Disasters such as Hurricane Katrina, Hurricane Sandy, the earthquake in Haiti, and the tornado in Joplin, Missouri, have served as vivid reminders of the challenge of providing health care when demand for health care services sharply rises and places overwhelming demand on resources and medical staff, all in the midst of infrastructure damage or destruction. Severe pandemic influenza or catastrophic terrorist incidents—such as the detonation of a nuclear device or the release of a bioterrorism agent—have the potential to place even greater demands on the health system.
Planning to provide care in these types of overwhelming situations can help health care organizations and providers, supported by the entire emergency response system, take proactive steps that enable them to provide patients with the level of care they would usually receive, or care that is functionally equivalent, for as long as possible. In catastrophic disasters, however, these proactive steps may become insufficient: health care resources may become so scarce that reallocation decisions are needed, staff may have to practice outside of their normal scope of practice, and the focus of patient care may need to switch to promoting benefits to the population over benefits to individuals. In this austere situation, planning is necessary to avoid greater illness, injury, and death by enabling more effective use of the limited resources through fair, just, and equitable processes for making decisions about who should receive treatments when there are not enough resources to provide patients with the level of care they would usually receive. Recent incidents such as the Boston bombing and the tornado in Moore, Oklahoma, have demonstrated the value of notification, planning, and exercising in avoiding what could have been far greater illness, injury, and death. The response to these incidents also emphasized the importance of a network of resources to absorb the demands of major incidents.
Decision making about the level of care that can be provided during a disaster is important and complex. Health care organizations and providers should not prematurely move to providing care that presents a risk of a compromised outcome to patients, but at the same time they should take proactive steps to use resources carefully if demand is expected to surge and/or resource shortages are anticipated. The amount of information available in health care today is enormous, and expanding, and determining how to use it to inform operational decision making is both challenging and critical. Information may be incomplete and contradictory; it is collected and stored by many different entities; it can be challenging to detect or characterize an emerging event amid usual variability in large and complex sets of data; forecasting demand is difficult; and decisions must be made in a novel, urgent, dynamic, and often chaotic set of circumstances.
Over the past decade, federal, state, tribal, and local governments, the Institute of Medicine (IOM), and
other entities have embarked on developing crisis standards of care (CSC) plans and guidance. As this body of work continues to evolve, the need for guidance on how to develop indicators and triggers that aid decision making about the provision of care in disasters has been identified as a gap. Indicators are measurements or predictors of change in demand for health care service delivery or availability of resources. An example indicator could be emergency department wait time. Triggers are decision points that are based on changes in the availability of resources that require adaptations to health care services delivery along the care continuum.1 An example trigger could be emergency department wait time exceeds X hours, which would trigger a variety of response tactics such as increased staffing.
Advance planning about indicators and triggers involves considering what information about demand and resources is available across the health care spectrum (from prehospital to end-of-life care), how this information is shared and integrated, how this information drives actions, and what actions might be taken to provide the best health care possible given the situation. Because of the stress, complexity, and uncertainty inherent in a crisis situation, it is particularly important that these conversations occur in advance. Planning for indicators and triggers has to occur at the level of the specific organization, agency, or community, because it depends on the usual resources and demand. For example, a tornado that touches down in a small, rural community may automatically warrant activation of the health care organization disaster plan, whereas additional information about the size and location of the tornado may be required before making this decision in a larger community with a higher ability to absorb a surge in demand.
At the request of the Assistant Secretary for Preparedness and Response at the Department of Health and Human Services, the National Highway Traffic Safety Administration in the Department of Transportation, and the Veterans Health Administration, in the fall of 2012 the IOM convened the Committee on Crisis Standards of Care: A Toolkit for Indicators and Triggers. The task was to prepare a conversation toolkit to guide stakeholders through the process of developing indicators and triggers that may govern the transition across the continuum of care, from conventional standards of care to contingency surge response and standards of care to crisis surge response and standards of care, and back to conventional standards of care.
