Birth Settings and Health Outcomes: State of the Science
Much of the research that has been conducted over the past three decades on birth settings in the United States has focused on health outcomes, including both maternal and neonatal health outcomes. Moderated by Holly Powell Kennedy, C.N.M., Ph.D., FACNM, FAAN, Yale University, New Haven, Connecticut, Panel 3 presenters discussed several major recent studies on birth settings and health outcomes conducted in the United States and elsewhere. This chapter summarizes those presentations and the panel discussion that followed. See Box 4-1 for a summary of key points made by individual speakers.
COCHRANE REVIEW OF ALTERNATIVE VERSUS CONVENTIONAL INSTITUTIONAL SETTINGS FOR BIRTH1
The impetus for the Hodnett et al. (2012) Cochrane review on clinical birth settings was rooted in prevailing concerns about the technological focus on birth in hospital settings. These concerns, combined with studies demonstrating that the built physical environment can influence length of stay, development of complications, and patient satisfaction with care, pointed to birth settings as an important area of study.
Hodnett et al. (2012) identified three types of alternative hospital settings: (1) “home-like,” or bedroom-like, room, or rooms, that exist either within the hospital labor ward or as separate units within the hospital; (2)
______________________________________
1This section summarizes information presented by Ellen Hodnett, R.N., Ph.D., FCAHS, University of Toronto, Toronto, Ontario, Canada.
BOX 4-1
Birth Settings and Health Outcomes: State of the Science
Key Points Made by Individual Speakers
- In a comparison of the effects of care in “alternative hospital settings” to care in a conventional labor room, the Hodnett et al. (2012) Cochrane review concluded that women randomized to alternative hospital settings were more likely to have no analgesia or anesthesia, spontaneous vaginal birth, and preference for the same setting next time; and less likely to have intrapartum oxytocin, epidural analgesia, Cesarean delivery, assisted vaginal birth, and episiotomy. They found no difference in postpartum hemorrhage, serious maternal morbidity or mortality, serious perinatal morbidity or mortality, 5-minute Apgar, admission to neonatal intensive care unit, or perinatal death.
- Jane Sandall reported the Birthplace in England Collaborative Group prospective cohort study showed a low incidence of adverse perinatal outcomes in all birth settings for low-risk women. While there were no differences in perinatal outcomes for nulliparous women between midwifery units and obstetric units or for multiparous women between any settings, there were significantly more adverse outcomes among nulliparous women in births planned at home compared with those planned in obstetric units. The researchers also reported fewer interventions among women planning births at home or in midwifery units compared to women planning births in obstetric units; and a higher percentage of nulliparous women transferred from either home or a midwifery unit to an obstetric unit, compared to multiparous women.
- Based on a growing collection of reports and studies on intrapartum care principles and processes, the “emerging mosaic” coming into view, in Carol Sakala’s opinion, is that undisturbed, physiologic childbearing confers benefits to women and babies and that common intrapartum practices may have many consequential, sustained, and unintended consequences. Sakala observed that care in birthing centers and home births appears to be associated with fewer interventions and more favorable care practices. Birth center settings do not compromise any measured outcome and, in fact, favor several outcomes. While home births have been associated with lower rates of many maternal and neonatal morbidity measures, they have also been associated with an increased rate of neonatal mortality. Sakala noted that the latter finding is controversial.
- Esther Sternberg explored the growing body of evidence suggesting that a person’s physical environment can influence health via the body’s stress response system and expressed hope that a greater understanding of the brain-immune connection can help designers build healthier, safer birth environments that support both mental and physical health of the mother, fetus, and child. Sternberg called for more research on physiological outcome measures and suggested some methods that might be useful.
- Kristi Watterberg described planned home births as “the most emotional and least data-driven issue” that she has encountered in neonatology, with the possible exception of circumcision. In her opinion, data are limited by researchers from different backgrounds having different expectations of what they will find; splintered systems making it difficult to collect reliable and complete data; and the difficulty, or impossibility, of randomizing study participants in clinical trials.
ambient rooms, which were named as such because of their health-promoting aspects, such as nature scenes (either natural scenes that can be viewed through a window or artificially imposed scenes on the walls of the room), music, freedom to move, and mats and pillows instead of a labor bed, all of which are intended to promote feelings of control, freedom of movement, and calmness; and (3) the Snoezelen room, a type of room that is used more frequently for people with neurologic brain disorders and which is characterized by multiple sensory stimuli, such as fiberoptic lights, sounds, and aromatherapy. The review covered only care in alternative institutional birth settings; it did not cover home births.
The primary objective of the review was to evaluate effects of care in an alternative birth setting compared to care in a conventional labor room. The secondary objectives were to determine if effects vary based on certain characteristics, namely, (a) whether the alternative setting was staffed by the same or separate staff (i.e., conventional labor ward staff), (b) whether continuity of care was also part of the alternative setting, (c) location of the alternative setting (i.e., within the conventional labor and delivery ward, elsewhere in the hospital, or as a freestanding unit), and (d) type of room (i.e., bedroom-like, ambient, or Snoezelen).
Methods
The authors searched the literature from around the world, regardless of language. As with nearly all Cochrane reviews, they sought only randomized controlled trials. Additionally, they analyzed only prespecified outcome measures (both primary and secondary outcome measures). All analyses were by intent to treat. They conducted independent assessments of the eligibility of trials based on methods used and risk of bias; they also conducted sensitivity analyses (e.g., removed weaker trials from the review to see if their removal affected the conclusions). The reviewers ended their search with a total of 10 randomized controlled trials involving 11,795 women.
Of the 10 trials, one trial provided no relevant data, that is, no data for any of the prespecified primary or secondary outcomes. Of the remaining nine, two were conducted in Canada, one in Ireland, one in Australia, one in Sweden, three in the United Kingdom, and one in Norway. One of the nine was a pilot randomized controlled trial (N = 60) of the ambient room setting; the other eight were randomized controlled trials of bedroom-like settings. The reviewers found no randomized controlled trials of either Snoezelen rooms or freestanding birth centers. The eight studies on bedroom-like settings varied in some of their characteristics. Five provided some antenatal care as well as intrapartum care, indicating some level of continuity, and three had separate staff in the alternative care setting, com-
pared to the hospital’s conventional labor and delivery ward, with all three operating with continuity of care as their modus operandi.
All of the alternative study settings included in the review shared a common philosophy that labor and birth is a fundamentally normal experience, and all restricted use of technology during labor and birth. Generally, physicians were not involved in labor and birth in the alternative study settings unless needed. The settings were characterized by high transfer rates either before or during labor, with rates ranging from 29 percent in one study to up to 67 percent in another study.
Results and Conclusions
Women randomized to alternative birth settings were more likely to have no analgesia or anesthesia (based on data from six trials, N = 8,953), spontaneous vaginal birth (based on data from eight trials, N = 11,202), and preference for same setting next time (based on data from two trials, N = 1,207); they were less likely to have intrapartum oxytocin (based on data from eight trials, N = 11,131), epidural analgesia (based on data from eight trials, N = 10,931), Cesarean birth (based on data from nine trials, N = 11,350), assisted vaginal birth (based on data from eight trials, N = 11,202), and episiotomy (based on data from eight trials, N = 11,055). The reviewers found no significant differences in postpartum hemorrhage (based on six trials, N = 10,712), serious maternal morbidity or mortality (based on four trials, N = 6,334), serious perinatal morbidity or mortality (based on five trials, N = 6,385), 5-minute Apgar (based on seven trials, N = 7,665), admission to neonatal intensive care unit (NICU) (based on seven trials, N = 10,798), or perinatal death (based on eight trials, N = 11,206).
