Efforts to integrate health care services and efforts to improve health at the population level (e.g., beginning with the work of public health agencies) are already under way at the state and local levels. To showcase several approaches that have potential for scaling and replication through implementation of the Affordable Care Act (ACA), four panelists described their experiences with ongoing programs and addressed the challenges associated with these promising models. Janine Janosky, Vice President of Austen BioInnovation Institute in Akron (ABIA) and head of the Center for Community Health Improvement in Akron (Ohio) presented a nonprofit perspective. Joshua Sharfstein, Secretary of the Maryland Department of Health and Mental Hygiene and Chair of the Maryland Health Benefit Exchange, and Lillian Shirley, Director of the Multnomah County (Oregon) Health Department, spoke about a state and a local effort, respectively. Stella Whitney-West, Chief Executive Officer of NorthPoint Health and Wellness Center in Minnesota, provided an example of a community health center’s program. An open discussion moderated by Sanne Magnan, President and Chief Executive Officer of the Institute for Clinical Systems Improvement and member of the Roundtable on Population Health Improvement, followed the panel presentations.
A NONPROFIT MODEL OF INTEGRATION
ABIA is a 501(c)(3) nonprofit established to coordinate activities among three independent health care systems and two universities in northeastern Ohio, explained Janine Janosky. By taking advantage of ACA provisions, ABIA has created an accountable care community (ACC), an extension of the accountable care organization (ACO) concept, but one that does not depend on providers’ adoption of a Medicare infrastructure. The Akron ACC, whose vision is to improve the health of the community through a collaborative, integrated, multi-institutional approach that emphasizes shared responsibility for the health of the community, includes the 5 core institutions and partners with public health and more than 65 additional social services and education entities, including the local faith community and Cuyahoga Valley National Park (ABIA, 2012). Doing good for the community, she explained, can mean taking risks and considering the community’s needs in tandem with those of the individual organization. “Some of these institutions and organizations are leveraging their resources for the good of the accountable care community, and some made decisions to sundown or to expand programs because that is what the community would benefit from,” said Janosky.
In addition to going beyond the Medicare-based structure, Janosky discussed how the ABIA-led ACC includes a large grassroots component that aims to give equal voice to all the constituents in the community, not just those who have a particular health insurance policy or belong to a specific health system. Key components of the ACC include integrated, collaborative medical and public health models; interprofessional medical teams; a robust health information technology infrastructure that standardizes data across the multiple electronic health records (EHRs); a community health surveillance and data warehouse; and a dissemination infrastructure to share best practices. This data-driven system also includes a data analysis team to measure the impact of the ACC on community-wide health and a group dedicated to policy analysis and advocacy.
Outlining the steps that ABIA took to create the ACC, Janosky explained that the system is based on the Healthy People 2020 framework of health promotion, disease prevention, improved access to care and services, and health care delivery. “All of the members of the ACC fall within one or more of these realms,” she said. The first step to build this system involved conducting a community-wide inventory of assets and resources and mapping it to the Centers for Disease Control and Prevention’s (CDC’s) Health Impact Pyramid (see Figure 3-1) (Frieden, 2010). ABIA then took each of the metrics of Healthy People 2020 and conducted
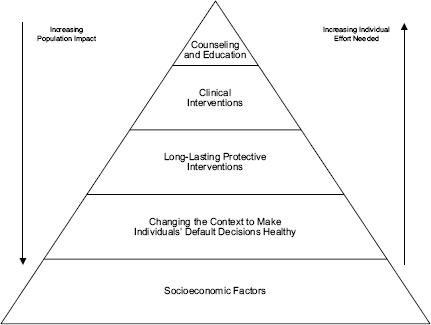
FIGURE 3-1 The health impact pyramid.
SOURCE: Frieden, 2010.
a broad-based examination of what resources were available that could address health priorities at the bottom of the community-wide health impact pyramid. Where the analysis identified gaps, the partners developed programs to address those gaps and shifted resources when needed. The partnership also established a set of benchmark metrics that include short-term process measures, intermediate outcome measures, and longitudinal measures of impact. It will use those measures to demonstrate the economic case for health care payment policies that lower the preventable burden of disease, reward improved health, and deliver cost-effective care across the broad community. In addition, said Janosky, the accountable care community involves cost avoidance and cost recovery models that will help reinvest savings in the coalition’s work.