REPORT DESIGN AND ORGANIZATION
Chapter 1 provides background on crisis standards of care. Chapter 2 discusses key concepts, limitations, and systems-level considerations related to developing indicators and triggers. Chapters 3-9 constitute a discussion toolkit designed to help stakeholders have discussions about indicators and triggers. Chapter 3 provides the overarching framework for the toolkit and should be read by everyone. Chapters 4 through 9 are customized for each major component of the emergency response system: emergency management (Chapter 4), public health (Chapter 5), behavioral health (Chapter 6), emergency medical services (EMS) (Chapter 7), hospital and acute care (Chapter 8), and out-of-hospital care (Chapter 9).2 Because
____________________
1 “The surge capacity following a mass casualty incident falls into three basic categories, depending on the magnitude of the incident: conventional, contingency, and crisis. These categories also represent a corresponding continuum of patient care delivered during a disaster. As the imbalance increases between resource availability and demand, health care—emblematic of the health care system as a whole—maximizes conventional capacity; then moves into contingency; and, once that capacity is maximized, moves finally into crisis capacity. A crisis situation may lead to an overwhelming demand for services and result in shortages of equipment, supplies, pharmaceuticals, personnel, and other critical resources, necessitating operational adjustments” (IOM, 2012, p. 1-6)
2 The out-of-hospital care delivery system includes diverse ambulatory care environments (public, private, tribal, veterans health, military), home health and hospice, assisted living and skilled nursing, specialty care and resources, and others.
what occurs in one of the emergency response disciplines is likely to affect, or be affected by, what occurs in other components of the emergency response system, readers should read the chapter(s) specific to their discipline and also review the other chapters.
BACKGROUND ON CRISIS STANDARDS OF CARE
This report builds on two previous IOM reports on crisis standards of care: Guidance for Establishing Crisis Standards of Care for Use in Disaster Situations (2009), which presented key concepts related to CSC, and Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response (2012), which further developed an operational framework for planning for and implementing CSC. This section briefly summarizes concepts from these two reports, focusing on those that are essential to understanding the approach taken in this report.
Both reports emphasize the importance of developing indicators and triggers in CSC plans. The 2009 report described five key elements that should underlie all CSC plans:
1. A strong ethical grounding that enables a process deemed equitable and just based on its transparency, consistency, proportionality, and accountability;
2. Integrated and ongoing community and provider engagement, education, and communication;
3. The necessary legal authority and legal environment in which CSC can be ethically and optimally implemented;
4. Clear indicators, triggers, and lines of responsibility; and
5. Evidence-based clinical processes and operations.
These reports also emphasized the need to continually monitor demand and resources, and to strive to move back toward conventional care as quickly as feasible.
A Systems Approach to Catastrophic Disaster Response
Successfully responding to a catastrophic disaster will require integrated planning, coordination, cooperation, consultation, and follow-through among many response disciplines and agencies, including state and local governments, EMS, health care coalitions, health care organizations, and health care providers in the community. The 2012 report developed a systems framework for catastrophic disaster response, which includes, but is not limited to, the development and implementation of CSC plans. In this framework, ethical considerations and the legal authority and environment form the foundation that undergirds crisis standards of care planning and implementation. A number of key elements underlie the development of CSC plans, including provider engagement, community engagement, development of indicators and triggers, implementation of clinical processes, and operations. Education and information sharing are the cornerstones of the framework; together with the process of performance improvement, they support the key elements of CSC planning and enable midcourse corrections during the implementation of the framework. The systems framework has five pillars of medical surge: hospital care, public health, out-of-hospital care, emergency medical services, and emergency management and public safety. To ensure a unified disaster response, these
different components of the disaster response system need to be well integrated. The final components of the systems framework are the federal, state, tribal and territorial, and local governments, which have an overarching responsibility for the development, institution, integration, and proper execution of CSC plans, policies, protocols, and procedures.
Integrated planning within and across a tiered system of relationships among individual health care organizations, health care coalitions, and local, state, and federal governments is critical for a coordinated response and to avoid prematurely moving to a different level of response along the continuum of care that may adversely impact patient care. The Medical Surge Capacity and Capability framework outlines such a tiered system, and the 2012 IOM report integrates CSC planning and implementation into this framework (Barbera and Macintyre, 2007, 2009; IOM, 2012). As described below, the toolkit is designed to support discussions at all tiers in this system and among all components of the emergency response system.
