2
Proceedings
Day 1
February 25, 2013
WELCOME, INTRODUCTIONS, AND OVERVIEW
Welcome from the Institute of Medicine
Dr. J. Michael McGinnis
DR. MCGINNIS: Good afternoon. I’m Michael McGinnis, from the Institute of Medicine (IOM), and it’s my pleasure and privilege to welcome all of you to the IOM and to our wonderfully restored historic National Academy of Sciences building.
This year is our sesquicentennial year. Because we were oversubscribed, some of you are watching via video feed in the Board Room. You will be viewing under the watchful eyes of President Lincoln, who was captured in a striking portrait with the assembled scientific community of 1863, the year that Congress passed and President Lincoln signed the Charter for the National Academies. The year 1863 tells us that the National Academy of Sciences was founded during a war that led to fundamental progress in extending and deepening the democratization of our political and social processes across the citizenry. In many ways, it is entirely fitting then that we’re having our conversation on patient partnering here today in the National Academy of Sciences building. Without overplaying the comparison, it seems appropriate to point out that this workshop, Partnering with Patients to Drive Shared Decisions, Better Value, and Care Improvement, is aimed at a further expansion of citizen empowerment, dedicated as it is to the democratization and deepening of the direct engagement of each individual, as participant and advocate, in the effectiveness and the efficiency of their health care, as well as in the capture of each care experience to improve the knowledge base that is the bedrock for medicine’s progress.
Before we move into the day’s proceedings, in addition to thanking each of you here today as presenters and participants, I would like to acknowledge and thank, in particular, three groups especially central to making our meeting possible. First, the Gordon and Betty Moore Foundation and the Blue Shield of California Foundation, for their generous support in sponsoring and leading the discussions up to the meeting. With us today are George Bo-Linn and Dominick Frosch from the Moore Foundation, and Richard Thomason from the Blue Shield of California Foundation. Thanks both to your foundations and to your colleagues for the support.
Second, thanks to the Planning Committee and its Chair, Christine Bechtel. This workshop is being hosted by the IOM Roundtable on Value & Science-Driven Health Care in accordance with the National Academies’ rules and procedures. An independent Planning Committee, whose roster is in your folders, has organized the workshop with the support of the IOM staff, and they clearly have done a superb job; when you look at the list of Planning Committee members, you’ll know why this meeting turned out so well.
This brings me to the third group: the IOM staff. In particular, I would like to thank Leigh Stuckhardt, who has moved on to the Centers for Medicare & Medicaid Services; Julia Sanders, with the guiding hand of Dr. Claudia Grossmann, our Senior Program Officer coordinating the work; and Valerie Rohrbach, Barret Zimmermann, and Liz Johnston, who are here to facilitate the sessions. Please join me in thanking the Foundations, the Planning Committee, and the IOM staff for their work.
I would like to flag several additional items before I turn to stage-setting comments from Dominick, on behalf of the Moore Foundation, and from Christine, on behalf of the Planning Committee. First, each of you has received the briefing materials that were assembled by the IOM staff with recommendations from the Planning Committee. You also have received a folder that contains the agenda, participant list, one-page overview of the Roundtable’s work, and background material from the recent and important Health Affairs special issue on the topic of patient engagement, including both a table of contents from that issue and one key article. In addition to these materials, you will find a one-page summary that provides an overview of the strategy map for the work of the Roundtable. In particular, I draw your attention to this document because it includes a list of the ongoing projects that are under way in the various Collaboratives of the Roundtable, which underscores the essence of this meeting’s focus on action. What we want, in effect, is to emerge from the series of conversations with an action agenda that will allow us to be more focused as we work collaboratively across our various organizations to foster progress.
The Roundtable’s projects fall into three categories: value and improving the science of transparency; science and knowledge generation as real-time processes; and culture—strong public and patient engagement. The patient as a vital leader for each of these three aims—value, science, and decision making—and the focus on patients during this workshop are obviously clear. The conference sets the stage for success across all three domains, and we’re very hopeful about the outcomes of the discussions in providing guidance for the work ahead. Finally, when it comes to action, I would like to acknowledge those of you in the room who are participants in the session and who bring to this conversation the kind of commitment that is so important to the progress ahead.
The Planning Committee has worked very hard to ensure that this is truly a patient-centered set of discussions. Of course, each of us at one time or another has been or will be a patient and witness, and thus brings occasionally painful perspectives to these sorts of discussions. In addition to the primary cadre of attendees from the patient community, some of the agenda sessions are organized with patients as co-presenters, in order to ensure that the perspectives at every level are truly representative of the issues at hand. We also have here in the room individuals who have built, and are building, important organizational capacities to lead change and help foster follow-up to our discussions. Examples include Michael Barry, President of the Informed Medical Decisions Foundation; David Blumenthal, President of The Commonwealth Fund; Bob Kaplan, Director of the National Institutes of Health’s Office of Behavioral and Social Sciences Research; Lygeia Ricciardi, Head of Consumer Health at the Office of the
National Coordinator; John Santa, of Consumer Reports; Sue Sheridan, Deputy Director of Patient Engagement at the Patient-Centered Outcomes Research Institute; and Daniel Wolfson, Chief Operating Officer at the ABIM Foundation. We could go down each and every row and it would become clearly evident to us, as if isn’t already, that this room contains the kind of leadership that can really make a difference moving forward. Please take advantage of our time together to link deeply with each other on behalf of our mutual commitments to progress.
Now, it is my privilege to turn the meeting over to those who will frame the sessions. First, Dominick Frosch will speak on behalf of the sponsors to put the meeting in the context of the Moore Foundation’s plans for leadership in this arena. Following his comments, Planning Committee Chair Christine Bechtel will lead us into the agenda. Thank you all very much.
Opening Remarks and Meeting Overview
Dr. Dominick Frosch
DR. FROSCH: Thank you very much, Michael, and good afternoon everyone. I am delighted to be here today and to welcome such a large group for discussion on this very important topic: meaningfully engaging patients and families in their health care.
On behalf of the Gordon and Betty Moore Foundation, I want to express my sincere thanks to Michael McGinnis and the tireless staff at the Institute of Medicine for all of their hard work in developing this terrific agenda that we have here. And I especially want to thank Christine Bechtel and members of the Planning Committee for all of their work. Finally, I extend my appreciation to today’s presenters for sharing your work with us here.
Now, before we delve into the specifics of how we advance the engagement of patients and families in creating a health care system that produces better outcomes and better value, I would like to spend just a few moments sharing a personal story with you. And I would like to think that this story captures some of the spirit of why we’re all here and working so hard to transform health care.
Some of you know me as a researcher, and I have been interested in shared decision making for over a decade. In recent years, I have concentrated my work on trying to implement shared decision making in routine care. Later today, Grace Lin will present work that she and I led together.
But there’s also a very personal side to this research and it’s a large part of why I was drawn to this issue in the first place. Just before I turned 17, I was diagnosed with type 1 diabetes; it was a diagnosis that was life changing. I was fortunate enough to be diagnosed in a hospital where, after I was stabilized on an insulin regimen, I went through a training program that lasted 5 full days and taught me everything that I needed to know to be able to manage the condition, to understand what it did and what I needed to do every day to be able to avoid the complications that can result from diabetes.
Now I wasn’t a model patient right away, and it took me about 6 years until I woke up one day and fully realized that all of my care was really in my hands, and that my ability to avoid the complications that can result from diabetes depended on what I did every day. So I test my blood sugar an average of eight times a day and I always know the trajectory of that blood sugar and where it’s going. In the language of medicine, I practice tight control and I’ve been doing that for almost 20 years.
The benefit of all this is that, so far, I have been able to avoid complications, and every year I go to see an ophthalmologist for an annual exam to determine whether or not I have any traces of retinopathy. Every year as that appointment approaches, I’m a little bit nervous because I expect that maybe this will be the year when the first shoe drops and there are some initial traces of retinopathy that indicate that something may need to be done. And 3 years ago when I went for this exam, the physician made a very interesting statement. First she spent a few silent minutes conducting the exam and then she stopped and said, “Everything looks clear, no trace of retinopathy,” and I said, “Whew, okay. What I’m doing is still working.” But then she said this: “You must be really good at following orders.” And I was taken aback a bit.
Her remark was in my view really both inaccurate and inappropriate. Inaccurate because I don’t do the things to manage my condition because somebody else tells me to do them; I do them for me. And it was inappropriate because imagine if she had said this to someone who didn’t know as much about managing the condition, or didn’t feel as confident about managing it as I did. As a psychologist, I can say that hers was a comment that undermines patients’ sense of what they can do and what they need to do to stay healthy. And it really sort of gets in the way of meaningfully engaging patients in their own care.
I tell you this story because I think it illustrates what we mean by changing the paradigm of health care delivery. The place where we want to get is one where the patient is a true partner with health care professionals. In fact, the most important team member, not someone who simply follows and obeys orders. Most patients don’t want to follow orders any more than doctors do, and we need to change the culture of health care and put the tools in place to make engaging patients the way we all work because it’s the right and the respectful thing to do.
It was this vision of a health care system in which patients and families are truly at the center that drew me to the Gordon and Betty Moore Foundation. Our goal in the Foundation’s new Patient Care Program is bold. We want to eliminate all preventable harm and eliminate unnecessary costs, and we include among preventable harms the loss of dignity and respect that many patients experience when they encounter the health care delivery system. We see a clear path to how this goal can be achieved. We need to meaningful engage patients and families in a redesigned system that is supportive of patients and families: a system that optimally integrates medical and information technology, interdisciplinary teams, evidence-based practices, and continual learning; a system that considers patients and families as integral partners and embraces their engagement in all aspects of health care.
We know that this goal is extraordinarily ambitious, but we all know that for patients, families and ourselves, it is the right thing to do and we must strive for nothing less. We hope that you will join us in achieving this goal. I look forward to an important and engaging discussion over the next 2 days. Again, thank you all for joining us, and now let’s get to work with advancing patient and family engagement. Thank you.
Ms. Christine Bechtel (Moderator)
MS. BECHTEL: Thanks, Dominick, and let me start by thanking the Planning Committee and to the IOM staff in particular, who really did the hard work of putting this great workshop together.
We are going to spend the next day and a half diving in to some of today’s most critical issues in health care with experts in the field that are well known for their innovation and dedication to patient and family engagement. We would like for this to be very, very interactive.
We will focus on this idea of patient, family, and citizen engagement in the three areas that Michael outlined so eloquently—shared decision making, knowledge generation for research to improve population health, and changing our expectations for value in health care. And we’ll examine the question of how we can engage patients, families, and citizens in each.
That begs the question, what is “patient and family engagement”? For most people the meaning of the phrase is kind of like a Rorschach test—it means different things to different people. I think we can do better. In fact, the Health Affairs article that you have in your packet begins to really dive into a more multifaceted definition of engagement, focused on engaging patients and families at three levels. The first, and the most often thought of, is of course engagement in their own care; we know a fair amount about that and we’re going to continue to talk about engagement in care and find even more effective ways to do so. The second is engagement in organizational or institutional design and governance. So this could be, for example, how an institution might collaborate with a group of patients and families to design a shared decision making program to figure out how the institution can build it into the workflow, not just of their clinicians, but also of their patients and families. In other words, patients and families themselves are really part of designing the process. We’ve seen this strategy work successfully and have a great impact in a number of areas, whether it’s designing a patient-centered medical home or having individual hospitals embed patients and families on safety committees, et cetera. Then the third level is policy making: engaging patients and families and their representatives in policy making. That might be at the national, state or the local level. We have some great examples of that today in the Health Information Technology Policy Committee, and other esteemed policy making bodies where patients, families and their representatives sit alongside clinicians and employers and health plans and researchers to shape public policy. PCORI is another good example of that as well.
So our goal is that, together with our terrific speakers, with the audience, with the Planning Committee panel, we can use this day and a half to start to outline a concrete and actionable pathway toward how we really accelerate progress in patient and family engagement in those three areas that I’ve outlined. The output of the day and a half will be a report of what we find and discuss, so that means that audience participation and interaction are really critical. We want to make sure that the audience has a chance to get up and not just ask questions, but also give your viewpoints and your comments.
We also have hundreds of individuals joining us online, and there is a way for you online to send in your questions, so we really encourage that as well.
Right now we’re going to start in exactly the right place, in my opinion, and that is with a voice for patients and family caregivers: Dr. Jonathan Welch. He has experiences as a family caregiver, but also as a physician, and he brings a very unique perspective to this discussion that we thought was essential to lead off with. He’s an instructor in medicine at Harvard Medical School and a practicing emergency physician at Brigham and Woman’s Hospital in Boston, and his work focuses on patient and family-centered care. He also serves on his department’s Patient and Family Advisory Council. Some of you may have seen his writing. It has been featured in Health Affairs, Roll Call, the Washington Post, and also the Chicago Tribune. So please join me in welcoming Dr. Welch.
LUNCH KEYNOTE
To Improve, Health Care Must Partner with Patients and Families
Dr. Jonathan Welch
DR. WELCH: Thank you. I’d like to begin by sharing a story about my family’s journey through the health care system and what that really taught us about the importance of patient- and family-centered care. It started about 2 years ago on a sunny September morning, on a Monday morning, when I got this call that all of you, all of us, would dread. That somebody who we care about, who we love, was in real trouble and that catastrophe could be around the corner. And on the line was an emergency physician from my Wisconsin hometown and he told me that my mother was sick. My mom, who was a retired high school teacher, she taught pregnant teen mothers and tried to get their lives back on track, had been undergoing chemotherapy treatment for breast cancer and we were really grateful. The chemotherapy had kept her cancer at bay. And we really were just taking every day and being grateful for it.
But on that day she suddenly changed. My father had found my mother very somnolent at home and he called 911. And when my mother arrived at the emergency department her heart was racing, she had a high fever, and her infection-fighting cells were very low. Now, as an emergency physician, I knew exactly what was going on. This is something that I treat in my own practice. It’s called neutropenic sepsis, and for our non-clinicians in the room this just essentially means that an individual’s infection fighting cells are low, and at the same time there’s a systemic infection.
Now there was some good news and some bad news. The bad news was that this is a life-threatening diagnosis. The good news was that there has really been a transformation over the last decade or so where the treatment of systemic infection has really been revolutionized. We now know more than 15 years ago exactly what patients with systemic infection need. Oftentimes, there are now protocols in hospitals that dictate what happens to patients with this condition. What this means is that individuals oftentimes are getting antibiotics. They are getting IV fluids and if they are particularly sick, they are getting care in an ICU center where they can get even more intensive therapies. But these studies told me something else. They told me that we were on the clock. These studies have shown that timely care of sepsis really is of the essence. It can be the difference between life and death.
And so after hearing this troubling phone call, I moved quickly from Boston to the Wisconsin Hospital where my mother was. Sequestered on that flight, really out of touch with what was going on, and knowing though that those hours really were of the essence. When I arrived in Wisconsin, I went directly to my mother’s hospital bed and you can imagine, it’s about 9:00, 12 hours after my mother initially went into this emergency department. She is now on a hospital floor and it’s a quiet city community hospital. The lights are on. She looks pale. She looks weak and it’s quiet. Her doctors have gone home for the day. It’s me, my family, and her nurse.
Now I remember talking to her, and she was very stoic, and I remember her telling me she felt fair, as if this life-threatening infection were just a little bit of a bump in the road. And one of the things I was very eager to determine early on, just a quick look, was what her blood pressure was like. This is a poor man’s way of essentially figuring out how people are responding to systemic infection treatments. So I went to the nurse’s log and looked in her book and I saw this terrifying picture with her blood pressures crashing through the day. Her blood pressure is now
half the values of what they were when she arrived in the emergency department 12 hours earlier. And I thought, “What’s going on?” I have to admit I was a little surprised that she was on a normal hospital floor, and that she wasn’t in an intensive care unit already. So I did a little bit of extra detective work and very quickly I realized that these to me very familiar systemic infection treatments still hadn’t been delivered.
So the clock is ticking, it is 10:00 p.m., 13 hours after my mother initially arrived at the hospital and I’m thinking about how I’m going to be the best advocate for my mother that I possibly can. I have to ask that the nurse call my mother’s oncologist and that we request a transfer to the intensive care unit and I’m hopeful, after the oncologist did indeed approve this, that we are going to turn the corner. I just hoped it wasn’t too late.
So I sent my family home. I stayed with my mother and we got transferred to an intensive care unit. It was about midnight, 15 hours on. Over the next hour, it became clear that things still weren’t changing and many of these critical interventions weren’t being implemented. And so I got confused. I was scared. I was tired. I was exhausted. And at one point my mother’s nurse came into the room and she said something to me that I think was a veiled criticism of my mother’s physician but at the time, to be honest with you, I was trying to get my bearings in a new hospital. I was tired and I just was very nervous about what was happening. I said, “Well, why haven’t these treatments been delivered?” And she said, “Well, we do have a treatment protocol for this condition, for systemic infection, but your mother’s oncologist hasn’t ordered it.”
This surprised me for a number of reasons. The first being that usually, in my experience, by the time somebody gets to an intensive care unit and is very sick, you have an intensive care doctor taking care of the patient. Secondly, I just still couldn’t understand why these treatments hadn’t been started. I felt a little bit like I was in the Twilight Zone where realties had been flipped upside down and I couldn’t quite get my bearings. Over the coming hours, I really was, I was torn and I was scared. On one hand, I wondered, what is it going to be like if I advocate for my mother again; am I the pushy family member? And I knew all too well about that dynamic and how that dynamic could play out in the clinical care setting. What would happen if my mom survived this situation, and she needed to restart chemotherapy, and now I’ve criticized her oncologist? What is it like if you’re too demanding and your ICU nurse starts avoiding your mother’s room?
I was psychologically becoming off-balance, and my confidence as a doctor was eroding as I was both trying to marshal resources in the wee hours of an intensive care unit, and at the same time really becoming a caregiver for my own mother. I remember her calling me to the bedside every 15 minutes. She was very uncomfortable in her ICU bed. The lights are on and blazing. You can hear the suction, the white noise of the suction machine in the background, [and her] saying, “I’m really uncomfortable, you have to let me get up,” and me always having to tell her, “We can’t do that, we need to keep you here,” and me kind of on my own trying to reposition her in her bed with the nurse outside the room, who I thought was probably doing more important work at the time.
Ultimately, through the night, we were able to eventually get my mom the care that she needed, and it ended up taking a request from me that we transfer outside of this hospital to another facility. And we didn’t need to transfer her, but it did compel her oncologist to transfer care to a capable intensive care doctor later that morning. By the time that happened, it was about 8:00 on Tuesday morning, so 23 hours after the initial presentation to the emergency
department. And I remember my mom telling me, “This is really, really tough. This is difficult but I want you to push me. I want to live. I want to make it through this.”
She did push over the coming days in the hands of this capable intensive care doctor. She did get the treatments that she needed for systemic infection. But that literature that told us that time is of the essence held true for her as well. And over the coming days, she got sicker. And I remember toward the end, when she was mostly sleeping all the time. She was not awake. And there was this one moment when she just briefly opened her eyes and she just whispered to me, very weakly, she said, “I never got to say goodbye.” And she was dead by the end of the week.
Now I have to ask you, after experiencing a loss like that, this sense of wasted opportunity, what would you do? For us, it seemed like, in our minds, that mainly we had two options, both very blunt instruments, but the only tools that were available to us as family members and as a patient. And that was that we could either sue the hospital, or we could write a letter. And we didn’t want to sue. I really feel like that was something that was too destructive. I’m in a high-risk field myself. I’ve never gone through that process, but I worry about it. We really just wanted to make sure that future patients who came through that hospital door never had the same experience that my mother had, that there was never that lost opportunity. So we constructively put together a letter, and in it we really referred to these national treatment protocols and pointed to specific elements of my mother’s care where this hospital fell short and offered suggestions for improvement.
