Global Perspectives on Transmission and Infection Control
Key Messagesa
• Undergirding efforts at effective infection control is a comprehensive approach that includes redesigning health care facilities and implementing rapid diagnosis and early treatment of DR TB.
• The focus of infection control in China has been on engineering controls and personal protective equipment as opposed to administrative and managerial practices.
• The spread of TB among health care workers points to the need for continued strengthening of infection control programs.
• Although infection control programs can be expensive, they are much less costly than treating people with DR TB.
__________________
a Identified by individual speakers.
Participants in the workshop focused substantial attention on the potential for MDR TB to spread from person to person. Speakers discussed general findings on the transmissibility of DR TB and implications for infection control, as well as specific issues in the context of individual countries, particularly relating to the need to protect health care workers from infection. Many speakers and participants recognized in their remarks a common theme echoed throughout the workshop, that MDR TB is acquired more often by transmission than by incomplete or inappropriate treatment.
THE VALUE OF GENOTYPE MAPPING1
In the past, most of the emphasis on DR TB has been on resistance acquired through incomplete or inappropriate treatment, said Neel R. Gandhi, Associate Professor, Departments of Epidemiology, Global Health, and Medicine, Rollins School of Public Health, Emory University. As a result, TB programs have concentrated on understanding how best to keep individuals from developing resistance through multidrug therapy, directly observed therapy, and other adherence measures. However, individuals also can become infected with DR TB through transmission from another person. This primary, or transmitted, resistance can occur even in individuals who have never been on anti-TB therapy.
The interventions used to treat acquired and transmitted resistance are very different, Gandhi noted. With acquired resistance, the way to prevent additional DR TB is to strengthen the drug-susceptible TB treatment program. With transmitted resistance, transmission needs to be prevented through infection control programs.
In the past, it has commonly been believed that the same mutations that create resistance to medications will exert a fitness cost, making these strains less likely to propagate and generate clinical disease through transmission. According to this perspective, existing drug-resistant strains eventually will die out, and thus the focus should be on ensuring that new drug-resistant strains are not being generated. The advent of genotyping methods in the 1990s enabled a much better understanding of transmission. Genotyping allowed assessment of whether patients had very similar drug-resistant strains, and in those cases one could conclude that transmission likely occurred between them.
Also in the 1990s, high-profile outbreaks in the United States and in Western Europe, and somewhat later in other parts of the world, demonstrated that DR TB strains can be transmitted quite efficiently. These outbreaks of transmitted strains occurred most commonly in congregate settings, such as hospitals. Most TB control programs in hospitals at the time relied on smear microscopy, which cannot reveal drug susceptibility or resistance; the result was delays in diagnosing drug resistance. Delays in performing culture and DST added more time to the process. As a consequence, many patients were not diagnosed as having MDR TB until weeks or months after they had arrived at an institution, during which time many other patients and workers may have been exposed to the disease.
The hospitals where many of these outbreaks occurred had few, if any, infection control measures in place. They tended to have congregate wards
__________________
1 This section is based on the presentation by Neel R. Gandhi, Associate Professor, Departments of Epidemiology, Global Health, and Medicine, Rollins School of Public Health, Emory University.
where a number of people shared the same air space with little ventilation. Even hospitals that had isolation facilities did not use them effectively. Patients were isolated only when a confirmed diagnosis was made, after weeks or months of delay. Isolation rooms also tended to be poorly maintained. Airflow studies in several facilities showed that, instead of having negative pressure to prevent air from the isolation room from spreading elsewhere, many rooms had positive pressure because of poor maintenance of the ventilation systems. When the doors were open, the air from those rooms spread into the hallway and adjacent rooms.
These conditions resulted in significant transmission to health care workers. In many settings, health care workers’ tuberculin skin test (TST) conversion rates were on the order of 30 to 60 percent. For many who developed active TB, the strains could be traced back to the outbreak strain.
As knowledge of these problems grew, significant interventions in the United States and Europe turned the tide and reduced the number of DR TB cases. But those lessons were not applied globally. Gandhi showed a picture of the Tugela Ferry, South Africa, hospital TB ward where he has worked for the past 10 years. It has congregate beds with up to 40 patients per ward. When the ward was crowded, the hospital accommodated additional patients by placing mattresses on the floor between the beds—“a scenario for widespread transmission.”
