3
Proceedings
Day 2
February 26, 2013
WELCOME, BRIEF AGENDA OVERVIEW
Ms. Christine Bechtel
MS. BECHTEL: Welcome back. Hopefully, you have consumed enough coffee. A very exciting day that we have ahead of us. We have a really great lineup of topics and speakers and interesting points to engage with you guys. We are actually going to start the day focusing with this illustrious panel on patient and family engagement in what we have called knowledge generation for care improvement, a.k.a. research.
We are going to then move into a discussion led by John Santa, where we will talk about how we might change expectations around cost and quality for consumers. There has been a lot of discussion about that over the last couple of weeks. In particular, many of you probably saw Pauline Chen’s blog. I think it was yesterday or the day before in The Wall Street Journal. There are a lot of topics to be had in terms of how we move to version 2.0 of the consumer use of cost and quality data.
We are going to break for lunch at 1:00 and we are going to hear, as I mentioned yesterday, from David Goldhill, who is the CEO of the Game Show Network, about his experiences trying to care for his father in our health care system.
We are then actually going to go into a discussion around some crosscutting strategies that can advance patient and family engagement and partnership. One of the observations that a planning committee member made as we were putting these workshops together was about the fact that there is a common theme that does tend to underlie all of these three topical areas we have been focused on. Of course, we have talked about partnership. But the other common thread is this idea of decision making. Yesterday we talked about decision making in care. But today we are going to talk really about the decision to share your personalized clinical data for improving population health through research. And we are going to talk about the decision to choose a high-value health care provider, the decision to use tools that would help you identify high-value health care providers. We are going to have a great discussion around some crosscutting strategies that might support that kind of information dissemination and decision making, again, through that lens of partnership.
And then we are going to end with some reflections from a very diverse and very interesting set of our planning committee members on this pathway forward. If you recall, that is really what we are thinking about. How do we accelerate progress in these areas by building on what we already know? That is what our lineup looks like for the day. We will adjourn at 4:30. Lots of tearful goodbyes, hugs, things like that. And, again, I will just encourage you guys online as well as in the audience. We really do want to continue to have a robust and dynamic discussion like
we did yesterday. We have microphones. We have e-mail and online strategy. Please do avail yourselves of them.
I am going to turn it over to Sue Brown Trinidad. She is a research scientist in the Department of Bioethics and Humanities at the University of Washington. She is going to moderate our panel. I will say that she focuses in her research on ethical, legal, and social implications of genomic research. She also is interested in studies, communication, and decision making, and health care settings, health equity, community-based participatory research, and more. She is a terrific thought leader and member of our planning committee for which we are grateful. I will turn it to you. Thank you, Sue.
KNOWLEDGE GENERATION AND CARE IMPROVEMENT
Dr. Susan Brown Trinidad (Moderator)
DR. TRINIDAD: The first thing is always, I apologize if you cannot see me. But I also saw that girl fall down at the Oscars. It is a trade-off always. We have a lot of work to do this morning before 10:45. I know my panelists and thank you all for being here. On behalf of the Planning Committee, thank all of you for being here and all of you out there as well.
I do want to point out there was a comment on the website last night saying, “Why aren’t there any patients up here?” I am pleased to say that today we will have patients participating as panelists.
Knowledge generation and care improvement. The research world. I think there are a couple of big trends that are converging to bring us toward a direction that looks more like progress on a lot of the things that most of us in this room care about. Translational science and the research space. There is a lot of talk right now about how we move from the bench to the bedside. There has been less discussion of where patients fit in that translational process. I am hoping we will talk a little bit about that today. We will look at comparative effectiveness research, patient-centered outcomes. All of those things I think are beginning to grow in the direction of a critical mass to actually get patients involved in a way that is more reciprocal than what we have seen in the past.
One way of framing what we will be thinking about and talking about this morning is, what do we know? The first question is, who are we? We have been in the research realm and historically a pretty limited set of people. There was some talk yesterday about culture and the important shaping that culture has that can sometimes be invisible to us because we are in it all the time. That definition of who we are when we are thinking about what we know is starting to get broader. And I think that is a really positive development and I think bringing patients into that definition of “we” is an important piece.
The other issue is what we know, what do we know, how do we know that we know it, and what counts as knowledge. I come from the bioethics area. I have training in philosophy. All of these questions about epistemology, how do we know it is knowledge, what counts? Those are actually important issues from a policy standpoint. Whose input counts?
I just came back from Bethel, Alaska. People in villages of fewer than a thousand people. Their ideas about what their health priorities are finally beginning to get some currency in the people who are providing services. That is important and that is an important change.
We will address all of these issues. We will be shaping these around four directed questions. The first thing we will talk about is what the current state of play is. A lot is happening in the research world that is quite different from the way that things have traditionally been set up, with a bright line between the clinical realm and the research realm. That is getting blurry. And we have not yet caught up with what that means in terms of implementation or regulatory protections. Patient views about what is happening with research, research realities, and then the regulatory environment are all things that will fit under that section heading.
We will also talk a little bit about public and patient opinions. In my own work, and my colleague Evette Ludman will talk a little bit about some of the work we have done together. People are supportive of improvement. We will hear a little bit about what they want from us in the research space. We have traditionally thought of people participating in research. It turns out there are some things they like in return. We need to think about that.
Now, I would like to move on to introducing our distinguished panel. We have Dr. Nancy Kass who will start us off. She is the Phoebe R. Berman Professor of Bioethics and Public Health in the Department of Health Policy and Management at Johns Hopkins Bloomberg School of Public Health and the Deputy Director for Public Health in the Berman Institute of Bioethics. Her current research projects examine ethics for a learning health care system, including quality improvement and comparative effectiveness, informed consent in randomized trials, ethics issues that arise in international health research, and ethics and public health preparedness.
We will hear from Alice Leiter from the Center for Democracy and Technology about meaningful choice. She is Policy Counsel for the Center for Democracy and Technolog’s Health Privacy Project. Her work focuses on developing policies for the advancement, adoption, and implementation of health information technology and electronic health information exchange to improve health care.
Ken Mandl will speak to us about the infrastructure we need for patient-engaged translational research. He is from Boston Children’s Hospital and is an associate professor at Harvard Medical School and the Louis Diamond Investigator at Children’s Hospital Boston, where he directs the Intelligent Health Laboratory within the Children’s Hospital Informatics Program. He has pioneered and published extensively in the areas of personal health records and biosurveillance. Under a major HHS initiative, he co-leads the SMART Platforms project, which seeks to create an apps store for health.
We will close with a joint presentation from Peter Margolis and Jill Plevinsky from Cincinnati Children’s Hospital Medical Center. Dr. Margolis is a professor of pediatrics and director of research at the James M. Anderson Center for Health Systems Excellence at Cincinnati Children’s. His work encompasses the application and study of quality improvement methods and a broad range of areas, including primary and subspecialty care, communities, and public health settings to improve the health outcomes of children, families, and communities. Jill Plevinsky is currently a clinical research coordinator for the Inflammatory Bowel Disease Center at Boston Children’s Hospital and recently completed graduate work in child development at Tufts University. She was diagnosed with Crohn’s disease at age 7 and immediately became involved in awareness, education, and fundraising efforts through the Crohn’s and Colitis Foundation, for which she served as the Philadelphia Delaware Valley Chapter’s first youth ambassador and the founding chair of the National Youth Leadership Council.
Thank you all very much. I will turn it over to Nancy.
Ethical Challenges of a Changing Research Paradigm
Dr. Nancy Kass
DR. KASS: Thank you, Sue. Thank you for the organizers for inviting me. I apologize that I was unable to be here yesterday. It sounds like it was a really lively and terrific discussion and I apologize. I was saying to Sue that I always feel a little awkward and embarrassed coming in what feels like the middle of the discussion, but I was not here for the beginning. Correct me and bring things to my attention afterwards for things to which I should have paid attention.
I want to start by acknowledging my partners in crime. Pieces of what I am going to be talking about today are drawn from a particular project on ethics in the learning health care system that I conducted with my fabulous and lovely colleagues. Here they are (Ruth Faden, Tom Beauchamp, Peter Pronovost, Steven Goodman, and Sean Tunis).
Let me tell you what I want to do today. I was asked to talk about changing ethical paradigms. And what I want to do is introduce you to what I am going to call paradigm one, which you might call a historic paradigm, but I guess I would also argue is one that is alive and well today. There are some good reasons for that, but I also want to argue that I think there are some problems with it. Paradigm one is what I will also call the “distinctions paradigm.” I am going to tell you what the current ethical requirements of that paradigm are, and again, what I see as some of the problems.
I am then going to say just a little bit about patient engagement. Probably not necessary to say very much for this audience, but I want to bring it in as a bridge to get to paradigm number two, which is what I am going to call the “ethics in learning health care system paradigm.” I will again then talk about what our ethical requirements are for paradigm number two. I will then suggest that some of what I see as the potential paradoxes that can come up in patient engagement are maybe not such a paradox at all.
I want to start with paradigm one, which is where we are coming from, and again what I will call the distinctions paradigm. To rehearse a little bit of history, in the 1960s and 1970s, the American public became aware of research that our federal government had either funded or conducted that illustrated a variety of scandals or research abuses, often involving vulnerable populations who were often led to believe that they were being cared for as patients, when instead research was being done without their knowledge and in ways that was not helpful to them, provided no benefit, and often provided some abuse. This appropriately led to American outrage and Congressional action.
Following this, in 1974, federal regulations were passed for the first time in this country to oversee human research. That led to a variety of ethics requirements, or I guess what I will call legal requirements, in the name of ethics. One that we are all familiar with is IRB review. All human research has to be looked at by an ethics committee before it can go into the field. Informed consent has to happen in most but not all cases of human research. Because the new regulations said research activities have to go through this oversight, and yet clinical care activities do not, an immediate first requirement was to define what these regulations apply to? That meant research had to be defined, and the regulations did that. Subsequently, a lot of academic scholarship also began to define what is research. Again, these distinctions and definitions became important because of the important practical application that things that were called research had to have a lot of ethical oversight, and things that were clinical care were not required to have any such oversight.
I have a slide here with five things that my colleagues and I have said are categories of distinctions, the things that have been used in the literature and in regulatory definitions to distinguish research from practice. I have put under each of them what was implied, by contrast, about clinical care. The regulations say research is an activity that is intended from the get-go to produce generalizable knowledge, the assumption being that practice is intended to help the patient at hand exclusively. Research is where there is a systematic collection of data where there is an assumption that in clinical care (again, think back to the 1970s) there is no systematic data collection; we only collect data for the patient at hand and put it in his or her chart.
There are then additional claims from the literature about what research is and how it differs from clinical practice. One such claim is that research poses risks. We have uncertainty about whether there is clinical benefit from the intervention we are giving to a patient, whereas the assumption in clinical care is that we only give treatments where we know that the benefits outweigh the risk. Another claim is that in research, there are burdens that arise from activities that are not necessary for clinical care. We ask patients to do things above and beyond what is necessary for their clinical care, extra questionnaires, extra tests. Again, the assumption is that in practice every single intervention or test, duplicated test, triplicate test, contributes to good care management. And then in research, the last piece of what we will call a distinguishing claim is that in clinical research there are protocols that dictate which treatment you or I receive as a patient, whereas in clinical care, it is physician autonomy or patient autonomy or the dyad autonomy that decided what care you get.
Problems with this paradigm: We would argue that there are practical problems, conceptual problems, and moral problems with this approach. The practical problems are that there is complete confusion. One of the things we did in our work, and I do not have time to show it, is focus groups both with patients and with providers. There are some really stunning, and I would say amusing, quotes about the ways that people try to navigate this distinction when to them the activities look remarkably similar.
There are conceptual problems. I am guessing that if I went back to this slide, each of you could point to some problems with this logic, and again some of it becomes almost comical. I was being a little tongue in cheek in talking about things like the duplicate and triplicate test, but it is actually no joke. There are multiple things done in clinical care where we do not know whether they work, and there are multiple additional burdens that are placed on us as patients for all sorts of reasons that have to do with the health care system not being properly integrated.
This slide is pointing to some of those conceptual problems. A conceptual problem for people who do not live in our kind of academic wordsmithing context, is a problem where the words and claims are not working. For a good conceptual definition you could say, for example, the characteristics of a table are blah, blah, blah. All the things that have those characteristics are a table and things that do not have those characteristics are not a table. It is a way to provide a definition.
We are saying that those words and claims of the conceptual definition of research are not working. The idea that producing generalizable knowledge happens in research but not in practice is conceptually problematic. We learn from ordinary medical care, and we learn from quality improvement activities and both types of learning are applied to future patients. Systematic data collection also is not unique to research. We collect data systematically in practice whether we want to or not. It is now required in so many ways. For your hospital to be accredited, systematic data collection on many outcomes is required. Again, for quality
improvement, it is required. There are many ways in which clinical care data must be aggregated in the current American health care context.
There are many errors and risks in ordinary clinical care. Nobody wants that to happen. It is not on purpose. People are working really hard to avoid it. But this idea that clinical care is absent of risks or will never impose an intervention that has more risks than benefits is erroneous. And at the same time, the flip side of the coin is that the research paradigm of the 1970s and 1980s, where clinical research was only about testing experimental treatments, also is false. There is so much research today that is comparing different treatments that have been FDA approved for decades to see which one is better, monitoring different treatments that have been used for 30 years to see how they really play out in different populations of patients, and in these types of studies it is hard to argue that the research poses any more risks than the regular clinical care patients would have experienced receiving those exact same treatments. And as I already said, practice will often include many unnecessary burdens.
This leads to what people in my world of ethics call a moral problem, which is that there is overprotection. Again, remember that these ethics rules—and I will be the first to say I have taught these. There are so many pieces of these that I believe in. I have sat on many IRBs in my life. The whole foundational purpose of having these ethics rules is to protect patients or healthy volunteers from what they may not be aware of as significant and important risks done, if you will, at their expense for the sake of others. It is a very important concern that we always have to have for those of us who want to dedicate part of our professional lives to learning.
At the same time, if the purpose of drawing a line between research and clinical care is to demarcate activities that need to be looked at to see if they pose too many risks to people or might be exploiting people, we may not be using the right set of criteria. The moral argument would be that there are some patients who are being overprotected and others who are being underprotected. In other words, tons of activities currently have to go to IRBs for review and oversight when the activities pose very little risk—certainly no more risk than daily clinical care; while a bunch of other activities that likely carry a lot of risks and chance for errors go forward with no oversight whatsoever.
Let me move briefly to a couple of things about patient engagement. There is a lot of discussion, appropriately, currently about patient engagement, and of course this is much of the focus of today’s meeting. I imagine part of what you talked about yesterday was the need to have a lot more shared decision making in clinical care. And one of the articles that I read in preparing for this meeting, the Health Affairs article, which I loved, talked about shared decision making relying on three things, one of which being that doctors and patients be really open with each other about all of the evidence. There is this assumption that to have patient engagement you need good clinical evidence.
Now, there is also this idea that in research, as a sign of respect, there has to be disclosure and discussion about what the research is about. There are two paradoxes in this space that I want to raise. One starts with the commitment that shared decision making relies on good evidence. It is sort of like a catch-22, because we have so little evidence available, that it is hard to be able to tell people the evidence related to their care or options. And then there is the paradox that one of the reasons we have so little good evidence is because of the hurdles and barriers that this large system of ethics oversight, and related concerns about privacy, have put in place.
Paradox number two is that we believe ourselves to be very concerned about patients’ rights and our rights as citizens to know what it is going on, and thus demand to be told all details
about all sorts of research activities, and yet because of this historical distinction between how we treat research versus clinical care, we basically say nothing to patients or communities about the extraordinary amount of data that is collected and aggregated every day in the health care system health departments and the CDC, and certainly all hospitals are routinely collecting data. This is why we know about obesity rates, cancer rates, what makes a difference in infections, in patient falls in hospitals, et cetera.
I want to really briefly introduce what I will call paradigm number two, which is to introduce alternative ways to think about ethics and the learning health care system. The learning health care system. Again, I am going to make the assumption that a lot of you in the audience are really familiar with this. It draws on language from the Institute of Medicine. The learning health care system is where care and learning are deliberately integrated. It is not just that research is going on at the same time as care. There is a philosophical view that these must be and can be integrated. There is an assumption that high-quality care and learning depend on each other. There is a synergy there. Research with experimental drugs will still happen, but that is a little bit separate and not what I am talking about.
When we can learn systematically from care, we ask questions like What are the outcomes of different treatment choices that are given all the time? What are the outcomes of different care approaches? This slide is the one slide that introduces some of the work that my colleagues and I have done that says a learning health care system is an ethical good. If we want evidence to give to patients for shared decision making, we have to have good evidence. And in order to ensure that such evidence is developed in an ethically acceptable way, there need to be seven foundational ethical commitments as you structure and run a learning health care system. Some will sound familiar and some maybe are a little bit less so. You always have to respect the rights and dignity of patients. You have to respect clinical judgments. You have to have a commitment to providing what you understand to be optimal clinical care to patients—it can never be compromised for the sake of learning. You must avoid imposing nonclinical burdens and risks. And certainly, talk to people about them if there will be any. And then some newer ones. We must address health inequalities. And really maybe not part of a traditional ethics guidelines, there must be some commitments on the part of clinicians and on the part of patients to participate in the learning process when it will not compromise your clinical care and when it will not pose unnecessary burdens.
I think this is my last slide, which just says, so maybe this paradox is not quite so great. Patients are clamoring for better evidence and data. We have done some focus groups with patients ourselves, where it is often the people with the most significant chronic illnesses who are saying, Give us more data. Do not protect us so much that we cannot learn. There are so many more books, videos, websites today that are advocating for people to contribute their data for better treatments. Patients in trusting relationships are more willing to share their data. That gives us something we have to think about.
And there are many possible strategies for engaging and disclosing and discussing this whole learning idea with patients in health care systems. It is important now to do the work to find out from patients how to do that. We were recently funded by PCORI to gather some preliminary data with patients about what their views are about disclosure, consent, and authorization in the context of a learning health care system. But I guess I will close by saying it seems that that is the way that honors what patient engagement is really designed to do and gather the data that patients need to have. Thank you.
DR. TRINIDAD: Now, we will hear from Alice and we will hold questions until the end of the panel. Thank you.
Meaningful Choice in a Learning Health Care System: The Relationship Between Privacy and Data Sharing for Research
Ms. Alice Leiter
MS. LEITER: Good morning. Thanks so much for the introduction and thank you so much for that presentation, Nancy. What I am going to talk about hopefully builds nicely upon it, because I have the great pleasure of talking to you all about the law or the system of obstacles and burdens as some of you may see it. Unfortunately, if we are going to talk about meaningful choice, if we are going to talk about privacy protections, and if we are going to talk about data sharing, you cannot really have an effective policy discussion about these issues until you first understand what is not possible legally. I will do my best despite some fairly dense slides to go not quickly in my speaking, but briefly at a high level through these first slides so that I can at least keep you somewhat awake.
First, a little bit about the Health Privacy Project at the Center for Democracy and Technology. The project is premised upon the notion that I am sure we would all agree with, that health IT and the exchange of electronic health information are really the drivers and engines of health reform with the greatest potential to improve health. And certainly, in this new electronic health environment, some progress has been made to update and resolve some of the privacy and security challenges that arose when our system got turned on its head and became digitized. But as everyone is far too familiar with, a number of questions and challenges and implementation issues still exist, not withstanding some really solid and important and meaningful efforts on the part of HHS and CMS to update the HIPAA medical privacy rule and others to better fit this new environment.
This last bullet is to hopefully toot our own horn a little bit and saying that the solutions that we advocate are really those that are practical. Too often, I think, privacy advocates are seen as hysterical. Consumer advocates are seen as hysterical. We really try to work with people like you who are like-minded to find workable solutions to not only keep privacy and security central and paramount, but to get data liquid and freely flowing, so that it can be leveraged for all of the purposes that it needs to be.
I think these first couple of bullets about what a learning health care system is are written by people in this room. I certainly know this first one comes from Nancy. There are a lot of different ways to talk about a learning health care system and to define it. For my purposes in my work, the focus is really this need to safely and securely leverage clinical data for purposes that are beyond treatment and payment, and that a learning health care system is not going to be possible unless we find ways to do this.
A little bit about HIPAA. Big question when it comes to research is, first of all, does HIPAA—again, this is the medical privacy law applied, the federal medical privacy law. These bullets are about the identifiability of the data, because if data is de-identified, HIPAA does not apply. There are numerous and technical ways to de-identify your data. There are legal standards. There are methodologies to do it. And limited data sets are familiar to all of you in the research community because they are a close cousin to de-identify data. They involve some removal of categories of information. They are permitted for research. Data holders are required
to execute data use agreements to use limited data sets or information limited data sets, but individual consent is typically not required, which makes that quite attractive.
Again, the reason that this is important is because, as many of you know, in order for information that is patient identifiable to be used for research purposes, you have to obtain patient authorization. Authorization is the legal term. Consent is more typically the policy term. We will talk a little bit about that. With a few exceptions, a privacy board waiver or an IRB waiver or some exceptions found in the law, this individual authorization is necessary. Now, that is not easy to obtain and often seen as incredibly onerous. It makes perfect sense that research on data that is qualified as de-identified is largely not regulated and therefore enormously attractive to those who are engaging in research.
Unfortunately, it is not just HIPAA that we all have to worry about. I am not going to go through all of these, but there are numerous other state and local laws and regulations that can apply depending on the nature of the data, depending on the nature of the study, everything from the common rule—which I will talk about briefly on the next slide because it governs federally funded research to state laws—to health information exchange policies, to grant conditions and sometimes even international laws.
The Common Rule, the big research rule for federally funded research unidentifiable data—it is not that it is not worth talking about it, but some of you may know about 18 months ago what is called Advance Notice of Proposed Rulemaking, kind of an early heads-up that we are going to do some regulating on this subject, was released that proposed some fairly significant changes. And the good news is that they all seemed to be designed to bring it in line with the HIPAA law. There are some gaps and there is some confusion. There are a number of headaches caused by the relationship between HIPAA and the Common Rule. We are hoping that once we get a little bit farther down the regulatory process with this rule, we will feel a little bit better.
As we heard a little bit, and I will just say more specifically that there are some really common and legitimate criticisms of this legal framework that we have right now. As you could argue from my presentation, there is a disproportionate focus on whether or not the data is identifiable and whether or not patient consent is required. Having sort of laser beam focused on whether the data is stripped of these 18 or 16 or however many identifiers, and do we need to obtain patient authorization or consent, ignores a number of other valid and hugely important privacy protections that are available to us. Unsurprisingly, there is a real tendency to be conservative on the part of researchers and their interpretation of these rules and requirements for obvious reasons. You do not want to get in trouble and it is better to be safe than sorry. Unfortunately, that ends up causing or creating obstacles and barriers to research and to data sharing more broadly that may not actually exist or should not exist.
What we would like instead? A comprehensive privacy and security framework is desperately needed, not just for medical information, but really for consumer individual information writ large. Until we have that, it is probably not going to be this open, safe, secure, facilitating of health IT and health information exchange that we would like. There should be less focus on consent and more focus on the rest of the so-called fair information practice principles. Sometimes they are FIPs. I have a slide about those in a couple of minutes or a couple of slides. The notion is that let’s broaden our focus and think about all the different tools in our arsenal and try to get away from this headache of consent.
Central to this and fitting in with this broader theme of this whole meeting of consumer and patient engagement is that any privacy and security framework has to incorporate notions of consumer and patient expectations. This idea of context. When you are deciding which of the
tools to pull out from your toolbox to protect privacy is important because in different contexts patients expect different things. And what you want is for no one to ever feel surprised or shocked or upset about a particular use of their health information. But you also do not want to assume that they are going to be—that a person is going to be shocked or upset or unwilling to share health information in a particular context. You do not know that until you have had full open transparency and engagement. If we can get all of these, you really have the basis for meaningful choice.
Meaningful choice, and this does not just apply to research, but really consumer choice for use and exchange of health information in general, centers around a number of principles. The most important ones I have highlighted here. You have to be able to make the choice in advance. You have to be free to make the choice. You cannot feel like if you say no to something that something is going to be withheld from you, for example, medical treatment. And there needs to be absolutely full transparency and education about what that choice entails. Without that, it is not meaningful. This notion of opt in or opt out in the endless hours of discussion and debate that yours truly and many probably of you have sat in about what is going to be opt in or opt out should not matter as much if the choice, regardless of the system for giving it, is meaningful.
These fair information practice principles—this list that I have given—was developed or articulated by the Markle Connecting for Health Initiative, but they can be found in a number of different articulations. The Federal Trade Commission, the Department of Health and Human Services, the Office of the National Coordinator for Health IT has its own set. But they have similar themes that are the most relevant. I will not read them all out for you, but you can see that this idea of choice is but one. The idea that you should be able to consent to the use and exchange of your health information is certainly important, but so too is openness and transparency, understanding the purpose, feeling that the very least of your data that is necessary is going to be used, that you have some ability to participate and control, that the data is accurate, that it is safe, and that there is some accountability and oversight for the use of your information.
My next couple of slides are on ways to structure research networks to achieve this. Distributed networks versus centralized networks. I am running out of time and I think that that is maybe left best to more specific conversations later offline if you would like. I think ending on the fair information practices is most relevant to this presentation. I look forward to the discussion afterwards. Thank you.
The Infrastructure Needed for Patient-Engaged Translational Research
Dr. Kenneth Mandl
DR. MANDL: Hello everybody. Good morning. Thank you for those excellent presentations that set up this idea of a learning health system and one in which there is progress and protection of patients.
Now, I am going to focus on the plumbing. I am the IT talk here. And the plumbing is about how to hook patients. I do not mean this in a derogatory way because when I look at the whole idea of patient engagement, I am usually thinking about it as a patient or a father of a patient. It is very important to think about this learning health system, and that is the context in which we are discussing this today. There is an assumption that the care, the science, and the evidence are all in some way become much more aligned, interconnected, that there is a virtuous cycle, and that
the patients are very much engaged in both contributing information as well as receiving back information, so that they can improve care and improve quality of life.
Let’s just look at the way we do this. How do we hook patients into a system like this technically? In 1998, I wrote my first paper and it was extremely controversial. It was the idea that doctors and patients will actually e-mail each other and that this is something that could possibly be safe. There was a sense that, what if a patient e-mails that they are having a heart attack or doctors are just going to be overwhelmed by these unruly crowds that now have unlimited access to them 24 hours a day. We actually built the first doctor/patient e-mail system and tried it in 1998. It was for pediatrics. It has a cute giraffe on it. But since then, what we found is there have been very large-scale efforts. My HealtheVet, the Epic MyChart system, which is used across Kaiser and Group Health and many places. Millions and millions and millions of messages have gone back and forth. Most of the fears were never realized. Of course, this is one form of access and getting patients engaged. But this is mostly a free text thing, just a first step in the learning health system.
Now, we have activated patients. Here are patients who come in. In the era of genomic medicine, patients plus Internet know a lot more than most of the doctors. I have here Dave, here in the second row. He has actually brilliantly formalized a whole conceptual structure around this idea of a technologically enabled and informed patient that he calls the e-Patient. Now, how do you then get information flowing back and forth between patients? There are these federal initiatives to try to do this. We have been screaming in the wilderness that patients need to have some access to their data. I am sure Alice can tell you better than I, but HIPAA was supposed to—the original HIPAA, 1976—was supposed to facilitate electronic access by patients to their data. But there was this little phrase that was in the regulation that said “if feasible.” For basically since then, since 1996, every single organization has decided that it is not feasible to give them electronic access to their data. And in fact, HIPAA was of course used as an excuse not to share the data with the patients most commonly.
But then in HITECH there was language that once again promised data to the patients. That sort of did not quite work because the technological alignment was not perfect. You could get electronic access to data through, for example, a PDF file or something that really did not give you the opportunity to use your data in a Web 2.0 apps kind of way. We will talk about that a little more. But now there are projects that are quite formalized in the structure. One is called Blue Button. Blue Button is supposed to be a disruptive innovation. In the Department of Veterans Affairs, they can literally push a Blue Button, it looks like this, on their health record and get a copy of their data. The only problem is it comes out of no particular format and you cannot read it or understand anything that is in it. But it is there. You get your data. And then there is something called the Direct Project, which is about an e-mail system for health.
The question is if there is going to be this kind of data liquidity, in other words, that data is now going to move out of systems toward patients so that we can begin to—one way to begin to engage them is we have seen these portals like Epic MyChart. The one is just I am going to show you the data. Here it is on a screen. But it is trapped. It is behind the screen. You cannot get it. You can knock on the screen or something, but it is there and there is nothing you can really do with it. Then there is this Blue Button, which is are we going to actually give you a copy of the data, hopefully, one day in a way that you can use it. And then under this thing called Meaningful Use, which is how we have described the properties of health information technology that make it useful and is the basis of certification and payments. There is this new thing called CCDA. Do not worry about it. But it is a standard for how the data comes out,
supposedly in a way that is going to be really reusable by electronic systems as it communicates between electronic systems and between electronic systems for doctors and for patients.
Now, assuming the data comes out, where do we put it? You can stick it on your PC or your Smartphone. I hope you do not lose it. Or if you use one of the tens of thousands of apps that are in the Apple iTunes store or in Android, you may be able to store your data on some company’s server under some privacy policy that you probably cannot find or did not read. And it may still be very useful and it may be worth the privacy trade-off, but that is where it is. Or maybe your data just lives in your institution’s electronic health record. But what if you go to two different institutions? Does that work for you? Or maybe it is in something called a personal health record. This is another idea we had that the patient should get a copy of their data. It should be stored in a repository under their control and on top there should be apps that let you use the data the same way you are used to using data on iPhones now.
Clayton Christensen thought this was a very interesting idea and wrote about it in his book, The Innovator’s Prescription, because this gets the data instead of in institutional electronic health records. It gets it under the patient’s control. Then you do not need this idea of health information exchange because the data is all there under the patient’s control. The idea got some traction. We created the system called Indivo and interesting things happened. Microsoft took Indivo and created with the code something called HealthVault. Google took the model and created Google Health, but they deep-sixed it within the last year. And one reason is because this data liquidity just was not there. Anyone in the country could have a Google Health record, but no one could have anything in it. That was a problem. Also, do people trust Google to manage their health data?—that is a question. It is not clear—there was this data liquidity and the trust issue. Some composite issues there.
Dossia Consortium of large employers worked with us and we actually built out Indivo for use in hundreds of thousands of their patients. And Jim Hansen is here who knows that story well. The question is, why would this great idea and these big companies jumping in, Walmart, AT&T, Intel, Dossia, Google—why isn’t everyone using data in personal health records? I do not know exactly, but I think that there are other hooks too that are important. One is social. Social seems to be important. We started to do experiments. We said everyone is being offered personal health records, but everyone is hanging out on social networks. We did some experiments where we, for example, got—can we get data from patients in a social network context? And in a big website called TuDiabetes where there are tens of thousands of patients with diabetes, we actually ran a data donation drive. We activated the community. By contributing data about your diabetes, you provided community support and you populated a map. We turned it into an interesting contest and a game. We got thousands of people participating contributing data. There is this idea of data donation.
Hook number five is feedback. It turns out that if you actually give folks back information when you ask it from them, you actually make this a collaborative relationship. It becomes very interesting. Last week in JAMA Internal Medicine, we published a piece where we actually elucidated quite a bit of information about the harms attributable to hypoglycemia and diabetes in this population on TuDiabetes. We got some very interesting data, and data in a bidirectional communication mode where we get data from the population and we can return interventions to populations about potentially very high morbidity conditions.
Also, there is another hook. That is, I am contributing to information that helps my condition get cured or treated better. PatientsLikeMe. You are going to hear more about PatientsLikeMe that had tremendous success with the amytrophic lateral sclerosis community, Lou Gehrig’s
disease, where the majority of patients in the world with Lou Gehrig’s disease were sharing information about their condition.
There is this idea too beyond social networks of these kinds of registries where we actually accumulate through large health systems large numbers of patients in particular structure where we collect data from them; electronic health record data plus data that we collect meticulously plus data directly from patients. We are doing experiments with those. You will hear more from Peter, I think, about ImproveCareNow, which has many patients with inflammatory bowel disease including my own son who is a member of Peter’s database. We are doing work with a professional organization called CarraNet where we have more than 50 percent of kids with pediatric rheumatologic conditions in one system with bidirectional access. And PPHNet where kids with pulmonary vascular disease. We are just getting starting on that.
I am going to wrap up to tell you that also there is a very interesting opportunity to actually go right to the point of care and do patient engagement right there right at the point of care. This is a project that I would love to tell you more about, but not right now. But this is a $15 million project from the Office of the National Coordinator where we are re-imagining electronic health records as apps platforms. And the idea is can we take an EHR and actually add to it apps that extend its functionality and that open up electronic health records to a large community of software developer innovators, so that electronic health records can have all kinds of functionality that face both patients and clinicians. I have to thank David Blumenthal who funded this project 3 years ago.
I just want to show you one small slice of the project, which is how are we using this to actually begin to engage patients. Here is an app. Hook number seven: decision support. Maybe we can actually tell patients exactly what they need to do or what their risks are. We took this picture from Wired magazine, which is a laboratory information system of the future, and we turned it into an app that shows your cardiac risk. It pulls data out of the electronic medical record. And instead of your standard information display in electronic health record, this is something that we actually created in 8 days. We can tweak it any way you want. It shows you your risk.
This is a tool for getting doctors and patients talking at the point of care. And the last hook here is the opportunity to actually bring your data to the point of care. This is in collaboration with Microsoft. This is at the point of care. The doc pulls out the information from the electronic medical record on diabetes and goes out to the personal health record, pulls the patient observations of diabetes and merges them together. You can actually do conversations at the point of care. These are our patients of the future. Sorry for going over 2 minutes.
Patient Engagement and Data Sharing for Improvement, Innovation, and Discovery
Dr. Peter Margolis and Ms. Jill Plevinsky
DR. MARGOLIS: We are going to give a more concrete example of how we are struggling through many of the issues that everybody else has raised. This is a bit of a tag team talk between Jill and me. I just want to acknowledge the support we have gotten from the NIH Transformative Research Program and the AHRQ enhanced registries program.
Just to motivate the discussion, I want to do it by talking about the participants in the chronic illness care system. This is Bianca, and the system of chronic illness care is not working for her. She is 11. She has Crohn’s disease and she is obviously in a lot of pain. That is the least of her
problems. Without optimal treatment, she will have stomach growth, possibly experience arthritis, and a significant risk of surgery. She cannot go anywhere without knowing exactly where the bathrooms are. And normal childhood events like sleepovers are extremely difficult.
It (the system) is also not working for Bianca’s doctor, whom we call Dr. Roan. She has a variety of treatment options, but the best evidence is evidence that comes from clinical trials, and it cannot provide information on what will work best for a particular patient. It is also not working for Bianca’s mom (we call her Anna), because the care delivery model does not facilitate her participation. She is wondering about trying dietary modifications to see how best to control Bianca’s symptoms. She keeps her eye on what is going on, but feels it is the doctor’s role to come up with solutions. She does not really see the collaborative possibilities. And finally, it is not working for the one whom we call Dr. Vincent Kapur. He is a researcher interested in improving GI care. But he is faced with small and representative data sets in a lack of easy and productive ways to share data and increase the impact and reach of his research.
Our project to develop what we call a collaborative chronic care network focuses on this question. What if we could harness—what if we could create a vastly better chronic care system by harnessing the inherent motivation and collective intelligence of patients and clinicians? If you think of Wikipedia—or in science, how open sharing in the human genome project in advance of publication dramatically accelerated the discovery process. These are examples of how the production of knowledge and information and know-how can be distributed over a large group of people.
Yochai Benkler, who is a professor at the Harvard Berkman Center for the Internet, calls this form of production “network-based” or “social production.” In health care, networks for clinical research have been central to accelerating discovery, and networks of patients have served as potent patient advocates for more effective research management and greater investment, and now even in developing new knowledge.
The model that we are presenting brings together all the stakeholders in the process—the patients, the clinicians, the researchers—to improve health outcomes as part of a learning health system. Our effort began in 2007, when the pediatric gastroenterology community as part of the American Board of Pediatrics Maintenance of Certification program organized a collaborative network called ImproveCareNow that was dedicated to improving the health and lives of children with Crohn’s disease and ulcerative colitis. These are some data from the centers that have enrolled more than 75 percent of their patients in the register. The red lines show the variation in the monthly rates that would be expected by chance alone. What you can see is that with no new therapies and no blockbuster drugs, the percentage of children with IBD in remission has risen from about 60 to now over 75 percent. How did the clinicians do this? They did it by sharing. They were sharing knowledge, sharing know-how, sharing the work of figuring out how to improve the care delivery center. Every center has pulled their data. They have standardized their outcomes care and learned from one another about how to get better results. There are currently 51 care sites, 425 physicians, more than 15,000 patients. The ImproveCareNow network is now working with—this is 30 percent of the patients in the country with IBD.