As an example of a desired outcome, Janosky described the ACC’s diabetes program, which aims to reduce the incidence of disease from its current level of approximately 8 percent of the population of Akron. This initiative is broad-based in that it includes patients with diabetes at three independent health systems and with varying insurance status—including nearly a third of the population that has no insurance—and it touches every aspect of the health impact pyramid. The program relies on a multidisciplinary team with multifocal modules of medical care, nutrition, physical activity, social and emotional well-being, and self man-
agement. The cost of the program, over the 2 years it has been operating, has been about one-third less per person per contact hour than the comparable National Diabetes Prevention Project, and it has produced better clinical and behavior outcomes. More than half of the participants have lost weight, realized a substantial reduction in body mass index, and reduced their waist circumference. Emergency department visits have declined and there have been no amputations related to diabetes during the 2 years. Overall, the average cost per month of care of individuals with diabetes fell by 10 percent, and after 1 year of involvement there was a consistent reduction in costs. Using national figures for cost savings associated with improved blood sugar control and weight loss, Janosky estimated that this program saved more than $3,700 per person per year.
Janosky reviewed the metrics for success that the ACC uses and the two impact equations that serve as a proxy measure for the overall benefit and costs of the ACC effort. The first equation, which focuses on overall costs and benefits of the community-wide approach and which is useful for considering the impact of specific projects, examines three elements: quality improvement, the scope of the population served, and the costs of a disease in the community. The second equation measures burden in terms of delay of disease progression, the cost of treatment, and the loss of productivity, and it frames the impact of the ACC from a population perspective. “These two equations let us look more broadly as to what are the outcomes and successes, then we also have those metrics that looked specifically as to what might be happening for an individual patient, individual practice plan, individual hotspot within the community,” Janosky explained.
In terms of sustainability, Janosky noted that systemic changes have made collaboration the standard across the partners in the ACC and those changes are shifting the operating model to one of collective impact. The ACC is moving in the direction of routinely using sophisticated knowledge management tools to inform its work and also to inform local and state government about other approaches, such as zoning and planning policies that could help improve the health of the community by shifting the focus from disease treatment to health promotion and disease prevention. Finally, the ACC also hopes to support payment reform with the data it is generating.
ALL-PAYER HOSPITAL PAYMENT REFORM
Maryland is the only state in the country that sets hospital rates that apply to all payers, said Joshua Sharfstein. The system has consistent rules, results in no cost shifting, covers uncompensated care, and provides a platform for innovation in the area of payment reform. One
such innovation is Maryland’s Total Patient Revenue program, which establishes a global budget for a hospital independent of patient volume. This population-based rate method is offered to 10 rural hospitals and is consistent with these hospitals’ mission to serve the health needs of a community. The global budget covers all inpatient and outpatient facility revenues and creates a strong incentive to control unnecessary admissions and readmissions and to shift care to less costly settings. This program, which is now in its third year and received an extension for another 3 years, covers about $1.5 billion in funds and accounts for about 10 percent of net hospital revenue in the state.
Sharfstein described how in their efforts to better control costs, hospitals participating in the Total Patient Revenue program have established case management teams in the emergency department and have worked to address barriers that limit patient access to primary care. There has been an intense focus on reducing readmissions, transitioning patients to nursing home care, and managing chronic conditions. One lesson that has emerged is that many of the readmitted patients have behavioral health problems. There is now an effort in progress to find the behavioral health care these individuals may need. In one case, the local hospital has taken over the school health program because it learned that it was seeing too many children with uncontrolled asthma coming into its emergency department.
Maryland has also organized local health improvement coalitions, involving public health agencies and other partners across the state, and the local hospitals have helped to support these. Sharfstein noted there is robust participation in the areas where the Total Patient Revenue program is operating. Hospitals are recognizing that partnerships with public health agencies can help them succeed in the face of new financial incentives, e.g., to keep people out of the hospital by helping them improve their health. “My message to the hospitals is that they can get a huge amount of value by partnering with public health,” he said, and also noted that these partnerships can benefit public health when funding is tight.
