The Workforce Caring for Patients with Cancer
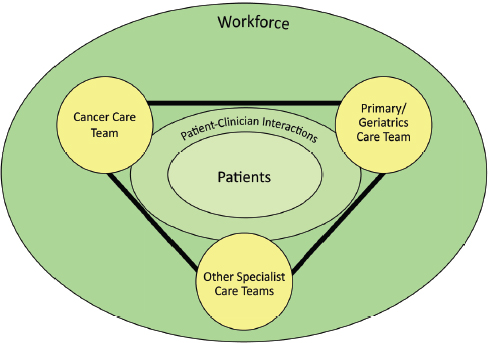
Adiverse team of professionals provides cancer care, reflecting the complexity of the disease, its treatments, and survivorship care (C-Change, 2013). The cancer care team includes those with specialized training in oncology, such as oncologists and oncology nurses, other specialists and primary care clinicians, as well as family caregivers and direct care workers. Patients, at the center of the committee’s conceptual framework, are encircled by the cancer care workforce (see Figure S-2), depicting the idea that high-quality cancer care depends on the workforce providing competent, trusted interprofessional care that is aligned with the patients’ needs, values, and preferences. To achieve this standard, the workforce must include adequate numbers of health care clinicians with training in oncology. The members of interprofessional cancer care teams must be coordinated with each other and with the patients’ other care teams (e.g., primary care/geriatrics care teams or other specialty care teams). Additionally, the workforce must have the skills necessary to implement the committee’s conceptual framework for a high-quality cancer care system. The focus on the workforce caring for patients with cancer is consistent with the Institute of Medicine’s (IOM’s) 1999 report on the quality of cancer care, which recognized the importance of cancer care being delivered by coordinated, experienced professionals (IOM and NRC, 1999).
Current practice falls far short of this standard. Workforce shortages among many of the professionals involved in providing cancer care are projected to worsen in the near future, and the educational system lacks the capacity to quickly train new members of the workforce (IOM, 2009b).
Care is often uncoordinated among the various clinicians and care teams, leaving patients to navigate a fragmented cancer care delivery system. Caregivers are also expected to assume a significant amount of medical tasks without any training or support (Reinhard and Levine, 2012).
At the same time, shifting demographics are placing new demands on this delivery system, with the incidence of cancer increasing due to the aging population and cancer survivors living longer (see Chapter 2). Medical advances, such as new chemotherapy regimens that involve less toxic, but more frequent administration, are increasing the volume of cancer care (IOM, 2009b). In addition, the Patient Protection and Affordable Care Act (ACA)1 is expected to expand health insurance coverage to an estimated 25 million previously uninsured persons, many of whom are likely to require cancer care at some point during their lifetimes (CBO, 2013). A number of studies show that the quality of care is detrimentally impacted by workforce shortages (AHRQ, 2004; Aiken et al., 2010; Blegen et al., 2011; Needleman et al., 2011). Patients can experience delays in diagnosis and treatment, longer wait times to see a clinician, less frequent interaction with clinical and supportive services, delays in the evaluation and management of symptoms, worsening health disparities, and decreased clinical trial enrollment.
This chapter assesses the capacity and competence of the workforce to meet the growing need for high-quality cancer care. The first section provides a review of the cancer care team members, including estimates of workforce supply and demand. The next section focuses on strategies for ensuring the quantity and quality of the clinicians on cancer care teams, including the recruitment and retention of clinicians, the importance of team-based cancer care, training the workforce, and telemedicine. The chapter concludes with a discussion of the role of family caregivers and direct care workers in providing cancer care. The committee relied heavily on the IOM’s previous research on the health care workforce to derive the evidence base for this chapter, including the National Cancer Policy Forum’s workshop summary on Ensuring Quality Cancer Care Through the Oncology Workforce (2009b) and recent consensus studies addressing the geriatric, nursing, and mental health workforces (IOM, 2008b, 2011a, 2012c). The committee identifies two recommendations to strengthen the workforce that cares for patients with cancer.
________________
1 Patient Protection and Affordable Care Act, Public Law 111-148, 111th Congress (March 23, 2010).
DEFINING THE WORKFORCE CARING FOR PATIENTS WITH CANCER
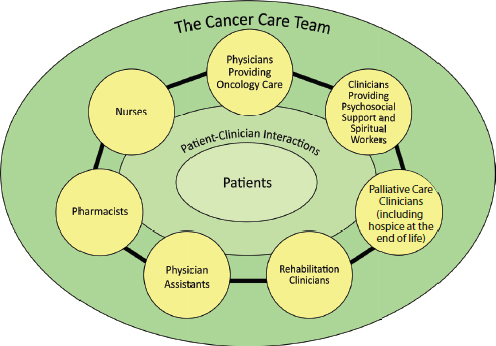
High-quality cancer care is provided by a diverse team of professionals. This portion of the chapter reviews many of the clinicians who comprise the cancer care team: physicians, nurses, advanced practice registered nurses, physician assistants, palliative care specialists, clinicians providing psychosocial support, spiritual workers, rehabilitation clinicians, pharmacists, and, for care at the end-of-life, hospice clinicians. Each section describes the general role of the profession in cancer care and the projected workforce supply and demand. Many other professionals are also involved in cancer care teams, such as laboratory personnel, public health workers, and cancer registrars. Annex 4-1 provides a detailed list of professionals involved in cancer care, their general roles on the cancer care team, and an overview of available information about the workforce.
In general, data suggest that the growth in the absolute number of older adults is likely to result in a greater total volume of patients with cancer and a greater need for services than our current workforce can provide. As noted in previous IOM reports, however, it can be challenging to accurately translate data on illness prevalence into estimates of workforce supply and demand (IOM, 2005, 2008b, 2012c). Data on health care professions are not routinely or systematically collected across the multiple disciplines involved in cancer care, giving an incomplete picture of the current workforce. Several provisions of the ACA may improve available information on the workforce, including the National Center for Health Workforce Analysis and National Health Care Workforce Commission, but it is unclear whether funding will continue for these activities (see Annex 2-1). In addition, many factors can lead to forecasting errors, such as changes in utilization patterns of medical technologies, changes in the organization of care, and changes in patient demands.
Physicians
Several recent studies estimate that the physician workforce lacks the capacity to meet the future demand for health care services. The Association of American Medical Colleges (AAMC) estimated that the United States will have a shortage of 90,000 physicians in the next 10 years due to the aging and growing population (AAMC, 2011b). Sargen and colleagues (2011) projected further into the future, calculating a current physician shortage of around 8 percent, which could rise to more than 20 percent by 2025 if the rate of medical residents being trained does not increase. The escalating amount of time physicians are devoting to documentation, compliance, and other indirect patient care services could further increase
demand for physician services by an additional 10 to 15 percent during the same time period.
A major driver of the physician shortage is the aging workforce. Currently, 40 percent of practicing physicians are older than 55 and roughly one-third of physicians are expected to retire over the next 10 years (AAMC, 2011b, 2013). These physicians are being replaced by a younger generation of physicians who more often prefer to work part time or in specialties that have less demanding on-call responsibilities (Hauer et al., 2008). A study by Staiger and colleagues found that the mean hours worked by physicians decreased by more than 7 percent between 1996 and 2008, with the largest decrease in hours worked among physicians younger than 45 years (Staiger et al., 2010).
The distribution of physicians across urban and rural areas may also contribute to the physician shortage. For example, only 11 percent of the 300,000 primary care physicians practicing in the United States are located in rural areas (UnitedHealth, 2011). Specialists are also more concentrated in urban areas than in rural areas. Thus, patients in rural areas have less access to medical services, including oncology, and often have to drive long distances to receive health care services.
The medical education system is unlikely to keep pace with the rising demand for physician services. Although medical school enrollment has increased by 30 percent over the previous 5 years (AHR, 2012b), the federal government has not substantially increased the number of residency slots that it supports to train newly graduated medical students. This is problematic because Medicare is the largest payer of Graduate Medical Education (GME) (Health Affairs, 2012). The Balanced Budget Act of 1997 froze the number of resident slots and fellowships funded by Medicare without regard to whether the number of physicians generated would meet future demands for health care services (AAMC, 2011b). Recent proposals to reduce the federal debt have included further cuts to Medicare’s GME support. An ongoing IOM consensus study is examining this issue in more detail and will be proposing solutions to GME’s governance and financing (IOM, 2012b).
These general trends in the physician workforce have a substantial impact on the physicians and specialists who provide care for cancer patients, such as oncologists, primary care physicians, and geriatricians. These clinicians are the focus of the remainder of this section.
Physicians Providing Cancer Care
There are numerous types of physicians who provide cancer care, including surgical oncologists who operate, radiation oncologists who treat with radiation, and medical oncologists who provide systemic treat-
ments. There are also a limited number of geriatric oncologists who primarily conduct academic research on caring for older adults with cancer (Bennett et al., 2010). Additionally, many cancer patients are treated by other types of physicians, such as urologists for prostate cancer, pulmonologists for early-stage lung cancer, dermatologists for early-stage melanoma, and gastroenterologists for early-stage colon cancer. This section focuses on medical oncologists because they are the primary physicians involved in cancer care, and their workforce has been studied extensively by the American Society of Clinical Oncology (ASCO). Less information is available about other physician workforces who provide cancer care. The American Society for Radiation Oncology, however, is currently conducting a survey of the radiation oncology workforce in order to assess the profession’s supply, education, and employment situation (ASTRO, 2012b).
In order to become board certified in medical oncology, physicians must complete a 3-year residency program in internal medicine followed by an oncology fellowship (at least 2 clinical years of training, often with additional time for research). Few medical oncology fellowship programs currently have plans to increase the number of training slots, which limits the size of the workforce (AAMC, 2007; Erikson et al., 2007). Training new medical oncologists is expensive and there is little financial support available from the government to expand these programs.
In addition, merely increasing the size of existing oncology fellowship programs would not solve the workforce problem. The size of the oncology workforce is constrained by the pipeline of residents. Medical oncologists must first complete a residency in internal medicine, but the number of students undergoing training in internal medicine has increased only marginally in recent years. There is also a growing number of subspecialties available to internal medicine interns (Salsberg et al., 2008), and medical oncology fellowship programs must compete against interventional subspecialties, such as cardiology and pulmonology, for this limited supply of internal medicine residents. Moreover, many medical students are opting for specialties that do not require a residency in internal medicine, such as dermatology, orthopedic surgery, or radiology, as well as radiation oncology and surgical oncology.
A study commissioned by ASCO predicts that the demand for medical oncologists will increase dramatically between now and 2020 due to a 48 percent increase in cancer incidence and an 81 percent increase in people living with or surviving cancer (AAMC, 2007; Erikson et al., 2007). During this same time period, the supply of oncologists is predicted to increase only 14 percent. The study found that more than half of currently practicing medical oncologists are age 50 or older and will reach retirement age by 2020. Medical oncologists younger than 45 are also working
fewer hours on average than those ages 45 to 64, exacerbating the problem of an aging workforce. Based on these trends, the study concluded that there will be a shortage of 2,500 to 4,080 medical oncologists by 2020. It is likely that the other professionals involved in providing cancer care will also face similar imbalances between the workforce supply and demand.
Primary Care Physicians
Primary care physicians are generalists who provide comprehensive and continuous care to patients regardless of the diagnosis, the organ system involved, or the origin of the medical problem (biological, behavioral, or social) (AAFP, 2012). Box 4-1 describes the diverse roles that primary care clinicians play in caring for patients with cancer.
In 2007, there were more than 200,000 general internal medicine and family medicine physicians in the United States, the principal primary care medical specialties (AAMC, 2008). This number has been increasing steadily over the past several years because more medical students have been matching into primary care residencies (AAMC, 2011a). However, a number of factors may limit the long-term supply of primary care physicians.
In a survey of fourth-year medical students, only 2 percent of the respondents planned a career in internal medicine without specialization (Hauer et al., 2008). The respondents identified a number of concerns about careers in general internal medicine, including inadequate administrative and technical support to deal with the paperwork demands, the complexity of caring for older adults and chronically ill patients, and preferences for work schedules that provide fewer demands on time and more opportunities for personal satisfaction outside of work. A major deterrent to becoming a primary care physician is also the more than $135,000 median annual income gap between primary care physicians and subspecialists, a difference of $3.5 million in expected income over a lifetime (RGC, 2010). These factors have likely contributed to approximately 20 percent of primary care physicians departing from general internal medicine within a decade of becoming certified to practice, with many leaving to work in another medical field (Lipner et al., 2006).
It may be possible to offset the need for additional primary care physicians by diverting some patients to nonphysician professionals, such as advanced practice registered nurses and physician assistants (discussed below in the sections on advanced practice registered nurses and physician assistants), and using patient-clinician electronic communication (see discussion in Chapter 6) (Green et al., 2012; Kuo et al., 2013).
BOX 4-1
The Roles of Primary Care Clinicians in Caring for Patients with Cancer
Primary care clinicians fulfill a diverse set of roles in cancer care. They are often the first clinicians that patients see when they have signs or symptoms of cancer and are the most likely to screen their patients for cancer. Thus, they are usually the ones diagnosing cancer and providing patients with referrals to oncologists or other specialists for treatment.
During active cancer treatment, primary care clinicians provide patients with ongoing health promotion, disease prevention, health maintenance, counseling, education, and diagnosis and treatment of other acute and chronic illnesses. This is especially important in older adults with cancer who tend to require treatment for other chronic conditions, such as high-blood pressure and diabetes (Unroe and Cohen, 2012).
It is important for the cancer care team to effectively coordinate with a patient’s primary care clinicians during the acute cancer treatment phase. Primary care clinicians often have known their patients longer than the cancer care team and are more likely to be familiar with their patients’ needs, values, and preferences. It is also important that primary care clinicians be informed about their patients’ cancer treatments. They often provide continuous treatment for their patients’ concurrent illnesses and conditions, which may need to be adjusted or monitored differently during cancer treatment, as well as survivorship care and cancer surveillance after their acute cancer treatment is complete. Primary care clinicians can also play a role during active treatment in establishing advance directives and coordinating with family caregivers and direct care workers (IOM, 2011b; Klabunde et al., 2009).
Cohen (2009) has described the ideal relationship between the primary care team and the cancer team as “shared care,” where both care teams are involved in a patient’s care during the entire continuum of the disease, but have a bigger or smaller role at a given time depending on the needs of the patient and the disease status. In a survey by Del Giudice and colleagues, primary care clinicians reported that they are interested in being involved in their patients’ cancer care, especially if they have a long-term relationship with the particular patient, but often feel they lack the preparation and knowledge to do so effectively (Del Giudice et al., 2009). A more recent survey by Potosky and colleagues (2011) found that primary care clinicians differ significantly from oncologists in their knowledge, attitudes, and practices related to follow-up care for breast and colon cancer. Cancer care plans which summarize a patient’s needs, treatment information, and follow-up care, are tools to aid primary care clinicians in coordinating with the cancer care team and providing complementary health care services to their patients (see discussion on care plans in Chapter 3) (IOM, 2005, 2011b).
Geriatricians
Geriatricians are primary care physicians trained to meet the unique health care needs of older adults. Currently, the number of geriatricians does not adequately meet the health care needs of the older adult population, and the situation is growing worse (IOM, 2008b). There are over 9,000 certified geriatricians (ABIM, 2012). In 2011, there was 1 geriatrician for every 2,620 Americans 75 years or older. By 2030 that ratio is expected to drop to 1 geriatrician for every 3,798 Americans 75 years or older. Many geriatric fellowship slots are not being filled due to lack of interest. For academic year 2009-2010, only 56 percent (273 out of 489) of allopathic geriatric training slots were filled and only 2 out of 46 osteopathic geriatric medicine fellowship slots were filled (AGS, 2012).
The recent IOM report Retooling for an Aging America: Building the Health Care Workforce (2008b) made a series of recommendations intended to improve and grow the geriatric workforce by enhancing geriatric competence, increasing recruitment and retention of geriatric specialists, and redesigning models of care to meet the rising needs of older adults. The committee believes that these recommendations are important to improving the quality of cancer care in this country and efforts should be made to implement them.