ImproveCareNow is working with the C3N project to evolve from a network that is focused primarily on clinicians to one that involves all the stakeholders. And to do this we have concentrated on four main activities. The first is an ongoing focus on improving patient outcomes. The second is on building community. The third is on the effective use of technology. And the last is on developing the learning system, the use of system science, quality
improvement, qualitative and clinical research together. During the design phase of the project, our ethnographic research that was conducted by our partners at the design firm LIBA identified the needs and goals of patients with this disease. A particular interest for us was those patients who make a successful transition into adult care whose treatment decisions are driven by personal preferences. They come to make IBD part of their lives and want to share what they have learned and give back. We reach out to engage these young people who are innovators and lead users in the community. Jill Plevinsky, who will speak next, has made major contributions to designing and guiding and developing the system.
MS. PLEVINSKY: I am very excited to talk to you about the work going on in this project. I also wanted to tell you a little bit about my very brief patient story. I am happy to elaborate throughout the day, however. In introduction, I was diagnosed with Crohn’s disease when I was 7. Growing up with a chronic illness, as a lot of you know in the audience, is not an easy task. But I was definitely very able to find comfort through support groups and Camp Oasis, which was a weeklong camp for teens with IBD. At that point, [Camp Oasis] was my first patient community that I was ever a part of. But I did not realize that we could do more than raise awareness and raise money until I became a part of the C3N project. Definitely just excited to be able to partner with physicians and researchers. I have been playing a very active role in transforming care from the ground up.
There are a few reasons why I participate. Some of these may be familiar to some of the patients in the audience as well. No one likes to be sick. Like I said, having IBD is not easy. It is a difficult battle every day. I take medications daily, need to watch my diet, and as Peter mentioned, most of us always need to know if there is a restroom close by. Rather than just be defeated by the experience, I chose to get engaged. I also trust my physicians. I have incredible faith in all of my doctors. I believe that they can do everything that they can to ensure that I get the best care possible. But I know that they need my help in order to do that. I want to help my doctor help me do that.
As also mentioned, I work as a research coordinator at Boston Children’s. It is unrealistic to expect our physicians to give us the personalized care we expect if we do not help them do so. I witness every day how busy everyone is and how heavy caseloads can be. I definitely know that this partnership is essential to the success of care. With the new technologies like Ken was discussing, it is possible for patients to help.
I also want answers to difficult clinical questions based on facts, not just hunches. With IBD, there is no one perfect treatment for everyone and a lot of treatment decisions are made out of desperation. ImproveCareNow allows doctors to really access what works for certain patients across the whole country and can help one another make decisions based on data.
I also want to help make pediatric health care participatory. This movement obviously has already begun in the adult world. But as a now former pediatric patient, the fact is children and adolescents need to learn these skills too, especially as new diseases are being diagnosed at younger and younger ages. I also do not want other kids with IBD to feel as if their care is beyond their control. A lot of anxiety and depression in kids with chronic illness results from this feeling that they are not in control of their own health care. While some aspects of chronic disease are that way, it is important to remind young people that not everything is beyond their grasp and that is the first step to becoming an engaged patient in my opinion.
This is how we participate in C3N and ImproveCareNow. As part of the grant, I joined the design team to imagine new ways to create more continuous and collaborative care. It was at these meetings that we all realized it was really necessary to have a community-building
component. I along with other research team members, including physicians, researchers, nurses, and other patients, took a course by Marshall Ganz who was actually Cesar Chavez’s community organizer, now professor at Harvard Kennedy School. And one of the keys to his community building being a success was distributed leadership teams, meaning that, in order for a cause to truly take off, you need to start with one centralized leadership team, develop leadership and foster that control within that team, and then let them spread out to their local communities and start individual little communities all over the globe. It is a really nice way to allow leadership and ideas to flourish within a community. This can definitely be applied to patients, physicians, researchers, and so on.
Out of this framework, we decided to create a council of patients called the Patient Advisory Council. I will refer to it as the P-A-C. There are pictures of some lovely ladies up here who are members of the council. Basically, this is a group of young people with IBD who were diagnosed as children and adolescents. And the major purpose is to obviously foster leadership within the group. We developed a patient scholar progr m where we allowed these patients to attend our learning sessions, which involve all the clinicians from the ImproveCareNow centers so they can hear from patients at each learning session, which is awesome for us.
We also help the collaboratives develop tools as well. We actually used a match questionnaire to draw on their skills and expertise to match them to projects within the C3N. On six projects, we decided in mobile application to track patient passive health outcomes and online social networks, self-management tools, patient activation research, external communications as well. Once we did that, we have patients on just about every team working with doctors, researchers, developers to really develop and answer what they think is important to the patient community.
In my professional life, I see firsthand how traditional clinical research and translational work is done. The learning health system approach we use is very different. Patients are always asking me if they can see their results from studies personally and the answer is often always no. But the way that ImproveCareNow is different is that we use social media, Facebook, blogging, newsletters, and things like that to monthly share our data with the members of the database, so they can see this lovely chart of the increasing remission rates within the population (see Figure 2-7). Peter is going to describe some of the technologies that we use to do this.

FIGURE 2-7 ImproveCareNow social media.
SOURCE: Reprinted with permission from Peter Margolis.
DR. MARGOLIS: We have actually been building on some of Ken’s work at Harvard using the I2B2 registry to create what we call a data-in-once system, in which the same data the
clinicians enter in the electronic health record for clinical documentation is repurposed for analytics, QI, and comparative effectiveness research. We have worked with the EHR vendors Cerner, Centricity, and Epic to create standardized templates for data entry like the one shown here from Epic. The data are extracted locally from the EHR database and combined centrally for research once data are de-identified. And the data are used to automate chronic care processes like pre-visit planning … is a screenshot of the pre-visit planning tool that the clinicians use. We also use it for population management. Data are also used to produce monthly quality improvement reports where the sites can see their performance and compare themselves with all the other sites. And the registry can also be used to generate new comparative effectiveness evidence at multiple different levels—at the level of the population, the care center, and the individual. In the interest of time, I will just show two examples at the population individual level.
Doctors and patients wondered if we could use the registry to compare the effectiveness of biologic therapy, which costs about $50,000 per year, with usual care, typically steroids and thiopurines, which cost about $3,000 per year. There has never been a randomized trial in children to evaluate this question. None was likely to be done in the future because of ethical concerns of withholding treatment shown to be effective in adults. In a study that will be presented this spring, my colleagues Charlie Bailey, Marshall Joffe, and Chris Forrest from the University of Pennsylvania used new methodology to simulate a clinical trial by taking advantage of over 1,000 patients in the registry and naturally occurring variation in the use of biologic therapy (see Figure 2-8). This slide shows the percentage of patients in two groups who achieved clinical remission. The solid line is the patients receiving biologics. The dotted line is patients who did not receive them for two outcomes, clinical remission and steroid-free remission. This information will be used by the network to help guide decision making about the use of biologic therapies versus usual care.
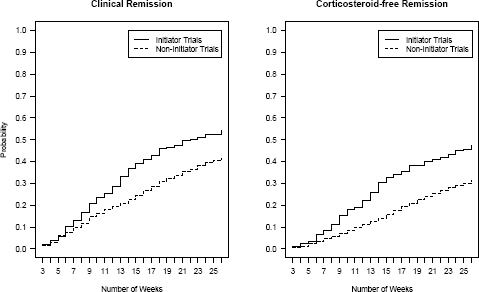
FIGURE 2-8 Cumulative probability of remission and corticosteroid-free remission for initiator and non-initiator trials during a 26-week follow-up period.
SOURCE: Reprinted with permission from Chris Forrest, Children’s Hospital of Philadelphia. Data from Forrest et al., 2013.
With the ability to collect data on a daily basis, we are also prototyping how to enable N of 1 learning, so individual patients and their physicians can work together to optimize their care. These are data from a college student with ulcerative colitis who had a colectomy when she was a young child, and she has been bothered by frequent nighttime stools and exhausted from getting up all night (see Figure 2-9). On the y-axis, you can see the number of stools per night and you can see the dates on the bottom. She and her doctor, Jeremy Adler, who is a gastroenterologist at the University of Michigan at the ImproveCareNow site, decided to start collecting daily data using an SMS text system. This revealed considerable variation. For example, there was a 6-day period when she went from waking up three to four times a night to waking up no times per night. When she reviewed the data together with her doctor, she recalled that she had been put on Amoxicillin by her primary care physician for sinusitis. This reduction in symptoms happened again and led the two of them to decide, rather than testing steroids as the initial treatment, to test treatment with Rifaximin, which is a locally released antibiotic. This is work being done by my colleagues Ian Eslick at the MIT media lab, Heather Kaplan and Dr. Adler and a team of gastroenterologists.
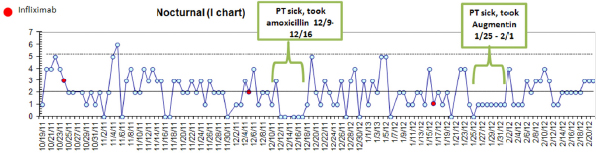
FIGURE 2-9 Data from a college student with ulcerative colitis.
SOURCE: Reprinted with permission from Jeremy Adler, M.D., M.Sc., Pediatric
Gastroenterology, University of Michigan.
The regulatory aspects of data sharing in the network are complicated because the system involves chronic illness care and research together. Regulatory oversight about the use of PHI for the production of the automated pre-visit planning and population management reports are addressed through H PAA notification and business associate agreements. These reports have patients’ names on them so that they can be used to guide clinical care. It is not only inconvenient not to have a report with a code on it; it is also not safe because you need to be sure that you are giving the right treatment to the right patient. A federated IRB and consent are required for data to be used for observational research. The comparative effectiveness research that I showed you is the limited data set, whereas the intervention health research uses full PHI. There is consent for participation in those projects.
I just want to touch on, because you all have talked about it, the complexity of the regulatory challenges. Virtually every physician in the network is extremely confused about HIPAA. any of them believe that there is no PHI shared outside their institutions. Buy-in for the federated IRB model that we are using is modest. About 38 percent of the centers have decided to rely on a central IRB despite the fact that this is a low-risk project. And the effort to gain IRB approval—legal approval is pretty extensive. It takes 22 hours for our research coordinator per center, 82 emails back and forth, on average 3 months to get this through IRB and business associates’ agreement. The maximum is 7 months. There is a direct impact of slower approval. It is fewer kids in remission.
In summary, the ImproveCareNow collaborative chronic network is an example of what we think is a learning health system that seeks to fundamentally redesign and restructure the research process by treating clinical care operational improvement and research as part of the same system, one that defines success based on better outcomes. Our hope is to bring the system to over a hundred care centers and 50,000 patients, vastly increasing the number of children in remission.
Our experience to date is that there are a number of challenges that we need to overcome. Bringing divergent groups together and overcoming the power, the language, the scientific, and technical differentials is significant. We believe that investment in creating this idea of distributed leadership that engages and connects all the stakeholder groups has the potential to not only spawn more cooperative behavior, but also produce improved engagement and participation. The policy and organizational constraints impose significant transactional costs, time, money, and effort to collaboration. And the execution of the privacy, the ethical and regulatory documents is time consuming, resource intensive, and challenging socially.
Investment in leadership by policy makers we think will be needed to test and disseminate new approaches to mitigate these costs and these are questions that are amenable to empirical research. Collaborative networks like the ImproveCareNow, with structured data and one’s technology, standardized care, and systems for virtually real-time scientific learning amount to labs where we can test and learn our way into future systems that enable patients and families and clinicians and researchers to work together to help young patients like Bianca live gracefully with chronic illness.
Audience Participation and Open Discussion
Dr. Susan Brown Trinidad (Moderator)
DR. TRINIDAD: Thank you very much. We will open up now for questions. Folks with questions, if you could head to one of the mics, please.
MR. DEBRONKART: I am thoroughly fascinated with looking into the use of science and the scientific method to produce research that can be, we hope, a stable foundation for making decisions—not just the patients, but the clinicians also, choosing among the available options. How do we move forward with as much certainty as we can have, given that there is no certainty?
I want to point to two quick things and then ask a question. First of all, on the slide about protecting people from risks that they are not aware of. Is Perry Cohen here today? Hi Perry. He has had a couple of episodes of studies into Parkinson’s treatments that were cut short or cancelled, invalidated, whatever, because the people protecting the patients decided that it was all placebo effect and that was noise and so the whole study should be thrown out. With somebody with a declining disease where their days are numbered, they may want to not be protected so much. They may say if there was a placebo effect, let’s figure out what that is. I would like to have that on the record.
Regarding the Blue Button, the data format may be cheesy and little and so on, but trust me as somebody who saw his own industry destroyed—typesetting—destroyed by desktop publishing, which started out as cheesy and meek, watch out, brother. There is a reason I am wearing the Blue Button here. And I get your point. We might have a gentleman’s bet of $100 to see where that is 5 years from now.
My question has to do—some of you I am sure are aware of the Reproducibility Initiative. In the several years I have been watching, trying to understand medicine, the only thing that has shocked me, except for the rate of medical errors, but the only thing in research was the discovery of the publication last year of the news that when Amgen tried to reproduce 53 landmark cancer studies, they failed to get the same result on 47 of them—tied to the news that most published studies are never replicated by another lab. One of the first things I learned as a grade school science student is when three people do the same thing, they better get the same result. With this august panel, I wonder. For instance, if I were to just wave a wand right now without it changing the practice, I would add a wobble score to every published finding saying whether anybody else has ever gotten the same result, because what we do is we take the results and then put them on patients hoping we will get the same result. Thanks. Thoughts on that on reproducibility. Is it important?
DR. MANDL: There are some important approaches that are being taken to try to regularize our approach to understanding all the research that has been done. For example, as you are probably familiar, ClinicalTrials.gov and the trial registration process has been shown to give insight into what was always suspected, but has now been very well demonstrated, that there is a publication bias. Studies that are positive are published. Studies that are negative are not published. The negative studies used to be dark matter. We never could see them. We could only infer them. Now, we can begin to see them as well. Yes, reproducibility is important.
It turns out that which organization and type of organization is funding the study is somewhat predictive about whether the results will be positive or not. Industry versus academia versus other not-for-profits. This area of understanding … the evidence whether the evidence is real. The fundamental assumption that there is evidence-based medicine is potentially flawed, and that is what is so interesting about the learning health system. It is a completely new way to produce evidence, and one which has its own set of methodological challenges, but that I think are fascinating and very promising.
MR. DEBRONKART: Just one closing note on this. To me this is absolutely not just a matter of patients’ rights, although obviously patients are the ones who are physically at stake. It is a disservice to the clinicians who have been trained to use evidence, for heaven’s sake. I would hope that somebody would—I will propose a practice that the funders of research that just become an ethical imperative that they—for instance, I think Reproducibility Initiative in Palo Alto is proposing something like a 10 or 15 percent additional charge to have a second lab try to reproduce the result. Thanks.
DR. TRINIDAD: Thanks. Let’s go here. And if I could ask the questioners to try to be as concise as possible so we can hear from everybody who is standing right now, that would be great. Thank you.
DR. GARDENIER: I am Turkan Gardenier from Pragmatica Corporation. Lots of commendation for both Dr. Mandl and Dr. Margolis. And by the way, I have heard of Dr. Margolis’s name in the statistical literature before now. My question relates to the exponential increase of data in these large databases, which are being called big data now. But also the question is, do they ever get decreased? For example, in industrial engineering, in inventory control there is a LIFO-FIFO system where once you converge upon a consensus of opinion, maybe you do not need the old data anymore. And relative to replicability, there is a lot of literature on meta-analyses, for example. Once studies converge upon agreed consensus maybe you do not need any more data of that kind. Do you run into questions like that? The idea of PatientsLikeMe, for example, is very interesting because you can do clusters of individuals that
will benefit from certain therapies. Are those ideas getting integrated into the increasing results and conclusions that are generated out of the interactive features of the wonderful databases?
DR. TRINIDAD: I can speak to biobanking because in that setting in genomic research, federated databases would be envisioned as an ongoing resource because you can ask many different questions against the same data sets. There is no plan to retire any of those data. I do not know if you wanted to add anything more to that.
DR. MANDL: In terms of the data management, I do not think there are any good plans along the way that you are proposing, which is very interesting. In a slightly orthogonal issue is just that we do sometimes perhaps try to get data across every place and every setting when in fact a subset of those data would be fine. It has been demonstrated again and again that these findings are fractal in the sense that you can see them in every place you look. It may be that certain associations between drugs and adverse events, for example, we have been able to demonstrate in a single health system with statistical significance in a way that is reproducible. Some work can be done much less expensively and with smaller big data, and sooner, because you can do these studies within even a single health system or a couple of health systems. That is a very important question.
DR. MONTORI: Victor Montori from Mayo Clinic. First, congratulations to the great panel. I have a couple of things. One is to the point, what Dave brought up. I want to make people aware of the Alltrials.net Initiative, that is a worldwide petition to have all clinical trials published in full—so, one more initiative to try to get the evidence record to be complete for all the reasons that Dave pointed as important.
The second thing is a question for Dr. Kass. I actually brought your papers with me to review. One of the things that I think is striking about this new framework is that it does require a lot less mental gymnastics to try to figure out what it is that you are doing vis-á-vis the IRB, and I suspect the IRBs are going to take a long time to come around. Maybe if patients and clinicians engage in health services research work to advocate for it, we may see some interesting experiments.
But one thing you said that struck me as something that may need empirical evidence, which is, beyond the many anecdotes, what is the evidence for opportunity cost of the ethical regulation we have now in relation to research that has not taken place because of it? You said there was a lot of work that probably has not taken place because of regulatory and ethical burdens. What is the empirical evidence of that?
My last point is all of you, I think, maybe I heard what I wanted to hear, made a big case for generosity. In many different ways, you all spoke about data fluidity and other things, but based on people volunteering generously or interconnecting. I think generosity was—maybe I heard it or maybe I imagined it, but I think it was at the base of this. But some of the concerns about big data are not really … big data is not getting into the hands of people that are being driven by generosity and altruism and trying to do good as their primary mission. There is a big industry evolving now around big data where the primary mission is not altruism. It could be a secondary side effect of it. There are some interesting stories around that, including the notion of medical information being combined with credit ratings and things like that. The individuals have not given the credit rating agencies any authorization, really we thought to combine that with your medical information. And some of the data is now being authorized to be combined. Because corporations can do it, they are doing it and the oversight is minimal. Comments on that.
DR. KASS: Great question. I do not know of good quantitative empirical evidence. There are two things I want to say though, because it is such an important question that speaks to the
kinds of empirical evidence that would be helpful. There is what I will call a growing amount of anecdotes, some of which are published. We have done now four focus groups with quality improvement and comparative effectiveness researchers who speak to the times when they did not embark on a project. I think there is one category, which is of people who thought about doing a project and abandoned the idea. That is one kind of opportunity cost, and one can think about how to collect more data.
The other kind of opportunity cost is where you do not even capture—I started an idea and then it was too much of a hassle to go through the IRB. But it is really more the number of clinical contexts where—I will make something up—where when you go to the doctor today, they give you the same two options that you would have been given 10 years ago, the identical two options. And there is really no more data than anybody brings to that discussion than they did 10 years ago. That is a really different kind of opportunity cost that we do not think about as concretely, but is probably more profound. It is a very different way to reveal what we have lost by not doing the constant learning.
DR. GARDENIER: My name is John Gardenier. I am retired after a career of scientific research using quantitative methods. I now consider myself a quantitative ethicist. As a patient diagnosed with prostate cancer, I found that there seems to be no medical science. There is a lot of medical practice, but no science related to this. I thought because I am a very experienced researcher and I understand math and statistics, I could go into the Internet. I could talk to doctors and I could really find out what is the best thing to do with my cancer. I found that is absolutely untrue.
The best site was the Prostate Cancer Association, which listed all the different kinds of treatments and said they all work, but they all have risks. That was not terribly helpful. I went to seven different physicians with various kinds of radiation oncology, various kinds of surgery, this and the other. And every one of them knew exactly what I should do and they were all different. Again, where is the science there? Ultimately, I decided on cryoablation because at least it would not do any damage to my organs or create a new cancer risk. But ultimately, it did not work. I had to back it up with external beam radiation, and finally I got cancer free. Talking to doctors did not help. Talking to patients does not help because the vast majority of people treated for prostate cancer get better no matter what treatment they give them. It is a very successful practice. I cannot find out by talking to patients what the relative risk is.
I would suggest a possibility that either we design studies where there are alternative treatments that attempt to get, in a quantitative manner, at the relative risks of and relative benefits of different types of treatments. Or if we are not able to do that, please just say, “I do not know, or, we do not know.”
DR. DARER: I also want to thank the panel for what I thought was just a brilliant series of discussions. My comments really mostly are for Nancy, which I thought was a brilliant framing of an issue. My name is Jonathan Darer. I am the Chief Innovation Officer for the Geisinger Health System. Innovation is this space frequently where you are implementing new things, not necessarily new drug therapies, but new modes of the delivery of care. If I want to evaluate that kind of work, it gets very complicated very quickly. I am permitted to do uncontrolled experiments all the time with no notion of whether they actually improve care. It is a very common thing. And innovation I think is this term that is picking up and nobody really is quite sure where it sits in this world of evaluation.
My comment is really about this culture issue, both from a funding perspective as well as a researcher perspective. I have run into a lot of resistance to this notion from people who consider
themselves to be more pure researchers, to actually improving the quality of care for patients. If they felt like it had a real patient at the end of it, they were not interested. It was not their purview. We even had this notion of this unsafe quality improvement activity. And they were like, “I do not care about that.” I just want to know if it is research or not. I wanted to get your comments from the panel. Is this something that other folks have been seeing, and what is the roadmap toward really bringing this cultural change, which I think needs to happen in order for us to be able to evaluate much more thoughtfully this kind of new world of this combined quality improvement and translational research?
DR. MARGOLIS: This is something that we think a lot about. From a system perspective, we call it playing the whole game. What we talk about at Cincinnati Children’s is the entire trajectory from what happens in the lab to what gets applied to patients. It is a matter of leadership to make it a priority that we are all aimed at the same thing, which is better outcomes for patients. What we found is that when we as leaders work in that way, it is not perfect, but there is much more alignment between the people who consider themselves researchers, the people who consider themselves quality improvement people, and the people who consider themselves doctors or patients about what they are doing and how important it is for their work to fit together. And what it produces, we think, is what we call a derived research agenda, in which the issues that patients and clinicians care about are being brought systematically to the researchers and the quality improvement people to inform the kinds of work that they do.
MR. CLIFFORD: Hi, I am Dave Clifford. I work with PatientsLikeMe. One of the questions that came to mind when Dr. Kass and Alice Leiter were speaking earlier in the panel was, “whose ethics?” We talk about ethical review, but we do not talk about the ethics of whom. If you go to one IRB and you go to another IRB and you go to a third IRB, you have different senses of ethics that are leading them to determine why things should be done. I am wondering if you can comment on collective standards for ethics, especially now that we are looking more at research processes with the patients involved directly with them or commenting or advising to those panels. For example, if I were to have a PCORI grant and it were to be a substantial grant and I had five people that were patients designing that study where in the case of Peter’s work, an institution might override my ability to do that study even if the patients thought there were robust and sufficient protections. I am just wondering if you could speak a little to those balances.
DR. KASS: It is a great question. There are tons of evidence that IRBs make decisions differently, and that has led some people to say, why do we do this review at all? Is the whole thing sort of bogus? But with the other example, we still go to doctors and they give us seven different recommendations too. You can say that is good or bad.
I think ethical norms really do shift. I actually think that even under our current regulatory … there are several of us who think that maybe it is time for a culture shift that would actually result in some changes to the regulatory language. But even short of that, I think that there are a lot of different ways to interpret something, like what does it mean to be respectful to a patient? I think historically what that meant was, you have to tell a patient everything. You need to get a written signature and you need to be extremely protective. That led to a bunch of decisions that resulted in a lot less learning.
There is right now a growing recognition, but I honestly think that it is in part through people hearing more stories like those said this morning. I cannot underscore that enough. That lead people to say—I am a firm believer that people have been trying to do what they thought was the right thing. People start to gain some recognition that maybe the way to be most respectful to
patients is to listen to what they are clamoring for and figure out new models to make sure that they are not exploited and harmed and given bad treatments as far as people can best assess, while honoring what it is that they are trying to get progress around.
MS. DAY: You just basically addressed what I was going to say, please remember in your research that it all comes down to one patient at a time, and that the numbers and the data are individual people and generally suffering people.
We have a new organization in Maine that is going to collect a healthy amount of data from all payers. HealthInfoNet, I think, is what it is called. I think today or tomorrow they will be presenting to the Maine Department of Health and Human Services their project. The concern I had is the opt-in/opt-out for patients. And as a nurse that sat at a triage desk for years and had people sign consents for treatment and consents to release information to insurance companies, the opt-out approach is just against my grain. Could somebody comment on that? It seems that we need to consent for, not consent against. I do not know how else to put that. That is a concern for me.
DR. TRINIDAD: If we can, I would like—I think that one of our talks in the next panel actually is going to come very close to exactly what you are asking about. If we could maybe address that when we get there. If yours is real quick, I have to ask nobody to stand up at this point because we are running behind. I do want to make sure that we do fair by the next panel.
MR. GORMAN: I will be very quick. Mark Gorman. I am a patient advocate. The last exchange here with Nancy—IRBs and stuff prompted me. There is a stakeholder who is lurking in the background of this whole panel who must be brought into the conversation, and that is the legal departments of the institutions and their colleagues. I am really convinced, and I am trained as a lawyer, that a lot of the variability on a lot of these issues is driven by lawyers who are doing what they are trained to do. And if they do not have the context of what patients and clinicians are actually trying to do, a lot of these problems are never going to go away.
DR. TRINIDAD: Thank you very much to our first panel. Now, we are switching gears to our second half. We will start off with hearing from Evette Ludman from the Group Health Research Institute in Seattle. She is a psychologist and senior research associate and an affiliate associate professor in the Department of Psychiatry and Behavioral Sciences at the University of Washington School of Medicine. Her research focuses on designing and evaluating innovative health services interventions to promote health behavior change and improve the quality of care for common, chronic, physical, and mental conditions.
Following Evette, we will have a joint presentation from the folks at PatientsLikeMe. That will be Sally Okun and Laura Phillips. Sally is the vice president for Advocacy, Policy, and Patient Safety. She is responsible for the company’s patient advocacy initiatives and participates and contributes to health policy discussions at the national and global level. She is the company’s liaison with government and regulatory agencies. Laura M. Phillips is a patient member of PatientsLikeMe. She was diagnosed in 1999 with multiple sclerosis after being hospitalized with a debilitating headache.
Following that presentation, we will hear from Greg Biggers from Genomera. He is a patient, caregiver, and innovator and a champion for the consumer voice across all of health care and research. He is also chief instigator and CEO at Genomera, a community fueling the participant-driven research movement, where people move from subjects to research collaborators, and where patients drive the agenda and engage with one another to grow and test health science evidence.
We will wrap up this part of the panel with Holly Potter from Kaiser Permanente. She is the vice president of public relations and oversees efforts to promote the company’s story and achievements through both traditional and social media. In addition, her team is responsible for broad, public relations partnerships, and stakeholder management programs that help to build Kaiser Permanente’s reputation among opinion leaders and partners in the health, business, philanthropic, and advocacy communities.
Thank you very much, panel. We will go ahead and start with Evette Ludman.
Patient Perspectives on Consent for Information Use
Dr. Evette Ludman
DR. LUDMAN: Thank you, Sue. I am excited this morning to be sharing with you some data about what our patients think about data sharing. I am Evette Ludman from the Group Health Research Institute. We do practical research that helps people like you and me and our families stay healthy. We are part of Group Health, a learning health care system.
The context for the data I am going to present this morning builds off what we were talking about this morning. Existing, as well as newer kinds of research, such as genome scale, require large and diverse pools of samples and data. Thus, there is a lot of interest in reusing and pooling existing data sets for efficiency and reliability. But not much is known about what people think about data sharing, especially in the case of data and samples that were already collected for a different purpose.
Group Health in partnership with the University of Washington were a participating site in a network called eMERGE. The eMERGE Network was funded to explore the feasibility of conducting genome-wide association studies using existing research cohorts and phenotypes derived from electronic medical records. All sites were required to submit de-identified study data to dbGaP, a federally administered data repository. Out of all of the eMERGE sites, only the Group Health IRB ruled that living participants in the original research cohort should be asked for their consent to submit their data to dbGaP. Fortunately, we recognized this as a chance to learn about what our members expect and what they would want regarding re-consent for data sharing.
The existing cohort study that was being examined at Group Health is the Adult Changes in Thought (ACT) study. The ACT study is a longitudinal cohort study of aging and dementia. Participants are 65 years or older with no dementia at the time they are enrolled. Currently, there are 2,000 participants ages 65 to 102 and they have been Group Health members for a median of 30 years. ACT study members were sent an informed consent document asking if they would be willing to share their data with dbGaP, the federal repository. Participants were called two to three weeks later if the document was not received back. Our study addressed the following four questions: (1) Will the ACT study participants give consent for data sharing?; (2) What are the reasons, values, and beliefs that drive their decisions about re-consent for data sharing?; (3) Do they feel that the re-consent was needed?; and (4) What do they think about the process used to ask for consent for data sharing?
Question number one. Will the ACT study participants give consent for data sharing? Eighty-six percent of them did. Of those, we recruited 400 for a telephone interview survey. Three hundred and sixty-five participants, or 91 percent of those approached, completed the interview. The telephone survey included a mixture of open-ended questions and forced choice questions.
The first question asked was, what was their main reason for deciding to sign the consent for data sharing? Not surprisingly, generosity and altruism was the number one reason, as this was an elderly population. They said, “This is something I can do. I am too old to volunteer for other stuff, but I can do this.” “As I read the letter, it would not be any benefit to me, but it would help someone else down the line.” “I thought that is not a bad thing to do. I think it is important for people to contribute. If everybody did not want to, what would be the point?”
The other main reason, which echoes what we heard this morning, is a sense of trust. Patients in the study liked and trusted Group Health. They also appreciated being part of the particular original study, the ACT study. And finally, they said, “Why not? It is easy to do.”
We asked in the forced choice format how important or unimportant each reason was in making their decision (see Figure 2-10). As you can see, there is incredibly high endorsement of the importance of all the following reasons: Research could improve patient care, prevent or treat illness. It could help increase knowledge for society. It could help me or someone like me in the future. Group Health researchers are leading this study. And the ACT study researchers are leading this study. These were all important reasons.
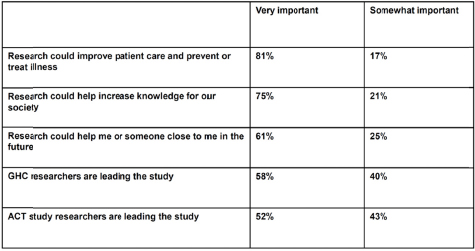
FIGURE 2-10 Importance of reasons in making the decision to be re-consented for the study.
SOURCE: Reprinted with permission from Evette Ludman.
We also asked them about concerns they might have (see Figure 2-11). We asked them about concerns that their privacy would be invaded or that their identity might be revealed. Concern about the kind of research this data bank could be used for in the future. Concern that their information could be used by others for their own profit and concern or confusion about the study itself or not sure what they would have to do about this study. And you can see patients did endorse these things as important, but at a much lower rate than they endorsed the reasons why they would want to participate.
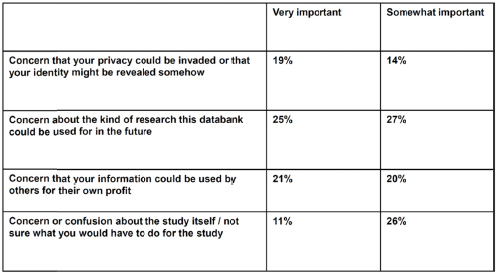
FIGURE 2-11 Importance of concerns related to the re-consent process.
SOURCE: Reprinted with permission from Evette Ludman.
We asked open-ended questions about other concerns, and only 27 individuals mentioned specific concerns. One identified concern was potential misuse of information. One was potential for profit, and finally, privacy concerns. Many of the participants did not have any concerns. They said things like, “I do not think there is anything that you could use it for that would bother me,” or again they mentioned their trust in Group Health or the UW. On the other hand, the word concern may not have been specific enough. Others took it to mean interests. When we asked them about other concerns, they said things like, “I would like them to go into the cancer field.” “I do not see a lot of research with ovarian cancer.”
Finally, we asked them how acceptable would it have been if we had had different types of strategies rather than the opt-in strategy that we used for giving consent for data sharing (see Figure 2-12). What if we sent a letter, asked you to contact us only if you did not want to agree to place your information in the data bank? In other words, an opt-out strategy. About 40 percent said that would be unacceptable. What if we just let you know by letter that we had already sent your information to the data bank, in other words, notification only? You can see a large percentage, about 67 percent, said that would have been unacceptable. And what if we added your research information to the national data bank without telling you or asking for your permission? Also a large percentage (70 percent) said that would be unacceptable.
We asked: How important was it to you that we did ask your permission? Sixty-nine percent said it was very important and 21 percent said it was somewhat important that we asked their permission. Comments about this included the full range of opinion. “It is always important to ask a subject for permission.” “I do not think I would be too upset if you had and did not tell me, but I think it is nice that you let people know.” “You are going through an awful lot of trouble for very little.”
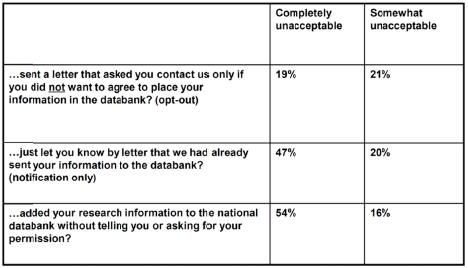
FIGURE 2-12 Acceptability of different types of strategies rather than the opt-in strategy.
SOURCE: Reprinted with permission from Evette Ludman.
In summary, even though our respondents were willing to allow their data to be shared, the majority thought it was important that researchers asked for their active consent. The drivers of participation were belief in value of medical research and trust and appreciation for the health care system, the University of Washington, and the original ACT study that they had been part of. They placed high value on the benefits of health research, trust and appreciation for their health care system, but they also highly valued their personal autonomy.
We conclude that high rates of re-consent do not equal open-ended use of previously collected research data without future need for individual consent. Our consenters endorsed reasons against as well as reasons for consenting to data sharing, although reasons for outweighed concerns in importance.
Finally, I will mention that our ACT study participants are elderly, very altruistic, and have extraordinary trust in Group Health and the ACT study research, yet they still wanted to be asked for permission. This strengthens the argument that re-consent may be appropriate in other situations; or does it? Would a younger cohort be more or less inclined to feel the need to give active consent? I leave that question to you.
New Paradigms for Patient Engagement in Research for Care Improvement
Ms. Sally Okun and Ms. Laura Phillips
MS. OKUN: Good morning. Thank you so much for the opportunity to be here today on behalf of myself and as well my co-presenter, Laura Phillips. I am from PatientsLikeMe and I am delighted to be able to give you a little more information about what we do, why we do it, and how we do it. Laura s going to tell you a little bit about her participation on this site as well.
I am going to start by saying first that, as we heard yesterday and I think as we will hear more today, everything starts with a story in health care. The story is really so personal and important for us to appreciate and understand. I want to give you just a little bit of information about the story behind PatientsLikeMe. It began as a result of the experience of the Heywood family, and who you see here is Steven Heywood. He was diagnosed at the age of 29 with ALS,
a devastating disease. Clearly, his family was overwhelmed with what they would need to do to try to change his outcome. What they found before long was that there really was not going to be a lot of change in outcome. But what they did learn along the way was that there were a lot of people that they were meeting, not clinicians and not researchers, but other patients and family who taught them more than they could ever learn from anything else that they would be able to find in the literature.
The story behind Steven’s experience and his family’s experience is what has motivated PatientsLikeMe to become what it is today, and that is an opportunity for patients and families to be able to connect with each other about what these experiences are like. But I want to be sure that we leave you with this one statement here. Behind every bit of data that we collect and all the data we talk about today is a patient story and getting at that story is really what we are all about. What we try to do is harness the power of patients’ stories to give it some framework, to give it some substance.
What you see here is our home page. I just wanted to give you a sense of a little bit about what patients can do. This is our public home page. You can go to this page and you can click on a number of different links here to learn to connect with patients. About a third of our patients, we have 180,000 of them today, over that at this point, but about a third of them have their profiles public. You could click in there, connect to start to find patients who might be like you or a family member with a condition that they share, and you would be able to find people who have publicly put their profiles out there for you to be able to look at and review.