Now, I have to admit, I felt like I was well positioned to make a change in this hospital. After all, I was a physician who treated this exact complaint and condition in my own practice. I could speak in the technical language that the hospital administrators and the physicians could understand. And I felt like I had insider information here. I had almost a view that even some patients perhaps may not have had, and that was going to set us up for having a good opportunity to improve care. And initially after we sent the letter, holding our breath, there were some hopeful signs. Within a week, the head of the emergency department had called and left me a voice mail saying, “Look, we got your letter. We wanted to let you know that we’ve heard you. We’re going to review the case. Call me if you have any questions at all.” So I did, reaching the physician’s voice mail, and I waited for a response. And I continued to wait. And slowly but surely, weeks passed, months passed. I was initially thinking, “Man, give them time, be patient, don’t be the pushy family member. Let them do their due diligence and review the case.”
But as time went on, and 4 months ultimately went on with absolutely no reply, I felt like they must have tossed this case to the side. That this was either going through a medical legal process or they just weren’t going to respond to me. So 4 months later I called back. And this time my call was returned by a head administrator in the hospital, an intensive care physician himself. And we had a phone call with my wife and me, both physicians, and he said, “We reviewed the case and clearly there wasn’t the degree of urgency that was really required to treat her.” So we kind of hung on to that sanitized admission of error but an admission nonetheless.
Then we really focused on what could change within this hospital based on some of our suggestions in my mother’s case. And some things did change; a small number of things did change. For example, protocols for systemic infection were being implemented in the coming months in the emergency department where my mother received care. Other suggestions and other problems kind of were left hanging. To this hospital we had recommended that they consider a rapid response team. I know many of you probably know what these are, but for those who don’t, these are teams that are called when patients on hospital floors are quickly decompensating, and we’re trying to get a rapid assessment and rapid action to hedge off the
kind of impending disaster. So, physicians and administrators come to the bedside and rapidly assess the patient. It turned out that they had one of these systems within my mother’s hospital, it just wasn’t called. And my sense is that probably this was done, or not done, because the nurse and perhaps even the oncologist didn’t know about how to recognize the systemic infection condition.
Then still other things nothing really happened at all. There was really no system for identifying when a hospital was not enacting protocols for conditions like systemic infection. There was no warning system for that. And additionally, I think one of the biggest things that hit us toward the end of my mother’s care was the lack of an intensive care physician coming in to her care. We had said it might be a good idea, especially for a subset of these patients, if intensive care doctors are brought in immediately when patients come to ICUs, and this physician said, “Look, we’ve tried that, but politically it’s just been impossible to do.” So, concluding the call, there was this one other burning question still kind of in my gut. And that was: why 4 months? What took so long? And the physician just said, “We were really trying to get improvements in care before we called you back and I’m sorry about that.” That was the only apology that we ever heard from the hospital, and that concluded our entire communication with the hospital.
Now, by a show of hands, I’d like to see how many of you personally, or maybe in the care of a loved one, have had a health care experience, whether it’s kind of a small bad outcome or a major bad outcome? So if you turn around and look, I mean this is a majority of people who have hands who are in the room. Now what I would ask you to do is, of those of you who raised your hands, how many of you felt that the health care system, the hospital, or the clinic where you were cared for made a change as a result of your experience? So, look at that missed opportunity there.
Now I’ll just say that this is not an uncommon experience, what we’re seeing here in this room. I’ve had clinicians, nurses in my own practice, readers who’ve read what I’ve written, come to me and say that they’ve had very similar experiences. This experience is exceedingly common. So what’s the way forward for health care? I think there are a couple of things that we can do. The first really goes without saying: that patients and families need to play an active role in the care that they receive. And for us, this was really exemplified by the anguished 4 months of waiting as we were listening and hoping for a hospital response. That time emphasized to us how unimportant we were in the care improvement process. I think if you think about health care as any other service, when you compare it to other service sectors, other industries that make products, and you look at how those industries use user input, or customer input, to design their products and transform their care, health care really underutilizes that voice. It’s not partnering with patients and families in a way that transforms the care that we deliver. And I think that has a real impact on the quality and the costs of the care that we provide.
But I think there’s a way forward that has been outlined already, but I’ll just say a few things from a clinician’s perspective. Where do we go from here? I think there are two things that we can do. The first is that we need to find new ways of listening to patients and families. Hear their experiences, understand their frustrations in the continuity of care and know what their preferences are. The second is that we need to even more actively engage with patients to transform the care that they receive. And I think this can play out at the individual clinical level, at the health care administrative level, and then as I know we’ll talk about later in the conference, at the knowledge generation level, and even as consumers in the marketplace and having transparency in quality and cost data.
I’ll share a few examples here of things that I’ve seen after I’ve had this experience. On the clinical level, there’s a program called Condition H at the University of Pittsburgh. This is a program where the hospital has had a rapid response team, one of these teams that bring clinicians to the bedside of a decompensating patient. But they’ve actually now allowed family members to kind of pull the emergency lever and enact that system. And I think if we had had that in my mother’s hospital that could have been one way that there would have been a difference in her outcome, I can’t say for certain. But it certainly would have been beneficial to us.
But I would emphasize that you don’t need to be a doctor tracking care and knowing the intricacies of clinical care in order to play a role here that’s valuable to the health care system. Especially in our era of contracting residency hours, increasing salaried physicians and individuals of my generation, who are prioritizing quality of life more than in the past. As we transition more to shift-based care within health care, there are going to be times where the family member is the only individual who knows what that patient looked like 12 hours ago on that hospital floor. So those family members really provide us with incredibly important information, and in the era of team-based care, we need to have patients and families included.
I think another example would be sharing medical notes. So clinicians’ medical notes traditionally have not been available to patients, and now through electronic medical records, we’re seeing that patients can get access to their notes. And there was an Annals of Internal Medicine piece within the last 6 months that looked at patients who had access to their notes; 75 or so percent of them said that they felt more in control of their care, and between two-thirds and three-quarters said that they were adhering to their medications more faithfully. So here’s another example, especially when you look at the Health Affairs work that’s been going on in the last couple of months and with their current issue, when you think about the activated patient, when you think about enhancing patient engagement, here’s one of the mechanisms by which this actually happens.
One final clinical level innovation that I think provides us with some hope, one that I’ve seen that I think is a really innovative and interesting way for moving forward, is Anthony Digioia’s in Pennsylvania. He’s a hip and knee orthopedic surgeon. And so he’s basically said this, in the era of ACOs and care redesign and transformation to taking care of patients and including patients in team-based care, we really need to design this system from the inside out again and start with the patient’s perspective. So what he’s done, with patient consent, he has shadowers who follow patients through the entire continuum of care, not just the surgery, from the parking lot to the pre-op appointment, to post-op period, to rehabilitation period, and they found some really interesting opportunities for improvement.
One of the big challenges that I didn’t know about initially until learning about this example was that about 90 percent of patients who undergo hip or knee replacements nationally end up after surgery going to an inpatient rehabilitation facility to continue their rehab. So what Dr. Digioia and his team realized after having patients talk to these shadowers, and the shadowers making their own observations, was that there were two problems that they identified in their clinic. The first is that patients really weren’t prepped for how to think about and what to do to manage their postoperative pain well. And that wasn’t communicated in preoperative appointments. Additionally, they noticed that patients had a lot of pain after the postoperative period. So they went to the anesthesia literature and collected best practices, optimized pain control. They had numbers that 99 percent of patients on post-op day one said that pain was not a problem keeping them away from rehabilitation time, and they decreased the percentage of
patients going to inpatient rehab to 30 percent, down from the 90 percent national average. So these are real opportunities. You think about the cost implications of something like that, and the quality implications of why patients are needlessly suffering from pain after a surgical procedure. You see how some of these methods can start transforming care.
I think the other major area that I would just highlight briefly is on the administrative side. One of the things I always wonder about with us is if we had sat on my mother’s hospital’s intensive care unit quality improvement committee, and we shared her story and we pointed out how difficult it was and how detrimental it was for her not to have a critical care doctor taking care of her in those early hours, would that have been more powerful than a letter or a lawsuit? Maybe. This is I think a really important way that patients also can engage in health care. In my state, Massachusetts, we now have patient and advisory councils that are mandated by the state to be present in every hospital. And I think the best way that these processes play out is that you have these expert patients who’ve had good or bad experiences within the hospital. But they are able to contextualize their experience into a larger picture, really constructively sharing how they think the hospital can tackle some of its most vexing problems. And you get this new collaboration and information stream that you never ever had before.
In one of the most profound examples that I read about where a patient and family advisory council played an important role, was one hospital that bravely wrote about this experience where their patient and family advisory council told them, “We have in your clinic, in your obstetrics clinic, pregnant women with healthy pregnancies that are expected to be carried to term, sitting adjacent to women who are pregnant but where there was fetal demise or severe genetic anomalies, and where it was going to become clear that they were not going to be able to carry the pregnancy.” So, you had this profoundly inhumane juxtaposition of people who were living a joyous part of their life and people who were suffering through a loss. And you hear that story and I think the first reaction that we all have is, how could they have done this? What in the world would’ve made a clinic set up a waiting room like this? But I think the answer is probably this. Both of those groups of patients are seen by the same clinicians. They are seen in the same clinic rooms. And a lot of the same equipment is used and utilized for both patients. So this was the care process that started from the clinician and the facility and built out, as opposed to originating from the patient experience through the continuum of care and then very early realizing something is wrong here.
So as we move forward, I think examples of partnerships like this give me hope. I think there’s promise there. And the challenge now is to expand the breadth of these interventions and to roll them out, to scale up these interventions. And my hope is that many of you in this room will be building the tools and the new sets of approaches that enable us to do this. This experience for me has really opened up my eyes to the importance of patient- and family-centered care, so I’m sitting on patient and family advisory councils now and thinking about new opportunities for partnership and collaboration in care. And I think the need for those of us working in health care to incorporate patient and family voices is really urgent.
Today and tomorrow across the nation, there are patients whose survival will really depend on this. Their lives, like my mother’s, and they have a photo of her here, really hang in the balance. With these lives on the clock and as hours and days tick by, we need to do everything within our power, everything possible to listen to family voices and partner with patients to avoid repeating these terrible mistakes and improve health care. Thank you.
MS. BECHTEL: Thank you so much, Jon. That was incredibly powerful and moving. And I think you could not have possibly done a better job of sharing with us the reasons that we look to
patients and family members as partners in this endeavor. So we do have a few minutes for questions, if you all want to approach the microphones. We’ll start with you, and please introduce yourself as well.
DR. DARER: John Darer from Geisinger Health System, and I’m the co-PI on the Open Notes Initiative that you mentioned with folks from Beth Israel in Seattle and Harborview. What an incredible talk and thanks so much for sharing that.
In the process of the Open Notes Initiative, about 20 percent of folks shared notes with their family members, and we are now beginning to think through our next iteration of the investigation, and caregivers is a big focus. I’m curious if you can comment upon what you think it would mean to families. We know that patients really, really value the information, but we are still in that process of really understanding what caregivers need in terms of information and how that’s going to be transacted. I’d love to get your thoughts.
DR. WELCH: Thank you, it’s a great question. I think that family members are oftentimes, even when we’re thinking about patient-centered care, still a missing piece of the puzzle in engaging patients and families in care. I think even in my own clinical practice, one of the mistakes that I see some of my own colleagues make or my residents make is that they may be great with the patient, but they kind of ignore the family member who is sitting in the room. And I think we forget that more than half the time probably, it’s the family member, it’s the concerned wife, who is motivating the patient to seek care. And they really, in addition to other members of the community, are going to be key tools for us to gather more information about how things are going for a patient. And I think we need to make sure that our interventions are the appropriate ones. I think there are fantastic opportunities there and I think people will be really grateful to have that information accessible to them.
MR. DEBRONKART: Hi, Dave DeBronkart. I have not a question but comments.
Jonathan, your story in Health Affairs, unbelievable. A few things I want to toss in. When my mom had her hip replaced a year and a half ago, at her transfer to rehab, because they didn’t have electronic medical record transfer so stuff had to get printed out and typed back in, they were not interested in proofreading, so her hyperthyroid showed up as hypo in the new system—potential disaster. My two what I call “alpha sisters” were on top of everything, and the patient and family engagement there saved the day. It’s really clear that that’s one instance of patient and family engagement taking a burden off of the providers who are not supported by good systems, good technology, getting patients involved in teams and change teams.
I’m going to speak in a couple of months at Kingston General Hospital in Ontario. They have gotten it into their practice now to engage and involve patients on every team whether or not it apparently is something that directly affects the patients. On hand hygiene, they are hallway observers, the so-called Purell Nazis. They notice 30 to 60 percent compliance on the part of the physician.
By the way, why, with patients, do we call it compliance, and with clinicians we call it quality of care? I’ve got a point here. We have a cultural disconnect, and I’m not complaining here. You know, in my talk I didn’t say this place sucks or anything like that, I said, look, let patients help.
So at the Kingston General Hospital, that hand hygiene team, one of the patients said, “You know what we ought to do: take each unit’s numbers and post it on the door going into the unit.” Shocking idea. Within 6 months the hospital is up to 92 percent hand-washing compliance. What is keeping any of us from doing this everywhere else?
One final thing, and Christine, you really should talk about your definition of patient-centered, but there was a Dutch in vitro fertilization clinic that gave their patient community a wiki and 6 months to talk, and said, “What do you guys want?” And the third thing on the list, after “We want more attempts at fertilization,” the third thing was “We want empathy from our doctors, not just more information.” The fourth thing was separate waiting rooms for families who’ve conceived.
I was saved by great medicine, and I think Govandi blames penicillin, right? He wrote an article where he said this medical miracle of penicillin made us look to the lab for all value in health care. But I think what I’m hearing here is that there’s great value to be had also from listening to patients, so thanks.
MS. BECHTEL: Thank you, Dave. I just want to say one thing, which is we made a concerted effort as a Planning Committee to reach out to patient and family representatives, individual patients, family members, and consumer organizations. Dave is one of those. We’re grateful for you being here today and we do have a number of you. I just wanted to give a shout out to the patients and families and consumer groups here today and encourage you to do as Dave has done and speak up as the day goes forward. Do you want to comment?
DR. WELCH: Thanks for your comments. Again, I think your important example really underlines first of all how common this kind of experience is. One of the things I think I’ve noticed about these important mechanisms of feedback is that we probably really need to look to other sectors or their wikis or other mechanisms for thinking about how other sectors develop products and services with the user in mind. And I think that’s a great example.
The other thing I would say is, when you went through the list of priorities amongst patients at IVF clinics, is that it actually highlights a little bit of a danger zone, at least on the clinician’s side; for the most part I really do think that physicians and nurses try to have their patient’s best interests in mind. There’s a professional ethic there that for the most part we all try to follow. The problem is that you get into this conceptual shortcoming when you think that you can intuit actually what a patient needs. And when you start finding new mechanisms for listening to patients, you get really surprised about some of the shortcomings in your care. So, we really need to develop those more, and when I think about physician and health care provider engagement, that’s a real intellectual challenge that we have to confront in our field.
MS. DAY: I just wanted to thank you, Dr. Welch, for sharing your story. It was very compelling and I have a story regarding my father that’s eerily similar to yours.
I’m from Bangor, Maine. I’m an independent patient safety activist and advocate. I’m a liberated, retired RN, so now I can say whatever I want. I’ve been a recent patient and I’m the survivor of hospital-acquired MRSA victim. The difference between your mother’s case and mine is that I was sitting in the room when he went into sepsis, septic shock under the nurse’s nose. She was in the room doing electronic records. My mother and I returned from lunch and I noticed that he was gray, ashen-colored, and somnolent. And she said, “Oh, he’s just worn out, he’s worn out because he just had a lung scan, he just got back from the lung scan.” And I said, “This is different.” “Oh, I think he’s fine.” So I raised a ruckus.
You asked what we can do. In the words of Lisa McGifford from Consumer’s Union, you raise a ruckus. If you don’t have a cord to pull to get the team there to take care of your loved one, you raise a ruckus. You can do that in a quiet, nice way or you can yell if you have to. But that’s your loved one, and that’s their life that’s in the hospital’s hands, and if you know the difference between them being okay and them not being okay, and who knows better than
family, seriously, then you speak out and you don’t take no for an answer. So, I didn’t ask a question, I answered your question; I think you said, “What do you do?”
Actually the other thing that they did for my father that they did differently is move him to ICU, but he had MRSA and they picked up all of his things from the windowsill, the other bed in the room, took everything down the hall to the ICU, rolled a clean bed into the room without cleaning it. So, I saw it from both a nurse and the patient perspective.
You asked if they had made change, and yes, they did. I wrote letters. I went to my state legislature, I won’t go into all the things that I did but anyhow, they made the change of isolating all patients. And they didn’t have any nosocomial MRSA the next year. My father was the third of three that year.
So, thank you so much for your work and your story and sharing your story. It’s important that we all do that. Thank you.
DR. WELCH: Thank you. That’s a fantastic accomplishment. I think hospitals need to find ways to culturally transform so that patients can feel comfortable speaking up, and there’s still a real deep regret that I have for not really getting much more outspoken and aggressive in the wee hours of the morning.
Having said that, I’ve also learned now though that if you have a safety system within a hospital that relies on patients raising a ruckus in order to get the care that you need, we’re probably in trouble. So, I think we’re always going to need both sides of these mechanisms, but especially with sepsis care, where we are still in that 10- to 15-year window where knowledge is being brought out into the public, into the clinical space. I think we need to keep both of those things in mind, and patients being able to speak up is incredibly important.
MS. LIND: My name is Cristin Lind, and first I just want to say thank you so much for sharing your story. It’s really powerful. And Christine, I’m kind of the classic mom turned advocate. My son is 10 years old. He has a genetic syndrome called Coffin-Lowry syndrome. Not that rare, not that common.
But I’m just here to share a really short example of something that’s happened recently that I think speaks to one of the hugest barriers that we have when we talk about this subject, which is culture. So, 2 weeks ago I was reading a Swedish medical publication. The title of the publication roughly translates into “Dare to Let Patients Partner.” And I was so excited to hear about what the Center for Person-Centered Care at the University of Gothenburg was doing, the fact that they even acknowledged that it was person-centered care and not patient-centered care, I thought was significant. I made a comment to the article and talked about some of the work that I’m doing here in the United States and supporting what conclusions they had come to. So, I support family and patient partners who are working in quality improvement teams. You just wrote a great article, Christine, which I keep quoting left and right, thank you so much. And I was really surprised because, about 24 hours later, I noticed that my comment was gone. And I was a little bit nervous because I wrote my comment in English, even though I do speak Swedish, my husband is from Sweden. And I just dropped them a note and said, “Did I do something wrong? I want to be able to make sure that I can stay part of this conversation.”
Well, I got a reply about a day later saying that your comment was removed because you’re not a professional health care worker. So it’s a very short story, and conversation has continued with this publication. My comment has been restored, but I think that, nevertheless, their stance is that patients have a lot of space that they get to take up in the media, and there need to be places where we protect professional voices and allow them to be able to speak frankly and openly with each other.
So, I lend this little anecdote as a litmus test or a barometer of what we are facing as we talk about partnering with patients, because my new mantra is “culture eats strategy for lunch.” It just is really going to come down to that often. So, I just share that and I want to say thank you so much for making sure that patients have such a strong voice here. It would have been really easy to do something else, so, thank you so much.
MS. BECHTEL: Thank you very much. We continue with the “us versus them,” and I don’t think health care providers want to be in that position as much as patients don’t as well. So, we’re going to take one comment from Paul Grundy in the room, because we do want to get into our next session, and if there’s anything from the Web, maybe you all can bring that up as well. So, Paul, please go ahead.
DR. GRUNDY: Thank you, Jonathan. I have a couple of questions. The first question I have is: What was the total cost of that experience for your mom in the hospital, do you have any idea?
DR. WELCH: Great question, and I am still working to dig through her charges.
DR. GRUNDY: I think the Time magazine article is worth reading for all of us.
And I guess the second thought I had is that you and I are physicians that grew up in the world of Flexner, in which we’re master builders. I mean, we look at the world not in a view of data or accountability toward data, but in a world where we’re master builders. Where you wouldn’t have done that in that system if it was somebody who was constructing your house and you saw an error occurring, because there would have been a plan, an accountability to that plan that would have been happening in the system.