Nurses
The American Nurses Association defines nursing as “the protection, promotion, and optimization of health and abilities, prevention of illness and injury, alleviation of suffering through the diagnosis and treatment of human response, and advocacy in the care of individuals, families, communities, and populations” (ANA, 2012). Nursing is a multilevel profession, and includes (1) licensed practical nurses who are trained through 12- to 18-month programs in vocational/technical schools or community colleges; (2) registered nurses (RNs), who must complete a 4-year bachelor’s degree program, a 2-year associate degree program, or a 3-year diploma program and pass a national licensure examination; and (3) advanced practice registered nurses (APRNs), who have master’s or doctorate’s degrees in nursing and work with more independence. There are currently more than 3 million nurses in the United States and they make up the largest segment of the health care workforce (IOM, 2011a).
A number of analyses suggest that the existing nursing workforce is insufficient to meet the rising demand for services. The Bureau of Labor Statistics has predicted that nursing will be one of the fastest-growing professions in the United States and that the country will need over 1 million new nurses by 2020 to fill new jobs and replace vacancies resulting from
retiring nurses (BLS, 2012a). Juraschek and colleagues (2012) forecasted the RN job shortage in all 50 states between 2009 and 2030 and assigned letter grades based on the projected RN job shortage ratio. The number of states receiving a grade of “D” or “F” for their RN job shortage ratio is projected to increase from 5 in 2009 to 30 by 2030. This translates into a deficit of almost 1 million RNs by 2030.
Buerhaus and colleagues published several studies showing that people who have turned to nursing in response to the recent economic downturn have eliminated the current nursing shortage (Buerhaus et al., 2009; Staiger et al., 2012). Older nurses are delaying retirement or returning to the workforce and part-time nurses are becoming full-time employees in response to their own and their spouses’ employment insecurity. In addition, the number of RNs has grown faster than predicted (Auerbach et al., 2011). Between 2002 and 2009, the number of full-time RNs between the ages of 23 and 26 increased by 62 percent. Nonetheless, Buerhaus and colleagues cautioned that these trends may not continue and that a number of factors suggest there will be nursing shortages in the future (Buerhaus et al., 2009; Staiger et al., 2012).
The workforce is rapidly aging, with an increasing number of baby boomers nearing retirement. There has also been a decline in RN earnings relative to other career options. Nurses express more dissatisfaction with their jobs than do people in other professions, and the changing demographics in the United States have led to an older and less healthy population, which discourages younger generations from entering nursing (AHR, 2012a). In a survey of the current RN workforce conducted by AMN Healthcare, almost one-third of the nurses reported planning to make career changes in the next 1 to 3 years (AMN Healthcare, 2012). Only 56 percent of respondents said that if they were starting out today they would choose nursing as their career.
The shortage of nursing faculty is compounding the shortage of nurses. A recent IOM study recommended that the nursing workforce increase the number of nurses with a baccalaureate degree from 50 percent to 80 percent of the workforce and double the number of nurses with a doctorate by 2020 (IOM, 2011a). However, nursing schools lack the capacity to train this workforce. A 2007 survey by the American Association of Colleges of Nursing (AACN) found that 85 percent of nursing schools have faculty vacancies or need more faculty members but lack the budget to pay their salaries (AACN, 2012b). In 2011, more than 75,000 qualified nursing applicants were not accepted into a nursing program due primarily to a shortage of faculty and resource constraints (AACN, 2012a).
One of the major factors contributing to the faculty shortage is the requirement for faculty to hold Ph.D.s (Berlin and Sechrist, 2002). In 2007, enrollment in nursing Ph.D. programs was up less than 1 percent
from previous years despite the demand for nurses with this qualification (AACN, 2008). A major deterrent to nurses becoming faculty is the fact that advanced practice registered nurses earn significantly higher salaries if they work in clinical positions than if they work in academic positions. The aging workforce is also a factor. Nursing faculty tend to retire earlier than other medical professions, with an average retirement age of 62.5 years (Berlin and Sechrist, 2002). The average age of doctorate-level faculty in nursing is currently 60.5 years for professors (AACN, 2011).
This nursing shortage means that there is likely to be an insufficient number of nurses knowledgeable in oncology and able to meet the needs of the growing number of patients with cancer and cancer survivors. General nursing programs cover a limited amount of information about oncology, and the number of nursing schools with a specialty in oncology has been drastically reduced in recent years (Ferrell et al., 2003; IOM, 2005). Out of the more than 1 million registered nurses with a certification in a clinical specialty, only 1.2 percent are certified in oncology (HRSA, 2010).
Advanced Practice Registered Nurses
APRNs are nurses who have completed graduate-level education and have national certification and licensure from a state board. Nurses meeting this requirement include certified registered nurse anesthetists, certified nurse-midwives, clinical nurse specialists, certified nurse practitioners, and individuals who hold a doctorate of nursing practice (DNP). APRNs are credentialed to practice in a specific patient population (e.g., family/individual across lifespan, adult-gerontology, neonatal, pediatrics, women’s health/gender, or psychiatric—mental health), and their credentials allow them to work independently or in collaboration with a physician (NCBSN, 2010, 2012).
In most states, APRNs can diagnose disease, order tests, refer patients to specialists, and prescribe medication without physician oversight (Christian et al., 2007). As a result, they often serve as patients’ primary care clinicians and develop long-term relationships with their patients. (See Box 4-1 for a description of the role of primary care clinicians in cancer care.) The inclusion of APRNs on care teams has been shown to improve the quality of care that health care delivery organizations provide to patients, especially when they are involved in patients’ transitions between care settings (Naylor and Keating, 2008; Naylor et al., 1994, 1999, 2004, 2005, 2009, 2011).
APRNs wishing to become certified in oncology can go through one of the Oncology Nursing Certification Corporation’s three advanced oncology nursing certification programs: (1) Advanced Oncology Certified Nurse Practitioner, (2) Advanced Oncology Certified Clinical Nurse Spe-
cialist, or (3) Advanced Oncology Certified Nurse (ONCC, 2012). In 2008, there were approximately 250,000 APRNs and 2.6 percent were certified in oncology (HRSA, 2010). The DNP was launched in 2008, and as of April 2013, there were 217 DNP programs with 97 additional programs in the planning stages (AACN, 2013). DNPs play an important role in collaborative cancer care teams, specifically because of their training as agents of system change and their focus on quality as clinical leaders (Bajorin and Hanley, 2011).
Physician Assistants
Physician assistants (PAs) are medically trained and licensed professionals who practice medicine as part of a care team. They perform duties under the supervision of a physician, including providing physical examinations, diagnosing and treating illnesses, ordering and interpreting lab tests, providing patient education, and establishing and managing care plans. They have prescription privileges in all 50 states and the District of Columbia (AAPA, 2012b).
The American Academy of Physician Assistants projected that the number of PAs will increase from 75,000 in 2008 to between 137,000 and 173,000 certified in 2020 (AAPA, 2012a). They are the second-fastest-growing profession behind nurses. PAs receive a generalist education and then must pass a national certification examination, which includes content on the diagnosis and treatment of all of the major cancers for each organ system. There is also one postgraduate PA residency program in oncology (Coniglio et al., 2011). However, the majority of PAs who work in oncology receive on-the-job training though mentorship with their cancer care team (Ross et al., 2010), and they are playing an increasingly important role on collaborative cancer care teams (Coniglio, 2013; Coniglio et al., 2011).
Palliative and Hospice Care Clinicians
Palliative care and hospice care are essential components of high-quality cancer care (see discussion in Chapter 3). Palliative care is specialized medical care that provides patients with pain and symptom management, counseling on goals of treatment, coordination of care services, support when ending anti-cancer therapy, and end-of-life care. It can be provided at any point along the continuum of cancer care, often in conjunction with anti-cancer therapy. Hospice care is a form of palliative care and is focused on maintaining the quality of life for patients with advanced cancers. In order to provide these services, the cancer care team should include clinicians with training in palliative and hospice medicine.
Integrating palliative care and hospice care into standard cancer practice, however, is likely to strain the palliative and hospice workforce due to the increased utilization of these clinicians.
Currently, there are 4,400 physicians specializing in palliative and hospice medicine. A study sponsored by the American Academy of Hospice and Palliative Medicine estimated that this equates to a shortage of around 3,000 to 7,000 full-time physicians, or 6,000 to 18,000 part-time physicians (Lupu, 2010). It is unlikely that the education system will be able to quickly train new physicians in this field because there are only 234 palliative and hospice medicine fellowship positions. Similarly, the number of nurses with this expertise may be insufficient to meet increased demand. There are currently 17,000 certified hospice and palliative nurses (NBCHPN, 2013a). Nurses with this certification must hold a registered nursing license, have 2 years of relevant experience, and recertify every 4 years (NBCHPN, 2013b).
Cancer care teams are exploring new models of integrating palliative care and hospice care into their practices. For example, U.S. Oncology embeds a palliative care clinician directly within its oncology practices (Alesi et al., 2011). Other oncology practices refer patients with advanced cancer to a palliative care specialist soon after their diagnoses (Yoong et al., 2013). Many academic cancer centers, such as MD Anderson and Memorial Sloan-Kettering, have internal pain management programs to which cancer care teams can refer patients (MDACC, 2013; MSKCC, 2013).
Quill and Abernethy (2013) proposed creating a palliative care model that differentiates between primary palliative care (skills that all clinicians should have) and specialist palliative care (skills for managing more complex and difficult cases). For this model, the physicians and nurses providing cancer care would meet most of their patients’ palliative care needs but refer patients to a palliative care clinician for complex and refractory problems. They would refer all patients to hospice clinicians for end-of-life care.
Clinicians Providing Psychosocial Support and Spiritual Workers
A recent IOM report concluded that attending to patients’ psychosocial needs is an integral part of high-quality cancer care (IOM, 2008a). It is also a key consideration in developing patients’ care plans across the cancer care continuum (see Chapter 3). A wide range of clinicians can provide psychosocial support, including social workers, psychologists, psychiatrists, and chaplains. Because it is important that the provision of psychosocial support be coordinated with a patient’s biomedical health care (IOM, 2008a), clinicians providing psychosocial support and spiritual workers should be included on the cancer care team.
Social workers are one of the main professions providing psychosocial support to cancer patients. They assist “individuals, groups, or communities to restore or enhance their capacity for social functioning, and work to create societal conditions that support communities in need” (NASW, 2013b). They help patients manage the stress of a cancer diagnosis, decide on a care plan, and adapt to daily life with this disease (Lauria et al., 2001). For older adults with cancer, they often assist with advance care planning, loss and grief, independent living, and lifestyle adjustments, among many other issues related to the aging process. They can also provide emotional support for individuals serving as family caregivers (NASW, 2013c).
To practice, social workers must obtain a bachelor’s, master’s, or doctoral degree and be licensed to practice in the state where they work (BLS, 2013f). Master’s-level social workers may specialize in health care by meeting specific continuing education and supervised work requirements (NASW, 2013a) and can further specialize in oncology or gerontology, although many social workers practice in health care settings without obtaining these certifications. Of the estimated 650,500 social workers in the United States (BLS, 2013f), 13 percent of licensed social workers specialize in health care (NASW, 2006). There are 1,000 oncology social workers and 4282 certified oncology social workers (AOSW, 2013; Blum et al., 2006). In a survey from 2006, 78 percent of licensed social workers reported working with older adults; however, only 9 percent identified aging as their primary field of practice (NASW, 2006). Because the social work workforce is significantly older than the U.S. civilian labor force, these numbers may decline (NASW, 2006).
Psychologists also provide psychosocial services to cancer patients, typically using psychotherapy and behavior modification interventions (APA, 2013b; BLS, 2013e). Psychologists can teach cancer patients strategies for controlling their stress, grief, fear, and depression stemming from their disease. For example, some people lose sleep, stop exercising, eat unhealthily, or turn to alcohol and drugs following a diagnosis with cancer. Psychologists can help these patients develop better coping strategies, such as relaxation exercises, meditation, self-hypnosis, imagery, and techniques to relieve nausea or other side effects of treatment. They can also help patients to communicate more effectively with the other members of the cancer care team and help them to decide on an appropriate care plan. In addition, psychologists can play an important role in helping the families of cancer patients cope with their own stress, as well as work through sexual and relationship challenges (APA, 2013a; Clay, 2010).
To practice, psychologists must obtain licensure in the state where
________________
2 Personal communication, G. Vaitones, Board of Oncology Social Work Certification, March 1, 2013.
they work (BLS, 2013e; IOM, 2008a). Licensing laws vary by state; however, most states require a doctoral degree, a 1-year internship, several years of work experience, and passage of the Examination for Professional Practice in Psychology (BLS, 2013e). Psychologists may become board certified in over 10 specialty areas, including clinical psychology, counseling psychology, school psychology, child psychology, clinical health psychology, family psychology, and rehabilitation psychology (APA, 2013c; BLS, 2013e; IOM, 2008a). However, board certification is not a requirement for practice and has not been obtained by the majority of psychologists (IOM, 2008a).
Due to the increasing number of cancer survivors and older adults, the demand for psychologists is expected to grow, as is the number of professionals in the field (BLS, 2013e; IOM, 2008a). There were an estimated 174,000 psychologists in 2010, with 154,300 practicing clinical, counseling, or school psychology. By 2020, projections suggest there will be roughly 211,600 psychologists, with 188,000 practicing clinical, counseling, or school psychology (BLS, 2013e).
Psychiatrists also provide psychosocial support for cancer patients. According to the American Psychiatric Association, “a psychiatrist is a medical doctor who specializes in the diagnosis, treatment and prevention of mental illnesses, including substance use disorders” (American Psychiatric Association, 2013, p. 1). The main difference between psychiatrists and other clinicians providing psychosocial support is that psychiatrists are medically qualified to treat both the mental and the physical aspects of psychological disorders; thus, they can prescribe medication and other medical treatments (American Psychiatric Association, 2013). In cancer care, they often prescribe drugs to treat patients’ psychiatric disorders stemming from their diagnosis, including anxiety and depression. They can also provide cancer patients with psychotherapy, which can help patients to cope with their disease and reduce distress (Arehart-Treichel, 2012; Barraclough, 1997). To practice, psychiatrists must complete a medical degree, at least 4 years of residency training, and pass written and oral examinations (American Psychiatric Association, 2013). There were roughly 24,210 psychiatrists practicing in the United States in 2012 (BLS, 2012b).
In addition, chaplains are an important group of professionals involved in meeting the psychosocial needs of cancer patients. Although accrediting groups often require hospitals to meet their patients’ spiritual needs, the role of chaplains on the cancer care team is often less prominent and less recognized than it should be. In one study, close to 90 percent of cancer patients receiving palliative radiation therapy reported that their spiritual needs were an important component of their psychological
health. More than 90 percent of cancer patients, however, said that the cancer care team did not ask them about those needs (Balboni et al., 2013). Patients whose spiritual needs are supported by the cancer care team, compared to patients whose spirital needs are not, have better quality of life, better quality of care near the end of life, with less aggressive end-of-life care (intubation, ventilation, resuscitation), and use hospice care three to five times more frequently (Balboni et al., 2010). Patients whose spiritual needs are not supported by the cancer care team are more likely to receive hospice care for less than 1 week, more likely to die in an intensive care unit, and generally have higher end-of-life care costs (Balboni et al., 2010). Because chaplains are not reimbursed, however, it is difficult to expand chaplaincy care services. The new models of payment discussed in Chapter 8 may help address this obstacle.
Rehabilitation Clinicians
Cancer and its treatment can lead to changes in individuals’ physical, cognitive, and emotional well-being. Rehabilitation clinicians, including physical therapists and occupational therapists, are trained to address these changes and help individuals with cancer maximize their quality of life. Physical therapists are experts in movement and function. They help individuals maintain and restore strength, stamina, flexibility, gross motor function, and mobility (Stubblefield, 2011). Occupational therapists are experts in modifying “activities and environments to allow individuals to do the things they want and need to do to maintain quality of life” (Longpré and Newman, 2011, p. 1). They assist individuals in tasks related to self-care, orthotic fabrication and fitting, home safety, and cognitive function (Stubblefield, 2011).