The reviewers intended to use prespecified subgroup analyses as a way to determine whether the effects of care observed in alternative settings varied depending on certain characteristics of the trial. However, it was only possible to conduct one subgroup analysis, specifically, whether outcomes varied depending on whether the setting was staffed by the same individuals who staffed the hospital’s conventional labor and delivery ward. The reason for conducting that particular subgroup analysis was the feeling that it was a lot to ask of midwives and nurses working in tertiary units to shift gears the next day and work in a birth setting where risks are lower and where care is based on a different philosophy. However, results of the subgroup analysis revealed that whether staff was the same or separate did not affect spontaneous vaginal birth or serious maternal or perinatal morbidity or mortality.
Hodnett et al. (2012) concluded that their results were consistent with other studies on the independent effects of hospital architecture on health outcomes. However, the benefits of an alternative setting may be overpow-
ered by institutional norms and policies. Hodnett emphasized that it is important to keep in mind that each of these settings is part of an institution and, as such, is subject to the same norms and policies, both stated and unstated, of that institution.
Implications for Practice and Policy
The implications for practice are that pregnant women should be informed that alternative hospital birth settings are associated with lower rates of medical interventions during labor and birth and higher levels of satisfaction, without increasing risk either to themselves or to their babies.
The implications for policy are that decision makers who wish to decrease rates of medical interventions for women experiencing normal pregnancies should consider developing birthing units with policies and practices to support normal birth and labor. More evidence is needed to help decision makers make decisions about staffing models, organization of care, autonomy of the setting, and architectural features.
Recommendations for Future Research
The authors identified several methodological recommendations for future research: measure and report serious perinatal morbidity as well as mortality, provide clear protocols for consultation and transfer of care, address potential confounding effects of continuity of caregiver (i.e., when trying to determine whether setting makes a difference), use evidence-based approaches to encourage high response rates to postal questionnaires, and include cost-effectiveness analyses.
With respect to areas of study, Hodnett et al. (2012) recommended several types of future studies: randomized controlled trials of freestanding birth centers; randomized controlled trials of alternative birth settings that are specifically designed to promote freedom of movement, feelings of calmness, and a sense of control; studies to determine optimal organizational models of birth center care; qualitative studies of impact of transfer on women, care providers, and decision-making processes regarding the need for intervention; and qualitative studies on the impact of competing philosophical, political, and administrative pressures on the operation of alternative settings.
Hodnett also argued that a shift in focus from trying to change providers’ and women’s behavior to altering the clinical environment for labor and birth is worthy of rigorous evaluation. Cesarean delivery rates for otherwise healthy childbearing women continue to increase, despite widespread efforts to encourage providers to adopt evidence-based practices.
Hodnett closed with two slides depicting a hospital labor room before
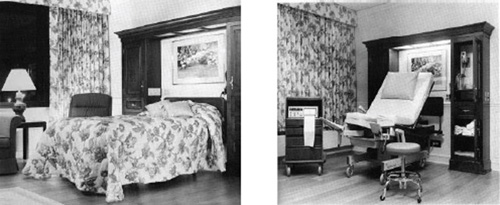
FIGURE 4-1 Questioning the intention to promote feeling of calmness. Left: a bedroom-like hospital labor room as the laboring woman enters it. Right: The same room after the woman has been admitted to the labor room.
SOURCE: Fannin, 2003. Reprinted with permission from John Wiley and Sons.
and after admission of a woman in labor (see Figure 4-1). She said that many of these settings are now called family birth centers.
BIRTHPLACE IN ENGLAND COLLABORATIVE GROUP STUDIES2
The Birthplace in England Collaborative Group is a team of midwives, obstetricians, health economists, epidemiologists, maternity service user organizations, and colleagues led by the National Perinatal Epidemiology Unit at the University of Oxford. The group has produced a series of reports and studies that can be viewed on the project website (http://www.npeu.ox.ac.uk/birthplace). After providing workshop participants with some statistics about deliveries in England, Jane Sandall described in detail one of these studies, a prospective cohort study on perinatal and maternal outcomes by planned place of birth (Brocklehurst et al., 2011).
Having a Baby in England
About 680,000 babies are born in England every year, with the majority of women giving birth in the National Health Service (NHS) sector (i.e., England’s public health system). Forty percent of deliveries are attended by obstetricians or other hospital doctors, 60 percent by midwives. Based on NHS maternity statistics, in 2010-2011, the majority of women (92
______________________________________
2This section summarizes information presented by Jane Sandall, Ph.D., M.Sc, B.Sc, RM, HV, RN, King’s College London, United Kingdom.
percent) gave birth in an obstetric unit (177 obstetric units nationwide), 3 percent delivered at home, 3 percent gave birth in alongside midwife units colocated on the same site as an obstetric unit (53 such units nationwide), and 2 percent delivered in freestanding midwife units geographically separate from any obstetric unit (59 such units nationwide). Both alongside and freestanding midwife units are led by midwives who have clinical accountability for the women in their care. Sandall emphasized that the maternity care system in England is integrated, such that women can transfer from outside of an obstetric unit into an obstetric unit with her midwife. There are no barriers to transfer, according to Sandall. In 2012, there were 21,249 midwives (plus another 5,000 in training), 1,570 consulting obstetricians, and 2,635 registrars (obstetricians in training) practicing as NHS providers nationwide.
Current policy is that women should be provided choices for where to give birth and that those choices should be informed by evidence. However, there is a lack of accurate quantification of the risks associated with births planned in different settings. What evidence does exist has been difficult to interpret because actual place of birth has often been used to make inferences about planned place of birth. “It is absolutely crucial,” Sandall stated, “to be able to look at outcomes by planned place of birth … and to use an intention-to-treat analysis.” Thus, the Birthplace in England Collaborative Group was commissioned by the Department of Health to conduct such an analysis. Other studies conducted by the group include a mapping survey of NHS providers in England, a cost-effectiveness study, and case studies on how care is organized and delivered.
A Prospective Cohort Study on Perinatal and Maternal Outcomes by Planned Place of Birth
The primary objective of the project’s prospective cohort study was to compare intrapartum and early neonatal mortality and morbidity by planned place of birth (i.e., at the start of care of labor) and among women judged to be at “low risk” of complications according to current national clinical guidelines (Brocklehurst et al., 2011). Sandall explained that the national guidelines for identifying low-risk births also contain a set of indicators identifying women who should be advised to give birth in an obstetric unit. The guidelines do not use the word “allow.” Rather, they state that women should be informed that the guidelines are based on a review of international evidence.
The sample population included all NHS trusts providing intrapartum care at home, all freestanding midwifery units, all alongside midwifery units, and a stratified random sample of 142 obstetric units. The sample totaled 64,538 eligible “low-risk” women, that is, women with a singleton,
term pregnancy (greater than or equal to 37 weeks). A power calculation based on a composite perinatal primary outcome measure indicated a need for 57,000 participants, a target that was more than achieved. Unplanned births were excluded from the analysis.
The comparison groups included planned place of birth at the start of care of labor for low-risk women at (a) home, (b) freestanding units, (c) alongside midwifery units, and (d) obstetric units. All comparisons were made with the obstetric unit, not because obstetric units were considered safer but because of the statistical power achieved by using that comparison. Analyses were adjusted for maternal age, ethnicity, and various sociodemo-graphic characteristics; adjustments were made because women who chose to birth at home and in freestanding midwifery centers were more likely to be older, white, better educated, and living in less disadvantaged areas.
Are There Differences Between Planned Birth Settings in Outcomes for the Baby?
The researchers found a higher-than-expected prevalence of complicating conditions recorded at the start of labor, but with marked differences among planned place of birth. Almost 20 percent of women in obstetric units had at least one complicating condition recorded at the start of care compared to 7 percent or fewer in each of the other settings. The complicating conditions included meconium stain, proteinuria, abnormal vaginal bleeding, and other phenomena. According to Sandall, these various complicating conditions probably arose because the system works so well, with women calling their midwives and being advised to go to an obstetric unit. Because the complicating conditions were unexpected, the researchers’ planned analysis had not taken them into account. Thus, the investigators conducted additional analyses of outcomes that were restricted to women without complicating conditions at the start of care in labor.