From 2005 to 2009, 516 XDR TB cases from this one hospital were diagnosed and culture confirmed. This equates to an incidence of 52 XDR TB cases per 100,000 population in that community—“astounding rates,” according to Gandhi. Genotype testing showed that more than 85 percent of these cases could be traced to a single predominant clone. Most of those patients had been exposed to 1 or more infectious XDR TB patients on the hospital’s wards, with a mean period of overlap of 18 days.
Further analysis showed that instead of a single, point-source outbreak, the XDR TB epidemic in Tugela Ferry arose as a result of multiple generations of transmission of DR TB strains. It was found that at least 5 generations of XDR TB transmission had occurred over the 2-year period 2005–2007, and other observations point to a similar phenomenon with MDR TB strains. With this mode of transmission, there are circumstances in which the number of DR TB cases can rise exponentially. In 2001, KwaZulu-Natal had only 210 MDR TB cases. By 2007, it had more than 3,000, and the number for 2012 is approximately 4,500, which, Gandhi said, is still likely to be a two- to threefold underestimate. By way of comparison, the United States had fewer than 100 MDR TB cases in a recent year.
Gandhi closed by drawing some general conclusions about genotyping in the context of MDR TB:
• Pooling of genotyping data allows identification of transmission across large geographic areas.
• Epidemiological investigation and network analysis allow better characterization of transmission relationships between clustered cases.
• Clustering can occur not just across cities and states but also across national boundaries. In a study of cases from 19 European countries, as many as 43 percent were clustered across European borders (Devaux et al., 2009). Furthermore, many of these cases actually began in Eastern Europe, Central Asia, or West Africa.
• These findings suggest that transmission is occurring not just in hospital settings but in other settings as well. For example, studies have documented transmission in households (Becerra et al., 2011; Vella et al., 2011).
Studies also have shown that people previously treated for TB who develop DR TB—historically assumed to be a sign of acquired resistance—often are instead being reinfected with drug-resistant strains through transmission. For example, a study in San Francisco looking at patients who developed resistance while on treatment found that 45 percent had an isolate completely different from their susceptible baseline isolate (Small et al., 1993). Li and colleagues (2007) found a reinfection rate of 84 percent in a study in China, and a study in South Africa, in a high-HIV-prevalence setting, found a reinfection rate of 100 percent (Andrews et al., 2007).
Beginning in 2010, WHO began estimating transmitted versus acquired cases differently, with transmitted cases now including both new TB cases and those who relapse after having had successful TB treatment. These new estimates indicate that close to three-quarters of the MDR TB cases that are estimated to arise globally are a result of transmission rather than acquired resistance (WHO, 2010). Similarly, a study released in China in 2012 found a transmission rate for MDR TB of 78 percent (Zhao et al., 2012).
Two decades of experience have definitively demonstrated that transmission plays a significant role in the development of MDR and XDR TB cases, Gandhi said. Halting transmission therefore needs to be a critical element of efforts to address the epidemic of DR TB. To this end, a comprehensive strategy is required that includes the redesign of health care facilities and rapid diagnosis and early treatment of DR TB.
Complementing Gandhi’s presentation were remarks by a speaker from China who discussed the characteristics of the hospital system in China and how patients use the system for TB care. This presentation is summarized in Box 7-1.
BOX 7-1
The Hospital System in Chinaa
According to Liang Li, Director, Administration Office, Clinical Center on Tuberculosis, China CDC; Vice-Director, Chinese Tuberculosis Society; Chief-Director, Beijing Chest Hospital, China has more than 3,000 TB dispensaries. It also has 203 TB specialty hospitals, to which general hospitals transfer identified TB patients. However, these TB hospitals are unevenly distributed, so that an outbreak in, for example, the western part of China is a much bigger problem than an outbreak where TB hospitals are more numerous.
The TB hospitals in China include a total of 6,000 doctors and 8,000 nurses, according to Li. But they have only about 300 laboratory personnel, which he described as a very small number.
TB dispensaries, or local clinics at the county or district level usually located at the site of the local China CDC, diagnose more than 60 percent of TB patients, with TB hospitals finding another 20 percent and general hospitals finding 15 percent. More than 60 percent of the TB hospitals can conduct DST and culture. However, the fact that less than 20 percent of TB dispensaries can perform these tests is problematic because of the large number of MDR TB patients in China and the large numbers that rely on the dispensary system for diagnosis.