But the other piece of this that I think is important is to keep in mind that we have about 1,800 conditions represented. While we started out with some very serious neurological conditions, ALS being included, and you will hear more from Laura about MS, we actually have expanded that platform quite dramatically over the last year and a half, and it is really starting to represent some very unusual and rare conditions for which there are very few people who ever find each other around the globe who are now connecting with each other. I think this has come up a lot and I want to reinforce this. This is really important. These are our core values. One of the things that we decided early on—and these have stood the test of time from the very beginning 7 years ago—it is patients first. That if we do not put patients first, we will not be able to engender their trust. We have to have their trust in order for us to be able to get the data that we need in order to be able to inform them about anything new. We have to have openness on the platform. Patients come into the system knowing that the data they are going to be sharing within the system is going to be viewable by other patients. If they decide to make their profile public, which is something they have to opt-in to do, so they have to give permission to do that, it will also be shared on the Internet.
But we speak about transparency a lot. We try very hard to be sure that we are transparent with our patients about what we are using the data for when we actually do aggregate it and share that for use. We want to create wow.
I think one thing I want to be sure that people do know here is our site is free to patients. We accept no advertising on this site at all. There is no cluttering of the view for the patient with any other kinds of information other than patient-reported data. Our business model is that we aggregate the data. We de-identify it, aggregate it, make it available to people, researchers, academics, pharmaceutical companies who are looking for some patient insight, and make that available to them at a cost. That is our business model and it seems to have started to take some understanding within the system to realize that this is a way of being able to get data that is
important about patients’ experiences without necessarily having other burdens on the patient as far as charges are concerned.
We take their stories. We transform their stories into data. This process is sort of an outline. They come in. They create a profile. They find support from some other patients. They might find some other people that they want to connect with. They can learn from our aggregated reports. They can download a doctor visit sheet when they go to see their physicians or the clinicians. And ultimately, they can play an integral role in their own health care.
I want to bring attention to this and then I am going to be introducing Laura’s section here. This is a fundamental question that we sought to address as we created this site. One thing that we believe in firmly is that if patients give us something, we need to give them something back. I heard a little of that earlier this morning, I think, with Peter’s project, that you really need to be sure that you are always giving something back for the time patients will take to give the data that they have given. But what we want to be able to do is help people answer this question. Given my status, what is the best outcome I can hope to achieve, and how do I get there? And we put hope in there purposely. It is not a given that we are going to be able to help people achieve cure for all of the conditions that we might have within the system, nor will we in our research or in our clinical trials, but we want to give them hope. That is a key component. I am going to turn this over to Laura and let her introduce herself.
MS. PHILLIPS: I am Laura Phillips. I have been a member of PatientsLikeMe since 2008. I want you to know how PatientsLikeMe has changed my life. It really saved me. When you go to the doctors and you get diagnosed, they give you information. They send you home. What do you do? You have nobody to talk to. They cannot tell you who to go talk to because they cannot give you the names of any other patients.
Going to PatientsLikeMe, you get to talk to hundreds of other patients with your same condition and same concerns. You get out of the fishbowl and you can look out and talk to other people and get ideas and learn about the treatments and what treatment is best and why this treatment worked for them and why this person liked that. You cannot describe it well enough.
You put your profile out. Other people can go and look at it. Twelve thousand people have looked at mine to see if I had anything in common with them that they can contact me on. Your own records. You are responsible for your own records. It is important to keep track of your own records so you can look back and say I was on this drug and I stopped it at some point. I do not remember when it was. I can go back and look. It is really important for patients to keep really good physical records of their own care. And they really need to keep hard copies of any tests that their doctor does for them, blood tests, MRIs, anything. They need to request a copy of that and keep it for themselves. Most patients do not think they are entitled to that. But they really need to do it. It is very important to them. When they go back and look later and see how things progress, they will know what they have done and how they got to where they are going and what they can maybe change at this point to do something different.
They can keep track of their MSRS scores that lets them know how they have progressed, have they improved. The scores can go up, but they can also go down depending on the treatment that you are on. It is important to know. You answer seven questions and that gives you your score. It makes it very easy for you to look at your own thing.
MS. OKUN: I was just going to say that MSRS scores are a “multiple sclerosis rating scale,” and it is something that we actually have validated against other tools to be able to be sure that the kinds of questions we are asking actually are representing quite well and correlating to the symptoms MS patients experience.
MS. PHILLIPS: I have been on three different drugs. The first one did good for a good many years. The second one I did not want to be on, but I had to do something because the first one was not working, and the third one that I am on now was off the market temporarily and that is Tysabri, which is really I think the best treatment out there for many MS patients, if you catch it early enough—I wish I had started it 10 years earlier than I did, but I could not. For me, it is the best treatment out there. I learned a lot about the drug from other patients on the drug starting from the trial all the way through. We have people that were on the trials to get the drug to market. For me, it has been important for me to find and listen to other people on how they have done with the drugs and whatnot.
We need to be able to share our data with other people. Researchers cannot do anything if they do not know what is working and what is not. They need the information. Most of the patients give the information because it might not be able to help me, but I might be able to help my daughter should she come down with it. We do not know if it is hereditary or not. But somebody out there is going to come down with it. They need to know what will and will not work.
MS. OKUN: You think you covered it?
MS. PHILLIPS: I think so.
MS. OKUN: Thank you, Laura. I want to say a couple of things that Laura talked to me about yesterday. One was the issue of data sharing. We have talked about some of that today. For her, data sharing is just so important that she cannot really imagine not sharing her data. That the value of that for her personally is in being able to help other people who have her condition and to be able to then try to improve that situation for them.
But there was another quote that she mentioned yesterday that I do have to share. She did not in this one. And that is that when she goes to her doctor now and she has actually worked with her doctor quite closely, the doctors says to her, “What lesson do you have for me today?” I thought that was a perfect opportunity for us to understand that the physicians and clinicians—we have to say to our patients, “What can you teach me today that I can actually even use with you and then use with my other patients as well?”
I want to move right into the next part of this, which is partnering with our patients for research that matters to them. I have some results here. Some of these are in your packets. Some of them I am not going to go into too much detail on because of time. But I want to bring your attention to this (see Figure 2-13). This was a user survey we did across this site and I just pulled out one of the factors, medication adherence, which is a big economic issue. What we demonstrated was that, across the board, almost all of our conditions (and at the time we had a limited number of conditions) patients were reporting that being on this site actually helped them improve their adherence to their treatment regimens. It was particularly significant in HIV, where drug holiday conversations were quite pervasive on the forum. What a lot of the patients actually did was, they took snapshots of their charts, put them into the forum conversations to show what happened to their viral loads and other symptomatology when they took a drug holiday, and said, “Just do not do it. It is not worth it.” It is incredibly important to have that kind of data sharing happening among patients.
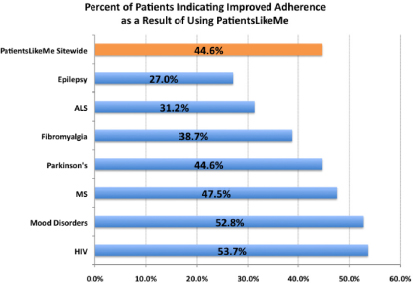
FIGURE 2-13 Percent of patients indicating improved adherence as a result of using PatientsLikeMe.
SOURCE: Reprinted with permission from PatientsLikeMe. Data from Wicks et al., 2010, 2012.
This is our epilepsy user experience and again this is in the packet. It has a lot of information in it. But it was very clear that we had patients who were really learning a lot about things that they did not know about prior. But the one thing that really struck me in this particular survey was that one-third of our epilepsy patients had never spoken with another patient with epilepsy. It is an isolating disease as it is. Imagine that you have never actually had someone else that you could share your experiences with.
The other work that we do is—this was a research project that we did on off-label use. We have a huge amount of data in our system. And patients and their clinicians are working with drugs that have not been approved for the purpose that they are using it for. We believe quite strongly that our data is actually quite useful for us to be able to better understand the prescribing practices on off-label use. I think the good example is ALS patients are using amitriptyline, which was approved in the 1960s for depression. It has never been approved for anything else, although we know we use it for lots of different things. They use it for the primary side effect of dry mouth, because it dries their secretions a d quite effectively actually.
The one study I want to bring your attention to that really brought, I think, a lot of attention to the power of a social media environment was our lithium study that was done in ALS. The original study looked at 16 patients in Italy with 29 controls. It showed that there was some indication that lithium was slowing the progression of ALS. That type of news is quite important for people with ALS. What we were able to show in a relatively short period of time by using historical controls, using a matching algorithm that we created because of all the data that we had, which was functional rating scores, similar end points that are used in clinical trials, was that there was actually no indication that lithium was going to decrease the progression. We did that, and in about 6 months, we had that data. We had 10 times the amount of people that were in the study originally, and actually in the end, three additional studies were funded after our findings at the cost of $30 million; all ended in futility. I think it is just an opportunity to think about a new novel data source. You can also see that whole article written up in Nature Biotech. And then The Wall Street Journal did a little study on that.
I want to introduce you to an exciting new development that has just come out. We have recently been funded by the Robert Wood Johnson Foundation to start an open science initiative, which is going to be doing a partnership with patients and researchers, where we will begin to develop PROs, patient-reported outcome measures, that are actually iterated and worked on within the system. We can have researchers who are coming up with questions, put it out into the field, test it with patients, come back and say this did not go so well. We are going to try a different approach. But we will begin to gain a lot of knowledge about what it is going to take to come up with the right sets of PROs in order to measure patient experiences. We do not have a lot of those that are relevant today. Some of them are quite old. This will all be done in creative comments as well. All of this information will be open. We are quite excited about the opportunity and grateful to Robert Wood Johnson for the funding on that.
I am going to close with something I think we have heard a lot about. One of the things that have resonated a lot over the last day and a half is that we have to listen. This haiku I wrote in response to a—I will say it to you because I know it. “To learn, listen well, to impressions voiced by, patients first.” It encompasses everything we are about and I think it is everything that we have been talking about. We need to learn to listen well and I think we are up to the task.
Thank you very much. And thank you, Laura, so much for your participation.
New Paradigms for Patient Engagement in Research for Care Improvement (Part 2)
Mr. Greg Biggers
MR. BIGGERS: Good morning. I wish a special, good very early morning to those of you watching online from my native land, the Pacific Time zone. In addition to leading Genomera, I am also on the Board of Genetic Alliance. I am helping them as an entrepreneur-in-residence launch some initiatives like Reg4ALL, which I will talk about this morning.
Sue opened our session this morning talking about epistemology, how we know, and identity, who are we. I want to highlight a couple of projects where we are learning new kinds of epistemology and where we are answering I think, maybe not so much who are we, but who is “we.” We see a new form of “we” emerging. In fact, I invite you if you are the twittering tweeting type to join a bunch of us who are using a new hashtag, #thenewwe, to talk about this new world, where we stop othering one another in the research and health care ecosystem and find ways to work together in partnership.
I will talk about a couple of these projects and then also enumerate some cultural principles driving what we are doing. Here is the context for Genomera participant-driven studies. They are a bottleneck, constricting the flow of discovery in health research, the flow of evidence development. There is already a pool of questions that the health sciences should be able to answer. But everyone assumes that getting that work done is constricted by two major factors. It is either the need for government or foundation funding. Here in DC, it is on the news all the time. The sequester is coming and the threats that even agencies like the NIH are under to reduce funding. Or, it is waiting for the mass market economics of the drug industry to get around to caring about whatever a person’s particular question is.
Hopefully, with no offense to my colleagues in the room from the pharma industry, if you look at what is happening there, the drug industry is under threat from absolute pharmageddon as the economics of their system collapses upon itself. We can quickly reach the conclusion that
there is little hope there to solve the long-term problem in health. And the result is too many questions go unanswered.
The Genomera community has found a way to invert those constraints to grow the number of people who can organize and operate health science studies and dramatically grow the number of people who will participate, orchestrated largely through online means, using a cloud-based technology infrastructure to reduce the cost, grow the speed, and serve a matchmaker function connecting the people necessary to dramatically grow the rate of discovery. It is a place where anyone can come with a question that health science could answer. We help them turn that question into a study with a hypothesis to test, with a protocol to follow, inclusion/exclusion criteria, things like that. The basic structure of a typical clinical study or trial made accessible to people who have questions they want to answer.
Then they can launch the study, invite others to join them. In fact, they often invite others to help design the study as it is emerging. People who will join the study follow the protocol on themselves and allow their data to be shared with the group for joint analysis. It is intensely participant-driven health research. And people are applying it to the entire spectrum of health topics, ranging from awfully complex genomics and biomarker discovery to simple surgical outcomes and everything in between. That is a quick vignette about Genomera participants driving research and evidence development.
Next, I want to talk about a new project that was funded by a grant from Sanofi at the end of last year as a winner of their collaborate activate challenge called Reg4ALL, a participant-controlled, cross-disease registry. Reg4ALL grew from a few key insights. While there are plenty of registries sprinkled around the world, industry-controlled registries are often high quality where they exist. But there are too many diseases to cover. And it has been immensely difficult to build sustainable communities of trust in those registries.
Disease advocacy organizations and their registries also lack cross-disease capabilities. They are often hampered by difficult economic sustainability questions in the nonprofit world, and too many organizations feel forced to reinvent the wheel every time they want to spin up a new registry. And all the while we are missing our most important resource, which is people and their data coordinated.
The world has various groups looking for the needles in the haystacks, and great experts are doing this work. But the haystack, it turns out, is made of needles. We are discovering that our subtle health issues influence our acute health issues. Our comorbidities are ignored in our payroll. And rare diseases may contain keys to unlocking more common conditions. In other words, my thyroid condition, my vitiligo, and the effects of an automobile collision are all integral parts of my whole health. It is time for an approach to registries that recognizes that reality, that welcomes people and their data spanning all of health and disease. We are building the software, developing a new kind of governance, and growing a community that will engage together across diseases.
Speaking of culture and the ethics-oriented panel we just heard from, we are doing it in a way with a culture of individualized locus of control as one of the cultural foundations exhibiting a participant-centric approach to everything about the registry, including granular and dynamic consent or a normal person language sharing permissions, so that a member of the Reg4ALL community exercises explicit control over what data they store, for what purposes their data can be used, what projects may use their data or not, and who may or may not contact them for additional studies or follow-up work.
We are seeing two really interesting phenomena across these two projects. The first one is a tremendous appetite to engage. We first watched and are now guiding people through a transformation and how they think about themselves in relation to the research enterprise. Beginning with N is someone else. N equals they. I have a question about my health. I hope that someone somewhere who I am sure I will never meet is in a trial about it, and the results will be written up in JAMA or the New England Journal or Nature or wherever. Eventually, my doctor or I will read about it, and we will know what to do. N equals me in this world of digital health. The data liquidity we just heard about. I ought to be able to ask that data about my own data questions about myself. It is kind of seductive to get in there and look at this. And the quantified self-world is right at this point, N equals me.
But then people realize that in order to handle anomalies, in order to achieve statistical significance on a population basis and to practice good scientific rigor, it is really helpful to work together and come around to this notion of N equals we. In these communities, with our individual locus of control, but expressing it collectively, we are marching into this future. N equals we, an appetite to engage.
The second phenomenon we are seeing is we are watching roles expanding and blurring people, the people doctors call patients. We tend to just call them people. They are moving from subjects to participants to often collaborators in the research endeavor. And ultimately the roadmap goes to people becoming shareholders and the benefits of research. And this continuum of roles and power has been really foundational in our thinking about participation and the governance of these projects.
What are the underlying cultural drivers of this new era of participation, of engagement in health science and development? These are the desires we are seeing over and over again that are now driving the cultural foundation for both of these projects. Let’s just talk through these. This is my last slide actually. I think this is the summary of all that we have experienced in the last 3 years. The first one is control. We want influence over data, tissue, intent, outcomes, and of course, you should ask permission to use my data or tissue and offer the choice to participate. In the age of social networking and tweeting and Facebook and Foursquare, it is not that hard to ask sometimes every time you want to use a piece of data and let me know when you are doing it. We want trust. We do want to cooperate with all of the stakeholders and engage, but it has to be a conversation where a single consent event is replaced by ongoing governance, dynamic choice making where communication is bidirectional. We want impact. This is the part that often goes unsaid, because we assume it is obvious, but let’s make it said. We want impact. In our communities, we are constantly asking ourselves what is at stake, and we join in common cause so that we will make a difference.
We will be shareholders in the benefits, including I think future economic benefits, because we are already shareholders in the misery and in the risks. Let’s be careful here in this room, where we are excited about the new paradigms emerging. Let’s be careful that we do not inadvertently bring to the world new schemes that we call sharing, but really look like a form of data share-cropping rather than true participation. We want to be owners and partners.
And finally, and I think this is the biggest change inflection point we are seeing in this cultural foundation for these projects we are doing, is we are seeing that people want to express their rights in addition to having them protected. It is exciting that we finally have the technologies and tools and policies that help us do that. A bit about these two projects and some cultural underpinnings. Thank you.
Research That Improves Care as a Competitive Advantage: Communicating the Importance of Data Sharing to the Public
Ms. Holly Potter
MS. POTTER: Hello. I am Holly Potter with Kaiser Permanente. Many of you may be familiar with me or familiar with the organization as a nonprofit health plan and care delivery organization. We serve nine million members across the country. In addition, given the makeup of this room, I suspect many of you are familiar with our use of information technology. We have one of the largest electronic health records in the world, with more than nine million members being cared for daily through the use of an electronic health record, and they have access to that data through a personal health record on kp.org.
But what many people are not aware of is we are also one of the largest non-university-based research institutes in the country. We have research institutes in each of our nine operating regions and actually conduct about 2,000 studies per year. In 2012, we published a thousand studies in peer-reviewed journals.
As a learning health care organization, we believe that research is critical to improving our clinical practice on a day-to-day basis. As many of the folks in this room have talked about this morning, there is an acknowledged gap between the evidence and practice that each patient and provider is faced with each and every day. We are very fortunate. I am sure many people in this room were influenced by the 2003 findings of Elizabeth McGlynn that demonstrated just how stark that gap between evidence and practice was. She is now part of the Kaiser Permanente Research Institute. She is leading our Center for Effectiveness and Safety Research, helping us look into how can we more effectively translate research into practice and speed the discovery of what works and what does not work for each individual patient population.
As the introduction earlier noted, I am a communications person. I am in Brand Communication at Kaiser Permanente. I am not a researcher. I am not a doctor. My job is to help various publics, ranging from our workforce to our members to other stakeholders like those in this room, better understand what Kaiser Permanente does for the sake of advancing health research and transforming health care. As I look at that role, I think one of the things that we have struggled with is helping not only our patients, but actually our providers, understand how critical that intersection is between day-to-day practice, our electronic health information, and the research that can result from that, and then ultimately translating that research into practice. This is not a simple concept and it does not come naturally. Helping people better understand the benefits is one of the objectives of the team that I lead.
One of the projects that I wanted to share here today that had some really specific findings about some of those gaps in knowledge is a program called the Research Program for Genes, Environment, and Health. In 2005, we began an endeavor to go beyond the information in our electronic health record and actually begin to systematically collect DNA data from our members. We set a very bold target of a half a million DNA samples so that we could begin to analyze longitudinal health data, genomic information, as well as the environment that our patients live in.
We are very fortunate as an organization that we have members who we often refer to as “sticky.” They are particularly in our regions like Northern California, Southern California. It is not unusual for a member to be with us from the day they are born to the day they die. Because we were an early pioneer in electronic health records, we actually very often have 40 years or
more of clinical information about the patients that we serve. We see that as an opportunity to really dive deeply into better understanding the clinical outcomes that those patients experience. But because some of our patients are also not very mobile, they are not moving from one city to another very frequently. We have patients who have lived in the same city, for example, Richmond, California, since the days of the shipyard, when our health plan was created, and still live there today. What would it mean to analyze their clinical data, their genomic data, and the environment in which they live in to better understand what really influences the clinical outcomes that come to be?
As we began the process of trying to recruit members to donate DNA to this effort, we began with the way everybody does. We send a letter. Very old school. We sent letters to every member in Northern California. I was one of the people who received them. I actually was someone who knew about the study, knew about why we were doing it. And I immediately filled out the first survey and said I want to do this. I want to participate. I was part of the 25 percent response that we got back of people saying, “I am very interested in this.”
Then I got the second packet, which were all the IRB consent forms. I am fairly well educated, fairly well informed. They were hard to understand. It took quite a while to fill that out. I had to fill that paperwork out, submit it, send it in, before I could even get the ability to basically spit in a cup and send my DNA back to the lab.
By the time we went from the 25 percent of people saying absolutely, I am interested in this, I care about this, I want to participate—by the time people went through the actual consent, that dropped down to 5 to 7 percent response within that 25 percent.
Fortunately, we have a very large group of people to start with. To date, we have collected 200,000 DNA samples. We have done genotyping on 100,000 of those samples for an NIH-funded study. But we also recognize that of those that were returned, it was a self-selecting group, and we had a very high percentage of predominately white women, 40 or above, which does not lead to a lot of actionable data if one of our stated intents is to look at the environmental and demographic factors that may be creating health disparities, which is one of the core objectives of this study.
We had to take a step back and really look at what was it going to take to bring in a more diverse set of data. We have tried a couple of things since then. We have done e-mail recruitment and that increased outcomes a little bit. We were able through kp.org, which is our personal health record, to change opt-in features so that people could start receiving requests for participating in this study via e-mail. We have also done clinical interventions. We specifically tested it with pregnant women. And we were able to find an uptick in participants by that doctor-patient conversation. That, while it shows promise, is also very complicated, because if we are looking holistically, number one, doctors do not need another thing on their list to do in their very short time period with their patients.
But in addition, if we want to look holistically at the populations and what is or is not causing clinical outcomes, we need to be looking at the young and healthy and people who are not actually coming into the clinic for services. We are looking at new strategies for reaching those populations and particularly have identified a gap in young men of color who we have not been able to reach through traditional mechanisms. Moving into 2013, we are looking at increasing digital strategies for communicating with those populations and recruiting them to be part of these studies.
Overall, as I noted earlier, these are complex subjects and getting people to understand not only that they are doing something altruistic for the better of science, understanding that there is
an easy in to participation is one of the challenges that we continue to struggle with because of the regulations and expectations of all of the various consent processes. Communications will continue to be a critical piece of this intervention and this effort. But we are hopeful that as we begin to publish information and demonstrate the value of this data, we will be able to continue to recruit people into this program so that we have the data necessary to do really groundbreaking research.
Audience Participation and Open Discussion
Dr. Susan Brown Trinidad (Moderator)
DR. TRINIDAD: Thank you very much. And please join me in thanking the panel and we are getting closer to getting back on time. If the folks in the audience have questions, if people on the webcast have questions and you like to send those in now, we are ready for you.
MS. CAMPBELL: My name is Janet Campbell. I am a software developer. I work on finding ways of giving patients access to their information to engage them more. That is not what my question is about.
I am having a moral quandary actually. I was thinking about this. It is really interesting. I had always taken the perspective that would be consistent with HIPAA, and some of the things that Alice was talking about, that said that if data is de-identified, there is very little potential for harm. I could consent. I would not need to consent, because how would you know it was my data? I started thinking about that though, and realized morally and ethically that if my data was being used by people whose methods I did not agree with, like by big pharma, if I did not agree with the way they practiced this, or if it was being used for purposes that I did not believe in, should I have that ability to offer consent? I think that would be what Gregory would argue.
I was wondering if maybe Nancy or anyone, actually the two panels before, could speak to that trade-off in my moral obligation, or the moral obligation to me, to be able to consent to that, versus the practicality and definitely the self-selection bias that you talked about there as well.
MR. BIGGERS: That is a deep question actually. The two projects that I highlighted today are beginning with populations of people who already know how to make themselves somewhat accessible. And fortunately for the world, those mechanisms are becoming much more widespread very rapidly. In the pioneering phases of this project, the fact that the first people to engage with other people who are already relatively comfortable using the Internet in some form has afforded us I think a temporary flexibility or maybe moral power even to access that moral choice point in a pretty context-specific and broad enough form. I think that we do not know yet how that will be operationalized as we engage with the next group of people and we let them engage with us, and we let them change us and our expectations and our governance.
Because of that, because of some of that uncertainty about how do we do that, making that moral choice accessible enough to each participant, we have emphasized some ethics team kinds of gatherings way up front of the actual operationalizing of the consent process. For example, Reg4ALL has convened an ethics team, not an IRB. These are pre-IRB kinds of things. But an ethics team that is part of the foundational set of teams running the program to help us think way in advance of when those things need to happen. I hope that was not a copout answer, but that is how we are thinking about it so far.
DR. TRINIDAD: I think that is helpful and I think what you are alluding to in terms of participatory governance models moving forward in … we have talked a lot about trust and
groups that are standing, trusted bodies possibly as a trade-off against one-on-one consent processes as things have worked in the past. Let’s go to Matt and then we will go over here.
DR. WYNIA: Matt Wynia from the American Medical Association. I want to continue on this same theme because one of the things that Holly mentioned toward the end was really intriguing to me. There were a couple of reasons why it was challenging, or maybe even inappropriate, to rely on physicians asking patients to enroll. You mentioned a couple of pragmatic things. You only get sick people if you ask doctors to be in charge of enrollment. The concerns we usually have about asking doctors to be in charge of enrollment are that you get implicit pressure on the patient to enroll, because the patient wants to please the doctor often, and that there is a therapeutic misconception risk that the patient may believe that enrollment holds direct therapeutic benefit to them. After all, everything else the doctor offers is supposed to offer direct therapeutic benefits. It gets all the way back to what Nancy started with: the distinction between clinical care and research. And when you start asking doctors to enroll their patients in clinical trials, you worry a good deal about therapeutic misconception and the pressure that could come to bear.
In this instance, I think one could make an argument that in fact, maybe it is not morally obligatory for patients to be enrolled in this, but it is certainly morally praiseworthy. It is a good thing for them to do and their doctor may actually feel that. This gets to—I guess maybe the same thing the prior question was asking about, is to what extent should we use moral suasion or even notions of shame and communitarianism to encourage people to be parts of these shared communities? It is not quite as simple as just opt-in or opt-out. I think there is a sense in which some folks are asking us—I am going to try and be agnostic here—are asking us to use a bit of moral persuasion to get people enrolled and to get people involved and to share their data.
I was involved in a project a few years ago with the Hastings Center, looking at ethics and quality improvement and what kinds of review should quality improvement projects undergo since they do not have an IRB. There were a fair number of people around the table who really strongly believed that when you come to a health care setting, you are in effect taking part in an enterprise where you get benefit from all those other people who allowed their data to be used for quality improvement over the years. As a result, you had an obligation to allow your data also to be used, that there was an implicit agreement. Granted that is an implicit agreement you cannot walk out of. In many instances with QI, you actually cannot segregate those people whose data are being used and those who are not. There are a lot of practical issues there.
I want to ask the moral question about using shame, guilt, or altruism explicitly as a way to engage people in research enterprise.
MS. POTTER: I think in particular for the cohort that we did use physicians to recruit, it was with pregnant women—not only did that have the moral suasion of a physician suggesting they may want to do that, it was also the moral suasion of you can make the world a better place for your child. There certainly is that heartstring to pull. I think there is an altruism that in the health care setting we can bring into that conversation. It is interesting that you talked about physicians being perceived as putting pressure on the patient. At the same time physicians are such a trusted voice for patients, and having that conversation and building that trust about why they are being asked for that information I think is a valuable conversation to have.
MR. BIGGERS: Can I add one quick thing to that? At Reg4ALL, one of the ways we are handling that conflict is we are being cautious to not make any kinds of motivation normative for the whole community. And to help us do this, we are developing a set of guide personae, where you will actually be able to watch a video of somewhere between three and five people who
represent a kind of typed view on what level of sharing they are comfortable with. And one of those people will be almost isolationist. Very privacy concerned. They do not want to share very liberally. They want to be asked every single time. One of those people will be on the far other end of the spectrum. What the quantified self people are sometimes accused of, being data exhibitionists. We will probably have someone like that. There will be a couple in the middle. We are trying not to have that system norm, a certain kind of reason that you are participating, but still let various kinds of participation.
DR. GARDENIER: Turkan Gardenier from Pragmatica Corporation. The database that Holly Parker described of Kaiser Permanente certainly addresses a lot of data gaps that we as researchers trying to link health and environment and locational effects do face. Now, my question is if a private researcher who also happens to be in the past a member of Kaiser Permanente who is doing some research and wants to further her efforts on data gaps, would that be available to people like me? If I do not release their residence or identity, but I want to get groups of people who have lived in certain environmentally exposed areas, for example.
MS. POTTER: We do partner with others outside of Kaiser Permanente. We typically pair those researchers up with our own researchers. And then in addition of course any study that is used with the data is also subject to IRB approval. It would have to go through the traditional processes and be an approved project through all of the standard processes.
DR. GARDENIER: Through your organization?
MS. POTTER: Yes.
DR. GARDENIER: Would you have to go back to the patients?
MS. POTTER: The patient’s information would all be de-identified by the time it reaches the research stage.
DR. TRINIDAD: I am just going to ask to limit questions to the folks who are currently standing so that you all will get a break.
MS. BINGHAM: My name is Paige Bingham. I am with the Medtronic Foundation. One of the quotes that Greg put on his slide was in the 1990s, patients were occasionally invited to the table, and today patients control the table or something along those lines. I raise that question because through the Medtronic Foundation’s philanthropy, we have been able to support patient advocacy groups starting in 1998. One of the groups that we have supported has been the Epilepsy Foundation. Sally commented about PatientsLikeMe and a third of the population of patients indicated that they had epilepsy and had never connected with another individual with the disease, even though Epilepsy Foundation is one of the very strong organizations out there that makes an effort to connect with patients.
I do look at the range of patient organizations from Juvenile Diabetes Research Foundation that I believe a huge percentage of type 1 diabetics and their families are supported by and connect with other type 1 diabetics. And I think of Dr. Frosch’s opening comments where he talked about diabetes and the need to be highly engaged family caregivers from the very beginning. I also think about the Parkinsons Action Network, which is actually meeting these 2 days right now. That is the PAN network going across American Parkinson Disease Association, national Parkinson’s.
There is a combination question here, which is how do patients really get to the table. Who represents them? How do we help organize them so that they have a strong voice? And then also, how do we engage patient organizations to help the access for those that are underserved—the African American males who are not readily participating. I look at the Parkinson’s UK model where they actually are actively engaged with NHS and providing clinical nurses at the regional
centers. That is a philanthropy effort through Parkinson’s UK that really gets into access. We would love to hear the panel talk about patient organizations, the new ones that are developing, the old ones that exist, and how do we help individuals with the disease continue to be empowered. Thank you.
MS. OKUN: Great question. I will let you know a little bit about what we have been doing for a while now. We actually do partner with nonprofit organizations to help them get their patients who might want to be a participant on PatientsLikeMe. And we do that in a few different ways. We may work with that nonprofit and develop what we call a “landing page” that is unique to them. We have a number of those so the MS society and the psoriasis society and a number of others where they provide a link on their sites. We do not want to be siloed. We want to have an opportunity where the good work that is being done in some of these other organizations can come together with what we are trying to do. I think what we can offer is that longitudinal view of what the experience is like, and then provide that social component that could be a link to yours as well.
We have a whole variety of ways of being able to address that. I think it is becoming more and more apparent all the time with some of the very rare diseases that have small groups really that formed at the kitchen table, in fact, and some of them still at the kitchen table where they can come to our environment. We can talk with them. And we do a bit of a trade-off on that. We are looking for them to help them activate their members to become active engagers on our site, so that we can actually gather the data that they might need to answer important questions to that population. We see it as a trade-off and we work with them all the time to try to figure out the best economical way for them to be able to be a participant with us as well as still maintain the mission that they have with their own organization. We welcome that opportunity for any organizations that might want to do that with us. We are very happy to do that.
MS. STERLING: Good morning. MaryAnne Sterling from Sterling Health IT Consulting. I wear many hats, but the most important one is I just started my 17th year, that is 17 years as a caregiver, health care system navigator, and health coach for my aging parents and in-laws, three out of the four of whom have some form of dementia.
The point I want to make is not a new revelation, but I think it bears repeating. As a nation, we need to step up and recognize the critical role played by the family caregiver. We are not only key members of a patient’s care team, but storehouses of rich information for research purposes. I encourage everyone to include the family caregiver in their research initiatives. Sally, I still believe we need CaregiversLikeMe.
MS. OKUN: We have had that conversation before. What we are trying very hard to do is to make our functionality much more robust for caregivers on the site. We are actually seeing more and more children as patients on the site. It is their caregivers and parents who are actually the ones providing a lot of the data entry. We actually are working very hard on that. We have a large autism population. And, again, as I talk about the rare diseases, many of them are with children. We are finding that our functionality for caregivers and their clinicians—we are actually doing some provider portals now as well where we are able to demonstrate if we can make the access available to the clinician as well as the caregiver, the patient’s outcomes will actually improve overall. Thank you.
DR. MONTORI: Victor Montori, Mayo Clinic. A couple of brief points. The first one is that we need to avoid compartmentalizing our heads. Yesterday we were talking very actively of our shared decision making. And obviously one of the choices that patients can make is to participate very actively in the kind of opportunities that you are talking about. Interestingly, I do not know
that there are robust shared decision making offers for people to come in and something like Gregory was mentioning, for instance, those personae they are talking about. There may be some sophisticated ways to help people make informed decisions about participating and beyond consent and other things. Just a compartmentalization alert.
And then the second thing is going back to my previous question, which went unanswered and had to do with the issue of generosity. When you have a generosity base for repository of goodwill and data and it is used to advance science, which is a common good, and then you turn it into a revenue-generating for-profit institution, the risk that I think we run is not fear of misusing those. Of course, they are there. What concerns me is then it becomes an economic transaction. If I participate, what do I get back in terms of dollars? It becomes an economic transaction, and the behavioral economists have pointed out the motivation driven by economic transactions lasts very little. And then the goodwill that was the basis for the enterprise is not recoverable once you introduce the economic transactions. I want to bring that up as an issue and see if there are any comments this time.
MS. POTTER: I would actually love to comment. I think that is something we struggle with every day. We have 9 million patients who entrust us with their data for their patient care. We have the opportunity. We also believe the obligation to mine that data and better understand what drove those outcomes.
With that in mind, we are very strict in terms of how we regulate that usage of that data and are very careful to make sure that we never do anything to betray the trust that our patients have given us. I think as we look at this field right now, trust is something that each of us have to earn. Each of our organizations needs to learn from the patients that we work with to ensure that the data that we use truly advances the science and advances their own clinical outcomes.
MR. BIGGERS: I think the world is facing new ground on this topic, because we are seeing a much more imminent collision of generosity-based communities with economic-based corporations. By law, most for-profit corporations are economic interests, not missional interests. This has always existed. But something feels more imminent about this collision now that is happening in near real time, and I think we will learn a great deal about the conflicts and how to work them out. That is why I introduced us to this term of shareholder-ness, even for patients and participants. But something is shifting. And the network economy is going to look different. But the generosity and the goodwill I am afraid is not sustainable if it is not reciprocal. There is conflict coming.
PARTICIPANT: I just want to make one comment on that and I agree completely. I think it is important as a for-profit company, it is important for us to have those core values. They drive what we do and how we make decisions. I think that there is a tension. It is starting to collide. It is sort of, we are accustomed to having research done in what are typically considered nonprofit and nonprofit-making organizations. But where innovation really lies is within areas where people can invest money into something to try to make a difference within the usual paradigm and come out with something that could be quite different, but that actually is going to have an impact that will be for the betterment of the rest of us.
I think it is important. We have talked about this much. I feel very committed to it, and I know my company is as well, to this concept of trust and building it. And then once you have it, you had better protect it. You had better take care of it. If we are not free and open with what we are doing with the data that we are collecting, and letting patients know how that it is being used, and giving it back to them in a way that they can make useful in things that matter to them, then we will fail to get that trust. We should not then be allowed to continue and be able to collect that
data. There definitely is a tension. It is shifting. I feel it every day, but I feel like there is an opportunity for new innovation when we allow investment in new ideas. I think that would be important to have that on the table. Thanks.
DR. TRINIDAD: Thank you all very much. One last closing thought would be, I struggle sometimes with the problem being defined as a lack of trust. I think there is a problem of trustworthiness that we need to be thoughtful about. I am really appreciative of everyone that has spoken on the panel this morning. I think these are folks who have a handle on how to get at some of these issues. Now, you are off to your breaks. Thank you very much to everyone on this panel and to our earlier panel. Thanks for your attention.
Break
CHANGING EXPECTATIONS: BRINGING TRANSPARENCY TO COST AND QUALITY INFORMATION
Dr. John Santa (Moderator)
DR. SANTA: My name is John Santa and I am the moderator for this panel. I am from Consumer Reports. I am thrilled to be the moderator for this panel. We use the work of these panelists every day at Consumer Reports. We do not always get it right. Advice like they provide is crucial to us.
