4
Payment and Organizational Reforms to Improve Value
The delivery of health care involves myriad decisions made by a wide range of decision makers, including solo practitioners, single-specialty group practices, multiple-specialty group practices, hospitals, health care systems, and in some cases community-based multistakeholder collaboratives (Sennett et al., 2011; Share et al., 2011; Shih et al., 2008). As discussed in detail in Chapter 3, the committee’s research, analyses, and deliberations led to the conclusion that Congress should relate provider payments to outcomes arising from the actions of specific health care decision makers rather than to average outcomes in geographic areas. Perhaps the most important reason to target policies at decision makers is that incentives would otherwise be misdirected; an area-level payment incentive, for example, might do little to cause an individual physician or hospital to seek efficiency in delivering care.
Misdirected incentives are not the only reason to favor payment policies targeting providers. The committee’s research and analyses revealed how variation in spending and quality exists in progressively smaller units, down to the hospital, single-specialty group practice, and even individual physician level, suggesting that opportunities exist for improving value at all levels of health care decision making.1 Decision makers differ in their abilities to maximize efficiency and improve value (Audet et al., 2005; Goldberg et al., 2013; Landon et al., 1998; Shih et al., 2008; Sterns, 2007). For example, an individual practitioner or small group practice can
_________________
1See the committee’s conceptualization of value, given the current state of the art, in Chapter 1, pp 8-9.
take small-scale steps to improve quality and efficiency (e.g., by following evidence-based guidelines or recommending equally efficacious lower-cost treatments to patients) (Wolfson et al., 2009). Group practices, hospitals, health care organizations, and multistakeholder collaboratives, on the other hand, can track and manage patient care across many providers (to different degrees) and may be able to improve value through broader initiatives—for example, through efforts that increase care coordination and target high-risk individuals for disease management programs (Paulus et al., 2008; Shih et al., 2008). As Guterman and colleagues (2009) argue, citing such examples as Geisinger Health System, the North Carolina Community Care model of medical homes, and Medicare’s Physician Group Practice Demonstration, when providers are accountable for a broader continuum of health care for their populations, they can increase the value of the care they deliver (Guterman et al., 2009).
Payers can help align the financial goals of these health care decision makers with high-value care. Today in traditional Medicare, the Centers for Medicare & Medicaid Services (CMS) largely pays physicians on a fee-for-service basis and pays hospitals using the diagnosis-related group (DRG) system (a form of bundled payment for inpatient services and diagnoses). Because of the importance of Medicare, many providers find it convenient to contract with private insurers using the same methods (Mayes and Berenson, 2006). Such a payment system does not promote high-value care for several reasons. First, because providers are paid for the number and intensity of services rendered, not for treating patients efficiently and effectively, fee-for-service payment does not reward providers for sharing information or coordinating care plans. In fact, coordination of care in this environment often penalizes health care providers financially, as providing health care more efficiently means reducing the number of services charged for (Enthoven, 2009; McClellan, 2011; MedPAC, 2012a; Miller, 2007) and may result in a loss of competitive position in a local market. Consequently, “there is little systematic coordination of a patient’s care among multiple providers and settings” (MedPAC, 2012a, p. 36). Second, since all financial risk in fee-for-service payment is relegated to the payer, providers have no financial incentive (and often have a financial disincentive) to select equally efficacious lower-cost care options (McClellan, 2011). Finally, beneficiary cost sharing in traditional Medicare and for the most part under private insurance is unrelated to the benefit of services. Patients, like physicians, have no financial incentive to select lower-cost treatment options that may be equally efficacious (Partnership for Sustainable Health Care, 2013).
The statement of task for this study asked the committee to recommend payment reforms that would promote the delivery of high-value care, taking into consideration the Patient Protection and Affordable Care Act (ACA)
(P.L. 111-148)2 and related changes already under way. Medicare payment reform has the potential to promote high-value care by encouraging provider organizations to develop the capacity to manage the continuum of care for their patient populations efficiently. The following sections address in turn (1) the importance of clinical and financial integration to building a high-value health care delivery system, and how payment reforms are designed to promote such integration; (2) why, under the tenets of a learning health care system,3 it is important for CMS to evaluate and refine new payment models; and (3) strategies for encouraging broader adoption of new payment reforms.
BUILDING A HIGH-VALUE HEALTH CARE SYSTEM THROUGH CLINICAL AND FINANCIAL INTEGRATION
Fragmentation characterizes the organization and delivery of health care services in the United States at the national, state, community, and practice levels (Shih et al., 2008). With no overarching system as a guide, health care services are delivered across an increasing array of distinct and often competing providers and entities, each with different objectives, obligations, and capabilities (Cebul et al., 2008). Providers practicing within the same geographic area, sometimes caring for the same patients, often work independently from and not communicating with one another (Bodenheimer, 2008; Shih et al., 2008).
Increasingly, this fragmented health care delivery system is ill equipped to manage the continuum of health care for an aging population with complex needs. In 2010, 21 million (68.4 percent) and 11 million (36.4 percent) Medicare beneficiaries (in Traditional Medicare Part A and B) had two and four or more chronic conditions, respectively (Lochner and Cox, 2013). Beneficiaries with multiple chronic conditions are the most frequent and intensive users of Medicare services; they see on average as many as three primary care physicians and eight specialists, and typically receive care in seven unique health care facilities (Pham et al., 2007). Understandably care coordination for these patients is exceedingly difficult, as indicated by a 2009 Robert Wood Johnson Foundation finding that for every 100 Medicare patients treated, coordinating care would require that
_________________
2Patient Protection and Affordable Care Act, Public Law 111-148, 111th Cong., 2nd sess. (March 23, 2010).
3A learning health care system is defined as “a health care system that generates and applies the best evidence for the collaborative health care choices of each patient and provider; drives the process of discovery as a natural outgrowth of patient care; and ensures innovation, quality, safety, and value in health care” (Institute of Medicine [IOM] Roundtable on Value &Science-Driven Health Care Charter).
each primary care physician communicate with 99 other physicians in 53 practice locations (Pham, 2009). According to Guterman, “Currently, even when individual services meet high standards of clinical quality, there is often insufficient coordination of care across settings and over time to meet the needs of patients” (Guterman et al., 2011, p. 9).
Fragmentation, particularly in the context of chronic or comorbid conditions spurs inefficiency through a lack of information sharing, duplicate testing, poor care coordination, and mismanagement of care transitions (American Hospital Association, 2010b; IOM, 2012; Shih et al., 2008; Stremikis et al., 2011). The Institute of Medicine’s (IOM’s) Committee on the Learning Health Care System in America concluded, “Chronic diseases and comorbid conditions are increasing, exacerbating the clinical, logistical, decision-making, and economic challenges faced by patients and clinicians” (IOM, 2012, p. S5).
What Health Care Systems Can Do
A growing body of evidence supports the corollary to the consequences of fragmentation that clinical and financial integration best positions health care systems to manage the continuum of care for their complex populations efficiently (Casalino et al., 2003; Chuang et al., 2004; Landon, 1998; McWilliams et al., 2013; Moullec et al., 2012; Shih et al., 2008; Sterns, 2007). Clinical integration denotes a minimum level of coordination and alignment of goals among providers (physicians, hospitals, and other practitioners) caring for a population (Burns and Muller, 2008). In clinically integrated environments, providers share clinical data, agree on plans of care, and collaborate to achieve favorable patient-centered outcomes. Hence, at a minimum, they must foster care coordination among individual providers of care, as well as share data and track service use and outcomes to measure progress (Shortell et al., 1994). Financial integration often hastens clinical integration. Financially integrated health care systems have the capability to receive payments and distribute them to individual care providers, which in turn allows health care systems to align financial incentives among providers within organizations (Hastings, 2012). However, financial integration is not a unitary goal; historically, financially integrated health care organizations lacking management, infrastructure, and processes to coordinate care (i.e., clinical integration) generally have not succeeded in substantially lowering costs or improving care quality, and sometimes have completely failed in this regard (Frakt and Mayes, 2012).
