-AIM framework. American Journal of Public Health 89(9):1322-1327.
Goodman, R. A., P. L. Remington, and D. N. Klaucke. 2000. Communicating information for action with the public health system. In Principles and practice of public health surveillance, edited by S. M. Teutsch and R. E. Churchill. New York: Oxford University Press. Pp. 168-175.
Green, L. W. 2001. From research to “best practices” in other settings and populations. American Journal of Health Behavior 25(3):165-178.
Green, L. W., and R. E. Glasgow. 2006. Evaluating the relevance, generalization, and applicability of research: Issues in external validation and translation methodology. Evaluation and the Health Professions 29(1):126-153.
Green, L. W., R. W. Wilson, and K. G. Bauer. 1983. Data requirements to measure progress on the objectives for the nation in health promotion and disease prevention. American Journal of Public Health 73(1):18-24.
Green, L. W., R. E. Glasgow, D. Atkins, and K. Stange. 2009. Making evidence from research more relevant, useful, and actionable in policy, program planning, and practice: Slips “twixt cup and lip.” American Journal of Preventive Medicine 37(6 Suppl 1):S187-S191.
Hallal, P. C., L. B. Andersen, F. C. Bull, R. Guthold, W. Haskell, and U. Ekelund. 2012. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet 380(9838):247-257.
Hammond, R. A., and R. Levine. 2010. The economic impact of obesity in the United States. Diabetes, Metabolic Syndrome, and Obesity: Targets and Therapy 3:285-295.
Howard, C. 2012 (December 15). The big picture. The world is getting wider, says Charlotte Howard. What can be done about it? The Economist.
Huhman, M., and C. D. Patnode. 2013. Communities leveraging the assets of a national social marketing campaign: Experiences with VERB™. It’s what you do! In Advances in communication research to reduce childhood obesity, edited by J. D. Williams, K. E. Pasch, and C. A. Collins. New York: Springer Science+Business Media. P. 439.
Huhman, M. E., L. D. Potter, M. J. Nolin, A. Piesse, D. R. Judkins, S. W. Banspach, and F. L. Wong. 2010. The influence of the VERB campaign on children’s physical activity in 2002 to 2006. American Journal of Public Health 100(4):638-645.
IOM (Institute of Medicine). 1997. Linking research and public health practice: A review of CDC’s program of centers for research and demonstration of health promotion and disease prevention. Washington, DC: National Academy Press.
IOM. 2004. Preventing childhood obesity: Health in the balance. Washington, DC: The National Academies Press.
IOM. 2007. Progress in preventing childhood obesity: How do we measure up? Washington, DC: The National Academies Press.
IOM. 2010a. Bridging the evidence gap in obesity prevention: A framework to inform decision making. Washington, DC: The National Academies Press.
IOM. 2010b. For the public’s health: The role of measurement in action and accountability. Washington, DC: The National Academies Press.
IOM. 2012a. Accelerating progress in obesity prevention: Solving the weight of the nation. Washington, DC: The National Academies Press.
IOM. 2012b. An integrated framework for assessing the value of community-based prevention. Washington, DC: The National Academies Press.
Isaacs, S. L., and S. A. Schroeder. 2001. Where the public good prevailed. Lessons from success stories in health. American Prospect. June 4.
Jacobson, D. M., and D. Lotstein. 2013. Performance improvement: Using rapid-cycle improvement techniques to improve public health services. In Public health practice: What works, edited by J. E. Fielding and S. M. Teutsch. New York: Oxford University Press. Chapter 7.
Keith, S. W., D. T. Redden, P. T. Katzmarzyk, M. M. Boggiano, E. C. Hanlon, R. M. Benca, D. Ruden, A. Pietrobelli, J. L. Barger, K. R. Fontaine, C. Wang, L. J. Aronne, S. M. Wright, M. Baskin, N. V. Dhurandhar, M. C. Lijoi, C. M. Grilo, M. DeLuca, A. O. Westfall, and D. B. Allison. 2006. Putative contributors to the secular increase in obesity: Exploring the roads less traveled. International Journal of Obesity (London) 30(11):1585-1594.
Kerr, J., S. Duncan, and J. Schipperijn. 2011. Using global positioning systems in health research: A practical approach to data collection and processing. American Journal of Preventive Medicine 41(5):532-540.
Knowler, W. C., E. Barrett-Connor, S. E. Fowler, R. F. Hamman, J. M. Lachin, E. A. Walker, D. M. Nathan, and Diabetes Prevention Program Research Group. 2002. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New England Journal of Medicine 346(6):393-403.
Koh, H. K., G. Graham, and S. A. Glied. 2011a. Reducing racial and ethnic disparities: The action plan from the Department of Health and Human Services. Health Affairs 30(10):1822-1829.