Of the approximately 65,000 women who participated in the study, there were about 250 adverse perinatal outcomes. The outcome measure was a composite measure. Examining each outcome separately would not have provided enough statistical power to conduct an assessment. Of the 250 primary composite outcome events, 13 percent were intrapartum stillbirths or early neonatal deaths, 46 percent were neonatal encephalopathy, 30 percent meconium aspiration, and 12 percent shoulder injuries. The overall event rate was 4.3 adverse perinatal outcome events per 1,000 births. The rate was higher for nulliparous women (5.3 events per 1,000 births) than for multiparous women (3.1 events per 1,000 births).
There were no statistically significant differences in adverse perinatal outcome among the different planned places of birth. However, in a subgroup analysis by parity, there were significant differences. Among nul-
liparous women (nullips), there were significantly more adverse outcomes in births planned at home (9.3 per 1,000) compared with those planned in obstetric units (5.3 per 1,000). There were no significant differences for nullips who were planning to give birth in midwife units compared to those planning to give birth in obstetric units, and no significant differences for multiparous women (multips) among any of the four settings.
For the restricted sample of women without any complicating conditions at the start of labor, the effect for nullips who were planning to give birth at home was strengthened. Restricting the sample had no impact on results for the other settings.
In summary, for low-risk women, the incidence of adverse perinatal outcomes is low in all birth settings. For multiparous low-risk women, there are no differences in adverse perinatal outcomes among settings. For nulliparous women, the risk of an adverse perinatal outcome appears to be higher among women who plan to give birth at home compared to women planning to give birth in obstetric units.
How Does Planned Birth in Different Settings Affect Intrapartum Interventions and Other Maternal Outcomes?
The researchers evaluated several secondary outcomes: mode of birth, maternal morbidity and mortality, and interventions during labor and birth (e.g., forceps delivery versus intrapartum Cesarean section versus “normal birth”). Normal birth was defined as birth without any of the following interventions: induction of labor, epidural or spinal analgesia, general anesthetic, forceps or ventouse, Cesarean section, or episiotomy (Maternity Care Working Party, 2007). In 2012, 47 percent of women who gave birth in the United Kingdom had what would be defined as a normal birth. The analysis of maternal outcomes by planned place of birth revealed that the Cesarean delivery rate for women planning to give birth in obstetric units was 11 percent, compared to 2 to 4 percent for women planning to give birth in one of the other settings. The pattern was similar for other interventions (forceps and syntocinon) although not quite as stark. The pattern was reversed for normal births, with a smaller percentage of women who plan to deliver in obstetric units having normal births compared to the other settings. For women with access to water or pain relief in labor, the discrepancy in rates for normal birth between the obstetric unit group and the other groups was greater.
Conclusions of the Prospective Study
In sum, the Birthplace in England Collaborative Group (Brocklehurst et al., 2011) concluded that, for low-risk women, the incidence of adverse
perinatal outcomes is low in all birth settings (4.3 adverse perinatal outcome events per 1,000 births). For multiparous low-risk women, there are no differences in adverse perinatal outcomes among planned place of birth settings. For nulliparous women, the risk of an adverse perinatal outcome appears to be higher among women who plan to give birth at home compared to women who plan to give birth in obstetric units. There were no observed differences in risk among women who plan to give birth in freestanding or alongside units compared to women who plan to give birth in obstetric units.
Among maternal outcomes, all low-risk women planning births at home or in either freestanding or alongside midwifery units experienced fewer interventions than those planning births in obstetric units.
How Often Are Women Who Plan Birth in Nonobstetric Settings Transferred During Labor or Immediately After the Birth?
A key concern with birth settings, in Sandall’s opinion, is women who transfer. Overall, 21 to 26 percent of the prospective study participants transferred to obstetric units during labor or shortly after birth. A far higher percentage of nulliparous women transferred (36 to 45 percent), compared to multiparous women (9 to 12 percent). The most common reasons for transfer were failure to progress in the first and second stages and signs of fetal distress.
In addition to the prospective cohort study described above, the Birthplace in England Collaborative Group also conducted a qualitative study on women’s experience of transfer (Rowe et al., 2012). The investigators observed that concerns around transfer distance meant that many women, especially women living in rural areas, did not feel they had any realistic choice of place of birth. They were concerned about the arrangements and the time and travel that transfer would require. Among those who transferred, most women were prepared for the unpredictability of childbirth and the possibility of transfer; however, some were not expecting transfer. Some women found transfer to be worrying, disempowering, or disappointing. Careful explanation of events by professionals had a positive effect on women and their partners’ experiences (Rance et al., 2013).
Economic Analysis
The economic analysis conducted by the Birthplace in England Collaborative Group was a bottom-up costing of all resources used for intrapartum care and during the immediate postnatal period after birth, including any higher-level care administered to either mothers or babies (Schroeder et al., 2012). Costs were allocated to planned places of birth. The research-
ers reported a cost per birth gradient with planned births in obstetric units being the most expensive (£1631), followed by planned births in alongside midwifery units (£1461), planned births in freestanding midwifery units (£1435), and planned births at home (£1067).
Implications for Practice
Results of the various Birthplace in England Collaborative Group studies have several implications for practice. First, guidance to women on planned place of birth should be updated with more accurate information about maternal and perinatal outcomes and transfer rates. Second, variation in out-of-hours cover, training, experience, and support for midwives should be reduced (McCourt et al., 2012). Likewise, variation in transport arrangements for home birth provision needs to be improved. Third, the higher intervention rates and low normal births in obstetric units need to be addressed. Fourth, midwife-unit provision should be expanded. Sandall observed that expanding alongside, rather than freestanding, units seems to be the more popular option for logistical reasons. However, maternity services across the United Kingdom are being reconfigured, with many small obstetric units closing and being reconfigured into freestanding midwife units. Finally, results of the Birthplace in England Collaborative Group work call for an audit and review of intrapartum transfers and management.
Issues that the Birthplace project cannot address include health economics beyond intrapartum and postpartum care costs. The economic analysis was limited to a short time frame around birth. Also, it is not clear why, for women having their first baby, planned home births appear to be more risky than planned obstetric unit births.
Implications for Further Research
Sandall listed several questions that the Birthplace group identified as priorities for future research:
- What aspects of clinical care and service delivery are associated with poorer intrapartum outcomes? Which are potentially modifiable?
- How can the frequency of interventions be reduced for low-risk women planning birth in obstetric units?
- To what extent do socially disadvantaged women have reduced access to choice of birth setting? What strategies might improve equity?
- How can the experience of intrapartum transfer be better managed and the experience improved for women and partners?
- How can ongoing assessment of complications and early detection and referral in late pregnancy and early labor be improved?
- Do models of care that provide continuity of care across settings improve the quality and safety of care?
PROCESS OF CARE DURING CHILDBIRTH3
Carol Sakala addressed three questions related to the process of care during childbirth: (1) What intrapartum care principles and processes are optimal for healthy, lower-risk childbearing women and newborns?; (2) What settings most reliably implement these principles and processes?; and (3) What criteria should be used to assess intrapartum care within and across birth settings?
What Intrapartum Care Principles and Processes Are Optimal for Healthy, Lower-Risk Childbearing Women and Newborns?
To answer this question, Sakala shared some insights from Childbirth Connection’s consensus report, 2020 Vision for a High-Quality, High-Value Maternity Care System (Carter et al., 2010, p. S8). The report was based on work done by a multistakeholder, multidisciplinary team of individuals who were provided with systematic reviews and other best evidence about the effects of different elements of the maternity system. The draft document was reviewed by all members of the organization’s Transforming Maternity Care steering committee and all 10 co-chairs of the project’s five stakeholder work groups. The final report describes several values and principles, including the six quality aims identified in the Institute of Medicine (IOM) 2001 report Crossing the Quality Chasm: A New Health System for the 21st Century, but adapted for maternity care. The report also emphasizes care processes that protect, promote, and support physiologic childbirth, and care that is evidence based. Also consistent with the IOM (2001) report, the Childbirth Connection report defines quality as “the degree to which maternity care services provided to individuals and populations increase the likelihood of optimal health outcomes and are consistent with current knowledge” (p. S8) and value as “the optimal cost to quality ratio in the delivery of maternity care services” (p. S8).