Health care systems in which physician groups and hospitals are under the same ownership (integrated at the corporate level) reflect one common organizational model, but clinical and financial integration exists across a large spectrum of relationships among hospitals, practitioners, and other
entities (Guterman et al., 2011; Shih et al., 2008). Group model health maintenance or prepaid health organizations represent one well-established form of integration (Gaynor et al., 2001). In recent years, moreover, formerly independent or loosely linked providers have pursued tighter integration (Advocate Health Care, 2013). One example is Fairview Health Services (FHS), an academic medical center in Minneapolis. It embarked on a clinical and financial integration program4 across all partnering physicians, even though their practices reflect varying relationships with FHS. These relationships include (1) 500 primary care physicians employed by FHS, (2) 700 specialist physicians within the University of Minnesota practice plan, (3) 1,000 primary care and specialty physicians belonging to a physician hospital organization, and (4) 1,500 primary and specialty physicians practicing independently (American Hospital Association, 2010b).
Maintaining a robust health information technology infrastructure is crucial for both clinical and financial integration. Electronic health records (EHRs), data warehousing, and analytics (leveraging data captured in EHRs) are critical for providers to receive timely quality and cost data with which to track their performance, and were considered essential for the successful implementation of bundled payment in the PROMETHEUS experiment5 (Hussey et al., 2011). An emerging body of studies suggests that provider use of health information technology (HIT) may help improve disease management and care coordination processes and positively impact health outcomes, especially for patients with multiple chronic conditions (Cebul et al., 2011; Herrin et al., 2012; Kern et al., 2012). Further, well-designed EHRs can promote care coordination by increasing providers’ access to patient information and support high-quality care by incorporating evidence-based clinical pathways (Mechanic and Zinner, 2012). Providers and hospitals have made significant progress in adopting HIT systems; however, much more remains to be done. As of 2011, just over half of physicians had adopted EHRs (Decker et al., 2012; Jamoom et al., 2012), 75 percent of which met minimum federal standards.6
One caveat of note is that clinical and financial integration may in some
_________________
4FHS’s quality improvement and cost reduction program has two main components: (1) “care packages” detailing best practices for 12 conditions and procedures (e.g., low back pain, diabetes, prenatal care, knee replacement), and (2) a shift in provider reimbursement away from fee-for-service to a single fee covering the entire package of services (American Hospital Association, 2010a).
5PROMETHEUS, an acronym for Provider Payment Reform for Outcomes, Margins, Evidence, Transparency, Hassle Reduction, Excellence, Understandability and Sustainability, is a bundled payment pilot project. Its development and evaluation were sponsored by The Commonwealth Fund and the Robert Wood Johnson Foundation (Hussey et al., 2011).
6CMS provides incentives to providers who make “meaningful use” of EHRs. The requirements for meaningful use are available at https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Meaningful_Use.html.
markets increase provider concentration (a potential violation of antitrust laws), enabling providers in those markets to charge commercial carriers higher prices (RWJF, 2012).7 Antitrust enforcement often raises a difficult trade-off between production efficiencies and market power, and health care is no exception (RWJF, 2012). Nonetheless, greater value clearly requires greater coordination among providers.
What Payers Can Do
Payers can promote value through payment and organizational reforms that foster the above elements of clinical and financial integration. In fact, many payment reforms included in the ACA and tested in the commercial market (e.g., value-based purchasing [VBP], bundled payment, accountable care organizations [ACOs], patient-centered medical home (PCMH) models, and dual-eligible care integration demonstrations, all discussed later in this chapter) do just that. Early provider reaction has been positive, as reflected in the larger-than-anticipated number of organizations contracting with CMS to join pilot programs (CMS, 2013f; Muhlestein, 2013). However, the U.S. health care delivery system spans a diverse array of provider organizational relationships, which vary in size, level of integration (both clinical and financial), and ability/willingness to assume financial risk (Guterman, 2010). The Commonwealth Foundation developed a graph (see Figure 4-1) depicting the interaction between provider organizational models and alternative payment mechanisms. Because these reforms are relatively new, evidence on their influence on value, particularly in less integrated organizational settings, is limited. Therefore, it would be advisable for CMS to test payment models that are compatible with less as well as more clinically integrated providers to see how reforms impact the value of care in different settings (Guterman and Drake, 2010).
Also critical is for payers, including CMS, to make real-time data on service use and relative performance levels available to provider organizations. To identify opportunities for improving value, providers require ongoing data collection and analysis concerning the effects of value improvement interventions. Where regional collaboratives have constructed multipayer databases, data on Medicare patients have generally been excluded or out of date. According to Miller (2011, p. 14), “In the few communities where Medicare data has been made available, it has typically
_________________
7The increase in commercial payments would raise total health care spending directly. But if Medicare kept its prices at some proportion of commercial prices, say 80 percent, it would also spend more; if it did not do so, Medicare beneficiaries might experience access problems since the gap between commercial and Medicare payments in such markets would be particularly large.
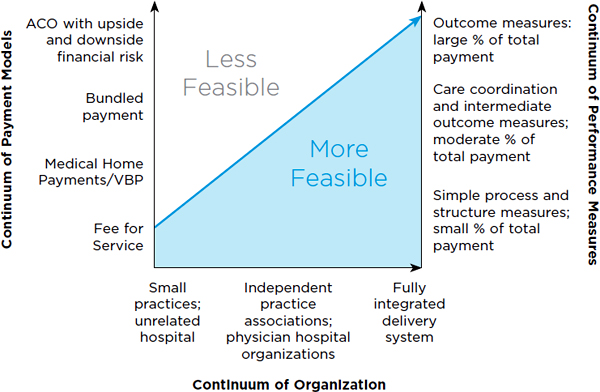
FIGURE 4-1 Organization and payment methods.
NOTE: “Global case” is equivalent to bundled payment (discussed in the text). P4P = pay for performance.
SOURCE: Adapted from The Commonwealth Fund, 2008.
been several years old. Data that are out-of-date are of relatively little value in communities where there are active efforts to improve the quality and cost of care; indeed, using old data can be counterproductive since it may unfairly imply that problems exist when, in reality, they have already been addressed.”
What Patients Can Do
Finally, patients are also health care decision makers and can be encouraged through alternative cost-sharing arrangements to share in the savings of higher-value care. In this connection, it is important to acknowledge that “clinical services vary in the value they provide to patients, and that not all patients with a specific clinical condition receive the same level of benefit from a specific intervention” (Fendrick and Chernew, 2006, p. SP10). There is little debate that cost sharing (increasing or decreasing patients’ out-of-pocket costs) influences the use of health care services (Fendrick and Chernew, 2006). Introducing value-based cost sharing into a health
care system may encourage patients to frequent high-value providers and/ or higher-value care options. However, increasing cost sharing has been shown to decrease the use of both effective and ineffective services; thus, more information is needed on how best to tailor a program to encourage the selection of higher-value care options (IOM, 2012). CMS should therefore consider piloting programs that seek to align patient cost-sharing arrangements with value.
RECOMMENDATION 3: To improve value, the Centers for Medicare & Medicaid Services (CMS) should continue to test payment reforms that incentivize the clinical and financial integration of health care delivery systems and thereby encourage their (1) coordination of care among individual providers, (2) real-time sharing of data and tracking of service use and health outcomes, (3) receipt and distribution of provider payments, and (4) assumption of some or all of the risk of managing the care continuum for their populations. Further, CMS should pilot programs that allow beneficiaries to share in the savings due to higher-value care.
EVALUATING AND REFINING NEW PAYMENT MODELS
Payment reforms can target the full spectrum of health care decision makers, encouraging individual providers in highly fragmented areas to maximize their own efficiencies and coordinate with each other while allowing more organized health care systems and collaboratives to assume additional risk (and potential reward) in managing the health of their patient populations (IOM, 2012; Shih et al., 2008). This can be done directly by paying health care providers that achieve selected quality and efficiency metrics (e.g., VBP) or implement care coordination programs (e.g., PCMHs), or indirectly by shifting some or all financial risk to health care systems (e.g., bundled payment, ACOs, Medicare Advantage plans). Many payment and organizational reforms include both of the above strategies; in the Pioneer program, for example, ACOs must achieve specific quality measures as well as assume some financial risk (CMS, 2012). The following sections briefly offer the rationale for and evidence supporting selected payment reforms in the ACA and illustrate why it is necessary to continue testing and refining new payment models before generalizing them to the broader Medicare population.
