Papers and Commentary from Speakers
II.1 INTRODUCING TRANSDISCIPLINARY PROFESSIONALISM
Cynthia D. Belar, Ph.D., A.B.P.P.
American Psychological Association
What is transdisciplinary professionalism? For the purposes of the Global Forum on Innovation in Health Professional Education workshop, it has been defined as “an approach to creating and carrying out a shared social contract that ensures multiple health disciplines, working in concert, are worthy of the trust of patients and the public.” In an effort to promote a shared understanding, this paper provides a broad-brush review of some of the terminology related to the concept of transdisciplinary professionalism.
There has been considerable emphasis in higher education on the relationships among disciplines and how to create new knowledge that addresses the challenges of society. Yet, as Brewer (1999) has noted, “The world has problems but universities have departments.” The counterpart to this saying is that “Patients and their communities have health problems, but health care has guilds.” There are different ways in which disciplines can work together to address problems, and some approaches are probably better than others, depending on the issue. The following definitions are based on the work by Rosenfield (1992):
- Unidisciplinary—Professionals from a single discipline work together to address a common problem.
- Multidisciplinary—Professionals from different disciplines work independently, each from a discipline-specific perspective, with the goal of eventually combining efforts to address a common problem (in practice, this is “parallel play,” and it describes most of outpatient health care delivery).
- Interdisciplinary—Professionals work jointly, each from a discipline-specific perspective. This is an interactive way to address a common problem (in practice, interdisciplinary work is common in rehabilitation and specialized teams and units such as organ transplant and burn units. It is increasingly common in primary care).
- Transdisciplinary—This approach synthesizes and extends discipline-specific theories/concepts/methods to create new models/language to address a common problem. It is an integrative process (in practice, it refers to the blurring of disciplinary boundaries and the overlapping of roles and functions).
When issues related to health education and practice are discussed, however, the word “profession” is often used, rather than “discipline.” This is done for at least two reasons: (1) not all health professions are actually academic disciplines, and (2) some health professions refer to their internal practice specialties themselves as disciplines. Simply stated, the words “profession” and “discipline” do not have consistent usage in the literature, and we will not resolve those issues here. But it was found that the term “interprofessional” seems to be used more often than “interdisciplinary” in describing the interactive team process in patient-centered collaborative care—so, “interprofessional” is the term used here to reflect that concept. This term may convey more depth of mutual involvement among the professions than the word “interdisciplinary,” but it also could exclude members of the health care team not labeled “professionals.” However, because the focus of the Global Forum is on health professional education, we believe it will suffice. The term “interprofessional practice” is the current terminology for “two or more professions working together as a team with a common purpose, commitment and mutual respect” (Freeth et al., 2005). Members rely on one another to deliver high-quality health care.
Another core concept in our discussions is that of professionalism. This concept is fundamental to all professions, although standards for professionalism are articulated within the silos of the professions. Definitions abound and include descriptions of attributes, behaviors, and values that professionals should exemplify, such as accountability, altruism, beneficence, compassion, competence, integrity, non-maleficence, respect, and sensitivity to diversity. Professionalism also serves as the basis for a
profession’s relationship to society, characterized as the social compact or social contract. A profession “professes” to the public that it will be altruistic, competent, self-regulating, and address societal concerns in return for its autonomy, prestige, and the public trust. As described by planning committee co-chair Matt Wynia from the American Medical Association, professionalism transcends a list of desired behaviors and codes of ethics; it is the reason for creating such lists and acting in accordance with them. Professionalism is also a belief system, an ideology.
Many health professions articulate professionalism as a core competency to be developed and ensured through education and training programs. Indeed, there is a considerable literature across professions addressing issues related to their social contracts with society and how they perceive their roles and responsibilities—which change over time. Figure II-1 provides one way to depict these relationships.
With the increased focus on collaborative care as a means to reduce error and improve quality, there has also developed a need to examine bridges across the health care professions. Rather than conceptualizing professionalism totally within the silos of the professions, efforts have been made to articulate elements of professionalism that are uniquely relevant to collaboration across the health professions. The term “interprofessional professionalism” refers to the “consistent demonstration of core values evidenced by professionals working together, aspiring to and wisely applying principles of, altruism and caring, excellence, ethics, respect, communication, accountability to achieve optimal health and wellness in individuals and communities” (Stern,
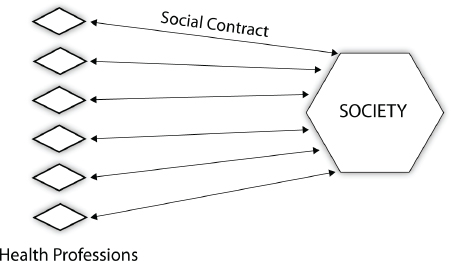
FIGURE II-1 Professionalism.
SOURCE: Belar, 2013.
2006). Interprofessional professionalism underscores cooperation and communication across professional boundaries (see Figure II-2).
Proponents of interprofessional professionalism warn that, given the increased complexity of health care, siloed approaches to professionalism may actually undermine safety and quality as well as patient/family/community centeredness, as was described by workshop speaker Jody Frost. Our question is, If a well-developed interprofessional professionalism is ever reached, will it lead to a transdisciplinary professionalism? Will there be movement toward a shared social contract that transcends all the professions but is connected to all the professions by a unifying set of beliefs and behaviors that they profess to the public? (See Figure II-3.)
Will the multiple health disciplines/professions work together to ensure that they are worthy of the trust of patients and the public? It is important to note that transdisciplinary professionalism is not the equivalent of transdisciplinary practice. It is not assumed that disciplinary boundaries are “transcended” at the level of knowledge, skills, or competencies in patient care. As noted before, transdisciplinary practice is a concept that describes a blurring of professional boundaries, where health professionals take on aspects of each other’s roles. Rather, transdisciplinary professionalism has to do with a transcendent ideology. What would that mean for the education of future health professionals?
The Global Forum’s workshop on transdisciplinary professionalism may have raised more questions than it answered, but we do not see that as
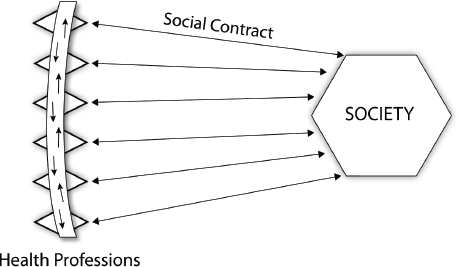
FIGURE II-2 Interprofessional professionalism.
SOURCE: Belar, 2013.