Rehabilitation clinicians do not currently play a prominent enough role in cancer care (Alfano et al., 2012). Most cancer patients have limited access to comprehensive rehabilitation services due to limited reimbursement and the dependence on referral for these services (Alfano et al., 2012). The importance of including rehabilitation clinicians as members of the cancer care team, however, is increasingly being recognized in the cancer community (Alfano et al., 2012; Stubblefield, 2011; Stubblefield et al., 2012). Rehabilitation clinicians can be involved in patients’ care across the cancer care continuum (Stubblefield, 2011; Stubblefield et al., 2012). There are around 200,000 physical therapists and 100,000 occupational therapists in the United States (BLS, 2013b,d) and both workforces are rapidly increasing. To practice, individuals must obtain a graduate-level degree and state licensure (BLS, 2013b,d).
Pharmacists
Pharmacists are an integral part of the cancer care team. They are typically responsible for filling prescriptions, checking for potential drug-drug and drug-disease interactions for patients using multiple medications, instructing patients on how and when to take their medication, and working with clinicians and insurance companies to ensure that patients are receiving the medication they need. To practice, pharmacists must be licensed by the state where they work, which usually requires a Pharm.D. degree and passing two licensing exams (the first tests pharmacists’ skills and knowledge and the second tests pharmacists’ understanding of the state licensing laws). Pharmacists may obtain an advanced pharmacy position, often in clinical settings. This requires completion of a 1 to 2-year residency program.
There were approximately 274,900 pharmacists practicing in the United States in 2010. This number is expected to increase by 25 percent by 2020, to approximately 344,600 pharmacists (BLS, 2013c).
ENSURING THE QUANTITY AND QUALITY OF THE WORKFORCE
The current workforce crisis has created an opportunity for reforming the cancer care delivery system. This portion of the chapter reviews the main strategies for ensuring that the workforce caring for patients with cancer has sufficient numbers of professionals to meet the demand for cancer care; that the team of professionals providing care is functional and well-coordinated; and that the workforce is prepared with the knowledge, skills, and experiences necessary to provide high-quality cancer care.
Recruitment and Retention of Professionals Who Provide Cancer Care
A key aspect of ensuring that there are sufficient numbers of professionals to care for patients with cancer is attracting individuals into oncology careers and retaining individuals once they choose a career in oncology. Many professionals who provide cancer care experience tremendous career satisfaction from administering care and developing relationships with their patients (Grunfeld et al., 2005; Shanafelt et al., 2006). However, there are numerous challenges to improving the recruitment and retention of professionals in cancer care, and many groups are developing strategies to overcome these challenges.
Job dissatisfaction and job-related stress are major deterrents to recruiting professionals to provide cancer care. Careers in oncology require individuals to deal with death and grieving regularly. Oncology profes-
sionals are particularly vulnerable to stress and career burnout due to the limited number of successful treatment options for many cancers and the difficult conversations about end-of-life decisions (IOM, 2009a; Losses, 2006). More general systemic pressures may also lead to dissatisfaction with oncology jobs and high rates of job-related stress, such as a heavy clinical workload, seeing high numbers of patients, short patient visits, the increasing levels of documentation required for reimbursement, and unpredictable work schedules that are driven by patient needs (Shanafelt et al., 2006). These problems are magnified during periods of workforce shortages (AAHC, 2008).
Surveys of medical oncologists confirm that professionals providing care to cancer patients experience significant career burnout, defined as emotional exhaustion and the lack of motivation to continue working in a given field (Allegra et al., 2005; Grunfeld et al., 2005; Kash et al., 2000; Ramirez et al., 1995, 1996; Shanafelt et al., 2005; Whippen and Canellos, 1991). In addition, many professionals who work in oncology report that their professional responsibilities regularly interfere with their family and personal lives, and lead to feelings of guilt and personal dissatisfaction (Allegra et al., 2005; Geurts et al., 1999; Grunfeld et al., 2005; Linzer et al., 2001; Warde et al., 1999). Similar levels of job dissatisfaction and stress are reported among other professionals involved in cancer care. For example, a 2001 survey of nurses found that hospital nurses were three to four times more likely than the average U.S. worker to be unhappy with their job and almost one-quarter of U.S. nurses reported that they were planning on leaving their jobs in the next year (Aiken et al., 2001).
Student debt also impedes the recruitment of physician-level professionals who provide cancer care. Medical school tuition has increased over the last two decades by 165 percent in private medical schools and by 312 percent in public medical schools (Jolly, 2005). In a survey conducted for the AAMC, students who appeared to be academically qualified for medical school were asked why they had not applied. All of the respondents listed cost as a major factor, with African American, Hispanic, and Native American students identifying cost as the top deterrent (Jolly, 2005). At the same time, reimbursement rates for medical care have declined and the threat of malpractice liability has increased (AAHC, 2008). When these factors are weighed against the number of training years required to become an oncologist or any of the other physician-specialists who provide cancer care, many potential recruits may choose alternate professions.
The recruitment of racial and ethnic minorities is particularly challenging. A previous IOM report recognized that increasing the proportion of populations underrepresented in medicine is an important mechanism for addressing disparities in care (IOM, 2003a). However, the clinical workforce is not currently representative of the general population. For
example, 75 percent of the physician workforce is White and just over 12 percent is composed of African Americans, American Indians/Alaska Natives, and Hispanics (AAMC, 2010). Similarly small proportions of minorities are represented in the nursing and social work workforces (HRSA, 2010; NASW, 2006).
The health care community has implemented several strategies to improve the recruitment of oncology and other health professionals, including national campaigns, early exposure to health professionals, and loan forgiveness and scholarship programs. For example, the Johnson & Johnson Campaign for Nursing’s Future was a national campaign that emphasized the positive aspects of nursing. An evaluation of this program showed that the campaign successfully improved nursing students’ attitudes about their decisions to become nurses (Donelan et al., 2005).
Many academic cancer centers have created opportunities for students to gain early exposure to careers in oncology, such as providing speakers to schools and hosting high school and college students as interns (IOM, 2009b). In a survey of nurses, 65 percent of respondents reported that they were motivated to go into nursing due to information and advice from practicing nurses (Buerhaus et al., 2005).
There are also several examples of loan forgiveness and scholarship programs in oncology. ASCO’s Loan Repayment Program will pay off up to $70,000 in loans for oncologists who commit to providing cancer care in medically underserved regions of the United States for 2 years (ASCO, 2009). The National Cancer Institute’s (NCI’s) Cure Program is similarly designed to draw underserved minority students into oncology professions by providing promising high school through junior investigator—level individuals with funding opportunities (NCI, 2012a). The National Institutes of Health also has a loan-forgiveness program that will provide payment for up to $35,000 in loans each year for clinical researchers who work to meet critical health needs, including cancer care needs (NIH, 2013).
Retaining professionals with training in cancer care is equally important to recruiting professionals who provide cancer care. The average turnover rate for health care professionals changing their place of employment is around 15 to 20 percent, depending on the region of the country (Jenkins and Fina, 2008; Kosel and Olivo, 2002). The average turnover rate for nurse practitioners and PAs is more than 12 percent; for nurses, 14 percent; and for physicians, around 6 percent (AACN, 2012b; AMGA, 2012).
The first few years are the most important for retention. A study by PricewaterhouseCoopers found that the average annual nursing turnover rate in hospitals was 8 percent, but average annual turnover rate for first-year nurses was 27 percent (PricewaterhouseCoopers, 2007). Factors that influence the retention of health care workers include salary, benefits,
work culture, potential for promotion, and flexible work schedules (IOM, 2009b).
Duke University Hospital is an example of an organization that has instituted extensive programs and policies to retain its health professionals. The hospital offers training programs and educational-assistance programs; orientation, coaching, and mentoring programs for new employees and emerging leaders; and flexible work arrangements. The hospital’s professional development institute allows employees who work part time to be paid for full-time work while they go to school; as a result, the annual turnover rate is 12 percent overall and only around 5 percent for first-year hires, significantly below the average for academic hospitals (IOM, 2009b).
Some health policy experts, however, are concerned that retention efforts like the program at Duke University may be unsustainable and too expensive (May et al., 2006). Thus, additional strategies for retaining professionals who provide cancer care may be needed.
Team-Based Cancer Care
Team-based care is an essential component of high-quality, patient-centered cancer care. It can be defined as “the provision of health services to individuals, families, and/or their communities by at least two health clinicians who work collaboratively with patients and their caregivers—to the extent preferred by each patient—to accomplish shared goals within and across settings to achieve coordinated, high quality care” (Mitchell et al., 2012, p. 5). A white paper published by the IOM recently identified a core set of principles common to high-functioning health care teams (see Box 4-2).
Several literature reviews have found that team-based care can improve health care quality and outcomes (Boult et al., 2009; IOM, 2011c; Naylor et al., 2010). Team-based care can also lead to better care coordination among clinicians by establishing standard practices for transmitting information, communicating, and providing follow-up care (NQF, 2010). Health information technology can be a tool for facilitating the coordination of care between team members and across care settings (see discussion in Chapter 6).
A clinician’s ability to work well in interdisciplinary teams is particularly important in cancer care because, as discussed throughout this chapter, cancer is a complex disease that requires the coordination of multiple professionals to treat and alleviate the symptoms of the disease. It is unlikely that merely increasing the number of oncology professionals will adequately address oncology workforce needs. A number of innovative strategies for organizing the cancer care team and delivering care
BOX 4-2
Principles of Team-Based Health Care
Shared goals: The team—including the patient and, when appropriate, family members or other support persons—works to establish shared goals that reflect patient and family priorities, and can be clearly articulated, understood, and supported by all team members.
Clear roles: There are clear expectations for each team member’s functions, responsibilities, and accountabilities, which optimize the team’s efficiency and often make it possible for the team to take advantage of division of labor, thereby accomplishing more than the sum of its parts.
Mutual trust: Team members earn each other’s trust, creating strong norms of reciprocity and greater opportunities for shared achievement.
Effective communication: The team prioritizes and continuously refines its communication skills. It has consistent channels for candid and complete communication, which are accessed and used by all team members across all settings.
Measurable processes and outcomes: The team agrees on and implements reliable and timely feedback on successes and failures in both the functioning of the team and achievement of the team’s goals. These are used to track and improve performance immediately and over time.
SOURCE: Mitchell et al., 2012.
have been proposed that rely more heavily on team-based care compared to traditional oncology practice, such as collaborative practice arrangements and in survivorship care (see Box 4-3), as well as oncology patient-centered medical homes and accountable care organizations (see discussion in Chapter 8).
In a high-quality cancer care system, all of the professionals involved in a patient’s care should act as a single, coordinated care team. In practice, a patient’s care team will usually be composed of a number of smaller care teams that work in coordination, and an individual with cancer will be treated by a cancer care team and a primary care or geriatrics care team (see Box 4-1), as well as other specialty care teams (e.g., clinicians addressing a patient’s comorbidities) (see Figure 4-1). The committee identified as a goal that all of the members of the cancer care team coordinate with each other and with primary/geriatrics and specialist care teams to implement patients’ care plans and deliver comprehensive, efficient, and patient-centered care (Recommendation 3). The cancer care team
should include all of the clinicians involved in implementing a patient’s care plan, including the clinicians focusing on cancer treatment and those providing psychosocial support and pain management (see Figure 4-2).
There are a number of obstacles to team-based care. A recent IOM report concluded that the “coordination and integration of patient services currently are poor” (IOM, 2012a, p. 24). The sheer number of individuals involved in patients’ care make coordination challenging. For example, patients with Medicare see an average of seven physicians, including five specialists, split among four different practices per year (Pham et al., 2007). The typical primary care physician coordinates with 229 other physicians in 117 different practices in a single year for his or her Medicare patients (Pham et al., 2009). A national survey in 2011 found that around one-quarter of patients reported that their clinicians failed to share important information about test results or medical history with other clinicians involved in their care (Stremikis et al., 2011). Establishing effective care teams requires time and effort, and there are few incentives for health care clinicians to make this investment. Health care organizations often lack the experience and expertise to form clinical teams, and the “siloed” nature of the professionals involved in care creates cultural barriers. Additionally, the health care infrastructure and reimbursement system are not set up to support team-based care (IPEC, 2011b; Mitchell et al., 2012).
Regulatory and policy barriers prevent many of the professionals on cancer care teams from practicing to the full extent of their education and training. The IOM recognized this problem in Crossing the Quality Chasm: A New Health System for the 21st Century (2001), noting that achieving high-quality care will mean modifying the regulation of health professionals, such as scope-of-practice acts and other workforce regulations. More recently, in Future of Nursing: Leading Change, Advancing Health (2011), the IOM found that the regulations defining scope-of-practice limitations for nurses often limit nurses in the types of tasks they are allowed to perform, for reasons unrelated to their ability, education, or training. The report recommended a number of steps to remove scope-of-practice barriers for nurses, including changing Medicare reimbursement policy to cover nursing services and encouraging state legislatures to reform scope-of-practice regulations to conform to model laws (IOM, 2011a).
Policy makers, however, have made limited progress in implementing these recommendations (Iglehart, 2013). Similar changes in federal and state laws will be necessary to enable all members of the cancer care team to be fully functioning, valuable team members. The reimbursement system must also create incentives for engaging all members of the cancer care team to the full extent of their abilities (IOM, 2012a). Thus, the committee recommends that federal and state legislative and regulatory bodies eliminate reimbursement and scope-of-practice barriers
BOX 4-3
Examples of Team-Based Cancer Care
Collaborative Practice Arrangements
Collaborative practice arrangements address the anticipated shortfall of oncologists by expanding the roles of physician assistants and nurse practitioners, also called nonphysician practitioners. The American Society of Clinical Oncology (ASCO) has taken the lead in pursuing this strategy. In 2005, ASCO commissioned the American Association of Medical Colleges to conduct a national survey of oncology practices and their use of nonphysician practitioners (n=226) (AAMC, 2007). Half of the practices reported working with nonphysician practitioners, and more than two-thirds of these practices reported that using nonphysician practitioners benefited their practice by improving patient care, efficiency, and physician satisfaction. In response to this positive feedback, ASCO initiated a pilot program to assess how oncologists can work most efficiently with nonphysician practitioners (Towle et al., 2011). The pilot was conducted in 33 oncology practices that varied in terms of practice size, structure, and geography. These practices submitted data to ASCO on staffing information, volume of patient visits, and expenses, and also completed physician, nonphysician practitioners, and patient surveys. The results of the pilot indicated that patients were aware when an nonphysician practitioner provided their clinical care, and were almost universally satisfied with this arrangement. Both the physicians and nonphysician practitioners were also highly satisfied with their collaborative practice models. Nonphysician practitioners were most productive in sites where they worked with all of the physicians in the practice, as opposed to sites where they worked exclusively with one or more physicians in the practice.
Survivorship Care
Another model of team-based care in oncology is treating patients who no longer require active cancer treatment (e.g., chemotherapy, radiation) in settings out-side of an oncologist’s office. The vast majority of visits to an oncologist’s office are currently for the provision of survivorship care (AAMC, 2007). However, there are a number of other potential sites of care for meeting patients’ survivorship needs.
to team-based care. This could have the added benefit of improving job satisfaction among professionals involved in cancer care as well as the recruitment and retention of oncology professionals.
The new models of payment discussed in Chapter 8, such as bundled payments, accountable care organizations, and oncology patient-centered medical homes, may remove many of the reimbursement barriers to team-based care. These models reward clinicians for providing high-quality of care at lower costs, unlike traditional fee-for-service models that incentivize the volume of services provided and reimburse certain clinicians at
Primary care clinicians often play a significant role in their patients’ surveillance and ongoing survivorship care (Grunfeld et al., 2006; McCabe et al., 2013). In an analysis of Medicare claims data, Earle and Neville (2004) concluded that there is a lack of clarity around the roles of the primary care clinician and oncologist in survivorship care. Approximately 50 percent of cancer survivors in their study saw an oncologist for survivorship care and 8 percent of those saw only an oncologist; 38 percent of survivors saw only a primary care physician; and 46 percent saw both an oncologist and a primary care physician. The patients who saw only a primary care physician were more likely to receive preventive health interventions, but were less likely to receive ongoing cancer surveillance. In contrast, the patients who only saw an oncologist were unlikely to receive preventive care, but did receive follow-up cancer care. Thus, the type of doctor that the patients visited had a significant impact on the type of care that they received. More recently, Snyder and colleagues also found that there is a need to clarify the role of primary care clinicians and oncologists in survivorship care. In their review of the SEER-Medicare database, adults with a history of cancer were most likely to receive appropriate survivorship care and preventive care if they saw both an oncologist and a primary care clinician (Snyder et al., 2008, 2009, 2011).