And I guess the fact now in health care is we’re moving away from Flexner toward a model of care in which there is going to be data and there’s going to be accountability to data, and I think we need to think about that in reference to how the consumer engages with those data. Clearly, the experience in places like Denmark and others is to make sure that those data are available to the patient, to the consumer, to the person as a clear element of that. The system that you engaged and encountered with your mom is a system that’s so flawed and so broken, it just has to be frustrating for you. You express that frustration so well by not knowing quite what to do at any stretch of the imagination, because you know down the road there are going to be blocks put in place for everything you really try to do.
But, that’s changing, because for the first time in history, we are going to have the data to begin to hold a system accountable, and a place where those data flow in a medical home where accountability begins to occur. My question for this group and for us is, How do we really guarantee that the consumer, that the patient, is part of that? Because that is going to be absolutely essential. Thank you.
DR. WELCH: It is a great point. I, too, am hopeful as slowly but surely we move to these systems where we are holding our health care system accountable for results. And I think the hopeful thing is that we’re building an evidence base that shows that these tools—patient activation, patient engagement, even from a very utilitarian standpoint, to say nothing of the intrinsic good of centering on patients—that that improves results. And if people and the citizens are paying attention to results, and hospitals and clinics are getting paid for results, I think this will become part of a larger package that transforms care.
MS. BECHTEL: Thank you again, Jon, for your terrific story, and also for giving us some insight into a productive way forward. I think my summary of that session would be defined as: it’s all about culture, stupid. And I think Jon’s story does a terrific job of illustrating that while we keep saying, well, gee, if patients would just get active in their care we would really have a
better system. But when they get active, what we heard from the audience, what we heard in Jon’s story, is that we tell them no, they can’t be part of the care team. No, they can’t have their notes. No, they have to get limited to visiting hours. No, you can’t be part of designing what this primary care practice looks like, we’re going to design it for you and that’s the system we have today.
So I’ll say two things as we jump into the next session. One is I’m thrilled with the level of audience engagement and the fact that you guys are getting up not just to ask a question, but to offer your viewpoints and your experiences and I want that to continue. And I know we’re running a little late, which is something that I raise only because I don’t want to rein in the audience, but I do want to get a heads-up to the speakers that we want to leave time for exactly this interaction.
The second thing that I would observe is that the central theme of this discussion so far has been about partnerships. So, as we go forward and we hear from some absolutely phenomenal experts in the field and people with really innovative programs to build on, and that’s our goal, to figure out how to build on what has been successful so far, look for that theme of partnership and where it’s happening, and if you don’t see it, we should ask about it. And we should find the ways; not everybody has done it and they can still succeed, so we need to find the ways to rein that partnership into even the most successful strategies, so that they can be accelerated and even more impactful.
So with that, I’m going to turn it over to Lyn Paget, who is going to moderate our next session. We’re going to spend the rest of the day focusing on shared decision making and Lyn is one of the world’s foremost experts, and she is the managing partner at Health Policy Partners. Thank you.
PATIENT-CLINICIAN COMMUNICATION AND THE TOOLS FOR CHANGE
Lyn Paget (Moderator)
MS. PAGET: I would like to ask the panel members for the next session if they would please come up and take their seats.
Thank you very much, Christine, and thank you for the opportunity to moderate this afternoon’s session. I have to say that, as a resident of Boston, I hope that if I or a family member ends up in the emergency room that we will be there during Jonathan’s shift.
But all kidding aside, I think that it’s clear to say that, for both Dominick and Jonathan, their personal experience has informed and created a whole different way that they approach their research and their clinical care. And I think it is part of our job to decide the best way to systematically infuse that across all clinicians and across all care settings in this country, and that’s no small task.
Before I introduce our speakers today, let me just review a little bit of what we hope to accomplish. This session is titled “Patient-Clinician Communication and Tools for Change,” and I want to underscore “change.” We need change. Why we need to change is perhaps one of the most disappointing stories of American health care. But here we are today, poised to bring us to a new place where we can be proud to be part of the renewed system that we know will allow clinicians to be our guiding experts, and where we and those we care for will be treated with dignity and respect always.
For this workshop, we are framing these presentations and those to come later this afternoon, by thinking about four necessary steps to change. And I challenge us as we listen to these sessions and these presentations to think about what it is that we’re learning, because this is really a hearts and minds issue, what it is that we’re learning that we can bring back to our individual spheres of influence. What is the action that we can take? How can we infuse the knowledge from today and bring it forward?
So, these four steps really guided the development of this workshop, and Christine mentioned one, which is pathways. How do we create that road or that avenue for us to open up opportunities for the kinds of changes that we know that are needed, particularly in the culture of care? Infrastructure is number two. That has to do with systems design. We’ve heard a little bit about that this morning. But we know for sure that in order to embed systematic and sustainable change, we really need to design things differently, and as Jonathan pointed out so eloquently, from the inside out. Making sure that the patient and family is in that inside. The third is culture. These are customs of care that are deeply embedded in our system of health care. These are not easy changes. But these are changes that are going to be required in order for us to see the kind of successful results that we want. And last is competency. And that’s really an important word in my mind—competency on both sides of the coin. We’re talking about skill sets. We’re talking about competence. We’re talking about competency so that communication happens both ways, and it’s respectful, coming from both sides. That doesn’t happen quite much in our system today.
As I was looking at the participant list last night, while I was watching the Academy Awards, it occurred to me that, for most of you, this is a workshop that’s a distinct recognition of the professional commitment that you have made to make health care a better place for all of us. Because, as Dominick so eloquently pointed out, we are all patients. We are all people but we are all patients. So, we’re really pleased today to have these dedicated professionals here with us to start this session. We have three presentations that are going to take us from the science that underscores the problem to innovative concepts for actually making infrastructural change to competencies. What does it need to look like for clinicians to be better at communicating and recognizing the value of patient and family contribution?
So, let me introduce our panel. Each of them has roughly 10 minutes to speak, and then after all the presentations, we’re going to open it up for some conversation, questions, and dialogue. We’re going to begin today with Gary Langer. Gary is the founder and president of Langer Research Associates. He is an internationally recognized public opinion researcher with expertise in analysis of political, policy, economic and social attitudes, questionnaire design and data interpretation, survey methodology, and survey management.
Following Gary, we have Sherrie Kaplan, who is the Assistant Vice Chancellor for Healthcare Measurement and Evaluation, as well as Professor of Medicine at University of California, Irvine, School of Medicine, and Executive Co-Director of the Center for Health Policy Research at University of California, Irvine. She is a leading social scientist in medicine and has pioneered a number of areas of research including demonstrating that patient involvement clearly leads to better outcomes.
And our last speaker today is Eric Holmboe. He is from the American Board of Internal Medicine. He is a Board Certified Internist. He is the Senior VP of the American Board of Internal Medicine and the ABIM Foundation. His research interests include interventions to improve quality of care and methods in the evaluation of clinical competence.
So, on behalf of the Planning Committee, I’d like to thank all three of you for being with us today and I’m going to turn it over to Gary. Thank you.
The Key Elements of Information, Connectedness, and Continuity for Patient Engagement in Health Care Decisions
Mr. Gary Langer
MR. LANGER: Thanks, Lyn. Thanks for having me. I’m grateful to be here. I’d like to say that I think Jonathan Welch’s presentation is a call for patient involvement through the prism of his own painful personal experience, and the comments we heard after segue nicely into the presentation I want to make. I come to you not as a medical professional, but as a survey researcher. Public opinion research is my field. And the purpose of the research we do is to bring the voice of the public, in this case, the voice of patients, to the table—exactly the goal that we’re hearing discussed so far this morning.
So, I am grateful for the opportunity to bring these voices to you in the quantified form that we do. I am grateful also not only to the IOM, but particularly to the Blue Shield of California Foundation, which has sponsored and partnered in this research with my group over the last few years, conducting high-quality, rigorous public opinion surveys of low-income Californians to understand better their experience of care and the motivators of their empowerment and engagement in the health care system. I’m going to talk to you a little about this.
The research program we’ve done with the Foundation is based on statewide surveys, telephone surveys, landline and cell phone, of a random sample of low-income Californians; those at less than 200 percent of the federal poverty level, a safety-net population, if you will. The notion is that the ACA is going to introduce competitive forces within the provision of care to this population. Providers need to respond.
So, in spring 2011 we did a baseline survey of the experiences and preferences of this population to learn about the drivers of patient loyalty and satisfaction. Two drilldowns emerged from that, two facets of that first line of research that we thought were interesting and needed further exploration. One is the expressed desire among these patients for a regular personal doctor. A primary interest of theirs was that they wanted to have one of those. And the second was the substantial, and perhaps surprising, resistance to the concept of shared decision making as we tested it.
So, we conducted an additional survey in the spring of 2012, a year ago, to explore these and other potential drivers of patient empowerment and engagement. Connectedness and continuity is the concept that we came up with that really seems to drive the empowerment and engagement of patients, particularly in terms of relationships. When you ask patients what they want in their health care, they say they want a regular personal doctor. What came to us, as we explored this theme and additional questioning, is that patients are using this concept of Dr. Welby to describe really the most familiar route to their real aim: Connectedness, a sense that someone where you go for care gets you, knows you pretty well; and continuity, the assurance that you’ll be seeing the same caregiver over time.
Connectedness and continuity, as I will present this morning, drive patient engagement and patient empowerment, in a powerful way, above and beyond and apart from this simple presence of Dr. Welby. Indeed, wanting but lacking a personal doctor independently negatively predicts satisfaction with care and patient loyalty. But when connectedness and continuity as I’ve described them are present, are added to the equation, they independently positively predict satisfaction, empowerment, engagement alike, and having a regular personal doctor does not. It falls out of the equation.
Then we looked at shared decision making, and we were surprised by this result. Among this population, about 6 in 10 said they would like an equal say in decision making with their care provider. That is, frankly, fewer than you might expect; coming from the prism of an educated, involved base, you would expect an overwhelming majority, 8 in 10 or more perhaps, at least I did. But a fairly substantial minority, 4 in 10, said no, they prefer to leave decision making up to the care provider.
Now, what was that about? Well, we ask d a few follow-up questions; one was, “What if the doctor chose options for you and explained them to you in information that you can clearly understand, would you then like to have an equal say in decision making?” And you can see what happens (see Figures 2-1 and 2-2). The role of information in decision making is a powerful factor in sign-up among patients to this concept.
And indeed it fundamentally levels the playing field. The blue lines show you the initial interest in shared decision making, and we can see some significant socioeconomic gaps. Willingness to participate in shared decision making is far lower among less empowered populations, less than high school compared to college grad, look at those blue lines, whites versus Latinos, non–English speakers versus English speakers, enormous gaps. Now when you provide information, those gaps largely disappear. That information levels the playing field in terms of willingness to participate in shared decision making; again, a powerful example of the important role of information and communication.
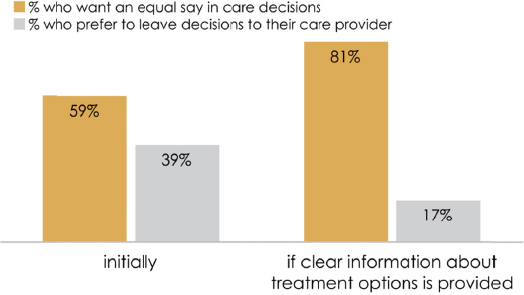
FIGURE 2-1 Preference for shared decisions with or without clear information on
treatment options.
SOURCE: Reprinted courtesy of Blue Shield of California Foundation.
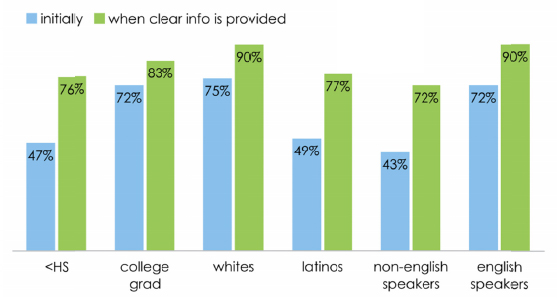
FIGURE 2-2 Preference for shared decisions with or without clear information on
treatment options, by demographic.
SOURCE: Reprinted courtesy of Blue Shield of California Foundation.
We take this information through a series of regression analyses; build a mediation model that predicts a path to patient-centered care through a model of empowerment and engagement. This is what it looks like (see Figure 2-3). Connectedness and continuity as I’ve described them to you, the sense that someone there knows you and that you’ll see the same caregiver over time, independently of demographic variables—having a regular personal doctor, health status, a place of care, insurance status and the rest—independently predict empowerment. “Empowerment” meaning feeling informed about your health, comfort in asking questions, comprehension, understanding the answers, and confidence in your ability to make health care decisions. Those empowerment measures in turn independently predict engagement, the sense that you’re taking an active role in your own care, really the goal fundamentally of patient-centered care as we’re discussing it. I’ll point out that information, the first empowerment measure, is a particularly strong one, the standout, because it also independently predicts the other empowerment measures we talk about here.
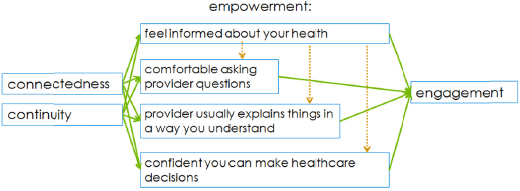
FIGURE 2-3 Schematic of The Path to Patient-Centered Care: A Model of
Empowerment and Engagement.
SOURCE: Reprinted courtesy of Blue Shield of California Foundation.
I’m going to break these out a little bit to show you the impacts, the effects of these variables. It’s really quite impressive I think. First is connectedness, predicting feeling informed about your health. Among low-income Californians who feel a personal connection at their place of care, 64 percent feel very informed about their health. Among those who lack a personal connection, it’s 37 percent, an enormous impact or effect of that sense of connectedness. In terms of continuity as well, similarly, if you usually see the same provider, 56 percent feel very informed about their health. If you don’t usually see the same provider, that goes down to 35 percent—again, a dramatic impact. Also consider connectedness in terms of predicting our other empowerment indicators of comfort, comprehension, and confidence: if you’re feeling connected, feeling someone at your place of care knows you well, you’re vastly more likely to feel comfortable asking questions, to say you understand the provider’s instructions, and somewhat more likely to be confident in your decision-making ability.
BOX 2-1
Rx for Patient Engagement
- Connectedness and continuity pave the path to patient empowerment and engagement.
- Information is essential:
- It predicts self-efficacy even when connectedness and continuity are held constant, and
- It does so more strongly than education, income, gender, race, and other demographic variables.
SOURCE: Reprinted with permission from Langer Research Associates.
Continuity has similar impacts. Among those who always see the same provider, you see a lot more comfort in asking questions, a lot more comprehension of answers, and somewhat more confidence in decision making as well. These are fairly powerful impacts.
Then we talk about information and its predictive capability in comfort, comprehension, and confidence. And there it is similar as well. Among those who feel very informed about their health, comfort asking questions of their provider, comprehension particularly of the provider’s answers, and confidence in decision making are all dramatically higher.
Finally is the sense to which each of these predicts the outcome, the Holy Grail of patient engagement, self-efficacy in their care. These are the percentages of patients who report having a great deal of say in their own care. Those who feel very informed are more than twice as likely to say they are engaged in their care. Those who feel very comfortable asking questions, again, are very substantially more likely to be engaged in their care; those who understand the provider’s answers; those who are confident in their decisions in each case; in each of these there’s a strong influence on patient engagement.
One route to patient engagement beyond the regular personal doctor we discussed earlier is team-based care. And I want to describe to you briefly its impact and some patient sentiment that we’ve measured in this population. Among patients who have team-based care, the satisfaction with their care is significantly higher, and their sense of information, and we’ve seen its importance, is significantly higher. Understanding or comprehension of the provider’s instructions is higher as well. Similarly, people who have team-based care are more likely to feel
there is someone at their place of care who knows them well, connectedness. I think these last three bars show it perhaps best (see Figure 2-4). There are both positives and negatives from this stack. First, among private doctor’s office patients, 51 percent say there is someone at their place of care who knows them well. On one hand, that’s fairly devastating, only 51 percent of private doctor’s office patients feel someone at their place of care knows them well. Clinic patients who are in team-based care, however, match that population in their sense of connectedness. It is clinic patients who don’t have team-based care who fall off the charts in terms of connectedness.
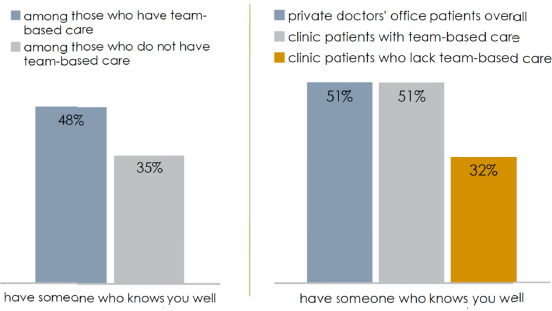
FIGURE 2-4 Patients who feel their clinician knows them well, based on care setting.
SOURCE: Reprinted courtesy of Blue Shield of California Foundation.
So, team-based care at least lifts clinic patients to the level of private doctor’s office patients in the sense of connectedness that patients achieve. It’s helpful in that regard. That’s the positive. The negative is that there is still a lot of room for improvement.
So our prescription for patient engagement then is that connectedness and continuity pave the path to patient empowerment and engagement, and that information is essential. It predicts self-efficacy, even when onnectedness and continuity are held constant. And it does so more strongly than the demographic variables.
Now, I’m going to wrap up, just a last comment and just a word about measurement. In doing this research, we start with a review of the existing literature and I know there are a number of researchers here or those who are involved in publishing on the subject, and as a survey researcher, I wanted to make a couple of quick comments about this. We need to recognize that non-probability samples are not reliably generalizable. Agree/disagree and yes/no questions are inherently biasing. Unlabeled or partially labeled number scales often lack internal validity. Knowledge question are problematic in an opinion survey format.
I’d be happy to discuss these with anyone later but there are many examples in the literature of the use of suboptimal approaches to survey research that I think could and should be addressed as we move down the road of bringing patients’ voices into the discussion. Also it’s worth remembering is that data analysis is very much enriched by rigorous modeling, as I’ve tried to present today.
Thank you very much. I appreciate it.
Planned Patienthood: Setting the Expectation for Shared Decision Making
Dr. Sherrie Kaplan
DR. KAPLAN: Thank you very much. I am going to talk to you about some stuff that we have been doing for quite a long time. In fact, this was sent to me by Alan Kaplan; apparently I gave a very similar talk at AARP in 1991. So, in terms of progress, I cannot promise anything exciting about progress, but at least I’m going to give you a fill-in about where we’re going.
So, patienthood is this notion that we become patients as opposed to staying in that role. We become patients, we leave patienthood, we become patients, we leave patienthood. So, what are we asking patients to do now? Well, we ask them to choose and change health plans, choose and change providers, give “informed consent,” participate in some treatment decisions (although going up that’s rare still), follow through on treatment plans, pay the bill increasingly, and interpret health information, particular performance data.
So, what help do we give people being patients? Well, not very much. I mean, you can see sort of in order the things we do. And we are open enrollment. I don’t know if you all have had this experience but at open enrollment time, I get the data on the health plans options available to me in font the size that takes me a very heavy magnifying glass to read, and physician directories, even these give you increasing information about quality, but they are mostly giving you information you don’t know how to interpret, appointment reminders, et cetera. And we really don’t give them very systematic help in making any of these; systematic is the underscore because we’ve got great examples of each of these individually.
So, currently there’s no systematic training preparation for being a patient in the United States right now. There’s no systematic training. It shouldn’t surprise us then that the average patients ask fewer than four, you could argue five, lexical questions in a 15-minute office visit, including “Can you validate my parking?” and questions like that. And most patients don’t participate effectively in treatment decisions, and although we have really good patient education programs in some areas, those improve knowledge but they tend not to be associated with important health outcomes. I’m going to get in trouble for that later.
But why haven’t we done this yet? Well, there are some prevailing things. One is that patients are too poorly educated. They are not well enough prepared to participate effectively in care. Another one, as we just heard, is that patients don’t want to participate in care. Some people really do want to be passive recipients of their care. If you increase patient participation and care, you’ll lengthen the office visit untenably, and if you encourage patients to participate, they’ll become difficult patients. And patient training, and I will come back to sort of challenging these myths in a second, patient training to participate in care is too new.