Value-Based Purchasing
In Medicare, the program now known as VBP began as pay-for-reporting (paying providers for reporting quality data) and then was called pay-for-performance (paying providers for meeting quality standards). The newer VBP models require providers to meet quality and cost reduction goals (paying for efficiency or value). One benefit of VBP is that it can target any level of health care decision making, including individual practitioners (Folsom et al., 2008).
Pay-for-performance and VBP have been touted as effective interventions for improving health care outcomes, yet evaluation results are mixed. Although a large-scale Medicare hospital demonstration of pay-for-performance showed promise in the first 2 years (Lindenauer et al., 2007), quality improvement, as indicated by reductions in mortality, was not achieved over the full 6-year duration of the program (Jha et al., 2012; Ryan et al., 2012; Werner et al., 2011). Similarly, the United Kingdom’s universal pay-for-performance program for primary care physicians, implemented in 2004, showed improved results on all quality measures in the first year, but several measures subsequently leveled off (Campbell et al., 2009; Doran et al., 2011).
More than 40 private-sector pay-for-performance programs operate throughout the United States. One example, Integrated Health Association’s (IHA’s) California Pay-for-Performance Program, is the largest private physician incentive program in the United States (James, 2012). Rosenthal and colleagues (2005) evaluated how California physician groups participating in the program (intervention group) compared to Pacific Northwest physician groups (control group) on three quality measures (cervical cancer screening, mammography, and hemoglobin A1c testing) (Rosenthal et al., 2005). Although the intervention group improved on all three quality measures over the course of the study, control comparisons showed the intervention group’s quality to be higher only for the cervical cancer screening measure. The authors concluded that the study results do not justify the program’s price tag of $3.4 million. In a complementary follow-up study, Mullen and colleagues (2008) concluded that overall, the program resulted in a “small and mixed return on investment” (Mullen et al., 2008, p. 26). More specifically, Mullen and colleagues concluded that the size of incentives matters. IHA’s program will be transitioning to include value-based cost measures starting in 2014 (Dolan and Yanagihara, 2011).
CMS launched a Medicare hospital-based VBP program in October 2012. Evaluation measures for the program’s first year include process measures and patient satisfaction; CMS plans to extend these measures to include health outcomes and costs. Hospitals are eligible for incentives
based on overall achievement and improvement relative to previous years. Program funding comes from a 1 percent withhold from regular fee-for-service payments to participating hospitals; this withhold increases each year up to 2 percent in 2017 and beyond. The level of incentive payments depends on hospital performance. CMS estimates that about half of hospitals will see a net increase in payments, but expected changes in payment are small even for best and worst performers (Werner and Dudley, 2012).
Although VBP has not yet been shown to produce substantial improvements in health care value, it does encourage providers and health care organizations to invest in the HIT systems needed to track patient cost and care measures (Folsom et al., 2008). In conjunction with other payment changes, therefore, it may produce value in other ways.
Patient-Centered Medical Homes
The PCMH is a health care delivery model that organizes the care continuum around a practitioner team with the primary care provider at the center, helping patients coordinate care and manage chronic conditions. The PCMH also generally incorporates evidence-based medicine and quality improvement activities (Cassidy, 2010; Jackson et al., 2013). Proponents believe the PCMH will reduce care costs and improve quality. For example, one analysis of 43 primary care clinics participating in the Geisinger ProvenHealth Navigator project between 2006 and 2010 found that increased length of time in the program was significantly associated with lower total cost and with the total cumulative cost savings over the study period of 4.3 to 7.1 percent (Maeng et al., 2012). Group Health Cooperative of Seattle estimates that it generated a return of $1.50 for every $1 invested in its medical home demonstration (Reid, 2010).
The PCMH model has been widely implemented by provider organizations, CMS, and other third-party payers. By 2011, more than 1,500 provider practices nationwide had received medical home recognition from the National Committee for Quality Assurance (NCQA) (NCQA, 2011).8
CMS currently is participating in three PCMH initiatives. First, under the Medicare Multi-Payer Advanced Primary Care Demonstration, CMS is joining state reform initiatives involving multiple payers (including Medicaid and private health plans) by paying a monthly care management fee for beneficiaries receiving medical home care. This program, operating in eight
_________________
8NCQA created a self-report evaluation for physician practices, which has become the evaluation tool used to judge most ongoing demonstrations. This tool has three levels and assesses nine standards: access and communication, patient tracking and registries, care management, patient self-management support, electronic prescribing, test tracking, referral tracking, performance reporting and improvement, and advanced electronic communications.
states over a 3-year period, covers more than 1,200 provider practices and nearly 1 million beneficiaries (CMS, 2013g). Second, CMS, partnering with the Health Resources and Services Administration (HRSA), supports the Federally Qualified Health Center (FQHC) Advanced Primary Care Practice Demonstration, which pays a monthly care management fee for each eligible Medicare beneficiary receiving primary care services through 1 of 492 FQHCs meeting NCQA requirements for a medical home. CMS and HRSA also will provide technical assistance (e.g., webinars on quality standards) to help FQHCs achieve quality and cost goals (CMS, 2013e). Finally, the Comprehensive Primary Care Initiative is another multipayer program, in which CMS and participating private insurers give primary care providers bonus payments for improving care coordination (CMS, 2013c).
A small but growing body of research is devoted to evaluating the effects of the PCMH model. A recent review of 19 studies revealed “moderately strong evidence suggest[ing] that the medical home has a small positive effect on patient experiences and small to moderate positive effects on preventive care services” (Jackson et al., 2013, p. 175). According to the authors, however, current evidence is insufficient to determine how the PCMH will influence most clinical and economic outcomes.
Bundled Payment
Under bundled payment, a payer makes a single payment for all services (a bundle) provided during an episode of care. The definition of an episode of care is challenging and fundamental to the implementation of this payment approach (Hussey et al., 2012). Episodes of care range from single acute medical conditions to periods of treatment for chronic disease. Bundled payment targets an entity (e.g., hospital, health care organization or network) capable of receiving payment, which then divides the payment among those providing episode-based care (e.g., the hospital, the laboratory, physicians, post-acute care providers) (CMS, 2013b; Pham et al., 2010). If patients are treated by providers not affiliated with the entity receiving the bundled payment, payers may reimburse those providers on a fee-for-service basis, adjusting each payment to the overarching organization so that total payment to all service providers does not exceed a predefined bundled cost. This process is referred to as “virtual” bundling (American Medical Association, 2012). Bundled payment approaches usually incorporate quality measures, increasing provider payments when quality standards are met.
Proponents note that bundled payment has the potential to decrease health care waste by reducing incentives to provide unnecessary services as part of an episode of care and increasing care coordination (Burton, 2012). More specifically, if bundled payment includes services received from mul-
tiple providers, such as physicians, hospitals, and post-acute care providers, incentives are offered to coordinate care (share information), shift care to more efficient providers, and reduce duplicative tests and unnecessary physician visits (Painter, 2013).
As previously stated, CMS’s long-standing (since 1983) inpatient DRG payment system is a form of bundled payment in that it bundles facility-only services for a given hospital stay. By no longer paying hospitals per diem, the DRG system removed the financial incentive to keep patients in the hospital longer, leading to significant reductions in hospital patients’ lengths of stay (Guterman and Dobson, 1986; Zuckerman et al., 1988). However, studies found that hospitals responded to the new payment system by shifting patients to exempt hospitals (Newhouse and Byrne, 1988) and subsequently to post-acute care facilities that were not included in the DRG payment, causing a spike in the use of home health care and skilled nursing facilities. Quality of care was found not to be impacted by any of these changes (Rogers et al., 1990).
The DRG example demonstrates that providers do respond to payment changes. Many policy makers have further concluded that bundled payment should therefore be broadened to include services from multiple providers (e.g., outpatient and post-acute care providers) because the broader the scope of the bundles, the less latitude there is for substitution (Burton, 2012; Guterman et al., 2009).
Several bundled payment pilots now under way may provide additional evaluation evidence (CMS, 2013b; Hussey et al., 2011). For example, the Center for Medicare and Medicaid Innovation’s Bundled Payments for Care Improvement program varies several elements across four models. The first model includes only inpatient care in an acute care hospital for all DRGs, excluding physician services. Hospitals receive a discounted payment but can share any savings with physicians. The second model includes acute inpatient and post-acute care ending either 30 or 90 days after an acute care discharge for selected DRGs. The third model includes only post-acute care beginning within 30 days of an inpatient discharge for selected DRGs. Finally, the fourth model incorporates all care services, including those of a physician, provided during an acute inpatient stay and readmissions. All of these arrangements include shared savings, and participants have considerable discretion in designing payment allocations (CMS, 2013b).
