What are the ethical goals of elder abuse prevention? What are the ethical challenges and issues in preventing and intervening in abuse and neglect? Workshop panelists discussed these issues in the context of providing care and services, and opportunities for prevention.
Workshop speaker Susan Lynch from the Department of Justice suggested that the goals of elder abuse prevention are to prevent unnecessary suffering, maintain autonomy, and maintain quality of life. Within this context, she laid out four principles to consider in elder abuse prevention:
1. Autonomy is the right to self-determination, independence, and freedom. Autonomy expresses the concept that professionals have a duty to treat the person according to the person’s desires, within the bounds of accepted treatment, and to protect the individual’s confidentiality.
2. Justice is the obligation to be fair to all people.
3. Beneficence requires that health care providers do good for individuals under their care by understanding the individual from a holistic perspective that includes the individual’s beliefs, feelings, and wishes as well as those of the individual’s family and significant others.
4. Nonmaleficence is the requirement that health care providers do no harm to their patients and that they protect their patients from harm.
In making decisions on which ethical issues to focus its resources, Lynch noted that the Department of Justice, with funding support from the Department of Health and Human Services, developed a concept map of the field of elder abuse. They started the process by inviting 750 professionals from the field to respond to this statement: “To understand, prevent, identify, or respond to elder abuse, to collect or exhortation we need.” The feedback from this process was used to generate ideas that were categorized and rated for feasibility and importance. Through this process, the key ethical issues that were identified were brain health and function, elder abuse reporting, provisions under the Health Insurance Portability and Accountability Act of 1996 (HIPAA), and long-term care quality and abuse prevention.
BRAIN HEALTH AND FUNCTION:
DECISION-MAKING CAPACITY AND COMPETENCY
Within the area of brain health and function, the primary concern is an individual’s decision-making capacity and competency. Lynch defined decision-making capacity as the ability to understand the nature and consequences of different options, to make choices among those options, and to communicate that choice. Decision-making capacity is required in order to give informed consent. Such capacity may fluctuate over time, given the state of health of the individual as well as the particular issue.
Another issue related to brain function and health is the notion of competency. Competency is defined legally and determines if an individual is fit and qualified to give testimony or executive a legal document. In the United States, the law presumes all adults are competent and have decision-making capacities to make health decisions unless deemed otherwise in court. Lynch discussed ethical issues within the legal system about the capacity of a vulnerable adult to testify in an elder abuse case. She noted that a lack of competency could be used as a defense litigation strategy to preclude testimony from victims or witnesses of abuse.
Lynch also discussed ethical issues around informed consent in research studies and the decisional capacity of older adults. She noted that, after being given information, a person gives informed consent when he or she can make a choice, understand and appreciate the issues, rationally manipulate information, and make a stable and coherent decision. Several considerations for what may impede an older adult’s ability to give informed consent are sensory deficits, impaired ability to ask questions, and values and beliefs about making health care choices.
Assessing Capacity
Workshop speaker Jason Karlawish from the University of Pennsylvania expanded on the issue of assessing decisional capacity. Both the theory and practice of capacity assessment have made substantial progress in developing a coherent set of concepts and practices that are legally and ethically acceptable. Karlawish has studied the history of the concepts of decisional capacity and competency since the 1960s, and much of the debate about capacity and competency has centered on different meanings being applied to the same words or the same word being used with different meanings. However, he believes the field has arrived at a reasonable place with legally and ethically acceptable concepts. Decisional capacity is the continuum of decision-making abilities: choice, understanding, appreciation, and reasoning. Assessments of adequate capacity for decision making are used to make judgments of competency.
Karlawish discussed in detail financial capacity, which is defined as “the ability to manage money and financial assets in ways that meet a person’s needs and which are consistent with his or her values and self-interest” (Marson et al., 2011). Karlawish suggested that financial capacity is a multidimensional construct that consists of four elements: (1) having basic monetary skills, (2) carrying out cash transactions, (3) managing a checkbook and bank statement, and (4) exercising financial judgment. Karlawish noted that this specific kind of capacity can be thought of not as a “decisional capacity,” but as an activity of daily living akin to cooking, shopping, or cleaning. He suggested there should be an instrument for assessing financial capacity that is standard practice for Adult Protective Services (APS) workers.
Assessment for the Capacity for Everyday Decision Making
Karlawish and his colleagues have developed an instrument called the assessment for the capacity for everyday decision making (ACED), which helps providers answer the question “are patients who refuse interventions to help them manage their IADL [instrumental activity of daily living] disabilities capable of making this decision?” (Lai and Karlawish, 2007). Through validation of the tool, they found that a substantial number of older adults with cognitive impairments caused by Alzheimer’s or its variants, from very mild to moderate severity, could all express a choice; that is, all of them could tell you what they would want or not want. Most of them could reason through that choice; that is, they could give you consequences. However, they exhibited problems with understanding the information, such as what their checkbook is for or how cooking works. He noted that in many capacity cases there are two distinct questions: Can someone
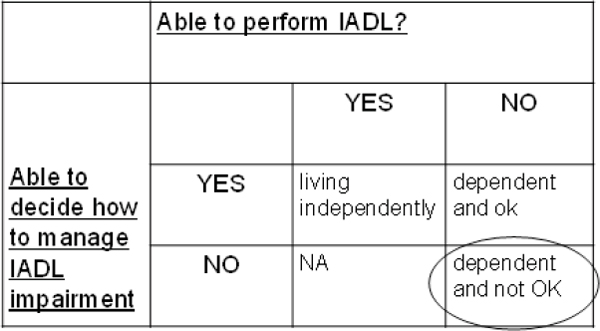
FIGURE 4-1 Ethical considerations in research and care.