China has eight TB hospitals that have been authorized to perform clinical trials of new drugs and recently established a National TB Clinical Trials Consortium that will involve additional TB hospitals. In addition, TB hospitals have the capacity to conduct basic and clinical research, said Li, such as a recent effort to develop new methods of MDR TB diagnosis.
__________________
a This box is based on the presentation by Liang Li, Director, Administration Office, Clinical Center on Tuberculosis, China CDC; Vice-Director, Chinese Tuberculosis Society; Chief-Director, Beijing Chest Hospital.
INFECTION CONTROL CHALLENGES FOR HEALTH CARE WORKERS IN CHINA2
Chinese hospitals tend to be large and crowded, some having between 500 and 1,000 beds, said Carol Rao, Chief of Epidemiology Section, International Emerging Infections Program, Global Disease Detection, U.S. CDC, China Office. TB cases usually present to village doctors or to gen-
__________________
2 This section is based on the presentation by Carol Rao, Chief of Epidemiology Section, International Emerging Infections Program, Global Disease Detection, U.S. CDC, China Office.
eral hospitals first, rather than specialty TB hospitals. China has national guidelines but no national policies on surveillance monitoring specifically for TB infection control.
Current infection control practices in both TB and general hospitals generally include ultraviolet germicidal irradiation (UVGI). But they do not employ the upper-room shielded ultraviolet (UV) lights used in many countries; rather, they employ unshielded UV lights that are turned on for 10 to 15 minutes after a patient leaves a room to disinfect surfaces and the air and are then turned off before another patient arrives.
TB hospitals also have increasingly established infection control departments, particularly after the SARS epidemic. N95 respirators or gauze masks are issued intermittently to the health care workers, but with little training in their use. The focus of infection control is on engineering controls and personal protective equipment, said Rao, as opposed to administrative and managerial practices.
China CDC and U.S. CDC undertook a joint project to examine the prevalence and incidence of TB infection among Chinese health care workers. At the time of the study, no accurate, representative estimates of TB infection were available for China.3 The study sought to establish a baseline against which to measure the impact of infection control, thus strengthening the commitment to infection control. The study, conducted in Inner Mongolia, also looked at the knowledge, attitudes, and practices of hospital-based health care workers in 43 health care facilities. For the study, 4,000 people completed the survey questionnaire; 2,000 of these people underwent a chest X-ray and TST; and 1,000 were administered a QFT, despite its not yet being licensed in China. Only 17 percent of participants reported ever having received a TST, and two-thirds of them said they had received the test more than 5 years ago. Among the small number who had been tested, 42 percent said the test result was positive.
In general, said Rao, people knew the right answers to questions on the knowledge, attitudes, and practices survey. They had good knowledge of how TB is transmitted and how transmission is prevented. One notable finding was the mistaken belief that cleaning tables, beds, and floors with bleach would prevent TB transmission, a misconception that was promulgated in Chinese policy documents.
Most participants said they wear a mask when they are working with a TB patient. But when asked what type of mask, only 40 percent said a respirator. Moreover, Rao noted, some may have given this answer because they knew it was correct, even if they did not always wear a respirator.
__________________
3 Previous surveys used TST, because at the time QuantiFERON-TB test (QFT) was not licensed for use in China. Moreover, the tuberculin used in China for testing was a BCG derivative and not the international standard that is used in other countries.
Of the 2,000 people who received a chest X-ray and TST, 2 percent had an X-ray consistent with TB, which, together with other signs of possible TB, led to 102 participants being suspected of having TB. But none of these people were smear-positive, which is the hallmark for diagnosing TB in Inner Mongolia.
Among the 1,000 health care workers who underwent QFT, the rate of positive results was higher in the general hospital where the testing was done than in the TB hospital. The higher prevalence in the general hospital may be the result of sick patients presenting to village doctors or general hospitals before being referred to a TB hospital. Among the risk factors for positive results were several activities associated with work tasks, such as having a coworker with TB, spending more time with patients, and the number of years spent in health care.
A follow-up a year later among the 1,000 workers who underwent QFT revealed that 12.5 percent of those who participated in the follow-up had converted to positive results over the course of the year. Among those who had a follow-up TST, the conversion rate was 9.1 percent, which translated to about 6.7 per 100 person-years. Thus, both the prevalence and incidence of TB infection in health care workers in Inner Mongolia were relatively high.