Private-sector payers and providers also are experimenting with bundled payment, and related findings should be relevant to Medicare’s pursuit of a long-term payment bundling strategy (Bandell, 2011; Business Wire, 2012; Healthcare Finance News, 2011; Orthopedic & Sports Institute, 2012; SSM Health Care, 2011). For example, Geisinger Health System developed a successful bundled payment program for coronary artery bypass
graft surgery (Casale et al., 2007) and has begun implementing bundled payment for additional services (Paulus et al., 2008).
Evaluation literature on bundled payment programs remains scant. In the early 1990s, CMS selected seven hospitals to participate in a bundled payment demonstration for bypass surgery that included all hospital, physician, and other practitioner services provided during a hospital stay plus related readmissions occurring from 3 days to 6 weeks postdischarge. Bundled payments were not adjusted for illness severity. An evaluation of the program showed promising results, with savings of 5 to 10 percent for five hospitals and 20 percent for two hospitals. According to Nelson (2012, p. 20), “Those savings reflect the estimated difference between the bundled payments and the amounts that Medicare would have spent for services provided to those bypass patients in the absence of the demonstration.” A systematic review of bundled payment programs found weak but consistent evidence that they reduce costs without adversely impacting quality, although most previous programs have had a more limited scope than the Bundled Payments for Care Improvement program and other recent bundled payment initiatives (Hussey et al., 2012).
Accountable Care Organizations
The ACO is a health care delivery and financing model currently being tested by CMS and commercial insurers. ACO reforms target organized provider organizations and networks that assume responsibility for the quality, cost, and overall care of their patient populations (Correia, 2011; Fisher et al., 2007). ACOs are designed to improve value by giving provider-led organizations a stake in maximizing efficiency within and across delivery settings to meet cost and quality targets. To achieve goals, ACOs might focus on a variety of activities, such as quality improvement, care coordination and discharge processes, protocols for home health referrals favoring efficient providers for referrals, or targeting high-risk individuals for disease management programs. ACOs are expected to emphasize initiatives most effective in lowering the cost of care and improving outcomes for their populations (Guterman et al., 2011; Nelson, 2012; Share and Mason, 2012).
ACOs vary in structure, ranging from fully integrated health care organizations to networks of hospital(s) and independent primary care and specialty physicians (CMS, 2013d). However, ACOs must meet a base level of organizational capacity in order to assume their responsibilities. Recognizing that ACOs need to have adequate organizational capacity, CMS and private payers call for these health care delivery systems to have (1) a sufficient number of primary care clinicians providing care for a mini-
mum number of beneficiaries, (2) data systems for monitoring and evaluating quality and cost, (3) processes promoting evidence-based medicine, and (4) the ability to receive and distribute performance-based payments (Muhlestein, 2013).
ACOs resemble managed care organizations, but typically are provider organizations rather than traditional insurers.9 Under Medicare, ACO beneficiaries are not restricted to using ACO-affiliated physicians or facilities; rather, they have full access to all providers accepting Medicare (CMS, 2013a). In the private-sector ACOs, however, the design of insurance benefits steers patients to affiliated providers. For example, health maintenance organization (HMO) plans restrict patients to plan providers, while preferred provider organization (PPO) plans allow for out-of-network service but with higher cost sharing for patients who receive care from out-of-network providers. Medicare ACO providers will need similar incentives to encourage patients to receive their care within network (Van Citters et al., 2012).
CMS currently has three programs promoting ACOs: the Pioneer ACO Model program, the Medicare Shared Savings Program (MSSP), and the Advanced Payment Models ACOs. There are currently 269 health care delivery organizations participating in these programs—32 in the Pioneer ACO Model program, 222 in the MSSP, and 15 in Advanced Payment Model ACOs—reaching more than 4 million Medicare beneficiaries (CMS, 2013h). The three programs differ primarily in the degree of financial risk health care delivery systems agree to assume; plans can choose a payment option that gives them larger rewards when they reduce expenditures if they also agree to accept losses when Medicare expenditures are too high.
Additionally, several states are exploring the possibility of forming ACOs for their Medicaid populations. Medicaid ACO programs vary by state, and are thought to be influenced by the state’s managed care experience. Examples include Massachusetts’s capitated, multipayer model and Vermont’s community-based ACO model (Kaiser Commission on Medicaid and the Uninsured, 2012). Oregon has launched an initiative involving ACO-like coordinated care organizations and currently has 15 such organizations operating in the state (Oregon.gov, 2013).
As indicated earlier, the ACO concept has been adopted by the private sector as well; in fact, more than 150 private-sector ACOs were in existence or in the planning stages prior to the launch of CMS’s Pioneer ACO Model program (Muhlestein, 2013). Many provider organizations have entered into contractual relationships with private payers to implement payment approaches resembling the MSSP. Other health care organizations have
_________________
9Much like insurers, however, an ACO may and often will contract with physician groups on either a risk or fee-for-service basis, as indeed the FHS example discussed earlier illustrates.
entered into contracts with private payers, such as Blue Cross Blue Shield of Massachusetts’s Alternative Quality Contract, under global payment10 (Song and Landon, 2012) or other arrangements (e.g., partial capitation11 and bundled payment) (Muhlestein, 2013). Finally, in recent years, multiple stakeholders (e.g., payers, providers, employers, local governments) have formed region- or community-based “collaboratives” focused on improving the value of health care for their populations. Like ACOs and other integrated organizations, such collaboratives vary in size and structure and may or may not align with traditional geographic units. Thus, they are distinct from geographic areas targeted by a geographically based value index. Box 4-1 presents selected examples of these collaboratives.
Given that the ACO concept is new, evidence demonstrating its impact is sparse. Studies on CMS’s Physician Group Practice Demonstration (PGPD), the model for the ACA’s ACO provisions, found substantial heterogeneity in results across demonstration sites and population subgroups. One study found that on average, the PGPD saved a mean of $114 annually per beneficiary assigned to a multispecialty physician group in 1 of 10 ACO demonstration sites. However, “Among dually eligible beneficiaries, PGPD physician groups achieved a mean annual per capita savings of $532, or 5%, while savings among non-dually eligible beneficiaries were not statistically significant” (Colla, 2012, p. 1020). Unfortunately, neither the overall results nor even the dually eligible results are likely to be statistically significant when one accounts for heterogeneity among organizations.12 Another study determined that all 10 participating multispecialty groups met at least 29 of 32 quality measures, yet only 5 of the groups generated Medicare savings, totaling $38.7 million. Further, just one group (Marshfield Clinic) earned more than half of the $31.7 million that was returned to the physician groups (Iglehart, 2010).
One study examined Blue Cross Blue Shield of Massachusetts’s ACO-style Alternative Quality Contract (Song and Landon, 2012). The authors found that although the program improved quality scores and produced savings of 2.8 percent over its first 2 years, additional payments (e.g., shared savings and infrastructure) to groups exceeded the savings. Because this program was designed for implementation over a 5-year period and because the savings in the final years are expected to be larger, it may be premature to judge the program’s ultimate success.
_________________
10Under global payment, an ACO is at financial risk for all of the items and services covered.
11Under partial capitation payment, an ACO is at financial risk for some, but not all, of the items and services covered (Center for Healthcare Quality and Payment Reform, 2010).
12The authors did not cluster standard errors on organization, but the results among the dually eligible population in the 10 organizations in the demonstration spanned a wide range, from an estimated savings of $2,499 per dual-eligible at the low end to a cost of $598 at the high end. In 4 of the 10 organizations studied, costs increased for the dually eligible.