Sakala shared some excerpts from the report. First, with respect to a goal for care around the time of birth, “All maternity caregivers have knowledge and skills necessary to enhance the innate childbearing capacities of women. Each woman is attended in labor and birth in the manner
______________________________________
3This section summarizes information presented by Carol Sakala, Ph.D., M.S.P.H., Childbirth Connection, New York, New York.
that is most appropriate for her level of need and that of her baby and experiences only interventions that are medically indicated, supported by sound evidence of benefit, with least risk of harm compared with effective alternatives. Women and babies at high risk for complications for whom a higher level of specialized care is appropriate have specialty care available to them that adheres to the same basic values and principles” (p. S11).
With respect to the care system and settings for care around the time of birth, the 2020 Vision report states: “A full range of safe birth settings is available and receives system-wide support, so that each woman is free to choose the setting that is most appropriate for her level of need and that of her fetus/baby and that best reflects her values, culture, and preferences. This choice can be made with confidence because each setting assures her a consistent standard of safe, effective, risk-appropriate care, within an integrated system that provides for coordinated consultation, collaboration, or transfer in either direction should her level of need or that of her baby change”(p. S13).
In addition to the 2020 report, Sakala also referred workshop attendees to a forthcoming commissioned report on the hormonal physiology of childbearing (Buckley, forthcoming). Based on a large body of evidence, that report states that, when protected, promoted, and supported, endogenous hormone systems optimize physiologic adaptation of women and fetuses and newborns from before the onset of labor through labor, birth, breastfeeding, and attachment. Benefits include helping with stress and labor pain, providing fetal neuroprotection in labor, preventing postpartum hemorrhage, and optimizing breastfeeding initiation. The report also presents available evidence, clarifying that common maternity care interventions can disrupt hormonal processes and interfere with these benefits.
Related to the Buckley report, Sakala described what she referred to as a “burgeoning literature” on the developmental origins of health and disease and how medical, nutritional, and environmental exposures during sensitive periods of rapid development can have lifelong consequences for immune, metabolic, neurologic, and other body systems (Csaba, 2008; Hyde et al., 2012; Newbold et al., 2006; Penders et al., 2006; van Nimwegen et al., 2011). These consequences include epigenetic effects. Studies showing multigenerational effects of DES (diethylstilbestrol) exposure are especially sobering, in Sakala’s opinion (Newbold et al., 2006). Some of the studies demonstrate variation in effects by birth setting, with less intervention generally associated with fewer adverse consequences. Effects also vary by mode of birth and infant feeding, which themselves vary by birth setting. Mothers too may experience lasting or long-term effects of intrapartum care processes which often vary by setting (Buckley, forthcoming; Ip et al., 2007; Kim et al., 2010; Silver et al., 2006). The evidence is especially
impressive for Cesarean deliveries (lasting reproductive and gynecologic effects) and breastfeeding (long-term effects).
Sakala expressed her view that the appropriate focus of research about the effects of care processes should be the mother-baby dyad, rather than an exclusive focus on the effects on either the baby or the mother.
In conclusion, the “emerging mosaic” that is coming into view suggests that undisturbed, physiologic childbearing confers benefits to women and babies and that common intrapartum practices may have many consequential, sustained, and unintended consequences. Sakala urged exercise of the precautionary principle (Kriebel and Tickner, 2001; Tickner et al., 2003); that is, whenever possible, minimize deviation from what Sakala called “our mammalian heritage” and limit exposure to interventions that do not offer a clear benefit.
What Settings Most Reliably Implement These Principles and Processes?
To answer this question, Sakala referred to the “Milbank report” on evidence-based maternity care (Sakala and Corry, 2008). The report was based on data from Childbirth Connection’s Listening to Mothers II survey of women who gave birth in U.S. hospitals in 2005 and on systematic reviews of maternity practices experienced by a large proportion of women and newborns. The report identified many overused practices, including labor induction, epidural analgesia, Cesarean delivery, continuous electronic fetal monitoring (EFM), rupturing membranes, and episiotomies. Conversely, the report also identified numerous underused effective, beneficial, and noninvasive practices in U.S. hospital-based maternity care, including family physician maternity and midwifery care; smoking cessation interventions for pregnant women; external cephalic versions for breech presentation fetuses; vaginal births after Cesarean deliveries; continuous labor support; measures for comfort, pain, relief, and labor progress; non-supine positions for giving birth; delayed cord clamping in term and preterm babies; early skin-to-skin contact; breastfeeding and interventions to support its initiation and duration; practices to foster women’s satisfaction with childbirth experience; and interventions for postpartum depression.
Sakala emphasized that her intention was not to assess the weight of the evidence or derive precise estimates, but to identify studies that help to clarify whether there are differences in practice patterns across the various birth settings. First, she examined studies that compare care in hospitals versus birth centers. Fullerton and Severino (1992) conducted a secondary analysis of the first National Birth Center Study, comparing participants in that study with a group of women experiencing care in hospitals. Both groups had predominantly midwifery care, with no medical or obstetric risk factors (as defined by the investigators) and no prenatal or intrapartum
complications. All eight interventions and care practices examined favored birth centers: (1) external electronic fetal monitoring (7 percent in birth centers, compared to 50 percent in hospitals); (2) intravenous fluids (8 percent in birth centers, compared to 24 percent in hospitals); (3) artificial rupture of membranes (41 percent in birth centers, compared to 51 percent in hospitals); (4) more than four vaginal exams (44 percent in birth centers, compared to 53 percent in hospitals); (5) solid food during labor (15 percent in birth centers, compared to 11 percent in hospitals); (6) shower or bath during labor (40 percent in birth centers, compared to 24 percent in hospitals); (7) episiotomy (21 percent in birth centers, compared to 34 percent in hospitals); and (8) Cesarean section (4 percent in birth centers, compared to 10 percent in hospitals).
A second study, by Jackson et al. (2003), compared birth center women who had received midwifery care (N = 1,808) to women in hospitals who were eligible for birth center care (N = 1,149). Jackson et al. (2003) performed an intention-to-treat analysis; the investigators adjusted for race/ethnicity, parity, history of Cesarean delivery, age, marital status, country of origin, smoking, and height. All 11 interventions and care practices examined favored birth centers: (1) labor induction (8 percent in birth centers, compared to 15 percent in hospitals), (2) labor augmentation (16 percent in birth centers, compared to 27 percent in hospitals), (3) intravenous fluids (67 percent in birth centers, compared to 97 percent in hospitals), (4) artificial rupture of membranes (53 percent in birth centers, compared to 57 percent in hospitals), (5) continuous EFM (48 percent in birth centers, compared to 94 percent in hospitals), (6) walking in labor (75 percent in birth centers, compared to 67 percent in hospitals), (7) tub or shower in labor (37 percent in birth centers, compared to 3 percent in hospitals), (8) epidural analgesia (30 percent in birth centers, compared to 69 percent in hospitals), (9) episiotomy (13 percent in birth centers, compared to 38 percent in hospitals), (10) assisted delivery (8 percent in birth centers, compared to 18 percent in hospitals), and (11) Cesarean section (11 percent in birth centers, compared to 19 percent in hospitals).