Early data have shown that Total Patient Revenue hospitals are seeing declines in admissions, readmissions, and avoidable admissions compared to hospitals that are not participating in the program. However, there are a number of challenges confronting the program, some of which have the potential to be addressed through implementation of the ACA. One challenge is that hospital and physician incentives are misaligned. Sharfstein said the potential for synergy is tremendous if the state can establish medical homes that work closely with community coalitions. The adoption of health information exchanges, for which ACA provides incentives, offers the opportunity to develop maps that can help hospi-
tals and coalitions focus on areas of greatest need. Expanded coverage offers the potential for more stable finances for hospitals, and the ACA gives the state the opportunity to modernize the Medicare waiver that serves as the basis for Maryland’s all-payer system. Although the state is discussing such changes with the Centers for Medicare & Medicaid Services (CMS), health officials would also like to develop opportunities for sharing cost savings with physicians, expanding collaboration with public health coalitions, and expanding population-based budgeting to suburban and urban areas.
“We want to use this tool of an all-payer system to fundamentally realign and coordinate with other public health initiatives,” Sharfstein said in closing. “What we are trying to do is create a system where the incentives flow naturally to those types of interventions that can produce better outcomes.” The goal, he added, is to have such a system operating throughout the state to realize savings and improved health care across the entire health care system. “If we can get health care payment aligned to better patient experience and better outcomes, we will see a better coordinated experience for patients, and ultimately we will have improved health outcomes. When we do that, we get more financial incentives back into the health care system and we get a virtuous cycle.”
STATE-WIDE HEALTH SYSTEM TRANSFORMATION
Although the state was once advised to start small, Lillian Shirley said, Oregon is tackling a statewide effort to change the way health care is delivered and paid for by using its 15 coordinated care organizations (CCOs) to meet the goals of the Triple Aim1: improving population health and health outcomes while lowering costs. Toward that end, she explained, Oregon has made a commitment to CMS to reduce the annual increase in the cost of care by two percentage points, ensure that quality of care and population health improve, establish a quality incentive pool that increases every year as a percentage of the global budget, and report to the public about how these CCOs are performing according to CMS’s core metrics.
As an incentive to the CCOs to participate in this effort, there will be quality pool funds of up to 2 percent of their global budget available based on comparative performance on 17 measures. In addition, Oregon as a whole will be assessed annually on the CCO measures plus an additional 16 metrics and will face financial penalties if it does not meet
______________
1 The Institute for Healthcare Improvement introduced the concept of the Triple Aim in 2006, and it has since been adopted by many health care organizations and also adapted for use in the activities of the CMS as the Three-Part Aim.
quality goals. To meet its goals, the state has enumerated seven quality improvement focus areas:
1. Improving behavioral and physical health coordination
2. Improving prenatal and maternity care
3. Reducing preventable re-hospitalizations
4. Ensuring appropriate care is delivered in appropriate settings
5. Reducing preventable and unnecessarily costly usage by super-users
6. Addressing discrete health issues (e.g., asthma, diabetes, high blood pressure)
7. Improving primary care for all populations
Shirley explained that the state has identified six attributes of CCO and ACO systems of care that lead to better management of care and is identifying metrics for each of these areas, including public health measures and activities based on such things as best practices and the Task Force on Community Preventive Services. The state public health agency, she pointed out, is not only at the “table,” but acts as a steward of metrics. Moreover, the broad use and adoption of an EHR across the state contribute to data collection and analysis needed to determine not merely if the health of individuals in a certain health system is improving, but whether or not a community’s health is improving.
Shirley discussed the strategy to combat diabetes in Portland and surrounding Multnomah County, Oregon. This multifaceted approach includes primary, secondary, and tertiary prevention. Primary and secondary prevention include individual-level education and community-level school-based healthful eating and healthy retail initiatives, as well as policy-level efforts to enable health impact assessments to identify place-based strategies for prevention. At the tertiary level, efforts focus on chronic disease self-management education, diabetes care, and case management. She also noted that public health agencies can work with local CCOs and communities to identify the 10 leading causes of mortality and morbidity in each local community. One example in Multnomah County is end-stage liver disease. It is number nine on the list, and major causes are hepatitis and alcoholism. Incentives are being considered that might improve education and treatment efforts. In each of these efforts, local advisory groups are looking at a wide range of factors, such as public safety and education, that are normally not part of the health care spending discussion, but that negatively impact health. The work that public health agencies do in partnership with other sectors in prevention efforts can help decrease the medical costs associated with these outcomes.
THE COMMUNITY HEALTH CENTER PERSPECTIVE
Health happens in healthy communities, said Stella Whitney-West in her opening remarks, and NorthPoint Health and Wellness Center is focused on working in North Minneapolis. In that community, 91 percent of residents have incomes below 275 percent of the federal poverty line2 and among the highest rates of health disparities, the highest unemployment rate, and the highest housing foreclosure rate in the state. NorthPoint, she explained, was established in 1968 as a community health center and operates as a federally qualified health center in partnership with Hennepin County. It offers integrated health and social services that include medical, dental, and behavioral health services as well as food and housing services, chemical dependency treatment, and even a public art gallery. As a community health center, 51 percent of its board members are patients.