Continuum of Care: Conventional, Contingency, and Crisis
Rather than just focusing on the most extreme circumstances, the committee that authored the 2009 and 2012 reports, as well as the current committee, envision surge capacity as occurring along a continuum based on resource availability and demand for health care services. One end of this continuum is defined by conventional care, which describes services that are provided in health care organizations on a routine or daily basis. In the middle of the continuum, contingency care provides care that is functionally equivalent to usual patient care (e.g., one medication substituted for another that is not usually used in that circumstance but provides the same or a similar effect). At the far end of the continuum is crisis care, when the best possible care is provided to the population of patients as a whole because of the very limited resources available. Significant changes are made in the methods and locations of care delivery, and decision making shifts from patient-centered to population-centered outcomes.
It is important to recognize that transitions along the continuum of care do not always occur abruptly. For example, a slow-onset incident such as an influenza pandemic may result in a relatively gradual transition through the continuum, while an improvised nuclear device detonation near a downtown medical center may require an immediate transition to crisis care. Along this continuum, indicators demonstrate the potential for movement toward a different level of care: from conventional to contingency, from contingency to crisis, or from crisis back toward conventional. The triggers are decision points, based on changes in the availability of resources, which require adaptations to health care services delivery along the care continuum. In this report, triggers that lead to the implementation of crisis standards of care have been specifically designated as crisis care triggers because this is the point at which resource allocation strategies focus on the community rather than the individual, carrying the greatest potential adverse impact to patient outcomes; the implementation of crisis standards of care at this point aims to minimize adverse patient outcomes to the extent possible given the circumstances and available resources.
INDICATORS AND TRIGGERS
Indicators and triggers represent the information and actions taken at specific thresholds that guide incident recognition, response, and recovery. When specific indicators cross a threshold that is recognized by the com-
munity to require action, this represents a trigger point, with actions determined by community plans. These include activation of a general disaster plan, which often occurs at the threshold between conventional and contingency care, or activation of CSC plans, which would occur at the threshold between contingency and crisis care.
Developing Useful Indicators and Triggers
It is attractive to look at many of the metrics available in health care today and consider their use as indicators. However, multiple factors may make data monitoring less useful than it originally appears, and it can be complex to detect actionable information or an evolving event amid usual variability in large sets of data. Specific numeric thresholds for indicators and triggers are concrete and attractive because they are easily recognized. For certain situations they are relatively easy to develop (e.g., a single case of anthrax), but for many situations the community/agency actions are not as clear-cut or may require significant data analysis to determine where a reasonable threshold may be established (e.g., multiple cases of diarrheal illness in a community).
The report outlines key concepts related to indicators, data, triggers, and tactics that will help inform decisions about how best to develop and use them. Depending on the nature of the indicator and data, different types of triggers and tactics may be required.
Actionable and predictive indicators: Actionable indicators can be impacted through actions taken within an organization or a component of the emergency response system (e.g., a hospital detecting high patient census). Predictive indicators cannot be impacted through actions taken within a health care organization or other component of the emergency response system (e.g., a hospital receiving notification that a pandemic virus has been detected may lead to the implementation of response tactics, but the indicator is considered predictive because the hospital’s actions cannot impact or reverse the virus having been detected).
Indicators are comprised of data, broadly understood to include measurements, predictions, or events (for example, a 911 call or witnessing a tornado). Data may be certain or uncertain: Certain data require minimal validation or analysis (e.g., temperature, emergency department wait times), allowing rapid decision making and lending themselves more readily to the assignment of discrete thresholds at which a trigger is implemented. Uncertain data require interpretation to determine the appropriate response; triggers based on uncertain data may involve expert analysis before action. An important note is that decision making in crises often requires acting on uncertain information. The fact that information is uncertain means that additional assessment and analysis may be required, but this should not impede the ability to plan and act.
Scripted and non-scripted triggers: Scripted triggers are decision points that require minimal analysis and lead to scripted tactics. Non-scripted triggers are decision points that require analysis and lead to implementation of non-scripted tactics.
Scripted and non-scripted tactics: Scripted tactics are a predefined action or set of actions that are easily and quickly implemented by frontline personnel. Non-scripted tactics vary according to the situation; they are based on analysis of multiple inputs, recommendations, and, in certain circumstances, previous experience, and are tailored to the requirements of the situation.