BOX 4-1
Multistakeholder Community-Based Collaboratives
Much like accountable care organizations (ACOs) or other integrated organizations, multistakeholder community-based collaboratives may implement a vast range of initiatives, such as those designed to improve data collection and dissemination, promote efficient health care delivery, and provide financial incentives for high-value care (Alliance for Health Reform, 2013; Sennett et al., 2011). Examples of these collaboratives include those found in the Agency for Healthcare Research and Quality’s (AHRQ’s) learning network for chartered value exchanges and the Brookings Institution’s evaluation of three community-based reforms in care for chronic conditions:
• AHRQ’s learning network for chartered value exchanges since 2007 has brought together 24 community multistakeholder collaboratives from 22 states across the country representing 124 million lives. Thirteen of these collaboratives are statewide programs, while the rest have a substate or regional focus. The value exchanges’ main mission is to improve quality and transparency through public reporting of quality and efficiency measurement, provider and consumer incentives, and collaborative leadership (AHRQ, 2011).
• The Primary Care Information Project in New York City is an electronic health record adoption and data exchange initiative designed to improve access to preventive services in the ambulatory care setting, primarily for prevention of chronic diseases among the city’s underserved (PCIP, 2013).
• Vermont’s Blueprint for Health is a statewide medical home program for patients with chronic conditions (Vermont.gov, 2013).
• The Wisconsin Health Information Organization is a statewide initiative designed to create an all-payer database with which to track health care costs and quality measures, data that can be used to improve the value of care for Wisconsinites with chronic diseases (Wisconsin Health Information Organization, 2013).
Given differences in population demographics, health information technology and other health service infrastructure, and resources among communities, regions, and states, collaboratives differ in their stated health objectives, their chosen initiatives, and the robustness of their interventions (Sennett et al., 2011). To the extent that these community or regional efforts can demonstrate that they improve value, however, payment incentives could be directed toward these collaboratives.
Dual-Eligible Care Integration Demonstrations
The more than 9 million Americans who are eligible for both Medicare and Medicaid benefits account for a disproportionate share of Medicare expenditures: Although they constitute 18 percent of traditional Medicare beneficiaries, they account for 31 percent of Medicare spending (MedPAC, 2012b). Differences between Medicare and Medicaid policies associated with provider reimbursement, beneficiary benefits, and financial incentives result in a health care delivery system more fragmented and uncoordinated for this population than for other Medicare beneficiaries. In April 2011, CMS provided grants to 15 states to undertake care integration initiatives for dual-eligible populations (states will test capitated and/or managed fee-for-service models). One goal of the demonstrations is to determine which care integration and payment models are most effective in improving the quality and efficiency of care for this heterogeneous population. According to the Medicare Payment Advisory Commission (MedPAC, 2012b, p. 63), “The demonstrations are also an opportunity to test how to tailor capitated and [fee-for-service] overlay models to different subgroups of dual-eligible beneficiaries.”
The Future of New Payment Reform Models
By creating the Center for Medicare and Medicaid Innovation, the ACA generated a thousand pilot demonstrations of new payment models. It is too early to know which of these models will prove to control health care costs and improve quality. As illustrated by the examples provided above, evidence supporting the effectiveness of new payment models such as VBP, PCMH, bundled payment, and ACOs in controlling costs and improving health outcomes is limited (GAO, 2011; Petersen et al., 2006; Rosenthal, 2008; Scott et al., 2011; Werner et al., 2011). Results of such efforts have been uneven; in the PGPD, for example, 5 of 10 provider organizations achieved CMS’s required cost savings to collect bonuses (Iglehart, 2010). Because these models are still in the early stages of development, however, it is critical that CMS continue to evaluate them and use the results to refine their design (IOM, 2012; The National Commission on Physician Payment Reform, 2013). In the interim, the new payment models require payers and providers to make decisions about major design elements despite the lack of adequate evidence to guide those decisions. They must decide (1) which quality and cost indicators to use, (2) how large incentives should be in absolute terms and relative to provider revenue, (3) which services to include in bundles (for bundled payment), and (4) how to assign beneficiaries to particular providers or provider organizations (Miller, 2007). As McClellan (2011, p. 75) noted, “As capacity to measure healthcare processes and outcomes continues to expand rapidly, in conjunction with at least some
growing confidence that we are measuring the right things, the linkages between provider payments and measured quality are likely to strengthen.”
New payment reforms are designed to reward efficient providers of care and stimulate inefficient providers to improve the care they deliver. In accordance with its statement of task, the committee commissioned RAND Corporation to perform an impact analysis of its recommendations. RAND modeled the impact of pay-for-performance (equivalent to VBP), bundled payment, and ACOs on hospitals, hospital referral regions (HRRs), and total Medicare spending.13 RAND’s analysis demonstrates that payment reforms targeting health care decision makers can result in large changes (by design) in payments to providers within HRRs, even if those reforms do not substantially affect geographic variation in spending among HRRs. In the case of VBP, for example, payment redistributions had no impact on geographic variation, largely because there was no relationship between performance on the quality measures and Medicare spending. The bundled payment policy, however, did reduce geographic variation in Medicare spending since high-spending providers (for selected bundles) were in areas with high overall Medicare spending. Some providers/health systems will flourish with these new incentives; others will struggle, particularly in the first few years (Haywood and Kosel, 2011). It is also likely that local market factors (e.g., population demographics, provider competition) will influence providers’ abilities to handle the new payments (Guterman et al., 2011; Pollack and Armstrong, 2011; Werner, 2010); thus, models suited for some areas will face greater challenges in others.
Finally, although some disruption to the current system is inevitable and even warranted, it is critical that Medicare beneficiaries’ access to medical care not be diminished. As reforms transition from pilot demonstrations to broader programs, CMS will need to monitor Medicare beneficiaries’ access to care.
RECOMMENDATION 4: During the transition to new payment models, the Centers for Medicare & Medicaid Services (CMS) should conduct ongoing evaluations of the impact on value of the reforms included in Recommendation 3 by measuring Medicare spending and beneficiaries’ clinical health outcomes. CMS
_________________
13Time constraints limited the scope of RAND’s work to these three payment reforms. Further, given that the committee’s research did not yield recommendations on the specifics of payment reforms, the committee did not comment further on the many scenarios modeled by RAND. RAND’s report can be accessed at www.iom.edu/geovariationmaterials.
should use the results of these evaluations to iteratively improve these payment models. CMS should also monitor how these reforms impact Medicare beneficiaries’ access to medical care.
ENCOURAGING BROADER ADOPTION OF NEW PAYMENT REFORMS
If evaluations of pilot reforms demonstrate improvements in value, the next step will be generalization of the reforms to broader populations. Congress might direct the Secretary of Health and Human Services to make the reforms mandatory for all (or a subset of) health care providers that accept Medicare patients. Alternatively, Congress might direct CMS to encourage providers to accept the new payment models through lower updates for traditional Medicare than for new payment models. Translating pilot programs into national policy will be a challenge (Chernew and Goldman, 2013; Greenwald, 2011). As stated earlier, new payment models require major investments in infrastructure (e.g., HIT systems, care managers) if it is to be managed effectively (Korda and Eldridge, 2011). If the new models were mandated before a majority of health care providers had developed the required infrastructure, many organizational failures (e.g., bankruptcies) might result, negatively affecting Medicare beneficiaries’ access to care. Similarly, provider organizations will accept new payment models voluntarily only if they believe that bonuses or shared savings will be sufficient to cover their investment in the infrastructure required to achieve efficiencies (Pham et al., 2010). Particularly in the beginning, therefore, Congress might avoid prescribing an immediate wholesale change in payment instead directing CMS to accelerate the adoption of payment reforms by authorizing differential payment updates for new payment models and traditional Medicare (Davis and Guterman, 2007). It should also be noted that providers serving disproportionately low-income populations may face especially difficult challenges in accessing the necessary resources and may require additional funding to build the organizational capacity to transition to the new payment models (Pollack and Armstrong, 2011; Werner, 2010).
Additionally, Congress should give CMS the flexibility to experiment with the mix of payment mechanisms, rates, and performance metrics that will align provider incentives with high-value care. For example, CMS might test a blended model for payment to PCMHs that combines fee-for-service payments, per-member-per-month (PMPM) care coordination fees, and bonuses for meeting quality and efficiency metrics (e.g., generic prescribing, reduced emergency department use, better management of selected chronic conditions) (Davis and Guterman, 2007). While evaluations are ongoing, CMS should be allowed to alter the levels and payment rates within models to determine those that are most effective.
RECOMMENDATION 5: If evaluations of specific payment reforms demonstrate increased value, Congress should give the Centers for Medicare & Medicaid Services the flexibility to accelerate the transition from traditional Medicare to new payment models.