Recently, NorthPoint developed a strategic plan focusing on primary care, community health, social determinants of health, and health equality to ensure that it has an impact on health outcomes. “We want to make sure that the first entry into the health care system is through primary care, as opposed to the hospital or emergency department,” explained Whitney-West. She noted that NorthPoint is also providing training opportunities for health care jobs and scholarships for those students from the community who want to pursue a career in health care. A central component of its action plan was to become the state’s first patient-centered health care home, which enables it to receive state reimbursement for its community health workers and care coordination for patients enrolled in the health care home. As examples of community-centered health projects, she cited programs aimed at successfully convincing the entire county to be smoke-free, which included working with landlords and churches not to allow smoking in apartments and on church property, and programs to increase the availability of fresh produce in North Minneapolis and educate the community about the value of urban gardening.
NorthPoint is about to enter a new partnership aimed at reducing the rate of chlamydia infection, a sexually transmitted infection, in the community. Currently, the NorthPoint clinic has one of the highest screening rates in the state, but with little effect on reducing what is the highest rate of chlamydia infection in the state. NorthPoint will use its participatory model of partnering with community residents to identify solutions and interventions to reduce the chlamydia infection rate.
It will also hold its second Fit 4 Fun community health event. The first
______________
2 The Department of Health and Human Services Office of the Assistant Secretary for Planning and Evaluation provides a listing of current poverty guidelines at http://aspe.hhs.gov/poverty/13poverty.cfm (accessed September 27, 2013).
event was held in 2012 at the suggestion of NorthPoint’s health care providers, who pointed out the lack of a place in North Minneapolis to exercise safely. This event features bicycle rides and repairs, a 5K walk/run, and a bicycle raffle for youth who complete the fitness activities. The first event far exceeded expectations with more than 700 people participating.
In the area of health equity, NorthPoint is trying an approach that aims to use culture and ethnicity as a means to promote healthy behaviors. As part of this effort, staff participate in training to become more culturally appropriate and to learn how to tap into cultural practices as a means of encouraging patients to change harmful behaviors and seek routine health care and screening.
One of NorthPoint’s most promising ventures, said Whitney-West, is as a partner member of Hennepin Health, an integrated health care network functioning as an ACA demonstration accountable care organization. Since January 2012, this partnership has been targeting the Medicaid expansion population of adults ages 21 to 64 without dependent children. The demonstration aims to reach some 10,000 members per month. She noted that this target population, which represents about 5 percent of the county’s population, accounts for an estimated 64 percent of the health care spending, largely because care is usually crisis-driven in this group of county residents. The partners placed particular emphasis on addressing social disparities and increasing preventive care, an approach that has reduced inpatient admissions by 14 percent and emergency department visits by 13 percent and cut health care expenditures by 5 percent, far exceeding the goal of achieving a 2 percent cost savings. Equally important was the finding that 87 percent of the patients treated said they were likely to recommend Hennepin Health to friends and family, a substantial increase in patient satisfaction compared to the care received from other health service providers.
Hennepin Health is also making investments in areas that Whitney-West said are expected to yield cost reductions ranging from 30 to 80 percent. These include creating a Sobering Center to reduce emergency department visits, repositioning a community center to serve as transitional housing, developing a behavioral health continuum based on a psychiatric consult model, providing vocational services, and expanding a clinic that provides intensive primary care. She added that NorthPoint is involved in several community grants and will be part of Minnesota’s Health Exchange. She and her colleagues are working to increase collaboration between providers and payers, but she said that barriers to data-sharing data between social services and health care providers need to be addressed.
In response to a question from session moderator Sanne Magnan about the difficulty of closing programs that are no longer useful, Janosky said that doing so is only possible when all the partners agree from the start that the community’s long-term needs will outweigh any short-term challenges that arise from decisions to, for example, end or merge duplicative programs. Every partner has to buy into the vision that aligning or ending programs is sometimes necessary to yield better results. As an example of how this attitude translates into action, she explained how every funding request for health initiatives that comes into the local United Way office must align with the programs and goals of the ACO.
