In the United States, approximately 14 million people are cancer survivors and more than 1.6 million people are newly diagnosed with cancer each year. By 2022, it is projected that there will be 18 million cancer survivors and, by 2030, 2.3 million people are expected to be newly diagnosed with cancer each year. However, more than a decade after the Institute of Medicine (IOM) first addressed the quality of cancer care in the United States, the barriers to achieving excellent care for all cancer patients remain daunting. The growing demand for cancer care, combined with the complexity of the disease and its treatment, a shrinking workforce, and rising costs, constitute a crisis in cancer care delivery (see Box S-1).
The complexity of cancer impedes the ability of clinicians, patients, and their families to formulate plans of care with the necessary speed, precision, and quality. As a result, decisions about cancer care are often not evidence-based. Many patients also do not receive adequate explanation of their treatment goals, and when a phase of treatment concludes, they frequently do not know what treatments they have received or the consequences of their treatments for their future health. In addition, many patients do not receive palliative care to manage their symptoms and side effects from treatment. Most often this occurs because the clinician lacks knowledge of how to provide this care (or how to make referrals to pal-
________________
1 This summary does not include references. Citations for the findings presented in the summary appear in the subsequent chapters.
BOX S-1
The Crisis in Cancer Care Delivery
Studies indicate that cancer care is often not as patient-centered, accessible, coordinated, or evidence-based as it could be, detrimentally impacting patients. The following trends amplify the problem:
• The number of older adults is expected to double between 2010 and 2030, contributing to a 30 percent increase in the number of cancer survivors from 2012 to 2022 and a 45 percent increase in cancer incidence by 2030.
• Workforce shortages among many of the professionals involved in providing care to cancer patients are growing, and training programs lack the ability to rapidly expand. The care that is provided is often fragmented and poorly coordinated. In addition, family caregivers and direct care workers are administering a substantial amount of care with limited training and support.
• The cost of cancer care is rising faster than are other sectors of medicine, having increased from $72 billion in 2004 to $125 billion in 2010; costs are expected to increase another 39 percent to $173 billion by 2020.
• Advances in understanding the biology of cancer have increased the amount of information a clinician must master to treat cancer appropriately.
• The few tools currently available for improving the quality of cancer care–– quality metrics, clinical practice guidelines, and information technology––are not widely used and all have serious limitations.
liative care consultants) or does not identify palliative care management as an important component of high-quality cancer care.
Complicating the situation further are the changing demographics in the United States that will place new demands on the cancer care delivery system, with the number of adults older than 65 rapidly increasing. The population of those 65 years and older comprises the majority of patients who are diagnosed with cancer and who die from cancer, as well as the majority of cancer survivors. The oncology workforce may soon be too small to care for the growing population of individuals diagnosed with cancer. Meanwhile, the Centers for Medicare & Medicaid Services (CMS), the single largest insurer for this population, is struggling financially. In addition, the costs of cancer treatments are escalating unsustainably, making cancer care less affordable for patients and their families and creating disparities in patients’ access to high-quality cancer care.
To address the increasing challenges clinicians face in trying to deliver high-quality cancer care, this report charts a new course for cancer care. There is great need for high-quality, evidence-based strategies to guide
cancer care and ensure efficient and effective use of scarce resources. Responding to these new and continuing challenges, this IOM report updates the 1999 report and revisits the need to improve the quality of cancer care.
The IOM appointed an independent committee of experts with a broad range of expertise, including patient care and cancer research, patient advocacy, health economics, ethics, and health law. The committee was charged with examining challenges to and opportunities for the delivery of high-quality cancer care and formulating recommendations for improvement. The committee’s recommendations aim to ensure the delivery of high-quality cancer care across the care continuum, from diagnosis through end of life. Prevention, risk reduction, and screening were not addressed by the committee. Another way to conceptualize the period of the cancer care continuum that this report addresses is through the three overlapping phases of cancer care: (1) the acute phase, (2) the chronic phase, and (3) the end-of-life phase (see Figure S-1).