Advocate Health Care. 2013. 2013 value report: Clinical integration program evolution. http://www.advocatehealth.com/clinical-integration-program-overview (accessed July 18, 2013).
AHRQ (Agency for Healthcare Research and Quality). 2011. Overview: AHRQ learning network for chartered value exchanges. http://www.ahrq.gov/professionals/quality-patient-safety/quality-resources/value/lncveover.html (accessed July 10, 2013).
Alliance for Health Reform. 2013. Select community quality initiatives map. http://allhealth.org/community-initiatives.asp (accessed February 19, 2013).
American Hospital Association. 2010a. Accountable care organization synthesis report. Washington, DC: American Hospital Association.
———. 2010b. Clinical integration—The key to real reform. Washington, DC: American Hospital Association.
American Medical Association. 2012. Bundled payments. http://www.ama-assn.org/ama/pub/physician-resources/practice-management-center/claims-revenue-cycle/managed-care-contracting/evaluating-payment-options/bundled-payments.page (accessed July 18, 2013).
Audet, A.-M. J., M. M. Doty, J. Shamasdin, and S. C. Schoenbaum. 2005. Measure, learn, and improve: Physicians’ involvement in quality improvement. Health Affairs 24(3):843-853.
Bandell, B. 2011. Blue Cross signs first bundled payment deal with Miami firm. http://www.bizjournals.com/southflorida/print-edition/2011/04/08/blue-cross-signs-first-bundled.html?page=all (accessed June 18, 2013).
Bodenheimer, T. 2008. Coordinating care—A perilous journey through the health care system. New England Journal of Medicine 358(10):1064-1071.
Burns, L. R., and R. W. Muller. 2008. Hospital-physician collaboration: Landscape of economic integration and impact on clinical integration. Milbank Quarterly 86(3):375-434.
Burton, R. 2012. Improving care transitions. http://www.rwjf.org/content/dam/farm/reports/issue_briefs/2012/rwjf401314 (accessed July 18, 2013).
Business Wire. 2012. 21st Century Oncology and Humana break new ground with case rate reimbursement agreement. http://www.businesswire.com/news/home/20120808006089/en/21st-Century-Oncology-Humana-Break-Ground-Case (accessed June 18, 2013).
Campbell, S. M., D. Reeves, E. Kontopantelis, B. Sibbald, and M. Roland. 2009. Effects of pay for performance on the quality of primary care in England. New England Journal of Medicine 361(4):368-378.
Casale, A. S., R. A. Paulus, M. J. Selna, M. C. Doll, A. E. Bothe, Jr., K. E. McKinley, S. A. Berry, D. E. Davis, R. J. Gilfillan, B. H. Hamory, and G. D. Steele, Jr. 2007. “ProvenCareSM”: A provider-driven pay-for-performance program for acute episodic cardiac surgical care. Annals of Surgery 246(4):613-621; discussion 621-613.
Casalino, L., R. R. Gillies, S. M. Shortell, J. A. Schmittdiel, T. Bodenheimer, J. C. Robinson, T. Rundall, N. Oswald, H. Schauffler, and M. C. Wang. 2003. External incentives, information technology, and organized processes to improve health care quality for patients with chronic diseases. Journal of the American Medical Association 289(4):434-441.
Cassidy, A. 2010. Patient-centered medical homes. http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=25 (accessed July 18, 2013).
Cebul, R. D., J. B. Rebitzer, L. J. Taylor, and M. E. Votruba. 2008. Organizational fragmentation and care quality in the U.S. healthcare system. Journal of Economic Perspectives 22(4):93-113.
Cebul, R. D., T. E. Love, A. K. Jain, and C. J. Hebert. 2011. Electronic health records and quality of diabetes care. New England Journal of Medicine 365(9):825-833.
Center for Healthcare Quality and Payment Reform. 2010. Using partial capitation as an alternative to shared savings to support accountable care organizations in Medicare. http://www.chqpr.org/downloads/PartialCapitationPaymentforACO.pdf (accessed July 18, 2013).
Chernew, M., and D. Goldman. 2013. Transitioning to bundled payments in Medicare. In 15 ways to rethink the federal budget. Washington, DC: The Hamilton Project. Pp. 12-16.
Chuang, K. H., H. S. Luft, and R. A. Dudley. 2004. The clinical and economic performance of prepaid group practice. In Toward a 21st century health system: The contributions and promise of prepaid group practice, edited by A. C. Enthoven and L. A. Tollen. San Francisco, CA: Jossey-Bass. Pp. 45-60.
CMS (Centers for Medicare & Medicaid Services). 2012. Pioneer accountable care organization model: General fact sheet. http://innovation.cms.gov/Files/fact-sheet/Pioneer-ACO-General-Fact-Sheet.pdf (accessed July 18, 2013).
———. 2013a. Accountable care organizations (ACO). http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ACO/index.html?redirect=/aco (accessed July 18, 2013).
———. 2013b. Bundled payments for care improvement (BPCI) initiative: General information. http://innovation.cms.gov/initiatives/bundled-payments (accessed July 18, 2013).
———. 2013c. Comprehensive primary care initiative. http://innovation.cms.gov/initiatives/comprehensive-primary-care-initiative (accessed May 23, 2013).
———. 2013d. Fast facts—All Medicare shared savings program and Medicare pioneer ACOs. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/PioneersMSSPCombinedFastFacts.pdf (accessed July 10, 2013).
———. 2013e. FQHC advanced primary care practice demonstration. http://innovation.cms.gov/initiatives/FQHCs (accessed May 23, 2013).
———. 2013f. More doctors, hospitals partner to coordinate care for people with Medicare: Providers form 106 new accountable care organizations. http://www.cms.gov/apps/media/press/release.asp?Counter=4501&intNumPerPage=10&checkDate=&checkKey=&srchType=1&numDays=3500&srchOpt=0&srchData=&keywordType=All&chkNewsType=1%2C+2%2C+3%2C+4%2C+5&intPage=&showAll=&pYear=&year=&desc=&cboOrder=date (accessed July 18, 2013).
———. 2013g. Multi-payer advanced primary care practice. http://innovation.cms.gov/initiatives/Multi-Payer-Advanced-Primary-Care-Practice (accessed May 23, 2013).
———. 2013h. Shared savings program: Program news and announcements. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/News.html (accessed July 18, 2013).
Colla, C. H. 2012. Spending differences associated with the Medicare physician group practice demonstration. Journal of the American Medical Association 308(10):1015-1023.
Correia, E. W. 2011. Accountable care organizations: The proposed regulations and the prospects for success. American Journal of Managed Care 17(8):560-568.
Davis, K., and S. Guterman. 2007. Rewarding excellence and efficiency in Medicare payments. Milbank Quarterly 85(3):449-468.
Decker, S. L., E. W. Jamoom, and J. E. Sisk. 2012. Physicians in nonprimary care and small practices and those age 55 and older lag in adopting electronic health record systems. Health Affairs 31(5):1108.
Dolan, E., and D. Yanagihara. 2011. Value based pay for performance in California. Issue brief no. 4. Oakland, CA: Integrated Healthcare Association.
Doran, T., E. Kontopantelis, J. M. Valderas, S. Campbell, M. Roland, C. Salisbury, and D. Reeves. 2011. Effect of financial incentives on incentivised and non-incentivised clinical activities: Longitudinal analysis of data from the UK Quality and Outcomes Framework. British Medical Journal 342:d3590.
Enthoven, A. 2009. Integrated delivery systems: The cure for fragmentation. American Journal of Managed Care 15:S284-S290.
Fendrick, A. M., and M. E. Chernew. 2006. Value-based insurance design: Aligning incentives to bridge the divide between quality improvement and cost containment. American Journal of Managed Care 12 Spec no. SP5-SP10.
Fisher, E. S., D. O. Staiger, J. P. W. Bynum, and D. J. Gottlieb. 2007. Creating accountable care organizations: The extended hospital medical staff. Health Affairs 26(1):w44-w57.
Folsom, A., C. Demchak, and S. B. Arnold. 2008. Rewarding results pay-for-performance: Lessons for Medicare. http://www.hcfo.org/pdf/monograph0308.pdf (accessed July 18, 2013).