I am going to go right to the intro. I like to use sports analogies. I think most of you will get these. You should know actually this year I watched Downton Abbey rather than the Super Bowl. But I am not sure that I am familiar enough with it to use Downton Abbey analogies, but they are in my future.
Judy Hibbard is going to start. Judy and I are Oregonians. Like the University of Oregon Ducks where she teaches, she is going to come right at you with a spread offense, no huddle. You are going to need to listen to everything she says, because at any moment she could go right over your head and score. This is a woman whose work really is changing how we are communicating to consumers.
Following Judith, Shoshanna Sofaer. Judith and Shoshanna have teamed up a lot on their work now. Shoshanna is a New Yorker. She will tell you that she is on sabbatical. The New Yorker on sabbatical is like an Oregonian after five cans of Red Bull. Shoshanna is just so great at synthesis. She is so great especially in the question and answer session. Save those questions. She reminds me of that New York Giants receiver who in the Super Bowl, the final drive catches the ball with his head, puts it up against his helmet as he is hit, and manages to keep position of it as he falls and scores. Shoshanna is like that for a lot of really tough questions.
Following Shoshanna is Barbra Rabson from Massachusetts Health Quality Partners. Barbra really is an expert of the art of collaboration. She is in the middle of so much of what goes on in Massachusetts and trying to get the word out about performance and especially performance of physicians. In many respects, as Barbra and I know, she has to deal with the players union, and in Boston that is like dealing with the Red Sox players, a group not very easy to deal with these days. She has done a great job of that.
Dan Wolfson is really the genius behind Choosing Wisely. This guy has managed to get stuff done that many of us try decades to do with physicians and professional societies. He has
managed to get them to step up to their professional responsibilities. Now, Daniel is going to do what every good coach does. He is going to show you some film. He is going to get you right down in the trenches and show you what the interaction between the players on the playing field is like.
The last speaker is Marge Ginsburg. Marge has to be one of the last idealists in California. She actually thinks you can get the owners, players, and fans on the same playing field and get something done. It will be very interesting I think to see what she has to say.
These folks are each going to go 10 minutes. They are on the clock. I am not a replacement referee because our biggest objective is to get to the discussion part because that is what we really want to see—a free-for-all with all of you interacting with them. Thanks to the panelists.
What Patients Perceive as Valuable—and How to Effectively Communicate Information on Cost and Quality
Dr. Shoshanna Sofaer and Dr. Judith Hibbard
DR. SOFAER: To continue as much of a sports analogy as I can possibly pull off, we are doing tag-team. Judy and I have worked together for so long that it comes naturally to us to pass the ball back and forth, so that is what we are going to do.
What we are going to talk about are the challenges. A lot of people want to give consumers information about price and about cost and about resource use. Take a deep breath because this is not easy. In fact, this is potentially dangerous. Judy and I got to do a little study with a lot of help from our friends, including our friend Barbra Rabson, about the challenges in communicating with consumers about cost and resource use. It had two phases. I am going to talk about the first phase. Judy is going to talk about the really needy second phase, where we have an actual randomized trial. And then I am going to wrap up with some of the implications.
The overall study was designed to identify how could we provide consumers with comparative information about provider cost and resource use. We were funded by AHRQ. They should get the credit for this. It was done in collaboration with The Health Collaborative in Cincinnati, Ohio, which was for the first phase, and Massachusetts Health Quality Partners. Let me tell you as a resource how fabulous it is today as opposed to maybe 10 or 20 years ago, to have these kinds of partners out in the field interested in learning, interested in participating in research, and using research. I just want to put that out there because it is a change in what our environment is as researchers.
In the initial exploration, we did focus groups. And in the second phase, we did a Web-based randomized trial of alternative formats for sharing cost information. The three focus groups were conducted in Cincinnati, Ohio, with the folks from the collaborative there. All of them, we should note from a sampling perspective, were people who were getting their insurance through employers. This particular collaborative is particularly influenced by the purchaser stakeholders. That is one of the things that it has in common. And one of the things about that market is that there are a lot of folks in that market whose employers are offering them high deductible health plans or consumer-driven health plans. Of the three puny little focus groups that we did, but there have been more focus groups done since, about two of the three groups were with people who had high-deductible health plans. Note that one would have an expectation that those folks would be more price-sensitive and more cost-sensitive. Not really. Then we also had about half the participants with chronic conditions.
Here is what we found out in these groups. Consumers tend to think that when it comes to medical care, more is better. These are the mountains that we have to climb. Some consumers, many consumers, really equate higher costs with higher quality care. And as Judy says, since that is true in every other part of our economy, we should not be surprised that they have this view, not to mention the fact that the health care delivery system has carefully inculcated these beliefs in consumers these many decades. We should not be surprised.
Many consumers would rather not consider costs in their health care choices. Health insurance is something else. Health care. Some of the people in these groups were flat out offended at the idea that they might have to look at cost and take it into consideration. Also, for these groups of people, the term value, as we will explain, just does not compute the way that we use it. Not going there. For example, we asked consumers to respond to a list of definitions of “high value” in health care. I sent Claudia a handout for you folks, which I hope you will get, which is a list of the statements that we came up with, and we asked people to say which ones they really liked and which ones they really hated. When we said they could pick three of each, they wanted to know could they pick only three of the ones they hated. That tells you where we are going.
All of the definitions that people really liked focused pretty much exclusively on quality. All the definitions they did not like focused only on cost. Consumers are afraid that getting value means getting less than the best quality and this is a core challenge. We need to help people believe that they can get high-quality care at a reasonable price and the term “value” per se does not work, and we still need to do some more work to figure out what works. I am now going to throw the ball to my dear friend Judy Hibbard.
DR. HIBBARD: Thank you, Shoshanna. Good morning. As Shoshanna said, we are really at the beginning of this process of giving consumers information about cost. It reminds me of when we were at the beginning of giving consumers information about quality. We just put it out there and they will come. In this case, they may come to it in a way that we did not intend that they understand and use it.
There are some key challenges and there are some real potential pitfalls with putting out cost information without understanding how consumers may interpret that. In what we learned is that consumers’ greatest concern in looking at cost information and using it is that they do not want to get cut-rate health care. Low cost is scary. In the way that we present information, we have to counteract that.
As Shoshanna said, we did a randomized, Web-based trial, where we tested different ways to present quality information and cost information in a way that would encourage high-value choices, that is, higher quality, lower cost. Our experiment included employees in high-deductible plans as well as those in more traditional plans.
We know that consumers do care about quality, but we also know that they have a hard time understanding and using the information that is out there. And then when you introduce cost into this, you really increase the complexity of what you are doing as well as this overlay of beliefs that you have to deal with.
We tested an approach where we looked at no quality information, where we sent what we called a low or a weak quality signal, where it was, I am sorry to say, like most quality information, a little hard to understand and take in. And then we tried with a strong signal of quality signal, and how did that affect people’s choices and were they more likely to choose high value.
Just to give you some background here. Here is what the no quality signal looked like. There was comparative information. It did not include any quality information. We did actually test different ways of presenting that cost information. I am just showing you one. This is the weak quality signal. The information is there. It is a little hard to determine how these things may relate to quality. The information is not presented in a way that is easy to take in. This was the strong quality signal. It has what I call the 3-second rule, in it that if you cannot see the best options and the worst options in 3 seconds, your presentation does not really work. Here you can pick out I think within 3 seconds at least the top performers and we also showed top performers that were high cost and low cost.
What we found was that when the quality signal was absent, more people were more likely to use cost as a proxy for quality. They would choose higher cost. When we presented the weak quality signal that was moderated just a little bit, still the tendency was to use cost as a proxy for quality and to choose higher cost. When the quality signal was strong, we still saw a little bit of it, but mostly it was gone, that tendency to use cost as a proxy and choose high cost. People were more likely to choose the high value when they could quickly and easily discern that they were not compromising on quality when they chose the lower cost option. We also observed that confidence in choices was stronger when we gave people a strong quality signal.
We also saw and this is true—we have seen this in other work that actually interpreting information for consumers helps them. They are in an unfamiliar territory. And the information is complex often and difficult to use. If you interpret information for the user, it actually is more likely to get used. Our strong signal in a sense did that by saying this is better and this is not. That is a way to interpret data.
But we also interpreted data for people by calling out the high value options. We showed them where the quality was. We showed them about cost. And then we put just a check mark next to the high value options. We actually called it that. But we showed them both, so that they did not trust us that this was both high quality and lower cost. And that did help. And people were more likely to choose high value options when you essentially did some of the cognitive work for them.
Our findings actually did not differ for those who were in a high-deductible plan versus those in a traditional HMO or PPO, which was interesting because these are people who are more exposed to the cost of care. But they still had that core belief that cost is a proxy for quality. Even if they were paying out-of-pocket, they were more likely to make that high-cost choice when they were not sure about the quality.
We also found that the findings did not differ by demographics. And they did not differ based on health status. We did not include people who did not have insurance, as this was all employees.
What are our key takeaways here? Where possible, help people out by interpreting data for them. The task that people face in using comparative quality information is for them to map a good/bad scale onto that information. That is part of the task. If you do that for them, they are more likely to use the information. Instead of saying 80 percent did this and 30 percent did that, say this is good or this is excellent. That helps people.
And then the other really big takeaway is I think we always need to pair cost information with quality information, or show this information within quality strata to upfront address consumers’ worries, that it is okay to choose a lower cost option then, if you are assured of the quality.
I forgot to mention. One of the things that we did learn was we went out with this experiment using dollar signs. One dollar sign, less cost; three dollars signs, more cost. We also tested dollar amounts. We thought this would work because it is easier to take in than actual numbers. But it turned out it did not work very well in the sense that a single dollar sign is actually pretty scary because we know—would you want to stay at the hotel that is the one-dollar sign? Would you want to go to that restaurant? Maybe not. It is too ambiguous and fuzzy. When we actually put the dollar amount in, people were a little more, “that much difference feels okay.” A lot of websites use this dollar approach, and our findings suggested that was not really a good idea.
In addition to pairing cost information with quality information, we want to make it immediately easy to identify high performers across the various measures using that strong signal. That really means one screenshot. People should be able to see their options and not have to hold information in their mind and be able to use the 3-second rule see the best options. Calling out high value can also help consumers.
But I think that the big takeaway here is that if we do not do this right, we have raised the stakes on the quality reporting by adding cost. Because if we do not do it right, we are essentially undermining our purpose. If they do not understand the quality information, they are going to use cost as a proxy and the result will be just the opposite of what was intended. With that, I am going to hand it back to Shoshanna.
DR. SOFAER: What are these negative consequences that we think are going to happen? Not only will the—if this consumer choice thing works at all, that would mean that the market share would shift to the higher cost providers. What I am worried about actually even more is that the lower cost providers will start becoming higher cost providers. Judy was just talking last night about her very first study, about the same time I was doing my very first study in the mid-1980s, was about physician fee information. It was the physicians rather than the patients that were more interested in seeing other physicians’ fee information. One of the things we have learned with quality information is that it is the providers who really pay an enormous amount of attention to this and that changed their behavior in response to it.
I am really worried, as Judy is, about continuing down the line we have been going in terms of a rapid movement toward price transparency. I want to raise some issues that are really broader and underlining. First of all, I really question the quality of the data that we have about cost and resource use in the first place. There were lots of screams and yells about the quality of the quality information that we had, and there were a lot of things put in place to ensure the quality of that information including the creation of the whole organization called the National Quality Forum. We do not have a parallel kind of situation here. We do not know very much about the data.
And anybody who read the Time magazine article from a couple of weeks ago talking about how hospitals bill and what they know about costs would be terrifying to, for example, use the charge master as a basis, which is totally not reality. What we could get really in trouble with is not only that, but using wrong data.
The other thing is that the consumers are not interested, this is very clear, in overall costs. They are interested in the cost to them. They are interested in their out-of-pocket cost. My 25-years-ago research project was how to present out-of-pocket cost proxies to consumers, and they really respond to it. But what we need to recognize is that consumers are not interested in—one of the reasons they are not interested in cost at all is because they figure that is why they have health insurance. That really is why they have health insurance—so they do not have to worry about cost. We have really done a number on ourselves in terms of this situation.
Presenting bad cost data is, I think, worse than presenting no cost data, and presenting cost data alone, even if it is good, is not as good as what we have just said, which is presenting the cost data with the quality data with the framing. Ultimately, we have to work to change the mental model that consumers hold right now. And something like the Choosing Wisely campaign is in one way a step in that direction. But even just the kind of sensitization of the public to what health care costs are all about, the way that Marge Ginsburg does in a lot of her work—these are critical things that are all a part of this situation. I am exactly 33 seconds over. Thank you.
The Road to Increased Patient Engagement Through Public Reporting of Performance Information
Ms. Barbra Rabson
MS. RABSON: Good morning. It is a great honor to be here, and I want to thank the Institute of Medicine for inviting me to be a part of this panel to tell my organization’s story. I am going to talk about the journey that the Massachusetts Health Quality Partners has been on to increase patient engagement through public reporting of performance information. It is a journey that we have been on for quite a while.
First, I will tell you a little bit about my organization. MHQP has been in existence for over 18 years. We are one of the oldest regional health improvement collaboratives in the country. MHQP’s mission is to drive measurable improvements in health care quality, patient’s experiences of care, and use of resources in Massachusetts through both patient and public engagement and through broad-based collaboration. Our commitment is to provide health information you can trust.
The last panel talked a lot about trust. I am also going to mention trust a lot. Trust is key when you are trying to get people to act on information that you give them. MHQP has dual goals of providing trusted information to physicians to improve the care they provide their patients, and providing trusted information to the public so they can better inform their decision making. Sometimes there is a tension between those two goals. The story I will tell shows some of those tensions.
MHQP is a regional health improvement collaborative that brings many stakeholders together; people who provide care, people who pay for care, and people who receive care. We have strong relationships with our physician community. Our governance has included a physician council for more than a decade, which has helped us build trust in the community. That trust is important because we want the physicians to use the data that we provide to them.
We also have a health plan council. The health plans have been a major funder of MHQP’s core measurement work. And just recently in the last 18 months, our Board of Directors established a Patient and Public Engagement Council. This was a result of our board realizing that MHQP is not going to make the improvements in our mission unless we engage patients and the public. While we have had consumer representatives on MHQP’s board for the last decade, we felt it was important to increase our consumer involvement and set up a council on par with our physician council and our health plan council. Members of MHQP’s patient council sit on our board and executive committee, and every other working group that we have. Having the patient voice at the table for all of our work has had a significant impact on MHQP.
By way of background, MHQP has been a national pioneer for publicly reporting physician performance information. Since 2006 we have conducted and publicly reported the results of a statewide patient experience survey of 500 primary care practices in Massachusetts. We have a patient experience survey based on what the Institute of Medicine has said is important in the visit between the patient and the primary care physician (see Figure 2-14). We look at communication, integration of care, knowledge of the patient, and health promotion. We also look at some organizational issues around access, visit-based continuity, and care and service from the office staff. We collect results from 65,000 commercially insured patients in Massachusetts in each survey cycle and have seen solid improvements in patient experiences on all of the dimensions of care.
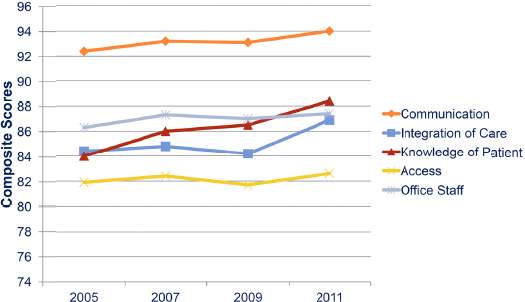
FIGURE 2-14 Patient Experience Survey statewide results—adult primary care.
SOURCE: Reprinted with permission from Massachusetts Health Quality Partners.
Since 2005 MHQP has reported on clinical data using over 30 HEDIS measures at the medical group level for over 150 medical groups. Both reports can be found on our website, and with funding from Robert Wood Johnson as an Aligning Forces for Quality alliance, we are creating a consumer facing website that will make it easier for consumers to access and use MHQP’s performance data. It will look much more like what Judy Hibbard and Shoshanna Sofaer are recommending.
MHQP’s board recently approved a patient and public engagement strategy recognizing that we would not achieve our quality improvement goals without patient engagement. We realized that MHQP will never be a household name and in order to get consumers interested in using MHQP’s data we should partner with a consumer organization. Through a pilot also funded by Robert Wood Johnson we agreed to work together with Consumer Reports to jointly publish a special Massachusetts insert of MHQP’s statewide patient experience survey results. MHQP’s partnership with Consumer Reports was a milestone for MHQP in terms of our commitment to patient and public engagement. We teamed up together because both our organizations value sound data; MHQP has reliable information on physician performance and Consumer Reports has a 75-year history in sharing information with people in a way that helps them make
decisions. Working with Consumer Reports, MHQP was able to share data with 120,000 Massachusetts Consumer Reports subscribers.
However, some of our physicians had a visceral reaction to being rated in Consumer Reports along with toasters and refrigerators. When I say physicians, it was not all physicians. Many of our physicians felt it was much better to have MHQP’s trusted data out there since there is so much garbage on the Web, but others just said, “You have no right to do this.” They felt that it diminished their professionalism. We have a problem here if putting data out to the public in a way that consumers can understand is an affront to physicians’ professional integrity. This is the problem MHQP is navigating.
While the display of the physician ratings was sensitive, the editorial that surrounded the ratings was not. The editorial focused on educating the public about improving their patient clinician relationship rather than finding a new doctor, and included actions for patients to take to improve their own care. The editorial included question from MHQP’s survey such as “How often did your doctor explain things in a way that was easy to understand?” As patients read these questions, they could think about their own experience as a patient and ask themselves, “How often did my doctor explain things?” And then the report noted that in Massachusetts, 84 percent of patients responded “Always.” Maybe your experience was different, maybe worse. The editorial also offered suggestions to get the most from your physician visit such as taking detailed notes, repeating your doctor's instructions back to them to make sure you understand the information, and if you are confused then say so.
The below figure illustrates how the data was displayed using Consumer Reports’ standard display that their subscribers can easily interpret (see Figure 2-15). This display was different than what MHQP had used on its website in the past and some of our physicians were not comfortable with it, but our aim was to present the data in a way that consumers would find meaningful and easy to interpret.
The response was terrific. Here are just some quotes both from Consumer Reports’ surveys and comments we got: This is what transparency looks like. This was an outstanding public service. Thank you. So what? So, Massachusetts residents have a new resource to help choose the best primary care practices. It is a milestone in providing consumers with valid, reliable, and useful health information. Let’s hope consumers take advantage of it.
The day the joint publication went public MHQP had 2,500 hits on our website. Our Facebook activity went up 700 percent. Our Twitter activity went up 200 percent. There were about 4.5 million hits on the stories. Consumer Reports’ newsstand sales went up 110 percent of this edition of the magazine.
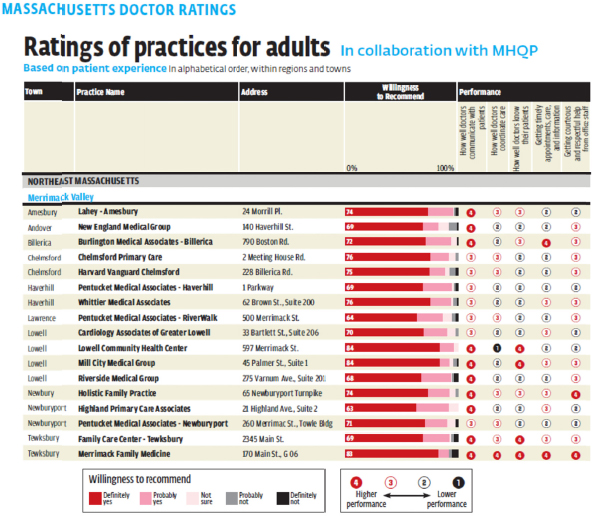
FIGURE 2-15 Massachusetts doctor ratings—Consumer Reports.
SOURCE: Reprinted with permission from Consumer Reports.
As far as lessons learned, there is tension over how physicians want data to be publicly reported and how to present data in a way that is actionable to the public. Partnering with consumer organizations to get trusted performance information is an effective way to engage patients and the public. Physicians do not want to be judged, and they do not want overall summary measures because quality performance is multifaceted and performance can be good in one area and poor in another. Patients want reports to include overall scores that summarize for them whether or not a doctor’s performance is good or bad. Patients want the differences emphasized so that they can make an informed choice based on performance variations. Physicians prefer to minimize differences. We need to publicly report data in a way that is going to engage the public, and the public is eager to see physician performance data, but we also need to be sensitive to physicians’ concerns. Because patients trust and turn to their physicians for care and advice, we must keep the physicians’ trust in the information. We need to be respectful of both s des. It is through open and ongoing dialogue where we identify patient and provider needs and concerns that we will be able to make the progress we need to improve patient engagement through transparency of information. Thank you.
Raising Awareness on Quality and Waste
Mr. Daniel Wolfson
MR. WOLFSON: Thank you for the opportunity. Thank you, IOM. A great job. A great meeting. I appreciate the opportunity to be here. Audience participation. How many people, raise your hand, know anything about the Choosing Wisely campaign? You warm my heart. How many of you actually experienced any unnecessary care in your life or your family? How many have done that? Wow. How many have been harmed by this? Wow. Would you raise your hands again? Could people look around and see that? That is amazing.
I have a story, and I like to tell stories because I think that is a way of getting emotions going around this campaign. It is not a sad story. It is just a friend that had a stress test, age 60. Said the doctor, “You need a stress test.” Well, a lot of people will fail a stress test. It is not unusual. What do you do when you fail a stress test? You get a catheterization. The catheterization showed nothing in my friend, but she had a pain in her leg and she had a burn on her chest. She was harmed, not badly, but unnecessarily.
My son walked in—and by the way, I have a blog. I promote my blog. I tell people that it is actually on a fee-for-service basis and they laugh, which is amazing. We cry when we think about health care being provided in a fee-for-service basis. My son goes into a clinic. He has a cough. He is 26 years old. He goes to the law school here, at American. He has a cough. He gets a chest X-ray. He has been overexposed to radiation unnecessarily. This is a true story. My son is a lawyer. He speaks the truth. He gets an antibiotic. A public health hazard and a hazard to himself. He gets an asthma inhaler. I do not know what for. And he gets a prescription cough medicine instead of Robitussin. The next week he is home. He is fine. He has an enormous bill. This is just stories that you probably have as well about unnecessary care.
I have another question for you. What does Choosing Wisely invoke in you when you hear that name? We think it is a pretty good name. What does it invoke in you when you hear Choosing Wisely? Good.
PARTICIPANT: There is data. There is information. There is knowledge and wisdom. Information that is in the context of experience that turns it into—
MR. WOLFSON: Anybody else? Just one word.
PARTICIPANT: Waste.
MR. WOLFSON: Thank you. To me, it invokes evidence, clinical evidence, and we need much better evidence. We have gone through the experience of doing these recommendations, and the evidence is not as good as it should be. We need better critical judgment about when tests are necessary and when they are not. We have a lot of pulling of triggers in health care now. They are protocol-based and they are not really using clinical judgment. I think last but not least, for this audience. It means patient engagement and informed conversation.
Let me tell you what is Choosing Wisely’s objective. It is an initiative to help physicians and patients engage in informed conversation. We are going to see an informed conversation today. I have a video. I am going to stop talking and show a video, which I am really looking forward to. But now that I see the audience, I am really freaked out because you guys are going to criticize the tape. It is informed conversations about overused tests and procedures and support affects to help patients make smart and effective care choices.
What have we received to date from the Choosing Wisely campaign? We are going to by October 2013—and we have already received 25—but we will have over 40 specialty societies,
each identifying five things, tests and procedures that are not necessary. Under most situations, it is not an absolute. These are not “never events” in most situations, unless there is a red flag or an exception not indicated.
We will have over 200 tests and procedures identified and we are still counting. They will not be, I believe, any major specialty society in America that is not a part of the campaign in October. There are a lot of specialty societies in America as you probably know, and we will not have the tiny ones. But the major ones we will all have by October.
I want to emphasize this. This came out of a foundation, the ABIM Foundation whose goal is to advance professionalism. We have a charter that was produced in 2002 that said something about social justice. It said you must manage resources. It is a physician’s responsibility as a physician to manage resources. The underpinning of this is totally within that, although we do not use that language in the campaign, but we do use it when we talk to physicians about this campaign.
We did 2 years of talking to physicians about this campaign. This just did not come out of our heads. We sat with physicians for 2 years, surveyed them, did focus groups about how we could enter a conversation about resource use. We do not use cost as an item in the campaign. We talk about better care. We talk about removal of waste. And as a by-product of that, if we save money, fine. Actually, one of our recommendations will actually increase cost. We talked about tube feeding, not doing tube feeding on people with advanced dementia and really doing manual feeding. Manual feeding in a nursing home costs more money, but much better care and actually does not kill somebody.
We have, through John Santa, over 35 translations now by Consumer Reports to convert, which are very technical reports. Go to choosingwisely.org to see all the lists. But these translations on Consumer Health Choices have all these translations, easy-to-read, low-literacy formats, some translated into Spanish.
We also produced this because we want this to inform conversation. We want the physicians to be skillful at talking about unnecessary care and having the courage to do that. We want the patient to think about overuse too and have the materials in front of them. It is this informed conversation that I am going to show you in a second. That has been a key point of this campaign. We want to teach the physicians about how to communicate. We teamed up with Drexel University. They have been doing a thing called doc.com for the American Association of Communication in Healthcare for years. We think they did a terrific job. Let me set that up. It is a real doctor, but it is not a real patient. It is an actor or actress in this case.
Here is a conversation. The specialty societies have two to three of these based on recommendations, so real recommendations, conversations, and real recommendations. This one is a generic one that we distribute widely to everybody. What is really neat about this—and this is the technology that we bought—was when they get to the teaching point, it is going to move down. This is how you teach effective and efficient communication skills to physicians. It is a little patronizing to the patient, but it is listening and being empathetic to the patient (see Box 2-7).
Video Shown
BOX 2-7
Script of Video Shown During Mr. Wolfson’s Presentation
Doctor: So Mrs. Rogers, I have done your history. We have done your physical and your neurological exam, and I am happy to say that everything looks really normal.
Actor Patient: It does not feel normal, doc. I have been dealing with this for the past week and it is not getting better. I feel like something is going on.
Doctor: What are you worried about?
Actor Patient: I recently reconnected with a college roommate who told me she had been diagnosed with a brain tumor.
Doctor: I am sorry to hear that.
Actor Patient: Leading up to that diagnosis, she had been having headaches for long periods of time. I am worried that this could be something like that.
Doctor: I understand. You are really concerned. And I can understand given the stress you have and that recent news, that that must be really worrisome for you. But I can tell you that when I did your physical exam, your neurological exam, I took a look behind your eye. There was no sign of any increased pressure that might be symptomatic of a brain tumor. When you looked at your visual fields, and I tested your visual fields and I said look here, look there, there was nothing abnormal about that. That is all very reassuring that this is not related to a tumor. It is really most likely just stress or tension headache.
Actor Patient: You think we should get a CAT scan just to be sure?
Doctor: Well, a CAT scan really is not indicated at this time, because when your history and our physical exam are normal, and when you are looking at tension headaches, we do not need to do a CAT scan at all. Actually, it can pose more harm with unnecessary radiation.
Actor Patient: Really?
Doctor: Absolutely. That is one less test that we have to order. One less thing you have to wait for and be concerned about. Would you feel more reassured if I give you some information on when CAT scans and MRIs are necessary?
Actor Patient: Maybe. Yes.
Doctor: I took the liberty of printing out a handout for you that goes over when CAT scans are necessary for headaches.
MR. WOLFSON: A Consumer Reports is being given to her.
Doctor: And basically, from studies that they have done with people with common headaches, there is no CAT scan necessary. Like we said, it could pose more of a risk. You can take that home and read it.
Now, are there things that we can do to help you reduce your stress to help your headaches?
(End of Video)
MR. WOLFSON: I am way over my time, aren’t I? You are going to yank me. I just want to give you one quote. This is a quote that is in Modern Healthcare this week by a cardiologist—by one doctor in Montana in a conversation with each patient, and later in a note to the referring physician. That doctor cites the Choosing Wisely campaign, a specialty initiative, created to curb overuse. “We have created a medical oncology based on over prescription and over consumption
on the part of both physicians and patients. What Choosing Wisely has done is legitimize our ability to cut back on what is unnecessary.” We have given cover to the health care professionals and patient advocates about overuse. Thank you.
Seeking the Citizen Voice
Ms. Ginsburg
MS. GINSBURG: Good morning. I am here to argue for another role for patients as citizens who are helping to define the principles and values that should govern our most challenging policy dilemmas. I am going to use the term “citizens” and “public” interchangeably, meaning the collective or social perspective, rather than the individual perspective.
Why is a social perspective needed now? The public certainly has plenty on its plate trying to absorb the role of patients. To illustrate, I am going to give you an example of something that came up in the 1990s, a real pharmaceutical breakthrough. I am sure you guys all recognize this. When Viagra was introduced in the mid-1990s, erectile dysfunction went from being a personal annoyance to a ubiquitous medical problem. Kaiser Permanente interestingly took a bold—as it turns out, futile—stand saying that it was not going to cover it. In its explanation, Dr. Sharon Levine, who is a national Kaiser leader, testified. “We must ask ourselves when astronomically expensive new drugs for toenail fungus, afternoon drowsiness, and hay fever come to market at the same time as expensive drugs for conditions that threaten life and cause serious disability, will we be able to create a social consensus on how to balance the costs of each with the benefits derived? Or will we simply avoid responsibility until the entire insurance system comes crashing down around us?”
All the ills of the health care system cannot actually be foisted on to erectile dysfunction. This example illustrates the difficulty of saying no to anything that is new in health care. What makes health care particularly relevant as an issue for a societal perspective is because it is highly individualized and personal to each particular person, but it is paid for communally. When there are more options than resources, as there always will be in health care, then whatever standards are applied should be based on an understanding of social priorities. But how do we begin to understand those priorities?
We have many ways in this country, as you know, of getting public input. I certainly cannot elucidate them all. And they are all important and they are all necessary. But this type of town hall meeting, say, is definitely public input, but it is definitely not public deliberation. What we need by deliberation, really, is the societal version of shared decision making. But with a lay public that sees itself first and foremost as patients and family members, can people switch roles? Can they actually reflect on their inner patient and try to come up with what is acceptable as an outer citizen? You can imagine that some of those challenges will be formidable.
I want to briefly go through what I see as the different roles. How do we articulate the role of the individual as a patient decision maker and the role of the citizen as a societal decision maker? (See Figure 2-16.) As you know obviously, the chart on the left has a number of characteristics that I think all of you are familiar with. The individual in deciding among treatment options considers all the treatment options that are available. It considers the benefits and burdens to them as an individual. It looks at the impact on themselves and their family, reflects on their personal goals and values and the extent to which their treatment options will meet those goals and values, and ultimately their decision is what is in their best interest. But that same person
acting as a citizen in trying to look at what is going to impact the many, rather than impact the individual, has a different role entirely. In this case, they are not looking at necessarily individual treatment options, but looking at different policy options that deal with a particular health care issue … needs to consider the trade-offs among those options, informed by other people’s views, because if it is a societal perspective then it is never about the individual by themselves. We actually do not often know what our own views are when we look societally, until we start talking to others who look like us. Rather than PatientsLikeUs, it is CitizensLikeUs.
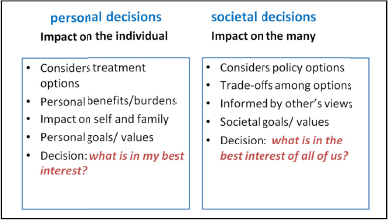
FIGURE 2-16 The impact of different roles in decision making.
SOURCE: Reprinted with permission from the Center for Healthcare Decisions.
And the goal of course is, what are those societal values that we are trying to achieve, if in fact we need to make these difficult decisions—all decisions to be made here from the societal perspective? All have trade-offs. They all have tensions embedded in them. Whatever you pick, someone else is going to disagree with it. It is going to be wrong on one hand, and right on the other. But at the end, the decision is what is in the best interest of all of us.
I want to point—you do have your package of information online that has all the various materials. And of course, I want to call out to you in complete self-interest, on page 182 of your booklet is a chapter on public deliberations that was in the Essential Benefits report that was put together as part of the implementation of the ACA. I would urge you all to memorize it.
What are the kinds of topics that we are talking about that are related particularly to coverage and cost? Not all of public deliberation is about money. There are many other issues that are involved in health care. But right now money is a very big one. Here are examples of projects we have done over the last few years. Should the cost of the treatment ever be a factor in treatment or coverage decisions?
We did a project with Medicaid beneficiaries in California and asked them to figure out how to cut 15 percent out of the budget, which is what the governor was facing several years ago and every year since then. Uninsured Californians design a basic benefits package. We did this preACA. I do not think the government necessarily took our report. They might well have. But we wanted to find out, what does basic mean? How is basic different than not basic? What are those characteristics of health care that are so critical that they absolutely must be covered and which ones should not?
On a project we did last year on the principles of a fair cost-sharing model that we did on behalf of the California Exchange. What I want to do is just—because there is no way to give
you answers to all of what people said. I captured just a few of the quotes that came from a number of these different projects of how people actually react to this role. Putting our personal experiences aside, because there is a lot of stuff on there that I personally would not use, but we are talking about the working people in Sacramento. By the way, they were using a process called CHAT I think some of you may be familiar with. It is a computer simulation that we have used a lot in helping people decide what a health care coverage should really look like when there are more options than there are resources. But what you have here is the recognition. This does not come quickly of someone who realizes, “Oh, wait a second. If we are sitting here trying to decide for a much larger group of people, then what I want may not necessarily be the most important thing and it is time to think about what other people want.”
Another quote. “I think when you are designing it for the whole state, then you have to look at not just individuals, but everybody combined.” This is a breakthrough in thinking. Most people do not know that in fact insurance coverage has to do with pooled risk. Everybody puts in. Some people take out a lot. Some people take out a little. Most of the public thinks health insurance has their name written all over the dollars in there that go to them. The fact that they are sharing these resources and that means one has to look at the needs for everyone is a critical insight.
“I have real mixed feelings about it. It is very expensive and it only happens to a few people, but if it is someone that you care about, it is the biggest deal in the world.” Here we are talking about the tension of do we spend money on something that affects very few people and very expensive, or is it better to spend it on something where a lot of people use, but maybe they could afford it individually—a lot of that tension of what is fair, when in fact you cannot get everything.
“I am just stating why I would want it. We do not have to vote for it, but still I just want to be heard.” This one I really love because what happens in processes like this is that not everybody gets what they want. It is a communal process of making a decision of what is fair. We have someone who says I get it. I am not going to get my way on this one. But my opinion is important and it counts and I want to make sure you know what that is. That is extremely powerful when people decide afterwards whether this process was something that they could live with.
I want to make one point about the project we did with Medi-Cal beneficiaries in California about cutting the budget 15 percent. This was the most uncomfortable project I had ever done, because I thought we were going to be strung up to go to actual beneficiaries and say, “Using this CHAT process takes 15 percent away from what you have now.” I worried that people would just walk out, that they would not want to participate. That was not their response at all. And one of the last questions we asked on a survey question afterwards was “If the Medi-Cal budget is cut, I think it is important for Medi-Cal users to have a role.” And obviously, 89 percent agreed strongly. Give us a voice. Not just our advocates. And there are many consumer advocates whose voices are very important, but the fact that they want to have a voice themselves if something is going to impact them directly.
Current issues. Unfortunately, I do not have time to go over them. There are lots of issues now that are just ripe for civic deliberation. I just want to mention the last one because that is one we are doing. Revisiting Medicare benefits, we are starting this project statewide in California to relook at the way Medicare is designed and what it serves and what it does not serve. We have 20 organizations working with us on this project. I have a handout and a small number of copies.
I am happy to give them for anybody who is interested. We welcome other states as well to join in this, if you want to learn more about it.
Last quote. The wisdom of the masses. “If these decisions were easy, we would not be here.” Thank you.
Audience Participation and Open Discussion
Dr. John Santa (Moderator)
DR. SANTA: Please come to the microphones. Let’s move to the discussion phase.
DR. VOLPP: Kevin Volpp, University of Pennsylvania, Philadelphia, PA. I have a question for Daniel. The Choosing Wisely initiative is something which I think is really amazing, really visionary, really unprecedented. A lot of us are really hoping that this initiative does what you are hoping it will, which is providing cover for physicians to do less of these low-value services.
But one concern is that the reason a lot of these services are on the list is that there have been strong incentives for both the providers and the health systems they work in to provide these services. They are providing them not because they do not know that the value is marginal, but there are a lot of decision-making biases that lead them to think maybe for this patient this is beneficial, even if I understand that for other patients, on average, it is not. I am wondering how you see that evolving. There is obviously somewhat of a shift going to a more population-based financing, but we do not know how far that is going to go and how quickly that is going to go. In the meantime, all these providers are out there in a fee-for-service world where there are very strong incentives to keep doing what they are doing.