Cancer care for older adults, as noted throughout this report, is especially complex. Age is one of the strongest risk factors for cancer, and there are many important considerations to understanding the prognoses of older adults with cancer and formulating their care plans, such as altered physiology, functional and cognitive impairment, multiple coexisting morbidities, increased side effects of treatment, distinct goals of care, and the increased need for social support. The current health care delivery system is poorly prepared to address these concerns comprehensively. Thus, meeting the needs of the aging population will be an integral part of improving the quality of cancer care.
CONCEPTUAL FRAMEWORK
The committee’s conceptual framework for improving the quality of cancer care takes into account the heterogeneity of clinical settings where cancer care is delivered as well as the existing models of high-quality care. The central goal of its conceptual framework is delivering comprehensive, patient-centered, evidence-based, high-quality cancer care that is accessible and affordable to the entire U.S. population, regardless of the setting where cancer care is provided. The committee identified six components of a high-quality cancer care delivery system that will be integral to this transformation:
1. Engaged patients: A system that supports all patients in making informed medical decisions consistent with their needs, values, and preferences in consultation with their clinicians who have
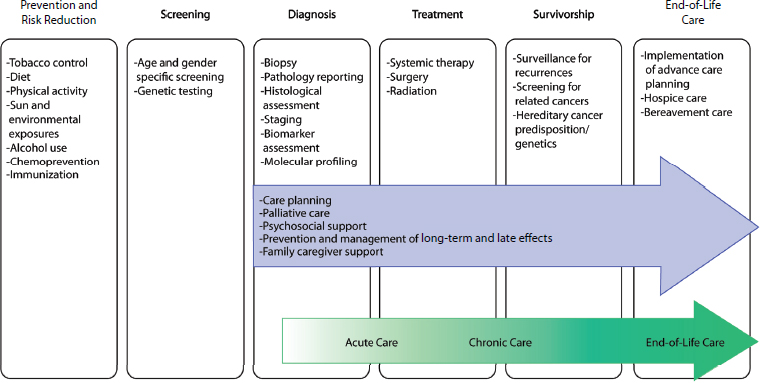
FIGURE S-1 Domains of the cancer care continuum with examples of activities in each domain. The blue arrow identifies components of high-quality cancer care that should span the cancer care continuum from diagnosis through end-of-life care. The green arrow identifies three overlapping phases of cancer care, which is a way of conceptualizing the period of the cancer care continuum that is the focus of this report.
expertise in patient-centered communication and shared decision making (see Chapter 3).
2. An adequately staffed, trained, and coordinated workforce: A system that provides competent, trusted, interprofessional cancer care teams that are aligned with patients’ needs, values, and preferences, as well as coordinated with the patients’ noncancer care teams and their caregivers (see Chapter 4).
3. Evidence-based cancer care: A system that uses scientific research, such as clinical trials and comparative effectiveness research (CER), to inform medical decisions (see Chapter 5).
4. A learning health care information technology (IT) system for cancer: A system that uses advances in IT to enhance the quality and delivery of cancer care, patient outcomes, innovative research, quality measurement, and performance improvement (see Chapter 6).
5. Translation of evidence into clinical practice, quality measurement, and performance improvement: A system that rapidly and efficiently incorporates new medical knowledge into clinical practice guidelines; measures and assesses progress in improving the delivery of cancer care and publicly reports performance information; and develops innovative strategies for further improvement (see Chapter 7).
6. Accessible, affordable cancer care: A system that is accessible to all patients and uses new payment models to align reimbursement to reward care teams for providing patient-centered, high-quality care and eliminating wasteful interventions (see Chapter 8).
Figure S-2 illustrates the interconnectivity of the committee’s six components for a high-quality cancer delivery system.