With respect to outcome, the conservative style of care typical of a birth center setting did not result in any compromise of the measured outcomes and, in fact, favored several outcomes. Specifically, there was no difference in positive pressure ventilation, NICU admission, major complication composite measures, preterm birth or low birthweight, intrapartum maternal febrile morbidity, or maternal and newborn readmissions. Outcomes that favored birth centers included fetal heart abnormalities (11 percent in birth centers, compared to 19 percent in hospitals), spontaneous vaginal births (81 percent in birth centers, compared to 63 percent in hospitals), and maternal length of stay greater than 72 hours (10 percent in birth centers, compared to 16 percent in hospitals).
Sakala also pointed to the Birthplace in England study, noting that the odds ratio for the composite “normal birth” (with neither labor induction nor epidural/spinal analgesia, general anesthesia, forceps or vacuum extraction, Cesarean, or episiotomy) measure that Dr. Sandall had referenced in her presentation was 3.86 for freestanding midwifery units compared to obstetric units (Brocklehurst et al., 2011). For a recent summary of these and other studies on birth center versus hospital care, see Goer and Romano (2012).
With respect to care in a home setting, Sakala pointed to the Wax et al. (2010) meta-analysis. In a comparison of planned home births versus planned hospital births, Wax et al. (2010) identified several high-impact interventions that favored planned home births: epidural analgesia (9 percent in a home setting, compared to 23 percent in hospitals), electronic fetal heart rate monitoring (14 percent in a home setting, compared to 63 percent in hospitals), episiotomy (7 percent in a home setting, compared to 10 percent in hospitals), assisted delivery (4 percent in a home setting, compared to 10 percent in hospitals), and Cesarean section (5 percent in a home setting, compared to 9 percent in hospitals).
Additionally, the investigators identified several maternal morbidity outcomes that also favored planned home births: third- or fourth-degree laceration (1 percent in a home setting, compared to 3 percent in hospitals), infection (1 percent in a home setting, compared to 3 percent in hospitals), postpartum bleeding or hemorrhage (4.9 percent in a home setting, compared to 5 percent in hospitals), vaginal laceration (8 percent in a home setting, compared to 22 percent in hospitals), and retained placenta (1 percent in a home setting, compared to 2 percent in hospitals). In contrast, one maternal morbidity outcome, perineal laceration, favored hospital births (43 percent in a home setting, compared to 37 percent in hospitals). Another maternal morbidity outcome, cord prolapse, was no different between the two settings.
With respect to newborn morbidity outcomes, two favored planned home births: prematurity (1 percent in a home setting, compared to 5 percent in hospitals) and low birthweight (1 percent in a home setting, compared to 2 percent in hospitals). Two newborn morbidity outcomes showed no difference between the two settings: newborn ventilation and perinatal death. Two favored planned hospital births: total neonatal death (0.20 percent in a home setting, compared to 0.09 percent in hospitals) and nonanomalous neonatal death (0.15 percent in a home setting, compared to 0.04 percent in hospitals). The last finding—the greater percentage of neonatal deaths in home versus hospital settings—has been a very controversial finding. Sakala mentioned that a number of concerns have been discussed in the literature, including the inclusion of women with unplanned, high-risk
births in some of the studies in the meta-analysis. She pointed out that the absolute risk difference in neonatal deaths is small.
In addition to the results of Wax et al. (2010), Sakala referred to findings reported in the Birthplace in England national prospective cohort study (Brocklehurst et al., 2011), where the odds ratio for that study’s “normal birth” measure was 4.47 for the births planned at home compared to births planned in obstetric units. For a recent summary of these and other studies on home versus hospital birth, see Goer and Romano (2012).
Sakala expressed concern that the United States does not have an integrated system, one characterized by licensure of all providers and routine electronic sharing of health records, care collaboration, performance measurement and reporting, and quality improvement initiatives.
What Criteria Should Be Used to Assess Intrapartum Care Within and Across Birth Settings?
When assessing intrapartum care within and across birth settings, several outcomes of interest to women and families are often excluded from studies. These include quality of life, physical and emotional functioning and recovery, breastfeeding, adaptation to parenthood and family functioning, new-onset maternal morbidity, and payer and out-of-pocket cost of intrapartum care.
Sakala emphasized her belief in the importance of considering optimal outcomes (e.g., spontaneous vaginal birth, exclusive breastfeeding), as well as harms. Sakala indicated harms are generally understudied. Harms of interest with respect to assessing intrapartum care include effects of unneeded interventions; disruption of hormone systems (both short- and long-term effects); perinatal origins of disease and impact on immune, metabolic, and other systems; new-onset maternal morbidity; child morbidity; and mortality.
Additionally, Sakala emphasized the importance of assessing whether the policies, protocols, and systems in place are promoting physiologic childbearing. For example, do personnel have the skills and knowledge to support physiologic childbearing? Furthermore, do personnel protect physiologic childbearing by ensuring a quiet and private environment or by ensuring that mothers and babies are not disturbed by routine early separation? And, do personnel support physiologic childbearing by routinely promoting comfort and labor progress through rest, hydration, positioning, comfort measures, and encouragement?
Many studies of intrapartum care do not measure outcomes after hospital discharge or after the intrapartum period. Thus, very little is known about the longer-term effects of different settings (Teune et al., 2013). Although costly, research follow-up to at least 1 year would help fill what
is basically a “black box” in terms of what is known about long-term outcomes.
Additionally, according to Sakala, experience of care surveys (e.g., the Consumer Assessment of Healthcare Providers and Systems [CAHPS] hospital survey) are poorly suited to maternity care. She suggested, as an example, maternity CAHPS surveys are needed to measure the experiences of both mother and newborn across the various settings and with different types of care providers.
Finally, Sakala indicated the fact that many women have difficulty finding ready and willing “essential maternity care services” that should be routinely available. These include vaginal birth after Cesarean, external cephalic version, vaginal breech birth, vaginal twin birth, skillful judicious assisted delivery, measures to foster comfort and labor progress, and tubs and showers. Thus, in evaluations, questions should be asked whether any given setting provides essential maternal care services appropriate to its level of care and whether it supports women’s informed choices.
Summary Points
Sakala concluded with four summary points:
- The precautionary principle is a prudent consideration when assessing processes of care during childbirth.
- Hospitals are much more likely to provide the type of childbirth care needed by women and babies at higher risk or with significant established problems than that needed by most lower-risk child-bearing families.
- Care around the time of birth in birth centers and home births appears to be more closely aligned with needs of lower-risk child-bearing families, but our broader health care system needs to better integrate and support these settings, and to hold all settings accountable.
- Current research cannot answer many priority questions about the comparative effectiveness of childbirth care in birth settings. We need to expand the questions, measures, outcomes, and designs.
EFFECT OF BUILT ENVIRONMENT ON THE NEUROENDOCRINE
IMMUNE AXIS AND HEALTH: IMPLICATIONS FOR
DESIGN OF HOSPITAL BIRTHING ENVIRONMENTS4
Can a place make you well or sick? The answer is “yes,” according to Esther Sternberg. How does physical environment affect health? Sternberg explained that the answer lies within a field of science related to the mind-body, or brain-immune, connections (Sternberg, 2009).
The brain regulates the immune system in many ways; the immune system, in turn, sends signals to the brain (Sternberg, 2006). The brain’s hypothalamic-pituitary-adrenal axis regulates the immune system via anti-inflammatory glucocorticoids released by the adrenal glands. Additionally, the brain regulates the immune system at the regional level via the sympathetic nervous system and innervation of the spleen, lymph nodes, and thymus. Finally, the peripheral nervous system regulates immunity at sites of inflammation. The parasympathetic nervous system also plays a role.
Basically, when stressed, or when someone perceives stress, the brain’s hormonal stress response turns on and releases corticotropin-releasing hormone from the hypothalamus, adrenocorticotropic hormone from the pituitary gland, and glucocorticoids from the adrenals. At the same time, the sympathetic nervous system is activated and releases norepinephrine from adrenergic nerves and adrenaline from the adrenal medulla. Together, these constitute the physiologic stress response: feeling anxious, sweating, feeling your heart beating fast, urgency to defecate, etc.