Koh, H. K., J. J. Piotrowski, S. Kumanyika, and J. E. Fielding. 2011b. Healthy People: A 2020 vision for the social determinants approach. Health Education and Behavior 38:551-557.
Kottke, T. E., L. I. Solberg, A. F. Nelson, D. W. Belcher, W. Caplan, L. W. Green, E. Lydick, D. J. Magid, S. J. Rolnick, and S. H. Woolf. 2008. Optimizing practice through research: A new perspective to solve an old problem. Annals of Family Medicine 6(5):459-462.
Langmuir, A. D. 1963. The surveillance of communicable diseases of national importance. New England Journal of Medicine 268:182-192.
Lee, L. M., S. M. Teutsch, S. B. Thacker, and M. E. St. Louis, eds. 2010. Principles & practice of public health surveillance. 3rd ed. New York: Oxford University Press.
Maibach, E. W., L. C. Abroms, and M. Marosits. 2007. Communication and marketing as tools to cultivate the public’s health: A proposed “people and places” framework. BMC Public Health 7:88.
Majumdar, S. R., and S. B. Soumerai. 2009. The unhealthy state of health policy research. Health Affairs 28(5):w900-w908.
McKinnon, R. A., J. Reedy, M. A. Morrissette, L. A. Lytle, and A. L. Yaroch. 2009. Measures of the food environment: A compilation of the literature, 1990-2007. American Journal of Preventive Medicine 36(4 Suppl):S124-S133.
McQueen, D. V., and P. Puska, eds. 2003. Global behavioral risk factor surveillance. New York: Klewer Academic/Plenum Publishers.
Mercer, S. L., B. J. DeVinney, L. J. Fine, L. W. Green, and D. Dougherty. 2007. Study designs for effectiveness and translation research: Identifying trade-offs. American Journal of Preventive Medicine 33(2):139-154.
Mercer, S. L., L. Kettel Khan, L. W. Green, A. C. Rosenthal, R. Nathan, C. G. Husten, and W. H. Dietz. 2010. Drawing possible lessons for obesity prevention and control from the tobacco control experience. In Obesity epidemiology: From aetiology to public health, edited by D. Crawford, R. W. Jeffery, K. Ball, and J. Brug. Oxford Scholarship Online.
Mittman, B. S. 2012. Implementation science in health care. In Dissemination and implementation research in health: Translating science to practice, edited by R. C. Brownson, G. A. Colditz, E. K. Proctor. New York: Oxford University Press. Pp. 400-418.
Morrison, R. M., L. Mancino, and J. N. Vairyam. 2011. Will calorie labeling in restaurants make a difference? Amber Waves 9(1):10-17.
Noar, S. M. 2006. A 10-year retrospective of research in health mass media campaigns: Where do we go from here? Journal of Health Communication 11(1):21-42.
Ogden, C. L., M. D. Carroll, B. K. Kit, and K. M. Flegal. 2012a. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. Journal of the American Medical Association 307(5):483-490.
Ogden, C. L., M. D. Carroll, B. K. Kit, and K. M. Flegal. 2012b. Prevalence of obesity in the United States, 2009-2010. NCHS Data Brief (82):1-8.
Ottoson, J. M., and D. H. Wilson. 2003. Did they use it? Beyond the collection of surveillance information. In Global behavioral risk factor surveillance, edited by D. McQueen and P. Puska. New York: Kluwer Academic/Plenum Publishers. Pp. 119-131.
Ottoson, J. M., L. W. Green, W. L. Beery, S. K. Senter, C. L. Cahill, D. C. Pearson, H. P. Greenwald, R. Hamre, and L. Leviton. 2009. Policy-contribution assessment and field-building analysis of the Robert Wood Johnson Foundations Active Living Research Program. American Journal of Preventive Medicine 36(2 Suppl):S34-S43.
Ottoson, J. M., A. G. Ramirez, L. W. Green, and K. J. Gallion. 2013. Exploring potential research contributions to policy: The Salud America! Experience. American Journal of Preventive Medicine 44(3 Suppl 3):S282-S289.
Perna, F. M., A. Oh, J. F. Chriqui, L. C. Masse, A. A. Atienza, L. Nebeling, T. Agurs-Collins, R. P. Moser, and K. W. Dodd. 2012. The association of state law to physical education time allocation in US public schools. American Journal of Public Health 102(8):1594-1599.
Rogers, E. M. 2003. Diffusion of innovations. 5th ed. New York: The Free Press.
Rosen, L., O. Manor, D. Engelhard, and D. Zucker. 2006. In defense of the randomized controlled trial for health promotion research. American Journal of Public Health 96(7):1181-1186.