More studies are needed to measure continuing incidence and to compare these results with community infection rates, which today are unknown in Inner Mongolia, said Rao. Results from such studies could strengthen infection control, guide best practices, and ensure that policies are based on evidence.
INFECTION CONTROL CHALLENGES FOR HEALTH CARE WORKERS IN SOUTH AFRICA4
Health care workers are at increased risk of both latent and active TB (Joshi et al., 2006; Menzies et al., 2007). A study of eight public hospitals conducted in eThekwini district in KwaZulu-Natal province, the district where Durban is located, found an incidence of TB of more than 1,000 per 100,000—higher than the national incidence of TB in South Africa (Naidoo and Jinabhai, 2006). Also in Durban, a chart review of patients who had identified themselves as health care workers found that they had a five- to sixfold greater risk of MDR or XDR TB than those who had not identified themselves as health care workers (O’Donnell et al., 2010).
Carrie Tudor, Fogarty Global Health Postdoctoral Fellow, Johns Hopkins School of Nursing, University of North Carolina at Chapel Hill,
__________________
4 This section is based on the presentation by Carrie Tudor, Fogarty Global Health Postdoctoral Fellow, Johns Hopkins School of Nursing, University of North Carolina at Chapel Hill.
has been involved in a study looking at occupational risk factors for TB in KwaZulu-Natal province. In three general hospitals with specialized MDR TB wards, 1,682 health care workers were employed in 2011. After eliminating charts that had inadequate information, just more than 1,400 employee medical records were available. All of the hospitals, which ranged in size from 170 to 280 beds, had occupational health nurses, but only two had nurses who worked full-time. Only one of the occupational health nurses had postgraduate occupational health training, and there were no occupational health and safety officers at any of the hospitals. All the hospitals had full-time infection control nurses.
Each of the hospitals had recommended occupational health and infection control policies and guidelines, although the extent to which these policies and guidelines were observed varied. For example, only one hospital reported receiving good-quality N95 respirators, while the other two reported receiving fake or poor-quality N95 respirators.
In these hospitals, there are no standardized TB screening tools or guidelines for how often health care workers should be screened. In 2010, only 19 percent of the health care workers in these hospitals were screened for TB. Each hospital identified one case of active TB in 2010 through its screening efforts. Many cases were not detected until the health care worker was symptomatic and sought care.
A retrospective cohort analysis of the data collected through employee medical records compared the incidence of TB among those health care workers who worked in a TB ward and those who did not. Based on just more than 1,300 charts that included work location information, a higher percentage of those who worked in TB wards had been diagnosed with TB. But among those with DR TB, none had worked in a TB ward. Also, clinical staff were more likely than nonclinical staff to have DR TB, and those with drug-susceptible TB were more likely to be HIV positive.
Those who work in MDR wards are reportedly screened more frequently than those working in other areas of the hospitals, said Tudor. An infection control assessment of all the wards of all the hospitals revealed that infection control practices in the MDR TB wards were far superior to those in the non-MDR TB wards. Windows were always open, N95s were available and were used, and sputum samples were collected outdoors.
A multilevel mixed model was used to calculate the incidence rate ratios of TB among health care workers in the three hospitals. The incidence of TB among those working in various TB and non-TB wards of the hospitals, including pediatric wards, was higher than the average among the general population of KwaZulu-Natal, as was also the case among those who were HIV positive. Compared with the general population, the incidence rate ratio among health care workers was 1.7 to 2.5 times greater.
The researchers also compared the experiences of a sample of staff
members diagnosed with active TB between January 2006 and December 2010 and controls who worked in the same hospital but did not develop TB. The cases and controls were similar on most characteristics, including duration of employment, but cases were much more likely to be HIV positive. Also, mean household crowding was higher among cases than among controls. A slightly higher percentage of cases than controls had household TB contacts, but the difference was not significant.
The overall study of occupational health medical charts had several limitations, said Tudor:
• The charts were not always complete.
• The use of a self-report questionnaire for the case-control studies may have introduced a social desirability bias if respondents knew what responses the researchers would view in a positive light.
• The case-control study had a small sample size, and TB and HIV status were probably underreported.
An implication of this study is the need to improve regular TB screening of health care workers so as to detect cases more quickly. In addition, effective infection control measures are needed in all wards, not just in TB or MDR TB wards. And all health care workers need to receive HIV counseling and testing, which will require reducing the stigma associated with HIV and TB and alleviating concerns about confidentiality.