Prioritization
The committee recognizes that improving the quality of the cancer care delivery system will take substantial time and effort to achieve and that implementation will require efforts by all stakeholders in the cancer care community. The committee numbered its six components for high-quality cancer care in order of priority for implementation, taking into account both the need and the feasibility of achieving each component of the framework. Thus, achieving a system that supports patient decision making is the top priority, followed by an adequately staffed, trained, and coordinated workforce, evidence-based cancer care, a learning health care IT system, the translation of evidence into practice, measurement of outcomes and performance improvement, and, finally, accessible and af-
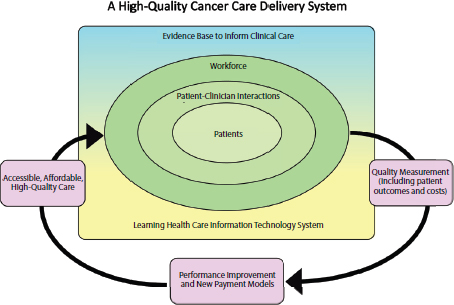
fordable cancer care. The top priorities for implementation are depicted within the rectangle in Figure S-2, with the most important component in the center (i.e., patients). The committee recognizes the importance of access and affordability in a high-quality cancer care delivery system but expects the Patient Protection and Affordable Care Act (ACA) to make substantial changes in these areas of health care. Because much of the law has not yet been implemented, these issues will need to be revisited once the law’s full impact is known.
Approach to Implementation
The committee utilizes a variety of approaches in its recommendations to improve the quality of cancer care. In many circumstances, the recommendations provide specific direction to individual stakeholders. However, fully achieving the goals of the committee’s framework will also necessitate collaboration among relevant stakeholders to define the best path to implementation. Although there are numerous challenges to such collaboration, examples of ongoing collaborations among diverse stakeholders in the cancer community already exist and there may be greater incentives for such coordinated efforts in the current environ-
ment. For example, the ACA is focusing national attention and resources on improving the coordination and quality of the U.S. health care system. Many stakeholders are already making changes in response to health care reform and the committee’s framework provides guidance on this process. In addition, the current financial situation in the United States is placing pressure on the health care delivery system to develop actionable solutions for eliminating waste in care while maintaining or improving quality. Again, the committee’s conceptual framework charts a new course for achieving this task.
RECOMMENDATIONS
The committee structured its recommendations for action around the six components outlined in its conceptual framework. Each component is discussed briefly below and elaborated on in more detail in the respective chapters. Box S-2 provides an overview of the committee’s recommendations.
BOX S-2
Goals of the Recommendations
1. Provide patients and their families with understandable information about cancer prognosis, treatment benefits and harms, palliative care, psychosocial support, and costs.
2. Provide patients with end-of-life care that meets their needs, values, and preferences.
3. Ensure coordinated and comprehensive patient-centered care.
4. Ensure that all individuals caring for cancer patients have appropriate core competencies.
5. Expand the breadth of data collected in cancer research for older adults and patients with multiple comorbid conditions.
6. Expand the depth of data collected in cancer research through a common set of data elements that capture patient-reported outcomes, relevant patient characteristics, and health behaviors.
7. Develop a learning health care information technology system for cancer that enables real-time analysis of data from cancer patients in a variety of care settings.
8. Develop a national quality reporting program for cancer care as part of a learning health care system.
9. Implement a national strategy to reduce disparities in access to cancer care for underserved populations by leveraging community interventions.
10. Improve the affordability of cancer care by leveraging existing efforts to reform payment and eliminate waste.
Patient-Centered Communication and Shared Decision Making
Patients are at the center of the committee’s conceptual framework (see Figure S-2), which conveys the most important goal of a high-quality cancer care delivery system: meeting the needs of patients with cancer and their families. Such a system should support all patients in making informed medical decisions that are consistent with their needs, values, and preferences. In the current system, information to help patients understand their cancer prognoses, treatment benefits and harms, palliative care, psychosocial support, and costs of care is often unavailable or not regularly communicated. Additionally, patient-clinician communication and shared decision making is often less than optimal, impeding the delivery of patient-centered, high-quality cancer care. For example, several recent studies found that approximately 65 to 80 percent of cancer patients with poor prognoses incorrectly believed their treatments could result in a cure.