Rutten, A., R. Rzewnicki, H. Ziemainz, W. T. M. Ooijendij, F. Schena, T. Stahl, Y. Vanden Auweele, and J. Welshman. 2003. Towards a European health monitoring system. Results of a pilot study on physical activity. In Global behavioral risk factor surveillance, edited by D. McQueen and P. Puska. New York: Kluwer Academic/Plenum Publishers. Pp. 73-93.
Serdula, M. K., D. Ivery, R. J. Coates, D. S. Freedman, D. F. Williamson, and T. Byers. 1993. Do obese children become obese adults? A review of the literature. Preventive Medicine 22(2):167-177.
Shadish, W. R., T. D. Cook, and D. T. Campbell. 2002. Experimental and quasi-experimental designs for generalized causal inference. 2nd ed. Boston, MA: Houghton Mifflin.
Shea, M. K., D. K. Houston, B. J. Nicklas, S. P. Messier, C. C. Davis, M. E. Miller, T. B. Harris, D. W. Kitzman, K. Kennedy, and S. B. Kritchevsky. 2010. The effect of randomization to weight loss on total mortality in older overweight and obese adults: The adapt study. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 65(5):519-525.
Snyder, L. B., and M. A. Hamilton. 2002. Meta-analysis of U.S. health campaign effects on behavior: Emphasize enforcement, exposure, and new information, and beware the secular trend In Public health communications: Evidence for behavior change, edited by R. C. Hornik. Mahwah, NJ: Lawrence Erlbaum Associates, Inc. Pp. 357-383.
Solar, O., and A. Irwin. 2010. A conceptual framework for action on social determinants of health. Social determinants of health discussion paper 2 (policy and practice). Geneva: World Health Organization.
Sumithran, P., L. A. Prendergast, E. Delbridge, K. Purcell, A. Shulkes, A. Kriketos, and J. Proietto. 2011. Long-term persistence of hormonal adaptations to weight loss. New England Journal of Medicine 365(17):1597-1604.
Taber, D. R., J. F. Chriqui, and F. J. Chaloupka. 2012. Differences in nutrient intake associated with state laws regarding fat, sugar, and caloric content of competitive foods. Archives of Pediatrics and Adolescent Medicine 166(5):452-458.
Teutsch, S. M., and R. E. Churchill, eds. 2000. Principles and practice of public health surveillance. 2nd ed. New York: Oxford University Press.
Thacker, S. B. 2007. Public health surveillance and the prevention of injuries in sports: What gets measured gets done. Journal of Athletic Training 42(2):171-172.
Thacker, S. B., and R. L. Berkelman. 1988. Public health surveillance in the United States. Epidemiologic Reviews 10:164-190.
Thacker, S. B., and D. F. Stroup. 2006. Public health surveillance. In Applied epidemiology: Theory to practice, edited by R. C. Brownson and D. B. Petitti. New York: Oxford University Press. Pp. 30-67.
Thacker, S. B., R. L. Berkelman, and D. F. Stroup. 1989. The science of public health surveillance. Journal of Public Health Policy 10(2):187-203.
Thompson, D. R., E. Obarzanek, D. L. Franko, B. A. Barton, J. Morrison, F. M. Biro, S. R. Daniels, and R. H. Striegel-Moore. 2007. Childhood overweight and cardiovascular disease risk factors: The National Heart, Lung, and Blood Institute Growth and Health Study. Journal of Pediatrics 150(1):18-25.
Turner, L., J. F. Chriqui, and F. J. Chaloupka. 2012. Healthier fundraising in U.S. elementary schools: Associations between policies at the state, district, and school levels. PLoS ONE 7(11):e49890.
Valente, T. W., and W. P. Saba. 2001. Campaign exposure and interpersonal communication as factors in contraceptive use in Bolivia. Journal of Health Communication 6(4):303-322.
Ward, J. W., and C. Warren. 2006. Silent victories: The history and practice of public health in twentieth-century America. Oxford: Oxford University Press.
Warren, C. W., L. Riley, S. Asma, M. P. Eriksen, L. Green, C. Blanton, C. Loo, S. Batchelor, and D. Yach. 2000. Tobacco use by youth: A surveillance report from the global youth tobacco survey project. Bulletin of the World Health Organization 78(7):868-876.
Worden, J. K., B. S. Flynn, B. M. Geller, M. Chen, L. G. Shelton, R. H. Secker-Walker, D. S. Solomon, L. J. Solomon, S. Couchey, and M. C. Costanza. 1988. Development of a smoking prevention mass media program using diagnostic and formative research. Preventive Medicine 17(5):531-558.




