So why do it? Well, this is an article that we published about 2 years ago in Medical Care that in fact shows when the physician effect begins to stop and the patient effect takes off, and that’s right about where exactly the targets for physician control are, this is blood glucose control, hemoglobin A1C values, and this is just about where the definition of “out of control” begins. So, if you want to reduce patients’ values on this down to the target, you have to get patients involved. That patient effect takes off, at the definition of out of control. And the same thing is true, although it’s a little harder to see for LDL.
So, to address the question of whether people should be passive about their care, we actually have some empirical data based on a bunch of questionnaire data that we’ve accumulated over the years about passivity. These are passive patients. They have a high provider dependence
score, and you can see that 40 percent of passive patients will have an important decline in their functional status of 10 points or more in a 1-year period.
So, maybe passivity is hazardous to your health. Greater passivity, and this is just recently where this is a manuscript under revision right now, leads to—and poorer confidence—leads to poor glycemic control, independent of race and ethnicity, and you can’t see this slide, but control for the kitchen sink in terms of access to care, process of care, interpersonal care, and disease burden, management mastery is still a predictor of glycemic control.
So, what’s the evidence for shared or participatory decision making? Participatory decision-making style, we’ve shown and I gave the conference organizers a big long bibliography, is positively associated with outcomes, health outcomes, patient retention, and patient experience ratings, and it occurs less frequently; that is, doctors don’t involve patients in care without intervention. Now, some patients participate more effectively in treatment decisions than others. Younger people do. Women do, and I have some data to follow up on that. And obviously people with more active orientation to their health care do. In terms of gender in patienthood, the most common (this is from audiotape data) number of questions asked by men in a 15-minute office visit is zero. The mean number of questions asked by women is six. Women respond more, in addition, when you try to involve them in care and you develop interventions to involve them in care. Women respond, men tend not to, and I’ll come back to the need for maybe remedial gender work on participatory decision-making style in a second.
So, training people to involve care, is it new? Well, my husband, when he should have been paying attention to something else in synagogue, actually came upon this algorithm in Leviticus (see Figure 2-5). So, the idea here, and the slides are obviously available, all of this information leads you to, you can actually graph this information into a treatment algorithm. It turns out that with certain kinds of symptoms, that is what you diagnose, leprosy, and then you observe them and if not, you quarantine them, and if the lesion becomes stable, you quarantine them, et cetera, et cetera. So we’ve been about disclosing information to patients in treatment algorithms for a long time.
So building, not on that evidence exactly but building on that notion, we actually developed what we called Coached Care. And using personalized information in the patient’s medical record in an algorithm that maps treatment decisions, we actually met with patients before an office visit, coached them to be more effective during the visit, and followed them up with phone calls. And more recently, we’ve actually implemented that with volunteers from community-based clinics and matched for, not gender because we couldn’t find enough male coaches that were really good at it, but matched for race and ethnicity. And we trained coaches to support people during those visits, and actually found that compared to controls, we have very good documented evidence of reduction in biomarkers and also reduction in symptoms and improvements in function.
This is the most recent data we have. This is also under revision. The intervention actually decreases, still decreases, hemoglobin A1C values in poor minority communities after 1-year follow-up. So, in summary, with coaching, patients can participate effectively in treatment decisions that improve patients’ outcomes, and contrary to expectation, it really doesn’t lengthen office visits.
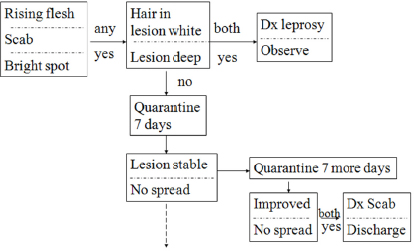
FIGURE 2-5 An early algorithim for treatment.
SOURCE: Reprinted with permission from Sherrie Kaplan.
So what should we be doing with patients? Well, building on that and all the expertise and experience in this committee and this enterprise here in our conference, we should also be involving patients in care in a much more systematic way. The details of that are in the first slide. Plus, we should also be teaching patients how to obtain, protect, and use personal health information, how to understand and navigate the health care system effectively and efficiently and, by the way, Choosing Wisely and other initiatives like that are going to make this even more important: how to teach physicians how to talk patients out of things. Make sure they understand things don’t need to be done. How to protect personal safety in hospitals, and I think Jonathan’s example was excellent, but we have a far way to go. Even things like if you see the rails are down on your bed, either you or your family member needs to pull them up. I mean basic stuff to keep people safe in hospitals.
And finally, where do we go next? Well, in the very voluminous briefing document that you have, there’s a piece by Shelly and myself that describes the notion of centers for planned patienthood. We really need to take this on as a national policy. Right now, after 22 years of being at this, apparently longer than that, it is time to make that a national initiative, we need to teach people about patienthood. We may need to begin in childhood. Some evidence suggests that we learn these notions of patienthood very early on. We can use technology to advance the whole principle. We don’t need to have actual centers, they could be virtual centers. And we need to target specific groups of patients that may be more in need of additional help or basic remedial help to participate effectively, like men, the elderly, and people with an additional disease burden that we call the “potential for benefit.” Maybe we should be offering degrees in effective patienthood, so if you get a degree rom our University of Planned Patienthood, you may get some benefits on your premiums. You may get additional things that were down to you, because you’ve actually done the work of trying to be more involved in your care. Thank you very much.
Clinician Competencies for Effective Shared Decision Making
Dr. Eric Holmboe
DR. HOLMBOE: Thank you very much for having me. I’m really excited to be able to participate here today. I’m actually feeling a little bit overwhelmed. I feel like a bit of a fraud because I’m looking at all the names on the lists and all the experts here. I’m not one of them.
But I’m going to hopefully share with you the flipside of what Sherrie just talked about with regard to the clinician competencies that are needed. And as Sherrie alluded to, there’s a boatload of evidence that this stuff actually works, and we just haven’t spent enough time really helping physicians, nurses, whatever, clinicians over their career, to acquire these skills, and they are very useful skills.
One other thing I’ll say before I start is I think one of the things that’s very important and again, in the context of Sherrie’s talk, I feel this is really an obligation to make sure we help patients acquire the competencies they need to most effectively help themselves; and it’s not just the patients, it’s often families. I very much resonate with Jonathan’s story. I literally have three parents now who are engaged in the health care system in various ways, some effectively, some quite dysfunctionally, and it’s really interesting to experience that. A lot of it has to do with just their understanding of even what’s happening to them. And I’m fortunate, being in the health care world, I’m a filter. I’m an interpreter to help them through that and balancing that, but it would be pretty frightening to me to think about what if I wasn’t there, and people who don’t have that sort of resource to help them navigate at times the very overwhelming system.
So, let me just give you a quick definition of competency. It’s a term you heard from Lyn, and I totally agree, this is an important concept. And sometimes it gets overused and people treat it like it’s the Holy Grail and there’s a lot of cynicism around it. But I think it’s a really important concept, and it’s really taken hold in medical education, but I also think it has real value for continuous professional development. And this is a definition that was developed by a group of international folks. This is an international phenomenon. It’s not just a U.S. sort of thing, but there’s literally hundreds of countries that are embarking on trying to change the way they train their health care providers. And it’s really focused on outcomes and it uses an organizing framework of competencies and I think that’s really important. The outcomes are really what matter now and it’s not like, well, this is what we think is important. These are the outcomes that matter and I’ll get more to that in a minute.
But competency has become a framework to help us make sense and help our clinicians be better. And I really love this slide. If this is the one thing you remember from my 10-minute talk, I would have you hang onto this from Julio Frenk and colleagues, from a Lancet article a couple years ago. What they did is, they took a look, and you heard Flexner alluded to earlier from Paul, but this is what we used to do. We had a curriculum developed by a bunch of experts sitting around a table and then we would design tests. And that worked okay for 100 years but it’s not going to work moving forward, and what Frenk and colleagues really called out is that when you design any sort of educational system across the continuum, you start with what the health needs of the population are, that’s what matters. And you talk about what the health system needs are. That’s where you ground [the training], and then from there you design the competency outcomes of interest, and then and only then do you really get into curriculum and assessment. If you don’t meet the population needs, and we’ve seen this disconnect, then it’s not going to work, and you’re going to get the system that we currently have.
So, what’s competency, and this is just again from that international group, an easy way to remember. It’s “an observable ability of a health professional, integrating multiple components such as knowledge, skills, values, and attitudes.” I want to highlight that attitudes matter. Attitudes are really important. We have already heard about how culture eats strategy every day for lunch, dinner, snack, breakfast, that’s true. And attitudes are an incredibly important part of communication skills and patient engagement.
So, what are some of physician competencies that have been talked about?—and again these apply, I’m using a physician lens because of where I work. But these are the sort of things that are evidence-based, and I’m going to call out just a couple of them. And yes, they are written in a list, so I don’t want to leave you with the kind of belief that yes, you just check these off and you’re fine. No, these are highly complex. They have to interact to be most effective. But they are helpful things to keep, again, as a framework in mind (see Box 2-2).
BOX 2-2
Physician Communication Competencies
Ability to:
• Set agendas with patients
• Assess and improve patient adherence
• Elicit patients’ beliefs, perspectives, and concerns about illness
• Communicate treatment plans
• Manage conflict and negotiate with patients
• Counsel patients, families, and caregivers
SOURCE: Henry et al., 2013.
So, just learning literally to set agendas with patients would seem like such a simple thing to do, but I can tell you, and Sherrie knows this well, most clinicians don’t do it. They just plow right into their visits. “So, Mrs. Jones, you’re here for your blood pressure today, it looks like it’s up still a little high, I’m going to adjust medication, I’ll see you in 3 weeks, is that okay?” Done. It’s a very doctor-centered sort of approach. Instead of, “What’s important to you today? What concerns are you coming into the visit with?” And there is a lot of good data that the very simple act of negotiating the agenda with the patient, which doesn’t take more time, getting to Sherrie’s point, makes a big difference in the visit. And then things like communicating a treatment plan, managing conflict, and then family and caregivers, all these things that you’ve already heard about.
Shared decision making, this is just again a definition of why it’s important (see Box 2-3). But it’s really about partnerships, getting to Christine’s partnership collaboration team. And again you have to incorporate the patient’s values, beliefs, and preferences as part of that process. And as Sherrie points out, patients will have varying amounts of interest in playing various roles within the conversation, and one of the things that often is forgotten is that there are certain parts of the visit that are a little different. Patients actually don’t want to be involved in the problem solving as much as they want to be involved in the decision making, and Raisa Deber some years ago nicely called those two things out. Problem solving is why they come to see you for the visit, whether it be a nurse, nurse practitioner, or physician, they want you to
figure out what’s going on. But when it comes time to make the decision, most patients want to be involved to some degree, and what the clinician has to figure out is what that degree is and how to help them do that. And then I’m not going to go through the evidence again, like I said, there’s a ton of it.
BOX 2-3
Shared Decision Making
- Physicians and patients make health-related decisions collaboratively, based on best available evidence and patients’ values, beliefs, and preferences.
- Patient engagement through shared decision making is linked to increased patient satisfaction, health outcomes, and quality of decisions.
- Requires competency at the patient, provider, and system level.
What about some of the process basics? This is just a really nice article from Clarence Braddock (see Box 2-4). These are just seven things, very basic, they’re not complete. Michael Barry, who I see here in front is one of my heroes, can tell you a lot more about the nuance around these, but this study that was done about 10 years ago found that only 9 percent of the time did physicians even cover these seven basic things, that’s it. And that’s only if they did it, not if they even did it well. And so it goes to show you that these are things you would think would be important here, considering a procedure and a medication, what are my alternatives, what are the pros and cons, the side effects of what I’m taking, is this really going to help me, is there a chance it might not, thinking about joint replacement therapy as an example.
What does the patient understand? There are some simple techniques you can use, like teach-back and even follow-up, all these things which again don’t require fancy tools, just part of good care and good conversation can make a difference. And this is some nice work done by Towle and others (see Box 2-5). It is also highlighted in the recent Health Affairs. These are just some other competencies really targeting the kind of shared informed decision making. Again, the attitude and skills are important, but here is another thing that has been shown in the literature. Many times we have to negotiate our own professional biases and emotions. We tend to frame things hoping for the outcome we think is important. “You really don’t want that niacin, what you really want is that statin because niacin has all these nasty side effects, but that statin’s great, you only have to take it once a day.” That framing can actually greatly affect what patients choose to do, and be careful about that. Again, partnership, making sure the patient’s preferred role is clear. That is part of the negotiation that we often forget about, and then again, when you present the evidence, just simple things like not using jargon, making sure it’s done in understandable terms, and again, watching out for those framing effects.
BOX 2-4
Shared Decision Making Process Basics
- Discussion of patient’s role in decision making
- Discussion of the clinical issue or nature of the decision
- Discussion of alternatives
- Discussion of the pros (benefits) and cons (risks) of the options
- Discussion of the uncertainties associated with the decision
- Assessment of the patient’s understanding
- Exploration of patient preference
SOURCE: Braddock et al., 1999.
BOX 2-5
Physician Competencies
- Physicians must first agree that patients should be part of the decision-making process.
- Shared decision making requires attitudes and skills that many physicians may not possess or be familiar with.
- Physicians may also need to negotiate their own professional biases and emotions.
- Develop partnerships with patients.
- Establish and/or review patient preferences for information
- Establish patient’s preferred role in decision-making process and uncertainty.
- Present evidence taking into account patient’s own competencies, watch for farming effects.
- Help patient reflect and assess alternative decisions with regard to patient values.
SOURCE: Bernabeo and Holmboe, 2013.
So, I’m going to stop there. I just want to give you kind of a quick run-through and just highlight a couple other things I think really relate to the first talk. All these kind of behaviors, these things that are very competency based and behavioral based, they all tie in by the way to things like connectedness, continuity, and empowerment. It has been shown to be a very important part of that. We also know these very same competencies can be used in a team-based kind of model, and so Lagare’s work, which was highlighted in some of the articles in Health Affairs, really gets at that. And at the end, all these things have to interact with regards to the clinician competencies, the patient competencies, and the system competencies. And Beth Bernabeo has a nice article that really lines up how those three things need to interact. It is not an
either/or, all three have to work in concert to be most effective. So I am going to stop there and look forward to the conversation.
Audience Participation and Open Discussion
MS. PAGET: Thank you very much Gary, Sherrie, and Eric. Okay, so folks, we have ample time for conversation, discussion, suggestions, clarifications, and keep in mind, as Christine pointed out, there is going to be a document, and so your contribution here is really valued and will live forever in that document. So think about how you can contribute, that’s why you’re here today.
I think that we have some really nice pieces of information to be dealing with, Gary sharing with us that information really levels the playing field, information is power, but we’re challenged with how we then universalize routine use of accurate, unbiased information. Sherrie’s model of coach care and asking us, Is passivity dangerous? Do we need to really believe that if patients are passive they are in an unsafe situation? Virtual centers for coach care, what do you think about that? And then Eric’s presentation, starting with system needs, that we need to make sure that when we start with those needs, that we’re addressing both the patient’s needs as well as the clinical needs, and that clinicians negotiating with biases and emotions, that’s a really important issue.
Okay, go right ahead.
DR. GARDENIER: My name is John Gardenier. I’m retired. I have my doctorate in business administration and a career in science and that doesn’t seem to make sense, but it really does. My concern is the framing of the whole issue, and I think that everything that is being said about the physician-patient interaction here is helpful and useful, but it’s a tiny piece of the overall problem.
When I took my doctorate I concentrated on information technology, operations research sometimes called management science or systems engineering or industrial engineering; all those terms basically mean the same thing. How do you get the system to work in an optimal way and the implementing mathematics aside from operations research with statistics and accounting? And it’s that bunch of things that needs to be brought together and you need to look, I believe, at a health care management system that starts from the overview.
We know the U.S. health care system is continually getting more expensive and less effective. This should be a major concern. It takes systems engineering and expertise to help resolve that. At the individual hospital level or even the individual clinician’s office level, systematic management practices should be involved to try to improve the health care system. Just information technology is just a basic thing. I don’t see a lot of electronic medical record systems, but the ones I have seen certainly never had any involvement by any professionally trained information technologist. And they should. I mean the knowledge is there. We spend hundreds of thousands or millions of dollars training people to have the professional skills to do this stuff right, but in the health care business we don’t use those skills. And to me that is a problem, which if implemented in a systematic manner, would incorporate what you’re talking about with patient, caregiver, and provider interactions as measurable parts of an overall systemic effort at improvement.
MS. PAGET: Thank you. Thank you very much. Sherrie, you’re at an academic medical center. Do you have any comment about that? Any success stories that you could share?
DR. KAPLAN: No, we are right in the middle of implementing an electronic medical record system, and it’s really an amazingly difficult thing to do. And yes, because I think that that is the time when you can actually try and incorporate some of the personal health record information, but more importantly teach people how to use it. So, if you intersected the technology that creates information about the patient with a training program for how to use it effectively when you come the next time to talk to your doctor—that I think really is important.
MS. PAGET: Lots of opportunity there. Sally?
MS. OKUN: Hi, thank you very much. Great presentations. My name is Sally Okun and I’m from PatientsLikeMe. A couple of comments.
Sherrie, I want to follow up on your comments. I actually went back through some of my slide decks recently and found things that I could refer to that I talked about in the mid-90s; it is time for us to just really make some change and make it happen. So, oftentimes I find myself pretty amused at the cartoons that are still relevant today that I was using in consumer-based education at the time, and it’s just really a little distressing.
A couple of tips though. I am a palliative care specialist. I’ve spent most of my career with patients in their homes, sitting at their kitchen tables, listening to them talk to me. And one of the things that I actually learned really early on in my work was that I couldn’t go in with my own agenda. I needed to go in and just sit with them for a moment and let them tell me something. And so I would oftentimes open the conversation with, gosh, you look tired, what’s keeping you up at night? Or just, what’s on your mind today? Now oftentimes what I heard had nothing to do with their health or their health care or anything to do with illness, it was totally unrelated. What it offered me was an opportunity to hear how they framed things. I heard the words they used, and I heard how they would put phrases together. And then I would train myself to think about ways of taking that and give it back to them in similar ways that I would talk to them, so that I would no longer be talking in the way that Sally Okun, RN, would come in and talk, but I was starting to learn a patient vocabulary.
Now, one of the things I’m quite proud of with PatientsLikeMe is we have developed a patient vocabulary and it’s been from the patients’ reports themselves. And what we’ve done is we’ve taken that in and we’ve coded it against clinical taxonomies and clinical vocabularies but we retain the patient voice always. If someone wants to know what it translates to in a clinical term, we can tell you that, but we’re more interested in what the patient actually said.
So, to your point, I think PatientsLikeMe could become a degree granting center for the Centers for Patienthood. I appreciate the comment. I think it’s great and I’m really looking forward to more comments from the patients from the audience. But keep that in mind, what’s on your mind or what’s keeping you up at night and you’ll hear and you’ll learn quite a bit because patients will tell you a lot more than you think. Thank you.
MS. PAGET: Thank you.
MR. THOMAS: Hi, I am Richard Thomas. I’m the Program Director with Blue Shield of California Foundation; thanks for putting together a great panel.
My question is actually for Eric, as the representative, I think, on this panel of organized medicine. So I’m wondering if you could give us some more insight as to how physicians are viewing this drive-pull-push desire for more patient engagement. And what advice you have for those of us who are not physicians about how to create and support physician champions whether in medical education and training or elsewhere for this general effort.
DR. HOLMBOE: Wow, there are a lot of things we can do. And we actually have an expert who is standing right behind you. So, Mike Barry has spent a career developing tools, so there’s
clearly ways to leverage shared decision making tools that Mike has developed in his work that I think could be very helpful.