Recommendation 1: Engaged Patients
Goal: The cancer care team should provide patients and their families with understandable information on cancer prognosis, treatment benefits and harms, palliative care, psychosocial support, and estimates of the total and out-of-pocket costs of cancer care.
To accomplish this:
• The National Cancer Institute, the Centers for Medicare & Medicaid Services, the Patient-Centered Outcomes Research Institute, as well as patient advocacy organizations, professional organizations, and other public and private stakeholders should improve the development of this information and decision aids and make them available through print, electronic, and social media.
• Professional educational programs for members of the cancer care team should provide comprehensive and formal training in communication.
• The cancer care team should communicate and personalize this information for their patients at key decision points along the continuum of cancer care, using decision aids when available.
• The cancer care team should collaborate with their patients to develop a care plan that reflects their patients’ needs, values, and preferences, and considers palliative care needs and psychosocial support across the cancer care continuum.
• The Centers for Medicare & Medicaid Services and other payers should design, implement, and evaluate innovative payment models that incentivize the cancer care team to discuss this information with their patients and document their discussions in each patient’s care plan.
Patients with advanced cancer2 face specific communication and decision-making needs. Clinicians should discuss these patients’ options, such as implementing advance care plans, emphasizing palliative care and psychosocial support, and maximizing quality of life by timely use of hospice care. These difficult conversations do not occur as frequently or as timely as they should, resulting in care that may not be aligned with patient preferences.
Recommendation 2: Engaged Patients
Goal: In the setting of advanced cancer, the cancer care team should provide patients with end-of-life care consistent with their needs, values, and preferences.
To accomplish this:
• Professional educational programs for members of the cancer care team should provide comprehensive and formal training in end-of-life communication.
• The cancer care team should revisit and implement their patients’ advance care plans.
• The cancer care team should place a primary emphasis on providing cancer patients with palliative care, psychosocial support, and timely referral to hospice care for end-of-life care.
• The Centers for Medicare & Medicaid Services and other payers should design, implement, and evaluate innovative payment models that incentivize the cancer care team to counsel their patients about advance care planning and timely referral to hospice care for end-of-life care.
The Workforce Caring for Patients with Cancer
A diverse team of professionals provides cancer care, reflecting the complexity of the disease, its treatments, and survivorship care. These
2 Cancer that has spread to other places in the body and usually cannot be cured or controlled with treatment.
teams include professionals with specialized training in oncology, such as medical, surgical, and radiation oncologists and oncology nurses, as well as other specialists and primary care clinicians. In addition, family caregivers (e.g., relatives, friends, and neighbors) and direct care workers (e.g., nurse aides, home health aides, and personal and home care aides) provide a great deal of care to cancer patients. Patients, at the center of the committee’s conceptual framework, are encircled by the workforce (see Figure S-2), depicting the idea that high-quality cancer care depends on the workforce providing competent, trusted interprofessional care that is aligned with patients’ needs, values, and preferences. To achieve this standard, the workforce must include adequate numbers of health care clinicians with training in oncology. New models of interprofessional, team-based care are an effective mechanism of responding to the existing workforce shortages and demographic changes, as well as in promoting coordinated and patient-centered care.
Recommendation 3: An Adequately Staffed, Trained, and Coordinated Workforce
Goal: Members of the cancer care team should coordinate with each other and with primary/geriatrics and specialist care teams to implement patients’ care plans and deliver comprehensive, efficient, and patient-centered care.
To accomplish this:
• Federal and state legislative and regulatory bodies should eliminate reimbursement and scope-of-practice barriers to team-based care.
• Academic institutions and professional societies should develop interprofessional education programs to train the workforce in team-based cancer care and promote coordination with primary/geriatrics and specialist care teams.
• Congress should fund the National Workforce Commission, which should take into account the aging population, the increasing incidence of cancer, and the complexity of cancer care, when planning for national workforce needs.