Tudor recommended that isoniazid preventive therapy be offered to HIV positive staff, a measure initiated in South Africa in May 2011 through occupational health clinics. HIV positive staff should be reassigned to low-risk areas when possible, although such areas are lacking in some hospitals, and the study results indicate that the MDR TB ward is a relatively safe place to work. Starting HIV positive patients and health care workers on antiretroviral therapy sooner—economics aside—might help protect the workers. Finally, symptom screening of all patients when they are admitted to the hospital for any reason could help protect both patients and workers.
INSTITUTIONAL INFECTION CONTROL IN RUSSIA5
Vladimir Oblast is a relatively small region with a population of about 1.5 million in the European part of Russia. Grigory V. Volchenkov, Vladimir Oblast TB Dispensary, Center of Excellence for TB Infection Control, described the region’s TB infection control program. This program, which
__________________
5 This section is based on the presentation by Grigory V. Volchenkov, Chief Doctor, Vladimir Oblast TB Dispensary, Center of Excellence for TB Infection Control.
involves both the civil and penitentiary sectors, was launched in 2002 in the wake of joint efforts with the WHO TB control program in the Russian Federation and with U.S. CDC in 1999.
Before the program began, occupational TB infection among health care workers was common. The average active TB notification rate for health care workers in the Vladimir Oblast TB Dispensary was 1,080 cases per 100,000 population in the 10 years before the program began (Volchenkov et al., 2004). The risk of TB among health care workers was 22 times higher than that among the residents of the surrounding area. The cross-transmission of TB and MDR TB among patients also was high (Gelmanova et al., 2007).
In 2001, a 28-year-old anesthesiologist who worked in the bronchoscopy room, where effective risk-reduction measures were lacking, died of TB. This tragic event helped motivate the dispensary to implement effective infection control measures.
In 2003, the dispensary was moved into a former children’s hospital in Vladimir. In the old facility, patients were not triaged, and those for whom smear positivity raised suspicion of drug resistance were placed with other patients in rooms that could include 18 beds. Not all staff used gauze masks; there were no upper-room open UVGI fixtures; and open windows were the only form of ventilation.
In the new facility, mechanical ventilation systems were installed in high-risk departments. Patients were separated into low-, medium-, and high-risk zones, with special signage indicating the risks. With the support of U.S. CDC, 160 upper-room UVGI fixtures were installed in the high-risk zones. And a personal respiratory protection program was implemented for high-risk staff.
The new facility housed only patients receiving effective treatment. Patients were separated based on the results of smear and DST, molecular testing not being available at the time. More recently, the facility has implemented GeneXpert devices; there are now five such devices being used for the oblast. Adoption of a diagnostic and treatment protocol using this method has reduced the risk of transmission of DR TB.
The MDR TB ward in the prison sector also was reconstructed to reduce the risk of transmission. With support from the Global Fund, an 80-bed MDR TB ward was constructed for imprisoned patients, with low-, medium-, and high-risk zones. Rooms are mechanically ventilated and have upper-room UVGI.
These interventions reduced the risk of occupational TB to a level lower than the risk of TB among the general population. During the past 4 years, no cases of occupational TB have occurred among the staff in the region overseen by Volchenkov (Figure 7-1).
In light of this success, WHO and U.S. CDC helped organize the
Vladimir Center of Excellence for TB Infection Control, with additional support from the Central TB Research Institute, Moscow. The center provides six to eight courses per year for health care workers, administrators, laboratory managers, chief nurses, engineers, architects, and other professionals. Professionals from almost all the countries of the former Soviet Union have taken these courses, and the center has supported TB infection control programs in many of these countries, as well as elsewhere.
A safe TB control program is no more expensive than a traditional one, said Volchenkov. Reducing the hospitalization rate saves resources, and providing safer conditions for a limited number of infectious cases leaves more resources available for the TB control program.
Volchenkov listed several scientific and practical impacts of the Vladimir project:
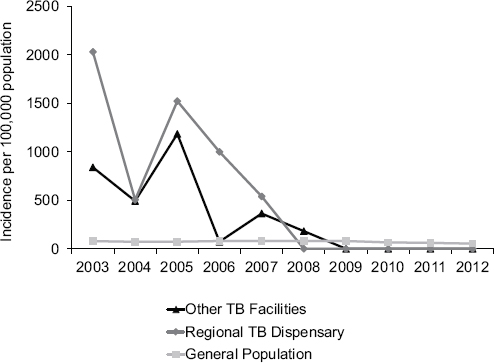
FIGURE 7-1 The incidence of occupational TB infection among health care workers providing TB services in the Vladimir region of Russia fell to zero after an infection control program was implemented.