James Knickman, President and Chief Executive Officer of the New York State Health Foundation and a member of the Roundtable on Population Health Improvement, asked the panelists to comment on any common themes heard during the sessions presentations. Whitney-West was of the opinion that the four presentations reaffirmed that “we are all rowing in the right direction.” She added that she saw some good opportunities to learn from one another, noting that there was nothing that she heard that she could not replicate in her community. Shirley said that she was encouraged by the efforts being made to identify successful programs and scale them across communities while keeping the emphasis at the community level, which is where people need to be engaged. Magnan noted that all of these programs have a focus on meeting the goals of the Triple Aim, and that this focus means that cost becomes part of the outcomes measured. She saw this as an important change in attitude in public health.
During the discussion, Flores remarked on the energy that many different groups are bringing to the conversation on how to expand the role of population health. Community residents are getting involved and so are younger adults, who he said have not gotten engaged in health issues before. Foundations and others are now talking about the need to increase the number of professionals and other workers who can go into communities and help them become more resilient.
In response to a question about how the Office of the National Coordinator for Health Information Technology (ONC) could help public health agencies’ efforts as ONC develops the third phase of the meaningful use requirements for health information technology, Shirley said it would be highly informative to funding decisions if EHRs could be mined for race and ethnicity data, but she acknowledged the cost and challenges implicit in adding lines of code to EHR. Flores said that ONC could help facilitate the deployment of telemedicine for population health purposes in a way that uses the nation’s communications infrastructure so that data from remote parts of the country could be analyzed using analytic systems that
primarily are available in more heavily populated areas. Whitney-West agreed with this idea and noted that Minnesota has a communications system that links smaller communities with major hospitals. She added, however, that creating such a system and enabling the EHRs to transmit data to remote locations is expensive, and even when such a system is in place, finding trained analysts who can mine the data to generate the expected insights is difficult. Also, an unclear issue is how to manage all of the data generated in an EHR, how to get that data into the hands of practitioners, and how to use that data to get patients more involved in their own health care. “There is still a lot of groundwork that needs to be covered,” she said.
A webcast participant asked the panelists how they set community-wide goals for their initiatives. Shirley said that by law, all of Oregon’s CCOs must include members of the community on their boards and the community members have been actively involved in setting the goals for each CCO. Janosky said that ABIA identified what she called the “soft leaders” in the community, those individuals who hold no official position but are well connected with the community. This group serves as ABIA’s final check before it rolls out any new program and its members play a central role in engaging the broader community.
In her community, Whitney-West convenes listening groups that include patients of different ethnicities who speak different languages. Although putting these groups together is expensive and time consuming, they provide important real-time feedback that is proving to be more valuable than the information generated by the usual focus groups that attract the most engaged individuals. Her program uses the input from these listening groups to develop and refine its blueprint for action. She added that “when the majority of your board members are from the community and are patients of the health center, it keeps us focused on the needs of the community.”
Another webcast participant asked the panelists if they had any ideas on how to organize drug treatment and long-term care as part of the ACA expansion. Shirley said that in Oregon, behavioral health and addiction are included in the global health care budget, so it is up to each community to decide how its CCO spends its funds given the community’s needs. This is where data from EHRs would be useful, she noted. She added that there are number of early public health interventions that have been proven effective in pilot studies, particularly among adolescents, and the CCOs in Oregon are working to incorporate those as part of the continuum of care they provide. Janosky and Whitney-West both said their programs are taking the same approach of integrating behavioral health into larger health programs. At NorthPoint, a psychologist is now “embedded” in the primary care clinic.
Judith Monroe, Director of the Office for State, Tribal, Local and Territorial Support at the CDC and a member of the roundtable, asked the panelists if they thought there was an opportunity for public health departments to become more involved with healthcare organizations. Each of the panelists said that their organizations all have partnerships with local public health departments, but Flores noted that in his experience public health officials do not understand the depth of commitment that is needed to address population health at the community level. “They are used to a command and control approach to infectious diseases,” he said. He added that public health departments would be the entity that would be truly able to sustain population health efforts under the ACA, but they lack leadership and resources in too many places. Often, he said, public health departments are restricted in terms of how involved they can get beyond the core focus. Another roundtable member, Marthe Gold, who is a visiting scholar at the New York Academy of Medicine, asked about the opportunity under the ACA to ensure a robust public health infrastructure. The panelists noted the importance of public health accreditation, regionalization, forming partnerships with organizations outside of the health community, and strong leadership.