The workforce must also have the distinct set of skills necessary to implement the committee’s conceptual framework for a high-quality cancer care delivery system. The recent IOM report Retooling for an Aging America: Building the Health Care Workforce recommended enhancing the geriatric competency of the general health care workforce. The committee
endorses this recommendation as it is especially important to cancer care, where the majority of patients are older adults. Currently, many clinicians also lack essential cancer core competencies.3
Recommendation 4: An Adequately Staffed, Trained, and Coordinated Workforce
Goal: All individuals caring for cancer patients should have appropriate core competencies.
To accomplish this:
• Professional organizations that represent clinicians who care for patients with cancer should define cancer core competencies for their memberships.
• Cancer care delivery organizations should require that the members of the cancer care team have the necessary competencies to deliver high-quality cancer care, as demonstrated through training, certification, or credentials.
• Organizations responsible for accreditation, certification, and training of nononcology clinicians should promote the development of relevant core competencies across the cancer care continuum.
• The U.S. Department of Health and Human Services and other funders should fund demonstration projects to train family caregivers and direct care workers in relevant core competencies related to caring for cancer patients.
The Evidence Base for High-Quality Cancer Care
Because a high-quality cancer care delivery system uses results from scientific research, such as clinical trials and CER, to inform medical decisions, the committee’s conceptual framework (see Figure S-2) depicts the evidence base as supporting patient-clinician interactions. The committee envisions clinical research that gathers evidence of the benefits and harms of various treatment options, so that patients, in consultation with their clinicians, can make treatment decisions that are consistent with their needs, values, and preferences.
Currently, many medical decisions are not supported by sufficient evidence. Additionally, research participants are often not representative of the population with the disease, which makes it difficult to generalize
____________________
3 The tasks or functions that providers of health care should be able to do or perform.
the research results to a specific patient. Another limitation of the current evidence base is that it frequently does not capture information about the impact of a treatment regimen on quality of life, functional and cognitive status, symptoms, and overall patient experience with the disease. Given that the majority of cancer patients are over 65 years and have comorbid conditions complicated by other health (e.g., physical and cognitive deficits) and social (e.g., limited or absent social support, low health literacy) risks, the committee is particularly concerned about the lack of clinical research focused on older adults and individuals with multiple chronic diseases.
Recommendation 5: Evidence-Based Cancer Care
Goal: Expand the breadth of data collected on cancer interventions for older adults and individuals with multiple comorbid conditions.
To accomplish this:
• The National Cancer Institute, the Agency for Healthcare Research and Quality, the Patient-Centered Outcomes Research Institute, and other comparative effectiveness research funders should require researchers evaluating the role of standard and novel interventions and technologies used in cancer care to include a plan to study a population that mirrors the age distribution and health risk profile of patients with the disease.
• Congress should amend patent law to provide patent extensions of up to 6 months for companies that conduct clinical trials of new cancer treatments in older adults or patients with multiple comorbidities.
Recommendation 6: Evidence-Based Cancer Care
Goal: Expand the depth of data available for assessing interventions.
To accomplish this:
• The National Cancer Institute should build on ongoing efforts and work with other federal agencies, the Patient-Centered Outcomes Research Institute, clinical and health services researchers, clinicians, and patients to develop a common set of data elements that captures patient-reported outcomes, relevant patient characteristics, and health behaviors that researchers
should collect from randomized clinical trials and observational studies.
A Learning Health Care Information Technology System for Cancer
The committee’s conceptual framework for a high-quality cancer care delivery system calls for implementation of a learning health care IT system: a system that “learns” by collecting data on care outcomes and cost in a systematic manner, analyzing the captured data both retrospectively and through prospective studies, implementing the knowledge gained from these analyses into clinical practice, evaluating the outcomes of the changes in care, and generating new hypotheses to test and implement into clinical care.
A learning health care IT system is a key requirement for implementing the components of the committee’s conceptual framework for high-quality cancer care. In the committee’s conceptual framework (see Figure S-2), a learning health care IT system supports patient-clinician interactions by providing patients and clinicians with the information and tools necessary to make well-informed medical decisions. It plays an integral role in developing the evidence base from research (e.g., clinical trials and CER) and by capturing data from real-world care settings that researchers can then analyze to generate new knowledge. Further, it is used to collect and report quality metrics data, implement performance improvement initiatives, and allow payers to identify and reward high-quality care.