Frakt, A. B., and R. Mayes. 2012. Beyond capitation: How new payment experiments seek to find the “sweet spot” in amount of risk providers and payers bear. Health Affairs 31(9):1951-1958.
GAO (Government Accountablility Office). 2011. Value in health care: Key information for policymakers to access efforts to improve quality while reducing costs. Washington, DC: GAO.
Gaynor, M., J. B. Rebitzer, and L. J.Taylor. 2001. Incentives in HMOs. Cambridge, MA: National Bureau of Economic Research.
Goldberg, D. G., S. S. Mick, A. J. Kuzel, L. B. Feng, and L. E. Love. 2013. Why do some primary care practices engage in practice improvement efforts whereas others do not? Health Services Research 48(2, pt. 1):398-416.
Greenwald, L. M. 2011. Converting successful Medicare demonstrations into national programs. In Pay for performance in health care: Methods and approaches, edited by J. Cromwell, M. G. Trisolini, G. C. Pope, J. B. Mitchell and L. M. Greenwald. Research Triangle Park, NC: Research Triangle Institute. Pp. 315-340.
Guterman, S., and A. Dobson. 1986. Impact of the Medicare prospective payment system for hospitals. Health Care Financing Review 7(3):97-114.
Guterman, S., and H. Drake. 2010. Developing innovative payment approaches: Finding the path to high performance. New York: The Commonwealth Fund.
Guterman, S., K. Davis, S. Schoenbaum, and A. Shih. 2009. Using Medicare payment policy to transform the health system: A framework for improving performance. Health Affairs 28(2):w238-w250.
Guterman, S., S. C. Schoenbaum, K. Davis, C. Schoen, A.-M. J. Audet, K. Stremikis, and M. A. Zezza. 2011. High performance accountable care: Building on success and learning from experience. New York: The Commonwealth Fund.
Hastings, D. 2012. Medicare ACOs: The integration of financial and clinical integration. http://healthaffairs.org/blog/2012/04/11/medicare-acos-the-integration-of-financial-and-clinical-integration (accessed July 18, 2013).
Haywood, T. T., and K. C. Kosel. 2011. The ACO model—A three-year financial loss? New England Journal of Medicine 364(14):e27.21-e27.23.
Healthcare Finance News. 2011. Caromont Health and BCBSNC announce bundled payment program for knee replacement. http://www.healthcarefinancenews.com/press-release/caromont-health-and-bcbsnc-announce-bundled-payment-program-knee-replacement (accessed June 18, 2013).
Herrin, J., B. da Graca, D. Nicewander, C. Fullerton, P. Aponte, G. Stanek, T. Cowling, A. Collinsworth, N. S. Fleming, and D. J. Ballard. 2012. The effectiveness of implementing an electronic health record on diabetes care and outcomes. Health Services Research 47(4):1522-1540.
Holroyd-Leduc, J. M., D. Lorenzetti, S. E. Straus, L. Sykes, and H. Quan. 2011. The impact of the electronic medical record on structure, process, and outcomes within primary care: A systematic review of the evidence. Journal of the American Medical Informatics Association 18(6):732-737.
Hussey, P. S., M. S. Ridgely, and M. B. Rosenthal. 2011. The PROMETHEUS bundled payment experiment: Slow start shows problems in implementing new payment models. Health Affairs 30(11):2116-2124.
Hussey, P. S., A. W. Mulcahy, C. Schnyer, and E. C. Schneider. 2012. Bundled payment: Effects on health care spending and quality closing the quality gap: Revisiting the state of the science. In Evidence Report/Technology Assessment Number 208. AHRQ Publication No. 12-E007-EF.
Iglehart, J. K. 2010. Assessing an ACO prototype—Medicare’s physician group practice demonstration. New England Journal of Medicine 364(3):198-200.
IOM (Institute of Medicine). 2012. Best care at lower cost: The path to continuously learning health care in America. Washington, DC: The National Academies Press.
Jackson, G. L., B. J. Powers, R. Chatterjee, J. P. Bettger, A. R. Kemper, V. Hasselblad, R. J. Dolor, R. J. Irvine, B. L. Heidenfelder, A. S. Kendrick, R. Gray, and J. W. Williams, Jr. 2013. The patient-centered medical home: A systematic review. Annals of Internal Medicine 158(3):169-178.
James, J. 2012. Pay-for-performance. New payment systems reward doctors and hospitals for improving the quality of care, but studies to date show mixed results. http://healthaffairs.org/healthpolicybriefs/brief_pdfs/healthpolicybrief_78.pdf (accessed July 18, 2013).
Jamoom, E., P. Beatty, A. Bercovitz, D. Woodwell, K. Palso, and E. Rechtsteiner. 2012. Physician adoption of electronic health record systems: United States, 2011. NCHS Data Brief 98:1-8.
Jha, A. K., K. Joynt, J. Orav, and A. Epstein. 2012. The long-term effect of premier pay for performance on patient outcomes. New England Journal of Medicine 366:1606-1615.
Kaiser Commission on Medicaid and the Uninsured. 2012. Emerging Medicaid accountable care organizations: The role of managed care. Washington, DC: Kaiser Family Foundation.
Kern, L. M., A. Wilcox, J. Shapiro, R. V. Dhopeshwarkar, and R. Kaushal. 2012. Which components of health information technology will drive financial value? American Journal of Managed Care 18(8):438-445.
Korda, H., and G. N. Eldridge. 2011. Payment incentives and integrated care delivery: Levers for health system reform and cost containment. Inquiry 48(4):277-287.
Landon, B. E., I. B. Wilson, and P. D. Cleary. 1998. A conceptual model of the effects of health care organizations on the quality of medical care. Journal of the American Medical Association 279(17):1377-1382.
Lindenauer, P. K., D. Remus, S. Roman, M. B. Rothberg, E. M. Benjamin, A. Ma, and D. W. Bratzler. 2007. Public reporting and pay for performance in hospital quality improvement. New England Journal of Medicine 356(5):486-496.
Lochner, K. A., and C. S. Cox. 2013. Prevalence of multiple chronic conditions among Medicare beneficiaries, United States, 2010. Preventing Chronic Disease 10:E61.
Maeng, D. D., J. Graham, T. R. Graf, J. N. Liberman, N. B. Dermes, J. Tomcavage, D. E. Davis, F. J. Bloom, and G. D. Steele, Jr. 2012. Reducing long-term cost by transforming primary care: Evidence from Geisinger’s medical home model. American Journal of Managed Care 18(3):149-155.
Mayes, R., and R. A. Berenson. 2006. Medicare prospective payment and the shaping of U.S. health care. Baltimore, MD: The Johns Hopkins University Press.
McClellan, M. 2011. Reforming payments to healthcare providers: The key to slowing healthcare cost growth while improving quality? Journal of Economic Perspectives 25(2):69-92. McWilliams, J. M., M. E. Chernew, A. M. Zaslavsky, P. Hamed, and B. E. Landon. 2013. Delivery system integration and health care spending and quality for Medicare beneficiaries. JAMA Internal Medicine 173(15):1439-1444.
Mechanic, R., and D. E. Zinner. 2012. Many large medical groups will need to acquire new skills and tools to be ready for payment reform. Health Affairs 31(9):1984-1992.
MedPAC (Medicare Payment Advisory Commission). 2012a. Medicare and the health care delivery system. In Report to the Congress: June 2012. Washington, DC: MedPAC.
———. 2012b. Medicare payment policy. In Report to the Congress: March 2012. Washington, DC: MedPAC.
Miller, H. D. 2007. Creating payment systems to accelerate value-driven health care: Issues and options for policy reform. Washington, DC: The Commonwealth Fund.
———. 2011. Testimony of Harold D. Miller. http://democrats.energycommerce.house.gov/sites/default/files/image_uploads/Testimony_Miller_05.05.11_SGR.pdf (accessed July 18, 2013).
Moullec, G., K. L. Lavoie, K. Rabhi, M. Julien, H. Favreau, and M. Labrecque. 2012. Effect of an integrated care programme on re-hospitalization of patients with chronic obstructive pulmonary disease. Respirology 17(4):707-714.
Muhlestein, D. 2013. Continued growth of public and private accountable care organizations. http://healthaffairs.org/blog/2013/02/19/continued-growth-of-public-and-private-accountable-care-organizations (accessed July 18, 2013).