In order to more effectively transition from acute cancer care to primary care, oncologists and primary care clinicians need to be better coordinated and the role of the primary care clinician in cancer survivorship care needs to be clearly delineated. Care should be tailored to the individual patient based on the type of cancer, treatment intensity, and risk of cancer-related complications. Nurse practitioners can help ease this transition (Oeffinger and McCabe, 2006). At the University of Pennsylvania, for example, the same nurse practitioners meet with patients throughout their cancer treatment and for the duration of a survivorship program. One of the goals of the survivorship program is to develop a treatment summary and care plan that can be used to inform the primary care clinician about the patients’ cancer follow-up needs (Penn Medicine, 2012).
An alternative model of survivorship care relies on nurse practitioners to provide survivorship care. At Memorial-Sloan Kettering Cancer Center, nurse practitioners administer examinations and preventive care, evaluate and manage long-term or late effects of cancer and its treatment, provide cancer screening, and coordinate with each patient’s primary care team through disease-specific survivorship clinics (MSKCC, 2012).
a higher rate than others. Thus, new models of payment may reduce the disincentive for physicians to work together with other clinicians. In addition, several other components of the committee’s conceptual framework will facilitate team-based care. These include care plans, which facilitate coordinated care by summarizing all relevant information into a single location that can be shared among members of the cancer care team, the primary care/geriatrics care team, and other clinicians involved in a patient’s care (see Chapter 3). Shared electronic health records also may
make it easier for clinicians to communicate, share information, and provide coordinated care (see Chapter 6).
Interprofessional Education
Interprofessional education is designed to teach health professionals how to engage in teamwork and improve individuals’ abilities to work in interdisciplinary environments. It occurs “when students from two or more professions learn about, from, and with each other to enable effective collaboration and improve health outcomes” (WHO, 2010, p. 7). The Pew Health Professions Commission identified working with interdisciplinary teams as one of the key competencies for all health professionals in the 21st century (PHPC, 1998). Six professional organizations formed the Interprofessional Education Collaboration to develop and endorse competencies in interdisciplinary care, including the American Association of Colleges of Osteopathic Medicine, AAMC, AACN, the American Association of Colleges of Pharmacy, the American Dental Education Association, and the Association of Schools of Public Health (IPEC, 2011a). Interprofessional education is also consistent with the vision statement included in a previous IOM report on health professional education, which stated that “all health professionals should be educated to deliver patient-centered care as members of an interdisciplinary team, emphasizing evidence-based practice, quality improvement approaches, and informatics” (IOM, 2003b, p. 45).
The majority of health professional education is currently conducted in silos where professional students are isolated from each other based on the professional degree they are pursuing. However, a growing number of universities are undertaking efforts to develop successful interprofessional education programs (see Box 4-4 for several examples) (IOM, 2013; NHPF, 2011). Some universities are even establishing interprofessional education programs that involve the collaboration of multiple institutions. For example, Hunter College, which offers coursework in nursing, public health, and social work, has partnered with Weill Cornell College of Medicine to offer a full range of interprofessional classes (JMF, 2013; Thibault and Schoenbaum, 2013).
As the delivery of cancer care becomes more team based, academic institutions and professional societies should develop interprofessional education programs to train the workforce in team-based cancer care and promote coordination with primary/geriatrics and specialist care teams. These programs could be provided by academic institutions or by oncology, geriatric, and primary care/internal medicine professional societies, and should target both current and future workforces.
Additional research is needed to identify the most effective methods
BOX 4-4
Examples of Interprofessional Educational Programs
Rush University Medical Center’s Geriatric Integrated Team Training Program
Rush University Medical Center’s Geriatric Integrated Team Training Program provides interprofessional training in the care of older adults for students from 12 different disciplines, including medicine, nursing, social work, and pharmacy. In this program, interprofessional classes meet weekly for 3 hours and students are placed in clinical settings that offer interprofessional practice opportunities. The program has received positive alumni feedback regarding job placements and subsequent team performance.
University of Colorado’s Interprofessional Educational Program
The University of Colorado’s interprofessional educational program consists of two major components: (1) the Realizing Educational Advancement for Collaborative Health (REACH) program and (2) the Frontier Center Project. In the REACH program, all health professional students participate in a longitudinal curriculum that integrates preclinical and clinical training, and helps students develop competencies in teamwork, communication, collaborative interprofessional practice, quality, and safety. Hoping to “forge a new link between dentistry and medicine for better patient care,” the Frontier Center Project provides educational and clinical activities to students from a variety of disciplines. Its activities are designed to focus on oral health and preventive practices in primary care.
of aligning interprofessional education programs with health care delivering organizations to advance team-based cancer care (Thibault and Schoenbaum, 2013). Fortunately, the Health Resources and Services Administration’s Coordinating Center for Interprofessional Education and Collaborative Practice is currently providing financial support for efforts to develop successful interprofessional educational programs (HRSA, 2013). A number of private foundations have also pledged additional resources to this coordinating center (Thibault and Schoenbaum, 2013).
It is possible that the predicted workforce shortages may persist and create an obstacle to high-quality cancer care, even in an environment of interprofessional, team-based cancer care. The National Workforce Commission is charged with collecting health workforce data to predict future workforce needs. The committee recommends that Congress fund this Commission, and that the Commission take into account the aging population, the increasing incidence of cancer, and the complexity of cancer care in this planning.
University of Minnesota’s 1Health Program
The University of Minnesota’s 1Health Program is an interprofessional program that gives students an opportunity to learn from and interact with their counter-parts from other health disciplines. This program consists of three phases: (1) orientation, (2) necessary skills, and (3) expertise in practice. Over the course of these three phases, students from a variety of disciplines meet in six moderated, face-to-face interprofessional groups, participate in workshops geared toward developing the skills necessary for interprofessional collaboration, and engage with community-based partners while applying the concepts of interprofessional collaboration. While this program is still evolving, it has already received positive feedback from alumni.
University of Washington’s Center for Health Science Interprofessional Education, Research, and Practice
The University of Washington’s Center for Health Science Interprofessional Education, Research, and Practice provides educational opportunities for students to develop interprofessional skills and for faculty to be leaders and facilitators of interprofessional education. The goal is to integrate interprofessional educational content into existing core health sciences curriculum, expand student access to opportunities to become involved in collaborative practice, and build facilities that encourage formal and informal interprofessional interactions.
SOURCES: RUMC, 2012; UMN, 2013; University of Colorado, 2013a,b; UW, 2012, 2013.
Training the Workforce That Cares for Patients with Cancer
Training the workforce that cares for patients with cancer to ensure appropriate skills, knowledge, and experiences is a key component of ensuring the quality of cancer care. Professionals trained in oncology and nononcology professionals who often provide care to patients with cancer need distinct sets of skills. The committee identified as a goal that all individuals caring for patients with cancer have appropriate core competencies (Recommendation 4). To achieve this, professional organizations that represent clinicians who care for patients with cancer should define cancer core competencies for their memberships. In addition, professionals caring for patients with cancer should be able to respond to the changing demographics in the United States. The committee strongly endorses the IOM’s previous recommendation that the “maintenance of certification for health care professionals should include demonstration of competence in the care of older adults as a criterion” (IOM, 2008b, p. 9).
Competencies for the Members of the Cancer Care Team
Cancer care delivery organizations should require that members of the cancer care team have the necessary competencies to deliver high-quality cancer care, as demonstrated through training, certification, or credentials. These competencies should include all of the components of the committee’s conceptual framework for high-quality cancer care, such as
• Providing patient-centered communication in order to support all patients and caregivers in making informed medical decisions that are consistent with their needs, values, and preferences, and documenting these decisions in each patient’s care plan; this includes communicating about advance care planning and end-of-life decisions (see Chapter 3)
• Working in interprofessional care teams and coordinating with other care teams (see discussion above in the section on team-based cancer care)
• Demonstrating knowledge about established and evolving clinical and health services research (see Chapter 5)
• Participating in a learning health care system for cancer and using advancements in information technology to improve cancer care delivery and health outcomes (see Chapter 6)
• Investigating and evaluating care practices, translating knowledge gained from research into the delivery of patient care, and improving patient care practices (see Chapter 7)
• Understanding how the larger health care system influences the accessibility and affordability of cancer care (see Chapter 8)
Core Competencies for Nononcology Clinicians
Primary care clinicians and other medical and surgical specialists—such as urologists, pulmonologists, dermatologists, and gynecologists, who have not spent years training in oncology—provide much of the cancer care in the United States. Facilitating the development of core competencies among these professionals can improve their basic skills and knowledge about cancer that are essential for delivering high-quality cancer care. For example, C-Change has started a Cancer Core Competency Initiative to develop a web-based toolkit that other organizations can use to create programs in cancer core competencies (C-Change, 2012). The tools can be applied to a wide variety of disciplines, including medicine, nursing, social work, and public health, and can be used to educate individuals with varying levels of experience and expertise. Several pilot
programs have demonstrated measurable improvement in participants’ knowledge, skills, and attitudes after using C-Change’s toolkit (Cox et al., 2012; Smith et al., 2009).
The potential of these programs to improve the health care workforce’s knowledge of basic cancer care is enormous. For example, there are only 21,000 oncology-certified nurses. However, there are close to 3 million RNs in this country, many of whom work with cancer patients and cancer survivors. If a larger proportion of these 3 million nurses had basic knowledge about cancer care, the health care system would be better equipped to meet the needs of people at risk of or living with cancer (C-Change, 2012). It would also be beneficial if other specialists understood, for example, the effects of chemotherapy on cardiac, pulmonary, and endocrine systems, and the interactions of treatment for cancer with many noncancer care treatments. Thus, the committee recommends that organizations responsible for accreditation, certification, and training of nononcology clinicians promote the development of relevant core competencies across the cancer care continuum.
Training in core competencies can take place during academic training, continuing education programs, or work-site training programs. The relevant professional organizations representing primary care clinicians and other medical specialists who work in oncology should define the cancer core competencies for these workforces. In order to ensure that members of the cancer care team have core competencies in other relevant fields, professional organizations representing nononcology clinicians should reciprocate by sharing tools and information about their specialties with the cancer care community.
Telemedicine in Cancer Care
Telemedicine or telehealth is “the use of electronic information and communications technologies to provide and support health care when distance separates participants” (IOM, 1996, p. 1). Increasing the use of telemedicine in cancer care may help to address the projected workforce shortages and ensure that patients with cancer have access to clinicians with the necessary expertise. Telemedicine’s potential to improve access to high-quality care is especially great for patients living in rural, vulnerable, or underserved communities (IOM, 2012d).
There are a number of ongoing initiatives that are exploring the potential of telemedicine to improve the quality of care. The Centers for Medicare & Medicaid Services (CMS) Innovation Center has awarded several grants for innovative telehealth programs targeted at Medicare- and Medicaid-eligible populations (CMS, 2013). For example, the University of New Mexico received a grant for its Extension for Community Health-
care Outcomes (ECHO) program, which is using telemedicine to educate clinicians and bring expertise to rural communities (UNM, 2013). The Veterans Health Administration has also invested significant resources in adopting telehealth strategies. It currently operates the world’s largest telehealth program and serves more than 50,000 veterans (VHA, 2012).
There have been a number of clinical trials, pilot programs, and other initiatives that utilize telehealth to improve care for patients with cancer. Examples include programs in the areas of managing patient risk, addressing treatment-related dermatologic toxicities, managing pain and depression, monitoring long-term side effects of treatment, providing genetic counseling, and treating patients in rural areas (Gibelli et al., 2008; Gordon, 2012; Hitt et al., 2013; Kroenke et al., 2010; MacDonald et al., 2010; Pruthi et al., 2013; Zilliacus et al., 2011). Telemedicine is also being applied in radiology and pathology, where images can easily be captured digitally and read by clinicians at off-site locations (IOM, 2012d). As discussed in Chapter 8, the committee recommends that CMS and other payers evaluate new models of care delivery and payment for cancer care, which could include telemedicine.
There are a number of obstacles to the widespread use of telemedicine, however, that will need to be addressed in order for it to reach its full potential. One of the major obstacles is reimbursement policies. Medicare and Medicaid both place restrictions on telehealth coverage based on the patient populations, clinicians, sites of care, and services.3 For example, Medicare Part B only reimburses patients living in rural areas for telehealth services.4 In addition, few states have laws requiring private health insurance plans to cover telehealth services. As a result, there is great variability in what services are reimbursable (NCSL, 2013).
Professional licensure is another obstacle to telemedicine. As mentioned above, many clinicians are required to be licensed by the state where they practice. This limits the ability of telehealth programs to cross state lines. Similarly, many state medical boards require in-person consultations before initiating telemedicine services, further limiting the potential geographic reach of telemedicine programs (IOM, 2012d).
Caregivers, including family caregivers and direct care workers, are critical members of the cancer care team. The IOM has defined family caregivers (also called informal caregivers) as “relatives, friends, or neigh-
________________
3 Medicare, Medicaid, and SCHIP Benefits Improvement and Protection Act of 2000, Public Law 554, 106th Cong., 2nd sess. (December 21, 2000).
4 Social Security Act § 1395m(m)(4)(C).
bors who provide assistance related to an underlying physical or mental disability, but who are unpaid for those services” (IOM, 2008b, p. 247). Direct care workers are the primary clinicians of paid hands-on care, and they include nurse aides, home health aides, and personal and home care aides (IOM, 2008b). Both family caregivers and direct care workers are particularly important in cancer care because of the debilitating effect of the disease; the side effects associated with many of the common cancer treatments; the complexity of the medical decisions; and the ongoing need for medical treatment, home care, and surveillance. The fragmented nature of the current cancer care delivery system, which requires individuals to take the lead in coordinating their own care, furthers the importance of caregivers.
Family Caregivers
In Retooling for an Aging America: Building the Health Care Workforce, family caregivers were characterized as “the backbone for much of the care that is received by older adults in the United States” (IOM, 2008b, p. 241). Between 2008 and 2009, approximately 65.7 million people served as unpaid family caregivers, and on average, they spent approximately 20 hours each week providing care (NAC and AARP, 2009). Live-in caregivers often provide more intensive care and can spend around 40 hours per week providing care, equal to time spent in a full-time job (NAC and AARP, 2009). The overall burden of care is considered high for 32 percent of caregivers, moderate for 19 percent of caregivers, and relatively low for 46 percent of caregivers (NAC and AARP, 2009). Many individuals providing family caregiving serve in this role for an extended period of time, with the average length of time being 4.6 years. Thirty-one percent of family caregivers have provided care for 5 years or more (NAC and AARP, 2009).
The demographic trends of family caregivers are similar to the trends in the general population. Family caregivers and their care recipients are now older than their counterparts were 5 years ago. The average age of individuals caring for adults has increased from 46.4 to 49.2 years of age. The average age of a person receiving help from a caregiver has also increased from 66.5 to 69.3 years over the past 5 years. The majority of caregivers are female (NAC and AARP, 2009).
Distance caregiving, or providing care remotely, is an increasingly common alternative to the more familiar caregiving models where the care recipient and caregiver(s) live nearby or in the same household.
Approximately 5 to 7 million Americans act as distant caregivers,5 a statistic expected to double by 2022 (Benefield and Beck, 2007). Examples of common support provided by distance caregivers include ensuring the coordination of care, maintenance of independence, and socialization.
Serving as a family caregiver can be a rewarding experience. Although few studies have examined the benefits of caregiving for the care provider, existing research suggests that the experience of caring for an individual with cancer leads to personal growth, an improved sense of self-worth, a deepening of the relationship with the cancer patient, the discovery of personal strength and mastery, and a greater appreciation for life and family (NCI, 2012b; Sanjo et al., 2009). Caregivers are more likely to report a positive experience if they receive psychological support, the care team validates the care they are providing, and health care professionals assist in solving any problems that arise with the care recipient (Haley, 2003; Kim et al., 2007).