I think right now part of it is honestly generational. The younger folks coming through see this as something valuable. This is something that is being much inculcated into them. So it is like anything, if you kind of grow up with it in your training, it just becomes part of what you do. I think that training programs have gotten much more systematic about training people and I think they have been able to show that it makes a difference. The biggest challenge we have is not so much that we lack training methods, particularly in medical school and residency, but it’s that once you put the trainees out in the clinical environment it gets completely undone. And it’s what Fred Hafferty calls the hidden curriculum. So say, hey, this is the right way to do it. And then this is one of my favorite stories from Dan Duffy, one of my heroes who brought it to the board: he would spend all this time teaching shared decision making to medical students, and then they would come back 2 weeks later, and he would have them go through a refresher and they would look awful. He’d say, “We just talked about this 2 weeks ago, what happened?” “Well, I tried that in the emergency room and the resident told me I don’t have time for that, just simply do X.” And so I think part of it is culture again, part of it’s going to have to create the space.
I also think the boards can be helpful here by creating tools and mechanisms to help people get better at this. I’m always struck that when I work with older physicians, and we had a couple examples of this at Yale, that when the older physicians learn communication skills, they actually find greater satisfaction in their practice and there are actually some good data around that. Many times the reason they are struggling is that they don’t have good communication skills so they become inefficient, patients keep coming back, patients aren’t happy, and when they learn better communication skills it’s a revelation to them. They just weren’t taught it. They were taught to be so doctor-centric.
So, I think the boards are working to create some tools, but clearly there is lots of opportunity in continued professional development to build this in. So, I think the patients could use a certificate program, frankly, and so could a lot of the clinicians. And we just haven’t done a good job of that. And I think Clarence Braddock’s article for me really stands out. That was 1,058 audiotapes of surgeons, family medicine, and internists, and 9 percent of them even bothered to cover those things. So I think CPD as well as education, but we also need a culture that allows people to have some opportunity to use those skills.
MS. KORNBLAU: Hi, I am Barbara Kornblau and I’m the Executive Director of the Society for Participatory Medicine. What we are, by the way, we are pilot testing a pledge for physicians, which will eventually be extended to other providers.
But I just wanted to make the point, in our organization we treat patients and providers equally, it’s an egalitarian organization. And I think that there is a real need for patients to be the ones, with all due respect to the engineer who stood up, I think one of the problems in health care is that a lot of things are decided from the top down. And I find as an e-patient myself that I’ve had to train my providers and teach them. Like the ophthalmologist who offered my father, at 95, three alternatives for treatment for his macular degeneration and told him to go on the Internet and look for it, make a decision. I had to train him that my father doesn’t have to turn a computer on, he can’t see, that’s why he’s seeing you. So the computer’s not going to be very helpful to him. So you need to give alternatives. You can call me, I am the caregiver, but you can’t expect him to make decisions. However, my 25-year-old can make very good decisions. If you give him
option he can go on the Internet and he can find more information than I can about just about anything in the world.
So I’ve taught all of my kids; I have six children with chronic conditions. They go into the doctor and they ask questions before the doctor opens his mouth. They give their history. I’ve trained them. They bring their file with them. And I think that that’s how we’re going to change the culture, is from the bottom up. And physicians will start respecting—there will be this mutual respect, where when someone comes in with the information they need that the provider, and not just physicians, PAs, nurse practitioners, everybody else in the team, will have an understanding of: this person is giving me information that’s valuable, that’s going to prevent medical errors, that’s going to improve quality of care, and make the visit faster because I don’t have to hunt and peck, they know what’s important.
DR. BARRY: Mike Barry from the Informed Medical Decisions Foundation. Thanks all, a lot of great points. I’ll just pick up on one that Gary talked about.
There is such clinician pushback sometimes around the shared decision making stuff that it is okay for college professors but not really for regular folks and the importance of asking the right way that Gary highlighted, that contingent on having the right tools, the feeling is quite different. To extend that in our foundation in our demonstration sites, actually catch people in the decision window, and give them information about their condition, those numbers then go up over 90 percent and that seems generalizable across age, educational level and even gender, amazingly. So again, this notion that the idea is ubiquitous, but people need different kinds of help in their situations.
MR. DEBRONKART: Yes indeed, information boosts engagement. How on Earth, it just stuns me that this is a surprise and research finding worth publishing. How on Earth can anybody participate in any discussion if they don’t have information, and yet, what Cristin said about culture eats strategy for lunch, this is so important. I see this loop, all the conferences I go to where we say “Don’t give patients information, they can’t understand this stuff,” and then they get insulted for not knowing anything.
And when I first spoke at the Meaningful Use hearings a couple years ago, I mean this is really important, that I tweeted something about a certified e-patient. It’s a great idea, but it’ll be for naught as long as patients get smacked down by clinicians, which is why, as Barbara said, the society has met the program with matching pledges, I the provider promise to do this, I the patient promise to do this. I told the story in my Meaningful Use testimony that 50 years ago, more than 60 years ago, my mother had to learn to drive because she had three kids and a traveling salesman husband who was never home, and in the early 1950s a lot of women didn’t drive. In fact, the cultural conversation was that women drivers were depicted in cartoons and late night comics with the bumper wrapped around the telephone pole, and indeed mom within a couple of months of getting her license bumped back into a pole, put a dent in the bumper. The irony here, my dad said, “Well, good, I’m glad this happened in a harmless way so you could learn.” The irony is that today insurance statistics show that women have one-third fewer accidents than the men who used to make fun of them.
Okay, so while we work on the facts, obviously people perform better when they are informed better, that applies to clinicians as well as patients but we also really need to work on the culture, because as long as people think that patients can’t understand anything useful, it’ll be for naught, so let’s do both.
MS. ROHRBACH: Two questions from the Web. The first is from Shilpa Amin, MD: Can the panel and audience address the role of cultural competency and multilingual skills as part of
the needed skill sets in our health care communications approach with an increasingly diverse demographic shift in our patient populations?
The second question is from Petra Langer from the Schwartz Center for Compassionate Health Care: What can be done to relieve stress that many caregivers feel today, which can impede their ability to connect effectively with patients and families?
MS. PAGET: So that first question I would open up for both our panel as well as anyone in the audience who has any experience or knowledge in that area of cultural competencies.
MR. LANGER: We have data like that in our survey for Blue Shield of California Foundation. We do show first that willingness to participate in shared decision making is largely sociocultural socioeconomic in basis. Individuals who are traditionally less empowered in our society are more hesitant to take an active role in their care; less educated, lower income, noncitizen, non–English speaking.
So, cultural competency is again a way of getting across the information that levels the playing field, and we do find that these populations desire cultural competency, want to work with care providers who understand where they are coming from, who speak their language. That’s an essential element of the communication that is so essential in getting across the information that leads to connectedness, continuity, engagement, and empowerment. So, we do see that in the data, yes, that cultural competency is important. And that’s why facilities such as traditional safety net clinics continue I think to thrive, because they have a specialty in that area.
MS. PAGET: So the second question about caregiver stress, any of our panel members want to address that?
DR. HOLMBOE: I am no expert here, but it is a big issue. And it’s going to only grow with the kind of silver tsunami that’s coming for all of this. We know that that’s a really growing problem. There are some good examples of respite programs. The VA has had a respite program. When I was at Yale they would give the caregiver some time when they were taking care of a family member—that was huge because they really can experience burnouts. I think we have to be attentive to that, and as we have an aging population, we’re going to see probably more and more of this, and it can actually have its own health effects.
There’s some literature that it too can be not only disempowering, but can also have its own health effects. So I don’t have an easy answer there. Like I said, there are some examples that are usually with enclosed systems, the VA and the military being two of those, but I certainly resonate with the question as somebody who is experiencing some of that now on my own level.
MS. SALMOND: My name is Sue Salmond. I am from the University of Medicine and Dentistry in New Jersey. And I just wanted to refer to the concepts of connectedness and the coaching. We have a community health clinic in an underserved area that is really very transdisciplinary in terms of physicians, nurses, and other health care providers working together. But perhaps the uniqueness in our model is that we hire and train from the community that we serve; community health workers that serve in the capacity of that cultural broker and help the physicians, the nurses; and other health providers understand how to teach from a culturally competent perspective, how to present information. We have teams of physicians, nurses and other health providers that are led by the community health workers, and they see clients in the community, which is where culture lives. And I think we have to look at getting out of our classic organizational health care into the community, valuing many different people on the team that can truly change health care, and we have seen a tremendous difference in patient engagement with this model.
DR. MONTORI: Victor Montori, Mayo Clinic. Our team has been working developing decision aids since 2004, and we’ve taken the approach of creating very lightweight, very small footprint tools that can be put in front of the patient and the clinician. And the clinician and the patient can then review them together, and the tools will contain the options and risk and benefits of each of them and they can discuss together and arrive at a decision together in the office.
Those tools have been developed with participation of the patients and the clinicians actively through a series of prototypes. So, we don’t have the problem of work that usually happens in the way we normally do things, which is go to the conference room, get a bunch of experts, close the door, figure out exactly how you want to do it, refine the intervention to the point that it’s perfect, then take it to the practice, put it in front of clinicians, and then write the paper about barriers and the fact that these people do not know how to use your tool and do not know how to incorporate it into their workflow; we have had that problem.
And we also had a couple of other problems. The first one is the notion that clinicians and patients will have different knowledge bases. They are looking at the same material. They could have other backgrounds and as the conversation is created they will bring those backgrounds to bear. What I’ve recently discovered is that if we set up the knowledge level for the patient, it’s actually good enough for the clinician. Sometimes we overestimate the clinician’s cognitive abilities and we try to educate the clinician, for instance, for maintenance of certification or other purposes; we actually raise the bar so high that it becomes impossible for a burnout clinician which is becoming the average clinician. And so by creating tools for patients, those tools actually help the clinician also stay up to date.
The reason I’m telling you that is that even though we are intervening during the consultation, the duration of the consultation does go up, but not massively so. So, on average it’s about 3 additional minutes for a consultation average of 20 minutes. So, it’s a small amount, particularly if you don’t use the duration of that visit as your denominator, that duration as a relationship, a series of visiting continuity as a denominator, as well investment in time that could potentially pay off.
The fourth thing that we’ve uncovered is that most of the demographic determinants of whether somebody will participate in decision making fall apart. If you actually engage patients by meeting their needs, informational needs, you have young and old, women and men, participate actively in shared decision making. And we have video recordings to demonstrate that is the case, and we have done now a meta-analysis of all our randomized trials where we tested these tools, and in the meta-analysis all socioeconomic differences are based like in terms of education levels, actually these things levels it up after intervention.
The average, this will be my next-to-last point, the average age of our participants is 65. So this notion that only young people are interested or are able to participate goes away once you develop tools for everyone; that way people are happy to participate. They know what’s at stake and they have a lot more experience to rely on to participate in an encounter.
My last point is that a lot of the things that we know about these things come from observation and experimentation of the system as is. And in the system as is, we find a lot of clinicians who have given up, have learned helplessness, and they feel they are not under control, that it is cost and cost containment and the economic reality that are dominating the day, and these things hurt details.
In parallel, there is an industry that is beginning to emerge around patient empowerment and shared decision making that is making these things also another factor, another thing to consider in the business plan. And in a study that we did with our designers at Mayo, we actually
interviewed patients in the hospital and asked them, “What meaningful experience of care have you experienced?” Then we collected all that and tried to find out what creates meaningful experiences of care for people that are very sick, and the way in which you can tell there is a meaningful experience was when somebody went out of their way. So if rounds came around and then one doctor came back and said, “You look confused, you look distressed, what went on?” If a doctor on the way home off the white coat actually comes back and talks with the patient and makes everything clear, are you comfortable, talks to the family member who just flew in but was late for rounds, every time somebody goes out of their way it creates a meaningful experience.
So, I would encourage us that when we talk about empowerment and shared decision making things, we keep going back to the fact that these are two human beings that actually by nature would like to have an engagement, would like to talk to each other and let’s not over-script this, not make it an economic transaction, and make it a meaningful experience.
MS. TARINO: I am Danielle Tarino from the Substance Abuse and Mental Health Services Administration, which is an operating division of HHS. Eric, I really appreciated your slide that you wanted us to remember, talking about health systems and health populations. And being that we live in a country where one in five adults will be diagnosed with some sort of behavioral health issue whether it be a substance use disorder or a mental disease, we have an extremely vulnerable population who don’t always know how to have those conversations with their doctors.
We deal with a lot of confidentiality and privacy issues. I have spent my entire federal career trying to figure out how to relay the information that I hear at all of these meetings to my population. And I’m having a bit of problem, because I come from a clinical world. Before I came to the government, I worked at a university in a mental health and substance abuse clinic on campus. And if you had paranoid schizophrenia and I tried to tell you and inform you that you had paranoid schizophrenia, you thought that I was out to get you. So, we have a population that is extraordinarily vulnerable, and when it comes to informed patient decisions, the families really need to be on board as well, because, the majority of the time, families are the advocates for the vulnerable communities that I have experience working with.
And also along the line of curriculum, there’s an extraordinarily large amount of bias that we’ve heard our consumers talk about feeling from their physical care providers. In a world where we’re going to be exchanging health information and my diagnoses are going to be on my electronic health record, do I want my podiatrist knowing that I once tried to commit suicide? So, as we move on with the workshops, I just came up here to kind of plant the seed of the idea of mental health and behavioral health needing to be considered in these processes, because we have a large amount of people that suffer with these conditions who have less access to information than we would think. And that’s all I had. Thank you.
MS. PAGET: Thank you very much for sharing that perspective.
MS. DAY: I am back. I am perhaps the most engaged patient in the State of Maine. And that’s because I’ve worked with, I’ve networked with patient safety activists and advocates through the Consumers Union Safe Patient Project. It’s a phenomenal project and a wonderful group of people, and about 2 weeks before the 2011 Summit, where we all get together once a year, I was diagnosed with uterine cancer and needed cancer surgery. Well, I’m 63 years old, 62 at that time, and I’d never had surgery for anything. I’ve been very lucky.
So, I had all of these people to talk with and I really truly became engaged. I took a full 2 weeks to make my decision about where I would go and where I would have that surgery. And I
will comment that it’s not easy to be an engaged patient. I was considering three different hospitals and I tried to find out the complication rates for the particular surgery that I was facing, and that was impossible. The infection rates were a little bit easier, but I was particularly blown away by the infection control nurse that said, “We don’t have to report those infections until next year.” And I said, “Unfortunately I have cancer this year.” And I did not choose that hospital. It’s awful that I based my choice on that but it really did turn me off.
But when you talked about engaging patients, a couple of things came to mind. Before I went into the hospital to have my surgery—and I had a wonderful outcome by the way, I’m cancer free and happy about that—I wrote a letter to the patient safety officer at that hospital, which not too many people have done. I would suggest it. I told them who I was. I told them I was scared and I wasn’t there for a social call. Basically, I was there to get rid of cancer, and today I wasn’t one of them, I wasn’t one of us, I was one of them because it is an us and them thing when you’re on the other side of it sometimes. And I laid out my expectations, and one of those expectations was that I wanted my husband to stay with me overnight. I only had to be there one night. And nobody ever responded to the letter but when I showed up for pre-op, I had all kinds of visits from administration. I was very quiet because I was scared, but they got it. They got it that I didn’t just write that letter for myself, I wrote it for everybody. I wrote it for all patients.
So what came to mind when we talk about engagement and all of that is that maybe it’s time to review patient rights, and rather than things being ideas and hit or miss, and maybe this hospital will allow you to keep your loved one with you overnight and that is the greatest source of comfort that I had, but that one won’t, and if you’re in a semiprivate room, you can’t have your advocate stay with you overnight. I think it should be a patient’s right to have an advocate by their side when and where they want unless it creates a hazard or puts them in jeopardy somehow. And the other right I think that we should have is the right to our own personal health information, and that shouldn’t be anybody’s decision, it should be our right as patients to have that information. A lot of discussions wouldn’t even need to be held if they became rights.
MS. PAGET: Thank you very much. I am going to be a moderator police now and make the decision that on this side, Mark, you’ll be the last on that side, and Grace, is there anyone behind you? All right. We are going to continue with this topic after the break so thank you. Perry.
DR. COHEN: I have had Parkinson’s for 17 years and sometimes it is hard to get the words out. But I’ll give it a shot. My name is Perry Cohen, Parkinson Pipeline Project. I want to focus on the issue of change.
I agree with all the stuff you’re saying about patient empowerment, but to me technology is what’s going to drive the change and our friend, the Mr. Engineer, had it right. But the other person who commented on that also had it right, that you have to have involvement of the patients and the teams that are creating the change. We have an opportunity now with $18 million or $17 million going into electronic medical records to do that engineering so that this is what’s going to drive the change. And to get the patients who are involved and get the physicians more involved with patients. We also ought to be looking at the personal health records as well as the electronic medical records. I actually was working with a doctor to do that in her specialty care for Parkinson’s care.
So the bottom line is it’s specialty driven. Each disease entity ought to be able to organize itself to create the culture and environment to train the patients and train the doctors that have their own certification system like they do now for like the Board of Internal Medicine. That’s about all I have to say.
DR. KAPLAN: One of the things about information is, we know information alone doesn’t change behavior. You need training programs around how to use the information, and one of the things I wanted to make clear is with the personal health record, and the new Choosing Wisely Initiative by the American Board of Internal Medicine in concert with specialty boards, is they’re teaching physicians what not to do.
At the same time, we’ve got an indemnified population out there committed to the notion that they deserve service and they deserve expensive service. They deserve the kinds of services they want and need. Teaching people how not to use may be a place to start—what you don’t need and what kinds of things that training modules are for, if you want to know how to talk to doctors about this, link up here, or talk to a professional society. But learn how to use information and how to ask better questions, how to ask, “Do I really need this?” Those are things that we still don’t do systematically with patients and I think this is a great opportunity to start.
DR. GARDENIER: My name is Turkan Gardenier from Pragmatica Corporation. For many years I have worked as a health statistician and researcher, and my comment and perhaps question to the panel members refers to the new trend for early intervention and risk benefit assessment concurrently developing with genetic marker evaluations, those getting into databases. And in any models I have seen along with patient data, there’s the query about exposure assessment, air quality indices, water quality indices, and they all are in different places.
As a family, my husband was the engineer who posed the question, we were at the annual meetings of AAAS, American Association for Advancement of Science, and I heard fascinating presentations on air quality levels and their association with 911 calls, especially in July and August. And the number of apartments that had no air conditioning, and also the statistic that because of lack of CPR or adequate CPR 90 percent of the people who made the 911 calls did not survive. Well, as a senior, if I lived in a metropolitan area and didn’t have much air conditioning I would move, having the flexibility to do so even before anything happened. And then I delved into the databases for environment indicators in different areas using geographical information systems, and I couldn’t really understand the data there. Is it risky? Is it within standard? Or not within standard?
So, aside from training patients who already are patients, we also have to work with the databases that exist to individualize the information so that people who are semi-knowledgeable about this can make interpretations for themselves even before going to a physician.
DR. JIMISON: Hi, I’m Holly Jimison from Oregon Health Science University doing a rotation through NIH and Bob Kaplan’s Office of Behavioral and Social Science Research. I have a comment and a question about the roles and responsibilities leading to defining competencies.
So to start with Eric’s list of competencies where the last one was have the physician ask the patient what their preference is or decision, I want to emphasize that many physicians seem to take that as well, “What do you want to do?” being the question. As opposed to needing to make an optimal decision or even an optimal recommendation for a patient, you need to understand their values on the outcome, not just what do you think you want to do. They are the experts in diagnosis, prognosis, understanding the probabilities of complications, although oftentimes other patients are more the experts in what it’s like to live with the health outcome that may be part of important information systems that get at that.
But from both patient competencies and physician competencies, I just want to make sure there’s an emphasis to not just saying, “What do you want to do?” but, “You are a unique
individual with your own values and very legitimate differences of opinion on living with complications of treatment,” and getting that information during the visit or before. Thanks.