Actionable indicators comprised of certain data can often appropriately lead to scripted triggers and tactics; examples of this would be a hospital trauma team activation or a first alarm response to a report of
fire in a building. With some exceptions, predictive indicators, usually comprised of uncertain data, most appropriately lead to non-scripted triggers and tactics. An example would be the decision-making process leading to the declaration of an influenza pandemic. Regardless of the certainty of the data, each pathway requires a “filter” process in which information is analyzed, assessed, and verified. With certain data, this filter process may be minimal. These concepts are illustrated in Figure S-1.
When developing plans for indicators and triggers, stakeholders should keep in mind the following types of limitations and issues associated with indicators: the accuracy of the data being used as an indicator; naming conventions and “rules of reporting,” particularly when indicators are being shared among multiple entities (e.g., to determine how many intensive care unit beds are available in a city, it will be important to know whether hospitals are counting and reporting only staffed beds or currently unstaffed beds as well); the dynamic environment in which data are reported; and the challenge of detecting evolving changes amid usual data variability. When developing plans for indicators and triggers, the time required for an entity to report data may detract from response efforts. Automating the information exchange, where possible,
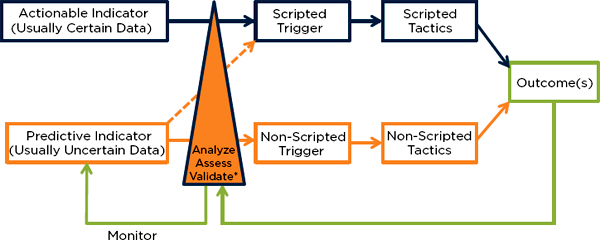
FIGURE S-1
Relationships among indicators, triggers, and tactics.
*Interpret indicators, other available data, impact, and resources—this may occur over minutes (e.g., developing an initial response to a fire) or days (e.g., developing a response to the detection of a novel virus).
NOTE: In this figure, an indicator is comprised of either certain data, sufficient to activate a trigger, or uncertain data, which require additional analysis prior to action. It is important to note several characteristics that may be helpful in shaping planning:
• All actions require at least minimal validation of data or processing of data—the triangle at the center of the figure shows the relative amount of processing expertise and time required (i.e., the thicker base of the triangle represents more processing required).
• Indicators that are actionable typically involve certain data that can lead to scripted triggers that staff can initiate without further analysis (e.g., if a mass casualty incident involves >20 victims, the mass casualty incident [MCI] plan is activated).
• Indicators that are predictive (e.g., epidemiology data) typically involve uncertain data that require interpretation prior to “trigger” action.
• The smaller the community or the fewer resources available, the more certain and scripted the triggers can become.
• The larger the community (or state/national level) and the more resources available, the less certain the data become as they do not reflect significant variability in resource availability at the local level—thus, the more expert interpretation is often required prior to action (e.g., state level data may reveal available beds, but select facilities and/or jurisdictions may be far beyond conventional capacity).
• The larger or more direct the impact, the more certain the data (e.g., when the tornado hits your hospital, there is no question you should trigger your disaster plan and implement contingency or crisis care tactics as required).
• Scripted triggers are quickly implemented by frontline personnel with minimal analysis—the disadvantage is that the scripted tactics may commit too few or too many resources to the incident (e.g., first alarm response to report of a fire in a building).
• Non-scripted triggers are based on expert analysis rather than a specific threshold and allow implementation of tactics that are tailored to the situation (non-scripted tactics). Trigger decisions may be based on expertise, experience, indicator(s) interpretation, etc., and may be made quickly or take significant time based on the information available.
• Ongoing monitoring and additional analysis of indicators will help assess the current situation and the impact of the tactics.
is valuable. To avoid making unnecessary requests for information, an important consideration is how the information will drive specific operational decisions and actions.
Return to Conventional Care
As conditions improve, it is important to watch for indicators that the system can move back toward conventional care status. These indicators may be incident specific and not included in an agency’s usual data or list of indicators. Examples of these indicators may include decreasing call or emergency department volumes, restored systems (utilities, etc.), and decreasing use of hotlines and dispensing sites. These indicators may fluctuate over the course of a disaster response, so return to conventional may be temporary. Return to conventional care status is not the same as recovery, although it may be an indicator of transition into the recovery phase. Recovery implies a more permanent return to normal operating status and the restoration of the impacted systems and communities.