SOURCE: Volchenkov, 2013. Presentation at the IOM workshop on the Global Crisis of Drug-Resistant Tuberculosis and the Leadership of the BRICS Countries: Challenges and Opportunities.
• Upper-room UVGI fixtures, the first of which in Russia were installed in the Vladimir Oblast TB Dispensary, now are being used throughout the former Soviet Union and have proven to be an inexpensive and effective engineering method for controlling infection.
• Negative-pressure sputum collection booths have been beneficial for countries with a cold climate.
• In-duct UVGI has been implemented to disinfect exhaust air from high-risk areas.
• A study was performed to compare the cost-effectiveness of various engineering controls.
• An inexpensive but effective and sustainable respiratory protection program has been instituted throughout facilities in the region.
• Separate wards for MDR and XDR TB patients and for children were nearing completion in the Vladimir Oblast TB Dispensary at the time of the workshop.
• A well-equipped training laboratory for engineers and architects was built in the dispensary.
• Diagnostic, separation, and treatment algorithms based on rapid molecular diagnostic methods were developed.
• The Vladimir Center of Excellence for TB Infection Control provided support to several countries for the development of national guidelines on TB infection control.
Volchenkov also listed the specific infection control challenges Russia has faced, some of which may apply to other BRICS countries as well:
• A cold climate requires mechanical ventilation in areas with high-risk TB patients.
• Long-term hospitalization with general neglect of administrative measures for TB infection control is common.
• The weak involvement of primary health care services in TB outpatient services can severely limit community-based care for TB patients.
• National guidelines focused only on contact and droplet transmission neglect to cover precautions for airborne transmission.
• Investments in TB infection control lacked prioritization so that, for example, resources were spent on waste disposal and decontamination even though airborne transmission is not affected by these interventions.
• UVGI is not always used effectively. In settings where airborne infection is generated continuously, upper-room UVGI is necessary and requires expertise and good design to be effective.
• An effective respiratory protection program was lacking in most of the institutions of the Russian Federation.
• Engineers and architects lacked the expertise to design, maintain, and commission engineering systems for infection control in hospitals.
Finally, Volchenkov listed opportunities that exist in Russia and could also apply to other BRICS countries:
• The universal availability of electricity allows the use of effective measures, such as upper-room UVGI and ventilation, in high-risk settings.
• Federal and regional funding for infection control has increased substantially in the past 10 years.
• FLD and SLD supply has been sufficient in recent years.
• Rapid molecular methods are becoming available at the regional and district levels, and rapid diagnoses have allowed resources to be devoted to infection control.
• Updated guidelines have improved knowledge of infection control among health care workers and administrators.
At the same time, a lack of knowledge and understanding of several key issues continues to create problems, Volchenkov said. More needs to be learned about the risk of household and community transmission by patients being treated. Questions remain about the criteria for discharge and hospitalization. More evidence also is needed on when isolation can be discontinued for MDR and XDR TB patients in the hospital.
Volchenkov concluded by observing that infection control programs need to have short- and long-term components. They also need to be based on comprehensive risk assessment in the facility, the region, or the country so that policies and regulations are adapted to the situation at hand. Moreover, programs must take health care trends into account, such as the ongoing paradigm shift toward reduced hospitalization and the implementation of new molecular methods. And infection control programs need expert support. Finally, policy makers and politicians should understand that infection control interventions save considerable resources by reducing the incidence of DR TB. Administrative controls can limit the areas, personnel, procedures, and time for which engineering controls and personal respiratory protection are needed. Without effective administrative controls, more expensive environmental interventions are not effective and sustainable.
STOPPING TRANSMISSION IN INSTITUTIONAL AND COMMUNITY SETTINGS6
Transmission has become the “elephant in the room” of the MDR TB epidemic, said Edward A. Nardell, Associate Professor, Division of Global Health, Brigham and Women’s Hospital, Harvard Medical School. In the past, transmission and reinfection were underestimated, and previously treated patients were said to have acquired drug resistance. But previously treated TB patients can be reinfected, as demonstrated by research results from Russia (Gelmanova et al., 2007), South Africa (Sonnenberg et al., 2001), China (Shen et al., 2006), and other locations. Especially where exposures are common in high-burden areas—including those with high rates of HIV infection—reinfection is to be expected.