DR. HOLMBOE: I’ll just quickly respond. In no way do I intend to say, “So what do you want to do?” I mean that’s the worst thing and again that’s a skill. It’s interesting, even in that study, that even what you just said, which I totally agree is not a functional way to do it, that was rarely done, which is fascinating. So even saying, “What do you want to do?” is not commonly done and you’re absolutely right. I think it was wonderfully said by a patient, I apologize, a patient like me, “You’ve got to know who your individual is,” so taking a couple minutes to get a sense of how they view their illness, who they are, is absolutely critical and it is part of that connectedness right. And then if you saw one of the first things on the list from Braddock and Wendy Levinson it was you have to have a conversation, invite them to participate. Tell me a little bit about who you are, and I want you to help me make this decision. I’m not just going to leave it out for you to lay a bunch of choices. In fact, we know that’s not a very functional way, and in fact Mike Barry’s work in decision aids is designed to help avoid some of that. So I totally get it and I’m glad you raised that.
MS. PAGET: I think it begs the question of the definition of what we need when we start to use these phrases like “elicit preference.” That’s a really good point. Okay, Grace, you’re up.
DR. LIN: Grace Lin, University of California, San Francisco. I appreciate the comments from the panel and from the audience, and one of the things that struck me was the fact that, and I think Eric you touched on this, that we have a very disorganized system.
Medicine doesn’t happen as a system, it happens in a silo. I’m a clinician. What happens with me and my patient happens right then. I’m not in the room with somebody else when they are talking with their patient. And so it occurs to me that we haven’t really talked about how, as a clinician or as a patient, how we know we are doing well. How we know that we’ve achieved what patient-centered care is, how we know we’ve achieved that we’ve educated the patient appropriately, that the patient is engaged appropriately, and how we let the physician know or the hospital know or the health care system know that we have reached the goal, the goals that were laid out here in this conference.
So I just put that out there, I don’t think there are easy answers but I put that out there as sort of a challenge and for comment.
DR. HOLMBOE: I just resonate with that and I think measurement, I’m sitting next to one of the gurus of measurement. I do think we have some things, and like Judy Hibbard, who I believe will be here tomorrow, her patient activist measure is actually very useful tool. We don’t use enough of that.
One other comment I want to make about the system is we tend to think of the system being the information technology, and I really like the way Paul Ginsburg and the Dartmouth group think about it—no, no, no, it’s not the system, it’s the facilitator. Information and IT should sit as a hub of information, but system is mostly about how people work together and how they coordinate and do care as a team over multiple locations, and I think we have to be careful to not always think of systems in terms of just technology. “Systems” is mostly about people.
MS. PAGET: Thank you. I think, Grace, your point about accountability is really important. We’ve got to bake that into the whole conversation. Okay, Mark?
MR. GORMAN: Mark Gorman, patient advocate. Actually this has been a very rich discussion and an excellent panel, and I think certainly exceeded my expectations as a member of the Planning Committee. And Eric, you actually were here very intentionally as a representative of organized medicine so I’m glad that came through. But nobody was trying to
put you on the spot. You got the invitation because several members of the Planning Committee have been listening to you for many years talk about the concomitant competencies that clinicians need to acquire. And the discussion here today highlighted sort of the tension between everything has to be on the patient’s shoulders to learn how to be effective as well as, and Dave pointed out, the most activated patient is potentially going to be profoundly frustrated encountering a brick wall.
So, we need to find a way to meet the happy medium there. You’ve used the word “skill” at least once, maybe a couple of times, so just to conclude, when I think about these things, it’s an extremely important distinction on this physician communication skill competency. It’s not a trait. It’s not something that somebody got because they were raised in a household and learned to be a good communicator. I mean once, on the clinician side, these competencies are put in the box of being skills, then you have things that can be taught, you’ve alluded to that, for which clinicians can be accountable, and even as you just said, measured for having acquired.
So I hope that you and your colleagues in organized medicine will be encouraged to continue your good work. You alluded to multiple boards here earlier. We have to become collaborators and I’ll have a couple of things to say about that in the concluding panel tomorrow. This business of culture of patients and clinicians being at each other’s throats, that’s got to change.
MS. PAGET: Thank you, Mark. That was a nice wrap-up. Okay, I have permission from the powers that be to give you a full 15-minute break even though we’re 5 minutes late. So we are going to reconvene at 3:20. I would like to ask the panel members for the next session to come back about 3 minutes prior to 3:20 and I want to thank Gary, Sherrie, and Eric.
Break
PATIENT-CLINICIAN COMMUNICATION AND THE TOOLS FOR CHANGE (CONTINUED)
Ms. Lyn Paget (Moderator)
MS. PAGET: So, given the conversation that we’ve had this morning and the information that we’ve been going over, I think it’s clear to all of us that what happens when you get in these kinds of environments and start talking about this is, we create a lot of energy, number one. But number two, we start to ask the questions around implementation. What does this really look like in the trenches? How does it affect clinicians? How does it affect patients? Are people happy, are they not happy? What does it really look like?
We know this isn’t easy. We know there are challenges and what we have for this afternoon is a group of people who have been doing this not for a few months, but for several years. So their experience is a real testament to what we all need to learn in order to implement the kinds of protocols that we know will support patients and families. And we’re asking the question, does this work to change the environment to one that respects the goals and concerns of every patient?
And before we start this, I just wanted to read for you something that was written in the Health Affairs journal that everyone has referenced this morning by Jessie Gruman. I know a lot of you know Jessie, and she writes a narrative piece about her fourth cancer diagnosis. And as she is summarizing, she makes these statements that I think are pretty compelling, and she uses a
phrase that I really want us to be thinking about. “No clinician, insurer, or regulator could have devoted as much time and attention as I did to determining how I wanted to be treated or how I want to live. In retrospect, I am awed by the gravity of the decisions I made about my health care and by the limited evidence on which those decisions were based. At the same time, it took full scale, sustained efforts by me and my family to develop and carry out my treatment plans to get the most out of my care. I am concerned about those who cannot summon such energy. They will suffer unnecessarily.”
I think we’ve had a lot of people make the points this morning that we do have unnecessary suffering. And if we don’t underscore the point that we are doing harm and not good, and that this is about colossal cultural change—but we also need to do the kinds of systems and infrastructure work that we know will sustain this from here on out. We owe this to every patient and family member and we owe it to ourselves.
With that said, I am very pleased to introduce our completely West Coast panel, thank you for making the trip here today, I’m not sure what that says about innovation but we can figure that out I guess. So, we are going to lead off today with a presentation by Grace Lin. She is an Assistant Professor of Medicine at the Phillip Marley Institute for Health Policy Studies at that University of California, San Francisco. Her research agenda focuses on resource utilization, appropriateness of care, shared decision making, and measuring the quality of decision-making process, particularly in cardiology.
Following Grace’s presentation, we actually have three professionals from UCSF, including Jeff Belkora, who is an Associate Professor of Surgery and Health Policy at the University of California, San Francisco. His professional mission is to help people grow in their capacity for leadership, teamwork, and decision making. Margot Zarin-Pass is a first-year medical student at UCSF. She was previously a premed intern at the UCSF Breast Cancer Center. There she provided decision support services to patients and conducted patient engagement research. Lastly from UCSF, we have Ekene Obi-Okoye. She is a premed intern. Her current projects include studying the biology surrounding breast cancer recurrence, designing support programming for metastatic breast cancer patients, and participating in the patient decision support program at the Breast Care Center.
And to round out the presentations today, we have David Arterburn from GroupHealth in Seattle. He’s a general internist and a health services researcher who holds positions as an associate investigator at GroupHealth Research Institute, and as an affiliate associate professor with the University of Washington School of Medicine in Seattle. His research covers a broad range, including comparative effectiveness of weight management interventions, pharmacoepidemiology, pharmacogenetics, bariatric surgery, and shared decision making related to elective surgery.
So welcome to all of you, and Grace, you’re up.
Building a Culture That Promotes Shared Decision Making
Dr. Grace Lin
DR. LIN: Thank you, Lyn, and thank you for the opportunity on behalf of my colleagues at the Palo Alto Medical Foundation and Palo Alto Medical Education Research Institute to share our experience building a culture that promotes shared decision making. I’d like to start with an overview of the Palo Alto Medical Foundation and what we call the Partners in Medical
Decision Making Program, and then move to how we promoted awareness of our program to physicians and to patients, and then end with some lessons learned.
The Palo Alto Medical Foundation is a multispecialty medical group in the San Francisco Bay Area consisting of over 750 physicians and serving more the three-quarters of a million patients, mostly in a fee-for-service model. I tell you this just to set the stage for what I’m going to say. Being in the heart of Silicon Valley, PAMF has been an early adopter of such things as the electronic medical record and the online patient portal, as well as having commitment to patient education supporting community health education centers and shared medical appointments. What I speak to you about today is an initiative that was funded by the Informed Medical Decisions Foundation, the Partners of Medical Decision Making Program, which is a demonstration program designed to implement decision aids into primary care practices.
So, what’s the problem? The problem is that the use of decision aids is not common in current practice. And here I have some quotes, one by a patient who says, “It would have been nice had it been offered during my visits to the sports doctor, the primary care doctor, the orthopedic doctor.” He’s been to several doctors and he says, “None of these people offered me this decision aid.” But on the other side, we have physicians saying that the patients “don’t really want the decision aid if I offer it, because they don’t want to think about something like colon cancer screening, or you just kind of run out of time.”
So, what do we need to do? We need to promote awareness to facilitate a cultural change. And who are we trying to engage? Obviously, we’re trying to engage everyone from physicians to patients to institutional leadership, and so what we did was we made a strategic decision to develop a social marketing campaign to increase awareness of shared decision making and decision aids. And social marketing in this context in health care has to do with promoting a health idea. So that’s what we wanted to do, a concept. And as you all know in marketing and when you promote an idea, branding is really important.
So, one of the first things we did was we actually named our program, Partners in Medical Decision Making and in it we wanted to reflect our goal, which was to promote physician-patient partnership and to empower patients. So, we then came up with these three taglines: empowering patients to make personalized decisions with their health care team, prescription strength information for better decisions, and better decisions together. And these are the taglines that are on anything that we produce, whether it’s educational material, whether it’s branded products as you can see here, our newsletters, so that patients and physicians and whoever is reading this are reminded that this is what Partners in Medical Decision Making is about.
We also engage practitioners in leadership through various and many channels. And you see an example of some of those here, including grand rounds, newsletters, sort of more traditional things, but I wanted to draw your attention here to academic detailing. And you might be familiar with academic detailing from the pharmaceutical industry, where the pharmaceutical representative comes to the physician’s office, talks to them about their product and educates them and tries to sell them on their product basically. We took this idea and instituted the same principles. Our wonderful shared decision making navigator Caroline would go and do visits to each clinic every other week, talk to the physicians, talk to the nurses, medical assistants, whoever was involved with the decision aids, just to remind them that the decision aids were there, but also to train them on how to use the decision aids and to get feedback on the program. And this was a tremendous time investment, but really was necessary to keep the visibility of our program high in the clinics.
We simultaneously promoted decision aids to patients in the form of posters, brochures in the exam rooms, and then again, being very IT savvy, had Facebook, Twitter, blogs, newsletters, and the like, so we got mentioned there. And then we directly engaged patients through two mechanisms, which I’ll briefly mention. One is the self-screening survey and the other is shared medical appointments. The brief survey was a survey when the patient checked into the clinic to assess the need for a colon cancer screening decision aid. So we had a series of questions that asked, Are you over 50? Have you had colon cancer screening? And if the patient was eligible and expressed interest in receiving the decision aid, the medical assistant or the front desk staff would give the patient decision aid prior to seeing the physician.
And really this was very successful. You can see before the screener, the clinic was passing about four decision aids per week. During the time that the screener was in use, decision aid distribution went up to about 18 to 20 per week and then all of a sudden it dropped off again. And we were wondering why. So, we went back to the clinics and what we found out was that the physicians actually, although they initially gave their approval, they withdrew it. For example, a physician said, “We don’t want to continue the self screener because the volume of patients who are interested in materials is difficult to manage.” In other words, they didn’t like having to talk about colon cancer screening when it wasn’t on their agenda. Or another physician said, “If we give the decision aid to patients, we won’t be providing personalized care,” which was sort of interesting because that’s exactly what the decision aid is designed to do.
So, even though we were successful in engaging the patients, what we found was that the patients and the physicians, if the incentives aren’t aligned and they aren’t on the same page, we really were not going to be successful distributing a decision aid. And this was a theme that was prevalent throughout our in-clinic distribution and, you can see here, just briefly, this is from our Health Affairs paper, this red line represents the percentage of patients for colon cancer screening that we feel like we reached and that number by and large was under 10 percent of eligible patients. So even though we distributed over 6,000 decision aids in this project we think we reached less than 10 percent of patients. So there’s a lot of work still to be done.
A more successful intervention is what we call shared medical appointments. For those of you who don’t know, shared medical appointments are when a group of patients with the same condition see a physician together; instead of having individual appointments, they come together and they discuss their condition. And early on in our project, our steering committee said, “You know, I think that shared medical appointments would be a great way to institute shared decision making and engage patients and try to distribute decision aids.”
So, we solicited interest from our geriatricians who were interested in doing shared medical appointments. And we set up a series of three 90-minute sessions whose goal is to engage patients in care and perform functional assessments for conditions that have a high impact on health outcomes and aren’t consistently done in primary care; things like memory assessments, fall assessments, screening for depression. Really, this is a way to both achieve the physician’s agenda and engage patients. And because individual assessments are made and documentation is done in the electronic health record, it can be billed as a standard level three visit, so all of these are billed at a 99213 level. We’ve enrolled over 150 patients to date in a variety of ages. And actually, I’m going to let this, we have a video that was produced by PAMF Public Affairs. I’m just going to show you a little bit to let you experience the shared medical appointment. (Shows video.) So, that just gives you a little bit of a sense of what happens at a shared medical appointment and the goals of it.
So, just to finish up quickly, what we found from our experience is that culture change is very hard. And that engagement at all levels of the health care system is really required, from the patients up to the leadership, because it doesn’t happen otherwise. Physicians may need more training. Team-based models where physicians aren’t the only people involved work best. And then incentives need to be aligned, as I mentioned earlier. And patients need encouragement to become engaged. And then, as we show with our shared medical appointment, models of care such as these might be more conducive to shared decision making and patient engagement.
So I thank you for your attention. I just wanted to acknowledge our funders, the Informed Medical Decisions Foundation, the PAMF leadership physician staff, and our fantastic PMDM team which Dominick mentioned. He and I led this project before he left to go to the Gordon and Betty Moore Foundation. Thank you.
The Patient Support Corps: An Innovative Staffing Approach to Support Patients in Shared Decision Making
Dr. Jeffrey Belkora, Ms. Obi-Okoye, and Ms. Zarin-Pass
DR. BELKORA: Thank you. I am Jeff Belkora. I’m with the University of California, San Francisco. And I want to present today on an innovative staffing model for supporting patients in being informed and involved in their treatment decisions. And I do want to acknowledge some funding sources. We don’t have any commercial conflicts of interest to disclose, but the Informed Medical Decisions Foundation has been funding our project since 2004 as a demonstration project. Of course, I also want to thank the organizers of the conference today, the Institute of Medicine, and the sponsors, the Moore Foundation and Blue Shield. And of course the conference staff; thank you for helping us attend here.
And I say “us” because I brought two students—Ekene and Margot are actually going to do the bulk of the presentation. But I do want to just introduce what we’re talking about a little bit, to say that we did start with a needs assessment about 10 years ago in the area of breast cancer, where I was lucky to have a partner, Dr. Laura Esserman, who is a real champion, along with other colleagues at the UCSF Breast Care Center, a real champion of patient-centered care. And they felt like they could be doing more to address particular patient needs. And we focused in on what patients told us in their own words which was that, during that time when they had a diagnosis but they were waiting for an appointment with the specialist, that was a time of real information anxiety. That they were conflicted, they were bombarded with either conflicting information or too much information or they didn’t have enough good information. At the same time, they would be lying in bed at night thinking of issues, but then freeze up when they got to the doctor’s appointment and forget to ask about those very issues that have been keeping them awake at night. And if the doctor did happen to address the questions that they had been concerned about, the information went in one ear and out the other.
So, we were happy to learn of course that there were evidence-based strategies to address these information and communication needs, specifically, many randomized control trials showing the effectiveness of decision aids in orienting patients to an unfamiliar condition in terms of knowledge and other measures. But there are also other “communication aids,” I call them, that would help people with the other concerns, such as making a list of questions. A very simple act of writing things down and bringing that list into the appointment and referring to it, helps people remember, not surprisingly, what they wanted to ask about. As well as after-visit
summaries and recordings, which help people review the information in a more relaxed setting and benefit from repetition.
So, we turned our attention to really asking who can deliver these decision and communication aids in our clinic, and what we found was that we tried initially to get existing staff, for example, schedulers, to really facilitate the use of these tools, but they were already overloaded with their existing tasks. So we then had, and it was really Laura Esserman who said, well, we have these premedical interns who are in our program doing work as program and research assistants on other tasks, but what about if we had them set aside a day each week to accompany patients on their journey and facilitate the use of decision and communication aids.
And so Ekene is today one of these premedical interns. While she is coming up here, I wonder if you could get to your packet and look on the right side and find the next-to-last piece of paper, and I understand for those of you on the Web that this handout is also available to you electronically, but if you can find the one that says Question List. It’s a handout for Patient Support Corps presentation, that’s us. So in my packet it was the next-to-last piece of paper on the right side. And Ekene is going to tell you a little bit more about the program.
MS. OBI-OKOYE: Thank you, Jeff. So, hello. My name is Ekene. I am 1 of the 10 premedical interns at the UCSF Breast Care Center, and I am the Tuesday morning intern, which means that I call all the newly diagnosed breast cancer patients coming in with Tuesday morning appointments.
So, to demonstrate a little bit of our process, I’m going to tell you about my patient Ella. When Ella makes her appointment at the Breast Care Center, she shows up on my call list. So, I call her and I offer our services to her and she accepts. What does that service look like? Well, step one of this process is I have to determine what is the correct decision aid for her. So, during the offering call, we determine that she needs the decision aid on ductal carcinoma in situ, which is pre-cancer, stage-zero cancer, and that looks like this. It’s a booklet and it comes with a DVD.
So, I put that in the mail for her and then in about 3 days, I call her, and we spend about 30 minutes going over her primary concerns, her major pressing questions. And I get them all down on a piece of paper for her, which is step two of the process and that is what you have in front of you. Is everybody looking at it? Underneath the situation heading, you can see that one of her major concerns is that she doesn’t understand why she needs to have surgery if DCIS is a stage-zero cancer. Under the objective section, you can see that she’s also really concerned about working, because she’s a firefighter, and she is also concerned about how she’s going to come out to her kids about her diagnosis. These are all the questions that are her major concerns, and I would like to say that these are her own words. I’ve gotten these words from her using a neutral, nondirective approach in the question listing session, not giving her any of these questions; these are all her questions.
So, I send these to her and then I send this also to her doctor. And then about a few days later, I attend her appointment with her. I have my laptop and my recorder in hand, this is what the recorder looks like, and we wait for the doctor to come in. The surgeon walks in and he has the question list in hand, and he actually uses the question list as the patient agenda for the appointment. So, he uses it to guide how the appointment runs. And I sit there and I take notes and I also record the appointment, which are steps three and four. At the end of the appointment, I produce a CD recording for Ella so that she can take that home and her husband, who couldn’t make it to the appointment, can listen. And the next day I also send her the appointment summary, which is on the back of that handout.
From all of this, after 4 weeks of time has gone by, we send a survey to all the patients who have received this service. And in Ella’s survey she says that she really appreciated having someone there to listen to her and listen for her. And I think that that is really what I’ve taken away from this service—is the ability to listen first and to listen fully, and I truly hope to take that with me as I continue on this path to becoming a doctor. And now to talk a little bit from the perspective of someone down the line, Margot.
MS. ZARIN-PASS: Yes, my name is Margot. I’m a first-year medical student at UCSF, and before that I was a premedical intern like Ekene for 2 years at the Breast Care Center. And what Ekene just told you about her patient Ella being very grateful for our service is a very typical reaction. We have years of qualitative and quantitative survey data from our patients that we’ve published telling us how much they appreciate the service. So, here are some representative quotes about the decision aid. One woman said, “This was exactly the material that I was looking for all over the Web, but having a hard time finding in a consolidated format that made sense.” And about the question list, another patient said, “It was hugely helpful to have my questions prepared beforehand.” Finally, about the recording and summary, “They were invaluable in filling in parts of the conversation that this patient and her family were finding hard to remember.”