Generally, the stress response is what Sternberg called a “good thing.” By focusing one’s attention on being vigilant and getting out of danger, the stress response can be life saving. But when activated for too long or in the wrong circumstances, as in chronic stress, the stress response can create problems. The total load of stress on the body is known as “allostatic load” (McEwen, 2007). It is that heavy load of stress which can cause illness.
There is a wealth of information on the association between chronic stress and numerous stress-related diseases and conditions: increased severity and frequency of viral infections (Cohen et al., 1991; Glaser and Kiecolt-Glaser, 2005), decreased vaccine take rate (Glaser and Kiecolt-Glaser, 2005), prolonged wound healing (Glaser and Kiecolt-Glaser, 2005), accelerated cancer growth (Armaiz-Pena et al., 2009), and accelerated chromosomal aging (Epel et al., 2004). Of these, prolonged wound healing in particular has great implications for birthing. In a study on chronically stressed caregivers of Alzheimer’s patients, Kiecolt-Glaser and colleagues (1995) measured healing time for skin biopsies. In subjects who had re-
______________________________________
4This section summarizes information presented by Esther M. Sternberg, M.D., Arizona Center for Integrative Medicine, Tucson, Arizona. Andria Pizzato, Doctor of Nursing Practice graduate student, contributed to the background research for the presentation.
ceived biopsy wounds, 50 percent of nonstressed individuals were fully healed in 6 weeks, while only 15 percent of caregivers were healed. All of the healthy nonstressed controls were healed by 8 weeks, compared to only 85 percent of caregivers.
There is substantial literature in the field of integrative medicine demonstrating that mind-body interventions can reduce perceived stress and the impact of the stress response on the immune system (Benedetti et al., 2003; Davidson et al., 2003; Kjaer et al., 2002; Lutz et al., 2008; Newberg et al., 2003; Peng et al., 2004; Pollo et al., 2003). These interventions include meditation, exercise, breathing, yoga, tai chi, prayer, and placebo (a belief that something will heal). Numerous studies have shown that these interventions reduce the neuroendocrine (hypothalamic-pituitary-adrenal axis) and adrenergic stress responses, activate the parasympathetic relaxation response, activate brain opioid pathways and dopamine reward pathways, and enhance the immune response. These studies have used a variety of measures, including brain imaging (positron emission tomography, functional magnetic resonance imaging), heart rate variability (reflecting autonomic—adrenergic sympathetic and cholinergic parasympathetic—responses), neuroendocrine responses (salivary cortisol), and antibody response to vaccine (Benedetti et al., 2003; Davidson et al., 2003; Kjaer et al., 2002; Lutz et al., 2008; Newberg et al., 2003; Peng et al., 2004; Pollo et al., 2003).
Can Place Affect the Stress Response System?
According to Sternberg, although more data need to be gathered, evidence collected thus far suggests that the physical environment can either foster or reduce the stress response. Elements of place that trigger the stress response include noise, crowding, light (either too much or too little), odors, mazes, and novelty (unfamiliarity).
A study on recovery of surgery (Ulrich, 1984) launched the field of evidence-based design. Ulrich (1984) showed that patients recovering from gallbladder surgery, all of whom were cared for by the same staff, recovered differently depending on the view from their hospital room. Patients in rooms with views of trees had shorter hospitalizations (by approximately 1 day), fewer analgesic medications, and fewer negative nurse notes than patients with views of brick walls. The findings from Ulrich (1984) have been reproduced many times in multiple settings (e.g., patients with various forms of depression left the hospital 2 to 4 days sooner if their rooms were on the sunny side of the ward [Beauchemin and Hays, 1998; Benedetti et al., 2001]).
According to Sternberg, this suggests that elements that improve both mental and physical health should be incorporated into our hospitals, in-
cluding in our birthing units. What kinds of physical environment changes could be introduced into these settings to reduce the stress response? She imagined spaces for contemplation, meditation, and prayer; green spaces with gardens or views of nature; spaces for social support, which is hugely important for coping with stress; areas for exercise; and areas for activities that engage the senses (e.g., art, music).
The Pebble Project (Center for Health Design, 2013), a project started by the Center for Health Design in San Francisco, California, involved measuring health outcomes associated with the physical changes caused by retrofitting various types of hospital units (e.g., intensive care units, pediatric units, cancer units, and regular wards). For example, the Clarian Health Partners Methodist Hospital in Indianapolis, Indiana, merged critical care and step-down units5 in an effort to reduce complications associated with transfer of critical care patients from critical care units to step-down units; the Pebble Project reported that the merging of the units resulted in 90 percent fewer patient transfers, fewer medical errors, and greater satisfaction (Voelker, 2001). Sternberg reported that when the Center for Health Design collated findings from participating hospitals they found fewer patient falls, fewer medical errors, fewer hospital infections, and a reduction in pain medication use among patients in the retrofitted units. She said they also found less nursing turnover and greater staff and patient satisfaction (Ulrich et al., 2004, 2008). Moreover, Berry et al. (2004) calculated that it would have cost an additional $12 million up front to build a “fable” hospital with all of the physical features associated with improved health outcomes but that the cost would be recouped in the first year of operation, due to savings from improved health outcomes.
Based on a literature search on the effects of birthing environment on stress and health outcomes, Sternberg observed that most of the evidence is subjective (e.g., subjective scale scores, interviews) (Burges Watson et al., 2007; Diette et al., 2003; Dijkstra et al., 2008; Duncan, 2011; Fink et al., 2011; Foureur et al., 2010; Hauck et al., 2008; Hodnett et al., 2012; Lohr and Pearson-Mims, 2000; Park and Mattson, 2009; Raanaas et al., 2012; Stichler, 2007; Tse et al., 2002; Vincent et al., 2010; Walch et al., 2005). The evidence suggests that women who deliver in alternative birth environments experience decreased perceived stress, decreased emotional distress and anxiety, decreased fatigue, increased pain threshold and tolerance, increased patient satisfaction, improved physical and mental wellness, and improved patient safety. For example, the Snoezelen room, an alternative birth environment that creates not just visual cues but also other sensory cues such as aroma and sound, has been associated with increased distrac-
______________________________________
5Intermediate care between a critical care unit and a regular inpatient room.
tion from pain, increased relaxation, increased comfort, increased safety, and increased maternal satisfaction.
In terms of objectively measured physiological effects, some studies have associated alternative birth environments with decreased labor time, decreased need for epidurals, decreased length of stay, decreased systolic blood pressure, decreased sensory pain, decreased analgesic use, and decreased pain medication cost (Burges Watson et al., 2007; Diette et al., 2003; Dijkstra et al., 2008; Duncan, 2011; Fink et al., 2011; Foureur et al., 2010; Hauck et al., 2008; Hodnett et al., 2012; Lohr and Pearson-Mims, 2000; Park and Mattson, 2009; Raanaas et al., 2012; Stichler, 2007; Tse et al., 2002; Vincent et al., 2010; Walch et al., 2005). Sternberg observed that pain medication is a fairly easy way to gauge in an objective manner the effect of an environment on an individual.
Sternberg recommended more research on physiological outcome measures at psychological, physiological, and molecular levels. She encouraged noninvasive research methodologies and highlighted two case studies that exemplify the type of noninvasive research needed. First, Thayer et al. (2010) compared office workers who worked in old versus new office space using salivary cortisol and heart rate variability as outcome measures. Both outcome measures were sensitive enough to detect physiological changes associated with working in an old versus new office space. Heart-rate variability, which provides an indication of the balance between the parasympathetic relaxation and sympathetic stress responses, was higher in workers in the new office space. Such was the case even at night after the workers went home. Higher heart-rate variability is associated with a healthier rhythm; the parasympathetic relaxation response slows the heart and increases variability between beats. Among the same subjects, workers in the new office space had a lower salivary cortisol response. So both components of the stress response indicated an effect of the built environment. Sternberg noted that, interestingly, the subjects’ subjective reports of stress showed no statistical difference in the old and new office space.