DR. WOLFSON: Good question, Kevin. We have the right messenger credibility with the specialty societies and Consumer Reports. We have the right message that has been honed I think pretty well and we have the right time. Is it the right time? If this was 5 years ago, this campaign would go nowhere. I think the environment in some parts of this country is changing toward value. If we do not have that, this campaign is dead in the water. We are hoping that ACOs—any organization that is trying to look at a value equation rather than a volume equation—will want to do this. People who are stuck on fee for service and volume-based will not want to do this campaign. Hopefully, they will be in the minority and they will not look good when we have a different metrics to look at what is value in the system. I totally agree with you. We will not have any uptake unless we have an environment that is conducive.
We have 20, 30 large health systems that are on the phone with us on a quarterly basis telling us what they want to do, including the VA. There are a lot of organizations that want to do this, but there are a lot of organizations that are not ready for it. We need to get the early adopters.
DR. SANTA: I cannot resist. Brent James, Intermountain, elective deliveries at 30 weeks, inappropriate inductions, hard stop on inappropriate inductions. In 2011, he saved Utah $50 million. Reduced inappropriate inductions from 28 percent to 2 percent. The system lost $9 million. The problem is not Brent James and others not doing this, the problem is, why do we still have a system that has spent $9 million on making babies sicker? Good for Brent that he got it done and did not need to keep making money making that baby sick.
DR. WOLFSON: And they have a health plan that helps them. Let me say something about Intermountain, because they have used Choosing Wisely. It is called Choosing Wisely at Intermountain. They put out a brochure. They are having a lecturer with their patients. I asked them—Intermountain, you have the best care, best quality. Why are you doing this Choosing
Wisely thing? They said, “We do not want to be the only one on the cornfield talking about this. We need your backing and the credibility of the specialty societies to keep this moving.”
MR. LEVIN: Thank you, John. Art Levin, Center for Medical Consumers. This is a question for our double play team, for Shoshanna and Judith. I agree and understand about the need to translate and put information data in a format that is easily understandable and recognizable. I wonder if that raises an issue of who is the trusted translator and how do we deal with that. How do we create some way for the public to know which translation is accurate and which is fantasy?
DR. HIBBARD: Thank you for that question. I talked about this in a very blithe way. But it really puts a burden on the report sponsor. It is more responsibility to interpret information than just to simply put it out.
In terms of a trust source, I think we still need that trust regardless of how we put the information out. One thing that supports the trust is when the information is underneath. Up here, we have an overall score or three summary measures that tell us the big picture. But underneath that, you should have the information so that people can see and the same with the cost information and value. That is the overall cost. We can put that check mark there, but we do not want to that conclusion. We want to be able to see the information. But we do not want to overwhelm people with all of the information upfront.
DR. SOFAER: It is a very good question, Art, because I think it has a whole other layer of concern, and that has to do with what happens to the fundamental relationship between a clinician and a patient. We in public reporting, and even in patient engagement, we are often in a situation that really reflects what Barbra Rabson was talking about, and how they have to walk in that narrow corridor in terms of getting patients to be skeptical, helping them understand that all doctors are not spectacular and wonderful human beings, that a large percentage are, but that you do have to be careful. To try to explain the kind of financial pressures that physicians are under is also very terrifying.
We do have to be very careful to not totally undermine positive relationships between clinicians and patients, at the same time that we do, in a sense, say to patients, “You are not insulting your doctor by asking her or him a question.” That is what many of them feel. Or as Dominick’s research has said, they are worried that they are going to be punished, which is wild. I have to tell you. This is not just true of physicians. I have done research with patients about nurses, the most trusted profession, and it is even true with nurses that they are afraid that they are going to get retribution. Let me tell you.
I think we have to keep a watch on this because it is very important that we not go overboard and get everybody to mistrust doctors or mistrust the health system. We have a thousand voices blooming in our society, and a lot of things are going at people. That Time magazine article. One of the things about that Time magazine article was they really gave physicians as a group a pass. It was all about the hospitals that were the evil empire. I commented on that. You get other voices on that.
But the other thing, just practically speaking, we know a good deal about who is and is not trusted. The government—they want the information from the government. They do not necessarily want the government to make the decisions for them. Their employer. It depends. The insurance companies. Forget about it. Medical societies. Not bad. Coalitions like MHQP, independent nonprofit organizations. That is whom they trust. That is whom we really have to go
with. We really need to know also that that landing page that was talked about earlier, that has to say right away who are these people and why should you trust them, otherwise we are lost.
DR. CARMAN: Kristin Carman for the American Institutes for Research. I want to make a couple of quick connectors and then make a small offering of some information if you are interested. The first connector is on Choosing Wisely. We actually met with the ABIM Foundation folks based on the work we did on a communication toolkit that we developed for the California HealthCare Foundation and NBGH. We really focused on this communication about value. There is a lot of talk about cost and value. And what we found is that where you are talking about, Dan, the notion of Choosing Wisely is about applying evidence, the benefit of talking about wise and wide use of resources and Choosing Wisely, and we found—what we communicated is that everyone gets nervous about this notion of when you start talking about value of my health care, you are talking about putting a bargain basement pricing on it. But we can all talk about wise use of resources. We have to do that every day in our life.
It is a really important point, because it also, per Marge’s conversation, starts to nudge people a little bit past just what is in it for me, but starting to think about, I even have to think about managing resources. And suddenly the conversation opens up that everybody has to figure this out. It is a subtle thing, but a really crucial communication piece.
The other thing that I wanted to note back to Dr. Volpp’s comment is, Marge, and we have a framework in the Health Affairs’ recent edition where we talk about a framework for patient engagement—I will talk about it in the far right corner—but we are talking about patients and families and consumers being engaged in decision making and a policy-making level. It is going to have a huge impact on people’s linkage and uptake into all of this as well. This notion of public deliberation and the public being involved in deciding on this architecture, in deciding on what is supposed to be happening at a policy level, I think is going to be much more impactful on an individual level for individuals just as it is for physicians.
And finally I just want to note for those of you interested in public deliberation, AHRQ has just put up on the Effective Health Care website a great deal of early materials from our study. We were doing a very large randomized controlled study of public deliberation on how consumers think about applying evidence in health care to themselves, their physicians, insurers, public entities, and purchasers and otherwise. I do not have the linkage, but it is on the Effective Health Care Program. There is a large literature review and then lots of materials that help starting wrapping your brain around what this looks like and how this method can be used. We will be having findings in a bit.
MS. RABSON: Community forum is what you should be looking for. Can I also just say that Kristin and her team did a fabulous article on public reporting on cost and quality that is in the recent Health Affairs. I put that in the materials that you have. Take a look at that. She does a really nice job talking about how quality reporting tends to come from nonprofit organizations, and then all the cost reporting is separate for, now for-profit, organizations like Castlight that have access to claims and big money. There is this disconnect that we are going to have to reconcile.
MS. MOBLEY: Erica Mobley from the Leapfrog Group, attending on behalf of Leah Binder who expresses her regrets she could not be here today. Shoshanna and Judy, I want to thank you for your fantastic and fascinating work. I cite your studies all the time in talking to a wide variety of stakeholders. I am so grateful that we have that information available.
My question is somewhat related to the last question from this side of the room. Shoshanna already partially answered it. But if we found that people do not trust their employer, health plan,
to provide them with this cost and quality information, and they just assume that it is the employer health plan, trying to save money, are they better off not providing it all? Should this information only be coming from groups like the Massachusetts Coalition that are considered unbiased?
DR. SOFAER: Partner. That is what you have to do. Because when you are part of a multi-stakeholder collaborative of some kind, and you have a partner, that automatically means that it is not just your interest that is there. It has been an interest that has been to some extent moderate. Certainly, we get the message all the time over and over again for AHRQ sites, for the Chartered Value Exchanges, the idea that they are an independent community or state-based collaborative of different stakeholders. That goes over well. You have to use the right language obviously. Or partnering with John Santa.
DR. WOLFSON: I forgot to mention, and thank you for reminding me, that the employers like Leapfrog are a part of the Choosing Wisely campaign, and the National Business Group on Health and the Pacific Business Group on Health came out with an employer kit that you can find on your website as well that explains for an employer to begin to talk to the employees about this. We have received a grant from the Robert Wood Foundation to work with regional health collaboratives. In those regional health collaboratives are usually employers and health plans. People like Barbra are going to hopefully be working with us as well as state societies and specialty societies. I just want to recognize the Leapfrog’s great support and under John Santa’s leadership.
PARTICIPANT: What about adding some patient groups, Daniel?
DR. WOLFSON: We have many groups, including—I will let John answer the question.
DR. SANTA: First of all, let me say I think this is going to be a daunting task. Check out Change Health, who is mostly working through insurers, and see if you can get them to talk to you about the engagement results they are experiencing from their strategy. They reach out and communicate to folks who are covered and say, “You did not get a very good deal on your health care the last time you had an interaction. You did not get the cheapest drug.” They have a very active engagement model. At least from their numbers, they are very impressive. It is going to be hard for organizations like ours to afford that.
In 2013, many of the folks in this room are lining up to purchase physician data. It is expensive. It is complex. I do not know if we will be able to afford it. I think you are going to see in-the-field folks who have very substantial resources and technology who may or may not play by all of these rules and may figure out ways to totally change them.
The one I am most proud of, that a colleague of mine, Tara Montgomery, figured out, is we have a wonderful partner in Choosing Wisely—is Wikipedia, one of the five largest websites in the world. We do not say what is going on in Choosing Wisely. Wikipedians do. And we now have Choosing Wisely content up and a couple hundred Wikipedia pages, topics that are related to the first 45 and getting to work. Wikipedia just launched their Choosing Wisely page a couple of days ago. We are getting to tens of millions of people through Wikipedia. We are going to have to be smart, do things in a variety of out-of-box ways to do this.
MR. WOLFSON: I just want to recognize AARP who is in this room as part of this campaign and the National Partnership for Women and Families is a part of this consumer-oriented side. Thank you for your support.
MS. BRUESSOW: Diane Bruessow, Gay and Lesbian Medical Association. On this panel and throughout the entire discussion, I have heard language using doctor and nurse, health care provider, clinician. As a physician assistant, I am a little more tuned into this and I am actually
looking for more explicit information. But I also understand. It is not just what we are doing in this room and throughout the discussion, but it is also what our patients do. My question is directed toward Barbra and Dan as well. Do you know whether your respondents, when you ask them about their doctor, if they actually are responding as who their primary care provider is that may be inclusive of PAs and NPs? Were you explicit in any way in differentiating? Did you make an explicit decision about saying doctor PA/NP? Can you tell me a little bit about that?
I would actually ask the same question of Dan, if you do not mind putting two questions out there. There are, I think, 100,000 members of AAPA and we practice so PAs have practiced autonomously. We may not get the kind of—if you are trickle down, it may not happen with autonomous providers and has there been any discussion to broaden the audience?
MS. RABSON: Great question and something we have dealt with for a long time. The survey that we do is actually a survey of the primary care physician. When we send it out, we have the primary care physicians’ name and the first question is our understanding is that you have Dr. Cammack as your physician. And the reason we do that is from a methodological standpoint. If you ground it in a particular individual, people have a better response rate. The response is more reliable.
Having said that, we know that primary care is a team sport. It is not just the primary care physician. In fact, we have a visit continuity question that we threw out because people said—one of the questions was, “Did you get to see your doctor or your clinician?” And if they did not, sometimes—we did not say they said okay. We just said—we are grappling with this. We actually received hate mail from the nurse practitioners. Both my kids were delivered by nurse practitioners and it was horrendous to get hate mail. It is an issue, but it is a methodological issue.
We do a top-down survey based on the claims. We target physicians. Now, in Massachusetts, nurse practitioners are able to bill. We are looking to—they do not always bill under the nurse practitioner. It is an issue that we are on to. We are making some progress. It is really important and we are going to have to get there. Every year we look at our survey and now we are using the patient-centered medical home model. It is even more important that we have that. But there is this challenge from a research perspective about centering this on an individual. We will get there, but it is not there yet.
MR. WOLFSON: We are trying to figure out what our next steps are. This is on the table. I would love to talk to you. It is non-answer. I know.
MS. BRUESSOW: Actually, I would like to introduce you to Jim Delaney who is the president of the AAPA before the meeting is over.
MR. WOLFSON: Good. I would love to talk to him.
MR. DEBRONKART: Stick to your guns, please. In my speaking all over creation, I have heard a lot of responses from different physician communities, local, and medical communities where—
PARTICIPANT: Who should stick to their guns?
MR. DEBRONKART: Dave DeBronkart.
PARTICIPANT: No. Who should stick to their guns?
MR. DEBRONKART: Dave DeBronkart. The message that I heard consistently is there is evidence. There is information out there. I have never in my career seen a profession that screams in protest and whines at any attempt to measure it. The reality is we all have tons of data that some providers are more effective and safer than others. We cannot let that information be buried or disregarded.
Regarding consumer behavior—at a Robert Wood Johnson conference a year and a half ago somebody made the point that it is abusive to keep people uninformed and then insult them for being clueless. That pretty much is the situation. A year and a half ago my COBRA ended and I went on high deductible, $10,000 high deductible. I blogged a lot about this. I will not go into it in depth. But the first thing I got was a CAT scan for $1,736 out of my pocket. Every line item on the EOB said the single word “hospital.” I asked my insurance company and said, what are these? They said, we do not know. I said, what if they are errors or fraud. And they said, if there were, we would do something. I am not kidding.
Many years ago in my career, I got involved with a professional supervisory discipline called HPT, Human Performance Technology. And if an employee is failing to do a particular task, you have to consider, do they know how to do it. Do they know when they are supposed to do it? Do they have the necessary information? It is a mistake, a trouble-shooting mistake, a diagnostic error to not consider whether the person clearly had the information—this is where they do the cognitive work. Give them the equivalent of a Consumer Reports car reliability guide. Please let’s do that.
Literacy. The term “health literacy.” It drives me nuts. Even the article about a health literate care model in Health Affairs. The interventions—I have always said you cannot discuss literacy unless you discuss in the same breath the clarity of what they were presented. The interventions described in the article were all about improving the clarity, but they still call it literacy. Do what we can to put the information clearly in the consumer’s hands, and then we will see whether people know what they are talking about.
This is so persuasive. At TEDMED last year, the chief medical officer for Quest Labs gave an insulting talk about how patients make lousy consumers. While in the process of shopping for my next CAT scan, I call his lab to see what the blood tests would cost. He said the lab said, “We do not know. Ask your insurance company.” I called them and they said, “We do not know.” I could go on and on.
The bottom line of all this is given that—I would say, Judy and Shoshanna, uninformed consumers think that more expensive is better. Can we design some interventions? Treat that as a baseline. Design some interventions and measure afterwards.
DR. SOFAER: I think we would love to do that. I think we do not really know how, Dave. That is the reality. I think going back to the word you used, John, this is daunting to change the minds of people. In the meantime, what we are suggesting is at least, do not make it worse. At least give patients and consumers a chance to not have to overspend.
MR. DEBRONKART: Before I sit down, my great concern is that with the coming changes in medicine, this is not just a matter of wrapping up the bad performance. I want the best performance to be rewarded and how can consumers choose that if they do not have the information?
DR. SANTA: Let’s be as efficient as possible.
MS. RABSON: Just one response about sharing cost and quality information. Even though we have quality information and we have cost information, they do not align. For example, how much does this mammogram cost? Did your doctor’s office recommend a mammogram? Was it an effective mammogram? Did you get the results? We have a long way to go even on the measurement road and moving into specialty measures and the data. Daunting is the right word, since it is sort of a 360 how to present it, but also getting access to the right data.
MR. WOLFSON: I caution addressing the public about cost at this time still. I think we just got out of rationing and death panels, and we are not out of them yet, probably. But I think we are getting out of there. I think couching this discussion in a different way will help us, and talking about cost will get us back to rationing in-depth panels. It drives me nuts when people are talking about end-of-life and they say it saves money. I am not sure it does and I would not want to frame it in that conversation like that.
DR. MARGOLIS: I am Peter Margolis from Cincinnati Children’s. I am interested actually in hearing a little bit about how you are thinking about presenting data over the next couple of years. I see what you are doing now. And as obviously somebody who is interested in transparency, it is important to me.
I also look at data transparency from a systems engineering perspective. Most of the variation that we see among physicians is actually due to the system in which physicians practice. That system includes board recertification and payment and training and data feedback and all kinds of things. The variation is relatively small among physician practices. There are some physician practices that are outliers and outperform everybody else.
If our real goal is to cause improvements in outcomes to take place, it seems to me that we want to use data presentation in order to stimulate action among caregivers, rather than fear. Can you just talk a little bit how you see this evolving over the next couple of years, what you would like to do in the future, and how you imagine doing experiments, and whether there are opportunities to do experiments and how to do this better?
DR. HIBBARD: What we are going to see is more linkages between where people are going on the Web and the kind of comparative data. If people are going to read about knee replacements, they may not be thinking of the issues that they should be thinking of, and embedding in those sites, WebMD or the different sites that people are going to go to learn about their condition or their procedure, that will then highlight for them that these are the things to be thinking about. Here is some comparative data for your region to think about.
The other issue that I see emerging is that comparative performance data, especially on procedures, does not address the issue of appropriateness often. One of the things that we can do is, when we are presenting comparative outcome data on hip replacement or knee replacement or especially the back surgeries, where appropriateness is a big issues, is to embed in those sites decision support. Wait a minute. Not everyone benefits from back surgery. Are you going to benefit, and use this button to find out about for you, if back surgery is right. Those are some directions that I see.
DR. SOFAER: I just want to mention that the Agency for Healthcare Research and Quality has just started a new initiative called Improving the Science of Public Reporting. The three of us are all involved with one of the projects that we were funded, as is Kristin Carman, who spoke a couple of moments ago. She is actually leading the project. These are all efforts to use R21s, which are more exploratory research, to push those boundaries in public reporting.
What we are focusing on is what Judy was talking about: linkages between the kind of information that people are naturally looking for and the kind of information that we would like them to see. We happened to have chosen childbirth as our focal point because that is what we call a shoppable condition. But I think we really do have to start thinking out of the box.
And a project that I was involved several years ago, it became very clear that really patient engagement needed to be the overarching frame in which comparative quality cost information is put out there. If you look at the engagement of behavior framework that the Center for
Advancing Health has issued with 42 behaviors that represent engagement, one whole bucket of that is choosing and using your providers.
You can also give people information that they can use because we think about this all and it’s about choice. But what about asking your doctor some specific questions and giving people advice about what questions to ask based on what the information is. I have to tell you. As good as we can make it, it is boring. I have been doing this for a long time. It is not terribly interesting. I helped Barbra with her first issue of her public report. Compared to most of the things that I look at on the Web, it is boring.
MR. SANTA: Just a quick comment. We are not going to be boring. We are going to take the folks who are not trusted by consumers and we are going to attack them. We are going to attack the drug industry, the device industry, and I am sad to say, hospitals. We are going to attack them on safety. We are not going to break anything that cannot be fixed. But when there is a fix, we are going to attack them and attack them and attack them. We are going to collaborate with physicians because we think they are still capable of behaving professionally. Let’s hope we are right.
MR. ALSTON: Chuck Alston with MSL Washington. My perspective is based on 6 years of research with Aligning Forces for Quality. And just for what it is worth, almost word for word our research validates everything that was said this morning, with one exception, and maybe Tresa is going to talk about it this afternoon. We did focus groups last year. Part of the groups was Medicare patients that had supplemental coverage. Part of the other groups was people with thousand dollars and up deductibles. They were two separate conversations that bore no resemblance to one another. We began to see some things in the high deductible that we had never heard before. Now, we were not doing choice architecture like you were. We were just having a discussion because RWJ wanted to take the temperature. The anger was palpable. People on their own brought up tests that did not need to be done or procedures that did not need to be done. This was unsolicited. And in 6 years of doing work on quality, cost, we had never heard anything like this before.
There is something changing out there, now that the price is being made apparent and that they see that there is a cost other than their insurance premium, and it was also worth noting that everybody and every group knew their premium down to the penny that they paid each month.
MS. ROHRBACH: I am reporting questions from the webcast. The first is from Kevin Kenworth of the Health Research and Educational Trust who asks, “With such variability in costs for the same treatments and procedures, how are these costs determined and how is this cost information explained to the patient?”
I have a second question from Alan Kaplan who is the co-author of a recent review paper called Family Caregiver Alliance and he directs his question to Mr. Wolfson asking, “Can you comment on the possible impact on the Choosing Wisely campaign on the standard of care and malpractice litigation?”
DR. SANTA: Why don’t you do the second one first?
MR. WOLFSON: That is a really good question. What I have heard is two sides. One side is you develop a new standard that people could shield from liability. The other side of course is you are not doing a test. You are exposing yourself to more liability. I do not know the answer. I would think that doing the right thing is more defensible. I also think there is a flip side. You did the wrong thing and you hurt somebody. You did something unnecessary and you hurt somebody. I think that will certainly count as being liable.
But this is a big concern of a lot of physicians. Emergency room physicians are coming to see
me based on this notion that we should get involved in medical tort reform. I do not know where we stand except we want to keep focused on what we are trying to do. But it is a huge issue. It is real. It is real because it is in the minds of physicians when they do tests and procedures and saying I have to cover my basis. Of the many things that drive overuse, there is certainly a lot to say about liability.
DR. SANTA: Let me try the first question. Go to NQF. There is a variety of cost measures that have been approved by NQF. NCQA, for example, has RRUs, relative resource units. They are by diseases. For example, heart disease, diabetes, COPD I think. Look at those methodologies.
One that we have found very interesting and we have written about is the HealthPartners comprehensive cost measures, the only NQF comprehensive cost measure that has been approved. To HealthPartners’ credit, they have put it in the public domain. You can look at all the information on their website. They will help you understand it. I think it is a first and really important step in terms of understanding cost.
MR. WOLFSON: I am serving on an NQF cost measure committee that will look at it again.
DR. BELKORA: Jeff Belkora from the University of California, San Francisco. I would like to ask Daniel if he could comment a little bit on—I was encouraged about the idea that the Choosing Wisely campaign is not just about overuse. It is also about underuse. For example, with the story you told about in-person feeding as opposed to tube feeding. I wonder if that is something that can be more emphasized because, as a consumer, I am suspicious of focusing on just one side of the equation. I think there are a lot of people in our system who are at risk for underuse. I understand that in orthopedics, for example, older and minority patients may not be getting access to hip and knee replacement surgeries that actually maybe appropriate and underused in those populations. It would seem to me that telling the Goldilocks’ story about Choosing Wisely, that it is about getting it just right. In some cases, that is going to mean more treatment. In many cases, it is going to mean less. Is that some direction you are going?
MR. WOLFSON: We certainly want to get the message across about appropriate care and best care. Frankly, some of us have been working for 30 years on underuse. I think it is about time we focused solely on overuse. Our campaign is going to continue to look at overuse. Waste is the beginning of a conversation. We hope that we can evolve maybe into more difficult conversations about marginal benefit, palliative care, and end of life. We wanted to start with the basic. We are a small foundation. We are leveraging lots of organizations out there in trying to stimulate them. I think if we changed our message to underuse, we would not get across our objectives.
DR. BELKORA: I am not suggesting you change the message to underuse. I am suggesting that maybe you put aside your personal history or the collective personal history people who had been working on it or do not feel like that is—I think it is a credibility issue for consumers. I think it is a big mistake to say Choosing Wisely, your message, your brand is perfectly suited to saying we need to thread the needle and get appropriate care, and in many cases, maybe the majority of cases, we are worried about overuse. Maybe higher risk if you have insurance. And you are not in a marginalized or underserved community. You are maybe at higher risk of being exposed to the risk of overuse. But there are many people who are exposed to the risk of underuse. It is just a recommendation I would have.
DR. SANTA: Let me share with you that in our consumer translations, we have heard over and over again if you break it, you have to fix it. If you tell me what not to do, you need to tell me what to do. The section that we have on what you should do is the most popular section and
actually people want to hear about what they should do that does not involve a physician, that they do not need to go to a physician for. You are right. I think you are on the right track. I think we are trying to do both.
DR. SOFAER: We did something in the three Cincinnati groups and then we did another eight groups for the Robert Wood Johnson Foundation Aligning Forces for Quality. There was one thing that we did in those groups, which was different from anything else. And that is that we used something that is called a Prometheus model, which was set up as a reimbursement model. What Prometheus does is it breaks health care costs into two buckets. In some circumstances, those two buckets are in reverse relationship to each other. Let me explain. The first bucket is getting typical, what one might call “recommended care” for a chronic condition. It is the cost of that typical care. And then there are the costs of the avoidable complications related to that condition. When we show people a chart, which I do not have with me, that shows the relationship and compares doctors in terms of how they do on these two buckets, a fascinating thing happens. The consumers interpret the bucket with avoidable complications as a quality measure inherently, because their view is avoidable complications should not happen. That is bad quality care. If they are getting more avoidable complications, they are a bad doctor.
What is fascinating to me though is that by doing that breakdown, we are implicitly saying some costs are good. You need to get what you need to get because if you do not get what you need to get, you may end up with all of these other expenses that were essentially avoidable and often even higher than what it would cost to do that. That is a very complex set of ideas. We were kind of stunned in our groups that people got it and that they immediately started to interpret this number, the cost for avoidable complications, as a very acceptable quality measure. I think we have to be very creative about this.
MS. RICH: My name is Pamela Rich and I am from the National Business Group on Health. We are a membership organization of over 360 large companies. I would like to add a perspective to the mix when it comes to the employer and price transparency and quality transparency tools. This is something that we have been working on for quite some time with our members and something we hear about all the time. It takes a big cultural change as has been mentioned. Employers, consumers for that matter, do not know how to shop for health care. They know how to shop for everything else, but they do not know how to shop for care.
We are hearing all the time about our members who are large employers taking upon themselves to partner with transparency vendors like Castlight, like Change Healthcare, like Truven Health to implement price transparency tools that offer not only prices for services, but quality metrics as well and do what we talked about earlier. Embedding information into these tools so that employees can find a decision aid, can find information about their health care need, and it is all in one place. From what our employers have told us about the engagement levels, they are off the charts. Once employees know how to do this, they go back and they do it over and over again for the services that they can.
Although this is a daunting task, I think it can be done and I think that there is hope for Americans being able to shop for services. I just hope that once the health care exchanges open up, the private marketplaces, that these tools will also be available in those.
PARTICIPANT: National Business Group on Health is a member of the Choosing Wisely campaign.
MS. DAY: Kathy Day, patient safety activist. We have not had a lot of conversation about the uninsured here, and I think we have to really keep that in mind. A lot of us who are insured tend to be a little bit smug when we approach our own health care and I am one of them. When I
faced surgery for uterine cancer 2 years ago, I heard from my first doctor that, because of my girth, I needed robotic surgery. I went to the second doctor and she did not guarantee that up front, but she went for robotic surgery. I looked for all of the complications. I connected with other patients online. I researched. I made phone calls. It is hard to get quality information. I did not even consider getting cost information because I have this great federal insurance plan. My husband is a federal retiree. Don’t shoot me, please. I did not even consider the cost. But I did get an itemized bill because I am interested, and it blew me away. I had a bill for $44,000 for an overnight stay after I had robotic surgery. Some of those little tiny disposable instruments that go on the end of the five arms of the da Vinci robot were many thousands of dollars. I am a little embarrassed that I did not get an estimate.
When I take Louie, that is my Pekinese Maltese mix, to the vet, they give me an estimate. And then I can sit with the doctor and I can ask out of these four or five diagnostic measures, which are the priorities. Which one or two are the priorities? That is the exact kind of conversations I think that we need to be having, all of us, with our providers when we approach health care.
DR. SANTA: Thank you. We have 4 minutes. Two questioners left. Go ahead.
MS. KORNBLAU: Barbara Kornblau, the Society for Participatory Medicine. I want to go back to the example of the feeding tube versus feeding. In a prior life, I was an occupational therapist and I taught people in nursing homes to feed themselves. And what would happen is they would say to me you cannot make that recommendation, because in order for it to be skilled care, they need the feeding tube. Number one. Number two, there was not enough staff. Because there was not enough staff, my clients would aspirate and they would yell at me and say, “You said she could eat.” Well, if you feed at a normal pace or you allow her to feed yourself, she can eat. I think that is why everybody in nursing homes has tubes. When nursing homes are owned by hedge funds, the only thing they can cut back on is staff.
DR. MONTORI: Victor Montori, Mayo Clinic. First, congratulations for fighting against the corruption in health care, which is I think—that is the word that came to mind when you asked what word comes to mind about Choosing Wisely, for me was corruption because—care about itself and how to get bigger than about patients. This is trying to revert that. I congratulate you for what is going to be a great battle. I want to join you.
The second thing is that that battle has some interesting edges. When do you get quick wins and when do you keep pushing? We heard one about a second ago regarding robotic surgery. JAMA this week has an article showing that for that particular kind of procedure—that it was for benign disease—robotic surgery for hysterectomy is not superior to laparoscopic surgery and costs more money. If somebody had to choose wisely, they would have to choose against robotic surgery in that circumstance. There will be some edges that have to be crossed over in that situation, and some fights will have to be fought. They may need to be prioritized lower for the campaign to be successful. I am interested to hear about the strategy related to that.
And related to that issue, there is good evidence that for-profit hospitals and for-profit dialysis facilities are associated with higher mortality and higher cost. If one were to choose wisely, one should avoid for-profit hospitals and for-profit dialysis units. And again, we have problems with crossing certain ages and bumping into some toes. I would like some comments in regard to that.
MR. WOLFSON: I think you brought up a marginal benefit discussion, and whether we move away from $210 billion worth of waste and go to marginal benefit is an open question for us. Some people are saying keep focused on just waste. If we take out that, that will be great.
Marginal benefit is very difficult. I think if we are going to do that, we are going to study for about 2 years about how to talk about it. Right now, we have no way of thinking about how to talk about it. I am glad Mayo is going to join the campaign. We need everybody in this room to join the campaign. I wish I had time to say that. This campaign will be nothing unless we have everybody in this room participating and doing research to see what is effective in implementation.
DR. SANTA: Just a comment. As my earlier comments suggested, I think we need folks who have both confrontation and collaboration skills. And we need folks who are comfortable around really aggressive conflict and confrontation.
MR. WOLFSON: I will do the collaboration. You do the conflict.
DR. SANTA: I was at a meeting yesterday where industry was over here, doctors over here, consumers. There was a lot of conflict. By the end, it was amazing how everybody said this is the best discussion we have ever had.
PARTICIPANT: With all of this conflict, what is our hope out there for patients to really think like citizens? Do you really think that that is possible? But what do I take back to the docs?
DR. GINSBURG: It actually came up in a discussion group we had in a project called Visible Fairness having to do with the use of cost-effectiveness as a coverage decision. And what one woman said was, “I support it. I get it. I think it should be used, but I do not want to hear it from my doctor when they are taking care of me. Do it behind the scenes, but I want to know is this treatment right for me? If it is not, fine. I do not get it. But do not talk to me that cost went into the equation.” That is the divide. The patient at the bedside and the patient who is now in the voting booth or whatever is that there are only so many miracles you can do to get them to completely merge at the same time. You can bring up cost directly.
But I guess where I am so wedded to is when you take the public and you put them around the table and you ask them to help live it, they are ready for the most part, lots of nuances here, to dump low-value care. The question is do the other stakeholders—are they brave enough to say, “Let’s see how we actually put that into practice in a way that really marries the values of this larger group without totally trampling on the values of the individual”? I think it can be done.
DR. SANTA: Thanks, everyone. Let’s have lunch.
LUNCH KEYNOTE—HOW AMERICAN HEALTH CARE KILLED MY FATHER
Mr. Mark Gorman (Moderator)
MR. GORMAN: So our lunch keynote today is David Goldhill. Christine and I just met David personally, just a few minutes ago. I think we are going to have a very interesting, and possibly even somewhat provocative and challenging, talk from him, but fully in the context of what we have been talking about over the last day and the remainder of our meeting about how to engage patients better.
David is the President and CEO of the Game Show Network, I am not going to read all his background, it is in the materials in the green folder, he has a long and distinguished career in television. We can ask him at some point—are you going to be with us for the rest of the afternoon?
MR. GOLDHILL: No, I will not, unfortunately.
MR. GORMAN: In our brief Q&A after his talk, if you want to ask some preemptive questions about using the mass media to try and get our message across, we might try to pick his brain on that. David is also a son, he has got some prominence in the health care field as a result of his experience with his father’s illness, although that’s not primarily what he’s going to talk about with us today. He also will be speaking to us partly on his experience as a father and as a patient himself. But the principal focus he wants to share with us is his perspective on the topics of our workshop from that of a businessman, a highly successful businessman, dealing with the issues of how to engage patients in making better use of their health care and their health care dollars in our system.
MR. GOLDHILL: Thank you, Mark. I left a shameless plug for my new book up on the screen here. It’s not really what I’m going to talk about today. What I want to talk about relating to the issue of shared decision making is something very radical in our current context. What my work has been about since my father’s death has been looking at health care as an industry. And specifically as an industry serving consumers, what patients are called in everything else.
And one of the questions I ask really is, can we find industrial reasons that it’s so broken? It is unusual to have an industry this size that is so bad at so many things. And that’s probably a moment to say that there are parts of this presentation that may very well offend some of the people in the room. So I want to make clear that I really do come at this from an outsider’s perspective, which doesn’t mean that I don’t have a lot of respect for all the excellent work that’s done in the field, and I hope no one takes it that way. It’s more about comparing what we talk about in health care, how we think about health care, with how we think about everything else.
I will tell you that this book that I’ve written is an argument for rebalancing the system to be a true consumer-driven industry. And when I talk about rebalancing, what I mean is taking us away from assuming there is going to be someone between us—and by us here I mean the patients—and the providers. Almost every interaction is intermediated in this system. And what’s missing is consumers as the direct economic force. There’s a lot of work I know going on in this conference about how this profession can be better at providing care, at being safe, at offering quality, and at providing appropriate amounts of care.
But since the dawn of professions—all professions—we have a lot of data that says no profession is ever very good at reforming itself. Whether we like it or not, the fundamental economic incentives that a society provides drive behavior. I want to come back to that in a second.
Let me just start with why I’m here. This is a picture of my dad and my first son taken about 4 years before his death. We brought my dad into a hospital for precautionary reasons. They admitted him, he was a bit short of breath. Within between 24 and 48 hours, he had developed a series of infections that meant he never left the hospital. We all know the numbers, they’re very large, the type of people who suffer errors, preventable infections, what have you, and the enormous damage that causes. That’s not what I want to talk about.
I think it was 4 or 5 weeks after my dad’s death, I read an article that Atul Gawande wrote about the effort to get hand washing and other sanitary protocols into hospitals. That’s the first time I learned how common hospital-acquired infections were. I had no idea, I’m not part of the health care system. But I learned something else that has really driven everything I’ve written about and thought about since then, which is that it’s really strange that a business needs to be lobbied for a low cost way to save customers’ lives.
I was in the movie theater business. It doesn’t seem like a comparable business. But we had very strict rules on how long between a soda spilling on a floor and it being mopped up. Very
strict. Why? Because someone might slip and fall. You think, “Oh well, you’re just trying to avoid being sued. What difference does it make?” We had very strict rules, and they were enforced. And if you see a well-run movie theater chain, people are spilling stuff all the time and people aren’t sliding around.
Now this isn’t about slipping over sodas, to some degree it’s more complex. But what does it say that these reformers have to run around the country basically begging hospitals to adopt something that costs almost nothing that saves lives? Now if you’re in the profession, you say, “Well, have to do a better job.” If you’re in business, what you say is “something is wrong with those incentives.” “Incentives” is misunderstood, and I want to come back about it. But one of the things that need to be understood about incentives is they’re not just about money. We talk a lot about money in health care, which is really weird, of course, because we deal endlessly in matters of life and death. And my interest in health care, although I will talk a lot about money, isn’t about money. It is about knowing that I’m going to be a patient one day, knowing my kids are going to be patients, still having a mother who is a senior citizen, and recognizing that money is a proxy for quality and the incentives around quality and service. That’s why I’m here.
I mentioned incentives. I must tell you in the time I’ve spent in health care in the last 5 or 6 years, I have been amazed at how many people there are who are near saints. Undoubtedly a lot of you focus on the bad apples and the doctors who shouldn’t be practicing and the institutions who aren’t well run. But I have to tell you I’ve been in the business world my whole life. I was a banker to start off my career. We had nobody in banking who went into banking to make the world a better place. I know I didn’t. But in health care we have a lot of people like that. And so it tells you the power of economic incentives that almost everything that happens in health care, if you step back and stop thinking of health care as special, you can explain by an economic incentive.