Caregiving, however, can also have a negative impact on the quality of life, health, and well-being of the care provider (Girgis et al., 2013). Family caregivers are required to balance the competing demands of providing care and meeting all of their other obligations. There are serious financial repercussions of serving as a caregiver, which may include the burden of insurance deductibles, copayments, and uncovered services (e.g., transportation, home care) (NCI, 2012b). There is also the cost of taking the time to provide the needed care, such as helping with transportation for medical appointments, waiting with the patient for appointments, preparing for surgery and medical procedures, visiting the hospital, and addressing insurance issues (Glajchen, 2009; NCI, 2012b). This can lead to missed work, reduced wages, and disruptions in family and friendships.
Many caregivers experience social isolation due to the lack of time they spend on their usual activities and relationships. Caregivers are also prone to neglecting their own health by not getting enough sleep or exercise (NCI, 2012b). In addition, caregivers are likely to experience distress from witnessing someone close to them suffer, with some studies suggesting that caregivers may experience the same level of distress as patients (Hodges et al., 2005; Weitzner et al., 1999).
Direct Care Workers
Direct care work is the fastest-growing job in the United States due to the aging population’s need for in-home care. In 2008, there were approximately 3 million individuals serving as direct care workers in
________________
5 Distant caregivers are defined as individuals who live at least an hour from the care recipient.
the United States (Hess and Henrici, 2013). The size of this workforce is expected to increase by 70 percent between 2010 and 2020 (BLS, 2013a). The workforce is predominantly female and includes many individuals who are racial or ethnic minorities. A study from the Institute for Women’s Policy Research estimated that immigrants make up approximately 28 percent of the workforce, with around 20 percent being undocumented (Hess and Henrici, 2013). There are no formal education requirements for most of these workers and most training takes place on the job (BLS, 2013a).
Serving as a direct care worker is a physically and emotionally demanding job that is poorly rewarded. Direct care workers have higher than average work-related injuries due to overexertion during the care of patients (BLS, 2013a; Burnham and Theodore, 2012). At the same time, the average hourly salary is only $9.70, or approximately $20,000 per year (BLS, 2013a). Many individuals work part time and do not get benefits (Burnham and Theodore, 2012). More than 40 percent rely on public assistance programs, such as Medicaid or food stamps (Kurtz, 2013).
A primary reason for the low salaries is that many direct care workers are exempt from federal minimum wage and overtime laws, due to a provision in the Fair Labor Standards Act of 1974. In 2011, the Department of Labor issued a Notice of Proposed Rulemaking to amend this law; however, the health care industry has blocked any changes (DOL, 2012). A survey by the National Domestic Workers Alliance found that almost one-quarter of direct care workers are still paid wages less than those required by state minimum wage laws (Burnham and Theodore, 2012).
Integration with the Cancer Care Team
Caregivers may provide assistance at any point in the continuum of cancer care, starting with diagnosis, treatment, palliative care, survivorship, through the end-of-life phases of cancer care. They may assist with various patient responsibilities, such as taking medication, managing symptoms, ensuring adherence to care plans, running errands, paying bills, providing emotional support, coordinating care, monitoring use of medical devices, and communicating with clinicians. They may also assist with activities of daily living including bathing, dressing, feeding, and toileting. In addition, many of the tasks these individuals provide require physical activity, such as lifting, positioning, and transferring the care recipient.
To successfully provide care, these individuals may have to rely on an expansive set of everyday skills (e.g., planning, interpreting, decision making, problem solving, time management, accessing resources). They
must also learn new skills (e.g., negotiating with the health care system and providing hands-on direct care). Medical skills that many caregivers learn include administering intravenous infusions and injections, providing wound care, using feeding tubes, running mechanical ventilators, and gaining knowledge of specialty pharmacies and medications (Given, 2011; Reinhard and Levine, 2012).
It is equally important that the cancer care team communicate as effectively with a patient’s caregivers as with the patient. In Crossing the Quality Chasm, the IOM committee recognized that clinicians should “focus on accommodating family and friends on whom patients may rely, involving them as appropriate in decision making, supporting them as caregivers, making them welcome and comfortable in the care delivery setting, and recognizing their needs and contributions” (IOM, 2001, p. 50).
The cancer care team often does not know the best methods for better involving caregivers, but it should make an effort to incorporate caregivers in decision-making processes. Family caregivers and direct care workers often have different informational needs and ways of communicating (e.g., technological sophistication) compared to the patient, and there are sometimes conflicting values and preferences between patients and family caregivers (IOM, 2011c). Any incongruence between the patient and family caregiver will need to be addressed by the care team to ensure the quality of care and an ongoing beneficial caregiving relationship. Ultimately, it is the patient’s values, preferences, and needs that should dictate the care plan (Gillick, 2013).
A lack of available training and support makes the task of integrating caregivers with the cancer care team challenging. Caregivers are regularly asked to perform a number of tasks for which they may feel unprepared. For example, a survey by Reinhard and Levine (2012) found that almost half of family caregivers report performing medical/nursing tasks but the majority reported that they had received little or no training (Reinhard and Levine, 2012). Similarly, many direct care workers have no more than a high school education and report that they could benefit from further training (Menne et al., 2007; Montgomery et al., 2005; Smith and Baughman, 2007). Instructions on how to perform basic care tasks, as well as education and informational resources, could improve patient care and reduce the stress and burden placed on caregivers.
There are a few programs that support research, training, and pilot programs to increase knowledge and test approaches to assist caregivers (HJWF, 2013; RCIC, 2013; VA, 2013). The IOM committee on Retooling for an Aging America recognized a growing need in this area and recommended further education and training for both direct care workers and family caregivers (IOM, 2008b). More recently, Naylor (2012) recom-
mended prioritizing research on the best methods of training family caregivers and direct care workers to be integrated members of care teams. The committee echoes these findings and recommends that HHS and other funders support demonstration projects to train family caregivers and direct care workers in relevant core competencies related to caring for cancer patients.
Specific areas in cancer care where additional information could be helpful are the disease trajectory, the anticipated course of treatment, and the management of pain, weakness, and fatigue (Wong et al., 2002). Caregivers’ informational and training needs change depending on the point in the cancer care continuum. Periods when trainings should be administered include at diagnosis, during hospitalization, at the start of new treatments, at recurrence, and during end-of-life care (McCorkle and Pasacreta, 2001).
A diverse team of professionals provides cancer care, reflecting the complexity of the disease, its treatments, and survivorship care. These teams include professionals with specialized training in oncology, such as medical, surgical, and radiation oncologists and oncology nurses, as well as other specialists and primary care clinicians. In addition, family caregivers (e.g., relatives, friends, and neighbors) and direct care workers (e.g., nurse aides, home health aides, and personal and home care aides) provide a great deal of care to cancer patients. Patients, at the center of the committee’s conceptual framework, are encircled by the workforce (see Figure S-2), depicting the idea that high-quality cancer care depends on the workforce providing competent, trusted interprofessional care that is aligned with patients’ needs, values, and preferences. To achieve this standard, the workforce must include adequate numbers of health clinicians with training in oncology. New models of interprofessional, team-based care are an effective mechanism of responding to the existing workforce shortages and demographic changes, as well as in promoting coordinated and patient-centered care.
Recommendation 3: An Adequately Staffed, Trained, and Coordinated Workforce
Goal: Members of the cancer care team should coordinate with each other and with primary/geriatrics and specialist care teams to implement patients’ care plans and deliver comprehensive, efficient, and patient-centered care.
To accomplish this:
• Federal and state legislative and regulatory bodies should eliminate reimbursement and scope-of-practice barriers to team-based care.
• Academic institutions and professional societies should develop interprofessional education programs to train the workforce in team-based cancer care and promote coordination with primary/geriatrics and specialist care teams.
• Congress should fund the National Workforce Commission, which should take into account the aging population, the increasing incidence of cancer, and the complexity of cancer care, when planning for national workforce needs.
The workforce must also have the distinct set of skills necessary to implement the committee’s conceptual framework for a high-quality cancer care delivery system. The recent IOM report Retooling for an Aging America: Building the Health Care Workforce recommended enhancing the geriatric competency of the general health care workforce. The committee endorses this recommendation as it is especially important to cancer care, where the majority of patients are older adults. Currently, many clinicians also lack essential cancer core competencies.
Recommendation 4: An Adequately Staffed, Trained, and Coordinated Workforce
Goal: All individuals caring for cancer patients should have appropriate core competencies.
To accomplish this:
• Professional organizations that represent clinicians who care for patients with cancer should define cancer core competencies for their memberships.
• Cancer care delivery organizations should require that the members of the cancer care team have the necessary competencies to deliver high-quality cancer care, as demonstrated through training, certification, or credentials.
• Organizations responsible for accreditation, certification, and training of nononcology clinicians should promote the development of relevant core competencies across the cancer care continuum.
• The U.S. Department of Health and Human Services and other funders should fund demonstration projects to train family caregivers and direct care workers in relevant core competencies related to caring for cancer patients.
AACN (American Association of Colleges of Nursing). 2008. Enrollment growth in U.S. Nursing colleges and universities hits an 8-year low according to new data released by AACN. http://www.apps.aacn.nche.edu/Media/NewsReleases/2008/EnrlGrowth.html (accessed January 9, 2009).
———. 2010. Shortage of faculty and resource constraints hinder growth in U.S. nursing schools according to the latest AACN data. http://www.aacn.nche.edu/news/articles/2010/faculty-shortage (accessed June 18, 2013).
———. 2011. 2011 annual report: Shaping the future of nursing education. http://www.aacn.nche.edu/aacn-publications/annual-reports/AR2011.pdf (accessed June 18, 2013).
———. 2012a. New AACN data show an enrollment surge in baccalaureate and graduate programs amid calls for more highly educated nurses. http://www.aacn.nche.edu/news/articles/2012/enrollment-data (accessed September 10, 2012).
———. 2012b. Nursing shortage fact sheet. http://www.aacn.nche.edu/media-relations/factsheets/nursing-shortage (accessed September 20, 2012).
———. 2013. Dnp fact sheet. http://www.aacn.nche.edu/media-relations/fact-sheets/dnp (accessed April 18, 2013).
AAFP (American Academy of Family Physicians). 2012. Primary care. http://www.aafp.org/online/en/home/policy/policies/p/primarycare.html#Parsys0004 (accessed September 7, 2012).
AAHC (Association of Academic Health Centers). 2008. Out of order, out of time: The state of the nation’s health workforce. http://www.aahcdc.org/policy/AAHC_OutofTime_4WEB.pdf (accessed September 19, 2012).
AAMC (Association of American Medical Colleges). 2007. Forecasting the supply of and demand for oncologists: A report to the American Society of Clinical Oncology from the AAMC Center for Workforce Studies. http://www.asco.org/ASCO/Downloads/Cancer%20Research/Oncology%20Workforce%20Report%20FINAL.pdf (accessed January 14, 2009).
———. 2008. 2008 physician specialty data. https://www.aamc.org/download/47352/data/specialtydata.pdf (accessed September 7, 2012).
———. 2010. Diversity in the physician workforce: Facts & figures 2010. https://members.aamc.org/eweb/DynamicPage.aspx?Action=Add&ObjectKeyFrom=1A83491A-9853-4C87-86A4-F7D95601C2E2&WebCode=PubDetailAdd&DoNotSave=yes&ParentObject=CentralizedOrderEntry&ParentDataObject=Invoice+Detail&ivd_formkey=69202792-63d7-4ba2-bf4e-a0da41270555&ivd_prc_prd_key=A6A4AF05-91F1-47EC-9842-F60CB45F2356 (accessed March 21, 2013).
———. 2011a. For second year, more U.S. Medical school seniors match to primary care residencies. https://www.aamc.org/newsroom/newsreleases/2011/180410/110317.html (accessed September 7, 2012).
———. 2011b. Physician shortages factsheet. https://www.aamc.org/download/150584/data/physician_shortages_factsheet.pdf (accessed September 6, 2012).
———. 2013. Policies targeted toward aging physicians may keep doctors working longer, smarter. https://www.aamc.org/newsroom/reporter/april2013/334334/agingphysicians.html (accessed June 18, 2013).
AAPA (American Academy of Physician Assistants). 2012a. Quick facts. http://www.aapa.org/the_pa_profession/quick_facts/resources/item.aspx?id=3840 (accessed September 10, 2012).
———. 2012b. What is a PA? http://www.aapa.org/the_pa_profession/what_is_a_pa.aspx (accessed September 10, 2012).
ABIM (American Board of Internal Medicine). 2012. Candidates certified—all candidates. http://www.abim.org/pdf/data-candidates-certified/all-candidates.pdf (accessed October 22, 2012).
ACCP (American College of Chest Physicians). 2012. ACCP: The global leader in clinical chest medicine. http://www.chestnet.org/accp/accp-global-leader-clinical-chest-medicine (accessed October 22, 2012).
ACG (American College of Gastroenterology). 2012. Membership. http://gi.org/membership (accessed October 22, 2012).
ACOG (American Congress of Obstetricians and Gynecologists). 2011. ACOG workforce fact sheet. http://www.acog.org/~/media/Departments/Government%20Relations%20and%20Outreach/WF2011CO.pdf?dmc=1&ts=20120918T1601427427 (accessed September 18, 2012).
ACR (American College of Radiology). 2012. About us. http://www.acr.org/About-Us (accessed September 18, 2012).
ACS/HPRI (American College of Surgeons/Health Policy Research Institute). 2010. The surgical workforce in the United States: Profile and recent trends. http://www.acshpri.org/documents/ACSHPRI_Surgical_Workforce_in_US_apr2010.pdf (accessed October 22, 2012).
AGA (American Gastroenterological Association). 2012. About AGA. http://www.gastro.org/about-aga (accessed October 22, 2012).
AGS (American Geriatrics Society). 2012. Frequently asked questions about geriatrics. http://www.americangeriatrics.org/advocacy_public_policy/gwps/gwps_faqs (accessed October 18, 2013).
AHR (Alliance for Health Reform). 2012a. Health care workforce: Nurses. http://www.allhealth.org/publications/Cost_of_health_care/Nursing_Toolkit_FINAL_8-27-12_111.pdf (accessed September 10, 2012).
———. 2012b. A toolkit: The physician workforce. http://allhealth.org/publications/Physician_Workforce_Shortage_110.pdf (accessed September 6, 2012).
AHRQ (Agency for Healthcare Research and Quality). 2004. Hospital nurse staffing and quality of care. http://www.ahrq.gov/research/findings/factsheets/services/nursestaffing/index.html (accessed May 9, 2013).
Aiken, L. H., S. P. Clarke, D. M. Sloane, J. A. Sochalski, R. Busse, H. Clarke, P. Giovannetti, J. Hunt, A. M. Rafferty, and J. Shamian. 2001. Nurses’ reports on hospital care in five countries. Health Affairs (Millwood) 20(3):43-53.
Aiken, L. H., D. M. Sloane, J. P. Cimiotti, S. P. Clarke, L. Flynn, J. A. Seago, J. Spetz, and H. L. Smith. 2010. Implications of the California nurse staffing mandate for other states. Health Service Research 45(4):904-921.
Alesi, E. R., D. Fletcher, C. Muir, R. Beveridge, and T. J. Smith. 2011. Palliative care and oncology partnerships in real practice. Oncology 25(13):1287-1290, 1287-1290, 1292-1293.
Alfano, C. M., P. A. Ganz, J. H. Rowland, and E. E. Hahn. 2012. Cancer survivorship and cancer rehabilitation: Revitalizing the link. Journal of Clinical Oncology 30(9):904-906.
Allegra, C. J., R. Hall, and G. Yothers. 2005. Prevalence of burnout in the U.S. oncology community: Results of a 2003 survey. Journal of Oncology Practice 1(4):140-147.
American Psychiatric Association. 2013. About APA & psychiatry. http://www.psychiatry.org/about-apa--psychiatry (accessed July 31, 2013).
AMGA (American Medical Group Association). 2012. Survey reveals physician shortage challenges medical groups and increases demand for advanced practitioners. http://www.amga.org/AboutAMGA/News/article_news.asp?k=569 (accessed September 20, 2012).
AMN Healthcare. 2012. 2012 survey of registered nurses: Job satisfaction and career patterns and trajectories. http://www.amnhealthcare.com/uploadedFiles/MainSite/Content/Healthcare_Industry_Insights/Industry_Research/AMN%202012%20RN%20Survey.pdf (accessed June 18, 2013).
ANA (American Nurses Association). 2012. What is nursing ? http://www.nursingworld.org/EspeciallyForYou/What-is-Nursing (accessed September 7, 2012).