In a second study, Marques-Deak et al. (2006) used sweat patches to measure immune biomarkers associated with stress. In a proof-of-principle study, Cizza et al. (2008) used the sweat patches to detect patterns of biomarkers associated with major depressive disorder and found elevated proinflammatory cytokines; elevated neuropeptide Y, reflecting adrenergic nervous system activation; elevated pain neuropeptides; and decreased levels of vasoactive intestinal polypeptide, which reflects parasympathetic nervous system activity. This pattern of a proinflammatory state and a shift toward the adrenergic stress response and away from the parasympathetic relaxation response is consistent with the expected pathophysiology seen in major depressive disorder. Levels of biomarkers also correlated closely with Hamilton Depression and Hamilton Anxiety scores in these women consid-
ered to be clinically in remission. This indicates that such patterns of sweat biomarkers could be useful for detecting health status of individuals non-invasively. New methods to collect and detect sweat analytes are currently being developed (Jia et al., 2012). Sternberg indicated that in combination these studies indicate that new noninvasive methods are becoming available that could be used in any birth environment to ensure the health and safety of mother and fetus with minimal intrusiveness to the birthing experience. In conclusion, Sternberg reiterated that a greater understanding of the brain-immune connection can help designers build healthier, safer birth environments that support both mental and physical health in the mother, fetus, and child.
BIRTH SETTINGS AND HEALTH OUTCOMES: STATE OF THE SCIENCE6
Kristi Watterberg, a member of the American Academy of Pediatrics (AAP) Committee on Fetus and Newborn and lead author on the AAP policy statement on planned home birth, reflected on the four Panel 3 presentations. Before summarizing what she perceived as the key messages of each presentation, she remarked that, with the possible exception of circumcision, planned home births may be the most emotional and least data-driven issue that she has encountered in neonatology. The emotional nature of the issue seems at least partly due to conflict over control of the process. Who does it belong to? Who is in charge of it? Who needs to help and how? It is also driven in part by perceptions of beneficence versus autonomy. Who knows best? On what basis do they know best? And finally, it is driven by opinions of relative value. That is, what is important to one individual may not be as important to someone else.
With respect to why the data are so limited and flawed, Watterberg suggested several reasons. First, what one looks for may determine what one finds. Researchers approach problems from different backgrounds and with different expectations of what they will find. Related to this is the reality that many people have strongly held opinions regarding the value of interventions and outcomes, leading to a lack of equipoise. Second, it is difficult to gather reliable and complete data from the type of splintered systems that exist in the United States. Third, most of the existing structures are conflicting, not cooperative, with limited options for birth centers, great isolation of home birth providers, and highly variable credentialing among care providers. Finally, and arguably most challenging, it is often difficult or impossible to randomize study participants. Watterberg said,
______________________________________
6This section summarizes information presented by Kristi L. Watterberg, M.D., University of New Mexico School of Medicine, Albuquerque, New Mexico.
“You can’t pull a card and randomize a woman to home birth.” Without randomization, populations are different in unknowable ways. While it may be possible to adjust for some factors, such as socioeconomic status or maternal education or parity, there will always be other unknowable but significant factors.
Reflections on Hodnett’s Presentation
In the Cochrane review that Hodnett summarized in her presentation (Hodnett et al., 2012), only one alternative birth setting considered by the reviewers had been studied in randomized controlled trials: the bedroom-like setting within or alongside a standard obstetrical unit. Results from the trials demonstrated less intervention and fewer maternal complications associated with the bedroom-like setting, but a high transfer rate (29 to 67 percent). There was no difference in perinatal death rate.
Watterberg noted Hodnett’s emphasis on the difference between the place and the environment of a planned birth. For example, a woman may be giving birth in a hospital (the place), but the environment of that hospital can be anything from accommodating and friendly to sterile and difficult. This distinction is particularly important in Watterberg’s opinion because the vast majority of women give birth in a hospital setting. Thus, as much attention needs to be focused on the hospital setting as is focused on other settings. Watterberg also noted Hodnett’s suggestion that the focus on changing individual behaviors should be shifted to changing the environment.
Reflections on Sandall’s Presentation
The Birthplace in England study (Brocklehurst et al., 2011) that Sandall summarized in her presentation was focused on four settings: home births, freestanding midwifery units, alongside midwifery units, and hospital-based obstetric units. The three non-hospital-based obstetric units were associated with decreased obstetrical interventions and increased normal (nonintervention) births compared to hospital-based obstetric units, but high transfer rates (21 to 26 percent overall, 36 to 45 percent among primiparous women). Home births were associated with increased risk for a composite adverse neonatal outcome (death, neonatal encephalopathy, meconium aspiration, or shoulder injury) for first pregnancies.
Watterberg’s “take-away” message from Sandall’s presentation was that not all “low-risk” pregnancies are the same. In addition to the need to develop a good way to identify low risk, Watterberg also called for an examination of the higher intervention rates and lower normal birth rates in hospital settings. Again, she emphasized the difference between place and
environment. Giving birth in a hospital should not mean that a woman has to experience a higher intervention rate.
Reflections on Sakala’s Presentation
Sakala’s definition of quality (i.e., quality of care during childbirth) was the following: “The degree to which … care services increase the likelihood of optimal health outcomes and are consistent with current knowledge.” Watterberg emphasized the “consistent with current knowledge” component of the definition. She said, “We have almost no knowledge that is really very helpful.” Many unanswered questions remain regarding optimum principles and practices, which settings best implement those, and which criteria should be used to assess care across settings.
Watterberg noted Sakala’s emphasis of the precautionary principle: “Minimize deviation from mammalian heritage and exposure to interventions that do not offer a clear benefit.” In Watterberg’s opinion, the precautionary principle is very similar to the physician’s “first, do no harm” principle.
Another noteworthy theme of Sakala’s presentation, in Watterberg’s opinion, is that, while there may be different ideas about how to move forward, a common goal is an integrated system that provides for coordinated consultation, collaboration, and transfer.
Reflections on Sternberg’s Presentation
Sternberg’s main themes, in Watterberg’s view, were that there are clear biochemical effects of stress on the neuroendocrine immune axis and health and specific effects of birthing environments on stress, health, and pain outcomes. Sternberg’s presentation raised this question for Watterberg: Is childbirth a unique situation such that experience of pain might have positive, as well as negative, hormonal effects? In Watterberg’s opinion, this is something worth keeping in mind when introducing interventions that change hormones.
Common Themes
A common theme among the four presentations, in Watterberg’s opinion, was that alternative birth settings are associated with fewer interventions and high transfer rates and that home deliveries are associated with an increased neonatal risk. Regarding the last trend, several studies suggest that home birth is associated with increased neonatal mortality. Wax et al. (2010) concluded that home births are associated with a two- to threefold increase in neonatal mortality, although the absolute incidence
is low. Watterberg explained that the Wax et al. (2010) meta-analysis was based on a set of heterogeneous studies conducted in different countries, in different time periods, and using different methodologies. However, she pointed to two other studies which she considered more compelling than Wax et al. (2010). First, Malloy (2010) used birth and death certificate data to compare midwife-attended home births to hospital births in the United States and reported greater neonatal mortality rates in homes compared to hospitals (0.05 percent), both for births attended by nurse midwives (0.10 percent) and for those attended by other midwives (0.18 percent). And in a third study, Symon and colleagues (2009) compared independent midwife-attended births to NHS births in the United Kingdom and reported greater perinatal mortality in the independent midwife-attended births, although there was no difference in perinatal mortality if high-risk cases were excluded.