There’s one thing I ought to make clear about an economic incentive. It’s not binary. It’s not if Medicare pays you per procedure, you operate on every single patient no matter how healthy. It’s all about at the margin, at the moment where I’m at the border between do I recommend a procedure or not. It’s the marginal physician, the marginal institution, the marginal procedure. That’s where incentives operate. And I notice a lot of people in this field don’t understand that. They’ll say I would never give somebody a drug they didn’t need or a test they didn’t need. That’s not what an incentive is, that’s not how it works. It works at the margin, and that’s what makes it so powerful, is it moves decisions from A to B when they’re close.
There is no escape from incentives. As the communist world found out, you simply cannot eliminate incentives. You can hide them, you can distort them, you can morph them; they always exist. All of us are dominated by incentives. We all have to feed our families and ourselves. The other thing is they’re not static. And this is something that is very much misunderstood by the government. The government thinks it can give you a penalty for killing a patient, we’ve changed the incentives. But it’s static. Real incentives have feedback loops, and I want to come back to that. So, if you want to incent people to use technology, you don’t have meaningful use rules because they’re rules, they’re targets. You have competition. And I want to show how that works in the world outside of health care and why information technology has failed inside of health care.
But first I want to talk about all of the fictions and myths that prevent us from seeing that health care should be a consumer driven industry. And that’s really what I’m going to talk about for the rest of this. All of the things we all believe, we all nod our head at, as absolutely true, that are completely false—and that represent pure IOM thinking, and in some cases in fairness were
true a while ago, but with health care at 18 percent of GDP and a substantial amount of everybody’s consumption, they’re no longer true.
Let me start with the biggest thing we all believe, which is that none of us can afford health care without insurance. Besides the fact that that can’t possibly be true, somebody must pay for it, it’s not true for the overwhelming bulk of our population. So Becky is an actual 23-year-old who started with us 2 years ago. And I sat down and said, if I looked at all of the ways that Becky is going to pay into the health care system over her lifetime, everything, her share of premiums, my share of premiums, I’m just taking out of her pay, where else would I get it from? Her Medicare taxes, the percent of her federal and state taxes that go to fund Medicare and Medicaid, her Medicare premiums down the road, how much is Becky going to put in the system?
I put a couple of big assumptions on this. One is that Becky is the sole breadwinner in her family, which reduces the number. The second is that Becky remains solidly middle class her whole life, which reduces the number. Becky started out earning $35,000 a year, I assumed her income grew 3 percent a year, which historically has been the case in this country for most people just by aging. Just by getting older your income grows. I also assume Becky never gets really sick. She never has meaningful out-of-pocket costs. And then I did one other assumption so absurd that you probably shouldn’t even look at the slide. And that assumption is that health care costs grow only at the CBO’s projections, which are 10 years. And so the balance of Becky’s life, health care costs grow at zero.
I had Becky live to 80 and I had her husband leave her at 65 so she wouldn’t have to pay his bills. So Becky will put almost $1.9 million into our health care system over her life. If I look at her real compensation—what I pay her really, not just her salary but all her benefits and everything—that’s close to 30 percent of what she’ll earn over her life. She’ll fund her kids, she’ll fund her spouse.
For those of you who are skeptical about the analysis, if health care costs grow at zero from now till the end of time, Becky’s number will only be $1.2 million. Now why is this the first slide? Because everything I’m about to say has to be in reference to this slide. We are talking to a population that we’re asking to put in a middle-class lifestyle $1.2 to $1.8 million, if they’re lucky, over their lives. And when you talk about the value of these intermediaries, remember that.
One other thing before I move into this more quickly. Let’s talk about the neediest in our society. So, between Medicare and Medicaid the federal and state governments will spend about $850 billion in subsidy this year on top of what the beneficiaries pay themselves. If we wanted to we could give 100 million people $8,500 a year to spend on their health care. For a family of four that’s $34,000.
I’m not suggesting we do that. But when you think about just the money, remember how much is in the system today. And we think we’re protecting ourselves, what we’re really doing is deluding ourselves. What this system is great at is hiding how much Becky and everyone else is putting in. We all know why we have to have an insurance-based system. You want everyone to agree with you at a health care conference, make the following statement: Only 10 percent of people in the country consume 70 percent of the health care in a year. So we know we must have insurance. So has anyone not heard that statement?
Here is the problem with that statement. One hundred percent of the cars every year are bought by less than 10 percent of the population. One hundred percent of college educations
every year are paid for by less than 10 percent of the population. One hundred percent of the weddings. One hundred percent of the refrigerators. Now, it’s a little unfair, but it’s worth thinking about health care, instead of being something special, as being an expensive good and service that we all use over our lives like all these other things. We use it a lot some years and very little other years. We have tons of industries like that.
Now, health care is a little different because there are some people who every single year are in that top 10 percent who are just sick over their lives for long periods of time. But for most of us we’re going to spend a year or two in that top 10 percent, just like we’re going to buy four or five cars and go to college and maybe send kids to college and have one, two, or three weddings, and buy a refrigerator every decade. Expensive capital goods and services all look like this. Health care is not special. What makes health care special is that the other 90 percent of us use 30 percent. That’s not true in any other good or service. That only 30 percent is over $800 billion a year. By itself it would be the largest consumer industry in the country.
We all know that consumers can’t do the work necessary to be health care consumers. So what’s the point? That’s why we need the system we have now, because there’s somebody out there taking care of it for you. I don’t think anybody who says that has ever looked at any other industry. Because what makes consumer-driven industries consumer-driven is that the providers do all the work. They’re chasing you.
I think a lot of people in health care economics seem to think that Walmart was created when an angry mob marched on Neiman Marcus and said we demand lower prices. What happens in the world outside of health care is somebody wakes up in the morning and says you know how I’m going to make my billion? I’m going to be the low price leader. You think anyone has ever said that in health care? You know how I’m going to make my billion? I’m going to be the service leader. I’m going to be the quality leader. I’m going to be the appropriate amount of medicine leader, and I’m going to invest in that brand and make sure everybody knows about it.
So, all over I hear, well, consumers just can’t possibly—you get hit by a bus, you can’t negotiate your care. So let’s be clear about this. In consumer-driven anything, you don’t negotiate anything. You don’t go into Walmart and say, “Toothpaste, huh? What was the cost of that toothpaste? I only want to pay 5 percent over cost.” They give you a price, they say it’s the price, you pay it or don’t pay it. In our system we have this. This is the real cost of having an intermediary. My son had a ruptured appendix, and he needed an appendectomy, at least according to 99.9 percent of medical literature. He had an emergency appendectomy, and here’s the first response from our insurance company: Our medical reviewer has determined we cannot approve your hospital stay for acute appendicitis, we do not have enough facts to show it was medically necessary.
Now, I don’t blame them. It’s what I would do if I ran an insurance company. Make it as hard as possible, administrative complication goes into the rate base, it’s smart. But whenever somebody says to me the problem with consumer-driven care is consumers have to do so much work, I really wonder what on Earth they’re comparing it to. I’m the CEO of this company that these guys insure. I had to fight with them.
Many of you know who Kenneth Arrow is. He wrote one of the most important policy papers in health care, arguing that information asymmetry between customer and doctor meant that you could never possibly have a functioning market, the customer would just do whatever the doctor said. This is one of those things that I think we’ve outgrown in health care. And we’ve outgrown it for a few reasons. One is we have TripAdvisor, or we have PatientsLikeMe, to be more
specific about our care. And we have a lot of ways that people get information about health care other than from their doctor that truly didn’t exist when Kenneth Arrow wrote 50 years ago.
But here’s what’s more important: we require our patients to do that work. And I know that’s a lot of what the work is going on here. Health care is no longer just about your house is on fire, we have to put it out, we have to fix this. Health care is not like auto repair. It’s increasingly about a variety of treatment alternatives, often long term, involving interaction between the patient and the health care system. That requires patient effort. And so whatever you believe about Kenneth Arrow’s original point, it’s irrelevant. There is no health care system without patient involvement; there are too many decisions patients have to make.
The last thing of course is we’ve now had about 50 years, 60 if you just look at private insurance, of having intermediaries play the role that Kenneth Arrow said they should play; they should be the customer for us. And they’re horrible at it. They’re just unimaginably bad at it. And so if you still think Kenneth Arrow was right, you have to consider the story about the bear and the two guys in the forest. Everybody knows this. The bear is chasing the two guys, one guy stops to change into sneakers. And his friend says you idiot, you can’t outrun a bear. And he says I don’t have to outrun a bear, I just have to outrun you. And so whatever you think about the theoretical correctness of Kenneth Arrow, all we have to do as consumers is be better than intermediaries for the system to be a lot better. Maybe you saw Steven Brill’s piece last week about prices in health care. This is a point he makes very strongly. Prices in health care have no meaning. So if we move to a consumer-driven system this still isn’t what would happen.
On the left you see Medicare’s statement to us from the hospital for killing my father. They charged only $636,000 for the service. And then on the right you see my effort to say if I had rented out a room at the Four Seasons, which is the most expensive hotel in New York at $1,000 a night. I leased a million dollars of hospital equipment, put it in his room. Gave him an hour a day with a physician which is probably about five or six times what he got, and gave him nurses around the clock. I also gave him room service we included in here. That most extravagant possible treatment is $155,000.
Now, obviously nobody paid $636,000. Because in the health care system we don’t use prices the way we do everywhere else, to communicate actual information on costs, scarcity, need for investment, you name it. Here is what we communicate, because every bill communicates something important. And I’m sure all of you have gotten bills from your insurers. They communicate the following: You’re lucky to have us, you can never handle this yourself. My aunt got a bill from her insurer which said the hospital charges were $105,000, her share was $300, and the insurance company had paid $800 and the rest was other insurance credits. Nothing is being communicated there except thank goodness you have insurance.
A lot of people think we can fix this just through payment reform, or by making health care cheaper. That if we can just improve efficiency in health care, we can bring cost down and make it more responsive. And we’ve been doing this forever, right? Productivity in health care has gone through the roof, but of course it has had no impact on prices, because there are no competitive mechanisms for it to have an impact on prices.
Let me give you the ultimate example. I love this example. Many of you obviously know that the Reagan administration enacted a prospective payment system for hospitals. And that for the most part most hospital bills—in-patient for a long time, out-patient for shorter—have been what would be called “bundled” or “fixed payment” on diagnosis. And the impact on usage has been extraordinary. The days-in-hospital per Medicare beneficiary have dropped by 63 percent since prospective payment. The total days-in-hospital—even though we have so many more Medicare
beneficiaries, the population has almost doubled—itself has declined by almost 50 percent. And the total days in the hospital are down almost 60 percent.
You will never see a reform that has a greater impact on true cost. When this reform happened, a night spent in hospital was by far the most expensive element in the system. So you know what happened. Once we cut 60 percent of the cost out of the system, prices tumbled. Right? No. Weirdly, we reimburse five times as much, which is somehow bigger than minus 60. If we’d cut the hospital days by 99 percent, the result would not have been we save money, we would have reimbursed by more. And here is a hint to what is really going on. So, Medicare reimburses five times what it did before prospective payment reform. The hospitals claim their costs have grown seven and a half times. So, in other words, Medicare has cut the usage in half, paid five times as much, and convinced itself it’s getting a better deal. It only paid five-seventh of the increase in cost.
One of the problems with not using prices is it causes us to do things and think things that are weird. So, here’s what we think is happening in health care. We think that Medicaid is paying a lot less than Medicare, which is paying a lot less than private insurance. This is from a single study done in Michigan on I believe appendectomies in the mid-2000s. It’s obviously very hard to get true comparable pricing. So, here’s what we think. There is some cost shifting going on, something unique to health care that private insurance is really paying. Because we all know all Medicare patients are served at a loss, so private insurance is paying for that and for Medicaid, right?
And you only can believe that if you’ve never been outside the health care system. Because here’s hamburger pricing. McDonald’s makes money at 99 cents. They’re not actually being subsidized by DB Bistro. Cheesecake Factory makes money at $11.95. DB Bistro makes money at $32. They don’t sell many of them. There’s foie gras on the burger. I’ve had it. I’ve had all three of those. What’s important about all three of those? They’re all hamburgers. They’re all lunch. If you stand outside of health care, what you would say is if I’ve got three different price regimes that are this wildly different, what I’ve got is three different products. And I think it’s something actually that people who focus on price miss, which is where the customer is obsessed with volume as in private insurance, I charge a lot of money. Where the customer is obsessed with price, as in Medicare and Medicaid, I do a ton of volume, which means I perform the service differently.
Now, I’m not here to tell you how doctors perform their services and hospitals do. But this can’t be false. This is how the world actually works. We may not recognize it in health care, we may not believe it in health care, but if you have a price imposed upon you, you figure out a way to make money at those prices. If you were really losing money on Medicare and Medicare patients, you wouldn’t take them, there would be no cost shifting.
Here’s something else from outside the island. What is innovation? What is growth and technology? There are only two industries where anyone seriously says technology is driving up costs. We say it in health care, we say it in defense. So, in 1965, there were somewhere between 10 and 20,000 computers on Earth. There weren’t many more people who knew how to use them. And that’s what a hospital room looked like in 1965. Both industries have undergone a lot of technological change. In computers, what happened is 100 percent of the world population got PhDs in computer science, which enabled us all to carry a little computer in our pocket, the single most complicated thing on Earth. I’ve actually got two of them right in front of me. If in 1965, you said every person on Earth was going to have one of these, you would have been committed. The most personal, individualistic, heterogeneous service on Earth is the one on the
right (health care). The one on the left (smartphone) is the most accessible industry on Earth, even though 45 years ago or 50 years ago it was thought of as impossibly complicated for anybody other than 50,000 to 100,000 people on Earth to understand. The one on the right (health care) is now complex beyond understanding for even the people in this room, who know more about it than anything else.
That’s my dry cleaning bill on the left. This is the most important lesson that I can offer, which is do not have your dry cleaning done in New York. The prices are ridiculous. This is the most expensive dry cleaner in New York. And what is interesting about what they have done is in response to the Congressional Dry Cleaning Technology Act, they invested in information technology and they took it an extra step. They actually can tell you every single shirt. Look at the first one. A Barneys New York shirt, blue, solid cotton. A Paul Smith, white with stripes, light blue. Why? Interestingly, that’s incredibly bad for them. Because when they lose one, I know exactly what shirt it is. So what do they do? They sat there and said all the other dry cleaners now have computerized bills. I’m going to take it a step further so I can charge more. So, yes, I take the risk of if I lose a shirt, I can’t say three shirts, I only took in two shirts, that’s a mistake in the bill. You say you lost my Paul Smith shirt. So, that’s now the digital age works, right? It’s that we’re all endlessly playing with stuff, what makes sense. That dry cleaner literally made this decision to compete with the guy across the street.
This is my completely unfair representation of the Meaningful Use Rules, and these are the instructions to an iPad. All of you who have bought an iPad know an iPad has no instructions. That’s how information technology actually works; if it’s not usable, it’s useless. And we know this everywhere, except one place.
This is going to be an unfair slide, I’m sorry. I’m going to bring this one on Otis Brawley. Otis Brawley wrote, if your institution has a center of excellence you probably have an excellence problem. If you call yourself patient-centered, you aren’t, you’re talking to yourself. This is how people talk to customers. This is a customer-centered retail establishment. They don’t use the word customer-centered anywhere, no one does.
This is the single stupidest idea in the history of mankind, and as a result it completely transformed the world economy; in thinking about innovation around health care, you have to think about the shipping container. So, the shipping container has changed everything in our world. And it was a terrible idea. What happened? The most expensive thing you can do is put something on a ship and run that ship across the world, right? Incredibly expensive to send a ship somewhere. So what did the shipping container do? The shipping container said, do you know what we’re going to do? We’re going to fill ships with empty space, instead of having ships carefully loaded to maximize the use of space. You put a motorcycle on a car or a ship, that’s a puzzle, right? How do I fit that? We’re not going to do that. We’re going to put everything in a box. Most of a box is empty space. If you ever opened up a shipping container, most of it is empty space. And so ships are filled with empty space. Could there be a dumber idea to take the most expensive thing you can do, ship, and fill a ship with empty space?
Well, of course, what the shipping container did was it meant that you could load and unload ships almost instantaneously, within hours. I’ve lived next to the Port of Miami, they turned massive ships around in hours. You can build much bigger ships. It’s actually impossible to build a big ship unless you use a standardized container. You can’t reach everything to make sure that the toys are packed correctly with the motor vehicles.
And so everybody hated this idea because it cost everybody their job. It meant that all the ports that were great ports lost out to new ports that invested in computerized shipping, and it is
the reason that the prices of most goods have declined over the last 50 years and that supply chains are now earth long, instead of having to be near a river or near the plant. The economic transformation of this may be greater even than the Internet. It’s in the trillions of dollars in cost saved. And it’s a terrible idea. Everybody in the business hated it.
So it’s about a very important phrase, which is “creative destruction.” I was at a meeting the other day where the head of one of our local hospitals in New York got angry at me for saying that there was no real incentive for saving cost in health care. He said that he had sat down with a group of the other hospitals, the insurers, the doctors, the nurses, and a couple other people, and they all sat around and tried to find the best cost saving ideas. So, it’s the reason we don’t ask turkeys what to serve for Thanksgiving. Really innovative ideas hurt peoples’ businesses. And so when we sit around and say, how do the stakeholders agree, we’re not talking about real innovation. It’s sad, it’s ugly, it’s the reality of our world, but it’s what’s changed every single other industry on Earth. Real innovation is truly disruptive and truly destructive.
I’m actually going to skip over this except to make one point. Obviously, there are some bigger public policy issues here, and there are a couple things that I think aren’t widely understood about where the United States stands. The United States actually spends relatively little of its health care spending out-of-pocket. Less than most OECD countries. It’s now closer to 11 percent. France spends a little less, the UK spends a little less. Not a lot less. Most countries have more consumer skin in the game. The United States spends relatively little of its health spending from the government, but the gross number itself is one of the highest in the world.
Now for a little perspective, here’s Singapore. Singapore is the only rich country with a truly consumer-driven health system. Fifty-four percent of the amount spent in Singapore is spent out-of-pocket. And what’s interesting about that 54 percent is every single health care decision in Singapore is made by a patient. They actually buy it. Even if they’re going to be fully reimbursed, the government isn’t the payer, the patient is. We’re so used to insurers and Medicare paying on our behalf, we forget they could also give the money to pay and that would transform the system. In Singapore, only a third is explicit health spending. Interestingly, some of it is to run a parallel health care system that competes on price. Singapore spends only $2,400 per capita on public health, but here’s the killer. Singapore spends 4 percent of GDP on health care. It’s as rich as we are, people live as long, the health care system is as good. Fourteen percent of GDP less than us, and less than almost any other single payer or other country.
It’s a lot of policy stuff. Let me come back to what I think this really is about. One of the things that is unique about health care is that there are 310 million of us that have a health care story. Sometimes it’s as simple as the doctor forgot who I am, or they lost my test, or the generalist didn’t talk to the specialist, or one specialist didn’t talk to another. Sometimes it’s much more serious. Sometimes it’s about being taken for procedures that were meant for another patient. My father was twice. And as we all know, they tell you if you have a family member in a hospital, try to be there at all times. Imagine if FedEx said we’ll deliver your package, but it’s best to hold onto it during the process. In a high-tech world this is insane. We’re so used to it we don’t even realize how absolutely absurd that is, but we all know it’s necessary. And obviously all the way to the extremes of people dying from mistakes.
We talk a lot in health policy about very big picture things—about money, because there’s a lot of it, about big incentives and big economic ideas. What needs to inform us, though, is that this all translates into the little picture and that every single one of us has a story. That’s way too many of us to have a story. Thanks very much.
MR. GORMAN: We have time for a few questions.
DR. MONTORI: Hi, Victor Montori, Mayo Clinic. Thanks for a very good presentation. I’m disappointed I didn’t get offended. I was looking for it. The Cheesecake Factory thing I think just went through the threshold.
The newspaper piece that was published at the Star Tribune in Minneapolis put it together as well. You make the case that there is insufficient for-profit health care. And you were not here, but in the previous panel we were talking about how there is actually good evidence that for-profit health care is actually more expensive and is associated with increased mortality. And I suspect that it’s because of the conditions or environment in which it learns to operate. You’re suggesting a fundamental change in the conditions or environment. Do you want to elaborate on that?
MR. GOLDHILL: Thank you for bringing that up. You’ve made the point for me, but I think it’s so important it’s worth pointing out. We have the worst of both worlds. We have a profit-driven system with the wrong customer. So your point is exactly right.
First of all, there are no nonprofit systems. We’re all working for a living. So, at some level, all of us are doing this to pay our way. There may be no shareholders, but they are still people earning a living, and how they’re incented is important. But your point is completely correct.
I wrote a piece for Bloomberg about 2 months ago saying the profit-driven system is producing terrible results, the nonprofit system is delivering, for the most part, terrible results. The problem is the economic incentives for both are fundamentally the same, and they’re distorted by the fact that we’ve decided to let an intermediary be the customer for everything.
And I would argue that between the market power that these intermediaries have allowed providers and that the intermediaries themselves have, and the policital power accumulated, the way to make money in health care is for the most part to do bad things. And the fact that we don’t do terrible things speaks to how many good people there are in health care. Because in fact, purely economically, if health care was an investment bank, remember what we have. We have a system that says we’ll pay for any care the patient needs. And we’ve got somebody with a monopoly in determining how much the patient needs. If in investment banking we said we will subsidize any deals bankers think are worth doing, we would be an entirely deal-based economy. The only reason in health care we’re not is, again, because of the professional requirements of people.
But I think those incentives can be changed meaningfully. And without them, the for-profit system and the not-profit system are both going to produce terrible results. The relative difference I can’t tell.
PARTICIPANT: I agree with you, I feel like you’re my twin. And I wanted you to know that in Portland, we have been trying to get the consumers in Portland to design a new benefit package to ask for warrantees for certain services and to change things up substantially. And a large orthopedic consortium got together and redesigned how they’re going to provide services. And they’re going to charge one flat fee and they’re going to give a warrantee for services. So if anything goes wrong for a long period of time the patient can come back and know that that’s all covered under the warrantee. And because of that, they built in shared decision making to make sure that people who get the services really want the services. They prep the patient much more up front, and then they prepare them for after the fact, including how to rearrange your furniture for when you come back and what to do with your throw rugs, et cetera. So I think it is very important.
The second thing I wanted to tell you is a couple of years ago we had the author of a book called The Healing of America come to Maine, I think that’s why he won’t go anywhere else. The poor fellow, Maine is eight hours long and we took him over most of Maine. We reached 16,000 people, and we had over a million media impressions which in Maine is good because that’s how many people we have. And what I learned from going over most of Maine with him is that our system has a lot of unnecessary un-value-added costs, beginning with just how we reimburse for services. And each of these insurance companies has a different way of doing things. It’s not uncommon for hospitals in Maine to have twice as many people who are doing billing than they do beds in the hospital. And they have very expensive computer systems that they have to work. Most countries have one electronic medical record that they buy for everybody; we have a thousand, and everybody has to connect to those different thousand. So I think we don’t do a lot of things to try and make sure that we get more value from our system. And when we keep on paying for insurance the way it’s offered to us, and not ask for something different, we are contributing to the problem.
MR. GOLDHILL: Thank you. One point that you raise that I think is worth thinking about, one of the things we think about in health care that we actually don’t think about in anything else is that there is the right way to pay for things. In anything else, we’re willing to have things exist side by side. Different business models, different ways of paying. I think it’s actually a mistake in health care.
I think one of the nice things about bringing consumers into a more balanced role is that we’ll have people compete for their business on different things. People will bundle their services and say here’s my package you can buy. Others will do fee for service.
In fact, rather than sit around and say what’s the right way to pay, I think what we need to think about is that having different business models exist at the same time is the feedback loop that causes endless innovation and endless improvement. There are very few things on Earth that there’s only one thing to buy, but in health care our best minds are endlessly looking for the perfect way. And I think that conceptually is an error.
The other thing I should mention is when I talk about patients, what I’m really talking about is balance, bringing consumers into the system, not having everything be intermediated. It doesn’t mean you get rid of the government role or get rid of insurers’ role completely, but it does mean rebalancing the system.
MS. BECHTEL: I’m Christine Bechtel and I work for a consumer advocacy organization here in town. I want to fundamentally ask you, what’s the pathway? That’s sort of the theme of this meeting. And I think conceptually there is not much that you’ve described that someone in this room would say that’s not the right idea in terms of a way.
But the question is the way to get there, and I want to preface that question by saying historically, the words consumer-driven health care have a bad connotation for the consumers, because that’s usually the place like high-deductible health plans, where we just voice the problems that the health insurance companies and the employers and congress have been unable to solve, so let’s get them to fix it.
I don’t think that’s what you’re saying. But I think on the other hand it would be helpful to know what is the pathway, the next three things we need to do to make progress in that system? Is it blow up the insurance companies? That’s kind of what I heard. Is it end meaningful use?
MR. GOLDHILL: My belief actually is the more that consumers pay out-of-pocket, the more good things happen, including meaningful reduction in prices. Interestingly, before we decided that preventive care should be covered without a deductible, we were starting to see real
competition in the preventive care services. We were starting to see minute clinics that did things for fractions of prices available in the mainstream health care system, and that’s what you see. If you’ve spent any time in communities that are heavily illegal immigrant, you actually see how a cash-based health care system works. We’re all of the belief that if it costs less, it can’t be good. And some of these are good and some of them aren’t good. Obviously these aren’t the best customers in the system, they’re the lowest price paying. But in fact systems do develop.
So what can we do? Well, I think some of it is about to be done for us. The reality is we’re a couple years away from no company in America being able to offer anything other than very high deductible health care insurance. And when you get that sort of scale of people paying out of their own pocket I suspect you’ll see the provider industry start to reorganize itself to get their business, and the same thing that we were seeing in preventive care before the Affordable Care Act.
I’ve called for insurance to shrink, to cover only the most catastrophic things. I’m spending $23,800 for an employee’s family plan this year in standard deductible. I think if you had a very high deductible, say somewhere in the $15,000 to $20,000 range, the premium is probably somewhere in the $5,000 to $7,000 range. Which means I could write that person a check if it was tax neutral for $15,000 a year. Which means they basically have enough money to cover their deductible every year and a half or 2 years. And the reality is if you had millions of people with that, as opposed to just those that were too disadvantaged to have anything else, I think you’d have a very different health care system. Same amount of money, just flowing differently into people’s pockets and into the system. But I must admit, it’s very hard to get political support for that. I think what we’re going to see happen is it happens anyway. When you look at how the exchanges will work, the cost of standard health insurance, because of the exchanges, is going to go through the roof. There’s no other way they can work. They’re price-capped. None of their customers care about prices? What does that do to prices? It causes them to go through the roof.
And that’s going to drive the rest of our businesses. They’re already high to begin with. I think you’re very close to seeing the end of standard deductible health insurance privately offered outside of the government context. And that will change, that will make a big change.
DR. COHEN: My name is Perry Cohen and I’m a Parkinson’s patient. My first job, after I got my master’s degree with Massachusetts Blue Cross Blue Shield, I was an analyst. And one of the things I learned there is that the insurance that the doctors and the hospitals get paid really wasn’t patient protection…. I’m going to pass.
MR. GOLDHILL: Can I address your point though, Perry? I think one of the strange things about public policy debates about health care is the role that’s assigned to insurers. You hear politicians talk all the time about relying on insurers to control the cost of care.
I guess none of those politicians have been in the insurance business. Because insurers have no way of growing their profits by demand for care shrinking. And demand for care is volume times price. And what people get confused by is when they put in a claim and an insurer says, like mine did, nope, we’re not paying for that—sounds like they’re pretty tough on cost. But the fact is we’ve had private insurance dominate pay in this country now basically since the mid-1950s. We saw cost go up much faster than GDP and inflation, and insurer profits have been fine. If you spent time in other insurance businesses, for example when there’s a hurricane, the stock prices of the insurance companies go up, not down. Why? Because premiums are going to go up, margins go up.
The idea that insurers are going to somehow bring discipline to a system—if none of us needed any health care and insurers did such a good job of driving a better system, we were all
so healthy, there wouldn’t be health insurance. They’d earn nothing. And so insurers at best have an ambivalent relationship with cost. They don’t want to pay for your procedure, but they do want your company to have higher premiums next year. That hasn’t made them great guardians of the system, at least in terms of cost. And I think many of us would probably argue they’re not great guardians in terms of quality and safety either. I don’t know if that gets at your question.
DR. COHEN: Yes, it does. But the point I was trying to make is that the health care system is really more doctor- and provider-centered, rather than patient-centered. I like your idea of having the patients be the purchasers more so.
MR. GOLDHILL: Thank you. I think we’re unable to achieve the balance that a lot of people in this room have been talking about the last couple of days unless you bring the economic incentives in line with the therapeutic ones, which is to have patients take more control, be more active. It doesn’t mean they all will, but it means the system will push that more on them.
In the same way that in any other industry things are made easy for us, the health care system does the opposite. We’ve got to do the work if we want to do the work. That shouldn’t be the case.
DR. COHEN: Well, there is an advantage of patients being involved, a health care advantage.
MR. GOLDHILL: And that’s where this comes from. This comes from that more than economics. Because I think unless the economics match what you’re hoping to accomplish, you’re not going to accomplish it.
DR. COHEN: Thank you.
MR. GORMAN: We’ll have two more here, and then Lyn.
PARTICIPANT: Not as an argument for status quo, but just in looking for an expansion of the concepts, competition requires more than one provider, and in small-town America and rural America there may not be enough room to make investments for more than one provider group or set of hospitals, et cetera. The current system of course creates that sort of environment, and there is competition emerging in small cities, where you have hospitals that are duplicating capacity to the same area, and then of course getting patients through it that are able to pay for it.
In the re-imagined system that you have, how would it work not in New York or in large urban environments, but what happens in rural America environments where competition may not be able to play out?
MR. GOLDHILL: It’s a great question. In a re-imagined system, it really does look like other things, which is there’s also not enough scale for competition in most goods and services in rural America. What happens is, and I think this is more likely to happen in health care than anything else, is that the competitive price in truly rural areas is the cost of traveling to a less rural area to achieve a service. That’s what keeps anybody from charging insane amounts in rural areas for anything. Health care is actually not that different. And it’s a very difficult thing for people to understand. We have plumbers in rural America. They can’t charge you a million dollars to fix your faucet because the town is only a thousand people and therefore only one plumber. That plumber can only charge what it takes for a plumber from the next big town to drive over. That is the only marginal difference he can charge.
In this country, in health care, we’ve somehow decided health care is so different that we need to regulate the rural markets in such a way to assure there’s never any competition. That’s all we’ve done. And that concerns me. Because again, there are lots of expensive goods and services consumed by people in rural America.
And the other day, someone said to me, I agree with you that much of health care is now about things that we have time—they’re chronic illnesses, I’m going to have my hip replaced—they’re all sorts of things we can actually make a decision and we have time for the system to say use this procedure instead of that, this one is safer, that one is cheaper, whatever. There is time for that decision making. But a lot of health care is still about emergency stuff. And how can that possibly work in a consumer-driven system? So, if you’ve ever had a flat on a highway you know that the tow truck that came to you didn’t say, “Let me see your balance sheet before I decide how to charge you for this.” The economy figures out ways to handle emergency services. Most people pre-pay that stuff so that they know there is somebody there at a reasonable price when they have a flat tire. But even if you haven’t prepaid there is a limit. And that limit is created by really functioning markets existing around us.
One of the problems with billing $640,000 for killing somebody—when you know you’re never going to collect, it has nothing to do with cost, price reimbursement, anything else—is that none of us have comparable prices to even think about. There’s no market for anything that’s real in a way we can understand it. So I’m not disagreeing with your point. It does cost more to live in a rural area than an urban area. But it costs a certain amount more, and it does in every other good and service.
MS. PAGET: Hi, my name is Lyn Paget. I’m from Boston, Massachusetts, and I have about 18 questions for you, but I’m actually going to only ask two quick ones. One is that we of course have pretty active exchanges. In addition to working in the health policy arena, I run a small business unrelated to health. And quite frankly I haven’t seen the competitive pricing from the exchanges that I would hope to see.
Second, is I agree with you completely on the high-deductible plans, that’s our future. What do you think the protection mechanism is going to be to keep those premiums at some point, matching what we’re paying now without a high deductible? That was my number one question. My number two was if there’s one thing if you could pick as a disruption similar to the container, what would it be?
MR. GOLDHILL: That’s a really good question, so let me ignore it. First of all, just quickly on the exchanges, any business that competed on price on an exchange structure is beyond stupid, it’s never going to happen. You tell somebody you cannot underwrite, you cannot design the benefit package, compete on price, there is going to be one price on every exchange. It may not happen the first year, but it’s inevitable. Exchanges were designed by people who have never bought or sold anything in their lives. That’s the only explanation for it. They’ve never competed in anything ever. They think it’s supposed to be like commodity exchanges I guess, but in commodity exchanges or Expedia or wherever else they use as an example, you don’t care who the customer is. So you offer this broad range of products and whoever has a credit card can buy it. In insurance markets, all you care about is who the customer is, and you have to be completely blind to that. Nobody is going to compete on exchanges, it’s going to be a wonderful mechanism for raising prices.
But in terms of what’s disruptive, my argument is what is truly disruptive, what changes everything, is that we’re paying out-of-pocket. And that rather than look at these thousands and thousands of goods and services as a single thing, health care, we say to ourselves there are some things, some people, some conditions, that need insurance. Born unlucky, terrible accident, got one of those diseases that’s just horrible, right? We need to insure that as a society, because we want to. And I actually believe in national health insurance to cover that. Single pool, all of us.
A lot of health care is just routine. Just like anything else. And insuring it makes it less responsive, higher priced, and of lower quality. And then there is stuff in the middle, which we save for. We’re used to this. Most people in this country actually will buy a house at some point in their lifetime. None of us have problems with the idea that the down payment comes out of savings. The bulk of it we borrow depending upon what stage of life we’re at. If we’re older, we may just pay for the whole house because we’ve had savings. Routine maintenance comes out of our pocket, accident comes out of insurance—a house burning down or anything. None of us have problems that there’s four, five, six, seven different ways at a time we might fund our shelter or our food. Nobody says we need to pay for the poor to have food the same way we need to fund upscale restaurants. Nobody says that. No one seriously says that. But in health care, which is the broadest possible range of goods and services, we somehow think it all has to be the same way and that’s enormously distortive to the system.
So once we start paying for more and more of it—and it needs to be real scale, it can’t just be the poorest of us who pay out-of-pocket, it has to be all of us who pay out-of-pocket—this industry will restructure itself like every other industry on Earth did. 1965, the customers of the computer business were NASA, the Defense Department, the IRS. The customers of the computer business are sitting in this room. That change happened because somebody said they could sell to these folks. It changed everything.
The last point you made which is the hard point, how do we stop it from happening all over again, just with catastrophic. I have a half-baked answer to it, which is in my half-baked book, and that is that we should think about moving to defined benefit. One of the interesting things about health care of course is that it has very little marginal cost. So, prices have a lot of room for variation, which means that actual cost for providing a service is relatively low, no matter what people think. This is true of industries like airline, software, telecoms. But the actual marginal cost of producing a pill is almost nothing. For providing a physician’s service is the physician’s time, which is a wide variation of possible price. Of using a diagnostic machine, it’s almost zero, although because of the market’s dysfunction they actually charge you for that, but they shouldn’t.
If you actually had a defined benefit system for catastrophic care, say we’re going to collect a trillion dollars of premiums, we’re going to pay out a trillion dollars according to this schedule of diagnoses, the entire system would have to reorganize itself to fund care at that price. And it’s so different from the way we think about it now that I don’t push it, because if we can move to catastrophic it would be 10 years before what you mentioned happened happens to the point where we have to think about it.
But ultimately at some point we want to say we want this country to be healthy, we’re not going to spend so much money on health care, we’re going to spend more on consumption and recreation and diet and environment and exercise and lower stress in our life, those are the things that drive health. And the only way to do it at some point is for some part of the system to probably have a budget. The catastrophic function probably should. But that’s a little theoretical at this point. Thank you, though.
MR. WOLFSON: This is Daniel Wolfson, I spent most of my career actually with prepaid group practices. And one thing we realized even though we were capitated a group, that is changing the incentives was just half the game, it was really the start. So I wanted you to react to that, because I think it’s a little bit more complicated than just changing the incentives. We’ve been talking about shared decision making here and the difficulties of that.
And the other thing is Shelly Greenfield was here yesterday and he did a study a long time
ago that showed when you increase the cost to the consumer you delay care. And it was a trivial amount actually at that time. So I wanted you to react to that. And I’m not sure if you’ve said this, you’re leaning toward consumer health savings accounts.