Recognition of the importance of transmission and reinfection has a major impact on priorities in TB infection control, on the viability and effectiveness of initiatives focused on latent TB, and on vaccine development. First, known and treated TB patients are not likely to be the major sources of transmission, whether in hospitals or in the community. The greater problem is unsuspected TB patients or unsuspected drug resistance. Nardell cited research from Arzobispo Loayza Hospital in Lima, Peru, where 250 of 349 patients admitted to one female ward in 1997 were screened for TB using sputum, a chest X-ray, a medical history, and a physical exam (Willingham et al., 2001). Forty patients had positive cultures for TB. Two-thirds were smear positive, but 33 percent were unsuspected. Twenty percent had MDR TB, and 6 of the 8 MDR TB patients were unsuspected. Under such circumstances, transmission in a general medical ward is likely, said Nardell.
The configuration and usage of buildings and other aspects of the physical environment are often neglected, but building design matters, said Nardell. Unpublished data, again from Peru, show that the rate of skin test positivity among Peruvian medical students grew from 3.5 percent to 45.9 percent over 7 years. However, the increase was much more substantial for a hospital with a low volume of air space per bed and poor ventilation. The infection rate was much lower in a second hospital with more air space per bed, large windows, and a breezy seaside location.
Since 2008, Harvard Medical School has provided a summer course on building design and engineering approaches for airborne infection control. The course has had a demonstrable effect on the design of facilities to make them less likely to contribute to TB transmission, Nardell said.
Ventilation is another important factor in transmission. Upper-room UVGI can be highly effective and inexpensive compared with other options.
__________________
6 This section is based on the presentation by Edward A. Nardell, Associate Professor, Division of Global Health, Brigham and Women’s Hospital, Harvard Medical School.
However, few guidelines exist for its use, and its implementation and maintenance can be poor. In general, air filtration machines and other room air cleaners move too little air to be helpful, said Nardell. UV in ducts and direct UVGI also are not recommended.
Nardell described an experiment in a six-bed ward in which air exposed or not exposed to UV was sent to a set of guinea pigs, animals that are highly susceptible to TB. Treatment with UV light showed about 80 percent efficacy, which was the equivalent of adding approximately 18 air changes to the room. UV treatment requires expertise to design the fixtures and some maintenance, but it can be highly effective.
Nardell concluded by discussing the advantages of avoiding hospitals altogether and relying on community-based treatment. A systematic review of the cost-effectiveness of treatment for MDR TB found that community-based treatment is much less expensive than treatment in hospitals (Fitzpatrick and Floyd, 2012). Experience in Cambodia, Ethiopia, Lesotho, Peru, South Africa, and elsewhere also has demonstrated that such treatment can be highly effective while creating less opportunity for institutional transmission.
Greater likelihood of transmission is a concern with community-based care, but Nardell presented evidence that smear- and culture-positive TB patients on effective therapy do not infect close contacts. Smear and culture positivity correlates with transmission before but not during treatment. In fact, a classic study on infectivity using guinea pigs demonstrated that the effect of treatment on both drug-susceptible and drug-resistant patients was almost immediate (Riley et al., 1959). In contrast, the common rule of thumb that patients need to be treated for 2 weeks before they are no longer infectious appears to have little empirical backing. Patients who infect others are largely those with unsuspected TB or those with DR TB who are on an ineffective therapy, because everyone else is on effective therapy, which stops transmission very quickly. However, effective treatment requires performing rapid and accurate diagnosis and then starting patients on the appropriate therapy quickly.
The situation is somewhat different for XDR TB, whose transmission cannot be stopped with the standard drugs. In these cases—and for TB control in general—Nardell advocates a paradigm known as FAST, for Find TB cases through rapid diagnosis, perform Active case finding by focusing on cough surveillance, Separate safely and reduce exposure through infection control, and Treat effectively based on rapid DST. This approach requires political will and resources, but it can stop transmission in facilities and provides for effective assessment through process indicators and monitoring of cases in health care workers.
This page intentionally left blank.
