AOSW (Association of Oncology Social Work). 2013. About us. http://www.aosw.org/html/about.php (accessed February 28, 2013).
APA (American Psychological Association). 2013a. Breast cancer. http://www.apa.org/health-reform/breast-cancer.html (accessed August 16, 2013).
———. 2013b. Public description of clinical psychology. http://www.apa.org/ed/graduate/specialize/clinical.aspx/specialize/clinical.aspx (accessed July 31, 2013).
———. 2013c. Recognized specialties and proficiencies in professional psychology. http://www.apa.org/ed/graduate/specialize/recognized.aspx (accessed July 31, 2013).
Arehart-Treichel, J. 2012. Cancer patients have much to gain from psychiatric treatment. http://psychnews.psychiatryonline.org/newsarticle.aspx?articleid=1032923 (accessed August 16, 2013).
ASCO (American Society of Clinical Oncology). 2009. ASCO announces new program designed to increase workforce diversity and reduce cancer care disparities. Journal of Oncology Practice 5(6):315-317.
ASCP (American Society for Clinical Pathology). 2004. The medical laboratory personnel shortage. http://www.ascp.org/pdf/MedicalLaboratoryPersonnelShortage.aspx (accessed January 13, 2009).
ASH (American Society of Hematology). 2011. About ASH. http://www.hematology.org/About-ASH (accessed November 9, 2012).
ASHP (American Society of Health-System Pharmacists). 2007. ASHP pharmacy staffing survey results. http://www.ashp.org/DocLibrary/Policy/WorkFrorce/PPM_2007StaffSurvey.pdf (accessed January 15, 2009).
———. 2008. Confronting the public health workforce crisis. http://www.asph.org/document.cfm?page=1038 (accessed January 14, 2009).
ASTRO (American Society for Radiation Oncology). 2012a. About ASTRO. https://www.astro.org/About-ASTRO/Index.aspx (accessed September 18, 2012).
———. 2012b. ASTRO’s 2012 workforce survey. https://www.astro.org/Research/Initiatives/ASTRO-Workforce-Survey.aspx (accessed October 24, 2012).
Auerbach, D. I., P. I. Buerhaus, and D. O. Staiger. 2011. Registered nurse supply grows faster than projected amid surge in new entrants ages 23–26. Health Affairs (Millwood) 30(12):2286-2292.
Bajorin, D. F., and A. Hanley. 2011. The study of collaborative practice arrangements: Where do we go from here? Journal of Clinical Oncology 29(27):3599-3600.
Balboni, M. J., A. Sullivan, A. Amobi, A. C. Phelps, D. P. Gorman, A. Zollfrank, J. R. Peteet, H. G. Prigerson, T. J. Vanderweele, and T. A. Balboni. 2013. Why is spiritual care infrequent at the end of life? Spiritual care perceptions among patients, nurses, and physicians and the role of training. Journal of Clinical Oncology 31(4):461-467.
Balboni, T. A., M. E. Paulk, M. J. Balboni, A. C. Phelps, E. T. Loggers, A. A. Wright, S. D. Block, E. F. Lewis, J. R. Peteet, and H. G. Prigerson. 2010. Provision of spiritual care to patients with advanced cancer: Associations with medical care and quality of life near death. Journal of Clinical Oncology 28(3):445-452.
Balboni, T., M. Balboni, M. E. Paulk, A. Phelps, A. Wright, J. Peteet, S. Block, C. Lathan, T. Vanderweele, and H. Prigerson. 2011. Support of cancer patients’ spiritual needs and associations with medical care costs at the end of life. Cancer 117(23):5383-5391.
Barraclough, J. E. 1997. Psycho-oncology and the role of the psychiatrist in cancer patient care. International Journal of Psychiatry in Clinical Practice 1:189-195.
Benefield, L. E., and C. Beck. 2007. Reducing the distance in distance-caregiving by technology innovation. Clinical Interventions in Aging 2(2):267-272.
Bennett, J. M., W. J. Hall, D. Sahasrabudhe, and L. Balducci. 2010. Enhancing geriatric oncology training to care for elders: A clinical initiative with long term follow-up. Journal of Geriatric Oncology 1(1):4-12.
Berlin, L. E., and K. R. Sechrist. 2002. The shortage of doctorally prepared nursing faculty: A dire situation. Nursing Outlook 50(2):50-56.
Blegen, M. A., C. J. Goode, J. Spetz, T. Vaughn, and S. H. Park. 2011. Nurse staffing effects on patient outcomes: Safety-net and non-safety-net hospitals. Medical Care 49(4):406-414.
BLS (Bureau of Labor Statistics). 2012a. Economic and employment projections. http://www.bls.gov/news.release/ecopro.toc.htm (accessed September 10, 2012).
———. 2012b. Occupational employment and wages, May 2012. 29-1066 Psychiatrists. http://www.bls.gov/oes/current/oes291066.htm#nat (accessed July 31, 2013).
———. 2013a. Occupational outlook handbook, 2012-13 edition, home health and personal care aides. http://www.bls.gov/ooh/healthcare/home-health-and-personal-care-aides.htm (accessed March 21, 2013).
———. 2013b. Occupational outlook handbook, 2012-13 edition, occupational therapists. http://www.bls.gov/ooh/healthcare/occupational-therapists.htm (accessed April 29, 2013).
———. 2013c. Occupational outlook handbook, 2012-13 edition, pharmacists. http://www.bls.gov/ooh/Healthcare/Pharmacists.htm#tab-1 (accessed July 31, 2013).
———. 2013d. Occupational outlook handbook, 2012-13 edition, physical therapists. http://www.bls.gov/ooh/healthcare/physical-therapists.htm (accessed April 29, 2013).
———. 2013e. Occupational outlook handbook, 2012-13 edition, psychologists. http://www.bls.gov/ooh/Life-Physical-and-Social-Science/Psychologists.htm (accessed July 31, 2013).
———. 2013f. Occupational outlook handbook, 2012-13 edition, social workers. http://www.bls.gov/ooh/Community-and-Social-Service/Social-workers.htm (accessed February 28, 2013).
Blum, D., E. Clark, P. Jacobsen, J. Holland, M. J. Monahan, and P. D. Duquette. 2006. Building community-based short-term psychosocial counseling capacity for cancer patients and their families: The individual cancer assistance network (ICAN) model. Social Work in Health Care 43(4):71-83.
Boult, C., A. F. Green, L. B. Boult, J. T. Pacala, C. Snyder, and B. Leff. 2009. Successful models of comprehensive care for older adults with chronic conditions: Evidence for the Institute of Medicine’s “Retooling for an aging America” report. Journal of the American Geriatrics Society 57(12):2328-2337.
Buerhaus, P., K. Donelan, L. Norman, and R. Dittus. 2005. Nursing students’ perceptions of a career in nursing and impact of a national campaign designed to attract people into the nursing profession. Journal of Professional Nursing 21(2):75-83.
Buerhaus, P. I., D. I. Auerbach, and D. O. Staiger. 2009. The recent surge in nurse employment: Causes and implications. Health Affairs (Millwood) 28(4):w657-w668.
Burnham, L., and N. Theodore. 2012. Home economics: The invisible and unregulated world of domestic work. http://www.domesticworkers.org/pdfs/HomeEconomicsEnglish.pdf (accessed March 21, 2013).
CBO (Congressional Budget Office). 2013. CBO’s Estimate of the net budgetary impact of the Affordable Care Act’s health insurance coverage provisions has not changed much over time. http://www.cbo.gov/publication/44176 (accessed September 5, 2012).
C-Change. 2012. Project overview. http://www.cancercorecompetency.org/index.php?page=project-overview (accessed September 21, 2012).
———. 2013. A national strategy to strengthen the cancer workforce: Position statement and call to action. http://c-changetogether.org/Websites/cchange/images/Documents/C-CHANGE_WORKFORKCE_POSITION_STATEMENT-_February_2012v1.pdf (accessed March 19, 2013).
Christian, S., C. Dower, and E. O’Neil. 2007. Chart overview of nurse practitioner scopes of practice in the united states. http://www.health.state.mn.us/healthreform/workforce/npcomparison.pdf (accessed October 24, 2012).
Clay, R. A. 2010. Psychologists’ new interventions are helping families cope with what can be a devastating diagnosis. Monitor on Psychology 41(7):69.
CMS (Centers for Medicare & Medicaid Services). 2013. The CMS innovation center. http://innovation.cms.gov (accessed May 1, 2013).
Cohen, H. J. 2009. A model for the shared care of elderly patients with cancer. Journal of the American Geriatrics Society 57(Suppl 2): S300-S302.
Coniglio, D. 2013. Collaborative practice models and team-based care in oncology. Journal of Oncology Practice 9(2):1-2.
Coniglio, D., T. Pickard, and S. Wei. 2011. Commentary: Physician assistant perspective on the results of the ASCO study of collaborative practice arrangements. Journal of Oncology Practice 7(6):283-284.
Cox, K. A., A. P. Smith, and M. Lichtveld. 2012. A competency-based approach to expanding the cancer care workforce part III: Improving cancer pain and palliative care competency. Journal of Cancer Education 27(3):507-514.
CWS (Center for Workforce Studies). 2006. Assuring the sufficiency of a frontline workforce: A national study of licensed social workers. http://workforce.socialworkers.org/studies/health/health.pdf (accessed September 18, 2012).
Del Giudice, M. E., E. Grunfeld, B. J. Harvey, E. Piliotis, and S. Verma. 2009. Primary care physicians’ views of routine follow-up care of cancer survivors. Journal of Clinical Oncology 27(20):3338-3345.
DOL (Department of Labor). 2012. Notice of proposed rulemaking to amend the companionship and live-in worker regulations. http://www.dol.gov/whd/flsa/companionNPRM.htm (accessed March 21, 2013).
Donelan, K., P. I. Buerhaus, B. T. Ulrich, L. Norman, and R. Dittus. 2005. Awareness and perceptions of the Johnson & Johnson Campaign for Nursing’s Future: Views from nursing students, MSs, and CNOs. Nursing Economics 23(4):214-221.
Earle, C. C., and B. A. Neville. 2004. Under use of necessary care among cancer survivors. Cancer 101(8):1712-1719.
Erikson, C., E. Salsberg, G. Forte, S. Bruinooge, and M. Goldstein. 2007. Future supply and demand for oncologists: Challenges to assuring access to oncology services. Journal of Oncology Practice 3(2):79-86.
Ferrell, B. R., R. Virani, S. Smith, and G. Juarez. 2003. The role of oncology nursing to ensure quality care for cancer survivors: A report commissioned by the National Cancer Policy Board and Institute of Medicine. Oncology Nursing Forum 30(1): E1-E11.
Geurts, S., C. Rutte, and M. Peeters. 1999. Antecedents and consequences of work-home interference among medical residents. Social Science & Medicine 48(9):1135-1148.
Gibelli, G., B. Gibelli, and F. Nani. 2008. Thyroid cancer: Possible role of telemedicine. Acta Otorhinolaryngol Italica 28(6):281-286.
Gillick, M. R. 2013. The critical role of caregivers in achieving patient-centered care. Journal of the American Medical Association 310(6):575-576.
Girgis, A., S. Lambert, C. Johnson, A. Waller, and D. Currow. 2013. Physical, psychosocial, relationship, and economic burden of caring for people with cancer: A review. Journal of Oncology Practice 9(4):197-202.
Given, B. 2011. The challenge of quality care for family caregivers in adult cancer care. Paper read at Improving Quality of Life and Quality of Care for Oncology Family Caregivers, July 13, Anaheim, CA.
Glajchen, M. 2009. Role of family caregivers in cancer pain management. In Cancer pain: Assessment and management, edited by E.D. Bruera and R. K. Portenoy. New York: Cambridge University Press. Pp. 597-607.
Gordon, J. 2012. Dermatologic assessment from a distance: The use of teledermatology in an outpatient chemotherapy infusion center. Clinical Journal of Oncology Nursing 16(4):418-420.
Green, L. V., S. Savin, Y. Lu. 2012. Primary care physician shortages could be eliminated through use of teams, nonphysicians, and electronic communication. Health Affairs (Millwood) 32(1):11-19.
Grunfeld, E., L. Zitzelsberger, M. Coristine, T. J. Whelan, F. Aspelund, and W. K. Evans. 2005. Job stress and job satisfaction of cancer care workers. Psychooncology 14(1):61-69.
Grunfeld, E., M. N. Levine, J. A. Julian, D. Coyle, B. Szechtman, D. Mirsky, S. Verma, S. Dent, C. Sawka, K. I. Pritchard, D. Ginsburg, M. Wood, and T. Whelan. 2006. Randomized trial of long-term follow-up for early-stage breast cancer: A comparison of family physician versus specialist care. Journal of Clinical Oncology 24(6): 848-855.
Haley, W. E. 2003. Family caregivers of elderly patients with cancer: Understanding and minimizing the burden of care. Journal of Supportive Oncology 1(4 Suppl 2):25-29.
Hauer, K. E., S. J. Durning, W. N. Kernan, M. J. Fagan, M. Mintz, P. S. O’Sullivan, M. Battistone, T. DeFer, M. Elnicki, H. Harrell, S. Reddy, C. K. Boscardin, and M. D. Schwartz. 2008. Factors associated with medical students’ career choices regarding internal medicine. Journal of the American Medical Association 300(10):21154-21164.
Health Affairs. 2012. Health policy briefs: Graduate Medical Education (Updated). http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=75 (accessed June 18, 2013).
Hess, C., and J. M. Henrici. 2013. Increasing pathways to legal status for immigrant in-home care workers. Washington, DC: Institute for Women’s Policy Research.
Hillborne, L. 2008. The other big workforce shortage. As laboratory technology wanes as a career choice, a staffing crisis grows. Modern Healthcare 38(22):23.
Hitt, W. C., G. Low, T. M. Bird, and R. Ott. 2013. Telemedical cervical cancer screening to bridge medicaid service care gap for rural women. Telemedicine Journal and E-Health 19(5):403-408.
HJWF (Harry and Jeanette Weinberg Foundation). 2013. Family and informal caregiver support program. http://www.hjweinbergfoundation.org/ficsp (accessed May 2, 2013).
Hodges, L. J., G. M. Humphris, and G. Macfarlane. 2005. A meta-analytic investigation of the relationship between the psychological distress of cancer patients and their careers. Social Science & Medicine 60(1):1-12.
HRSA (Health Resources and Services Administration). 2010. The registered nurse population: Findings from the 2008 national sample survey of registered nurses. http://bhpr.hrsa.gov/healthworkforce/rnsurveys/rnsurveyfinal.pdf (accessed September 10, 2012).
———. 2012. Occupational outlook handbook. http://www.bls.gov/ooh/healthcare/occupational-therapists.htm (accessed October 22, 2012).
———. 2013. Coordinating Center for Interprofessional Education and Collaborative Practice. http://www.hrsa.gov/grants/apply/assistance/interprofessional (accessed May 2, 2013).
HWS (Health Workforces Solutions). 2007. Closing the health workforce gap in California: The education imperative. San Francisco, CA: Health Workforce Solutions.
Iglehart, J. K. 2013. Expanding the role of advanced practiced nurse practitioners: Risks and rewards. New England Journal of Medicine 368(20): 1935-1941.
IOM (Institute of Medicine). 1996. Telemedicine: A guide to assessing telecommunications for health care. Washington, DC: National Academy Press.
———. 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
———. 2003a. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: The National Academies Press.
———. 2003b. Health professions education: A bridge to quality. Washington, DC: The National Academies Press.
———. 2005. From cancer patient to cancer survivor: Lost in transition. Washington, DC: The National Academies Press.
———. 2008a. Cancer care for the whole patient: Meeting psychosocial health needs. Washington, DC: The National Academies Press.
———. 2008b. Retooling for an aging america: Building the health care workforce. Washington, DC: The National Academies Press.
———. 2009a. Assessing and improving value in cancer care: Workshop summary. Washington, DC: The National Academies Press.
———. 2009b. Ensuring quality cancer care through the oncology workforce: Sustaining care in the 21st century: Workshop summary. Washington, DC: The National Academies Press.
———. 2011a. Future of nursing: Leading change, advancing health. Washington, DC: The National Academies Press.