MR. GOLDHILL: Oh no, I do believe in consumer health savings accounts. I believe in mandatory, catastrophic. Basically what I say is, let’s take what I think is the best idea on the left, which is single pool national insurance, but the best idea on the right, which is leave as much of health care as possible to become a normal industry. And I think the way to do that is to shrink insurance to catastrophic, make it mandatory. Because our system starts at such an insanely high price point, we can only really pay for it with savings accounts, we can only really let people save against it until the prices start coming down to a point as they have, for example, in Singapore. The average person in Singapore’s health savings account would fund 11 hospitalizations as of 2 years ago. I don’t think the average person’s savings account can afford one. Not health savings account, savings account period, just to give you a sense of the difference.
I want to talk about incentives though. The key to incentives being incentives and not goals is they have a natural feedback loop. When the government has meaningful use rules, you have to hit the numbers, you have to hit the targets. When we have hospital readmission rules, you have to hit the numbers, you have to hit the targets. Same with hospital infection and all the other things that are going to have bonuses and penalties. It doesn’t ever work.
The feedback loop that consumers provide is we don’t know what’s going to work. That first dry cleaner who went to an IT system so you got a fancy computer printout bill instead of the 12 shirts written down, he got a lot of customers. The guy across the street saw it and said, “I have to do that.” He’s not losing any shirts, customers are more impressed, he seems more organized. So he did that, and he said, “I have to add something.” So he added, “I divide between shirts and pants or men and women.” If you’ve been to dry cleaners you can literally see this in action. It never stops.
The bill I showed you from the high price guy is going to be the bill that the low price guy has in a year or two. The key is a feedback loop. My first meeting of Leapfrog, when they asked what was my view of what would finally cause hospital related deaths to end, I said that it would be a billboard that said go to uptown hospital, downtown will kill you. It’s funny, somebody said to me, “I would never go to a hospital that advertised, because it just tells me something about their commercial approach.” And I held up my iPad. This person was a big techie person. I said you know, “I almost didn’t buy this because Apple advertised it. I thought, shouldn’t they be spending that money on research and design? I’m a little suspicious. How good could this be if they had to tell me about it?”
And really we think health care is so different, we don’t think to ourselves that one way to solve quality might be to have competitive advertising. It’s a feedback loop. There is no incentive that is a silver bullet, nothing. It’s the accumulation of who am I responsive to. And yes, some of it will wind up being petty. Customers will wind up preferring hospitals that are painted in this year’s color. That sounds terrible to people in health care. But outside of health care, if you’re used to serving consumers, it gives you a chance to prove you’re responsive. If you spend any time in a hospital as just a patient, it is astonishing to you how far hospitals have fallen behind the DMV, not to mention any single consumer business on Earth. At every single stage you have to be told you are just a patient.
And again, it’s not because the people are bad. The people are great. Trust me, they’re much better than bankers. But if you’re a customer of an investment bank, you’re made to feel like
you’re a prince, because they’re going to charge you a lot of money. In hospitals we’re all spending a lot of money. All of us are spending a million dollars over a lifetime, and we’re all paupers. And again, we talk about money a lot. This isn’t about money. It really is about incentives for quality care, safety, appropriateness, and I think a lot of what you’re talking about in here, which is having a doctor/patient relationship, a provider/patient relationship that brings to bear what you need for the best outcome, which is a patient that understands there’s no one out there taking care of them except for him. I think that will add to all the work you’re doing in here on that subject. Thanks, Mark.
MS. BECHTEL: That was a mind melter. So, we knew that not one person could follow that, so we have three. So, let me invite the next panel up to the stage. I think this panel follows brilliantly on both Mr. Goldhill’s speech, but also the panel before that around value. This panel is on driving the demand. And I think, before David, I probably would have said, is it even responsible to drive demand for something that doesn’t exist? But now I’m rethinking that.
Anyway, let me go ahead and introduce Susan Reinhard, who is a member of our planning committee, and she is going to moderate this session. She is the Senior Vice President at AARP, heads its public policy institute, and she’s also the chief strategist for the Center to Champion Nursing in America at AARP. Go ahead and don’t worry about the time because we’re going to take that away from the wrap-up Planning Committee members at the end.
DRIVING THE DEMAND
Dr. Susan Reinhard (Moderator)
DR. REINHARD: Thank you, and thank you for staying. And I hope most of us can stay until we really do hear the committee members synthesize this. But I know we need to get going. I do have to make one comment about the introduction yesterday. Is Sherrie Kaplan still here? I don’t know if you remember this, but one of Sherrie’s PowerPoints was how she had written for the AARP public policy institute in 1991. Now, I wasn’t running the AARP public policy institute in 1991, but I did read a lot of it, and I actually remember patienthood, that was what she was writing about. And then it occurred to me, that’s almost 25 years ago, that we ought to get her to do a 25th anniversary paper on that and incorporate a lot of these ideas. So I’ll have to follow up after this conference.
So, I just do want to also mention that I have my AARP hat on of course. I have lots of different hats, as all of us do. But AARP does have a pretty big stake in this discussion. I’m sure that’s part of why we’ve been involved in this, and in all three of the areas that we’re going to be talking about.
I love the title for this, I can’t take the credit for Driving the Demand, I really do love that title. It has a lot of power into it. But behavioral economics, this is something that AARP, as the largest consumer membership organization actually in the universe, is very interested in what Kevin is going to be talking about. We keep trying to figure out what we can learn about what drives people to make health care decisions in health. I should also say retirement security. What can behavioral economics teach us? Communications, and how we can message important information. AARP has like hundreds of people working on communications, always about that message. And we get lots of information. Consumers get tons of information. So how do you
message it and help them sort through all of that information? And then certainly social media and how to use it as a tool for change.
So, I do feel privileged to moderate this panel, and I’m going to start by going over the session goal. Each of these panelists, as we’ve just been reassured, get their full 10 minutes, so that’s good, and you get that opportunity to exchange with them as you have after each session, so it’s been pretty good—including people outside the room, if they’re still watching on the Web.
So, you have this description of the session goal in front of you. It’s exploring cross-cutting strategies to advance patients—you could say consumers—of course in partnership with providers, as leaders. We haven’t talked about leaders yet. Leaders and drivers of care delivery improvement through informed shared decision making and authorized use of clinical data for research and value improvement.
So, we’re going to take this from three points of view as I said. First with the focus on behavioral economics and value generation. I hope that we talk about that word, value, and how Shoshanna warned us that term itself isn’t necessarily understood by consumers. Kevin, many of you know him, is the Founding Director of the Center for Health Incentives and Behavioral Economics at the Leonard Davis Institute, which is one of only two NIH-funded centers on behavioral economics in health in the United States. He is co-director of the Penn Medicine Center for Innovation, and he is a professor of medicine at the University of Pennsylvania School of Medicine and Healthcare, Management at the Wharton school, and, I have to add, he is a practicing physician at the Philadelphia VA Medical Center, so that always keeps him grounded.
Second, we will consider communicating value to the public, and Tresa Undem—we’ve worked with Tresa at AARP, many of you have already referred to her. Tresa is a partner at PerryUndem Research in communication, she leads public opinion research on a whole variety of health-related policy issues, including health reform implementation, delivery system reform, access, affordability, cost, quality; she is perfect for this panel.
And then we will turn to a true patient leader. And we are delighted that she is going to be discussing social media as a tool for change. This is Kelly Young. Kelly is the founding president of the Rheumatoid Patient Foundation. So in a very short period of time—I think hopefully she’ll tell a little bit of her story—she went from zero to 100 in how she has moved. Talk about leadership in this whole area. She is the founder of RAWarrior.com, a comprehensive website about RA of about 700 pages and the hub of one of the most large and vibrant patient communities online. In 2006, she was diagnosed with rheumatoid arthritis after years of periodic symptoms and trying to sort that out, and she works to provide ways for patients to be better informed and have a greater voice in their health care.
So, it’s a really good mix of a panel as you can see, and we’re going to start with Kevin.
Behavioral Economics and Value Generation
Dr. Kevin Volpp
This section is omitted at speaker’s request.
Communicating “Value” to the Public
Ms. Tresa Undem
MS. UNDEM: Again, my name is Tresa. I am going to jump right in, because I have not too much time. And it was a real struggle putting together this presentation because we’ve gone at this in our research issue from so many different angles, not totally head-on. And I’ll sort of end on that note, why I think that is. But we’ve done a number of studies on health care cost, quality, payment reform. Chuck from MSL we worked with, for RWJ on a recent project that he mentioned on health care cost, and just where our consumers are—going to draw a lot on that. We’ve done work for Aligning Forces, communication work for them, with Chuck as well as Patrick McCabe at GYMR—delivery system reform, comparative effectiveness. We’re now doing a lot of work on exchanges. So probably about 80 percent of my work is health care, and about 100 percent of that relates to cost and quality in some way.
So what I’m going to go through is first just where the public is on value, because I think we need to meet the public where they are at, or any audience that you’re trying to communicate to them, you need to understand where they are. And then I am going to talk about some global recommendations around talking to the public, consumers, and patients about value, cost and quality, some overall points. And then some key takeaways. I went through some different studies we did on shared decision making on payment reform, and I just sort of cherry-picked some of the best sort of practical advice we could give around these topics.
So, first, where the public is. The public is not there yet as we all know, but we’re on the way. Listening to David, I think what he is seeing I’ve been seeing in the last year or so, the last couple years, as people pay more out-of-pocket they really are snapping awake, they’re really becoming alert. They’re changing behaviors.
So, the study we did for RWJ, there were a couple Medicare focus groups as Chuck said, they were different. And then it was everybody had a deductible of $500 or more—that was the screening to get in. And these people, it’s shocking, they were changing behaviors. One or two in every group said, “I’m not going to fast food anymore,” or “I’m exercising more,” because they’re paying more. It was really shocking to see this. They’re forgoing unnecessary care. I have a guy who said, “My doctor ordered an X-ray for my foot, he thought it was broken, I thought it was gout, I said I’m not paying the $400, I’ll wait a week or two, see what happens, didn’t need it. I’m going to call the nurse instead of going in to the doctor.” All of these sort of consumer behaviors—I just never saw 4 years ago, or even 3 years ago, or 5 years ago. The downside, people are forgoing necessary care. That’s absolutely happening, especially among the uninsured. Broken bones, even for preventive care, all of it.
But in terms of the attitude around value, I think that is shifting. We had one or two people in every group ask about cost before they were going to get a procedure or test at a hospital. Again, this didn’t happen 3 years ago. We never heard this. I know there has been a lot of research that the public links quality with cost, and we’ve seen that in our research as well. We’re starting to see that shift a little bit, especially with people who are paying more out-of-pocket and are more alert to these issues.
With these focus groups, we gave people the hypothetical situation, this surgery costs this much here, this much here. What do you think the difference is? About half of people said something related to quality. Maybe they have better technology, maybe they specialize in that procedure. About half said it was unrelated to quality. Maybe it’s a socioeconomic status of the
market, maybe it’s their concierge, maybe they’re a teaching hospital that costs more. I’m seeing that kind of change, I’m seeing some openings for that talking about cost.
The final point on value is we’re just seeing there are all of these factors coming together that are really driving people to be engaged. You just have to be engaged in health care now. You have to take on more responsibility. It’s a fragmented system. We have caregivers bringing their file folders from doctor to doctor. You have less time with your doctor. So you leave and you go home and you spend 2 to 3 hours on the Internet. By the way, this is really just women. There are a lot of things going on, even with exchanges. Now this is a self-service environment, you have to make these decisions about your health care plan, what health care plan is right for you. I think all of these factors provide an opening for talking about value and getting the public there.
So, just some global recommendations on talking to the public. The first thing is, talk about the impact on the patient. The patients don’t care about the health care system. Consumers don’t care about the health care system. We’re out there talking about payment reform or talking about changes, the number one thing they want to know is, how does this affect me? And then the second thing is their doctor. And that’s what they care about. When you talk about quality, link it to the quality between themselves and their doctor and how those specific things are going to change. So really think about the individual patient, emphasize solutions more than problems. We’ve seen this a lot. The public is skeptical, they are worn down, they don’t want to hear about problems. But especially in health care, you almost see a wall come up when you, for example, talk about getting the wrong tests. I mean they just don’t want to think about it. I think you need a psychologist to help figure that out. But there’s just a wall up. Talk about getting the right test, not the wrong test. Talk about solutions, back into problems. I’ll give you an example of that in a second.
I think what we’re seeing is the top motivator for changing for engagement again is out-of-pocket cost. And also getting the best care possible, I think Chuck may have come up with that language. Getting the best care possible we’ve seen is again another big motivator and another thing to talk about. The Choosing Wisely Campaign chose their name wisely. And all of the work we’ve done in the last couple years, the best phrase we’ve found to talk about cost is that health care is so expensive it’s important we spend every dollar wisely. The goal is not to spend more money; it’s to spend money in ways that best serve the patient. But that phrase, spend dollars wisely, is the one phrase that sort of everybody can get behind. It doesn’t trigger a bunch of negative reactions.
As we’re thinking about different efforts, whether it’s shared decision making, delivery system reform, when we link it in messaging to credible prestigious health care systems like the Mayo clinic or like a local respected health care system, that peaks interest and it also lowers peoples’ fear about the change. If they’re doing it, why can’t I? So that’s been successful in a number of different topics. Use examples. Value is such an abstract thing for consumers, it’s just really hard to get your head around. You don’t have experience, you don’t have exposure. So examples are really important. I’ll give you an example of an example in a minute.
Talking about women, I was doing an interview in Dallas a couple weeks ago on hospital readmissions, and I had this guy who was about 55 years old, really quite healthy, I think he had some chronic conditions but quite healthy, I think he golfs every week. He was recently remarried so he was divorced for a time, taking care of himself. And I said, “Does your wife have to bug you about getting in to see a doctor?” Trying to get at his wife’s role. Newly married, he was on his own. He said, “Yes, she does, and she lays out my medications every night for me.” And I just thought, really? Does this happen? How did you survive on your own?
And again, it just reminded me that it’s really women who are making these decisions and who are really going to lead the change. It’s women 35 to 64 who have a parent who’s getting sick, who have a child who has asthma and has been dealing with the health care system, who have a husband who won’t get a colonoscopy. Women in these age groups are really the ones who are going to lead efforts, I think.
I’m just going to touch on a couple different things we’ve studied around value. First, on shared decision making, I think there are people in this room who know a lot more than me. But when you’re talking to patients about this, the top motivation that we’ve found is getting the best care possible. That’s a reason to participate in decision making. Because I know me best, I know my body best. Improving the doctor/patient relationship. And then learning more about health and your treatments.
We found that one piece of advice when you’re talking about shared decision making or communicating that to the public, the examples we think to use are surgery and medications, you guys probably already know this—surgery is seen as the most risky. These two things are what patients most want involvement in: surgery number one, then medications. Because of side effects, and there is still an instinct to not want to go on the medication if you don’t need to. Diagnostic tests, screenings, they’re more apt to just say the doctor can tell me when I need to take that.
We tested a different number of different messages. A takeaway message that worked well among consumers as part of getting the best care possible is having a doctor who listens to you, answers your questions, includes you in making decisions about what treatments are best for you. So, just a few takeaways around that. Price transparency. So we did in this recent RWJ study, we wanted to get the public’s reaction to the wide range of prices. And we tested about eight different examples. This is the one that did the best. A recent study looked at hospital charges to remove an appendix. In California, the price ranged from $1,500 to $182,000. These were not outliers. Many were more than $100,000 and many were less than $2,000. While some patients were sicker, about a third of the price differences could not be explained.
This again woke people up. This was persuasive to people. And they thought okay, I’m going to start paying attention to this. It was motivating. We looked at a number of different examples. The reason this one did best was number one, that huge variation, just the range itself. The second one was using dollar amounts. Some of the ones we tested, we said this was 12 times as expensive or 7 times more likely to get this procedure. It was really the dollar amount that appealed to people, that they were not outliers, that the statement about the cost could not be explained was very important, and that this was a routine procedure. People thought it should first of all cost less, and the prices should be more routine. That was a very good example on that.
One last thing. We did a few years ago for the National Partnership for Women and Families, they asked us to do research on delivery system reform. How do we talk about care coordination, medical home, health IT, payment reform? And that was our introduction. And we said back away slowly from payment reform and turn around and run and don’t talk about it at all. It was so hard. And then RWJ decided they wanted to figure out how to talk about payment reform. And it took us about 25 focus groups to get it right between both projects.
So, just a few dos and don’ts. I think this highlights some lessons we learned for other topics as well. Don’t talk about how doctors are paid. That’s where consumers start thinking all doctors drive Porsches, and they get down that road which is really distracting, takes them off issue. Instead, we found that when we said “how insurance companies pay for care,” so, shifting that
focus from how doctors are paid to how insurance companies pay for care. And it wasn’t really villainizing insurance companies, it just seemed to neutralize the discussion.
Don’t talk about doctors giving too many tests because of incentives and that kind of thing. People don’t want to throw the doctors under the bus. So talking about blame, again, a little bit better on the insurance company. But again it was just more sort of neutralizing, saying “Right now insurance companies pay doctors based on how many patients they can squeeze in in a day or how many different procedures.” Rewards and incentives fails every single time, 100 percent of the time with the public. Doctors shouldn’t be rewarded for something they already should be doing. They already should be providing quality care, they shouldn’t be rewarded for that. So, we found instead, “Make sure the way insurance pays for health care is consistent with the way you want to receive it, sort of take at that high level.”
Getting the wrong tests. Again, talk about getting the right tests instead. Getting necessary tests. Whenever we have that language “unnecessary” in it, three people in the focus group say, “Unnecessary to whom?” So we found “getting the same test twice” helps, we also found, for some reason, “tests you don’t need,” for some reason that does better than just flat unnecessary test.
I think I’ll just wrap up. And there is a study online from RWJ on this. But we did walk away with a successful, effective way to talk about payment reform, it is shocking. And it’s really about finding the best ways to provide quality care, backing into it. This means X, Y, and Z, how patients see quality. It also means communication and coordination with your doctors. Then we bring up finding better ways to pay for care in the way you want it based on medical evidence, your doctor’s recommendations. The goal is not to spend more money, but to spend money more wisely.
I think that’s it. I think the last thing I will say is part of the problem here, is the public doesn’t have an understanding of rising health care cost, they just don’t. If there was a baseline understanding of that, I think all of our jobs would be much easier. I don’t see a coordinated effort around that. Consumers think about health care cost in terms of health insurance cost. That’s changing with the high deductibles. But there is just a real lack of knowledge about rising health care cost. So I think that’s the last thing I will say. Thank you.
Social Media as a Tool for Change
Ms. Kelly Young
MS. YOUNG: Being a patient doesn’t define me. I’m a Redskins fan. And a mom, and a teacher. But I grew up here in Washington. I was born on the Marine Corps base, and I learned to be tough as a kid, and as a young mom. I did a lot of tough things. One summer I spread two tons of concrete stucco on the outside of my house. And this is me with a 6-week-old baby and two other children under 5 backpacking in the mountains in California. So I was healthy and strong.
And I woke up one morning 7 years ago with my toe joint so swollen I couldn’t walk on my foot. Within a day the other foot was the same. A couple weeks later I woke up at 2:00 a.m. thinking I’d been shot in my shoulder. I had all five of those kids at home. I have a high tolerance for pain. This pain in my shoulder was like labor. One hour later the other shoulder was the same. This continued. My knees, and then my ankles, and then my wrists. You get the idea. So somebody who could do 100 pushups, I couldn’t pull up the sheets, couldn’t put the socks on my baby. You might think it’s neat, I can’t iron, right?
I got on state-of-the-art treatment within a few months, but it continued to spread. Who knew there are joints in your vocal cords that can leave you silent? Little joints here along your ribs that can make it hurt to breathe. Patients learn a lot of anatomy from this disease. But everybody offers you juice and Tylenol Arthritis. One neighbor actually walked away shaking his head, saying you’re too young to have that. And it doesn’t seem like the doctors understand either. Every time I saw my rheumatologist, I would say, when can I run again? And she would say, soon you will be running on the beach. But that didn’t happen.
So, where do people turn when their life is upsidedown and nothing works and they can’t get help and nobody gets it? Well, they go to the Internet, and that’s where I went. Twitter and Facebook, Blogger, where I started my blog. First I talked with dozens, and then hundreds, and then thousands of other patients. And I met people and read their experiences at the same time I was devouring journal articles and seeing what the medical profession was saying about this disease.
And I still have people ask me every day what this woman is saying, what I asked back then: Why is this so different from what we’ve been told it is? See, if you ask a patient, RA is a disease, it makes you ill. It causes disability, pain, and lots of health problems. But there’s a false conception of RA that it’s just a type of arthritis with occasional extra-articular symptoms, like coronary artery disease. It killed my grandfather. The prevalence with RA is twice that in the general population. And this is only one of many ways that RA affects the heart.
Here is a partial list of ways that RA affects the body outside of the joints. Your veins, your eyes, your heart, your lungs. But I learned that only 60 percent of us show up positive for tests for inflammation, even when we have this disease activity. They test CRP and sed rate, and yet this is what’s used by rheumatologists to measure disease activity. And the other thing that’s used so often by rheumatologists is external swelling; 96 percent of us in a very large study have inflammation that’s detectable with ultrasound, and patients, believe me, know it’s there, but the external swelling is not. And so the rheumatologist would judge these patients to be in remission. And unfortunately, not a large percentage of us have an excellent response to treatment.
This is a typical clinical trial. We have about one-third nonresponders to the treatments that are available. And we hear from the media to eat blueberries, that it’s just a little morning stiffness, and we’re sarcastically asked, why is your disease so expensive when it’s so subtle and you don’t know if you have it? And when the FDA is approving a new drug for the first time in a decade, a new kind of drug for RA, it’s described as an inflammatory disorder that affects the small joints of the hands and feet.
So here are a few shots from my website. This is how I have spent the last 4 years, working far more than full-time, talking to patients, trying to get good information, the most solid and current information, and bring that to patients. But at the same time, bring that patient experience back to the scientific and medical communities.
Ann is one of the stories on my site. Her feet never swelled, but RA destroyed them. I have a few pictures, I have lots more of the six surgeries she had on her feet. And after 20 years with the disease, she finally had a little swelling in her hands. That’s the main diagnostic criterion for RA, swelling in your hands. We asked 1,500 of our patients in our community whether they had swelling without damage or damage without swelling. Because we started to realize we’re not the only ones. We defined damage as bone erosion seen on X-ray or permanent deformity. You put these two together and you see that three-fourths of the patients in our community said that they’d had either damage without swelling or swelling without damage. And only 6 percent had the swelling and damage correlate perfectly.
So we’ve come to recognize that the disease experience living with RA is distinct from what we call textbook RA, what’s being considered in research and most clinical trials. We’re told it’s just a type of arthritis, that it mainly affects the hands, that when joints are affected, you can tell because they’re red and swollen, that there are seldom systemic symptoms, and that patients tend to exaggerate that. Unfortunately what we see is that patients minimize symptoms, hide symptoms, delay care, and the vast majority of them do experience systemic symptoms.
So, I wonder, would this be a really good idea? It was a dream come true for movies at first, right? What if we could go up, like we get the blood pressure machine at the Publix, and stick our arm in? What if they could take out a little blood and the CRP or the sed rate were good enough, and then they could tell us whether we were under control?
I’ve also been a thyroid patient since I was 15, and I know that in endocrinology, this is kind of a struggle with patients, whether or not you can just measure the TSH and get your prescription and know whether you have enough. We know what’s obviously missing is the patient experience, the patient voice. So, 2 years ago we created the first nonprofit foundation in this country specifically for rheumatoid patients where we’re bringing the patient experience out of the box.
We have done two surveys in the last 2 years as preliminary to more extensive studies and surveys that we’ve been collaborating with in the Mayo Clinic and other institutions. But just to give you an idea how motivated patients are to participate in making change, our last survey we had 1,000 people answer that survey in the first 24 hours, 2,000 within 48 hours, and we cut it off on the third day at 2,500. Over the last couple years we have created a couple of posters to present at the American College of Rheumatology in our exhibit, and the copy of both sides of this poster from that survey is in the handbook for the workshop. Of course, we did not discover patient-reported outcomes. This man on the left is a hero to me. He is Dr. Ted Pink, he’s kind of the godfather of patient-reported outcomes in RA. And he has worked for decades to prove that patient-reported outcomes are the most accurate predictor of disease outcome in RA. And yet these are seldom used to measure disease activity.
And so patients ask me every day, why does my doctor say that I’m in remission because of my labs, when my disease is so much worse? And I have to explain to them no, there is no test that can show that. What test did they do? There isn’t even an RA test to show that you have RA with a blood test. You have some inventive methods for imaging, such as a nuclear bone scan or a musculoskeletal ultrasound, that are not widely used yet in this country because we do not have the machines and we don’t have the training yet for them. And we know that we need better communication about evidence. But what the patients I know would like to tell you is that we need communication with patients that will create better evidence.
This is a wonderful abstract I just found the other day in Tokyo, where they’re rejecting evidence-based medicine in favor of evidence of their own patients that they will use to help their other patients. This is just a quick blip from our recent, first-ever Rheumatoid Awareness Day, just to show you that we also use social media for advocacy and awareness. But take a quick gander at these numbers. Almost four million impressions on Twitter. A 12-day campaign, our first ever press release, 250 comments in 1 hour on Facebook. These are motivated patients. They want to make an impact, they want change.
People seek patient communities for information, but it is support that holds all that together. People run toward a patient community like this in social media, because what they’re being told and what they’re reading does not make sense with their experience. And I’m not sure, I hope
you can see it back there, even my hands swell sometimes. People don’t want to be patients. People want to be healthy. But people who become patients need and deserve evidence that more reliably reflects their condition and that they can use to help make better decisions. And that kind of evidence only comes from participation with patients. Thank you.
Audience Participation and Open Discussion
Dr. Susan Reinhard (Moderator)
DR. REINHARD: Thank you. And please, this is your time. I’ll just say a few words as people are getting up, assuming that you’re going to interact with these fabulous presenters. I just want to say a few words as you’re doing that and just summarize a little bit that for Kevin—and there’s so much that you could say about what you had to say, Kevin—just this idea that cost sharing is still somewhat, I don’t want to say mysterious, but there is a lot going on in the equation.
And yet, Tresa is saying in the last 3 years it seems to be making a difference. Those are the two connections I made, that you didn’t see that even a few years before that. What’s going on? I don’t know if it’s the recession, I’d love to hear more about other peoples’ thoughts about why it does seem to be grabbing people more.
And then of course, Kelly, where do people go when nobody gets it? And it just seems like this social media is offering something that just wasn’t there before, and boom, people are finding a vehicle to express themselves and earlier presentations of using those stories as data, just connecting back to our previous discussion. So, let me turn to those who were waiting to talk.
DR. SOFAER: So, I’m concerned about the last speaker who spoke also about incentives, but Tresa is telling us that that word is a terrible word. The problem that I have, and I’m seeing it popping up in health care over and over again, is that we are incenting people—and this is for both patients and providers who don’t understand what they’re being incented to do, they don’t even know that there is an incentive there. I feel like it is magical thinking, what we sometimes do around incentives. And maybe it’s because of what David says, that if you don’t have a feedback loop the incentive isn’t going to show.
But I guess I would like to ask all of the panelists, what is it that we can do to use incentives effectively, as opposed to just use them and think of them as some kind of magic bullet? We did some focus groups to follow up on the focus groups I reported on earlier, and we had some presentations about provider tiering, where there were lower copayments for some providers. People had no idea at all why there was a lower copayment for some than others. Some very cynical people would say, “Oh yeah, I’m being pushed to that provider.” We had one person say, “Maybe they’re trying to give these doctors more money, so that’s why they’re giving them a higher copay.” The extent to which incentives are not understood or misunderstood, what does that mean about our ability to use them?
MS. UNDEM: I think people understand incentives when it’s explained to them.
DR. SOFAER: But we don’t, and it’s often part of the—
MS. UNDEM: We don’t, you’re right. And it’s part of the big mystery of health care cost. And they’re increasing, and people don’t know, and I think we haven’t explained it to the public. I think we’re trying to find ways to do that. I don’t know.
DR. SOFAER: We also have right now, five different economic incentive-based value purchasing things going on in the Medicare program, all directed at the hospitals. I don’t know how they can tell the difference with penalties and rewards and all that stuff.
DR. VOLPP: Every system has underlying incentives. A lot of times they’re not well communicated. I think on the patient side it is really critical that we think about how to make these programs much simpler than they are. Because it’s just ridiculously complex and I think very few people really understand the benefits.
One of the things that we hope is that in the future, we might have a far simpler world where you can imagine that there is a constellation of high-value treatments, and all of those treatments should have no cost sharing. There is no reason for us to be putting cost barriers in the way of a diabetic patient taking their Statin, it’s just self-defeating. And what typically happens now is that typically there isn’t a lot of thought behind this. So there is a copayment for a medication based on what the medication costs that has nothing to do with the value it provides. So if we had a much simpler system, you could imagine we’d have no cost sharing for a whole array of high-value treatments we actually want people to use, and then you could have much higher cost sharing for treatments that people probably shouldn’t be using and which might actually harm them. But we’re a long way from figuring that out.
MR. WOLFSON: I have a comment and a question. I wanted to just underscore what Tresa said about don’t follow your instincts with messages, they’re usually wrong. And we were going to call the campaign Stewardship Campaign. That was going to be our name. And we tested that out and the physicians said, “You mean like a union steward, or you want me to steward all of society’s resources?”
And as we learned from the research, as soon as you went beyond the patient/physician relationship and their well-being and the well-being of the patient—as long as you talked about quality improvement of their patients you were fine. If you talked about an organization and if you went to the society you totally lost them. So, it’s really important. And I also just want to correct that you did select Choosing Wisely. At least half of it. And testing out messages is what we did and the words really did make a big difference. I have a question for you. As far as the incentives, are we talking about a difference of premium versus point of care cost? Is that what’s maybe making a difference in what you’re learning about cost now versus what Kevin is talking about? Because they’re much different.
MS. UNDEM: I think where I’m really seeing it is in the deductible. So, paying—is that called point of care cost? I don’t know the right language. But it’s less about people paying the premiums, it’s more about having the high deductibles and when they have to go, they’re deciding do I need this or do I not, and they’re making those decisions because of the deductible.
MS. OKUN: Sally Okun from PatientsLikeMe, very good conversation, I’m enjoying it a lot. I think to Tresa’s point, vocabulary is so critically important. I communicate a lot with patients online, and a lot of times I have to be very careful and mindful of how I’m choosing the words because the communication first of all is not face-to-face. And then there are always embedded messages within e-mail or other kinds of electronic messaging that you have to be so mindful and careful about, so I find myself getting more and more aware of that all the time.
I want to follow up with Kelly, though. As a colleague in the social media space, I’m interested. You’ve actually quite obviously provided a way of being able to meet an unmet need for the population of patients that you’re meeting with RA. I’m always wondering because this is an area we’re always interested in, is there anything you feel the social media space is not
meeting at this stage that we could be doing better, and how might you articulate that based on what your experiences have been?
MS. YOUNG: Did you mean specifically for RA?
MS. OKUN: Well, your experience has been with RA. Obviously you are gathering a lot of patients and their opinions, and you’re talking with them a lot about the things that maybe they’re not getting in the traditional sense, but they’re getting a lot from having the opportunity to complete surveys or just to connect online.
And my worry is even in our work where we spend a lot of time doing user evaluations and doing persona-based design and trying to understand what do the users of social media really want to meet the needs that they have—I’m just wondering if there’s anything among your population of patients that you’ve been working with that you really felt like, I just wish we could do this, and it would make a difference for so many other people with RA to meet an unmet need that they have that social media still is not even meeting.
MS. YOUNG: I have a very long list of to-do and projects for my own website, RAWarrior.com. I’ve worked between 60 and 80 hours a week as volunteer for 4 years. So I don’t have enough time or staff to get done everything.
So we created the nonprofit a couple of years ago and we have a working board and we have some volunteers and one staff and we hope to be able to work harder, build that into a large organization, and help patients to meet patient needs through that using the resources of patients and partnering together with organizations and government.
As I said, with Mayo Clinic, we’ll work with anybody. We want to see these needs met. But I have to say, what you ask me is something that I’m asked three or four times a month, I get an email or a question asking, can you please tell me what the unmet needs are, and I say we’re working very hard on meeting those.
MS. OKUN: That’s a great answer. And I think that we are trying really hard to do the same. It’s a new place, it’s a new place to do things, and so I think all of us who are in that space really need to be always testing our assumptions that we’re trying to meet the needs that people have out there.
MS. YOUNG: I had to run past it because I was running short, but that slide about information and support with the three points underneath, I’ll go ahead and send you that too. I really think this is what drives patients and these are the unmet needs.
Whether it’s confusion about what the researcher really is or confusing research, conflicting research, about whether a shot works better than an infusion or how different is that than traditional DMR—there’s conflicting research. But all kinds of questions like that that are specific about information about the treatment to information about the disease, these same kinds of questions I imagine that would apply for other conditions.
MS. OKUN: They do. And I think again, as a person who is trying to think forward and really be thinking, what can we be doing in another year or 2, 3, 4 years with this new novel environment where we actually are going to expand the abilities beyond what we can do today? MS. YOUNG: I think the big difference is when people are looking for information in cooking and gardening and other things, the big difference between that and a condition if you’re a patient or you’re caring for a patient is that support part. That’s what holds that together and creates that atmosphere where that information can be freely exchanged.
MR. DEBRONKART: Kevin and Tresa, I want to say last year, truly my life was changed when I read Kahneman’s book, Thinking Fast and Slow. And I came to understand the body of research that drives what you’re talking about. I honestly don’t think anybody can think about
designing an intervention that’s really going to change behavior without studying that field really to the point where they really understand it. So thank you. Very important, I’m glad it came up here.
I’ve known Kelly for a long time, and when she spoke I heard things at a different level than the words that are coming out of her mouth. And what I saw was, I got this thing about what are the nutrients that travel through the information circulatory system, and what drives that? And please if you are at all interested in what a patient community can do, go study Kelly’s blog, because this is not an ordinary blog. I do blogging where I spout my mouth. She has so many links and resources, and it’s a technically incredible website.
And the thing that occurred to me, this morning we heard about Marshall Ganz saying distributed leadership, and they said, we have this issue of if we can’t get change through the establishment, how do we get it where it needs to be? Well how about we go through sort of the underground railroad of information going directly to the people whose lives are at stake?
And what I’ve seen over the last couple of years on Kelly’s blog, if we want change it’s really worth studying this, what’s going on there that causes these supposedly slacker consumers who we can’t get to change behavior to step up and be hungry for information. What’s going on here that’s different than the paradigm? Thanks.
DR. MONTORI: One aspect resonating with Kelly’s presentation in relation to the outcomes that we measure and that we incent or promote in pay-for-performance or other strategies that are doomed from my point of view but still exist. And the quality of life in patient reported outcome stories is very interesting. But one outcome that I would like particularly the patient communities in the room to start paying more attention to is the notion of burden of treatment. There are a lot of discussions out there about burden of illness and how it affects the ability to function. But in the case of patients, particularly that accumulate multiple chronic conditions, the burden of treatment plays a huge role in impairing peoples’ ability to perform and to live lives that are spontaneous.
And so there is a notion out there of a new kind of medicine that tries to reduce the burden of treatment in patients like alongside pursuing patient goals, and that’s called minimally disruptive medicine. And so I want the patient community in the room to be more attuned to this and to begin to advocate for alongside measures of quality of life, measures of burden of treatment.
MS. LIND: Hi, I’m Cristin Lind and I was the one who stood up yesterday and talked about my concern about culture eating strategy for lunch. And so I’ve been thinking about that as we’ve gone through the last day and a half, and I was very happy to hear you talk, Kelly, because I think you kind of raised something that I as a mom who for many years wasn’t activated and wasn’t engaged and then suddenly was. And I’m very curious about how something like that could happen. How could somebody as unengaged as I was be standing here in this room today?
And as we think about partnering with patients and engagement and activation and trust and cultural competence, I think that there is also a very special role for patients and families as representatives in the health care system to be a bridge, to be a liaison between medicine and patients.
And I hope that I’m articulating this well, but I’m going to try to wrap it up. Whether it’s as family and patient partners on QI teams or through patient and family navigators or liaisons, I think that as we think about trying to build a pathway toward partnership, we think about what is a very specific role that people with lived experience can play in bridging this partnership which has a lot of cultural obstacles to it. So, thank you so much.
MR. ROEHR: Hi, I’m Bob Roehr. One of the problems I have, everyone likes value, but so often in the past, value has been defined as value to the health care system or to someone else, not necessarily to the patient. And when it has been defined as value to the patient, it has been defined according to data and generally according to the mean or the average.
So it doesn’t deal very well with the outliers, the people who don’t respond well to drug A, but do respond to drug B, even though it’s the secondary one with higher copays or whatever else. The system also doesn’t respond very well to different values of the patient in terms of what they’re seeking, whether it is relief from certain symptoms, better functionality, quality of life versus quantity of life, things like this.