Mullen, K. J., R. G. Frank, and M. B. Rosenthal. 2008. Can you get what you pay for? Pay-for-performance and the quality of healthcare providers. Cambridge, MA: National Bureau of Economic Research.
NCQA (National Committee for Quality Assurance). 2011. New NCQA standards take patient-centered medical homes to the next level. http://www.ncqa.org/Newsroom/2011NewsArchives/NewsReleaseJanuary282011.aspx (accessed July 10, 2013).
Nelson, L. 2012. Lessons from Medicare’s demonstration projects on disease management and care coordination. Washington, DC: Congressional Budget Office.
Newhouse, J. P., and D. J. Byrne. 1988. Did Medicare’s prospective payment system cause length of stay to fall? Journal of Health Economics 7(4):413-416.
Oregon.gov. 2013. Coordinated care organizations. http://www.oregon.gov/oha/ohpb/pages/health-reform/ccos.aspx (accessed July 18, 2013).
Orthopedic & Sports Institute. 2012. Anthem Blue Cross and Blue Shield and Orthopedic & Sports Institute of the Fox Valley announce bundled payment. http://www.osifv.com/component/content/article/269-bundled-payment.html (accessed June 18, 2013).
Painter, M. W. 2013. Bundled payments: This way toward a challenging yet better place. Newtown, CT: Health Care Incentives Improvement Institute.
Partnership for Sustainable Health Care. 2013. Strengthening affordability and quality in America’s health care system. Washington, DC: Robert Wood Johnson Foundation.
Paulus, R. A., K. Davis, and G. D. Steele. 2008. Continuous innovation in health care: Implications of the Geisinger experience. Health Affairs 27(5):1235-1245.
PCIP (Primary Care Information Project). 2013. Primary Care Information Project. http://www.nyc.gov/html/doh/html/hcp/pcip.shtml (accessed July 10, 2013).
Petersen, L. A, L. D. Woodward, T. Urech, C. Daw, and S. Sookanan. 2006. Does pay-for-performance improve the quality of health care? Annals of Internal Medicine 145(4): 265-272.
Pham, H. H., D. Schrag, A. S. O’Malley, B. Wu, and P. B. Bach. 2007. Care patterns in Medicare and their implications for pay for performance. New England Journal of Medicine 356(11):1130-1139.
Pham, H. H., A. S. O’Malley, P.B. Bach, C. Saiontz-Martinez, D. Schrag. 2009. Primary care physicians’ links to other physicians through Medicare patients: The scope of care coordination. Annals of Internal Medicine 150(4):236-242.
Pham, H. H., P. B. Ginsburg, T. K. Lake, and M. Maxfield. 2010. Episode-based payments: Charting a course for health care payment reform. Washington, DC: National Institute for Health Care Reform.
Pollack, C. E., and K. Armstrong. 2011. Accountable care organizations and health care disparities. Journal of the American Medical Association 305(16):1706-1707.
Reid, R. J., K. Coleman, E. A. Johnson, P. A. Fishman, C. Hsu, M. P. Soman, C. E. Trescott, M. Erikson and E. B. Larson. 2010. The group health medical home at year two: Cost savings, higher patient satisfaction, and less burnout for providers. Health Affairs 29(5): 835-843.
Rogers, W. H., D. Draper, K. L. Kahn, E. B. Keeler, L. V. Rubenstein, J. Kosecoff, and R. H. Brook. 1990. Quality of care before and after implementation of the DRG-based prospective payment system. A summary of effects. Journal of the American Medical Association 264(15):1989-1994.
Rosenthal, M. B. 2008. Beyond pay for performance—Emerging models of provider-payment reform. New England Journal of Medicine 359(12):1197-1200.
Rosenthal, M., R. G. Frank, Z. Li, and A. M. Epstein. 2005. Early experience with pay-for-performance: From concept to practice. Journal of the American Medical Association 294(14):1788-1793.
RWJF (Robert Wood Johnson Foundation). 2012. Health policy snapshot: Health care quality. Princeton, NJ: RWJF.
Ryan, A. M., J. Blustein, and L. P. Casalino. 2012. Medicare’s flagship test of pay-for-performance did not spur more rapid quality improvement among low-performing hospitals. Health Affairs 31(4):797-805.
Scott, A., P. Sivey, D. Ait Ouakrim, L. Willenberg, L. Naccarella, J. Furler, and D. Young. 2011. The effect of financial incentives on the quality of health care provided by primary care physicians. Cochrane Database of Systematic Reviews 9:CD008451.
Sennett, C., K. Matsuoka, S. L. Kocot, M. B. McClellan, and M. Chidester. 2011. Evaluating community-based reforms in care for chronic conditions: A multi-payer template for information technology initiatives. Washington, DC: Brookings Institution.
Share, D. A., and M. H. Mason. 2012. Michigan’s physician group incentive program offers a regional model for incremental “fee for value” payment reform. Health Affairs 31(9):1993-2001.
Share, D. A., D. A. Campbell, N. Birkmeyer, R. L. Prager, H. S. Gurm, M. Moscucci, M. Udow-Phillips, and J. D. Birkmeyer. 2011. How a regional collaborative of hospitals and physicians in Michigan cut costs and improved the quality of care. Health Affairs 30(4):636-645.
Shih, A., K. Davis, S. C. Schoenbaum, A. Gauthier, R. Nuzum, and D. McCarthy. 2008. Organizing the U.S. health care delivery system for high performance. New York: The Commonwealth Fund.
Shortell, S. M., R. R. Gillies, and D. A. Anderson. 1994. The new world of managed care: Creating organized delivery systems. Health Affairs (Millwood) 13(5):46-64.
Song, Z., and B. E. Landon. 2012. Controlling health care spending—The Massachusetts experiment. New England Journal of Medicine 366(17):1560-1561.
SSM Health Care. 2011. Anthem Blue Cross and Blue Shield in Missouri and SSM Health Care-St. Louis collaborate on payment innovation. http://www.ssmhealth.com/030911anthemorthopayment (accessed June 18, 2013).
Sterns, J. B. 2007. Quality, efficiency, and organizational structure. Journal of Health Care Finance 34(1):100-107.
Stremikis, K., C. Schoen, and A. K. Fryer. 2011. A call for change: The 2011 Commonwealth Fund survey of public views of the U.S. health system. Issue Brief (Commonwealth Fund) 6:1-23.
The National Commission on Physician Payment Reform. 2013. Report of the National Commission on Physician Payment Reform. http://physicianpaymentcommission.org/wp-content/uploads/2013/03/physician_payment_report.pdf (accessed July 18, 2013).
Van Citters, A. D., B. K. Larson, K. L. Carluzzo, J. N. Gbemudu, S. A. Kreindler, F. M. Wu, S. M. Shortell, E. C. Nelson, and E. S. Fisher. 2012. Four health care organizations’ efforts to improve patient care and reduce costs. Washington, DC: The Commonwealth Fund.
Vermont.gov. 2013. Blueprint for health. http://hcr.vermont.gov/blueprint (accessed July 10, 2013).
Werner, M. 2012. Physician leadership as an essential capability for transformation and accountable care. Minneapolis, MN: Fairview Health Services.
Werner, R. M. 2010. Does pay-for-performance steal from the poor and give to the rich? Annals of Internal Medicine 153(5):340-341.
Werner, R. M., and R. A. Dudley. 2012. Medicare’s new hospital value-based purchasing program is likely to have only a small impact on hospital payments. Health Affairs 31(9):1932-1940.
Werner, R. M., J. T. Kolstad, E. A. Stuart, and D. Polsky. 2011. The effect of pay-for-performance in hospitals: Lessons for quality improvement. Health Affairs 30(4):690-698. Wisconsin Health Information Organization. 2013. The Wisconsin Health Information Organization. http://www.wisconsinhealthinfo.org (accessed July 10, 2013).
Wolfson, D., E. Bernabeo, B. Leas, S. Sofaer, G. Pawlson, and D. Pillittere. 2009. Quality improvement in small office settings: An examination of successful practices. BMC Family Practice 10(1):1-12.
Zuckerman, S., J. Feder, and J. Hadley. 1988. Hospital responses to Medicare’s prospective payment system. Bulletin of the New York Academy of Medicine 64(1):52-62.


