Many of the elements needed to create a learning health care system are already in place for cancer, including electronic health records, cancer registries, a robust infrastructure for cancer clinical trials, and biorepositories that are linked with clinical data. Unfortunately, they are incompletely implemented, have functional deficiencies, and are not integrated in a way that creates a true learning health care system. In addition, relevant regulations that govern clinical care and research could pose a challenge to a learning health care system. The learning system will either need to comply with the relevant regulations or, alternatively, the regulations may need to be updated to accommodate such a system.
Recommendation 7: A Learning Health Care Information Technology System for Cancer
Goal: Develop an ethically sound learning health care information technology system for cancer that enables real-time analysis of data from cancer patients in a variety of care settings.
To accomplish this:
• Professional organizations should design and implement the digital infrastructure and analytics necessary to enable continuous learning in cancer care.
• The U.S. Department of Health and Human Services should support the development and integration of a learning health care information technology system for cancer.
• The Centers for Medicare & Medicaid Services and other payers should create incentives for clinicians to participate in this learning health care system for cancer, as it develops.
Translating Evidence into Practice, Measuring Quality, and Improving Performance
A high-quality cancer care delivery system should translate evidence into clinical practice, measure quality, and improve the performance of clinicians. This involves developing clinical practice guidelines (CPGs) to assist clinicians in quickly incorporating new medical knowledge into routine care. Also critical are measuring and assessing a system’s progress in improving the delivery of cancer care, publicly reporting the information gathered, and developing innovative strategies to further performance improvement. In the figure illustrating the committee’s conceptual framework (see Figure S-2), knowledge translation and performance improvement are part of a cyclical process that measures the outcomes of patient-clinician interactions and implements innovative strategies to improve the accessibility, affordability, and quality of care.
CPGs translate evidence into practice by synthesizing research findings into actionable steps clinicians can take when providing care. The development of CPGs is not straightforward or consistent because the evidence base supporting clinical decisions is often incomplete and includes studies and systematic reviews of variable quality. In addition, organizations that develop CPGs often use fragmented processes that lack transparency, and they are plagued by conflicts of interest. The committee endorses the standards in the IOM report Clinical Practice Guidelines We Can Trust to address these problems and produce trustworthy CPGs.
Performance improvement initiatives can also be used to translate evidence into practice. These tools have been described as systematic, data-guided activities designed to bring about immediate, positive change in the delivery of health care in a particular setting, as well as across settings. They can improve the efficiency, patient satisfaction, health outcomes, and costs of cancer care. These efforts are typically implemented in a single organization or health system; as a result, they often lack the pace, mag-
nitude, coordination, and sustainability to transform health care delivery nationwide.
Cancer care quality measures provide a standardized and objective means for assessing the quality of cancer care delivered. Measuring performance has the potential to drive improvements in care, inform patients, and influence clinician behavior and reimbursement. There are currently serious deficiencies in cancer care quality measurement in the United States, including pervasive gaps in existing measures, challenges in the measure development process, lack of consumer engagement in measure development and reporting, and the need for data to support meaningful, timely, and actionable performance measurement. A number of groups representing clinicians who provide cancer care, including the American Society of Clinical Oncology and the American College of Surgeons’ Commission on Cancer, have instituted voluntary reporting programs, through which program participants have demonstrated improvements. U.S. Department of Health and Human Services (HHS) has also attempted to influence quality measurement for cancer care through various mandatory reporting programs.
Recommendation 8: Quality Measurement
Goal: Develop a national quality reporting program for cancer care as part of a learning health care system.
To accomplish this, the U.S. Department of Health and Human Services should work with professional societies to:
• Create and implement a formal long-term strategy for publicly reporting quality measures for cancer care that leverages existing efforts.
• Prioritize, fund, and direct the development of meaningful quality measures for cancer care with a focus on outcome measures and with performance targets for use in publicly reporting the performance of institutions, practices, and individual clinicians.