So, I think we have to start thinking of value as being very individualized to the health plan of the patient based on their desires and what works for them, and not simply fall back into what is easiest for the system, which is a bunch of numbers.
DR. VOLPP: I think it’s a really important point. And I see this as one of the big challenges to implementing recommendations like the Choosing Wisely Initiative. Because in essence, as you’ve said, there is a heterogeneity of treatment effect, and so, on average, the service may be extremely low-value, but there is going to be some portion of people for whom it may be at least moderately high-value. And figuring out how to come up with defensible and simple rules that, for example, a health plan could use to adjudicate who gets this coverage and who doesn’t is actually very complicated.
We’ve had a number of discussions with health plans about trying to do that, and it becomes a stumbling block very quickly. So, somehow we have to figure this out. I don’t think it’s a reason not to proceed to help the 95 percent or 90 percent or 80 percent or whatever it is for people who are low value. But it is a big challenge to figure out.
MS. KORNBLAU: Barbara Kornblau from the Society for Participatory Medicine. I just want to give kudos to Kelly. I have arthritis and I worked with a lot of arthritis support groups in the Miami area. And what we did is if someone called the Arthritis Foundation and they were diagnosed with RA, they were immediately referred to one of my friends, Linda, who has had 31 joint replacements. And she would give them the introduction and help them through the system. So I just want to stress that power of patients again.
And one additional point, and that is on quality of life. We measure quality of life. Providers will often ask people how much sleep do you get, are you taking your meds, all those standard questions. And one of the studies that I’ve worked on in my occupational therapy hat looked at a concept called occupational autonomy. And it was very simple; it was being able to choose to do the occupations or things that are meaningful and purposeful to you when you wanted to do them. To be able to do the things you wanted to do when you wanted to do them. And we call that quality of life.
And I think it’s very important to ask the patient when you have chronic pain, when you have days that you can do things and can’t do things, to just say what do you want to be able to do? What’s your goal? What can’t you do now that you want to be able to do? Let’s work toward that.
DR. REINHARD: Thank you so much. Please join me in congratulating them.
BUILDING A PATHWAY FORWARD
Ms. Christine Bechtel (Moderator)
MS. BECHTEL: We have had an absolutely terrific day and a half, and we thought that maybe the best way to kind of wrap up, given how intense we knew it would be, would be to ask a number of our esteemed planning committee members to join us here and provide their observations, having been here with us all along the way and having been part of the discussions that really had a substantive role in shaping the agenda.
So, I have up here with me first Mark Gorman, who is a patient advocate and a cancer survivor. Many of you know him from his leadership role at the National Coalition for Cancer Survivorship. We have Art Levin from the Center for Medical Consumers. We have Sue Sheridan from PCORI, the Patient-Centered Outcomes Research Organization. And we have Terry Adirim from the Health Resources and Services Administration, or HRSA.
So, I’ve asked you guys to give a 2-minute snapshot, key takeaways, whatever it is you’d like to say, and then we’ll have a little back and forth. So let’s start with Mark.
MR. GORMAN: I have a few talking points that I put together last night, which I will get to in 1 second and I will be very close to my 2-minute limit here.
But I am trying still to wrap my head around a lot of what David Goldhill had to say. And I think one point that is buried in there is I think I hear him saying that the status quo which nobody is happy with depends a lot on an assumption that the patients who are supposedly the principal beneficiaries of the health care enterprise are at some level just incapable of being able to fend for themselves. So, we have the intermediaries in the insurance industry that have built up, and all kinds of other people trying to protect us from harm being done to us. That does need to be challenged, and I think that’s actually a central theme that we’re trying to get at today.
Other observations that I think are worth sharing. I was taken by the three-level framework for engagement that was just mentioned at the beginning of the meeting yesterday that’s in the policy brief from Health Affairs that was in the materials. And there is another I guess longer paper that maybe actually you guys can dig out and make available to us that has been referred to as well. In cancer advocacy, this sort of three level, what we’ve referred to as an advocacy continuum, was described by Ellen Stovall and Elizabeth Clark in 1996, and has been used by those of us in cancer patient advocacy extensively ever since then. We’ve used slightly different kind of language though, which I think is very helpful to insert here. We’ve talked about personal or self-advocacy on one end of this advocacy continuum, community advocacy in the middle, and then public interest or policy advocacy on sort of the other end of the continuum. My observation working with cancer survivors over close to a dozen years now is that individuals actually can evolve along that continuum.
And I think this is implicit in this paper, and I’ve learned from doing policy or public interest advocacy training with cancer survivors and their families over the years that initially the word advocacy and this whole language of advocacy is kind of off-putting to them, until I’ve explained to them how they’ve always been, in order to navigate health care successfully in the cancer context, effective self-advocates. Then they start to warm up to the idea. But the skills in being an effective self-advocate are actually transferable skills to being effective as an advocate for the patient perspective in the public interest arena. It’s just you have to learn how to be able to frame the context of your experience and story differently. Instead of trying to get good care in
your immediate clinical encounter, you’re trying to use your experience to policy makers and not just legislatures.
So that’s one point. Another point I think is important to make is let’s not hope for too much of an outcome from one particular element of patient engagement. I refer you all to Dr. Berwick’s paper on the wedges for dealing with waste, I think he called it, which was published in JAMA at the end of April of last year. And he cites failures of care delivery, failure of coordination, overtreatment, which we’ve spent a lot of time talking about here, administrative complexity, pricing failures. We heard a whole talk about pricing failures and fraud and abuse cumulatively as driving the problems with health care costs.
The kind of patient engagement we’ve been talking about here can be helpful in the clinical encounter, but we can’t solve all these problems there. However, getting back to my idea of the advocacy continuum with the stages of evolving patient engagement—as Kelly just explained to us from her own story’s experience, people become motivatable to become advocates on the policy or public interest aspect of trying to deal with health care problems as a result of their need, oftentimes, to become effective advocates on their own behalf. So I’ll stop there. I had maybe one more paragraph but maybe I’ll insert it another time.
MR. LEVIN: So, I have 20 pages of handwritten notes sitting here. I want to assure you that there is going to be a report of the workshop, so I feel that there will be the opportunity to show you the details that way.
So, I am going to talk a little bit about strategy in politics. I think we would all agree that what we talked about during this day and a half is complex. It’s difficult politically, and culturally. We heard that culture eats strategy for lunch. Maybe. I think that if you’re a good strategist, you need to take that into account and just maybe you can bite it back.
I think we’re in an era where people are struggling to keep their heads above water in all aspects of their life. And I mean as patients, as families, as caregivers, as clinicians, as CEOs of hospitals, people running rehabs and long-term care; for everyone these are difficult, difficult times politically and economically a lot of uncertainty. And we’re dealing with a sector that is probably the most resistant to change of any I know. So, we have a sort of difficult job ahead of us.
I think that we have to be careful about how big a boat we are trying to float at any one time here. We have to really get to be strategic and political in how we think about it. So, I would suggest—and I’m not going to ask Michael to sponsor it, but he might—to convene a priority setting exercise, hopefully driven by the people we’ve been focused on: patients, families, and caregivers. We want to put caregivers in, because some people don’t have family members as caregivers, they have friends and others. I think we need to think about what’s the most important place. And by we, I mean the bigger we, the royal we. Where do we need to begin? What’s the most urgent? And then we sort of need to create another grid, which is what’s the most attainable. What do we think we’d have the best chance of getting? And then crosswalk those and see if we could come up with one or two potential “wins” in the short term that would get us moving along the pathway.
I think we need to always be cognizant of the barriers. We need to evaluate what the barriers are and how difficult it is to overcome them. We all agree we need payment reform. Do we really think we’re going to get to that payment reform nirvana tomorrow? I don’t think so. I think that there is a long battle ahead of us.
I would argue that engagement is not a theoretical exercise, that we must present real and practical values and benefits to what we’re suggesting. And let me just give you a quick analogy.
I have argued with efforts to educate the public about the benefits to them of HIT and HIE that we don’t have much to show them. We’re asking them to enter into a social contract to give us their data and for us to use it, and we’re sort of promising that their care is going to get better. It’s very hard to demonstrate that. So, I think we have in sort of creating this priority list, we have to think about where can we really deliver, to use Ken’s word, the “hook”? Where can we really say to patients, we promise you this, and we’re going to deliver it next year to you, and you’re going to see the value of what we’re talking about. We need to demonstrate that a learning health care system and shared decision making, has real value for the public
Lastly, the one thing I worried about, and I think somebody else has mentioned this, that we’re spending tens of billions of dollars on health information technology exchange. I don’t see very much attempt to integrate patients, families, and caregivers into the process, other than give them a portal and let them look at their lab values. I think we need to be thinking far differently about that. For one, they should be in at the ground floor. It’s a problem because vendors don’t even have clinicians in at the ground floor, which is one of the problems with the usefulness of their product. But we really need to have that community of patients, families, consumers, whatever we want to call them, caregivers, really engaged in this. And we have to design a system that meets their needs. And maybe patient portal and looking at lab values is good for some people. It might not be the priority of some other people. I don’t think we understand what is, as yet, but I worry that the horse will be out of the barn, we will have spent tens of billions of dollars on a system that doesn’t even begin to deal with the concerns that we’ve been talking about for the last day and a half.
DR. ADIRIM: I’m Terry Adirim. I am from the Department of Health and Human Resources, the Health Resources and Services Administration. My agency serves the underserved by providing funding to health care entities to provide health care services. I had the great pleasure of being on this planning committee. I want to thank you so much for including me. I learned so much from my colleagues and I learned so much from all of you in the last day and a half.
My remarks are very brief, and they’re centered around recapping what I heard from our workshop speakers were the barriers to achieving partnering with patients to drive shared decision making, and to summarize some of the approaches and solutions that came from our speakers.
Health care has been transforming very quickly. An example includes a recent experience I had with the health care system. I got a mammogram, and received the results from the radiologist by e-mail before my doctor did, which I thought was kind of amusing. These changes give all of us the opportunity to impact the way medicine is practiced going forward. And I think listening to all the patients over the last day and a half really gives me a sense of urgency to do this and I really appreciated hearing everybody’s stories.
So, what I heard over the last day and a half—that some of the barriers to achieving what we’re all trying to achieve, is that we’re still seeing within patients some passivity with regard to their health care, that there is a top-down authoritative culture within the medical profession, among both physicians and other practitioners. In fact, at this workshop someone told me about one of her experiences in the emergency department where a nurse authoritatively told her something, it wasn’t entirely accurate and gave her a look like who was she?
I also heard articulated that there is a skills gap for both practitioners and patients with regard to how to practice shared decision making. There are also barriers with regard to access to
information. And many of these gaps and challenges, as my colleagues have articulated, are due to technological challenges that I think we need to overcome.
Part of the issue is that health care is not really a system because it is fragmented and siloed. It’s not really oriented to patients and patient needs. It’s really focused—and I’ll be the first to say as a physician—it’s really centered on the practitioners and our needs. So, until we change that culture it’s going to be very difficult to make the changes that we’re looking for.
I think there are also real or perceived external pressures on us as practitioners. As everybody has talked about over the last day and a half, are the challenges within the payment structures. Fee-for-service payment leads to pressure to see more patients. And there are also regulatory and policy issues, including the way that we interpret these regulations and policies that are real barriers to being able to get where we want to go.
With regard to solutions, what I’ve heard from all of you is that we really need a multi-prong, multidisciplinary approach. And what I took away from our keynote speaker is that we can learn a lot from people outside of medicine and people in other industries. Even though I didn’t agree with some of what he had to say, it is useful to include all views while determining strategies to improve health care. For example there is so much with regard to the manufacturing industry with regard to quality and other industries such as systems engineering to improve efficiency that we in medicine can learn from. So we need to bring other people to the table.
Yesterday, in fact, a speaker mentioned that some of the issues could be ameliorated through a systems engineering approach. Some of us may agree and others may not but it would be useful to include some customer-focused strategies in our thinking about health care improvement. Even things on when and where patients get their treatment. Who said that you have to go to the doctor’s office to get your treatment? Who said that primary care must be available only on Monday through Friday 9 to 5? So, even just engineering the system so it’s more patient focused would be something to move toward.
I heard a lot of physician and patient blaming language, and I caution people from blaming any people about this. Blaming does not help us to indentify the issues to address. It’s the process, not the people. So I think that we really need to spend a lot more time focusing on the process.
We really need to address competency development, and training. We need to look at where we’re training our health care providers, how we’re training them. We are moving more toward team-based approaches, and I know at my agency a lot of the funding for health care is moving to interdisciplinary approaches care. So we’re moving in that direction, we need to keep promoting that.
I think, too, listening today to our speakers, that we need a new research paradigm. Emerging is a more inclusive type of patient approach, and I think that’s really good, especially when it comes to governments’ opening up of data sources, use of data, and the giving back to patients who participate. And as we heard today that technology and social media are very important tools for reaching patients and facilitating communication between patients and their clinicians.
Transparency too was a running theme over the last day and a half especially with regard to research. With regard to that there may need to be regulatory solutions. Transparency with regard to health care costs is important. And the Time article that came out recently made a huge impression with many of us with regard health care pricing. I think though we need to approach health economics with caution because health care is not a commodity like other commodities or like my iPad. Everybody will eventually enter the system and need health care and many of us
believe that we’re entitled to it. So there may need to be different economic principles applied to health care.
MS. SHERIDAN: Great, that’s a nice segue for me. It’s been fascinating for me to participate in this because I wear two hats. I am the Director of Patient Engagement at PCORI, Patient-Centered Outcomes Research Institute, but I also wear the hat of a mom. Like Cristin, I have a son who is a young man, who has cerebral palsy, multiple disabilities—we are frequent fliers in the health care system. And his condition was caused by newborn jaundice 17 years ago that was completely preventable.
I also speak as a widow. I speak as a widow, where my husband Pat died 12 years ago of cancer. And it was a cancer that was diagnosed properly but the pathology got lost for 6 months and it was not communicated. So I listened the past 2 days through the patient lens, and also the research lens. And it’s a lovely combination.
PCORI is about the perspective, the wisdom, and the outcomes of the patient population. When I say patients, it includes caregivers, family members, and advocates. Combining that with rigorous research I think that THAT is going to be the kind of science that drives change.
And so what I walk away with today is hope. I am aware of barriers, I am aware of government challenges, I am aware of cost. But 10 years ago there would not have been patients in this room, and today we have patients in this room. And we have a lot of patients in this room.
And I want to thank Dave and Kelly and Perry and Cristin and Greg and Ronny and Linda—all of you. We are here because of you. And you are our teachers, and we’re all teachers and learners. You gave us vision today, and this is important for us to focus on vision and hope.
So, what I heard today—and I’m sorry if I don’t remember your names—I heard today to listen to what patients are clamoring for. I love that, because we are clamoring. And I heard that we want to be safe. We want to be informed, we want to be empowered. We want compassion. We want to survive. We want outcomes that we decide and we want quality of life amongst many other things. And I think addressing some of these challenges that we have, if we keep this paramount we can make a difference.
So, Greg Biggers mentioned the “new we,” and I loved that. Thank you, Greg. And we’re talking about a new we. Sally talked about a patient-powered network which I think is really important to think about. Patients are powerful. Our data is powerful. Our experiences are powerful.
So, something that was described earlier today—I suffered this when I was a patient advocate. We wanted change and we wanted it fast. So, we demanded solutions from The Joint Commission and from NIH and from CDC and from researchers who partnered with us. And they said hang on, good solution, but we need evidence. So, we backed up a little bit and we joined researchers and we developed the evidence and we gave it to CDC and we gave it to The Joint Commission and we gave it to those who regulate and create protocols for our country. And we saw change. It took us 8 years, but it happened. It happened in partnership. It happened in partnership with HHS, with researchers, with parents, and those parents drove that change.
So, what I’m seeing regarding patient engagement is coming from the research world at PCORI. We are bringing patients in. And we are learning. We want you to help us. We’re trying to infuse patients at every step of research. And so we’re inviting patients to submit research questions. Tell us what’s missing. Tell us what you need us to research based on you and your life and your challenges and what information is missing.
We’re bringing patients in and we’re training them. We have patients who are sitting at the table with scientists reviewing proposals and deciding what PCORI funds through their lens.
We’re bringing patients in to help disseminate when we have research results. Traditionally, research goes into peer-reviewed journals; moms and dads and patients typically don’t read those. How do we find these creative pathways? We bring the patients in to help us do that.
And then how do we evaluate ourselves? We want the patient population and caregivers and stakeholders, we want clinicians to tell us how are we doing and how can we do this better. So we’re creating an infrastructure right now, bringing people in as much as possible as we can. We’re going to be empaneling a patient engagement advisory panel in about 6 weeks to help guide us, help make sure that we are patient-centered and we are engaging patients every step of the way.
So, what I am hearing and feeling over the past 12 years as a patient advocate or activist, whatever we call ourselves, we were pushing. We were calling for change, we were pushing. I’m seeing a shift now, where we are going to be pulling for change. We are going to be in front pulling along the system with us as partners. And that’s a difference. And I see that pull effect going on with these discussions.
So, in conclusion, I think that we have an opportunity to make a difference in patient lives by really bringing in the patient points at every step of the way, whether it’s research, whether it’s as a patient themselves, if it’s in policy making, if it’s at the institutional level. Let’s look for every avenue where we can plug the patients in.
Peter Margolis said, what if? Consider the what if. What if we did this? What if we had patient-powered networks and patients sitting on QIs and IRBs and in research? And that’s what I invite you to envision. I challenge you and I invite you. And I think that collectively we can make a difference. Thank you.
MS. BECHTEL: So, I have three questions, one in each of the areas that we talked about. I probably have 500, but I’ve tried to narrow it down to three so that anyone who feels like taking a shot at it could.
The first is in shared decision making. We heard from Gary Langer that more than 80 percent of patients would like to have shared decision making. We know from actually the research that Tresa talked about earlier that my organization asked them to do, we tested the idea of shared decision making in juxtaposition to some other health reforms like payment reform and IT and patient-centered medical home. And it wasn’t particularly compelling, because everybody said that’s just a fundamental right.
So, I think we have a situation where there is a lot of openness and willingness to engage from patients. So I guess my question is what you guys sort of think the holdup is. Because I’m not sure it’s consumers on this. As we think about a pathway forward for shared decision making, where do we start?
Audience Participation and Open Discussion
MR. LEVIN: I have to do a disclaimer. I’m on the Board of The Foundation for Informed Medical Decisions, so I just want to make that clear. I think shared decision making is important. I think we’re talking about a democratic process. Sort of philosophically, I see this as democracy. In my more than 30 years of advocacy talking about the need for giving patients and families and caregivers the information they need to make informed choices before it was ever a foundation, I just saw that as basic democracy.
And if you go back to when I started, we lived in a really closed world. There was one medical reporter, Larry Altman of The New York Times, who was an MD. There was no one else
around. If you wanted to look at the PDR it wasn’t in Barnes & Noble, you only got it if you were a practitioner. You couldn’t get into a medical library. You could get into regional medical libraries like the library of medicine, but it was a nightmare to get through it.
So it really was the control of information. That’s the opposite of a democratic state. So I always thought of it as a basic principle that in a democracy we needed to share information. There is also—and I have forgotten the name of the report although Michael may remember it—in 1982 there was a President’s Report commissioned on biomedical—long name. And there was one chapter of that, which is one book on self-autonomy in decision making. And this is going way back. So they probably did this study in the 1980s. And they asked people from various backgrounds, demographics, do you want information so that you can make a more informed choice? And the vast majority of people said yes. And this was in an era when there was no information. So I think that longing for information, that longing for participation, has been around for a long time.
The other thing is if we really believe in informed consent as an ethical and medical imperative, how do you give informed consent if you don’t have any information? You’re just signing a piece of paper which is mostly what happens now. It’s a sham. People are not really giving informed consent to whatever it is they’re being asked to undergo.
So I really think that shared decision making is a critical point. I think there are ways out there where people are experimenting. Washington State, for example. You can imagine mandating things. You can imagine payers saying we’re going to pay more or we’re not going to pay, unless there’s some documentation that’s reliable that there’s a shared decision making process.
So I think that may be one of the priorities in the sense that we sort of understand it well, we have a lot of evidence about its effectiveness. And it’s probably doable. It’s not easy, but it’s probably doable. And we have a lot of examples throughout the country where people have done this successfully, either through mandates or on their own initiative or through grant programs. So it would be a good place to begin.
MS. SHERIDAN: Something I think that in terms of shared decision making and participation, I was at the WHO for 7 years working with patients all over the world, and the WHO did a survey on outcomes and if patients wanted to participate in assuring their own outcomes. And we sent out a survey, got a response from 59 countries, and the overwhelming response was yes, we want to participate. It didn’t matter the culture, the country, the government, the economic status, yes.
And then we said, what do you need to participate? And the answer was an invitation. And so have we, as a health care system, appropriately invited our patients and caregivers to participate in improving good outcomes? It was a simple response by the patient population, and the WHO honestly thought it was one of the sexiest pieces of surveys that they’ve ever done because it was so simple that it was overlooked prior to this. And so I ask, are our clinicians, are our hospitals, are our systems, is our government, are we extending that invitation to come participate with us?
MS. BECHTEL: I think that is actually a good segue into a question about value. I thought the sessions today were really phenomenal. But they pointed to a real tension point for me. So on the one side we had—and Chuck Alston has a great slide on this, where he says value, VALU, is a four letter word for patients, for consumers. And we heard a lot about why that is today. And we heard Marge Ginsburg talk about the need for more public deliberation, and how do we shift expectations. In fact, that was the title of the session, changing expectations.
On the other hand, we heard from Dave Debronkart, and this has been my experience as well
and we’ve heard from a couple of other folks in the room, that when they were all ginned up to go get the cost information to find the high-value providers, because clearly they had either deliberated their way there or they had a high-deductible health plan, what we found was that the system was absolutely ill-equipped to give it to them.
So, on the one hand, it feels to me like we want to invite patients to engage in this discussion about value and cost and quality. And on the other hand, when they accept the invitation, we say you go over there, we’re not ready for it. So I think Dave also used that four-part hierarchy of data, information, knowledge, and wisdom. So if we think about that, I don’t even know where on the spectrum we’re at with respect to cost information. We’re not at the knowledge part, we know that.
AUDIENCE: Are we at the data part?
MS. BECHTEL: That’s what I want to know, right. Are we even at the data part? How do we move forward?
MR. GORMAN: I would say that we’re not at all. For most of the last year I’ve been branching out in my life as a patient advocate. I’ve spent a lot of time in Texas with my 92-year-old mother who is in good spirits, but has a lot of things going on. Last May, she was in hospital for a month. Part of that was necessary, but when the summary came from Medicare and I added up all the punitive charges, it was close to $500,000.
What David was talking about before, there is virtually no honest pricing information available. So pricing has completely failed. It’s what Dr. Berwick is talking about as one of the problems. Pricing has completely failed to send signals that are meaningful to patients in any role as buyers, except we’re starting to get some and maybe more on high-deductible plans. But even there, I think people are going to end up in sort of one-off negotiations at the time of service and the point of service with the provider they’re talking to with an eye toward what is going to be the impact on the deductible. I mean it’s not going to be market-based decision making.
MR. LEVIN: Excuse my ignorance on this, but I’d like to ask people at the table out there. Is there any evidence giving people cost with how it works right now makes any difference? Because if we’re all evidence based—
DR. SOFAER: (Off mic response)
MS. BECHTEL: For those of you who couldn’t hear because poor Shoshanna doesn’t have a mic, was that her work found that it actually could be dangerous to give consumers cost information. And I would say I think you mean in this context in particular, in this health care system. My sense is that—and I would love to know what you guys think, my sense is that what David Goldhill was really arguing was that if we open it up, actually forget giving them cost information, just make consumers responsible for burying the cost, the market will restructure itself.
Now, I have to tell you, being at the age where a lot of people in this room are probably going to be on Medicare, certainly before I will, but before this David Goldhill system comes about, I don’t want to be caught in the middle. So I have to tell you. I mean, what do you guys think about this idea that let’s just put the burden on them because in some period of time the market will restructure? Will it work?
MR. LEVIN: There is no question that people are more sensitive to what they have to pay if they have to actually pay it out-of-pocket. I think that’s a no-brainer. Is that the right way to deal with health? David was up there saying we’ll deal with catastrophic illness, we’ll deal with this, we will deal with that. One of the assurances of that, I was glad to hear he was in favor of National Health Program, very nice.
But I think we really have to pilot that kind of idea to see what the risks are. We have a growing vulnerable population, not just by age, but by all kinds of disabilities and disease that require a lot of care. I know the 90-10 is an interesting artifact, and I think all the things we said are sort of fascinating challenges to the exceptionalism of health care.
Whether the answer is to simply give all of us the $10,000 or the $15,000 to go out and buy our own care, I’m not sure. Because I don’t really know if we’re ready, if we can equip people with the information and the skill sets they need to make the right choices. I don’t think we’ve been very successful in doing that even without the challenge of, you’re going to pay for this out of your own pocket.
So it isn’t really a marketplace, right? If I know what a copier is supposed to do—so when a company makes a bad copier, it means I go to the copier and I push the button and it jams or it doesn’t produce a copy. I’m not sure we know if I break my knee what the outcome necessarily should be. I want to be better, but I don’t know how much better it can be. It’s a very different world. I don’t think you can make just a transfer that this is like any other business, it’s like any other marketplace. It is in some respects, it isn’t in others.
DR. ADIRIM: I agree with that because what happens is if you’re responsible for paying for something which could have a huge impact on whether or not you have a good quality of life or live or die, you have people in certain age groups who would forgo that care. It has been shown in certain studies that people of a certain age group, older, elderly, will give up whatever they have for younger generations. So that’s why social security was created, so that we could take care of elderly people. I don’t think health care runs by the same economics as other commodities. So I think you have to be very careful.
That said, I think he had an interesting point because there is a difference between emergency type care, critical care, versus preventive care. So perhaps doing demonstrations or models where people would pay for routine care as opposed to more catastrophic, what’s now considered higher cost care, could be something to look at and then develop that evidence that you’re looking for, whether or not you can change people’s behavior with regard to use of health care.
MS. SHERIDAN: Well, maybe this is a bit Pollyanna-ish but going back to patient engagement and having patients guiding change in research—and the reason that I say this is just the “what if,” Peter’s “what if.” If we did bring in patients at every level of research and solutions and systems and policy making, could we expedite change? And could we expedite better health care and better outcomes? And the reason why I think this is because, when I referenced what this mothers group in changing the standard of care for newborn jaundice, within 4 years of when we started with our researchers and the system, Brent James from Intermountain Health and Hospital Corporation of America implemented the solution even before there was evidence, and they reduced newborn readmissions by 30 percent. Somebody was saving money.
And so I think the patient piece of driving change can be an expediter. Patients rarely give up, and honestly the researchers that we’ve worked with said the patients kept us on task and they kept us going when we were wearing out. But it was also the other way around. When the patients were getting worn out and frustrated, the researchers kept us going.
And so can we use patients as a catalyst to expedite change that will help save us money? I know that’s not a short-term solution, it’s not the whole solution. But it’s part of the solution that I witnessed that I think it would be great to study. I know somebody who might be able to study that.
MS. BECHTEL: Might have the funding for it, huh? A neurologist told me that when you hear a new idea, it fires the same receptors as pain in your brain. So I was feeling a little bit of pain in David’s presentation, but I don’t want to dismiss it because I get the point. All it takes is the one doc practice who everybody suddenly realizes they’ll see patients after hours, they post their prices on their website. We have little teeny examples here and there of people doing that.
And I think it is really notable to point out what Tresa said, and what Chuck Alston also said in his public comment, that for the first time just in the last year or two, they’re really sensing a bigger or deeper anger and frustration with cost issues and that there may be kind of a change on the horizon.
So, I’ll say before we wrap up, maybe we got the agenda order backwards. Maybe it has to be the research pathway first to set the stage and provide the evidence for shared decision making, which is how we’re going to get ultimately to value. So we’re going to wrap up and turn it back to our host Michael McGinnis here. But before we do that, any burning comments from our panel?
MR. LEVIN: Just one comment I want to make. I think it’s important to keep in mind the rapidity of change right now; we’re in a world of rapid change. And a lot of what we have talked about is today, and not about tomorrow. And so by tomorrow, what we talked about today will be out of date. It’s a new paradigm of thinking that we really have to be thinking far down the road. We have to deal with today’s problems, but we have to deal with tomorrow’s problems even more. So we need to really always be doing that stretch.
And as people have mentioned, we have a whole new generation coming up who doesn’t have a laptop like I do or a desktop, but really a device in their pocket. And it’s the way they get information. They go out to a restaurant, they don’t read a magazine; they look it up, get the rating.
So, we just have to bear in mind the rapidity of changes is overwhelming. And we really have to sort of train ourselves to say whoops, we’re thinking in today’s world and we really need to think about what tomorrow’s world is going to look like.
SUMMARY AND NEXT STEPS
MS. BECHTEL: I want to say two thank yous. One is to the planning committee members, not just those up here on the stage, but those in the audience, if you want to stand and we can recognize everybody. And I also want to say thank you to our host, the Institute of Medicine and Michael McGinnis for his passion and commitment, and the staff for their support. We’re very grateful for your interest in the topic. Thank you.
DR. MCGINNIS: Thank you, Christine, and thanks to all of you. This has been an extraordinarily rich and stimulating set of discussions, informed, directed, and inspired, as Susan said, by the patients who are here to help lead the discussion. In many ways, it has been a pioneering activity for the Institute of Medicine and the National Academies in focus, in scope, and in importance.
This workshop embraces the central challenges that face the health care system today—better outcomes, lower costs, faster progress—and it has done so by seeking the Holy Grail of motivating and mobilizing the people who are served by health and health care in our nation as drivers for change—how can we democratize and grow the influence of people on care improvement, on lower costs, and on quicker progress? Not surprisingly, when pursuing a holy
grail, the path can be elusive or, at least uncertain. That is clearly the case here. As Art just pointed out, we are looking into the future. We have to keep our eyes on the future very squarely, continuing to look as far beyond the horizon as we can, because things are changing very rapidly and we can’t be held back or held down by perspectives shaped in circumstances today that may not pertain tomorrow.
We have heard a number of very interesting ideas, as well as a number of expressive take-home phrases. I have jotted down a few of them in each of our three categories: care decision strategies, value and quality, and knowledge generation. With respect to care decision strategies, we heard that a meaningful care experience is when someone goes out of their way. We heard “listen first, listen fully.” We heard “patient engagement is a skill, not a trait.” We heard “connectedness and connectivity count.” From one provider, we heard “decision aids save me time.” And we heard that “culture eats strategy for lunch every time.” We have heard that “real innovation is truly disruptive,” and, for us, truly disruptive would be the movement of care choice to the point of the individual. We heard about “the power of distributed leadership.” These concepts shape our thoughts about what we can do with respect to care decision strategies that will improve the future of health and health care.
On the count of value and quality, we heard that “money is a proxy for quality in every industry but health care.” And, of course, that is true. However, we also heard that “wise use of resources resonates with people” and offers a foundation on which we can build. We were advised to let quality lead on value. We heard about the importance of the 3-second rule—“if it’s not engageable in 3 seconds, forget about it”—as a means of motivating change. We heard that absolute dollars register more than dollar signs when conveying information on outcomes and quality and cost. We heard the question, “Who is the trusted translator?” as a very important perspective to bear in mind. We heard that real incentives have feedback loops, and that “getting the dynamic of the feedback loop right is just as important as getting the initial message right.”
In the area of knowledge generation, we heard that “patients represent untapped data streams.” We heard about the “paradox of protection.” In protecting patient privacy and prerogative, we have left patients unprotected with respect to the loss of evidence that otherwise could be generated. We heard that there is little hope of solving the long-term problem without integration of care and learning. We heard that data sharing will drive change, but “data sharing is not sharecropping.” This offers us an important admonition that “permission matters” when we are expanding our ability to mine clinical data. As a nod to the higher calling in knowledge generation, we heard that we owe it to ourselves, to our families, and to society to draw upon this resource for improving the public good in its most fundamental fashion.
From these and many other take-home phrases throughout the course of this workshop, we’ve heard a number of suggestions about what needs to happen as we look to the future with respect to care processes, with respect to scientific insights, and with respect to price, cost, and value. In the care decision arena, we clearly need to focus on ways in which decision aids and decision information can be mobilized and delivered as efficiently as possible. To begin to work on the issues of trust, we need to work on the challenges affiliated with the multiple loci of information that is produced, and improve access to trusted information across the board. Of course, programs like Choosing Wisely are fundamentally important steps in that respect, and there is much more that we can do. We also can explore, it was suggested, possible approaches to shared decision making as a covered benefit. What are the strategies here to provide the economic incentives possible? If we’re really interested in care culture that changes both professional care culture and other elements of the culture that shape our future care delivery
processes, we can make sure that we’re clearly future-oriented as we train health professionals. We can make it clear in our training processes that it’s not just team care, but that it is team care with the patient firmly embedded in the center of the process, and that the learning really draws from the patient.
In the quality and value arena, possibilities include those just mentioned about marshaling information on quality, costs, and value in a more reliable fashion: building the science of transparency. To do that, we are going to have to better marry the processes of gathering cost information with those of gathering quality information, so that we have a more level playing field in sharing information with the public. We need to work on the graphic strategies for communicating information on quality, cost, and value. We should not despair of the fact that our current set of data points on cost and pricing is lacking at this point. We have a fundamental societal obligation to improve those data points. We can’t just ignore them. This may be our most fundamental challenge: doing everything we can to marshal honesty in our information on costs and prices.
In the knowledge-generation arena, we have to develop a communication strategy to better make the case to the public that they can and should be advocates for using their information for care improvement. We need to develop practical, trusted approaches to privacy and consent as we deal with the imperative to draw on clinical data in a seamless fashion for scientific advances. And we need feedback approaches that will bring the utility of the information closer to home and to patients themselves; not just to society as a whole, but to patients themselves.
Moving forward, we will review the transcript to identify common themes and strategies. We urge you to send in any other thoughts that you have, and we will send out an appeal for input on ways in which we can both refine the strategies that are most important, and again, as Art said, develop some priorities around ways in which we can all work together to move forward.
I want to take this opportunity now to again thank Claudia and Julia for the great work that they did in putting this meeting together. I thank each of you, both presenters and participants in the effort, and again thank our Planning Committee who made this meeting possible: Terry Adirim, Leah Binder, Veronica Goff, Mark Gorman, Paul Grundy, Art Levin, Jim Mangia, Lyn Paget, Eric Racine, Susan Reinhard, Craig Robbins, John Santa, Susan Sheridan, Susan Trinidad, and last, but certainly not least, Christine Bechtel. Thank you all very much.
REFERENCES
Bernabeo, E., and E. S. Holmboe. 2013. Patients, providers and systems need to acquire a specific set of competencies to achieve truly patient-centered care. Health Affairs 32:250-258.
Braddock, C. H., K. A. Edwards, N. M. Hasenberg, T. L. Laidley, and W. Levinson. 1999. Informed decision making in outpatient practice: Time to get back to basics. JAMA 282(24):2313-2320.
Forrest, C. B, W. V. Crandall, L. C. Bailey, P. Zhang, M. M. Joffe, R. B. Colletti, J. Adler, H. I. Baron, J. Berman, F. del Rosario, A. B. Grossman, E. J. Hoffenberg, E. J. Israel, S. C. Kim, J. R. Lightdale, P. A. Margolis, K. Marsolo, D. I. Mehta, D. E. Milov, A. S. Patel, J. Tung, M. D. Kappelman. 2013. Comparative effectiveness of anti-TNFα therapy for pediatric Crohn’s Disease. Under review.
Henry, S. G., E. S. Holmboe, and R. M. Frankel. 2013. Evidence-based competencies for improving communication skills in graduate medical education: A review with suggestions for implementation. Medical Teacher 35(5):395-403.
Towle, A., and W. Godolphin. 1999. Framework for teaching and learning informed shared decision making. BMJ 319:766-769.
Wicks, P., M. Massagli, J. Frost, C. Brownstein, S. Okun, T. Vaughan, R. Bradley, and J. Heywood. 2010. Sharing health data for better outcomes on PatientsLikeMe. Journal of Medical Internet Research 2(2):e19.
Wicks, P., D. L. Keininger, M. P. Massagli, C. de la Loge, C. Brownstein, J. Isojärvi, and J. Heywood. 2012. Perceived benefits of sharing health data between people with epilepsy on an online platform. Epilepsy & Behavior 23(1):16-23.














































































