———. 2011b. Patient-centered cancer treatment planning: Improving the quality of oncology care: Workshop summary. Washington, DC: The National Academies Press.
———. 2012a. Best care at lower cost: The path to continously learning health care in America. Washington, DC: The National Academies Press.
———. 2012b. Governance and financing of graduate medical education. http://www.iom.edu/Activities/Workforce/GMEGovFinance.aspx (accessed September 7, 2012).
———. 2012c. The mental health and substance use workforce for older adults. Washington, DC: The National Academies Press.
———. 2012d. The role of telehealth in an evolving health care environment. Washington, DC: The National Academies Press.
———. 2013. Interprofessional education for collaboration: Learning how to improve health from interprofessional models across the continuum of education to practice: Workshop summary. Washington, DC: The National Academies Press.
IOM and NRC (National Research Council). 1999. Ensuring quality cancer care. Washington, DC: National Academy Press.
IPEC (Interprofessional Education Collaborative). 2011a. Core competencies for interprofessional colaborative practice: Report of an expert panel. www.asph.org/userfiles/collaborativepractice.pdf (accessed July 26, 2013).
———. 2011b. Team-based competencies: Building a shared foundation for education and clinical practice. http://macyfoundation.org/docs/macy_pubs/Team-Based_Competencies.pdf (accessed November 5, 2012).
Jenkins, W., and M. C. Fina. 2008. Realize the benefits. http://www.hrmreport.com/article/Issue-7/Incentives-AND-Recognition/Realize-the-Benefits (accessed January 21, 2009).
JMF (The Josiah Masy Jr. Foundation). 2013. Integrating transdisciplinary education at Cornell Hunter. http://macyfoundation.org/grantees/profile/integrating-transdisciplinary-education-at-cornell-hunter-iteach (accessed July 26, 2013).
Jolly, P. 2005. Medical school tuition and young physicians’ indebtedness. Health Affairs (Millwood) 24(2):527-535.
Juraschek, S. P., X. Zhang, V. Ranganathan, and V. W. Lin. 2012. United States registered nurse workforce report card and shortage forecast. American Journal of Medical Quality 27(3):241-249.
Kash, K. M., J. C. Holland, W. Breitbart, S. Berenson, J. Dougherty, S. Ouellette-Kobasa, and L. Lesko. 2000. Stress and burnout in oncology. Oncology 14(11):1621-1633.
KHN (Kaiser Health News). 2011. Senior boom creates a demand for home health workers. http://www.kaiserhealthnews.org/stories/2011/august/16/direct-care-workers-in-demand-as-seniors-ranks-grow.aspx (accessed September 18, 2012).
Kim, Y., R. Schulz, and C. S. Carver. 2007. Benefit-finding in the cancer caregiving experience. Psychosomatic Medicine 69(3):283-291.
Klabunde, C. N., A. Ambs, N. L. Keating, Y. He, W. R. Doucette, D. Tisnado, S. Clauser, and K. L. Kahn. 2009. The role of primary care physicians in cancer care. Journal of General Internal Medicine 24(9):1029-1036.
Kosel, K. C., and T. Olivo. 2002. The business case for workforce stability. Irving, TX: Voluntary Hospitals of America.
Kroenke, K., D. Theobald, J. Wu, K. Norton, G. Morrison, J. Carpenter, and W. Tu. 2010. Effect of telecare management on pain and depression in patients with cancer: A randomized trial. Journal of the American Medical Association 304(2):163-171.
Kuo, Y., F. L. Loresto, L. R. Rounds, and J. S. Goodwin. 2013. States with the least restrictive regulations experienced the largest increase in patients seen by nurse practitioners. Health Affairs (Millwood) 32(7):1236-1243.
Kurtz, A. 2013. America’s fastest growing job pays poorly. http://money.cnn.com/2013/03/11/news/economy/fastest-growing-job/index.html?hpt=hp_t3 (accessed March 21, 2013).
Lauria, M. M., E. J. Clark, J. F. Hermann, and N. M. Stearns. 2001. Social work in oncology: Supporting survivors, families, and caregivers. Atlanta, GA: American Cancer Society.
Linzer, M., M. R. Visser, F. J. Oort, E. M. Smets, J. E. McMurray, and H. C. de Haes. 2001. Predicting and preventing physician burnout: Results from the United States and the Netherlands. American Journal of Medicine 111(2):170-175.
Lipner, R. S., W. H. Bylsma, G. K. Arnold, G. S. Fortna, J. Tooker, C. K. Cassel. 2006. Who is maintaining certification in internal medicine—and why? A national survey 10 years after initial certification. Annals of Internal Medicine 144(1): 29-36.
Longpré, S., and R. Newman. 2011. The role of occupational therapy in oncology. http://www.aota.org/Consumers/Professionals/WhatIsOT/MH/Facts/OT-Role-Oncology.aspx (accessed April 29, 2013).
Losses, G. 2006. Managing stress and burnout in oncology. Journal of Oncology Practice 2(3):130-131.
Lupu, D. 2010. Estimate of current hospice and palliative medicine physician workforce shortage. Journal of Pain and Symptom Management 40(6):899-911.
MacDonald, D. J., K. R. Blazer, and J. N. Weitzel. 2010. Extending comprehensive cancer center expertise in clinical cancer genetics and genomics to diverse communities: The power of partnership. Journal of the National Comprehensive Cancer Network 8(5):615-624.
May, J. H., G. J. Bazzoli, and A. M. Gerland. 2006. Hospitals’ responses to nurse staffing shortages. Health Affairs (Millwood) 25(4): W316-W323.
McCabe, M. S., S. Bhatia, K. C. Oeffinger, G. H. Reaman, C. Tyne, D. S. Wollins, and M. M. Hudson. 2013. American Society of Clinical Oncology statement: Achieving high-quality cancer survivorship care. Journal of Clinical Oncology 31(5):631-640.
McCorkle, R., and J. V. Pasacreta. 2001. Enhancing caregiver outcomes in palliative care. Cancer Control 8(1):36-45.
McDonald, K., and J. Sutton. 2009. Surgical workforce: An emerging crisis. http://www.facs.org/fellows_info/bulletin/2009/mcdonald0509.pdf (accessed October 20, 2012).
MDACC (MD Anderson Cancer Center). 2013. Pain Management Center. http://www.mdanderson.org/patient-and-cancer-information/care-centers-and-clinics/specialty-and-treatment-centers/pain-management/index.html (accessed June 18, 2013).
Menne, H. L., F. K. Ejaz, L. S. Noelker, and J. A. Jones. 2007. Direct care workers’ recommendations for training and continuing education. Gerontolology and Geriatrics Education 28(2):91-108.
Mitchell, P., M. Wynia, R. Golden, R. McNellis, S. Okun, C. E. Webb, V. Rohrbach, and I. Von Korhorn. 2012. Core principles and values of effective team-based health care. Washington, DC: Institute of Medicine.
Montgomery, R. J., L. Holley, J. Deichert, and K. Kosloski. 2005. A profile of home care workers from the 2000 Census: How it changes what we know. Gerontologist 45(5):593-600.
MSKCC (Memorial Sloan-Kettering Cancer Center). 2012. Adult survivorship program. http://www.mskcc.org/cancer-care/survivorship/adult-survivorship (accessed September 20, 2012).
———. 2013. Palliative care & pain management. http://www.mskcc.org/cancer-care/palliativecare (accessed June 18, 2013).
NAC (National Alliance for Caregiving) and AARP. 2009. Caregiving in the U.S. http://www.caregiving.org/data/Caregiving_in_the_US_2009_full_report.pdf (accessed September 27, 2012).
NASW (National Association of Social Workers). 2006. Assuring the sufficiency of a frontline workforce: A national study of licensed social workers. http://workforce.socialworkers.org/studies/nasw_06_execsummary.pdf (accessed January 14, 2009).
———. 2013a. The certified social worker in health care. http://www.socialworkers.org/credentials/specialty/c-swhc.asp (accessed February 28, 2013).
———. 2013b. Social work profession. http://www.socialworkers.org/pressroom/features/general/profession.asp (accessed February 28, 2013).
———. 2013c. The social worker in gerontology. http://www.socialworkers.org/credentials/specialty/sw-g.asp (accessed February 28, 2013).
Naylor, M. D. 2012. Next research steps in caregiving. Bethesda, MD: National Institute of Aging.
Naylor, M. D., and S. K. Keating. 2008. Transitional care: Moving patients from one care setting to another. State of the science: Supporting family caregivers. American Journal of Nursing 108(S9):58-63.
Naylor, M., D. Brooten, R. Jones, R. Lavizzo-Mourey, M. Mezey, and M. Pauly. 1994. Comprehensive discharge planning for the hospitalized elderly: A randomized clinical trial. Annals of Internal Medicine 120(12):999-1006.
Naylor, M., D. Brooten, R. Campbell, B. Jacobsen, M. Mezey, M. Pauly, and J. Schwartz. 1999. Comprehensive discharge planning and home follow-up of hospitalized elders: A randomized controlled trial. Journal of the American Medical Association 281(7):613-620.
Naylor, M. D., D. A. Brooten, R. L. Campbell, G. M. Maislin, K. M. McCauley, and J. S. Schwartz. 2004. Transitional care of older adults hospitalized with heart failure: A randomized clinical trial. Journal of the American Geriatric Society 52(5):675-684.
Naylor, M. D., C. Stephens, K. H. Bowles, and M. B. Bixby. 2005. Cognitively impaired older adults: From hospital to home. A pilot study of these patients and their caregivers. American Journal of Nursing 105(2):40-49.
Naylor, M. D., P. Feldman, S. Keating, M. J. Koren, E. T. Kurtzman, M. Maccoy, and R. Krakauer. 2009. Translating research into practice: Transitional care for older adults. Journal of Evaluation in Clinical Practice 15:1164-1170.
Naylor, M. D., K. D. Coburn, E. T. Kurtzman, J. Prvu Bettger, H. G. Buck, J. Van Cleave, and C. A. Cott. 2010. Inter-professional team-based primary care for chronically ill adults: State of the science. Paper presented at ABIM Foundation meeting to Advance Team-Based Care for the Chronically Ill in Ambulatory Settings, Philadelphia, PA, March 24-25.
Naylor, M. D., K. H. Bowles, K. M. McCauley, M. C. Maccoy, G. Maislin, M. V. Pauly, and R. Krakauer. 2011. High-value transitional care: Ttranslation of research into practice. Journal of Evaluation in Clinical Practice, doi: 10.1111/j.1365-2753.2011.01659.x.
NBCHPN (National Board for Certification of Hospice and Palliative Nurses). 2013a. Certification for hospice and palliative registered nurses. http://www.nbchpn.org/DisplayPage.aspx?Title=RN Overview (accessed March 13, 2013).
———. 2013b. Welcome! http://www.nbchpn.org (accessed March 13, 2013).
NCI (National Cancer Institute). 2012a. Continuing umbrella of research experiences (cure). http://crchd.cancer.gov/diversity/cure-overview.html (accessed September 19, 2012).
———. 2012b. Impacts of caregiving on the caregiver’s quality of life. http://www.cancer.gov/cancertopics/pdq/supportivecare/caregivers/healthprofessional/page5 (accessed September 27, 2012).
NCRA (National Cancer Registrars Association). 2006. Frontline workers in cancer data management: Workforce analysis study of the cancer registry field. http://www.ncra-usa.org/files/public/execsum0506.pdf (accessed January 15, 2009).
NCSBN (National Council of State Boards of Nursing). 2010. APM consensus model frequently asked questions. https://www.ncsbn.org/APRN_Consensus_Model_FAQs_August_19_2010.pdf (accessed October 24, 2012).
———. 2012. APM consensus model legislation. https://www.ncsbn.org/aprn.htm (accessed October 24, 2012).
NCSL (National Conference of State Legislatures). 2013. State coverage for telehealth services. http://www.ncsl.org/issues-research/health/state-coverage-for-telehealth-services.aspx (accessed May 1, 2013).
Needleman, J., P. Buerhaus, V. S. Pankratz, C. L. Leibson, S. R. Stevens, and M. Harris. 2011. Nurse staffing and inpatient hospital mortality. New England Journal of Medicine 364(11):1037-1045.
NIH (National Institutes of Health). 2013. Loan repayment programs. http://www.lrp.nih.gov/index.aspx (accessed June 18, 2013).
NQF (National Quality Forum). 2010. Preferred practices and performance measures for measuring and reporting care coordination. http://www.qualityforum.org/Publications/2010/10/Preferred_Practices_and_Performance_Measures_for_Measuring_and_Reporting_Care_Coordination.aspx (accessed November 5, 2012).
Oeffinger, K. C., and M. S. McCabe. 2006. Models for delivering survivorship care. Journal of Clinical Oncology 24(32):5117-5124.
ONCC (Oncology Nursing Certification Corporation). 2012. Advanced practice. http://www.oncc.org/Advanced (accessed September 7, 2012).
Passiment, E. 2006. Update on the laboratory workforce-shortage crisis. Medical Laboratory Observer. http://www.mlo-online.com/articles/0306/0306washreport.pdf (accessed January 13, 2008).
Penn Medicine. 2012. Livestrong Cancer Survivorship Clinic. http://www.penncancer.org/patients/centers-programs-services/livestrong-cancer-survivorship-center (accessed September 20, 2012).
Pham, H. H., D. Schrag, A. S. O’Malley, B. Wu, and P. B. Bach. 2007. Care patterns in medicare and their implications for pay for performance. New England Journal of Medicine 356(11):1130-1139.
Pham, H. H., A. S. O’Malley, P. B. Bach, C. Saiontz-Martinez, and D. Schrag. 2009. Primary care physicians’ links to other physicians through medicare patients: The scope of care coordination. Annals of Internal Medicine 150(4):236-242.
PHPC (Pew Health Professions Commission). 1998. Recreating health professional practice for a new century. http://futurehealth.ucsf.edu/Content/29/1998-12_Recreating_Health_Professional_Practice_for_a_New_Century_The_Fourth_Report_of_the_Pew_Health_Professions_Commission.pdf (accessed September 21, 2012).
Potosky, A. L., P. K. Han, J. Rowland, C. N. Klabunde, T. Smith, N. Aziz, C. Earle, J. Z. Ayanian, P. A. Ganz, and M. Stefanek. 2011. Differences between primary care physicians’ and oncologists’ knowledge, attitudes and practices regarding the care of cancer survivors. Journal of General Internal Medicine 26(12):1403-1410.
PricewaterhouseCoopers. 2007. What works: Healing the healthcare staffing shortage. http://www.pwc.com/extweb/pwcpublications.nsf/docid/674d1e79a678a0428525730d006b74a9 (accessed January 15, 2009).
Pruthi, S., K. J. Stange, G. D. Malagrino, Jr., K. S. Chawla, N. F. LaRusso, and J. S. Kaur. 2013. Successful implementation of a telemedicine-based counseling program for high-risk patients with breast cancer. Mayo Clinic Proceedings 88(1):68-73.
Quill, T. E., and A. P. Abernethy. 2013. Generalist plus specialist palliative care—creating a more sustainable model. New England Journal of Medicine 368(13):1183-1174.
Ramirez, A. J., J. Graham, M. A. Richards, A. Cull, W. M. Gregory, M. S. Leaning, D. C. Snashall, and A. R. Timothy. 1995. Burnout and psychiatric disorder among cancer clinicians. British Journal of Cancer 71(6):1263-1269.
Ramirez, A. J., J. Graham, M. A. Richards, A. Cull, and W. M. Gregory. 1996. Mental health of hospital consultants: The effects of stress and satisfaction at work. Lancet 347(9003):724-728.
RCIC (Rosalynn Carter Institute for Caregiving). 2013. Education & training. http://www.rosalynncarter.org/national_quality_caregiving_network (accessed May 2, 2013).
Reinhard, S. C., and C. Levine. 2012. Home alone: Family caregivers providing complex chronic care. http://www.aarp.org/home-family/caregiving/info-10-2012/home-alone-family-caregivers-providing-complex-chronic-care.html (accessed March 29, 2013).
RGC (Robert Graham Center). 2010. Income disparities shape medical student specialty choice. http://www.graham-center.org/online/graham/home/publications/onepagers/2010/op67-income-disparities.html (accessed September 7, 2012).