So, we know that our service is working well for our patients and we have anecdotal evidence from intern alumni like myself that they are using the skills they got as interns in their medical education and further down the line medical practice. One example of this is a friend of mine named Meredith, she’s in medical school, and she has a class where they learn how to interview patients. So, her day to interview a patient, and the patient walks in, and the first words out of his mouth were “Do you think I’m going to die?” So, she tells me that she froze up for a second, not really knowing what to say. Then she remembered a “Jeffism,” one of the phrases that we’re taught to use with patients. And so she says to this patient, “What is your understanding of your situation?” That allows them from there to have a whole discussion about his recent diagnosis, how he feels about it, his recent hospital stay, and they have a very productive discussion there. And that is the feedback Meredith got from her facilitator and peers who were watching this interaction. That having that sort of opening question in her toolbox allowed that conversation to go so well. And she attributes that to her time in our program where we use that sort of question all the time.
So, Jeff and I got curious—do all of our alumni have this experience? Where they are using the skills they got in our program to this day? So we did a survey this summer of all 47 of our alumni. They are at various stages, and we got 21 responses. Seven of them have completed medical school. Eight are currently in medical school and other stages of the process as well. And here are some sort of typical responses we got. One person said, “Decision Services helped me actually learn the art of listening through practice, patience and silence. I learned to silence my own voice and let the content of the patient and the physician guide my own work.” That’s really echoing what Ekene just said about learning to listen to our patients through our program. We also got a response from someone who is currently a practicing physician saying, “Now, as a doctor, I believe the core values I developed as a premedical intern are still there: a nonjudgmental attitude, a careful approach to humor, and an avoidance of saying things that I truly can’t control, like everything is going to be okay.”
What this is getting into is, Ekene made reference to our neutral and nondirective style of interviewing our patients, and as premedical interns, we’re not giving advice to our patients. We’re not answering their questions because we’re not qualified to be doing that. So, we’re very
conscientious about how we talk to patients in this role. And this person is saying that they are taking those skills they learned about conscientious communication forward with them through their medical training and into practice. And so that was very gratifying for us to see, that we knew this program was a win for our patients. We now know it’s sort of a win for our intern alumni and Jeff’s going to talk about how we can expand it.
DR. BELKORA: Thanks, Margot. We do feel fortified in our motivation to expand this program, given the successes we’ve had with patients and then also the educational trajectory that we’re putting premedical students on. There is a question about these paid staff interns. So how do we expand this program and keep things somewhat affordable? We’d like to get beyond the Breast Care Center to other clinics. We’d like to get beyond our institution.
So, we looked across the Bay. At UCSF we don’t have an undergraduate patient population, but we realized across the Bay in Berkeley, there are 30,000 undergraduates and about 3,000 of them at any given time are premedical students. So, we decided that we would look to a volunteer workforce to extend our coaching capacity, again moving out from the Breast Care Center into other clinics. And actually Lindsey Forbes is here, who is one of the first Berkeley students, and is now working at Johns Hopkins, so our alumni are spreading all over the place.
But Lindsey and her peers are coming over now and working in our orthopedics clinic, in the urology clinic, in the spine center, and in head and neck cancer. And that’s just in the first year really of the program as we’ve been expanding. So, we feel good about the possibility of expanding this into what we’re calling the Patient Support Corps, using kind of the metaphor of a service learning program. The students, or possibly other volunteers, get academic credit or get other benefits and the mission really is to provide this workforce as coaches for patients and families, so that the patients and families can be as informed and involved as they want to be.
So, this has been working well and, in fact, the program has now been replicated at Dartmouth. And at Dartmouth they’ve said, well, let’s not just use undergraduates. Let’s also use public health students, also MPH candidates and medical students. So, we’re quite optimistic about the potential for this program to expand. And of course in the days of telemedicine, it would be possible to deliver these kinds of services at least in part remotely. So, I work in rural areas in Northern California as well, and we definitely want to be able to reach people and help them with question listing and even attend their appointment if necessary by speakerphone and take notes for them and do all those sorts of things. It’s all possible now, I think with technology.
But the value proposition overall for the Patient Support Corps, I have high hopes that we can make this sustainable in the sense that clinics should be willing to put some money on the table to support the administration, the training, and supervision of the volunteer workforce. And also the academic institutions, colleges, and such should also be willing to put some money on the table, I hope, because they’re getting tuition and they should be diverting some of that for this kind of service learning experience.
So, we’re cautiously optimistic that this can in fact scale and be sustainable because of these kind of win-win benefits for, ultimately for patients, but then also for students. We’re right now in the very beginning of what we hope will be a 3-year startup period, recruiting other members to the network, we feel like we have UCSF on the West Coast, Dartmouth on the East Coast, let’s fill in the rest of the country now. And we want to refine our service and product offerings and refine the business model. And frankly, we’re looking for funding and other partners so this seems like a good audience for me to do a little bit of networking in. And I consider myself a mentor for Ekene and Margot, and I told them that when we come on a trip like this we’re not
allowed to have dinner together, so we’re going to be looking for ways to network with you all and please come find us and talk to us.
Of course, we’ll also be on the panel now. So thank you very much and thanks again to Margot and Ekene for coming out.
Implementing Decision Aids for Increased Patient Engagement and Reduced Costs
Dr. David Arterburn
DR. ARTERBURN: Good afternoon. It is a pleasure to be here. I’m David Arterburn from Group Health Research Institute in Seattle, and I’ll be talking with you today about our work and our story behind implementing patient decision aids to improve patient engagement and to reduce costs.
First, with a financial disclosure, that I have received research funding and salary support from the Informed Medical Decisions Foundation and serve as a medical editor for the foundation in developing their bariatric surgery decision aid. The Informed Medical Decisions Foundation, in partnership with their for-profit partner Health Dialogue, produced the decision aids that we’ll be talking about today.
First, sticking with the themes for this session, I want to talk about our pathway toward shared decision making, and really there were two routes that really drove us that way, beginning with an overview of who we are. Group Health is a consumer-governed, nonprofit health care system that integrates care and health care coverage for over 600,000 Washington State residents and also some residents of Northern Idaho. That’s about 1 in 10 patients in Washington State who get their care through Group Health. We have both salaried providers through which two-thirds of our patients receive their care, and a network of contracted providers.
Group Health was motivated by two things, as I mentioned. One was unwarranted variation, and I think you’re all very familiar with Dartmouth Atlas and Group Health was very familiar with that work as well. But there had been 20 years of complacency around that, because we believe within our own system that we really didn’t have unwarranted variation, until we actually did the analyses of our data and found, as this graph showed, that three of the regions in Group Health, the solid lines, had very different rates of knee replacement (see Figure 2-6). And that they differed actually from what the state and regional averages or rates of knee replacement were in the state, here in the dotted lines, and then with the Group Health regions in the solid lines, we had very different regional rates of knee replacement.
So, although the patients we felt were the same, providers were all salaried, we had very different rates of knee replacement, which suggested unwarranted variation that wasn’t in alignment with patient preferences, but may be more likely to be driven by surgeons’ opinions about treatment practices.
Another key influence here of shared decision making is that Washington State in 2007 passed legislation which recognized shared decision making and the use of it along with the high quality patient decision aid as the highest standard of informed consent for patients in Washington State. It also mandated, but did not fund, the State Health Care Authority to implement shared decision making demonstration projects, and Group Health was one of the sites that took that challenge on. And that’s what I’m talking about today.
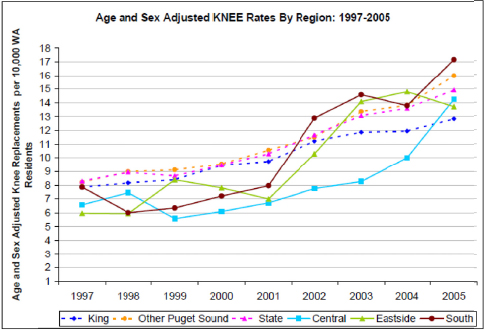
FIGURE 2-6 Group Health rates of surgical procedures rising.
SOURCE: Reprinted with Permission of David Arterburn, Group Health Research Institute.
In 2012, Washington State updated their legislation, giving the Health Care Authority the power to certify high-quality decision aids for use in Washington State. So, what were the infrastructure elements that we put in place to support shared decision making at Group Health? Well, it was a system-wide implementation with video-based patient decision aids, which you’ve heard about previously by Jeff and his team. There were 12 preference-sensitive health conditions that we targeted related to elective surgeries and they are listed all here (see Box 2-6). I won’t go through them all, but there are six different specialty service lines throughout Western Washington where we’re working with different specialty clinics and different specialty providers in Tacoma, in Olympia, in Group Health, in Seattle and in Bellevue.
We gave providers access to these patient decision aids through our electronic medical record, which was EpicCare. They could just type in SDM, shared decision making, into the order field, and it would pop up a list of all the different decision aids that they could order. They could then place the order, and that order would be routed to the patient’s home through the mail where they could watch it with the patient with their family members. Patients could also be routed to watch the video online, so they could go onto our secure patient portal and watch these streaming videos. You can see that many of them actually are quite long, up to 50 minutes in many cases, but patients didn’t complain about the length. These are treatment decisions that they were facing. And so we had many patients, one-quarter of our patients viewed decision aids online.
For providers, we also provided smart phrases. These are Epic tools which allow them to more easily document that they had referred a patient to a patient decision aid, or once they have actually referred them and they are seeing them back or having a conversation about the patient decision aid and the patient’s treatment options, could more easily document that they discussed the content, documented their treatment preferences, and where they are going with their treatment services.
BOX 2-6
Physician Communication Competencies
- Orthopedic Surgery
- Hip Osteoarthritis
- Knee Osteoarthritis
- Cardiology
- Coronary Artery Disease
- Urology
- Benign Prostatic Hyperplasia
- Prostate Cancer
- Women’s Health
- Uterine Fibroids
- Abnormal Uterine Bleeding
- Breast Cancer – General Surgery
- Early Stage Breast Cancer
- Breast Reconstruction
- Ductal Carcinoma In Situ
- Neurosurgery
- Spinal Stenosis
- Herniated Disc
SOURCE: Reprinted with permission from David Arterburn, Group Health Research Institute.
Another key piece of this implementation package was project managers, who were critical. Three FTEs of staff are working with these clinics on the frontline during our first year of implementation doing a plan/do/check/act process of working with providers and quality improvement in an ongoing way to meet the needs of the different providers. The endpoint there is ongoing quality improvement initiative, a PDCA process. And these project managers were critical throughout the process to understand the workflows and to get the decision aids in practice, because each practice had different workflows and work styles. This work with project managers led to streamlining of the process for pre, during, and post visit care, which dramatically influenced the rates of decision aid delivery.
But how did group health create a culture of expectation around shared decision making with providers and begin to build competencies for providers, which is work that we’re doing? Most providers have this attitude when we first talk to them: I already do shared decision making. But we realize that that probably looks like this: Of course, it’s totally up to you but if it was up to me I’d choose to have the surgery. And this is the attitude that most providers actually had toward shared decision making when we first began talking with them about it.
But GroupHealth leaders really wanted to set a different tone. And it was not, “This is nice to do if you have the time and the inclination,” but is more toward, no patient should undergo a preference-sensitive procedure without documented evidence that they got all the information they needed and had a conversation with their provider in which their preferences were documented before they made their decision. Among the key steps that were required to initiate this culture change was requiring all the providers in specialty care to review the patient decision aids that their patients were going to watch. Also, within the second year, we had a half-day CME where we pulled all the specialty providers and the surgeons out of clinical practice and had them work with outside experts on training around shared decision making. We provided them monthly feedback on volume of decision aids ordered, number of surgical procedures, the total cost that those surgical procedures added up to, and the number or percent of patients who had a preference-sensitive surgery who had not watched a decision aid.
But perhaps most importantly for culture change, patient satisfaction data really influenced provider opinion about these decision aids, and I’ll present some data about that a bit later. We told providers that we expected that these decision aids would improve patient knowledge, that it would improve their satisfaction with care. It would help us understand what is the real rate of demand for these procedures, and would probably reduce unwarranted variation in our care. But most importantly, we told our providers that we thought this was a question of patient safety. It’s not wrong-site surgery that we’re worried about, it is wrong-patient surgery that we’re worried about; where uninformed patients making decisions about surgery, it’s wrong patient surgery.
What were the outcomes that we observed throughout our process? Well, now 4 years into implementing this work, we’ve delivered over 31,000 patient decision aids in these 12 different elective surgical procedure areas, as of January 2013. Over time, we have dramatically reduced our defect measure, which means we have fewer missed opportunities for patients to receive a decision aid prior to going to elective surgery. This graph shows that at the beginning, 100 percent of our patients were going on to surgery without receiving a decision aid. Now, we’re down to about 35 percent of our patients, and these are in the areas of hips, knees, low back, hysterectomy, and benign prostatectomy, in terms of the proportion of patients getting surgery who have not had an opportunity to view a decision aid. We’re not all the way to 100 percent but we’ve made dramatic improvements over time.
We surveyed patients in the first year and this, again, influenced providers dramatically—96 percent of our patients said that these videos were very good, excellent, or good, at helping them understand their treatment choices. And 95 percent of them said that these were very good, good, or excellent, in helping them prepare to talk with their provider. And we documented outcomes with help from the Commonwealth Fund to fund an evaluation of this. We showed that implementing patient decision aids was associated with sharply lower hip and knee surgery rates and costs. Where we had 26 percent fewer hip replacement surgeries, 38 percent fewer knee replacements, and 12 to 21 percent lower costs of care for these health conditions over 6 months. We’ve seen similar reductions in rates of surgery in areas related to women’s health, abnormal uterine bleeding, and uterine fibroids, as well as in BPH and prostate cancer. The impact on costs of care has varied by the health condition but overall, we’ve seen consistent reductions in rates of surgery. In the case of knee and hip osteoarthritis, we’re saving on average roughly about $3,000 per hip OA, and $2,000 on knee OA per patient within the population.
So, overall our conclusions as a result of this work are that large scale implementation of patient decision aids is feasible in the scale of an organization like Group Health. And that shared decision making really appears to be headed toward achieving the triple aim of health
care, where we are getting higher patient satisfaction, lower costs of care, and improving patient quality through improved knowledge.
Our next steps are to add five to seven new decision aids in this year, five we’ve already committed to, two more that we’re considering and two key elements that are very patient centered. One is that we’re moving this conversation upstream from specialty into primary care, and having conversations and decision aid ordering being centered there for most of these health conditions. And the second key thing is that we’re automating recording of patients’ knowledge, their values, and their treatment choices in the electronic medical record; they can complete this information online and it goes into electronic medical record, where the provider can access it at the point of care and have a more engaged discussion with the patient about their treatment choices.
I want to acknowledge the funders as well as the many collaborators and clinicians that were involved in the work to actually get this work done and the slew of external advisors as well. And thank you very much for your time and the opportunity to present.
Audience Participation and Open Discussion
MS. PAGET: Thank you all very much. So, now is the time for you all to think about what you want to contribute to this dialogue. What kinds of questions you want to ask and while you’re thinking about that, I have a question for any and all of you.
Clearly there’s a role here for leadership and there’s a role here for system support, infrastructural support. You all are several years into what you’re doing. As you reflect back, is there anything—I’m seeing Jeff as kind of a clinical champion—is there anything that you think might have made things easier or is there anything that, as you reflect upon it, would make other institutions’ process smoother in knowing what you know, because now you’ve got multiple years of experience? David, you want to start with that?
DR. ARTERBURN: Sure. I think the key thing that comes to mind for me is that having a partnership with the Informed Medical Decisions Foundation was really critical from the outset, because having expertise in how you do shared decision making and being able to bring that to Group Health, an organization that actually valued all these things, patient education and higher quality of care, they really understood unwarranted variation. But they really didn’t have a clue how to actually get shared decision making into practice, and drawing on the resources of the Foundation and others like them, and me being able to play a role in helping translate that into the system was critical, I think.
DR. BELKORA: Well, I don’t want to belabor it too much, but having a workforce, so we had the clinical champion, but then having coaches. And so if you can afford it on a staff basis, and I think as we’re moving toward accountable care partnerships at our institution, I’m starting to see real investment, as opposed to, I think in the past fee-for-service organizations have been a little bit reactive, like the clock starts ticking when the patient shows up for a visit.
Now, we’re investing in nurse outreach and other kinds of outreach to patients well before a visit and follow up afterwards. So, I think coaching and the kind of human element at the right level, doesn’t need to be necessarily a very highly licensed person, it can be a trainee or someone somewhere in between, that would be the other key element I would point to.
MS. PAGET: Grace, what would you do differently if you had to do it all over again?
DR. LIN: That is a good question, Lyn. I think one of the things that we really underestimated was the amount of manpower and amount of time that this was going to take. We
were very optimistic, as everybody is at the beginning of projects, saying, “This is going to be great. We have a good champion. We have willing patients.” And really what we found was that the steps needed to change the culture first of all take a long time, but also take a lot of sustained effort from the top down and the bottom up. The patients need to push. But also the organizational leadership needs to be there to lead the change.
MR. CLIFFORD: My name is Dave Clifford. I’m a consultant to PatientsLikeMe as well as a number of other organizations. I tend to think about these things from a policy perspective, which is somewhat different. And, looking for a solution in this framing, I think that one of the things discussed was the very positive impact of using people who had planned on becoming doctors both on outcomes in the clinic, as well as professional outcomes. Would there be any way for an organization such as the American Association of Medical Colleges to start thinking about using these sorts of experiences as a criteria or bonus points for getting into some of the higher level medical schools? To me, that seems like an implementable pathway, especially as we’re reconsidering what the MCATS should look like in the future. Thanks.
MS. DAY: My name is Nancy and I’m from the State of Maine, too. And I would like to help you get into the only medical school we have in Maine. We only have one, so we can go to 100 percent quickly.
The second thing I wanted to ask David was, I have been doing some work to embed shared decision making into a new kind of value-based insurance plan. And as I talk to consumers about shared decision making, the module that seemed to resonate best with them was the one on colon cancer screening, and I was wondering why that wasn’t one of the modules that you incorporate now. They seem to love to know there are choices.
DR. ARTERBURN: That has to do with a cultural timing issue, where we had an opportunity to really engage our specialty care providers, so the specialty care providers were taking ownership over these elective surgical procedures, and our state legislation actually specifically called out elective surgery as being a high-variation and high-cost concern. So, we were focusing in specialty care for that reason. Now, we’re moving toward primary care, and there are many more opportunities there, and many of the treatment decisions that we’re talking about will include those in the future. So we’re moving toward primary care.
MS. RICCIARDI: My name is Lygeia Ricciardi. I’m with the Office of the National Coordinator for Health IT, and I wanted to make a couple of comments that I think are relevant, not only to this panel but to some other discussion earlier this morning.
There is a lot of discussion about the important role that technology can play, could play, should play in enabling real patient engagement and shared decision making. There was a comment earlier this morning about whether we should have a right as patients and consumers to have access to our information. That right exists already under the HIPAA privacy rule, but many people are not aware of that. As we bring the health system increasingly from a paper-based one to an electronically based one, it becomes easier to access that right. And specifically through something we call Blue Button. We’re enabling patients to access their records directly themselves in electronic format, which again is a given right.
Under the program that we’re rolling out right now, called Meaningful Use, which is a large incentive program, we are requiring participating providers and health care hospitals to provide patients access to visit summaries, so that they know what’s going on when they have an interaction with the health care system as well as educational materials. And in the current stage, which is now currently rolling out, we’re requiring patients to be able to view, download, and access their health care information electronically, which is a big deal. So by this fall and next
January, any patient who sees a provider who participates in this program will have that ability, and I think that will really free up a lot of opportunities for exchange of information.
MS. PAGET: Lygeia, could you comment a little bit on what the picture is going to be for assessing the patient’s access and ability and success in doing so? I hear from a lot of folks, “My pediatrician has introduced a patient portal, but it’s not meaningful for me in my needs.” What is the office’s plan—what are we going to learn?