The question for Watterberg is, why are these alternative settings associated with increased neonatal mortality? She said that the answer is unclear. She asked: Is there a difference in caregiver education or training or a difference in the equipment available? Are high-risk pregnancies inappropriately being delivered at home? Is the problem because of the time required for transport? Is there an inescapable, unavoidable problem with emergencies that occur far from a hospital? Or is it a system failure (because there is no system in the United States)? In a relatively small study of home births in British Columbia, Canada, where a unified system is in place, with registered midwives mandated to offer home or hospital care depending on very specific safety criteria, home births were associated with fewer interventions and no increase in baby morbidity or mortality (perinatal death was 0.35 per 1,000 in planned home births with midwives, compared to 0.57 per 1,000 in hospital births with midwives and 0.64 per 1,000 in hospital births with medical doctors) (Janssen et al., 2009).
Watterberg emphasized the many gaps in research on outcomes associated with variation in birth settings. Pain control is just one example. In a Cochrane review on pain management for women in labor, Jones et al. (2012) wrote: “A major challenge in compiling this overview … has been the variation in use of different process and outcome measures in different trials, particularly assessment of pain and its relief, and effects on the neonate after birth … despite concerns for 30 years or more about the effects of maternal opioid administration during labour on subsequent neonatal behaviour and its influence on breastfeeding, only two out of 57 trials of opioids reported breastfeeding as an outcome” (p. 2). Another pain-control measure, epidural analgesia, was administered to 61 percent of all singleton births in the United States in 2008 (22 to 78 percent, depending on state) according to birth certificate data (Osterman and Martin, 2011). Although epidural analgesia does relieve pain (ACOG, 2004), it also increases ma-
ternal fever, hypotension, length of second stage, assisted vaginal delivery, Cesarean section for fetal distress, and urinary retention (Anim-Somuah et al., 2011).
The challenge with assessing interventions is that no two individuals are alike. What might be good for one woman might not be good for another. There is tremendous variability in risk and the implications of risk not just for the mother (e.g., successful breastfeeding as a maternal outcome), but also for the baby, including the baby’s long-term health (i.e., longer-term health outcomes related to the development origins of health and disease). Watterberg concluded by echoing Sakala’s thoughts on the precautionary principle and the importance of distinguishing between what is known, what is incompletely known, and what is completely unknown.
DISCUSSION WITH THE AUDIENCE7
Following Watterberg’s presentation, workshop attendees were invited to comment or ask questions of the Session 3 panelists. Topics covered included the Wax et al. (2010) meta-analysis; the need for a patient perspective on birth setting research needs; the Birthplace in England study discussed by Sandall and whether any follow-up analyses are being conducted; the importance of conducting research that will help to improve outcomes for high-risk, as well as for low-risk, pregnancies; variation in midwife education; the need for research on the relative costs of deliveries in different settings; and the need for research on long-term outcomes.
Concerns About the Wax et al. (2010) Meta-Analysis
A workshop attendee expressed concern over the central place the Wax et al. (2010) meta-analysis occupied in the dialogue, given limitations of a key study included in that analysis (i.e., Pang et al., 2002). According to the attendee, Pang et al.’s (2002) study on home births in Washington State was flawed in several ways, most importantly by the lack of a subgroup analysis of home births attended by licensed midwives or certified nurse midwives. The attendee asked, “Why are we still talking about this study? When we are looking at the safety of home birth, what can we do to remove these studies from the dialogue and move forward?” Watterberg responded by describing the controversy that ensued when the Wax et al. (2010) meta-analysis was published and how the journal editors recruited an independent group of researchers to reanalyze the data. The independent group of reviewers ended up with the same results. Watterberg indicated
______________________________________
7This section summarizes the workshop discussion that took place at the conclusion of Panel 3.
that it is part of the literature and cannot be removed. She believes other studies will come along and either confirm the Wax et al. (2010) findings or disagree with them.
Calls for a Patient Perspective on Research Needed
There was concern expressed about the lack of a patient panel at the workshop, especially given the subjective nature of the perceived risk of childbirth and the relative risks associated with the different settings. An audience member remarked that “optimal childbirth” means different things to different women. For some, it means making it through childbirth without a ton of pain. For those women, pain relief is very important. One participant remarked that the workshop represented a missed opportunity to let patients express their thoughts on what research they think is important.
Questions About the Birthplace in England Studies
When asked whether any follow-up analyses to the Birthplace in England study were under way, Sandall mentioned examination of variation in service organizations and its impact on maternal outcomes; the relationship between intrapartum transfer and adverse outcomes; outcomes among high-risk women; and staffing (e.g., how different midwife units are configured and how those configurations impact women’s experiences). She clarified that the observed increased rate of adverse outcomes among planned home births reported in the Birthplace in England Collaborative Group study (Brocklehurst et al., 2011) was among nullips only. There was no significant difference in the rate of adverse outcomes among multips. She emphasized the importance of not disseminating the message that home birth is unsafe for all women and remembering that the overall adverse outcome rate was low.
There was another question about the cost analyses conducted by Schroeder et al. (2012) and concern that the analysis did not include the hidden costs of home births (e.g., cost of transport, lifetime costs of caring for infants who experience lasting adverse health outcomes). Sandall agreed that long-term costs associated with lasting adverse health outcomes could be modeled. However, the focus of the Birthplace in England project was on short-term outcomes and costs. Another participant remarked that all birth settings have hidden costs and that home births have many hidden cost savings as well (i.e., savings accrued by not intervening with a Cesarean delivery, epidural, vacuum extraction, etc.); she encouraged a study on the relative costs, including hidden costs, associated with different birth settings.
The Importance of Research That Will Help to Improve Outcomes for High-Risk Pregnancies
One participant cautioned that most of the focus of research on birth settings is on low-risk women and that a research agenda is needed for high-risk women as well. The participant encouraged researchers to think about how lessons learned about low-risk women can help to improve outcomes for higher-risk women.
Variation in Midwife Education and Training
There was a question about variation in midwife education and training, specifically whether there are differences between UK and U.S. midwife education and training. Sandall replied that all UK and U.S. midwife education and training programs strive for International Confederation of Midwives (ICM) competency standards. In the United Kingdom, certified midwives must achieve nationally approved competencies. “Of course,” she said, “even with a national system like that, you have variation between different training providers.” Post-training experience and skill development vary as well, such that women working in community-based practices inevitably develop specialist skills associated with working in those practices whereas women working in high-risk settings develop a separate set of specialist skills.
Several members of the audience contributed to a discussion on three types of U.S. midwife education and training: certified nurse midwives (CNMs), certified professional midwives (CPMs), and certified midwives (CMs). CNMs and CMs attend education programs accredited by the American Commission of Midwifery Education, which is recognized by the U.S. Department of Education. They are certified by the American Midwife Certification Board upon passing a national certification exam and before they can apply for state licensure. CNMs and CMs are educated on performing births in all settings. In a recent analysis of educational programs for midwives, the American College of Nurse Midwives found that its criteria for national certification meet ICM standards. The major difference between the two credentials is whether they are registered nurses (CNMs) or enter midwifery without nursing (CMs). One participant said, “For all intents and purposes, at the midwifery level, they are identical midwives.” A master’s degree is required for all current CNM and CM graduates.
CPMs are certified through the North American Registry of Midwives (NARM). CPMs enter the profession through an educational program accredited by the Midwifery Education Accreditation Commission or through a Portfolio Evaluation Process assessed by NARM. CPMs must pass a national hands-on skills exam and a national written exam before receiving
the certification. Once certified, the CPM can apply for state licensure in 27 states where it is recognized. CPMs do not have an educational degree requirement, but some hold advanced degrees.
The Need for Long-Term Research
Some concern was expressed about the lack of research on long-term outcomes. Most studies do not examine outcomes that occur after discharge from care. Thus, it is not clear how interventions impact long-term health for either the women or her child. Sakala replied that, although long-term research is expensive, ignorance is even more expensive. “I don’t think we can afford not to look at these questions,” she said.






