• Implement a coordinated, transparent reporting infrastructure that meets the needs of all stakeholders, including patients, and is integrated into a learning health care system.
Accessible and Affordable Cancer Care
The committee’s conceptual framework for a cancer care delivery system is one in which all people with cancer have access to high-quality,
affordable cancer care. Several IOM reports have called on the U.S. government to ensure that all people have health insurance coverage. Expanding health insurance coverage is a primary goal of the ACA, which is expected to result in 25 million individuals gaining insurance coverage. However, much of the ACA has not yet been implemented and its full impact on access to cancer care is unknown. Many individuals will likely remain uninsured or underinsured. There are also major disparities in cancer outcomes among individuals who are of lower socioeconomic status, are racial or ethnic minorities, or lack insurance coverage. Many of these disparities are exacerbated by these individuals’ lack of access to cancer care.
Recommendation 9: Accessible, Affordable Cancer Care
Goal: Reduce disparities in access to cancer care for vulnerable and underserved populations.
To accomplish this, the U.S. Department of Health and Human Services should:
• Develop a national strategy that leverages existing efforts by public and private organizations.
• Support the development of innovative programs.
• Identify and disseminate effective community interventions.
• Provide ongoing support to successful existing community interventions.
The affordability of cancer care is equally as important as accessibility in a high-quality cancer delivery care system. The committee’s conceptual framework (see Figure S-2) illustrates the concept of using quality measurement and new payment models to reward the cancer care team for providing patient-centered, high-quality care and eliminating wasteful interventions. The current fee-for-service reimbursement system encourages a high volume of care, but it fails to reward the provision of high-quality care. This system is leading to higher cancer care costs, which are negatively impacting patients and their families. One survey found that more than one-third of personal bankruptcies in the United States are due to medical problems and that three out of four families studied had insurance at the onset of illness. From a system perspective, health care costs, including the costs of cancer care, are on an unsustainable trajectory and could pose serious fiscal consequences for the United States.
Payers are experimenting with numerous models that could be employed to reward clinicians for providing high-quality cancer care, such as rewarding care that is concordant with CPGs, coordinated, based on meaningful patient-clinician communication and shared decision making, and includes palliative care and psychosocial support throughout treatment, advance care planning, and timely referral to hospice care (e.g., bundled payments, accountable care organizations, oncology patient-centered medical homes, care pathways, coverage with evidence development, and value-based purchasing and competitive bidding programs). Clinicians are also undertaking efforts to discourage wasteful interventions, such as the Choosing Wisely Campaign.
Recommendation 10: Accessible, Affordable Cancer Care
Goal: Improve the affordability of cancer care by leveraging existing efforts to reform payment and eliminate waste.
To accomplish this:
• Professional societies should identify and publicly disseminate evidence-based information about cancer care practices that are unnecessary or where the harm may outweigh the benefits.
• The Centers for Medicare & Medicaid Services and other payers should develop payment policies that reflect the evidence-based findings of the professional societies.
• The Centers for Medicare & Medicaid Services and other payers should design and evaluate new payment models that incentivize the cancer care team to provide care that is based on the best available evidence and aligns with their patients’ needs, values, and preferences.
• If evaluations of specific payment models demonstrate increased quality and affordability, the Centers for Medicare & Medicaid Services and other payers should rapidly transition from traditional fee-for-service reimbursements to new payment models.
CONCLUSIONS
This report outlines a conceptual framework to improve the quality of cancer care for patients. Changes across the board are urgently needed. All participants and stakeholders, including clinicians, patients and their families, researchers, quality metrics developers, and payers, as well as
HHS, other federal agencies, and industry, must reevaluate their current roles and responsibilities in cancer care and work together to develop a high-quality cancer care delivery system, starting with improving patient-clinician interactions. By working toward this shared goal, the cancer care community can improve the quality of life and outcomes for people facing a cancer a diagnosis.


















