This is an auspicious time in our history to be discussing the nexus between health care and population health in the context of health care reform, said George Flores, planning committee co-chair and program manager for The California Endowment. To drive home that point he quoted President Barack Obama, who said, “Simply put, in the absence of a radical shift towards prevention and public health, we will not be successful in containing medical costs or improving the health of the American people.” Although there is no precise definition of population health, Flores continued, it can be viewed as an approach that treats the population as a whole (including the environmental and community contexts) as the patient. Citing For the Public’s Health: The Role of Measurement in Action and Accountability, he framed the nexus between health care and population health as the application of health strategies, interventions, and policies at the population level in a way that can advance current approaches to the nation’s most pressing health concerns more efficiently than is possible with isolated, intensive, individual-level actions within the clinical care sector (IOM, 2011).
After reviewing previous and ongoing IOM activities pertinent to the workshop topic,1 Flores noted that the Affordable Care Act (ACA)
______________
1 IOM activities include the reports Toward Quality Measures for Population Health and the Leading Health Indicators (2013); Primary Care and Public Health: Exploring Integration to Improve Population Health (2012); Living Well with Chronic Illness: A Call for Public Health Action (2012); An Integrated Framework for Assessing the Value of Community-Based Prevention (2012); Best Care
provides unprecedented resources to prevent illness and keep people healthy and includes, for the first time, a National Prevention Strategy. Although the ACA will take years to produce results, its potential is great. It could be generations until resources for population health such as those reflected in the legislation re-appear. Along the way, the ACA presents the opportunity to realize what Flores called the “health dividend” by transferring funds now spent on medical care to social and infrastructure investments that can both stabilize the nation’s fiscal health and improve the well-being of its citizens. Today, 97 percent of national health expenditures go to health care services, with only 3 percent going to prevention even though the biggest determinants of health are not medical care or even genetics, but rather, behaviors and environmental factors (Bipartisan Policy Center, 2012). “Health largely depends on conditions where we live, learn, work, and play, not just on the medical treatment we receive,” said Flores. “Health is not just in pills and surgeries and hospitals. We need to think more broadly than that.”
A more productive approach to thinking about health comes from considering it in the context of the social ecology model that the state of California uses. This model consists of four domains—the social milieu, the community, the family, and the individual (see Figure 2-1)—and it reflects the importance of socioeconomic factors, public health interventions, and health awareness education as key determinants of individual health. Flores said the ACA is creating opportunities to deal with each of these domains and providing incentives for developing innovations that will shift health care from today’s high-volume and high-cost health care system focused on personal service to a future system that stresses healthy lifestyles and healthy environments. In his view, achieving this transformation is essential if the nation is to reduce morbidity and enable people to live longer, healthier lives through a sustainable investment in individual medical care.
Flores stated that the critical path for reform of the health care delivery system will first move from the current acute care system that focuses on episodic, non-integrated care to one that is coordinated, seamless, and provides care in a manner that is that is accountable for outcomes. A next step would create a community-integrated, learning health care system that uses population health strategies capable of rapidly deploying best
________________________________________________________
at Lower Cost: The Path to Continuously Learning Health Care in America (2012); For the Public’s Health: The Role of Measurement in Action and Accountability (2011); A Population-Based Policy and Systems Change Approach to Prevent and Control Hypertension (2010); an IOM workshop summary, Interprofessional Education for Collaboration: Learning How to Improve Health from Interprofessional Models Across the Continuum of Education to Practice: Workshop Summary (2013); and the IOM Roundtable on Health Literacy and the IOM Roundtable on the Promotion of Health Equity and the Elimination of Health Disparities.
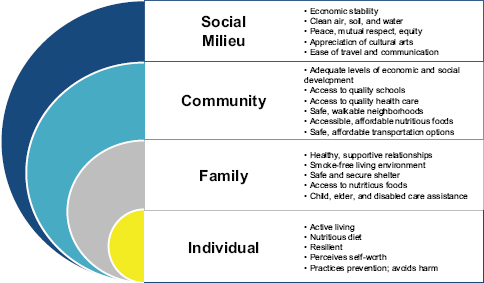
FIGURE 2-1 The California Department of Public Health’s social ecology model of health.
SOURCE: Office of Health Equity, California Department of Public Health, 2013.
practices for both prevention and treatment. Such a system will comprise integrated networks linked to community resources capable of addressing psychosocial and economic needs of the community, with the goal of reducing the health disparities that characterize the current system and thereby improving the health of the entire population. Beyond the main purpose of the ACA, the law’s implementation affords the opportunity to move down the path of integrating population health into the health care system, elevate the priority for primary prevention and health equity, bridge clinical care and community health in “health homes,” empower consumers and communities to improve health outcomes, and provide incentives to improve workplace wellness.
There are a number of challenges to shifting the focus of the health care delivery system toward a population health perspective, Flores explained. Clinical care is better understood (and subsequently more valued) by the public than are the broader notions of health and community health. Partly as a result, the aims of public health agencies (that focus on the health of communities) and health care organizations (that typically focus on individual patients) are not aligned, nor are the resources and political visibility associated with them comparable. Governmental public health practice already lacks the capacity and resources to sufficiently provide for the public’s health and ACA implementation could
shift some traditional public and population health services into the care delivery system.
California is implementing the ACA by creating health exchanges and policies and committing to develop and enforce language and cultural competency standards. The state is conducting a massive outreach campaign, said Flores, to enroll people by 2014 and is pushing for coverage for the remaining uninsured. The state is also developing consensus indicators for population health, creating community centers of care that will act as health homes that reach into the community, and training community connectors and promotores to act as educators, facilitators, and advocates, as well as expanding the health workforce in underserved areas. All of these changes are not happening easily, he said, and budget conflicts are creating challenges in balancing short-term fiscal concerns with long-term benefits. Flores noted that discussions about ACA implementation are commonly dominated by clinical care interests, with too little focus on prevention, population health, and social aims.
Investing the savings that ACA implementation will generate in prevention will be an uphill battle as well, he predicted. He stressed the importance of learning how to build bridges and create partnerships; ascertaining the level of understanding among policy makers and the public; and making business cases for prevention, public health, and population health. “Community empowerment and giving communities the capacity to work on behalf of population health should be among the highest priorities,” said Flores, who noted that community empowerment is a priority of the many Community Transformation Grant program recipients in California. The goals of this program are to maximize health impact through prevention, advance health equity and reduce health disparities, and expand the evidence base so that local policy, environmental, and infrastructure changes have a positive impact on health.
In closing his presentation, Flores quoted remarks made by Lawrence Brilliant, President of the Skoll Global Threats Fund, at the 2013 Commencement for the Harvard School of Public Health: “Somehow, these two sides of our national health debate—one outward looking at social justice and inclusion and one looking inward at high quality patient care that is exclusionary, met then [1960s “Great Society”] and must meet now on sacred ground, sharing the profound obligation—and great joy—of improving the health of the people.”