Systems-Level Considerations
Integrated planning among all major components of the emergency response system is critical for an effective and coordinated response. Integrated planning for indicators and triggers also needs to occur among these components of the system, both horizontally and vertically. In addition to thinking about limitations and issues inherently associated with the indicators themselves, it is important to think about how the information will be shared and synthesized and used by different components of the emergency response system.
DISCUSSION TOOLKIT
The objective of the toolkit is to facilitate discussions about indicators and triggers within and across health care organizations, health care coalitions, emergency response agencies, and jurisdictions. Specifically, the toolkit focuses on indicators and triggers that guide transitions along the continuum of care, from conventional standards of care to contingency surge response and standards of care to crisis surge response and standards of care, and back to conventional standards of care. Agencies and stakeholders should understand what information is available to support operational decision making in this kind of situation, and what triggers may automatically activate particular responses or may require expert analysis prior to a decision. This toolkit is intended to help agencies and stakeholders have these discussions. The outcomes of these discussions can be used to drive policy, planning, and exercises.
Toolkit Design
The discussion toolkit is structured around two scenarios (one slow-onset and one no-notice), a series of key questions for discussion, and a set of example tables. The example indicators and triggers encompass both clinical and administrative domains.
Chapter 3 provides the introduction to the toolkit and material relevant to the entire emergency response system, including the scenarios, a set of key overarching questions, and example indicators, triggers,
and tactics related to worker functional capacity, an important crosscutting issue for all components of the emergency response system. The second part of the toolkit is provided in Chapters 4 through 9, which are each aimed at a key component of the emergency response system: emergency management, public health, behavioral health, EMS, hospital and acute care, and out-of-hospital care. These chapters provide additional questions intended to help participants drill down on the key issues for their own discipline. These chapters also contain tables that provide example indicators, triggers, and tactics across the continuum of care, followed by a blank table for participants to complete. The scenarios, questions, and example table are intended to help facilitate discussion that would result in completing the blank table. The examples provided are not exhaustive and are just intended as examples. The tables need to be discussed and developed at the organization, agency, and jurisdiction levels because of variability in daily resource availability, demand, infrastructure, information sources, and actions that may be taken.
This toolkit has been designed to be scalable for use at multiple levels. Discussions need to occur at the facility, organization, and agency levels to reflect the level of detail about organizational capabilities needed for operational decision making. Discussions also need to occur at higher tiers of the emergency response system to ensure regional consistency and integration; it is important to understand the situation in other organizations and components of the emergency response system to avoid prematurely moving to a more austere level of care when resources might be available elsewhere.
For communities that have already begun CSC planning, this toolkit can be used to develop or expand the indicator and trigger components of their plan. For communities that are beginning the CSC planning process, the use of this toolkit—and the exploration of community-, regional-, and state-derived indicators, triggers, and the process by which actions are then taken—would be an excellent place to start this important work. The toolkit discussions will provide much of the needed detailed understanding about what it means to transition away from conventional response and toward the delivery of health care that occurs in contingency conditions, or in worst cases, under crisis conditions. For additional guidance on the development of CSC plans, including planning milestones and templates, see the IOM’s 2012 report.
These discussions will provide a foundation for future policy work, planning, and exercises related to CSC planning and disaster planning in general. The indicators and triggers developed for CSC planning purposes are subject to change over time as planned resources become more or less available or circumstances change. It will be important to regularly review and update CSC plans, including indicators and triggers.
REFERENCES
Barbera, J. A., and A. G. Macintyre. 2007. Medical surge capacity and capability: A management system for integrating medical and health resources during large-scale emergencies, 2nd ed. Washington, DC: U.S. Department of Health and Human Services. http://www.phe.gov/preparedness/planning/mscc/handbook/documents/mscc080626.pdf (accessed April 3, 2013).
Barbera, J. A., and A. G. Macintyre. 2009. Medical surge capacity and capability: The healthcare coalition in emergency response and recovery. Washington, DC: U.S. Department of Health and Human Services. http://www.phe.gov/preparedness/planning/mscc/documents/mscctier2jan2010.pdf (accessed May 14, 2013).
IOM (Institute of Medicine). 2009. Guidance for establishing crisis standards of care for use in disaster situations: A letter report. Washington, DC: The National Academies Press.
IOM. 2012. Crisis standards of care: A systems framework for catastrophic disaster response. Washington, DC: The National Academies Press.