Ross, A. C., M. N. Polansky, P. A. Parker, and J. L. Palmer. 2010. Understanding the role of physician assistants in oncology. Journal of Oncology Practice 6(1):26-30.
Routson, J. 2010. Shortage of oncology nurses could get worse as population ages. http://www.healthecareers.com/article/shortage-of-oncology-nurses-could-get-worse-as-populationages/158441 (accessed September 7, 2012).
RUMC (Rush University Medical Center). 2012. Geriatric integrated team training. http://www.rush.edu/professionals/training/geriatrics/index.html (accessed September 21, 2012).
Salsberg, E., P. Rockey, K. Rivers, S. Brotherton, and G. Jackson. 2008. U.S. residency training before and after the 1997 Balanced Budget Act. Journal of the American Medical Association 300(10):1205-1207.
Sanjo, M., T. Morita, M. Miyashita, M. Shiozaki, K. Sato, K. Hirai, Y. Shima, and Y. Uchitomi. 2009. Caregiving consequences inventory: A measure for evaluating caregiving consequences from the bereaved family member’s perspective. Psychooncology 18(6):657-666.
Sargen, M., R. Hooker, and R. Coolper. 2011. Gaps in the supply of physicians, advanced practice nurses, and physician assistants. Journal of the American College of Surgeons 212(6):991-999.
Shanafelt, T. D., P. Novotny, M. E. Johnson, X. Zhao, D. P. Steensma, M. Q. Lacy, J. Rubin, and J. Sloan. 2005. The well-being and personal wellness promotion strategies of medical oncologists in the North Central Cancer Treatment Group. Oncology 68(1):23-32.
Shanafelt, T., H. Chung, H. White, and L. Lyckholm. 2006. Shaping your career to maximize personal satisfaction in the practice of oncology. Journal of Clinical Oncology 24(24):4020-4026.
Sheldon, G. F. 2010. The surgeon shortage: Constructive participation during health reform. Journal of the American College of Surgeons 210(6):887-894.
Smith, A. P., M. Y. Lichtveld, K. R. Miner, S. L. Tyus, and L. N. Gase. 2009. A competency-based approach to expanding the cancer care workforce: Proof of concept. http://c-changetogether.org/Websites/cchange/Images/MedSurg%20Journals/2009/MSJN109_Cancer.pdf (accessed November 5, 2012).
Smith, K., and R. Baughman. 2007. Caring for america’s aging population: A profile of the direct-care workforce. Monthly Labor Review 130(9):20-26.
Snyder, C. F., C. C. Earle, R. J. Herbert, B. A. Neville, A. L. Blackford, and K. D. Frick. 2008. Trends in follow-up and preventive care for colorectal cancer survivors. Journal of General Internal Medicine 23(3):254-259.
Snyder, C. F., K. D. Frick, K. S. Peairs, M. E. Kantsiper, R. J. Herbert, A. L. Blackford, A. C. Wolff, and C. C. Earle. 2009. Comparing care for breast cancer survivors to non-cancer controls: A five-year longitudinal study. Journal of General Internal Medicine 24(4):469-474.
Snyder, C. F., K. D. Frick, R. J. Herbert, A. L. Blackford, B. A. Neville, M. A. Carducci, and C. C. Earle. 2011. Preventive care in prostate cancer patients: Following diagnosis and for five-year survivors. Journal of Cancer Survivorship 5(3):283-291.
Staiger, D., D. I. Auerbach, and P. I. Buerhaus. 2010. Trends in the work hours of physicians in the United States. Journal of the American Medical Association 303(8):747-753.
———. 2012. Registered nurse labor supply and the recession—Are we in a bubble? New England Journal of Medicine 366(16):1463-1465.
Stremikis, K., C. Schoen, and A. Fryer. 2011. A call for change: The 2011 Commonwealth Fund survey of public views of the U.S. health system. http://www.commonwealthfund.org/~/media/Files/Publications/Issue%20Brief/2011/Apr/1492_Stremikis_public_views_2011_survey_ib.pdf (accessed May 2, 2013).
Stubblefield, M. D. 2011. Cancer rehabilitation. Seminars in Oncology 38(3):386-393.
Stubblefield, M. D., M. L. McNeely, C. M. Alfano, and D. K. Mayer. 2012. A prospective surveillance model for physical rehabilitation of women with breast cancer: Chemotherapy-induced peripheral neuropathy. Cancer 118(8 Suppl):2250-2260.
Thibault, G. E., and S. C. Schoenbaum. 2013. Forging collaboration within academia and between academia and health care delivery organizationsL Importance, successes, and future work. http://www.iom.edu/forgingcollaboration (accessed July 26, 2013).
Towle, E. L., T. R. Barr, A. Hanley, M. Kosty, S. Williams, and M. A. Goldstein. 2011. Results of the ASCO study of collaborative practice arrangements. Journal of Oncology Practice 7(5):278-282.
UMN (University of Minnesota). 2013. 1health. http://www.ahceducation.umn.edu/1Health (accessed August 2, 2013).
UnitedHealth. 2011. Modernizing rural health care: Coverage, quality and innovation. http://www.unitedhealthgroup.com/hrm/unh_workingpaper6.pdf (accessed September 6, 2012).
University of Colorado. 2013a. Frontier Center. http://www.ucdenver.edu/academics/colleges/dentalmedicine/CommunityService/Pages/Frontier-Center.aspx (accessed August 2, 2013).
———. 2013b. Interprofessional education for quality and collaborative care. http://www.ucdenver.edu/academics/degrees/health/REACH/Pages/Default.aspx (accessed August 2, 2013).
UNM (University of New Mexico). 2013. Project ECHO. http://echo.unm.edu (accessed July 26, 2013).
Unroe, K. T., and H. J. Cohen. 2012. Chapter 31: Multidisciplinary models of care. In Cancer and aging handbook: Research and practice. First ed, edited by K. M. Bellizzi and M. A. Gosney. Hoboken, NJ: John Wiley & Sons, Inc.
UT (Urology Times). 2007. Is there a urologist in the house? Maybe not for long. http://urologytimes.modernmedicine.com/urologytimes/News+Feature/Is-there-a-urologist-in-the-house-Maybe-not-for-lo/ArticleStandard/Article/detail/423954 (accessed September 18, 2012).
UW (University of Washington). 2012. Interprofessional education at the University of Washington: Vision for a collaborative future. Final report of the Health Sciences Interprofessional Education and Facilities Committee. http://sph.washington.edu/strategicplan/implementation/IPE_report.pdf (accessed August 2, 2013).
———. 2013. Center for Health Science Interprofessional Education, Research, and Practice. http://collaborate.uw.edu (accessed August 2, 2013).
VA (Department of Veterans Affairs). 2013. Caregiver services. http://www.caregiver.va.gov/support_services.asp (accessed May 2, 2013).
VHA (Veterans Health Administration). 2012. A new era of telehealth expansion. VHA Telehealth Quarterly. http://www.telehealth.va.gov/newsletter/2012/021312-Newsletter_Vol11Iss01.pdf (accessed May 1, 2013).
Warde, C. M., K. Moonesinghe, W. Allen, and L. Gelberg. 1999. Marital and parental satisfaction of married physicians with children. Journal of General Internal Medicine 14(3):157-165.
Weitzner, M. A., S. C. McMillan, and P. B. Jacobsen. 1999. Family caregiver quality of life: Differences between curative and palliative cancer treatment settings. Journal of Pain and Symptom Management 17(6):418-428.
Whippen, D. A., and G. P. Canellos. 1991. Burnout syndrome in the practice of oncology: Results of a random survey of 1,000 oncologists. Journal of Clinical Oncology 9(10): 1916-1920.
White, S. 2005. Will there be a pharmacy leadership crisis? An ASHP Foundation scholar-in-residence report. American Journal of Health-System Pharmacy 62(8):845-855.
WHO (World Health Organization). 2010. Framework for action on interprofessional education & collaborative practice. http://whqlibdoc.who.int/hq/2010/WHO_HRH_HPN_10.3_eng.pdf (accessed September 21, 2012).
Wong, R. K., E. Franssen, E. Szumacher, R. Connolly, M. Evans, B. Page, E. Chow, C. Hayter, T. Harth, L. Andersson, J. Pope, and C. Danjoux. 2002. What do patients living with advanced cancer and their carers want to know? A needs assessment. Supportive Care in Cancer 10(5):408-415.
Yoong, J., E. R. Park, J. A. Greer, V. A. Jackson, E. R. Gallagher, W. F. Pirl, A. L. Back, and J. S. Temel. 2013. Early palliative care in advanced lung cancer: A qualitative study. JAMA Internal Medicine 173(4):283-290.
Zilliacus, E. M., B. Meiser, E. A. Lobb, P. J. Kelly, K. Barlow-Stewart, J. A. Kirk, A. D. Spigelman, L. J. Warwick, and K. M. Tucker. 2011. Are videoconferenced consultations as effective as face-to-face consultations for hereditary breast and ovarian cancer genetic counseling? Genetics in Medicine 13(11):933-941.
ANNEX 4-1 PROFESIONALS INVOLVED IN CANCER CARE
| Health Care Professional | Role in Cancer Care | Overview of Available Information |
| Physicians | ||
| Physicians (general) |
• Principal clinicians of medical care |
• Current shortage of ~8% • Shortage will increase to >20% by 2025 if no new residency slots are added |
| Oncology Physicians | ||
| Geriatric Oncologists |
• Diagnose and treat cancer in older adults |
• No information available |
| Hematologists |
• Diagnose and treat blood disorders, including cancer |
• American Society of Hematology has +14,000 members |
| Medical Oncologists |
• Diagnose and treat cancer |
• Shortage of 2,500-4,080 oncologists by 2020 predicted • More than 14,000 medical oncologists and 8,000 hematologists in 2012 |
| Radiation Oncologists |
• Treat cancer with radiation therapy |
• The American Society for Radiation Oncology has ~10,000 members |
| Surgical Oncologists |
• Specialize in the surgical management of cancer |
• The number of general surgical subspecialties, including surgical oncology, grew 20% between 2004 and 2008 |
| Medical and Surgical Specialists | ||
| Gastroenterologists |
• Diagnose and treat cancers in the digestive system |
• 15,000 in 2012 |
| Gynecologists |
• Diagnose, treat, and manage patients with gynecological cancers (e. g., ovarian, cervical) |
• 49% of counties in the United States lack an ob-gyn physician • 18% shortage by 2030 and 25% shortage by 2050 • 15,000+ will likely retire in next 10 years |
| Hospice and Palliative Care Physicians |
• Palliative care physicians prevent and relieve the suffering of patients throughout the continum of cancer care • Experts in hospice care relieve the symptoms of terminally ill patients and provide emotional support |
• 4,400 hospice and palliative care physicians • Majority work part time in the palliative care field. Current shortage of 2,787 to 7,510 full-time employees, which equals 6,000-18,000 individual physicians |
| Pulmonologists |
• Diagnose and treat patients with cancers in the respiratory track |
• ~15,000 certified in pulmonary disease in 2012 • American College of Chest Physicians has 18,500 members |
| Radiologists |
• Use imaging and radiation technologies to diagnose and treat cancer |
• The American College of Radiology has +35,000 members, including radiation oncologists |
| Surgeons |
• Remove diseased tissue from the body |
• The workforce decreased by 16.3% between 1996 and 2006, and is projected to increase by only 3% between 2005 and 2020 • One-third of critical access hospitals lack a surgeon in the county |
| Urologists |
• Diagnose, treat, and manage patients with urological cancers (e. g., prostate, kidney, bladder) |
• Ranks last among all specialties in “production rate” of new physicians • 45% of all urologists are 55 years or older |
| Primary Care Clinicians | ||
| Geriatricians |
• Specialize in the care for older adults |
• 9,000+ in 2012 |
| Primary Care Physicians |
• Provide comprehensive and continuous care for patients regardless of diagnosis, organ system, or problem origin |
• More than 200,000 primary care physicians in 2007 • Only 2% of internal medicine residents planned to go into primary care in 2009 |
| Nurses and Physician Assistants | ||
| Nurses (general) |
• Focused on caring for and dealing with individual responses to health problems |
• 3 million registered nurses • Shortage of 1 million registered nurses predicted by 2020 • 6.9% nursing school faculty vacancy rate in 2010 • 30% drop-out rate for first-year nurses |
| Health Care Professional | Role in Cancer Care | Overview of Available Information |
| Advanced Practice Registered Nurses (APRNs) |
• Have master’s degrees, doctorates of nursing practice, or Ph.D.s in nursing and work with a high level of independence in the care of patients |
• 250,000 APRNs in 2008; 2.6% were certified in oncology |
| Oncology Nurses |
• Provide care to individuals with cancer |
• The Oncology Nursing Society has more than 35,000 members • 2.6% of advanced practice nurses are trained in oncology |
| Physician Assistants |
• Provide care under the supervision of a physician • Prescription privileges across the entire United States |
• Fastest-growing profession behind nursing • Projected to increase from 75,000 professionals in 2008 to between 137,000-173,000 in 2020 |
| Other Health Professionals | ||
| Cancer Registrars |
• Collect and analyze data for national and regional cancer priority research |
• 72,800 registrars in 2006 • 800 new registrars will be needed by 2020 |
| Direct care workers (i. e., personal and home care aides) |
• Provide long-term care and personal assistance • Help clients bathe, dress, and other daily tasks |
• 3.2 million people • Predicted to account for 40% of new health care jobs in 2008-2018 |
| Laboratory personnel |
• Collect samples and perform tests to analyze body fluids, tissue, and other substances |
• 60% of the health care workforce • By 2015, an additional 81,000 clinical laboratory technologists are needed to replace retiring personnel; 68,000 to fill newly created positions • Aging 78% faster than the general U.S. labor market |
| Occupational Therapists |
• Help patients develop, recover, and improve skills necessary for everyday living that are impaired due to cancer or cancer treatment |
• ~100,000 in 2010 • 33% increase between 2010 and 2020 |
| Patient Navigators |
• Help patients navigate through the various components of the health care system, including physicians’ offices, clinics, hospitals, outpatient centers, insurance and payment systems, and patient-support organizations |
• No information available • Education and training varies widely |
| Pharmacists |
• Provide chemotherapy, medications for palliative care, and patient education on drug side effects and interactions |
• 25% of pharmacists are approaching retirement age • 75% of pharmacy directors and middle managers anticipate retiring from their positions within the next decade • 6.4% vacancy rate in 2007 |
| Physical Therapists |
• Promote mobility, functional ability, quality of life, and movement potential |
• ~200,000 in 2010 • 39% increase projected between 2010 and 2020 |
| Public Health Workers |
• Screening, prevention, and early detection of cancer • Surveillance of cancer incidence, prevalence, and mortality |
• 250,000 more workers are needed by 2020 • 50,000 fewer workers in 2000 than in 1980 • 23% of the current workforce was eligible to retire in 2012 • Schools of public health would have to train three times the current number of graduates to replenish the workforce |
| Social Workers |
• Provide patient navigation, psychosocial screening and assessment, and support for cancer-related depression and anxiety |
• 650,500 social workers; 1,000 in oncology • 13% of licensed social workers specialize in health care • 29% of licensed social workers are over 55 years • 85% of all health care social workers are likely to practice in metropolitan areas; 2% are likely to practice in rural areas |
NOTE: The information presented for each professional varies, depending on what information is available about that workforce.
SOURCES: AACN, 2010; AAMC, 2007, 2008; AAPA, 2012a; ABIM, 2012; ACCP, 2012; ACG, 2012; ACOG, 2011; ACR, 2012; ACS/HPRI, 2010; AGA, 2012; AOSW, 2013; ASCP, 2004; ASH, 2011; ASHP, 2007, 2008; ASTRO, 2012a; BLS, 2013b,f; Blum et al., 2006; Buerhaus et al., 2009; CWS, 2006; Hauer, 2008; Hillborne, 2008; HRSA, 2010, 2012; HWS, 2007; IOM, 2011a; KHN, 2011; Lupu, 2010; McDonald and Sutton, 2009; NASW, 2006; NCRA, 2006; Passiment, 2006; PricewaterhouseCoopers, 2007; Routson, 2010; Sargen et al., 2011; Sheldon, 2010; UT, 2007; White, 2005.
This page intentionally left blank.