MS. RICCIARDI: That is a great question. One of the things we have done is to build into this Stage Two requirement that patients be able to view, download, and transmit their information to actual thresholds to show that patients are actually doing so. So, 5 percent, and I know that that isn’t an incredibly high number, but 5 percent of patients must actually have taken advantage of these services. Which we’re thinking will really encourage providers to have a conversation, not just to turn on this functionality and say nothing about it, but to really start that conversation.
I also want to mention that we have a pledge program, called the Blue Button Pledge Program, through which we’re working with providers, but also payor organizations, to encourage people to provide digital access to health information to consumers and to start having these conversations, so patients can really be partners in their care, and we’re providing a lot of materials that providers and others can use.
MS. PAGET: Thank you. So that is the second pledge program we’ve heard about today. We might need to think about unifying our pledges in some way. Matthew.
DR. WYNIA: Hi, I am Matt Wynia. I’m with the American Medical Association. I’m the Director of Physician and Patient Engagement for the Improving Health Outcomes team and I just could not be more enthusiastic about the panel. Both this afternoon, but to me this really dovetailed nicely with where we were heading this morning.
So the issue I want to try and raise is to bring together I think, some of what David started to get at, in going into primary care. And some of what the program, well, to a certain extent both PAMF and UCSF are doing in terms of—one of the challenges or limitations of decision aids as we currently know them is that they are all about making a discrete decision around a preference-sensitive point in time, and so it’s a little bit like taking a class. And when you’re done with the class, you move on, and hopefully it made a big difference in your life, but you’re going to continue in most instances, for my patients at least, to be managing the condition that you’ve got. It’s not a one-time decision.
I’m an infectious disease doctor. Most of my patients have AIDS. There isn’t a great decision aid out there for me. Because I’m probably making, I’m going to say 50 decisions in an average patient encounter, and none of them are entirely discrete or they are rarely entirely discrete. This is about managing a condition over a long period of time, and my patients don’t need a single decision aid. It’s not a class. They need course work that lasts for weeks, months; this should look in my view something more like the diabetes prevention program or lifestyle coaching.
And that’s where I’m so happy to hear what you guys are doing in terms of that. Because I think breast cancer can be analogous to HIV infection. It can be a chronic condition that you manage for some period of time, not always, but it can be. And I’m wondering whether there is more thinking around moving this sort of discrete point-in-time decision aid philosophy back a step, toward managing conditions over a long period of time that are not so much a single preference-sensitive point in time, but a series of decisions that you have to make at home all the time about whether to eat this or that, whether to exercise now or later, whether to take my meds, whether to take a break, whether to trade off; the things that our patients talk to us about in terms
of the actual life situations that make it hard for them to do what they often know to be the right thing, sometimes don’t know to be the right thing.
MS. PAGET: David, do you want to speak? Or should we, we also have Michael Barry next at the mic, so we could actually have Michael talk about that, too.
DR. ARTERBURN: There are decision aids that help—so there’s Living Well with Chronic Disease. There are decision aids that can help prepare patients to understand key management philosophies about managing their diabetes, managing their depression, managing their anxiety over the long term. And also I note in our knee osteoarthritis cohort, many patients get these decision aids more than once, because they are coming back to see the orthopedic provider and the first time they said no, now they are thinking about it again.
So I agree with you, there are many opportunities here. We can’t have decision aids to support all of them per se, but more of a culture change around providers and patients’ expectations and the way they use information at the point of care.
DR. BARRY: Just on that point, in my own practice, where we can electronically prescribe decision aids, I just had a woman who I had prescribed a colorectal cancer screening decision aid a couple years ago, and we talked through it; then [she] comes in with her hip bothering her progressively [and] said, “Gee, do you have something about that?”
That’s the kind of culture change. Now, how much of that we can do outside the context of decisions they are facing, the general education Sherrie talked about; or do we do it in the context of, if you will, earlier decisions, like about screening that first medicine you take, maternity decisions, and then norm people up for the big problems later with heart disease and cancer and other things? So it is a long haul and I think figuring out how to change the culture is what it’s about.
I’ll just come back to a question around the aligning incentives. Because at GroupHealth, although it doesn’t make it easy, there are aligned financial incentives, and maybe we’re moving in that direction with the ACO movement. There’s a lot of fee-for-service medicine out there and even how clinicians are paid under an ACO umbrella may be some component of piecework there. Grace had mentioned that one of her successful interventions with a group visit was being able to bill a 99213, and as a primary care doctor we think about that all the time. People worry about, “Gee, why should we have to pay clinicians to do the right thing?” But since we’re comfortable with sometimes paying clinicians to do the wrong thing, I’m okay with it.
As an example, I just got a memo from my own physicians’ organization that to get billing a 99214—really the pot of gold at the end of the rainbow—in order to do the detailed exam that’s part of that, it was no longer sufficient to examine two or more organ parts, you had to examine five or more organ parts. I had missed the randomized trial that showed if you examined five organ parts people were happier and healthier. But it strikes me, could we just move that to saying that if we could check the six steps of decision making, we’re now developing metrics, were patients informed, did someone ask—could we move the reimbursement from doing things that clearly don’t work, or more the tradition-based medicine, to now, with 86 randomized trials of shared decision making and more on the way with Cochran, to really shaping how care is paid for, to things that do make a difference?
MS. PAGET: That’s a nice vision. Val, do we have something from the radio audience?
MS. ROHRBACH: Yes, two questions. The first from Kevin Kenward of the Health Research and Educational Trust. Kevin asks, “How can costs be inducted in shared decision making when physicians don’t always know what the costs of a treatment or medication or procedure are?”
The next question is from David at Johns Hopkins, who asks, “Our doctor friends all tell us they don’t have time during the brief time they have during a patient visit for the kind of patient engagement being discussed today. How does the panel respond to that?”
MS. PAGET: Let’s take the time question first. I believe there are some data out there that are pretty much indicating that that’s not an issue, but who wants to speak to that?
DR. LIN: I can start. We actually heard that a lot. We surveyed our physicians at the beginning of the project, and a lot of them said actually what David’s physician said, “We’re already doing shared decision making, but even if we aren’t, we don’t have time to do it.” When we went back and we did focus groups with the physicians later on, the ones that had actually utilized decision aids—we actually held focus groups with physicians who were high utilizers and those who are low utilizers. What the high utilizers said in large part was, “You know the decision aids saved me time. The patients came in with better questions, they had a knowledge base, I could have a better conversation with them,” so really I think this whole notion—I think once the physicians had the experience they no longer thought that shared decision making took too much time.
DR. ARTERBURN: Our experience at Group Health paralleled what Grace found, it was that the providers didn’t think this took more time and the patients actually were just better educated and had better questions.
MS. PAGET: Thank you. The cost issue, if I’m understanding it correctly, is kind of how to build that in, and this comes up a lot because we have such variance in costs in this country, and I know that from the perspective of the developers of tools, it’s all been very challenging to address the cost issue in that. And then costs in general is a very broad category because there’s financial costs, there’s also quality of life costs, and so forth.
But I wonder if any of you, and maybe Jeff from the breast cancer program, what do you find that is important to patients; does that come up, when the interns are soliciting questions from patiens?
DR. BELKORA: We keep track—we keep copies, deidentified copies of all the question lists that patients have and you know, we have looked at them to see what kind of recurring themes come up and in the area of costs, there is a concern. And we see it reflected in the question list about out-of-pocket costs and that sort of thing. I think the question was about financial cost; clearly patients also have a lot of questions about the costs in terms of their time and attention and quality of life and other issues. So, I have to say though that we’re treating an insured population in this Breast Care Center, and so perhaps it’s just not quite as salient and not as reflected in our question list as it will be when we are spreading this model much more broadly. And I think we need to point to the Choosing Wisely program and other kinds of initiatives to say this is a really big deal that we need to get our hands around.
MS. PAGET: I know we are going to spend some time tomorrow on this topic as well.
MR. ROEHR: Hi, I am Bob Roehr. I’m here today as a journalist. I’m writing for BMJ. I’m also drawing upon my experience as a patient activist on a couple of advisory committees at NIH, going back to HIV activism and things like that. And what I’ve heard today basically has been sort of a just-in-time education involvement, decision-making type thing, which is well and good as far as it goes, but I think there really needs to be a more fundamental look at educating the general American public to their obligations, in many ways, as citizens to participate in this.
You can say that when most of our health care structures were created, health care was 3, 4, maybe 5 percent of our GDP; today, it’s almost 18 percent. Nobody believes it’s ever going to shrink; it’s going to continue to grow. It’s only a question of at what rate. And when they were
created, interventions were primarily for acute conditions. Now it’s predominately chronic conditions, so the role of the person is changing, the role of the patient is changing, and we have to, I think, as citizens, understand this and begin to educate our people at the primary level of their role as good citizens in taking care of their own health and participating in the health care process.
There’s one model that has been developed at STEM, education, science, technology, engineering, and mathematics, which I think could be very much of a model to build upon though. That’s aimed at primarily college-aged people but we could start there and move back downstream.
I think it’s very important to do more than simply train people to respond to the immediate decision. We have to make the framework and the education broader than that.
MS. BROWN-TATUM: Good afternoon, I am Crystal Brown-Tatum. I’m the founder of Sisters Network, Shreveport. We’re an affiliate chapter of Sisters Network, Inc., which is the only national African American breast cancer survivorship organization in the United States.
And my question is, I used to be on the Board of Susan G. Koman, and we funded a patient navigator at LSU Shreveport Hospital and it was, in my opinion, a dynamic opportunity for a nurse practitioner or PA. And after the first year of implementing the navigator, the grant was not renewed with the Northwest Louisiana affiliate, and she just went away. And based on my own horrific experience as a breast cancer patient and working with some of the most underserved women in the breast cancer arena, that patient navigator role was critical because LSU had a dynamic rate. If a woman was diagnosed with breast cancer, she was having surgery within 48 hours.
On my own journey, I had a 4-month gap in treatment from diagnosis to chemo, because I wanted to keep my hair over the summer, I didn’t know any better. I didn’t have anybody that was a champion for me. I just was very uneducated and ignorant and I just thought, oh, I’ll just start treatment in 4 months.
So, my question is, the decision-making aids, can those replace the patient navigator role or do you feel that they strengthen the patient navigator role? If the hospital or clinic doesn’t have someone that’s serving as a navigator, are those tools going to be enough to possibly fill the gap that may exist because the role’s not there?
MS. PAGET: Crystal, can I ask you for clarification here, is this kind of coming from a resource issue, saying if there’s not funding for a navigator, can the tools stand alone?
MS. BROWN-TATUM: Yes.
MS. PAGET: What do you think, Jeff and your team?
DR. BELKORA: Well, Harold Freeman and others who have kind of defined this field of navigation have begun to just define it as helping patients overcome barriers whatever they are, and so some of the barriers are logistical access to care. Some of them are emotional support and other forms of support, and we focused in this decision-making area on the kind of cognitive information processing and decision-making issues.
So, I would say is it one or the other, I think they’re complementary. A navigator that’s sort of high-touch facilitation and coaching that my team provides is very complementary with the written materials. In the decision-making arena, this all boils down to critical reflection, to getting people to think and process, and so that doesn’t just happen one way or the other, it happens through multiple kinds of modalities. I think you could prioritize depending on your population and the needs. In some populations, it might make more sense to invest in patient navigators who are trying to get people access to this system, and if that’s the biggest barrier—I
mean I guess I would just start with sort of the biggest barriers and design the program around the local need, but I think there’s room for really both.
MS. DAY: I’m just going to talk about when I finished up with my treatment, after I had my surgery, at my post-op recheck. I volunteered as a patient, actually said to my doctor, “Is there anything I can help you with?” because I was just so relieved to be over with my treatment, and she looked at me like I had two heads.
I wondered if you considered recruiting experienced patients to do some of this work; this would be for Jeffrey and the other groups, maybe would be nurses would get a great deal of experience from this. Pharmacologists and social workers would all gain from this type of experience too.
I have one more question. The other question I had is for David. What do you think about advertising for joint replacements and pelvic floor problems and that sort of thing? There’s been a very creative advertisement in my local newspaper with a long full newspaper page length ad with a roll of toilet paper on it, and Consumers Union just recently used that as, what is this ad selling? It seems to me that that kind of advertising would increase procedures rather than decrease, which is when you’re educating and engaging the patients, actually the procedures are going down so I wondered what your comment might be on that.
DR. ARTERBURN: I do think they are potentially competing. I think it depends on the way in which the advertisements are being done. But I think in most cases, in our region in Seattle, we have other partners that are advertising for hip and knee replacement products. And Group Health is taking a different approach, and I think it’s one that’s innovative, and we’re eager to partner with other organizations to help try to do that even within our own community, to help translate the kind of shared decision making approach that we can, because many of our patients in outlying community areas see network providers who are in a fee-for-service setting and have the same sort of financial incentives to do the kinds of procedures and to advertise for the types of procedures. We really want shared decision making to be the norm for all our patients and it is a different approach than the advertising approach.
MS. PAGET: Jeff, do you want to speak to the first question?
DR. BELKORA: Absolutely. We have used pure volunteers already. Survivors of conditions who have either volunteered or been paid to accompany patients and do similar tasks as Ekene and Margot. And I think that is also a potentially kind of sustainable model.
So, yes on that one, and I think there was a second component for question—other professionals, right. So I think yes, absolutely the practicum experience as a social worker or as a psychologist or as a nursing student; we’re using premedical students, but we’ve had experience with students who’ve gone on to other professional schools. So yes, I’m very much in favor of that.
MS. PAGET: Thank you, and we are now kind of getting close to wrap-up time, so I see we have three people, we won’t make you sit down.
DR. MANTEUFFEL: I am Brigitte Manteuffel. I represent the Children’s Mental Health Network at this meeting. I wanted to talk a little bit about SAMHSA’s System of Care Initiative, the Children’s Mental Health Initiative, and that history because it’s very much related to this discussion. That initiative has been funded for the last 20 years to change the way interagency collaboration and family involvement and cultural competence and other factors are addressed in changing how systems that support the mental health needs of children with serious emotional disturbance and their families operate, so that their experience is less fragmented and so that they have the support that they need to actually keep their children in their home and keep their
families together and get their children care that actually helps them improve outcomes and gets them stabilized.
One thing that has been very important in that process has been the family involvement factor. And I evaluated the program for 13 years, and one of the things that have evolved over that time is some of the language. So, the language moved originally from family-focused to family involvement, and then a decision was made to move that language to family-driven, so that the level of engagement with the family was taken from a much more passive stance to a much more active stance. And that’s been very important in driving that agenda to make sure that you move to a position of equal partnership.
Over the past 10 years we’ve also seen that change with youth involvement. There was a lot of resistance to involving youth in the decision making about their mental health care in the early days, when there was a greater push to youth involvement. But over that time, the program has changed its language, so that it equally represents family and youth in terms of the shared decision making process, with providers, and the acceptance of youth as partners in decision making has moved ahead by light years really, just by integrating families and youth into meetings and integrating their voice and by moving that process along.
One of the things that we’ve learned through the evaluation around family involvement is that communities implement as they want to roll out their grants. And there’s a lot of variability in terms of how those models look, and they can range from education to advocacy and some combination in between. So, models like yours and models like patient navigator models and so forth, they run a spectrum. But in the recent few years, there’s been a greater emphasis in trying to understand what the core elements are, and to understand how you can do that in a more organized and sort of data-driven approach to being able to understand what those core competencies are, and then also build a licensing requirement, so that that can also become a reimbursable service; some states have been able to make that a reimbursable service for children’s mental health. So, I think there’s a lot to be learned across programs, and I know how difficult it sometimes is for the mental health community and the physical health community to have time for dialogue, so I wanted to share that with you.
MS. PAGET: Thank you very much, that’s really, really helpful.
MS. KORNBLAU: I just wanted to bring up again—this is Barbara Kornblau from the Society for Participatory Medicine—the importance of the patient. I hear people talking about the patient as a coach, a navigator, fulfilling the role, but I hear it sort of as an afterthought and I think that I—I haven’t had breast cancer but I have two best friends who have and it looks to me like a fraternity. And they go out of their way to volunteer to help other women with breast cancer, and I see that in other chronic conditions as well, and I think that we need to harness that power because those patients have been through it, they know it, they know more about it than many providers to. They know what to look for.
I have a colleague who had a liver transplant, and part of her treatment is to look at lab results and tell the doctor when lab results go at certain levels. So I think that we need to harness the power of patients as equal partners in this to be the coaches. I appreciate medical students, and I think you are all learning a lot and students in physical therapy, occupational therapy, nursing, all of the allied health professions, but I think that we can’t underestimate that role of the empowered patient, the knowledgeable patient who has been through it. And it also gives an extra sense to the person who is now going through it, because there’s that camaraderie, that fraternity.
MS. PAGET: Thank you very much. Really important message. I just want to say thank you for Grace, Jeff, and Ekene, Margot, and David for traveling all this way and for sharing your experience with us. And this has been a real pleasure and rewarding for me to be a moderator today for all of these sessions, and I’ve thoroughly enjoyed hearing all of the comments and suggestions and ideas from our audience here and online, so thank you very much for the opportunity and I think—Christine.
SUMMARY AND PREVIEW OF NEXT DAY
Ms. Christine Bechtel
MS. BECHTEL: So, this won’t take terribly long. I could take all day, but I won’t because I’m actually eager to get back here for tomorrow. This is exciting stuff.
So, first I want to thank all of our panelists from both panels today again, and also just say what a terrific job Lyn did in moderating, but I also want to thank you guys, the audience, for being really engaged and really dynamic throughout this day. I think we had a great day, we heard a lot about partnership, beginning with Jonathan Welch, who shared with us a really sobering story about what happens when we fail to listen to patients and families, let alone engage with them. But he also gave us some concrete ideas for the ways that we might engage in actually redesigning the system. We heard a lot about culture change and the need for culture change, and that we can’t get to genuine engagement without that kind of culture change, and when we talked, I think those threads were throughout.
But when we talked about shared decision making, I heard a number of key things that would help us accelerate our progress on the pathway. One being leadership, two being a workforce, and three also being competency, and I think we heard that in two different ways. One was competency among clinicians, and the first of all belief, maybe it’s physician activation, that patients should be involved in their own decision making, that families are actually members of the care team and play an important role. We also heard about competency for patients though, and we heard both in the sense of coaching and having the skills and the confidence and the ability to really engage in their own care.
But I think we also heard a lot about, and I’m not sure this is the right phrase, it’s sort of this chicken and egg theme that I keep hearing, which is one dimension of yes, we need activated and engaged patients. But then there’s the other dimension of the brick wall they can run into in a health care system that is uninviting and unwelcoming in many examples to patients and families who have that desire to be involved. And we heard a lot of examples of that today, and so I think that again points us back to the need to change culture.
I think another observation that I would make is we had some examples where, once somebody got experience in doing something, whether it was shared decision making or maybe engaging patients and families in redesign, their resistance began to melt away and the culture began to change. So I think the question coming into tomorrow will be, how do we think about patients in doing just that, patients as the greatest untapped resource in health care? I heard them described today as a new data stream. How do we harness their power, as Barbara just said to us?
So with that, tomorrow we’re going to tackle issues of engagement in the research enterprise. And how we engage patients as partners in generating the knowledge that we need to actually improve care on a population level. We’re also going to dive into how we can engage consumers
in a different discussion around costs and quality; again we heard that previewed today. We’re also going to hear from David Goldhill, who is CEO of the Game Show Network, and I don’t think he’s going to tell us how to do game shows, as much as I would like that, I do love Plinko and The Price is Right. However, he is going to, again, kind of coming back to our theme of, “let’s start with the patient and family members,” he’s going to share his experience with the health care system, and it will be riveting so we’re looking forward to that.
Breakfast is at 7:30 tomorrow; we’re going to start at 8:00. We will have coffee, gallons and loads of it. And we will be done by 4:30, so please join me again in thanking all of our terrific speakers from today.






























