NOTE: IADL = instrumental activity of daily living.
SOURCE: Karlawish, 2013.
independently perform an IADL? and When presented solutions to manage a problem performing an IADL, can the person use those solutions to solve the problem? These are two separate decisions, and an individual could be capable of doing one, but not the other. Karlawish presented a two-by-two matrix that pairs assessing the ability to perform IADL with the ability to decide how to manage IADL impairment (see Figure 4-1).
These abilities are both issues of capacity—one ability is about doing a task and the other is about making a decision on how best to manage a problem with that task. Karlawish suggested that the field is at a point of being able to train individuals in performing this assessment so ethical decisions can be made about an individual’s ability to perform an IADL and, if they are impaired, their ability to make a decision about how to manage that impairment. Education on and dissemination of tools for assessment are needed for those in the field, such as APS workers, who are expected to assess these capacities on a regular basis.
ELDER ABUSE REPORTING
Lynch discussed ethical considerations as well as barriers for elder abuse reporting, which has led to underreporting. Focusing on provider issues, she noted that, most states have mandatory reporting requirements for both abuse and neglect that apply to medical professionals, health care providers, mental health counselors, service providers, and government agents who come in contact with the elderly. However, to overcome some of the barriers to reporting, Lynch suggested that providers will need at least:
(1) a common definition of what abuse is and the different types of abuse, (2) awareness of reporting laws, and (3) knowledge and understanding of the next steps after reporting.
HIPAA
Lynch noted that HIPAA, which was created to protect medical information, has been perceived as a barrier to information sharing on elder abuse issues between emergency medical services and prosecutors; between hospitals and prosecutors; and among emergency medical services, hospitals, and APS. However, there are several exceptions to HIPAA that allow covered entities to provide protected health information to law enforcement and social service agencies. Lynch said a better public education effort is needed to explain these exceptions. Lynch identified several of these exceptions:
• Required by law/mandatory reporting laws: A covered entity may disclose protected health information to law enforcement officials if it is required to do so by law. An example would be a state law mandating the reporting of certain wounds or other physical injuries.
• Victims of a crime: Health care entities may also provide law enforcement officials with an individual’s protected health information if the individual is a suspected victim of a crime. In such cases, covered entities can only disclose information if (1) the individual agrees to disclosure, or (2) the covered entity cannot obtain the individual’s agreement because of incapacity or an emergency.
• Victims of abuse, neglect, or domestic violence: A covered entity that believes an individual has been the victim of abuse may disclose the individual’s protected health information to a government agency that is authorized by law to receive reports of abuse, neglect, or domestic violence.
LONG-TERM CARE
Lynch outlined several legal remedies for issues of elder abuse in long-term care facilities. Cases can be brought through the False Claims Act (FCA), under which individuals who knowingly file false claims for Medicare or Medicaid payments can be liable for damages and penalties. Through FCA, providers who render substandard or no care that may harm the patient and bill Medicare or Medicaid can be pursued. Cases have been brought against nursing facilities, assisted living facilities, psychiatric and acute care hospitals, and group homes.
MOVING FORWARD
The panelists offered suggestions for priority issues in the area of ethical considerations to move the field forward. Lynch suggested there is a need for more evidence and, when appropriate, more prosecution of elder abuse cases. Noting the availability of assessment tools, Karlawish suggested that education on and dissemination of tools for assessment are needed for professionals in the field, such as APS workers, who are expected to assess decisional capacity on a regular basis. Speaker Sidney Stahl suggested there is an ethical imperative for more research and research funding, specifically in the areas of APS interventions and primary and secondary prevention.
REFERENCES
Karlawish, J. 2013. Elder abuse and neglect: Ethical consideration in research and care. Presented at Elder Abuse and Its Prevention: A Workshop. Institute of Medicine, Washington, DC, April 17.
Lai, J. M., and J. Karlawish. 2007. Assessing the capacity to make everyday decisions: A guide for clinicians and an agenda for future research. American Journal of Geriatric Psychiatry 15(2):101-111.
Marson, D. C., K. Hebert, and A. C. Solomon. 2011. Assessing civil competencies in older adults with dementia: Consent capacity, financial capacity, and testamentary capacity. In Forensic neuropsychology: A scientific approach, edited by G. J. Larrabee (2nd ed.). New York: Oxford University Press. Pp. 401-437.






